An 18-month follow-up study on the effect of a neuromuscular stabilization technique on Cobb’s angle in adolescent idiopathic scoliosis: A single-blind, age-matched controlled trial
Abstract
BACKGROUND:
The benefits of spinal realignment and stabilization in scoliosis need to be examined.
OBJECTIVE:
We aimed to investigate the long-term effect of a neuromuscular stabilization technique (NST) on Cobb’s angle in patients with adolescent idiopathic scoliosis.
METHODS:
Twenty females recruited from two hospitals participated in this study. On the basis of convenience of location, participants were allocated to either the experimental group (EG) that underwent the NST, or the control group (CG) that received education for a home exercise program. The NST for the EG was performed for an average of 30 min per session, three times a week for six months, and consisted of spinal realignment and stabilization. Then, 12- and 18-month measurements for long-term follow-ups were conducted for the EG. The outcome measure was Cobb’s angle.
RESULTS:
Between-group comparison revealed a statistically significant difference at post-test (
CONCLUSION:
This study shows that the NST may be a beneficial option to correct spinal alignments in patients with adolescent idiopathic scoliosis.
1.Introduction
Idiopathic scoliosis is a typical spine disease in adolescents characterized by a three-dimensional spinal deformity [1], which results in respiratory complications, decreased functional capacity, and poor cosmetic appearance [2]. In addition, given that scoliosis is frequently developed due to poor posture, it has also been associated with musculoskeletal trauma such as low back pain, herniation of the intervertebral disc, and sciatic nerve disease [3].
Treatments for adolescent idiopathic scoliosis aim to restore spinal mobility by correcting the alignment of the spinal segments, and optimizing the mechanical interaction in the spine and trunk to promote healing. However, the correction of misaligned spinal segments may not be the best solution to fully treat the symptoms caused by scoliosis. Further steps are needed to facilitate neuromuscular control to prevent the displacement of spinal segments to the pre-treatment positions after its correction. Therefore, exercise therapy should be performed to strengthen the deep trunk-stabilizing muscles, which helps to maintain the position of each segment after the spinal correction [3].
Because segmental instability leads to back pain and disability, it is also important to establish spinal stability [4]. Strengthening of the deep trunk-stabilizing muscles helps reduce spinal deformation and asymmetric loading on the vertebrae, thereby stabilizing the positions of spinal segments. Furthermore, it may help to enhance curve magnitude and postural symmetry, subsequently improving spinal mobility and preventing spinal disorders and their recurrence [5]. In general, physical therapy, manual therapy, exercise therapy, and postural training have been applied as therapeutic interventions to prevent these problems [3].
Traditionally, bracing and exercise therapy have been used to facilitate postural correction, prevent additional curve progression, treat spinal pain, and reduce cosmetic problems in adolescent idiopathic scoliosis [6]. However, bracing often results in undesirable impacts such as psychological stress, discomfort in daily activities, negative self-esteem [7], and impaired respiratory function [8]. Furthermore, the effectiveness of exercise therapy is still controversial, although it has been well received as a conservative management for adolescent idiopathic scoliosis [9]. While surgery can be performed to correct spinal deformities, it does not necessarily result in positive outcomes [10], and is less effective for mild scoliosis. Patients often complain of fear due to invasive surgical procedures, post-surgical pain, risk of complications, and a longer recovery time.
The restoration of a neutral position in segmental joints is necessary to facilitate neuromuscular control of the trunk, which is more likely caused by exact treatment [11]. Therefore, the treatment of adolescent idiopathic scoliosis requires a scoliosis-specific treatment course that focuses on the correction of segmental positions in the spine and the improvement of neuromuscular stabilization [12]. However, to the best of our knowledge, there has been no research interest in the integration of joint alignment correction and spinal stabilizing techniques as an optimal treatment for scoliosis, and therefore there is a lack of appropriate protocols to treat spinal deformities in patients with scoliosis. Accordingly, this study aimed to illustrate the detailed procedure of the neuromuscular stabilization technique (NST) for adolescents with idiopathic scoliosis, and to report results using Cobb’s angle.
