Young people’s low back pain and awareness of postural habits: A cross-sectional study
Abstract
BACKGROUND:
Young people tend to spend most of their time in activities involving inappropriate positions, which can promote musculoskeletal alterations and disorders.
OBJECTIVE:
To investigate the prevalence of low back pain (LBP) in young people and analyse its associations with daily postural habits.
METHODS:
Cross-sectional and retrospective study evaluating 679 Brazilian young people (15 to 18 years old), using questionnaires about LBP and awareness of postural habits. The prevalence values were calculated for the present moment, the last three months and throughout life. The Mann-Whitney U test and the Chi-square test were applied.
RESULTS:
The prevalence of LBP at the present moment was 27.2%, 57.7% over the last three months and 73.9% throughout life. Boys and girls presented significantly different values, a larger number of girls manifesting pain for the three moments. The associated postural habits were: turning the body, reduction of lumbar lordosis when seated, not placing the feet on the floor, crossing the legs when sitting in the classroom and at home, sitting or lying in an inappropriate position, and distributing the body asymmetrically on the legs when standing.
CONCLUSIONS:
Young people from 15 to 18 years of age show a high prevalence of low back pain. Inadequate postural habits adopted during everyday activities are associated with this complaint. These findings could contribute to the implementation of prevention and rehabilitation strategies.
1.Introduction
Young people tend to spend most of their days sitting down while carrying out sedentary activities [1, 2, 3], combining long periods in this position during their classes with the time they spend at home using the computer (or other electronic devices) and watching television [1, 2, 4, 5]. By adopting inappropriate positions for these activities, some postural habits such as tilting the head and/or trunk forward, overload the muscles in these regions and other structures of the backbone [6, 7, 8, 9, 10, 11]. In addition, when sitting down the lower limbs remain flexed, which promotes a reduction in the flexibility of the thigh muscles, quadriceps and the lower back extension, provoking compensation in other regions [11]. The habit of slump sitting, very common among young people when watching TV and using the computer, causes a reduction in lumbar lordosis or even kyphosis in this region, increased kyphosis in the thoracic region, with great deformation and impact on the tissues in these regions [5, 12]. The habit of lying in a prone position in bed and when using the computer [4] the asymmetrical use of backpacks [13, 14] and other inappropriate postural habits promote musculoskeletal alterations which overload the backbone and are associated with pain [3, 13, 15], and the association between postural habits and low back pain (LBP) has often been reported [4].
LBP was identified as the most prevalent source of musculoskeletal complaint in young people and can be considered a public health issue [4]; the presence of back pain in 17-year olds is similar to that in adults [16], and may be associated with the use of medication, going to the doctor, school absenteeism, and reductions in the levels of physical activity and health quality [7, 9, 12]. However, the extension of the responsibility of the inappropriate positions adopted in the development of LBP is not known, since it has a multifactorial nature [17, 18, 19]. There are few studies investigating the role of postural habits in the LBP of adolescents [4, 20], and the evaluation of postures adopted during daily activities is important to understand the origin of the symptoms [4, 21, 22] and contribute to the implementation of preventative measures [4]. The acquisition of proper body behaviour and postural habits must be modelled while still in adolescence, reducing the risk of postural changes and/or symptoms in adulthood [20, 23].
For this study it was necessary to construct and previously validate a self-perception questionnaire concerning body posture, since the instruments used in other surveys did not correspond to the perceptions of young people with respect to their habits (a pilot study had been previously carried out). This study aimed to investigate the prevalence of low back pain and its associations with postural habits as perceived by young people between 15 and 18 years of age.
2.Methods
2.1Participants
This study was developed using 679 young people (15 to 18 years old) with an average age of 16.23 (0.89) years, from the first and second years of a high school in Florianópolis, Brazil. Students from both the morning and afternoon periods were included, indicated by the school direction board, and they accepted taking part in the study and presented no cognitive, physical and/or psychiatric problems that might prevent them from responding the questionnaire. There were more girls than boys matriculated in the high school used, and, in addition, more girls than boys agreed to take part in the study. The study was approved by the Ethics in Research Committee of the State University of Santa Catarina, (Certificate of Approval (CAAE) n
2.2Instruments
The participants filled in the Oliveira Questionnaire on Low Back Pain in Young People (OLBPYQ), which was developed and validated, and showed a reliability of (ICC
The OLBPYQ uses language which is accessible to the age group (10–18 years old) to which it was applied, is clear and objective, is mainly formed of closed answers and is fast to complete (10 to 15 minutes). LBP refers to all complaints of pain in the lower part of the back (acute or chronic) which might spread to the buttocks and legs, with a minimum duration of 24 hours [25]. Questions related to: age, gender and psychosocial variables related to the level of physical activity and tobacco use were answered. Regarding LBP, the questions were: occurrence, age of the first complaint, pain present in the same place in the last three months or throughout life frequency, intensity (measured using the pain analogue visual scale), activities that worsen the pain, need for a visit to the doctor for guidance.
Another instrument used in this study was the Questionnaire of Body Awareness and Postural Habits of Young People (Q-BAPHYP). This instrument was previously validated, tested and had the internal consistency (0.80) and reproducibility (ICC from 0.59 to 0.74) verified through the Cronbach Alpha [26].
