Influence of different protection levels of PPE on nurses’ physical fatigue during the COVID-19 pandemic
Abstract
BACKGROUND:
The continuous spread of COVID-19 globally has led to busier medical practices and nurses are having to provide medical services to patients while suffering from high levels of fatigue.
OBJECTIVE:
This study experimentally investigated the influence of different levels of personal protection equipment (PPE) on nurses’ physical fatigue.
METHODS:
We collected data from 12 participants by simulating a series of nursing tasks. The participants wore one of three different protection levels of PPE, and data recording their heart rate (HR), oral temperature, task completion time, and subjective fatigue were collected. Following this, relationship models between subjective fatigue and objective fatigue indices was established using multiple linear regression analysis.
RESULTS:
By analyzing the variation trends of single indices of HR, oral temperature, task completion time, and subjective fatigue, it was found that the higher the level of protection levels of PPE worn by the participants, the higher the degree of fatigue experienced by them. In addition, taking subjective fatigue variation as the dependent variable and objective fatigue indices as independent variables, relationship models of the three different protection levels of PPE were established.
CONCLUSIONS:
The results confirmed the influence of different protection levels of PPE on nurses’ physical fatigue levels. They also provide a basis for medical administrators to monitor the degree of fatigue experienced by nurses, attempt to arrange nurses’ work content accordingly, and schedule suitably to combat and manage recorded increases in fatigue.
1Introduction
The COVID-19 pandemic, which began in late 2019, has spread rapidly worldwide. As of December 17, 2021, the World Health Organization (WHO) has reported 271,963,258 confirmed cases of COVID-19, as well as 5,331,019 subsequent deaths globally [1]. Lately, the Omicron strain has exacerbated the effects of the pandemic due to it being more infectious than the Delta strain, which makes the prevention and control of the pandemic more difficult, ultimately indicating that the number of positive cases will continue to rise. As a result of this, healthcare workers face longer working hours, heavier workloads, and higher risks of infection [2]. WHO reported that between January 2020 and May 2021, nearly 115,500 healthcare workers died from COVID-19 worldwide [3]. The use of personal protection equipment (PPE) by healthcare workers while at work is, therefore, a primary infection protection strategy.
The issue of fatigue suffered by healthcare workers cannot be ignored and is an important subject which has concerned researchers for many years, even before the emergence of COVID-19. Fatigue refers to a state in which the body’s working efficiency declines due to long-term or over-stressed physical or mental work under certain environmental conditions [4]. The factors which influence fatigue are multifaceted and complex, and are closely related to human performance, physiology, cognition, and emotion amongst others [5]. Physical fatigue and mental fatigue are the two main aspects of fatigue research [6]. Physical fatigue is related to physical activity and leads to a decline in the ability to complete physical activity. Mental fatigue is related to mental activity and can be evaluated in terms of alertness and memory when completing tasks [7]. Fatigue is considered to be a multi-faceted concept that demands to be analyzed and measured from different dimensions [8]. As nurses account for the highest proportion of medical workers and are in direct and regular contact with patients to provide medical services, the increase in nurses’ fatigue has become a cause for concern [9]. Nursing work involves carrying out physical and mental tasks simultaneously, and there is a high chance for physical and mental fatigue to occur [11–13]. This is an important factor that may lead to the occurrence of medical errors [10].
Nurses provide a full range of medical and other services which require a lot of physical activity, and having to wear PPE increases their body’s thermal load [14, 15]. As a result, the body need to speed up external heat loss to achieve thermal balance, but is unable to do so due to the PPE preventing heat evaporation [14, 15]. This disturbance of the body’s thermal balance can increase fatigue, which in turn can affect health and performance in nurses [14, 15]. Although studies have been conducted on the impact of protective equipment on physical fatigue in the field of firefighting, this research is mainly based on virtual models, and the types of protective clothing and working conditions are different from those in nursing [16, 17]. The purpose of the present study was to determine whether the different protection levels of PPE influence nurses’ fatigue, and, if so, what the extent of this influence is.
2Methods
2.1Participants and environment
We recruited 12 participants for this experiment, including six males and six females, ranging in age from 20 to 22 years old, with a mean height of 167.1±7.0 cm and mean weight of 57.9±9.0 kg. and all the subjects were right-handed. The above participants were randomly selected from among the candidates. In order to observe whether gender factors affect the research results, we selected 6 male and 6 female participants respectively. Before conducting the experiment we ensured that all the participants were in good health, did not have any injuries that might affect the results of the experiment, and had not partaken in any strenuous exercise 24 hours before the experiment.
2.2Development of experimental tasks
We ascertained the daily tasks and working conditions of nurses in medical institutions during the COVID-19 pandemic through research and field visits. We designed seven tasks which are representative of a nurse’s daily tasks based on our research and related literature [18], which were combined as the experimental tasks of this study (Table 1).
Table 1
Experimental tasks
| Serial | Nursing tasks | Task description |
| number | ||
| 1 | Transport patients | The participants began from the starting point, pushed a wheelchair with a patient (50 kg in weight) in the corridor of the teaching building (approximately 130 m long and 2 m wide), went straight and turned according to the prescribed track. |
| 2 | Collect patients’ files | The participants entered the simulated ward, collected the patient’s nursing records, returned to the simulated nursing station, and placed the nursing records in the designated area. |
| 3 | Select and distribute medication | The participants entered the simulated pharmacy, selected different quantities of medications according to the instructions, placed them in the drug cup, and sent them to the simulated ward. |
| 4 | Record patients’ vital statistics | The participants entered the simulated ward, recorded the physical parameters (HR, blood pressure, blood oxygen saturation) of two patients with a pen, and then went to the simulated nursing station to input these parameters into the computer. The participants stood the entire time during this process. |
| 5 | Changing sheets | The participants entered the simulated ward, removed and folded a dirty bed sheet, then picked up a clean sheet and spread it flat on the bed. |
| 6 | Transport patients | The participants repeated Task 1. |
| 7 | Placement of supplies | The participants moved two 4 kg cuboid cartons from a 20 cm high shelf to a 130 cm high shelf, placed them steadily, and then moved the cartons back to the 20 cm shelf. |
In each experimental round, the participants repeated three rounds of the simulated nursing tasks; each round included the seven tasks listed in Table 1. The entire process was completed in a teaching building, which was equipped with a simulated “ward,” “nursing station” and “pharmacy.” These areas were equipped with computers, wheelchairs, shelves, and other related supplies to mimic the daily work and environment of an ordinary healthcare worker in a general hospital during the COVID-19 pandemic.
