Comparing two methods to record maximal voluntary contractions and different electrode positions in recordings of forearm extensor muscle activity: Refining risk assessments for work-related wrist disorders
Abstract
BACKGROUND:
Wrist disorders are common in force demanding industrial repetitive work. Visual assessment of force demands have a low reliability, instead surface electromyography (EMG) may be used as part of a risk assessment for work-related wrist disorders. For normalization of EMG recordings, a power grip (hand grip) is often used as maximal voluntary contraction (MVC) of the forearm extensor muscles. However, the test-retest reproducibility is poor and EMG amplitudes exceeding 100% have occasionally been recorded during work. An alternative MVC is resisted wrist extension, which may be more reliable.
OBJECTIVE:
To compare hand grip and resisted wrist extension MVCs, in terms of amplitude and reproducibility, and to examine the effect of electrode positioning.
METHODS:
Twelve subjects participated. EMG from right forearm extensors, from four electrode pairs, was recorded during MVCs, on three separate occasions.
RESULTS:
The group mean EMG amplitudes for resisted wrist extension were 1.2–1.7 times greater than those for hand grip. Resisted wrist extension showed better reproducibility than hand grip.
CONCLUSIONS:
The results indicate that the use of resisted wrist extension is a more accurate measurement of maximal effort of wrist extensor contractions than using hand grip and should increase the precision in EMG recordings from forearm extensor muscles, which in turn will increase the quality of risk assessments that are based on these.
1Introduction
Many occupations require excessive and/or prolonged muscular load, which in combination with repetitive work, may result in a high frequency of work-related wrist disorders [1–3]. The frequency is especially high for females in the assembly industry, and therefore, interventions in the physical work stations and in work organisations are needed, to decrease the risk for development of musculoskeletal disorders. The interventions are based on risk assessments, and it is important that the assessments are valid and reliable. Many observational risk assessment methods have been developed [4, 5]. However, visual assessments, as well as self-assessments of force and/or exertion intensity often show a low reliability [4]. It has been recommended that technical measurements should replace visual assessments when feasible [6], and surface electromyography (EMG) is a technical method that could be used to obtain quantitative measures of the forces exerted by the hand. One example of an observation method where the force assessment component can be replaced, is the ACGIH threshold limit value (TLV) for hand activity level [7]. The ACGIH hand activity level includes levels of force and repetitiveness (used to assess the risk of developing disorders in the hand, wrist or forearm), and EMG has been suggested for reliability reasons to determine the peak force when assessing the hand activity level, to be compared with the TLV in hand intense work. Furthermore, a direct association between the amplitude of muscular activity from EMG measures and pain has been demonstrated in several studies [3, 8–10]. Moreover, a low frequency of so called EMG gaps (short time periods with muscular rest) and/or a small time proportion with muscular rest, are associated with work-related musculoskeletal complaints [8, 11, 12].
The amplitude of EMG recordings differs between and within subjects carrying out the same working task [13, 14]. The difference between subjects may depend on technique, strength and skinfold thickness [15]. Therefore, large differences are seen between male and female workers performing the same working tasks [16, 17]. The difference in measurements made on one subject from one day to the next may also be influenced by the reproducibility of the electrode positioning, especially if the electrodes are positioned close to the innervation zone. Furthermore, to enable comparison of the muscular activity between subjects, EMG recordings are generally normalized to a reference contraction [18, 19]. Reference contractions can be obtained in a variety of postures and at different loads, e.g. maximal voluntary isometric contraction (MVC). The highest electrical activity obtained during the MVC is generally referred to as the maximal voluntary electrical activity (MVE) and the muscular load during work is then expressed as a percentage of the MVE. Work is often carried out in a variety of arm postures at different loads, and it is desirable that the reference contraction and the electrode position are appropriate during all these conditions.
Variation may be observed in the reference contraction of an individual when measured on different days. In fact, when evaluating the reproducibility of EMG measurements in a laboratory setting, we found that the muscular activity during work, expressed as % MVE in the right forearm extensors (Mm. extensor carpi radialis (longus et brevis); ECR), showed a high intra-individual coefficient of variation of about 33%. The corresponding variation in non-normalized data was 16%. For MVE during the contractions themselves, the coefficient of variation was 29% [14]. Thus, normalization itself introduces a variation.
Although the resisted wrist extension may be the most obvious manner to activate the extensor muscles, many research groups, including ours, elicit the MVC of the forearm muscles with a power grip (here referred to as the hand grip) in a mid-pronated (i.e. neutral) forearm posture [20–22]. This grip can be used for simultaneous MVCs for both the flexor and the extensor muscles. However, we occasionally see higher EMG amplitudes during industrial work than those obtained during the MVC performed with the maximum hand grip. We also see higher EMG amplitudes for some subjects when they perform a maximal active range of motion of the wrist in flexion-extension (maximal wrist extension) compared to when performing the MVC with the hand grip. These observations indicate that the muscles are not always fully activated during the reference contraction. Also the resisted wrist extension has been used as reference contraction for normalizing the forearm extensor muscle activity [17, 23–25]. However, we have considered this contraction to be more inconvenient to perform in work place recordings than the hand grip. Thus, there is clearly a need to re-evaluate the reference contractions.
Additionally, in some professions, such as dental hygienists [26, 27], a high force pinch grip is frequent. The impact of pinch grip on EMG from the forearm extensors has been discussed [28]. It would therefore be interesting to register both maximal wrist extension and pinch grip, when using the resisted wrist extension and the hand grip for normalization.
The effect of electrode positioning on EMG amplitude is also significant. If a pair of electrodes is placed symmetrically above the innervation zone, the recorded amplitude will be reduced, and will also be sensitive to small movements of the skin [29, 30]. To improve our knowledge on the location of the innervation zone, it would be interesting to find the motor point, i.e. the point where the nerve enters into the muscle, as this presumably is proximal to the innervation zone.
The aim of this study was to compare the amplitude and reproducibility of two different methods of measuring MVCs of the forearm extensors, and to examine the effect of electrode positioning on recordings of forearm extensor muscle activity.
2Methods
2.1Study design and subjects
Twelve right-handed employees at our department, six women and six men, without ongoing upper extremity complaints, participated in the study (Table 1). The electrical activity of the right forearm extensors was recorded on three separate occasions, at least seven days apart. On each occasion, three MVCs of two different types of contraction (the hand grip and the resisted wrist extension), and three maximal activations of two different types (pinch grip and maximal wrist extension), were performed, each followed by a short rest of about half a minute. The instructor actively encouraged the subject to perform at their best and they were asked to sustain the maximum contraction/activation for about 5 seconds. The subject was seated and body movements were controlled during each test.