This questionnaire uses language which is accessible to this age group, is clear and objective and is formed of 35 closed questions (items Likert) divided into 4 dimensions, grouped according to the postural habits and location: in the classroom (sitting 8 questions; standing 2 questions; body movement 1 questions), at home (sitting – 8 questions; body movement 1 question; standing 2 questions; position when watching TV 3 questions), carrying and lifting objects (backpack 2 questions, from the floor 2 questions) and teachers’ disciplinary guidance in relation to the student’s body position in the classroom (3 questions). The average time for completion was seven minutes. There were 5 alternative answers to each item: never, hardly ever, often, always, do not know/remember. The Likert scale used in this questionnaire was bipolar, for positive statements (good postural habits) the score starts at
2.3Variables
A tercile distribution was used to categorize the pain intensity variable: low (
The postural habit data was analysed using different methods: the first considered the scores of posture/dimension (sum of positive and negative values, which varied from
When presenting the data regarding the frequency of LBP in the last three months, some categories were created to facilitate visualization: 0 to 10 times, 12 to 30 and 40 to 100 times; as well as for the time of retreat of the worst pain reported in the last three months: hours, up to 7days, 8 to 15 days, 16 to 30 days and over 60 days.
2.4Statistical analysis
A descriptive analysis was applied using the mean, standard deviation and frequency distribution of the data. The Kolmogov-Smirnov test was used to analyse the data distribution indicating a non-parametric distribution. The inferential statistical analysis sought to identify possible differences in the awareness of postural habits, considering the three LBP dimensions evaluated (at the present moment, in the last three months, throughout life) using the Mann-Whitney U test. The same procedure was used to compare the scores for each gender. Considering the variables presented in percentage, the associations were analysed through the Chi-square test, adopting a
3.Results
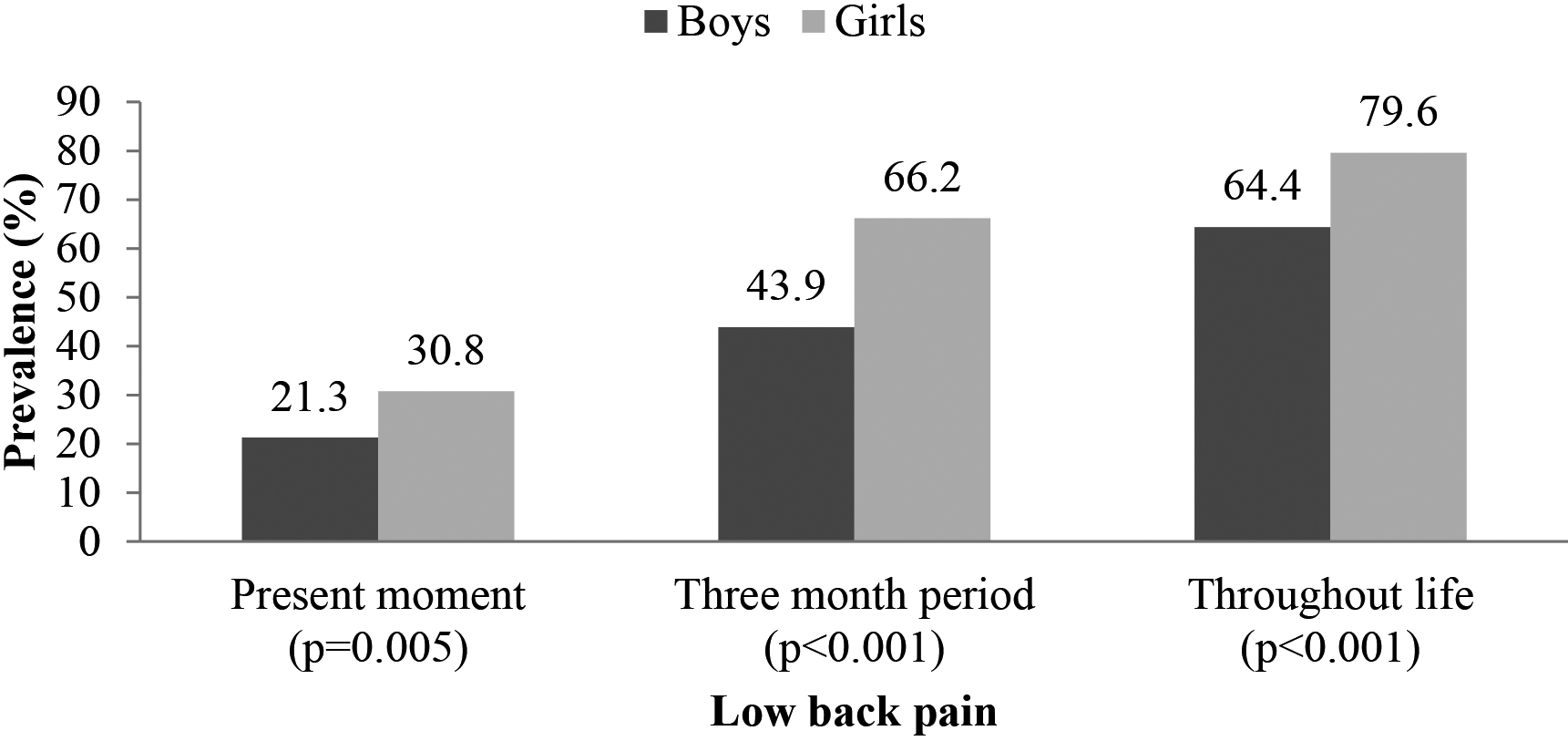
Of the 679 young people under evaluation, 37.26% were boys and 62.74% were girls. The girls had already started menstruating and most of them had their menarche when they were 12 years old (27.5%); 93.5% of the participants did not smoke and 81.0% did not work. Regarding the prevalence of LBP in this group, the current prevalence point was 27.2%, in the three-month period it was 57.7% and 73.9% throughout life. Boys and girls presented values that were significantly different for the current prevalence (
Figure 1.
Low back pain prevalence in young male and female people (%).
