Outcomes of an interdisciplinary return to work intervention including occupational therapy for mood and adjustment disorders: A single-arm clinical trial
Abstract
BACKGROUND:
Mood and adjustment disorders are two major causes of long-term sick leave among employees, leading to large social losses. Therefore, a return to work (RTW) intervention was attempted, targeting patients with mood and adjustment disorders.
OBJECTIVE:
This study aimed to investigate the outcome of an interdisciplinary RTW intervention including occupational therapy implemented within the Japanese healthcare framework.
METHODS:
An interdisciplinary RTW intervention including occupational therapy was conducted five times a week for approximately three months, targeting individuals with mood and adjustment disorders who took a leave of absence. Their mental symptoms, cognitive functioning, job performance, temperament, social adaptation, psychosocial state, and readiness to RTW before and after the intervention were evaluated. Full-time RTW ratios at 3, 6, 12, 18, and 24 months from baseline were followed up and compared with those of prior studies.
RESULTS:
A total of 30 individuals completed the intervention. After the intervention, participants’ psychological symptoms, cognitive function, vocational aptitude, temperament, social adaptation, psychosocial state, and readiness to RTW improved (p≤0.001–0.0279). The ratios of RTW at 3, 6, 12, 18, and 24 months from the baseline were 6.7%, 46.7%, 73.3%, 77.8%, and 82.6%, respectively, reflecting a higher pattern than prior reports.
CONCLUSIONS:
The interdisciplinary RTW intervention including occupational therapy has the potential to improve not only depressive symptoms but also cognitive functioning, job performance, social adaptation, and readiness to RTW. They can also raise RTW ratios.
1Introduction
Mood disorders, including unipolar depression and bipolar disorder, encompass conditions in which individuals experience an extreme in the continuum of typical moods— from a low, sad, unpleasant mood to the elevated, elated, energized mood of mania [1]. Adjustment disorders are a psychological response to an identifiable stressor or stressors that result in the development of clinically significant emotional or behavioral symptoms [2]. These are major causes of long-term sick leave in the workforce worldwide [3, 4]. Even if symptoms are alleviated and individuals return to work (RTW), they are highly likely to take additional sick leave [5, 6]. These disorders cause a loss of work productivity, incurring huge losses for corporations [7, 8]. Socioeconomic losses incurred due to mental health conditions of employees are predicted to increase from USD 2.5 trillion in 2010 to USD 6.0 trillion by 2030, and two-thirds of this amount appears to be indirect costs attributable to sick leave and reduced productivity, as opposed to direct costs spent on healthcare or treatment [9]. It is critical to protect the employment and employment opportunities of individuals with mood and adjustment disorders from a socioeconomic cost perspective [9].
Reports on interventions aimed at RTW of employees who had taken sick leave due to mood and adjustment disorders began to be published after 2000. In a meta-analysis that investigated the effects of interventions to promote the RTW of patients with mood and adjustment disorders, work-focused interventions were seen as a viable option to reduce the number of absent days due to sickness and depressive symptoms, as well as enhance productivity, more than with ordinary treatment [10–12].
A few reports on work-focused interventions explored occupational therapy combined with standard treatment; they verified the effects of alleviated symptoms of depression by means of randomized controlled trials (RCTs). Some reports showed a greater likelihood of long-term remission of symptoms, long-term improvement of RTW, and reduced work-loss days than achieved by standard treatment alone [13, 14]. Interventions carried out in this case, which included occupational therapy, were composed of group sessions and individual sessions performed by occupational therapists. In the individual sessions, the therapist first interviewed the patient regarding disease history. Next, the therapist observed the patient’s work simulation scenes through a video feed. They also contacted occupational physicians to identify the patient’s workplace status and problem areas. In the subsequent weekly group sessions, the patient was asked to assess their own workplace environments in the course of discussing topics such as workload, autonomy, relationships at work, job perspective, and work-home interference models. In the individual sessions conducted in parallel, the patients were encouraged to associate workplace stress with an inability to cope. In individual sessions centered on workplace meetings, the occupational therapists proposed that employers adjust the workplace environment to better suit the patients (employees). The key characteristic of this intervention is that the patient had been working at their workplace for two hours per week during the intervention period, based on the “place-and-train” model. Therefore, the occupational therapists made frequent contact with both the occupational physicians and the primary physicians [13].
Although the participants are slightly different, Individual Placement and Support (IPS) is a vocational rehabilitation program for people with severe mental illness [15]. A meta-analysis found that IPS showed a better vocational outcome compared with usual treatment conditions [16]. Eligibility based on client choice, focus on competitive employment, integration of mental health and employment services, attention to client preferences, work incentive planning, rapid job search, systematic job development, and individualized job support are the eight principles of IPS. These are also extremely important perspectives in the RTW interventions for individuals with mood and adjustment disorders [17].
In Japan, Akiyama [18] formulated the first-ever RTW assistance program specifically tailored to individuals who took sick leave because of depression. In 2018, a RTW program (called Re-Work program in Japan) was implemented at 220 medical establishments in Japan [19]. In a retrospective cohort study, in which multiple facilities participated, RTW programs were reported to have resulted in a significantly larger number of continuous working days after returning to work as opposed to standard treatment, which included only regular outpatient practices and medication by psychiatrists [20]. However, only 63.6% –77.2% of the employees who participated in the Re-Work program returned to work [21] and approximately 70% continued to work two years later [20], suggesting that the increase in the RTW ratios and a stable continuation of work after return are the main challenges faced by employers. The content of the Re-Work program includes individual work, group work, psychoeducation, cognitive behavioral therapy (CBT), assertiveness training and/or social skills training, and reflection on the process of illness onset [22]. The Re-Work program is carried out by the interdisciplinary team [19]. However, of the various healthcare services either inside or outside Japan, no RTW interventions employing occupational therapy have been reported.
Occupational therapy is a client-centered health profession concerned with promoting health and well-being through occupation. The primary goal of occupational therapy is to enable people to participate in the activities of everyday life [23]. Occupational therapists are increasingly working to expand work opportunities for people with mental health issues [24, 25]. As engagement in meaningful occupations, such as work, affects health and well-being, the occupational therapist needs to approach people’s work [26].
This study aimed to investigate the short- and long-term outcomes of an interdisciplinary RTW intervention including occupational therapy. Investigating the outcomes of the intervention increases the contribution of occupational therapy to people who take sick leave because of mood and/or adjustment disorders. This is the first study on an interdisciplinary RTW intervention using occupational therapy for people with mood and adjustment disorders in Japanese healthcare services.
2Method
2.1Participants
In this study, we selected patients who had either been hospitalized in or received outpatient treatment at Shinshu University Hospital’s Department of Psychiatry between April 2014 and April 2020 as participants. Those aged 20–60 years, who had been diagnosed with mood or adjustment disorders (according to the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition Text Revision (DSM-IV-TR) [1]) and those who had agreed to participate in the study were selected. The participants were required to be on sick leave at the time of providing their consent and had to have the intention of returning to work. Those who had left their jobs were required to be willing to be re-employed. Participants were recruited only if they had over 80% attendance rate in occupational therapy (2–3 hours/day, 5 days/week) conducted during the past month (because the average number of working days for Japanese people is five days a week [27], it was judged that participants were ready to be introduced into the RTW intervention by participating in occupational therapy, which is a pre-intervention, four days a week), and an average score of over 2.0 points in the Psychiatric Rework Readiness Scale (to be described later). We excluded patients with complications such as schizophrenia, intellectual disability, alcohol and drug dependence (substance abuse and dependence), dementia, epilepsy, head trauma, and cerebrovascular disorders and those who found it difficult to perform various tests. All participants received thorough explanations of the objectives of the study and provided their written consent based on their own free will to participate. This study was a single-arm longitudinal observational study.
Figure 1 illustrates the flow of the study. Forty-three participants signed up for the study during the study period. Of these, nine were excluded as they failed to meet the eligibility criteria. Therefore, a final group of 34 people were considered for the study. Four dropped out mid-way through the program (dropout ratio: 11.8%), and 30 people ultimately completed the RTW intervention (completion rate: 88.2%). Of the four people who dropped out, one was a female patient with depression in her 30 s. She wished to return to work early and did so mid-way through the intervention. Two males (patients with bipolar disorder in their 40 s and 50 s) discontinued the intervention as their condition deteriorated. The primary physician of another male patient with bipolar disorder in his 50 s recommended discontinuation of the study because of problematic behaviors during the group sessions. The number of participants whose progress could be tracked during the follow-up period was 30 for between 3–12 months; 27 for beyond 18 months; and 23 for beyond 24 months.
Fig .1
Study flowchart.
