The effects of nurses’ use of personal protective equipment on their vital signs during the COVID-19 pandemic
Abstract
BACKGROUND:
In order for nurses to provide the desired/expected care during the COVID-19 pandemic, the personal protective equipment (PPE) they use should not cause additional damage.
OBJECTIVE:
The current study examined the effect of nurses’ use of PPE on their vital signs during the COVID-19 pandemic.
METHODS:
The present study was executed in a public hospital located in Turkey between October 2020 and December 2020 with a total of 112 nurses, 54 of them were serving in COVID-19 clinics, and 58 of them were working in other clinics. The data of the study was collected by using the introductory information form, the vital signs measurement, and the Visual Analogue Scale. The numbers, percentages, means, standard deviation, Chi-square, ANOVA, Mann-Whitney U and Wilcoxon tests were used to analyze the data.
RESULTS:
The mean scores of SpO2, respiratory rate, body temperature, heart rate and blood pressure measurements of the nurses in the experimental group were compared before and after putting on the PPE. It was found that the difference between the two averages was statistically significant (p < 0.05).
CONCLUSION:
It was found that the use of PPE for a long time causes a decrease in SpO2, increase in respiratory rate, pulse and blood pressure, as well as the aches in face, ear, nose and head.
1Introduction
Coronavirus 2019 (COVID-19) was first identified in Wuhan, China, in December 2019, before it spread to the world. After everyone acted with the thought that nothing would happen to me, or it was too far from me in the beginning; and then an illness process was experienced, which was close to everyone, and it was not known, when they would be affected by the virus [1, 2]. The critical patients exceeded the capacity of intensive care units, operating rooms were converted into temporary intensive care units, and temporary satellite hospitals were built to direct care for non-critical patients [3].
The precautions such as social distance, use of masks, hand hygiene and working from home, which are among the social protection measures, continue to be taken. Healthcare workers do not have an alternative such as social distance and working from home, and their contact with infected patients 7/24, and their contact with contaminated surfaces cause them to be at a greater risk of virus transmission [2, 4]. In this respect, the importance of hand hygiene and the use of the personal protective equipment (PPE) in health institutions to protect against COVID-19 have increased. A number of problems have emerged in healthcare workers with long-term PPE use, such as hunger, difficulty in breathing, itching on the skin, facial redness, headaches, ear pain due to the use of N95 masks [5–7].
Nursing is defined as a profession that provides holistic and humanistic care to the physiological and psychosocial needs of the patient or healthy individuals’ existing or potential problems [8]. Today, as throughout the historical process, the nurses have been at the forefront of the fight against health-threatening epidemics worldwide, and will continue to fight on the front lines in the future [4]. In this struggle, it is important for nurses to provide holistic patient care, continuity in nursing care, shortening of hospital stay due to the pandemic, reducing mortality, reducing infection and increasing the quality of life [9]. In order for the nurses to provide the desired/expected care, they must have good working conditions, adequate nutrition and rest, and the PPE they use should not cause any harm. No study has been found in the literature that examines the effects of the PPE use on healthcare workers’ vital signs during the COVID-19 pandemic. In this respect, the current paper, which is expected to contribute to the literature, was carried out as a quasi-experimental study in order to examine the effect of PPE use by the nurses on their vital signs during the COVID-19 pandemic.
The hypotheses of the study
H0: The use of PPE does not affect the vital signs of nurses.
H1: The use of PPE affects nurses’ vital signs.
2Methods
The current research was designed using a pre-test-post-test control group quasi-experimental model.
The ethics and institution approval (Ethics Committee Number: 2020/27) were obtained from Clinical Research Ethics Committee of a university. Written informed consent was obtained from the nurses who agreed to participate after they were informed about the study.