The participants did not present significant differences between genders regarding most of the pain characteristics (age of onset, frequency, intensity, time of retreat of the most intense LBP, seeing a doctor and seeking treatment). The variable: presence of pain in another region simultaneously with the LBP of highest frequency was only observed in girls (
Table 1
Descriptive data of low back pain in the last three months according to gender
| Variables | General | Boys | Girls | |
|---|---|---|---|---|
| Age – years, mean (SD) | 16.23 (0.89) | 16.24 (0.91) | 16.22 (0.89) | 0.956 |
| Onset of low back pain (LBP) – age | ||||
| | 5.80% | 4.00% | 6.80% | 0.175 |
| 10 to 12 years | 16.4% | 20.1% | 14.4% | |
| 13 to 15 years | 67.7% | 64.0% | 69.7% | |
| 16 to 18 years | 10.1% | 12.0% | 9.10% | |
| Number of times LBP was felt | ||||
| 0–10 | 79.6% | 78.2% | 80.1% | 0.656 |
| 12–30 | 10.5% | 16.3% | 8.20% | |
| 40–100 | 9.6% | 5.4% | 11.7% | |
| LBP intensity (0–10 – AVS) | ||||
| | 27.6% | 30.0% | 26.6% | 0.702 |
| 4–6 | 50.3% | 47.3% | 51.5% | |
| | 22.2% | 22.7% | 21.9% | |
| Most intense pain time of retreat | ||||
| Hours | 12.4% | 12.5% | 12.4% | 0.706 |
| Up to 7 days | 34.3% | 41.8% | 31.6% | |
| 8 to15 days | 18.5% | 11.1% | 21.3% | |
| 16 to 30 days | 23.8% | 19.4% | 25.3% | |
| 31 to 60 days | 9.10% | 11.1% | 8.30% | |
| Over 60 days | 1.90% | 4.20% | 1.00% | |
| Pain in other regions simultaneously with the LBP | ||||
| Yes | 67.3% | 52.7% | 73.0% |
|
| No | 32.7% | 47.3% | 27.0% | |
| Cervical | 54.9% | 66.1% | 56.5% | – |
| Thoracic | 100 % | 95.8% | 99.2% | |
| Buttocks | 54.6% | 4.70% | 54.2% | |
| Thighs | 89.1% | 32.4% | 90.1% | |
| Lying down for a long time | 23.60% | 25.50% | 23.20% | – |
| Getting up from bed | 20.70% | 16.70% | 21.80% | |
| Sitting down for a long time | 35.40% | 33.70% | 36.00% | |
| Walking | 28.70% | 34% | 27.20% | |
| Putting on shoes | 8.50% | 9.10% | 8.30% | |
| Standing up for a long time | 34.40% | 25.10% | 36.90% | |
| Watching TV | 9.70% | 14.40% | 9.70% | |
| Using PC/tablet | 19.60% | 24.80% | 17.90% | |
| Carrying weight | 60.60% | 48% | 57.60% | |
| Bending the body forwards | 19.80% | 20.20% | 19.70% | |
| Doing housework | 17.70% | 2.70% | 21.30% | |
| Physical activity | 19.10% | 25.20% | 17.50% | |
| Other | 2.50% | – | 3.20% | |
| Visit to the doctor | ||||
| Yes | 13.80% | 15.80% | 12.90% | 0.455 |
| No | 86.20% | 84.20% | 87.10% | |
| LBP treatment | ||||
| Yes | 19.10% | 21.10% | 18.30% | 0.536 |
| No | 80.90% | 78.90% | 81.70% |
Differences were observed when comparing gender in relation to the perception of postural habits, and the girls usually showed more awareness of poor postural habits than the boys, except for the lying down posture and regarding disciplining by teachers related to student body positions in the classroom. Boys and girls showed significant differences with respect to their perceptions of posture in a seated position (
Table 2
Description of postural perception considering scores awarded for dimension/posture by boys and girls
| Score Max/Min | Scores/posture | Boys | Girls | |||||
|---|---|---|---|---|---|---|---|---|
| Classroom | Sitting, mean (SD) | 2.71 | (4.78) | 0.71 | (5.57) |
| 0.001 | |
| Positive scores, | 178 | (70.36) | 217 | (50.94) | ||||
| Negative scores, | 75 | (29.64) | 209 | (49.06) | ||||
| Standing up, mean (SD) | 0.58 | (2.26) | (2.30) |
| 0.001 | |||
| Positive scores, | 120 | (47.43) | 141 | (33.10) | ||||
| Negative scores, | 133 | (52.57) | 285 | (66.90) | ||||
| Carries out articular movements, mean (SD) | 0.07 | (1.40) | (1.35) | 0.006 | ||||
| Positive scores, | 131 | (51.78) | 160 | (37.56) | ||||
| Negative scores, | 122 | (48.22) | 266 | (62.44) | ||||
| Home | Sitting down, mean (SD) | 3.12 | (4.96) | 0.37 | (5.41) | 0.074 | ||
| Positive scores, | 178 | (70.36) | 206 | (48.36) | ||||
| Negative scores, | 75 | (29.64) | 220 | (51.64) | ||||
| Lying down, mean (SD) | 0.54 | (2.42) | 1.12 | (2.35) | 0.101 | |||
| Positive scores, | 128 | (50.59) | 256 | (60.09) | ||||
| Negative scores, | 125 | (49.41) | 170 | (39.91) | ||||
| Carries out articular movements, mean (SD) | (1.39) | (1.38) | 0.085 | |||||
| Positive scores, | 115 | (45.45) | 156 | (36.62) | ||||
| Negative scores, | 138 | (54.54) | 270 | (63.38) | ||||
| Standing up, mean (SD) | 0.85 | (2.33) | 0.03 | (2.32) | 0.471 | |||
| Positive scores, | 138 | (54.54) | 171 | (40.14) | ||||
| Negative scores, | 115 | (45.45) | 255 | (59.86) | ||||
| Posture when using the computer/similar or watching TV, mean (SD) | (2.68) | (2.81) | 0.059 | |||||
| Positive scores, | 109 | (43.08) | 103 | (24.18) | ||||
| Negative scores, | 144 | (56.91) | 323 | (75.82) | ||||
| Objects | Posture when carrying backpack, mean (SD) | 2.05 | (2.23) | (2.69) | 0.782 | |||
| Positive scores, | 194 | (76.68) | 87 | (20.42) | ||||
| Negative scores, | 59 | (23.32) | 339 | (79.58) | ||||
| Posture when lifting objects from the floor, mean (SD) | 0.40 | (2.20) | 0.34 | (2.08) | 0.206 | |||
| Positive scores, | 108 | (42.69) | 167 | (39.20) | ||||
| Negative scores, | 145 | (57.31) | 259 | (60.80) | ||||
| Teacher | Disciplining of student body behaviour, mean (SD) | (1.95) | (1.76) | 0.224 | ||||
| Positive scores, | 7 | (2.77) | 18 | (4.22) | ||||
| Negative scores, | 246 | (97.23) | 408 | (95.77) | ||||
| TOTAL | 253 | (100) | 426 | (100) | ||||
Positive scores correspond to the perception of proper postural habits; negative scores correspond to the perception of poor postural habits;
For boys (Table 4), the postural habits of turning the body, reducing lumbar lordosis or kyphosis in this region when sitting in the classroom, in the same position, rotating the body, not placing the feet on the ground and watching TV or using the computer or other similar devices in an inappropriate posture at home, are all associated with LBP. Disciplining by teachers who allow movement in the classroom was also significant regarding LBP. On the other hand, proper thoracic support in the classroom, lying in a prone position in bed and sitting in an appropriate position to watch TV or use the computer or similar device, were significantly associated with the absence of LBP.
