Characteristics of patients who dropped out after multidisciplinary pain management in Japan: A prospective cohort study
Abstract
BACKGROUND:
Because regular visits to distant hospitals may be a burden to patients, both in terms of time and cost, some patients with chronic musculoskeletal pain may discontinue multidisciplinary pain treatment, unable to maintain motivation to attend.
OBJECTIVE:
To evaluate and compare the pre-program characteristics of patients who dropped out and patients who continued treatment, thereby clarifying the characteristics of patients at risk of dropping out.
METHODS:
A multidisciplinary pain management treatment program was implemented for patients at the Pain Management Center, Hoshi General Hospital. From April 2015 to March 2018, 23 patients participated in the program. Twelve of the 23 patients lived outside the prefecture where the hospital is located. Of these 12 patients, five completed the program, while seven did not. We compared the dropout and continuation groups in terms of patient characteristics, pain severity, pain-related psychosocial factors, and quality of life.
RESULTS:
We found significant differences (
CONCLUSIONS:
The characteristics of patients who dropped out were older age, walking ability dysfunction, and low quality of life associated with low back pain.
1.Introduction
Pain management using a multidisciplinary approach for patients with chronic musculoskeletal pain is a useful method of treatment because of its efficacy, cost effectiveness, and the rarity of iatrogenic complications, as demonstrated in the United States since the 1950s [1, 2]. The biopsychosocial model of well-being [3, 4] is an important concept in multidisciplinary pain management. This is a general model or approach in which biological, psychological, and social factors are presumed to play important roles in human functioning with respect to disease or illness. Multidisciplinary pain treatment requires special facilities [5, 6] because of the requirement for cooperation with multidisciplinary medical staff; few facilities in Japan are able to provide a multidisciplinary approach for pain management – especially in the form of inpatient programs.
Table 1
Characteristics of the dropout group (patients from other prefectures treated through the inpatient program), presented according to order of treatment
| Patient (Distance from the patient’s home to our hospital) | Chief complaint | Structural disorder | Psychiatric diagnosis |
|---|---|---|---|
| 55-year-old woman (250 km [155 miles]) | Posterior cervical pain, bilateral upper extremity numbness | Ossification of posterior longitudinal ligament (after surgery) | Narcissistic personality disorder |
| 47-year-old woman (265 km [165 miles]) | Low back pain | None found | Attention deficit hyperactivity disorder, histrionic personality disorder, somatoform disorders |
| 51-year-old man (111 km [69 miles]) | Low back pain | None found | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
| 75-year-old woman (183 km [114 miles]) | Posterior cervical pain, bilateral omalgia, low back pain | Spondylosis | None diagnosed |
| 73-year-old woman (285 km [177 miles]) | Low back pain, bilateral leg pain | Spondylosis | None diagnosed |
| 42-year-old woman (1020 km [634 miles]) | Low back pain, bilateral leg numbness, cool feeling, burning sensation | None found | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
| 53-year-old woman (457 km [284 miles]) | Low back pain | Spondylosis | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
We implemented a multidisciplinary pain management program [5, 6] at Hoshi General Hospital based on the biopsychosocial model of well-being and guided by the recommendations of the International Association for the Study of Pain [3, 4, 5, 6, 7, 8, 9, 10]. Some patients with chronic musculoskeletal pain who desired treatment within the multidisciplinary pain management program lived outside the prefecture. Japan comprises four large islands and many smaller islands; it is divided into 47 prefectures. The center hospital (i.e., a university hospital) is the core medical institution in each prefecture in the Japanese medical system; this hospital primarily provides medical treatments to patients with intractable disease who reside near the hospital. However, when patients and their primary doctors seek multidisciplinary pain treatment, doctors may refer patients to a pain center located outside the patient’s prefecture of residence. Regular visits to a hospital located a long distance from the residential prefecture may be a burden to patients with chronic musculoskeletal pain. Although following up patients after the inpatient program is important for maintenance of patient motivation to control pain, visiting a hospital outside the prefecture of residence is difficult for patients because it requires additional time and expenses. For example, a typical patient in our dropout group (patient no. 5, 75-year-old woman with chronic low back pain) lived 285 km (177 miles) from our hospital (Table 1). Our inpatient multidisciplinary pain treatment program was attractive for her because of the ineffectiveness of all past treatments. She initially attended our inpatient program, and reported reduced pain severity, improved physical function, and better QOL immediately after attending our inpatient program However, she discontinued attending our hospital without notice, 2 months after the discharge from the inpatient program A previous study suggested that patients who discontinued attending a psychiatric clinic were dissatisfied with their experience at the clinic because the treatment offered was not consistent with their preferences, they feared severe side effects from the medications, were required to travel long distances to the clinic, and encountered other social and economic barriers [11]. Another study demonstrated that the dropout rate in a glaucoma clinic was high during early treatment, particularly among patients who were required to travel long distances to the clinic [12]. These previous findings suggested that patients who drop out of a treatment program might be required to travel long distances to the hospital.
