The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: A systematic review
Abstract
BACKGROUND:
Adhesive capsulitis is a debilitating condition which causes the capsule of the gleno-humeral joint to thicken and contract progressively. The effectiveness of various non-operative methods has been demonstrated to improve the pain, range of motion (ROM) and functional status of patients with adhesive capsulitis.
OBJECTIVE:
This study aims to review recent evidence on the efficacy of physiotherapy interventions in the treatment of adhesive capsulitis.
METHODS:
PubMed, Physiotherapy Evidence Database (PEDro), Science Direct and Cochrane databases were searched for studies published since 2013. The search terms included: Frozen shoulder, adhesive capsulitis, physical therapy, rehabilitation, manual therapy, mobilization, exercise, education, and electrotherapy. The search was limited to studies published in English and studies that used human subjects.
RESULTS:
Quality scores of 33 articles were reviewed according to the Sackett’s critical appraisal criteria and the grades of recommendation were determined for physiotherapy interventions used in the studies.
CONCLUSION:
The empirical evidence suggests that certain physical therapy techniques and modalities are strongly recommended for pain relief, improvement of ROM, and functional status in patients with adhesive capsulitis, while others are either moderately or mildly recommended. However, the efficacy of one treatment modality over another is uncertain. The poor methodological rigors demonstrated in most of the reviewed studies emphasize the urgent need of properly conducted, adequately sampled randomized controlled trials with adequate follow up to determine the superior combination of treatment.
1.Introduction
Adhesive capsulitis, which is also referred to as frozen shoulder, is a condition that results in the limitation of movements at the shoulder joint debilitating daily activities [1]. The condition was first clinically recognized as “periarthritis scapula-humerae” by Duplay in 1872 [2]. However, Codman in 1934 described it as frozen shoulder, indicating the possibility of developing shoulder stiffness and pain without the influence of external factors [3]. “Adhesive capsulitis”, indicating a pathology in the glenohumeral capsule, was coined by Neviaser [4]. Adhesive capsulitis is the leading cause of pain at the shoulder joint in middle aged and elderly persons [5]. The exact underlying cause for adhesive capsulitis is unknown, but the non-dominant hand and females are considered to be more affected [6]. It is also more prevalent in the 40–70 years age group [2, 5] and it is estimated that 2–3% of the general population is affected with this pathology [7].
Adhesive capsulitis is primarily categorized into two types: primary and secondary [8]. Primary or idiopathic adhesive capsulitis is characterized by a gradual onset of pain and stiffness at the gleno-humeral joint without a specific cause [9]. Secondary adhesive capsulitis is known to be caused by several predisposing factors. Several review articles have classified these secondary factors further into systemic, intrinsic and extrinsic factors according to its nature [7, 10, 11, 12]. Systemic factors include diabetes mellitus, thyroid dysfunctions and hypoadrenalism [7, 10, 11], intrinsic factors include rotator cuff pathologies, biceps tendinitis, calcific tendinitis and acromioclavicular arthritis, and extrinsic factors include cardiopulmonary dysfunctions, cervical disc disease, stroke, Parkinson’s disease and humeral fractures [7]. Some authors have revealed that patients with this condition may naturally recover within two to three years [13, 14], whereas others have reported that the disability may even persist up to seven years [15].
Adhesive capsulitis develops in four distinctive stages: inflammatory, freezing, frozen and thawing stages. Stage 1 can last for about three months in which the patient may experience sharp, acute pain at the end range of movements as well as at rest, as well as sleep disturbances due to pain. Stage 2 refers to the freezing stage and can last from three to nine months. The patient might experience pain predominantly at night where the movements are limited in the forward flexion, abduction, internal and external rotation. Stage 3 is referred to as the frozen stage which can last from nine to fifteen months. The patient may still experience pain at the end ranges and may experience restricted range of motion. In stage 4, which is the thawing stage, pain may be diminished with progressive improvement of movements [7, 10, 11].
Although the exact treatment method for adhesive capsulitis is unknown, the effectiveness of various non-operative treatment approaches has been evaluated in the literature. These include corticosteroid injections [16, 17, 18, 19, 20], oral medications [21, 22], electro therapy modalities [23, 24, 25, 26], stretching exercises [27, 28], joint mobilization [29, 30, 31], and muscle energy techniques (MET) [32, 33, 34]. There is no consensus on the best single treatment intervention and therefore a combination of treatment modalities are performed [26]. The objective of this review is to systematically analyze the efficacy of physiotherapy interventions in the treatment of patients with adhesive capsulitis and to critically examine the quality of the recently published studies.
2.Methods
2.1Protocol
This systematic review has been conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocol (PRISMA) statement guidelines.
2.2Eligibility criteria
2.2.1Types of studies
Inclusion criteria: Randomized controlled studies, prospective or retrospective studies written in English were selected. Exclusion criteria: Studies including reviews, letters, comments, opinions, conference proceedings, animal experiments, case reports and case series were excluded.
2.2.2Types of participants
Patients with adhesive capsulitis regardless of the ethnicity, gender and age were considered.
2.2.3Types of intervention
Physical therapy interventions including rehabilitation, manual therapy, electrotherapy, exercise and education were included. Articles were excluded if they compared a physiotherapy intervention with a surgical procedure, interventions which were not directly related to physiotherapy, or other shoulder disorders including rotator cuff injuries, osteoarthritis and economic evaluation studies.