For girls (Table 4), postural habits associated with LBP were to tilt and rotate the body, cross the legs when sitting in the classroom; and at home, tilting and rotating the body, reducing lumbar lordosis or kyphosis in this region, placing the feet on the floor when sitting, distributing the body weight asymmetrically on the legs when standing, inappropriate posture when lying down or sitting to watch TV or use the computer or other similar devices. Disciplining by teachers who allow student movement in the classroom was also associated with the complaint. On the other hand, the habits of sitting with proper thoracic support in the classroom and at home, with the feet placed on the floor in the classroom, and an appropriate position to watch TV or use the computer or other similar devices, and suitable support on both legs when standing at home, were associated with the absence of LBP.
The analyses of the association between postural habits and LBP were carried out at three different moments (at present, in a three-month period and throughout life) and the LBP throughout life was seen to have more associations for both boys and girls.
4.Discussion
This was a cross sectional and retrospective study that calculated the values for the prevalence of LBP, 27.2% at the present moment (moment of the survey), 57.7% in a three-month period (last three months), and 73.9% throughout life, in 679 young people (15 to 18 years old), seeking to identify the associations with postural habits noticed by the participants. A study with a group of 546 Danish youngsters, representing an age group similar to that used in this study, Skoffer et al. [27] found 51.3% prevalence of LBP in the last three months and 64.8% throughout life; Smith et al. [16] observed that 49.5% of 1126 17-year old Aus-
Table 3
Low back pain (present moment, three-month period and throughout life) and boys’ awareness of postural habits
| Boys | Present moment, mean (SD) | Three-month period, mean (SD) | Throughout life, mean (SD) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Postural habit perception | Yes | No |
| Yes | No |
| Yes | No |
|
| Proper thoracic support – sitting in the classroom | 1.19 (0.59) | 1.57 (0.65) |
| 1.30 (0.62) | 1.72 (0.54) |
| 1.43 (0.62) | 1.60 (0.71) | 0.050 |
| Rotating body – sitting in the classroom | 1.18 (0.85) | 0.85 (0.81) | 0.012 | 1.11 (0.84) | 0.81 (0.65) | 0.390 | 1.02 (0.80) | 0.73 (0.86) | 0.004 |
| Lumbar kyphosis – sitting in the classroom | 1.56 (0.96) | 1.30 (1.00) | 0.096 | 1.58 (0.95) | 1.28 (0.95) | 0.122 | 1.45 (0.96) | 1.19 (1.04) | 0.044 |
| Lumbar lordosis – sitting in the classroom | 1.18 (0.84) | 1.55 (0.97) | 0.018 | 1.41 (0.89) | 1.38 (0.99) | 0.828 | 1.40 (0.92) | 1.59 (1.00) | 0.143 |
| Proper weight distribution on both legs – standing in the classroom | 1.60 (0.88) | 1.77 (0.92) | 0.210 | 1.66 (0.86) | 1.61 (0.93) | 0.782 | 1.65 (0.88) | 1.90 (0.97) | 0.033 |
| Proper thoracic support – sitting at home | 1.30 (0.74) | 1.66 (0.90) | 0.005 | 1.41 (0.84) | 1.68 (0.96) | 0.073 | 1.50 (0.88) | 1.74 (0.87) | 0.034 |
| Rotating body – sitting at home | 0.98 (0.84) | 0.66 (0.76) | 0.014 | 0.88 (0.84) | 0.63 (0.68) | 0.109 | 0.80 (0.80) | 0.58 (0.75) | 0.032 |
| Feet not placed on the floor – sitting at home | 1.34 (0.98) | 1.04 (0.94) | 0.049 | 1.24 (1.00) | 0.85 (0.76) | 0.034 | 1.12 (0.95) | 1.08 (0.96) | 0.761 |
| Lying belly down – at home | 1.46 (1.00) | 1.83 (1.03) | 0.017 | 1.63 (1.08) | 1.92 (0.86) | 0.135 | 1.72 (1.02) | 1.81 (1.06) | 0.487 |
| Proper position watching TV/using PC – at home | 1.39 (0.98) | 1.57 (0.91) | 0.214 | 1.33 (0.88) | 1.76 (0.87) | 0.008 | 1.45 (0.90) | 1.67 (0.96) | 0.066 |
| Poor position watching TV/using PC – at home | 1.59 (1.00) | 1.08 (0.95) | 0.002 | 1.39 (0.98) | 1.22 (0.88) | 0.409 | 1.34 (0.95) | 0.92 (1.00) | 0.001 |
| Teachers who allow movement | 0.79 (0.67) | 0.71 (0.71) | 0.330 | 0.83 (0.70) | 0.60 (0.71) | 0.037 | 0.76 (0.71) | 0.66 (0.69) | 0.266 |
Table 4
Low back pain (present moment, three-month period and throughout life) and girls’ awareness of postural habits
| Girls | Present moment, mean (SD) | Three-month period, mean (SD) | Throughout life, mean (SD) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Postural habit perception | Yes | No |
| Yes | No |
