Evaluation of the effect of psychological recovery tools on back pain in an out-patient prevention program
Abstract
BACKGROUND:
Stress and recovery have recently been linked to health issues and back pain (BP) occurrence. However, the evaluation of these aspects in prevention programs has not been approached so far.
OBJECTIVES:
The primary aim of this study was to exploratively scrutinize the effectiveness of recovery interventions to reduce BP within a multimodal, out-patient prevention program. The secondary aim consisted in the evaluation of these recovery interventions in terms of reducing stress and increasing recovery.
METHODS:
A prospective cohort study with 58 employees was conducted. Thirty-one individuals participated in a multimodal out-patient prevention program for 12-weeks, with recovery interventions being conveyed as add-ons. The control group did not receive treatment. At baseline (T0) and after the prevention program (T1), both groups completed psychometric instruments assessing BP, stress, and recovery.
RESULTS:
A MANOVA indicated that Pain Intensity (p = 0.039), Disability (p = 0.011), and Overall Stress (p = 0.001) were significantly reduced in the intervention group compared to the control group. Overall Recovery (p = 0.008) significantly improved in the intervention group while deteriorating in the control group.
CONCLUSIONS:
The outcomes emphasize the relevance of recovery tools for BP prevention and for reducing stress and enhancing recovery in an out-patient prevention program.
1Introduction
The manifestation of chronic back pain (BP) portrays the final stage of a detrimental development which has been initiated by acute BP. To contain the enormous costs associated with a chronic BP condition, it is advisable to prevent a chronification via the implementation of effective multimodal prevention programs [1, 2]. These prevention programs ideally follow the idea of the biopsychosocial model, thereby addressing the multifactorial etiology of BP. Considering the biomechanical point of view, the relationship between specific body structures and prevalent BP remains unclear. Associations between overload, movement patterns, tissue damage, and BP vary interindividually and depend on other factors, such as neurophysiological alterations and psychosocial influences [3]. In contrast to earlier prevention approaches, focusing on the integration of psychological strategies to effectively reduce the risk for BP has gained significant attention [4, 5].
Psychosocial factors reflect substantial risk factors, as they affect an individual on a behavioral, biomedical, and physiological level. Etiological models ascribe psychosocial factors a catalytic role with regard to the perception and handling of pain and highlight the necessity to appropriately encounter BP in combination with psychosocial factors in early stages [6, 7]. Ramond et al. [8] examined psychosocial risk factors for chronic BP in primary care and identified 16 different psychosocial factors, with depression, psychological distress, passive coping strategies and fear-avoidance beliefs being linked to a poor outcome. However, a clear independent influence of a specific psychosocial factor could not be affirmed based on the literature analysis. The authors suggest targeting other aspects in the psychosocial spectrum which could possibly contribute to the onset and chronification of BP [8].
While some promising steps towards the early impediment of BP have been commenced, the majority of research has concentrated on rehabilitation concepts. Systematic reviews that analyze the effectiveness and structure of rehabilitation programs for BP share the opinion that a considerable heterogeneity between multimodal approaches exists. A range of different multimodal rehabilitation programs for BP in Germany was compared by Morfeld et al. [9]. Based on their literature synthesis, Morfeld et al. [9] report a considerable lack of conceptual overlap regarding the analyzed rehabilitation programs. This heterogeneity of the examined approaches hampered the comparison of efficacy between the approaches. However, the authors note that the programs share the commonality of some form of standardization with partly flexible elements within each program. From a psychological perspective, the examined curricula mainly implemented psychological elements for pain and stress management in order to address individual coping resources. Reese and Mittag [10] specifically investigated psychological interventions for chronic BP rehabilitation. Low- to moderate-quality evidence was obtained for stress management, relaxation therapy, fear-avoidance training, and behavioral therapy. According to the authors, subgroup-specific, tailored programs should be anticipated in the future to generate more effective outcomes for affected individuals [10]. Kamper et al. [11] synopsized randomized controlled trials of biopsychosocial approaches in the rehabilitation of chronic low BP. Although these programs provided stronger effects compared to physical care approaches, again only moderate quality was acquired. As shortcomings, the authors listed insufficient descriptions of the biopsychosocial elements as well as the considerable costs associated with the programs. The presented evidence highlights the satisfactory status quo of BP rehabilitation. However, chronic BP is accompanied by enormous costs for the health care system and affected companies due to sick leave and early retirement and should therefore be approached at an earlier stage [12– 14].
