In-depth analysis of life values and their corresponding inhibitors and facilitators in chronic low back pain patients: A mixed-method approach
Abstract
BACKGROUND:
The struggle with pain often interferes with the ability of chronic low back pain (CLBP) patients to pursue important life values due to psychological inflexibility.
OBJECTIVE:
This research examined life values, related inhibitors and facilitators relevant to personalized therapy planning.
METHODS:
Two hundred and forty-four CLBP patients completed the Chronic Pain Values Inventory (CPVI). Of these, 68 patients were interviewed to assess inhibitors and facilitators related to life values. Mixed-effects models quantitatively examined differences in the values, structuring content analysis served to qualitatively analyze the interviews.
RESULTS:
Participants rated the value “family” as being of highest importance and success. The largest discrepancy between importance and success was found for “health”. Content analyses revealed a broad range of inhibitors and facilitators related to the examined life values with the highest number of inhibitors related to “work”. Facilitators were also found to be of relevance to all life values, but to a lower extent than inhibitors.
CONCLUSIONS:
The perceived importance and success of life values and their related inhibitors and facilitators may differentially affect CLBP patients. Considering such individual aspects is therefore of utmost importance to improve patient care, as they enable treatment goals and the therapeutic strategies to be adapted accordingly.
1.Introduction
Chronic low back pain (CLBP) is considered to be a complex biopsychosocial syndrome [1, 2] and it has been found that the struggle with chronic pain often interferes with patients’ ability to take part in activities of daily life such as relationships, family commitments, and/or work [2, 3]. It has been argued that it is not only the pain intensity that affects patients’ level of functioning and their ability to participate in important parts of life, but also their behavioral response towards pain [4]. Pain behavior has repeatedly been suggested to be mainly associated with the psychological flexibility of CLBP patients [5]. Psychological flexibility, which is comprised of six components (acceptance, cognitive defusion, flexible present-focused attention, self-as-observer, values-based action, and committed action [5]), has been described as the ability to act in accordance with one’s personal values despite possibly interfering feelings and thoughts [6]. Higher psychological flexibility would enable CLBP patients to cope with pain in an appropriate way, whereas psychological inflexibility would be related to suffering and behavior problems that comprise the psychopathology of chronic pain [5]. One aspect of psychological flexibility, namely values-based action, is an individual’s ability to follow his or her individual life values [5], i.e., to follow his or her freely chosen, important, and ongoing desires [7]. A greater success in living according to these values has been associated with better functioning [8] and better outcomes in pain patients in several studies (e.g. [9, 10, 11]), including at the three-year follow-up point [12]. Acting in discrepancy with or neglecting specific life values due to a high level of attention given to pain can in turn be expected to be related to persisting disablement due to pain.
This highlights the importance of conducting a precise analysis of individual life values to enable therapy tailored to the individual needs of patients. The importance of personalized pain treatment has been pointed out before [13] and is also already included in assessment tools like the International Classification of Functioning, Disability and Health (ICF) [14], gaining even more relevance due to the inclusion of chronic pain as a diagnosis in the upcoming International Classification of Diseases 11th Revision (ICD-11) [15]. Accordingly, the Chronic Pain Values Inventory (CPVI) [9] provides a short, reliable and valid method to examine individual patient values, also in its Swedish version [16]. It assesses the importance and success, as well as the discrepancy between importance and success, regarding the six life values “family”, “intimate relations”, “friends”, “work”, “health”, and “growth and learning”. The term “importance” is defined as the relevance each individual patient allocates to each of the six values, whereas “success” describes how well or how badly patients feel they are able to live in a way consistent with these values. If the “success” is perceived by a patient as less relevant than “importance”, a discrepancy results, the degree of which can also be captured by the CPVI measure. In a sample of 140 participants (67.9% female, mean age
It can be presumed that there are numerous psychosocial factors that influence the discrepancy between importance and perceived success amongst the different life values. Whereas some of these factors would facilitate success within life domains, others could inhibit them, consequently leading to elevated levels of discrepancy between importance and success and thus hindering the level of contentment experienced by a patient. In order to optimize treatment and intervention setting in CLBP, identification of such facilitators and inhibitors is therefore of utmost interest. A literature review revealed that no study to date has examined such individual factors in detail. By applying a mixed-method approach this study aims to overcome shortcomings of a solely quantitative analysis through in-depth interviews. Within this mixed-method approach, the analysis of quantitative data from the CPVI examines the importance and success of the six life values, while the analysis of qualitative data provides insights on the complex connection between life values and their concrete implementations in low back pain patients. Thus, by using a German version of the CPVI, the aims of this study were:
1. To identify those life values that reveal the greatest importance, success, and discrepancy in CLBP patients, and to determine whether or not our findings would be consistent with those of a previous study performed in a different sample of chronic pain patients by McCracken and Yang [9]. This previous research observed highest relevance and success regarding “family”, least relevance regarding “friends”, and least success regarding “health”, respectively.
2. To identify those facilitators and/or inhibitors that are predominately linked to the success and discrepancies within the examined life values, and thus might influence therapy/rehabilitation outcome.
2.Materials and methods
2.1Participants and study design
Between January 2012 and July 2015, a total of 294 chronic low back pain patients who had been referred from various settings to an outpatient rehabilitation center were screened for eligibility for this cross-sectional study. Patients with a minimum age of 18 years were included in the study if they had low back pain lasting for more than three months at a minimum mean pain level of 30 on a visual analog scale [17] and had a good overall health status, i.e. no other acute or chronic illnesses like cardio-pulmonary diseases, spinal diseases, neurological diseases, or severe psychiatric disorders (see also exclusion criteria).
Exclusion criteria were: moderate to high pain levels in areas other than the lower back (larger or equal than 30 on a visual analog scale [17]); spinal fractures, infection or cancer; osteoarthritis; any kind of specific spinal disease; clinical findings indicative of neuropathological conditions or structural impairments; previous surgery involving the back region; functional capacity limiting cardio-pulmonary diseases; severe psychiatric disorders; a body mass index exceeding 35 kg/m
The study conformed to the ethical principles of the Declaration of Helsinki and was approved by the Ethics committee of the city of Vienna (Thomas-Klestil-Platz 8/2, TownTown, A-1030 Vienna (EK_11_181_VK_ NZ)). All patients willing to participate received oral and written information about the study and signed a consent form before they were included in the study.
2.2Measures
After screening for eligibility, a total of 244 patients were included in the study and were asked to complete psychological and pain-related questionnaires on the first test day. Of these, 68 randomly chosen CLBP patients also completed a semi-structured interview conducted by clinical psychologists on a second test day.
2.2.1Chronic Pain Values Inventory (CPVI)
The CPVI consists of two sub-scales measuring success and importance in six domains of life values (“family”, “intimate relations”, “friends”, “work”, “health”, and “growth and learning”). Two mean scores can be derived, and the discrepancy between importance and success in each of the items as well as the mean discrepancy can be calculated. The CPVI in its English version [9] has been shown to have good reliability and validity.
