Comparative efficacy of 12 non-drug interventions on non-specific chronic low back pain in nurses: A systematic review and network meta-analysis
Abstract
BACKGROUND:
Many non-drug interventions for decreasing non-specific chronic low back pain (NSCLBP) in nurses have been extensively studied, but the most effective approach is still unclear.
OBJECTIVE:
This systematic review and network meta-analysis evaluated the efficacies of 12 non-drug interventions in reducing NSCLBP in nurses.
METHODS:
PubMed, ScienceDirect, Web of Science, Cochrane, EMBASE, CINAHL, Medline, WANFANG, VIP, China Knowledge Integrated, and SinoMed were searched from their establishment to July 2019. Randomized controlled trials (RCTs) comparing non-drug interventions for NSCLBP in nurses were included and analyzed using Stata v15 statistical software.
RESULTS:
A total of 31 RCTs (
CONCLUSIONS:
Low back exercise plus health education may be the best approach to reduce NSCLBP in nurses. Considering the heterogeneity, our findings need to be confirmed in future multicenter large sample RCTs in different countries.
1.Introduction
Non-specific chronic low back pain (NSCLBP) is characterized by muscle stiffness, tension, or pain localized between the gluteal folds and the costal margin, with or without referred leg pain, without a specific somatic origin, and lasting more than 12 weeks [1]. With the development and application of diagnostic and therapeutic technologies and growing aging populations in many countries, the number of critically ill patients treated by nurses has increased, creating an environment where many physical, chemical, ergonomic, and other harmful factors coexist [2, 3]. NSCLBP in nurses is a major health problem with an increasing incidence worldwide. The incidence in this population is reported to be 60.98%–72% [4, 5, 6] and has resulted in frequent nursing staff resignations and absences due to ill health [7, 8]. NSCLBP in nurses can lead to significantly reduced quality of life [9] and is detrimental to the development of the nursing team and patient safety.
NSCLBP in nurses has similarities with low back pain of the general population, but also has certain particularities. Firstly, the reasons for NSCLBP among nurses differ somewhat from groups in other occupations; the working environment involves a heavy workload and high technical requirements, especially for nurses working in emergency wards and intensive care units. NSCLBP in nurses is often caused by specific occupational reasons such as assisting patients turn over, performing catheterization, or introducing a central venous catheter (CVC) [10]. Secondly, some non-drug interventions are specifically aimed at nurses, such as ergonomics training, unstable shoes, and assistive tools for transferring patients [11]. Better management and treatment of NSCLBP for nurses is important, particularly as drug treatments can cause gastrointestinal and cardiovascular system damage, and there is currently no effective surgcal treatment [1].
Many studies have shown that NSCLBP can be relieved by many types of non-drug interventions, such as yoga, low back exercise, physical exercise, multidisciplinary intervention, cognitive behavioral therapy, and health education [12, 13, 14]. However, the optimal choice is still unclear, which raises some challenges for nurses to manage NSCLBP with non-drug interventions. Due to the complications of broad non-drug interventions and the lack of head-to-head randomized controlled trials (RCTs), it is impossible to identify the most effective intervention in nurses with NSCLBP using traditional meta-analysis methods. To our knowledge, no network meta-analysis has compared the effects of 12 non-drug interventions on nurses with NSCLBP.
Considering this existing research gap, a systematic review of the literature and a network meta-analysis by direct and indirect comparison were conducted. The aim of this review was to compare the effects of 12 non-drug interventions for NSCLBP in nurses, so as to provide a scientific basis for nurses to choose more appropriate non-drug interventions for NSCLBP.
2.Data and methods
2.1Data sources and searches
PubMed, ScienceDirect, Web of Science, Cochrane Library, EMBASE, CINAHL, Medline, WANFANG, VIP Database, China Knowledge Integrated Database, and SinoMed were searched. The retrieval time spanned from database establishment to July 2019. Key search terms included “nurse/nurses/nursing*/clinical nurse/ personnel, nursing/nursing personnel/registered nurses/ nurse, registered/nurses, registered/registered nurse” AND “low back pain /lower back pain/back pain/ non-specific low back pain/*low back pain/low * pain/Back Pain, Low/Back Pains, Low/Low Back Pains/Pain, Low Back/Pains, Low Back/Lower Back Pain/Back Pain, Lower/Back Pains, Lower/Lower Back Pains/Pain, Lower Back/Pains, Lower Back” AND “randomized controlled*/*controlled.” The search strategy combined medical subject headings (MeSH) and free words with “AND,” “OR” the two logical operators. Studies were retrieved by computer and manual retrieval methods, and the search languages were Chinese and English.
2.2Inclusion and exclusion criteria
Inclusion criteria: (i) RCTs, (ii) Chinese or English language, (iii) nurses are the subject, clear inclusion criteria, (iv) reports the diagnostic criteria for NSCLBP, and (v) published in a peer-reviewed journal. Exclusion criteria: (i) unable to obtain the full text of the document; (ii) incomplete information, unclear, or in error; (iii) repeatedly published literature; (iv) non-RCT, or (v) drug intervention measures.
2.3Study selection and data extraction
Two researchers independently screened the literature according to the inclusion and exclusion criteria, extracted the data, and then evaluated study quality. In case of disagreement, further discussion was performed with a third reviewer to reach a mutual agreement. The extracted information included the first author, publication date, country, intervention, follow-up time, and outcome measurement. The data were extracted and cross-checked by the two researchers.
2.4Quality assessment
The Cochrane Collaboration tool [15] for RCT assessment was used by the two researchers to assess the risk of bias among the included studies. Disagreements between the reviewers were resolved through consensus or arbitration by a third-party researcher. This tool covered random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias. Each item was classified as having either a high, low, or unclear risk of bias.
