Comparing the occurrence of chronic physical disorders in self-employed individuals with that of employees: A systematic review
Abstract
BACKGROUND:
A stringent systematic review of population-based observational studies focusing on the physical health of self-employed individuals as a basis for the development of targeted prevention strategies is lacking.
OBJECTIVE:
We aimed to systematically evaluate all the studies of good quality that compared the occurrence of chronic physical disorders in self-employed individuals with that of employees.
METHODS:
We searched three major medical databases (MEDLINE, Web of Science, Embase) following the Cochrane guidelines. The quality of the studies was rated based on the slightly modified validated assessment tool that was developed by Hoy et al.
RESULTS:
We included 16 population-based studies of good quality, with data from 15,369,964 participants in total. The two longitudinal evaluations of Swedish national registers with the longest follow-up periods showed increased cardiovascular mortality and incidence estimates of cardiovascular disease in self-employed individuals compared with those of white-collar (i.e., nonmanual) employees but decreased risk estimates compared with those of blue-collar (i.e., manual) workers. The results of the shorter cohort studies were heterogeneous. In cross-sectional studies, prevalence estimates for musculoskeletal, respiratory and malignant diseases were higher among self-employed individuals than among employees.
CONCLUSION:
The long-term cardiovascular disease risk and mortality of self-employed individuals seemed to be higher than those of white-collar employees but lower than those of blue-collar employees. As a basis for targeted prevention strategies, further longitudinal studies in different settings are required to better understand the development of physical health disorders for specific self-employment categories such as sole proprietors, small entrepreneurs, family businesses and others.
1Introduction
Globally, 47% of the workforce was self-employed in 2019, ranging from 6% in the United States to 75% or more in some African or Asian countries [1]. Provisions in occupational health and safety legislation, such as regular risk assessments and occupational health management, generally do not affect self-employed individuals [2]. However, the prevalence of self-employment and atypical types of employment are increasing worldwide in conjunction with rapid technological and social changes and increasing global competition, all of which require special attention from social policy and preventive medicine decision-makers [3]. Previous research has found associations between self-employment and elevated stress levels, as well as worse general mental health for self-employed workers compared with that of employees. A population-based study has shown a higher prevalence of mental disorders, especially depression, burnout and suicidal thoughts, among self-employed individuals in comparison with employed workers [4].
Apart from mental illness, self-employment may also be associated with physical disorders. In 2019, 17.9 million people died from the global leading cause of death, namely, cardiovascular disease (CVD) [5]. A recent study found a two- to threefold risk for CVD among self-employed individuals versus employees. Middle to large employers fared even worse in this respect than did leaders of small businesses [6]. Prevalence rates of osteoarthritis, headache and widespread chronic pain were higher among self-employed individuals than among employees in some studies [7–10], whereas the findings of a study on the prevalence of pain were similar between the two groups [11]. Although some studies have shown a better self-rated health [12] or higher well-being ratings [13] among self-employed individuals, it remains unclear whether the prevalence of physical disorders among self-employed individuals differs from that among employed workers [14–19].
Previous studies about the extent of physical health problems among self-employed individuals have been heterogeneous and partly contradictory [20, 21]. Moreover, recent research has not precisely defined the “informal sector” under study, nor has it examined the health of the formal workforce for comparison [22]. A stringent systematic review that critically appraises adequate observational studies as a basis for the development of targeted prevention strategies is still lacking. Due to the extension of informal work, especially during the COVID-19 pandemic, effective approaches are needed [23]. Therefore, the purpose of the present systematic evaluation was to identify all population-based studies worldwide that have compared the occurrence of physical health problems in self-employed sole proprietors and entrepreneurs of small businesses with that of employees, stringently evaluate the study quality and summarize the findings for specific physical diseases.
2Methods
The methods for the present systematic review have been described in detail previously [4]. In brief, we adhered to the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions version 6.0 [24] and the recommendations of the Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA) statement [25]. This study, as a literature review, is exempt from Institutional Review Board approval.
2.1Search strategy
We searched the MEDLINE, Web of Science and Embase databases up to March 2020 without restrictions regarding languages or year of publication. Through this open search strategy, we aimed to conduct a complete global overview to assess the health status of the self-employed, since there has been no previous systematic summary on this topic. The detailed search strings for the three databases, that have been published previously [4], are the following:
– For MEDLINE: “((“Small Business” [Mesh]) OR “self-employed”) Sort by: Best Match Filters: Humans“.
– Web of Science: “TS = “Small business *“ OR TS = “small enterprise *“ OR TS = “micro business *“ OR TS = “small and medium-sized enterprise*“ OR TS = “self-employed“ OR TS = “freelanc *“ OR TS = “independent *“ OR TS = “free agent *“ AND TS = Disease * OR TS = illness * OR TS = sickness * OR TS = “ill health“ OR TS = ailment * OR TS = malad * OR TS = disorder * OR TS = complaint * OR TS = “health problem*“ OR TS = strain OR TS = “health burden“ OR TS = Health * OR TS = “well-being“ OR TS = “physical constitution*“ OR TS = “psychological constitution *“ OR TS = “state of health“ OR TS = Presenteeism OR TS = absenteeism OR TS = truancy”.
– Embase: “(’small business *’ OR ’small enterprise *’ OR ‘micro business *’ OR ’small and medium-sized enterprise *’ OR ’self employed *’ OR ‘freelanc *’ OR ‘free agent *’) AND (disease * OR illness * OR sickness * OR ‘ill health’ OR ailment * OR malad * OR disorder * OR complaint * OR ‘health problem*’ OR strain * OR ‘health burden *’ OR health * OR ‘well being *’ OR ‘physical constitution *’ OR ‘psychological constitution *’ OR ’state of health’ OR presenteeism OR absenteeism OR ‘truancy’) AND [embase]/lim”.
On the 7th of April 2021, we updated our search in MEDLINE to identify new results regarding the incidence of chronic physical disorders in self-employed individuals compared with that in employees that were published during the 13 months after our initial search (no additional studies were identified).
We screened the online abstracts of conferences and all references of the included studies to complement the systematic search.
2.2Inclusion and exclusion criteria
There is no general definition of either self-employment or small enterprises. Therefore, we used a broad definition of “self-employment”; i.e., we included everyone who works on his or her own in a sole proprietorship or who is an entrepreneur of a small business with or without the employment of other persons. We did not define company size, but rather used the definitions of the authors of the included studies.
We included primary observational studies, such as systematic reviews with or without meta-analysis, as well as original articles and cross-sectional and cohort studies. Studies were considered that examined self-employment versus employment in relation to a physical illness or disorder. The physical health outcomes that we included were as follows: all-cause and disease-specific mortality, heart disease, stroke, hypertension, diabetes, fatigue, headache, eye strain, respiratory disease, asthma, somatic disease, gastrointestinal disease, pain, or any musculoskeletal disease.
We excluded intervention studies, qualitative studies, narrative reviews, case reports and series, book chapters, editorials and letters. Additionally, studies that used convenience samples or those that examined mental conditions only were excluded. Since we wanted to focus on physical illnesses and disorders rather than unhealthy lifestyle behaviors, we excluded studies that examined smoking, alcohol or drug consumption, as well as unhealthy eating habits. Furthermore, we excluded studies that did not include or present results for employed workers as a comparison group. Studies that were rated as having a low or moderate methodological quality were also excluded from the present review.
2.3Assessment of studies
The first author (KW) performed the screening of the titles and abstracts found, while taking into account the inclusion and exclusion criteria. During this process, duplicates and studies that were not available via the German library network “Subito” were excluded.
External native-level speaking scientists or professional translators translated non-English and non-German full texts into English or German. Two authors (KW and PJ/KZ) independently performed the full-text screenings. In case of disagreement, a third author (TK) made a decision.
The first author (KW) performed the data extraction of all the included studies, and the extracted data were reviewed by the coauthors (PJ/KZ). In the event of very few discrepancies, a third author was consulted (TK). We extracted the following parameters: first author, publication data, country, study design, sample size, response rate, percentage of female participants, age of the study population, origin and main characteristics of the target group, occupational status, assessment tools and main results. The authors of the included studies were not contacted when data were missing.
2.4Quality assessment
The quality of the studies was evaluated independently by two authors (KW and PJ/KZ) using an assessment tool with high interrater agreement according to previous research [26, 27]. The slightly modified assessment tool by Hoy et al. includes nine items of potential study bias (Supplement), of which three items regard the external validity of the study (representation, sampling and random selection) and six items regard the internal validity (nonresponse bias, data collection, case definition, reliability/validity of tool, method of data collection, numerator(s) and denominator(s)).
The overall quality was scored from 0 (no risk of bias) to 9 (highest risk of bias) and divided into the following three categories: low risk (0–3 points), moderate risk (4–6) and high risk (7–9).
We slightly adjusted the tool for studies without prevalence data and did not assess the last question (“Were the numerator(s) and denominator(s) for the parameter of interest appropriate?”) in this case. We defined the classification of the study quality for these studies as follows: low risk (0-2), moderate risk (3-5) and high risk (6-8) (Supplement). The interrater agreement was 91%. In case of disagreement, a third author (TK) made a decision. Based on the underlying quality scores, we included only longitudinal and cross-sectional population-based studies with good quality; i.e., there was a low risk of bias in the present systematic review (Fig. 1).
Fig. 1
PRISMA flowchart showing the selection of studies on chronic physical disorders among the self-employed compared with that of employees [23].