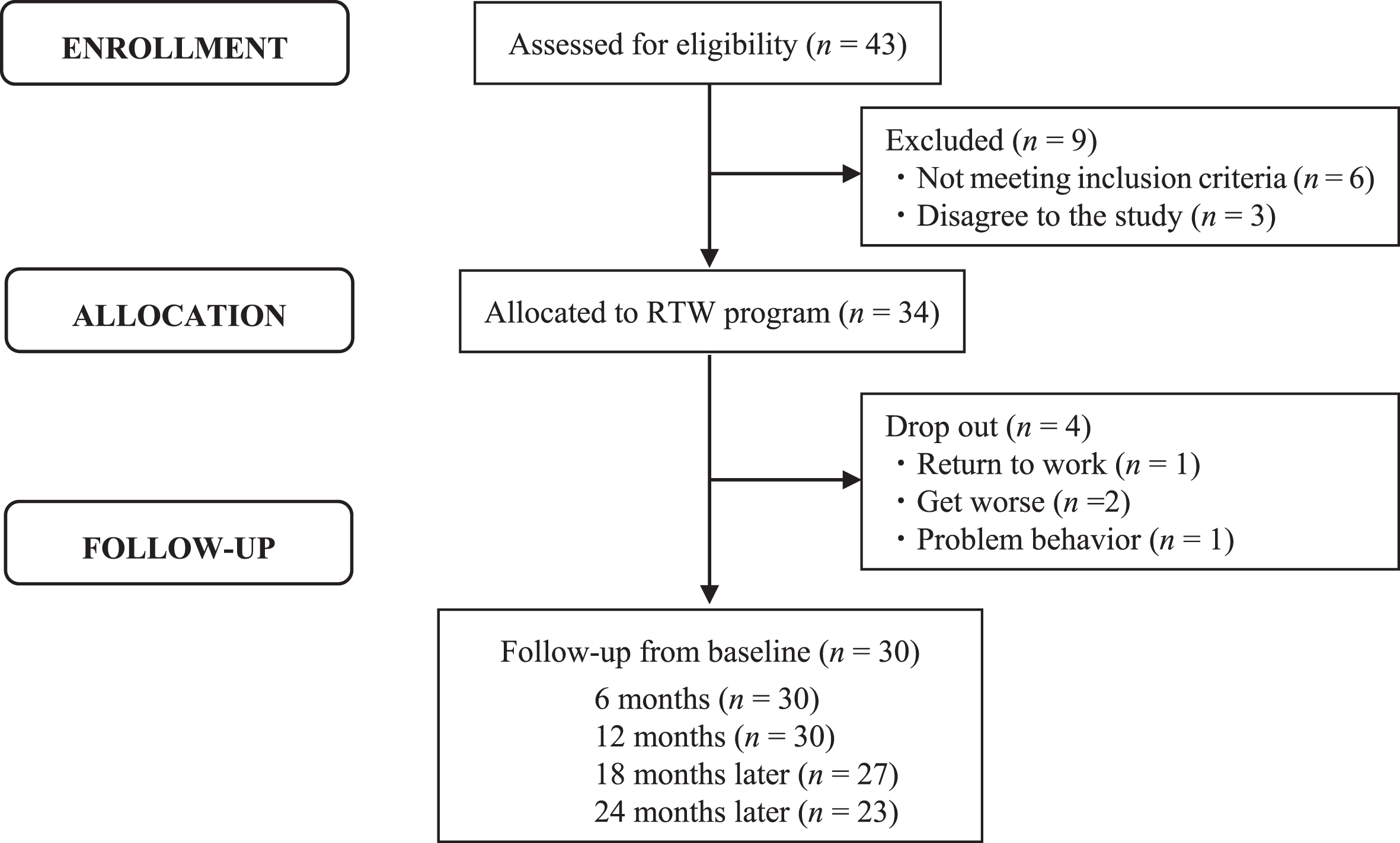
Table 1 shows the demographic data of the 30 participants who completed the RTW intervention. The average age of the participants was 37.1 years; their average number of sick leave was 2.2; and their total past sick leave period was 13.1 months. Eight participants were diagnosed with major depressive disorder, six with bipolar disorder, and 16 with adjustment disorders. The participants who were diagnosed by psychiatrists with attention-deficit/hyperactivity disorder or pervasive developmental disorder (including “not otherwise specified”) based on the DSM-IV diagnostic criteria were also included. The average duration of the intervention was 123.9 days. In terms of educational history, 10 had studied for 12–13 years and 11 for 14–16 years. Twelve participants were married. In terms of occupation, there were 13 engineers, 5 office workers, 4 sales workers, and 3 workers in management departments. By designation, all participants worked full-time and the sample included three directors or managers and six section managers or chiefs (Table 1).
Table 1
Demographic information of participants (n = 30)
| Variable | N | % | Mean | SD |
| Gender(male/female) | 25/5 | |||
| Age (years) | 37.1 | 8.7 | ||
| Sick leave period (months) | 13.1 | 7.46 | ||
| Number of sick leave (times) | 2.17 | 1.84 | ||
| Diagnosis | ||||
| Major depressive disorder | 8 | 26.7 | ||
| Bipolar disorder | 6 | 20.0 | ||
| Adjustment disorder | 16 | 53.3 | ||
| RTW program period (days) | 123.9 | 65.4 | ||
| Number of RTW program courses (times) | 1.2 | 0.5 | ||
| Education | ||||
| ≤12years | 3 | 10.0 | ||
| 12 years<, ≤13 years | 10 | 33.3 | ||
| 14 years≤, ≤16 years | 11 | 36.7 | ||
| >17 years | 6 | 20.0 | ||
| Marital status (married) | 12 | 40.0 | ||
| Occupation | ||||
| Engineer | 13 | 43.3 | ||
| Office worker | 5 | 16.7 | ||
| Sales representative | 4 | 13.3 | ||
| Managing department | 3 | 10.0 | ||
| Profession | 1 | 3.3 | ||
| Production line | 1 | 3.3 | ||
| Service business | 1 | 3.3 | ||
| Researcher | 1 | 3.3 | ||
| Other | 1 | 3.3 | ||
| Work position | ||||
| Director or Manager | 3 | 10.0 | ||
| Chief | 6 | 20.0 | ||
| Other | 21 | 70.0 |
2.2Interdisciplinary RTW intervention including occupational therapy
The interdisciplinary RTW intervention comprised a full-day program conducted thrice a week and a half-day program conducted twice a week. It was set up as a single cycle and implemented for a period of approximately three months. The group sessions and individual sessions were instructed and supervised by occupational therapists with more than 20 years of experience.
Group sessions were held four times a week, with each session lasting 1.5–2 hours. Each group session included two to eight participants. A learning program (Table 2) was implemented twice a week for a total of 22 modules. The program included psychoeducation, CBT, interpersonal and social rhythm therapy, assertiveness training, and anger management units that were based on illness management and recovery; the program also utilized an evidence-based practice toolkit [28]. We performed a 1.5-hour metacognitive training for depression (D-MCT) [29] once a week for eight times to make participants aware of non-functional thought patterns and rectify them. Moreover, as training for interpersonal exchanges, to share various roles and work together with other participants, an array of approximately two-hour group activity programs were carried out once a week, such as cooking, sports activities, team competitions, challenges, and planning and operation of events. Many of the programs were conducted by occupational therapists. Clinical psychologists were in charge of the CBT and Assertiveness Communication modules, psychiatric social workers were in charge of the Building Social Support modules, and pharmacists were in charge of the Using Medication Effectively modules of the learning program. These group sessions corresponded to the RTW program’s group work, psychoeducation, CBT, assertiveness training, and/or social skills training held in Japan. In these sessions, participants were encouraged to gain basic knowledge of the disorder, treatment, and recurrence prevention. They were also encouraged to acknowledge the deviation in their recognition of the self within the group as well as their behavioral patterns and to expand their sense of value as an individual.