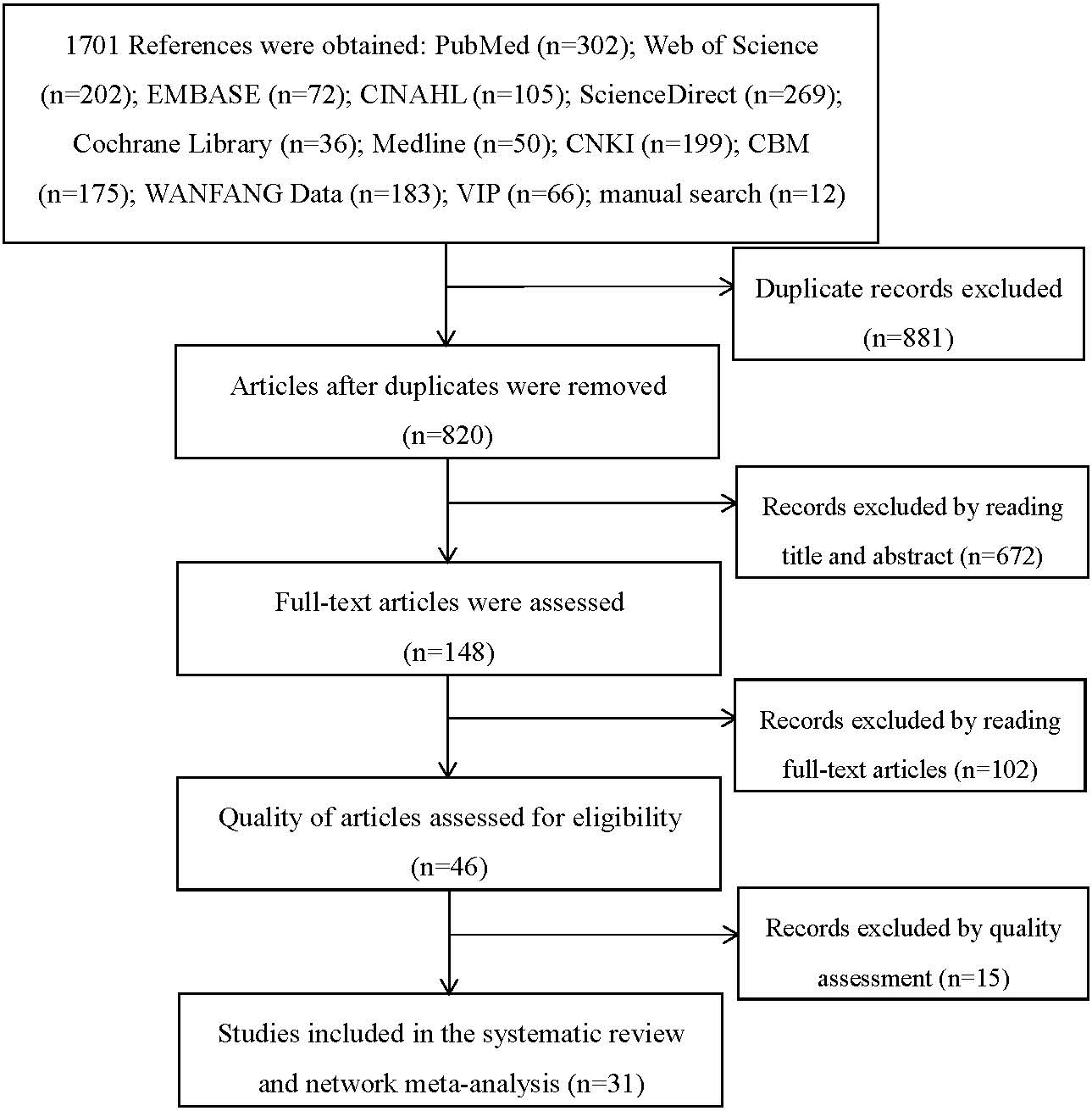
Figure 1.
Literature selection process and results.
2.5Interventions and outcome measurement
To facilitate network meta-analysis, non-drug interventions were divided into 12 types, excluding traditional Chinese medicine and western medicine, of which “none” was not included in the intervention measures. For statistical analysis, they were coded as follows:
A. Physical exercise: including stretching exercises and isokinetic exercises.
B. Physical exercise plus health education.
C. Health education: including ergonomics and mechanics knowledge training, consulting, and handling skills training.
D. Multidisciplinary intervention: the combination of health, education, physical exercise, and psychological intervention.
E. Manipulation treatment: including massage, acupuncture, and foot reflexology.
F. Manipulation treatment plus physical exercise.
G. None: including maintaining one’s lifestyle, simple lifestyle guide, and blank contrast.
H. Yoga.
I. Protective equipment: wearing orthopedic shoes and waist guards.
J. Low back exercise: including low back gymnastics, core stability training exercises, self-made low back gymnastics, and household low back gymnastics.
K. Low back exercise plus health education.
L. Self-management.
M. Self-management plus health education.
Table 1
Basic information used for the sample plots
| First author, year | Country | Year | Sample size | Intervention(I) | Follow- | Outcome | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Y1 | Y2 | Y3 | (n1/n2/n3) | I1 | I2 | I3 | up | measurement | ||
| Jie Yao, 2018 | China | 31.21 | 30.24 | – | 44/44/- | M | C | – | 6M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 7;(0pt, 0pt)circle (.5em) node 10;(0pt, 0pt)circle (.5em) node 11; |
| Xuebing Huang, 2018 | China | 31.21 | 30.24 | – | 11/11/- | M | C | – | 7M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 7;(0pt, 0pt)circle (.5em) node 10;(0pt, 0pt)circle (.5em) node 11; |
| Boqing Wang, 2016 | China | 32 | – | 17/17/- | J | G | 2M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 8; | ||
| Suzhai Tian, 2014 | China | 26.2 | 28.65 | – | 55/52/- | K | C | – | 6M | (0pt, 0pt)circle (.5em) node 2; |
| Jingjing Ji, 2019 | China | 27.00 | 28.00 | 20/20/- | H | G | – | 3M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3; | |
| Xiaojuan Guo, 2016 | China | 32.45 | 33.25 | – | 40/40/- | H | G | - | 3M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3;(0pt, 0pt)circle (.5em) node 7; |
| Weiwei Li, 2017 | China | – | – | – | 25/25/- | H | G | – | 2M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 8; |
| Lishi Yin, 2014 | China | – | – | – | 20/20/- | G | J | – | 6W | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 7;(0pt, 0pt)circle (.5em) node 8; |
| Ke Ma, 2016 | China | 32.1 | 31.4 | – | 38/38/- | K | C | – | 12M | (0pt, 0pt)circle (.5em) node 9;(0pt, 0pt)circle (.5em) node 13;(0pt, 0pt)circle (.5em) node 15; |
| Yu Wang, 2016 | China | 32.6 | 34.5 | 33.2 | 18/19/19 | E | A | F | 1W | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 13; |
| Shenghua Hu, 2014 | China | 28.4 | 27.96 | – | 30/30/- | J | G | – | 3W | (0pt, 0pt)circle (.5em) node 8;(0pt, 0pt)circle (.5em) node 13; |
| Chaomei Mo, 2019 | China | 29.4 | 29.1 | – | 35/35/- | I | J | – | 6M | (0pt, 0pt)circle (.5em) node 1;(0pt, 0pt)circle (.5em) node 8; |
| Yingxia Wen, 2016 | China | 35.52 | 35.38 | – | 40/40/- | C | D | – | 6M | (0pt, 0pt)circle (.5em) node 13; |
| Leila Ghadyani, 2016 | Iran | – | – | – | 66/70/- | D | C | – | 3M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3;(0pt, 0pt)circle (.5em) node 16; |
| Pardis | ||||||||||
| Noormohammadpour, 2018 | Iran | 43.3 | 41.3 | – | 10/10/- | H | G | – | 8W | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3;(0pt, 0pt)circle (.5em) node 7; |
| Hiroyuki Oka, 2018 | Japan | 35.1 | 35.5 | 35.5 | 1548/1430/ 1799 | G | C | B | 6W | (0pt, 0pt)circle (.5em) node 4;(0pt, 0pt)circle (.5em) node 18; |
| Maryam Movahedi, 2017 | Iran | 37.0 | 36.5 | – | 25/25/- | E | G | – | 4W | (0pt, 0pt)circle (.5em) node 22; |
| Thomas Ewert, 2009 | Germany | 37.9 | 41.1 | – | 92/91/- | D | A | – | 12M | (0pt, 0pt)circle (.5em) node 4;(0pt, 0pt)circle (.5em) node 7; |
| Eva Horneij, 2001 | Sweden | 43 | 45 | 44 | 16/17/28 | A | L | G | 12M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 13; |
| Mehdi Pakbaz, 2019 | Iran | 38.9 | 38.1 | – | 32/32/- | A | G | – | 2M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3; |
| Leila Ghadyani, 2017 | Iran | – | – | – | 66/70/- | D | C | – | 6M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3;(0pt, 0pt)circle (.5em) node 16; |
| Huei-Mein Chen, 2014 | Taiwan | 30.67 | 44.7 | – | 11/13/- | A | G | – | 6M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 17; |
| Edgar R Vieira, 2015 | USA | 34 | 31 | – | 10/10/- | I | G | – | 1.5M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 9; |
| Melinda Járomi, 2017 | Hungary | 41.7 | 41.1 | – | 67/70/- | C | E | – | 3M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 5; |
| Jaana Helena Suni, 2018 | Finland | Y1:45.1 | Y3:46.4 | – | N1:35/n2:40/ n3:31/n4:42 | I1:B / I2:A | I3:C/ I4:G | – | 12M | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 4;(0pt, 0pt)circle (.5em) node 7; |
| Naser Sharafkhani, 2015 | Iran | – | – | – | 48/50/- | D | G | – | 3M | (0pt, 0pt)circle (.5em) node 16; |