As no German version of this measure was available, we translated the CPVI into German in a two-way translation progress. The CPVI rating scales were changed from 6-point-scales (from 0
2.2.2Demographic list, pain, disability, and depression levels
Both a general demographic and a medical history checklist were used to assess patients’ gender, age, educational level, marital status, and pain history. Current pain intensity was rated on visual analog scales ranging from 0 (no pain) to 100 (most severe pain imaginable) [17]. Impairments in back related health level was assessed with both the German versions of the Roland-Morris Disability Questionnaire (RMDQ) [19, 20] and the Pain Disability Index (PDI) [21, 22].
Mental health as a relevant component of quality of life was assessed with the mental health sum score of the German version of the 36-Item Short-Form Health Survey (SF-36) [23]. To examine depression, the sub-scale mental health inventory (MHI) was used (higher values indicate a lower level of depression).
2.2.3Semi-structured interviews
Semi-structured interviews [24] were conducted by clinical psychologists in order to obtain in-depth knowledge pertaining to the CPVI values concerning “family”, “intimate relations”, “friends”, “work”, “health”, and “growth and learning”. The interviews also collected information about inhibitors and facilitators in these life domains, as well as why patients considered their performance in a life value as more or less successful. Each interview lasted for approximately one hour.
Table 1
Sample characteristics
| Characteristics | Mean (SD) od |
|---|---|
|
| 244 |
| 68 | |
| Age | 49.04 (17.64) |
| Gender (female) | 126 (52%) |
| Education | |
| University degree | 54 (22%) |
| Matura ( | 53 (22%) |
| Professional training | 113 (46%) |
| Secondary school | 14 (6%) |
| Primary school | 3 (1%) |
| Not specified | 7 (3%) |
| Marital status | |
| Married | 112 (46%) |
| Unmarried | 72 (30%) |
| Divorced | 39 (16%) |
| Other | 21 (8%) |
| Employment status | |
| Employed | 117 (48%) |
| Retired | 81 (33%) |
| Student | 23 (9%) |
| Self-employed | 5 (2%) |
| Leave/household | 2 (1%) |
| Unemployed | 11 (5%) |
| Not specified | 5 (2%) |
| Pain characteristics | |
| Current pain intensity | 27.56 (19.11) |
| Average pain intensity last three months | 51.70 (13.46) |
| Pain duration current pain period (weeks) | 56.73 (85.42) |
| Pain duration since initial manifestation (months) | 139.5 (124.37) |
| Disablement | |
| Roland-Morris Disability Questionnaire | 7.23 (4.08) |
| Pain Disability Index | 17.1 (11.14) |
| Mental health | |
| Mental health related quality of life (SF-36-mental health sum score) | 50.95 (9.62) |
| Depression (SF36-MHI) | 74.59 (15.82) |
| CPVI sum scales | |
| Importance | 7.43 (1.66) |
| Success | 5.79 (1.76) |
Notes:
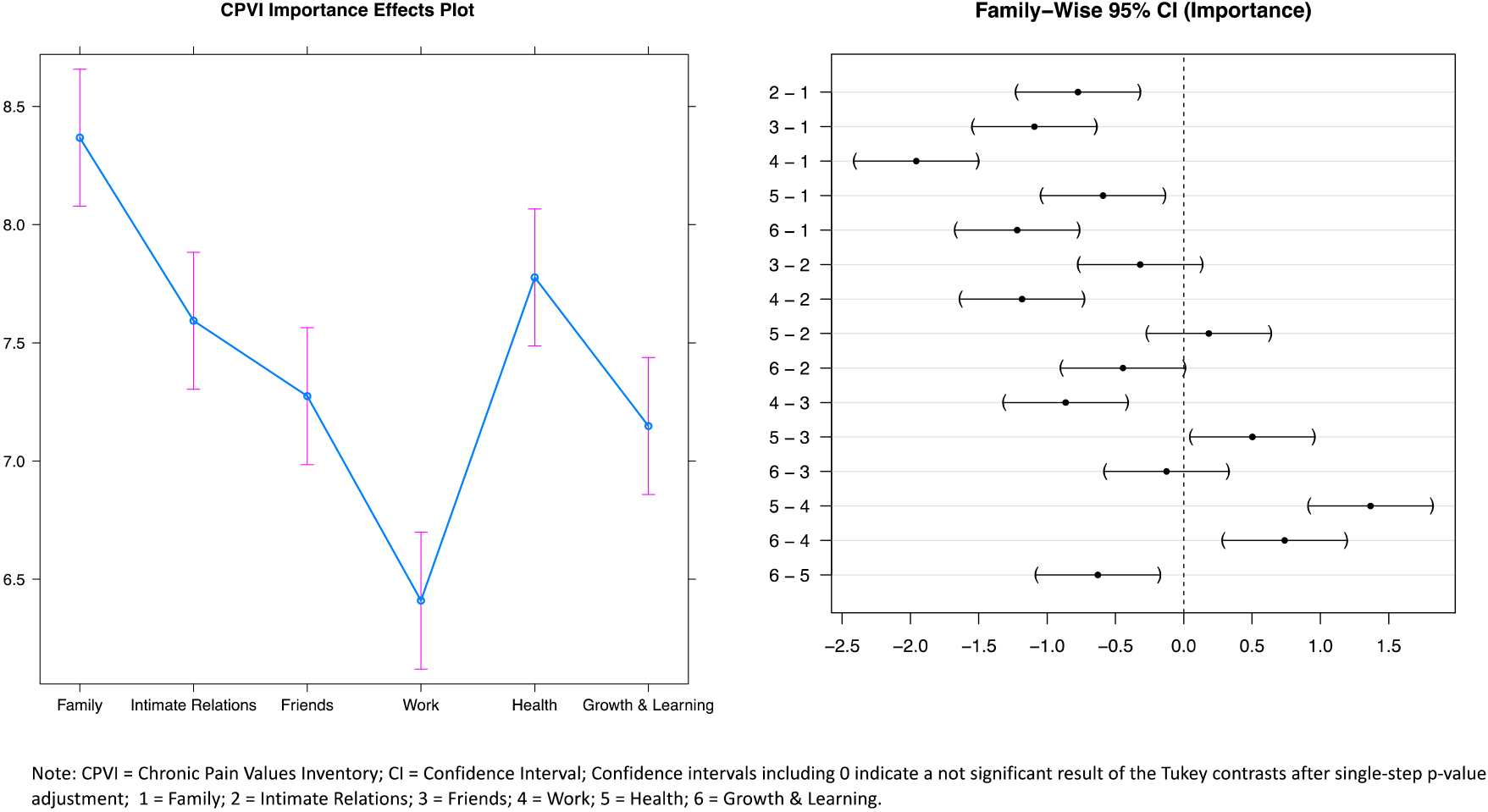
Figure 1.