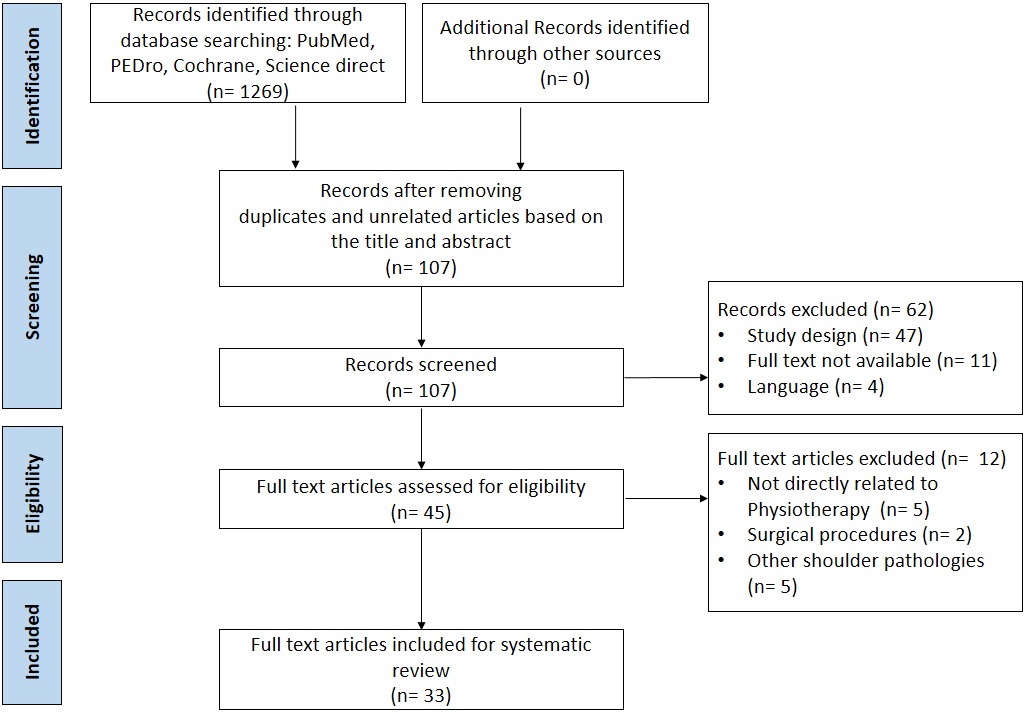
Figure 1.
Flowchart of the study selection.
2.2.4Types of outcome measures
The primary outcome measure was shoulder pain measured by any kind of pain scales. The secondary outcome measures were range of motion (ROM), functional status and the quality of life assessed by any associated scales.
2.3Information sources
Studies were identified by searching PubMed, Physiotherapy Evidence Database (PEDro), Science direct and Cochrane databases. A search was performed for articles published in English since January 2013, since the last review was conducted in 2013 [35]. The last search was run on 16 January 2020.
2.4Search
Since the terms frozen shoulder and adhesive capsulitis were used most to describe the condition, those search terms were used with “OR” operation. Then these two search terms were combined with “AND” operation with the following terms: “physical therapy”, “rehabilitation”, “manual therapy”, “mobilization”, “exercise”, “education”, and “electrotherapy”.
2.5Study selection process
Two authors independently screened the titles and the abstracts of the generated articles. The full papers were read if they met the inclusion criteria. Disagreements between authors were resolved by consensus.
2.6Data collection process
The first author extracted the data regarding basic information (authors, year of publication, gender, age and duration of symptoms), study design (sample size, randomization methods, allocation, blinding and reporting information), intervention details (type, session, frequency, intensity, dosage and duration) and outcomes (primary and secondary). The second author checked the extracted data. Disagreements were resolved by discussion between the two authors.
2.7Risk of bias in individual studies
Two authors evaluated the methodological rigor of the studies using a modified version [35] of Sackett’s critical appraisal criteria outlined by Mortenson and Eng [36] (Supplementary Table 1). Furthermore, the level of evidence supported by each article design and the grade of recommendation were identified according to the studies by Sackett [37] and Butler and Campbell [38] (Supplementary Table 2). Divergences between the two authors were resolved by a third author through discussion.
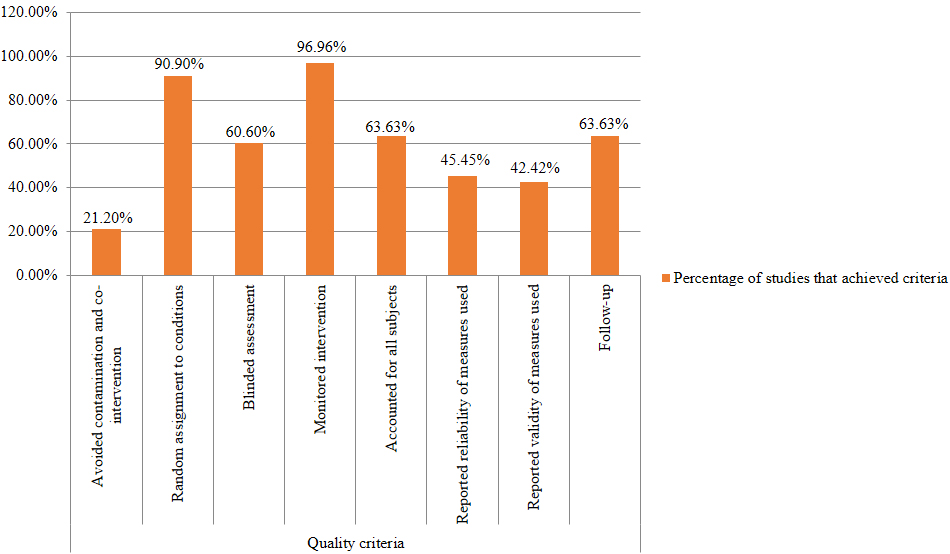
Figure 2.
Results of the quality review that shows the percentage of studies that met the criteria.
