Effect of the COVID-19 pandemic on depression, perceived stress and hypochondria of frontline dental staff (FDS): A cohort study
Abstract
BACKGROUND:
The coronavirus 2019 (COVID-19) pandemic had several mental effects on medical staff.
OBJECTIVE:
This study intended to evaluate deviations in Frontline Dental Staff (FDS) depression, perceived stress and hypochondria during the COVID-19 outbreak, and to assess whether the existence of potential risk-factors influenced these symptoms over time.
METHODS:
This prospective cohort study surveyed FDS three periods from February 1, 2021 to April 8, 2022. FDSs’ mental health was assessed through Beck Depression Inventory, Cohen Perceived Stress and the Evans Self-Illness Questionnaires; multivariate linear regression were used to identify potential factors associated with changes on each outcome (depression, perceived stress and hypochondria) over time. All analyses were performed in STATA ver. 14.
RESULTS:
In a total of 635 FDS, about 69%, 83%, and 71% reported relative depression, 77%, 87%, and 64% reported moderate to high stress level, and 60%, 76% and 74% reported moderate hypochondriac from first, second, and third survives, respectively. The mean and standard deviation of the variables increased dramatically at second survive (July 17 to October 21, 2021) and decreased again at third survive significantly. Being female, working in public sector, and low socioeconomic level were main predictors of higher levels of depression (p < 0.001) and perceived stress (p < 0.001). Perceived stress was a strong predictor of high-level depression (t = 7.79, p < 0.001).
CONCLUSION:
FDSs’ depression, stress and hypochondria were high and positively associated with being female, working in public-sector, and low socioeconomic level. To increase the effectiveness and decrease work burnout, psychological support should be provided.
1Introduction
Coronavirus 2019 (COVID-19) has developed into a global pandemic in a comparatively short time. The social distancing program has created several stressful events in life: loss of freedom, separation and reduced interaction with family and relatives, but also the inability to work affects mental health [1]. The COVID-19 pandemic has dramatically impacted the health system and population health as well as the practice of dental care [2, 3].
Dental workers are exposed to a variety of occupational hazards including noise and vibration, dental amalgam, and contaminants [4, 5]. Biological agents are another type of occupational hazard, in which dentists can become contaminated through saliva, blood, contaminated instruments and bioaerosols from patients in the environment or in the air. It consists of airborne dispersion of droplets or fine dust containing infectious agents such as SARS-CoV, and COVID-19 [6, 7]. Concerns about the transmission of the coronavirus in the dental office are widespread around the world. Depending on the type of dental procedure and the dental team proximity to the patient, the disease can easily be transmitted from infected patients to the dental team and vice versa and then to other patients if no suitable infection control measures are taken [8]. The Occupational Safety and Health Administration (OSHA) prepared a document which divides the risk of exposure into four categories, with dentistry in the highest risk category [9]. The occurrence of COVID-19 has had a mostly negative effect on the work of dentists. Routine dental procedures are discontinued with any dental care because of the several risk such as cross-infection. In addition, the oral mucosa has been recognized as a route of entry for infection that restricts dental activities to treat emergencies and emergency procedures to reduce the build-up of drops or aerosols. In addition, dental companies and industries have decided to suspend some of their staff. Dentists are ethically committed to reducing regular work to prevent the spread of infections among their families and patients. However, they are also very concerned about the financial consequences of imprisonment [10–12].
Mental disorders are one of the most important and significant components of the overall disease burden [13]. Communities around the world suffer directly from the high rates of infection associated with increased mortality and other indirect effects on physical and mental health [14]. Exposure to new unknown stressors carries the risk of developing new or worsening pre-existing mental health problems, such as symptoms of anxiety, depression, increased mental stress, and hypochondria [15]. These psychological stressors could not only affect the performance of healthcare professionals in addressing the challenges of the COVID-19 pandemic, but also affect their general well-being and long-term mental health [16]. Mohsin et al. demonstrated that COVID-19 has disrupted the readiness of dentists for clinical rotation and reduced their confidence in the clinical setting. Due to lack of preparation and lack of confidence, most dental interns are not willing to come to the hospital to work on time [5]. Although studies at the mental outcomes of the COVID-19 disaster remains with inside the early stages of development, there are posted research that help the belief that worry is a chief contributing aspect with inside the extended fees of despair and generalized tension which can be being located worldwide [17–19].
Depression is a mood disorder that causes prolonged feelings of sadness and loss of interest. Therefore, defend the intellectual fitness of healthcare experts as a great deal as viable to get the pandemic below manipulate and defend the intellectual fitness of healthcare experts with inside the quick and lengthy term [15]. Hypochondria, also known as health anxiety, is also a relatively enduring trait, but it specifically focuses on excessive anxiety or worry about serious illness and one’s own health [20]. Hypochondria correlates positively with depression and anxiety [21].
There has been controversy over the impact of the COVID-19 outbreak on the mental health of dentist especially FDS. Mekhemar et al. reported that German dental students showed a total of slight effects of the outbreak on the assessed psychological aspects [22]. Zhao et al. showed that during the COVID-19 pandemic, FDS were more likely to suffer from anxiety disorders than the general public [23]. In another study, Hakami et al. reported increased levels of depression, anxiety, and stress [24]. Nakhostin et al. found that there was no significant difference between depression and anxiety among Iranian medical students before and after the COVID-19 outbreak [25]. Sharma et al. showed that during the COVID-19 outbreak, dentists’ emotional well-being ratings were low. Gender, marital status, socioeconomic status, years of experience, practices in the clinic, and their average number of patients treated per month known as influencing factors on a dentist’s mental health [26].
Finally, there is no comprehensive evidence for the interactions of COVID-19 and the mental status of dental staff using multiple tools to detect precise interactions and effects, so we decided to analyze mental status during COVID-19 from different perspectives using different questionnaires. In addition, there are poor evidence in the field of analyzing of potential risk-factors influenced on mental health status of dental staff over time in developing countries. Therefore, the present study aimed to investigate depression, perceived stress and hypochondria during the COVID-19 outbreak in Frontline Dental Staff (FDS), and to assess whether the existence of potential risk factors influenced these symptoms over time.