Table 1
Characteristics of the six female (F) and six male (M) subjects, their skinfold thickness and maximal exerted force for the two maximal voluntary contractions (MVCs) and one of the two maximal activations, presented as the mean and standard deviation (SD) of measurements made on three occasions
| Subject | Sex | Age (year) | Height (cm) | Weight (kg) | Skinfold thickness (mm) | Force (N) | ||
| Contraction (MVC) | Activation | |||||||
| Resisted wrist extension | Hand grip | Pinch grip | ||||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| 1 | F | 43 | 168 | 61 | 8.9 (0.6) | 78 (2.5) | 337 (15) | 108 (6.2) |
| 2 | F | 66 | 160 | 63 | 7.1 (0.1) | 48 (6.0) | 262 (15) | 75 (6.0) |
| 3 | F | 53 | 153 | 51 | 9.0 (0.3) | 64 (3.1) | 275 (0) | 66 (5.8) |
| 4 | F | 46 | 166 | 71 | 7.9 (0.3) | 82 (4.9) | 422 (0) | 95 (7.6) |
| 5 | F | 34 | 167 | 60 | 5.6 (0.4) | 89 (2.1) | 405 (25) | 71 (2.9) |
| 6 | F | 50 | 165 | 57 | 4.4 (0.2) | 57 (4.9) | 373 (26) | 86 (2.5) |
| 7 | M | 57 | 169 | 72 | 4.7 (0.4) | 114 (4.9) | 464 (12) | 106 (5.8) |
| 8 | M | 31 | 173 | 62 | 3.1 (0.1) | 112 (3.2) | 405 (25) | 110 (4.6) |
| 9 | M | 61 | 171 | 81 | 4.0 (0.3) | 121 (4.4) | 520 (10) | 83 (4.0) |
| 10 | M | 55 | 178 | 73 | 5.5 (0.2) | 112 (1.7) | 493 (6) | 110 (4.6) |
| 11 | M | 37 | 185 | 74 | 4.1 (0.1) | 137 (8.1) | 510 (20) | 135 (0.0) |
| 12 | M | 58 | 194 | 90 | 5.0 (0.2) | 104 (7.4) | 582 (54) | 117 (8.5) |
All participants were colleagues at our research division, and were informed about the study according to the Declaration of Helsinki. They were informed verbally about the procedures, that participation was voluntary and that they were free to discontinue at any time without explanation. They all gave their verbal consent.
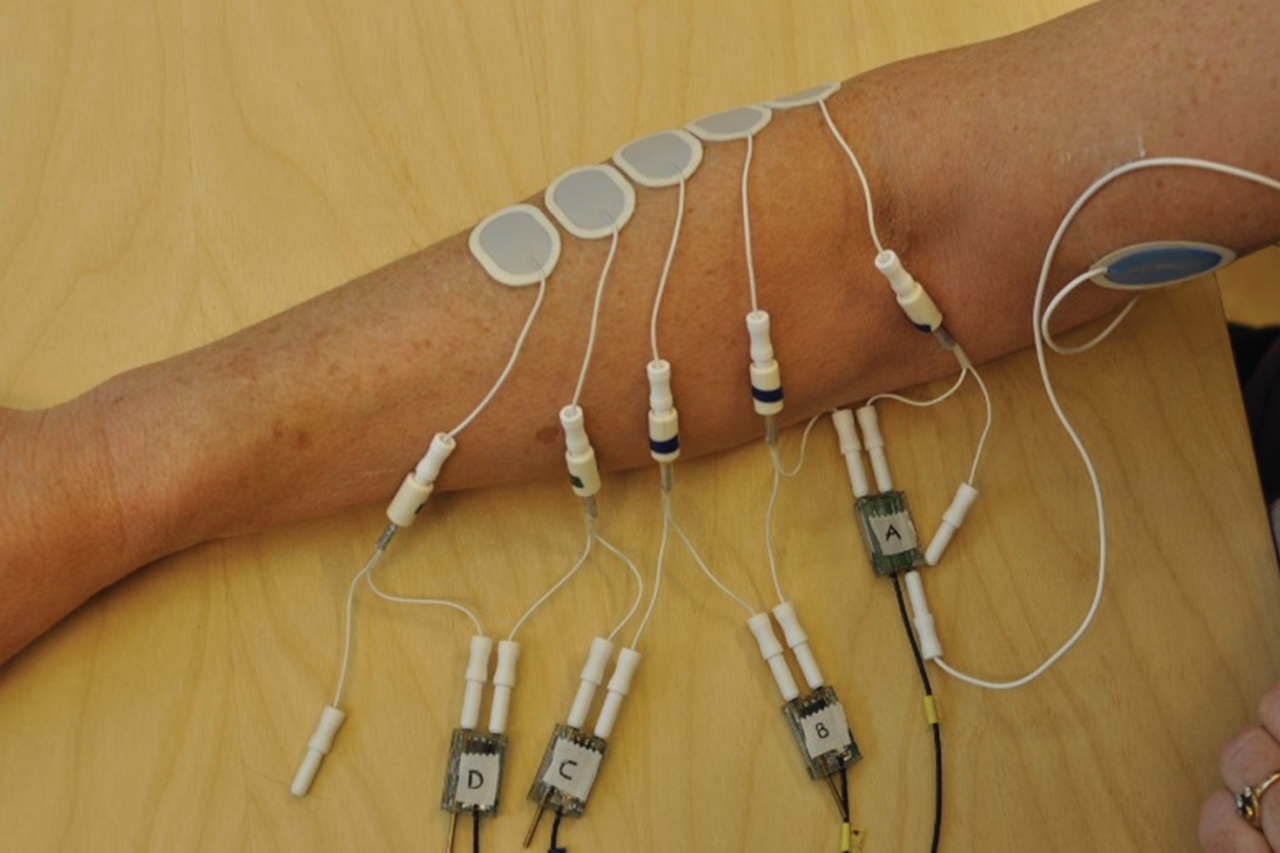
2.2Electromyography
Mm. extensor carpi radialis longus et brevis (ECR) were located, in the same way as we do in our work place recordings, in the right forearm by palpation, while the subject performed a voluntary contraction with the forearm pronated. The skin was cleansed with acetone and rubbed with emery cloth. Two Ag/AgCl electrodes (Ambu Neuroline 720, Ambu A/S, Ballerup, Denmark) were applied along the muscle fibres, on the skin above the most prominent part of the muscles, i.e. at approximately one third of the distance from the epicondylus lateralis humeri to the processus styloideus ulnae. Three additional electrodes were applied, two proximally to the original pair, and one distally, as shown in Fig. 1. This arrangement of five electrodes (numbered 1 to 5 starting from the elbow) allowed measurements to be made from four pairs of electrodes, labelled A to D in Fig. 1. The active diameter of the electrodes was 6 mm, and the centre-to-centre distance 20 mm. The impedance was measured for each pair, and if the value was >15 kΩ, the electrodes were removed and replaced after repeated skin cleansing. The ground electrode was placed on the inside of the distal part of the upper arm.
Fig.1
Electrode positioning on the right forearm extensor muscles. The electrodes are numbered 1 to 5 starting at the elbow. The large blue electrode is the ground electrode. The signals were measured between pairs of electrodes (A-D).
After performance of the MVCs/activations described below, the positions of the electrodes were marked on the forearm with a felt-tip pen before they were removed. A line was drawn between the epicondylus lateralis humeri and the processus styloideus radii, and the shortest perpendicular distance between this line and each electrode was drawn. The distance from the epicondyle to the projection of each electrode on the line was measured, as was the distance between the epicondyle and the styloid.
The signals were amplified, filtered (10–400 Hz) and sampled at a rate of 1024 Hz, and stored on portable data loggers (Logger Teknologi HB, Åkarp, Sweden) using exchangeable flash-memory cards [31]. After collection, the data were transferred to a computer for quality assurance and analysis. The signal was band-pass (30–400 Hz) and notch filtered, i.e. 50 Hz and all harmonics. The root-mean-square value was calculated for epochs of 0.125 s, and the noise was subtracted in a power sense [32]. A moving window with a width of 0.5 s was used to find the highest EMG activity recorded during the three contractions and the three activations, for each kind of contraction and activation [32, 33].