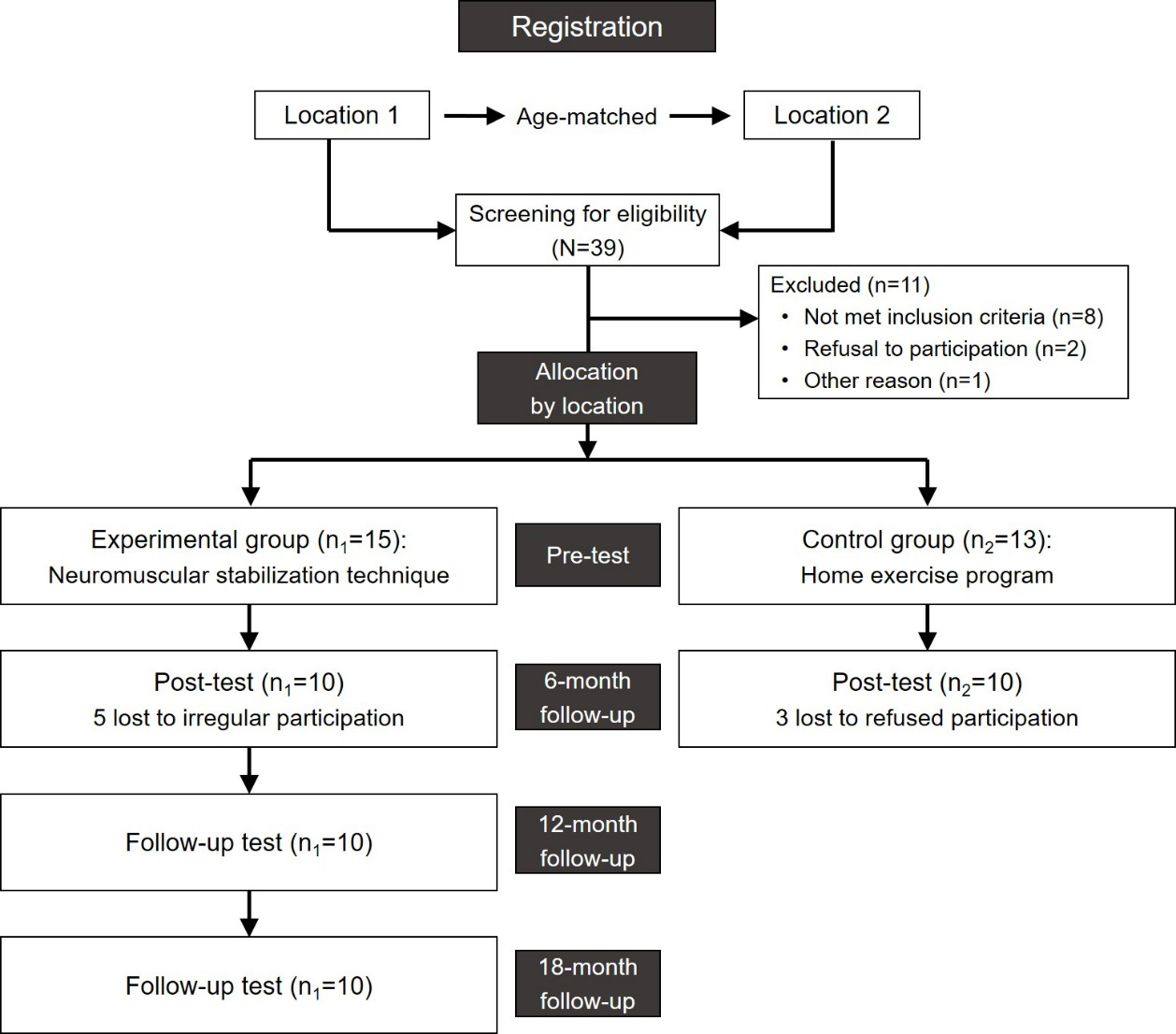
Figure 1.
Study diagram.