2Materials and methods
2.1Study design and setting
This prospective cohort study was conducted based on STROBE checklist. This study included three COVID-19 peaks (fourth, fifth, and sixth peaks) periods. The study period was from February 1 to March 2, 2021 (first survey, after peak 3), July 17 to October 21, 2021 (second survey, during peak 5, which was the most intense period), and March 10 to April 8, 2022 (third survey, after the complete subsidence of COVID-19 in Iran). The study setting was public dental clinics in Ardabil province, north-west of Iran. In Iran, the Deputy for Health at the Iranian Ministry of Health and Medical Education (MOHME) as Secretariat of the National Headquarters issued the legislation related to dealing with and controlling the COVID-19 pandemic. Data related to COVID-19 at all levels, including information related to its incidence, prevalence, and psychological and social effects, were recorded daily in the form of a comprehensive COVID-19 data registration system [27].
2.2Study participants and sampling
Snowball sampling method was used with focus on recruiting frontline dentists (working in public health system clinic settings during COVID-19) in Ardabil. Participating FDS were also encouraged to invite new respondents from their contacts. The minimum sample size in the present study was calculated for each data gathering round based on the total number of dentists of public and private clinics list according to the following formula (equation 1):
(1)
Inclusion criteria in this study was: obtaining informed consent, graduated dentists. Having at list 6 month work experiences, ability to answer questionnaire questions, ability to communicate and the absence of mental illness in self-declaration and no use of any drugs. Exclusion criteria was defined as declaration of illness or chronic mental disorder before the study, death of first-degree relatives three months ago by COVID-19, working as a dentist, and failure to complete the informed consent form. Conscious consent with inside the shape of studies ethics changed into acquired from all individuals earlier than the begin of the study.
2.3Data collection tools and techniques
A week after the third peak of COVID-19 in Iran, we started collecting data by sending e-mails to frontline dentist staff who were in the researchers’ contact list and posting information about the study in social networks. Participants involved in web-based interview by Google Meet (video-communication service developed by Google) and questionnaires were completed through an online platform (Google Forms). At the start of the interviews, the researchers provided the necessary explanations about the goals and stages of the research and the informed consent form was obtained from them. Then, four questionnaires including demographic information, Beck Depression Inventory (BDI), Cohen Perceived Stress Questionnaire (PSS-14) and the Evans Self-Illness Questionnaire for Completion were filled by the eligible FDS. All participants answered all questions because the online questionnaire platform was designed in such a way that it was impossible to move on to the next question without answering the previous question. The online survey questionnaire was organized in such a way that from the outset, the participants stated their consent to participate in the study by ticking the identified box. Participants were then asked for basic demographic information with predefined options. In the next step, participants were asked to answer questions from the depression questionnaire, the perceived stress questionnaire, and the Evans hypochondriac questionnaire. Finally, while thanking the participants for their time in the study, each received a free internet for a month as a reward for participating in the study. All questionnaires are in Persian, validity and reliability previously confirmed.
2.3.1Beck Depression Inventory (BDI)
The BDI, created by Aaron T. Beck, is a 21-question multiple-choice self-report inventory, one of the most commonly used psychometric tests to measure depression severity. Each question consists of four sentences. Each of these sentences in each question expresses a state of the person. The pupil needs to examine the terms of every organization so as and carefully. Then select a word in every organization that fine describes his or her present-day feelings. This check is for humans over sixteen years old. The interpretation of the scores for this questionnaire will be such that first the scores of each of the 21 questions presented in the questionnaire must be added together. Then, according to the sum of scores, the rate of depression in students is determined as follows:
[1–10: Natural]; [11–16: Slightly depressed]; [17–20: Need to consult a psychologist or psychiatrist]; [21–30: Relatively depressed]; [31–60: Severe depression]; [≥60: Excessive depressions].
The validity of the BDI has been confirmed and its reliability has been reported using Cronbach’s alpha method of 0.89 and even higher, which is acceptable [28].
2.3.2The Perceived Stress Scale (PSS)
The original 14-item PSS version assesses a person’s feelings and thoughts about events and situations that have occurred over the past month. So far, this questionnaire has been translated into various languages, including Arabic, Persian, Swedish, Spanish, Chinese, Japanese and Turkish. The minimum age that your research samples should have is 17 years old. The approach of scoring the Perceived Stress Questionnaire includes 14 gadgets wherein 7 gadgets are positive and seven gadgets are negative. The negative component evaluates the dearth of manipulate and negative emotional reactions, whilst the positive component evaluates the extent of cap potential to deal with outside stressors over the last month. Each item is evaluated on a scale of 5 options: 0 = never to 4 = many times. In this questionnaire, questions 4, 5, 6, 7, 9, 10, 13, and 7 positive items are scored upside down. PASS-14 scores range from 0–56, with higher scores indicating greater perceived stress. Score categories are: Low Stress (scores 0 – 18), Moderate Stress (scores 19 – 37), High Stress (scores 38 – 56) [29]. The validity of the Cohen Perceived Stress Questionnaire was confirmed and its reliability was reported to be 0.83 and even higher using Cronbach’s alpha method, which is acceptable [30, 31].
2.3.3Evans hypochondriac questionnaires
The hypochondria questionnaire was designed and developed in 1980 by Evans to familiarize with hypochondria. This questionnaire consists of 36 questions and individuals based on the score obtained in the healthy (0–20), borderline (21–30), mild (31–40), moderate (41–60) and severe (above 60) groups. The reliability of the questionnaire was calculated using Cronbach’s alpha method of 0.86 and its validity has been confirmed in most studies that have used this tool to measure self-morbidity [32, 33].
2.4Data analysis
The questionnaire assessed demographic variables, such as age, gender, marital status or socioeconomic status, intending to characterize the sample and to test its representativeness of the population (FDS who work in healthcare settings in Iran). Moreover, it assessed risk factors potentially associated with mental health symptoms among FDS, which can be divided into four major sections: (1) personal factors; (2) working conditions; (3) economic status; and (4) attitude towards COVID-19. Socioeconomic status was categorized into three levels (low, middle, and high) based on the participants self-report. The characteristics of the sample at baseline were summarized by mean and standard deviation (SD) for quantitative variables and by frequency and percentages for qualitative variables.
