Safe practices of biomedical and dental waste management amongst practicing dental professionals amid the COVID-19 pandemic
Abstract
BACKGROUND:
Biomedical waste can potentially compromise the environment and public safety if not safely disposed.
OBJECTIVE:
The aim was to assess the understanding and safe practices of biomedical and dental waste amongst the dental practitioners and practical year students amid the COVID-19 pandemic.
METHODS:
A structured and validated questionnaire consisting of 21 closed ended questions was used to collect data from dental practitioners and students working in hospitals and clinics. The questionnaire was distributed in paper and digital form amongst the participants. Descriptive analysis was performed for categorical and numerical variables. Spearman correlation test was used to assess the relationship between awareness and waste disposal practices of dentists. A p-value of≤0.05 was considered as statistically significant.
RESULTS:
More than three fourth of the participants were aware of proper dental waste disposal steps. One half was aware of the color-coded segregation of biomedical waste management. Two third of the participants were deploying safe biomedical waste practices. Nearly 68% subjects allocated separate labeled containers for disposal of COVID-19 suspected patient’s waste. Furthermore, 71.63% participants were practicing PCR test before aerosol procedures. While 88.65% participants believed that the COVID-19 pandemic has increased the financial burden in terms of safe practices and dental waste management.
CONCLUSION:
The awareness and practices of the participants towards dental waste management was found to be moderate. Satisfactory COVID-19 prevention and transmission measures were observed amongst the participants. BMW management lessons should be included in the academic curriculum and training program needs to be adopted for mass awareness.
1Introduction
Coronavirus disease-2019 (COVID-19) has affected more than 80 million people and have caused more than 1.8 million deaths worldwide as of December 2020. The disease has a wide range of symptoms reported including, fever, cough, shortness of breath, headache, nausea, vomiting, diarrhea and loss of smell or taste. Older people or who have severe underlying medical conditions like heart or lung disease, or diabetes seem to be at higher risk for developing more serious complications from COVID-19. Over a period of time vaccines were developed that continue to reduce a person’s risk of contracting the virus. But it is not known yet that how effective the vaccines will be against the new variants that may arise. In addition to severely compromising the health of people around the globe it has also left a lasting impact on the economies and healthcare infrastructures globally. Dental services like all other health services were forced to adopt immediate restrictions for all kind of oral procedures except for the emergency treatments [1–3]. As the situation improved, dental clinics resumed services and oral health care professionals are providing partial or full range of services depending on the spread of COVID-19 hotspots around the globe [4, 5].
Dental office is a vulnerable site for infection and spread of COVID-19 due to aerosol generation and close individual contact. Therefore, dental practitioners need to adopt standard procedures, not only to curb the transmission of COVID-19, but also to dispose the infectious waste in a manner to avoid cross contamination. As dental services are returning back to pre-pandemic practices, it is highly critical that dental practice be modified to prevent cross infection of COVID-19, not just in the clinical setting but also by other means including waste management [4–7].
The rising need of dental care in the recent times has also increased the demand for new dental clinics, ultimately increasing the amount of biomedical and dental waste [8]. Biomedical waste became a topic of interest back in the 1990s, when Human Immunodeficiency Virus (HIV) and Hepatitis B virus (HBV) became life threatening [9]. Biomedical waste (BMW) is produced during diagnosis, treatment or immunization of humans and animals in hospitals, research institutions, health care teaching institutes, clinics, laboratories, blood banks, animal houses, and veterinary institutes [10]. Waste management is the key for human health as well as for a healthy environment [8]. Inappropriate waste disposal and management can be a risk to healthcare workers, general public as well as the waste handlers, as contaminated waste if improperly managed, may cause health risks and physical injury. In addition, there may be greater risk of nosocomial infections and antibiotic resistance in the event of improper waste management [10].