![PRISMA flowchart showing the selection of studies on chronic physical disorders among the self-employed compared with that of employees [23].](https://content.iospress.com:443/media/wor/2023/75-4/wor-75-4-wor220145/wor-75-wor220145-g001.jpg)
3Results
3.1General study characteristics
The application of our search strategy resulted in the initial identification of 5,412 publications. We were able to include 16 primary studies (six longitudinal, ten cross-sectional), but no systematic review based on our inclusion and exclusion criteria was performed (Fig. 1). Among the excluded articles, six studies were not considered because of methodological quality concerns (Fig. 1 step eligibility; Tables S2 and S3). A quality assessment of the included studies with low concern of bias and thus good methodological quality is shown in detail in Table 1.
Table 1
Quality assessment by Hoy et al. of the included studies with good quality
| Risk of bias items | Quality assessment of the included studies | |||||||||||||||
| 1 = No (high risk of bias) | ||||||||||||||||
| 0 = Yes (low risk of bias) | ||||||||||||||||
| Toivanen 2018 [21] | Malki 2014 [33] | Tiikkaja 2008 [32] | Tüchsen 2003 [30] | Tüchsen 1992 [31] | Vagerö 1989 [29] | Cambois 2017 [35] | Hogan 2016 [28] | Lesage 2014 [38] | Ferré 2012 [36] | Stephan 2010 [20] | Holmberg 2004 [37] | Benavides 2000 [34] | Kim 2019 [41] | Park 2019 [39] | Lee 2015 [40] | |
| 1. The study‘s target population was a close representation of the national population. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2. The sampling frame was a true or close representation of the target population. | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3. A census was undertaken, OR, some form of random selection was used to select the sample. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| 4. Was the likelihood of non-response bias minimal (response rate≥75%)? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| 5. All data were collected directly from the subjects. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| 6. An acceptable case definition was used. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7. The study instrument had been shown to have reliability and validity. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 |
| 8. The same mode of data collection was used for all subjects. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9. Were the numerator(s) and denominator(s) for the parameter of interest appropriate? (* = not applicable) | * | * | 0 | 0 | * | * | 0 | 0 | 0 | 0 | 0 | * | 0 | 1 | 0 | * |
| Summary 0–3: low risk of bias for studies that reported prevalence estimates; 0–2: low risk of bias for studies that did not report prevalence estimates (assessed by question 9) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 3 | 1 | 1 | 2 | 3 | 0 | 2 |
The 16 studies included data from a total of 15,369,964 participants, ranging from 206 [28] to 4,776,118 [21] subjects per study. The identified studies were conducted in 8 countries from Europe [20, 21, 28– 38] and Asia [39–41] but not on other continents. All of the longitudinal and some of the cross-sectional studies were large-scale investigations using register data. The included studies were published between 1989 [29] and 2019 [39, 41]. The follow-up time of the longitudinal studies ranged from 2 years [30] to 23 years [33] (Tables 2 and 3).
Table 2
Basic characteristics and results of longitudinal observational studies of good quality on chronic physical disorders comparing self-employed individuals (s-empl) versus employees (empl)
| Author, publication year, reference | Study design, country, recruitment year | Baseline number, age, females | Follow-up length, last response | Source population | Physical health outcome definition | Results | ||
| EUROPE | ||||||||
| Toivanen 2018 [21] | Register cohort study, Sweden, 2003 | n = 4,776,118, mean 49.3 y (s-empl/sole), 49.6 y (s-empl/non-sole), 41.8 y (empl), 31% (s-empl/sole), 27% (s-empl/empl), 50% (empl) | 5 y, 100% | Swedish Work and Mortality Database, Total Population Registry, Cause of Death Registry, Hospital Discharge Registry | Hospitalization episodes for stroke or myocardial infarction: ICD-10 (I21, I61, I63, I64, G45, I60) | Stroke aIRR (95%-CI) | ||
| s-empl (without personnel): | 1.0 (1.0-1.1) | |||||||
| s-empl (with personnel): | 1.0 (1.0-1.1) | |||||||
| empl: | 1.0 (ref.-categ.) | |||||||
| Myocardial infarction aIRR (95%-CI) | ||||||||
| s-empl (without personnel): | 1.0 (0.9-1.1) | |||||||
| s-empl (with personnel): | 0.9 (0.8-0.9)* | |||||||
| empl | 1.0 (ref.-categ.) | |||||||
| Malki 2014 [33] | Register cohort study, Sweden, 1987 | n = 2,939,771, n.r., 48.4% | 23 y, 99% (census 1980), 98% (census 1990) | Total Population Registry, Cause of Death Registry | Incidence of stroke or myocardial infarction: ICD-9: 410 and 433-434, ICD-10: I21-22 and I63 | Myocardial infarction IR per 100,000 person-years (95%-CI) | ||
| s-empl: | 413 (405-421) | |||||||
| empl (high nonmanual): | 305 (302-309) | |||||||
| empl (low nonmanual): | 402 (395-409) | |||||||
| empl (high manual): | 433 (426-439) | |||||||
| empl (low manual): | 497 (492-503) | |||||||
| Ischemic stroke IR per 100,000 person-years (95%-CI) | ||||||||
| s-empl: | 225 (220-232) | |||||||
| empl (high nonmanual): | 173 (170-176) | |||||||
| empl (low nonmanual): | 215 (210-220) | |||||||
| empl (high manual): | 229 (224-234) | |||||||
| empl (low manual): | 252 (249-256) | |||||||
| Myocardial infarction IRR (95%-CI) 2010 data s-empl vs high | ||||||||
| nonmanual empl (ref.-categ.) | ||||||||
| male | 55-59 y: 1.4 (1.2-1.5) female | 55-59 y: 1.6 (1.2-2.2) | ||||||
| 60-64 y: 1.2 (1.1-1.3) | 60-64 y: 1.4 (1.2-1.7) | |||||||
| 65-69 y: 1.4 (1.3-1.5) | 65-69 y: 1.4 (1.2-1.8) | |||||||
| Ischemic stroke IRR (95%-CI) 2010 data s-empl vs high | ||||||||
| nonmanual empl (ref.-categ.) | ||||||||
| male | 55-59 y: 1.5 (1.2-1.7) female | 55-59 y: 1.4 (1.0-2.0) | ||||||
| 60-64 y: 1.2 (1.1-1.4) | 60-64 y: 1.3 (1.0-1.6) | |||||||
| 65-69 y: 1.3 (1.1-1.4) | 65-69 y: 1.3 (1.1-1.6) | |||||||
| Tiikkaja 2008 [32] | Register cohort study, Sweden, 1990 | n = 809,199, range 31-57 y, 0% | 12 y, 100% | Cause of Death Registry | Death from cardiovascular disease: ICD-9 (390-458), ICD-10 (I00-I99) | Myocardial infarction aHR (95%-CI) | ||
| s-empl: | 1.29 (1.1-1.5)* | |||||||
| empl (nonmanual): | 1.0 (ref.-categ.) | |||||||
| empl (manual): | 1.38 (1.2-1.6)* | |||||||
| Stroke aHR (95%-CI) | ||||||||
| s-empl: | 1.12 (0.8-1.5) | |||||||
| empl (nonmanual): | 1.0 (ref.-categ.) | |||||||
| empl (manual): | 1.53 (1.3-1.8)* | |||||||
| Tüchsen 2003 [30] | Register cohort study, Denmark, 1981 | n = 1,488,364, range 20-59 y, 0% | 2-5 y, 100% | National Patient Registry, Death Registry, Central Population Registry | Hospitalization for coxarthrosis: ICD-8 (713.00), ICD-10 (M16) | Coxarthrosis annual change rate / SHR (95%-CI) | ||
| s-empl: | -1.2 (-2.0- -0.4) / 140 (130-151) | |||||||
| empl (leading positions): | 1.7 (0.4-3.0) / 87 (80-95) | |||||||
| empl (not in leading positions): | 0.9 (-0.4-2.3) / 96 (87-106) | |||||||
| Tüchsen 1992 [31] | Register cohort study, Denmark, 1981 | n = 2,579,396, range 20-59 y, 49.8% | 4 y, n.r. | Central Population Registry, Heart Registry, National Inpatient Registry | Hospitalization for ischemic heart disease: ICD-9 (410-414) | Ischaemic heart disease SHR (95%-CI) s-empl vs empl | ||
| (skilled workers): | ||||||||
| Hotel/restaurant workers | ||||||||
| s-empl, female: | 225 (141-329) | |||||||
| s-empl, male: | 144 (119-175) | |||||||
| empl, male (mean SHR, all other groups): | 133 | |||||||
| empl, female (mean SHR, all other groups): | 131 | |||||||
| Agricultural occupations: | ||||||||
| s-empl, female | 455 (114-1818) | |||||||
| empl, female | n.r. | |||||||
| Hardware, radios, bicycles: | ||||||||
| s-empl, female | 319 (103-990) | |||||||
| empl, female | n.r. | |||||||
| Textile industry | ||||||||
| s-empl, male | 185 (103-335) | |||||||
| empl, male | n.r. | |||||||
| Hair dresser | ||||||||
| s-empl, male | 147 (108-201) | |||||||
| empl, male n.r. | ||||||||
| Bakers | ||||||||
| s-empl: | 132 (97-179) | |||||||
| empl (skilled): | 144 (99-210) | |||||||
| Vagerö 1989 [29] | Register cohort study, Sweden, 1961 | n = 2,654,369, range 20-65 y, 28.2% | 8 y, 100% | 1960 Census, Cause of Death Registry | Mortality from coronary heart disease or vascular disease: (ICD-7: 420, 330-34, 331, 420.1) | male | female | |
| All cause mortality SMR (95%-CI) | ||||||||
| s-empl: | 101 (100-102) | 105 (100-111) | ||||||
| empl (nonmanual): | 98 (97-100) | 93 (90-95) | ||||||
| empl (manual): | 100 (99-101) | 107 (104-109) | ||||||
| Coronary heart disease SMR (95%-CI) | ||||||||
| s-empl (all): | 102 (100-104) | 114 (100-129) | ||||||
| empl (nonmanual): | 109 (107-112) | 84 (78-91) | ||||||
| empl (manual): | 95 (94-97) | 110 (101-117) | ||||||
| s-empl (agricultural): | 87 (84-90) | 91 (73-112) | ||||||
| empl (agricultural): | 90 (85-95) | 75 (47-113) | ||||||
| Myocardial infarction SMR (95%-CI) | ||||||||
| s-empl (all): | 102 (99-101) | 115 (99-133) | ||||||
| empl (nonmanual): | 113 (109-116) | 87 (80-95) | ||||||
| empl (manual): | 94 (93-96) | 107 (100-115) | ||||||
| s-empl (agricultural): | 87 (84-91) | 90 (70-114) | ||||||
| empl (agricultural): | 91 (86-97) | 75 (44-120) | ||||||
| Cerebro-vascular disease SMR (95%-CI) | ||||||||
| s-empl (all): | 103 (100-109) | 113 (97-131) | ||||||
| empl (nonmanual): | 102 (96-107) | 89 (82-97) | ||||||
| empl (manual): | 97 (94-100) | 107 (100-115) | ||||||
| s-empl (agricultural): | 96 (90-102) | 107 (85-133) | ||||||
| empl (agricultural): | 88 (79-98) | 107 (69-158) | ||||||
| Cerebral haemorrhage SMR (95%-CI) | ||||||||
| s-empl (all): | 107 (101-113) | 105 (85-129) | ||||||
| empl (nonmanual): | 101 (94- 109) | 89 (79-99) | ||||||
| empl (manual): | 96 (91-100) | 109 (99-119) | ||||||
| s-empl (agricultural): | 98 (90-107) | 110 (81-146) | ||||||
| empl (agricultural): | 77 (66-90) | 116 (65-191) | ||||||
| Other causes of death except cardio-vascular | ||||||||
| diseases SMR (95%-CI) | ||||||||
| s-empl (all): | 100 (99-102) | 103 (97-109) | ||||||
| empl (nonmanual): | 94 (92-96) | 94 (92-96) | ||||||
| empl (manual): | 102 (101-104) | 106 (104-109) | ||||||
| s-empl (agricultural): | 95 (90-100) | 96 (88-105) | ||||||
| empl (agricultural): | 101 (98-105) | 97 (83-112) | ||||||
vs = versus, n.r. = not reported, y = years, *p≤0.05, (a)OR = (adjusted) odds ratio, CI = confidence interval, ref. = reference, IR(R) = incidence rate (ratio), SMR = standardized mortality ratio, (a)SHR = (adjusted) standardized hospitalization ratio, aHR = adjusted hazard ratios.
