Safe protocol of resuming routine dental procedures in a tertiary care hospital setting post COVID-19 lockdown
Abstract
BACKGROUND:
The outbreak of the COVID-19 pandemic greatly affected dentistry. Dental procedures are considered one of the modes of transfer of COVID-19 infection due to generation of aerosols. To prevent transmission of this virus through dental procedures, guidelines were issued by the World Health Organisation (WHO), Centers for Disease Control and Prevention (CDC) and Ministry of Health of each country.
OBJECTIVE:
The aim of this study is to establish a safe protocol for performing dental procedures in a crisis capacity situation of personal protective equipment (PPE).
METHODS:
A strategy for performing the dental procedures was formulated in accordance with the guidelines provided by the Ministry of Health, Pakistan before vaccination of HCPs against COVID-19. These guidelines also accorded the strategies provided by the WHO and CDC. 40 health care professionals (HCPs) participated in the study and were divided in two groups. Group A performed non-aerosol generating procedures (non- AGPs) and group B performed aerosol generating procedures (AGPs). A total of 6372 aerosol generating procedures were performed from 1 August 2020 to 31 March 2021. The safety of this protocol was established by the number of HCPs contracting COVID-19 infection.
RESULTS:
Only 1 HCP contracted COVID-19 infection preceding the AGPs from group B following the formulated strategy.
CONCLUSION:
Reported strategy based on the dental system in Pakistan is considered safe to be implemented worldwide during the COVID-19 pandemic.
1Introduction
Public health emergency of an international concern was declared on 30 January 2020 by the World Health Organisation (WHO), with the outbreak of novel coronavirus (COVID-19) worldwide [1]. The first case of COVID-19 was reported in Wuhan, China on 17 November 2019 [2]. Shortly after which the first case in Pakistan was reported on 26 February 2020 [3] WHO declared COVID-19 as a pandemic on 11 March 2020 [4]. Dental healthcare provision was among other health services which were affected during COVID-19 pandemic [5]. Based on current evidence the WHO concluded that respiratory droplets and contact exposures were major modes of transmission of COVID-19 [6]. Air borne transmission refers to microbes within droplet nuclei that < 5 m in diameter and travel more than 1m distance. This mode of transmission occurs via aerosols [7–9]. Dental procedures generate aerosols which generally include ultrasonic scaling, tooth polishing, air polishing, air abrasion, slow and high-speed rotary instrumentation, and use of air-water triple syringe [10] and intraoral radiographs [11]. The Occupational Safety and Health Administration subsequently designated all AGPs as ‘very high risk’ in patients with known or suspected COVID-19 due to aerosol’s travelling capability and their ability to survive on various inanimate surfaces for few days [12–14]. Performing these procedures with limited availability of PPE and other resources proves to be challenging, as various studies have reported lack of PPE availability globally including Pakistan [15]. Standard Operating Procedures (SOPs) were formulated for all dental procedures in accordance with the Universal Standard Protocols released by Ministry of Health, Pakistan [18] and after thorough review of international guidelines [16, 17]. Aim of the current study is to establish safety of performing AGPs and Non AGPs and whether protocol established was sufficient to prevent COVID-19 transmission.
2Methods
Dental procedures were started following resumption of services post COVID-19 lockdown on 1 August 2020 at an out-patient tertiary care dental hospital with 40 health care workers comprising of 12 specialists, 18 dentists, and 10 auxiliary staff members. Health care professionals (HCPs) were divided in two groups based on their specialities and previous experience. Group A comprised of 20 HCPs who performed non-AGPs while Group B which performed AGPs included 20 HCPs. Procedures were performed only in patients who were asymptomatic for COVID-19 virus, despite having history of travel (domestic or international). Patients who had recent history of contact with COVID-19 patients were considered as suspected cases of COVID-19. Such patients were provided with pharmacologic treatment, as they did not present with any dental emergency. All procedures were performed on the same day of patient’s visit, while appointments were only given for second visit if deemed necessary. The SOPs for both procedures are described below.