2.1Research design
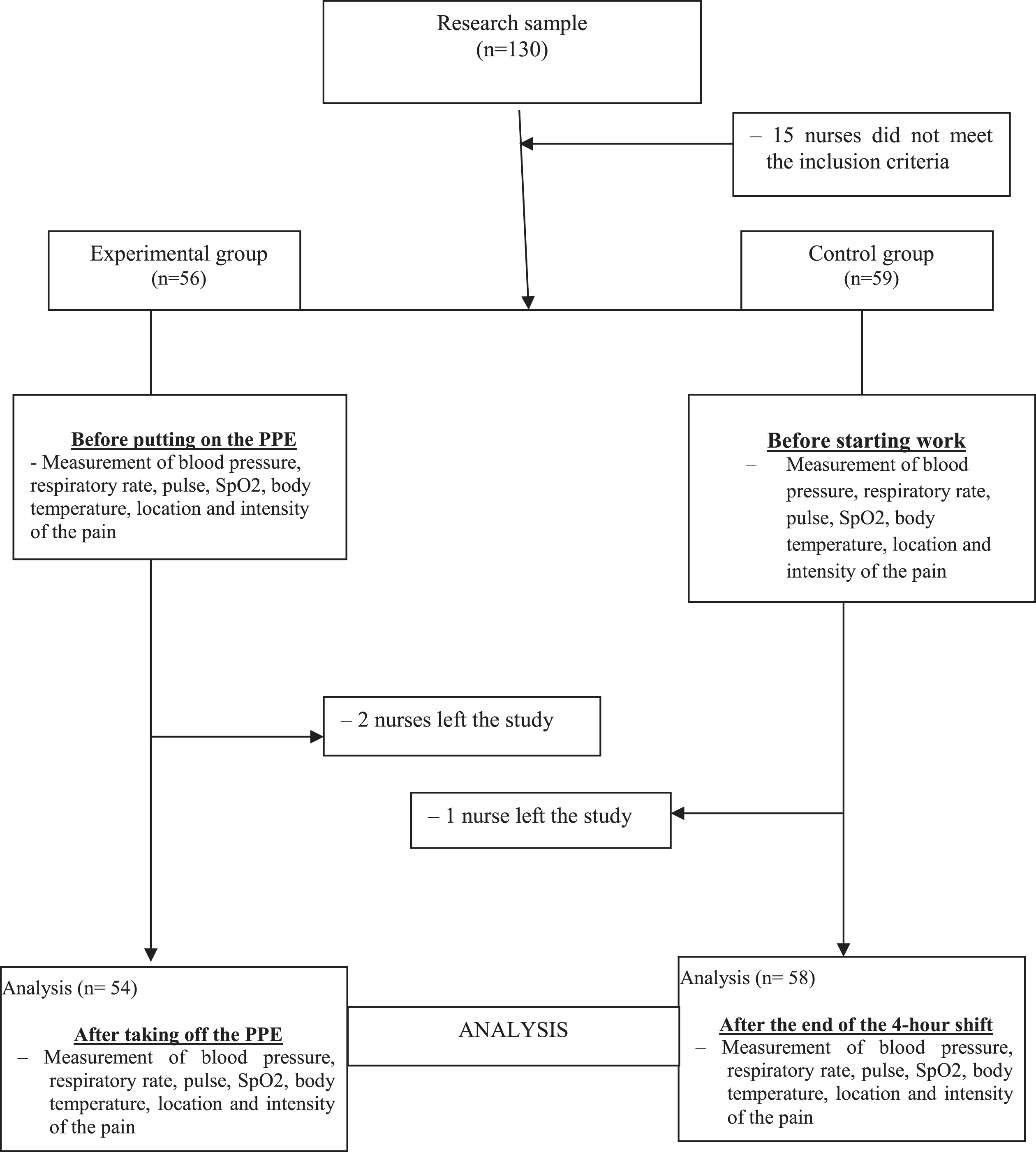
The present research was conducted in a public hospital located in Turkey between October 2020 and December 2020. The population of the study included all of the nurses in the chosen hospital. In the study, it was aimed to reach all nurses by not choosing a sample. A total of 130 nurses works in the hospital, 63 in COVID-19 clinics and 67 in other clinics. The study was conducted with a total of 112 nurses, as 15 nurses had chronic diseases and 3 nurses left the study.