During the COVID-19 pandemic, t-check became used to assess statistics regarding the traits and well-known occasions of FDS. The imply despair degree ratings and perceived pressure in FDS have been measured the use of the pupil t-check. Variance evaluation became used to assess FDSs’ despair, perceived pressure and hypochondria through well-known traits and well-known occasions, multiple regression evaluation became accomplished to research the correlation among depression, perceived stress and hypochondria with admire to explanatory variables. All analyses were performed in Stata software ver. 14, and a significance level of 0.05 was considered. To conduct a multivariate linear regression in Stata (equation 2), we used two commands, manova and mvreg. The manova command indicates if all of the equations, taken together, are statistically significant. The F-ratios and p-values for four multivariate criterion are given, including Wilks’ lambda, Lawley-Hotelling trace, Pillai’s trace, and Roy’s largest root. Next, we used the mvreg command to obtain the coefficients, standard errors, etc., for each of the predictors in each part of the model. We also showed the use of the test command after the mvreg command. The use of the test command is one of the compelling reasons for conducting a multivariate regression analysis.
(2)
3Results
3.1FDSs’ general characteristics
In total, 635 FDS were included in the study from three step survives (first round = 204, second round = 207, and third round = 214). About 53.2% of the participants were male, 46.6% of all participants were 30 to 36 years old, and 81.7% were married. Based on the results, 51.1% of all FDS categorized themselves in middle socioeconomic status. Table 1 indicates the demographic distribution of the studied samples.
Table 1
General characteristics and conditions of FDS during three survives during the COVID-19 outbreak (n = 635)
| Variables | Survive 1 (n = 214) | Survive 2 (n = 207) | Survive 3 (n = 214) | Time dif. | |||
| (February 1 to March 2, 2021) | (July 17 to October 21, 2021) | (March 10 to April 8, 2022) | |||||
| n | % | n | % | n | % | ||
| Gender | |||||||
| Male | 101 | 47.4 | 96 | 46.2 | 100 | 46.6 | 0.314 |
| Female | 113 | 52.6 | 111 | 53.8 | 114 | 53.4 | |
| Age (year) | |||||||
| <30 | 53 | 24.6 | 49 | 23.9 | 45 | 20.8 | 0.068 |
| 30–36 | 103 | 47.9 | 93 | 44.8 | 100 | 46.5 | |
| ≥36 | 59 | 27.5 | 65 | 31.3 | 70 | 32.7 | |
| Marital status | |||||||
| Married | 177 | 82.7 | 169 | 81.8 | 173 | 80.9 | 0.168 |
| Single | 37 | 17.3 | 38 | 18.2 | 41 | 19.1 | |
| Work at private section | |||||||
| Yes | 128 | 59.7 | 125 | 60.6 | 133 | 62.3 | 0.332 |
| No | 86 | 40.3 | 82 | 39.4 | 81 | 37.7 | |
| History of mental illness | |||||||
| Yes | 11 | 5.1 | 9 | 4.3 | 11 | 5.3 | 0.605 |
| No | 203 | 94.9 | 198 | 95.7 | 203 | 94.7 | |
| Socioeconomic status | |||||||
| Low | 42 | 19.4 | 42 | 20.3 | 46 | 21.5 | 0.229 |
| Middle | 105 | 49.2 | 107 | 51.5 | 113 | 52.6 | |
| High | 67 | 31.4 | 58 | 28.2 | 55 | 25.9 | |
3.2FDSs’ depression, perceived stress and hypochondria
Table 2 summarizes the continuous scores from of depression, perceived stress, and hypochondria among FDS during three survives based on participants’ general characteristics. Based on the results, the means of depression, perceived stress and hypochondria had significantly higher scores at second survive (July 17 to October 21, 2021), exactly during the fifth peak of COVID-19 in all subgroups (p < 0.05). Notwithstanding the notable impact of COVID-19 during different peaks across all subgroups, females, FDS aged≥36 years old, married, whom did not work at private section, and FDS with lower socioeconomic status reported significantly higher level of depression, perceived stress and hypochondria then males during all times.
Table 2
