Care workers’ positive health during the COVID-19 pandemic: Psychometric properties of the Finnish version of the Salutogenic Health Indicator Scale and an 18-month follow-up
Abstract
BACKGROUND:
There is a need to shift from biomedical and pathogenic approaches to salutogenic approach.
OBJECTIVE:
To validate the Finnish version of the SHIS by testing its psychometric properties in care workers and to assess the SHIS score over time.
METHODS:
We first conducted a survey in 2020 (T1) and tested the psychometric properties of SHIS among care workers. We repeated the survey in spring 2022 (T2) among the same subjects. We analyzed the changes in SHIS, self-rated health (SRH), work ability (WAS), sickness absence and occupational calling between T1 and T2. Thereafter, we compared changes between health care sectors’ and the other sectors’ care workers.
RESULTS:
The results showed an increase in positive health measured with the SHIS and the occupational calling, a decrease in the SRH, and an increase in the number of sickness-related absences among all the care workers between T1 and T2. There was no change in their WAS. The health care workers had a lower SHIS than the other sectors’ care workers in both T1 and T2, but the increase in their SHIS was parallel to that of the other workers.
CONCLUSION:
SHIS is a useful and reliable measure of positive health and can be used in studies when determining subjective health instead of, or in addition to, diagnoses. It was able to detect the health changes caused by the COVID-19 pandemic. SHIS is capable of capturing the underlying salutogenic approach of health promotive resources.
1Introduction
Positive health focuses on capabilities and is a more comprehensive conceptualization of health than the original definition of health by the World Health Organization [1]. More than merely achieving a degree of wellness, the positive health concept sees health as a resource for everyday life. This understanding was conceptualized in the WHO’s Ottawa Charter [2]. The salutogenic model of health introduced the health continuum, where health is understood as a movement in a continuum on an axis of total ill-health to total health. It seeks to find conditions that generate and improve health, i.e., to create positive health rather than concentrate on illness [3]. Bauer et al. [4] recognized the need to develop the original idea of health by embedding a positive health continuum from Antonovsky’s model. Health care systems in Western countries need this shift from biomedical and pathogenic approaches to this salutogenic approach [5].
A core concept of the salutogenic model of health is the sense of coherence (SOC), which is an individual’s perception of life as comprehensible (structured, organized, and consistent), manageable (can be dealt with due to the availability of enough resources), and meaningful (worthy of investment and engagement). Based on empirical evidence, SOC can promote and maintain positive health [6]. This is because while Antonovsky [3] stated that stressors will always be with us, we can manage the tension with which we humans respond to such stressors by, according to Mittelmark and Bauer [7], learning to mobilize our resources, such as our health. Antonovsky [8] and Antonovsky and Sourani [9] added that SOC strengthens when we have enough mobilizable resources to resist stressors.
A tool for measuring positive health based on salutogenic orientation is the Salutogenic Health Indicator Scale (SHIS). Developed by Bringsén et al. in 2009 [10], SHIS holistically considers well-being’s physical, mental, and social dimensions and does not forget illness, as it can prevent people from achieving their goals [10]. Thus, SHIS considers health a vital resource for achieving individual goals and coping with everyday strains. On the other hand, work is one of the main resources that can produce, maintain and promote health, or lead to illness [11].
SHIS was first validated in hospital staff (n = 483) [10]. Bringsén et al. [10] drew out two factors of SHIS from an exploratory factor analysis (EFA): the subject’s intrapersonal characteristics (α=0.90) and interactive functions (α=0.84). The internal consistency of the full scale was found to have been excellent (α=0.92). However, subsequent studies considered the scale one-dimensional. Nilsson Lindström et al. [12] conducted cognitive interviews to assess the validity of SHIS, and the results showed that SHIS had high validity from a qualitative perspective. Garmy et al. [13] validated the psychometric properties of SHIS in an adolescent population and found it one-dimensional. Warne et al. [14] adapted a shorter version of SHIS, the Positive Health Scale (PHS), to measure adolescents’ health.
SHIS has since been used in studies, often in the context of work and particularly among health care workers. A high SHIS score has been associated with supportive working conditions [15], positive internal work experiences [15–19], time experience in work [20], work-life balance [17, 21], energy [18], and recovery [17]. Bergström et al. [22] found that after relocation to open-plan offices, workers’ SHIS scores decreased, and Hansen et al. [23] showed that leader-based workplace health interventions in small-scale enterprises improved workers’ SHIS scores. Also, Persson et al. [16] found that belongingness in one’s work team and positive relationships with managers and care recipients were significant predictors of a high SHIS score among health care workers. In a comprehensive review, Masanotti et al. [24] showed that the salutogenic model provides a solid theoretical basis for examining work organization in health care. A healthy working environment fosters health workers’ positive health. Therefore, resolving the effects of stress and its management at an individual level may not resolve challenges in health care organizations. [25].
This study covered a period of 18 months of the COVID-19 pandemic, from fall 2020 to spring 2022. The COVID-19 outbreak in 2020 evolved from an acute to a chronic stress situation [26] and has continued to 2022. In line with the salutogenic model, the measurement of individuals’ SOC predicted changes in their psychopathological symptoms from before the COVID-19 outbreak to after its outbreak [27]. The results showed that higher levels of SOC buffered the negative impact of COVID-19 stressors on general health. Broetje et al. [28] demonstrated in a longitudinal study how job resources were related to coherence at work, which had a reciprocal relation to SOC. Notably, nurses experienced high levels of burnout during the COVID-19 pandemic [29]. During the pandemic’s peak, nurses’ employment and working conditions were associated with poor physical and mental health [30].
