Gait training using the Honda Walking Assist Device® for individuals with transfemoral amputation: A report of two cases
Abstract
BACKGROUND:
Independent walking is important for individuals who have undergone lower limb amputation. Recently, robot-assisted gait training has been widely used for individuals with abnormal gait. However, no study has evaluated the effect of the Honda Walking Assist Device
OBJECTIVE:
This study aimed to investigate the safety, feasibility, and effect of gait training using the HWA for individuals who underwent lower limb amputation.
METHODS:
This study included two elderly patients who underwent TF amputation due to a nontraumatic reason. Gait training interventions using the HWA were performed for a week (5 training sessions). Self-selected walking speed (SWS), step length, cadence, hip kinematic parameters, and symmetricity of single support time ratios during SWS were measured before and after the HWA interventions.
RESULTS:
SWS, step length, cadence, and hip angle range improved after the HWA interventions in both patients. Symmetricity of single support time ratios and maximum hip extension angle improved in patient 1, but not in patient 2. There were no adverse events in either patient.
CONCLUSIONS:
Gait training using the HWA was safe and effective for improving the gait of two TF amputees.
1.Introduction
Independent walking is an important goal for patients who have undergone lower limb amputation. The number of nontraumatic amputations performed increases with age and the presence of comorbidities such as dysvascular amputation [1]. Even though elderly people who have undergone transfemoral (TF) amputation are a major subgroup of amputees [1], they are identified as having a low success rate with prosthetic gait [2].
Gait characteristics of TF amputees include asymmetrical walking pattern [3] and abnormal pelvic movement due to the reduced range of motion (ROM) of the hip [4]. Regarding hip moment at the sagittal plane, TF amputees exhibit higher hip joint power than healthy subjects during the early stance phase in order to progress forward and compensate for the lost anatomical function [5]. For this reason, lower limb amputees required higher energy consumption and more effort to walk. In particular, elderly amputees have low aerobic capacity and slower walking speed [3, 6]; they need to use a wheelchair in their daily lives. Physical activity (e.g., daily step count recorded by pedometer) and physical functions (e.g., 6-minute walking distance, self-selected walking speed, and step length variability) are all related in lower limb amputees [7]. Therefore, improving walking ability using a prosthetic foot is important for improving the activities of daily living (ADL) and quality of life in lower limb amputees.