Five of the 12 inpatient-program patients from other prefectures completed our program, but the remaining seven patients did not. It is important to clarify the pre-program characteristics of patients with chronic musculoskeletal pain who may drop out of treatment. We presumed that patients with chronic musculoskeletal pain who dropped out of treatment would engage in repeated doctor shopping and/or enter a vicious cycle involving chronic pain Therefore, we hypothesized that dropping out of treatment was associated with specific patient characteristics, including pain severity, pain-related psychosocial factors, and quality of life (QOL). The purpose of this study was to evaluate and compare the two groups of patients (i.e., dropout and continuation groups) before the program to clarify the characteristics of patients with chronic musculoskeletal pain who may drop out of treatment, and to prospectively analyze some outcomes in both groups.
2.Methods
2.1Patients
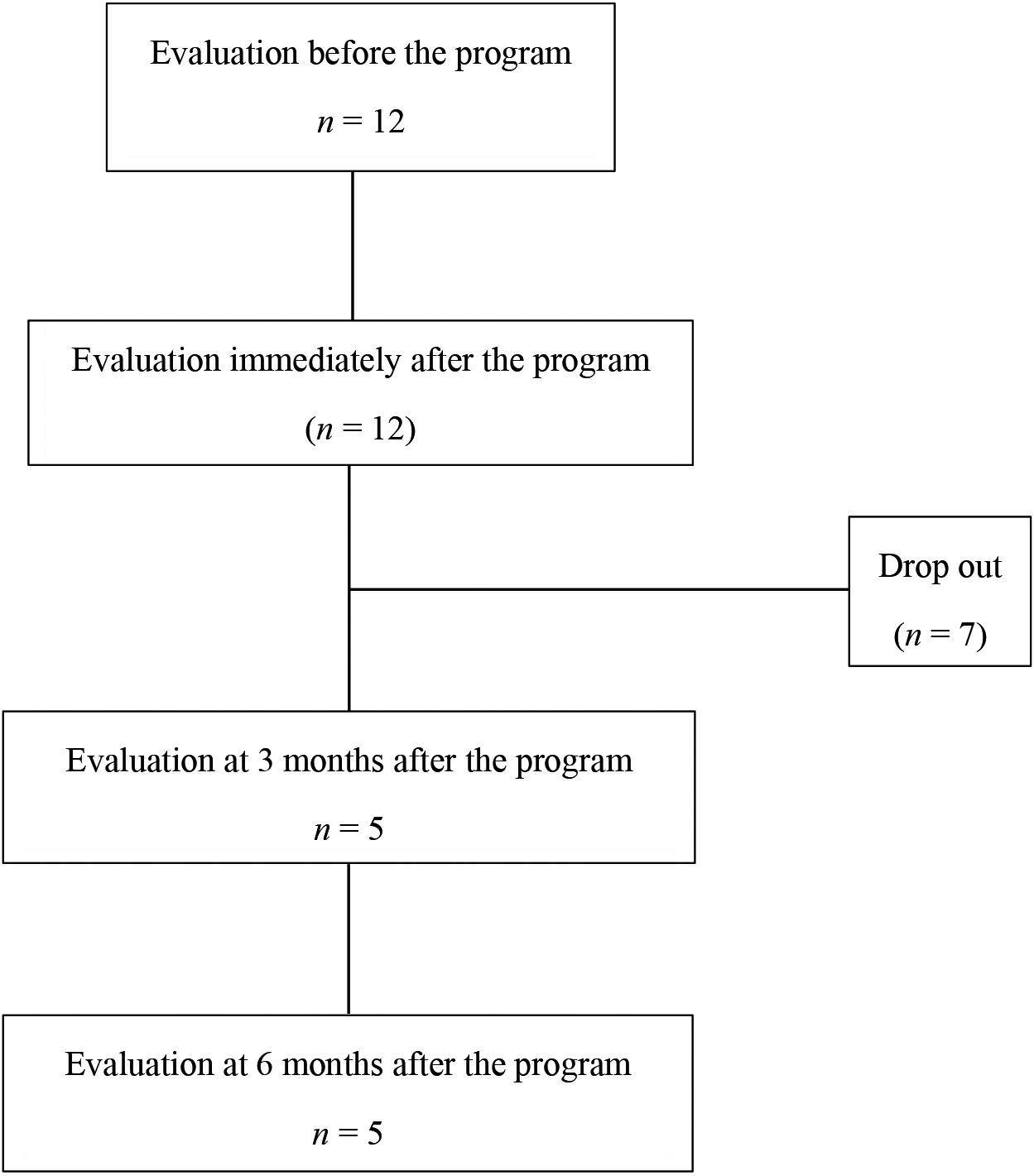
We evaluated 23 patients with chronic musculoskeletal pain who underwent multidisciplinary pain treatment at Hoshi General Hospital. Twelve (four men and eight women) of these 23 patients lived outside the prefecture where the hospital is located. Data regarding these 12 patients who lived far from the hospital (i.e., more than 111 km [69 miles]) were analyzed before and immediately after the program. Five of the patients (continuation group) were also assessed at 3 and 6 months after the program. The other seven patients (dropout group) could not be followed up because they did not attend regular hospital visits and/or satisfy the inpatient program (Fig. 1). None of the 12 patients had a regular occupation.