Dental waste includes the materials that have been used in the dental clinic and then discarded including cotton, latex, sharps, plastic, extracted teeth, lead foil and mercury from amalgam restorations. Dental waste can potentially compromise the environment and public safety if not properly and safely disposed [11]. Alarmingly, majority of the biomedical and dental waste produced is either dumped, incinerated in landfills or left untreated in a water body [12]. Usually, failure to dispose of used syringes and blades properly, increases the chance of reuse and transmission of diseases [13]. The first step towards effective biomedical waste management is the identification and segregation of the waste generated. According to the current guidelines for waste segregation, following colour coding is recommended: yellow container for infectious, pathological and anatomical waste marked “Highly infectious”; yellow plastic bag for sharps, that should be leak and puncture-proof marked “sharp”; brown plastic bag for chemical and pharmaceutical waste; radioactive waste in a lead box marked with a radiation symbol and black plastic bag for general healthcare waste [14].
There are usually two ways to dispose the biomedical waste (BMW) produced by the dental clinics i.e., landfills and incineration [12]. When landfills are not created carefully, it can contaminate drinking water; and incineration itself can emit harmful fumes and ashes. The waste management remains a major challenge in many countries including Pakistan as there is no conventional place for the disposal [14]. It is therefore important for all healthcare workers including dental care providers to have sufficient understanding regarding dental waste management, its segregation, treatment, storage, transportation and disposal [15–17]. The data on safe practices of biomedical waste is limited and the present study will provide baseline information for assessing future risks from improper waste management in pandemics. The present study thus aims to assess the understanding and safe practices of biomedical and dental waste amongst the dental practitioners and also provides an insight on the method of disposing infected/used needles in relation to the type of practice of the practitioners.
2Material and methods
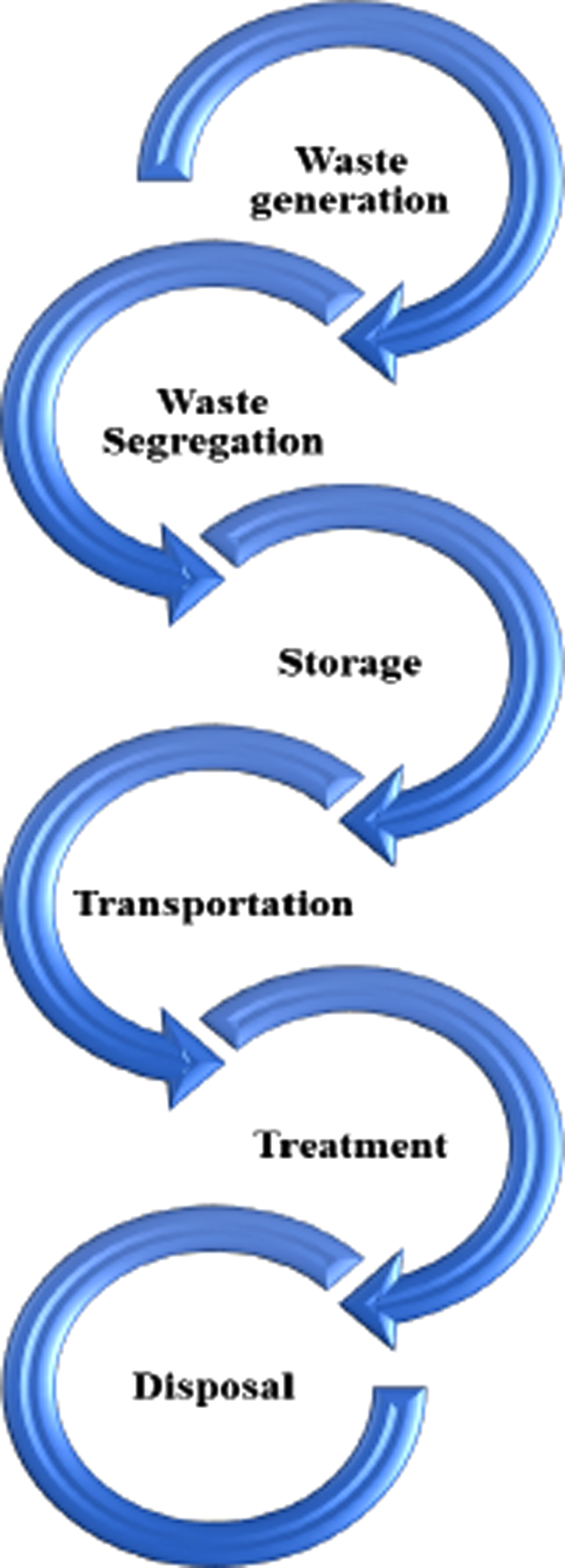
This cross-sectional study was conducted at dental hospitals and clinics, over a period of 5 months i.e., from September 2020 to January 2021. The sample size was calculated with OpenEpi software. Considering the mean knowledge and behaviour score of dentists (3.7±1.3), at 80% power and confidence interval of 95%, the estimated sample size was 505 participants [17]. The sample size was overestimated to 564 participants for maximum participation. A non-probability convenience sampling technique was applied to recruit participants. A self-administered structured questionnaire was used to collect the data (Appendix). Section one of the questionnaire focussed on assessment of the understanding about biomedical and dental waste and its management, using 12 close ended questions. The questions included, guidelines laid down by government, consequences without proper BMW management, BMW rules, categories and colour coded waste segregation. Section two assessed practices with six closed ended questions; including, BMW inclusion into the curriculum, use of PPE’s, method of disposal used in self-practice, items on COVID-19 patient waste disposal and emphases on the polymerase chain reaction (PCR) test to detect COVID-19 patients. The internal consistencies of questionnaire items were assessed through Cronbach’s alpha (α= 0.70). The flow diagram depicting standard BMW waste management is shown in Fig. 1.