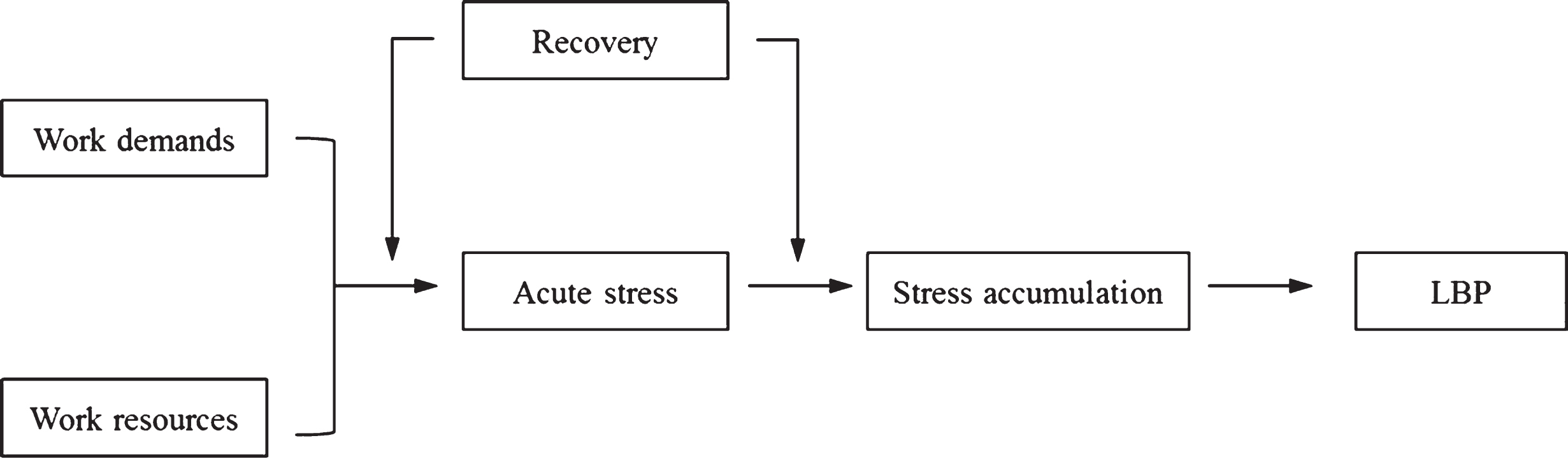
A more resource-efficient way to deal with pain syndromes is mirrored by the provision of suitable environments and strategies to prevent a negative health development. The required knowledge and skills to hamper a chronic course of BP should be disseminated in the context of preventive programs. Although the importance of early treatment of BP has been emphasized in research, a lack of potent multimodal preventive approaches for BP prevails [15, 16]. This status quo can be attributed to the difficulty of timely and adequately identifying specific psychosocial or biomedical risk factors for individuals [17]. Potential individualized risk factors continue to be challenging to grasp, as the causative course of BP represents a complex issue. Via the guidelines of the Working Group on European Guidelines for Prevention in Low Back Pain, Burton et al. [4] concluded that only scarce and insufficient evidence for the most common, monocausal interventions could be established (e.g., physical, psychosocial). The guidelines recommend the combination of biopsychosocial and physical activity elements into preventive programs for the general population. For physical activity, the existing evidence advocates a beneficial role of physical activity for BP, while no specific type of exercise or intensity can be determined and recommended up to the present moment. Research indicates to engage in modest physical activity in terms of recreational physical activities rather than specific back exercises. Physical activity supports the flexibility and strength of the back and has been associated with psychological well-being (e.g., decreased stress) in a bidirectional manner [4, 18, 19]. Nevertheless, Hendrick et al. [20] conclude that only scarce evidence for the positive impact of activity exists for the general population considering the propagated importance of activity in the management of BP. In addition, psychosocial aspects should be integrated into preventive programs of the working population [4, 21]. These psychosocial facets may encompass cognitive behavioral and problem-solving strategies as well as recovery techniques [22, 23]. While cognitive-behavioral aspects often require a specific educational background, techniques to enhance recovery are straightforward and offer the possibility to target the specific, individualized needs of specific groups to guarantee tailored interventions [4]. Kallus [24] defines recovery as “an inter- and intraindividual multilevel (e.g., psychological, physiological, social) process in time for the re-establishment of personal resources and their full functional capacity” (p. 42). In light of the fact that deficient recovery has been associated with health problems [25– 27] and BP in particular [28, 29], strengthening this psychological component may exhibit a beneficial influence on BP development. Heidari et al. [28] as well as Mierswa and Kellmann [29] have linked patterns of stress and recovery to the occurrence of BP. The studies suggest that a negative pattern of high stress and low recovery is accompanied by both increased back-related pain intensity and disability [28] and an increased risk to develop BP over time [29]. The association between work stress, recovery, and BP has also been proposed in the model (Fig. 1) by Mierswa and Kellmann [30].
Fig.1
The role of recovery for BP prevention and rehabilitation in the work context. Adapted from “The influences of recovery on low back pain development: A theoretical model,” by T. Mierswa and M. Kellmann, 2015, International Journal of Occupational Medicine and Environmental Health, 28, p. 258. doi: 10.13075/ijomeh.1896.00269.
It can be stated that evidence for biological, psychological, work-related and social factors in the etiology of BP exists [7, 31, 32]. However, the implementation into clinical practice and preventive programs is administered insufficiently and provides limited effects with regard to the anticipated BP-related outcomes [17]. Therefore, the central aim of this pilot study was to investigate the effect of recovery tools to diminish BP in employees in the context of a multimodal, out-patient prevention program in an explorative manner. In addition, the effect of recovery interventions on experiences of stress and recovery as psychological components was scrutinized. Specifically, it was hypothesized that:
(1) Pain Intensity and Disability diminish in the intervention group and remain on a steady level or even increase in the control group.
(2) Overall Stress decreases and Overall Recovery increases in the intervention group, while contrary developments were expected in the control group.
2Methods
2.1Participants
Prior to the data collection, a sample size calculation with the program G*Power 3.1 was performed [33]. We chose the MANOVA with repeated measures and within-between interactions as a statistical test. As input parameters, we applied a conventional alpha of 0.05, a power of 0.95 as well as an effect size of f = 0.50 to compute the required sample size. The number of groups and measurement points was set at two. As a result, we obtained a minimum sample size of N = 54.
Our analyzed sample comprised a total of 58 subjects (MAge = 44.9, SDAge = 10.1). The intervention group consisted of 31 individuals, while 27 participants formed part of the control group. A detailed overview of the selection process of our sample is displayed in Fig. 2.
Fig.2
Flow chart of the participant distribution and allocation.