2.1Tele-health and receptionist-directed triage protocols
We used tele-health strategies to provide better patient care and to reduce risk of COVID-19 transmission. Patients were instructed to call and inform if they noticed any symptoms after dental treatment. Also, all patients were called twice after first and second week of hospital visit and asked about symptoms of COVID-19 virus as mean incubation period of COVID-19 is 5 days (range 2–14 days) [19]. Based on tele-health protocols, record was maintained about number of patients contracting COVID-19 infection following dental treatment. All HCPs were also monitored for signs and symptoms and advised to immediately self-isolate and remotely inform in case of any symptoms for further contact tracing.
2.2Screening and triage of everyone entering hospital for signs and symptoms of COVID-19
COVID-19 sentinel was established at the single-entry point to the hospital facility. Emergency exit doors were used for exit separate from the entry doors. HCP in screening zone wore surgical face mask. Hand sanitisation was provided with 70% alcohol based disinfectant spray-bottles. Temperature was checked for everyone entering dental hospital with a non-contact thermometer and screening questionnaire was filled. Questionnaire was based on subjective symptoms as fever, dry cough, loss of taste and smell, myalgia, GI upset, previous history of COVID-19 infection, history of travel or contact with a COVID-19 infected person. Any person with fever ≥100.0 °F, suspected or confirmed COVID-19 infection was evaluated for urgency of dental care. According to the American Dental Association (ADA), these conditions include uncontrolled bleeding, facial space infection or cellulitis and facial trauma that compromises patient’s airway [20]. Suspected or confirmed COVID-19 infected patients presented only for acute pain and were provided pharmacologic treatment. Patient attendants were restricted from entering the facility except in the case of caregivers assisting handicapped individuals and parents accompanying children under the age of 14.
2.3Health care worker screening
Temperature of HCPs before entry into the hospital at the beginning of the day was checked. HCPs were prohibited from entering or remaining in the workplace if they had fever of 100.4°F or greater (or reported feeling feverish), or if screening results indicated COVID-19 infection. Infected HCP self-isolated and contact tracing was done, followed by screening of contacts for COVID-19 infection. HCPs strictly followed the source control measures.
2.4Universal source control measures
Source control measures were implemented by making it compulsory for all HCPs, patients and visitors to wear facemask or their own cloth face coverings upon arrival and throughout their stay at hospital facility. Patients and HCPs were educated about importance of hand hygiene before and after contact with face mask or cloth face covering. Visual alerts in form of posters were displayed at entrance, common areas (toilets and waiting area) and in strategic places (hallways, clinic entrance doors) in English and native language about COVID-19 awareness, wearing facemask for source control, social distancing and instructions about hand hygiene [12].
2.5Seating area
Seating arrangement and markings were made in waiting area for patients. Also, for HCPs group activities and for breaks, rooms and seating areas were designated to ensure social distance of 6 feet at all times. Most of group healthcare activities were modified by implementation of virtual methods.
2.6Universal use of personal protective equipment (PPE)
PPE used for dental procedures comprised surgical mask, eye protection (goggles), face shield, sterile gloves and sterilised surgical gowns. Hospital administration provided surgical masks for HCPs due to limited availability of KN95.
2.7Donning and doffing zones
Donning zone and Doffing zone were established in separate designated rooms inside each department. HCPs conformed to following sequence while donning PPE [21]: Hand hygiene adhering to WHO’s hand hygiene instructions; Sterilized surgical gowns; Face mask; Eye-protection; Face shield; Hand hygiene again before wearing sterile gloves.
After dental procedures, HCPs removed the gloves, performed hand hygiene. Surgical gowns were disinfected with 70% ethanol sprays [22]. Goggles and face shields were removed and disinfected with 0.1% sodium hypochlorite for 1 min and then washed with lukewarm tap water followed by hand hygiene again [23, 24]. Gowns and masks were not changed for each procedure unless visibly or knowingly soiled by saliva or blood. As CDC recommends extended use of mask and gown as part of contingency and crisis capacity strategies for asymptomatic patients [17]. Gowns were removed in separate designated room for doffing and placed in yellow labelled container. These were sent to central sterile supply department (CSSD) for sterilization.
