Suspected exertional heat stroke: A case study of worker cooling in a hot and humid field environment
Abstract
BACKGROUND:
In the event of a severe occupational heat-related illness, paramedic assistance may not be immediately available. A worker’s survival may depend on their co-workers access to efficacious field-based cooling modalities. One cooling method that has been claimed to be practical in field-based settings is the ice towel method.
OBJECTIVES:
This case study assessed the practicality of the ice towel method in an industrial setting, where criteria for use include cost effectiveness, portability, scalability, and implementation by a single worker under the stress of an emergency.
METHODS:
This case study describes the emergency application of the ice towel method while awaiting paramedics, for a worker suffering suspected exertional heat stroke on a remote job site.
RESULTS:
Ice towels were able to be transported to a remote field site and applied successfully by a single worker under the stress of a potentially life-threatening emergency.
CONCLUSIONS:
The ice towel method was cost effective, scalable, transportable, and rapidly applied in a field-based emergency. This case study demonstrates the importance of organizations assessing their heat-related risks, and determining controls based upon their efficacy and practicality for their unique setting.
1Introduction
Production schedules, physical work rates, mandatory protective clothing and prolonged heat exposure amplify the prospect of workers suffering a heat-related illness, including the medical emergency of exertional heat stroke (EHS). Despite likely under-reporting, current epidemiology identifies EHS as a workplace risk [1] that is predicted to worsen [2]. Since EHS mortality and morbidity are dependent upon the duration and severity of core temperature elevation [3], medical treatment seeks to minimize area under the core temperature curve to ensure survival and prevent long-term medical complications. This is achieved through rapidly lowering core temperature, ideally within 30 minutes of symptom onset [3].
A 30-minute window for EHS treatment poses issues for many field-based work environments, particularly where responding paramedics are relied upon to administer initial treatment. This potential for treatment delay implies that EHS survival may depend on co-workers provision of effective first aid, inclusive of cooling, while medical assistance is en route. Achieving this requires workers have the means to rapidly lower core temperature, irrespective of their work location. Hence, both efficacy and practicality of EHS cooling options are important considerations.
As outlined in Table 1, core temperature cooling rates vary between EHS treatment modalities, with cold water immersion considered the gold standard for treating EHS [4]. This method has produced cooling rates of up to 0.350°C/min [5], but is not considered feasible for many field-based work settings due to the equipment and volume of cold water required. Overcoming the need for dedicated facilities, Tarp Assisted Cooling with Oscillation (TACO) utilizes a tarpaulin for field-based immersion with cooling rates of up to 0.170°C/min [6]. While effective, successful implementation of the TACO method requires numerous personnel and cold water volumes that may not be available on-site nor practical for transportation to many work locations.
Table 1
Example mean core temperature cooling rates for various cooling modalities
| Cooling Modality | Cooling Rate (°C/min) | Estimated mean time to lower Tc 1°C (mins) | Reference |
| Ice water immersion (2°C) | 0.350 | 3 | [5] |
| TACO* (9.2°C)† | 0.170 | 6 | [6] |
| Ice towels/sheets‡ | 0.160 | 6 | [10] |
| Ice towels | 0.110 | 9 | [9] |
| Combined cooling§ | 0.036 | 28 | [7] |
| Passive rest (underwear only) | 0.027 | 37 | [7] |
| Passive rest (insulated clothing) | 0.004 | 250 | [17] |
†TACO: Tarp Assisted Cooling with Oscillation. ‡Cooling rate of 0.160°C/min achieved in casualties with an initial core temperature of ≥39°C/min. §Cold packs on groin, neck, and axillae plus splashing body with water while evaporating with compressed air.
Less resource intensive cooling modalities include splashing with water, fanning a wet body and application of ice packs to superficial arteries. Table 1 demonstrates that the reported cooling rates for these modalities are substantially lower than for cold water immersion or TACO. Combining splashing with water, evaporating with compressed air, and placing cold packs on the groin, neck, and axillae produced cooling rates of 0.036°C/min [7], approximately half the cooling rate threshold deemed to be acceptable for the treatment of EHS [8].