Figure 1.
Flowchart of patient dropout. Data regarding these 12 patients were analyzed before and immediately after the inpatient multidisciplinary pain management program. Five patients (continuation group) were also assessed at 3 and 6 months after the program. The remaining seven patients (dropout group) could not be assessed after the program.
2.2Multidisciplinary pain management program
The Pain Management Center was established at Hoshi General Hospital in April 2015, with technical support from the Department of Pain Medicine at Fukushima Medical University School of Medicine. The program is staffed by a team of orthopedic surgeons, psychiatrists, nurses, physical therapists, clinical psychologists, pharmacists, and nutritionists. The orthopedic surgeons and physical therapists screen patients for mechanical and biological changes in the body; the psychiatrists and clinical psychologists evaluate psychosocial and social factors Our program is indicated for patients who have difficulty working or attending school because of chronic musculoskeletal pain, as well as patients who are confined to their homes but wish to return to work or school. The multidisciplinary pain management treatment program includes a 3-week inpatient program and outpatient care for 6 months after the inpatient program. The program consists of three parts: exercise therapy, psychotherapy, and patient education. Our previous reports [5, 6] have described the multidisciplinary pain management program in detail. The objectives of the program are for patients to return to a functional daily life by acquiring new habits and methods of coping with their pain. One characteristic of the program is that family members or significant others can also participate in some of the lectures and psychotherapy sessions [5, 6].
The inclusion criteria for our 3-week inpatient multidisciplinary pain management program were: difficulty working or attending school because of chronic musculoskeletal pain; confinement to life at home but desiring to return to work or school; acceptance of our program; and ability to pay the hospital expenses for our inpatient program. Exclusion criteria were (one or more): older age and inability to answer the questionnaires; dementia or intellectual disabilities; and expectation of difficulty participating in the program (determined by multidisciplinary conference) [6].
2.3Evaluation of inpatients with chronic musculoskeletal pain
We evaluated patients with chronic musculoskeletal pain before the inpatient program, and collected relevant data. Specifically, we collected: 1) age; 2) distance from the patient’s home to our hospital; 3) pain severity assessed with the Brief Pain Inventory (BPI) [13]; 4) pain-related psychosocial factors assessed with several scales, including (a) the Brief Scale for Psychiatric Problems in Orthopedic Patients (BS-POP) (assessed by medical staff and/or the patient) [14], (b) the Pain Catastrophizing Scale (PCS) to evaluate the degrees of rumination, magnification, and helplessness [15, 16], (c) the Pain Disability Assessment Scale (PDAS) [17], (d) the Hospital Anxiety and Depression Scale (HADS) to assess anxiety and depression [18, 19] and (e) the Pain Self-Efficacy Questionnaire (PSEQ) [20, 21]; and 5) QOL assessed with several scales, including (a) the EuroQol Five-Dimensions Questionnaire (EQ-5D) [22, 23], b) the Roland-Morris Disability Questionnaire (RDQ) [24], and the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) [25]. Japanese validation studies of BS-POP [14], PCS [16], PDAS [17], HADS [19], PSEQ [21], EQ-5D [23], RDQ [24], JOABPEQ [25] were previously performed; all Japanese questionnaires were verified prior to this study. Our investigators comprised nine medical staff members: seven specialists (an orthopedic surgeon, a psychiatrist, a nurse, a physical therapist, a clinical psychologist, a pharmacist, and a nutritionist) to collect the data and two technicians to analyze the data for each patient. The data for patients with chronic musculoskeletal pain used in this study were: 1) age, 2) distance from the patient’s home to our hospital, and 3) questionnaires completed by the patients that evaluated pain severity, pain-related psychosocial factors (assessed with several scales), and QOL (assessed with several scales).
2.4Statistical analysis
We evaluated the dropout and continuation groups, then compared data between these two groups. Initial assessment of data normalization was performed using the Shapiro-Wilk test. Statistical analyses for each item were performed using the non-parametric Mann-Whitney
This study was focused on the patients with chronic musculoskeletal pain who lived outside the prefecture where our hospital is located and received treatment in the form of a 3-week inpatient program in our hospital. All of the patients (100%) completed the program. We could analyze these patients who completed the program. Therefore, the total sample size was small (
2.5Ethics approval and consent to participate
This study was approved by the ethics committees of the participating institutions at Fukushima Medical University (Reference number: 2429) and Hoshi General Hospital (Reference number: 27-3); it was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent for inclusion in the study.