Post hoc tests for comparisons regarding importance in the six values.
2.3Statistical analysis
To compare the response variables success, importance, and discrepancy across different life values, within-subject designs were applied with a within-subject variable consisting of the categories “family”, “intimate relations”, “friends”, “work”, “health”, and “growth and learning”. To examine potential differences between these categories in relation to the response variables success, importance, and discrepancy, mixed-effects models were fitted for each of the response variables. The model-fit was then checked with residual diagnostics. A Bonferroni correction was conducted to adjust the
Interviews from the 68 participants were transcribed and suitable for content analysis. Not every patient gave extensive answers regarding each of the domains. As the answers and comments of some of the patients on questions considering the life domains were either unspecific or uninformative, the number of available interviews is given for each life value. All the interviews were conducted by one of the authors who is an experienced clinical psychologist (EF), and the content analysis was done by another author (LF-G) of this paper. The content analysis was then reviewed by other authors (KT, EF) to ensure objectivity. Categories were composed via inductive content analysis and by using the structuring content analysis developed by Mayring [32, 33]. A quantitative content analysis was used to determine frequencies of categories.
3.Results
3.1Sample
A total of 244 CLBP patients with a mean age of 49.04 years (SD
Self-reported disability levels indicated moderate impairment, and are provided together with the demographic, social and clinical variables in Table 1.
Table 2
Results of the mixed-effects models
| Variable | Mean (SD) |
| |
|---|---|---|---|
| Importance | 34.66 (5,1215) | ||
| Family | 8.37 (2.04) | ||
| Intimate relations | 7.59 (2.53) | ||
| Friends | 7.27 (2.24) | ||
| Work | 6.41 (2.35) | ||
| Health | 7.78 (2.24) | ||
| Growth and learning | 7.15 (2.40) | ||
| Success | 15.57 (5,1215) | ||
| Family | 6.49 (2.39) | ||
| Intimate relations | 6.00 (2.72) | ||
| Friends | 5.94 (2.43) | ||
| Work | 5.74 (2.46) | ||
| Health | 5.07 (2.50) | ||
| Growth and learning | 5.48 (2.40) | ||
| Discrepancy | 30.15 (5,1215) | ||
| Family | 1.88 (2.19) | ||
| Intimate relations | 1.60 (2.44) | ||
| Friends | 1.33 (2.10) | ||
| Work | 0.67 (2.15) | ||
| Health | 2.71 (2.50) | ||
| Growth and learning | 1.67 (2.38) |
Notes:
3.2Quantitative data analysis – differences regarding the perceived importance, success, and discrepancy of the different values
Mixed effects models revealed significant differences in all three scales for the six different life values (see Table 2). Tukey contrasts demonstrated the value “family” to be significantly more important than any of the other values, whereas the value “work” was shown to be significantly less important than any of the other life values (Fig. 1). The perceived success of the life value “family” was found to be significantly higher than the success of any other values, while success concerning “health” was significantly lower than any other life value except for “growth and learning” (Fig. 2). Tukey contrasts further showed that the discrepancy between success and importance was significantly higher for the life value “health” than for any of the other values, whereas the discrepancy related to the life value “work” was significantly lower than in all other values (Fig. 3).
Figure 2.
Post hoc tests for comparisons regarding success in the six values.
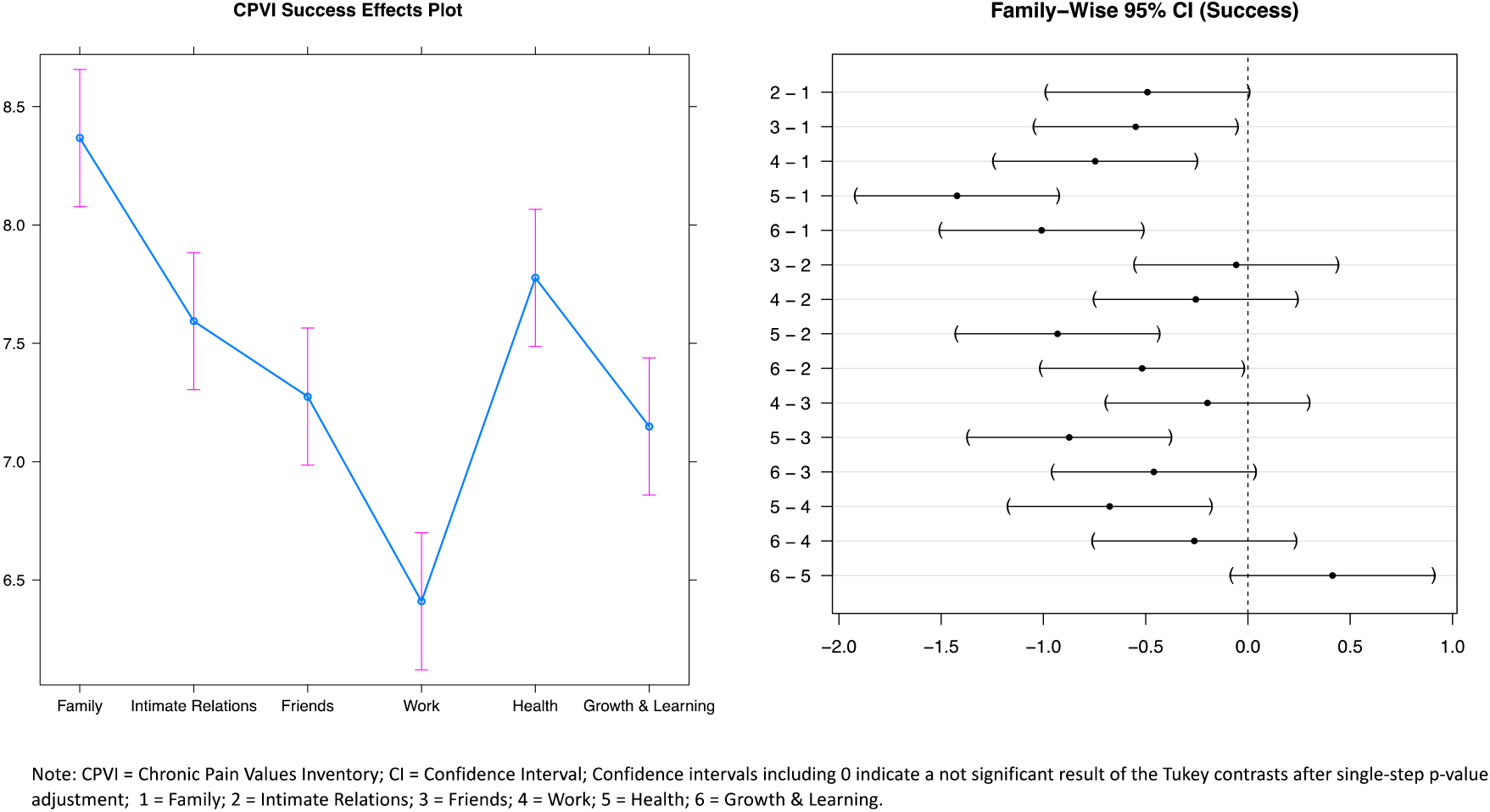
Figure 3.