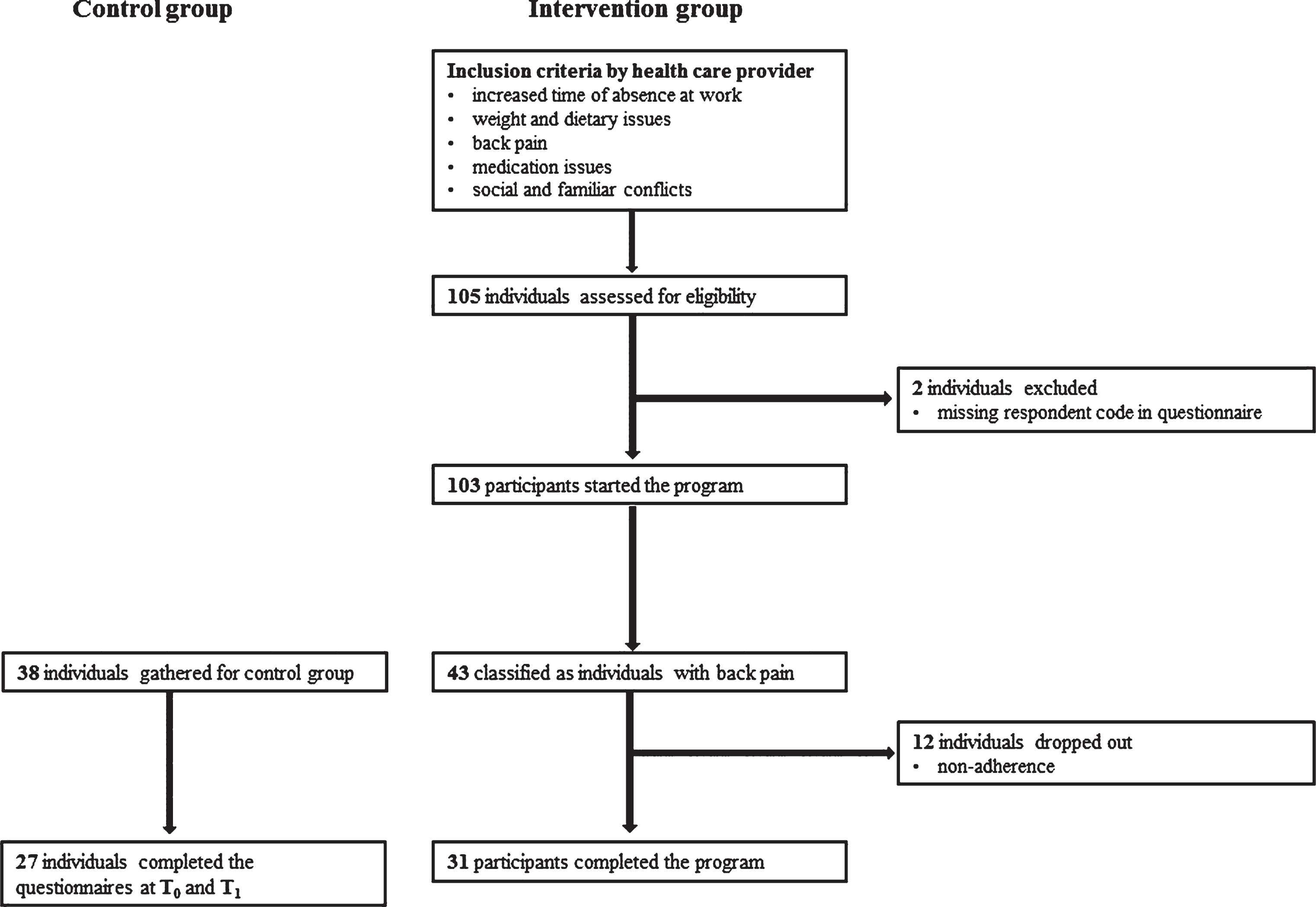
Potential participants were able to voluntarily register for the prevention program by contacting their company supervisor. As the program targets individuals with alarming health status with regard to continuous employability, the interested persons were examined by their company doctor to check for their eligibility. For this purpose, the responsible health care provider proposed a list of potential inclusion criteria. Unfortunately, we have not been granted access to all the specific inclusion criteria due to data privacy restrictions, but a number of potential eligibility criteria has been made available: a) increased time of absence at work, b) weight and dietary issues, c) BP, d) medication issues, as well as e) social and familiar conflicts. In case the employability was jeopardized by their present health condition, individuals could be included in the prevention program by the company doctor.
In the context of our study, BP had to be present and should have been listed as a primary complaint by the participants. BP was neither restricted to a specific location (lumbar, thoracic, cervical) nor a specific cause or origin and was therefore categorized as nonspecific BP [3]. Individuals eligible for this out-patient prevention program continued to work during their participation. The control group comprised individuals of the cooperating companies and matched the BP- and workplace-related characteristics of the participants enrolled in the program.
2.2Materials
2.2.1Instruments
The evaluation of the treatment effects was realized using various validated questionnaires. We obtained information about sociodemographic characteristics, BP parameters as well as stress and recovery. For the assessment of BP, we included the Chronic Pain Grade Scale (CPGS) as a multidimensional questionnaire to grade pain severity via the dimensions Pain Intensity and Disability [34]. We applied the validated German version of the CPGS, covering a time frame of the previous three months [35]. The dimension Pain Intensity comprises three different scales measuring Worst Pain Intensity, Mean Pain Intensity, and Current Pain Intensity and is expressed on a scale between 0– 100 points. Identically, the Disability dimension is rated between 0– 100 points and is composed of the four scales Interference with Daily Activities, Change of Ability to Take Part in Recreational, Social and Family Activities, and Change of Ability to Work, as well as the Number of Days BP interfered with the daily activities. Klasen et al. [35] reported moderate internal consistency values for the Pain Intensity (α= 0.68) and a good internal consistency for the Disability dimension (α= 0.88). The CPGS has been validated with several other clinical instruments to ensure its practical applicability [35].
The measurement of stress and recovery was conducted with the basic version of the Recovery-Stress Questionnaire (RESTQ-Basic) developed by Kallus [36]. The instrument consists of 48 items and evaluates stress- and recovery-related states and activities of the participants during the previous week. The dimension Overall Stress consists of the scales General Stress, Emotional Stress, Social Stress, Conflicts/Pressure, Fatigue, Lack of Energy, and Physical Complaints, while the Overall Recovery dimension covers the five scales Success, Social Recovery, Physical Recovery, General Well-being, and Sleep Quality. The two dimensions Overall Stress and Overall Recovery are calculated based on the mean values of all stress and recovery scales, respectively. Each stress and recovery scale comprises four items ranging between 0 (never) and 6 (always). According to Kallus [36], the Cronbach’s alpha values for Overall Stress range between α= 0.83 – 86 and between α= 0.73 – 77 for Overall Recovery in various German samples. In addition, the RESTQ-Basic-48 has been validated in various contexts using different samples to evaluate the convergent and discriminant validity of the instrument.