SHIS has not been used in studies during the COVID-19 pandemic to survey the effect of a pandemic on positive health. However, the positive health model of Huber [31] was used to study older people’s experiences at the start of the pandemic [32]. The cross-sectional study of Moens et al. [32] measured changes in positive health based on self-reports of recent experiences and experiences a year earlier and showed a decrease in positive health.
1.1Aims
This study has two objectives: (1) to validate the Finnish version of the SHIS by testing its psychometric properties in care workers (Phase 1) and (2) to assess the SHIS score over time (Phase 2).
2Methods
2.1Study design
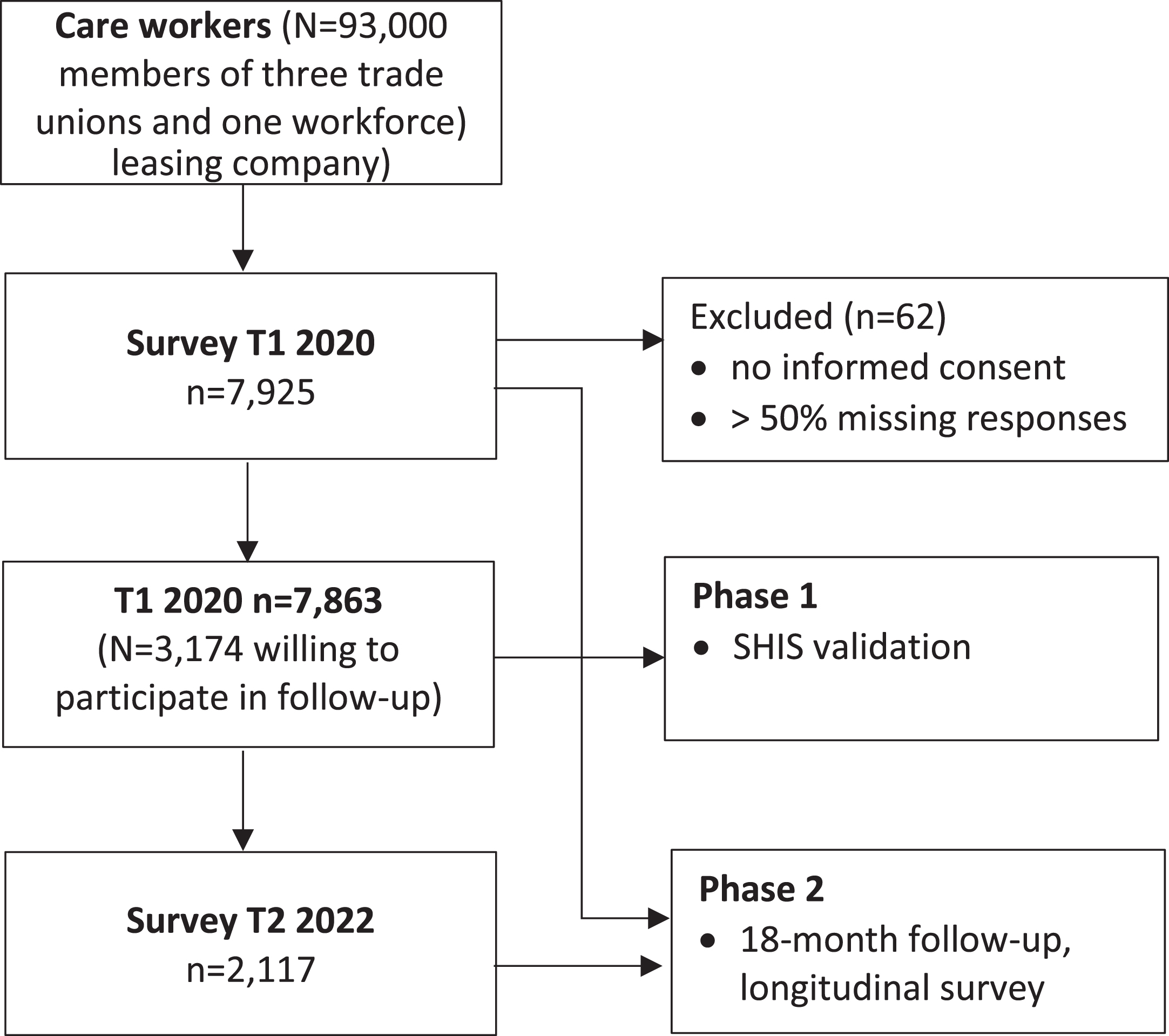
This study was conducted in two phases (Fig. 1). Phase 1 was a cross-sectional descriptive study of the validity of SHIS conducted in Finland in the fall of 2020 (T1). For the study, we followed the COSMIN (Consensus-based standards for selecting health measurement instruments) methodology [33]. Phase 2 was an 18-month follow-up longitudinal survey of the Phase 1 volunteer participants (n = 3,174) in spring 2022 (T2). For this phase, we followed the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines for reporting cohort studies [34].
Fig. 1
Flowchart of the study.
2.2Study context
This study included an extensive range of care sector workers in health care, social services, early education, school assistance, and youth services. Examples of these professions are workers in childcare, elderly care, and health care of all types. Care work constitutes a substantial labor market globally. A third of European women are employed in the care sector [35]. In Finland, the sector is female-dominated, and most women therein are registered nurses (requiring a bachelor’s degree) and practical nurses (requiring a professional degree). Finland is undergoing a remarkable reform in health and social services. The principal aim of the reform is to shift the focus from treatment to prevention, which, in the long term, is expected to decrease costs and help to prioritize the use of resources to reduce health inequalities. There are considerable health inequalities in Finland in several dimensions: geographic, educational, gender, and ethnic. Therefore, introducing all means of reliably assessing population health from the resource-based perspective is highly timely.