Post hoc tests for comparisons regarding discrepancy in the six values.
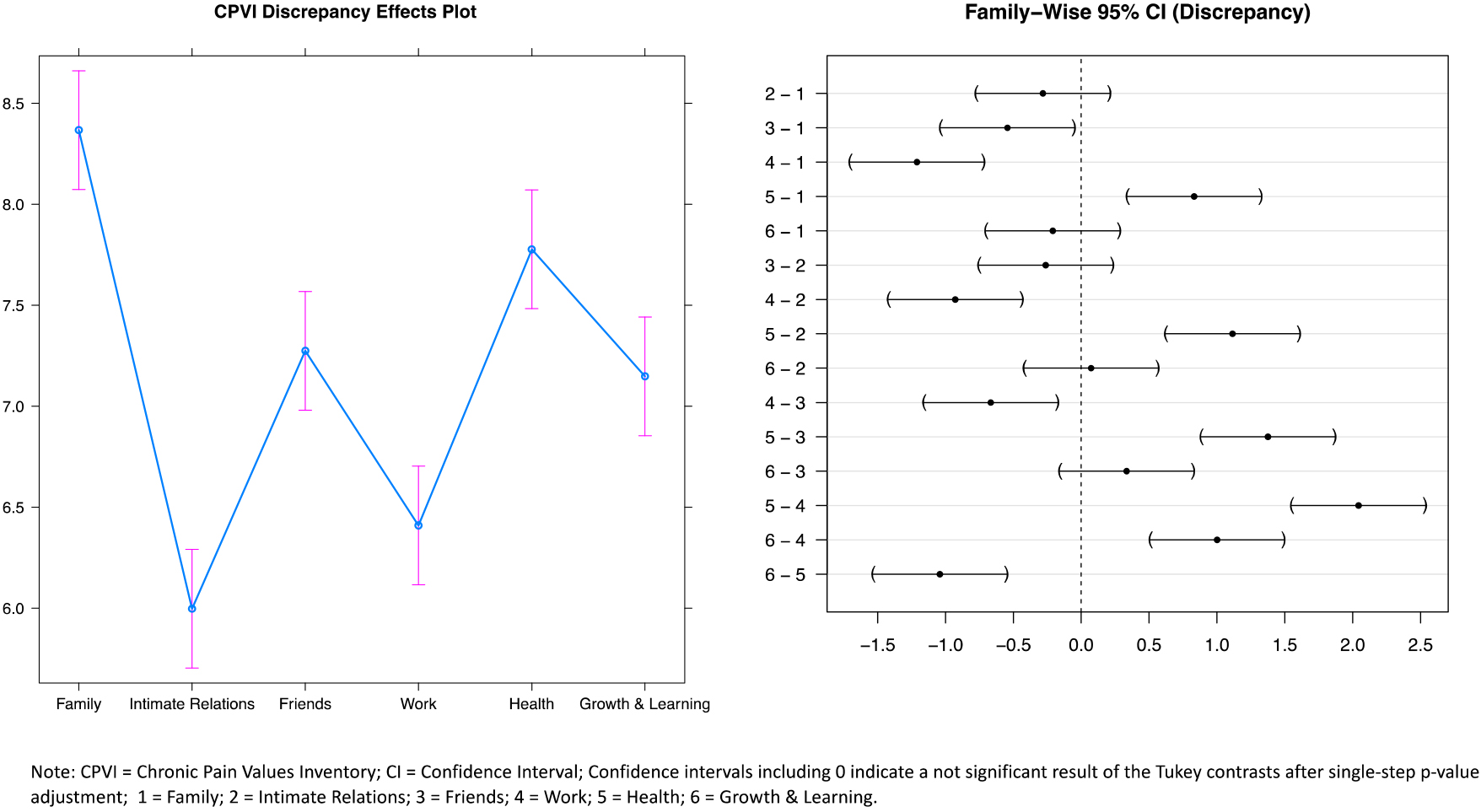
Table 3
Main categories and inductive categories derived for inhibitors and facilitators for the six life values
| Life value | Main category | % | Inductive categories | Quotes | |
|---|---|---|---|---|---|
| “Family” ( | Inhibitors | Conflicts | 29 | Disagreements/conflicts/dissatisfaction with family members, overload/self-sacrifice | “…started to set boundaries, after having self-sacrificed myself for […] the family” (ID A) |
| Experiences of loss of family members | 29 | Death and other experiences of loss, loss of contact, loneliness, geographical distance | “[I] have three children, one died with 31 years, […] I have very little contact with my family – [I am] not happy about that, but [I] have to accept that” (ID B) | ||
| Emotional strain due to problems or illnesses of family members | 26 | Worries about physical/mental health of family members, unspecified worries, care dependency of family members | “[I am] worried because my son suffers from burnout syndrome […]. It is not getting better and I am afraid he could lose his job” (ID C) | ||
| Changes of life circumstances | 12 | Children moving out, separation of one’s parents, general transitions | “[my] daughter is in the USA, my son moved out as well, [there is] an atmosphere of change” (ID E) | ||
| Stressful childhood experiences | 11 | Unstable conditions, traumatic childhood experiences, a strict upbringing, having to work as a child, not knowing one’s parents | “I had a burdened childhood, my father left the family and I was the oldest. There were a lot of brawls and problems with the police” (ID F) | ||
| Facilitators | Resources | 15 | Pride in one’s children/grandchildren, support, close emotional bonds, to spend time with family members, to have time for oneself | “[My family] is great, we have a strong family support” (ID G) | |
| “Intimate relations” ( | Inhibitors | Dissatisfaction with the current relationship | 28 | Bigger disagreements/conflicts, being unhappy or disappointed, sharing only little activities and interests/time/affections, little support by one’s partner, viewing the relationship as strain, thoughts of separation | “My husband works a lot. I have been happier [at earlier times]. We don’t do a lot together, we have a lot of work, and little affection” (ID H) |
| Experiences of loss of a partner/spouse | 19 | Divorce, separation, and death of one’s partner/spouse | “My first husband died in a car accident, my second husband filed for divorce. Those were hard times” (ID I) | ||
| Emotional strain due to problems or illnesses of partners/spouses | 13 | Physical or mental illness of the partner, care dependency of the partner, unspecified worries about the partner | “[My wife] suffers from breast cancer […]. The year after the operation was burdensome” (ID J) | ||
| Negative experiences in the past | 9 | Negative experiences with a(n) (ex-)partner (e.g., alcoholism, aggression), being disappointed by dating, fear of/not wanting new relationships | “My ex-partner was an alcoholic and was oftentimes very aggressive when inebriated” (ID K) | ||
| Unfulfilled wishes | 5 | The wish for a relationship, fear of being alone | “I currently don’t have a partner, but I would like to have [a relationship]” (ID L) | ||
| Facilitators | Resources | 25 | Support by one’s partner, having a good/ long lasting relationship, experiencing individuality, children/shared activities/work/ friends/living | “My partner supports me a lot, we are a good team” (ID M) | |
| “Friends“ ( | Inhibitors | Dissatisfaction with friends | 29 | Too little time/intimacy, too many friends, distance, disappointment in friends, feeling of being taken advantage of | “I have little time for friends […] I wish I had more time to spend with my friends” (ID N) |
| Experiences of loss of friends | 5 | Death of friends | “Friends are dying one after each other – that is rough” (ID O) | ||
| Facilitators | General resources | 32 | Experiencing less pain when being with friends, shared activities, having many/good friends/long lasting friendships, regular contact, having a good social environment | “I have good, long-lasting friendships, we do a lot together” (ID P) | |
| Sources of friendship | 21 | Leisure activities, hobbies, (competitive) sports, work, from youth/school, through one’s partner | “I have friends from leisure activities [like] tennis – and a few through work” (ID Q) | ||
| Being a friend | 5 | Being a good listener, being someone who supports others | “When a friend needs help, I support him/her” (ID R) |
|
Table 3, continued | |||||
|---|---|---|---|---|---|
| Life value | Main category | % | Inductive categories | Quotes | |
| “Work” ( | Inhibitors | External stressors | 82 | Time pressure, high workload/demands, additional workload, over/under burden, frustration/dissatisfaction/aimlessness, little free/vacation time, long hours, little recognition, inability to relax, stressful client contact, worries about business success, fear of dismissal | “I oftentimes have to work under time pressure, I have stress several day [a week]” (ID S) |
| Health stressors | 63 | Physical stress, shift work, sleep deprivation/ disturbances, sedentary work, psychosomatic complaints, “burnout”, work accidents, long duration of sick leave | “I am dissatisfied with the physical burden, especially since I already have back pain. Other colleagues have pain, too, but they are older” (ID T) | ||