Depression, perceived stress, and hypochondrias based on general characteristics and conditions of FDS during the COVID-19 outbreak (n = 635)
| Variables | BDI [Mean (SD)] | PSS [Mean (SD)] | Evans Hypo. [Mean (SD)] | |||||||||
| Rounds | First | Second | Third | Time dif. | First | Second | Third | Time dif. | First | Second | Third | Time dif. |
| Gender | ||||||||||||
| Male | 24.15 (3.67) | 23.45 (6.67) | 20.05 (4.02) | <0.001 | 28.05 (4.42) | 34.42 (3.47) | 27.15 (5.14) | <0.001 | 34.48 (4.03) | 42.34 (5.91) | 30.19 (7.01) | 0.069 |
| Female | 25.76 (5.36) | 29.76 (5.36) | 24.81 (5.02) | 34.44 (4.67) | 41.71 (5.91) | 32.70 (5.70) | 43.74 (5.61) | 62.13 (7.72) | 38.74 (4.76) | |||
| Group dif. | 0.059 | 0.03 | 0.001 |  | <0.001 | <0.001 | <0.001 |  | <0.001 | 0.068 | 0.104 |  |
| Age groups | ||||||||||||
| <30 | 23.45 (3.61) | 24.75 (2.91) | 23.14 (2.86) | <0.001 | 26.14 (3.48) | 32.31 (6.11) | 29.66 (4.62) | 0.853 | 35.31 (8.43) | 46.72 (8.03) | 33.41 (2.81) | 0.001 |
| 30–36 | 24.6 (4.66) | 25.6 (3.72) | 20.6 (4.66) | 34.71 (5.11) | 39.42 (7.31) | 27.28 (7.77) | 42.59 (8.12) | 57.41 (6.66) | 32.29 (7.40) | |||
| ≥36 | 26.70 (4.96) | 28.70 (4.01) | 22.70 (4.02) | 33.17 (7.42) | 43.05 (6.54) | 32.25 (6.31) | 42.03 (6.40) | 52.11 (4.65) | 37.30 (14.1) | |||
| Group dif. | 0.181 | 0.046 | 0.006 |  | 0.206 | 0.004 | 0.043 |  | 0.059 | 0.004 | 0.181 |  |
| Marital status | ||||||||||||
| Married | 26.51 (3.79) | 28.63 (4.09) | 24.93 (4.04) | 0.002 | 34.45 (4.45) | 36.01 (6.71) | 29.05 (3.66) | 0.002 | 43.75 (5.51) | 61.02 (5.16) | 47.11 (19.8) | 0.573 |
| Single | 23.41 (4.63) | 25.06 (4.13) | 19.86 (5.61) | 29.01 (4.99) | 42.14 (5.02) | 30.46 (5.51) | 34.77 (9.01) | 44.06 (9.11) | 49.04 (17.7) | |||
| Group dif. | 0.004 | <0.001 | <0.001 |  | 0.005 | <0.001 | 0.152 |  | <0.001 | <0.001 | 0.015 |  |
| Work at private section | ||||||||||||
| Yes | 22.04 (4.74) | 23.74 (3.78) | 20.94 (5.01) | 0.004 | 26.11 (3.78) | 32.41 (5.03) | 28.45 (5.33) | <0.001 | 42.33 (4.13) | 44.33 (4.32) | 33.14 (10.20) | <0.001 |
| No | 26.98 (4.04) | 29.11 (4.61) | 23.68 (4.33) | 38.14 (6.79) | 45.01 (4.13) | 31.05 (4.11) | 37.55 (8.05) | 61.02 (9.15) | 36.55 (8.96) | |||
| Group dif. | 0.006 | <0.001 | 0.004 |  | <0.001 | <0.001 | 0.061 |  | 0.012 | <0.001 | 0.069 |  |
| History of mental illness | ||||||||||||
| Yes | 25.11 (6.74) | 28.02 (4.33) | 23.60 (4.68) | 0.004 | 29.45 (5.70) | 34.02 (8.01) | 29.48 (6.32) | 0.006 | 41.03 (6.31) | 46.71 (2.65) | 45.11 (18.4) | 0.042 |
| No | 24.42 (3.25) | 25.84 (4.61) | 20.82 (3.19) | 33.55 (6.11) | 43.77 (7.41) | 30.41 (4.45) | 39.05 (5.03) | 58.34 (6.31) | 39.10 (8.71) | |||
| Group dif. | 0.147 | 0.015 | 0.004 |  | <0.001 | <0.001 | 0.239 |  | 0.227 | <0.001 | 0.003 |  |
| Socioeconomic status | ||||||||||||
| Low | 27.76 (5.18) | 32.03 (6.35) | 26.13 (4.03) | <0.001 | 32.41 (6.38) | 44.37 (6.19) | 34.41 (6.41) | 0.002 | 46.91 (6.72) | 61.60 (8.15) | 40.01 (7.62) | <0.001 |
| Middle | 24.84 (5.49) | 26.14 (4.14) | 23.19 (3.71) | 30.22 (5.10) | 38.12 (7.91) | 29.46 (6.61) | 37.60 (4.11) | 55.02 (7.13) | 31.69 (4.41) | |||
| High | 21.32 (5.33) | 22.42 (5.22) | 18.46 (4.11) | 30.40 (6.31) | 33.19 (6.08) | 25.71 (4.77) | 33.06 (6.57) | 41.32 (6.09) | 31.98 (7.65) | |||
| Group dif. | <0.001 | <0.001 | <0.001 |  | 0.412 | 0.019 | 0.004 |  | 0.218 | <0.001 | 0.218 |  |
BDI: Beck Depression Inventory, PSS: Perceived Stress Scale, Evans Hypo.: Evans Hypochondriac, FDS: Frontline Dental Staff, Group dif.: Group difference, SD: Standard deviation.
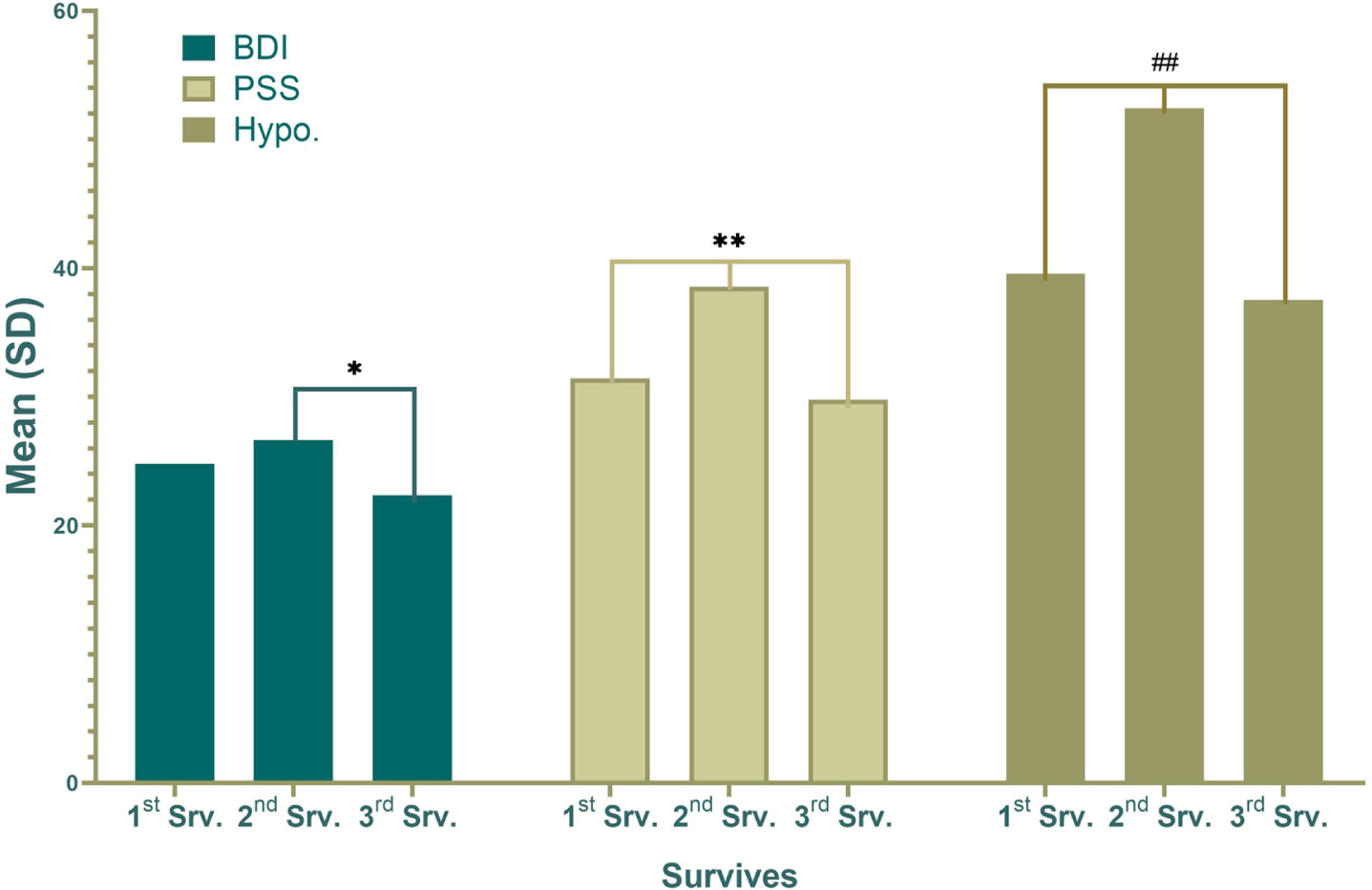
Figure 1 shows the total mean and standard deviation of depression, perceived stress, and hypochondria during three survives, where there were significant difference between survives and the mean and standard deviation of the variables increased dramatically at second survive (July 17 to October 21, 2021) and decreased at third survive (March 10 to April 8, 2022).