2.3Maximal voluntary contractions
2.3.1Resisted wrist extension
The subject was seated with a backrest, with the upper arm close to the body, the elbow flexed and the forearm pronated and supported on a table, adjusted to a comfortable height. The hand was inserted into a glove that was attached to a sheet of plywood on the dorsal side of the glove. The middle finger of the glove went through a metal ring that was mounted on the underside of the plywood. A non-flexible strap went through the ring, which was attached to a force transducer on the floor. The hand was outside the table while the wrist was supported on the table (Fig. 2). The subject was asked to attempt to perform a maximal extension of the wrist, while the wrist remained in the neutral position, and care was taken to ensure that the sheet of plywood remained horizontal when the wrist extensors were maximally activated (Table 1).
Fig.2
The maximal voluntary contractions and maximal activations.
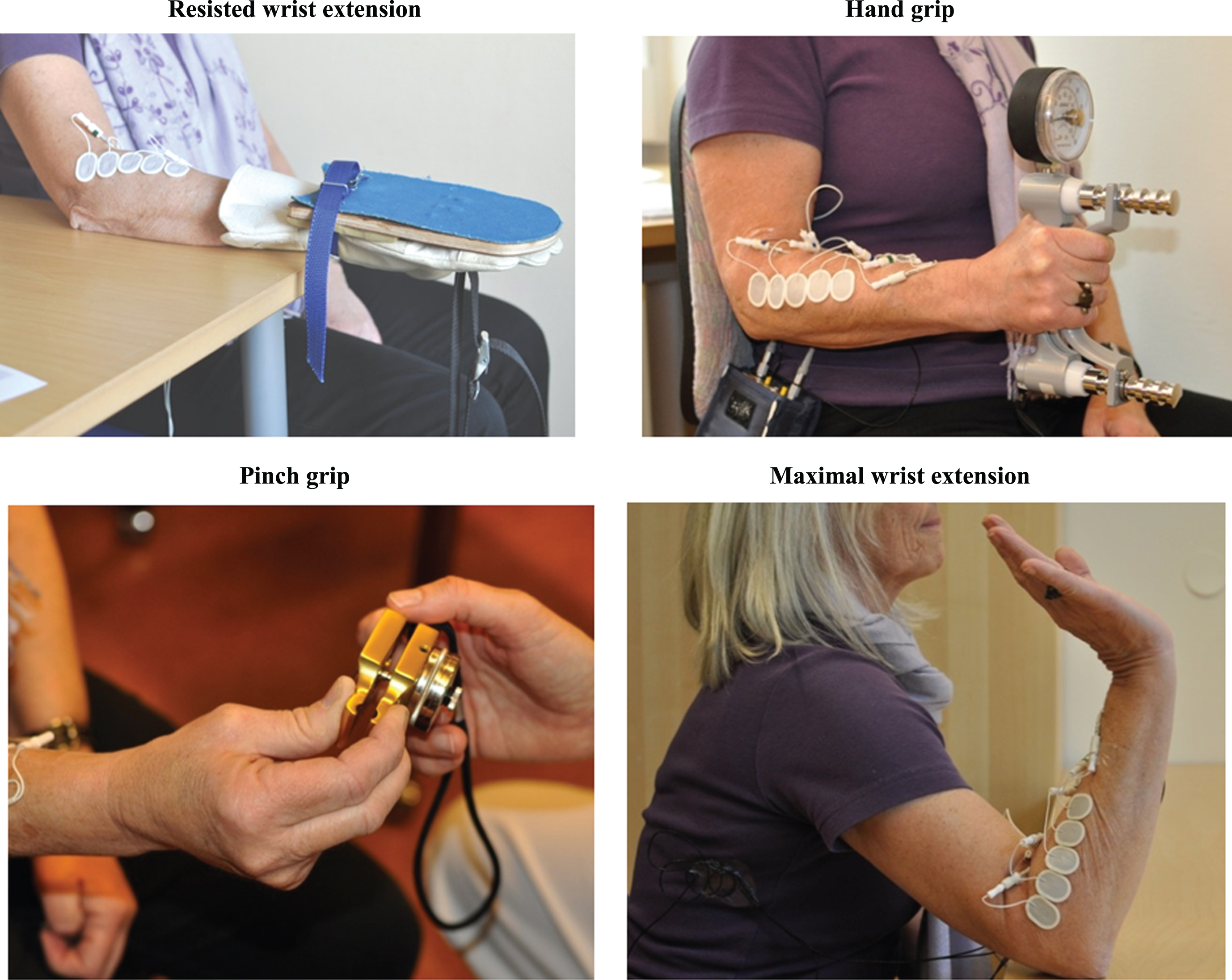
2.3.2Hand grip
The subject performed a maximal isometric grip around a Jamar hand dynamometer (Sammons Preston, Bolingbrook, IL, USA) while seated with a backrest, with the right upper arm close to the body, with the elbow flexed at 90° holding the forearm and hand without support, in a neutral position (Table 1, Fig. 2).
2.4Maximal activations
For the pinch grip, the subject was seated with the arm unsupported and somewhat forward flexed at the shoulder, with the elbow flexed to approximately 90°, holding the forearm in a neutral position. The wrist was in a functional position (0–30° extension, 0–15° ulnar deviation, Fig. 2). The examiner handed a pinch dynamometer (North Coast Medical, Gilroy, CA, USA) to the subject who was instructed to grip it by the thumb and the second and third fingers, and press as hard as possible (Table 1).
For the maximal wrist extension, the subject was seated with the elbow supported by the table, flexed at 90° (forearm pronated and approximately 45° upwards). The wrist was at maximal dorsal flexion, and the subject was instructed to continue to extend the wrist as much as possible (Fig. 2).
2.5Detection of the motor point
The motor point was detected using a transcutaneous electrical nerve stimulator (TENS, CEFAR Medical AB, Lund, Sweden). A carbon rubber electrode, 50×30 mm, was placed on the muscles on the flexor side of the forearm, and fixed with Mefix® (Mölnlycke Health Care AB, Gothenburg, Sweden). The extensor side was shaved, and covered with electrode gel. A smaller carbon rubber electrode (18 mm in diameter) was held in place on the skin over the muscle belly. The TENS was set to low-frequency stimulation, generating constant current trains of 8 square pulses with a repetition rate of 1.7 Hz. The amplitude was slowly increased while the electrode was slid up and down, as well as sideways, along the full length of the muscle. The point at which repeated extension of the index and/or the middle finger was observed at the lowest electrical stimulation was identified as the motor point. This point was marked, and the distance to the epicondyle was measured. Finally, the markings on the arm were photographed to allow subsequent quality checks.
2.6Skinfold thickness
The thickness of the subcutaneous tissue was measured at the area between the electrodes forming pair C, using a skinfold calliper (Harpenden, British Indicators, West Sussex, UK), according to the manufacturer’s instructions.
2.7Data analysis
The quality review of the collected data revealed no anomalies, and all the data were analysed. Calculations were performed separately for each pair of electrodes and each type of MVC and maximal activation. After inspecting the data and finding it reasonable, the mean EMG amplitude (μV) across occasions was calculated for each subject, as well as the group mean of these means.