| Internal stressors | 57 | High achievement goals/high ambition/ perfectionism, endurance behavior, self-criticism, the perceived need to function, self-sacrifice, work as highest priority | “I am very hardworking, I am a perfectionist, [and] critical. […] I have high ambitions” (ID U) | ||
| Stressors due to organizational climate/conflicts | 21 | Conflicts with superiors/colleagues, little support, bullying, negative organizational climate, staff reduction, sickness of colleagues, not taking sick leaves for fear of consequences, unemployment, low income | “There are always problems with one of my colleague and I don’t like my superior, she always wants to pass on work onto me” (ID V) | ||
| Facilitators | Resources derived from work | 36 | Joy in one’s work, supportive colleagues/ superiors, open time-management, high income, feeling of accomplishments, having no physical stress, feeling balanced, glad to be retired | “Work was oftentimes stressful, but it also gave me great pleasure” (ID W) | |
| “Health” ( | Inhibitors | Physical comorbidities | 73 | Musculoskeletal disorders, cardio-vascular disorders, metabolic disorders, thyroid diseases, diseases of the urogenital tract, tumors/cancer in the past | “I had to undergo a lot of operations, three by-pass-operations, [I suffer] from Hashimoto thyroiditis” (ID X) |
| Mental stressors | 62 | Stress, pain influencing one’s mood, symptoms of depression or anxiety, alcoholism, worries about one’s health, decline of memory performance, sleep disturbances/exhaustion | “I feel depressed, downcast, I just want to have my peace” (ID Y) | ||
| Possible explanations for back pain | 58 | Wrong movements, sedentary work, interaction with psychological stressors, family history, too much physical activity/strain, accidents, lack of physical activity | “When I am stressed, I have more pain […] My parents both had problems with their backs as well” (ID Z) | ||
| Content related to back pain | 42 | Perceived limitations caused by CLBP, reduction of quality of life due to pain | “I am in a great deal of pain and that decreases my quality of life” (ID AA) | ||
| Physically limiting factors | 23 | Overweight, smoking a lot, menopausal symptoms, dissatisfaction with one’s fitness, limitations due to aging | “I don’t feel fit, I am tired and exhausted” (ID AB) | ||
| Facilitators | Health promotion | 15 | Healthy diet, preventive medical check-ups, the intention to stop smoking, a healthy lifestyle in general, and to look after one’s health, body or weight | “I go to medical-check-ups and look after my health” (ID AC) | |
| “Growth and learning” ( | Inhibitors | Barriers to engage in growth and learning | 18 | Lack of interest/low priority, lack of endurance, the feeling that growth and learning is not as easy as it was, indecisiveness, lack of time, experiences of failures | “I don’t have time for new things […] I have to learn enough anyway” (ID AD) |
| Facilitators | Motivation/incentive | 61 | Relaxation, ambition/interests/curiosity, challenges, high learning ability, part of work/ further education, to stay mentally active/to prevent standstill, self-realization | “[I want] to learn something new, I am curious” (ID AE) | |
| Content | 32 | Sports, languages, hobbies, learning/playing instruments, computer, trips, doing something creative, and interest in stock exchange | “I learn a lot of new things, like ballet, and Spanish” (ID AF) | ||
Notes:
3.3Qualitative data analysis – content analysis of the interviews
Based on the analysis of the answers obtained from the semi-structured interviews, a total of five main categories were identified as inhibitors regarding the life value “family”. By contrast, only one facilitator related to a patient’s resources was identified for this life value (15%,
For the life value “intimate relations”, a total of five main categories of inhibitors were derived from the interviews (Table 3). Resources that would facilitate this life value were mentioned by 25% (
For the life value “friends”, two main categories were identified as inhibitors and three as facilitators (Table 3): The inhibitors were: dissatisfaction with friends (29%,
For the life value “work”, a total of four main categories (external stressors [82%,
Five categories were identified as being deleterious to the patients’ life value “health” (Table 3). By contrast, only one facilitating category (health promotion, 15%,
Regarding the life value “growth and learning”, three main categories were identified, of which only one was an inhibitor (barriers to engage in growth and learning); this inhibitor was mentioned by 18% (
4.Discussion
To the best of our knowledge, this study is the first to apply a mixed-method approach to quantitatively examine the relevance of different life values to CLBP patients in a German speaking sample, and to qualitatively examine which inhibitors and facilitators influence success in living according to these values.
Results of the mixed-effect models reveal that patients experienced significant differences in the perceived importance, success, and discrepancy amongst the six life values, and mostly replicates findings by McCracken and Yang [9]. Furthermore, results of the qualitative analysis yielded greater insight into which kinds of, and to which extent, inhibitors and facilitators modulate the perceived success within the individual life domains, such as work-related strain, experiences of loss, etc.