| Stéphane Armand, 2014 | Switzerland | 44.5 | 46.8 | – | 19/16/- | I | G | – | 6W | (0pt, 0pt)circle (.5em) node 2;(0pt, 0pt)circle (.5em) node 3; |
| Jamie Gannon, 2019 | USA | 53.3 | 62.4 | – | 31/31/- | D | C | – | 2M | (0pt, 0pt)circle (.5em) node 6;(0pt, 0pt)circle (.5em) node 3; |
| Lone Donbaek Jensen, 2006 | Denmark | 44.0 | 44.6 | 44.6 | 61/53/49 | C | L | G | 12M | (0pt, 0pt)circle (.5em) node 6; |
| Nitin J Patil, 2018 | India | 31.45 | 32.75 | – | 44/44/- | H | A | – | 6W | (0pt, 0pt)circle (.5em) node 14; |
| Melinda Jaromi, 2018 | Hungary | 32.3 | 31.5 | – | 56/55- | C | E | – | 6W | (0pt, 0pt)circle (.5em) node 2; |
Note: (0pt, 0pt)circle (.5em) node 1; faces pain scale, FPS; (0pt, 0pt)circle (.5em) node 2; verbal rating scale, VAS; (0pt, 0pt)circle (.5em) node 3; Roland Morris Disability Questionnaire, RMDQ; (0pt, 0pt)circle (.5em) node 4; fear avoidance beliefs, FAB; (0pt, 0pt)circle (.5em) node 5; the thickness of the muscle; (0pt, 0pt)circle (.5em) node 6; numerical rating scale, NRS; (0pt, 0pt)circle (.5em) node 7; SF-36 questionnaire; (0pt, 0pt)circle (.5em) node 8; Japanese Orthopaedic Association, JOA scores; (0pt, 0pt)circle (.5em) node 9; Oswestry disability index, ODI; (0pt, 0pt)circle (.5em) node 10; self-rating depression scale, SDS; (0pt, 0pt)circle (.5em) node 11; self-rating anxiety scale, SAS; (0pt, 0pt)circle (.5em) node 12; feeling of fatigue; (0pt, 0pt)circle (.5em) node 13; frequency of low back pain; (0pt, 0pt)circle (.5em) node 14;World Health Organization Quality of Life-brief questionnaire, WHOQOL-BREF; (0pt, 0pt)circle (.5em) node 15; Job satisfaction; (0pt, 0pt)circle (.5em) node 16; preventive behavior score; (0pt, 0pt)circle (.5em) node 17; self-efficacy; (0pt, 0pt)circle (.5em) node 18; occurrence rate. A: Physical exercise; B: Physical exercise plus health education; C: Health education; D: Multidisciplinary intervention; E: Manipulation treatment; F: Manipulation treatment plus physical exercise; G: None; H: Yoga; I: Protective equipment; J: Low back exercise; K: Low back exercise plus health education; L: Self-management; M: Self-management plus health education.
The main outcome was pain score measured by the numerical rating scale (NRS), visual analog scale (VAS), and facial expression pain scale (EPS). Secondary outcomes included back dysfunction, frequency of NSCLBP episodes, preventive behavior scores, and fear avoidance beliefs.
2.6Data synthesis and analysis
Stata 15 (Stata Statistical Software, Release 15, College Station, TX, USA) was used for network meta-analyses. The standardized mean difference (SMD) and 95% confidence interval (CI) were used to assess the effect. The random effects model was used for estimation, and an evidence network graph of the comparison of different treatment measures was drawn. A comparison-adjusted funnel plot was utilized to test the small-study effect, including publication bias. If the network formed a closed loop, used inconsistency factors, and 95% CI was used to evaluate the consistency of the closed-loop, the 95% CI contained 0 for more optimal consistency. If the network was not a closed loop, the node split method was used to evaluate network consistency.
If the difference between direct and indirect comparisons was not significant (
3.Results
3.1Included studies
In total, 1701 studies were retrieved, of which 881 duplicates were removed. There were 774 articles that were excluded after reading the title, abstract, and main text, and 15 documents were removed after quality assessment, leaving 31 studies that were included. Figure 1 displays the process of the filtering strategy.
3.2Characteristics of the included studies
We included 31 RCTs, of which 4 were three-arm trials and 1 was a four-arm trial. A total of 7116 nurses were included. There were 13 studies from China [12, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27], 6 from Iran [13, 14, 28, 29, 30, 31], 2 from the USA [32, 33], and 2 from Hungary [34, 35]. One study originated from each of the following countries: Japan [35], Germany [36], Sweden [37], Taiwan [38], Finland [39], Switzerland [40], Denmark [41], and India [42]. The basic information used for the sample plots is shown in Table 1.
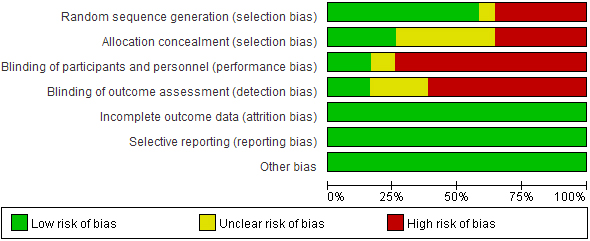
A decrease in NSCLBP intensity in nurses after 12 non-drug interventions was reported in 22 studies. Figure 2 shows the network plots detailing the treatment comparisons for 12 non-drug interventions for NSCLBP; the network diagram shows that the inclusion of physical exercise and health education was more frequent. The risk of bias of the included studies is shown in Fig. 3.
Figure 2.
Network map for the comparison of different interventions. The size of the node corresponds to the number of individual studies on the interventions. The directly compared interventions are linked with a line, the thickness of which corresponds to the number of studies that assessed the comparison. A: Physical exercise; B: Physical exercise plus health education; C: Health education; D: Multidisciplinary intervention; E: Manipulation treatment; F: Manipulation treatment plus physical exercise; G: None; H: Yoga; I: Protective equipment; J: Low back exercise; K: Low back exercise plus health education; L: Self-management; M: Self-management plus health education.