Inclusion criteria for the experimental group
– Working in any of the COVID-19 clinics and using PPE,
– Does not have a chronic disease such as hypertension, diabetes, asthma, COPD,
– Volunteer to participate in the study,
– The nurses without communication problems were included in the study.
Inclusion criteria for the control group
– Working in units other than COVID-19 clinics,
– Only using masks from the PPE,
– Does not have a chronic disease such as hypertension, diabetes, asthma, COPD,
– Volunteer to participate in the study,
– The nurses without communication problems were included in the study.
2.2Data collection tools
The data were collected by measuring the introductory information form and the vital signs. The PPE used can be listed as: Medical or N95/FFP2 masks, eye or face shield, apron/overalls, cap, gloves, and disposable foot protectors/galoshes.
2.2.1The introductory information form
This form was created by the researchers. It consisted of six questions including age, gender, educational status, marital status, and the duration of employment [7, 8, 10].
2.2.2The vital signs
The vital signs form consisted of six questions evaluating the nurses’ blood pressure, pulse, SpO2, body temperature, location and severity of the pain. The blood pressure, pulse and SpO2 values were taken through the monitor. A non-contact infrared thermometer with a screen sensitivity of 0.1 degrees was used for the measurement of the body temperature. The calibrations of the devices were made regularly.
2.2.3The assessment of pain
After removing the PPE, the locations and the severity of pain, which the nurses experienced, were questioned. The Visual Analogue Scale was used. The scale was used to measure the severity of pain, was accepted in the world literature, and it was also reliable and easily applicable. The Visual Analogue Scale was used to convert the values that could not be measured numerically. It is a scale that starts with -0- “no pain”, at the other end -10- “there is very severe pain” and each cm is given numerical values at intervals of one centimeter (cm) [11].
2.3Data collection
The data were collected by the researchers between October 2020 and December 2020 by face-to-face interviews in 20–25 minutes.
The preliminary interviews were made with the nurses, who met the inclusion criteria for the study. In the pre-interview with the volunteer nurses, the work schedule was discussed and the day the study would take place was determined.
2.3.1The experimental group
The nurses working in COVID-19 clinics and wearing PPE were included in this group. The PPE included N95/FFP2 masks, eye or face shield, apron/overall, cap, gloves, and disposable foot protector/galoshes. The nurses wore protective equipment for four hours (240 minutes). Sometimes this period was exceeded (in cases such as helping friends, emergency intervention). The blood pressure, heart rate, SpO2, respiratory rate and body temperature of the nurses were measured before wearing the protective equipment. Next, after removing the PPE, the blood pressure, pulse, SpO2, respiratory rate, and body temperature of the nurses were measured again.
2.3.2The control group
The nurses working in clinics other than COVID-19 clinics and wearing only masks from the PPE were included in this group. Before starting the work, blood pressure, heart rate, SpO2, respiratory rate, and body temperature of the nurses were measured. The blood pressure, pulse, SpO2, respiratory rate and body temperature of the nurses were measured again after four hours of work.
2.4Evaluation of the research data
The statistical analysis of research data was evaluated with the SPSS for Windows 24.0 package program. To examine the normal distribution, it was found that the data were not normally distributed using the Kolmogorov Smirnov test. The number, percentage, mean, standard deviation, Chi-square, ANOVA, Mann-Whitney U and Wilcoxon tests were used to analyze the data. While interpreting the results, the significance level was taken as p < 0.05.
3Results
No statistically significant difference was found between the experimental (n = 54) and control groups (n = 58) in terms of age, gender, educational status, marital status, years of employment in the profession (p > 0.05) (Table 1) and this shows that the two groups are similar.