In the study by McCracken and Yang, which examined 140 chronic pain patients, “family” was perceived as the most important and most successful life value, whereas “health” was perceived as the least successful one [9]. These results are therefore well in line with this present study. The rankings of life values in the McCracken and Yang study were similar to ours, although the differences between the importance of individual life values were found to be clearer in the post hoc comparisons of our study. There was, however, a striking difference between the two studies regarding the life value “work”. Whereas findings from our study suggest this value is significantly less important than any of the other values, the study by McCracken and Yang only found the life value “family” to be significantly more important than “work”. Differences in both education and employment status, as well as in primary pain location between the two study samples may serve as a possible explanation for such discrepancies. In the present study most of the patients were currently working and highly educated, and all suffered from low back pain, whereas in the study by McCracken and Yang most patients were on sick leave or unemployed because of pain and only 46.4% of the participants primarily reported back pain, whereas other participants stated pain in lower limbs, full body, upper limbs, and other pain locations. Especially the high number of not working participants in the study by McCracken and Yang might explain the high perceived importance of the value “work” in that sample possibly indicating a burden because of the unemployment.
The qualitative analysis of the interviews identified several inhibitors to the success of individual life values. This observation seems widely supported from evidence that suggested psychosocial stressors as risk factors for the chronification of low back pain. The flag system, a clinical assessment method for low back pain, assigns blue flags to perceptions about work, e.g., that work negatively influences health, and black flags to employer and insurance system characteristics and physical job demands [34, 35]. Co-morbidities as a risk for pain maintenance are subsumed under the orange flags, whereas unhelpful beliefs regarding pain, emotional responses, and maladaptive pain behavior are classified as yellow flags [35], and assessment of yellow flags is recommended in many practice guidelines [36]. Evidence suggests that mental suffering, which goes along with negative thoughts and depressed or anxious feelings, is considered an important risk factor for pain chronification, and mental illness is a common co-morbidity of back pain, both exacerbating each other [37, 38, 39, 40]. Next to these inhibitors, which impede greater success within the different life values, facilitators were also mentioned for every life value and might serve as important reinforcers of valued living in CLBP patients. Family and social contacts, for example, seem to be important resources when coping with health issues [41, 42, 43, 44].
The CLBP patients in this study rated “family” as the most relevant life value and the most successful, but nevertheless this life domain was identified as conflicted, with a relatively high load of inhibitors. Some of the inhibitors were not only found for the life value “family” but also for other social categories. For instance, experiences of loss were mentioned for the values: “family”, “intimate relations”, and “friends”, thus reflecting a high impact on individuals’ lives; caring for a loved one was mentioned within the values “family” and “intimate relations”; and, dissatisfaction both with “friends” and “intimate relations” was reported. These results are consistent with other studies reported in the literature, where both family and social life related stressors [45, 46, 47] were repeatedly observed in chronic back pain patients as was family-related negative strain [46, 48, 49]. The association between family strain and back pain has also been found to be mediated by depression [50].
Inhibitors concerning the life value “work” were more frequently reported than any of the other values in this study. This was despite the observation that “work” was rated the least important aspect; this result highlights the benefit of the mixed-method approach. The mentioned inhibitors included external stressors, health stressors, internal stressors, as well as organizational stressors. These results are consistent with studies that have revealed that beliefs about a negative effect of work on health is regarded as an important health stressor [34, 35], and that job stress constitutes an important risk factor for musculoskeletal pain [51]. Interestingly, high work load itself did not unequivocally represent a risk factor for back pain in earlier studies [52, 53, 54].
The high importance of “health” related to back pain or to co-morbidities observed in the CLBP patients of this study likely supports the assumption that it is not the pain intensity itself, but rather the aforementioned struggle against pain, that restricts them from participating in important areas of life [2]. This conclusion is further supported by the high discrepancy observed between importance and success for this life value.
The fewest occurrences were found for “growth and learning”. This result suggests that some patients might consider this life value as less important, or a lack of spare time due to high job demands may restrict their ability to engage in this domain of life. Negative associations between long work hours and work-life balance have been observed before, especially amongst women [55]. Nevertheless, life-long learning is related to a higher quality of life across all age groups, including in elderly people [56].
Analysis of the interviews revealed that, when provided the opportunity to respond in a semi-structured instead of a fully structured format, participants mentioned more external stressors or resources than internal ones. Since the CPVI is designed as a tool related to the Acceptance and Commitment Therapy (ACT) [7], a therapy which has been shown to enhance psychological flexibility [57], it focusses on what patients can influence through values-based action according to their predominant life values. The CPVI focusses on how patients fulfill the role of family member, partner, or friend, and on how they themselves can influence their work, health, and learning and growth. However, patients who participated in this study seemed to be more preoccupied with external factors than with themselves in different roles. Thus, therapy that guides patients to a greater focus on what they can control could lead to important new insights for patients and perhaps a greater sense of responsibility and therefore empowerment. In order to direct patients’ focus towards self-responsible values-based action, the CPVI is a suitable, reliable tool which can be applied easily in a therapeutic context.
The CPVI is not the only important questionnaire that explores life values. For example, the Valued-Living-Questionnaire [58] has 10 items and additionally includes the values: parenting, recreation, spirituality, and citizenship/community life. Different values could play an important role regarding back pain, for example, based on Maslow’s hierarchy of needs [59], or related to Petzold’s five columns of identity [60] which include financial security and ethical values. Although the CPVI seems to be a good tool for examining important values, it could be also useful to ask patients if there are additional values that are important to them, to ensure those value most important to patients for engaging in values-based action are identified.
4.1Limitations and implications for future research
Despite several strengths, some limitations of this study have to be reported. While the interview was designed to be open due to its exploratory nature and as an addition to the use of the CPVI, a fully standardized approach might have resulted in a more comprehensive dataset concerning all six values of life than the semi-structured approach used in this study. In addition, due to the time-intensive nature of the interviews and the skills required to conduct them, the interviews were only carried out with around a third of the participants and all interviews were carried out by one of the authors. We did not test intra-rater reliability because retesting after a few days would bear the likelihood of recall bias and a decreased participants’ motivation to undergo the same examination procedure again. However, testing the intra-rater reliability of this interview would be an interesting aspect in future studies. Taking a closer look at differences in cultural background of the participants was not an aim of this research, but would be an interesting aspect that deserves to be considered in future research. Additionally, it would also be interesting to examine age and gender in this context in future research as these factors have been found to influence restriction due to CLBP [61], and values-based action has been found to be associated with age [11].