3.Results
The use of the keywords in various combinations with the above-mentioned databases yielded 1269 articles. After excluding 1236 articles, 33 articles were included in the review. The study selection is shown in Fig. 1. Of the 33, 30 articles were randomized controlled studies. The other three articles included a prospective cohort study, a retrospective cohort study and a cross-sectional exploratory study. The total number of subjects used in the studies ranged from 26 to 122. The average number of patients used in a study was 51.97. The average number of females per study was 31.7 (61.1%), while the female-to-male ratio was not mentioned in six studies. The number of male patients was higher only in six studies. The minimum number of patients used per group was 12, the maximum was 53, and 24 was the average per group. The patients in the studies had a mean age of 53.64
3.1Level of evidence
Out of the 33 reviewed studies, 30 studies were randomized controlled studies (RCTs). Two studies were cohort studies with prospective and retrospective study designs and one study was a cross-sectional exploratory study. Five studies were assigned level I evidence because of the incorporation of at least one control group, a randomization of subjects and the large sample sizes (
3.2Quality review
A quality review was performed according to Sackett’s critical appraisal criteria in which eight criteria were evaluated in each study. According to this, all criteria were achieved by two studies [45, 56]. Seven studies managed to avoid contamination and co-interventions and thereby reduced confounding results by asking the subjects not to undergo any adjuvant interventions for the duration of the study [1, 40, 45, 54, 56, 60, 67]. The rest of the studies did not discuss the avoidance of co-interventions or contaminations. All the RCTs incorporated an experimental group and a control group or compared two or several interventions. Out of the 30 RCTs, one article did not indicate the method of randomization [46], where group allocation in one study was not strictly randomized [58]. A blinded outcome assessment was utilized in 20 studies. The rest of the studies either did not use a blinded assessment or did not formally discuss this. Interventions were monitored by a physical therapist or were done in a clinic or rehabilitation center in 32 out of the 33 studies, where it was not mentioned in one study.
The interventions have been accounted for all subjects in 21 studies, where some patients dropped out during the intervention or during the follow up period in 12 studies. Reliability and validity of the outcome measurements were discussed in only 23 studies (range of motion: seven studies, Pain: five studies, and functional status: 11 studies). Twenty studies discussed the validity of the measurements (range of motion: four studies, pain: six studies, and functional status: 10 studies). Twenty-one studies included a follow up period (Supplementary Table 1). Quality scores are presented as percentages. To determine whether a study is of high quality, the cut-off point was taken as six points or 75% [35]. Based on this, 14 out of the 33 studies were identified as high quality studies. This included three level I studies of which two had poor qualities ([51]: 62.5% quality scores and [64]: 50% quality scores) (Fig. 2).
3.3Interventions
Koh et al. [39] reported significantly better outcomes with bee venom acupuncture (BVA) along with physiotherapy with a 12 week follow up period compared to non-steroidal injections with a physiotherapy group. In order to examine the long term outcomes, the results were retrospectively reviewed by Park et al. [66] after one year. BVA combined with physiotherapy remained clinically effective in terms of functional status after one year, which demonstrates the long term effects in improving the quality of life in patients with adhesive capsulitis. The addition of whole body cryotherapy (WBC) to physiotherapy modalities and passive joint mobilization was found to be more effective in improving all outcomes [40]. Doner et al. [41] studied the efficacy of the Mulligan technique combined with hot packs and trans-cutaneous electrical nerve stimulation (TENS) for the treatment of adhesive capsulitis with at a three month follow up and found superior effects compared to stretching exercises.
Ali and Khan [48] indicated no significant difference between mobilization combined with exercises and exercise alone at a five week follow up period. Celik and Kaya Mutlu [1] compared mobilization combined with intermittent stretching and found significantly greater functional outcomes in the combined treatment group after one year follow up. Mobilization with the distraction technique according to Kaltenborn and a cycle ergometer was utilized by Espinoza et al. [49] and demonstrated significant treatment effects in comparison to conventional physiotherapy techniques. Kouser et al. [58] compared the efficacy of Kaltenborn mobilization in the end and mid ranges where end range mobilization was found to be more efficacious.
Shih et al. [68] performed a muscle release intervention on upper trapezius, infraspinatus, pectoralis major and posterior deltoid muscles following heat and warm up with a hand cycle and found immediate effects on shoulder muscle performance, shoulder joint kinematics and pain.
Stretching techniques either as static or dynamic mode were applied in some studies. Ibrahim et al. [28] used a static progressive stretch (SPS) device along with traditional physical therapy techniques and compared the effects with conventional physiotherapy alone. The SPS device had better long term effects in improving ROM, pain and functional status in the patients at 12 months follow up. Inferior capsular stretching was performed with the use of a counteraction apparatus by Paul et al. [43] and significant improvements in shoulder functions were found with the addition of counteraction to physiotherapy at two weeks follow up. Duzgun et al. [63] compared posterior capsular stretching with scapular mobilization and the two groups were crossed and reassessed after the first treatment. Significant ROM improvements were noted in the two groups compared to baseline. Nevertheless, significant group differences were not encountered. Akbaş et al. [47] indicated significant effects on night pain and flexion, and abduction ROM values with upper extremity and scapular proprioceptive neuromuscular facilitation (PNF) along with conventional physiotherapy compared to the control group, whereas Balci et al. [53] demonstrated significant improvements with scapular PNF, exercise and physiotherapy modalities, although group differences were not noted.
Çelik and Türkel [27] evaluated the difference between the matrix rhythm therapy and cyclic stretching technique and stretching was found to be superior to the matrix rhythm therapy for function, physical health and satisfaction of the patients. Further continuous passive motion was utilized by Ekim et al. [54] to increase the joint ROM along with other modalities in patients with diabetes mellitus and they found significant improvements over the conventional physical therapy group. Strengthening of the rotator cuff muscles was performed by means of isometric and isotonic exercises with the use of a theraband and dumbbells and was combined with TENS and mobilization in the study by Rawat et al. [59]. This combination had greater improvements compared to TENS and mobilization in the improvement of pain, ROM and function in patients with adhesive capulitis.