An alternative method that can be implemented by a single person is the application and rotation of ice towels over the body. This method requires an ice bin or cooler, ice, water, and towels. Towels are submerged in the cold water and placed over the exposed skin of the torso and limbs, facilitating heat exchange as they are rotated every 2–3 minutes or as they warm. Owing to its portability and simplicity [8], the use of ice towels can be initiated anywhere within seconds of EHS symptoms and is therefore, potentially well-suited to field settings. Ice towels produced cooling rates of 0.110°C/min when applied to the torso and limbs to treat hyperthermic athletes in a field medical station [9]. An extension of this method utilizes bed linen soaked in ice-cold water (ice sheets) for treatment of EHS in military settings during transportation to a medical facility. Ice sheet cooling rates were 0.160°C/min for exertional heat stroke casualties with an initial core temperature of ≥39°C/min [10]. Collectively, this evidence suggests that the use of towels or sheets to facilitate heat transfer from the body to cold water provides a viable alternative when practical constraints preclude cold water immersion.
Despite the reporting of acceptable cooling rates, there’s a paucity of information addressing the practicality of ice towel cooling in industrial settings, where criteria for use include cost effectiveness, portability, scalability, and implementation by a single worker under the stress of an emergency. Therefore, this case study describes an organizations experience from identifying a heat-related risk, assessing the evidence, implementing the ice towel method for suspected EHS, and use in a field-based emergency.
2Context
The current case occurred in a worker of an Australian state (QLD) electrical distributer of ∼4000 field-based employees that operate in climates varying from temperate to tropical. As for many industries with outdoor workers, the prospect of heat strain symptoms and/or heat-related illness is heightened by the combination of manual work tasks, seasonal heat exposure, mandatory protective attire, and proximity to radiant heat sources. The respective risk of workers enduring heat strain symptoms or heat related illness was assessed by a workforce survey and heat-related incident data analysis for October 2018 to April 2019, otherwise known as the 2018/19 storm season. These assessments confirmed that while chronic low-grade heat strain symptoms and minor heat related illness were more likely, there was a risk of EHS, with one hospitalization during the 2018/19 season [11]. In addition to implementation of a range of heat-related controls, treatments for EHS were reviewed to determine their efficacy and field suitability [12].
With the objective of rapidly reversing elevated core temperature in austere field conditions, various cooling methods were considered as part of the internal review. While ice towel cooling rates were available, there was limited published information for other industrial considerations. In December 2019, the organization distributed in excess of 1100 heat stroke kits (one per field vehicle), consisting of an ice bin (locally known as an esky) and two towels (cotton towels 1.2 m×0.6 m). Field workers also completed online heat stress training that included how the heat stroke kits were to be incorporated into the first aid response to EHS. In the event of EHS, the organizations heat stress standard recommended medical assistance be immediately sought and ice towels be applied to initiate cooling of the worker as an addition to the standard first aid response.
3Key elements of the event
In the current case, a worker, Worker A, was operating in Northern QLD, Australia, on a site approximately 8 km from the local township. At the time of the incident, ambient temperature 29.5°C, relative humidity 72% and a wind speed of 4 km/h were recorded at the nearest Bureau of Meteorology weather station, approximately 4.8 km from the work site.
Worker A, a 28 year old male Vacuum Truck operator was the first onsite, where he described conditions as hot, very humid and with limited airflow. It was reported that it had rained during the previous night. Worker A had been on site for approximately 3 hours, conducting work that was considered manual and strenuous when he began to feel very hot and unwell. He phoned his manager (Manager A) to indicate that he was going to take a break in the shade and pour water over his head to cool down. Manager A informed Worker A that he was travelling to site.
Another worker, Worker B, was immediately informed by Manager A of the situation and commenced travel to the site to perform a welfare check on Worker A, arriving approximately 20 minutes later. Initially, Worker B could not locate Worker A and confirmed that conditions onsite were very hot, humid with little to no breeze. The vehicle of Worker A was located but Worker A was not present. Worker B then located Worker A a short distance away under some vegetation. Worker A had been vomiting and was noted as semi-conscious, breathing, not responding to verbal stimuli, and having skin that was very hot to touch. Worker B had completed organizational heat stress training and recognized Worker A’s signs and symptoms as the potentially life-threatening EHS.
Worker B immediately called the QLD emergency hotline and described the situation and the organizations EHS first aid protocol involving the application of ice towels. The emergency dispatcher reassured Worker B to proceed with the application of the ice towels, and that paramedics were en route. Worker B removed the shirt of Worker A and began applying an ice towel to the torso of Worker A. Worker B continued to apply the towel to the torso and rather than rotating towels, he reapplied cold water to the towel as it heated up. Approximately 10 minutes later, two additional workers (Worker C and Worker D) arrived onsite. Worker C assisted Worker B with the ice towel, while Worker D waited to direct the paramedics to Worker A. A few minutes later, Manager A arrived on site. Cooling was applied to Worker A for a total of approximately 15 minutes until paramedics arrived and assumed responsibility.