2.3Data collection and participants
Survey data were collected from members of three trade unions and one workforce leasing company (N = 93,000) between September and November 2020 on the online survey site webropol.com. The three trade unions represented public and private sector workers in health care, social services, early education and childcare, and youth services. We asked the human resources personnel of two of the trade unions and the workforce leasing company to send their members our invitations to participate in this study, and one trade union advertised this study in its monthly newsletter. Two reminders were sent. The care workers were informed that they could participate in this study by responding to the webropol.com questionnaire. The only inclusion criterion was age: the respondent had to be between 15 and 74 years. A total of 7,925 workers participated, translating to a response rate of 9%. Seven participants were excluded because they did not give their informed consent. In addition, we excluded the participants with more than 50% missing responses. Thus, the final sample size was 7,863 care workers. The most common profession was a practical nurse (69%), followed by social sector workers (19%), such as social assistants and social counselors.
In Phase 2, a questionnaire was sent to the T1 respondents who consented to participate in the follow-up survey and gave their email addresses. The questionnaire was sent to 3,174 care workers, of whom 2,117 responded, for a response rate of 67%. Their age and gender were similar to those who were unwilling to participate in the follow-up survey. However, the latter had a significantly higher educational attainment than the Phase 2 participants.
2.4Measures
SHIS includes 12 statements that answer the following question: “How have you felt in the last four weeks with regard to the following?” The statements describe experiences of energy, state of morale, tension, sleep, concentration, creativity, resolution, expression of feelings, illness, energy level, social capacity, and physical function. The statements are presented in the form of a semantic differential, where options range from positive to negative on a scale of 6 to 1, respectively. Examples of statements are “In the last four weeks, I have felt alert (6)” and “In the last four weeks, I have felt exhausted (1).” SHIS can be used as a one-dimensional index of health, with the total score ranging from 12 to 72, where a higher score indicates better health.
The authors of SHIS [10] were permitted to translate the English version of the SHIS in this study to Finnish. The first author of this study translated the scale into Finnish, and then an official translator back-translated it into English. The translations were assessed and discussed in a research group in both phases. The final questions were tested with a group of 10 nurses and researchers and proved clear and easy to answer.
The self-rated health (SRH) was measured with one question about the respondent’s current health state. The score ranged from 1 (Poor) to 5 (Good). SRH is a one-item measure of a person’s perceived health status widely used in population-based epidemiological studies. It can describe health close to how a qualitative continuum describes it, as defined in the salutogenic approach [9]. It can be positive or negative [36]. Furthermore, it predicts all-cause mortality and morbidity [37].
The work ability score (WAS) measures a person’s perceived work ability with one question, the answer to which is scored on a scale of 0 (Totally disabled) to 10 (Excellent work ability). WAS is the first item in the larger-scale Work Ability Index (WAI), but it can measure work ability as reliably as the WAI [38]. It predicts disability pension, long sick leaves, and health-related quality of life [39].
The Calling and Vocation Questionnaire (CVQ) measures a person’s perceived calling [40] with 12 statements. An example of a statement is, “I believe that I have been called to my current line of work.” All the statements were assessed on a scale of 1 (Not at all true of me) to 4 (Absolutely true of me). The total score was the sum of the scores for all the statements and thus ranged from 12 to 48. A higher total score indicated a higher level of perceived calling.
2.5Statistical analyses
We assessed the types of missing data with Little’s MCAR test, assuming that if p > .05, data were missing completely at random. The incompleteness of the data due to missing responses for each item was considered acceptable if it was≤5%. The psychometric properties of SHIS were tested using exploratory factor analysis (EFA), reliability analysis, and assessment of criterion validity [41]. Concerning our sample size (n = 7,863), it was not only suitable for factor analysis because it was > 300, but it can even be considered excellent because it was > 1,000 [42]. Before running the EFA, we assessed the suitability of our data for factor analysis with the Kaiser-Meyer-Olkin (KMO) Measure of Sampling Adequacy and Bartlett’s Test of Sphericity [41]. A KMO index > 0.50 and a significant (p < .05) Bartlett’s Test of Sphericity indicated that our data were suitable for factor analysis. Inter-item correlations of r > 0.3 were also checked and set as an inclusion criterion for data suitability.
We assessed data dimensionality and homogeneity with EFA because earlier psychometric assessments of SHIS were somewhat contradictory [10, 13]. We applied EFA with principal component analysis and oblique factor rotation to allow for correlations between the factors [41]. In earlier studies, SHIS was shown to load either on one or two factors; when our data loaded on two factors, they were expected to be correlated. To determine the number of factors, we used eigenvalues > 1 and investigated scree plots [43]. The relevant factor structure was assessed with communalities > 0.40 and variances of loadings of at least 60%.
We also run confirmatory factor analysis (CFA) to confirm the scale structure [44]. Chi-square goodness of fit test (with a level p > 0.05) was used to evaluate whether a model departs significantly from one that fits exactly the data. Model fit was assessed acceptable when the following fit indices, the Normed fit index (NFI), Comparative fit index (CFI), Relative fit index (RFI), Incremental fit index (IFI), and Tucker-Lewis index (TLI) were≥0.90. Last, the root mean-square error of approximation (RMSEA) was considered a good fit if < 0.05.