Table 1
Comparison of the control variables of the experimental and control groups
| Introductory characteristics | Experimental group (N = 54) | Control group (N = 58) | *Significance | ||
| Age | Number | Percentage | Number | Percentage | |
| Between 18 to 25 years | 22 | 40.7 | 17 | 29.3 | x2 = 3.162, p = 0.206 |
| Between 26 to 30 years | 18 | 33.4 | 17 | 29.3 | |
| ≥31 years | 14 | 25.9 | 24 | 41.4 | |
| Gender | |||||
| Female | 30 | 55.6 | 34 | 58.6 | x2 = 0.107, p = 0.446 |
| Male | 24 | 44.4 | 24 | 41.4 | |
| Education status | |||||
| High school/Associate degree | 26 | 48.1 | 23 | 39.7 | x2 = 0.820, p = 0.237 |
| Undergraduate/Postgraduate | 28 | 51.9 | 35 | 60.3 | |
| Marital status | |||||
| Married | 28 | 51.9 | 24 | 41.4 | x2 = 0.812, p = 0.367 |
| Single | 26 | 48.1 | 34 | 58.6 | |
| Working years in the profession | |||||
| ≤1 year | 5 | 9.3 | 5 | 8.6 | x2 = 0.858, p = 0.835 |
| Between 2 to 5 years | 24 | 44.4 | 24 | 41.4 | |
| Between 6 to 10 years | 19 | 35.2 | 19 | 32.8 | |
| ≥11 years | 6 | 11.1 | 10 | 17.2 | |
| Experimental group X±SD | Control group X±SD | ||||
| Age average (years) | 28.20±6.04 | 30.03±7.18 | **F = 1.029, p = 0.449 | ||
| Personal protective equipment wear time (minutes) | 252.77±104.47 | 240.00±00.00 | |||
*Chi-square test **ANOVA.
When the mean scores of SpO2, respiratory rate, body temperature, heart rate and blood pressure were compared between the nurses in the experimental group (n = 54) before putting on the PPE and the nurses in the control group (n = 58) before starting to work, the difference between the groups was not statistically significant (p > 0.05). In other words, p > 0.05 is similar in terms of SpO2 and vital signs of the nurses in the experimental and control groups. When the average scores of SpO2, respiratory rate, body temperature, heart rate and blood pressure were compared between the nurses in the experimental group (n = 54) after taking off the PPE and the nurses in the control group (n = 58) after the 4-hour shift, it was found that the difference between the groups was statistically significant (p < 0.05) (Table 2).
Table 2
Comparison of the average vital signs of the nurses in the experimental and control groups before and after using PPE
| Vital signs | Before putting on the PPE | Before starting work | After taking off the PPE | After the 4-hour shift | ||
| Experimental group | Control group | Experimental group | Control group | |||
|
|
| Sig.* |
|
| Sig.* | |
| SpO2 | 98.00±1.21 | 98.00±1.55 | p = 0.057 | 95.00±3.01 | 95.00±3.01 | p = 0.033 |
| Respiratory rate/minute | 16.39±1.28 | 16.25±1.31 | p = 0.258 | 18.09±2.72 | 17.42±1.95 | p = 0.001 |
| Body temperature/°C | 36.33±0.29 | 36.45±0.30 | p = 0.351 | 37.11±0.75 | 36.67±0.36 | p = 0.001 |
| Pulse/minute | 84.47±12.07 | 83.34±10.02 | p = 0.156 | 98.75±14.08 | 81.18±9.09 | p = 0.001 |
| Blood pressure (mmHg) | ||||||
| Diastole | 111.13±10.54 | 110.78±10.43 | p = 0.944 | 114.80±13.61 | 110.37±12.35 | p = 0.001 |
| Systole | 65.31±8.85 | 65.53±8.86 | p = 0.468 | 71.39±11.87 | 66.81±10.25 | p = 0.030 |
| Experimental group | Control group | |||||
| Vital signs | Before putting on the PPE | After taking off the PPE | Before starting work | After the end of the 4-hour shift | ||
|
|
| Sig.** |
|
| Sig.** | |
| SpO2 | 98.00±1.21 | 95.00±3.01 | p = 0.001 | 98.00±1.55 | 95.00±3.01 | p = 0.001 |