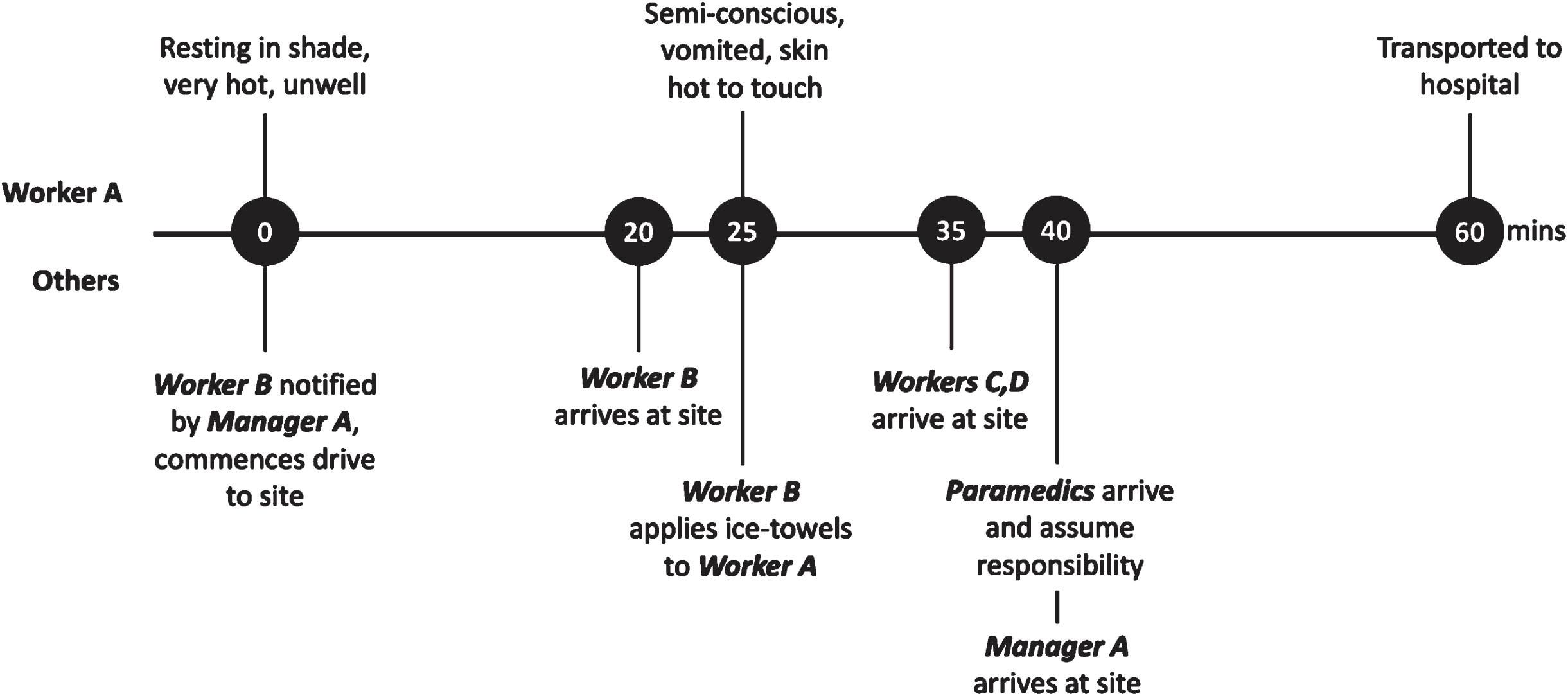
Paramedics remained onsite for approximately 20 minutes treating Worker A. Worker A was subsequently transported to the local hospital and reported being discharged without medical complications approximately 6 hours later with a diagnosis of heat stroke. Worker A has since made a full recovery, noting that he experienced a lack of heat tolerance in the weeks post-event. Worker B stated that paramedics indicated that if cooling had not been initiated when it was, Worker A would have likely suffered irreversible damage or even death. A timeline of key events from the reporting of symptoms is presented in Fig. 1.
Fig. 1
Timeline of key events from the reporting of symptoms.