Table 2
Study program
| Topics | Number of sessions | Person in charge |
| Orientation | 1 | Occupational therapist |
| Recovery strategies | 3 | Occupational therapist |
| Social rhythm therapy | 1 | Occupational therapist |
| Building social support | 1 | Social worker |
| Practical facts about depression and bipolar disorder | 1 | Occupational therapist |
| Cognitive behavioral therapy | 2 | Psychologist |
| Interpersonal therapy | 1 | Occupational therapist |
| Using medication effectively | 1 | Pharmacist |
| Anger management | 2 | Occupational therapist |
| Stress-Vulnerability Model and treatment strategies | 1 | Occupational therapist |
| Coping with stress | 2 | Occupational therapist |
| Assertive communication | 2 | Psychologist |
| Reducing relapses | 2 | Occupational therapist |
| Achievement presentation | 1 | All |
| Summary | 1 | Occupational therapist |
In the individual sessions, held five times a week for two to three hours each, the occupational therapists carried out individual support plans drawn up together with the participants according to the following seven processes: intake interview, assessment, extraction of problems to be solved, planning, execution, monitoring, and plan revision. In the intake interview, the occupational therapist listens to the goals of the participants and their families. In the subsequent assessment, the occupational therapist collects basic information (medical and occupational information, the results of various tests) to analyze the International Classification of Functioning, Disability and Health (ICF) [30]. In the ICF analysis, the occupational therapist evaluates the degree of disability for each ICF code related to RTW. (e.g., body functions such as b122 global psychosocial functions, b126 temperament and personality functions, b130 energy and drive functions, and activity and participation such as d220 undertaking multiple tasks, d240 handling stress and other psychological demands, and d720 complex interpersonal interactions are evaluated as one of “no problem,” “mild problem,” “moderate problem,” “severe problem,” or “complete problem.” Environmental factors such as e310 immediate family; e325 acquaintances, peers, colleagues, neighbors and community members; and e330 people in positions of authority were evaluated as facilitators or barriers using a 0–4 scale [30].) Then, the occupational therapist predicts the prognosis, after considering the relationship between these codes judged to be a problem of “moderate” or higher and their leave absence, agrees on goals with the patient and his/her family. In the extraction of problems to be solved, the occupational therapist prioritizes the participants’ tasks and analyzes the root cause. At this stage, occupational therapists identify factors that induce the participants’ leave of absence according to the functioning level, activity and participation level, and environment level. Furthermore, the occupational therapists also identify individual strengths and non-effective coping patterns in stressful situations (e.g., some participants believed that it was embarrassing to ask people what they do not understand and had a non-effective coping pattern of dealing with stressful situations without the help of others). In planning, occupational therapists develop an individual support plan and develop plans suited to each of the functioning levels, activity and participation levels, and environment levels. For the functioning level, the participants were offered additional individual CBT that corrects cognitive bias, such as rushing to conclusions or assigning the cause of failure to others. As a method of training to either enhance or maintain the necessary work performance skills, they received tasks using constitutive craftwork and computers. For the activity and participation levels, participants were encouraged to incorporate activities that they could eagerly tackle in their daily lives, check the balance between activity and rest, practice interpersonal relationships with the therapists, and carry out health management in their daily lives. For the environmental level, since the occupational performance of a person is greatly affected by the interaction between the environment and the person, we adjusted the environment in the workplace [1]. Additionally, adjustment of the participants’ workplace environment and family guidance were also carried out.
In addition to the aforementioned learning program and D-MCT’s homework tasks, the support plan included the formulation of a plan to prevent recurrent sick leave. This entailed the participants themselves looking back on the chronology of events that led to the taking of such leave, exploring their own tasks and challenges from both environmental and personal factors, and formulating concrete plans for preventing recurrent sick leave. These individual sessions were conducted by two mid-level occupational therapists.
Upon completion of the intervention, members of the RTW team comprising a psychiatrist, clinical psychologists, psychiatric social workers, a pharmacist, and occupational therapists discussed the pros and cons of the participants’ application for RTW. For participants who were judged capable of returning to work, the RTW team’s occupational therapist and psychiatric social worker held a support meeting with the participant and the person-in-charge at their workplace and adjusted the workplace environment based on the plan to prevent recurrent sick leave. Participants who were judged not to be fully ready to RTW were encouraged to rejoin the RTW intervention.
Generally, in Japan, the above group sessions are conducted as a RTW intervention. In our intervention, personalized individual sessions based on an occupational therapy perspective accounted for more than half of the program, and the workplace environment was actively adjusted based on the support plan.
2.3Outcome measures
To assess mental symptoms, we employed the Hamilton Rating Scale for Depression (HRSD) [31] and the Young Mania Rating Scale (YMRS) [32]. The HRSD is used to assess the severity of depression. It comprises 21 items, consisting of 17 items related to the severity of depressive symptoms and 4 items related to temperament and personality. A score of less than 7 points was considered an indication of remission of symptoms. The YMRS, comprising 11 items, is designed to assess the severity of manic symptoms. The higher the score, the more severe the symptoms. A score of 13 points or lower is considered indicative of remission of symptoms. Assessment of the HRSD and YMRS was performed by clinical psychologists, and that of other scales was performed by occupational therapists.
The Brief Assessment of Cognition in Schizophrenia (BACS) was used to assess cognitive function. It is a scale that enables quick and simple measurement of cognitive impairment in schizophrenia. Moreover, it also assesses the cognitive function of patients with mood disorders [33]. The Japanese edition of the BACS was developed by Kaneda [34], and its reliability and validity were confirmed. The BACS is composed of six subscales that measure verbal memory, working memory, motor speed, attention and speed of information processing, verbal fluency, and executive function. The higher the standardization score (z-score), the higher the cognitive function. The average of the six subscales’ z-scores was calculated as a composite score.
The General Aptitude Test Battery (GATB) was used to assess job performance. The Japanese version of the GATB was drawn up by the Ministry of Health, Labour, and Welfare [35]. The scale uses 12 kinds of tests to measure nine abilities or aptitudes (i.e., general intelligence, verbal aptitude, numerical aptitude, clerical perception, spatial aptitude, form perception, motor coordination, finger dexterity, and manual dexterity). The higher the scores, the higher the job performance.
A participant’s temperament was assessed using the Temperament Evaluation of Memphis, Pisa, Paris, and San-Diego-Autoquestionnaire (TEMPS-A), a self-administered scale of 110 items that measures depressive temperament, cyclothymic temperament, hyperthymic temperament, irritable temperament, and anxious temperament. A high or low score reflects a corresponding temperament level. The reliability and validity of the Japanese language edition was confirmed by Matsumoto et al. [36].
The status of social adaptation was measured using the Social Adaptation Self-evaluation Scale (SASS), a self-administered scale developed by Bosc et al. (1997) to measure the social adaptation of patients with depression. It comprises 20 questions that measure three factors: interpersonal relations, interest and curiosity, and awareness of the self. The higher the total score, the more favorable the social adaptation. The Japanese edition of the scale was developed by Ueda et al. [37] and the reliability and validity of the method were confirmed. The average score of general healthy participants was 36.1 points. The cutoff point (which indicated the score above which a patient will be able to work) for both the working and the non-working group was determined to be 25 out of 26 [37], and the cutoff point that predicted continuation of work one year later was determined to be 30 out of 31 [38].
The overall function was assessed using the Global Assessment of Functioning (GAF) [39] that comprehensively assesses mental and social functions. Its scale ranges from 0–100 points; the higher the score, the higher the overall function.
Participants’ readiness to RTW was assessed using the Psychiatric Rework Readiness Scale (PRRS) [40]. From their conditions during the past two weeks, participants were assessed on their basic living conditions (three items), symptoms (six items), basic sociability (two items), support status (two items), relationship with the workplace (two items), matters related to work skills/performance and operations (three items), state of preparation (two items), and status of health management (three items). A total of 23 assessment items were evaluated based on information from the participants themselves, according to a score ranging from 1–4. The total score of PRRS is suitable for predicting the duration of continuous employment of depressive patients. The cutoff point that predicts employment status six months after returning to work is 64 out of 65 points [41]. The Japanese Association of Rework for Depression recommends that the criteria of enabling participation in the RTW program is scoring an average total PRRS score of 2.0 points or more and permitting an application for RTW with an average total score of 3.0 or more points. Participants were tested by an occupational therapist.