The standard deviation and the coefficient of variation (CV: standard deviation/ mean) for the MVCs were calculated for each subject for the three different occasions. We then calculated the group mean of the CVs. To derive a combined measure of goodness, i.e. the combination of high amplitude and low CV, the ratio between the group mean EMG amplitude and the group mean CV (group EMGamp/CV) was calculated.
The effect of type of MVC on the EMG amplitude was calculated using a linear mixed regression model, with a random intercept for each individual and with MVC and occasion included as fixed factors. A p-value below 0.05 was considered statistically significant. To investigate the retest correlation for the two different MVCs, the intra class correlation coefficients (ICC) were calculated from the linear mixed regression models fitted for each type of MVC separately. Values above 0.6 were considered good or excellent [34], indicating a low between-days variation within subjects. The MVC with the highest group mean EMG amplitude was selected. For each subject, the mean EMG amplitudes for the other MVC and the maximal activations were normalized to this, and expressed as % MVE. Then, the group mean EMG amplitudes for the maximal activations were normalized to both the resisted wrist extension and the hand grip, and expressed as % MVE. IBM SPSS Statistics Version 22.0 (SPSS, Chicago, IL, USA) was used for the statistical analyses.
3Results
3.1Maximal voluntary contractions
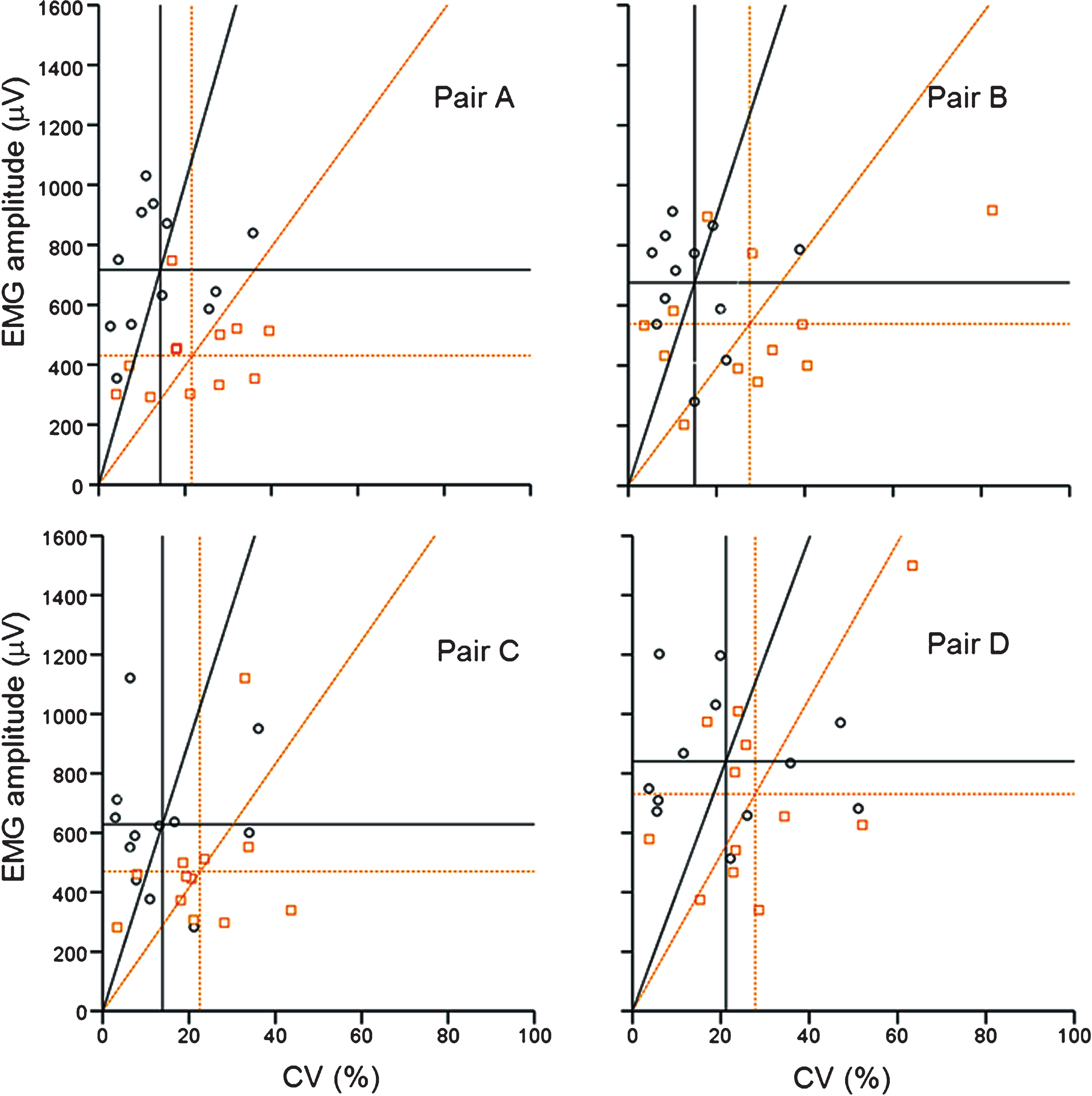
The highest group mean EMG amplitudes were, for all electrode pairs found for the resisted wrist extension (Table 2, Fig. 3). These values were 1.2–1.7 times higher than those obtained with the hand grip. The reproducibility in the resisted wrist extension over the three occasions, in terms of the group mean CV, was 14–15% for electrode pairs A, B and C, and 22–28% for the hand grip. For pair D, the corresponding values were 21% and 28%, respectively. The group mean CVs for force were 5% for the resisted wrist extension and 4% for the hand grip (derived from Table 1). The highest group EMGamp/CV ratio (the combined measure of goodness) over the three occasions was derived for the resisted wrist extension in all electrode pairs. Concerning the reliability, in terms of ICC, values above 0.6 was found in pair A, B and C for the resisted wrist extension, and in pair A and C for the hand grip (Table 2).