2.Methods
2.1Participants
Twenty females with left lumbar scoliosis volunteered to participate in this study. Ten participants were allocated to the experimental group (EG) and ten were allocated to the control group (CG) (Table 1). The inclusion criteria were: (1) lateral curvature of the lumbar region (Cobb’s angle
2.2Study design
This study was a single-blind, age-matched controlled trial, in which the assessors who performed the data collection were unaware of the group allocations. We compared the results of two hospitals that offered different treatment methods. Two hospitals that agreed to participate in our research program were chosen from different regions. One hospital was selected for the EG, in which 10 patients underwent our intervention. In addition, 10 age-matched participants were recruited from another hospital for the CG. Participants of the CG were paired within three years for the average age of the group. Participants of the EG underwent the NST for six months for correcting spinal alignments. Participants of the CG received education for a corrective exercise program in the first visit. All participants in both groups completed the pre- and post-tests, and additional follow-up measurements (12- and 18-month) were performed only for participants of the EG (Fig. 1).
2.3Outcome measures
The intervention effect was measured using Cobb’s angle, which is a common measurement for identifying the extent of scoliosis. Cobb’s angle was defined as the angle between lines parallel to the superior margin of the upper vertebral body and the inferior margin of the lower vertebra of the lateral curvature of the spine [14]. Intra- and inter-rater reliabilities were reported with intra-class correlation coefficients of 0.970 and 0.969, respectively [15].
2.4Procedures
X-ray examinations were performed to screen participants, which included anteroposterior views of the whole spine in the standing position with upright and bending of the trunk to both sides. In cases of a double major type of scoliosis, spinal alignment was tested by using views with side bending of the trunk in order to identify the major lumbar curvature. Based on the examination of the side-bending views, the lumbar type of scoliosis was determined when spinal alignment was not corrected in the lumbar region [16].
Table 1
Details of the neuromuscular stabilization technique
| Steps | Details |
|---|---|
| Manual contact | Manual contact is made by touch using the palmar side of the proximal phalangeal base of the index finger against the prominent transverse process of the apex vertebra on the convex side. |
| Correction of spinal alignment | While the participant straightens their trunk, the therapist applied a force towards the midline of the trunk by pushing the transverse process using a hand in contact for further correction, and the participant’s shoulders were anchored using the other arm and hand. Repetitions: twenty repetitions with a 10 second hold. |
| Segmental stabilization | The participants contract their spinal muscles of each segment on the convex side to maintain the corrected spinal alignment. Repetitions: twenty repetitions with a 10 second hold. |
| Sensory-motor training | The participants hold this posture while slightly pushing the upper part of their trunk back and forth. Repetitions: application of a 10 second resistance towards each direction. Repetitions: five series of ten repetitions for each direction. |
Figure 2.