Table 2
Characteristics of the continuation group (patients from other prefectures treated through the inpatient program), presented according to order of treatment
| Patient (Distance from the patient’s home to our hospital) | Chief complaint | Structural disorder | Psychiatric diagnosis |
|---|---|---|---|
| 20-year-old man (539 km [335 miles]) | Low back pain | None found | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
| 31-year-old woman (265 km [165 miles]) | Posterior cervical pain, bilateral omalgia, low back pain | None found | None diagnosed |
| 55-year-old man (159 km [99 miles]) | Posterior cervical pain, bilateral omalgia, back pain, low back pain, bilateral leg pain | None found | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
| 34-year-old man (161 km [100 miles]) | Low back pain | None found | Pervasive developmental disorder, attention deficit hyperactivity disorder, somatoform disorders |
| 42-year-old man (620 km [380 miles]) | Low back pain | None found | Pervasive developmental disorder, autism spectrum disorder, attention deficit hyperactivity disorder, somatoform disorders |
3.Results
The distance from the patient’s home to our hospital, clinical characteristics, chief complaints, structural disorders, and psychiatric diagnoses of the 12 patients from other prefectures who participated in the multidisciplinary pain management program are shown in Tables 1 and 2. All comparisons of assessed characteristics between the dropout and continuation groups are presented in Table 3. Some patients exhibited psychiatric disorders, but all were able to attend regular hospital visits. There was no statistically significant difference in the distance from the patient’s home to our hospital between the dropout and continuation groups (
Table 3
Comparison of characteristics, pain, and associated factors between the dropout and continuation groups (
| Continuation group ( | Dropout group ( |
| ||
|---|---|---|---|---|
| Age | 35.0 (25.5–49.0) | 53.0 (47.0–73.0) | 0.04 | |
| Distance from the patient’s home to our hospital (km) [miles] | 265 (160–579.5) (km) 166 (100–362.2) [miles] | 265 (183–457) (km) 166 (114.3–285.6) [miles] | 1.00 | 0.00 |
| BPI | 29.0 (11.5–33.5) | 25.5 (14.8–29.8) | 0.72 | |
| BS-POP (medical staff) | 15.0 (10.5–17.5) | 12.0 (0–14.0) | 0.33 | |
| BS-POP (patients) | 22.0 (19.0–24.0) | 19.0 (16.0–24.0) | 0.29 | |
| PCS (rumination) | 18.0 (16.0–19.5) | 9.8 (12.0–19.0) | 0.14 | |
| PCS (magnification) | 8.0 (5.0–8.5) | 4.0 (2.0–10.5) | 0.46 | |
| PCS (helplessness) | 11.0 (6.5–12.0) | 10.5 (6.5–17.3) | 0.64 | |
| PCS (total) | 34.0 (26.5–39.5) | 26.0 (19.0–47.0) | 0.84 | |
| PDAS | 22.0 (14.5–40.5) | 32.0 (27.0–42.0) | 0.33 | |
| HADS (anxiety) | 13.0 (8.0–13.0) | 6.0 (5.0–15.0) | 0.22 | |
| HADS (depression) | 8.0 (6.0–16.5) | 9.0 (4.0–11.0) | 0.51 | |
| PSEQ | 21.0 (11.0–24.0) | 19.0 (14.0–30.0) | 0.75 | |
| EQ-5D | 0.473 (0.419–0.759) | 0.482 (0.473–0.596) | 0.57 | |
| RDQ | 3.0 (1.5–4.0) | 8.0 (5.0–10.0) | 0.03 | |
| JOABPEQ | 64.0 (53.5–85.5) | 39.5 (5.3–44.8) | 0.02 |
4.Discussion
In this study, we assumed that a greater distance between the patient’s home and our hospital was a risk factor for dropout from the program; however, we could not prove this was a risk factor. Our analysis showed that compared with the continuation group, patients with chronic musculoskeletal pain living in other prefectures who dropped out after the inpatient multidisciplinary pain management program were characterized by older age, lower walking ability, and lower QOL associated with low back pain.
Previous studies have suggested that dropping out of chronic musculoskeletal pain management programs is associated with poor or negative treatment outcomes and low patient motivation to participate in the program [26, 27, 28]. Other previous work has revealed dropout incidence rates of approximately 20% and provided valuable insights regarding predictors of dropout [29, 30, 31, 32]. These barriers to retention in therapy can be categorized into five domains: 1) sociodemographic characteristics (patients who drop out tend to be younger and less educated) [29, 32]; 2) patient characteristics (patients who drop out tend to be less motivated for treatment, prefer alternative treatments, and have diagnoses of specific disorders, such as depression or substance use disorder) [29, 32]; 3) disease characteristics; 4) treatment characteristics (patients who drop out tend to have no pre-determined treatment time period and be enrolled in outpatient treatment); and 5) healthcare system/system domain characteristics (higher dropout rates are observed when the treatment is administered by trainees, instead of licensed therapists) [29].