Recently, the use of robot-assisted gait training has become widespread among individuals with gait disabilities [8, 9, 10]. The Honda Walking Assist Device
Figure 1.
(A) The Honda Walking Assist Device
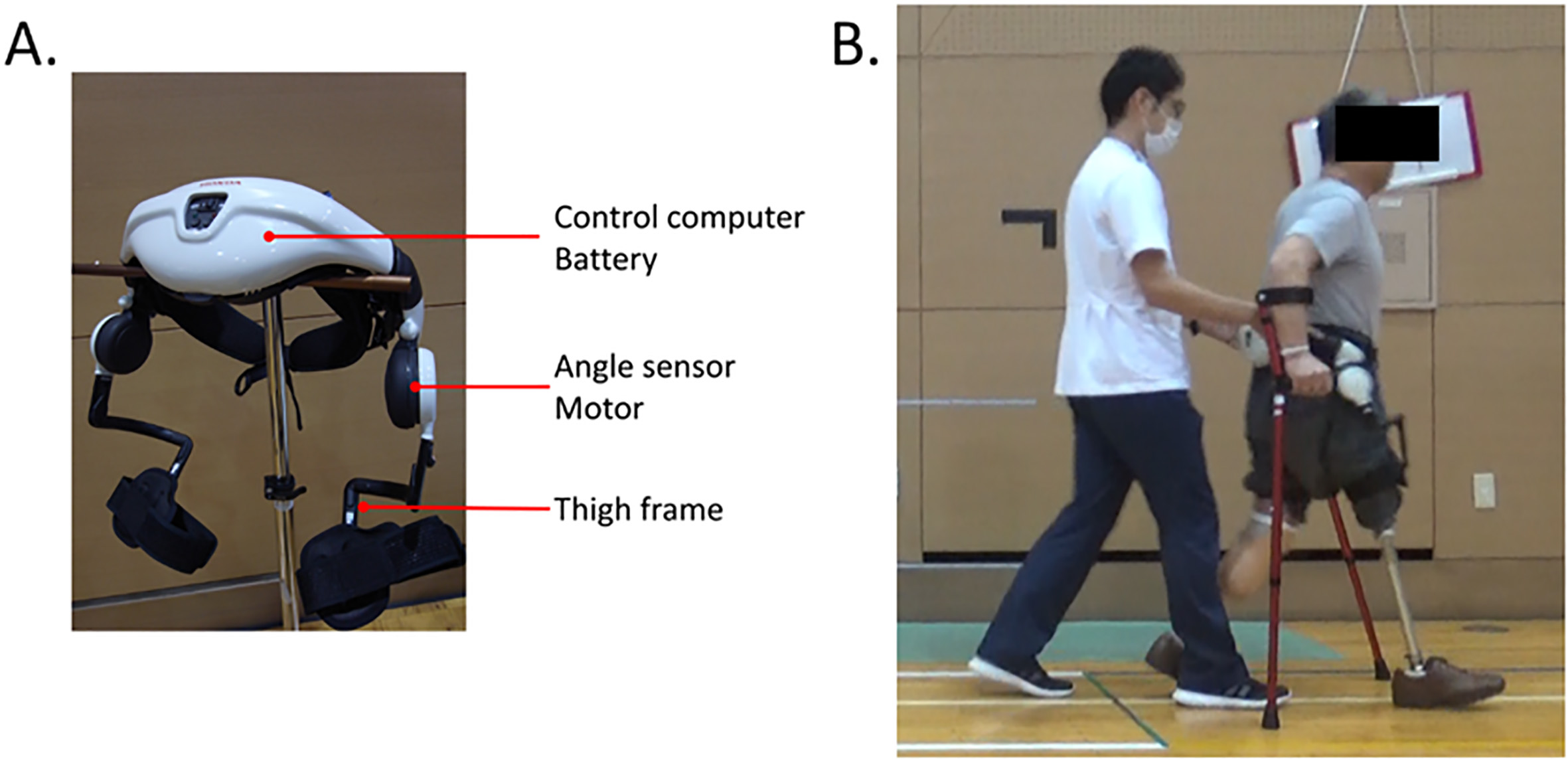
Although the HWA has previously been used as a means of gait training for individuals with stroke [12, 13], there is no study, to the best of our knowledge, that has used the HWA to improve the gait of amputees, i.e., the safety and feasibility of the HWA are unknown in TF amputees who have problems with stump shortness, socket-thigh cuff interference, and high susceptibility to skin problems. In this study, we investigated the safety, feasibility, and efficacy of gait training using the HWA in two amputees.
2.Case presentation
Patient 1: The patient was a 63-year-old man with TF amputation in his right leg and transtibial (TT) amputation in his left leg. Etiologies of his amputations were vascular occlusion due to atrial fibrillation. He started walking exercises with his prosthesis 4 months after undergoing lower limb amputation. He wore the Monolock Knee (Össur, Reykjavik, Iceland) for his right knee and the 1C11 Terion K2 (Ottobock, Duderstadt, Germany) for both feet. The length of his right femoral stump was 18 cm from the ischial tuberosity, and the length of his left tibial stamp was 15 cm from the lower border of the patella. Ten months after amputation surgery (at the start of the HWA intervention), he had mild limitations in right hip extension (0
Patient 2: The patient was a 60-year-old man with TF amputation in his right leg. The etiology was squamous cell carcinoma and related infection. He started walking exercises 2 months after amputation surgery using his prostheses. He wore the 3R41 modular knee joint (Ottobock, Duderstadt, Germany) for his knee and the 1C11 Terion prosthetic (Ottobock, Duderstadt, Germany) for his foot. His stump length was 23.0 cm from the ischial tuberosity. Five months after surgery (at the start of the HWA intervention), he had mild limitations in hip extension (5
Both patients were ambulatory with prostheses and bilateral crutches in the hospital area; however, they both needed a wheelchair to complete their activities of daily living. Gait characteristics included the lack of hip extension at the stance phase and asymmetric weight shift to the TF side, which led to inefficient forward progression. As discussed in the introduction, the HWA assists hip movement and leads to a more symmetric gait, which could be beneficial for these two patients. For this reason, we used the HWA for gait training to improve their gait.