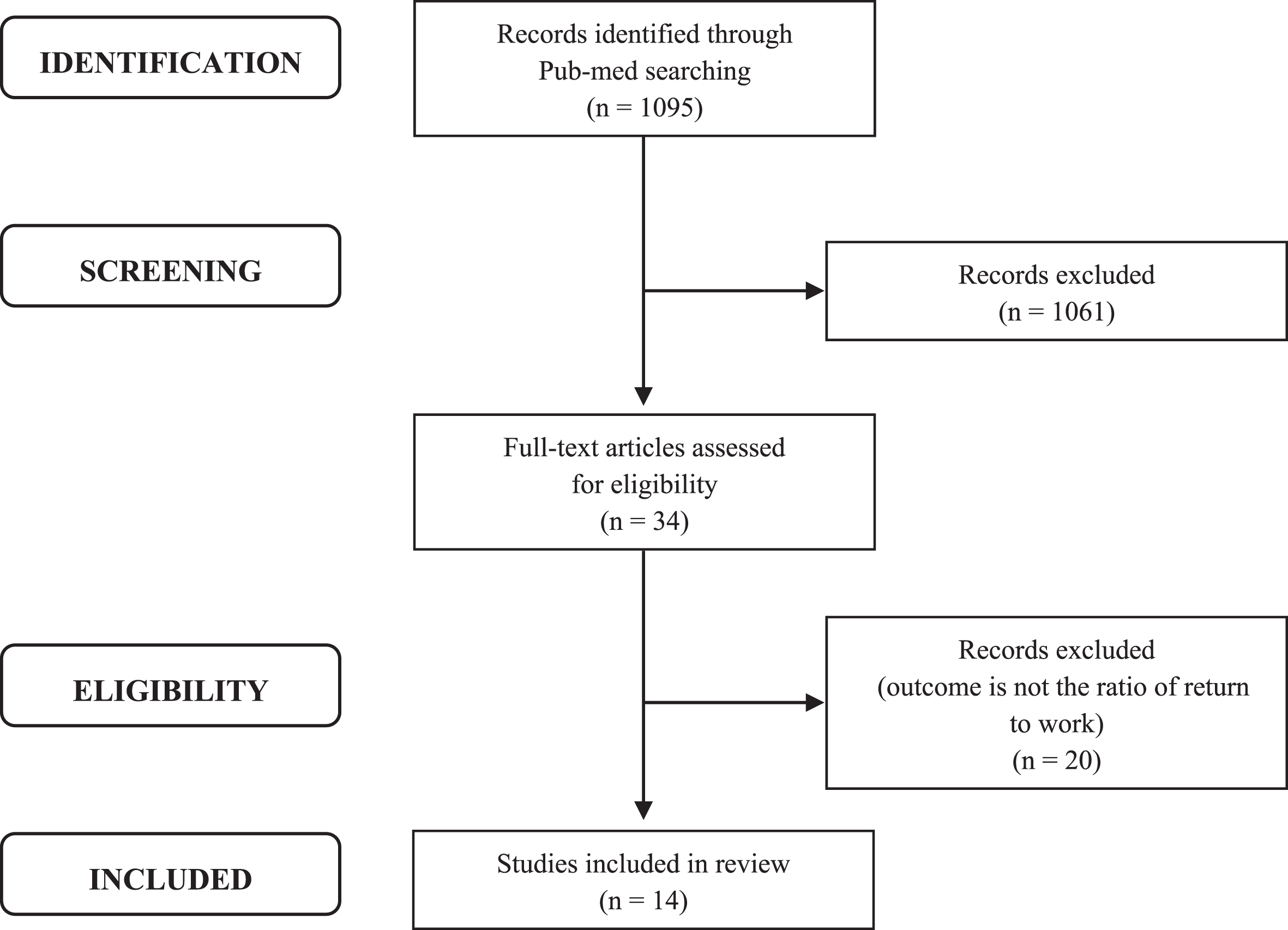
As an indicator of the long-term outcome of this program, the full-time RTW ratio was investigated at 3, 6, 12, 18, and 24 months from the baseline. Since the weekly working hours per Japanese worker in 2020 was listed at seven hours and 46 minutes [27], working eight hours a day and more than four times a week (32 hours/week) was designated “Full RTW,” and any work below this level was counted as “Non-working.” The RTW ratio thus calculated was compared with the working ratio reported in previous research (not statistical analysis). Previous research conducted literature searches in PubMed using keywords like “depression,” “common mental disorders,” and “return to work.” From the titles and abstracts of the papers found, we extracted papers that focused on common mental disorders, such as mood disorders, anxiety disorders, and adjustment disorders, and searched for intervention studies focusing on RTW. We read the entire text of the research papers that met the criteria and selected those whose outcome was RTW ratio. We identified 1,095 papers in our literature search between December 2003 and November 2020, as no related papers were published prior to 2003. Thirty-four papers were extracted via a screening of titles and abstracts, and, via a full-text review, we selected 14 papers in which the RTW ratio was mentioned (Fig. 2).
Fig. 2
Flowchart explicating the article selection process.
2.4Procedure
After obtaining written confirmation of participation, the participants were examined by a psychiatrist. They were confirmed to be at a stage of recovery that did not impede their participation in the intervention. Thereafter, they were asked to continue taking individual occupational therapy lasting two to three hours per session, five days a week for a month. Follow-up checks were conducted to see whether the rhythm of their daily lives had been re-established. As a preliminary evaluation, the HRSD, YMRS, BACS, TEMPS-A, SASS, GATB, GAF, and PRRS were measured during this period (before the inclusion), and participants who fulfilled the eligibility criteria were enrolled in the study. After taking the RTW intervention for three months, as a post-evaluation, the participants took the same tests as a preliminary evaluation. Moreover, at 3, 6, 12, 18, and 24 months after the baseline, their working status, including frequency and working hours, was confirmed by the researchers, either through phone or email.
2.5Data analysis
The required number of patients when the main outcome measure is used as the score of various evaluation scales was calculated from the sample size in a t-test, which agreed with the results generated by G*power 3.1.9.2. If we set the effect size to 0.5, an α error probability of 0.05, power of 0.8, and power (1-β error probability) as 0.8, the number of patients required was 34. Data of participants who had completed the RTW intervention were used for the analysis. To confirm the short-term outcome of the intervention, we used the Wilcoxon signed-rank test to compare the participants’ scores for each test scale in the preliminary and post-evaluation stages and calculated the effect size (r). IBM SPSS Statistics 26 was used for statistical analysis, and a risk ratio of less than 5% was considered significant. Thereafter, we calculated the Full-RTW ratios at 3, 6, 12, 18, and 24 months from the baseline and compared (but not statistically) them with the RTW ratios that had been reported in previous studies.
3Results
3.1Changes in the scores of various scales
Table 3 shows a comparison of the scores of various scales before and after the RTW intervention. The pre-intervention HRSD was 4.13 (SD = 3.73) and the YMRS was 1.13 (SD = 2.16), indicating that symptoms were at the remission level. Post-intervention, both HRSD and YMRS decreased to 2.33 (SD = 2.30) and 1.00 (SD = 1.45), respectively, with the HRSD showing a significant difference (p = 0.0201, r = 0.44). The GAF scores increased significantly from 56.50 (SD = 7.21) to 61.83 (SD = 6.23) (p < 0.001, r = 0.73). The post-intervention score was over 60, which is said to indicate “generally functioning pretty well, and having some meaningful interpersonal relationships” [39]. The BACS z-scores increased significantly in the post-intervention evaluations in terms of verbal memory, working memory, motor speed, and verbal fluency, and the composite score increased significantly from 0.26 (SD = 0.46-0.56, SD = 0.52; p < 0.001, r = 0.81). The TEMPS-A scores showed no significant differences in terms of hyperthymic temperament, depressive temperament, or anxious temperament, but dropped significantly after the intervention in terms of cyclothymic temperament (p = 0.0239, r = 0.43) and irritable temperament (p = 0.0067, r = 0.51). The total SASS scores increased significantly after the intervention, from 31.37 (SD = 5.69) to 34.13 (SD = 5.54) (p = 0.0047, r = 0.53). However, it did not reach the average for general healthy individuals (36.1). With the GATB, significant improvements were seen in all areas except “numerical aptitude” (p = 0.0279–<0.001, r = 0.42–0.78). With the PRRS, a significant increase in scores was seen in all items except social aptitude and workplace issues, and the total score increased from 63.73 (SD = 7.20) to 73.27 (SD = 4.91; p < 0.001, r = 0.82), which showed that the cutoff value (64/66) was exceeded.