The neuromuscular stabilization technique steps. (A) manual contact, (B) correction of spinal alignment, (C) segmental stabilization, and (4) sensory-motor training.
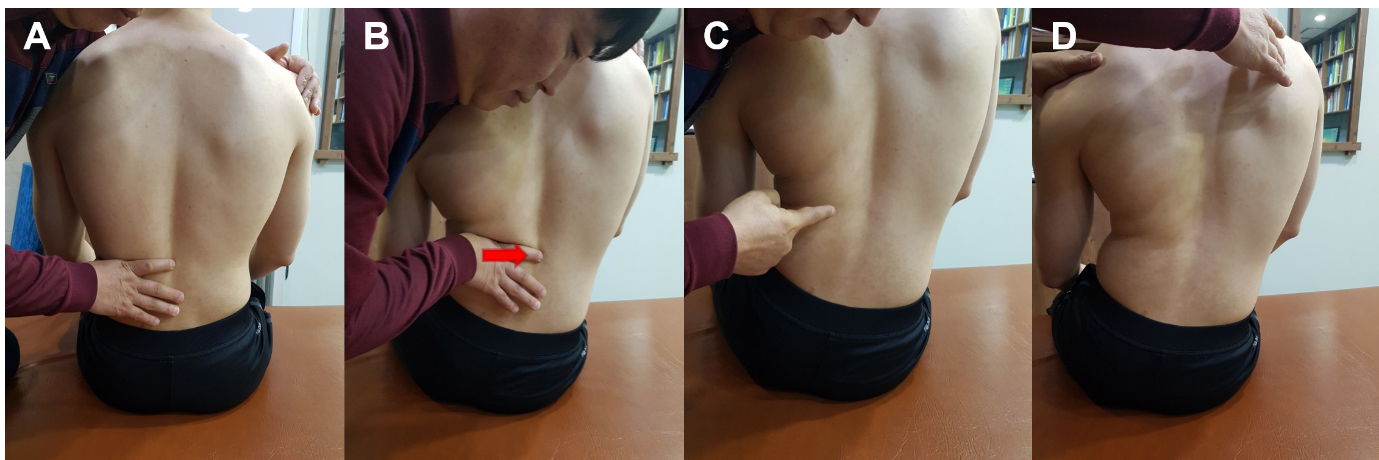
The NST for participants of the EG consisted of four steps: (1) manual contact, (2) correction of spinal alignment, (3) segmental stabilization, and (4) sensory-motor training (Fig. 2). The technique was performed with participants seated on a chair without arm and back rests. After manual contact on the transverse process (TP) of the convex side, the therapist often used joint mobilization of grade II or III in the second step to correct the spinal alignment as needed to facilitate segmental mobility. In the steps for active segmental stabilization, the therapist also offered minimal guidance using tactile stimulation to encourage the participants for segmental stabilization. The technique was then maintained during the sensory-motor training, which uses trunk perturbation to create more challenging conditions. The NST was performed for a period of 30 minutes on average, including rest intervals between the techniques, three times a week for six months. Follow-up measurement sessions for participants of the EG were carried out at 12 and 18 months. Moreover, participants of the EG underwent the NST once a week for a period of follow-ups. The first author with a 20-year long career as a physiotherapist was in charge of the whole NST process. Detailed information of the NST can be found in Table 1.
The corrective exercise program for CG participants comprised of pelvic tilt, alternate arm-leg raising on the floor, back extension, trunk side-bending on the convex side, cow pose exercise (neck and trunk extension with anterior pelvic tilting), and abdominal press [17], which were taught to patients during their first visit to the hospital. A flyer and check sheets with detailed information of the exercise program for regular performance at home were offered to improve compliance at home. A physical therapist confirmed the check sheets during patients’ regular visits to the hospital (once a month).
2.5Data analysis
Cobb’s angles collected from the participants of the EG and CG were analyzed by using the Statistical Package for the Social Sciences version 24.0 (SPSS Inc., Chicago, IL, USA). Data collected from the groups appeared to be normally distributed in the Shapiro-Wilk test (EG:
3.Results
3.1General characteristics of the participants
The age, height, and weight of the participants were not significantly different between the EG and CG (
3.2Comparison of pre- and post-test on Cobb’s angles between the groups
Table 2
General characteristics of the participants
| EG ( | CG ( |
| |
|---|---|---|---|
| Age (years) | 14.50 | 15.90 | |
| Height (cm) | 153.50 | 156.60 | |
| Weight (kg) | 49.20 | 48.30 | |
| Risser grade | 5/3/1/1 | 4/4/2/0 |
Table 3
Comparison of the pre- and post-test on Cobb’s angles between the groups
| Experimental group ( | Control group ( |
| |||||
|---|---|---|---|---|---|---|---|
| Pre-test | Post-test |
| Pre-test | Post-test |
| ||
| Values | 16.56 | 11.00 | 7.89 | 18.90 | 17.50 | 8.57 | |
| Ranges | 12–20 | 3–16 | 12–27 | 10–25 | |||
The results of the comparison of the pre- and post-test data between the EG and CG are shown in Table 2, and changes in Cobb’s angles across the follow-up sessions in the EG are shown in Fig. 2. Between-group comparison revealed a statistically significant difference at post-test (
4.Discussion
This study showed that the NST may be favorably used to restore spinal alignment in adolescents with idiopathic scoliosis.