Fig. 1
Steps of biomedical waste management.
The data were collected through distributing copies of the questionnaire as well as digital files using Google forms. The link of digital questionnaires was created and shared with the dental practitioners who could not be approached in person. The sample size for participants was 600 practicing dentists at private clinics and government dental hospitals including undergraduate students.
The data were analysed using Statistical program for social sciences (SPSS- version 25, IBM, NY, USA). Descriptive analysis was performed to analyse mean, standard deviation and frequency of categorical and continuous variables. Spearman correlation was applied to identify relationship between awareness and practices of BMW amongst dental practitioners. A p-value of≤0.05 was considered significant.
3Results
Five hundred and sixty four (564) participants’ submitted complete responses. 161 (28.5%) were males and 403 were (71.5%) females. Two hundred and forty three were undergraduate students, 204 were graduates, and 117 postgraduates. Both public and private sector dentist were included; 441 participants were from private sector while 123 were from public sector (Table 1).
Table 1
Demographics characteristics of participants (n = 564)
| Variables | N | % |
| Gender | ||
| Male | 161 | 28.5 |
| Female | 403 | 71.5 |
| Educational qualification | ||
| Undergraduate | 243 | 43.1 |
| Graduate | 204 | 36.2 |
| Postgraduate | 117 | 20.7 |
| Sector | ||
| Private | 441 | 78.2 |
| Public | 123 | 21.8 |
| Practice | ||
| General dental clinics | 144 | 25.5 |
| Training positions | 394 | 69.9 |
| Both | 26 | 4.6 |
N: Frequency, % : percentage.
Table 2 shows that 208(36.9%) participants believed that guidelines have been laid down by the government for BMW management, whereas 469 participants (83.2%) believed that an ongoing coordination between governmental bodies, institutes and health personnel will lead to proper BMW management. 477 (84.6%) participants agreed that there are consequences and health hazards without proper biomedical waste management, while 58.9% participants were aware of the different biomedical and dental waste categories.
Table 2
Distribution of biomedical and dental waste awareness level and its management amongst participants (n = 564)
| Variables | Yes | No | Do not know | |||
| N | % | N | % | N | % | |
| Guidelines laid down by the government for BMW management? | 208 | 36.9 | 91 | 16.1 | 265 | 47.0 |
| Coordination between governmental bodies, institutions and health personnel will lead to proper BMW management? | 469 | 83.2 | 40 | 7.1 | 55 | 9.8 |
| Consequences/ health hazards without proper biomedical waste management? | 477 | 84.6 | 44 | 7.8 | 43 | 7.6 |
| Aware of different categories of biomedical and dental waste? | 332 | 58.9 | 140 | 24.8 | 92 | 16.3 |
| Knowledge about the color coded segregation of BMW? | 324 | 57.4 | 101 | 17.9 | 139 | 24.6 |
N: Frequency, % : percentage; BMW: Biomedical waste.