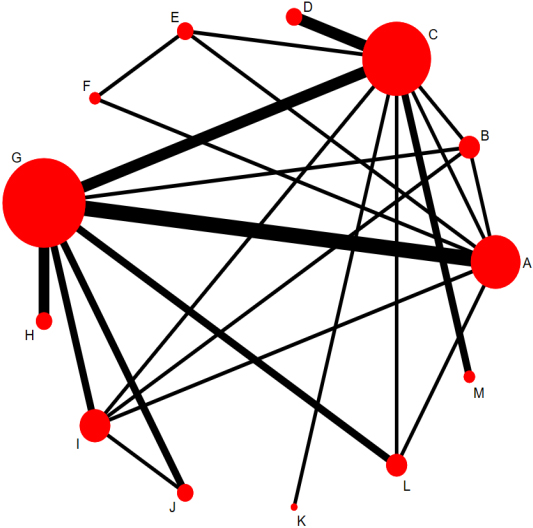
Figure 3.
Risk of inclusion bias.
3.3Network meta-analysis results
The SMDs and 95% CIs of 12 non-drug interventions for NSCLBP are reported in Table 2. The interventions with the greatest SUCRAs were low back exercise plus healthy education, low back exercise, and yoga (SUCRA: 79.4%, 76.2%, and 75.1%, respectively). Figure 4 shows the cumulative probability.
3.4Systematic review results
Three studies [28, 30, 33] reported that a more optimal effect on lumbar dysfunction was obtained with multidisciplinary intervention rather than simple health education. Two studies [14, 19] reported that yoga decreased lumbar and back dysfunction. Two studies [32, 40] reported that protective equipment decreased dysfunction of the small of the back, and only one study [13] reported that physical exercise improved function of the back dysfunction. Three articles [28, 30, 31] reported that health education improved the nurse NSCLBP
Table 2
League tables showing 12 non-drug interventions for NSCLBP
| M: Self-management plus health education | L: Self- management | K: Low back exercise plus health education | J: Low back exercise | I: Protective equipment | H: Yoga | G: None | F: Manipulation treatment plus physical exercise | E: Manipulation treatment | D: Multidisciplinary intervention | C: Health education | B: Physical exercise plus health education | A: Physical exercise | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M: Self-management plus health education | M | 1.10 ( | 0.25( | 0.09( | 1.36( | 0.42( | 0.46( | 0.77( | 4.31(1.37,7.25) | ||||
| L: Self-management | L | 0.26( | 0.58( | ||||||||||
| K: Low back exercise plus health education | 1.36( | 2.46( | K | 1.60( | 1.45( | 1.28( | 2.72( | 1.78( | 1.82( | 2.13( | |||
| J: Low back exercise | 4.46(0.80,8.12) | 5.56(1.48,9.64) | 3.11( | J | 4.71(1.50,7.91) | 0.83( | 4.55(2.56,6.54) | 4.38(0.31,8.46) | 5.82(1.75,9.90) | 4.88(1.38,8.38) | 4.92(1.73,8.12) | 5.23(2.04,8.42) | |
| I: Protective equipment | 0.86( | I | 1.12( | 0.17( | 0.22( | 0.52( | |||||||
| H: Yoga | 3.63(0.18,7.09) | 4.74(0.85,8.63) | 2.28( | 3.88(0.92,6.84) | H | 3.73(2.16,5.30) | 3.56( | 5.00(1.11,8.89) | 4.06(0.78,7.33) | 4.10(1.15,7.04) | 4.40(1.46,7.35) | ||
| G: None | 1.01( | 0.15( | G | 1.27( | 0.33( | 0.37( | 0.68( | 0.75( | |||||