2.3Three protection levels
After consulting the relevant documents and regulations [19], medical institutions have to take certain protective measures; the level of protective measures to be implemented depends on the possibility of healthcare workers encountering suspected or confirmed COVID-19 positive patients.
Three different levels of protection were used in this experiment, namely: low protection level (PL), medium protection level (PM), and high protection level (PH). The following table lists the forms of PPE used in the different protection levels.
Table 2
Different protection of levels of PPE
| Protection | Detailed equipment |
| states | |
| PL | Disposable surgical mask for medical use |
| PM | Disposable surgical mask for medical use, disposable protective clothing for medical use, disposable medical cap |
| PH | KN95 protective mask, disposable protective clothing for medical use, disposable medical cap, medical face shield, disposable sterile rubber examination gloves, medical isolation shoe cover |
All participants wore long-sleeved cotton tops, long sweatpants, and flat shoes, as shown in Fig. 1.
Fig. 1
Three protection levels of PPE.
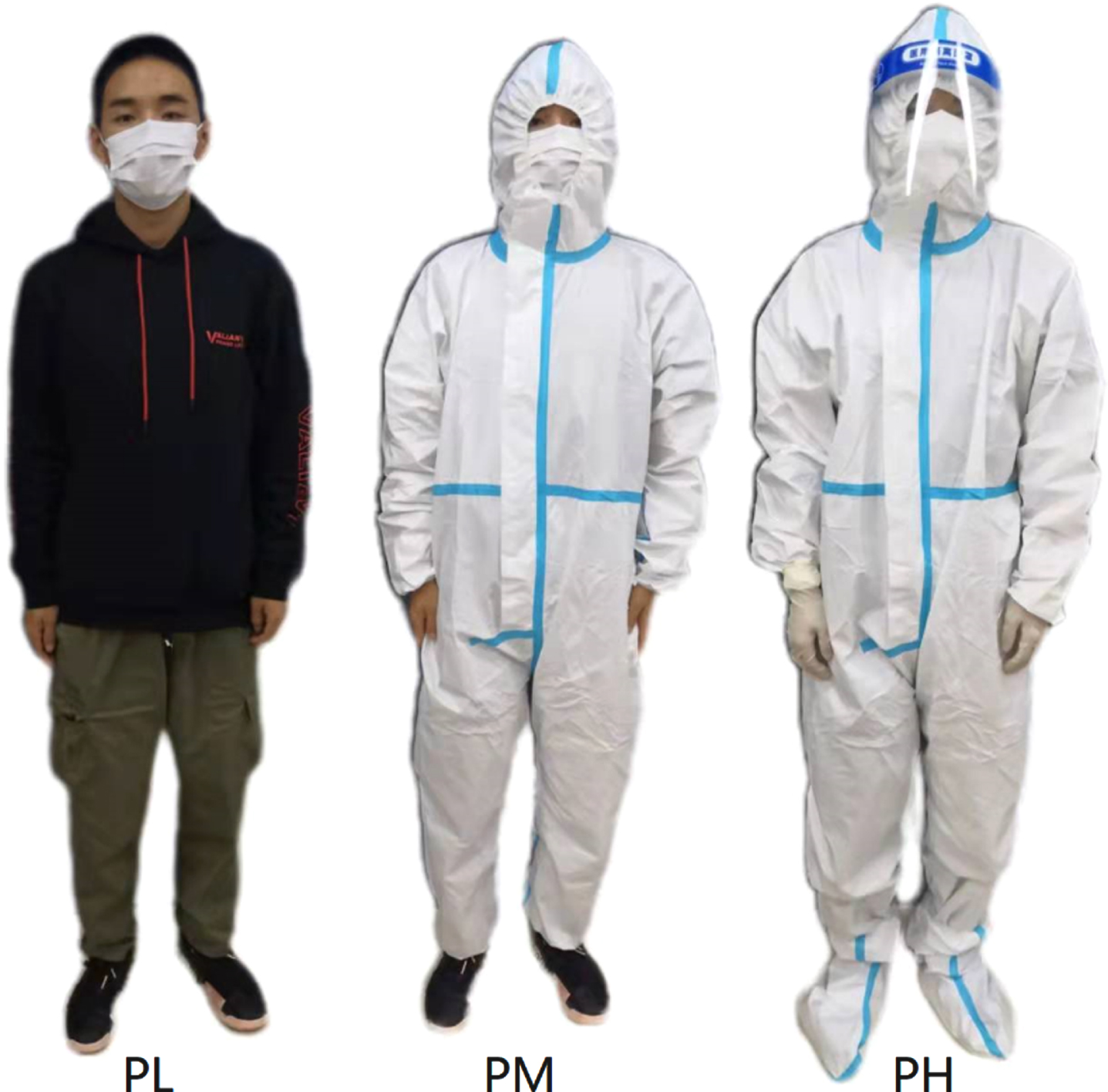
Figure 1 shows the three different protection levels, from left to right are PL, PM, and PH.
2.4Index measurements
During the experiment, we collected data on participants’ HR, oral temperature, and time taken to complete tasks. The HR is a commonly used physiological index to measure the degree of fatigue being experienced by an individual [20]. We used a fingertip pulse oximeter (YX306) on participants’ left index finger to measure their HR.