Tetsunaga et al. reported that multidisciplinary treatment at a liaison clinic for patients with intractable chronic pain was able to improve patient anxiety; however, severe anxiety at the initial visit was a risk factor for dropout from the clinic [33]. In the present study, we found no statistically significant differences between the dropout and continuation groups in terms of anxiety, as measured by the HADS.
Sloots et al. suggested that the major reason for dropout from the diagnostic or treatment phase of a rehabilitation program was that patient expectations differed from the expectations of their health providers regarding the aim of treatment, because of differing views regarding the origin and treatment of low back pain [34]. Consistent with this previous finding, patients with chronic musculoskeletal pain participating in our inpatient program may have been constrained by preconceived notions regarding their symptoms at initial examination. Specifically, these patients typically presumed that the cause of their pain must be a biological problem in their bodies. At the initial examination, these patients had difficulty accepting the notion that there are many causes of pain, including biological, psychological, and social factors. In our program, patients with chronic musculoskeletal pain receive detailed information regarding the biopsychosocial model of well-being [35] at their first examination. This patient education may be the first step in cognitive behavioral therapy to treat their pain. We typically explain that pain self-management is very important for reduction of pain and improvement of QOL. Some patients are able to accept this approach, but others are not; notably, patients who are unable to accept or understand the approach may be at risk of dropout. However, we were unable to examine this possibility in the present study.
Oosterhaven et al. explored predictors of dropout from an interdisciplinary chronic pain management program among patients with chronic musculoskeletal pain [36]. In their study, the dropout rate was 19% (35 of 188 patients). These researchers evaluated several outcomes, including PCS, PSEQ, and HADS scores, by means of multiple logistic regression analyses; they concluded that patients with chronic pain who catastrophized were more likely to drop out of the program. However, in the present study, we found no statistically significant differences between the dropout and continuation groups in terms of PCS, PSEQ, or HADS scores.
Hosogoshi et al. conducted a pilot study to develop a basic individualized cognitive behavioral therapy approach for chronic pain and assessed its feasibility for use in Japan [37]; they evaluated the results immediately after treatment and at the 3-month follow-up. The dropout rate in their study was 14%: two of 14 patients dropped out during the intervention period. Notably, this previous study did not involve an inpatient program.
In most previous studies, dropout has been assessed during the course of multidisciplinary or interdisciplinary pain management programs, without considerations of dropout that occurs after programs have concluded [26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36]. Very few facilities carry out patient follow-up for more than 6 months after multidisciplinary or interdisciplinary pain management programs, and it is rare for studies to report dropout rates at 6 months after such programs [38, 39, 40, 41, 42]. In the present study, no patients dropped out during the inpatient program; moreover, patients who were treated in the inpatient program did not demonstrate low motivation during the program. Because these patients were followed up for 6 months after the program, we were able to compare the characteristics of the dropout group with the characteristics of the continuation group. Therefore, this study is valuable because it presents an evaluation of the characteristics of patients with chronic musculoskeletal pain in Japan who dropped out within 6 months after an inpatient multidisciplinary pain management program. In our study, the dropout rate was high: seven of 12 patients (58%) dropped out during the study period (Table 4). Table 4 presents a comparison of dropout rates between our study and previous studies conducted at other institutions worldwide [38, 39, 40, 41, 42].