Table 2
Group mean EMG amplitude (EMGamp) from three separate occasions and group mean across these. Group mean CV (CV) and the ratio between the mean and CV (EMGamp/CV) for the maximal EMG amplitudes for two different contractions (MVCs) obtained using four different pairs of electrodes in twelve subjects. Statistically significant differences in EMG amplitudes between MVCs, and intraclass correlation coefficients (ICC), calculated by linear mixed regression models
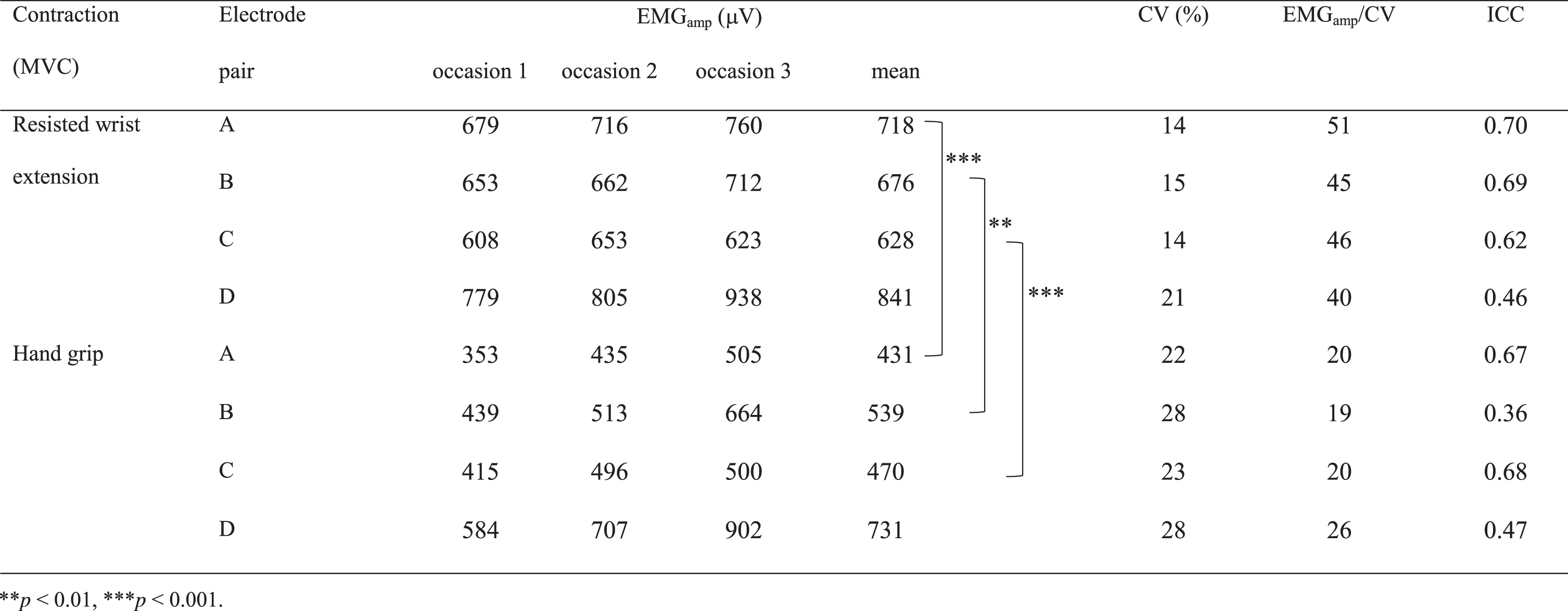 |
Fig.3
Mean EMG amplitude versus CV for two types of contraction. The EMG amplitude was measured on three separate occasions using four pairs of electrodes in twelve subjects (o and — = the resisted wrist extension,  and
and  = the hand grip). The horizontal lines represent the group mean EMG amplitude and the vertical lines the group mean CV for each type of MVC. The slopes of the lines through the origin represent the ratio between the group mean EMG amplitude and group mean CV for the twelve participants.
= the hand grip). The horizontal lines represent the group mean EMG amplitude and the vertical lines the group mean CV for each type of MVC. The slopes of the lines through the origin represent the ratio between the group mean EMG amplitude and group mean CV for the twelve participants.
When the mean EMG amplitudes for the hand grip was normalized to the mean EMG amplitude for the resisted wrist extension (expressed as % MVE of resisted wrist extension) for each participant in all four electrode pairs, a value greater than 100% was found for three subjects, two of the subjects in pair B and D and one in pair C and D (Fig. 4).
Fig.4
Normalized mean EMG amplitudes. The EMG amplitude was measured on three separate occasions for two types of MVC and two types of maximal activation using four pairs of electrodes in twelve subjects. The mean EMG amplitudes for the hand grip ( and
and  ), the pinch grip (
), the pinch grip ( and
and  ), and the maximal wrist extension (
), and the maximal wrist extension ( and
and  ), have been normalized to the mean EMG amplitude for the resisted wrist extension (
), have been normalized to the mean EMG amplitude for the resisted wrist extension ( and
and  ), and are presented as %MVE. The horizontal lines represent the group mean %MVE.
), and are presented as %MVE. The horizontal lines represent the group mean %MVE.
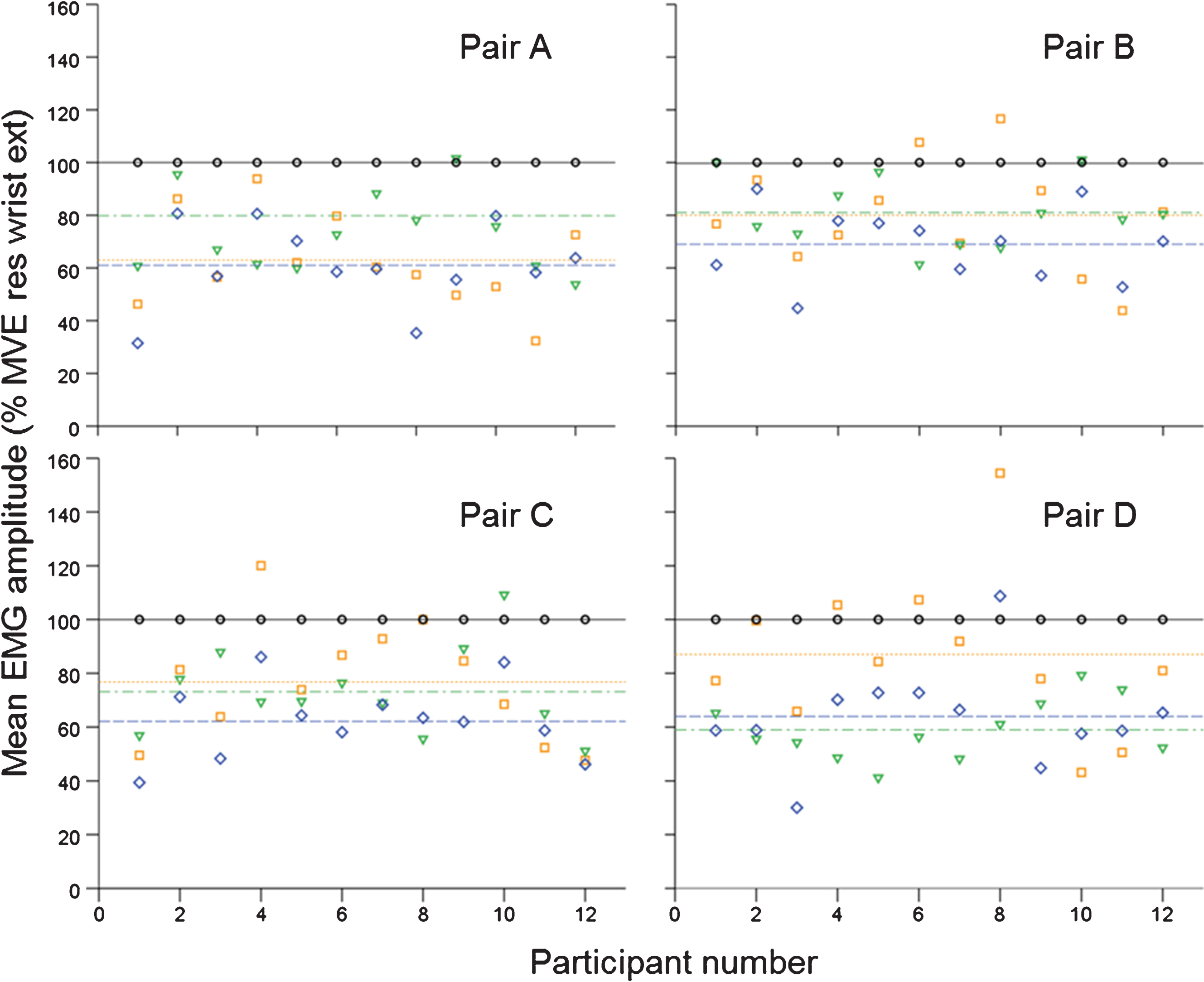
3.2Maximal activations
The pinch grip gave 60–68 % MVE when normalized to the resisted wrist extension, and 74–100 % MVE when normalized to the hand grip. For the maximal wrist extension, 58–80 % MVE was registered when normalized to the resisted wrist extension, and 67–121 % MVE when normalized to the hand grip (Fig. 4).