Scale reliability was assessed as internal consistency, and a Cronbach’s alpha coefficient value of 0.70 was considered acceptable. We assessed the convergent validity of the SHIS score with health indicators such as the SRH, sickness-related absence, WAS, and perceived calling (CVQ) as Pearson’s correlation coefficients. We hypothesized that SHIS correlates positively with SRH, WAS, and CVQ and negatively with sickness-related absence. We also compared the SHIS scores of the health care workers and the other sectors’ workers with ANOVA (Analysis of variance) to assess the known-group validity [42]. We hypothesized that the health care workers would have lower SHIS scores than the other sectors’ workers. This is because of the burden of the COVID-19 pandemic, the ensuing lack of personnel, and problems with the working conditions even in the pre-pandemic era, which were associated with decreased well-being.
To analyze the SHIS scores over time, we first assessed the reliability of SHIS in T2 with Cronbach’s alpha. Then, we compared the SHIS, SRH, sickness-related absence, WAS, and CVQ values of all 2,117 workers T1 and T2 using repeated measures ANOVA. Finally, we ran repeated measures generalized linear regression to determine the measures of the health care workers and other sectors’ workers in T1 and T2. The significance was set at p < .05. All the tests were performed with SPSS version 27.
2.6Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. According to Finnish law, this type of study does not need ethical approval. However, the Institutional Review Boards (IRBs) of the participating trade unions and workforce leasing company gave the authors their permission to collect their members’ data. The participants were asked in an online form for their informed consent to participate in this study and to have their results published before they were asked to answer the questionnaire.
3Results
The participants were mostly women (93%), half of them were aged between 35 and 54 years, and most of them were permanently employed (82%), had a professional degree (79%), and were working in health care (38%). Table 1 shows the participant profiles.
Table 1
Characteristics of care workers in T1 (n = 7,863)
| Mean (SD) | n | % | |
| Age, years | 48.2 (10.9) | ||
| <35 | 1,050 | 13.4 | |
| 35–54 | 3,929 | 50.0 | |
| ≥55 | 2,722 | 34.6 | |
| Gender | |||
| Male | 469 | 6.0 | |
| Female | 7,290 | 92.7 | |
| Other or don’t want to tell | 74 | 0.9 | |
| Education | |||
| Professional degree | 6,173 | 78.5 | |
| Bachelor’s degree or higher | 1,663 | 21.1 | |
| Sector | |||
| Health care | 2,970 | 37.8 | |
| Social services | 2,736 | 34.8 | |
| Education | 2,082 | 26.6 | |
| Othera | 40 | 0.5 | |
| Profession | |||
| Practical nurse | 5,417 | 68.7 | |
| Registered nurse | 444 | 5.7 | |
| Social worker | 1,494 | 19.0 | |
| Early education teacher | 140 | 1.8 | |
| Otherb | 127 | 1.6 | |
| Employment type | |||
| Permanent | 6,409 | 81.5 | |
| Temporary | 1,373 | 17.5 |
aTrade, service sector, etc. bSecretaries, cleaners, et al.
The SHIS items had very few missing values (0.3–0.6%), and the data were missing completely at random (p = .919). The data were suitable for factor analysis because the KMO index was 0.95, and the BTS was significant (p < .001). Also, all the inter-item correlations were significant (p < .01), ranging from r = 0.393 to r = 0.795, and all the items were applied in the EFA. The eigenvalues showed that only one factor (eigenvalue > 1) was extracted. This explains the 62.7% of the variance, which is acceptable. All the communalities were > 0.40 and varied from 0.41 to 0.78 (Table 2). The SHIS showed high internal consistency (α=0.94), and the deletion of any item would not have raised Cronbach’s alpha.
Table 2
Communalities, factor loadings, means (SD), and missing values of SHIS among care workers in T1 (n = 7,863)
| SHIS items | Communalities | Factor loadings | M (SD) |
| Energy experience | 0.72 | 0.85 | 3.49 (1.42) |
| State of morale | 0.74 | 0.86 | 3.84 (1.24) |
| Tension | 0.72 | 0.85 | 3.74 (1.30) |
| Sleep | 0.53 | 0.73 | 3.51 (1.48) |
| Concentration | 0.72 | 0.85 | 3.76 (1.29) |
| Creativity | 0.49 | 0.70 | 3.37 (1.34) |
| Resolution | 0.58 | 0.76 | 3.97 (1.21) |
| Expression of feelings | 0.62 | 0.79 | 4.13 (1.31) |
| Illness | 0.59 | 0.77 | 3.85 (1.41) |
| Energy level | 0.78 | 0.89 | 3.59 (1.33) |
| Social capacity | 0.41 | 0.64 | 4.84 (1.04) |
| Physical function | 0.61 | 0.78 | 3.92 (1.41) |
| Total score | 45.9 (12.49) |
SD: Standard deviation. SHIS: Salutogenic Health Indicator Scale.
Results from the CFA for unidimensional structure showed a good model fit as χ2(4)=9,080, p = 0.59 when variances were allowed to correlate. Also, fit indices were excellent (NFI = 1,000; RFI = 0,998; IFI = 1,000; TLI = 0,999; CFI = 1,000 and RMSEA = 0,013).
SHIS was correlated strongly with SHR (r = 0.65) and WAS (r = 0.65); moderately with CVQ (r = 0.32); and negatively with sickness-related absence (r = -0.20). All the correlations were significant (p < .05). The test of known-group validity confirmed our hypothesis, since the health care workers (M = 43.95, SD = 12.68) had significantly (p < .001) lower scores in SHIS than the other professionals (M = 47.11, SD = 12.22).