When asked about the first step for BMW management, 331 (58.7%) believed that it was segregation. However, 151 (26.8%) participants thought it was disposal, 49 (8.7%) opted for storage, 22 (3-0.9%) said treatment and 11 (2.0%) believed it to be transport. Regarding biomedical and dental waste storage duration, 191 participants (33.9%) said that it should not be stored beyond 48 hours, 157 (27.8%) said that waste should not be stored beyond 12 hours, 37 (6.6%) opted for 72 hours. 179 (31.7%) subjects did not know the storage duration for BMW (Table 3).
Table 3
Distribution of biomedical and dental waste awareness level and its management amongst participants (n = 564)
| Variables | N | % | N | % | N | % | N | % | N | % |
| Storage | Segregation | Treatment | Transportation | Disposal | ||||||
| The first step for BMW management? | 49 | 8.7 | 331 | 58.7 | 22 | 3.9 | 11 | 2.0 | 151 | 26.8 |
| Waste should not be stored beyond a time period of? | 12 hrs | 48 hrs | 72 hrs | 96 hrs | Do not know | |||||
| 157 | 27.8 | 191 | 33.9 | 37 | 6.6 | 179 | 31.7 | 179 | 31.7 | |
N: Frequency, % : Percentage, hrs: Hours.
Regarding color-coded segregation of BMW, 57.4% believed that they knew color coding of BMW (Table 2). However on assessment, 37.2% of the participants did not know about the color coded bag used for disposing off used impression materials, expired dental materials and discarded medicines, 17% said these are disposed off in black, 15.2% said yellow, 9.6% said blue, 13.7% said green while 7.3% said red. Regarding the color of bag for disposing used radiographic films, metals and gloves, 37.6% were unaware, 15.6% preferred black, 13.5% selected red, 13.1% chose green, 11.9% selected yellow while 8.3% opted for blue (Table 4). Regarding the color-coded bag used for disposing off used sharps and needles, 52.5% said red while, 25.2% were unaware. Other selections included 9.8%, 7.1%, 4.6% and 0.9% of yellow, black, blue and green respectively. Regarding the color of bag used for disposing extracted teeth and/or human tissues, 35.1% did not know, 29.3% selected red, 14.2% preferred yellow, 9.4% opted black, 8% chose blue and 4.1% selected green. However, when the understanding regarding the color of bag for mercury or scrap of silver amalgam was assessed, 47.2% did not know. However, 23.9%, 9.2%, 8.3%, 6.4% and 5% participants selected black, yellow, green, red and blue colors respectively.
Table 4
Distribution of awareness level of biomedical and dental waste disposal (n = 564)
| Red | Black | Yellow | Blue | Green | Do not know | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Bag for used impression materials, expired dental | 41 | 7.3 | 96 | 17.0 | 86 | 15.2 | 54 | 9.6 | 77 | 13.7 | 210 | 37.2 |
| materials and discarded medicines | ||||||||||||
| Bag for used radiographic films, metals and gloves | 76 | 13.5 | 88 | 15.6 | 67 | 11.9 | 47 | 8.3 | 74 | 13.1 | 212 | 37.6 |
| Bag for used sharps and needles | 296 | 52.5 | 40 | 7.1 | 55 | 9.8 | 26 | 4.6 | 5 | 0.9 | 142 | 25.2 |
| Bag for extracted teeth and/or human tissues | 165 | 29.3 | 53 | 9.4 | 80 | 14.2 | 45 | 8.0 | 23 | 4.1 | 198 | 35.1 |
| Bag for mercury or scrap of silver amalgam? | 36 | 6.4 | 135 | 23.9 | 52 | 9.2 | 28 | 5.0 | 47 | 8.3 | 266 | 47.2 |
N: Frequency, % : percentage.