This study was approved by the Ibaraki Prefectural University of Health Sciences Ethics Committee (approval no. e204). Sufficient explanations regarding the study procedures were provided to the patients prior to obtaining their written consent for participation in the study.
2.1Intervention
Gait training interventions using the HWA were performed for 1 week and included five training sessions. Each HWA intervention was performed for approximately 20 minutes, excluding the resting time. The assist torque was set for each intervention based on the level of comfort with walking and on the results of a gait assessment conducted by the physical therapist to obtain optimal walking parameters of the patient. Patients could use bilateral crutches during the HWA interventions to maintain balance. They also underwent conventional rehabilitation for 40–100 min per day, including ROM exercises, stretching, muscle training of the hip joint, and balance exercises, during the intervention period.
When using the HWA, one can choose the normal- or short type thigh frame. To attach the HWA to patients, the normal type thigh frame was used for the TT side in patient 1 and for the healthy side in patient 2. The short type was used for the TF side in both patients, and the fixing belt was fastened over the prosthesis socket. To verify the safety of the interventions, patients were carefully observed during each gait training with the HWA, and any adverse events, such as hip pain or skin problems (redness or scarring due to contact with equipment), were noted.
Table 1
Gait parameter and gait pattern measurements
| Patient 1 | Patient 2 | |||
|---|---|---|---|---|
| Parameter | Pre-HWA | Post-HWA | Pre-HWA | Post-HWA |
| SWS (m/s) | 0.74 | 0.87 | 0.65 | 0.85 |
| Step length (m) | 0.49 | 0.54 | 0.43 | 0.54 |
| Cadence (step/min) | 90.7 | 96.4 | 90.1 | 94.6 |
| Symmetricity of single support time ratios | 0.75 | 0.80 | 0.77 | 0.73 |
SWS, self-selected walking speed; HWA, Honda Walking Assist Device
Table 2
Results of the hip angle during self-selected walking at the trans-femoral side
| Patient 1 | Patient 2 | |||
|---|---|---|---|---|
| Pre-HWA | Post-HWA | Pre-HWA | Post-HWA | |
| Maximum hip extension angle ( | 10.2 | 16.4 | 4.0 | 4.5 |
| Maximum hip flexion angle ( | 25.2 | 30.5 | 23.3 | 30.5 |
| Hip angle range during one gait cycle ( | 35.5 | 46.8 | 27.3 | 35.0 |
HWA, Honda Walking Assist Device
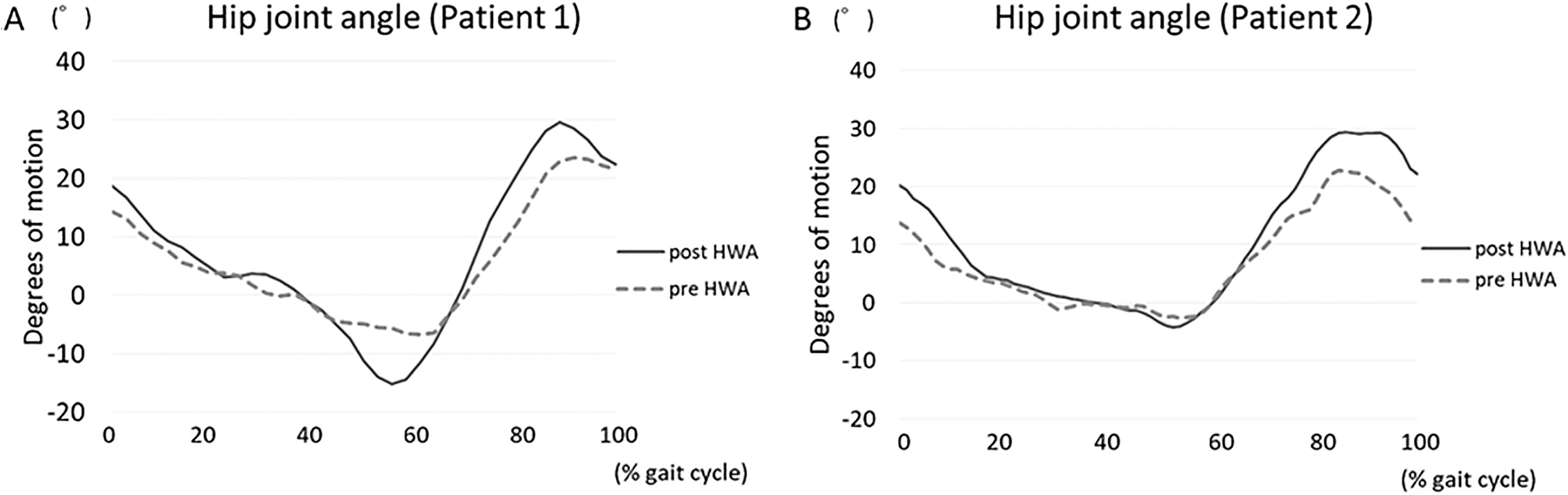
Figure 2.