Table 3
Assessment scores at pre- and post-RTW program (n = 30)
| Measures | Pre | Post | P value | Effect size (r) | ||
| Mean | (SD) | Mean | (SD) | |||
| HRSD | 4.13 | (3.73) | 2.33 | (2.30) | 0.0201* | 0.44 |
| YMRS | 1.13 | (2.16) | 1 | (1.45) | 0.075 | 0.01 |
| GAF | 56.5 | (7.21) | 61.83 | (6.23) | <0.001** | 0.73 |
| BACS z-score | ||||||
| Verbal memory | 0.49 | (0.84) | 1.15 | (0.81) | <0.001** | 0.67 |
| Working memory | 0.66 | (1.09) | 1.10 | (1.00) | 0.0064** | 0.52 |
| Motor speed | (0.48) | (0.89) | –0.26 | (0.87) | 0.0064** | 0.4 |
| Verbal fluency | 0.13 | (0.76) | 0.49 | (0.78) | 0.0013** | 0.61 |
| Attention | 0.13 | (1.11) | 0.29 | (1.45) | 0.1138 | 0.3 |
| Executive function | 0.79 | (0.88) | 0.92 | (0.95) | 0.2541 | 0.22 |
| Composite score | 0.26 | (0.46) | 0.56 | (0.52) | <0.001** | 0.81 |
| TEMPS-A | ||||||
| Hyperthymic | 4.17 | (2.46) | 4.30 | (3.17) | 0.9256 | 0.02 |
| Depressive | 10.60 | (4.14) | 10.30 | (3.79) | 0.6766 | 0.08 |
| Anxious | 11.3 | (5.98) | 10.07 | (5.88) | 0.1186 | 0.3 |
| Cyclothymic | 7.03 | (3.86) | 5.63 | (3.51) | 0.0239* | 0.43 |
| Irritable | 4.70 | (3.31) | 3.63 | (3.16) | 0.0067** | 0.51 |
| SASS | ||||||
| Interpersonal relationships | 13.10 | (3.58) | 13.80 | (3.41) | 0.0953 | 0.32 |
| Interest and curiosity | 12 | (3.26) | 13.53 | (2.42) | 0.0023** | 0.58 |
| Awareness of the self | 6.27 | (1.70) | 6.80 | (2.09) | 0.135 | 0.28 |
| Total | 31.37 | (5.69) | 34.13 | (5.54) | 0.0047** | 0.53 |
| GATB | ||||||
| General intelligence | 103.63 | (19.52) | 112.28 | (20.41) | 0.0016** | 0.6 |
| Verbal aptitude | 100.57 | (20.25) | 109.93 | (20.93) | 0.0019** | 0.59 |
| Numerical aptitude | 102.77 | (23.45) | 105.59 | (20.98) | 0.0837 | 0.33 |
| Clerical perception | 100.47 | (23.91) | 105.1 | (21.75) | 0.0160* | 0.46 |
| Spatial aptitude | 91.33 | (19.84) | 91.33 | (19.84) | <0.001** | 0.78 |
| Form perception | 84.70 | (21.21) | 91.24 | (18.56) | 0.0038** | 0.55 |
| Motor coordination | 58.50 | (21.31) | 73.00 | (21.31) | 0.0011** | 0.62 |
| Finger dexterity | 70.50 | (21.66) | 76.76 | (23.97) | 0.0279* | 0.42 |
| Manual dexterity | 65.23 | (26.15) | 76.48 | (26.04) | <0.001** | 0.62 |
| PRRS | ||||||
| Basic life rhythm | 7.93 | (2.35) | 9.53 | (1.40) | 0.0010** | 0.6 |
| Symptom | 16.02 | (3.22) | 19.43 | (2.06) | <0.001** | 0.77 |
| Social aptitude | 6.03 | (0.93) | 6.10 | (0.84) | 0.7299 | 0.06 |
| Support resources | 6.10 | (0.92) | 6.57 | (0.82) | 0.0038** | 0.53 |
| Workplace issue | 6.60 | (0.93) | 6.93 | (0.83) | 0.0910 | 0.31 |
| Work ability | 6.93 | (1.68) | 8.93 | (1.01) | <0.001** | 0.74 |
| Work preparation | 3.83 | (1.26) | 5.03 | (0.93) | <0.001** | 0.7 |
| Health management | 10.10 | (1.32) | 10.73 | (1.46) | 0.0084** | 0.48 |
| Total | 63.73 | (7.20) | 73.27 | (4.91) | <0.001** | 0.82 |
Wilcoxon signed-rank test, *p < 0.05, **p < 0.01. Estimated effect size (r): .10 (small), .30 (medium), .50 (large). HRSD: Hamilton rating scale for depression; YMRS: Young Mania Rating Scale; BACS: Brief assessment of cognition in schizophrenia; GATB: General Aptitude Test Battery; TEMPS-A: Temperament evaluation of Memphis, Pisa, Paris and San-Diego-Autoquestionnaire; SASS: Social Adaptation Self-evaluation Scale; GAF: Global Assessment of Functioning; PRRS: Psychiatric Rework Readiness Scale.
3.2Comparison of RTW ratios
The full RTW ratios from the baseline of the intervention were 2 of 30 people (6.7%) at three months, 14 of 30 people (46.7%) at 6 months, 22 of 30 people (73.3%) at 12 months, 21 of 27 people (77.8%) at 18 months, and 19 of 23 people (82.6%) at 24 months. Many participants were in the process of opting for the intervention three months after the baseline.
Of the 14 papers that we selected, 12 had calculated the RTW ratios at the time of follow-up from the baseline and two calculated the RTW ratios at the time of follow-up from the completion of the intervention (Table 4). Three papers had used interventions concerning occupational therapy (OT). Two papers used “Treatment As Usual (TAU) + OT” [13, 14], and one paper used “Cognitive Work Hardening” (CWH) [42]. This study calculated RTW from after the completion of intervention to three months post-intervention, which corresponded to our study’s period from the baseline to the time of follow-up six months later. In the intervention by Schene et al. [14] at 28 weeks, the RTW ratio from the baseline was 9% at 6 months, 39% at 12 months, 52% at 18 months, and 52% at 24 months. In the intervention by Hees et al. [13] at 13 weeks, the RTW ratio at 18 months was 66%.
Table 4
Literature showing the RTW rate
| Study and location | Participants | Intervention (period) | Outcome |
| Shene AH, 2007, UK | Major depressive disorder (DSM-IV) | TAU+OT (28 weeks) | Partial & full RTW 6 months: 9%, 12 months: 39% 18 months: 52%, 24 months: 52% 30 months: 52%, 36 months: 52% 42 months: 57% |
| Hees HL, 2013, Netherlands | Major depressive disorder (DSM-IV) | TAU+OT (13 weeks) | Full RTW 18 months: 66% |
| Wistenthal A, 2018, Canada | Depression | CWH (4 weeks) | Full RTW (from after intervention) 3 months: 76.2% |
| Kaldo V, 2018, Sweden | Depression Anxiety Subthreshold affective disorder | Internet-based CBT (12 weeks) | Partial & full RTW 3 months: 20.8%, 12 months: 60.0% |
| Lagerveld SE, 2012, Netherlands | Adjustment disorder Somatoform disorder Anxiety disorder Mood disorder (Major depressive disorder was excluded) (DSM-IV) | W-CBT (24 weeks) | Full RTW 3 months: 36% 6 months: 73% 12 months: 96% |
| Gjengedala RGH 2020, Norway | Mild-to-moderate depression Anxiety disorders Adjustment disorders (ICD-10) | MCT or CBT (17.4 weeks) | Full RTW At the end of treatment: 41.4% |
| Volker D, 2015, Netherland | Depression, Anxiety disorders Somatization disorder | Web based collaborative care | Full RTW 12 months: 67.7% |
| de Vente JH, 2008, Netherlands | Work related stress | SMT-I (4 months) | Full RTW: 52 weeks: 63% |
| SMT-G (4 months) | Full RTW: 52 weeks: 75% | ||
| Wormgoor, MEA, 2020, Norway | Mental complaints | Brief-PsT (15.1 weeks) | Full RTW 3 months: 44.0%, 12 months: 76.6% 24 months: 79.4% |
| Short-PsT (27.4 weeks) | Full RTW 3 months: 29.4%, 12 months: 64.3% 24 months: 75.5% | ||
| Folk F, 2012, Sweden | Unipolar depressive disorder (DSM-IV) | ACT (6 weeks) | Full RTW (from after intervention) 18 months: 33.3% |
| Hellström L, 2017, Denmark | Affective disorders Anxiety disorders (ICD-10) | IPS-MA (12 months) | Partial & full RTW 24 months: 44.4% |
| Lander F, 2009, Denmark | Stress-related disorders | Activating intervention (156 days) | Partial & full RTW 12 months: 75–80% |
| Rebergen, 2009, Netherlands | Sick leave due to mental health problems | GBC | Full RTW 12 months: 31% |
| Grahn P, 2017 Sweden | Depression Stress-related mental disorders (ICD-10) | NBR (24 weeks) | Full RTW 12 months: 14.7% |
| Our study, 2020 Japan | Major depressive disorder Bipolar disorder Adjustment disorder (DSM-IV) | Interdisciplinary Return to Work Intervention including Occupational Therapy (17.7 weeks) | Full RTW 3 months: 6.7%, 6 months: 46.7%, 12 months: 73.3%, 18 months: 77.8%, 24 months: 82.6% |
DSM: Diagnostic and statistical manual of mental disorders, ICD: International statistical classification of diseases, TAU: Treatment as usual, OT: Occupational therapy, CWH: Cognitive work hardening, CBT: Cognitive behavioral therapy, W-CBT: Work-focused CBT, MCT: Metacognitive therapy, SMT-I: Individual stress management training, SMT-G: Group SMT, Brief-PsT: Brief coping-focused psychotherapy, Short-PsT: Short-term psychotherapy, ACT: Acceptance and Commitment Therapy, IPS-MA: Individual placement and support modified for people with mood and anxiety disorders, GBC: Guideline based care, NBR: Nature-based rehabilitation.
Other than OT-related interventions, there were three papers on CBT [43–45] and one paper each on web-based collaborative care [46], stress management intervention [47], psychotherapy [48], acceptance and commitment therapy (ACT) [49], individual placement and support modified for people with mood and anxiety disorders (IPS-MA) [17], activating intervention [50], guideline-based care provided by occupational physicians [51], and nature-based rehabilitation [52]. The period of intervention varied widely, from six weeks to approximately 1 year. There were also two papers that did not show the intervention period. The follow-up period of intervention in each paper was also different. Three papers failed to separate the RTW ratio into “full” and “partial.” Four papers reported the RTW ratio at three months from the baseline, which ranged from 20% –44%. A study reported the RTW ratio six months later, which was 73% due to intervention by work-focused cognitive behavioral therapy (W-CBT) [44]. Eight papers described the RTW ratios 12 months later, including the data as of the 52 week-time point (13 months) shown by de Vente et al., with the ratios ranging between 14.7% and 96%. One study showed the RTW ratio 18 months later, after the end of the program, which was 33.3%. Two studies described the RTW ratios at 24 months, with Hellström et al. reporting 44.4% for IPS-MA and Wormgoor et al. reporting 79.4% for brief coping-focused psychotherapy (Brief-PsT) and 75.5% for short-term psychotherapy (Short-PsT).