In addition, AbdElhamed et al. [62] combined traditional physiotherapy with strengthening of the lower fibers of trapezius by means of modified prone cobra and prone row exercises to improve scapular tipping in patients with diabetic frozen shoulder. Significant improvements were obtained with the combined treatment with regard to scapular tipping distance at four weeks follow up. Mohamed et al. [65] examined the effectiveness of dynamic scapular recognition exercises using an audible biofeedback system to normalize the abnormal scapular movements that compensate the impaired glenohumeral movements. Scapular recognition exercises significantly improved scapular upward rotation, shoulder flexion and abduction at two weeks as well as shoulder external rotation and functional status scores additionally at six months.
Some other studies evaluated various electro- therapeutic modalities in the treatment of adhesive capsulitis. Chen et al. [42] compared extra corporeal shock wave therapy (ESWT) with oral steroids where ESWT showed better outcomes compared to the steroid group. Vahdatpour et al. [44] revealed significant improvements in the outcome measures for ESWT group along with analgesics and the exercises over the placebo group at five months follow up. Low level laser therapy was compared to reflexology by Soliman et al. [46] and they found significant improvements in the ROM and pain severity in adhesive capsulitis patients with diabetes mellitus at eight weeks follow up. Furthermore, a prospective cohort study performed by Ip and Fu [67] with 35 patients demonstrated long term effects with regard to functional status. Kim et al. [51] studied the effectiveness of high intensity laser therapy in the treatment of adhesive capsulitis. Significant pain relief was found in the interventional group compared to the placebo group at eight weeks follow up but no significant group difference was found thereafter.
The efficacy of ultrasound (UST), along with other techniques including stretching, mobilization and strengthening, has been evaluated by Ebadi et al. [57]. At three months follow up, continuous UST along with other techniques had no any additional effect on the outcome measures over sham UST. Similar results were found by Balci et al. [61], where the addition of UST to physiotherapy did not demonstrate a significant benefit compared to the control group in improving the outcomes. Additionally, Russel et al. [45] compared a hospital-based group exercise class with individual physiotherapy and to home exercises. At one year follow up, both physiotherapy interventions demonstrated significantly greater outcomes compared to home exercise alone although no significant group differences were noted between the physiotherapy interventions.
Moreover, the addition of supervised physiotherapy including mobilization and stretching to a home exercise program had no significant effect in improving the clinical outcomes compared to home exercises alone in patients after the hydrodilatation procedure at one year follow up [60]. Hsu et al. [50] showed that the introduction of 3 ml of 1% lidocaine injection prior to physiotherapy was effective in relieving pain during stretching and mobilization and thereby improved outcomes at six months follow up. Jellad et al. [64] introduced intra-articular distension (IAD) before and after physiotherapy sessions to compare with the physiotherapy alone group for 12 weeks. Accordingly, IAD followed by physiotherapy improved upper extremity function more compared to IAD preceded by physiotherapy. Nonetheless, IAD groups had no significant improvement on pain scores compared to physiotherapy alone. Furthermore, the addition of supra-scapular nerve block (SSNB) to a physical therapy program was evaluated by Klç et al. [52] for the treatment of adhesive capsulitis. It was revealed that the addition of SSNB to physiotherapy was more effective in reducing pain and functional disability in patients with adhesive capsulitis.
4.Discussion
This systematic review found 1269 articles of which 33 articles were used. The findings are discussed in terms of pain, range of motion and functional status.
4.1Pain
Out of the 33 studies, 26 assessed the level of pain. The interventions that assessed the pain include acupuncture, cryo-therapy, mobilization, extra corporeal shock wave therapy (ESWT), stretching, proprioceptive neuromuscular facilitation (PNF), laser therapy, ultrasound (UST), continuous passive motion, strengthening exercises, dynamic scapular recognition exercises, manual muscle release technique, conventional physiotherapy techniques, and physiotherapy compared to corticosteroid injections and suprascapular nerve block (SSNB) (Supplementary Table 3).
All interventions significantly improved the pain scores compared to baseline parameters. However, only a few studies were able to exhibit significant group differences. These include whole body cryotherapy (WBC), Mulligan mobilization technique, ESWT, static progressive stretch (SPS) device, sustained posterior capsular stretching, continuous passive motion, rotator cuff strengthening, dynamic scapular recognition exercises, lidocaine injection with physiotherapy, and SSNB with physiotherapy interventions. Most of the studies failed to do long term follow ups and evaluated the outcome measures only for a short period of time. ESWT, SPS device, dynamic scapular recognition exercises and lidocaine injection alone with physiotherapy were found to have long term effects in terms of pain. Bee venom acupuncture (BVA) combined with physiotherapy was found to improve pain levels compared to physiotherapy alone at rest and during motion. When dose-dependent comparisons were made, no significant difference was found between the two bee venom concentrations [39]. When the study results were retrospectively reviewed after a one year period, no significant difference was found between the groups in terms of pain [66].
When considering the Maitland mobilization technique, Ali and Khan [48] found a significant improvement in pain scores in the mobilization group after treatment, but no significant difference was noted compared to the control group. In contrast, mobilization with cycle ergometer improved pain scores compared to baseline and the control group. Upper extremity and scapular PNF was found to be effective in improving pain compared to baseline and in the conventional physiotherapy group [47]. However, in the study by Balci et al. [53], no significant group difference was noted between scapular PNF and physiotherapy modalities in terms of pain improvement.
4.2Range of motion
ROM was assessed as an outcome measure in 31 studies, with the exception of three studies. The interventions that assessed ROM include acupuncture, cryo-therapy, mobilization, ESWT, stretching, PNF, laser therapy, UST, matrix rhythm therapy, continuous passive motion, strengthening exercises, dynamic scapular recognition exercises, manual muscle release technique, supervised physiotherapy techniques, and physiotherapy compared to corticosteroid injections and SSNB (Supplementary Table 3).