Table 3
Basic characteristics and results of cross-sectional studies of good quality on chronic physical disorders comparing self-employed individuals (s-empl) versus employees (empl)
| Author, publication year, reference | Country, sample size, female | Age [Mean(SD) or range] | Source population | Physical health outcome definition | Results | ||
| EUROPE | |||||||
| Cambois 2017 [35] | France, n = 7,537, 53.2% | 45-74 y | French Population Survey 2006 | Physical limitations: new questionnaire developed for the study | Physical functional limitations | male | female |
| s-empl vs empl (skilled workers, ref.-categ.): | OR 1.72 vs 1.0* | OR 1.71 vs 1.0* | |||||
| Past change from s-empl to empl vs employees | |||||||
| (past upward career direction, ref.-categ.): | OR 1.52 vs 1.0 | OR 0.72 vs 1.0 | |||||
| Past change from empl to s-empl vs employees | |||||||
| (past upward career direction, ref.-categ.): | OR 1.04 vs 1.0 | OR 0.99 vs 1.0 | |||||
| Hogan 2016 [28] | Ireland, chartered: n = 206, 77%, athletic: n = 141, 53%, SLÁN 2007: n = 5,862, 51% | n.r. | Random sample of members of the Institute of Physical Therapy and Applied Science, Irish Association of Physical Therapists, Athletic Rehabilitation Therapy Certified Organisation | Low back pain: HITS questionnaire, yes-/no-question | s-empl therapists vs empl therapists (ref.-categ.) % (95%-CI) | ||
| Low back pain | |||||||
| Chartered physiotherapists: | 49% (39-59) vs 47% (39-59) | ||||||
| Physical and athletic therapists: | 48% (37-59) vs 46% (27-65) | ||||||
| All therapists: | 49% (41-56) vs 48% (39-57) | ||||||
| OR 1.0 (0.6-1.7) vs 1.0 | |||||||
| SLÁN: | 18% (16-20) vs 16% (15-17) | ||||||
| OR 1.1(0.9-1.3) vs 1.0 | |||||||
| Lesage 2014 [38] | France, n = 367, 0% | 47.1(8.1) y (s-empl), 39.9(10.7) y (empl) | All self-employed joiners in Champagne Ardenne, employees from 3 joineries, 1 plywood production plant, truckers | 1. Musculoskeletal function: medical examination 2. Lung function: spirometry | s-empl joiners vs empl joiners (ref.-categ.): | ||
| Dyspnea | 15.8% vs 7.7%, | aOR 2.46 vs 1.0* | |||||
| Restrictive syndrome | 4.7% vs 2.1%, | aOR 2.51 vs 1.0 | |||||
| Obstructive syndrome | 5.3% vs 1.6%, | aOR 3.56 vs 1.0 | |||||
| Mixed syndrome | 5.9% vs 7.8%, | aOR 0.77 vs 1.0 | |||||
| Musculoskeletal diseases | 63.2% vs 30.6%, | aOR 3.09 vs 1.0* | |||||
| Upper limb diseases | 24.1% vs 22.4%, | aOR 1.41 vs 1.0 | |||||
| Lower limb diseases | 29.3% vs 12.1%, | aOR 3.03 vs 1.0* | |||||
| Back diseases | 15.4% vs 4.3%, | aOR 3.03 vs 1.0* | |||||
| Ferré 2012 [36] | France, n = 9,050, 52.1% | >45 y | Fifth French health interview survey | Chronic bronchitis: interviews, new questionnaire developed for the study (chronic cough and dyspnea) | Chronic bronchitis % (95%-CI) | ||
| s-empl: 5.2% | OR 1.8 (1.1-3.1)* | ||||||
| empl (nonmanual): 2.2% | OR 1.0 | ||||||
| empl (manual): 5.6% | OR 1.8 (1.1-2.8) | ||||||
| Stephan 2010 [20] | Germany, n = 298, 26.5% | 46.2(8.7) y | Matched case-control design with participants from German National Health Survey 1998 | Blood pressure, somatic diseases: ICD-10 | s-empl vs empl (ref.-categ.) %, OR (95%-CI) | ||
| Hypertension: | 19% vs 34% | OR 0.47 (0.25–0.88) vs 1.0* | |||||
| Somatic morbidity: | 68% vs 77% | OR 0.41 (0.22–0.77) vs 1.0* | |||||
| Gastrointestinal ulcers: | 10% vs 5% | OR 2.07 (0.69–6.27) vs 1.0 | |||||
| Diabetes: | 3% vs 3% | OR 1.07 (0.22–5.23) vs 1.0 | |||||
| Rheumatoid arthritis: | 17% vs 16% | OR 1.02 (0.50–2.11) vs 1.0 | |||||
| Lower back pain: | 82% vs 81% | OR 0.91 (0.58–1.41) vs 1.0 | |||||
| Shoulder/neck pain: | 63% vs 64% | OR 0.90 (0.58–1.41) vs 1.0 | |||||
| Holmerg 2004 [37] | Sweden, n = 1,221, 0% | 50.3 y | Random sample of the National Farm Registry, National Population Registry | Low back pain: new questionnaire developed for the study | Low back | s-empl (farmers) vs s-empl (no farm) vs empl (no farm, ref.-categ.) | |
| aOR (95%-CI) | |||||||
| - pain: | 1.37 (0.95–1.98) vs 0.68 (0.38–1.24) vs 1.0 | ||||||
| - consultation: | 1.14 (0.80–1.63) vs 0.70 (0.38–1.29) vs 1.0 | ||||||
| - sick leave: | 0.76 (0.52–1.11) vs 0.64 (0.34–1.23) vs 1.0 | ||||||
| Benavides 2000 [34] | Spain, n = 15,146, n.r. | >15 y | Multi-stage random sample of the working population of 15 EU-countries (1000 cases per country) | Fatigue, backache, muscular pain: new questionnaire developed for the study | s-empl (without personnel) vs s-empl (with personnel) vs empl (full time permanent, ref.) | ||
| Fatigue OR (95%-CI): | 1.67 (1.47-1.89)* vs 1.55 (1.32-1.81)* vs 1.0 | ||||||
| 26.1% vs 25.8% vs 17.7% | |||||||
| Backache: | 34.6% vs 31.1% vs 28.7%* | ||||||
| Muscular pain: | 26.1% vs 19.4% vs 16.9%* | ||||||
| ASIA | |||||||
| Kim 2019 [41] | Korea, n = 32,630, 40.5% | 20-59 y | Third Korean Working Conditions Survey (KWCS, 2011) | Backache, muscular pain, headaches, fatigue: WHO-5 well-being index | s-empl (with personnel) vs empl (ref.-categ.) | ||
| %, aOR (95%-CI) | |||||||
| Headaches/eyestrain: | 14.7% vs 15.6% | aOR 1.05 (0.97-1.13) vs 1.0 | |||||
| Overall fatigue: | 25.6% vs 20.8% | aOR 1.02 (0.96-1.09) vs 1.0 | |||||
| Backache: | 12.8% vs 8.8% | aOR 1.16 (1.06-1.26) vs 1.0* | |||||
| Muscular pain upper limbs: | 34.9% vs 26.9% | aOR 1.19 (1.12-1.27) vs 1.0* | |||||
| Muscular pain lower limbs: | 23.7% vs 16.5% | aOR 1.14 (1.07-1.22) vs 1.0* | |||||
| Park 2019 [39] | Korea, n = 44,266, 48.1% | n.r. | 4th Korean Working Conditions Survey (KWCS, 2014) | 2. Pain: yes-/no-question | s-empl vs empl (nonmanual with cognitive | ||
| demands/service and sales/manual) | |||||||
| Back pain: | |||||||
| male | 9.5%*/11.1%*/28.1%* vs 5.9%/6.4%/15.3% | ||||||
| female | 8.6%/7.0%*/39.6%* vs 8.3%/14.2%/21.2% | ||||||
| Upper extremity pain: | |||||||
| male | 24.7%*/29.3%*51.6%* vs 16.6%/17.9%/36.4% | ||||||
| female | 21.6%/40.0%*/65.0%* vs 21.8%/32.5%/43.2% | ||||||
| Lower extremity pain: | |||||||
| male | 11.0%/20.4%*/43.9%* vs 7.6%/12.4%/25.1% | ||||||
| female | 11.2%/29.5%/61.3%* vs 11.1%/26.5%/32.3% | ||||||
| Lee 2015 [40] | Korea, n = 6,023, 46.8% | 25-65 y | Household Registries | Dry eye symptom: new questionnaire developed for the study | s-empl(ref.) vs empl aOR (95%-CI) | ||
| Dry eye syndrome: | 1.0 vs 1.22 (1.02–1.46)* | ||||||
vs = versus, n.r. = not reported, y = years, * p≤0.05, (a)OR = (adjusted) odds ratio, CI = confidence interval, ref.-categ. = reference category.