The Cronbach’s alpha in T2 (α=0.94) was as good as in T1. The SHIS score was higher in T2 than in T1 (Table 3). The SRH was significantly lower, and the CVQ was significantly higher in T2. The sickness-related absence increased significantly between 2020 and 2022. The WAS was higher in T2 than in T1, although the change was not significant.
Table 3
Means (SD) of the SHIS and test factors in T1 and T2 (n = 2,117)
| T1 | T2 | ||||
| M | SD | M | SD | p | |
| SHIS | 45.03 | 12.59 | 46.05 | 12.44 | .004 |
| SRH | 3.70 | 1.03 | 3.63 | 0.97 | .012 |
| Sickness-related absence | 16.18 | 33.88 | 20.08 | 40.11 | .001 |
| WAS | 7.21 | 2.04 | 7.32 | 1.91 | .057 |
| CVQ | 31.28 | 7.07 | 32.54 | 7.08 | <.001 |
SHIS: Salutogenic Health Indicator Scale. SRH: Self-Rated Health. WAS: Work Ability Score. CVQ: Calling and Vocation Questionnaire.
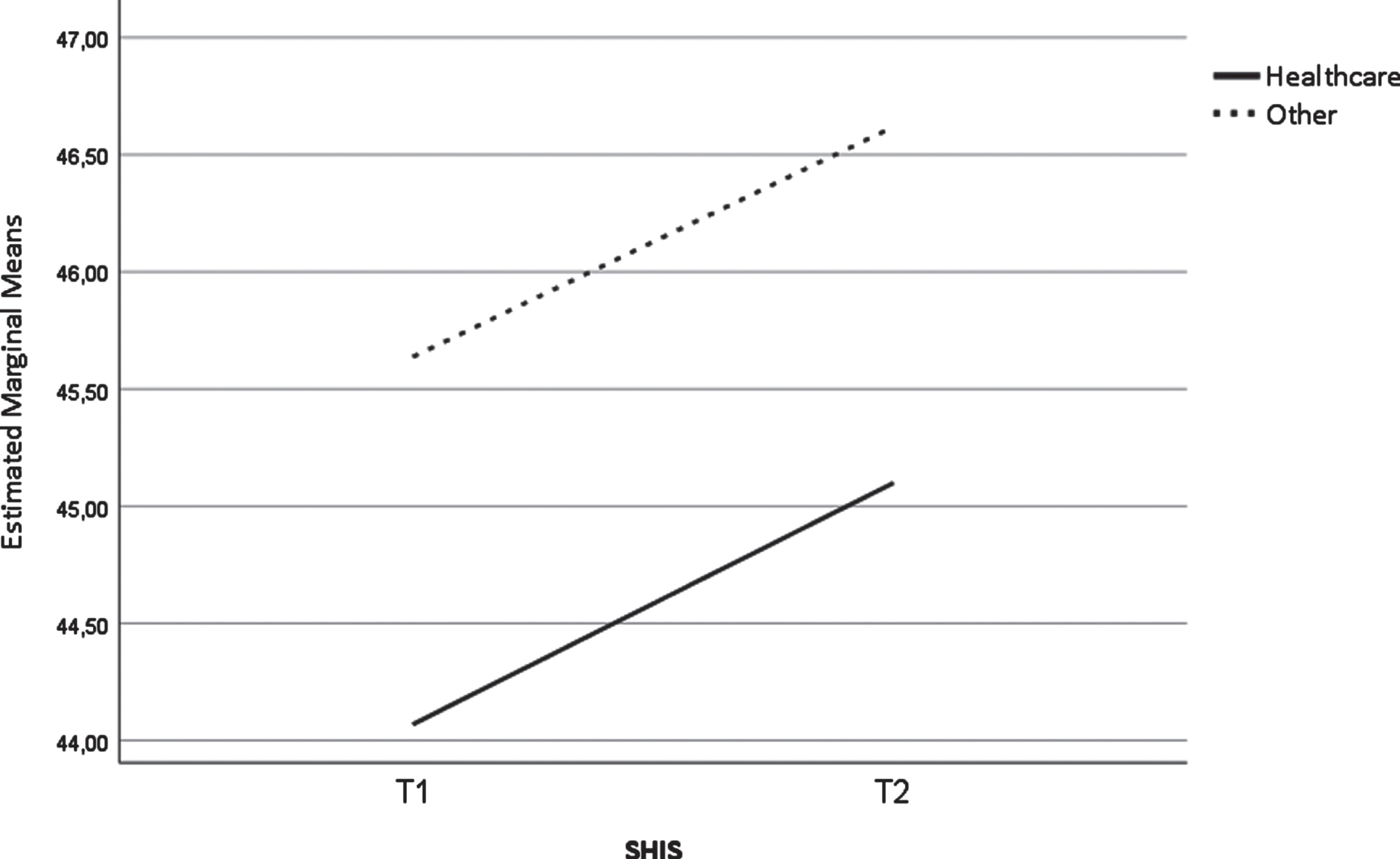
The SHIS scores of the health care workers were significantly lower in T1 (M = 44.08, SD = 12.06) and T2 (M = 45.10, SD = 12.60) than the SHIS scores of the other sectors’ workers (M = 45.64, SD = 12.83 and M = 46.62, SD = 12.28, respectively). The change in SHIS in time between the two sectors (Fig. 2) did not differ significantly [F(1,2102) = 0.005, p = .946].
Fig. 2
Change in the SHIS between the two time points among healthcare workers (n = 822) and other sectors’ workers (n = 1,286).