Fig. 1
The mean and standard deviation of depression based on the Beck Depression Inventory (BDI), stress level by the Perceived Stress Scale (PSS), and hypochondria by Evans Hypochondriac (Hypo.) during three round survives (first, second, and third). There was a significant difference in BDI mean between second and third survives (*: p < 0.05). In addition, there was significant difference in mean PSS (**:p < 0.001) and mean Hypo. (##:p < 0.001) between all three survives.
The results of multivariate regression regarding FDSs’ depression, perceived stress and hypochondria throughout the COVID-19 outbreak, are presented in Table 3. Being female was a predictor of higher levels of depression (t = 6.36, p < 0.001) and perceived stress (t = 4.51, p < 0.001). In addition, working in private section and being in higher socioeconomic level were predictors of lower level of depression and perceived stress. Perceived stress was a strong predictor of high-level depression (t = 7.79, p < 0.001). The consequences confirmed that a complete of 41.2% of the variance of FDSs’ depression (Adjusted R2 = 0.412), 34.6% of the variance of FDSs’ perceived stress (Adjusted R2 = 0.346), and 17.6% of the variance of FDSs’ hypochondria (Adjusted R2 = 0.176) may be defined through the variables entered with inside the model. Table 3 provides information about all variables included in the multiple linear regression models.
Table 3
Multiple linear regression estimates for depression, perceived stress, and hypochondria based on general characteristics during the COVID-19 outbreaks in FDS (n = 635)
| Explanatory variables | Depression | Perceived stress | Hypochondria | ||||||
| Coef. β | Contribution | Coef. β | Contribution | Coef. β | Contribution | ||||
| % 95 CI | P> |t| | % 95 CI | P> |t| | % 95 CI | P> |t| | ||||
| Gender | |||||||||
| Male (ref.) | – | – | – | – | – | – | – | – | – |
| Female | 6.36 | 2.02±8.69 | <0.001 | 4.51 | 1.74±6.55 | <0.001 | 1.97 | 0.88±6.40 | 0.232 |
| Age (year) | |||||||||
| 20–25 (ref.) | – | – | – | – | – | – | – | – | – |
| 26–30 | 0.82 | –1.74±1.70 | 0.978 | –0.94 | –2.78±0.88 | 0.310 | 3.70 | –2.67±10.08 | 0.253 |
| ≥31 | –1.46 | –5.14±2.20 | 0.432 | –1.84 | –5.55±1.86 | 0.328 | –1.05 | –14.6±12.5 | 0.879 |
| Marital status | |||||||||
| Single (ref.) | – | – | – | – | – | – | – | – | – |
| Married | 1.00 | –1.20±3.21 | 0.372 | 1.35 | –0.93±3.63 | 0.246 | –2.24 | –10.4±5.91 | 0.588 |
| Work in private section | |||||||||
| No (ref.) | – | – | – | – | – | – | – | – | – |
| Yes | –2.46 | –1.08±–2.83 | 0.005 | –3.54 | –1.73±–7.22 | <0.001 | 1.90 | 0.84±6.87 | 0.765 |
| History of mental illness | |||||||||
| No (ref.) | – | – | – | – | – | – | – | – | – |
| Yes | 1.42 | –2.61±4.02 | 0.622 | –0.86 | –4.30±2.58 | 0.622 | –5.29 | –17.5±6.95 | 0.395 |
| Socioeconomic status | |||||||||
| Low (ref.) | – | – | – | – | – | – | – | – | – |
| Middle | –0.60 | –2.84±1.62 | 0.593 | –0.44 | –2.73±1.85 | 0.704 | –4.27 | –12.5±3.97 | 0.308 |
| High | –3.97 | –1.28±7.24 | 0.004 | –4.35 | –2.66±–8.04 | 0.046 | 1.67 | –6.68±10.03 | 0.693 |
| Depression | |||||||||
| Score |  | 7.97 | 2.08±13.8 | <0.001 | 2.15 | 0.90±9.21 | 0.084 | ||
| Perceived stress | |||||||||
| Score | 7.97 | 2.08±13.8 | <0.001 |  | 1.92 | 0.81±6.15 | 0.468 | ||
| Hypochondria | |||||||||
| Score | 2.15 | 0.90±9.21 | 0.084 | 1.92 | 0.81±6.15 | 0.468 |  | ||
| Constant | 37.56 | <0.001 | 25.56 | <0.001 | 13.74 | 0476 | |||
| F | 5.86 | <0.001 | 3.79 | <0.001 | 3.05 | 0.006 | |||
| AR square | 0.412 | 0.346 | 0.176 | ||||||
4Discussion
In the COVID-19 pandemic crisis, the function of health care providers cannot be ignored. Health care providers such as medical, dental, pharmacy, and nursing are the frontline medical staff, who would possibly have close touch with the infected people during the COVID-19 pandemic [34, 35]. This survey, as a prospective cohort study, was the first study that examined the effect of COVID-19 pandemic on mental health issues among FDS in Iran from different perspective by evaluating depression, perceived stress, hypochondria, and their interaction during the different periods.