2.2.2Intervention tools
Two intervention tools aiming at the enhancement of psychological recovery were administered to the participants of the prevention program. First, a reflective recovery diary was explained to the participants. The reflective recovery diary allows the participants to monitor their recovery activities in written form. Over a period of seven days, individuals are instructed to reserve about 5– 10 minutes at the end of each day to think back to their recovery-related activities. These activities should be noted, described and rated on a scale from 0 (not restorative at all) to 10 (perfectly restorative). This tool intends to increase the participants’ sensitivity regarding their own recovery-related behavior as a potential beneficial resource. By this means, proactive recovery should be initiated which has been identified as a health-fostering construct [37].
Table 1
Elements of the prevention program
| Measurement point | Phase | Content of training/intervention | |
| Beginning of week 1 (T0) | Baseline assessment | Medical, sport scientific &psychological screening | |
| Week 1– 12 | Training phase | Five presentations/workshops, every 2,5 weeks | Twice per week (24 training sessions) |
| (1) Physical activity | Health-related physical training | ||
| (2) Workplace ergonomics I | |||
| (3) Stress management | |||
| (4) Workplace ergonomics II | |||
| (5) Nutrition | |||
| End of week 12 (T1) | Final assessment | Medical, sport scientific &psychological screening | |
Second, we implemented the concept of detachment as a central recovery mechanism into the prevention program [38]. Detachment characterizes a state of mental disengagement and dissociation of work-related thoughts in leisure time [39]. We presented various strategies to enhance detachment in the prevention program, such as structured to-do lists for work-related tasks, reduction of reachability, separation of work-related material and private material at home, and social support. The participants were advised to select the strategies most relevant to them in order to implement the detachment strategy into their daily life.
2.3Design and procedure
We conducted a prospective cohort study with sedentary employees. The sample consisted of two different groups, namely an intervention group enrolled in the prevention program and an inactive control group. We applied a 2×2 repeated measures MANOVA with group allocation (intervention vs. control) and time (baseline vs. post) serving as independent variables. Hence, group allocation represented the between-subjects factor, while time denoted the within-subjects factor. As outcomes, back-related pain intensity, disability and the dimensions stress and recovery were implemented. Pain Intensity and Disability were used as measures to quantify the BP development, whereas Overall Stress and Overall Recovery intended to evaluate the effectiveness of our add-on interventions.
With regard to the procedure, Table 1 provides a graphical overview of the different elements of the 12-week program. The central elements of the program were predetermined by the cooperating health care provider, with our interventions serving as additional elements within the preset program workshops. From October 2015 to April 2016, a new group with about 10– 15 participants started with the prevention program at the beginning of the month. At the beginning of the prevention program, a baseline assessment (T0) encompassing a physical evaluation of the participants was administered by the cooperating health care provider. During this baseline assessment, our questionnaire package was distributed to the participants for the first time (T0). Following to this, the participants received machine-based physical training under the guidance of a physiotherapist twice a week. In addition, five workshops on different health-related topics were provided. These workshops will be described and labelled with numbers (1) – (5) for reasons of clarity and comprehensibility. In the context of these workshops, our recovery-related intervention tools were conveyed and discussed. The main topics of these five workshops were: (1) physical activity, (2) workplace ergonomics I, (3) stress management, (4) workplace ergonomics II, and (5) nutrition. During the introductory workshop (1), we were granted 20 minutes to facilitate our add-on interventions. We focused on the theoretical underpinnings of recovery and stress and highlighted the relevance of these aspects for health in general and BP in particular. Moreover, the reflective recovery diary was explained and distributed to the participants. In the course of the second workshop (2), about 15 minutes were admitted to discuss the reflective recovery diary with the participants and address potential strengths and problems with the intervention tool. The third workshop (3) was used to extend the theoretical deliberations of the stress-recovery-BP relationship by introducing the concept of detachment. Throughout this 20-minute session, we presented the detachment strategies and provided a handout summarizing these strategies. As a final add-on, 15 minutes in the fourth workshop (4) were implemented to debate about the participants’ experiences with this tool and served as a feedback session for the detachment strategies. In accordance to the baseline assessment at the beginning of the program, the identical assessment was launched after the 12-week prevention program to evaluate the effectiveness of the program (T1). The control group did not receive any treatment, but filled in the identical questionnaire packages at the identical measurement points T0 and T1. The study was approved by the Medical Ethic Committee of the Ruhr University Bochum. All participants completed an informed consent document in accordance with the University Institutional Review Board.
2.4Statistical analysis
In preparation of the main analysis, a thorough data examination with regard to missing data and response patterns was conducted by two researchers. Irregular data patterns as well as logical inconsistencies were scrutinized and based on that inspection, four participants were excluded. In addition, we performed an outlier analysis in line with the recommendations by Iglewicz and Banerjee [40] without detecting any cases to exclude. In order to identify the effects of our recovery interventions, we calculated differences between the Overall Stress and Overall Recovery scores between T1 and T0 for both the intervention and control group. For Overall Stress, a negative value indicated a reduction of stress, while a positive value implied an increase of stress from T0 to T1. Conversely, negative values of Overall Recovery describe a reduction of recovery between T0 and T1, while positive values demonstrate higher levels of recovery at T1 compared to T0. In addition, the development of the two central BP parameters Pain Intensity and Disability should be determined. Again, the differences between these two variables with regard to T0 and T1 were calculated. In accordance with Overall Stress, a positive value between T1 and T0 corresponded to an augmentation of the pain parameters, while a negative value indicated a reduction of BP. After these preliminary steps, a MANOVA was conducted to evaluate potential effects. The two groups served as fixed factor, while the differences (T1 – T0) of the variables Overall Stress, Overall Recovery, Pain Intensity, and Disability were included as dependent variables. The Bonferroni correction was used to control for multiple testing. The statistical prerequisites for applying this method (e.g., measurement level, homogeneity of variances) were checked and met in compliance with Tabachnick and Fidell [41]. All analyses were conducted using SPSS Version 23.0 (SPSS, Inc., Chicago, IL).