4Discussion
4.1Short-term outcomes of the interdisciplinary RTW intervention including occupational therapy
Multiple meta-analyses have identified the effects of interventions aimed at the RTW of depressed people and improving depressive symptoms [10, 11]. Ours is the first study to investigate the outcomes of an interdisciplinary RTW intervention including occupational therapy in Japan. The intervention in question, lasting approximately three months, was shown to improve the participants’ depressive symptoms, cognitive functioning, job performance, global functioning, temperament, and personality, as well as global functions such as social adaptation and readiness to RTW.
Recent studies noted that patients with mood disorders have cognitive impairment, which limits their post-remission quality of life including their social functions, occupational outcomes, and work performance [53–55]. The average composite BACS score of the participants increased significantly after the intervention, from 0.26 (SD = 0.46) to 0.56 (SD = 0.52). Significant improvements were also seen in indices measured by the GATB such as general intelligence, verbal aptitude, clerical perception, spatial aptitude, form perception, motor coordination, finger dexterity, and manual dexterity. As shown in Table 1, our interdisciplinary RTW intervention including occupational therapy offered diverse study programs and learning tasks via D-MCT. In particular, individual sessions offered extensive training using constitutive craftwork and computer operations. Participants received training to activate their functions, such as spatial aptitude and form perception, as well as hand-eye coordination movements and finger–arm dexterity. In the course of executing various works, participants engaged in composite cognitive tasks, such as understanding written manuals and expansion drawings, collating them with the actual items (parts), and operating tools and materials. The improvement in the participants’ functions, which was confirmed with BACS and GATB, suggests the enhancement of work performance that had been induced by individual sessions performed five times a week.
Temperament and personality are factors that affect a person’s RTW and their working status [56]. It has been pointed out that the depressive, cyclothymic, and irritable temperaments are often seen in the Japanese population [57] and that cyclothymic temperament is a common trait seen in unipolar depression and bipolar disorder cases [58]. A Japanese study has shown that, compared with those who are not, individuals with a strong irritable temperament tend to receive less social support from their superiors, are liable to cause and play a role in intra-group conflicts, and see their symptoms worsen after returning to work [59]. In our study, cyclothymic and irritable temperaments decreased significantly after the program. It has been reported that changes in temperament and personality resulting from treatment of depression are caused by a reduction in demoralization [60]. Therefore, the improvements seen in the study may indicate improvements in emotional control and expression of anger that are attributable to the study program, such as CBT, interpersonal and social rhythm therapy, assertiveness training, and anger management. Although further studies are needed to address this point, it is possible that these changes may contribute to alleviating stress after returning to work.
Researchers have reported that the higher the total PRRS score, the longer the work continuation after returning to work [41]. The total PRRS scores of the participants in our study increased significantly after the program, from 63.73 (SD = 7.20) to 73.27 (SD = 4.91), sharply exceeding the cutoff (64/65), which predicts work continuation six months after RTW. Stabilization of “basic life rhythm,” which is a sub-item of the PRRS, appeared to have been promoted by the 5-times-per-week participation in the program as was the effect of “habit training” [61], which is considered important in occupational therapy. The GAF scores, which show severity, symptoms, or difficulty in social, occupational, or school functions, increased significantly from 56.50 (SD = 7.21) to 61.83 (SD = 6.23), with the participants being judged, after intervention, by an occupational therapist as “generally functioning pretty well, and having some meaningful interpersonal relationships” [39]. Enhanced readiness to RTW shown in the PRRS and improved functions shown in the GAF are deemed to be the comprehensive outcome of the interdisciplinary RTW intervention including occupational therapy. In contrast, the pre-intervention average of the total SASS scores of 31.37 (SD = 5.69) was lower than the average for general healthy individuals (36.1). Although it increased significantly after the intervention, it failed to reach the average seen in typical healthy individuals. Among the subscales, “interest and curiosity” showed a pattern of improvement, but “interpersonal relationships” and “awareness of the self” remained unchanged. With the SASS, it is said that the higher the score, the greater the prediction of work continuation [62]. To improve interpersonal relations and assessments of the self, it may be necessary to add new program elements that focus on these areas.
4.2Long-term outcome of the interdisciplinary RTW intervention including occupational therapy
A feature of this RTW intervention was that it included an individual session in which the occupational therapist planned and implemented an individual support plan, within the framework of healthcare services, over approximately three months. Although the parameters varied depending on the period, the full-RTW ratio from the baseline was 6.7% at 3 months, 46.7% at 6 months, 73.3% at 12 months, 77.8% at 18 months, and 82.6% at 24 months. It appears that, because our intervention went through a process lasting approximately three months, followed by adjustment conferences within the workplace, the RTW at three months was low.
Compared to interventions reported in three previous studies focusing on OT [13, 14, 42], our RTW ratio was higher than the RTW ratios seen via the TAU+OT technique, regardless of the period, but lower than the intervention via the CWH technique. CWH uses “work hardening,” a technique developed by occupational therapists targeting physical disability areas of employees and those with pain, which simulates the actual work environment and carries out work aimed at performance enhancement. It was then modified for use by knowledge workers diagnosed with depression. Knowledge workers, in this context, referred to individuals who used an abundance of cognitive skills, such as manipulation of information for their work. The technique simulated the intellectual labor environment by using computers in an office environment. However, the OT sessions offered with the TAU+OT technique were mainly language-based. A point of commonality in both our interventions and CWH interventions was that they contained numerous nonverbal sessions (practicing the movements needed in work activities and in actual work, etc.). In interventions that include OT, targeted at patients with mood and adjustment disorders, it may be effective to offer both verbal and nonverbal interventions. However, CWH targets are limited to knowledge workers who suffer from depression. The diagnosis of depression was not specified as a psychiatric diagnosis made by a psychiatric specialist. Moreover, since only a short-term RTW ratio of three months was observed, investigations of long-term prognosis were insufficient.
In interventions other than OT in previous studies, the participants in 6 of 11 papers did not undergo diagnoses by psychiatric specialists. Interventions that showed higher RTW ratios than our own after six months were those after W-CBT [44], group stress management training (SMT-G) [47], Brief-PsT [48], and activating intervention [50]. Of these, the participants of studies employing OT other than W-CBT were not diagnosed by psychiatric specialists. The participants of W-CBT, as reported by Legerveld [44], received a psychiatric diagnosis based on the DSM-IV. However, major depressive disorder was not included, and the intervention period was roughly twice as long as that of our program. These differences in the participants and duration of intervention are believed to have resulted in higher RTW ratios.
Few studies reported RTW ratios at 24 months after the baseline. The RTW ratio at 24 months of 82.6%, shown in our study, is the highest value ever reported, confirming the long-term outcomes of our interdisciplinary RTW intervention including occupational therapy.
Lastly, we note that 36.6% of the participants (11 of 30 people) had developmental disorder tendencies. Researchers have pointed out that a RTW program targeting depressive patients in Japan includes a set number of patients who concurrently suffer developmental disorders and that the special characteristics of developmental disorders have become one of the causes for chronic or recurring depression [63]. However, a detailed examination cannot be undertaken because little research has been conducted on the RTW of adult patients with developmental disorders but with no intellectual disabilities. However, the employment rate of individuals with developmental disorders appears to be decreasing [64, 65]. Nonetheless, as described previously, the RTW ratios shown in our intervention were not low. In assisting individuals with developmental disorders, individual support is regarded as extremely important [63]. Hence, our individualized RTW intervention has the potential to be applied to support the RTW of patients with depression and adjustment disorders who concurrently suffer developmental disorders.
4.3Limitations and future challenges
There are a few limitations to this study. The first limitation relates to the research design. We did not have a control group. Thus, comparative control groups are to be set up to show the effects of interdisciplinary RTW intervention including occupational therapy even more definitely. Additionally, we did not use the activity-based instrument that occupational therapy emphasizes. Therefore, we need to include occupation-related outcome measures, such as Model of Human Occupation-Based Instruments [66] in relation to RTW, and a clear theoretical and empirical foundation in occupational therapy in future research. The second limitation lies in the method of comparing long-term outcomes. Our intervention was costly, with many professionals participating in teams and coordinating with the workplace, but some of the comparative studies failed to do so. Careful judgment should be made regarding the comparison results of the long-term outcomes or for the cost-effectiveness of this study. Third, of the 34 patients needed for statistical analysis, we were short by four patients. The ongoing COVID-19 pandemic occurred during our study period requiring us to limit the number of days that we could visit the participants’ hospitals, which made it difficult for us to perform our intervention by visiting the hospital five days a week. In the future, it will be necessary to make adjustments, such as implementing programs at home, for example, by adding a web conferencing system and a remote system to this intervention.