2.8Infection control protocol for aerosol generating procedures
2.8.1Air quality
Air quality was maintained via natural ventilation through 5–7 windows in each department and 1 door which were kept open throughout the day. WHO recommends 12 air changes per hour (ACH) for hospital-based setting [25] ACH in each department was calculated as [26]:
(1)
Air speed was calculated using anemometer was 0.25m/s (at time of calm/no breeze)
Opening area is the area of the vent of all the windows in the room
3600 are the number of seconds in an hour
Room volume calculated by multiplying length, height and width
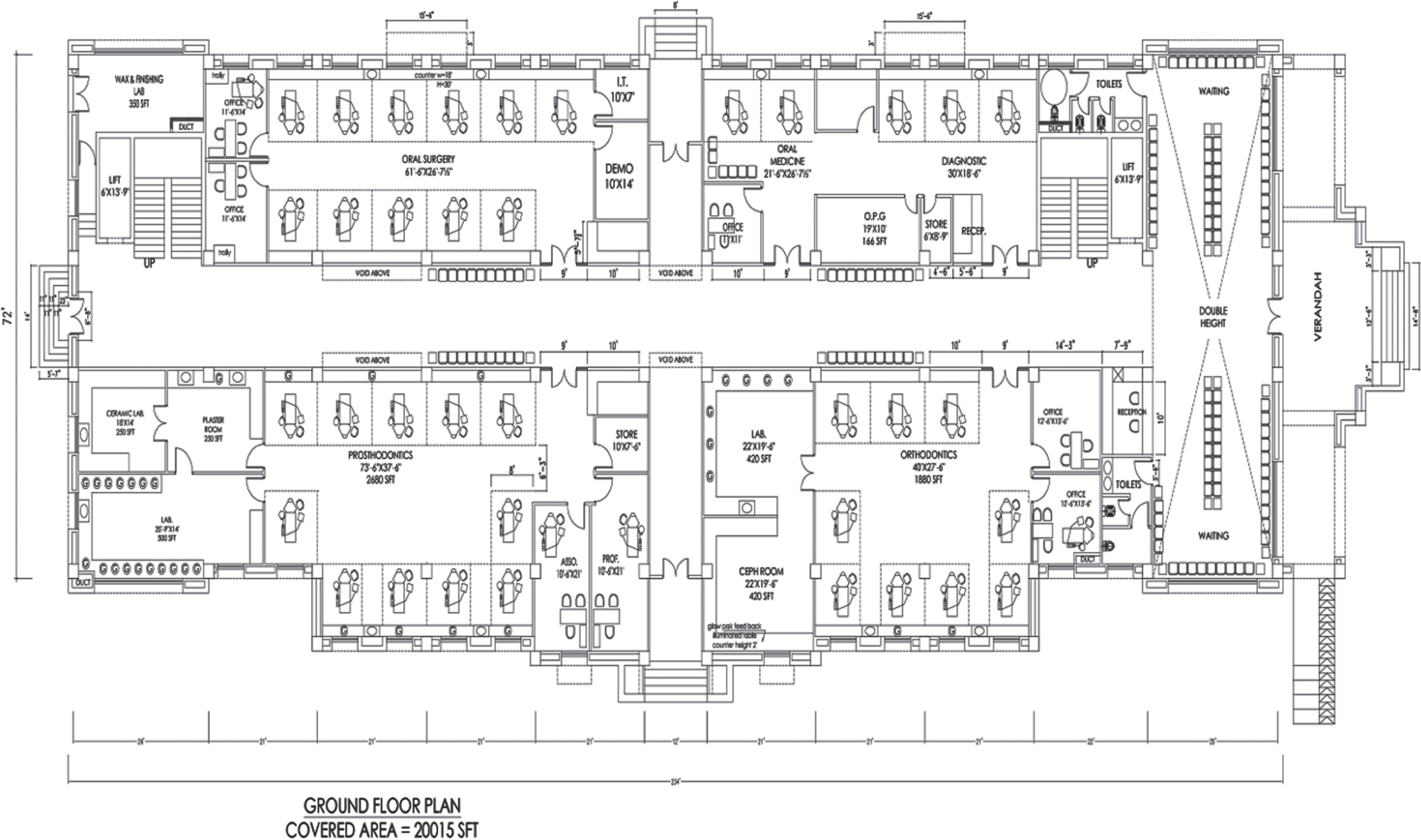
AGPs were performed in 2 departments each with 10–12 dental units. The departments where Prosthodontic and Restorative AGPs were performed had an ACH of 12/h, Oral Surgery and Periodontology had an ACH 25/h. Figure 1 shows architectural design and location of windows and dental units.