Table 2
Descriptive differences between intervention and control group
| Dependent variable | Intervention group (n = 31) | Control group (n = 27) | Total (N = 58) | Group comparison |
| Age (M; SD) | 46.3 (10.1) | 43.4 (10.0) | 44.9 (10.1) | F(1, 56) = 1.17, p = 0.28 |
| Gender (n; %) | χ2(1, N = 58) = 0.0, p = 0.99 | |||
| Male | 16 (51.6) | 14 (51.8) | 30 (51.7) | |
| Female | 15 (48.4) | 13 (48.2) | 28 (48.3) | |
| Education level (n; %) | χ2(3, N = 58) = 7.36, p = 0.06 | |||
| Low | 3 (9.7) | 0 (0.0) | 3 (5.2) | |
| Medium | 12 (38.7) | 5 (18.6) | 17 (29.3) | |
| High | 16 (51.6) | 22 (81.4) | 38 (65.5) | |
| Marital status (n; %) | χ2(3, N = 58) = 1.03, p = 0.79 | |||
| Single | 6 (19.4) | 6 (22.2) | 12 (20.7) | |
| Married/in a relationship | 21 (67.7) | 19 (70.4) | 40 (69.0) | |
| Divorced/widowed | 4 (12.9) | 2 (7.4) | 6 (10.3) | |
| Work activity (n; %) | ||||
| Sedentary work | 27 (87.1) | 25 (92.6) | 52 (89.6) | χ2(1, N = 58) = 0.40, p = 0.49 |
| Standing work | 2 (6.4) | 0 (0.0) | 2 (3.4) | χ2(1, N = 58) = 1.80, p = 0.18 |
| Moderate physical work | 3 (9.7) | 2 (7.4) | 5 (8.6) | χ2(1, N = 58) = 0.09, p = 0.76 |
| Intense physical work | 2 (6.4) | 0 (0.0) | 2 (3.4) | χ2(1, N = 58) = 1.80, p = 0.18 |
| Employment status (n; %) | χ2(1, N = 57) = 0.29, p = 0.59 | |||
| Full-time | 23 (76.7) | 19 (70.3) | 42 (73.7) | |
| Part-time | 7 (23.3) | 8 (29.7) | 15 (26.3) | |
| Pain frequency (M; SD) | ||||
| Lumbar spine | 1.8 (1.9) | 1.5 (1.9) | 1.7 (1.9) | F(1, 56) = 0.40, p = 0.53 |
| Thoracic spine | 0.3 (0.7) | 0.5 (1.0) | 0.4 (0.8) | F(1, 56) = 1.08, p = 0.30 |
| Cervical spine | 1.4 (1.8) | 1.1 (1.5) | 1.3 (1.6) | F(1, 56) = 0.49, p = 0.49 |
| Pain duration (M; SD) | ||||
| Lumbar spine | 69.7 (111.9) | 65.2 (95.3) | 67.6 (103.6) | F(1, 56) = 0.03, p = 0.87 |
| Thoracic spine | 8.6 (25.5) | 14.0 (31.3) | 11.1 (28.3) | F(1, 56) = 0.51, p = 0.48 |
| Cervical spine | 55.1 (100.1) | 32.9 (43.0) | 44.7 (79.0) | F(1, 56) = 1.15, p = 0.29 |
Note. M = Mean; SD = Standard Deviation; n = Number of participants; The percentages for work activity did not add up to 100%, as participants named various work activity patterns. Pain frequency was indicated on a scale between 0 (= never) and 6 (= always) regarding the previous three months. Pain duration was measured in months. None of the group comparisons became significant (p < 0.05).
3Results
3.1Descriptive results
As a first step, the intervention and control group were compared with regard to central demographic and pain characteristics for the purpose of identifying potential covariates. We performed one-way ANOVAs and chi-square tests with a number of different variables. Age, gender, education level, marital status, work activity, and employment status were analyzed, but no differences between the groups were identified (Table 2). Identically, one-way ANOVAs and chi-square tests were administered to compare the two groups considering BP duration and frequency in the last three months (Table 2). No significant differences were obtained between the groups.
3.2Pain variables
The two dependent variables Pain Intensity and Disability were implemented as outcome variables for assessing the development of BP between the intervention and control group via a MANOVA. The results of the MANOVA displayed a significant difference in Pain Intensity between the groups, F(1, 53) = 4.46, p = 0.039, ηp2 = 0.08. With regard to the intervention group, Pain Intensity decreased from 33.57±4.24 to 24.28±3.32 between T0 and T1 and from 29.14±4.15 to 27.90±3.34 between T0 and T1 in the control group, indicating a stronger drop in the intervention group. For Disability, a statistically significant group difference was also found, F(1, 53) = 6.85, p = 0.011, ηp2 = 0.11. While Disability diminished in the intervention group between T0 and T1 from 21.07±4.84 to 10.71±2.72, an increase between T0 and T1 from 10.12±3.30 to 13.21±3.27 was identified in the control group. Further details regarding these calculations can be gathered from Table 3.
Table 3
Analysis of treatment effects for Pain Intensity, Disability, Overall Stress, and Overall Recovery
| Intervention group | Control group | ||||
| (n = 28) | (n = 27) | ||||
| Time | M±SEM | Change, | M±SEM | Change, | MANOVA for differences between T1 – T0 |
| M±SEM | M±SEM | ||||
| Pain Intensity | |||||
| Baseline | 33.57±4.24 | – | 29.14±4.15 | – | F(1, 53) = 4.46, p = 0.039*, ηp2 = 0.08 |
| 12-weeks | 24.28±3.32 | – 9.29±2.67 | 27.90±3.34 | – 1.24±2.72 | |
| Disability | |||||
| Baseline | 21.07±4.84 | – | 10.12±3.30 | – | F(1, 53) = 6.85, p = 0.011*, ηp2 = 0.11 |
| 12-weeks | 10.71±2.72 | – 10.36±3.60 | 13.21±3.27 | +3.09±3.66 | |
| Overall Stress | |||||
| Baseline | 2.01±0.14 | – | 1.72±0.15 | – | F(1, 53) = 14.51, p < 0.001***, ηp2 = 0.21 |
| 12-weeks | 1.59±0.14 | – 0.42±0.12 | 1.96±0.18 | +0.24±0.12 | |
| Overall Recovery | |||||
| Baseline | 3.11±0.16 | – | 3.26±0.18 | – | F(1, 53) = 7.67, p = 0.008**, ηp2 = 0.13 |
| 12-weeks | 3.45±0.17 | +0.34±0.13 | 3.08±0.15 | – 0.18±0.13 | |
Note. Changes scores are changes since baseline; negative values indicate improvements, except for recovery, where positive values indicate improvements. Group differences were calculated with repeated measures MANOVA. *p < 0.05, **p < 0.01, ***p < 0.001.