| Respiratory rate/minute | 16.39±1.28 | 18.09±2.72 | p = 0.001 | 16.25±1.31 | 17.42±1.95 | p = 0.001 |
| Body temperature/°C | 36.33±0.29 | 37.11±0.75 | p = 0.001 | 36.45±0.30 | 36.67±0.36 | p = 0.001 |
| Pulse/minute | 84.47±12.07 | 98.75±14.08 | p = 0.001 | 83.34±10.02 | 81.18±9.09 | p = 0.242 |
| Blood pressure (mmHg) | ||||||
| Diastole | 111.13±10.54 | 114.80±13.61 | p = 0.001 | 110.78±10.43 | 110.37±12.35 | p = 0.609 |
| Systole | 65.31±8.85 | 71.39±11.87 | p = 0.001 | 65.53±8.86 | 66.81±10.25 | p = 0.249 |
SpO2 = Oxygen saturation of the blood, *Mann-Whitney U Test, **Wilcoxon Test, p < 0.05.
When the mean scores of the nurses in the experimental group (n = 54) for SpO2, respiratory rate, body temperature, heart rate and blood pressure were compared before putting on the PPE and after taking off the PPE, it was found that the difference between the two averages was statistically significant (p < 0.05). When the SpO2, respiratory rate and body temperature measurement mean scores of the nurses in the control group (n = 58) were compared before starting to work and after the 4-hour shift, the difference between the two averages was statistically significant (p < 0.05); It was determined that the difference between the heart rate and blood pressure measurement mean scores was not statistically significant (p > 0.05) (Table 2) (In other words, p > 0.05 reveals that the nurses in the control group (n = 58) did not have different results in terms of pulse and blood pressure before they started to work - after the 4-hour shift was over).
When the head, ear, nose and face pain severity scores of the nurses in the experimental group (n = 54) after taking off the PPE and after the 4-hour shift in the control group (n = 58) were compared, it was determined that the difference between the groups was statistically significant (p < 0.05); it was also determined that the difference between the groups in terms of eye and neck pain severity scores was not statistically significant (p > 0.05) (Table 3). In other words, p > 0.05 showed that the nurses in the experimental group (n = 54) after removing PPE and in the control group (n = 58) after a 4-hour shift did not show different results in terms of eye and neck pain intensity.
Table 3
Comparison of the average pain severity and its location of the nurses in the experimental group after taking off the PPE and the nurses in the control group after the end of the 4-hour shift (n = 112)
| Location of the pain | After taking off the PPE Experimental group | After the end of the 4–hour shift Control group | |
|
|
| Significance* | |
| Head | 4.08±3.39 | 2.34±2.47 | p = 0.033 |
| Ear | 3.62±3.67 | 1.75±2.05 | p = 0.001 |
| Nose | 3.85±3.32 | 1.45±1.99 | p = 0.001 |
| Face | 2.26±2.77 | 0.89±1.75 | p = 0.001 |
| Eye | 0.50±1.99 | 0.50±1.45 | p = 0.372 |
| Neck | 0.86±2.14 | 1.00±1.95 | p = 0.839 |
*Mann-Whitney U Test, p < 0.05.
Fig. 1
The study design.
4Discussion
The use of PPE in order to protect against infection for healthcare workers is becoming more and more important every day due to the increasing number of cases caused by COVID-19 worldwide and the concerns of not knowing when the pandemic will end. After the use of PPE, some negative consequences occur in nurses. The current study examined the effect of PPE use of the nurses on their vital signs during the COVID-19 pandemic.