Oral temperature is a stable index reflecting the surface temperature of the human body and can indicate the degree of fatigue being experienced by an individual [21]. Compared to the measurement of core temperature, it is quicker and easier to measure the oral temperature of healthcare workers in their work environment. The participants’ oral temperature was measured using a triangular rod type glass mercury thermometer. Different levels of fatigue have an impact on a nurse’s work performance; task completion time was used to measure participants’ work performance in this experiment. A stopwatch was used to record the time it took them to complete all tasks wearing different levels of protection.
Finally, The Borg Scale of Perceived Exertion was used to measure and record the participants’ subjective levels of fatigue. After completing each round of the task cycle, participants were asked to evaluate their state of fatigue according to their feelings at the time and select the appropriate fatigue level according to the scale.
2.5Experimental procedures
Each participant was required to complete a series of simulated nursing tasks wearing each of the three different protection levels of PPE. The experiment was carried out in a laboratory, where the temperature was controlled at 21±1 °C, humidity was controlled at 55±5 %, and noise was controlled below 40 dB. Each participant was tested wearing each of the three different protection levels of PPE using the balanced Latin square study design to eliminate the influence of a participant’s competency on the experimental data. The three experiments conducted on each participant were scheduled at the same time of the day, but on different dates and at least 48 hours apart. The specific experimental procedures for each experiment were as follows:
1) The participants were uniformly trained to understand and master the experiment process before the experiment started;
2) The HR and oral temperature of the participants were measured before the experiment began and this data was recorded as the initial HR and oral temperature;
3) In a single specified protection level of PPE, all participants completed the seven simulated nursing tasks, taking turns, according to the guidelines and instructions given. This was recorded as one round of the task cycle. The participants then took a 3-minute break, during which they could only sit quietly on a chair. During the experiment, the participants’ HR was measured and recorded at the time when each task was completed. The participants’ oral temperature and subjective fatigue were measured after each round of the task cycle was completed.
4) We repeated Step 3 twice.
5) We completed the experiment and paid the participants for their assistance.
3Results
3.1Physiological index
3.1.1HR
HR is the most commonly used index for fatigue. In this study, the HR data of the 12 participants was collected during the experiment while they were wearing the different protection levels of PPE. The data were sorted according to the different protection levels of PPE and the different experimental stages of each participant, as shown in Fig. 2.
The horizontal axis of Fig. 2(a) represents the participants, each number representing one participant, and the vertical axis of Fig. 2(a) represents the participants’ average HR. The variation curves of the average HR of each participant in the same experimental task wearing different protection levels of PPE are shown in the figure. As shown in Fig. 2(a), with the increase in the protection level of PPE worn (from low to high), the participant’s HR increased when completing the same experimental task. This shows that the participants were more prone to physical fatigue wearing a higher protection level of PPE for the same experimental task.
Fig. 2
HR data.
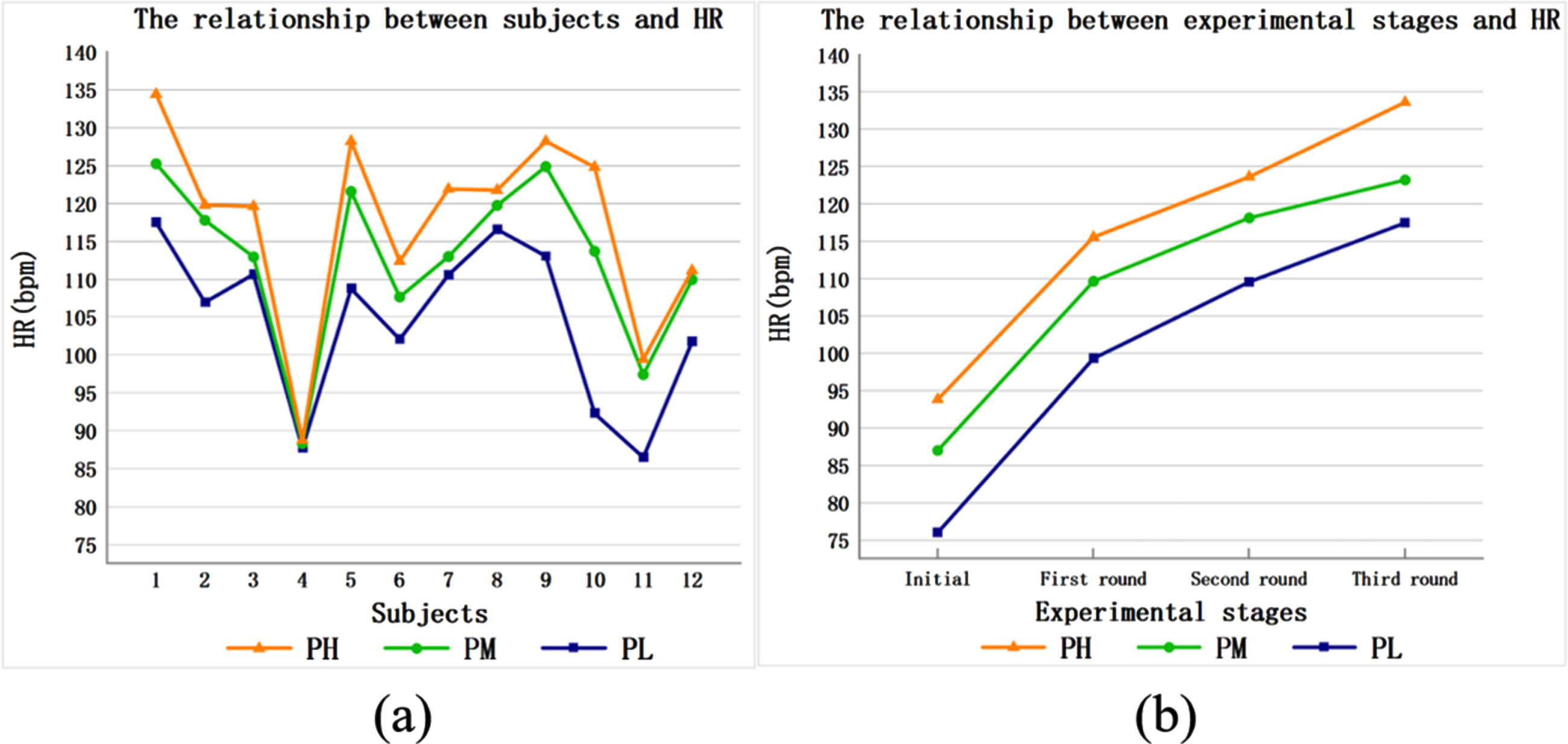
The participants carried out three rounds of the experimental tasks in Table 1 wearing the different protection levels of PPE. The horizontal axis of Fig. 2(b) represents each round of the experimental tasks, and the vertical axis of Fig. 2(b) represents the average HR of all participants in each round of experimental tasks. The variation curves of the average HR of the participants wearing the different protection levels of PPE, as the number of experimental rounds increased, was observed. It can be seen that with an increase in the number of experimental rounds, the average HR of the participants in each protection level of PPE increased. In addition, we recorded that with the increase in the protection level of PPE worn (from low to high), the HR of the participants increased sequentially. This could indicate that the physical fatigue of the participants increased with the increase in the protection level of PPE worn. In addition, we observed that gender factors did not affect the above results.