The hip joint angle during the SWS in the sagittal plane. Hip joint angles was the average angle obtained during the three walking cycles. Moving average smoothing was used to draw the figure. The dotted line indicates the pre-intervention, whereas the solid line indicates the post-intervention of the hip joint angle. Figure 2A shows Patient 1 and Fig. 2B shows Patient 2. HWA, Honda Walking Assist Device
2.2Measurements
Gait parameters and gait patterns without the HWA were measured before and after HWA interventions. Gait parameters (walking speed, step length, and cadence) and gait patterns were measured at the self-selected walking speed (SWS). SWS tests were conducted twice on a walking path that was 10 m in length, with an additional 3-m length before and after the 10-m measurement. Walking aids and settings of the prostheses were under the same conditions for all interventions. To calculate step length and cadence, the number of steps taken during the SWS tests was counted. The average values of the two trials were designated as the SWS, step length, and cadence, respectively. The symmetricity of the single support time ratios (right single support time/left single support time) was calculated to evaluate gait symmetricity.
To analyze the gait pattern, patient motions were recorded on a digital video camera (Handycam, Sony, Tokyo, Japan) in the sagittal plane. We analyzed three consecutive walking cycles using two-dimensional motion analysis software (Frame Dias V, DKH, Tokyo, Japan). The hip joint angle during the gait was formed by the acromion-greater trochanter-knee joint of the prosthesis. The maximum hip extension joint angle at the stance phase, maximum hip flexion angle at the swing phase, and hip flexion/extension range (hip range) during walking were compared. In patient 1, the patient wore a bilateral prosthesis. Here, we focused on the side of the TF amputation for the video analysis because the hip of the TF amputation side had a limited ROM and muscle weakness, whereas that of the TT amputation side was more intact.
3.Results
Interventions were successfully completed in both patients, and neither patient experienced skin trouble or pain during all gait trainings with the HWA. The HWA was attached on the socket of the TF side sing the short type thigh frame. Patients stated no complaints regarding this intervention.
Table 1 shows results of gait parameters and symmetricity of single support time ratios at the SWS. In both patients, walking speed, step length, and cadence after the HWA interventions increased compared to the measurements taken before the interventions. Symmetricity of single support time ratios increased from 0.75 to 0.80 in patient 1 but decreased from 0.77 to 0.73 in patient 2.
Figure 2 shows the right hip flexion and extension angle during the SWS. Table 2 shows the maximum hip flexion, extension angle, and hip joint range during the SWS. In both patients, the hip joint range after the HWA increased compared to the range before the interventions. In patient 1, both the maximum hip flexion and extension angle increased; however, in patient 2, only the maximum hip flexion angle increased.
4.Discussion
In this study, we investigated the safety, feasibility, and effectiveness of gait training using the HWA in two TF amputees. Though both patients had a short stump length, it was possible to install the thigh frame on the prostheses. We were able to perform all interventions safely, and there were no adverse events. Therefore, it is suggested that HWA intervention is a safe and feasible means of improving gait in patients who have undergone TF amputees.