3.2Study population characteristics
The studies investigated a higher proportion of men than women and covered an age range from 15 [34] to 74 [35] years. The five largest studies were based on analyses of national register data from Sweden [21, 29, 33] and Denmark [30, 31], with over one million study participants in each evaluation. The survey populations included up to 44,000 participants [39]. Only three studies examined less than 1,000 subjects [20, 28, 38].
3.3Assessment of employment categories
Information about employment status was mostly collected by questionnaires or, in larger studies, by information pulled from register data. The included studies examined different groups and subgroups of both self-employed individuals and employees. Nevertheless, the majority of the studies included both self-employed individuals and employees without further subdivisions. Sole proprietors (i.e., those without personnel) and small business owners (e.g., <10 employees) were investigated separately by three studies [21, 34, 41]. Categories of employed persons that were investigated separately by four studies included nonmanual and manual workers [29, 32, 33, 36]. Two of the included studies examined only one occupational group, namely, therapists [28] and joiners [38] (Tables 2 and 3).
3.4Outcome measures
The included studies examined the following results using various assessment tools: all-cause mortality (one study), cardiovascular and noncardiovascular mortality (two studies), CVD (four studies), musculoskeletal diseases (nine studies), and nonmusculoskeletal physical diseases (six studies) (Tables 2–5).
3.4.1Mortality and incidence of physical disorders in longitudinal studies
We identified six longitudinal studies of good quality, namely, four from Sweden, and two from Denmark (Tables 2 and 4).
The largest study with over four million subjects and five years of follow-up was a nationwide Swedish register-based study. In this study, Toivanen et al. showed that the proportion of self-employed sole proprietors hospitalized for stroke or myocardial infarction was the same as that for employees. However, self-employed individuals with own personnel had a significantly lower incidence rate of hospital admissions for myocardial infarction and the same incidence rate for stroke compared with those of employees [21].
The two studies with a 23- and a 12-year follow-up of the Swedish Total Population Registry and the Swedish Cause of Death Registry, respectively, found higher incidence and mortality rates of CVD in self-employed individuals compared with those found in nonmanual workers. When compared with manual workers, self-employed individuals had considerably lower incidence rates of cardiovascular diseases and mortality [32, 33].
Based on a four-year follow-up of national Danish registry data, Tüchsen et al. (1992) found a considerable excess risk of being admitted to hospital due to ischemic heart disease for self-employed female hotel and restaurant workers aged 20–59 years. The corresponding risks for employed women and self-employed men, as well as for employed hotel and restaurant workers, were also increased but to a much smaller extent (not significant) than those for self-employed female hotel and restaurant workers (significant). Furthermore, self-employed individual males in the textile industry and self-employed male hairdressers, as well as self-employed women with agricultural occupations and self-employed women from sectors that include hardware, radios, and bicycles, had increased rates of ischemic heart disease risk. For these occupational groups, the authors did not publish comparable data for employees. Among bakers, their slight increased risk of ischemic heart disease was not considerably different between self-employed and employed individuals. Other occupational groups, e.g., drivers and fishermen, also showed a notably increased risk of ischemic heart disease among both self-employed and employed workers. The authors reported only the results that separately regarded significant differences between self-employed and employed individuals, but further occupational groups were not examined. Therefore, only the selected significant results are presented in Table 4 [31].
Table 4
Overview of physical health outcomes among self-employed individuals compared with that of employees in longitudinal studies
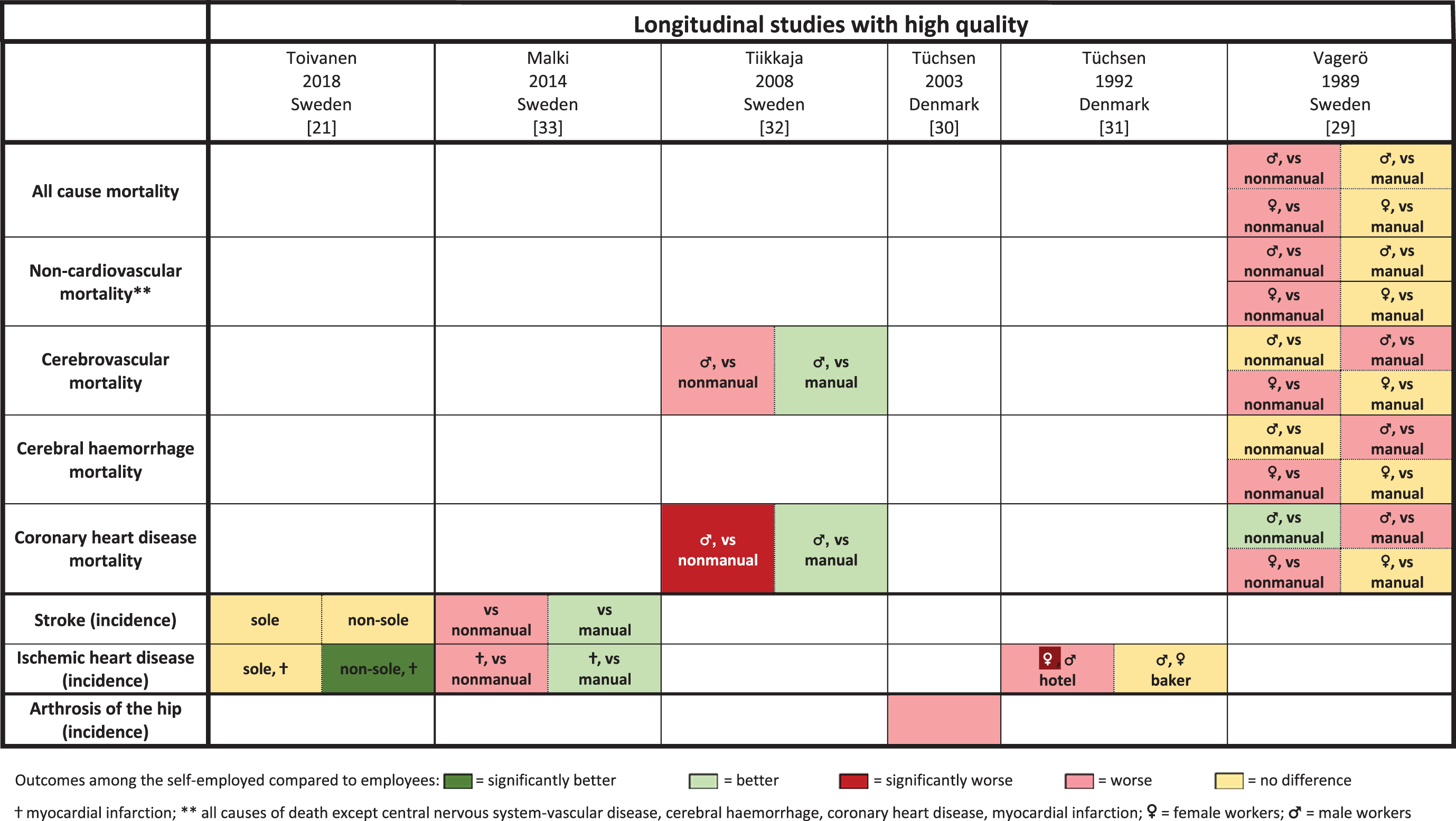 |
A nationwide Swedish register and census-based study from 1989 reported some inconsistent results for various groups of workers and diagnoses. In summary, the majority of the outcomes showed higher standardized mortality ratios for CVD parameters in self-employed individuals versus nonmanual workers, whereas in comparison with manual workers, the majority of the results showed no differences between the groups [29].
A more recent Danish register study investigated incidences of hospital admissions for arthrosis of the hip (coxarthrosis). Over a 5-year follow-up, self-employed individuals had a considerably (not significant) higher standardized hospitalization ratio compared with that of employees who were in leading positions or those who were not in leading positions [30] (Tables 2 and 4).