4.2Conclusion
The results of this study demonstrated that there is a high practical relevance in identifying the importance and success of relevant life values to CLBP patients. These individual life values provided valuable guides for personalized treatment. The in-depth analysis of the interviews revealed important content related to the values used in the CPVI. The analysis of inhibitors and facilitators provided a broader understanding related to values in life of CLBP patients. The interviews also showed that participants focused more on inhibitors that they do not control, or which would be difficult for them to influence. To address this tendency in patients, acceptance related processes as applied in therapies like ACT could be applied. The CPVI can be used as a tool to change patients’ focus and therefore, facilitate values-based action. Furthermore, it can serve as a tool to examine patients’ facilitators and inhibitors as a starting point for the therapeutic process.
Acknowledgments
The authors thank Savo Ristic for his support during the data collection and Haley Milko for providing English language corrections.
Conflict of interest
None of the authors have any conflict of interest to report. The authors received no financial support for the research, authorship, and/or publication of this article.
References
[1] | Andersson G. Epidemiological features of chronic low back pain. Lancet. (1999) ; 345: : 581–585. doi: 10.1016/S0140-6736(99)01312-4. |
[2] | Gada M. Chronic pain disorder. Archives of Indian Psychiatry. (2007) ; 9: : 1. |
[3] | Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. (2016) ; 9: : 457–467. |
[4] | McCracken LM, Gutiérrez-Martínez O. Processes of change in psychological flexibility in an interdisciplinary group-based treatment for chronic pain based on Acceptance and Commitment Therapy. Behav Res Ther. (2011) ; 49: (4): 267–274. doi: 10.1016/j.brat.2011.02.004. |
[5] | McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain. (2014) ; 15: (3): 221–234. doi: 10.1016/j.jpain.2013.10.014. |
[6] | Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. (2006) ; 44: (1): 1–25. doi: 10.1016/j.brat.2005.06.006. |
[7] | Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy. An experiential approach to behavior change. New York: Guilford Press; (1999) . |
[8] | McCracken LM, Vowles KE. A prospective analysis of acceptance and values in patients with chronic pain. Health Psychology. (2008) ; 27: : 215–220. doi: 10.1037/0278-6133.27.2.215. |
[9] | McCracken LM, Yang SY. The role of values in a contextual cognitive-behavioral approach to chronic pain. Pain. (2006) ; 123: (1): 137–145. doi: 10.1016/j.pain.2006.02.021. |
[10] | Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. J Consult Clin Psychol. (2008) ; 76: (3): 397. doi: 10.1037/0022-006X.76.3.397. |
[11] | McCracken LM, Velleman SC. Psychological flexibility in adults with chronic pain: a study of acceptance, mindfulness, and values-based action in primary care. Pain. (2010) ; 148: (1): 141–147. doi: 10.1016/j.pain.2009.10.034. |
[12] | Vowles KE, McCracken LM, Zhao-O’Brien J. Acceptance and values-based action in chronic pain: a three year follow-up analysis of treatment effectiveness and process. Behav Res Ther. (2011) ; 49: : 748–755. doi: 10.1016/j.brat.2011.08.002. |
[13] | Sarzi-Puttini P, Vellucci R, Zuccaro SM, Cherubino P, Labianca R, Fornasari D. The appropriate treatment of chronic pain. Clin Drug Investig. (2012) ; 32: (1): 21–33. doi: 10.2165/11630050-000000000-00000. |
[14] | World Health Organization. International classification of functioning, disability and health: ICF. Geneva, Switzerland: WHO; (2001) . |
[15] | World Health Organization. ICD-11 for Mortality and Morbidity Statistics. Version: 04/2019. (2019) [cited 2019 Oct 28] Available from: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1326332835. |
[16] | Åkerblom S, Perrin S, Fischer MR, McCracken LM. Further validation of the chronic pain values inventory in a swedish chronic pain sample. J Contextual Behav Sci. (2017) ; 6: (3): 261–267. doi: 10.1016/j.jcbs.2017.06.001. |
[17] | Scott J, Huskisson EC. Graphic representation of pain. Pain. (1976) ; 2: (2): 175–184. doi: 10.1016/0304-3959(76)90113-5. |
[18] | Kane M, Crooks T, Cohen A. Validating measures of performance. Educational Measurement: Issues and Practice. (1999) ; 18: (2): 5–17. doi: 10.1111/j.1745-3992.1999.tb00010.x. |
[19] | Roland M, Fairbank J. The roland-morris disability questionnaire and the oswestry disability questionnaire. Spine. (2000) ; 25: : 3115–3124. |
[20] | Wiesinger GF, Nuhr M, Qittan M, Ebenbichler G, Wölfl G, Fialka-Moser V. Cross-cultural adaptation of the roland-morris questionnaire for german-speaking patients with low back pain. Spine. (1999) ; 24: : 1099–1103. |
[21] | Chibnall JT, Tait RC. The pain disability index: factor structure and normative data. Arch Phys Med Rehabil. (1994) ; 75: (10): 1082–1086. doi: 10.1016/0003-9993(94)90082-5. |
[22] | Dillmann U, Nilges P, Saile H, Gerbershagen HU. Behinderungseinschätzung bei chronischen schmerzpatienten. Der Schmerz. (1994) ; 8: (2): 100–110. doi: 10.1007/BF02530415. |
[23] | Bullinger M. German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA project. Soc Sci Med. (1995) ; 41: (10): 1359–1366. doi: 10.1016/0277-9536(95)00115-N. |
[24] | Mey G, Mruck K. Interviews. In: Mey G, Mruck K, eds. Handbuch qualitative forschung in der psychologie. Wiesbaden, Germany: VS Verlag für Sozialwissenschaften; (2010) . pp. 423–435. |
[25] | R Core Team. R: A language and environment for statistical computing. [Computer program]. R Foundation for Statistical Computing 2019, Vienna, Austria. Available from: http://www.R-project.org/. |
[26] | Fox J, Weisberg S. An {R} Companion to Applied Regression, Second Edition. Thousand Oaks, CA: Sage, (2011) . Available from: http://socserv.socsci.mcmaster.ca/jfox/Books/Companion. |
[27] | Fox J, Weisberg S. Visualizing fit and lack of fit in complex regression models with predictor effect plots and partial residuals. J Stat Softw. (2018) ; 87: (9): 1–27. Available from: doi: 10.18637/jss.v087.i09. |
[28] | Fox J, Weisberg S. An R Companion to Applied Regression, 3rd Edition. Thousand Oaks, CA: Sage; (2019) . Available from: http://tinyurl.com/carbook. |
[29] | Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest package: tests in linear mixed effects models. J Stat Softw. (2017) ; 82: (13): 1–26. doi: 10.18637/jss.v082.i13. |