This study showed that during the COVID-19 outbreak in Iran about 69%, 83%, and 71% of FDS reported relative depression (21 < BDI < 30) during first, second, and third survives, respectively. In addition, 77%, 87%, and 64% of FDS reported moderate to high stress level (19 < PSS < 37) during first, second, and third survives, respectively. Finally, 60%, 76% and 74% of FDS reported moderate hypochondria during first, second, and third survives, respectively. A study by Ranka et al. in the UK declared that almost all the dentists in their survey were experiencing middle to high level of depression symptoms and stress during COVID-19 outbreak [36]. There are significant correlation between work-related stress and COVID-19 outbreak in dentists based on previous studies [36–38]. Zandian et al. in a cross-sectional study among Iranian nurses concluded that nurses suffered higher level of stress during COVID-19 outbreak and they need to proactive psychological support to prevent burnout and continue to provide nursing services [39]. Potas et al. found that psychological health, psychological effects of social isolation, and trait anxiety fully mediated the relationship between state anxiety and quality of life of nurses during COVID-19 [40].
COVID-19 related restrictions such as lockdowns are known to be the main factor of depression and stress among people. Al-Rawi et al. reported that stress, depression, and anxiety were prevalent during the pandemic among dentists because of COVID-19 restrictions [41]. Studies showed that COVID-19 pandemic has taken an additional psychological toll on the daily demands of dental professionals. The key is to strike a balance between the occupational health and well-being of dental providers while maintaining safe and paramount oral care for the public [4, 6].
In Iran, lockdowns were cancelled after the fifth peak of COVID-19, when the incidence of COVID-19 and its attributable mortality rate decreased significantly [42, 43]. Therefore, lockdown cancelation could be an important reason to decrease depression and other mental disorders related to COVID-19. In addition, increasing protective protocols because of COVID-19 such as social distance effect on population mental health status, where several studies detected this positive correlation [44–46].
Based on the results, at first, depression was increased during the COVID-19 outbreak and dramatically was decreased after the subsidence of COVID-19 in Iran (after cancellation of COVID-19 restrictions). Feter et al. showed that depressive symptoms among Brazilian adults increased significantly after the COVID-19 outbreak and implementation of social distancing restrictions [47]. A study by Liu et al. in China showed that depression symptoms among medical staff were increased significantly during COVID-19 [48], which is in line with results of this study. The level of depression reported by FDS in this study was lower than physicians [49] and nurses staff [50] based on the BDI. One of notable reason could be the lower level of stress among dentists in compare with physicians and nurses staff. Several studies showed that medical staff who perceived a higher level of stress such as nurses tend to develop more anxiety and depression symptoms [48, 51].
Depression, stress and hypochondria were prevalent among female and participants aged≥36 years old based on this study results. In a study conducted on Brazilian dentists, female gender and young age were shown to be associated factors with high level of depression, anxiety, and stress [52]. Single participants and privet sector workers had lower level of depression and stress. Al-Rawi et al. [41] detected being satisfied with the job and working in the private section as protective variables for depression and stress among dentists, which is in line with our findings. Mekhemar et al. stated that being unmarried and having no infant responsibilities was related to more healthy intellectual results than being wed, dating or elevating children [22]. Based on this study results, there were no differences between men and women in terms of depression, perceived stress, and hypochondria. A study conducted by Fink et al. also found that the prevalence of hypochondria was equal among men and women [53]. Hakami et al. reported that the woman college students had been statistically drastically extra depressed, anxious, and confused than the male college students [24]. In general, it can be concluded that all people experience a minimum level of stress and anxiety caused by COVID-19, because of fear of infection, its complications and unclear outcome due to infection. Most people did not have enough information about COVID-19 due to unclear approve information about it, which has caused an increase in anxiety, depression, and stress in different groups in society [52].
Based on the results, FDS with higher socioeconomic status had lower level of depression and stress. Bello et al. concluded from their systematic review and meta-analysis study that low socioeconomic level groups during the COVID-19 pandemic suffered higher level of depression and stress [54]. Reme et al. showed that depression, stress, and hypochondria were particularly high among women and those with lower levels of socioeconomic status during the COVID-19 outbreak [55]. Silva et al. showed that being female, having a high socioeconomic status, not working during social distancing, and having access to online modules were indirectly associated with mental health through psychosocial factors [56].
However, there is still a gap in the field of psychological and behavioural effects of COVID-19 on the performance of health system employees, especially dentists in term of efficiency, job satisfaction, financial performance, and its impact on their economic and social level, which should be investigated in different studies. In addition, the impact of COVID-19 on the performance of the health system from the perspective of health service utilization and its effect on population mental health should also be investigated at two individual and organizational levels in future studies.
4.1Limitations and recommendation
The study is not without limitations. First, there is strong evidence which confirmed that almost everyone is affected mentally by the COVID-19 outbreak and dental staff are not an exception. In addition, we used non-probability sampling method instead of a random sampling method due to the limitation during the COVID-19 pandemic. Online survey should also be considered as another limitation of this study because of limited access to online platform for some participants during COVID-19. Therefore, extrapolation of the results should be cautious. Finally, all the diagnoses in this study were mental health states, not mental disorders.
5Conclusion
This study offered a holistic view on FDS mental health status in different period of the COVID-19 pandemic by using strong methods and tools. Based on the study results, self-reported rates of depression, perceived stress and hypochondria were high among FDS. Being female, working in public sections, and lower socioeconomic level associated significantly with higher level of depression and perceived stress among FDS. Based on this, it can be concluded that in pandemics such as COVID-19, psychological support should also be provided to the treatment staff to increase the effectiveness and decrease their work burnout.