All interventions significantly improved the ROM compared to baseline parameters. A significant difference compared to the control group was noted only in the interventions including WBC, Mulligan mobilization technique, ESWT, SPS device, continuous passive motion, rotator cuff strengthening, dynamic scapular recognition exercises, supervised physiotherapy, physiotherapy with lidocaine injection, stretching exercises and group exercise class and physiotherapy modalities. Among them, long term ROM improvement was demonstrated in the interventions including ESWT, SPS device, dynamic scapular recognition exercises, supervised physiotherapy techniques, physiotherapy with lidocaine injections, stretching exercises and group exercise classes and physiotherapy modalities. Ali and Khan [48] exhibited no significant difference of the Maitland mobilization over the control group, whereas Celik and Kaya Mutlu [1] showed significant improvements in abduction and flexion ROM in the group which performed stretching along with mobilization. Espinoza et al. [49] and Kouser et al. [58] found a significant difference in posterior mobilization and end range mobilizations respectively over the control group.
BVA significantly improved the ROM values comparatively to the baseline ROM values, but there was no difference with the control group during the short term follow up period [39]. Long term effects were not evaluated. In the study by Akbaş et al. [47], the PNF technique (upper extremity and scapular) was found to be effective in improving ROM values, except for internal and external rotation values, compared to baseline and the control group, although no significant difference of scapular PNF was found in the control group in the study by Balci et al. [53].
Moreover, ROM values were improved comparatively to the baseline with high intensity laser therapy but no significant difference was demonstrated with the placebo group [51]. In contrast, Soliman et al. [46] found a significant group difference between low level laser therapy and reflexology.
Table 1
Grades of recommendation for outcome measures according to the level of evidence demonstrated in the reviewed studies
| Grades of recommendation for outcome measures in adhesive capsulitis | |||
|---|---|---|---|
| Pain | Range of motion | Functional status | |
| Extra corporeal shock wave therapy | Grade A | Grade A | Grade A |
| Stretching exercises | Grade A | Grade A | Grade A |
| Corticosteroid injections | Grade A | Grade A | Grade A |
| Laser therapy | Grade A | Grade A | Grade C |
| Bee venom acupuncture | Grade B | Grade B | Grade B |
| Cryotherapy | Grade B | Grade B | Grade B |
| Mobilization | Grade B | Grade B | Grade B |
| PNF technique | Grade B | Grade B | Grade B |
| Ultrasound therapy | Grade B | Grade B | Grade B |
| Continuous passive motion | Grade B | Grade B | Grade B |
| Strengthening of muscles | Grade B | Grade B | Grade B |
| Dynamic scapular recognition exercises | Grade B | Grade B | Grade B |
| Conventional physiotherapy | Grade B | Grade B | Grade B |
| Manual muscle release technique | Grade C | Grade C | – |
PNF
4.3Functional status
Functional status was assessed in almost all studies including all types of interventions, except for a few (Supplementary Table 3). All interventions had significantly improved the functional status scores compared to baseline parameters. Out of these, BVA, WBC, Mulligan mobilization technique, ESWT, SPS device, posterior capsular stretching along with scapular mobilization, continuous passive motion, rotator cuff strengthening, dynamic scapular recognition exercises, lidocaine injection with physiotherapy, SSNB with physiotherapy, UST, stretching exercises, and group exercise classes with physiotherapy were found to have a significant difference in the functional scores compared to their control groups.
When mobilization techniques are considered, Maitland mobilization did not improve functional scores significantly compared to the exercise group alone [48]. In contrast, a study that compared mobilization with stretching exhibited greater functional status scores than the stretching group after treatment and also at one year follow up [1]. Similarly, Espinoza et al. [49] and Kouser et al. [58] indicated greater functional scores for the glenohumeral joint posterior mobilization and end range mobilization than the conventional physiotherapy as short term effects. Furthermore, IAD followed by physical therapy was found to be beneficial in terms of upper extremity function in comparison to IAD preceded by physical therapy [64]. Grades of recommendations are provided for each outcome measure according to the levels of evidence demonstrated in the reviewed studies (Table 1).
Considering the limitations, most of the studies failed to use a sufficient number of patients per group, with 24 patients being the average. This is problematic for generalizing the results to a large population and also to make stronger conclusions. Only some studies managed to avoid contamination and cross-interventions. Moreover, double blinding was performed only in a few studies. The majority of the studies were single blind. In terms of physical therapy interventions, it is not always possible to implement double blinding. Most of the studies used the blinding of the outcome assessor to reduce the detection bias. A few studies failed to indicate the duration of the patients’ symptoms and it is thus difficult to know the stage of the disease (i.e. 1, 2 or 3). Most of the studies failed to perform a long term follow up leading to poor conclusions. The control groups in the studies had additional interventional approaches other than the placebo treatment due to ethical issues. This might lead to uncertainty about the efficacy of one treatment method over another. Although the improvement of these outcome measures could be partially due to the spontaneous recovery [69], it is shown that none of the patients with adhesive capsulitis demonstrated spontaneous recovery [15]. This emphasizes the importance of having long term follow ups to establish long term effects. Furthermore it would be better to have in-between follow ups to make continuous decisions regarding the efficacy of the treatment over the treatment period. Due to the variability of the measurements including tools and assessment methods, the efficacy of a single treatment method or a combination of treatments cannot be recommended. Instead, the efficacy of each interventional strategy towards the improvement of outcome measures can be discussed.
5.Limitations and future directions
In this study only four databases (PubMed, Science Direct, Cochrane databases and PEDro) were searched for articles published in English. In addition, the heterogeneity of the populations and the outcome measures used in the reviewed studies did not allow us to directly compare the results between the studies. Future studies should recruit subjects stratified according to the duration of illness, severity of the illness and other confounding variables. The findings of this review highlight the need of more prospective randomized controlled studies which incorporate large sample sizes (i.e. more than 30 subjects per group), long term follow ups (i.e. at least six months) and universally accepted valid and reliable outcome measures such as ASES, DASH and SPADI to study the efficacy of the treatment methods in patients with adhesive capsulitis.