Multidisciplinary/interdisciplinary pain management programs are generally presumed to have relatively high dropout rates; patient dropout from these programs is related to poor treatment outcomes and high financial costs. We had no instances of dropout among patients with chronic musculoskeletal pain during the inpatient portion of our multidisciplinary pain management program. All instances of dropout in our study occurred during outpatient treatment after discharge from the
Table 4
Comparison of dropout rates between the present study and previous studies
| First Author | Institution | Program (Duration) | Dropout rate, immediately after program (%) | Dropout rate, | |
|---|---|---|---|---|---|
| 3 months after program (%) | Dropout rate, | ||||
| 6 months after program (%) | |||||
| Angst et al. [38] | Reha Clinic Zurzach (Bad Zurzach, Switzerland) | Interdisciplinary pain treatment included: Adapted drug therapy, Standard rehabilitation, and CBT (total | 4.1% (7 dropouts of 171 patients: Refused to participate, | Not administered | 34.8% (57 dropouts of 164 patients: Refused to participate, |
| van Wilgen et al. [39] | Pain Centre of the University Medical Centre Groningen (Groningen, the Netherlands) | Multidisciplinary pain treatment included: CBT (3–6 weeks) | 12.5% (4 dropouts of 32 patients: No requirement for follow-up due to pain improvement, | Not administered | 7.1% (2 dropouts of 28 patients: No requirement for follow-up due to pain improvement, |
| Hampel et al. [40] | Center of Clinical Psychology and Rehabilitation, University of Bremen (Bremen, Germany) | Multidisciplinary pain treatment included: Rehabilitation and CBT (3–4 weeks) | 7% (22 dropouts of 311 patients: Personal reasons, | Not administered | 16.6% (48 dropouts of 289 patients: Discontinued participation, |
| Tlach et al. [41] Saha et al. [42] | Department of Internal and Integrative Medicine, Faculty of Medicine, University of Duisburg-Essen (Essen, Germany) | Multidisciplinary pain treatment included: physiotherapy, classical naturopathy, and psychotherapy (2 weeks) | 12.3% (38 dropouts of 310 patients: Discontinued study and/or withdrew consent for study participation, | Not administered | 30.1% (82 dropouts of 272 patients: Discontinued study and/or withdrew consent for study participation, |
| Takahashi et al. (this study) | Hoshi General Hospital (Koriyama, Japan) | Multidisciplinary pain treatment included: Physical therapy, Exercise therapy, Psychotherapy, CBT, and Pharmacotherapy (3 weeks) | 0% | 58% (7 dropouts of 12 patients: Discontinued study and/or withdrew consent for study participation, | 0% |
Abbreviation: CBT, cognitive behavioral therapy.
inpatient program. The patients who dropped out in our study had very high expectations to reduce their pain intensity and increase their activity; they consistently completed our inpatient program. We presumed that our inpatient program had no poor treatment outcomes because our previous analysis of 23 patients showed significant improvements in pain, associated factors, and physical functions, based on assessments performed before and immediately after the program [6]. However, these patients did not maintain reductions in pain, associated factors, and physical functions at home after discharge from the inpatient program; they could not continue to engage in exercise (e.g., walking, strengthening, and stretching) without assistance from our clinicians, and they could not maintain motivation to withstand the pain. The present findings indicate that patient dropout from treatment after the inpatient program was associated with older age, lower walking ability, and lower QOL associated with low back pain. Each of these variables may be associated with worsening of pain, associated factors, and physical functions after discharge from the inpatient program. Because of the additional time and expenses involved, it might have been difficult for our patients to maintain motivation for regular visits to a distant hospital. We have considered methods to improve the overall effectiveness of multidisciplinary and interdisciplinary pain management programs, especially during follow-up after discharge from an inpatient program. It is important to establish systems of cooperation with institutions located close to patients’ homes; these institutions can then manage follow-up for patients with chronic musculoskeletal pain after the completion of inpatient programs conducted at more distant institutions. Additionally, we have considered the need to clarify how to approach patients with chronic musculoskeletal pain who have older age, lower walking ability, and lower QOL associated with low back pain, prior to enrollment in our inpatient program. To the best of our knowledge, few studies have been published regarding long-term follow-up after multidisciplinary or interdisciplinary pain management programs. It is important to construct a system that enables long-term follow-up at all institutions, or (at least) at all cooperating pain centers. This system could facilitate the collection of information regarding treatment effects and improve treatment for patients with chronic musculoskeletal pain.
In addition to our program’s advantages, it has a few weak or controversial aspects. First, although our program is open to everyone, we must carefully consider each patient’s rehabilitation. Second, because it may be difficult to sufficiently change how patients think and behave within a short period of time, patients may require follow-up after discharge. Finally, a large number of medical personnel are involved in our inpatient program, and their incomes may be inadequate, given the insurance system for chronic pain in Japan. These points should be addressed before the findings for our inpatient program can be generalized to other areas. In addition, the present study had several important limitations. First, our study population was small, and larger populations should be analyzed in future studies. Second, the follow-up period was relatively short, and more studies with longer follow-up periods are needed to evaluate long-term outcomes.
In conclusion, this study showed that the characteristics of patients with chronic musculoskeletal pain living outside the prefecture who dropped out of treatment after an inpatient multidisciplinary pain management program were older age, lower walking ability, and lower QOL associated with low back pain. Previous studies regarding chronic musculoskeletal pain management programs have suggested that dropping out is associated with poor or negative treatment outcomes and low patient motivation to participate in the program. Our current study provides new insights regarding factors associated with dropping out of chronic musculoskeletal pain management programs.
Acknowledgments
The authors are grateful to all participants in this study and the clinical staff who supported this research: Koh Matsudaira, Akira Onda, Kenji Nihei, Minoru Iwasaki, Kazuaki Suzuki, Miho Ohuchi, Yuki Haruyama, Tikara Saitoh, Takahiro Yatsuda, Yoko Arase, Aki Kiryu, Yurika Saito, Yuki Moriyama, Megumi Sato, Yukie Moto, Mami Tanimoto, Akari Funao, Tomoko Fukuchi, and Mika Kanazawa. The authors also thank Jennifer Barrett, Ph.D., Ryan Chastain-Gross, Ph.D., and Audrey Holmes, Ph.D., from Edanz (https://jp.edanz.com/ac/) for editing a draft of this manuscript.