3.3Treatment effect
Apart from the pain development, we were interested in the effectiveness of our recovery interventions. For this purpose, we evaluated the differences of Overall Stress and Overall Recovery between the groups in reference to the two measurement points T0 and T1. A significant group discrepancy could be inferred for Overall Stress, F(1, 53) = 14.51, p < 0.001, ηp2 = 0.21. In the intervention group, a reduction of stress from 2.01±0.14 (T0) to 1.59±0.14 (T1) was noted. In contrast, stress levels within the control group intensified from a baseline value of 1.72±0.15 to a post assessment value of 1.96±0.18. Apart from that, the MANOVA with Overall Recovery as dependent variable yielded significant group differences, F(1, 53) = 7.67, p = 0.008, ηp2 = 0.13. Overall Recovery improved in the intervention group, increasing from a baseline score of 3.11±0.16 to a post score of 3.45±0.17. The development of Overall Recovery with regard to the control group showed a reduction from 3.26±0.18 (T0) to 3.08±0.15 (T1). Table 3 provides more information on the specifics of the MANOVA.
4Discussion
This study was conducted to analyze the effect of a multimodal, out-patient prevention program from two different perspectives. First, the baseline and post-test values of the BP parameters Pain Intensity and Disability were examined and compared between the intervention group and control group. Second, to evaluate the effectiveness of our add-on recovery interventions, the development of Overall Stress and Overall Recovery between the groups was examined. In line with our initial assumptions, Pain Intensity and Disability reduced significantly in comparison to the control group. Identical outcomes were found for Overall Stress and Overall Recovery. Overall Stress decreased in the intervention group and marginally increased in the control group, while Overall Recovery enhanced in the intervention group and declined in the control group.
This study introduces a new approach to address the issue of BP through the enhancement of recovery. The idea to concentrate on this psychological, resource-oriented aspect is derived from previous research which suggests focussing on the aspects stress and recovery. Mierswa and Kellmann [30] proposed a theoretical model which stressed the potential role of these two psychological concepts for the prevention of BP in working populations. A potential buffering role in the relationship between work stress and BP development is ascribed to recovery according to the model. On the one hand, sufficient recovery may inhibit stress development because it serves as a resource to deal with work strains. On the other hand, recovery may function as a resource to restore depleted reserves after work or general demands. Mierswa and Kellmann [30] conclude that the purposeful enhancement of recovery may manifest as relevant aspect to cope with BP. This relationship has now been scrutinized in our study and provided scientific evidence for the model for the first time. Thereby, our results connect to the preliminary findings gathered in light of the stress-recovery-BP relationship.
Heidari et al. [28] examined the association between three clusters of stress and recovery in light of pain intensity and disability in the lumbar spine in 265 physically active individuals. Those individuals with high stress and low recovery values showed significantly higher BP compared to the participants with low stress and high recovery values. The findings imply an association between an unfavorable stress and recovery ratio and the severity of BP. From a practical point of view, the outcomes as stated in Heidari et al. [28] formed the foundation to examine the role of recovery in our study within the prevention program. Mierswa and Kellmann [29] extended these associations by examining the predictive value of recovery-stress groups for BP occurrence in administrative university employees. After six months, the group with the highest stress and lowest recovery scores at baseline displayed a significantly higher proportion of BP occurrence compared to the group with the lowest stress and highest recovery scores. In general, the risk for BP occurrence increased with higher stress and lower recovery values. These outcomes highlight the relevance of considering stress and recovery in light of BP and served as a foundation for implementing the recovery tools into the prevention program.
Burton et al. [4] as well as Childs et al. [21] highlighted that individualized, psychological approaches are essential in the context of preventive programs to hamper the aggravation of BP at an early stage. As a means to meet these requirements, we imparted recovery tools which should be applicable and understandable for all participants. Based on our outcomes, it may be inferred that these tools have been adopted appropriately by the participants, as they contributed to an improvement of BP together with a subjective reduction of stress and increase of recovery. These effects may be compared to studies using similar recovery-oriented approaches concerning BP. Studies with recovery diaries and BP have not been conducted so far, but pain diaries represent a tool used with pain patients. However, Ferrari [42] points out that the utilization of a pain diary may exhibit a negative influence on BP by extending the time to recover. With regard to this study, we designed a reflective recovery diary. This diary aims at the resources of the participants that may help in coping with BP. The positive developments in the intervention group refute the future application of such a resource-oriented diary in pain patients. Furthermore, we introduced the concept of detachment as a method to enhance recovery. Detachment has also been linked to health problems in general [26, 27] and has been recently associated with BP in particular. Mierswa and Kellmann [43] conducted a prospective study with administration employees and reported a relationship between detachment in leisure time and the development of BP. Although only few and preliminary findings regarding the recovery tools currently exist, our results imply that a combined application of these recovery interventions contributes to a reduction of BP.
Improvements in terms of BP and the psychological aspects of stress and recovery resulted for the intervention group, but failed to materialize in the control group. Only Pain Intensity marginally reduced in the control group and represents an unanticipated finding. First, this outcome might have occurred as a simple incidental finding due to its small size and comparatively high standard error of the mean. Second, Pain Intensity depicts a fairly fluctuating construct which is interrelated with emotional states [44]. Hence, special circumstances in the company of the control group might have affected the perception of BP in a positive way.
Overall, the results of this study offer a positive summary of the prevention program in general and of the evaluated recovery add-ons in particular. It appears that the implementation of recovery strategies into prevention programs may constitute an empirically and practically meaningful way to deal with BP which has not been considered in research so far.