6.Conclusion
ESWT, stretching exercises and corticosteroid injections along with physical therapy techniques and modalities can be strongly recommended to improve the pain levels, range of motion and functional status of patients with stage 2 and 3 adhesive capsulitis. Laser therapy along with other conservative therapies are strongly recommended for pain relief and to increase the range of motion, despite mild evidence that supports the improvement of the functional status in stage 2 patients. The manual muscle release technique has mild evidence in terms of the relief of pain and improvement in range of motion where its efficacy in terms of functional status was not assessed in this study. All the other interventions including BVA, WBC, mobilization, PNF techniques, UST, continuous passive motion, strengthening exercises, dynamic scapular recognition exercises combined with conventional physical therapy techniques and conventional physical therapy techniques alone are presented with moderate evidence in terms of the pain relief, improvement of ROM and functional status of patients with stage 2 and 3 adhesive capsulitis. Almost all studies evaluated the efficacy of the combination of treatment approaches despite a single treatment. The interventions with mild to moderate evidence should be further examined with high methodological qualities, large sample sizes and long term follow ups in order to make strong conclusions in terms of their efficacy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supplementary files
The supplementary files are available from https://dx. doi.org/10.3233/BMR-200186.
Conflict of interest
The authors report no conflicts of interest.
References
[1] | Çelik D, Kaya Mutlu E. Does adding mobilization to stretching improve outcomes for people with frozen shoulder? A randomized controlled clinical trial. Clin Rehabil. (2016) ; 30: : 786–794. doi: 10.1177/0269215515597294. |
[2] | Segmüller HE, Taylor DE, Hogan CS, Saies AD, Hayes MG. Arthroscopic treatment of adhesive capsulitis. J Shoulder Elbow Surg. (1995) ; 4: : 403–408. doi: 10.1016/S1058-2746(05)80030-8. |
[3] | Codman E. Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. The shoulder. Boston, MA: Thomas Todd; (1934) . |
[4] | Neviaser JS. Adhesive capsulitis of the shoulder: a study of the pathological findings in periarthritis of the shoulder. JBJS. (1945) ; 27: : 211–222. |
[5] | Mao CY, Jaw WC, Cheng HC. Frozen shoulder: correlation between the response to physical therapy and follow-up shoulder arthrography. Arch Phys Med Rehabil. (1997) ; 78: : 857–859. doi: 10.1016/s0003-9993(97)90200-8. |
[6] | Wolin PM, Ingraffia-Welp A, Moreyra CE, Hutton WC. High-intensity stretch treatment for severe postoperative adhesive capsulitis of the shoulder. Ann Phys Rehabil Med. (2016) ; 59: : 242–247. doi: 10.1016/j.rehab.2016.04.010. |
[7] | Kelley MJ, Shaffer MA, Kuhn E, Michener LA, Seitz AL, Uhl TL, et al. Shoulder pain and mobility deficits: adhesive capsulitis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the american physical therapy association. J Orthop Sports PhysTher. (2013) ; 43: : A1–A31. doi: 10.2519/jospt.2013.0302. |
[8] | Warner JJ. Frozen shoulder: diagnosis and management. J Am AcadOrthop Surg. (1997) ; 5: : 130–140. doi: 10.5435/00124635-199705000-00002. |
[9] | Baslund B, Thomsen BS, Jensen EM. Frozen shoulder: current concepts. Scand J Rheumatol. (1990) ; 19: : 321–325. doi: 10.3109/03009749009096786. |
[10] | Laubscher PH, Rösch TG. Frozen shoulder: a review. SA Orthopaedic Journal. (2009) ; 8: : 24–29. |
[11] | Tasto JP, Elias DW. Adhesive capsulitis. Sports Med Arthrosc Rev. (2007) ; 15: : 216–221. doi: 10.1097/JSA.0b013e3181595c22. |
[12] | Zuckerman JD, Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. (2011) ; 20: : 322–325. doi: 10.1016/j.jse.2010.07.008. |
[13] | Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis: a prospective functional outcome study of nonoperative treatment. JBJS. (2000) ; 82: : 1398–1407. |
[14] | Loew M, Heichel TO, Lehner, B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. (2005) ; 14: : 16–21. doi: 10.1016/j.jse.2004.04.004. |
[15] | Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. JBJS. (1992) ; 74: : 738–746. |
[16] | Ranalletta M, Rossi LA, Bongiovanni SL, Tanoira I, Elizondo CM, Maignon GD. Corticosteroid injections accelerate pain relief and recovery of function compared with oral NSAIDs in patients with adhesive capsulitis: a randomized controlled trial. Am J Sports Med. (2016) ; 44: : 474–481. doi: 10.1177/0363546515616238. |
[17] | Shin SJ, Lee SY. Efficacies of corticosteroid injection at different sites of the shoulder for the treatment of adhesive capsulitis. J Shoulder Elbow Surg. (2013) ; 22: : 521–527. doi: 10.1016/j.jse.2012.06.015. |
[18] | Wang W, Shi M, Zhou C, Shi Z, Cai X, Lin T, et al. Effectiveness of corticosteroid injections in adhesive capsulitis of shoulder: a meta-analysis. Medicine. (2017) ; 96.e7529. doi: 10.1097/MD.0000000000007529. |
[19] | Koh KH. Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials. Singapore Med J. (2016) ; 57: : 646. doi: 10.11622/smedj.2016146. |
[20] | Roh YH, Yi SR, Noh JH, Lee SY, Oh JH, Gong HS, et al. Intra-articular corticosteroid injection in diabetic patients with adhesive capsulitis: a randomized controlled trial. Knee Surg Sports TraumatolArthrosc. (2012) ; 20: : 1947–1952. doi: 10.1007/s00167-011-1776-6. |