[30] | Hothorn T, Bretz F, Westfall P. Simultaneous inference in general parametric models. Biom J. (2018) ; 50: (3): 346–363. doi: 10.1002/bimj.200810425. |
[31] | Wickham H. Reshaping data with the reshape package. J Stat Softw. (2007) ; 21: (12). |
[32] | Mayring P. Qualitative Inhaltsanalyse. In: Mey G, Mruck K, eds. Handbuch qualitative forschung in der psychologie. Wiesbaden, Germany: VS Verlag für Sozialwissenschaften; (2010) . pp. 601–613. |
[33] | Mayring P, Fenzl T. Qualitative Inhaltsanalyse. In: Baur N, Blasius J, eds. Handbuch methoden der empirischen sozialforschung. Wiesbaden, Germany: Springer; (2014) . pp. 543–556. |
[34] | Nicholas MK, Linton SJ, Watson PJ, Main CJ. “Decade of the flags” working group. Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther. (2011) May; 91: (5): 737–53. doi: 10.2522/ptj.20100224. |
[35] | Shaw WS, Van der Windt DA, Main CJ, Loisel P, Linton SJ. Early patient screening and intervention to address individual-level occupational factors (“blue flags”) in back disability. J Occup Rehabil. (2009) ; 19: (1): 64–80. doi: 10.1007/s10926-008-9159-7. |
[36] | Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CWC, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. (2018) ; 27: (11): 2791–2803. doi: 10.1007/s00586-018-5673-2. |
[37] | Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, et al. Mental disorders among persons with chronic back or neck pain: results from the world mental health surveys. Pain. (2007) ; 129: (3): 332–342. doi: 10.1016/j.. |
[38] | Hagen EM, Svensen E, Eriksen HR, Ihlebæk CM, Ursin H. Comorbid subjective health complaints in low back pain. Spine. (2006) ; 31: (13): 1491–1495. doi: 10.1097/01.brs.0000219947.71168.08. |
[39] | Hüppe A, Raspe H. Amplifizierte rückenschmerzen und komorbidität in der bevölkerung. Der Schmerz. (2009) ; 23: (3): 275–283. doi: 10.1007/s00482-009-0783-8. |
[40] | Von Korff M, Crane P, Lane M, Miglioretti DL, Simon G, Saunders K, et al. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain. (2005) ; 113: (3): 331–339. doi: 10.1016/j.pain.2004.11.010. |
[41] | Bodenmann G. Dyadic coping and its significance for marital functioning. In: Revenson TA, Kayser K, Bodenmann G, eds. Decade of behavior. Couples coping with stress: emerging perspectives on dyadic coping. Washington, DC, US: American Psychological Association; 1(1); (2005) . pp. 33–50. doi: 10.1037/11031-002. |
[42] | Liebler CA, Sandefur GD. Gender differences in the exchange of social support with friends, neighbors, and co-workers at midlife. Social Science Research. (2002) ; 31: (3): 364–391. doi: 10.1016/S0049-089X(02)00006-6. |
[43] | Wellman B, Wortley S. Different strokes from different folks: community ties and social support. AJS. (1990) ; 96: (3): 558–588. |
[44] | Finlay KA, Peacock S, Elander J. Developing successful social support: an interpretative phenomenological analysis of mechanisms and processes in a chronic pain support group. Psychol Health. (2018) ; 33: (7): 846–871. doi: 10.1080/088704. |
[45] | Keeley P, Creed F, Tomenson B, Todd C, Borglin G, Dickens C. Psychosocial predictors of health-related quality of life and health service utilisation in people with chronic low back pain. Pain. (2008) ; 135: (1–2): 142–150. doi: 10.1016/j.pain.2007.05.015. |
[46] | Naidoo P, Pillay YG. Correlations among general stress, family environment, psychological distress, and pain experience. Percept Mot Skills. (1994) ; 78: (3_suppl): 1291–1296. doi: 10.2466/pms.1994.78.3c.1291. |
[47] | Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med. (2005) ; 62: (12): 851–860. doi: 10.1136/. |
[48] | Feuerstein M, Sult S, Houle M. Environmental stressors and chronic low back pain: life events, family and work environment. Pain. (1985) ; 22: (3): 295–307. doi: 10.1016/0304-3959(85)90030-2. |
[49] | Signs TL, Woods SB. Linking family and intimate partner relationships to chronic pain: an application of the biobehavioral family model. Fam Syst Health. (2020) ; 38: (1): 38–50. doi: 10.1037/fsh0000459. |
[50] | Boone D, Kim SY. Family strain, depression, and somatic amplification in adults with chronic pain. Int J Behav Med. (2019) ; 26: (4): 427–436. doi: 10.1007/s12529-019-09799-y. |
[51] | Amiri S, Behnezhad S. Is job strain a risk factor for musculoskeletal pain? A systematic review and meta-analysis of 21 longitudinal studies. Public Health. (2020) ; 181: : 158–167. doi: 10.1016/j.puhe.2019.11.023. |
[52] | Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. (2000) ; 25: (16): 2114–2125. |
[53] | Macfarlane GJ, Pallewatte N, Paudyal P, Blyth FM, Coggon D, Crombez G. Evaluation of work-related psychosocial factors and regional musculoskeletal pain: results from a EULAR task force. Ann Rheum Dis. (2009) ; 68: (6): 885–891. doi: 10.1136/ard.2008.090829. |
[54] | Hartvigsen J, Lings S, Leboeuf-Yde C, Bakketeig L. Psychosocial factors at work in relation to low back pain and consequences of low back pain; a systematic, critical review of prospective cohort studies. Occup Environ Med. (2004) ; 61: (1): e2. |
[55] | Albertsen K, Rafnsdóttir GL, Grimsmo A, Tómasson K, Kauppinen K. Workhours and worklife balance. Scand J Work Environ Health. (2008) ; 34: (5): 14. |
[56] | Escuder-Mollon P, Esteller-Curto R, Ochoa L, Bardus M. Impact on senior learners’ quality of life through lifelong learning. Procedia Soc Behav Sci. (2014) ; 131: : 510–516. doi: 10.1016/j.sbspro.2014.04.157. |
[57] | Hughes LS, Clark J, Colclough JA, Dale E, McMillan D. Acceptance and commitment therapy (ACT) for chronic pain. Clin J Pain. (2017) ; 33: (6): 552–568. doi: 10.1097/AJP.0000000000000425. |
[58] | Wilson KG, Sandoz EK, Kitchens J, Roberts M. The valued living questionnaire: defining and measuring valued action within a behavioral framework. Psychol Rec. (2010) ; 60: (2): 249–272. doi: 10.1007/BF03395706. |
[59] | Maslow A, Lewis KJ. Maslow’s hierarchy of needs. Salenger Incorporated. (1987) ; 14: : 987. |
[60] | Petzold HG. Integrative therapy in a nutshell – Integrative Therapie kompakt. “Integrative Therapy”: History, development and concepts of an innovative approach to “biopsychosocial”. Psychotherapy and bodyoriented intervention. Internetzeitschrift für Integrative Therapie. (2001) . 1. |
[61] | Fehrmann E, Kotulla S, Fischer L, Kienbacher T, Tuechler K, Mair P. The impact of age and gender on the ICF-based assessment of chronic low back pain. Disabil rehabil. (2018) . 1–10. doi: 10.1080/09638288.2018.1424950. |