It was found that the nurses in the experimental group had a decrease in their SpO2 averages after taking off the PPE, and their respiratory rate, body temperature, pulse and blood pressure measurements also increased; It was found that there was a statistically significant difference between the mean scores of the vital signs before putting on the PPE and after taking off the PPE. The face masks were vital in protecting healthcare workers against COVID-19. N95 masks were 95% effective at filtering airborne particles, including very small particles. Wearing a mask for a long time causes a series of physiological and psychological burdens and can reduce work efficiency. Because face masks cover both the nose and mouth, they cause a decrease in the cooling effect of the face temperature [12, 13]. Prolonged use of N95/FFP2 masks may cause hypercapnia as a result of the insufficient ventilation and elevated carbon dioxide levels. The exhaled CO2 accumulates in the part between the mask and the face, which causes an increase in lung ventilation and respiratory activity. Hypoxemia symptoms such as chest discomfort and tachypnea are also noted in healthcare workers who use masks for a long time. Due to the accumulation of CO2 in the blood, there is an increase in respiratory rate, heart rate, body temperature, blood pressure and a decrease in SpO2 levels. At the same time, the related situation causes confusion, cognitive impairment, and disorientation [14]. When using the PPE, the body’s need for nutrients and oxygen increases due to the effort exerted during the patient care, and the heart contracts more to send extra blood to meet this need. In addition, eating, resting, full and tight bladders are other factors that affect blood pressure. Again, the increase in body temperature while wearing the PPE causes an increase in pulse rate [15]. It was determined that there was a decrease in the SpO2 averages of the nurses in the control group before they started to work and after the 4-hour shift, and a significant increase in their respiratory rate and body temperature measurement averages. It was observed that the nurses in the control group wore medical masks and their respiratory rate, body temperature and SpO2 values were negatively affected by their vital signs during the 4-hour shift. The face masks increase perspiration and warmth in the perioral area. Wearing the face masks for a long time causes a decrease in heat loss from the body through various mechanisms such as conduction, convection, evaporation and radiation [16]. In the studies conducted in the literature, it has been determined that healthcare workers have difficulty in breathing with effort while wearing the face masks [8, 12, 17]. Due to long-term wearing of apron/overalls, foot protectors/galoshes, bonnets, an increase in body temperature develops, and because of the elevated heat of the body, sweating occurs.
There was no statistically significant difference between the mean scores of SpO2, respiratory rate, body temperature, heart rate and blood pressure measurements of the nurses in the experimental group before putting on the PPE and the nurses in the control group before starting to work. However, a significant difference was found between the mean scores of SpO2, respiratory rate, body temperature, heart rate and blood pressure measurements of the nurses in the experimental group after taking off the PPE and after the 4-hour shift of the nurses in the control group. This result shows that the use of PPE causes significant changes in SpO2, respiratory rate, body temperature, pulse and blood pressure. This result supports the H1 hypothesis that the use of PPE affects the vital signs of nurses.
It was found that pain in the head, ear, nose, face, eyes and neck due to the use of PPE were observed in both groups. Human skin is the first defense barrier against physical, mechanical and chemical factors. Long-term PPE use adversely affects the skin due to continuous pressure, friction, and moisture [18]. In the literature, the use of PPE causes redness and pain in the nasal bone, cheekbones, forehead, chin, ears and behind the ears where it contacts the skin [10, 18–20]. there are also studies reporting that long-term PPE use caused headaches [8]. It was determined that there was a statistically significant difference between the average points of pain severity in the head, ear, nose and face of the nurses in the experimental group after taking off the PPE and in the control group after the 4-hour shift. After taking off the PPE, the nurses in the experimental group had higher average points of pain in the head, ear, nose and face compared to the control group.