4Discussion
Rectal temperature is considered the gold standard for assessing core temperature, with the commonly utilized aural thermometry reported to consistently underestimate core temperature in hyperthermic individuals [13]. In the current case, rectal temperature was not measured, hence, the core temperature curve of Worker A remains undetermined. Feeling hot prior to collapsing, vomiting, skin that was hot to touch, and a semi-conscious state indicative of central nervous system impairment, are potential indicators of EHS [14]. Observation of EHS signs and symptoms are essential in work settings, where first aid provision to an EHS victim generally occurs in the absence of valid core temperature measurement. Previously it has been suggested that if collapse occurs during or immediately following the cessation of heavy physical work in hot environments, and a rectal temperature cannot be measured, EHS should be the presumptive diagnosis [15]. In the current case the collective of signs and symptoms were indicative of EHS, and verbal accounts of a heat stroke diagnosis from treating hospital staff, forms the basis for EHS diagnosis.
Despite recognition of ice towels as a potential field-based alternative to water immersion for EHS treatment [12, 16], we are not aware of reports describing their practical application in field based industrial settings. While this case study does not contribute data relating to core temperature cooling rates, it provides a pragmatic description of ice towel application during a suspected EHS in the field. For implementation of ice towels in an industrial setting, cost, portability, scalability, and number of personnel required to implement are relevant considerations that have not been reported in the literature.
Once notified of Worker A’s condition, Worker B transported the heat stroke kit to site without issue, and therefore, the ice towel method was considered practical in this context. Due to the minimal equipment required, once Worker A was located and assessed by his colleague, the ice towel method was administered immediately, thereafter. Given that mortality and morbidity are dependent on the duration and severity of hyperthermia [3], the prompt administration of cooling likely averted a far more serious outcome in this case as reasoned by the paramedics.
‘Worker B’ also indicated that the simplicity of the method facilitated its application under the cognitive stress of this emergency. Furthermore, the application of ice towels were initiated by a single person without issue, as opposed to the alternate field-based method of TACO which requires multiple people to successfully implement.
In the context of occupational use, the method is simple, cost effective, and scalable. In the current case the method was applied to an organization with thousands of vehicles, however the method could easily be scaled for an organization with as little as a single vehicle. Space availability can be an issue on commercial vehicles, yet in the current case the eskies had a volume of 25 liters with dimensions of 420 mm×350 mm×360 mm (L×W×H).
It should be noted that in the current case, all field-based employees completed online heat stress training, inclusive of EHS signs and symptoms and implementation of the ice towel method. All field workers are also trained in the provision of first aid.
Limitations of this case study should be acknowledged. This case study involved a single individual from the electrical utilities industry. When evaluating the suitability of the ice towel method, organizations should consider the existing and evolving evidence, in addition to the specific industrial environment in which the method will be applied. Likewise, legislative, regulatory and/or local customs need to be considered, as globally, these vary significantly.
Future research should consider broader applications of the ice towel method to other industrial environments. In addition to evaluating cooling rates, such research should account for the logistical considerations when applying the method in occupational settings.
5Conclusions
Climate change represents a significant challenge to Occupational Health and Safety [18]. It is important that organizations ensure adequate controls are in place to mitigate a hazard that is predicted to worsen [2]. This case study describes an organization’s experience from identifying a heat-related risk, assessing the evidence, implementing a field-based cooling treatment for suspected EHS, and describing its practicality when utilized in a field-based emergency. The organization in which this case study transpired involves workers operating in field environments where paramedic assistance is not always readily available. In this setting, the ice towel method proved to be cost effective, easily transportable, and simple to implement by a single worker under the stress of an emergency.
Ethical approval
Not applicable as this case study is a retrospective analysis of an occupational health and safety incident.
Informed consent
Both Energy Queensland and the workers referenced in this case study, gave consent for the case study to be published and the learnings to be shared.
Conflict of interest
S.R. is an employee of the organization in which the events of this case study transpired. M.B. is the managing director of Thermal Hyperformance Pty Ltd., which provides heat stress management services to maximize the health, safety and performance of heat-exposed workers. The results reported within this case study do not materially alter the nature of this work.
Author contributions
Both authors were involved in the manuscript preparation including drafting, editing, revising and approval of final version.
Funding
No funding was provided for this case study.
Acknowledgments
Appreciation is expressed to the workers involved in the documented incident, and Energy Queensland, for their assistance in the generation of the manuscript.