Table 5 presents the safe practices of biomedical and dental waste amongst the participants. 94.3% believed that there is a need of including educational program for BMW management in the academic curriculum, whereas 3.9% said no and 1.8% did not know. 92.4% of participants believed that waste handlers should use personal protective equipment, 2.8% said no while 4.8% did not know. Regarding practicing segregation of different types of waste, 56.4% participants agreed, 30.1% said no, while 13.5% did not know. 58.7% participants did not dispose of biomedical and dental waste themselves at their practice, while 34.8% agreed and 6.6% were unaware. 77.4% believed that sharp cutters should be used to cut all syringes and blades, 14.5% did not agree and 8.1% were unaware. 72.2% (407) participants disposed infected needles by breaking in sharp container, while 16.8% (95) broke needles and disposed them in common bin. 380 (67.37%) participants confirmed the use of separately labeled bins and container for the suspected COVID-19 patients and cross contamination prevention. To curtail the spread of SARS CoV-2; nasal swab and PCR test was practiced by 404 (71.63%) participants. 500 (88.65%) participants reported that due to the COVID-19 pandemic the financial burden has increased. Forty (7.09%) participants reported no financial burden so far at their dental practice.
Table 5
Distribution of safe practices amongst participants (n = 564)
| Variables | Yes | No | Do not know | |||
| N | % | N | % | N | % | |
| Need of including educational program for BMW management in the curriculum? | 532 | 94.3 | 22 | 3.9 | 10 | 1.8 |
| Waste handlers should use personal protective equipment? | 521 | 92.4 | 16 | 2.8 | 27 | 4.8 |
| Different types of waste segregated at practice? | 318 | 56.4 | 170 | 30.1 | 76 | 13.5 |
| Disposing biomedical and dental waste yourself? | 196 | 34.8 | 331 | 58.7 | 37 | 6.6 |
| Sharp cutters should be used to cut all syringes and blades? | 454 | 80.5 | 454 | 80.5 | 43 | 7.6 |
| Are there separately labelled bins and container for the suspected COVID-19 patient waste in your practice? | 380 | 67.37 | 120 | 21.27 | 64 | 11.34 |
| Are you prescribing nasal swab PCR to your patient prior aerosol generated procedures? | 404 | 71.63 | 100 | 17.73 | 60 | 10.63 |
| Has the COVID-19 pandemic increased financial burden on biomedical n dental waste management? | 500 | 88.65 | 40 | 7.09 | 26 | 4.60 |
N: Frequency, % : percentage.
Table 6, presents the relationship between the type of practice and the method of disposal of infected needles. Among the three fourth participants working in training positions, 281 (49.82%) broke needles and disposed them in designated sharp containers, 74 (13.12%) disposed needles in common dust bin after breaking, while 39 (6.91%) disposed them in common bins without breaking. Furthermore, among the one participants working in general dental clinics, 109 (19.32%) broke needles and disposed them in a sharp container, 15 (2.65%) disposed it in a common container and 20 (3.54%) participants disposed needles in a common bin without breaking. There was no significant relation (p = 0.37) between type of practices and awareness of dental waste disposal amongst the participants.
Table 6
Relationship between the type of practice and method of disposing infected needles (n = 564)
| Variables | Dispose in Common bin | Break needle and dispose in common bin | Break needle and dispose in sharps container | Correlationα | P valueβ | |||
| General dental clinics | 20 | 3.54 | 15 | 2.65 | 109 | 19.32 | –0.03 | 0.37 |
| Training positions | 39 | 6.91 | 74 | 13.12 | 281 | 49.82 | ||
| Both | 3 | 0.53 | 6 | 1.06 | 17 | 3.01 | ||
αSpearman correlation test; βlevel of significance was set at p≤0.05.
4Discussion
Adequate biomedical waste (BMW) disposal is one of the neglected aspects of health care for years especially in developing countries. The situation got worst due to the excessive use of PPEs, including gloves, masks, gowns and other protective equipment amidst COVID-19. According to a study by Jalal et al, healthcare practitioners (HCPs) of some countries lack adequate knowledge regarding BMW; they dispose the wastes in litterbins along with other general household waste instead of considering the use of specific color coded bags for disposal. This might increase the chances of infection and transmission especially in the current COVID-19 pandemic [18, 19]. Additionally, HCPs are expected to have sufficient knowledge regarding BMW since it is estimated that 10–25% of it is infectious [20]. Therefore, the present study was performed to evaluate the understanding and practices of dental professionals in relation to dental waste management.