[21] | Dehghan A, Pishgooei N, Salami MA, Nafisi-moghadam R, Rahimpour S, Soleimani H, et al. Comparison between NSAID and intra-articular corticosteroid injection in frozen shoulder of diabetic patients; a randomized clinical trial. ExpClinEndocrinol Diabetes. (2013) ; 121: : 75–79. doi: 10.1055/s-0032-1333278. |
[22] | Buchbinder R, Hoving JL, Green S, Hall S, Forbes A, Nash P. Short course prednisolone for adhesive capsulitis (frozen shoulder or stiff painful shoulder): a randomised, double blind, placebo controlled trial. Ann Rheum Dis. (2004) ; 63: : 1460–1469. doi: 10.1136/ard.2003.018218. |
[23] | Dogru H, Basaran S, Sarpel T. Effectiveness of therapeutic ultrasound in adhesive capsulitis. Joint Bone Spine. (2008) ; 75: : 445–450. doi: 10.1016/j.jbspin.2007.07.016. |
[24] | Leung MS, Cheing GL. Effects of deep and superficial heating in the management of frozen shoulder. J Rehabil Med. (2008) ; 40: : 145–150. doi: 10.2340/16501977-0146. |
[25] | Robertson VJ, Ward AR, Jung P. The effect of heat on tissue extensibility: a comparison of deep and superficial heating. Arch Phys Med Rehabil. (2005) ; 86: : 819–825. doi: 10.1016/j.apmr.2004.07.353. |
[26] | Page MJ, Green S, Kramer S, Johnston RV, McBain B, Buchbinder R. Electrotherapy modalities for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews 2014 (10). doi: 10.1002/14651858.CD011324. |
[27] | Çelik D, Türkel N. Comparison of matrix rhythm therapy and stretching exercises on frozen shoulder: randomised controlled trial. Fizyoterapi Rehabilitasyon. (2016) ; 27: : 81–88. |
[28] | Ibrahim M, Donatelli R, Hellman M, Echternach J. Efficacy of a static progressive stretch device as an adjunct to physical therapy in treating adhesive capsulitis of the shoulder: a prospective, randomised study. Physiotherapy. (2014) ; 100: : 228–234. |
[29] | Deshmukh SS, Salian SC, Yardi S. A comparative study to assess the effectiveness of soft tissue mobilization preceding joint mobilization technique in the management of adhesive capsulitis. Indian J Physiother Occup Ther. (2014) ; 8: : 93. |
[30] | Hussein ZA. Efficacy of mobilization techniques and range of motion in patients with adhesive capsulitis of the shoulder pain. International Journal of Research in Pharmaceutical Sciences. (2019) ; 10: : 313–317. |
[31] | Chen JF, Ginn KA, Herbert RD. Passive mobilisation of shoulder region joints plus advice and exercise does not reduce pain and disability more than advice and exercise alone: a randomised trial. Aust J Physiother. (2009) ; 55: : 17–23. |
[32] | Hemant PN, Suhas MB, Anil MA. Restoration of normal length of upper trapezius and levator scapulae in subjects with adhesive capsulitis. Indian J Physiother Occup Ther. (2013) ; 7: : 141. |
[33] | Kumar A. A comparative study on the efficacy of maitland’s mobilization and muscle energy technique on frozen shoulder. Indian J Physiother Occup Ther. (2015) ; 9: : 39–43. doi: 10.5958/0973-5674.2015.00143.4. |
[34] | Contractor ES, Agnihotri DS, Patel RM. Effect of spencer muscle energy technique on pain and functional disability in cases of adhesive capsulitis of shoulder joint. IAIM. (2016) ; 3: : 126–131.c. |
[35] | Jain TK, Sharma NK. The effectiveness of physiotherapeutic interventions in treatment of frozen shoulder/adhesive capsulitis: a systematic review. J Back Musculoskeletal Rehabil. (2014) ; 27: : 247–273. |
[36] | Mortenson PA, Eng JJ. The use of casts in the management of joint mobility and hypertonia following brain injury in adults: a systematic review. Phys Ther. (2003) ; 83: : 648–658. |
[37] | Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. (1989) ; 95: : 2S–4S. |
[38] | Butler C, Campbell S. Evidence of the effects of intrathecal baclofen for spastic and dystonic cerebral palsy. Dev Med Child Neurol. (2000) ; 42: : 634–645. |
[39] | Koh PS, Seo BK, Cho NS, Park HS, Park DS, Baek YH. Clinical effectiveness of bee venom acupuncture and physiotherapy in the treatment of adhesive capsulitis: a randomized controlled trial. J Shoulder Elbow Surg. (2013) ; 22: : 1053–1062. |
[40] | Ma SY, Je HD, Jeong JH, Kim HY, Kim HD. Effects of whole-body cryotherapy in the management of adhesive capsulitis of the shoulder. Arch Phys Med Rehabil. (2013) ; 94: : 9–16. |
[41] | Doner G, Guven Z, Atalay A, Celiker R. Evaluation of mulligan’s technique for adhesive capsulitis of the shoulder. J Rehabil Med. (2013) ; 45: : 87–91. |
[42] | Chen CY, Hu CC, Weng PW, Huang YM, Chiang CJ, Chen CH, et al. Extracorporeal shockwave therapy improves short-term functional outcomes of shoulder adhesive capsulitis. J Shoulder Elbow Surg. (2014) ; 23: : 1843–1851. |
[43] | Paul A, Rajkumar JS, Peter S, Lambert L. Effectiveness of sustained stretching of the inferior capsule in the management of a frozen shoulder. Clin Orthop. (2014) ; 472: : 2262–2268. |
[44] | Vahdatpour B, Taheri P, Zade AZ, Moradian S. Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J of Prev Med. (2014) ; 5: : 875. |
[45] | Russell S, Jariwala A, Conlon R, Selfe J, Richards J, Walton M. A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J Shoulder Elbow Surg. (2014) ; 23: : 500–507. |
[46] | Soliman AS, Mahmoud AM, Serry ZM, Dawood FG. Therapeutic effects of low-level laser and reflexology on adhesive capsulitis in elderly type 2 diabetic patients. Asian J Pharm Clin Res. (2014) ; 7: : 317–321. |