The nurses working in COVID-19 clinics had further use and duration of the PPE than the nurses working in other clinics. The nurses working in other clinics wore only masks or additional face shields, and they could periodically reduce the pressure on the skin. It should be noted that face shields and glasses reduce visual acuity and are suitable for head-neck anatomy [21]. In a study, it has been revealed that as the duration of PPE usage increases, serious damage is caused to the face, ears and back of the ears [19]. The studies in the literature indicated that healthcare workers had headache complaints due to the use of N95 masks [6, 7, 22]. The use of tight masks/glasses puts pressure on the face and cervical nerves and as a result, headache develops [6]. In addition, long-term use of masks caused irregular meal times, hydration and headaches due to stress [7]. The findings of this study are in line with the related literature.
5Conclusion
In the current study, it was concluded that using the PPE negatively affected the vital signs of nurses. This result is striking. It has been determined that the nurses working in COVID-19 clinics have been much more negatively affected by the use of PPE than the nurses working in other clinics. Long-term use of the PPE was found to cause a drop in SpO2, increased respiratory rate, heart rate and blood pressure, as well as the aches in face, ear, nose and head.
The pandemic still continues in the world, and it is predicted to continue in the future. In this respect, it is imperative for nurses to continue using the PPE to protect their health. In order to reduce the negative effects of PPE, short shifts, not to miss meal times, ensuring hydration, taking rest breaks, nurse changes (if possible) in case of hyperventilation, loosening the PPE at intervals to reduce the pressure on the skin, and in long-term use of the PPE, choosing a mask suitable for the face, and using tape to avoid the PPE injuries are recommended.
5.1Limitations
The present study has revealed important results in terms of changes in the vital signs of nurses who work at the forefront of the COVID-19 pandemic. Although the study has its strengths, it also has limitations. The nurses with high body mass index were not evaluated and their sleep quality, stress levels, physical activities, nutrition and smoking status were not included in the current study. These factors affect vital signs as well.
Acknowledgment
The authors are grateful to all individuals who participated in the study.
Author contributions
Study design: AD, FK, LY; Manuscript writing: AD, FK; Data collection: AD, FK, LY; Data analysis: FK; Study supervision: AD, FK; Critical revisions for important intellectual content: AD, FK.
Funding
During the present study, no financial support was received from institutions or organizations.
Conflict of interest
There is no conflict of interest between the authors and/or family members regarding this study.
References
[1] | Huang C , Wang Y , Li X , Ren L , Zhao J , Hu Y , Zhang L , Fan G , Xu J , Gu X , Cheng Z , Yu T , Xia J , Wei Y , Wu W , Xie X , Yin W , Li H , Liu M , Xiao Y , Gao H , Guo L , Xie J , Wang G , Jiang R , Gao Z , Jin Q , Wang J , Cao B . Clinical features of patients infected with novel coronavirus in Wuhan, China. The Lancet. (2020) ;395: (10223):497–506. |
[2] | Organization WH. Rational use of personal protective equipment for coronavirus disease (COVID-19) : interim guidance, 27 February 2020. World Health Organization; 2020. |
[3] | Baker HA , Safavynia SA , Evered LA . The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors. British Journal of Anaesthesia. (2021) ;126: (1):44–7. |
[4] | Karasu F , Öztürk Ç . E. ,“An ıntensive care nurse inthe forefront of the epidemic while increasing cases ofCovid“heroes in front-lıne”. Journal of Critical CareNurses. (2020) ;24: (1):11–4. |