Biomedical and dental waste (BMDW) is an emerging issue and therefore requires active involvement and harmonization between the government, medical vicinities and all healthcare personnel. However in the present study, only 36.9% of respondents believed that there are certain guidelines provided by the government for BMW management; majority i.e. 47% did not even know if there were any guidelines laid down by the government to be followed. This may be due to the fact that 43.1% of respondents were undergraduates and had limited knowledge in this regard. This is similar to a study by Singh et al, where less than 50% of the students were aware about the guidelines laid down by government of Nepal for BMW management [21]. In addition, 83.2% of the respondents in our study believed that a strong coordination between governmental bodies and institutions might help in proper waste management. Literature suggests that in addition to the policies given, the knowledge regarding dental waste management should be continuously updated and monitored by the authorized bodies. It is reported previously, that 94.3% of the respondents believe in the need of inclusion of educational program regarding BMW management in the curriculum [22, 23]. Furthermore, majority of the respondents of the present study (84.6%) were aware of the consequences/health hazards associated with improper waste management; however, 58.9% were aware of different categories of biomedical and dental waste. This is critical as inadequate knowledge of handling waste may result in environmental degradation and can harm the community especially during a pandemic [24].
Moreover, as literature proves that waste segregation is a vital step of waste management and color-coding helps in taking the waste to different sites for disposal, therefore putting wrong waste in a designated container would invalidate the efforts of appropriate waste disposal [25]. Although 58.7% of the respondents in this study correctly answered that segregation should be the first step of BMW management, however, 57.4% of the respondents believed that they knew about different color-coding for the biomedical waste. However, only 4.6% of the respondents in the present study knew the correct color code, showing lack of color-coding application amongst the dental professionals. However similar findings were also reported in previous studies [26].
The management of dental waste is of utmost importance in the pandemic due to risk of cross contamination. In the present study to prevent contamination, 67.37% participants used separately labelled bins for disposing off suspected COVID-19 patient’s waste. Dental waste from suspected and confirmed COVID-19 patients was considered as infectious medical waste and should be stored in a tight knot, double layered, yellow clinical bag. The surface of respected bag should be labelled and disposed as medical waste [27]. It was also found that participants were making sure to treat patients free of COVID-19, when aerosol generated procedures were performed, as a prior nasal swab and PCR test was ordered by 71.63% of participants for patients. COVID-19 testing should be required for suspected cases with or without COVID-19 symptoms in order to prevent transfer of infections in the community [28].
Furthermore, sharp instruments such as needles and syringes are the most common hazardous waste in dental practice. The nature of dental practice in terms of waste management was assessed in this study and it was found that majority of the respondents, (72.16%) is following safe practices as they break the needle and dispose it off in sharps container. These findings are similar to the study by Naidu et al, where 65.5% of the dentists practiced the recommended needle disposal protocol [29]. 56.4% of the dentists in the present study agreed to practice waste segregation. These numbers are very low, compared to a previous study by Reddy et al., which showed 99.2% of dentists to be segregating dental waste [30]. Therefore, despite the awareness among dental practitioners, training and surveillance is required to ensure waste segregation and management practices.
The present study highlights the critical problems, which can be avoided by safe BMW management practices, however a causal relationship of the awareness to the environmental hazards, specifically COVID-19 infections was not assessed. Therefore it is critical to correlate infection rates with BMDW management practices, in future studies. Moreover, it is suggested that the governing bodies should revise the guidelines and policies by keeping COVID-19 into consideration and should strictly implement them. Furthermore, training programs and regular refresher sessions should be organized on recommended BMW management protocols, including the segregation and color coding of the waste for the doctors, nurses, technicians and other staff members of dental hospital and clinics.
5Conclusion
The awareness and practices of the participants towards dental waste management was found to be moderate. Satisfactory COVID-19 prevention and transmission measures were observed amongst the participants. BMW management lessons should be included in the academic curriculum and training program needs to be adopted for mass awareness.