3.3Electrode positioning
The group mean EMG amplitudes for the two MVCs varied considerably with the electrode positioning (Table 2, Fig. 3). The lowest values were observed with electrode pair C (the pair used in our work place recordings) for the resisted wrist extension (Table 2), the pinch grip and the maximal wrist extension (data not shown), while the hand grip showed the lowest amplitudes for pair A (Table 2). The highest group mean EMG amplitudes were seen for pair D for the resisted wrist extension, the hand grip and the pinch grip, and for pair B for the maximal wrist extension. The highest group EMGamp/CV ratio was seen for pair A for the resisted wrist extension and for pair D for the hand grip.
The electrode positions for participants number 7 and 8 varied >20 mm between sessions, i.e. the electrode pair positions were interchanged (Fig. 5). These participants also showed high CVs between sessions.
Fig.5
Distances for right forearm. The distance (mm) from the epicondylus lateralis humeri ( ) to the electrodes (
) to the electrodes ( ), to the motor point (
), to the motor point ( ) and to the processus styloideus radii (
) and to the processus styloideus radii ( ), measured on three separate occasions in twelve subjects. The digit given for each participant is the distance between the epicondylus lateralis humeri and the motor point. The ratio of the median distance between the epicondylus lateralis humeri and the motor point, and the distance between the epicondylus lateralis humeri and the processus styloideus radii is given in brackets.
), measured on three separate occasions in twelve subjects. The digit given for each participant is the distance between the epicondylus lateralis humeri and the motor point. The ratio of the median distance between the epicondylus lateralis humeri and the motor point, and the distance between the epicondylus lateralis humeri and the processus styloideus radii is given in brackets.
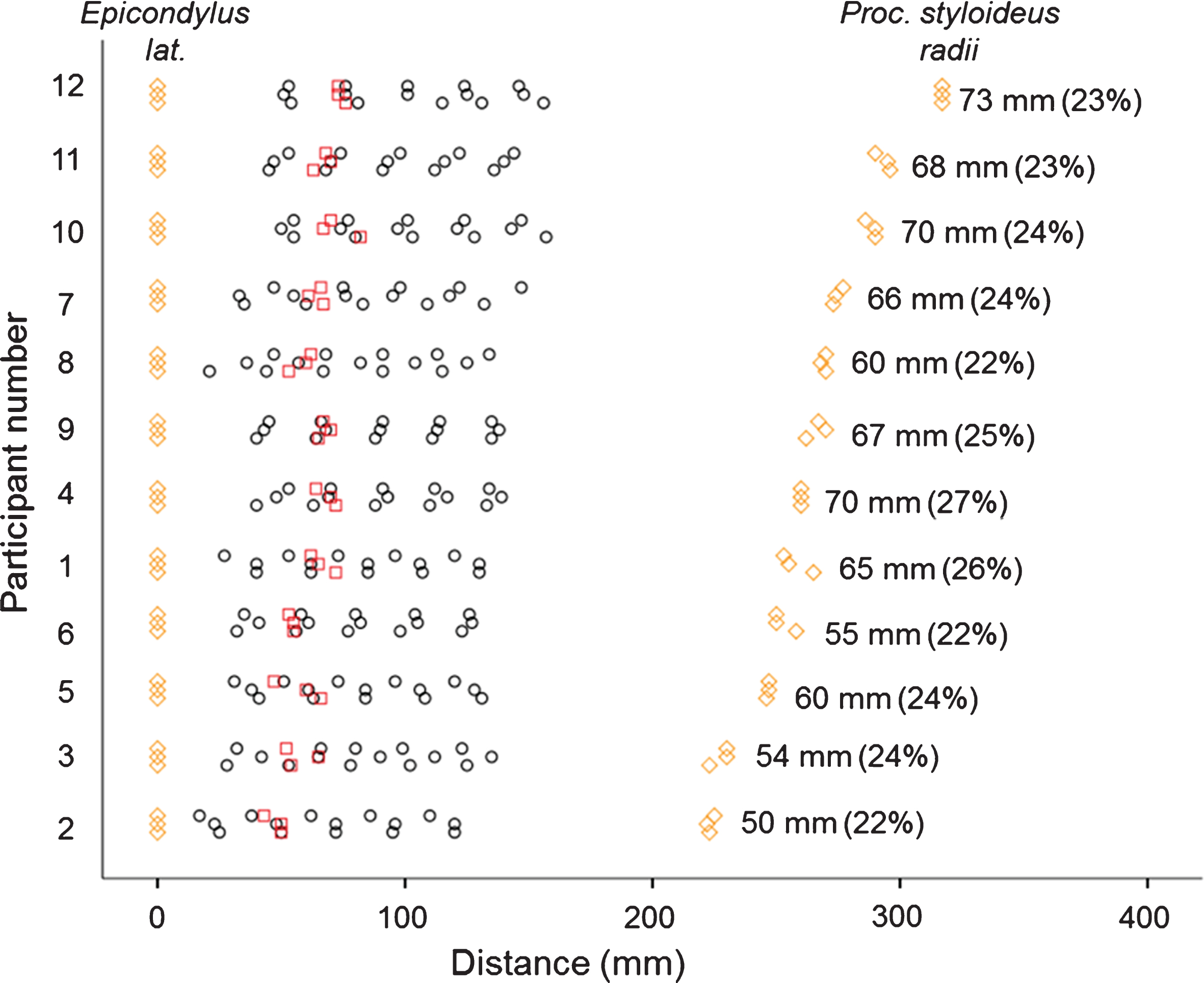
3.4Motor point
The median distance from the epicondylus lateralis humeri to the motor point was 63 mm (range 50–73 mm), approximately ¼ (range 22–27%) of the distance between the epicondylus lateralis humeri and the processus styloideus radii. This was very close to electrode 2, the one used in pairs A and B (Fig. 5).
4Discussion
In this comparison of two MVCs, and four electrode positions, the resisted wrist extension gave the highest group mean EMG amplitude for all electrode pairs, and the group mean CV was lower for the resisted wrist extension than for the hand grip for all electrode pairs. Furthermore, the group EMGamp/CV ratio was substantially higher for the resisted wrist extension than for the hand grip for all electrode pairs. ICC showed no substantial difference between the two contractions. Concerning electrode positioning, the highest group EMGamp/CV ratio in the resisted wrist extension was observed for pair A, the most proximal position, and in the hand grip for pair D. The motor point was located approximately ¼ of the distance between the epicondylus lateralis humeri and the processus styloideus radii.