3.4.2Prevalence of physical disorders in cross-sectional studies
Most of the cross-sectional studies were from Europe (7 studies) [20, 28, 34–38], and only three were from Asia [39–41]. The majority of these studies (8 studies) showed significantly higher prevalence of physical illness, especially musculoskeletal diseases, among self-employed individuals compared with that among employees [20, 28, 34, 35, 37–39, 41] by investigating different occupation types and the use of varying assessment tools (Tables 3 and 5).
Table 5
Overview of physical health outcomes among self-employed individuals compared with that of employees in cross-sectional studies
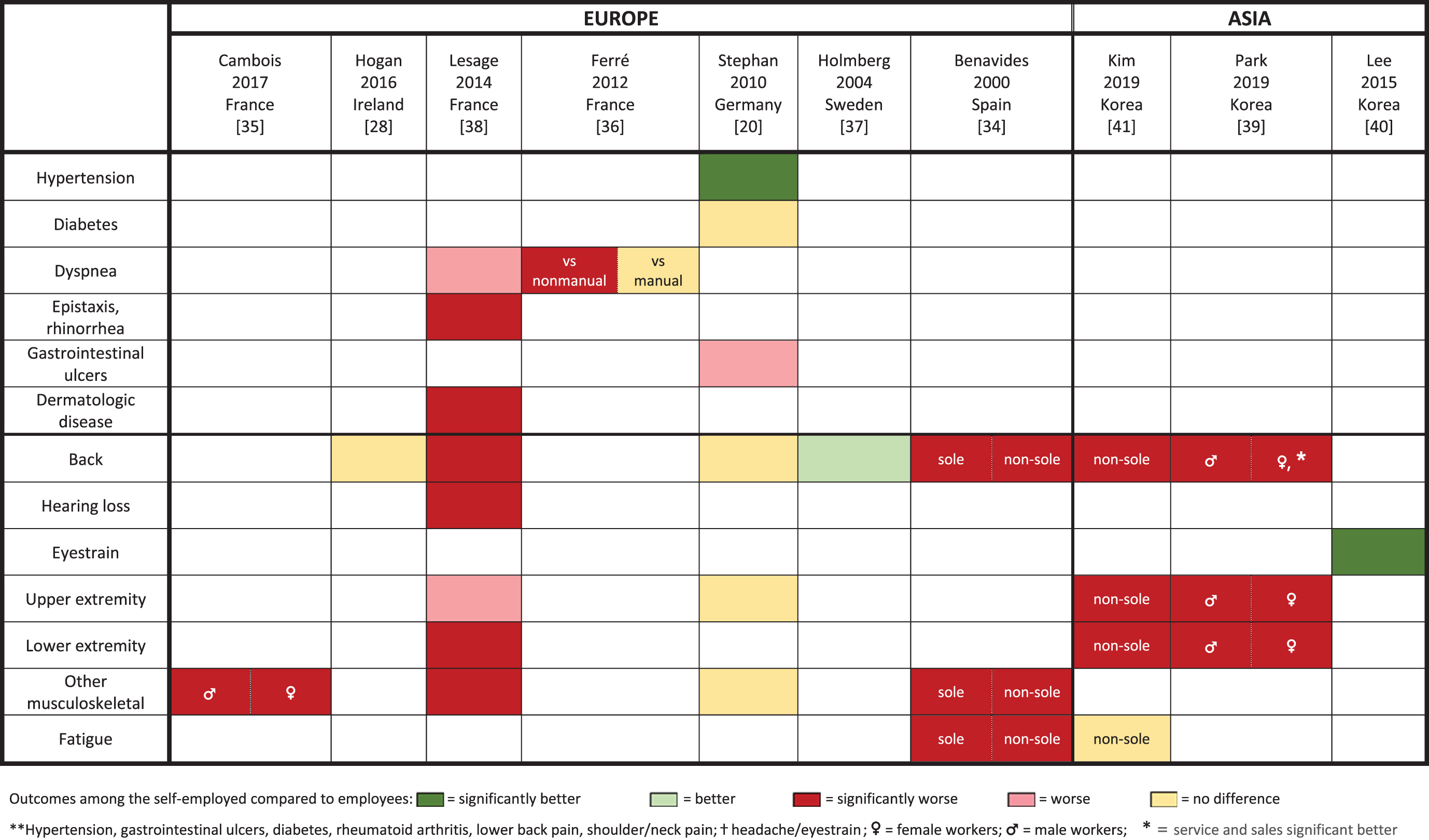 |
3.4.2.1. Nonmusculoskeletal disease. Only one cross-sectional study used the current International Statistical Classification of Diseases and Related Health Problems (ICD). Stephan et al. investigated a variety of aggregated physical disorders and showed lower risks of hypertension and any (i.e., at least one) of the following somatic diseases for self-employed individuals compared with those for employees: hypertension, gastrointestinal ulcers, diabetes, rheumatoid arthritis, lower back pain, or shoulder/neck pain. The risks were similar for diabetes, back pain, and upper and lower extremity pain. Higher risks for gastrointestinal ulcers were found in self-employed individuals than in occupation type-matched employed persons [20] (Tables 3 and 5).
Kim et al. reported no differences in the prevalence of headache and eye strain between self-employed individuals with personnel and employees [41], whereas Lee et al. found significantly more eye strain among all self-employed individuals combined than in employees [40] (Tables 3 and 5).
Two studies from France investigated respiratory outcomes: one measured lung function using spirometry, and the other assessed self-reported chronic bronchitis symptoms [36, 38]. Ferré et al. compared self-employed individuals with nonmanual workers and reported a higher prevalence of chronic bronchitis symptoms among self-employed workers, whereas the bronchitis prevalence of the latter showed no difference in comparison with that of manual workers [36]. Lesage et al. reported reduced lung function among self-employed joiners compared with that among their employed counterparts [38] (Tables 3 and 5).
Two studies applied questionnaires to assess fatigue [34, 41]. Benavides et al. used a nonvalidated questionnaire with a permanent employed reference group and showed a significantly higher prevalence of fatigue among self-employed individuals [34]. Kim et al. found no difference between self-employed individuals with their own personnel and employees of various occupations using a validated questionnaire [41] (Tables 3 and 5).
3.4.2.2. Musculoskeletal disease. The majority (5 studies) of the eight studies that investigated musculoskeletal disorders reported higher prevalences among self-employed individuals compared with those among employees. The same applies to male and female workers [9, 35, 39], except in the study by Park et al., who differentiated manual workers, service and sales workers, and nonmanual workers with cognitive demands. The authors found fewer musculoskeletal diseases among self-employed women than among employed female service and sales workers [39]. Two out of three studies that used occupation-matched references described similar prevalences of back pain among self-employed individuals compared with those among employees [20, 28, 38] (Tables 3 and 5).
Almost all of the studies that investigated mixed occupation groups reported a significantly higher risk of musculoskeletal disease among self-employed individuals compared with that among employees [34, 35, 39, 41]. In contrast, studies comparing self-employed and employed people in one specific occupational group showed inconsistent findings [20, 28, 37, 38]. Holmberg et al., who excluded farmers from two other groups reported even less lower back pain among self-employed nonfarmers than among nonfarming employees [37] (Tables 3 and 5).
4Discussion
4.1Main findings
Through a comprehensive literature search on the incidence and prevalence of physical illnesses among self-employed individuals versus employees, we were able to include 16 population-based studies of good quality (six longitudinal and ten cross-sectional) from Europe and Asia.
The present systematic review identified a lower incidence rate of CVD among self-employed individuals compared with that among manual workers, whereas a (partly significant) higher incidence rate was found in comparison to nonmanual workers. The largest included study reported no differences between sole proprietors and employed workers, while self-employed individuals with personnel showed significantly lower incidence rates of myocardial infarction in comparison to those among employees. The only longitudinal study that investigated arthrosis of the hip reported a higher but not statistically significant incidence rate in self-employed individuals versus employees.
Most of the cross-sectional studies (8 studies) that we included investigated musculoskeletal disorders. The majority (5 studies) of them showed a significantly higher prevalence rate for self-employed individuals compared with that for employees. The results of the few cross-sectional studies (4 studies) that examined nonmusculoskeletal diseases were less conclusive (Tables 2 to 5).
4.2Comparison of the studies
4.2.1Longitudinal studies
The results of the six longitudinal studies included in this review were partly inconsistent. Although all the studies were based on register data evaluating ICD diagnoses, there were some considerable differences in the study designs that may explain the varying outcomes.
The register study of Tiikkaja et al. in Sweden showed higher mortality rates for stroke and myocardial infarction among self-employed individuals compared with those among nonmanual workers and lower mortality rates compared with those among manual workers [32]. These results are in line with Rosén et al. who reported a 50–60% higher risk of death from myocardial infarction for manual workers than that for nonmanual workers in higher socioeconomic positions [42]. However, Vagerö et al. reported predominantly higher mortality rates regarding cardiovascular diseases in self-employed individuals compared with those for nonmanual workers, but hardly any differences in the mortality rates compared with those for manual workers [29]. Reasons for the different outcomes might be changes in working conditions, as well as lifestyle habits, e.g., smoking, over the long period between the studies (1961–68 and 1990–2002). Vagerö et al. mentioned high smoking rates in self-employed nonmanual workers at the time of their study [29], whereas manual workers were at higher risk for smoking at a later time [43, 44]. In contrast to nonmanual workers, who drastically decreased their overall smoking rate from 1978 to 1994, manual workers' smoking rate diminished in the beginning and remained stable after a few years [44]. These time-dependent behaviors may have influenced the results of the two studies that investigated cardiovascular mortality [45, 46]. Additionally, there might be a lack of comparability with respect to the data that were collected such a long time apart because of the changes made to work environments since then. Sweden enjoyed a booming economy in the second half of the 20th century [47], which slowed down in 1970 and ended in a crisis in the 1990 s [48]. These economic circumstances might have influenced the working conditions for self-employed individuals as well as for employees, and, consequently, may have affected the health of workers. Neither of the studies that investigated mortality examined nonmanual and manual self-employed workers separately; rather they compared all self-employed individuals combined with nonmanual and manual employees [29, 32]. The distribution of nonmanual and manual workers within self-employed individuals may cause disparities between the studies because a twofold risk of CVD mortality among manual workers has been previously reported [42].