Additional measures that were taken included: Use of rubber dam (when applicable); Use of high-volume suction; Air-water (triple) syringe was used with caution.
Fig. 1
Architectural design of hospital floor displaying routes of natural ventilation through multiple open windows and doors located in opposing direction in each department, allowing adequate air exchanges per hour (ACH). Thus, fulfilling the criteria of 12 ACH recommended by WHO for hospital setting. Area of each window and door is 8 ft2 and 37. 5 ft2 respectively.
2.8.2Hospital disinfection
Sodium hypochlorite 0.1% was used for disinfection of dental units after every procedure for 1 minute. All commonly touched areas as door handles, furniture, switches, sinks, soap dispensers, counters, x-ray unit were also disinfected and later wiped with wet cloth as sodium hypochlorite is toxic to skin after every four hours according to CDC guidelines [24].
2.8.3Waste disposal
Waste was collected by auxiliary staff member from yellow and white plastic bag-lined baskets designated for contaminated and non-contaminated waste respectively and sharps container. Auxiliary staff member wore mask and gloves during waste collection. Collected waste was sealed in leak resistant biohazard bags and sprayed with 0.5% sodium hypochlorite. The waste was then transported to central waste collecting area of hospital which was taken by waste management company every 12 hours for incineration [27, 28].
3Results
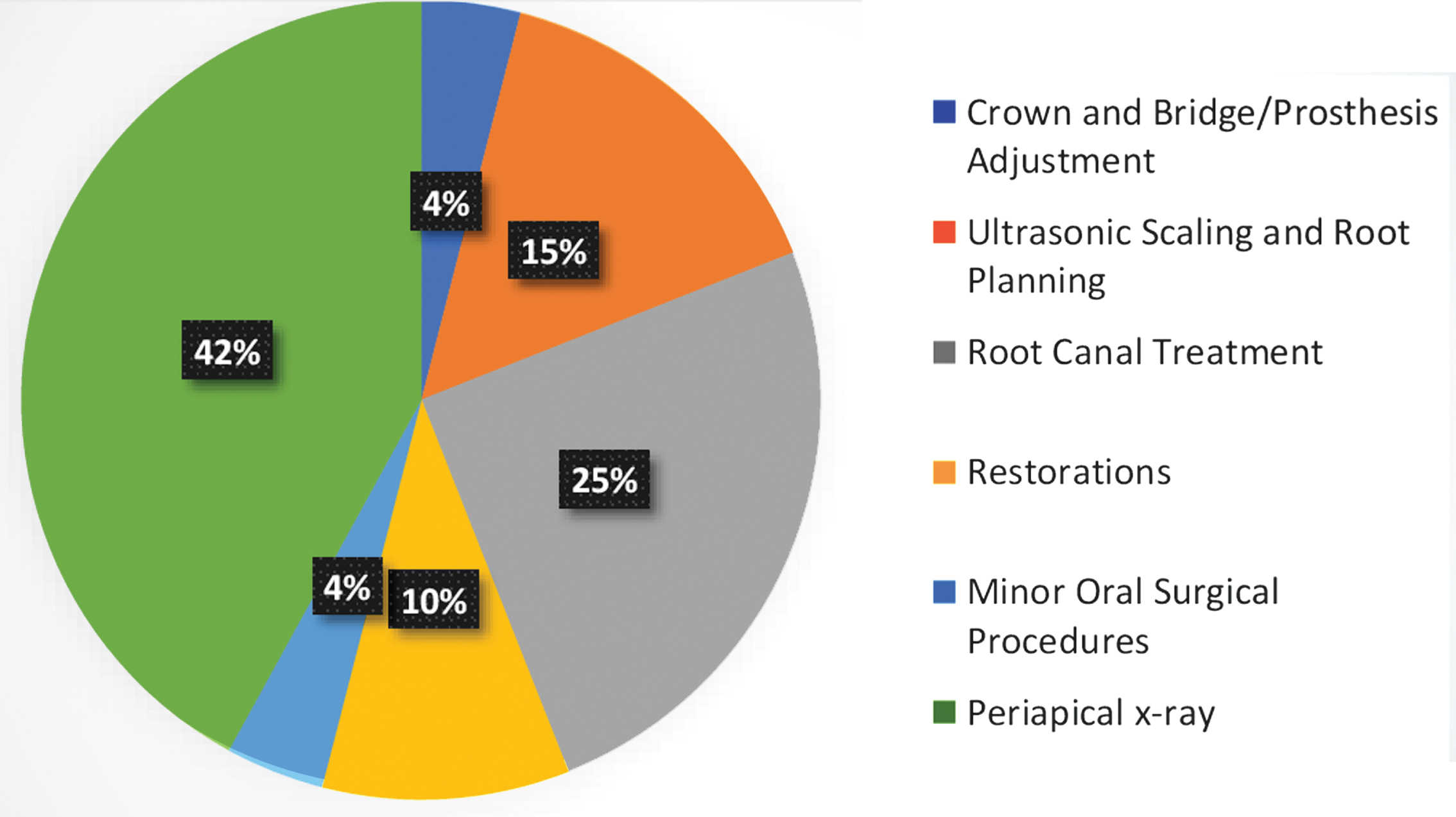
In total, 6372 patients were treated from 1 August 2020 to 31 March 2021. AGPs were performed in 4751 patients, while 1620 non-AGPs were performed. Figure 2 shows frequency of various AGPs performed. During this period no HCP contracted COVID-19 infection from group A. However, one HCP of group B acquired COVID-19 infection, source of which was uncertain. Student t-test between group A and B was insignificant. 1.12% of patients had recent history of contact with COVID-19 patient and were considered as suspected cases of COVID-19. 49.6% had history of domestic travel whereas 0.3% had a history of international travel within last 14 days.
Fig. 2
Frequency of various aerosol generating procedures performed.
4Discussion
The current study assesses the safety of SOPs and action plan followed by a tertiary care dental hospital post COVID-19 lockdown for AGPs and non-AGPs based on the guidelines of Ministry of Health, Pakistan.
The factors that can vary between hospital settings of different countries are the interest of discussion as each country may follow international and national guidelines for COVID-19 based on available resources.