| Yes | No |
|
| Proper thoracic support – sitting in the classroom | 1.12 (0.64) | 1.23 (0.70) | 0.012 | 1.16 (0.67) | 1.25 (0.58) | 0.380 | 1.18 (0.66) | 1.45 (0.76) | 0.001 |
| Thoracic tilt – sitting in the classroom | 2.00 (0.77) | 1.89 (0.77) | 0.171 | 1.98 (0.75) | 2.04 (0.71 | 0.649 | 1.99 (0.75) | 1.69 (0.83) | 0.004 |
| Rotating body – sitting in the classroom | 1.20 (0.88) | 1.18 (0.94) | 0.743 | 1.22 (0.91) | 1.33 (0.98) | 0.453 | 1.24 (0.92) | 0.96 (0.90) | 0.018 |
| Feet placed on the floor – sitting in the classroom | 1.88 (0.96) | 1.88 (0.90) | 0.915 | 1.83 (0.91) | 1.68 (0.94) | 0.318 | 1.81 (0.92) | 2.14 (0.87) | 0.003 |
| Crossed legs – standing in the classroom | 1.46 (0.98) | 1.43 (0.86) | 0.727 | 1.48 (0.92) | 1.55 (0.79) | 0.616 | 1.49 (0.90) | 1.26 (0.90) | 0.034 |
| Proper thoracic support – sitting at home | 1.19 (0.84) | 1.37 (0.86) | 0.026 | 1.24 (0.87) | 1.45 (0.76) | 0.052* | 1.27 (0.85) | 1.51 (0.87) | 0.022 |
| Thoracic tilt – sitting at home | 1.53 (0.85) | 1.37 (0.84) | 0.051* | 1.46 (0.84) | 1.49 (0.86) | 0.767 | 1.47 (0.84) | 1.24 (0.87) | 0.022 |
| Rotating body – sitting at home | 0.97 (0.88) | 0.83 (0.81) | 0.147 | 0.96 (0.86) | 0.89 (0.79) | 0.741 | 0.95 (0.85) | 0.60 (0.70) | 0.001 |
| Lumbar lordosis – sitting at home | 1.29 (0.92) | 1.36 (0.86) | 0.360 | 1.30 (0.89) | 1.27 (0.75) | 0.804 | 1.29 (0.87) | 1.53 (0.90) | 0.024 |
| Lumbar kyphosis – sitting at home | 1.36 (0.98) | 1.32 (0.94) | 0.574 | 1.42 (0.94) | 1.31 (0.89) | 0.421 | 1.40 (0.94) | 1.08 (0.96) | 0.005 |
| Proper weight distribution on both legs – standing in the home | 1.53 (0.98) | 1.39 (0.94) | 0.227 | 1.50 (0.97) | 1.51 (0.96) | 0.911 | 1.50 (0.97) | 1.18 (0.87) | 0.005 |
| Improper weight distribution on legs – standing in the home | 1.41 (0.86) | 1.51 (0.87) | 0.294 | 1.38 (0.85) | 1.57 (0.86) | 0.203 | 1.42 (0.86) | 1.73 (0.86) | 0.003 |
| Proper position watching TV/using PC – at home | 1.09 (0.93) | 1.13 (0.87) | 0.480 | 1.03 (0.89) | 1.19 (0.80) | 0.162 | 1.06 (0.87) | 1.38 (0.91) | 0.002 |
| Lying down position watching TV/using PC – at home | 2.29 (0.81) | 2.19 (0.83) | 0.203 | 2.27 (0.81) | 2.27 (0.80) | 0.897 | 2.28 (0.81) | 2.00 (0.85) | 0.004 |
| Poor position watching TV/using PC – at home | 1.43 (1.04) | 1.36 (0.97) | 0.520 | 1.47 (1.00) | 1.31 (0.89) | 0.286 | 1.44 (0.98) | 1.12 (0.99) | 0.009 |
| Teachers who promote movement | 0.36 (0.66) | 0.34 (0.65) | 0.588 | 0.39 (0.71) | 0.13 (0.33) | 0.008 | 0.35 (0.67) | 0.34 (0.59) | 0.655 |
tralian youngsters presented LBP. The values found in the studies were different, but it is important to consider that the methodologies, age groups, sample size and operational definition of the pain were different. However, the high prevalence values strengthen the concern with this health problem, since they mean that at least 1 of each 2 youngsters in the different studies (Brazil, Denmark and Australia) aged up to 17/18 years old, had already complained of LBP at some point in life.
The girls presented significantly higher values for LBP prevalence and this difference in gender was also observed in other studies [4, 14, 24, 28]. Noll et al. [14] reported that the poor postures of girls when carrying out daily activities, including sleeping, sitting to write or use the computer, watching TV, reading or studying in bed, helped to explain these complaints. In this study, in general the girls presented some awareness of inappropriate postural habits, differently from the boys, and significant differences were observed considering the habits of sitting, standing and moving around the classroom and when using the computer at home. However, poor postural habits adopted by most of the boys were also observed. Therefore, other factors have been suggested to explain the higher prevalence of LBP in girls, such as hormonal alterations due to sexual maturation prior to the boys, and the different kinds of hormones released [1, 29]. Regarding social and emotional aspects, girls are more motivated to show their feelings, to notice and express their complaints more often [28, 30]; considering behavioural habits, the girls present lower levels of physical activity and spend more time in sedentary activities [1, 14] and in poor positions that justify their complaints of pain [14].