4.1Maximal voluntary contractions
In the present study, 11 of the 12 subjects exhibited higher EMG amplitudes with the resisted wrist extension than with the hand grip (Fig. 4; electrode pair C). This differs from the results reported in a previous study, where both the resisted wrist extension and the hand grip were performed [23]. In that study, only 6 of the 11 subjects showed the highest EMG activity with the resisted wrist extension, while the rest of the participants showed the highest activity with the hand grip. Recalculation of the original data gave an MVE group mean of 114% when comparing the hand grip to the resisted wrist extension. In the present study, the corresponding value was 77%, which is in accordance with the results of a recent study by Meyland et al., who reported a value of 79% [17], approximately a factor of 0.8 for these studies. There is no obvious explanation for the difference between the present study and that carried out by Åkesson et al. However, in the study by Åkesson et al. the hand grip was performed with a supported forearm, which was not the case in the present study or that by Meyland et al.
The results in the current study are in good agreement with the results in a recent study by Ngo and Wells [35]. In their study, the ECR muscles also showed 1.3 times higher EMG amplitudes for the resisted wrist extension than the amplitudes obtained with the hand grip. The subjects in Ngo and Wells' study performed the resisted wrist extension with the forearm in a mid-pronated (i.e. neutral) position, while the subjects in the current study performed it in a pronated forearm position; the results from these two studies indicate that the forearm position may be of less importance when performing the MVC with the resisted wrist extension. For practical reasons, in workplace recordings, the resisted wrist extension in a pronated position may be preferred; especially if also the activity from the trapezius muscles is recorded. Then, a force transducer anchored to a heavy metal plate on the floor, can be used for both muscles.
In general, the ratio between EMG amplitude and CV, was more than twice as high for the resisted wrist extension as for the hand grip, whereas ICC showed no substantial differences between the two MVCs. Altogether, the results of this study show that the resisted wrist extension may be preferred for normalization of the forearm extensor muscles.
4.2Electrode positioning
The group mean EMG amplitude varied with the electrode position. The activity in the extensor muscles may differ considerably depending on the distance from the IZ, skin movements, arm position and the influence of surrounding muscles. Barbero et al. reported that the IZ could be located, starting from the epicondylus lateralis humeri, between 17% and 42% of the length of the forearm [36]. In the present study, lower amplitudes were obtained for most subjects with electrode pair C, compared to the other pairs of electrodes for one of the two MVCs and for both of the activations studied. It is possible that these lower amplitudes indicate the location of the IZ, and in agreement with that reported by Barbero et al. These facts, in combination with the highest ratio for the resisted wrist extension being found for pair A and for the hand grip with pair D, indicate that our present electrode pair position, pair C, is not optimal.
The highest EMG amplitudes were seen for pair D for the resisted wrist extension, the hand grip and the pinch grip. However, the reproducibility, in terms of CV, was low for these MVCs and for the activation. The reason could be that the electrodes constituting pair D are placed at the tapered and distal part of the extensor muscles, and very small changes in electrode positioning and a shortening of muscle length will result in higher CVs.
The motor point was located close to electrode 2, the electrode used in pairs A and B. This location, in combination with the lower amplitudes in pair C for one of the two MVCs and both activations, indicates that the IZ is located distally to the motor point and should not interfere with the signal given by electrode pair A. In fact, pair A seems to be located approximately half-way between the IZ and the attachment of the extensor muscles on the humerus and could therefore be a suitable alternative for electrode positioning.
Variation in electrode positioning may be one factor that influences the CV. We performed a sensitivity analysis by excluding the occasion with the most deviating positions for participant numbers 7 and 8, which reduced the CVs for both participants on average by 7% for the four electrode pairs and the MVCs and activations.
4.3Limitations
The results presented in this paper are based on the EMG amplitudes obtained in the laboratory with well-defined arm postures during specific MVCs and maximal activations, in contrast to the working situation, where there is a wide range of arm posture and wrist angles. The relations between the tested electrode positions in this study may therefore be different under real working tasks. The number of participants in the study was also small. Despite these limitations, we believe that the results make an important contribution to the discussion on recording forearm EMG.
4.4Practical implications
Since the resisted wrist extension showed a substantially higher EMGamp/CV ratio in comparison to the hand grip, the resisted wrist extension may be used as MVC in new EMG studies, both in laboratory and in work place recordings. Although there is not yet any comparisons performed in work place settings, it seems as the resisted wrist extension should give a lower inter- and intra-subject variation in comparison to the hand grip. The present findings should increase the precision in the measurements, which would also increase the quality of risk assessments that are based on EMG measurements from forearm extensor muscles. This is increasingly important as technical development make measurements more feasible also for practitioners [37], and reliable risk assessments are needed for efficient preventions of work-related musculoskeletal disorders.
In EMG research, the method of normalization and use of MVC versus reference contractions has been a controversial issue for a long time. We have hitherto considered the hand grip to be as good as the resisted wrist extension for recording the MVE of the forearm extensors [23]. However, when normalizing to the hand grip, we sometimes see unexpectedly large differences in amplitudes between the right and left forearm extensors, even when the tasks are performed bimanually. We suspect that this phenomenon occurs when the subject only activates the flexors in one of the forearms, but both flexors and extensors in the other, when performing the hand grip. By using the resisted wrist extension instead of the hand grip this problem might be solved.
5Conclusions
The best combination of reference contraction and electrode positioning, in terms of high EMG amplitude, low CV, high group EMGamp/CV ratio and a good ICC, was found for the resisted wrist extension with electrode pair A. Hence, the resisted wrist extension may be used as MVC in new EMG studies, both in laboratory and in work place recordings.
This study also indicates that the motor point is located approximately ¼ of the distance from the epicondylus lateralis humeri to the processus styloideus radii, and that the innervation zone does not interfere with the signal recorded from pair A, i.e. the most proximal electrode positions. A factor of 0.8 can be used, at group level, for comparisons between forearm extensor muscle recordings using the resisted wrist extension and the hand grip as MVCs. Further studies should be performed during actual work in work place recordings, including different work tasks with several different arm positions, to evaluate the effect of the different ways to perform MVC, and the different electrode positions.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgments
Thanks to participating colleagues at the Division of Occupational and Environmental Medicine.