4.1PPE variation (type of mask and gown used for AGPs) in asymptomatic patients
There has been controversy in the recommendation of type of mask used by HCPs for dental procedures. WHO, Public Health England and Swissnoso recommend KN95 respirator use only in suspected or confirmed COVID-19 patients during dental procedures [29–31], whereas CDC, the European Center for Disease Prevention and Control, and the German Robert Koch Institute recommend universal use of KN95 respirators for protection against COVID 19 [32–35]. However, a meta-analysis of 4 RCTs including 6418 patients did not provide any evidence that KN95 respirators were superior to medical/surgical masks for protecting healthcare workers against laboratory confirmed viral infection [36]. An anecdotal report describing no COVID-19 transmission in 35 HCW protected by surgical masks who were exposed to aerosol-generating procedures in the anesthesia department [37].
As in this study protocol, HCPs used surgical mask during dental procedures and only 1 HCP contracted COVID-19 infection. As Student t-test between two groups was insignificant, therefore it can be ascertained that the use of surgical mask is safe in asymptomatic patients for dental procedures. There has been variation in type of gown used in literature like isolation gowns, surgical gowns, and coveralls and each has different advantages and disadvantages [38, 39]. A literature review recommends use of disposable surgical gown [40], also recommended by Ministry of Health, Pakistan [18]. We decided to use sterilized surgical gowns as they effectively protect personnel and patients from cross contamination, are cost effective as they can be easily sterilised. Surgical gowns can be used safely for risk levels 1–4 [39].
4.2Ventilation method
Ventilation of the treatment room is an important factor to ensure safety of AGPs. Ventilation is the process of providing outdoor air to a space or building by natural or mechanical means [41]. Healthcare facilities in both developed and resource-limited countries with favourable climatic conditions can use natural ventilation [42]. Other methods of ventilation for dental hospital are through-the-wall exhausts [43], in-line exhausts with ducts [44], HVAC systems with HEPA filters and negative pressure dental surgery [43], aerosol collectors [45], and UV light [46]. We used natural means of ventilation with sufficient ACH to achieve 99% clearance in less than 10 minutes.