5Conclusion
This study is the first interdisciplinary RTW intervention including occupational therapy for people with mood and adjustment disorders in Japan. It is found that this RTW intervention has the potential to improve not only depressive symptoms but also cognitive functioning, job performance, social adaptation, and readiness to RTW. Moreover, this intervention was also shown to increase RTW ratios. These findings demonstrate the significant potential that occupational therapy has to contribute to RTW interventions for people with mood and adjustment disorders.
Ethical considerations
This study was approved by the Ethics Committee of Shinshu University School of Medicine (Approval numbers 2694 and 4310), and the results were registered with the UMIN Clinical Trials Registry (UMIN000036294).
Reporting guidelines
This paper was written in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Acknowledgments
The authors thank all participants in this study. They are grateful to Kasumi Kitazawa, Nozomi Inukai, and Susumu Sakaue for helping them implement the program. They thank Haruka Tanabe and Yuka Asai for helpful discussions that aided in the completion of this study.
Informed consent
This study was performed in accordance with the Declaration of Helsinki and written consent was obtained from all participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by JSPS KAKENHI (Grant numbers JP26780305 and JP20K13723).
References
[1] | Brown C , Stoffel VC , Phillip Muñoz JP . Occupational therapy in mental health: A vision for participation. 2nd ed. Philadelphia: F.A. Davis Company; (2019) . |
[2] | American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; (2002) . |
[3] | Heijbel B , Josephson M , Jensen I , Vingård E . Employer,insurance, and health system response to long-term sick leave in thepublic sector: Policy implications. J Occup Rehabil. (2005) ;15: (2):167–76. |
[4] | Shiels C , Gabbay MB , Ford FM . Patient factors associated with duration of certified sickness absence and transition to long-term incapacity. Br J Gen Pract. (2004) ;54: (499):86–91. |
[5] | Endo M , Muto T , Haruyama Y , Yuhara M , Sairenchi T , Kato R . Risk factors of recurrent sickness absence due to depression: A two-year cohort study among Japanese employees. Int Arch Occup Environ Health. (2015) ;88: (1):75–83. |
[6] | Lammerts L , Schaafsma FG , Eikelenboom M , Vermeulen SJ , van Mechelen W , Anema JR , et al. Longitudinal associations between biopsychosocial factors and sustainable return to work of sick-listed workers with a depressive or anxiety disorder. J Occup Rehabil. (2016) ;26: (1):70–9. |
[7] | Asami Y , Goren A , Okumura Y . Work productivity loss with depression, diagnosed and undiagnosed, among workers in an Internet-based survey conducted in Japan. J Occup Environ Med. (2015) ;57: (1):105–10. |
[8] | Beck A , Crain AL , Solberg LI , Unützer J , Glasgow RE , Maciosek MV , et al. Severity of depression and magnitude of productivity loss. Ann Fam Med. (2011) ;9: (4):305–11. |
[9] | Bloom DE , Jané-Llopis E , Abrahams-Gessel S , Bloom LR , Fathima S , Feigl AB , et al.. The global economic burden of non-communicable diseases. Geneva: World Economic Forum; (2011) . |
[10] | Nieuwenhuijsen K , Faber B , Verbeek JH , Neumeyer-Gromen A , Hees HL , Verhoeven AC , et al. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev. (2014) ;12: :Cd006237. |
[11] | Nieuwenhuijsen K , Verbeek JH , Neumeyer-Gromen A , Verhoeven AC , Bültmann U , Faber B . Interventions to improve return to work in depressed people. Cochrane Database Syst Rev. (2020) ;10: :Cd006237. |
[12] | Nigatu YT , Liu Y , Uppal M , McKinney S , Rao S , Gillis K , et al. Interventions for enhancing return to work in individuals with a common mental illness: Systematic review and meta-analysis of randomized controlled trials. Psychol Med. (2016) ;46: (16):3263–74. |
[13] | Hees HL , de Vries G , Koeter MW , Schene AH . Adjuvant occupationaltherapy improves long-term depression recovery and return-to-work ingood health in sick-listed employees with major depression: Resultsof a randomized controlled trial. Occup Environ Med. (2013) ;70: (4):252–60. |
[14] | Schene AH , Koeter MW , Kikkert MJ , Swinkels JA , McCrone P . Adjuvant occupational therapy for work-related major depression works: Randomized trial including economic evaluation. Psychol Med. (2007) ;37: (3):351–62. |
[15] | Drake AH , Bond GR , Becker DR . Individual placement and support: An evidence-based approach to supported employment. Oxford: Oxford University Press; (2013) . |
[16] | Frederick DE , VanderEeele TJ . Supported employment: Meta-analysis and review of randomized controlled trials of individual placement and support. PLoS One. (2019) ;14: (2):e0212208. |
[17] | Hellström L , Bech P , Hjorthøj C , Nordentoft M , Lindschou J , Eplov LF . Effect on return to work or education of individual placement and support modified for people with mood and anxiety disorders: Results of a randomized clinical trial. Occup Environ Med. (2017) ;74: (10):717–25. |
[18] | Akiyama T , Tsuchiya M , Igarashi Y , Ozaki N , Yokoyama M , Katagiri Y , et al. “Rework Program” in Japan: Innovative high-level rehabilitation. Asia-Pac. (2010) ;2: (4):208–16. |
[19] | Japanese Association of Rework for Depression [homepage on the internet]. Tokyo. The Association; 2018 [updated 2021 July 6; cited 2021 Sep 27]. Available from: https://utsu-rework.org/index.html |
[20] | Ohki Y , Igarashi Y , Yamauchi K . Re-Work program in Japan-Overview and outcome of the program. Front Psychiatry. (2020) ;11: :616223. |
[21] | Ohki Y , Yoshio I , Keita Y . Effectiveness of return to work program: Outcomes in domestic research and trends in foreign research. Jpn J Clin Med. (2012) ;41: (11):1561–71. [in Japanese]. |
[22] | Arima H , Akiyama T , de Moura PA , Bernick P , Sakai Y , Ozaki Y , et al. Resilience building for mood disorders: Theoretical introduction and the achievements of the Re-Work program in Japan. Asian J Psychiatr. (2021) ;58: :102580. |
[23] | World Federation of Occupational Therapists [page on the internet]. London: The Federation; (2021) [updated 2021 Oct 27; cited 2021 Oct 27]. Available from: https://www.wfot.org/about/about-occupational-therapy |
[24] | Edgelow M , Harrison L , Miceli M , Cramm H . Occupational therapy return to work interventions for persons with trauma and stress-related mental health conditions: A scoping review. Work. (2020) ;65: (4): 821–36. 10.3233/WOR-203134 |
[25] | Désiron HA , de Rijk A , Van Hoof E , Donceel P . Occupational therapy and return to work: a systematic literature review. BMC Public Health. (2011) ;11: :615. |
[26] | No authors listed: Occupational therapy services in facilitating work participation and performance. Am J Occup Ther. (2017) ;71: :71124100401–13. 10.5014/ajot.2017.716s05. |
[27] | Ministry of Health, Labour and Welfare of Japan. Comprehensive Survey of Working Conditions: Summary of Results: 2020 [updated 2020 Oct 30; cited 2021 Oct 9]. Available from: https://www.mhlw.go.jp/toukei/list/11-23c.html |
[28] | Substance Abuse and Mental Health Services Administration. Illness Management and Recovery: Evidence-Based Practice Toolkit. Location: The Administration; (2009) [updated 2006 May 12; cited 2006 Oct 17]. Available from: https://store.samhsa.gov/product/Illness-Management-and-Recovery-Evidence-Based-Practices-EBP-KIT/sma09-4462 |
[29] | Jelinek L , Moritz S , Hauschildt M . Patients’ perspectives on treatment with Metacognitive Training for Depression (D-MCT): Results on acceptability. J Affect Disord. (2017) ;221: :17–24. |
[30] | World Health Organization. International Classification ofFunctioning Disability and Health (ICF). Geneva: World Health Organization; (2021) [updated 2021 Oct 272; cited 2021 Oct 27]. Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health |
[31] | Hamilton M . A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) ;23: (1):56–62. |
[32] | Young RC , Biggs JT , Ziegler VE , Meyer DA . A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. (1978) ;133: :429–35. |