Author contributions
NA and MSA: Data interpretation, manuscript writing, final and critical approval. FV and TA: Manuscript drafting, literature review, final manuscript approval. AA and QM: Concept and study design, data collection, literature review, manuscript writing. RN: Data acquisition, data interpretation, literature review. AR: Data collection, writing, revise, editing.
Conflict of interest
The authors declare no conflict of interest.
Supplementary materials
[1] The appendix is available from https://dx.doi.org/10.3233/WOR-211099.
Acknowledgments
The authors are grateful to the Researchers supporting project at King Saud University for funding through Researchers supporting project No. (RSP-2020-240).
References
[1] | So MKP , Chu AMY , Tiwari A , et al. On topological properties of COVID- predicting and assessing pandemic risk with network statistics. Sci Rep. (2021) ;11: :5112. https://doi.org/10.1038/s41598-021-84094-z. |
[2] | Abbasi MS , Ahmed N , Sajjad B , Alshahrani A , Saeed S , Sarfaraz S , Alhamdan RS , Vohra F , Abduljabbar T . E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work. (2020) ;67: :549–56. |
[3] | Dargahi A , Jeddi F , Ghobadi H , Vosoughi M , Karami C , Sarailoo M , Hadisi A , Mokhtari SA , Haghighi SB , Sadeghi H , Alighadri M . Evaluation of masks’ internal and external surfaces used by health care workers and patients in coronavirus-2 (SARS-CoV-2) wards. Environ Res. (2021) ;196: :110948. doi: 10.1016/j.envres.2021.110948. |
[4] | Ahmed MA , Jouhar R , Ahmed N , Adnan S , Aftab M , Zafar MS , Khurshid Z . Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. International Journal of Environmental Research and Public Health. (2020) ;17: (8):2821. |
[5] | Ahmed N , Shakoor M , Vohra F , Abduljabbar T , Mariam Q , Rehman MA . Knowledge, awareness and practice of health care professionals amid SARS-CoV-2, corona virus disease outbreak. Pakistan Journal of Medical Sciences. (2020) ;36: (COVID19-S4):S49. |
[6] | Dargahi A , Jeddi F , Vosoughi M , Karami C , Hadisi A , Ahamad Mokhtari S , Ghobadi H , Alighadri M , Haghighi SB , Sadeghi H . Investigation of SARS CoV-2 virus in environmental surface. Environ Res. (2021) ;195: :110765. doi: 10.1016/j.envres.2021.110765. |
[7] | Sarailoo M , Matin S , Vosoughi M , Dargahi A , Gholizadeh H , Damavandi MR , Abbasi-Ghahramanloo A , Kamran A . Investigating the relationship between occupation and SARS-CoV2. Work. (2021) ;68: (1):27–32. doi: 10.3233/WOR-205066. |
[8] | Singh RD , Jurel SK , Tripathi S , Agrawal KK , Kumari R . Mercury and other biomedical waste management practices among dental practitioners in India. BioMed Research International. (2014) ;2014: . |
[9] | Awasthi PK , Kumar G , Sinha A . Biomedical Waste Management: An Approach To Reduce Environmental Pollution. Int J Innov Res Adv Stud. (2018) ;5: (2):1235. |
[10] | Hegde V , Kulkarni RD , Ajantha GS . Biomedical waste management. Journal of Oral and Maxillofacial Pathology. (2007) ;11: (1):5. |
[11] | Singh AK , Humagain M , Khanal N . Recommendations based on International Guidelines for Safe Dental Practice During Covid-19. Journal of Nepalese Society of Periodontology and Oral Implantology. 28. (2020) ;4: (1):22–30. |
[12] | Abhishek KN , Supreetha S , Varma Penumatsa N , Sam G , Khanapure SC , Sivarajan S . Awareness-knowledge and practices of dental waste management among private practitioners. Kathmandu Univ Med J. (2016) ;14: (53):17–21. |
[13] | Ranjan R , Pathak R , Singh DK , Jalaluddin M , Kore SA , Kore AR . Awareness about biomedical waste management and knowledge of effective recycling of dental materials among dental students. Journal of International Society of Preventive & Community Dentistry. (2016) ;6: (5):474. |