4.3Antimicrobial coolants and pre-procedural mouth rinse
Antimicrobial coolants and pre-procedural rinse were not used for AGPs due to limited sources as NHS Education of Scotland did not recommend its use based on literature review [47].
5Conclusion
Crisis capacity strategy, universal source control measures as well as natural ventilation implemented for dental treatment in asymptomatic patients was assumed to be safe for HCPs during the COVID-19 pandemic, provided patients are screened properly for COVID-19 symptoms, there is no breach in SOPs and room in which procedures are performed is adequately ventilated. Thus, protocols of the Pakistani dental system can be safely adopted worldwide during the COVID-19 pandemic.
Ethical Approval
Ethical approval of the original study was granted by the institutional review boards of the Research and Ethics Committee at the Rashid Latif Medical Complex (reference no. RLDC/005984/20).
Informed consent
Written informed consent was taken from all participants of the study.
Reporting guidelines
The manuscript adhered to the EQUATOR Network reporting guidelines relevant to the research design.
Acknowledgments
Not applicable.
Conflict of interest
None of the authors declare any conflict of interest.
Funding
Not applicable.
References
[1] | https://WHO-2019-nCoV-essentialhealthservices-2020.1-eng.pdf. |
[2] | Ma J . China’s first confirmed COVID-19 case traced back to November 17. In: South China Morning Post. 2020. https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-COVID-19-case-traced-back. Accessed 6 Nov 2020. |
[3] | Abid K , Bari YA , Younas M , Tahir Javaid S , Imran A , Progress of COVID-19 epidemic in Pakistan. Asia Pac J Public Health. 2020. https://doi.org/10.1177/1010539520927259. |
[4] | Cucinotta D , Vanelli M , WHO declares COVID-19 a pandemic. Acta Bio Medica Atenei Parm. (2020) ;91: :157–60. https://doi.org/10.23750/abm.v91i1.9397. |
[5] | Yang Y , Zhou Y , Liu X , Tan J , Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin Oral Investig. 2020;1-4. https://doi.org/10.1007/s00784-020-03267-8. |
[6] | Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-COVID-19-implications-for-ipc-precaution-recommendations. Accessed 6 Nov 2020. |
[7] | Wang J , Du G , COVID-19 may transmit through aerosol. Ir J Med Sci. (2020) ;189: :1143–44. https://doi.org/10.1007/s11845-020-02218-2. |
[8] | Tellier R , Li Y , Cowling BJ , Tang JW , Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect Dis. (2019) ;19: :101. https://doi.org/10.1186/s12879-019-3707-y. |
[9] | Clarkson J , Ramsay C , Richards D , Robertson C , Aceves M , Mitigation of aerosol generating procedures in dentistry - A rapid review. Httpsoralhealthcochraneorgnewsaerosol-Gener-Proced–Their-Mitig-Int-Doc. 2020. |
[10] | CDC. Coronavirus Disease 2019 (COVID-19). In: Cent. Dis. Control Prev. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html Accessed 17Nov 2020 |
[11] | MacDonald DSM , Colosi DC , Mupparapu M , Kumar V , Shintaku WH , Mansur A , Guidelines for oral and maxillofacial imaging: COVID-19 considerations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020. https://doi.org/10.1016/j.oooo.2020.10.017 |
[12] | COVID-19 - Control and Prevention | Denstistry Work- ers and Employers | Occupational Safety and Health Administration. https://www.osha.gov/SLTC/COVID-19/dentistry.html. Accessed 17 Nov 2020. |
[13] | Kampf G , Todt D , Pfaender S , Steinmann E , Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. (2020) ;104: :246–51.https://doi.org/10.1016/j.jhin.2020.01.022. |
[14] | van Doremalen N , Bushmaker T , Morris DH , Holbrook MG , Gamble A , Williamson BN , Tamin A , Harcourt JL , Thornburg NJ , Gerber SI , Lloyd-Smith JO , de Wit E , Munster VJ , Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1.. N Engl JMed. (2020) ;382: :1564–67. https://doi.org/10.1056/NEJMc2004973. |