| F: Manipulation treatment plus physical exercise | 0.08( | 1.18( | 0.32( | 0.17( | F | 1.44( | 0.50( | 0.54( | 0.85( | ||||
| E: Manipulation treatment | E | ||||||||||||
| D: Multidisciplinary intervention | 0.68( | 0.94( | D | 0.04( | 0.35( | 0.26( | |||||||
| C: Health education | 0.64( | 0.90( | C | 0.31( | 0.21( | ||||||||
| B: Physical exercise plus health education | 0.33( | 0.59( | B | ||||||||||
| A: Physical exercise | 0.41( | 5.55(1.98,9.12) | 0.40( | 1.24( | 0.69( | 6.82(2.36,11.28) | 0.09 ( | A |
Note: SMD (95% CI) for the column intervention versus the row intervention are shown above the diagonal. Note: The outcome was pain score. SMD
Figure 4.
Cumulative probability of decreasing NSCLBP in nurses with 12 non-drug interventions. Ranking indicates the probability of being the most optimal treatment, the second best, the third best, and so on, among the 12 non-drug interventions.A: Physical exercise; B: Physical exercise plus health education; C: Health education; D: Multidisciplinary intervention; E: Manipulation treatment; F: Manipulation treatment plus physical exercise; G: None; H: Yoga; I: Protective equipment; J: Low back exercise; K: Low back exercise plus health education; L: Self-management; M: Self-management plus health education.
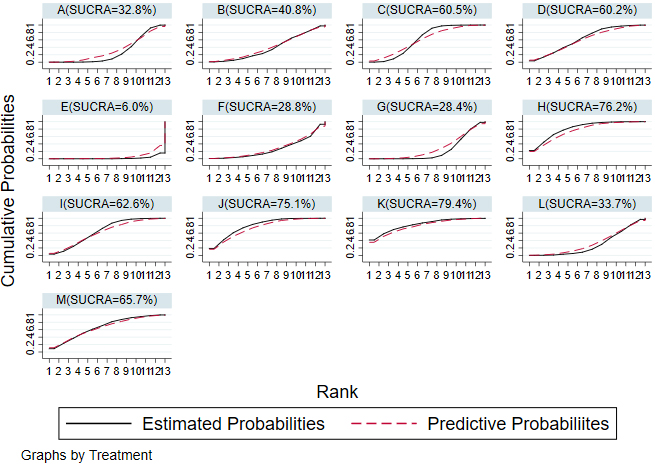
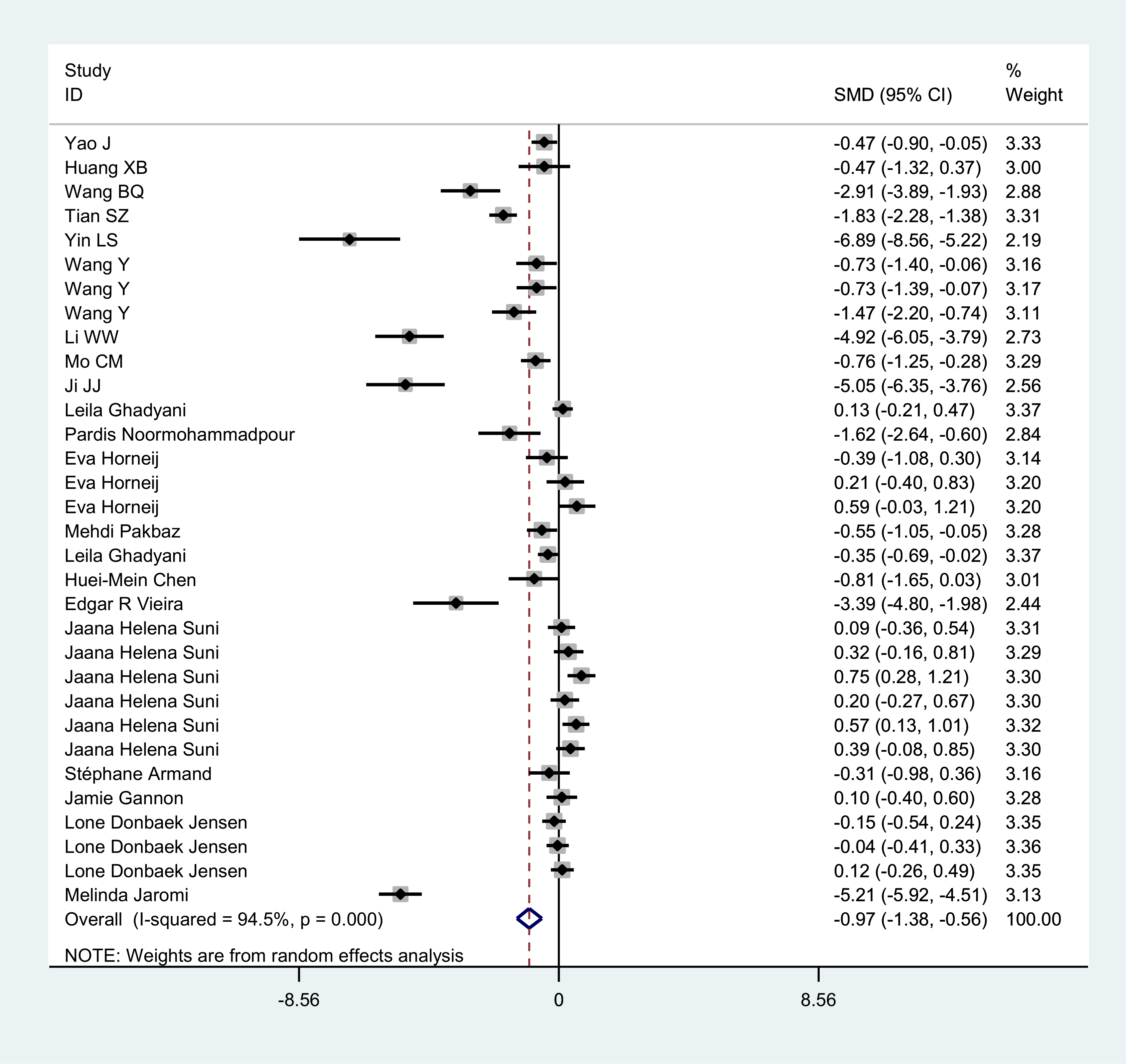
Figure 5.
Forest plot of comparison: non-drug interventions versus control.
prevention behavior score, and there were five
Figure 6.
Sensitivity analysis.
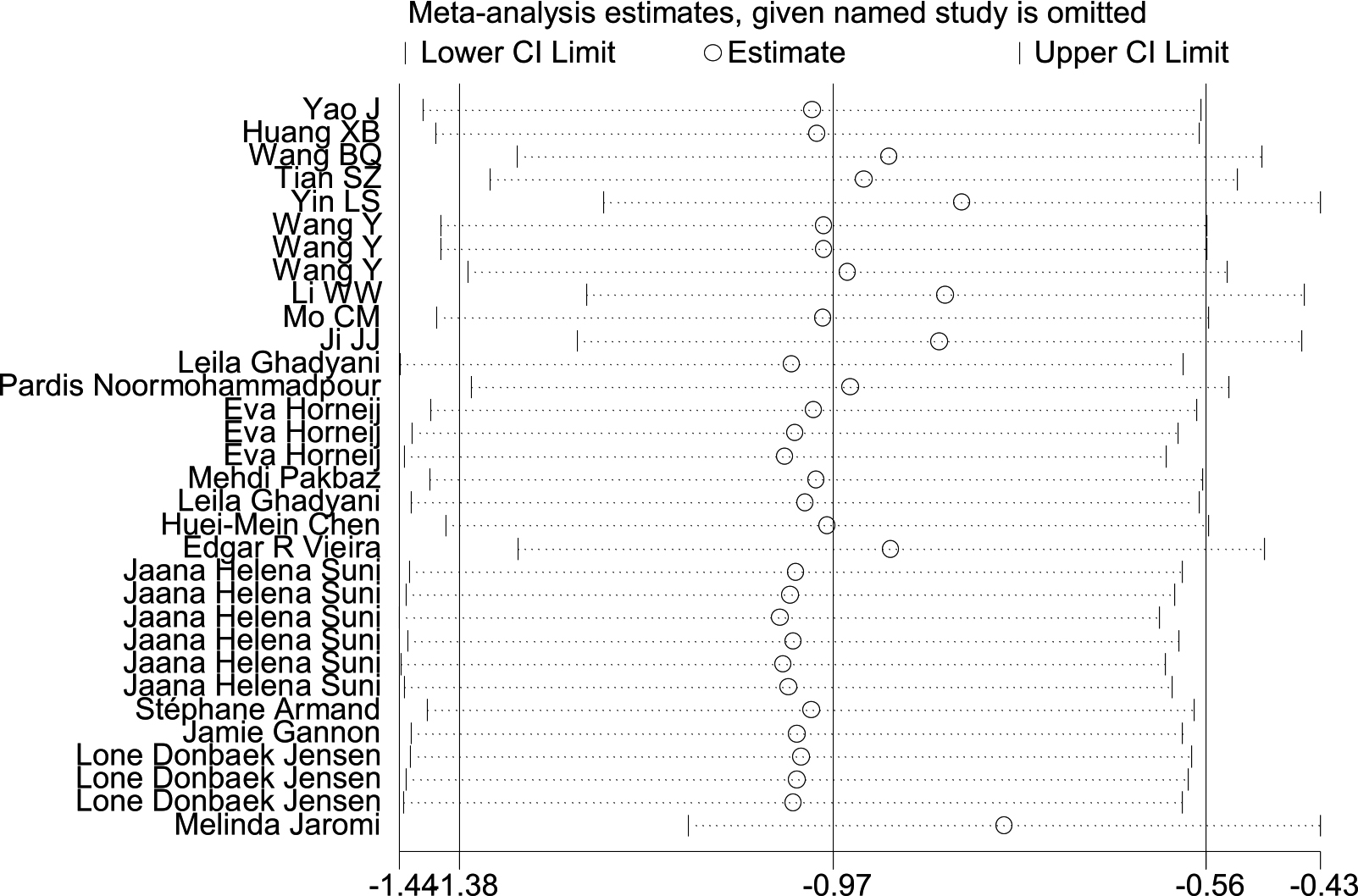
3.5Heterogeneity test
When we combined all the included studies, the pain score of the intervention group was significantly lower than that of the control group (SMD
4.Discussion
Given the high prevalence of NSCLBP in nurses, there is an urgent need to determine the efficacies of non-drug interventions. The rank probability showed that low back exercises plus health education was most likely to be ranked first (SUCRA: 79.4%), the second was single low back exercise (SUCRA: 76.2%), and the third was yoga (SUCRA:75.1%). Based on our network meta-analyses, low back exercises plus health education was the most effective intervention for NSCLBP management in nurses, followed by single low back exercise intervention and yoga.