Ethics statement
All participants read and signed the informed consent form before begin included in the study. The formal research ethics committee approved the study (reference number IR.ARUMS.REC.1399.455), after which the study was implemented in the dental teaching clinic of ARUMS.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgments
This study was part of a dental student’s dissertation at the School of Dentistry. The authors would like to thank the managers and staff of the central office for helping them conduct this study.
Funding
This project was not financially supported by any organization or institute.
References
[1] | Fiorillo A , Gorwood P . The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) ;63(1). |
[2] | Banakar M , Lankarani KB , Jafarpour D , Moayedi S , Banakar MH , MohammadSadeghi A . COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Health. (2020) ;20: (1):1–12. |
[3] | Yazdi-Feyzabadi V , Alipouri Sakha M , Zandian H , Zahirian Moghadam T . Alcohol-related mortality during the COVID-19 outbreak in Iran: a commentary on happening a crisis amid another crisis. Journal of Substance Use. (2022) ;27: (4):435–9. |
[4] | Banaee S , Claiborne DM , Akpinar-Elci M . Occupational health practices among dental care professionals before and during the COVID-19 pandemic. Work. (2021) ;68: :993–1000. |
[5] | Mohsin SF , Shah SA , Agwan MAS , Ali S , Alsuwaydani ZA , AlSuwaydani SA . Effect of the COVID-19 pandemic on dental interns in Saudi Arabia. Work. (2022) ;71: :825–31. |
[6] | Bizzoca ME , Campisi G , Lo Muzio L . Covid-19 pandemic: What changes for dentists and oral medicine experts? A narrative review and novel approaches to infection containment. International Journal of Environmental Research and Public Health. (2020) ;17: (11):3793. |
[7] | Mariam Q , Ahmed N , Abbasi MS , Nadeem R , Rizwan A , Vohra F , et al. Safe practices of biomedical and dental waste management amongst practicing dental professionals amid the COVID-19 pandemic. Work. (2022) ;71: :851–8. |
[8] | Coulthard P . The oral surgery response to coronavirus disease (COVID-19). Keep Calm and Carry On? Oral Surg. (2020) . |
[9] | OSHA. Worker Exposure Risk to COVID-19. Retrieved from: https://www.osha.gov/Publications/OSHA3993.pdf. (2020) . |
[10] | Consolo U , Bellini P , Bencivenni D , Iani C , Checchi V . Epidemiological aspects and psychological reactions to COVID-19 of dental practitioners in the Northern Italy Districts of Modena and Reggio Emilia. International Journal of Environmental Research and Public Health. (2020) ;17: (10):3459. |
[11] | Ahmed MA , Jouhar R , Ahmed N , Adnan S , Aftab M , Zafar MS , et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. International Journal of Environmental Research and Public Health. (2020) ;17: (8):2821. |
[12] | Meng L , Hua F , Bian Z . Coronavirus disease (COVID-19): emerging and future challenges for dental and oral medicine. Journal of Dental Research. (2020) ;99: (5):481–7. |
[13] | Aghazadeh-Attari J , Mohebbi I , Mansorian B , Ahmadzadeh J , Mirza-Aghazadeh-Attari M , Mobaraki K , et al. Epidemiological factors and worldwide pattern of Middle East respiratory syndrome coronavirus from 2013 to 2016. Int J Gen Med. (2018) ;11: :121. |
[14] | Bohlken J , Schömig F , Lemke MR , Pumberger M , Riedel-Heller SG . COVID-19 pandemic: stress experience of healthcare workers-a short current review. Psychiatr Prax. (2020) ;47: (4):190–7. |
[15] | Kang L , Li Y , Hu S , Chen M , Yang C , Yang BX , et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. (2020) . |
[16] | Kushal A , Gupta S , Metha M , Singh M . Study of stress among health care professionals: A systemic review. Int J Res Foundation Hosp Healthcare Adm. (2018) ;6: :6–11. |
[17] | Ahorsu DK , Lin C-Y , Imani V , Saffari M , Griffiths MD , Pakpour AH . The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction. (2020) :1–9. |
[18] | Lee SA , Jobe MC , Mathis AA . Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol Med. (2021) ;51: (8):1403–4. |
[19] | Das G , Ahmed S , Ahmed AR , Tirth V , Jamil S , Muhammad AA , et al. A study on the severity and prevention measures of COVID-19 among dental professionals in clinical practice management. Work. (2021) ;70: :387–93. |
[20] | Alberts NM , Hadjistavropoulos HD , Jones SL , Sharpe D . The Short Health Anxiety Inventory: A systematic review and meta-analysis. J Anxiety Disord. (2013) ;27: (1):68–78. |
[21] | Wheaton MG , Abramowitz JS , Berman NC , Fabricant LE , Olatunji BO . Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit Ther Res. (2012) ;36: (3):210–8. |
[22] | Mekhemar M , Attia S , Dörfer C , Conrad J . Dental Students in Germany throughout the COVID-19 Pandemic: A Psychological Assessment and Cross-Sectional Survey. Biology. (2021) ;10: (7):611. |
[23] | Zhao S , Cao J , Sun R , Zhang L , Liu B . Analysis of anxiety-related factors amongst frontline dental staff during the COVID-19 pandemic in Yichang, China. BMC Oral Health. (2020) ;20: (1):342. |
[24] | Hakami Z , Khanagar SB , Vishwanathaiah S , Hakami A , Bokhari AM , Jabali AH , et al. Psychological impact of the coronavirus disease 2019 (COVID-19) pandemic on dental students: a nationwide study. Journal of Dental Education. (2021) ;85: (4):494–503. |
[25] | Nakhostin-Ansari A , Sherafati A , Aghajani F , Khonji MS , Aghajani R , Shahmansouri N . Depression and anxiety among Iranian Medical Students during COVID-19 pandemic. Iranian Journal of Psychiatry. (2020) ;15: (3):228. |
[26] | Sharma A , Chhabra KG , Bhandari SS , Poddar G , Dany SS , Chhabra C , et al. Emotional well-being of dentists and the effect of lockdown during the COVID-19 pandemic: A nationwide study. J Educ Health Promot. (2021) ;10: :344. |