References
[1] | Morrissey MC , Kerr ZY , Brewer GJ , Tishukaj F , Casa DJ , Stearns RL . Analysis of exertion-related injuries and fatalities in laborers in the United States. Int J Environ Res Public Health. (2023) ;20: :2683. Doi:10.3390/ijerph20032683. |
[2] | Hunt AP , Brearley M , Hall A , Pope R . Climate change effects on the predicted heat strain and labour capacity of outdoor workers in Australia. International Journal of Environmental Research and Public Health. (2023) ;20: :5675. Doi:10.3390/ijerph20095675. |
[3] | Adams WM , Hosokawa Y , Casa DJ . The Timing of Exertional Heat Stroke Survival Starts prior to Collapse. Curr Sports Med Rep. (2015) ;14: :273–4. Doi:10.1249/JSR.0000000000000166. |
[4] | Casa DJ , McDermott BP , Lee EC , Yeargin SW , Armstrong LE , Maresh CM . Cold water immersion: The gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. (2007) ;35: :141–9. Doi:10.1097/jes.0b013e3180a02bec. |
[5] | Proulx CI , Ducharme MB , Kenny GP . Effect of water temperature on cooling efficiency during hyperthermia in humans. J Appl Physiol. (2002) ;94: :1317–23. Doi:10.1152/japplphysiol.00541.2002. |
[6] | Hosokawa Y , Adams WM , Belval LN , Vandermark LW , Casa DJ . Tarp-Assisted Cooling as a Method of Whole-Body Cooling in Hyperthermic Individuals. Ann Emerg Med. (2016) ;69: :347–52. Doi:10.1016/j.annemergmed.2016.08.428. |
[7] | Kielblock AJ , Van Rensburg JP , Franz RM . Body cooling as a method for reducing hyperthermia. An evaluation of techniques. S Afr Med J. (1986) ;69: , 378–80. |
[8] | McDermott BP , Casa DJ , Ganio MS , Lopez RM , Yeargin SW , Armstrong LE , Maresh CM . Acute whole-body cooling for exercise-induced hyperthermia: A systematic review. J Athl Train. (2009) ;44: :84–93. Doi:10.4085/1062-6050-44.1.84. |
[9] | Armstrong LE , Crago AE , Adams R , Roberts WO , Maresh CM . Whole-body cooling of hyperthermic runners: Comparison of two field therapies. Am J Emerg Med. (1996) ;14: :355–8. Doi:10.1016/S0735-6757(96)90048-0. |
[10] | DeGroot DW , Henderson KN , O’Connor FG . Cooling modality effectiveness and mortality associate with prehospital care of exertional heat stroke casualities. J Emerg Med. (2023) ;64: :175–80. Doi:10.1016/j.jemermed.2022.12.015. |
[11] | Rogerson S , Brearley M , Meir R , Brooks L . Influence of Age, Geographical Region and Work Unit on Heat Strain Symptoms: A Cross-Sectional Survey of Electrical Utility Workers. J Occup Environ Hyg. (2020) ;17: :515–22. Doi:10.1080/15459624.2020.1834112. |
[12] | Brearley MB . Are Recommended Heat Stroke Treatments Adequate for Australian Workers? Ann Work Expo Health. (2019) ;63: :263–6. Doi:10.1093/annweh/wxz001. |
[13] | Huggins R , Glaviano N , Negishi N , Casa DJ , Hertel J . Comparison of rectal and aural core body temperature thermometry in hyperthermic, exercising individuals: A meta-analysis. J Athl Train. (2012) ;47: :329–38. Doi:10.4085/1062-6050-47.3.09. |
[14] | Gauer R , Meyers BK . Heat-Related Illnesses. Am Fam Physician. (2019) ;99: :482–9. |
[15] | DeGroot DW , O’Connor FG , Roberts WO . Exertional heat stroke: An evidence based approach to clinical assessment and management. Exp Physiol. (2022) ;107: (10):1172–83. Doi:10.1113/EP090488. |
[16] | Casa DJ , DeMartini JK , Bergeron MF , Csillan D , Eichner ER , Lopez RM , Ferrara MS , Miller KC , O’Connor F , Sawka MN , et al. National athletic trainers’ association position statement: Exertional heat illnesses. J Athl Train. (2015) ;50: :986–1000. Doi:10.4085/1062-6050-50.9.07. |
[17] | Brearley M , Berry R , Hunt AP , Pope R . A Systematic Review of Post-Work Core Temperature Cooling Rates Conferred by Passive Rest. Biology. (2023) ;12: :695. Doi:10.3390/biology12050695. |
[18] | Ferrari GN , Leal GCL , Thom de Souza RC , Galdamez EVC . Impact of climate change on occupational health and safety: A review of methodological approaches. Work. (2023) ;74: (2):485–99. Doi:10.3233/WOR-211303. |