SWS, step length, and cadence improved after the HWA interventions in both patients. The hip angle range increased after the HWA interventions compared to the range before the interventions. In general, if the hip joint angle during walking is extended, the step length becomes wider, and a wider step length contributes to a faster SWS. From our results, the HWA interventions increased the hip joint range during walking, which contributed to the increased step length and improved walking speed.
Symmetricity of single support time ratios increased in patient 1, but not in patient 2. We think that this variance is caused by the difference in patients’ impairments. Patient 1 had TF amputation in his right leg and TT amputation in his left leg, while patient 2 had TF amputation in his right leg and fully intact left leg. Patient 1 had impairments in both legs, so he might need restraints in both legs; however, patient 2 did not need restraints in his left side. This might lead to the residual asymmetry in patient 2. To verify this state, we are going to accumulate additional number of patients including hemilateral and bilateral amputees for further studies.
In general, individuals with TF amputations who use a wheelchair in their daily life have joint contractures and muscle weakness caused by hip flexion during wheelchair use. Hip flexion and extension angles during walking are smaller in the TF amputated side than in the healthy side [14]. Moreover, in the hip joint of the amputated side, increased muscle activity and a greater muscle power peak are needed to compensate for the absence of the rocker function [15]. The excessive work produced by the hip may further contribute to the increased energy expenditure that is required for the lower limb amputees to proceed forward while walking [5]. These problems negatively impact the patient’s walking ability and hinder their gait improvement. In order to solve these problems, traditional approaches, such as stretching [16], muscle strengthening of the hip joint [17, 18], proprioceptive neuromuscular facilitation (PNF) techniques [19], and balance exercises [16], can be conducted. The characteristic of the HWA is to lead walking to a correct walking pattern by assisting the flexion/extension movements of the hip joint. Our results suggest that the HWA assisted the hip joint extension muscle and increased the hip joint extension moment during the early stance phase. Additionally, the device assisted in the gait timing to allow effective and efficient forward progression. We believe that the HWA intervention contributes to walking ability through these assistances.
Our gait training interventions using the HWA were performed for only 1 week and included five training sessions. For this reason, although HWA training improved gait parameters and patterns, the patients’ ADL did not change significantly. In the future, we need to verify whether HWA training contributes to ADL improvement with lager sample size.
The limitation of this study is that we included only 2 cases without control group, and evaluated the patients before and after the intervention period. To generalize our results, we need to accumulate additional number of patients with control group to develop a comparative study. Nonetheless, we think our study is important as an opening for further investigation.
5.Conclusions
As the life expectancy continues to increase, the number of elderly lower limb amputees with dysvascularity or other comorbidities is also expected to increase. Elderly individuals tend to have lower success rates for gait improvement. We suggest that the HWA intervention is an effective means of gait training for such individuals.
Acknowledgments
This work was partly supported by a Grant-in-Aid for Project Research of the Ibaraki Prefectural University of Health Sciences (1961-1, 1962-1) and Japan Society for the Promotion of Science KAKENHI (19H00479). We would like to thank the Physical Therapy Department at Ibaraki Prefectural University of Health Sciences Hospital, represented by Professor Kazuhide Tomita, the manager of Department of Rehabilitation, and Assistant Professor, Tomoyuki Matsuda, the manager of the Department of Physical Therapy.
Conflict of interest
Honda Motor Corporation lent us the HWA free of charge for this research.