[15] | Ahmed J , Malik F , Bin Arif T , Majid Z , Chaudhary MA , Ahmad J , Malik M , Khan TM , Khalid M , Availability of personal protective equipment (PPE) among US and pakistani doctors in COVID-19 pandemic. Cureus. (2020) ;12: (6): e8550. https://doi.org/10.7759/cureus.8550. |
[16] | https://www.who.int/publications/i/item/who-2019-nCoVoral-health-2020. https://www.who.int/publications/i/item/who-2019-nCoV-oral-health-2020. Accessed 18 Nov 2020 |
[17] | CDC. Coronavirus Disease 2019 (COVID-19). In: Cent Dis Control Prev. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/general-optimization-strategies.html. Accessed 18 Nov 2020. |
[18] | COVID-19 Health Advisory Platform by Ministry of National Health Services Regulations and Coordination. http://covid.gov.pk/guideline. Accessed 19 Nov 2020. |
[19] | Lauer SA , Grantz KH , Bi Q , Jones FK , Zheng Q , Meredith HR , Azman AS , Reich NG , Lessler J , The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020. https://doi.org/10.7326/M20-0504. |
[20] | ADA develops guidance on dental emergency, nonemergency care. https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-develops-guidance-on-dentalemergency-nonemergency-care. Accessed 6 Nov 2020. |
[21] | Qazi SR , Rehman N , Nasir S , Practice Guidelines Addressing Needs of Pakistani Dentists During the COVID-19 Pandemic Part 2: Recommendations. In: JPDA. http://www.jpda.com.pk/practice-guidelines-addressing-needs-ofpakistani-dentists-during-the-COVID-19-pandemicpart-2-recommendations-2/. Accessed 18 Nov 2020. |
[22] | Lee H-R , Lee Y-H , Yeo M-H , Park S-H , Kim H-R , Park M-J , Park J-Y , Chang K-S , Standardization of disinfection methods according to fabric type§ . Microbiol Soc Korea. (2020) ;56: :285–96. https://doi.org/10.7845/kjm.2020.0064. |
[23] | CDC. Coronavirus Disease 2019 (COVID-19). In: Cent Dis Control Prev. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/eye-protection.html. Accessed 17 Nov 2020. |
[24] | CDC. Communities, Schools, Workplaces, & Events. In: Cent Dis Control Prev. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/cleaningdisinfection.html. Accessed 7 Nov 2020 |
[25] | Atkinson J , World Health Organization Natural ventilation for infection control in health-care settings. World Health Organization, Geneva, 2009. |
[26] | Brouwer M , Katamba A , Katabira ET , van Leth F , An easy tool to assess ventilation in health facilities as part of air-borne transmission prevention: A cross-sectional survey from Uganda. BMC Infect Dis. (2017) ;17: :325. https://doi.org/10.1186/s12879-017-2425-6. |
[27] | Ilyas S , Srivastava RR , Kim H , Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci Total Environ. (2020) ;749: :141652. https://doi.org/10.1016/j.scitotenv.2020.141652. |
[28] | (2019) Air | Appendix | Environmental Guidelines | Guidelines Library | Infection Control | CDC. https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html. Accessed 7 Nov 2020 |
[29] | Requirements and technical specifications of personal protective equipment (PPE) for the novel coronavirus (2019-ncov) in healthcare settings - PAHO/WHO | Pan American Health Organization. http://www.paho.org/en/documents/requirements-and-technical-specifications-personal-protective-equipment-ppe-novel. Accessed 18 Nov 2020. |
[30] | HPS Website - COVID-19-guidance-for-infection-preven tion-and-control-in-healthcare-settings/. https://www.hps.scot.nhs.uk/web-resources-container/COVID-19-guidance-for-infection-prevention-and-control-in-healthcare-settings/. Accessed 17 Nov 2020. |
[31] | Swissnoso, the National Center for Infection Control. COVID-19. https://www.swissnoso.ch/forschung-entwicklung/aktuelle-ereignisse/. Accessed 7 Nov 2020 |
[32] | CDC. Coronavirus Disease 2019 (COVID-19). In: Cent Dis Control Prev. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html. Accessed 17 Nov 2020 |