Our results show that low back exercises plus health education may be the best intervention measures to decrease NSCLBP among nurses; a recent systematic review yielded similar results [44]. Huang et al. [45] also noted that exercises or exercises combined with education can prevent NSCLBP. The advantage of our research is the inclusion of a large number of interventions described in Chinese studies. This idea is supported by the cumulative probability showing that low back exercise plus health education have the highest probability of being the most optimal intervention to decrease nurse NSCLBP. There are several potential mechanisms that may underlie this effect. From the perspective of the causes of NSCLBP in nurses, it may be related to biomechanical imbalances [46]. For example, the process of turning a patient or assisting them to turn may require excessive and simultaneous bending and turning, subjecting the lumbar spine to shearing forces. This could induce intervertebral disc degeneration, which in turn leads to NSCLBP [47]. Health education for nurses such as mechanics, ergonomics, and reasonable posture training can effectively reduce their awkward postures and improve nurses’ knowledge of NSCLBP [48]. Secondly, from a physical point of view, some nursing operations including catheterization or introducing a CVC may damage the core muscles that maintain spine stability (including the rectus abdominis, abdominal obliques, back muscles, and other muscle groups). The waist muscles in particular are prone to fatigue, which will decrease the strength of the waist and weaken the stability of the core muscles to cause pain over time [49, 50]. Low back exercises use isotonic and isometric muscle contraction to restore the strength of the synergistic muscle groups and biomechanically balance the lumbar spine by enhancing the strength of the low back muscles, thereby improving or restoring the lumbar spine stability and reducing pain [51]. In addition, low back exercises can effectively train the muscles and decrease fatigue, increase abdominal muscle endurance, and expand the range of waist activities, thereby reducing the degree of NSCLBP [22]. Low back exercise is different and more targeted than physical exercise that is mostly stretching exercises, running, walking, and other body movements [38]. Health education stresses the advantages of low back exercises and nursing manipulation techniques used at work, thus increasing nurse compliance, which has synergistic effect with low back exercises and yields a greater pain improvement effect.
This study also confirmed that yoga may also be an important non-drug intervention to decrease nurse NSCLBP (SUCRA:75.1%), similar to the results of Feilong Zhu et al. [52]. There may be two reasons for this. First, from a physiological perspective, yoga can enhance muscle strength, low back stability, and spinal flexibility, thereby reducing NSCLBP [53]. This view was described in previous studies [54, 55]. Secondly, NSCLBP in nurses has a certain relationship with psychological factors such as anxiety and depression [56]. In addition to reducing low back muscle tension, yoga also combines posture, breathing, and meditation. Practicing yoga can reduce thalamic gamma-aminobutyric acid levels, thereby reducing anxiety and depression and possibly pain [57].
Our systematic review determined that physical exercise can reduce NSCLBP frequency, and it can reduce fear avoidance belief when combined with health education. Appropriate physical interventions such as isokinetic muscle strength exercises and stretching exercises can reduce NSCLBP frequency in nurses. This may be due to static load-bearing areas with poor blood circulation in nurses, resulting in an excess of free radicals that causes cellular dysfunction and muscle fatigue. Long periods of muscle fatigue increase the risk of low back pain [7], whereas targeted physical exercise moves muscles, promotes blood circulation, and reduces NSCLBP frequency. Physical training and health education can reduce fear avoidance beliefs that may be related to fear of movement due to the cognitive-behavioral model regarding sports. A positive experience can reduce fear avoidance [58] and reinforce the concept that appropriate physical exercise is not dangerous and will not cause additional pain. Health education can provide nurses with positive experiences of sports that can change fear avoidance beliefs
We found that most non-drug interventions effectively relieved NSCLBP in nurses, as reported in a previous study [59]. However, clearly defined outcomes, standardized interventions, and the use of international research tools would enable other investigators to categorize their research and summaries. There are fewer additional outcome indicators for studies, so they could not be incorporated into this meta-analysis. Thus, fear avoidance beliefs regarding NSCLBP and lumbar dysfunction in nurses may be a future research direction.
There are several limitations to this study. First, the network meta-analyses were based on a single time point, which may be considered as a shortcoming due to varying follow-up periods. Second, some non-drug interventions were classified in this study, which may weaken the effect of a specific intervention. Third, there are large sample size differences in the literature, and because the results may be biased to some extent, we recommend further investigation to verify the conclusions. Although we performed subgroup and sensitivity analyses, there was still heterogeneity in some pooled analyses. The subgroup analysis results show that the sources of heterogeneity may include type of intervention and follow-up time, so the conclusion needs to be confirmed in future multicenter, large-sample, high-quality RCTs in different countries. Some interventions in this study have also been applied in the general population, but due to professional and research direction issues, we only focused on nurses with back pain. We will continue to pay close attention to studies on the effects of non-drug interventions in other different occupational groups with low back pain and update our results
5.Conclusion
Our network meta-analysis provides support for the effectiveness of low back exercise plus healthy education for NSCLBP in nurses. The results of our study can provide some reference for the treatment of NSCLBP in this population. We recommend large higher-quality RCTs to validate our results.
Acknowledgments
The authors are thankful for the statistical assistance provided by the Department of Statistics teaching and research office at Hebei Medical University. We would also like to thank Mr. Jiang JianZhong, director of the library of The Second Hospital of Hebei Medical University, for guidance regarding literature retrieval.
Conflict of interest
No conflicts of interest exist in the submission of this manuscript. The manuscript has been read and approved by all authors for publication.
Supplementary data
The supplementary figures are available from https:// dx.doi.org/10.3233/BMR-200147.