In these patients, the therapeutic goal is to have the patients counteract the asymmetric loading on the spine and trunk [18]; therefore, it is important to develop appropriate methods for correcting poor spinal alignment during daily life, and optimize the load transfer on the spine This can be largely achieved via a manual technique and exercise therapy, which enhance the mobility and stability of axial structures and thereby normalize the function of spinal musculatures. Based on this concept, the NST used in this study focused on restoring the neutral position of spinal joints, and then facilitated active efforts for segmental stabilization to maintain their position.
In general, Cobb’s angle measured from the anterior-posterior X-ray image of the whole spine was useful to evaluate the extent of the lateral curvature in patients with scoliosis, by monitoring the stage of spinal deformity and curve progression. Curve progression in patients with scoliosis is related to their age and the extent of Cobb’s angle [19]. Because adolescents have a greater growth potential than adults, it is more likely to aggravate spinal deformity during growth. Therefore, it is important to establish benefits from treatments as rapidly as possible in order to prevent unwanted effects of scoliosis. A Cobb’s angle with a
Figure 3.
Changes in Cobb’s angles across the follow-up sessions in the experimental group. Bars indicate standard deviation. * indicates significant differences in comparison to the pre-test, and ** indicates significant differences in comparison to the post-test (six month follow-up).
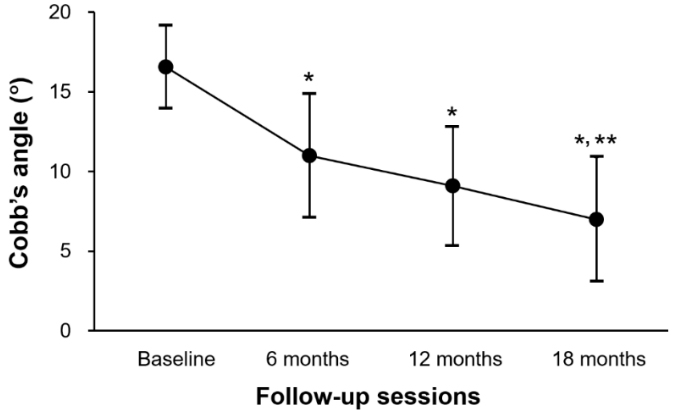
Our primary finding was the greater effects in the EG than in the CG, although significant improvement of Cobb’s angle was found in both groups after intervention. In general, supervision is considered to be necessary for improved efficacy of exercise therapy, helping patients to precisely perform the exercise and facilitate its compliance [21]. Therefore, as used in the CG, an unsupervised home exercise program may have disadvantages because of the lack of supervision.
Adolescents with idiopathic scoliosis frequently complain of a significant limitation on functional performance and ventilatory capacity, which is proportional to its severity [22, 23]. Furthermore, a recent study has reported that postural control strategies during activities may be correlated to the severity of scoliosis [24]. As shown in this study, the NST was beneficial for correcting spinal alignment in adolescent idiopathic scoliosis, with more gains after long-term use. Therefore, it may also be presumed that the enhancement of pulmonary capacity and exercise performance was obtained from our intervention, even though we did not measure these parameters.
Recent studies have shown that the integration of scoliosis-specific exercise therapy, such as the Schroth method, into standard care is superior to standard care alone to decrease curve severity in adolescent idiopathic scoliosis [6, 25, 26, 27]. These studies also demonstrated auto-correction in three dimensions including postural correction and stabilization, normalization of breathing patterns, and patient education [6, 28]. In addition, side-shift and hitch exercises have been demonstrated to correct spinal posture after repeatedly moving the lateral shift of the trunk to the concave side of the curve and then lifting the heel on the convex side with a straight leg to maintain the side-shifted position [29]. Although these exercises focus on regional straightening in the spine, it is difficult to recognize the exact correction of the segmental level.