4.1Limitations and strengths
A list of drawbacks needs to be addressed in order to appropriately assess the outcomes and implications of the current study. The participants to the two conditions were not randomized to allow clear causal derivations and to systematically check for biasing influences. Our prospective cohort design implies temporal sequence, but suffers from weaknesses such as loss of participants over time and potential, non-addressed confounders. The role and effect of physical activity on the quality of BP and the perception of the psychological outcomes was not evaluated in this study. As physical activity formed an essential part of the prevention program, it should have been considered in the assessment. Due to this, the specific isolated effect of the physical activity and the add-on recovery tools could not be assessed. The aim of this pilot study was to show the integrability and effectiveness of the recovery tools as a first step whereas subsequent studies should consider both physical and psychosocial aspects to obtain more generalizable outcomes. The tested methodology and add-on recovery tools in this pilot study should be modified for future studies to further rule out potential confounding variables. Concerning the sample size, we gathered relatively small groups. This hampers the generalizability of our results for the working population. A follow-up assessment to check for potential long-term effects was not implemented. As a result, it could not be assessed whether the recovery tools have been integrated into daily routines and how the quality of BP has developed over time. Data about long-term effects could contribute considerably to the understanding and meaningfulness of the interventions and the prevention program as a total package. Finally, the evaluation of the program in terms of BP and the analysis of our add-on recovery tools were embedded into the regular procedures of the cooperating health care provider. Therefore, some of the mentioned limitations manifest as a result of bureaucratic and organizational restrictions that had to be complied with. The design and content of the prevention program was predefined and determined the extent and timing of our add-on interventions. These regulations limited the data acquisition regarding the volume of our questionnaires as well as the number of participants.
In contrast, our study is characterized by the fact that an out-patient prevention program in a real-life setting was accompanied and replenished scientifically. This procedure has the potential to emerge as an approach to ensure high ecological validity and to connect science and practice in a convenient way. The recovery tools represent an individual, coherent and effective method to address the psychological dimension of BP. The outcomes could connect to current approaches aiming at the integration of feasible physical activity programs into work settings [45]. Consequently, psychological and physical interventions could be combined to prevent BP. Although the intervention as well as the control group displayed relatively low values of Pain Intensity and Disability, a significant reduction of both parameters was obtained in the intervention group. These results indicate that the combination of the standard contents program and the add-on recovery tools may prevent BP from developing into a chronic issue.
4.2Conclusion
The primary research purpose of this study consisted in the exploratory evaluation of the effectiveness of recovery tools for BP prevention. Based on our results in the context of an out-patient prevention program, it can be derived that the implementation of recovery interventions may be appropriate to a) reduce sub-chronic BP and b) decrease stress while increasing recovery. The recovery tools are characterized by comprehensibility, feasibility, and represent an individualized approach to deal with the needs of each participant. The outcomes of this study may serve as a starting point to elaborate and consider the topic of recovery for BP prevention and rehabilitation to a greater extent. The presented tools may be modified depending on the target population and can be considered as an innovative psychological aspect in dealing with BP.
Conflict of interest
No potential conflict of interest is reported by the authors.
Acknowledgments
This work was supported by the German Federal Institute of Sport Science under Grant number ZMVI1-08012A/11-18. We would like to thank Uli Kotthoff for his great support in acquiring a suitable control group. The study was approved by the Medical Ethic Committee of the Ruhr University Bochum. All participants completed an informed consent document in accordance with the University Institutional Review Board.
References
[1] | Boersma K , Linton SJ . Screening to identify patients at risk: Profiles of psychological risk factors for early intervention. Clin J Pain. (2005) ;21: :38–43. |
[2] | Nicholas MK , Linton SJ , Watson PJ , Main CJ Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain A reappraisal. Phys Ther. (2011) ;91: :737–53. |
[3] | Balagué F , Mannion AF , Pellisé F , Cedraschi C . Non-specific low back pain. Lancet. (2012) ;379: :482–91. |
[4] | Burton AK , Balague F , Cardon G , Eriksen HR , Henrotin Y , Lahad A et al., How to prevent low back pain. Best Pract Res Clin Rheumatol. (2005) ;19: :541–55. |
[5] | Pincus T , Burton AK , Vogel S , Field AP . A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. (2002) ;27: :109–20. |
[6] | Linton SJ , Shaw WS . Impact of psychological factors in the experience of pain. Phys Ther. (2011) ;91: :700–11. |
[7] | Taylor JB , Goode AP , George SZ , Cook CE , Incidence and risk factors for first-time incident low back pain: A systematic review and meta-analysis. Spine J. (2014) ;14: :2299–319. |
[8] | Ramond A , Bouton C , Richard I , Roquelaure Y , Baufreton C , Legrand E et al., Psychosocial risk factors for chronic low back pain in primary care - a systematic review. Fam Pract. (2011) ;28: :12–21. |
[9] | Morfeld M , Küch D , Greitemann B , Dibbelt S , Salewski C , Franke GH et al., Multimodale Interventionsprogramme in der Rehabilitation von Patienten mit chronischen Rückenschmerzen – Ein Vergleich [A comparison of multimodal programmes of patient education in the rehabilitation of chronic low back pain]. Rehabilitation. (2010) ;49: :66–79. |
[10] | Reese C , Mittag O . Psychological interventions in the rehabilitation of patients with chronic low back pain: Evidence and recommendations from systematic reviews and guidelines. Int J Rehabil Res. (2013) ;36: :6–12. |