References
[1] | Expert group of spinal and Spinal Cord Committee of Chinese Rehabilitation Medical Association. Expert consensus on acute/chronic nonspecific low back pain in China. Chin J Spine Spinal Cord. (2016) ; 26: (12): 1134-1138. doi: 10.3969/j.issn.1004-406X.2016.12.16. |
[2] | Alemayehu T, Worku A, Assefa N. Sharp injury and exposure to blood and body fluids among health care workers in health care centers of eastern Ethiopia. Int J Occup Environ Med. (2016) ; 7: (3): 172-180. doi: 10.15171/ijoem.2016.714. |
[3] | Serranheira F, Smith D. Work-related musculoskeletal disorders in nursing: current knowledge and ongoing challenges for occupational health. Med Lav. (2014) ; 105: (5): 395-397. |
[4] | Azizpour Y, Delpisheh A, Montazeri Z, Sayehmiri K. Prevalence of low back pain in Iranian nurses: a systematic review and meta-analysis. BMC Nurs. (2017) ; 16: : 50. doi: 10.1186/s12912-017-0243-1. |
[5] | Soroush A, Shamsi M, Izadi N, Heydarpour B, Samadzadeh S, Shahmohammadi A. Musculoskeletal disorders as common problems among Iranian nurses: a systematic review and meta-analysis study. Int J Prev Med. (2018) ; 9: : 27. doi: 10.4103/ijpvm.IJPVM_235_16. |
[6] | Jin L, Jia M, Xu F. Meta-analysis on the prevalence of low back pain among nursing staff in China. Chin J Pract Nursing. (2013) ; 29: (20): 45-47. doi: 10.3760/cma.j.issn.1672-7088.2013.20.016. |
[7] | Tian S, Tang L, Yin L. Factors influencing and protection against occupational low back pain in nurses. Chin J Nursing. (2012) ; 47: (9): 856-858. doi: 10.3761/j.issn.0254-1769.2012.09.035. |
[8] | Schofield P. Assessment and management of pain in older adults with dementia: a review of current practice and future directions. Curr Opin Support Palliat Care. (2008) ; 2: (2): 128-132. doi: 10.1097/SPC.0b013e3282ffb406. |
[9] | Mroczek B, Ubkowska W, Jarno W, Jaraczewska E, Mierzecki A. Occurrence and impact of back pain on the quality of life of healthcare workers. Ann Agric Environ Med. (2020) ; 27: (1): 36-42. doi: 10.26444/aaem/115180. |
[10] | Yoshimoto T, Oka H, Ishikawa S, Kokaze A, Muranaga S, Matsudaira K. Factors associated with disabling low back pain among nursing personnel at a medical centre in Japan: a comparative cross-sectional survey. BMJ Open. (2019) ; 9: (9): e32297. doi: 10.1136/bmjopen-2019-032297. |
[11] | Alperovitch-Najenson D, Weiner C, Ribak J, Kalichman L. Sliding sheet use in nursing practice: an intervention study. Workplace Health Saf. (2020) ; 68: (4): 171-181. doi: 10.1177/2165079919880566. |
[12] | Tian S, Tang L, Ning W. The effect of occupational backache exercises on ICU nurses’ lower back pain alleviation. Chin Nursing Manage. (2014) ; 14: (8): 881-883. doi: 10.3969/j.issn.1672-1756.2014.08.030. |
[13] | Pakbaz M, Hosseini MA, Aemmi SZ, Gholami S. Effectiveness of the back school program on the low back pain and functional disability of Iranian nurse. J Exerc Rehabil. (2019) ; 15: (1): 134-138. doi: 10.12965/jer.1836542.271. |
[14] | Noormohammadpour P, Kordi M, Mansournia MA, Akbari-Fakhrabadi M, Kordi R. The Role of a Multi-Step Core Stability Exercise Program in the Treatment of Nurses with Chronic Low Back Pain: A Single-Blinded Randomized Controlled Trial. Asian Spine J. (2018) ; 12: (3): 490-502. doi: 10.4184/asj.2018.12.3.490. |
[15] | Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) ; 11: (18): 343. doi: 10.1136/bmj.d5928. |
[16] | Yao J. Influence of self-management education on pain, negative emotion and quality of life for low back pain nurses. Chin Foreign Women’s Health Study. (2018) (18):; 11: -12. doi: 10.3969/j.issn.2096-0417.2018.18.007. |
[17] | Huang X. Effect of self-management on negative emotion and quality of life of nurses with low back pain in operation room. Chin Continuing Med Educ. (2018) ; 10: (29): 199-200. doi: 10.3969/j.issn.1674-9308.2018.29.093. |
[18] | Wang B, Jiang W. Effect of self-programmed low back pain gymnastics on professional low back pain of orthopaedic nurses. J Tradit Chin Med Manage. (2016) ; 24: (8): 152-153. |
[19] | Ji J, Lu J, Xia Y, Xu C. Effect of suspension core control training on nursing low back pain. Massage Rehabil Med. (2019) ; 10: (9): 10-11. doi: 10.19787/j.issn.1008-1879.2019.09.005. |
[20] | Guo X, Han L, Yang W, Li Z. Intervention study of yoga on occupational lower back pain among nurses. J Environ Occup Med. (2016) ; 33: (11): 1022-1025. doi: 10.13213/j.cnki.jeom.2016.16304. |
[21] | Li W, Wang X. Influence by yoga spine training intervention on occupational low back pain in ICU nurse. Chin Mod Drug Appl. (2017) ; 11: (6): 196-198. doi: 10.14164/j.cnki.cn11-5581/r.2017.06.100. |
[22] | Yin L. Effect analysis of lumbar back muscle function exercise gymnastics in rehabilitation treatment of occupational low back pain of ICU nurses [Maste]. Hebei Medical University; (2014) . |
[23] | Ma K, Zhu W. Effect of low back muscle exercise on professional low back pain of gynecology and obstetrics nurses. Journal of Community Medicine. (2016) ; 14: (8): 84-86. |
[24] | Wang Y. Clinical observation on the prevention and treatment of occupational low back pain in nurses by manipulation and muscle strength training technique. Chongqing Medical Science. (2016) ; 45: (20): 2843-2845. doi: 10.3969/j.issn.1671-8348.2016.20.036. |
[25] | Hu S. Effect of home lumbago gymnastics on professional lumbago back pain of nurses. Qilu Nursing Journal. (2014) ; 20: (9): 33-34. doi: 10.3969/j.issn.1006-7256.2014.09.019. |
[26] | Mo C, Xing J, Xu H. Comparison of the effects of waistband protection and lumbar muscle exercise on nurses with occupatinal low back pain. Industrial Hygiene and Occupational Diseases. (2019) ; 45: (3): 175-177, 181. doi: 10.13692/j.cnki.gywsyzyb.2019.03.005. |
[27] | Wen Y, Lai W, Fu F. The effect of BackSmart system on occupation-related lumbago and back pain among nursing staff. China Clinical Nursing. (2016) ; 8: (3): 213-215. doi: 10.3969/j.issn.1674-3768.2016.03.009. |
[28] | Ghadyani L, Tavafian SS, Kazemnejad A, Wagner J. Work-related low back pain treatment: a randomized controlled trial from tehran, iran, comparing multidisciplinary educational program versus physiotherapy education. Asian Spine J. (2016) ; 10: (4): 690-696. doi: 10.4184/asj.2016.10.4.690. |
[29] | Movahedi M, Ghafari S, Nazari F, Valiani M. The effect of acupressure on fatigue among female nurses with chronic back pain. Appl Nurs Res. (2017) ; 36: : 111-114. doi: 10.1016/j.apnr.2017.06.006. |
[30] | Ghadyani L, Tavafian SS, Kazemnejad A, Wagner J. Effectiveness of Multidisciplinary Group-Based Intervention versus Individual Physiotherapy for Improving Chronic Low Back Pain in Nursing Staff: A Clinical Trial with 3- and 6-Month Follow-Up Visits from Tehran, Iran. Asian Spine J. (2017) ; 11: (3): 396-404. doi: 10.4184/asj.2017.11.3.396. |