[14] | Arshad N , Nayyar S , Amin F , Mahmood KT . Hospital waste disposal: A review article. Journal of Pharmaceutical Sciences and Research. (2011) ;3: (8):1412. |
[15] | Naz S , Naqvi SM , Jafry SI , Asim S . Knowledge, attitude and practice regarding management of health care waste among private dental practitioners. JPMA. The Journal of the Pakistan Medical Association. (2020) ;70: (7):1259–62. |
[16] | Sibanda LK , Obange N , Awuor FO . Challenges of solid waste managementin Kisumu, Kenya. InUrban Forum. (2017) ;28: (4):387–402. |
[17] | Sabbahi DA , El-Naggar HM , Zahran MH . Management of Dental Waste in Dental Offices and Clinics in Jeddah, Saudi Arabia. Journal of the Air & Waste Management Association. (2020) ;12: (3):30. |
[18] | Jalal SM , Akhter F , Abdelhafez AI , Alrajeh AM . Assessment of Knowledge, Practice and Attitude about Biomedical Waste Management among Healthcare Professionals during COVID-19 Crises in Al-Ahsa. Healthcare. (2021) ;9: (6):747. https://doi.org/10.3390/healthcare9060747 |
[19] | Vosoughi M , Karami C , Dargahi A , et al. Investigation of SARS-CoV-2 in hospital indoor air of COVID-19 patients’ ward with impinger method. Environ Sci Pollut Res. (2021) ;28: :50480–8. https://doi.org/10.1007/s11356-021-14260-3 |
[20] | Mehta TK , Shah PD , Tiwari KD . A knowledge, attitude and practicestudy of biomedical waste management and bio-safety among healthcareworkers in a tertiary care government hospitalin Western India. Natl J Community Med. (2018) ;9: :327–33. |
[21] | Singh T , Ghimire TR , Agrawal SK . Awareness of biomedical waste management in dental students in different dental colleges in Nepal. BioMed Research International. 2018;9;2018. |
[22] | GV U DG , Basu M . Assessment of knowledge, attitude and practices of dental waste management among undergraduate dental students of Bapuji Dental College and Hospital in Davangere City-a cross sectional survey. Unique J Med Dent Sci. (2016) ;4: :8–13. |
[23] | Indhulekha V , Ganapathy D , Jain AR . Knowledge and awareness on biomedical waste management among students of four dental colleges in Chennai, India. Drug Invention Today. (2018) ;10: (12):32–41. |
[24] | Pawar PA , Patil TS . Knowledge, practice and attitude of dental care waste management among private dental practitioners in Latur city. International Dental Journal of Students Research. (2017) ;5: :80–4. |
[25] | Sudeep CB , Joseph J , Chaitra T , Joselin J , Nithin P , Jose J . KAP study to assess biomedical waste management in a dental college in south India. World J Pharm Pharm Sci. (2017) ;6: :1788–94. |
[26] | Al-Oufi L , Saker S . Knowledge and Practice of Dental Waste Management among Undergraduate Dental Students and Interns in College of Dentistry, Taibah University, Saudi Arabia. Journal of Advances in Medicine and Medical Research. (2018) ;30: :1–7. |
[27] | Fini MB . What dentists need to know about COVID-19. Oral oncology. (2020) ;28: :104741. |
[28] | Giudice A , Antonelli A , Bennardo F . To test or not to test? An opportunity to restart dentistry sustainably in the ‘COVID-19 era’. International Endodontic Journal. (2020) ;53: (7):1020–1. |
[29] | Naidu SG , Reddy VC , Kumar RV , Sudhir KM , Srinivasulu G , Athuluru D . Dental health-care waste management among dentists of Nellore City-A cross-sectional study. Journal of Indian Association of Public Health Dentistry. (2019) ;17: (2):136. |
[30] | Karami C , Dargahi A , Vosoughi M , et al. SARS-CoV-2 in municipal wastewater treatment plant, collection network, and hospital wastewater. Environ Sci Pollut Res (2021). https://doi.org/10.1007/s11356-021-15374-4 |