[11] | Kamper SJ , Apeldoorn AT , Chiarotto A , Smeets RJ , Ostelo RW , Guzman J et al., Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. (2015) ;350: :h444. |
[12] | Ma VY , Chan L , Carruthers KJ . Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. (2014) ;95: :986–95. |
[13] | Baumeister H , Knecht A , Hutter N . Direct and indirect costs in persons with chronic back pain and comorbid mental disorders - a systematic review. J Psychosom Res. (2012) ;73: :79–85. |
[14] | Hoy D , Bain C , Williams G , March L , Brooks P , Blyth F et al., A systematic review of the global prevalence of low back pain. Arthritis Rheum. (2012) ;64: :2028–37. |
[15] | Dorner TE , Crevenna R , Preventive aspects regarding back pain. Wien Med Wochenschr. (2016) ;166: :15–21. |
[16] | Roussel NA , Kos D , Demeure I , Heyrman A , De Clerck M , Zinzen E et al., Effect of a multidisciplinary program for the prevention of low back pain in hospital employees: A randomized controlled trial. J Back Musculoskelet Rehabil. (2015) ;28: :539–49. |
[17] | Pincus T , Kent P , Bronfort G , Loisel P , Pransky G , Hartvigsen J , Twenty-five years with the biopsychosocial model of low back pain - is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine. (2013) ;38: :2118–23. |
[18] | Heneweer H , Staes F , Aufdemkampe G , van Rijn M , Vanhees L . Physical activity and low back pain: A systematic review of recent literature. Eur Spine J. (2011) ;20: :826–45. |
[19] | Hurwitz EL , Morgenstern H , Chiao C . Effects of recreational physical activity and back exercises on low back pain and psychological distress: Findings from the UCLA low back pain study. Am J Public Health. (2005) ;95: :1817–24. |
[20] | Hendrick P , Milosavljevic S , Hale L , Hurley DA , McDonough S , Ryan B et al., The relationship between physical activity and low back pain outcomes: A systematic review of observational studies. Eur Spine J. (2011) ;20: :464–74. |
[21] | Childs JD , Wu SS , Teyhen DS , Robinson ME , George SZ . Prevention of low back pain in the military cluster randomized trial: Effects of brief psychosocial education on total and low back pain-related health care costs. Spine J. (2014) ;14: :571–83. |
[22] | Weiner SS , Nordin M . Prevention and management of chronic back pain. Best Pract Res Clin Rheumatol. (2010) ;24: :267–79. |
[23] | Linton SJ . A cognitive-behavioral approach to the prevention of chronic back pain, In: Turk DC , Gatchel RJ , editors. Psychological approaches to pain management: A practitioner’s handbook. 2 ed. New York, NY: The Guilford Press;(2002) . |
[24] | Kallus KW , Stress and recovery: An overview, In: Kallus KW , Kellmann M , editors. The Recovery-Stress Questionnaires: User manual. Frankfurt am Main:Pearson Assessment & Information GmbH; (2016) . pp. 27–48. |
[25] | de Croon EM , Sluiter JK , Frings-Dresen MHW . Need for recovery after work predicts sickness absence: A 2-year prospective cohort study in truck drivers. J Psychosom Res. (2003) ;55: :331–9. |
[26] | Sonnentag S , Kuttler I , Fritz C . Job stressors, emotional exhaustion, and need for recovery: A multi-source study on the benefits of psychological detachment. J Vocat Behav. (2010) ;76: :355–65. |
[27] | Sonnentag S , Fritz C . Recovery from job stress: The stressor-detachment model as an integrative framework. J Organ Behav. (2015) ;36: :72–103. |
[28] | Heidari J , Mierswa T , Hasenbring M , Kleinert J , Levenig C , Belz J et al. Recovery-stress patterns and low back pain: Differences in pain intensity and disability. Musculoskeletal Care. (2017) . |
[29] | Mierswa T , Kellmann M . Differences in low back pain occurence over a 6-month period between four recovery-stress groups. Work. (2017) ;58: :193–202. |
[30] | Mierswa T , Kellmann M . The influences of recovery on low back pain development: A theoretical model. Int J Occup Med Environ Health. (2015) ;28: :253–62. |
[31] | Ramond-Roquin A , Bouton C , Gobin-Tempereau AS , Airagnes G , Richard I , Roquelaure Y et al., Interventions focusing on psychosocial risk factors for patients with non-chronic low back pain in primary care - a systematic review. Fam Pract. (2014) ;31: :379–88. |
[32] | Rodrigues MS , Leite RDV , Lelis CM , Chaves TC . Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work. (2017) ;57: :563–72. |
[33] | Faul F , Erdfelder E , Lang AG , Buchner A . G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) ;39: :175–91. |
[34] | Von Korff M , Ormel J , Keefe FJ , Dworkin SF . Grading the severity of chronic pain. Pain. (1992) ;50: :133–49. |
[35] | Klasen BW , Hallner D , Schaub C , Willburger R , Hasenbring M . Validation and reliability of the German version of the Chronic Pain Grade questionnaire in primary care back pain patients. Psychosoc Med. (2004) ;1: :1–12. |
[36] | Kallus KW . Chapter RESTQ-Basic: The general version of the RESTQ, In: Kallus KW , Kellmann M , editors. The Recovery-Stress Questionnaires: User manual. Frankfurt: Pearson; (2016) . pp. 49–85. |
[37] | Sonnentag S . Recovery, work engagement, and proactive behavior: A new look at the interface between nonwork and work. J Appl Psychol. (2003) ;88: :518–28. |
[38] | Sonnentag S , Fritz C . The Recovery Experience Questionnaire: Development and validation of a measure for assessing recuperation and unwinding from work. J Occup Health Psychol. (2007) ;12: :204–21. |
[39] | Sonnentag S , Bayer UV . Switching off mentally: Predictors and consequences of psychological detachment from work during off-job time. J Occup Health Psychol. (2005) ;10: :393–414. |
[40] | Iglewicz B , Banerjee S , A simple univariate outlier dentification procedure. proceedings of the annual meeting of the American Statistical Association; 2001; Atlanta, GA. |
[41] | Tabachnick BG , Fidell LS . Using multivariate statistics. 6 ed. Boston, MA: Pearson; (2013) . |
[42] | Ferrari R . Effect of a pain diary use on recovery from acute low back (lumbar) sprain. Rheumatol Int. (2015) ;35: :55–9. |
[43] | Mierswa T , Kellmann M , Psychosoziale Arbeitsbedingungen und Rückenschmerz: Der moderierende Effekt von Detachment in der Freizeit [Psychosocial work factors and back pain: The moderating effects of detachment in leisure time], Z Gesundheitspsychol. (2014) ;22: :129–41. |
[44] | Mun CJ , Karoly P , Okun MAP- . Effects of daily pain intensity, positive affect, and individual differences in pain acceptance on work goal interference and progress. Pain. (2015) ;156: :2276–85. |
[45] | Shariat A , Lam ET , Kargarfard M , Tamrin SB , Danaee M . The application of a feasible exercise training program in the office setting. Work. (2017) ;56: :421–8. |