In the treatment of scoliosis, patients frequently need a direct technique that aims to control segmental alignment in the spine by restoring the neutral position of spinal joints and subsequently stabilizing it prior to its integration in daily life, which may help to facilitate the rapid correction of the spine [30]. This idea is supported by a recent study demonstrating the benefits of chiropractic and exercise therapy that focused on segmental correction in the spine and strengthening spinal muscles, although it was not specific for segmental stabilization [3]. Based on this concept, our findings showed great benefits to improving the symptoms of adolescents with idiopathic scoliosis, particularly after long-term use. Furthermore, the NST, which includes segmental correction and stabilization, might be a client-friendly approach with a relatively shorter treatment time [12]; therefore, it is suggested that the NST may be appropriate for integration into standard care, similar to that demonstrated by a brace and scoliosis-specific exercises, such as the Schroth method, at a higher level of evidence [31].
We acknowledge several limitations of this study that can be enhanced by further studies. First, our sample size was relatively small; therefore, the generality of our results may be difficult to expand beyond our sample group. However, based on our results, a power analysis (power of the study, 1-
5.Conclusion
In adolescent idiopathic scoliosis, professional techniques that aim to restore the alignment of spinal joints and facilitate the stabilization effort for its maintenance cover the whole symptomatic spectrum related to spinal deformity. This study reports the use of the NST as a novel treatment approach for adolescent idiopathic scoliosis, and the findings suggest that the NST can make significant changes in Cobb’s angle, with more gains after longer-term follow-ups. Therefore, the NST may be used as a practicable alternative to routine treatment protocols for patients with adolescent idiopathic scoliosis. Further studies with a more robust design are needed to describe optimal treatment strategies using the NST in order to demonstrate its effects on various aspects of adolescent idiopathic scoliosis.
Conflict of interest
None to report.
References
[1] | Weiss HR, Moramarco M. Scoliosis: Treatment indications according to current evidence. OA Musculoskeletal Medicine. (2013) ; 1: : 1. |
[2] | Sperandio EF, Alexandre AS, Yi LC, Poletto PR, Gotfryd AO, Vidotto MC, et al. Functional aerobic exercise capacity limitation in adolescent idiopathic scoliosis. Spine J. (2014) ; 14: (10): 2366-2372. |
[3] | Cheon M, Park J, Lee Y, Lee J. Effect of chiropractic and lumbar exercise program on lumbar muscle strength and Cobb’s angle in patients with scoliosis for u-Healthcare. EURASIP Journal on Wireless Communications and Networking. (2013) ; 132. |
[4] | Julie AH, Gwendolen AJ, Long-term effects of specific stabilizing exercise for first-episode low back pain. Spine. (2001) ; 26: : 243-248. |
[5] | Gür G, Ayhan C, Yakut Y. The effectiveness of core stabilization exercise in adolescent idiopathic scoliosis: A randomized controlled trial. Prosthet Orthot Int. (2017) ; 41: (3): 303-310. |
[6] | Negrini S, Aulisa AG, Aulisa L, Circo AB, de Mauroy JC, Durmala J, et al. 2011 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. (2012) ; 7: (1): 3. |
[7] | Durmała J, Blicharska I, Drosdzol-Cop A, Skrzypulec-Plinta V. The level of self-esteem and sexual functioning in women with idiopathic scoliosis: A preliminary study. Int J Environ Res Public Health. (2015) ; 12: (8): 9444-9453. |
[8] | Koumbourlis AC. Scoliosis and the respiratory system. Paediatr Respir Rev. (2006) ; 7: (2): 152-160. |
[9] | Negrini S, Carabalona R. Social acceptability of treatments for adolescent idiopathic scoliosis: A cross sectional study. Scoliosis. (2006) ; 1: : 14. |