Conflict of interest
The authors report no conflicts of interest in this work.
References
[1] | Bonica JJ. Management of chronic pain in general practice. J Lancet. (1959) ; 39: (6): 389-396. |
[2] | Bonica JJ. Management of intractable pain in general practice. GP. (1996) ; 33: (1): 107-123. |
[3] | Loeser JD. Conception of pain. In: Stanton-Hicks M and Boas R, editors. Chronic low back pain. New York: Raven Press; (1982) ; pp. 145-148. |
[4] | Flor H, Turk DC. Chronic Pain: An Integrated Biobehavioral Approach. Seattle: IASP Press, (2011) . |
[5] | Takahashi N, Kasahara S, Yabuki S. Development and implementation of an inpatient multidisciplinary pain management program for patients with intractable chronic musculoskeletal pain in Japan: preliminary report. J Pain Res. (2018) ; 1: : 201-211. |
[6] | Takahashi N, Takatsuki K, Kasahara S, Yabuki S. Multidisciplinary pain management program for patients with chronic musculoskeletal pain in Japan: a cohort study. J Pain Res. (2019) ; 12: : 2563-2576. |
[7] | Loeser JD, Turk DC. Multidisciplinary Pain Management. In: Loeser JD, et al., editors. Bonica’s Management of Pain. Philadelphia: Lippincott Williams and Wilkins, (2001) . |
[8] | Turk DC, Okifuji A. Multidisciplinary Pain Management. In: Loeser JD, et al., editors. Bonica’s Management of Pain. Philadelphia: Lippincott Williams and Wilkins, (2001) . |
[9] | Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. (2015) ; 350: : h444. doi: 10.1136/bmj.h444. |
[10] | Otis JD, Reid MC, Kerns RD. The management of chronic pain in the primary care setting. In: James LC, Folen RA, editors. Primary Care Clinical Health Psychology: a model for the next frontier. Washington D.C.: American Psychological Association Press, (2005) . |
[11] | Gill HP, Singh Sharma KC. Study of dropouts from a psychiatric clinic of a general hospital. Indian J Psychiatry. (1990) ; 32: (2): 152-158. |
[12] | Ashaye AO, Adeoye AO. Characteristics of patients who dropout from a glaucoma clinic. J Glaucoma. (2008) ; 17: (3): 227-232. |
[13] | Ceeland CS, Ryan KM. Pain assessment: global use of Brief Pain Inventory. Ann Acad Med Singapore. (1994) ; 23: (2): 129138. |
[14] | Yoshida K, Sekiguchi M, Otani K, Mashiko H, Shiota H, Wakita T, et al. A validation study of the Brief Scale for Psychiatric problems in Orthopaedic Patients (BS-POP) for patients with chronic low back pain (verification of reliability, validity, and reproducibility). J Orthop Sci. (2011) ; 16: (1): 7-13. doi: 10.1007/s00776-010-0012-4. |
[15] | Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. (2000) ; 23: (4): 351365. |
[16] | Matsuoka H, Sakano Y. Assessment of cognitive aspect of pain: development, reliability, and validation of Japanese Version of Pain catastrophizing scale. Japanese J Psychos Med. (2007) ; 47: : 95-102. |
[17] | Yamashiro K, Arimura T, Iwaki R, Jensen MP, Kubo C, Hosoi M. A multidimensional measure of pain interference: reliability and validity of the pain disability assessment scale. Clin J Pain. (2011) ; 27: (4): 338343. |
[18] | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) ; 67: (6): 361370. |
[19] | Matsudaira T, Igarashi H, Kikuchi H, Kano R, Mitoma H, Ohuhi K, et al. Factor structure of the Hospital Anxiety and Depression Scale in Japanese psychiatric outpatient and student populations. Health Qual Life Outcomes. (2009) ; 7: : 42. |
[20] | Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. (2007) ; 11: (2): 153163. |
[21] | Adachi T, Nakae A, Maruo T, Shibata M, Maeda L, Saitoh Y, et al. Validation of the Japanese version of the pain self-efficacy questionnaire in Japanese patients with chronic pain. Pain Med. (2014) ; 15: (8): 1405-1417. |
[22] | EuroQOL Group. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. (1990) ; 16: (3): 199208. |
[23] | Shiroiwa T, Fukuda T, Ikeda S, Igarashi A, Noto S, Saito S, et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. (2016) ; 25: : 707-719. |
[24] | Suzukamo Y, Fukuhara S, Kikuchi S, Konno S, Roland M, Iwamoto Y, et al. Validation of the Japanese version of the Roland-Morris Disability Questionnaire. J Orthop Sci. (2003) ; 8: (4): 543-548. |