[47] | Akbaş E, Güneri S, Tas S, Erdem EU, Yüksel İ. The effects of additional proprioceptive neuromuscular facilitation over conventional therapy in patients with adhesive capsulitis. Fizyoterapi Rehabilitasyon. (2015) ; 26: : 78–85. |
[48] | Ali SA, Khan M. Comparison for efficacy of general exercises with and without mobilization therapy for the management of adhesive capsulitis of shoulder-an interventional study. Pak J Med Sci. (2015) ; 31: : 1372. |
[49] | Espinoza HJG, Pavez F, Guajardo C, Acosta M. Glenohumeral posterior mobilization versus conventional physiotherapy for primary adhesive capsulitis: a randomized clinical trial. Medwave. (2015) ; 15: : e6267. |
[50] | Hsu WC, Wang TL, Lin YJ, Hsieh LF, Tsai CM, Huang KH. Addition of lidocaine injection immediately before physiotherapy for frozen shoulder: a randomized controlled trial. PloS one. (2015) ; 10. doi: 10.1371/journal.pone.0118217. |
[51] | Kim SH, Kim YH, Lee HR, Choi YE. Short-term effects of high-intensity laser therapy on frozen shoulder: a prospective randomized control study. Manual therapy. (2015) ; 20: : 751–757. |
[52] | Klç Z, Filiz MB, Çakr T, Toraman NF. Addition of suprascapular nerve block to a physical therapy program produces an extra benefit to adhesive capsulitis: a randomized controlled trial. Am J Phys Med Rehabil. (2015) ; 94: : 912–920. |
[53] | Balcı NC, Yuruk ZO, Zeybek A, Gulsen M, Tekindal MA. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis: a randomized controlled trial. J Phys. (2016) ; 28: : 1219–1227. |
[54] | Ekim AA, İnal EE, Gönüllü E, Hamarat H, Yorulmaz G, Mumcu G, et al. Continuous passive motion in adhesive capsulitis patients with diabetes mellitus: a randomized controlled trial. J Back Musculoskeletal Rehabil. (2016) ; 29: : 779–786. |
[55] | Elhafez HM, Elhafez SM. Axillary ultrasound and laser combined with postisometric facilitation in treatment of shoulder adhesive capsulitis: a randomized clinical trial. J Manipulative Physiol Ther. (2016) ; 39: : 330–338. |
[56] | Hussein AZ, Donatelli RA. The efficacy of radial extracorporeal shockwave therapy in shoulder adhesive capsulitis: a prospective, randomised, double-blind, placebo-controlled, clinical study. Eur J Physiother. (2016) ; 18: : 63–76. |
[57] | Ebadi S, Forogh B, Fallah E, Ghazani AB. Does ultrasound therapy add to the effects of exercise and mobilization in frozen shoulder? A pilot randomized double-blind clinical trial. J Bodyw Mov Ther. (2017) ; 21: : 781–787. |
[58] | Kouser F, Sajjad AG, Amanat S, Mehmood Q. Effects of kaltenborn mobilization in mid-range and end-range in patients with adhesive capsulitis. Rawal Medical Journal. (2017) ; 42: : 559–562. |
[59] | Rawat P, Eapen C, Seema KP. Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: a randomized controlled trial. J Hand Ther. (2017) ; 30: : 235–241. |
[60] | Robinson PM, Norris J, Roberts CP. Randomized controlled trial of supervised physiotherapy versus a home exercise program after hydrodilatation for the management of primary frozen shoulder. J Shoulder Elbow Surg. (2017) ; 26: : 757–765. |
[61] | Balci TO, Turk AC, Sahin F, Kotevoglu N, Kuran B. Efficacy of therapeutic ultrasound in treatment of adhesive capsulitis: a prospective double blind placebo-controlled randomized trial. J Back Musculoskeletal Rehabil. (2018) ; 31: : 955–961. |
[62] | AbdElhamed HB, Koura GM, Hamada HA, Mohamed YE, Abbas R. Effect of strengthening lower trapezius muscle on scapular tipping in patients with diabetic frozen shoulder: a randomized controlled study. Biomed Res. (2018) ; 29. |
[63] | Duzgun I, Turgut E, Eraslan L, Elbasan B, Oskay D, Atay OA. Which method for frozen shoulder mobilization: manual posterior capsule stretching or scapular mobilization? J Musculoskelet Neuronal Interact. (2019) ; 19: : 311–316. |
[64] | Jellad A, May W, Zrig A, Kalai A, Jguirim M, Frih ZBS, et al. Intra-articular distension preceded by physical therapy versus intra-articular distension followed by physical therapy for treating adhesive capsulitis of the shoulder. J Back Musculoskeletal Rehabil. [Preprint] (2019) ; 1–8. doi: 10.3233/BMR-181426. |
[65] | Mohamed AA, Jan YK, El Sayed WH, El Wanis MEA, Yamany AA. Dynamic scapular recognition exercise improves scapular upward rotation and shoulder pain and disability in patients with adhesive capsulitis: a randomized controlled trial. J Man Manip Ther. (2019) ; 1–13. doi: 10.1080/10669817.2019.1622896. |
[66] | Park YC, Koh PS, Seo BK, Lee JW, Cho NS, Park HS, et al. Long-term effectiveness of bee venom acupuncture and physiotherapy in the treatment of adhesive capsulitis: a one-year follow-up analysis of a previous randomized controlled trial. J Altern Complement Med. (2014) ; 20: : 919–924. |
[67] | Ip D, Fu NY. Two-year follow-up of low-level laser therapy for elderly with painful adhesive capsulitis of the shoulder. J pain Res. (2015) ; 8: : 247. |
[68] | Shih YF, Liao PW, Lee CS. The immediate effect of muscle release intervention on muscle activity and shoulder kinematics in patients with frozen shoulder: a cross-sectional, exploratory study. BMC Musculoskelet Disord. (2017) ; 18: : 499. |
[69] | Anton HA. Frozen shoulder. Can Fam Physician. (1993) ; 39: : 1773–1777. |