References
[1] | Harris C , Eisen EA , Goldberg R , Krause N , Rempel D . 1st place, PREMUS best paper competition: Workplace and individual factors in wrist tendinosis among blue-collar workers – the San Francisco study. Scandinavian Journal of Work. Environment & Health (2011) (2):85–98. |
[2] | Bonfiglioli R , Mattioli S , Fiorentini C , Graziosi F , Curti S , Violante FS . Relationship between repetitive work and the prevalence of carpal tunnel syndrome in part-time and full-time female supermarket cashiers: A quasi-experimental study. International Archives of Occupational and Environmental Health (2007) ;80: (3):248–53. |
[3] | Nordander C , Ohlsson K , Åkesson I , Arvidsson I , Balogh I , Hansson G-Å , et al. Exposure–response relationships in work-related musculoskeletal disorders in elbows and hands – A synthesis of group-level data on exposure and response obtained using uniform methods of data collection. Applied Ergonomics (2013) ;44: (2):241–53. |
[4] | Takala EP , Pehkonen I , Forsman M , Hansson GA , Mathiassen SE , Neumann WP , et al. Systematic evaluation of observational methods assessing biomechanical exposures at work. Scand J Work Environ Health (2010) ;36: (1):3–24. |
[5] | David GC . Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occupational Medicine (2005) ;55: (3):190–9. |
[6] | Forsman M . Ergonomic risk assessments – a need for reliable and attractive methods. Kuopio, Finland: Faculty of Health Sciences, (2016) . |
[7] | American Conference of Governmental Industrial Hygienists (ACGIH). Documentation of the Threshold Limit Values for Physical Agents, 7th Ed. Cincinnati, Ohio (2001) . |
[8] | Østensvik T , Veiersted KB , Nilsen P . Association between numbers of long periods with sustained low-level trapezius muscle activity and neck pain. Ergonomics (2009) ;52: (12):1556–67. |
[9] | Westgaard RH . Effects of physical and mental stressors on muscle pain. Scand J Work Environ Health (1999) ;25: (Suppl 4):19–24. |
[10] | van Rijn RM , Huisstede BM , Koes BW , Burdorf A . Associations between work-related factors and the carpal tunnel syndrome–a systematic review. Scand J Work Environ Health (2009) ;35: (1):19–36. |
[11] | Veiersted KB , Westgaard RH , Andersen P . Electromyographic evaluation of muscular work pattern as a predictor of trapezius myalgia. Scand J Work Environ Health (1993) ;19: (4):284–90. |
[12] | Nordander C , Hansson GA , Rylander L , Asterland P , Bystrom JU , Ohlsson K , et al. Muscular rest and gap frequency as EMG measures of physical exposure: The impact of work tasks and individual related factors. Ergonomics (2000) ;43: (11):1904–19. |
[13] | Mathiassen SE , Burdorf A , van der Beek AJ . Statistical power and measurement allocation in ergonomic intervention studies assessing upper trapezius EMG amplitude. A case study of assembly work. J Electromyogr Kinesiol (2002) ;12: (1):45–57. |
[14] | Nordander C , Balogh I , Mathiassen SE , Ohlsson K , Unge J , Skerfving S , et al. Precision of measurements of physical workload during standardised manual handling. Part I: surface electromyography of m. trapezius, m. infraspinatus and the forearm extensors. J Electromyogr Kinesiol (2004) ;14: (4):443–54. |
[15] | Nordander C , Willner J , Hansson GA , Larsson B , Unge J , Granquist L , et al. Influence of the subcutaneous fat layer, as measured by ultrasound, skinfold calipers and BMI, on the EMG amplitude. Eur J Appl Physiol (2003) ;89: (6):514–9. |
[16] | Nordander C , Ohlsson K , Balogh I , Hansson GA , Axmon A , Persson R , et al. Gender differences in workers with identical repetitive industrial tasks: Exposure and musculoskeletal disorders. Int Arch Occup Environ Health (2008) ;81: (8):939–47. |
[17] | Meyland J , Heilskov-Hansen T , Alkjær T , Koblauch H , Mikkelsen S , Svendsen S , et al. Sex differences in muscular load among house painters performing identical work tasks. European Journal of Applied Physiology (2014) ;114: (9):1901–11. |
[18] | Burden A . How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. Journal of Electromyography and Kinesiology (2010) ;20: (6):1023–35. |
[19] | Mathiassen SE , Winkel J , Hägg GM . Normalization of surface EMG amplitude from the upper trapezius muscle in ergonomic studies — A review. Journal of Electromyography and Kinesiology (1995) ;5: (4):197–226. |
[20] | Hansson G-Å , Balogh I , Ohlsson K , Granqvist L , Nordander C , Arvidsson I , et al. Physical workload in various types of work: Part I. Wrist and forearm. International Journal of Industrial Ergonomics (2009) ;39: (1):221–33. |
[21] | Mukhopadhyay P , O’Sullivan L , Gallwey TJ . Estimating upper limb discomfort level due to intermittent isometric pronation torque with various combinations of elbow angles, forearm rotation angles, force and frequency with upper arm at 90° abduction. International Journal of Industrial Ergonomics (2007) ;37: (4):313–25. |
[22] | Roman-Liu D , Bartuzi P . The influence of wrist posture on the time and frequency EMG signal measures of forearm muscles. Gait & Posture (2013) ;37: (3):340–4. |
[23] | Åkesson I , Hansson GA , Balogh I , Moritz U , Skerfving S . Quantifying work load in neck, shoulders and wrists in female dentists. Int Arch Occup Environ Health (1997) ;69: (6):461–74. |
[24] | Szeto GPY , Lin JKM . A study of forearm muscle activity and wrist kinematics in symptomatic office workers performing mouse-clicking tasks with different precision and speed demands. Journal of Electromyography and Kinesiology (2011) ;21: (1):59–66. |
[25] | Elcadi GH , Forsman M , Aasa U , Fahlstrom M , Crenshaw AG . Shoulder and forearm oxygenation and myoelectric activity in patients with work-related muscle pain and healthy subjects. European Journal of Applied Physiology (2013) ;113: (5):1103–15. |
[26] | Åkesson I , Balogh I , Hansson GÅ . Physical workload in neck, shoulders and wrists/hands in dental hygienists during a work-day. Applied Ergonomics (2012) ;43: (4):803–11. |
[27] | Dong H , Loomer P , Barr A , Laroche C , Young E , Rempel D . The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Appl Ergon (2007) ;38: (5):525–31. |
[28] | Mogk JPM , Keir PJ . Crosstalk in surface electromyography of the proximal forearm during gripping tasks. Journal of Electromyography and Kinesiology (2003) ;13: (1):63–71. |
[29] | Jensen C , Vasseljen O , Westgaard RH . The influence of electrode position on bipolar surface electromyogram recordings of the upper trapezius muscle. Eur J Appl Physiol Occup Physiol (1993) ;67: (3):266–73. |
[30] | Mesin L , Merletti R , Rainoldi A . Surface EMG: The issue of electrode location. J Electromyogr Kinesiol (2009) ;19: (5):719–726. |
[31] | Hansson GA , Asterland P , Kellerman M . Modular data logger system for physical workload measurements. Ergonomics (2003) ;46: (4):407–15. |
[32] | Hansson G-Å , Asterland P , Skerfving S . Acquisition and analysis of whole-day electromygraphic field recordings. In: Hermens HJ, Hägg G, Freriks B, editors. Proceedings of the Second General SENIAM (Surface EMG for Non-Invasive Assessment of Muscles) Workshop. Stockholm, Sweden: Roessingh Research and Development; (1997) . pp. 19–27. |
[33] | Jensen C , Vasseljen O Jr , Westgaard RH . Estimating maximal EMG amplitude for the trapezius muscle: On the optimization of experimental procedure and electrode placement for improved reliability and increased signal amplitude. Journal of Electromyography and Kinesiology (1996) ;6: (1):51–58. |
[34] | Hernaez R . Reliability and agreement studies: A guide for clinical investigators. Gut (2015) ;64: (7):1018–1027. |
[35] | Ngo BPT , Wells RP . Evaluating protocols for normalizing forearm electromyograms during power grip. Journal of Electromyography and Kinesiology (2016) ;26: :66–72. |
[36] | Barbero M , Merletti R , Rainoldi A . Upper Limb. Atlas of Muscle Innervation Zones: Springer Milan; (2012) . pp. 103–120. |
[37] | Dahlqvist C , Hansson G-Å , Forsman M . Validity of a small low-cost triaxial accelerometer with integrated logger for uncomplicated measurements of postures and movements of head, upper back and upper arms. Applied Ergonomics (2016) ;55: :108–116. |