4Discussion
This study validated SHIS, which measures subjective health and considers a person’s perception of his or her positive health. Our results showed that SHIS is a valid and reliable instrument for adult workers as it can accurately detect changes in their perceived positive health over time. Interestingly, our study also showed that the SHIS scores of all the workers in T2 were higher than in T1. This finding contrasts with the wealth of research evidence on the adverse health effects of the COVID-19 pandemic [26]. However, in line with earlier evidence [27], this study showed lower perceived health of health care workers than of other sectors’ care workers.
SHIS can show a person’s conception of life as comprehensible, manageable, and meaningful, which reflects the person’s mobilizable resource of positive health. Particularly interesting in our findings is the increase in calling during the pandemic. Our study suggests that despite the burden of the COVID-19 pandemic, it bared the meaningfulness and importance of the care workers’ profession, which gave them positive energy and well-being. Meaningful work is an essential dimension of nurses’ occupational calling that helps them engage in work and empowers them to cope with the burden of work [45]. Zhu et al. [46] showed that during the COVID-19 pandemic, nurses’ daily work emergencies were positively associated with their daily assessed calling. However, in ordinary times, the calling is more or less permanent [47]. While nurses were fighting COVID-19 on the front lines, their calling might have shone, and their positive health might have improved because they finally became visible in society [48]. To conclude, our findings suggest that during the COVID-19 pandemic, one of the resources of positive health for nurses was (meaningful) work, which is also one of the crucial determinants of health [49].
Our findings propose that SRH and salutogenic perception of health are two distinct constructs, even though they are strongly correlated. A comparison of the two health measurement instruments, SHIS and SRH, shows that SHIS clearly covers health perception more broadly than SRH. On the other hand, the one-item SRH may indicate a person’s physical condition more accurately, as it was found to predict morbidity and mortality [50]. Our results showed a decrease in SRH during the COVID-19 pandemic, which is in line with the result of previous research [51]. In another research, the decrease in SRH was more significant in women than in men, even without COVID-19 symptoms [52]. Of all the health care workers, nurses were the most exposed to the virus, as they worked in high-risk environments and care units. More than 3,000 nurses have died during the pandemic [27, 53]. However, increased burnout and a decline in mental health appear to have caused the greatest harm to nurses during the pandemic [26].
As expected, the health care workers had lower SHIS scores than the other sectors’ workers, and the difference between their SHIS scores remained similar between T1 and T2. Our results, which showed lower SHIS scores among the health care workers, registered nurses, and practical nurses, might reflect the global problems in nursing. The severe shortage of nurses [54] is one of the reasons for their poor working conditions and increasing physical, mental, and emotional burdens [55]. Other reasons are poor pay, lack of recognition and appreciation of the profession [48], and problems with management [56]. All these challenges detrimentally affect nurses’ well-being. While flexible working arrangements, which changed the time and place of work, have been associated with better health during the pandemic [57], such flexibilities affected nurses very little, if at all, during and before the pandemic.
To our knowledge, this study is the only one that performed salutogenic positive health measurements in the COVID-19 pandemic era. However, several studies have investigated SOC, which is expected to decrease with adversity [58]. Danioni et al. [59] identified SOC profiles among adult Italians at the start of the pandemic and after four months based on two dimensions: combined comprehensibility and manageability and meaningfulness. They identified seven profiles, the most common of which was stability in comprehensibility and manageability and a downward trajectory in meaningfulness. These results raise two questions: first, whether it is possible to distinguish between the dimensions of SOC, and second, whether such a short follow-up period as four months can show reliable changes.
4.1Limitations
This study’s strength is its longitudinal design, which covered 18 months of the current COVID-19 pandemic. However, the results should be viewed with caution, as the response rate for the first data collection round was only 9%. In addition to the burden of the COVID-19 pandemic, the low response rate might have been due to the inability of the researchers to communicate directly with the target group. In addition, one union advertised the study in its membership newsletter instead of sending emails, which may have further decreased the response rate. Because of the risk of bias due to the low response rate, we compared the first and last respondents, as the last respondents were assumed to be equivalent to the non-respondents [60]. However, there was no statistical difference in the age, gender distribution, and level of education of the two groups. According to the Finnish Nurses’ Association, the study participants represented well Finnish nurses’ age and gender distribution [61]. The second data collection response rate was adequate (67%). We compared the first-round respondents willing to participate in a follow-up survey with the non-willing first-round respondents and found no significant differences in their background and characteristics. Of course, all our health measurements were based on self-reports. The use of registers would yield more reliable health status results.
5Conclusion
Our findings showed that the COVID-19 pandemic was burdensome but, at the same time, provided care workers with meaningful work experience. The SHIS reliably assessed the positive health of the care workers and the changes therein over time. This short health scale could be used in population studies that conceive health as a holistic resource beyond epidemiological and pathogenic paradigms. A salutogenic approach to health is needed as health systems shift their focus and resources from treatment to prevention.
Ethical approval
The Institutional Review Boards (IRBs) of the participating trade unions and a workforce leasing company granted research permits.
Informed consent
The participants gave their informed consent in an online form.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgments
Not applicable.
Funding
This work was funded by the Finnish Work Environment Fund (200197). The funder had no role in the study design, data analysis, decision to publish, or manuscript preparation.