Two recent nationwide register studies from Sweden investigated the incidences of stroke and myocardial infarction [21, 33]. The 5-year follow-up study of Toivanen et al. reported no differences in the stroke incidence rates between the groups in the fully adjusted model (adjusted for sex, age, country of origin, previous health status, education, family, enterprise size). One self-employed subgroup, namely, the limited liability company owners, showed even lower incidence rates than those of employees. Therefore, various other factors may influence the physical health status of workers. Toivanen et al. also reported large differences between industrial sectors regardless of occupational group. They stated that “the results highlight the importance of the industrial sector for hospitalization rates due to acute CVD among sole proprietors and limited liability company owners” [21]. A limitation of the study by Toivanen was the lack of data for the occupational group and industrial sector together. This may explain the similar outcomes found for sole proprietors and self-employed workers.
Similar to Tikkaja et al., the 23-year follow-up study of Malki et al. indicated more protective health effects regarding stroke and myocardial infarction for self-employed individuals when compared with those for manual workers, whereas self-employed individuals showed higher incidence rates in comparison with those of nonmanual workers. Additionally, the authors reported similar outcomes for low-level nonmanual, self-employed and high-level manual workers, whereas high-level nonmanual and low-level manual workers showed clear differences in the manner of lower and higher incidence rates than those of self-employed individuals [33]. Although the included register studies did not integrate questionnaires to explicitly assess lifestyle factors, it is well known that risk factors such as smoking, physical inactivity and socioeconomic inequalities are associated with cardiovascular morbidity [49]. Therefore, lower socioeconomic positions indicate worse health outcomes compared with those of higher statuses [21, 42]. According to the Eurofound and International Labour Organization (2019), the tasks of upper-level nonmanual workers, including higher responsibility or having to solve more unforeseen problems, may be responsible for their better health compared with the tasks of manual workers [50]. Manual workers often have a lower decision latitude and heavier physical work. As Karasek‘s demand-decision-model described, these reasons could lead to problems of strain and feelings of dissatisfaction and consequently result in poor general health [51]. Self-employed individuals enjoy entrepreneurial scope but may perceive more financial pressure and less long-term security [13].
A third national register study from Sweden examined occupations that seemed to be at high risk for ischemic heart disease based on the outcomes of previous studies [31]. The authors argued that some occupational groups have an increased risk of ischemic heart disease, whereas the differences between self-employed and employees in the same industrial sector were mostly not significant. These results might be due to misclassifications of occupations because the study assessed the most important occupation during only one year. Unknown migration from one occupational group to another might have put the results into perspective. Self-employed and employed bakers showed minor differences, whereas female self-employed hotel and restaurant workers showed a higher increased risk of ischemic heart diseases compared with that of employees and males self-employed in hotels and restaurants [31]. A reason for these contradictory outcomes may be the lack of adjustment for potential risk factors such as work-family conflicts or alcohol consumption and smoking. Self-employed workers in food service industries seem to exhibit greater levels of alcohol consumption compared with the employees in this sector [17]. Work-family conflicts, especially for women, are related to physical health problems [52]. In hotel and restaurant working conditions, there could be more work-family conflicts because of shift work, including late work hours. In contrast, bakers can join in family activities in the afternoon. Their different working conditions might explain the different results between bakers and hotel and restaurant workers.
The only longitudinal study assessing coxarthrosis investigated the hospital diagnosis of all economically active men in Denmark. Since only 15% of those with severe arthritis undergo hip replacement, there might have been a high proportion of missing data. The study showed higher hospitalization rates among self-employed individuals versus employees, without an assessment of industrial sector or adjusting for social class. A dramatic fall in coxarthrosis incidence in self-employed individuals over time might be explained by the decrease in the number of self-employed farm workers that accounted for 70% of the cases in this group in the earliest period of the study. Tüchsen et al. also analyzed the differences between industrial sectors, but did so without a breakdown of the occupational groups; the authors concluded that “occupations with low risk can be characterised as nonmanual jobs performed mostly while sitting” [30]. Consequently, the Danish results might have been similar to the results of the Swedish studies by Malki et al. and Tiikkaja et al., if Tüchsen et al. would have subdivided nonmanual and manual workers instead of specific occupational groups [31–33].
The included longitudinal studies only considered ICD codes for their analysis. Further prospective research should aim for longitudinal designs to combine diagnoses from routine data sources or hospitalization rates with questionnaires because the latter may capture conditions at an early stage. These questionnaires should also include information on possible confounders, such as the industrial sector, the extent of partner or family support, dependent children and head-of-household status [53].
4.2.2Cross-sectional studies
The ten cross-sectional studies of good quality that we included in our systematic evaluation showed a rather heterogeneous picture in terms of the study characteristics and outcomes examined. Studies that found associations of self-employment with negative health outcomes predominantly investigated musculoskeletal, respiratory or malignant diseases [34–36, 38, 39, 41]. The following reasons may explain these findings. First, the most dangerous industries that include hard physical working conditions (e.g. forestry) often hire self-employed workers [39]. Second, some personal factors, such as long working hours or an increased age, apply to many self-employed individuals. Third, in Europe, self-employed individuals are not subject to occupational health legislations [39]. Furthermore, the majority of the included studies used no validated questionnaires. Cross-sectional study designs do not allow us to conclude whether the observed health problems occurred because of or independent of employment status. The employed reference groups of these studies were younger, had a higher educational status and income, and/or were more often nonmanual workers.
According to some studies, low-qualified or low-income workers are at higher risk of injuries and health-related problems [21, 39, 54]. For example, Kim et al. investigated a self-employed group comprising 60% caregivers and an employed group consisting of 50% nonmanual workers [41]. Consequently, the predominant negative effect of self-employment on musculoskeletal conditions could be due to a sample bias. The study by Holmberg et al. was the only one that found a lower prevalence for lower back pain in self-employed individuals compared with that in employees [37]. A reason for these contrary outcomes could be that this study excluded farmers from the group of self-employed individuals and rather examined them separately, whereas the group of employees included all occupations. Previous studies have shown that farmers are in poorer health than other occupational groups [55–57]. Holmberg et al. also found a higher prevalence of lower back pain among self-employed farmers than among employees. Nevertheless, the sick leave rate of farmers due to lower back pain was lower than that of employees [37], which indicated high presenteeism rates for self-employed individuals.
Regarding hypertension, diabetes, headache and eyestrain, the results showed slightly better or similar health outcomes among self-employed individuals than among employees [20, 40, 41, 55]. Different reasons might explain these contradictory results. The study by Stephan et al. was the only one that used ICD codes for assessment [20]. Since only a doctor determines ICD codes, a doctor visit provides the basis for a diagnosis. Previous studies have found that health problems and work hours negatively affect health care utilization. The loss of earning when being absent from work may discourage the solo self-employed from visiting a doctor [58]. Lee et al., who conducted the only study that examined dry eye symptoms, suggested that self-employed individuals may regulate their workplace environment [40]. This flexible regulation may help to relax the eyes, regularly.
4.3Strengths and potential limitations
This has been the first global systematic review about the occurrence of physical illness among self-employed workers. Furthermore, when searching for appropriate studies, we did not exclude any language or country. In addition to this comprehensive approach, we included only studies with a comparison group of employees. Another strength of our study was the stringent assessment of the methodological study quality, in particular the risk of bias with a widely used instrument for observational studies (Table S1).
However, several potential limitations must be mentioned. First, although we searched several large medical databases, which was complemented by hand searching other internet sources and the references of the included publications, we may have missed relevant studies if they were published elsewhere. Second, we observed that outcomes or employment status categories were too heterogeneous across the included studies to consider conducting a meta-analysis. In general, the studies of our systematic review used rather different assessment tools, which may hamper their comparability (Tables 2 and 3). We identified 14 different outcome measures, including nonvalidated questionnaires that were specifically developed for specific investigations. Third, the majority of the studies compared self-employed individuals with employees from different occupational sectors. In many studies, the self-employed individuals group was also rather heterogeneous. There were only four studies that examined self-employed individuals and employees from the same occupation (farmers, hotel staff, bakers, therapists, joiners) [28, 30, 31, 38]. In this respect, the Eurofond and International Labor Organization have stated that “wide-scale differences in job quality in all countries are evident, reflecting the different nature of work across sectors, occupations and workplaces” [50]. There is a need for research examining different classes and sectors within the self-employed [2]. Fourth, there is no official distinction between independent self-employed workers and persons who economically depend on an employer [59]. Fifth, the international comparability between the included studies may be further hampered due to considerably different working conditions. For example, the decision latitude of workers from South Korea is at least one-third less than the decision latitude of other countries. Additionally, cognitive demands at work, including “learning new things”, “complex tasks” and “solving unforeseen problems on your own”, are less common in China and the Republic of Korea than in European countries. Workers in European countries have also reported to be “working over 48 hour a week” less often compared with workers in other countries, while workers in China, the Republic of Korea and Turkey work the most hours per week [50]. Additionally, sole proprietors (i.e., self-employed individuals without employees), whose proportion in the general population is increasing due to the global demand for labor market flexibility, have a higher risk of entering into a precarious economic situation than do others. Self-employed individuals with employees, on the other hand, face less pressure than others because they have more financial resources [60, 61].