[10] | Westrick ER, Ward WT. Adolescent idiopathic scoliosis: 5-year to 20-year evidence-based surgical results. J Pediatr Orthop. (2011) ; 31: (1 Suppl): S61-68. |
[11] | Oh DW, Won SH, Park HJ, Kang TW, Shim JH. Novel approach for functional improvement of patients with chronic stroke: Theoretical background of ‘Neuromuscular Control and Reset’ concept. Kor J Neuromuscul Rehabil. (2017) ; 7: (2): 26-43. |
[12] | Won SH, Effects of the ‘Segmental Translation of Spine (STS)’ approach on Cobb’s angle and vital capacity in adolescences with idiopathic scoliosis. The Graduate School, Chonbuk National University. (2016) . |
[13] | Smith JR, Sciubba DM, Samdani AF. Scoliosis: A straightforward approach to diagnosis and management. JAAPA. (2008) ; 21: (11): 40-45. |
[14] | Coley BD. Caffey’s Pediatric Diagnostic Imaging, 12 |
[15] | Gstoettner M, Sekyra K, Walochnik N, Winter P, Wachter R, Bach CM. Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools. Eur Spine J. (2007) ; 16: (10): 1587-1592. |
[16] | Malfair D, Flemming AK, Dvorak MF, Munk PL, Vertinsky AT, Heran MK, et al. Radiographic evaluation of scoliosis: Review. AJR Am J Roentgenol. (2010) ; 194: (3): S8-S22. |
[17] | Kisner C, Thorp JN. The spine: Exercise and manipulation interventions. In: C. Kisner, L.A. Colby, eds. Therapeutic Exercise: Foundations and Techniques. Philadelphia: FA Davis, (2012) ; pp. 498-450. |
[18] | Stokes IA, Burwell RG, Dangerfield PH. Biomechanical spinal growth modulation and progressive adolescent scoliosis-a test of the ‘vicious cycle’ pathogenetic hypothesis: Summary of an electronic focus group debate of the IBSE. Scoliosis. (2006) ; 1: : 16. |
[19] | Horne JP, Flannery R, Usman S. Adolescent idiopathic scoliosis: Diagnosis and management. Am Fam Physician. (2014) ; 89: (3): 193-198. |
[20] | Silva FE, Lenke LG. Adolescent idiopathic scoliosis. Surgical management of spinal deformities. Philadelphia: Saunders Elsevier, (2009) ; pp. 97-118. |
[21] | Kim EY, Kim SY, Oh DW. Pelvic floor muscle exercises utilizing trunk stabilization for treating postpartum urinary incontinence: Randomized controlled pilot trial of supervised versus unsupervised training. Clin Rehabil. (2012) ; 26: (2): 132-141. |
[22] | Saraiva BMA, Araujo GS, Sperandio EF. Impact of scoliosis severity on functional capacity in patients with adolescent idiopathic scoliosis. Pediatr Exerc Sci. (2018) ; 30: (2): 243-250. |
[23] | Huh S, Eun LY, Kim NK, Jung JW, Choi JY, Kim HS. Cardiopulmonary function and scoliosis severity in idiopathic scoliosis children. Kor J Pedatr. (2015) ; 58: (6): 218-223. |
[24] | Bruyneel AV, Chavet P, Ebermeyer E, et al. Idiopathic scoliosis: Relations between the Cobb angle and the dynamical strategies when sitting on a seesaw. Eur Spine J. (2011) ; 20: (2): 247-253. |
[25] | Schreiber S, Parent EC, Moez EK, Hedden DM, Hill DL, Moreau M, et al. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis – an assessor and statistician blinded randomized controlled trial. PLoS One. (2016) ; 11: (12): e0168746. |
[26] | Fusco C, Zaina F, Atanasio S, Romano M, Negrini A, Negrini S. Physical exercises in the treatment of adolescent idiopathic scoliosis: An updated systematic review. Physiother Theory Pract. (2011) ; 27: (1): 80-114. |
[27] | Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, et al. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. (2012) ; 8: : CD007837. |
[28] | Otman S, Kose N, Yakut Y. The efficacy of Schroth’s 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Saudi Med J. (2005) ; 26: (9): 1429-1435. |
[29] | Maruyama T, Takeshita K, Kitagawa T. Side-shift exercise and hitch exercise. Stud Health Technol Inform. (2008) ; 135: : 246-249. |
[30] | Wang Q, Won S-H. A New technique for holistic and precise rehabilitation: Discovery of posture secret. Chin J Phys Med Rehabil, (2018) ; 40: (9): 644-646. |
[31] | Park JH, Jeon HS, Park HW. Effects of the Schroth exercise on idiopathic scoliosis: A meta-analysis. Eur J Phys Rehabil Med. (2018) ; 54: (3): 440-449. |