[33] | RKI - Coronavirus SARS-CoV-2 - COVID-19: Surveillance and Studies at the RKI. 2020. https://www.rki.de/EN/Content/infections/epidemiology/outbreaks/COVID-19/projects/projects.html. Accessed 17 Nov 2020. |
[34] | Sommerstein R , Fux CA , Vuichard-Gysin D , Abbas M , Marschall J , Balmelli C , Troillet N , Harbarth S , Schlegel M , Widmer A , Balmelli C , Eisenring M-C , Harbarth S , Marschall J , Pittet D , Sax H , Schlegel M , Schweiger A , Senn L , Troillet N , Widmer AF , Zanetti G , Swissnoso. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of health-care workers from COVID-19. Antimicrob Resist Infect Control. (2020) ;9: :100. https://doi.org/10.1186/s13756-020-00763-0. |
[35] | Infection prevention and control and preparedness for COVID-19 in healthcare settings - fifth update. In: Eur Cent Dis Prev Control. 2020. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and- preparedness-COVID-19-healthcare-settings. Accessed 18 Nov 2020. |
[36] | Matthews R , Young A , Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: A systematic review and meta-analysis of randomized tri-als. J Emerg Med. (2020) ;59: :165–66. https://doi.org/10.1016/j.jemermed.2020.06.075. |
[37] | Ng K , Poon BH , Kiat Puar TH , Shan Quah JL , Loh WJ , Wong YJ , Tan TY , Raghuram J , COVID-19 and the Risk to health care workers: A case report. Ann Intern Med. 2020. https://doi.org/10.7326/L20-0175. |
[38] | Considerations for Selecting Protective Clothing | NPPTL | NIOSH | CDC. https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html. Accessed 6 Nov 2020 |
[39] | Xiangdong C , You S , Shanglong Y , Renyu L , Henry L , Perioperative care provider’s considerations in managing patients with theCOVID-19 infections. Transl Perioper Pain Med 7. 2020. https://doi.org/10.31480/2330-4871/116. |
[40] | Villani FA , Aiuto R , Paglia L , Re D , COVID-19 and Dentistry: Prevention in Dental Practice, a Literature Review. Int J Environ Res Public Health 17. 2020. https://doi.org/10.3390/ijerph17124609. |
[41] | ISO 17772-1:2017(en), Energy performance of buildings — Indoor environmental quality — Part 1: Indoor environmental input parameters for the design and assessment of energy performance of buildings. https://www.iso.org/obp/ui/#iso:std:iso:17772:-1:ed-1:v1:en. Accessed 6 Nov 2020. |
[42] | Morawska L , Tang JW , Bahnfleth W , Bluyssen PM , Boerstra A , Buonanno G , Cao J , Dancer S , Floto A , Franchimon F , Haworth C , Hogeling J , Isaxon C , Jimenez JL , Kurnitski J , Li Y , Loomans M , Marks G , Marr LC , Mazzarella L , Melikov AK , Miller S , Milton DK , Nazaroff W , Nielsen PV , Noakes C , Peccia J , Querol X , Sekhar C , Seppänen O , Tanabe S , Tellier R , Tham KW , Wargocki P , Wierzbicka A , Yao M , How can airborne transmission of COVID-19 indoors be minimised? Environ Int. (2020) ;142: :105832. https://doi.org/10.1016/j.envint.2020.105832. |
[43] | Sehulster L , Chinn RYW , Guidelines for Environmental Infection Control in Health-Care Facilities: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5210a1.htm. Accessed 18 Nov 2020. |
[44] | Airborne Infectious Disease Management: Methods for Temporary Negative Pressure Isolation. 41. |
[45] | Liu Y , Ning Z , Chen Y , Guo M , Liu Y , Gali NK , Sun L , Duan Y , Cai J , Westerdahl D , Liu X , Xu K , Ho K , Kan H , Fu Q , Lan K , Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 582: ;582: :557–60. https://doi.org/10.1038/s41586-020-2271-3. |
[46] | Andersen BM , Bånrud H , Bøe E , Bjordal O , Drangsholt F , Comparison of UV C light and chemicals for disinfection of surfaces in hospital isolation units. Infect Control Hosp Epidemiol. (2006) ; 27: :729–34. https://doi.org/10.1086/503643. |
[47] | SDCEP Rapid Review onMitigation of Aerosol Generating Procedures in Dentistry published | Scottish Dental. https://www.scottishdental.org/sdcep-rapid-review-on-mitigation-of-aerosol-generating-procedures-in-dentistry-published/. Accessed 18 Nov 2020. |