[5] | Foo CCI , Goon ATJ , Leow YH , Goh CL . Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome–a descriptive study in Singapore. Contact Dermatitis. (2006) ;55: (5):291–4. |
[6] | Lim E , Seet R , Lee KH , Wilder-Smith E , Chuah B , Ong B . Headaches and the N95 face-mask amongst healthcare providers. Acta Neurologica Scandinavica. (2006) ;113: (3):199–202. |
[7] | Ong JJY , Bharatendu C , Goh Y , Tang JZY , Sooi KWX , Tan YL , Tan BYQ , Teoh HL , Ong ST , Allen DM , Sharma VK . Headaches associated with personal protective equipment–A cross-sectional study among frontline healthcare workers during COVID-19. Headache: The Journal of Head and Face Pain. (2020) ;60: (5):864–77. |
[8] | Atay S , Cura ŞÜ . Problems encountered by nurses due to the use of personal protective equipment during the coronavirus pandemic: results of a survey. Wound Management & Prevention. (2020) ;66: (10):12–6. |
[9] | Karasu F , Doğan A . COVID -19 Patient and Nursing Care: CaseReport. Van Sağlık Bilimleri Dergisi 13: (COVID-19Supplement):53–8. |
[10] | Yan Y , Chen H , Chen L , Cheng B , Diao P , Dong L , Gao X , Gu H , He L , Ji C , Jin H , Lai W , Lei T , Li L , Li L , Li R , Liu D , Liu W , Lu Q , Shi Y , Song J , Tao J , Wang B , Wang G , Wu Y , Xiang L , Xie J , Xu J , Yao Z , Zhang F , Zhang J , Zhong S , Li H , Li H . Consensus of Chinese expertson protection of skin and mucous membrane barrier for health-careworkers fighting against coronavirus disease 2019. Dermatol Therapy. (2020) ;33: (4):e13310. |
[11] | Kane RL , Bershadsky B , Rockwood T , Saleh K , Islam NC . Visual AnalogScale pain reporting was standardized. Journal of Clinical Epidemiology. (2005) ;58: (6):618–23. |
[12] | Rosner E . Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. (2020) ;6: (3):130. |
[13] | DuBois A , Harb Z , Fox S . Thermal discomfort of respiratory protective devices. American Industrial Hygiene Association Journal. (1990) ;51: (10):550–4. |
[14] | Johnson AT . Respirator masks protect health but impact performance: a review. Journal of Biological Engineering. (2016) ;10: (1):1–12. |
[15] | Guyton AC , Hall JE . GüneşTıp Kitabevleri; 2017. |
[16] | Wang L , Yin H , Di Y , Liu Y , Liu J . Human local and total heat losses in different temperature. Physiology & Behavior. (2016) ;157: :270–6. |
[17] | Purushothaman P , Priyangha E , Vaidhyswaran R . Effects of prolonged use of facemask on healthcare workers in tertiary care hospital during COVID-19 pandemic. Indian Journal of Otolaryngology and Head & Neck Surgery. (2021) ;73: (1):59–65. |
[18] | Zhou N-Y , Yang L , Dong L-Y , Li Y , An X-J , Yang J , et al. Prevention and treatment of skin damage caused by personal protective equipment: experience of the first-line clinicians treating 2019-nCoV infection. International Journal of Dermatology and Venereology. 2020. |
[19] | Lan J , Song Z , Miao X , Li H , Li Y , Dong L , Yang J , An X , Zhang Y , Yang L , Zhou N , Yang L , Li J , Cao J , Wang J , Tao J . Skin damage among health care workers managing coronavirus disease-2019. Journal of the American Academy of Dermatology. (2020) ;82: (5):1215–6. |
[20] | Schwartz D , Magen YK , Levy A , Gefen A . Effects of humidity on skin friction against medical textiles as related to prevention of pressure injuries. International Wound Journal. (2018) ;15: (6):866–74. |
[21] | de Oliveira E Silva AC , Nogueira WP , Gir E , de Almeida SA , de Lima Barroso BI , Freire MEM . ‘Limiting Factors of Face Shield Use for Health Professionals During the COVID-19 Pandemic’. Work. 2021;1-9. |
[22] | Rebmann T , Carrico R , Wang J . Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. American Journal of Infection Control. (2013) ;41: (12):1218–23. |