3.1.2Oral temperature
Oral temperature is a stable index and is not easily affected by external factors, such as the environment. In this study, the oral temperature data of the 12 participants was collected during the experiment while they were wearing the different protection levels of PPE. The data were sorted according to the different protection levels of PPE and the different experimental stages of each participant, as shown in Fig. 3.
Fig. 3
Oral temperature data.
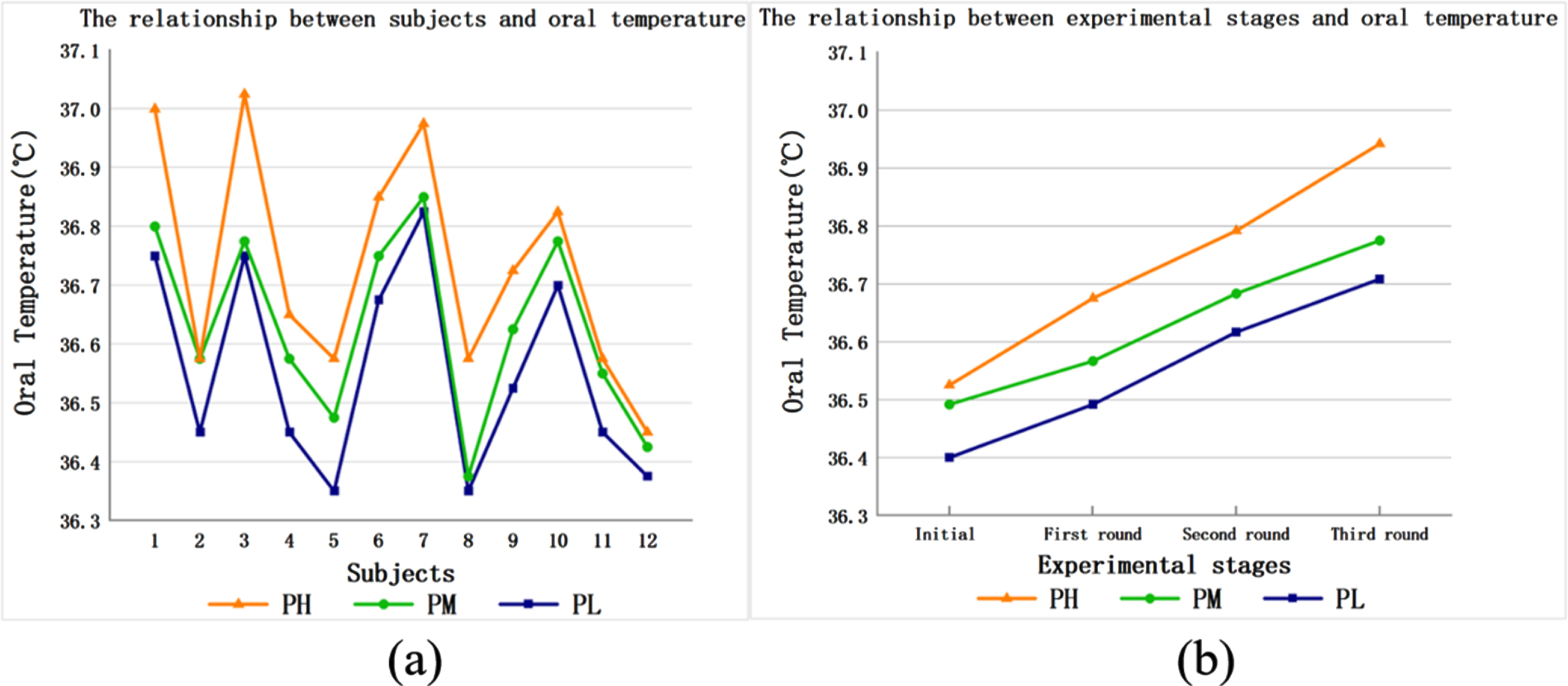
The horizontal axis of Fig. 3(a) represents the participants, each number represents one of the participants, and the vertical axis of Fig. 3(a) represents the participants’ average oral temperature. The changes in the average oral temperature of each participant in the same experimental task wearing different protection levels of PPE are shown in the figure. We noted that with the increase in the protection level of PPE (from low to high), the oral temperature of the participants increased. This shows that the participants were more prone to fatigue wearing a higher protection level of PPE for the same experimental task.
The participants carried out three rounds of the experimental tasks in Table 1 wearing the different protection levels of PPE. The horizontal axis of Fig. 3(b) represents each round of the experimental tasks, and the vertical axis of Fig. 3(b) represents the average oral temperature of all participants in each round of experimental tasks. The variation curves of the average oral temperature of the participants wearing different protection levels of PPE, as the number of experimental rounds increased, was observed. It can be seen that with an increase in the number of experimental rounds, the average oral temperature of the participants wearing the different protection levels of PPE increased. We also recorded that with the increase in the protection level of PPE (from low to high), the oral temperature of the participants increased sequentially. It is therefore possible that their fatigue increased with the increase in the protection level of PPE worn. In addition, we observed that gender factors did not affect the above results.