[25] | Kasai Y, Fukui M, Takahashi K, Ohtori S, Takeuchi D, Hashizume H, et al. Verification of the sensitivity of functional scores for treatment results – substantial clinical benefit thresholds for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ). J Orthop Sci. (2017) ; 22: (4): 665-669. |
[26] | Andrews NE, Strong J, Meredith PJ. Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2012) ; 93: : 2109-2121. |
[27] | De Rooij A, Roorda LD, Otten RHJ, van der Leeden M, Dekker J, Steultjens MPM. Predictors of multidisciplinary treatment outcome in fibromyalgia: a systematic review. Disabil Rehabil. (2012) ; 35: : 1-13. |
[28] | Van der Hulst M, Vollenbroek-Hutten MMR, IJzerman MJ. A systematic review of sociodemographic, physical, and psychological predictors of multidisciplinary rehabilitation-or, back school treatment outcome in patients with chronic low back pain. Spine. (2005) ; 30: : 813-825. |
[29] | Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol. (2012) ; 80: : 547-559. |
[30] | Swift JK, Greenberg RP, Tompkins KA, Parkin SR. Treatment refusal and premature termination in psychotherapy, pharmacotherapy, and their combination: a meta-analysis of head-to-head comparisons. Psychotherapy. (2017) ; 54: : 47-57. |
[31] | Fernandez E, Salem D, Swift JK, Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J Consult Clin Psychol. (2015) ; 83: : 1108-1122. |
[32] | Taylor S, Abramowitz JS, McKay D. Non-adherence and non-response in the treatment of anxiety disorders. J Anxiety Disord. (2012) ; 26: : 583-589. |
[33] | Tetsunaga T, Tetsunaga T, Nishie H, Ozaki T. Establishment of a liaison clinic for patients with intractable chronic pain. J Orthop Sci. (2015) ; 20: : 907-913. |
[34] | Sloots M, Dekker JH, Pont M, Bartels EA, Geertzen JH, Dekker M. Reasons of drop-out from rehabilitation in patients of Turkish and Moroccan origin with chronic low back pain in The Netherlands: a qualitative study. J Rehabil Med. (2010) ; 42: (6): 566-573. |
[35] | Turk DC, Monarch ES. Biopsychosocial perspective on chronic pain. In: Turk DC, Gatchel RJ, editors. Psychological Approaches to Pain Management: A Practitioner’s Handbook. New York: Guilford Press, (2002) . |
[36] | Oosterhaven J, Wittink H, Dekker J, Kruitwagen C, Devillé W. Pain catastrophizing predicts dropout of patients from an interdisciplinary chronic pain management programme: a prospective cohort study. J Rehabil Med. (2019) ; 51: (10): 761-769. |
[37] | Hosogoshi H, Iwasa K, Fukumori T, Takagishi Y, Takebayashi Y, Adachi T, et al. Pilot study of a basic individualized cognitive behavioral therapy program for chronic pain in Japan. Biopsychosoc Med. (2020) ; 14: : 6. |
[38] | Angst F, Verra ML, Lehmann S, Brioschi R, Aeschlimann A. Clinical effectiveness of an interdisciplinary pain management programme compared with standard inpatient rehabilitation in chronic pain: a naturalistic, prospective controlled cohort study. J Rehabil Med. (2009) ; 41: (7): 569-575. doi: 10.2340/16501977-0381. |
[39] | van Wilgen CP, Dijkstra PU, Versteegen GJ, Fleuren MJ, Stewart R, van Wijhe M. Chronic pain and severe disuse syndrome: long-term outcome of an inpatient multidisciplinary cognitive behavioural programme. J Rehabil Med. (2009) ; 41: (3): 122-128. doi: 10.2340/16501977-0292. |
[40] | Hampel P, Graef T, Krohn-Grimberghe B, Tlach L. Effects of gender and cognitive-behavioral management of depressive symptoms on rehabilitation outcome among inpatient orthopedic patients with chronic low back pain: a 1 year longitudinal study. Eur Spine J. (2009) ; 18: : 1867-1880. doi: 10.1007/s00586-009-1080-z. |
[41] | Tlach L, Hampel P. Long-term effects of a cognitive-behavioral training program for the management of depressive symptoms among patients in orthopedic inpatient rehabilitation of chronic low back pain: a 2-year follow-up. Eur Spine J. (2011) ; 20: : 2143-2151. doi: 10.1007/s00586-011-1810-x. |
[42] | Saha FJ, Bruning A, Barcelona C, Bussing A, Langhort J, Dobos G, et al. Integrative medicine for chronic pain: a cohort study using a process-outcome design in the context of a department for internal and integrative medicine. Medicine (Baltimore). (2016) ; 95: (27): e4152. doi: 10.1097/MD.0000000000004152. |