References
[1] | WHO. Constitution of the World Health Organization [Internet]. 1948 [cited 2022 May 26]. Available from: https://www.who.int/about/governance/constitution. |
[2] | WHO. Ottawa charter for health promotion [Internet]. 1986 [cited 2022 May 26]. Available from: https://www.who.int/publications/i/item/ottawa-charter-for-health-promotion. |
[3] | Antonovsky A. Health, stress, and coping: New perspective on mental and physical well-being. San Fransisco: Jossey-Bass, (1979) . |
[4] | Bauer GF , Roy M , Bakibinga P , et al. Future directions for the concept of salutogenesis: a position article. Health Promot Int. (2020) ;35: :87–195. |
[5] | Kalkowski P , Paul G . Wellness Customers and Their Needs. Leisure, Health and Well-Being. (2017) ;61–72. |
[6] | Eriksson M. The Sense of Coherence: The Concept and Its Relationship to Health. The Handbook of Salutogenesis. (2022) ;61–68. |
[7] | Mittelmark MB , Bauer GF . Salutogenesis as a Theory, as an Orientation and as the Sense of Coherence. The Handbook of Salutogenesis. (2022) ;11–17. |
[8] | Antonovsky A. The salutogenic model as a theory to guide health promotion. Oxford: Oxford University Press, (1996) . |
[9] | Antonovsky A , Sourani T . Family Sense of Coherence and Family Adaptation. J Marriage Fam. (1988) ;50: :79. |
[10] | Bringsén Å , Andersson HI , Ejlertsson G . Development and quality analysis of the Salutogenic Health Indicator Scale (SHIS). Scand J Public Health. (2009) ;37: :13–19. |
[11] | Bakker AB , Demerouti E . The Job Demands-Resources model: State of the art. J Manag Psychol. (2007) ;22: (3):309–328. |
[12] | Nilsson Lindström P , Ejlertsson G , Andersson I , et al. Evaluating the usability of two salutogenic instruments on health and work experience, using cognitive interviewing. J Workplace Behav Health. (2019) ;33: :241–259. |
[13] | Garmy P , Berg A , Clausson EK , et al. Psychometric analysis of the Salutogenic Health Indicator Scale (SHIS) in adolescents. Scand J Public Health. (2017) ;45: :253–259. |
[14] | Warne M , Snyder K , Gådin KG . Adaptation and Validation of a Positive Health Scale for Adolescents. Soc Indic Res. (2013) ;119: :1079–1093. |
[15] | Nilsson P , Andersson HI , Ejlertsson G . The Work Experience Measurement Scale (WEMS): a useful tool in workplace health promotion. Work. (2013) ;45: :379–387. |
[16] | Persson SS , Lindström PN , Pettersson P , et al. Workplace relationships impact self-rated health: A survey of Swedish municipal health care employees. Work. (2018) ;60: :85–94. |
[17] | Ejlertsson L , Heijbel B , Ejlertsson G , et al. Recovery, work-life balance and work experiences important to self-rated health: A questionnaire study on salutogenic work factors among Swedish primary health care employees. Work. (2018) ;59: :155–163. |
[18] | Ejlertsson L , Heijbel B , Brorsson A , et al. Is it possible to gain energy at work? A questionnaire study in primary health care. Prim Health Care Res Dev. (2020) ;21: :e65. |
[19] | Lindmark U , Wagman P , Wåhlin C , et al. Workplace health in dental care – a salutogenic approach. Int J Dent Hyg. (2018) ;16: :103–113. |
[20] | Andruškiene J , Kuzmiene A , Martinkenas A , et al. Psychosocial work experiences related to health: A study of Lithuanian hospital employees. Work. (2016) ;53: :669–677. |
[21] | Törnquist Agosti M , Bringsén Å , Andersson I . The complexity of resources related to work-life balance and well-being–a survey among municipality employees in Sweden. Int J Hum Resour Manag. (2017) ;28: :2351–2374. |
[22] | Bergström J , Miller M , Horneij E . Work environment perceptions following relocation to open-plan offices: A twelve-month longitudinal study. Work. (2015) ;50: :221–228. |
[23] | Hansen E , Landstad BJ , Gundersen KT , et al. Leader-Based Workplace Health Interventions - A Before-After Study in Norwegian and Swedish Small-Scale Enterprises. Int J Disabil. (2016) ;11: :e15. |
[24] | Masanotti GM , Paolucci S , Abbafati E , Serratore C , Caricato M . Sense of coherence in nurses: A systematic review. Int J Environ Health Res. (2020) ;17: :1861. |
[25] | Langius A , Bjorvell H , Antonovsky A . The Sense of Coherence Concept and its Relation to Personality Traits in Swedish Samples. Scand J Caring Sci. (1992) ;6: :165–171. |
[26] | Mana A , Catz O , Mana Y , et al. How Do People Cope During the COVID-19 Pandemic and Stay Well? A Salutogenic Longitudinal Study in Israel. Front Psychol. (2021) ;12: :729543. |
[27] | Schäfer SK , Sopp MR , Schanz CG , et al. Impact of COVID-19 on Public Mental Health and the Buffering Effect of a Sense of Coherence. Psychother Psychosom. (2020) ;89: :386–392. |
[28] | Broetje S , Bauer GF , Jenny GJ . The relationship between resourceful working conditions, work-related and general sense of coherence. Health Promot Int. (2020) ;35: :1168–1179. |
[29] | Galanis P , Vraka I , Fragkou D , et al. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. (2021) ;77: :3286–3302. |
[30] | Llop-Gironés A , Santillan-Garcia A , Cash-Gibson L , et al. COVID-19 and the global need for knowledge on nurses’ health. Int Nurs Rev. 2021; Epub ahead of print October 6. DOI: 10.1111/INR.12722. |
[31] | Huber M , André Knottnerus J , Green L , et al. How should we define health? BMJ. (2011) ;343: :d4163. |