3.1.3Task completion time
Task completion time is a typical index of work performance. It has been shown that as the degree of fatigue increases work performance is affected adversely. In this study, the task completion time data of the 12 participants were recorded during the experiment while they were wearing the different protection levels of PPE. The data were sorted according to the different protection levels of PPE and different experimental stages of each participant, as shown in Fig. 4.
Fig. 4
Task completion time data.
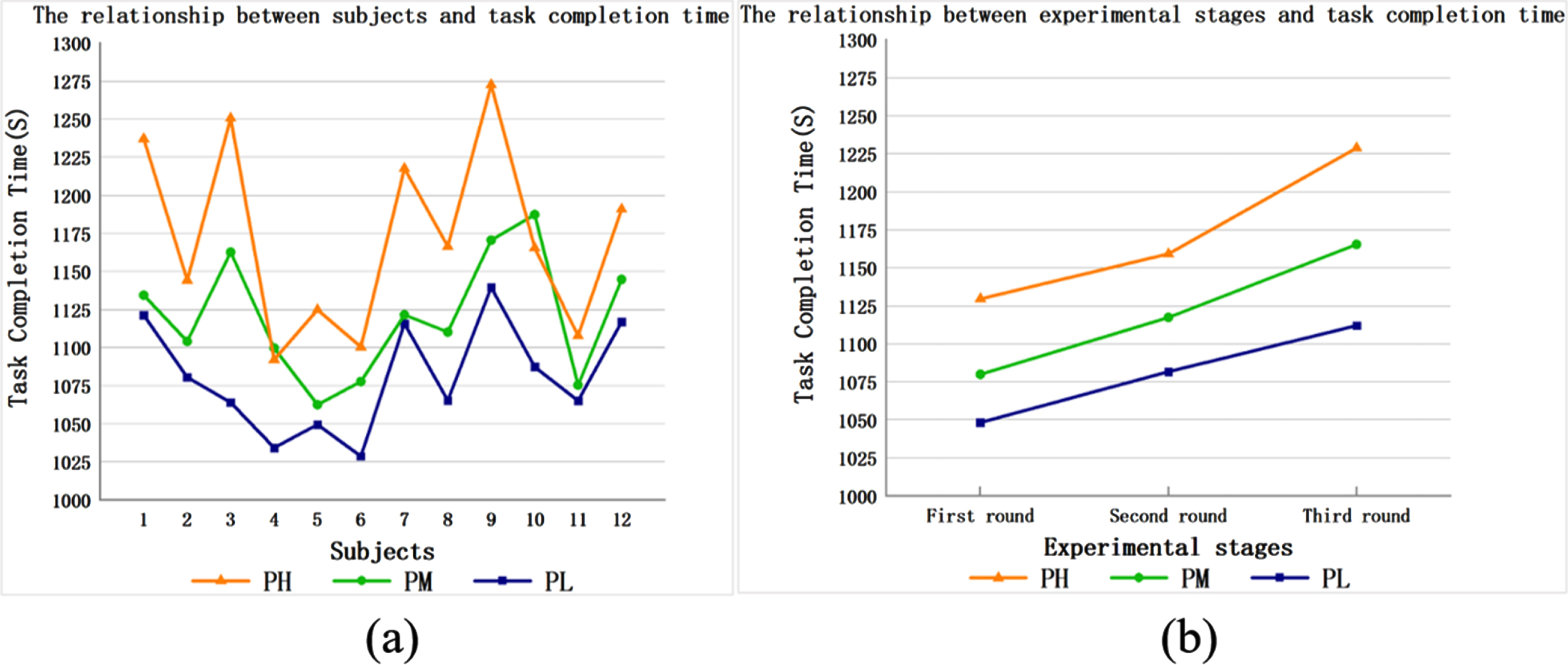
The horizontal axis of Fig. 4(a) represents the participants, each number represents one of the participants, and the vertical axis of Fig. 4(a) represents the participants’ average task completion time. The changes in the average task completion time of each participant in the same experimental task wearing different protection levels of PPE are shown in the figure. As shown in Fig. 4(a), with the increase in the protection level of PPE worn (from low to high), the task completion time of the participants when completing the same experimental task increased. This indicates that the participants were more prone to fatigue when wearing a higher protection level of PPE for the same experimental task.
The participants carried out three rounds of the experimental tasks in Table 1 wearing the different protection levels of PPE. The horizontal axis of Fig. 4(b) represents each round of the experimental tasks, and the vertical axis of Fig. 4(b) represents the average task completion time of all participants in each round of experimental tasks. The variation curves of the average task completion time of participants wearing the different protection levels of PPE, as the number of experimental rounds increased, was observed. It can be seen that with an increase in the number of experimental rounds, the average task completion time of the participants in each protection level of PPE increased. In addition, our research showed that with the increase in the protection level of PPE (from low to high), the participants’ task completion time increased sequentially. This indicates that wearing a higher protection level of PPE had a significant influence on the participants’ fatigue. In addition, we observed that gender factors did not affect the above results.
3.2Subjective index
Subjective fatigue evaluation is necessary in fatigue research [22]. In this study, The Borg Scale of Perceived Exertion (6–20 levels) was used to measure the subjective level of fatigue experienced by each participant. The subjective fatigue level data of the 12 participants were recorded during the experiment while they were wearing the different protection levels of PPE, and were sorted according to the different protection levels of PPE as well as the different experimental stages of each participant, as shown in Fig. 5.
Fig. 5
Subjective fatigue data.