The differences in the awareness of postural habits adopted and in the prevalence of LBP found in this study, when comparing boys and girls, reinforce the idea that groups of pain rather than the pain itself should be studied, and approached with specific measures for each gender. Confirming these findings, Straker et al. [31] reported the associations between pain and young people’s postural habits, and emphasized the importance of analysing these themes in clusters: boys and girls, as carried out in this study.
Although significant differences in habits have been noticed when comparing genders, the posture when sitting with reduction in lumbar lordoses or kyphosis in this region, turning and tilting of the body and not placing the feet on the floor in the classroom and at home, were all associated with LBP, while the habits of maintaining proper thoracic support, maintaining lumbar lordosis and placing the feet properly on the ground in the classroom and at home were associated with the absence of LBP for both genders.
Healthy postural habits are related to keeping the alignment of the backbone so that minimum tension is caused to this structure, with no waste of energy or discomfort [15, 32]. Young people who do not maintain suitable alignment or remain long periods in the same position have greater risks of feeling back pain due to the increase in mechanical load and tension [32, 33, 34]. For this reason, the position adopted by young people who sit for long periods in school has been investigated, since it tends to cause musculoskeletal disorders, such as trunk flexion and alterations in normal curves of the backbone, such as flattening or kyphosis in the lumbar region, causing overloads on the spinal discs, ligaments and muscles [3, 11, 12].
Proper placement of the feet on the floor (referred to by the girls) associated with pain seems to be incoherent, since this position tends to promote the adoption of a neutral posture [35]. In this case, feet support is believed to be accompanied by another frequent posture common to young people, that of slump sitting. While seated, they tend to lean the body backwards, supporting the thoracic region against the back of the chair and the sacrum on the seat, or even sitting with no thoracic support, altering the lumbar position (increasing lordosis or reducing the curvature) [4, 5, 12]. The participants of this study pointed out inappropriate sitting and lying down habits to watch TV or to use the computer, as being associated with LBP, while a good sitting posture was associated with those who did not present complaints.
In addition to the slump position, the use of computers and other electronic devices while sitting promotes biomechanical alterations such as cervical flexion and tension of cervical muscles [6, 7, 8, 10, 31, 36], trunk flexion and pelvic tilt, which originate complaints of discomfort and pain [10, 11, 22]. When using the lying down supine position with stretched legs, the psoas muscle becomes tense and increases the lumbar load [37], also, the head is leaning forward due to the cushion support which increases the stress on vertebral structures [38]; in the prone position (lying belly down) the lumbar region tends to be in hyperlordosis, also overloading the vertebrae [4].
Standing with more weight on one leg was associated with LBP, whereas standing with the weight distributed equally on both legs was associated with the absence of complaint. Although this is a posture frequently seen in clinical practice, no studies were found on the standing position with an asymmetrical distribution of the body weight on the two legs. This question of modifying the distribution of body weight on the lower limbs is assumed to have compensations in the upper regions, pelvis and backbone.
No associations were found between LBP and the posture adopted to sleep, however, the prone posture was associated with the absence of pain in boys. This data is different from literature findings in which this position is not advised for involving increases in lumbar lordosis [37] and vertebral rotation [39]. During sleep, when the body is in a neutral position, the intervertebral discs are hydrated and their elasticity restored, inappropriate posture might hamper this recovery [39] and result in LBP [40, 41].
The acquisition of inappropriate postural habits occurs during childhood, and it is in this phase that preventative measures of education and intervention are indicated [11, 20, 23]. The school seems to be the most suitable place to implement these programs and the participation of teachers is fundamental [20, 42]. Regarding disciplining from the teachers related to the students’ postural habits in the classroom, allowing and stimulating movements were associated with LBP. This is not in agreement with the literature, which advocates that sitting for shorter periods, standing up and moving around are measures to combat LBP. Therefore, teachers should promote and encourage these more dynamic habits [20]. The young people taking part in this study may have interpreted this question in an equivocal way, considering that inadequate postures, such as twisting the trunk to talk to a colleague or slump sitting, are permitted and not corrected by the teachers.
This study found no significant associations between LBP and the habit of carrying a backpack or lifting objects up from the floor. However, other studies observed that the use of backpacks asymmetrically was associated with LBP [13, 14, 27]. Regarding weight lifting, this is one of the activities most noted as responsible for LBP, and involves the object weight, the posture used and the time of this activity [41].
This study had some limitations such as the use of a self-reported questionnaires, which depended on interpretation, memory and self-knowledge, and for being a cross-sectional study, which did not allow the inference of causality. Future studies should explore awareness of postural habits involving a more thorough approach to the young people’s perception of their postural habits, emphasizing the sleeping position, distribution of body weight on one or another leg while standing, and the crossed legs position when sitting, due to few existing studies. The knowledge of factors associated with LBP makes it possible to adopt preventative and therapeutic measures related to the education and guidance of postures adopted for everyday activities. Longitudinal studies are also suggested which follow young people throughout their maturational period, analysing the interactions between the several bio-morphological and psychosocial variables related to their lifestyle.
5.Conclusions
The data produced by this study revealed that the 679 youngsters aged 15 to 18 years old reported a high prevalence of LBP, especially the girls. The participants with low back pain noticed some habits associated with their pain, such as rotating and tilting the body, maintaining the lumbar region with a reduction of lordosis or kyphosis (flexion), not placing their feet on the ground and crossing their legs when sitting in the classroom or at home, watching TV or using the computer sitting or lying down with a poor posture and distributing the body weight asymmetrically on the legs when standing.