Sixth, for the included studies from across the globe, we were not able to take into account the overall economic situation, i.e., whether the study was conducted during a period of growth or a recession. An economic crisis may lead to a higher percentage of precarious self-employment and thus increase the occurrence of physical and mental disorders, whereas a good economic situation could have the opposite effect [3]. Nevertheless, we included studies from across the globe to get an overview as a basis for the comparison of possible country-specific differences. However, before planning preventive intervention studies, more recent and local data needs to be evaluated to verify findings of studies from other countries or socio-cultural backgrounds.
Seventh, we included also older studies in this systematic review, because a systematic summary of all studies has not been published previously. However, due to economic, political and cultural changes in the last decades, we consider the inclusion of these older studies rather as a supplement for further ideas than a basis to develop prevention strategies. Eighth, with respect to the variety of presented physical health outcomes, we would like to point toward possible somatization effects of psycho-emotional disturbances. For example, well-known target areas for musculoskeletal complaints of psycho-emotional origin are the neck, the lower back, the shoulder, the temporomandibular joint or the widespread effect of fibromyalgia. This observation also entails the progressive, objectively verifiable physical manifestation of a primarily emotional burden over time [62, 63]. Moreover, somatic symptoms appear malleable and context dependent [64]. For example, the COVID-19 pandemic has been impacting especially the informal workers‘ psychological well-being by emphasizing the existing financial tensions and job insecurity [23]. We hence suggest a multidimensional interpretation of our findings that extends beyond their physical dimension and regards somatizing tendency as a possible confounder or effect modifier in further studies, especially of occupational risk factors for musculoskeletal pain [4, 65, 66].
4.4Implications and future studies
As the first systematic summary of all population-based studies of physical problems comparing the self-employed with employees, our work will contribute to a better understanding of the development of chronic diseases and health status among the self-employed. Our findings are intended to inform policymakers and decision-makers, as well as pointing out scientific knowledge gaps in this area for funding and planning specific intervention studies. For example, based on our findings, we can point to the need to mitigate barriers to seeking medical help for the self-employed. This impression was conveyed by the fact that studies that recorded ICD-codes made the health status of the self-employed appear better than lower-threshold studies that recorded symptoms and disorders with questionnaires.
Future studies on the health of the self-employed should be designed as longitudinal evaluations and ideally combine diagnoses from routine care data sources such as hospital and insurance data with self-reported questionnaires because the latter may capture additional conditions and at an earlier stage. These questionnaires should include more detailed assessments of competition stress, workload, and work hours. Some results of studies included in our review showed the possible influence of various other factors and a possibly complex interaction on the physical health status of workers. Additionally, the results pointed out the importance of the industrial sector for e.g. hospitalization rates. Economic instability might affect occupational sectors to different extents. Therefore, further research need to investigate different occupational sectors separately and include factors assessing the economic situation.
5Conclusions
Convincing evidence with representative results from two long-term evaluations of Swedish national registers showed increased incidence and mortality rates of CVD among self-employed individuals compared with those among nonmanual workers. However, the incidence and mortality estimates of CVD in self-employed individuals were lower than those in manual workers. Most cross-sectional studies found a higher prevalence of musculoskeletal, respiratory and malignant disease among self-employed individuals compared with that among employees.
Despite a comprehensive search for population-based studies on chronic physical disorders and mortality of self-employed individuals, we were able to identify only a relatively small number of studies of good quality. As a basis for targeted prevention strategies, further population-based studies with long-term observation periods in different settings are strongly required to better understand the development of (physical) chronic disorders among specific groups of the self-employed such as sole proprietors, small entrepreneurs, family businesses and others. This includes paying attention to somatizing tendency as a possible confounder or effect modifier in further studies.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Acknowledgments
The authors thank Caroline Bauer (Bad Kissingen, Germany) for her support with the literature search.
Conflict of interests
The authors declare that they have no conflict of interest.
Funding
The authors report no funding.
Supplementary materials
The supplementary materials are available from https://dx.doi.org/10.3233/WOR-220145.
References
[1] | International labour Organization. ILOSTAT database. Available from: URL: https://data.worldbank.org/indicator/SL.EMP.SELF.ZS (Accessed April 28, (2020) ). |
[2] | Khan TH , MacEachen , Ellen , Hopwood , Pamela , Goyal J . Self-employment, Work and Health: A Critical Narrative Review. Work. (2021) ;70: (3):945–57. |
[3] | International Labour Office: Geneva, editor. Universal social protection to achieve the sustainable development goals; (2017) . |
[4] | Willeke K , Janson P , Zink K , et al. Occurrence of Mental Illness and Mental Health Risks among the Self-Employed: A Systematic Review. Int J Environ Res Public Health. (2021) ;18: (16). https://doi.org/10.3390/ijerph18168617 [PMID: 34444369]. |
[5] | Cardiovascular diseases (CVDs): Key facts; 2021 [cited 2021 October 13]. Available from: URL: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) |
[6] | Min J-Y , Kim H , Park S-G , Hwang SH , Min K-B . Differences in suicidal behaviors between self-employed and standardly employed workers. Am J Ind Med. (2019) ;62: (12):1144–51. https://doi.org/10.1002/ajim.23050 [PMID: 31544263]. |
[7] | Rossignol M , Leclerc A , Allaert FA , et al. Primary osteoarthritis of hip, knee, and hand in relation to occupational exposure. Occup Environ Med. (2005) ;62: (11):772–7. https://doi.org/10.1136/oem.2005.020057 [PMID: 16234403]. |
[8] | Nikiforow R , Hokkanen E . Effects of Headache on Working Ability: A Survey of an Urban and a Rural Population in Northern Finland. Headache. (1979) ;(19):214–8. |
[9] | Atherton K , Power C . Health inequalities with the National Statistics-Socioeconomic classification: disease risk factors and health in the British birth cohort. Eur J Public Health. (2007) ;17: (5):486–91. https://doi.org/10.1093/eurpub/ckl269 [PMID: 17267523]. |
[10] | Kee D , Haslam R . Prevalence of work-related musculoskeletal disorders in agriculture workers in Korea and preventative interventions. Work. (2019) ;64: (4):763–75. https://doi.org/10.3233/WOR-193038 [PMID: 31815716]. |
[11] | Fischer SL , Woodcock K . A cross-sectional survey of reported musculoskeletal pain, disorders, work volume and employment situation among sign language interpreters. International Journal of Industrial Ergonomics. (2012) ;42: (4):335–40. https://doi.org/10.1016/j.ergon.2012.03.003. |
[12] | Oenning NSX , Goulart BNG de , Ziegelmann PK , Chastang J-F , Niedhammer I . Associations between occupational factors and self-rated health in the national Brazilian working population. BMC Public Health. (2019) ;19: (1):1381. https://doi.org/10.1186/s12889-019-7746-5 [PMID: 31655583]. |
[13] | Andersson P . Happiness and health: Well-being among the self-employed. The Journal of Socio-Economics. (2008) ;37: (1):213–36. https://doi.org/10.1016/j.socec.2007.03.003. |
[14] | Lewin-epstein N , Yuchtman-Yaar E . Health Risks of Self-Employed. Work and Occupations. (1991) ;18: (3):291–312. |
[15] | Ohta A , Takeuchi K , Yosiaki S , Suzuki S . Differences in Lifestyle and Perceived Health in Different Occupations in a Community. J Occup Health. (1998) ;(40):325–33. |
[16] | Yoon J , Bernell SL . The effect of self-employment on health, access to care, and health behavior. Health. (2013) ;05: (12):2116–27. https://doi.org/10.4236/health.2013.512289. |
[17] | Grégoris M , Deschamps F , Salles J , Sanchez S . Health assessment of self-employed in the food service industry. Int J Occup Environ Health. (2017) ;23: (3):234–42. https://doi.org/10.1080/10773525.2018.1470788 [PMID: 29722638]. |
[18] | Lissau I , Rasmussen NK , Hesse NM , Hesse U . Social differences in illness and health-related exclusion from the labour market in Denmark from 1987 to 1994. Scand J Public Health. (2001) ;29: (55):19–30. |
[19] | López-Ruiz M , Artazcoz L , Martínez JM , Rojas M , Benavides FG . Informal employment and health status in Central America. BMC Public Health. (2015) ;15: :698. https://doi.org/10.1186/s12889-015-2030-9 [PMID: 26206153]. |
[20] | Stephan U , Roesler U . Health of entrepreneurs versus employees in a national representative sample. Journal of Occupational and Organizational Psychology. (2010) ;83: (3):717–38. https://doi.org/10.1348/096317909X472067. |