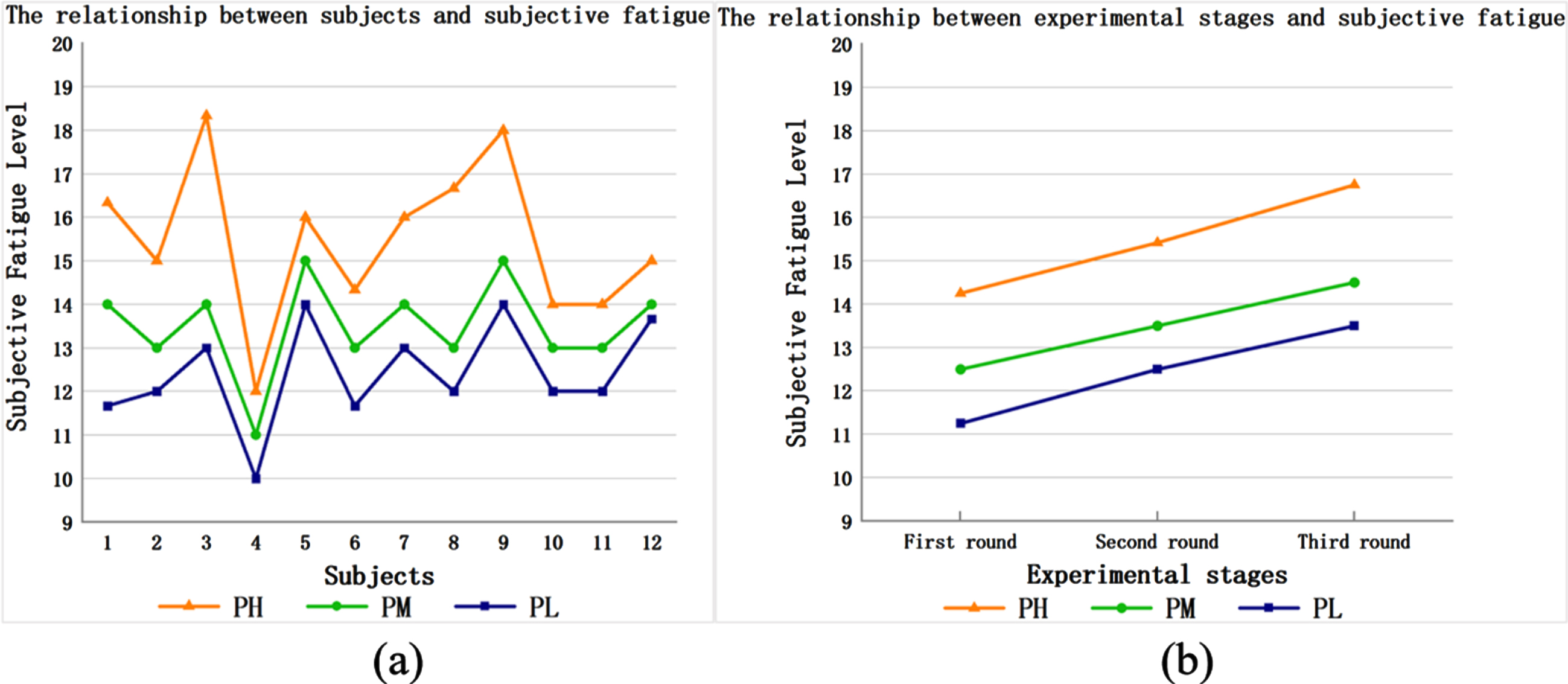
The horizontal axis of Fig. 5(a) represents the participants, each number represents one of the participants, and the vertical axis of Fig. 5(a) represents the average subjective fatigue level of the participants wearing the different protection levels of PPE. The changes in the average subjective fatigue level of each participant in the same experimental task wearing the different protection levels of PPE are shown in the figure. It can be seen that with the increase in the protection level of PPE worn (from low to high), the subjective fatigue level of the participants increased when completing the same experimental task. This indicates that the participants are more prone to fatigue wearing a higher protection level of PPE for the same experimental task.
The participants carried out three rounds of the experimental tasks in Table 1 wearing the different protection levels of PPE. The horizontal axis of Fig. 5(b) represents each round of the experimental tasks, and the vertical axis of Fig. 5(b) represents the average subjective fatigue level of all participants in each round of experimental tasks The variation curves of the average subjective fatigue level of the participants wearing the different protection levels of PPE, as the number of experimental rounds increased, was observed. It can be seen that with an increase in the number of experimental rounds, the average subjective fatigue level of the participants in each protection level of PPE increased. Moreover, with the increase in the protection level of PPE(from low to high), the participants’ subjective fatigue level increased. This could indicate that wearing the highest protection level of PPE had the greatest influence on the participants’ fatigue. In addition, we observed that gender factors did not affect the above results.
3.3Regression analysis
Multiple regression analysis is a statistical analysis method in which one variable is regarded as the dependent variable and one or more other variables are regarded as independent variables. The quantitative relations of mathematical models among multiple variables are established and analyzed using sample data [23].
In order to quantitatively express variations in the subjective fatigue of healthcare workers, variations in HR, oral temperature and task completion time were taken as independent variables, and variations in subjective fatigue were taken as dependent variable. The relationship between the was explored through the multiple regression analysis using IBM SPSS 25.0 software. We utilized the following process: firstly, we applied the Pearson correlation coefficient test, determining that there were significant correlations between subjective fatigue variations and HR variations (r = 0.746), subjective fatigue variations and oral temperature variations (r = 0.694), and subjective fatigue variations and task completion time variations (r = 0.769). Secondly, the regression model between objective fatigue indices and subjective fatigue index was established using IBM SPSS software (version 25.0) from the perspective of PL, PM, and PH. The specific results were as follows:
PL:
(1)
Adjusted R2 = 0.800, F(2, 33) = 47.682, P = 0.000< 0.05. The goodness of fit was good, and the model was acceptable.
PM:
(2)
Adjusted R2 = 0.630, F(2, 33) = 20.894, P = 0.000< 0.05. The goodness of fit was good, and the model was acceptable.
PH:
(3)
Adjusted R2 = 0.852, F(2, 33) = 68.286, P = 0.000< 0.05. The goodness of fit was good, and the model was acceptable.