[33] | Terachi S , Yamada T , Pu S , Yokoyama K , Matsumura H , Kaneko K . Comparison of neurocognitive function in major depressive disorder, bipolar disorder, and schizophrenia in later life: A cross-sectional study of euthymic or remitted, non-demented patients using the Japanese version of the Brief Assessment of Cognition in Schizophrenia (BACS-J). Psychiatry Res. (2017) ;254: :205–10. |
[34] | Kaneda Y , Sumiyoshi T , Keefe R , Ishimoto Y , Numata S , Ohmori T . Brief assessment of cognition in schizophrenia: Validation of the Japanese version. Psychiatry Clin Neurosci. (2007) ;61: (6):602–9. |
[35] | The Japan Institute for Labour Policy and Training. Location: The Institute; (2021) [updated 2021 Sep 82; cited 2021 June 26]. Available from: https://www.jil.go.jp/institute/seika/tools/GATB.html |
[36] | Matsumoto S , Akiyama T , Tsuda H , Miyake Y , Kawamura Y , Noda T , et al. Reliability and validity of TEMPS-A in a Japanese non-clinical population: Application to unipolar and bipolar depressives. J Affect Disord. (2005) ;85: (1-2):85–92. |
[37] | Ueda N , Suda A , Nakagawa M , Nakano H , Umene-Nakano W , Ikenouchi-Sugita A , et al. Reliability, validity and clinical utility of a Japanese version of the Social Adaptation Self-evaluation Scale as calibrated using the Beck Depression Inventory. Psychiatry Clin Neurosci. (2011) ;65: (7):624–9. |
[38] | Atake K , Hori H , Katsuki A , Yoshimura R . Predictors of return to work success among Japanese employees with major depressive disorder. Psychiatry Res. (2020) ;291: :113209. |
[39] | Jones SH , Thornicroft G , Coffey M , Dunn G . A brief mental healthoutcome scale-reliability and validity of the GlobalAssessment of Functioning (GAF). Br J Psychiatry. (1995) ;166: (5):654–9. |
[40] | Sakai K , Akiyama T , Tsuchiya S , Horii K , Tominaga M , Tanaka M , et al. A study of inter-reviewer reliability, internal consistence and forecast validity of the readiness for return to work evaluation sheet (Psychiatric Rework Readiness Scale). Japanese Journal of Psychiatric Treatment. (2012) ;27: (5):655–67. [in Japanese]. |
[41] | Horii S , Sakai Y , Tagawa A , Bernick P , Seki E , Akiyama T , et al. Predictive validity of the psychiatric rework readiness scale for work continuation for participants in the Re-Work program aiming to increase the resilience of patients returning to work with mental illness: Factors influencing work continuation. Psychiat Neurol Jap. (2019) ;121: (6):445–56. [in Japanese]. |
[42] | Wisenthal A , Krupa T , Kirsh BH , Lysaght R . Le réentraînement cognitif au travail pour favoriser le retour au travail à la suite d’une dépression: étude d’intervention [Cognitive work hardening for return to work following depression: An intervention study.] Can J Occup Ther. (2018) ;85: (1):21–32. |
[43] | Kaldo V , Lundin A , Hallgren M , Kraepelien M , Strid C , Ekblom Ö , et al. Effects of internet-based cognitive behavioral therapy and physical exercise on sick leave and employment in primary care patients with depression: Two subgroup analyses. Occup Environ Med. (2018) ;75: (1):52–8. |
[44] | Lagerveld SE , Blonk RW , Brenninkmeijer V , Wijngaards-de Meij L , Schaufeli WB . Work-focused treatment of common mental disorders and return to work: A comparative outcome study. J Occup Health Psychol. (2012) ;17: (2):220–34. |
[45] | Gjengedal RGH , Reme SE , Osnes K , Lagerfeld SE , Blonk RWB , Sandin K , et al. Work-focused therapy for common mental disorders: A naturalistic study comparing an intervention group with a waitlist control group. Work. (2020) ;66: (3):657–67. |
[46] | Volker D , Zijlstra-Vlasveld MC , Anema JR , Beekman AT , Brouwers EP , Emons WH , et al. Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: Results of a cluster randomized controlled trial. J Med Internet Res. (2015) ;17: (5):e116. |
[47] | de Vente W , Kamphuis JH , Emmelkamp PM , Blonk RW . Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: A randomized controlled trial. J Occup Health Psychol. (2008) ;13: (3):214–31. |
[48] | Wormgoor MEA , Indahl A , Andersen E , Egeland J . Effectiveness of briefer coping-focused psychotherapy for common mental complaints on work-participation and mental health: A pragmatic randomized trial with 2-year follow-up. J Occup Rehabil. (2020) ;30: (1):22–39. |
[49] | Folke F , Parling T , Melin L . Acceptance and commitment therapy for depression: A preliminary randomized clinical trial for unemployed on long-term sick leave. Cogn Behav Pract. (2012) ;19: (4):583–94. |
[50] | Lander F , Friche C , Tornemand H , Andersen JH , Kirkeskov L . Can we enhance the ability to return to work among workers with stress-related disorders? BMC Public Health. (2009) ;9: :372. |
[51] | Rebergen DS , Bruinvels DJ , Bezemer PD , van der Beek AJ , van Mechelen W . Guideline-based care of common mental disorders by occupational physicians (CO-OP study): A randomized controlled trial. J Occup Environ Med. (2009) ;51: (3):305–12. |
[52] | Grahn P , Pálsdóttir AM , Ottosson J , Jonsdottir IH . Longer nature-based rehabilitation may contribute to a faster return to work in patients with reactions to severe stress and/or depression. Int J Environ Res Public Health. (2017) ;14: (11). |
[53] | Gualtieri CT , Morgan DW . The frequency of cognitive impairment in patients with anxiety, depression, and bipolar disorder: An unaccounted source of variance in clinical trials. J Clin Psychiatry. (2008) ;69: (7):1122–30. |
[54] | Kaneda Y . Verbal working memory impairment in patients with current episode of unipolar major depressive disorder and in remission. Clin Neuropharmacol. (2009) ;32: (6):346–7. |
[55] | McIntyre RS , Cha DS , Soczynska JK , Woldeyohannes HO , Gallaugher LA , Kudlow P , et al. Cognitive deficits and functional outcomes in major depressive disorder: Determinants, substrates, and treatment interventions. Depress Anxiety. (2013) ;30: (6):515–27. |
[56] | Ervasti J , Joensuu M , Pentti J , Oksanen T , Ahola K , Vahtera J , et al. Prognostic factors for return to work after depression-related work disability: A systematic review and meta-analysis. J Psychiatr Res. (2017) ;95: :28–36. |
[57] | Akiyama T , Tsuda H , Matsumoto S , Miyake Y , Kawamura Y , Noda T , et al. The proposed factor structure of temperament and personality in Japan: Combining traits from TEMPS-A and MPT. J Affect Disord. (2005) ;85: (1-2):93–100. |
[58] | Akiyama T , Tsuda H , Matsumoto S , Kawamura Y , Miyake Y . Cyclothymia and typus melancholicus: Empirical study on personality character of mood disorder. Psychiat Neurol Jap. (2003) ;105: (5):533–43. [in Japanese]. |
[59] | Deguchi Y , Iwasaki S , Konishi A , Ishimoto H , Ogawa K , Fukuda Y , et al. The usefulness of assessing and identifying workers’ temperaments and their effects on occupational stress in the workplace. PloS One. (2016) ;11: (5):e0156339. |
[60] | Noordhof A , Kamphuis JH , Sellbom M , Eigenhuis A , Bagby RM . Change in self-reported personality during major depressive disorder treatment: A reanalysis of treatment studies from a demoralization perspective. Personal Disord. (2018) ;9: (1):93–100. |
[61] | Better Habits, Brighter Futures: Outcomes of a habit-training program for people in a community-based supported-housing program. Am J Occup Ther. (2020) ;74: (4 Suppl. 1):7411515380p1. 10.5014/ajot.2020.74S1-PO3513. |
[62] | Hori H , Katsuki A , Atake K , Yoshimura R , Nakamura J , Baune BT . Risk factors for further sick leave among Japanese workers returning to work after an episode of major depressive disorder: A prospective follow-up study over 1 year. BMJ Open. (2019) ;9: (9):e029705. |
[63] | Ebisawa T . The outpatient clinic and rehabilitation program specialized in adult developmental disorders. Seishin Shinkeigaku Zasshi. (2015) ;117: (3):205–11. [in Japanese]. |
[64] | Gjervan B , Torgersen T , Nordahl HM , Rasmussen K . Functional impairment and occupational outcome in adults with ADHD. J Atten Disord. (2012) ;16: (7):544–52. |
[65] | Shattuck PT , Narendorf SC , Cooper B , Sterzing PR , Wagner M , Taylor JL . Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. (2012) ;129: (6):1042–9. |
[66] | Taylor R . Kielhofner’s Model of human occupation: Theory and application. 5th ed. Philadelphia. Wolters Kluwer Health;(2017) . |