[27] | Raeisi A , Tabrizi JS , Gouya MM . IR of Iran National Mobilization against COVID-19 Epidemic. Arch Iran Med. (2020) ;23: (4):216–9. |
[28] | Khani H , Ghodsi H , Nezhadnik H , Teymouri S , Ghodsi A . Depression and its relationship with hypochondriasis in nurses in Neyshabur, Iran. (2016) . |
[29] | Reis RS , Hino A , Añez C . Perceived stress scale. J health Psychol. (2010) ;15: :107–14. |
[30] | Hasan Zadeh LifShagard M , Tarkhan M , Taghi Zadeh ME . Effectiveness of stress inoculation training on perceived stress in pregnant women with infertility. Journal of Holistic Nursing And Midwifery. (2013) ;23: (2):27–34. |
[31] | Shafaie FS , Mirghafourvand M , Rahimi M . Perceived stress and its social-individual predicors among infertile couples referring to infertility center of Alzahra hospital in Tabriz in 2013. International Journal of Women’s Health and Reproduction Sciences. (2014) ;2: (5):291–6. |
[32] | Evans C . Understanding yourself: Signet Book; (1980) . |
[33] | Khani H , Ghodsi H , Nezhadnik H , Teymori S , Ghodsi AR . Depression and its relationship with hypochondriasis in nurses in Neyshabur, Iran. Military Caring Sciences Journal. (2016) ;3: (1):34–40. |
[34] | Mackay IM , Arden KE . MERS coronavirus: diagnostics, epidemiology and transmission. Virol J. (2015) ;12: (1):1–21. |
[35] | Raeissi P , Zandian H , Mirzarahimy T , Delavari S , Moghadam TZ , Rahimi G . Relationship between communication skills and emotional intelligence among nurses. Nursing Management. (2022) ;29(4). |
[36] | Ranka MS , Ranka SR . Survey of Mental Health of Dentists in the COVID-19 Pandemic in the UK. Journal of International Society of Preventive & Community Dentistry. (2021) ;11: (1):104. |
[37] | Toon M , Collin V , Whitehead P , Reynolds L . An analysis of stress and burnout in UK general dental practitioners: subdimensions and causes. British Dental Journal. (2019) ;226: (2):125–30. |
[38] | Hekmatfar S , Piraneh H , Jafari K . Evaluation of the relationship between pH and titrable acidity of five different of iron supplements with the absorption of iron ions in the anterior primary teeth (an in vitro study). Dent Res J (Isfahan). (2018) ;15: (5):367–71. |
[39] | Zandian H , Alipouri Sakha M , Nasiri E , Zahirian Moghadam T . Nursing work intention, stress, and professionalism in response to the COVID-19 outbreak in Iran: A cross-sectional study. Work. (2021) ;68: :969–79. |
[40] | Potas N , Koçtürk N , Toygar SA . Anxiety effects on quality of life during the COVID-19 outbreak: A parallel-serial mediation model among nurses in Turkey. Work. (2021) ;69: :37–45. |
[41] | Al-Rawi NH , Uthman AT , Saeed M , Abdulkareem AA , Al Bayati S , Al Nuaimi A . Depression, Anxiety and Stress Among Dentists During COVID-19 Lockdown. The Open Dentistry Journal. (2022) ;16(1). |
[42] | Syed Zafar M . Lockdown ineffective as fifth COVID-19 wave peaks in Iran. (2021) . |
[43] | Gharebaghi R , Heidary F , Pourezzat AA . COVID-19 Resurgence in Iran, Lessons Learned. Lessons Learned (May 19, 2022). (2022) . |
[44] | Zandian H , Sarailoo M , Dargahi S , Gholizadeh H , Dargahi A , Vosoughi M . Evaluation of knowledge and health behavior of University of Medical Sciences students about the prevention of COVID-19. Work. (2021) ;68: :543–9. |
[45] | Sarsak HI . Psychological impact of the COVID-19 pandemic on medical and rehabilitation sciences university students in Saudi Arabia. Work. (2022) ;71: :473–80. |
[46] | Nemati R , Moradi A , Marzban M , Farhadi A . The association between moral distress and mental health among nurses working at selected hospitals in Iran during the COVID-19 pandemic. Work. (2021) ;70: :1039–46. |
[47] | Feter N , Caputo E , Doring I , Leite J , Cassuriaga J , Reichert F , et al. Sharp increase in depression and anxiety among Brazilian adults during the COVID-19 pandemic: findings from the PAMPA cohort. Public Health. (2021) ;190: :101–7. |
[48] | Liu Y , Chen H , Zhang N , Wang X , Fan Q , Zhang Y , et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. Journal of Affective Disorders. (2021) ;278: :144–8. |
[49] | Kannampallil TG , Goss CW , Evanoff BA , Strickland JR , McAlister RP , Duncan J . Exposure to COVID-19 patients increases physician trainee stress and burnout. PloS One. (2020) ;15: (8):e0237301. |
[50] | Murat M , Köse S , Savaşer S . Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. International Journal of Mental Health Nursing. (2021) ;30: (2):533–43. |
[51] | Schneiderman N , Ironson G , Siegel SD . Stress and health: psychological, behavioral, and biological determinants. Annual Review of Clinical Psychology. (2005) ;1: :607. |
[52] | Alencar CdM , Silva AM , Jural LA , Magno MB , Campos EAD , Silva CM , et al. Factors associated with depression, anxiety and stress among dentists during the COVID-19 pandemic. Brazilian Oral Research. (2021) ;35. |
[53] | Fink P , Ørnbøl E , Toft T , Sparle KC , Frostholm L , Olesen F . A new, empirically established hypochondriasis diagnosis. Am J Psychiatry. (2004) ;161: (9):1680–91. |
[54] | Bello UM , Kannan P , Chutiyami M , Salihu D , Cheong AM , Miller T , et al. Prevalence of Anxiety and Depression Among the General Population in Africa During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Frontiers in Public Health. (2022) ;10. |
[55] | Reme B-A , Wörn J , Skirbekk V . Longitudinal evidence on the development of socioeconomic inequalities in mental health due to the COVID-19 pandemic in Norway. Scientific Reports. (2022) ;12: (1):1–8. |
[56] | Silva ANd , Guedes CR , Santos-Pinto CDB , Miranda ES , Ferreira LM , Vettore MV . Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. (2021) ;18: (14):7215. |