The meaning of the related symbols in formulas (1), (2), and (3) are as follows:
SFLC: The variations in subjective fatigue level
HRC: The variations in HR
TC: The variations in task completion time
TempC: The variations in oral temperature
4Discussion
Nursing work is characterized by close contact with patients and other healthcare workers, 24-hour shift work, and diverse work content (including adjuvant therapy, patient care, and close coordination with other medical departments). Nursing staff comprise the largest number of healthcare workers and assume the largest workload in the medical field. As a result, the issue of the increase in nurses’ fatigue cannot be ignored [11, 24, 25]. An assessment of the previous studies on nurses’ fatigue shows that they focused mainly on physiological and psychological factors such as work flow, and organizational and management structures [11, 26, 27]. During the COVID-19 pandemic, related studies have indicated that nurses’ fatigue is increasing, but the cause for this increase has been attributed mainly to longer working hours, higher workload, and psychological stress [28, 29]. Being able to conduct nursing tasks in a safe and protected environment is critical to nursing during the COVID-19 pandemic. Although some studies have shown that PH affect nurses’ work performance [30], insufficient attention has been paid to the relationship between the different protection levels of PPE and nurses’ fatigue. In this study we explored the influence of different protection levels of PPE on nurses’ physical fatigue and verified that the differing protection levels are a new factor contributing to the increase in fatigue among nurses.
This study was conducted based on experimental settings closely simulating the daily work content and environment of nurses. Therefore, we submit that the study results truly reflect current issues in medical practice. Secondly, fatigue was measured using multiple indices; unlike earlier single-index fatigue evaluations, this study collected data based on multi-dimensional indices and confirms the influence of different protection levels of PPE on fatigue from multiple angles. We proposed that the use of PH by nursing staff causes higher levels of fatigue, as compared to the use of PM or PL. Thirdly, the regression models between the objective indices and subjective fatigue in different protection levels of PPEs were expressed quantitatively. The models not only theoretically explain the relationship between subjective fatigue and objective indices in the different protection levels of PPE, but also provide a basis for an objective evaluation of the degree of fatigue experienced by nurses in practical work settings.
Based on the results of this study, we would like to offer the following suggestions to medical administrators.
The higher level of PPE worn by healthcare workers the faster the rate of fatigue will increase. Working for an extended period of time while suffering high levels of fatigue can cause stress which could lead to medical errors. Medical administrators would be wise to acknowledge this problem and try to formulate effective measures to reduce fatigue for nurses and other healthcare workers. In addition, the results of our study showed that with the increase in the protection level of PPE, the oral temperature of the participants increased. Therefore, medical administrators should pay closer attention to the temperature of nurses in a high protection state, and correctly determine whether the high temperature is caused by physical fatigue or health problems. Furthermore, based on the findings of the study, we strongly recommend that medical administrators should provide more reasonable working hours, shifts and resting times for nurses in a high level of PPE.
Wearing different levels of PPE has an influence on task completion time. Our study showed that the higher level of PPE worn, the longer it took to complete certain tasks. Medical administrators need to be fully aware of this phenomenon in order to give nurses more time to complete tasks if they are wearing a high level of PPE or to make other suitable arrangements. This also means that in the same working environment as before the COVID-19 pandemic, more nurses who have to wear high protection levels of PPE are needed to complete the same tasks to prevent an excessive accumulation of fatigue and to prevent burnout in the nursing workforce.
While most medical administrators acknowledge the issue of nurses’ fatigue, we believe further research is required and administrators need to pay close attention to the degree of fatigue experienced by nurses in their employ as well as the rate at which fatigue is increasing. We suggest that medical institutions actively adopt testing mechanisms using objective indices such as HR, oral temperature, and task completion time to evaluate variations in the fatigue experienced by their nurses to enable them to take effective steps against further increase in fatigue.
We must mention certain limitations to our research. Firstly, this experiment employed the use of only three common levels of PPE protection. During the COVID-19 pandemic, there are many different levels of PPE protection, some higher than those used in our study, such as wearing a positive pressure headgear or comprehensive respiratory protection equipment. Since higher protection levels of PPE are usually applied to several special and specific situations, such as surgery, we did not include them in the scope of this study. Secondly, this study only evaluated nurses’ physical fatigue. We believe it will be necessary to carry out further studies on mental fatigue and to pay more attention to other healthcare workers in addition to nurses. Finally, although this study proposes that higher protection levels of PPE will increase the of levels of fatigue and calls for medical safety administrators to pay take cognizance of this issue, it does not provide any specific methods to reduce fatigue or its aggravating factors. This issue will be the subject matter of our future research and we hope to carry out in-depth discussions and interviews with cooperative medical institutions and be able to actively report to readers when we have further feedback.
5Conclusion
This study confirmed the influence of different protection levels of PPE on nurses’ fatigue during the COVID-19 pandemic from an experimental perspective. This study not only utilized objective indices such as HR, oral temperature variations, and task completion time but also made use of data collected through the Borg scale in respect of the participants’ subjective feeling of fatigue (subjective index). We demonstrated that the wearing of a higher protection level of PPE would lead to an increase in fatigue from a multidimensional perspective. In addition, by proposing relationship models between subjective fatigue and objective indices according to the different levels of PPE protection, we believe that the level of nurses’ fatigue can be monitored and evaluated. The results of this study not only clarify the influence of the different protection levels of PPE on nurses’ physical fatigue, but also provide a basis for medical administrators to acknowledge this issue and find ways to monitor and manage nurses’ fatigue levels, arranging nurses’ work content accordingly to improve employee satisfaction and ensure medical safety.
Ethical approval
This study followed the Declaration of Helsinki and has been approved by the ethics committee of Northeastern University, China (Reference number: NEU-EC-2021B003S).