Strategies for the prevention and rehabilitation of LBP in young people should be based on the education and guidance of postural habits adopted in daily activities.
Conflict of interest
The authors reported no conflicts of interest.
References
[1] | Costigan SA, Barnett L, Plotnikoff RC, Lubans DR. The health indicators associated with screen-based sedentary behavior among adolescent girls: A systematic review. J Adolesc Health. (2013) ; 52: (4): 382-392. doi: 10.1016/j.jadohealth.2012.07.018. |
[2] | Owen N. Ambulatory monitoring and sedentary behaviour: A population-health perspective. Physiol Meas. (2012) ; 33: (11): 1801. doi: 10.1088/0967-3334/33/11/1801. |
[3] | Castellucci HI, Arezes PM, Viviani CA. Mismatch between classroom furniture and anthropometric measures in Chilean schools. Appl Ergon. (2010) ; 41: (4): 563-568. doi: 10.1016/j.apergo.2009.12.001. |
[4] | Meziat Filho N, Coutinho ES, Silva GA. Association between home posture habits and low back pain in high school adolescents. Eur Spine J. (2015) ; 24: (3): 425-433. doi: 10.1007/s00586-014-3571-9. |
[5] | Dockrell S, O’Grady E, Bennett K, Mullarkey C, Mc Connell R, Ruddy R, et al. An investigation of the reliability of Rapid Upper Limb Assessment (RULA) as a method of assessment of children’s computing posture. Appl Ergon. (2012) ; 43: (3): 632-636. doi: 10.1016/j.apergo.2011.09.009. |
[6] | Abelin-Genevois K, Idjerouidene A, Roussouly P, Vital JM, Garin C. Cervical spine alignment in the pediatric population: A radiographic normative study of 150 asymptomatic patients. Eur Spine J. (2014) ; 23: (7): 1442-1448. doi: 10.1007/s00586-013-3150-5. |
[7] | Scheer JK, Tang JA, Smith JS, Acosta FL Jr, Protopsaltis TS, Blondel B, et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg. (2013) ; 19: (2): 141-159. doi: 10.3171/2013.4.SPINE12838. |
[8] | Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. Clin Spine Surg. (2012) ; 25: (2): E41-E47. doi: 10.1097/BSD.0b013e3182396301. |
[9] | O’Sullivan K, O’Keeffe M, O’Sullivan L, O’Sullivan P, Dankaerts W. The effect of dynamic sitting on the prevention and management of low back pain and low back discomfort: A systematic review. Ergonomics. (2012) ; 55: (8): 898-908. doi: 10.1080/00140139.2012.676674. |
[10] | Straker LM, Smith AJ, Bear N, O’Sullivan PB, de Klerk NH. Neck/shoulder pain, habitual spinal posture and computer use in adolescents: The importance of gender. Ergonomics. (2011) ; 54: (6): 539-546. doi: 10.1080/00140139.2011.576777. |
[11] | Jacobs K, Hudak S, McGiffert J. Computer-related posture and musculoskeletal discomfort in middle school students. Work. (2009) ; 32: (3): 275-283. doi: 10.3233/WOR-2009-0826. |
[12] | Astfalck RG, O’Sullivan PB, Straker LM, Smith AJ, Burnett A, Caneiro JP, et al. Sitting postures and trunk muscle activity in adolescents with and without nonspecific chronic low back pain: An analysis based on subclassification. Spine. (2010) ; 35: (14): 1387-1395. doi: 10.1097/BRS.0b013e3181bd3ea6. |
[13] | Minghelli B, Oliveira R, Nunes C. Postural habits and weight of backpacks of Portuguese adolescents: Are they associated with scoliosis and low back pain? Work. (2016) ; 54: (1): 197-208. doi: 10.3233/WOR-162284. |
[14] | Noll M, Candotti CT, Rosa BN, Loss JF. Back pain prevalence and associated factors in children and adolescents: An epidemiological population study. Rev Saude Publica. (2016) ; 50. doi: 10.1590/S1518-8787.2016050006175. |
[15] | Caneiro JP, O’Sullivan P, Burnett A, Barach A, O’Neil D, Tveit O, et al. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. (2010) ; 15: (1): 54-60. doi: 10.1016/j.math.2009.06.002. |
[16] | Smith AJ, O’sullivan PB, Beales D, Straker L. Back pain beliefs are related to the impact of low back pain in 17-year-olds. Phys Ther. (2012) ; 92: (10): 1258-1267. doi: 10.2522/ptj.20110396. |
[17] | Pincus T, Kent P, Bronfort G, Loisel P, Pransky G, Hartvigsen J. Twenty-five years with the biopsychosocial model of low back pain – is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine. (2013) ; 38: (24): 2118-2123. doi: 10.1097/BRS.0b013e3182a8c5d6. |
[18] | Trevelyan FC, Legg SJ. Risk factors associated with back pain in New Zealand school children. Ergonomics. (2011) ; 54: (3): 257-262. doi: 10.1080/00140139.2010.547608. |
[19] | Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. (2010) ; 24: (6): 769-781. doi: 10.1016/j.berh.2010.10.002. |
[20] | Cardon G, De Clercq D, De Bourdeaudhuij I, Breithecker D. Sitting habits in elementary schoolchildren: A traditional versus a “Moving school”. Patient Education and Counseling. (2004) ; 54: (2): 133-142. doi: 10.1016/S0738-3991(03)00215-5. |
[21] | Lindegård A, Wahlström J, Hagberg M, Vilhelmsson R, Toomingas A, Tornqvist EW. Perceived exertion, comfort and working technique in professional computer users and associations with the incidence of neck and upper extremity symptoms. BMC Musculoskelet Disord. (2012) ; 13: (1): 1. doi: 10.1186/1471-2474-13-38. |