References
[1] | Cumming JC, Barr S, Howe TE. Prosthetic rehabilitation for older dysvascular people following a unilateral transfemoral amputation. Cochrane Database Syst Rev. (2015) ; 1: : CD005260. doi: 10.1002/14651858.CD005260.pub3. |
[2] | Davies B, Datta D. Mobility outcome following unilateral lower limb amputation. Prosthet Orthot Int. (2003) ; 27: : 186. |
[3] | Jaegers S.M, Arendzen JH, de Jongh HJ. Prosthetic gait of unilateral transfemoral amputees: a kinematic study. Arch Phys Med Rehabil. (1995) ; 76: : 736. |
[4] | Sagawa Y Jr., Turcot K, Armand S, Thevenon A, Vuillerme N, Watelain E. Biomechanics and physiological parameters during gait in lower-limb amputees: a systematic review. Gait Posture. (2011) ; 33: : 511. doi: 10.1016/j.gaitpost.2011.02.003. |
[5] | McNealy LL, Gard SA. Effect of prosthetic ankle units on the gait of persons with bilateral trans-femoral amputations. Prosthet Orthot Int. (2008) ; 32: : 111. doi: 10.1080/02699200701847244. |
[6] | Wezenberg D, van der Woude LH, Faber WX, de Haan A, Houdijk H. Relation between aerobic capacity and walking ability in older adults with a lower-limb amputation. Arch Phys Med Rehabil. (2013) ; 94: : 1714. doi: 10.1016/j.apmr.2013.02.016. |
[7] | Lin SJ, Winston KD, Mitchell J, Girlinghouse J, Crochet K. Physical activity, functional capacity, and step variability during walking in people with lower-limb amputation. Gait Posture. (2014) ; 40: : 140. doi: 10.1016/j.gaitpost.2014.03.012. |
[8] | Lo K, Stephenson M, Lockwood C. Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients: a systematic review. JBI Database System Rev Implement Rep. (2017) ; 15: : 3049. doi: 10.11124/JBISRIR-2016-002957. |
[9] | Holanda LJ, Silva PMM, Amorim TC, Lacerda MO, Simao CR, Morya E. Robotic assisted gait as a tool for rehabilitation of individuals with spinal cord injury: a systematic review. J Neuroeng Rehabil. (2017) ; 14: : 126. doi: 10.1186/s12984-017-0338-7. |
[10] | Yoshikawa K, Mutsuzaki H, Sano A, Koseki K, Fukaya T, Mizukami M, et al. Training with Hybrid Assistive Limb for walking function after total knee arthroplasty. J Orthop Surg Res. (2018) ; 13: : 163. doi: 10.1186/s03018=018-0875-1. |
[11] | Koseki K, Mutsuzaki H, Yoshikawa K, Endo Y, Maezawa T, Takano H, et al. Gait training using the Honda Walking Assistive Device® in a patient who underwent total hip arthroplasty: A single-subject study. Medicina (Kaunas). (2019) ; 55: : E69. doi: 10.3390/medicina55030069. |
[12] | Buesing C, Fisch G, O’Donnell M, Shahidi I, Thomas L, Mummidisetty CK, et al. Effects of a wearable exoskeleton stride management assist system (SMA®) on spatiotemporal gait characteristics in individuals after stroke: a randomized controlled trial. J Neuroeng Rehabil. (2015) ; 12: : 69. doi: 10.1186/s12984-015-0062-0. |
[13] | Tanaka N, Matsushita S, Sonoda Y, Maruta Y, Fujitaka Y, Sato M. et al. Effect of stride management assist gait training for poststroke hemiplegia: A single center, open-label, randomized controlled trial. J Stroke Cerebrovasc Dis. (2019) ; 28: : 477. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.025. |
[14] | Devan H, Carman A, Hendrick P, Hale L, Ribeiro DC. Spinal, pelvic, and hip movement asymmetries in people with lower-limb amputation: Systematic review. J Rehabil Res Dev. (2015) ; 52: : 1. doi: 10.1682/JRRD.2014.05.0135. |
[15] | Sadeghi H, Allard P, Duhaime PM. Muscle power compensatory mechanisms in below-knee amputee gait. Am J Phys Med Rehabil. (2001) ; 80: : 25. |
[16] | Esquenazi A, DiGiacomo R. Rehabilitation after amputation. J Am Podiatr Med Assoc. (2001) ; 91: : 13. |
[17] | Visser J, McCarthy I, Marks L, Davis RC. Is hip muscle strength the key to walking as a bilateral amputee, whatever the level of the amputations? Prosthet Orthot Int. (2011) ; 35: : 451. doi: 10.1177/0309364611422268. |
[18] | Nolan L. A training programme to improve hip strength in persons with lower limb amputation. J Rehabil Med. (2012) ; 44: : 241. doi: 10.2340/16501977-0921. |
[19] | Yigiter K, Sener G, Erbahceci F, Bayar K, Ulger OG, Akdogan S. A comparison of traditional prosthetic training versus proprioceptive neuromuscular facilitation resistive gait training with trans-femoral amputees. Prosthet Orthot Int. (2002) ; 26: : 213. |