Informed consent
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Funding
This work was supported by the National Natural Science Foundation of China (Grant nos 72171042 and 71701039) and the Fundamental Research Funds for the Central Universities (Grant no. N2106007)
Acknowledgments
This research was carried out under the support and cooperation of two medical institutions in China and has received valuable views and suggestions from experts in the medical care field. We would like to express our sincere gratitude to all experts and scholars for their help in completing this thesis. We would also like to thank Editage (www.editage.cn) for English language editing. Furthermore, we thank the editor and anonymous reviewers for their valuable comments and advice.
References
[1] | |
[2] | Danesh MK , Garosi E , Golmohamadpour H , The COVID-1pandemic and nursing challenges: A review of the early literature, Work (2021) ;69: (1):23–36. |
[3] | WHO The impact of COVID-19 on health and care workers: a closer look at deaths 2021. |
[4] | Lee E , Jang I , Nurses’ fatigue, job stress, organizational culture, and turnover intention: A culture–work–health model, Western J Nurs Res Research (2020) ;42: (2):108–16. |
[5] | Ream E , Richardson A , Fatigue: a concept analysis, Int J Nurs Stud (1996) ;33: (5):519–29. |
[6] | Maman ZS , Yazdi MAA , Cavuoto LA , Megahed FM , A data-driven approach to modeling physical fatigue in the workplace using wearable sensors, Appl Ergon. (2017) ;65: :515–29. |
[7] | Herlambang MB , Taatgen NA , Cnossen F . The role of motivation as a factor in mental fatigue, Hum Factors. (2019) ;61: (7):1171–85. |
[8] | Gifkins J , Johnston A , Loudoun R , Troth A , Fatigue and recovery in shift working nurses: A scoping literature review, Int J Nurs Stud (2020) ;112: :103710. |
[9] | Khanikosarkhizi Z , Mohammad ASR , Mehdi R , Safety climate and related factors in rehabilitation nurses of hospitals in Iran, Work (2021) ;68: (1):189–96. |
[10] | Jin H , Chen H , Munechika M , Sano M , Kajihara C , The effect of workload on nurses’ non-observance errors in medication administration processes: A cross-sectional study, Int J Nurs Pract (2018) ;24: (5):e12679. |
[11] | Knupp AM , Patterson ES , Ford JL , Zurmehly J , Patrick T , Associations among nurse fatigue, individual nurse factors, and aspects of the nursing practice environment, J Nurs Admin (2018) ;48: (12):642–8. |
[12] | Alnazly E , Khraisat OM , Al-Bashaireh AM , Bryant CL , Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers, PLOS ONE (2021) ;16: (3):e0247679. |
[13] | Ebrahimi H , Jafarjalal E , Lotfolahzadeh A , Kharghani M , The effect of workload on nurses’ quality of life with moderating perceived social support during the COVID-19 pandemic, Work (2021) ;70: (2):347–54. |
[14] | Holmér I , Protective clothing in hot environments, Ind Health (2006) ;44: :404–13. |
[15] | ISO. ISO 9886:2004 Ergonomics - Evaluation of thermal strain by physiological measurements. 2004. |
[16] | McQuerry M , Barker R , DenHartog E , Relationship between novel design modifications and heat stress relief in structural firefighters’ protective clothing, Appl Ergon (2018) ;70: , 260–8. |
[17] | McQuerry M , Den Hartog E , Barker R , Ross K , A review of garment ventilation strategies for structural firefighter protective clothing, Text Res J (2016) ;86: :727–42. |
[18] | Barker LM , Nussbaum MA , The effects of fatigue on performance in simulated nursing work, Ergonomics. (2011) ;54: (9):815–29. |
[19] | Omidi L , Moradi G , Mostofi S , Nasim , Risk of COVID-19 Infection in workplace settings and the use of personal protective equipment. Work. 2020:377-8. |
[20] | Barrero A , Cunuder AL , Carrault G , Carré F , Schnell F , Le Douairon Lahaye S , Modeling stress-recovery status through heart rate changes along a cycling grand tour, Front Neurosci-Switz (2020) ;14: :1–11. |
[21] | Chari N , Frikha M , Alibrahim M , Souissi N , Fifteen-minute warm-up best assists perception, power output and subsequent fatigue in morning high-intensity exercise among physical education students, Med Sport. (2020) ;73: (4):598–609. |
[22] | Mixter S , Mathiassen SE , Hallman D , Alternations between physical and cognitive tasks in repetitive work –effect of cognitive task difficulty on fatigue development in women, Ergonomics (2019) ;62: (8):1008–22. |
[23] | Konecný V , Brídziková M , Marienka P , Research of bus transport demand and its factors using multicriteria regression analysis, Transportation Research Procedia. (2021) ;55: :180–7. |
[24] | Wolf LD , Potter P , Sledge JA , Boxerman SB , Grayson D , Evanoff B , Describing nurses’ work: combining quantitative and qualitative analysis, Hum Factors (2006) ;48: (1):5–14. |
[25] | Min A , Min H , Hong HC , Work schedule characteristics and fatigue among rotating shift nurses in hospital setting: An integrative review, J Nurs Manage (2019) ;27: (5):884–95. |
[26] | Campbell A , Harlan T , Campbell M , Mulekar S , Wang B , Nurse’s Achilles heel: Using big data to determine workload factors that impact near misses, J Nurs Scholarshi (2021) ;53: (3):333–42. |
[27] | Westley JA , Peterson J , Fort D , Burton J , List R , Impact of nurse’s worked hours on medication administration near-miss error alerts, Chronobiol Int (2020) ;37: (9–10):1373–6. |
[28] | Shoja E , Aghamohammadi V , Bazyar H , Moghaddam HR , Nasiri K , Dashti M , Asgari A , Covid-19 effects on the workload of Iranian healthcare workers, BMC Public Health (2020) ;20: (1):1–7. |
[29] | Lucchini A , Iozzo P , Bambi S , Nursing workload in the COVID-19 era, Intens Crit Care Nur (2020) ;61: :102929. |
[30] | Serin S , Caglar B , The effect of different personal protective equipment masks on health care workers’ cardiopulmonary resuscitation performance during the Covid-19 pandemic, J Emerg Med (2020) ;60: (3):292–8. |