[22] | Hakala PT, Saarni LA, Ketola RL, Rahkola ET, Salminen JJ, Rimpelä AH. Computer-associated health complaints and sources of ergonomic instructions in computer-related issues among Finnish adolescents: A cross-sectional study. BMC Public Health. (2010) ; 10: (1): 1. doi: 10.1186/1471-2458-10-11. |
[23] | Manchikanti L, Hirsch JA. What can be done about the increasing prevalence of low back pain and associated comorbid factors? Pain. (2015) ; 5: (3): 149-152. doi: 10.2217/pmt.15.10. |
[24] | Coelho L, Almeida V, Oliveira R. Lombalgia nos adolescentes: Identificação de factores de risco psicossociais [Low back pain in young people: identification of psychosocial risk factors]. Estudo epidemiológico na Região da Grande Lisboa. Rev Port Saúde Pública. (2005) ; 23: (1): 81-90. Português. |
[25] | Schwertner DS, Oliveira R, Marinho APR, Benetti M, Beltrame TS, Capistrano R. Reliability, stability and validity of the brazilian adaptation of the Oliveira Questionnaire on Low Back Pain in young people. Acta Med Port. (2017) ; 30: (10): 691-698. doi: 10.20344/amp.8270. |
[26] | Schwertner DS, Oliveira RANDS, Beltrame TS, Capistrano R, Alexandre JM. Questionnaire on body awareness of postural habits in young people: Construction and validation. Fisioter Mov. (2018) ; 31: : 1-11. doi: 10.1590/1980-5918.031.ao16. |
[27] | Skoffer B. Low back pain in 15-to 16-year-old children in relation to school furniture and carrying of the school bag. Spine. (2007) ; 32: (24): E713-E717. doi: 10.1097/BRS.0b013e31815a5a44. |
[28] | Shehab DK, Al-Jarallah KF. Nonspecific low-back pain in Kuwaiti children and adolescents: Associated factors. J Adolesc Health. (2005) ; 36: (1): 32-35. doi: 10.1016/j.jadohealth.2003.12.011. |
[29] | Yao W, Luo C, Ai F, Chen Q. Risk Factors for Nonspecific Low-Back Pain in Chinese Adolescents: A Case Control Study. Pain Medicine. (2012) ; 13: (5): 658-664. doi: 10.1111/j.1526-4637.2012.01369.x. |
[30] | Trevelyan FC, Legg SJ. Back pain in school children – where to from here? Appl Ergon. (2006) ; 37: (1): 45-54. doi: 10.1016/j.apergo.2004.02.008. |
[31] | Straker LM, O’Sullivan PB, Smith AJ, Perry MC. Relationships between prolonged neck/shoulder pain and sitting spinal posture in male and female adolescents. Man Ther. (2009) ; 14: (3): 321-329. doi: 10.1016/j.math.2008.04.004. |
[32] | Smith A, O’Sullivan P, Straker L. Classification of sagittal thoraco-lumbo-pelvic alignment of the adolescent spine in standing and its relationship to low back pain. Spine. (2008) ; 33: (19): 2101-2107. doi: 10.1097/BRS.0b013e31817ec3b0. |
[33] | Dunk NM, Callaghan JP. Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work. (2010) ; 35: (1): 3-14. doi: 10.3233/WOR-2010-0953. |
[34] | Pillastrini P, Mugnai R, Farneti C, Bertozzi L, Bonfiglioli R, Curti S, et al. Evaluation of two preventive interventions for reducing musculoskeletal complaints in operators of video display terminals. Phys Ther. (2007) ; 87: (5): 536-544. doi: 10.2522/ptj.20060092. |
[35] | Harisinghani MG, Blake MA, Saksena M, Hahn PF, Gervais D, Zalis M, et al. Importance and Effects of Altered Workplace Ergonomics in Modern Radiology Suites 1. Radiographics. (2004) ; 24: (2): 615-627. doi: 10.1148/rg.242035089. |
[36] | Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. (2014) ; 25: : 277-279. |
[37] | Normand MC, Descarreaux M, Poulin C, Richer N, Mailhot D, Black P, et al. Biomechanical effects of a lumbar support in a mattress. J Can Chiropr Assoc. (2005) ; 49: (2): 96. |
[38] | Gordon SJ, Grimmer-Somers KA, Trott PH. A randomized, comparative trial: Does pillow type alter cervico-thoracic spinal posture when side lying? J Multidiscip Healthc. (2011) ; 4: : 321. doi: 10.2147/JMDH.S23028. |
[39] | Leilnahari K, Fatouraee N, Khodalotfi M, Sadeghein MA, Kashani YA. Spine alignment in men during lateral sleep position: experimental study and modeling. Biomed Eng Online. (2011) ; 10: (1): 1. doi: 10.1186/1475-925X-10-103. |
[40] | Lusa S, Miranda H, Luukkonen R, Punakallio A. Sleep disturbances predict long-term changes in low back pain among Finnish firefighters: 13-year follow-up study. Int Arch Occup Environ Health. (2015) ; 88: (3): 369-379. doi: 10.1007/s00420-014-0968-z. |
[41] | Oliveira VC, Ferreira ML, Refshauge KM, Maher CG, Griffin AR, Hopper JL, et al. Risk factors for low back pain: Insights from a novel case-control twin study. Spine J. (2015) ; 15: (1): 50-57. doi: 10.1016/j.spinee.2014.06.021. |
[42] | Vidal J, Borràs PA, Ponseti FJ, Cantallops J, Ortega FB, Palou P. Effects of a postural education program on school backpack habits related to low back pain in children. Eur Spine J. (2013) ; 22: (4): 782-787. doi: 10.1007/s00586-012-2558-7. |