[21] | Toivanen S , Härter Griep R , Mellner C , Nordenmark M , Vinberg S , Eloranta S . Hospitalization due to stroke and myocardial infarction in self-employed individuals and small business owners compared with paid employees in Sweden—a 5-year study. Small Bus Econ. (2019) ;53: (2):343–54. https://doi.org/10.1007/s11187-018-0051-3. |
[22] | Elvis C , France N , Patience E . Risk factors for work-related musculoskeletal disorders among welders in the informal sector under resource constrained settings. 2022 Apr 12. doi: 10.3233/WOR-205275. Epub ahead of print. PMID: 35431204. WORK. (2022) ;Pre-press: (Pre-press):1–14. |
[23] | Anholon R , Rampasso IS , Dibbern T , Serafim MP , Filho WL , Quelhas OLG . COVID-19 and decent work: A bibliometric analysis. Work. (2022) :1–9. https://doi.org/10.3233/WOR-210966 [PMID: 35253711]. |
[24] | Higgins J , Thomas J . Cochrane Handbook for Systematic Reviews of Interventions: Version 6;2019 [cited 2020 May 4]. Available from: URL: https://training.cochrane.org/handbook/current. |
[25] | Moher D , Liberati A , Tetzlaff J , Altman DG . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Available from: URL: http://www.prisma-statement.org/ [cited 2020 May 4]. |
[26] | Hoy D , Brooks P , Woolf A , et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. (2012) ;65: (9):934–9. https://doi.org/10.1016/j.jclinepi.2011.11.014 [PMID: 22742910]. |
[27] | Moher D , Liberati A , Tetzlaff J , Altman DG . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement: Version 6;2019 [cited 2020 May 4]. Available from: URL: https://www.prisma-statement.org/ |
[28] | Hogan DAM , O’Sullivan LW , Nolan S , Greiner BA . Are Irish therapists at heightened risk for low back pain? Occup Med (Lond). (2016) ;66: (5):351–7. https://doi.org/10.1093/occmed/kqw020 [PMID: 26968686]. |
[29] | Vagerö D , Norell SE . Mortality and Social Class in Sweden - Exploring a New Epidemiological Tool. Scandinavian Journal of Social Medicine. (1989) ;(17):49–58. |
[30] | Tüchsen F , Hannerz H , Jensen MV , Krause N . Socioexonomic status, occupation, and risk of hospitalization due to coxarthrosis in Denmark 1981–99.. Annals of the Rheumatic Diseases. (2003) ;(62):1100–5. |
[31] | Tüchsen F , Bach E , Marmot M . Occupation and Hospitalization with ischaemic Heart Diseases: A new Nationwide Surveillance System Based on Hospital Admisssions. International Journal of Epidemiology. (1992) ;21: (3):450–9. |
[32] | Tiikkaja S , Hemstrom O . Does intergenerational social mobility among men affect cardiovascular mortality? A population-based register study from Sweden. Scand J Public Health. (2008) ;36: (6):619–28. https://doi.org/10.1177/1403494808090635 [PMID: 18775818]. |
[33] | Malki N , Koupil I , Eloranta S , et al. Temporal trends in incidence of myocardial infarction and ischemic stroke by socioeconomic position in Sweden 1987–2010. PLoS ONE. (2014) ;9: (8):e105279. https://doi.org/10.1371/journal.pone.0105279 [PMID: 25170919]. |
[34] | Benavides FG , Benach J , Diez-Roux AV , Roman C . How do types of employment relate to health indicators? Findings from the Second European Survey on Working Conditions. Journal of Epidemiology and Community Health. (2000) ;(54):494–501. |
[35] | Cambois E , Garrouste C , Pailhé A . Gender career divide and women’s disadvantage in depressive symptoms and physical limitations in France. SSM Popul Health. (2017) ;3: :81–8. https://doi.org/10.1016/j.ssmph.2016.12.008 [PMID: 29349207]. |
[36] | Ferré A , Fuhrman C , Zureik M , et al. Chronic bronchitis in the general population: influence of age, gender a nd socio-economic conditions. Respir Med. (2012) ;106: (3):467–71. https://doi.org/10.1016/j.rmed.2011.12.002 [PMID: 22197577]. |
[37] | Holmberg S , Thelin A , Stiernström E-L , Svärdsudd K . Psychosocial factors and low back pain, consultations, and sick leave among farmers and rural referents: a population-based study. J Occup Environ Med. (2004) ;46: (9):993–8. https://doi.org/10.1097/01.jom.0000137715.33662.02 [PMID: 15354066]. |
[38] | Lesage F-X , Salles J , Deschamps F . Self-employment in joinery: an occupational risk facor? Int J Occup Med Environ Health. (2014) ;27: (3):355–63. https://doi.org/10.2478/s13382-014-0261-0 [PMID: 24763900]. |
[39] | Park J , Han B , Kim Y . Comparison of occupational health problems of employees and self-employed individuals who work in different fields. Arch Environ Occup Health. (2019) ;75: (2):98–111. https://doi.org/10.1080/19338244.2019.1577209 [PMID: 30896344]. |
[40] | Lee J-H , Lee W , Yoon J-H , Seok H , Roh J , Won J-U . Relationship between symptoms of dry eye syndrome and occupational characteristics: the Korean National Health and Nutrition Examination Survey 2010–2012. BMC Ophthalmol. (2015) ;15: :147. https://doi.org/10.1186/s12886-015-0147-3 [PMID: 26511443]. |
[41] | Kim H-J , Min J-Y , Min K-B . Physical and mental health problems of self-employed small business owners in South Korea. Am J Ind Med. (2019) ;62: (9):783–90. https://doi.org/10.1002/ajim.23023 [PMID: 31328810]. |
[42] | Rosén M . Chapter 5. major public health problems - cardiovascular diseases. Scand J Public Health Suppl. (2006) ;67: :51–8. https://doi.org/10.1080/1403495060067686. |
[43] | Ham DC , Przybeck T , Strickland JR , Luke DA , Bierut LJ , Evanoff BA . Occupation and workplace policies predict smoking behaviors: analysis of national data from the current population survey. J Occup Environ Med. (2011) ;53: (11):1337–45. https://doi.org/10.1097/JOM.0b013e3182337778 [PMID: 21988795]. |
[44] | Gaudette LA , Richardson A , Huang S . Which workers smoke? Health Reports. (1998) ;10: (3). |
[45] | Nilsson S , Carstensen JM , Pershagen G . Mortality among male and female smokers in Sweden: a 33 year follow up. Journal of Epidemiology and Community Health. (2001) ;55: (11):825–30. [https://doi.org/10.1136/jech.55.11.825] [PMID: 11604439]. |
[46] | Wald N , Hackshow A . Cigarette smoking: an epidemiological overview. British Medical Bulletin. (1996) ;(52: (1)):3–11. |
[47] | Baten J . A history of the Global Economy. From 1500 to the Present. Campridge University Press; (2016) . |
[48] | Seinmo S . Bucking the Trend? The Welfare State and Global Economy: The Swedish Case Up Close; (2001) . |
[49] | Steptoe A , Marmot M . The role of psychobiological pathways in socio-economic inequalities in cardiovascular disease risk. Eur Heart J. (2002) ;23: (1):13–25.. [https://doi.org/10.1053/euhj.2001.2611] [PMID: 11741358]. |
[50] | Eurofound and International labor Organization. Working Conditions in a Global Perspective; (2019) . |
[51] | Karasek RA . Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Administrative Science Quarterly. (1979) ;24: (2):285–308 . |
[52] | Beutell NJ . Self-Employment, Work-Family Conflict and Work-Family Synergy: Antecedents and Consequences. Journal of Small Business & Entrepreneurship. (2007) ;20: (4):325–34. https://doi.org/10.1080/08276331.2007.10593403. |
[53] | Jang S-Y , Jang S-I , Bae H-C , Shin J , Park E-C . Precarious employment and new-onset severe depressive symptoms: a population-based prospective study in South Korea. Scand J Work Environ Health. (2015) ;41: (4):329–37. [https://doi.org/10.5271/sjweh.3498] [PMID: 25909824]. |
[54] | Hessels J , Rietveld CA , van der Zwan P . The Relation Between Health and Earnings in Self-Employment. Front Psychol. (2020) ;11: :801. [https://doi.org/10.3389/fpsyg.2020.00801] [PMID: 32528341]. |
[55] | Saarni SI , Saarni ES , Saarni H . Quality of life, work ability, and self employment: a population survey of entrepreneurs, farmers, and salary earners. Occup Environ Med. (2008) ;65: (2):98–103. [https://doi.org/10.1136/oem.2007.033423] [PMID: 17666452]. |
[56] | Holmberg SAC , Thelin AG . Predictors of sick leave owing to neck or low back pain: A 12-year longitudinal cohort study in a rural male population. Ann Agric Environ Med. (2010) ;(17):251–7. |
[57] | Holmberg S , Thelin A , Stiernström E-L , Svärdsudd K . The Impact of Physical Work Exposure on Musculoskeletal Symptoms among Farmers and Rural Non-Farmers. A Population-based Study. Ann Agric Environ Med. (2003) ;(10):179–84. |
[58] | Bosio G , Minola T , Origo F . Healthy, wealthy or busy?: Self-employment and healthcare services utilization in Europe (2016) . |
[59] | Böheim R , Mühlberger U . Dependent self-employment: workers between employment and self-employment in the UK. ZAF. (2009) ;42: (2):182–95. [https://doi.org/10.1007/s12651-009-0014-x]. |
[60] | Westerveld M . The “New” Self-Employed: An Issue for Social Policy? Journal of Social Security. (2012) ;14: (3):156–73. |
[61] | Horemans J , Marx I . Poverty and Material Deprivation among the Self-Employed in Europe: An Exploration of a Relatively Uncharted Landscape: IZA DP No. 11007. SSRN Electronic Journal. (2017) . |
[62] | Glise K , Ahlborg G , Jonsdottir Jr. IH . Prevalence and course of somatic symptoms in patients with stress-related exhaustion: does sex or age matter. BMC Psychiatry. (2014) ;14: (118). |
[63] | Kroenke K . Patients presenting with somatic complaints: epidemiology, psychiatric co-morbidity and management. International Journal of Methods in Psychiatric Research. (2003) ;12: (1):34–43. |
[64] | Beutel ME , Klein EM , Henning M , et al. Somatic Symptoms in the German General Population from 1975 to 2013. Sci Rep((2020) ;10: (1):1595. [https://doi.org/10.1038/s41598-020-58602-6] [PMID: 32005895]. |
[65] | Palmer KT , Calnan M , Wainwright D , et al. Disabling musculoskeletal pain and its relation to somatization: a community-based postal survey. Occup Med (Lond). (2005) ;55: (8):612–7. [https://doi.org/10.1093/occmed/kqi142] [PMID: 16174664]. |
[66] | McBeth J , Macfarlane GJ , Benjamin S , Silman AJ . Features of somatization predict the onset of chronic widespread pain: Results of a large population-based study Arthritis & Rheumatism. (2001) ;44: (4):940–6 . |