[31] | Sharafkhani N, Khorsandi M, Shamsi M, Ranjbaran M. The Effect of an Educational Intervention Program on the Adoption of Low Back Pain Preventive Behaviors in Nurses: An Application of the Health Belief Model. Global spine journal (2015) ; 6: (1): 29-34. doi: 10.1055/s-0035-1555658. |
[32] | Vieira ER, Brunt D. Does wearing unstable shoes reduce low back pain and disability in nurses? A randomized controlled pilot study. Clin Rehabil. (2015) ; 30: (2): 167-173. doi: 10.1177/0269215515576812. |
[33] | Gannon J, Atkinson JH, Chircop-Rollick TD, Andrea J, Garfin S, Patel S, et al. Telehealth therapy effects of nurses and mental health professionals from 2 randomized controlled trials for chronic back pain. The Clinical Journal of Pain (2019) ; 35: (4): 295-303. doi: 10.1097/AJP.0000000000000678. |
[34] | Jaromi M, Kukla A, Szilagyi B, Simon-Ugron A, Bobaly VK, Makai A, et al. Back School programme for nurses has reduced low back pain levels: A randomised controlled trial. J Clin Nurs. (2017) ; 27: (5-6): e895-e902. doi: 10.1111/jocn.13981. |
[35] | Oka H, Nomura T, Asada F, Takano K, Nitta Y, Uchima Y, et al. The effect of the “One Stretch” exercise on the improvement of low back pain in Japanese nurses: a large-scale, randomized, controlled trial. Mod Rheumatol. (2019) ; 29: (5): 861-866. doi: 10.1080/14397595.2018.1514998. |
[36] | Ewert T, Limm H, Wessels T, Rackwitz B, von Garnier K, Freumuth R, et al. The comparative effectiveness of a multimodal program versus exercise alone for the secondary prevention of chronic low back pain and disability. PM R. (2009) ; 1: (9): 798-808. doi: 10.1016/j.pmrj.2009.07.006. |
[37] | Horneij E, Hemborg B, Jensen I, Ekdahl C. No significant differences between intervention programmes on neck, shoulder and low back pain: a prospective randomized study among home-care personnel. J Rehabil Med. (2001) ; 33: (4): 170-176. doi: 10.1080/165019701750300636. |
[38] | Chen HM, Wang HH, Chen CH, Hu HM. Effectiveness of a stretching exercise program on low back pain and exercise self-efficacy among nurses in Taiwan: a randomized clinical trial. Pain Manag Nurs. (2014) ; 15: (1): 283-291. doi: 10.1016/j.pmn.2012.10.003. |
[39] | Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. (2018) ; 18: (1): 1376. doi: 10.1186/s12889-018-6293-9. |
[40] | Armand S, Tavcar Z, Turcot K, Allet L, Hoffmeyer P, Genevay S. Effects of unstable shoes on chronic low back pain in health professionals: A randomized controlled trial. Joint Bone Spine. (2014) ; 81: (6): 527-532. doi: 10.1016/j.jbspin.2014.05.006. |
[41] | Jensen LD, Gonge H, Jørs E, Ryom P, Foldspang A, Christensen M, et al. Prevention of low back pain in female eldercare workers: randomized controlled work site trial. Spine. (2006) ; 31: (16): 1761-1769. doi: 10.1097/01.brs.0000227326.35149.38. |
[42] | Patil N, Nagaratna R, Tekur P, Manohar PV, Bhargav H, Patil D. A randomized trial comparing effect of yoga and exercises on quality of life in among nursing population with chronic low back pain. International Journal of Yoga. (2018) ; 11: (3): 208-214. doi: 10.4103/ijoy.IJOY_2_18. |
[43] | Babadi ME, Nazari F, Safari R, Abdoli S. The effect of reflexology on pain perception aspects in nurses with chronic low back pain in Isfahan. Iran J Nurs Midwifery Res. (2016) ; 5: (21): 487-492. doi: 10.4103/1735-9066.193395. |
[44] | de Campos TF, Maher CG, Fuller JT, Steffens D, Attwell S, Hancock MJ. Prevention strategies to reduce future impact of low back pain: a systematic review and meta-analysis. Br J Sports Med. (2020) ; 0: : 1-10. doi: 10.1136/bjsports-2019-101436. |
[45] | Huang R, Ning J, Chuter VH, Taylor JB, Christophe D, Meng Z, et al. Exercise alone and exercise combined with education both prevent episodes of low back pain and related absenteeism: systematic review and network meta-analysis of randomised controlled trials (RCTs) aimed at preventing back pain. Br J Sports Med. (2020) ; 54: (13): 766-770. doi: 10.1136/bjsports-2018-100035. |
[46] | Young L, Ouyang L, Chen D, Lin Q. A biomechanical analysis of low back pain. Chinese Journal of Tissue Engineering Research. (2020) ; 24: (33): 5267-5271. doi: 10.3969/j.issn.2095-4344.2848. |
[47] | Kim J, Yang SJ, Kim H, Kim Y, Park JB, Dubose C et al., Effect of shear force on intervertebral disc (IVD) degeneration: an in vivo rat study. Ann Biomed Eng. (2012) ; 40: (9): 1996-2004. doi: 10.1007/s10439-012-0570-z. |
[48] | Shojaei S, Tavafian SS, Jamshidi AR, Wagner J. A Multidisciplinary Workplace Intervention for Chronic Low Back Pain among Nursing Assistants in Iran. Asian Spine J. (2017) ; 11: (3): 419-426. doi: 10.1136/bjsports-2018-100035. |
[49] | Barr KP, Griggs M, Cadby T. Lumbar stabilization: a review of core concepts and current literature, part 2. Am J Phys Med Rehabil. (2007) ; 86: (1): 72-80. doi: 10.1097/01.phm.0000250566.44629.a0. |
[50] | Barr KP, Griggs M, Cadby T. Lumbar stabilization: core concepts and current literature, Part 1. Am J Phys Med Rehabil. (2005) ; 84: (6): 473-480. doi: 10.1097/01.phm.0000163709.70471.42. |
[51] | Bellido-Fernández L, Jiménez-Rejano JJ, Chillón-Martínez R, Gómez-Benítez MA, De-La-Casa-Almeida M, Rebollo-Salas M. Corrigendum to “Effectiveness of Massage Therapy and Abdominal Hypopressive Gymnastics in Nonspecific Chronic Low Back Pain: A Randomized Controlled Pilot Study". Evid Based Complement Alternat Med (2018) ; 2018: : 3601984. doi: 10.1155/2018/3601984. |
[52] | Zhu F, Zhang M, Wang D, Hong Q, Zeng C, Chen W. Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLoS One. (2020) ; 15: (9): e238544. doi: 10.1371/journal.pone.0238544. |
[53] | Telles S, Sharma SK, Yadav A, Singh N, Balkrishna A. Immediate changes in muscle strength and motor speed following yoga breathing. Indian J Physiol Pharmacol. (2014) ; 58: (1): 22-29. |
[54] | Kim SD. Twelve weeks of yoga for chronic nonspecific lower back pain: a meta-analysis. Pain Manag Nurs. (2020) ; 21: (6): 536-542. doi: 10.1016/j.pmn.2020.07.002. |
[55] | Berlowitz J, Hall DL, Joyce C, Fredman L, Sherman KJ, Saper RB, et al. Changes in perceived stress after yoga, physical therapy, and education interventions for chronic low back pain: a secondary analysis of a randomized controlled trial. Pain Med. (2020) ; 21: (10): 2529-2537. doi: 10.1093/pm/pnaa150. |
[56] | Jradi H, Alanazi H, Mohammad Y. Psychosocial and occupational factors associated with low back pain among nurses in Saudi Arabia. J Occup Health. (2020) ; 62: (1): e12126. doi: 10.1002/1348-9585.12126. |
[57] | Manocha R, Black D, Sarris J, Stough C. A randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers. Evid Based Complement Alternat Med. (2011) ; 2011: : 960583. doi: 10.1155/2011/960583. |
[58] | Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. (1995) ; 62: (3): 363-372. doi: 10.1016/0304-3959(94)00279-n. |
[59] | Van Hoof W, O’Sullivan K, O’Keeffe M, Verschueren S, O’Sullivan P, Dankaerts W. The efficacy of interventions for low back pain in nurses: A systematic review. Int J Nurs Stud. (2018) ; 77: : 222-231. doi: 10.1016/j.ijnurstu.2017.10.015. |