[32] | Moens IS , van Gerven LJ , Debeij SM , et al. Positive health during the COVID-19 pandemic: a survey among community-dwelling older individuals in the Netherlands. BMC Geriatr. (2022) ;22: (1):51. |
[33] | Mokkink LB , de Vet HCW , Prinsen CAC , et al. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual Life Res. (2018) ;27: :1171–1179. |
[34] | Vandenbroucke JP , von Elm E , Altman DG , et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. (2007) ;4: :1628–1654. |
[35] | ILO. Care work and care jobs for the future of decent work, [Internet]. 2018 [cited 2022 May 26]. Available from: https://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/—publ/documents/publication/wcms_633135.pdf. |
[36] | Reile R , Leinsalu M . Differentiating positive and negative self-rated health: Results from a cross-sectional study in Estonia. Int J Public Health. (2013) ;58: :555–564. |
[37] | Szybalska A , Broczek K , Puzianowska-Kuznicka M , et al. Self-rated health and its association with all-cause mortality of older adults in Poland: The PolSenior project. Arch Gerontol Geriatr. (2018) ;79: :13–20. |
[38] | el Fassi M , Bocquet V , Majery N , et al. Work ability assessment in a worker population: Comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health. (2013) ;13: :1–10. |
[39] | Kinnunen U , Nätti J . Work ability score and future work ability as predictors of register-based disability pension and long-term sickness absence: A three-year follow-up study. Scand J Public Health. (2018) ;46: :321–330. |
[40] | Dik BJ , Eldridge BM , Steger MF , et al. Development and Validation of the Calling and Vocation Questionnaire (CVQ) and Brief Calling Scale (BCS). J Career Assess. (2012) ;20: :242–263. |
[41] | Boateng GO , Neilands TB , Frongillo EA , et al. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front Public Health. (2018) ;6: :149. |
[42] | Costello AB , Osborne J . Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. (2005) ;10: :7. |
[43] | Williams B , Onsman A , Brown T . Exploratory factor analysis: A five-step guide for novices. Australas J Paramedicine. (2010) ;8: :1–13. |
[44] | Crowson M. Confirmatory factor analysis using AMOS with CAT Personality Disorder Subscale Data. University of Oklahoma. 2020. |
[45] | Kallio H , Kangasniemi M , Hult M . Registered nurses’ perceptions of having a calling to nursing: A mixed-method study. J Adv Nurs. (2022) ;78: :1473–1482. |
[46] | Zhu Y , Chen T , Wang J , et al. How critical activities within COVID-19 intensive care units increase nurses’ daily occupational calling. J Appl Psychol. (2021) ;106: :4–14. |
[47] | Dik BJ , Shimizu AB . Multiple Meanings of Calling: Next Steps for Studying an Evolving Construct. J Career Assess. (2018) ;27: :323–336. |
[48] | van der Cingel M , Brouwer J . What makes a nurse today? A debate on the nursing professional identity and its need for change. Nurs Philos. (2021) ;1–7. |
[49] | Ahonen EQ , Fujishiro K , Cunningham T , et al. Work as an Inclusive Part of Population Health Inequities Research and Prevention. Am J Public Health. (2018) ;108: :306–311. |
[50] | Mutz J , Lewis CM . Cross-classification between self-rated health and health status: longitudinal analyses of all-cause mortality and leading causes of death in the UK. Sci Rep. (2022) ;12: :459. |
[51] | Stubbs JM , Achat HM , Schindeler S . Detrimental changes to the health and well-being of healthcare workers in an Australian COVID-19 hospital. BMC Health Serv Res. (2021) ; 21. Epub ahead of print December 1. DOI: 10.1186/S12913-021-07013-Y. |
[52] | Wels J , Hamarat N . A shift in women’s health? Older workers’ self-reported health and employment settings during the COVID-19 pandemic. Eur J Public Health. (2022) ;32: :80–86. |
[53] | ICN. International Council of Nurses COVID-19 Update [Internet]. 2022 [cited 2022 May 26]. Available from: https://www.icn.ch/sites/default/files/inline-files/ICN%20COVID19%20update%20report%20FINAL.pdf. |
[54] | WHO. Nursing and midwifery [Internet]. 2020 [cited 2022 May 27]. Available from: https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery. |
[55] | Matilla-Santander N , Ahonen E , Albin M , et al. COVID-19 and Precarious Employment: Consequences of the Evolving Crisis. Int J Health Serv. (2021) ;51: :226–228. |
[56] | Majeed M , Fatima T . Impact of exploitative leadership on psychological distress: A study of nurses. J Nurs Manag. (2020) ;28: :1713–1724. |
[57] | Shifrin NV , Michel JS . Flexible work arrangements and employee health: A meta-analytic review. Work & Stress. (2021) ;36: :60–85. |
[58] | Braun-Lewensohn O , Sagy S , Sabato H , et al. Sense of coherence and sense of community as coping resources of religious adolescents before and after the disengagement from the Gaza Strip. Isr J Psychiatry Rel Sci. (2013) ;50: :110–117. |
[59] | Danioni F , Sorgente A , Barni D , et al. Sense of Coherence and COVID- A Longitudinal Study. J Psychol. (2021) ;155: :657–677. |
[60] | Rönmark EP , Ekerljung L , Lötvall J , et al. Large scale questionnaire survey on respiratory health in Sweden: effects of late- and non-response. Respir Med. (2009) ;103: :1807–1815. |
[61] | Finnish Nurses. Finnish Nurses is a professional association for nurses [Internet]. 2022 [cited 2022 May 27]. Available from: https://sairaanhoitajat.fi/meista-enemman/. |




