Healing the wounds of workplace bullying: Evaluating mental health and workplace participation among victims seeking treatment for common mental disorders
Abstract
BACKGROUND:
Victims of workplace bullying represent a group characterised by severe negative health complaints at risk of losing their foothold in working life. To date, very few studies have investigated the effect of psychological treatment of the health-related problems often facing victims of bullying.
OBJECTIVE:
The aim was to investigate if victims of workplace bullying suffering from common mental disorders (CMD) benefit from clinical treatment for their mental health problems at an outpatient clinic treating patients using Metacognitive or Cognitive Behavioural Therapy with work-focus. Criteria were symptom reduction and change in workplace participation. Comparisons were made between the victims of workplace bullying with CMD, a wait-list control group consisting of patients who had also been exposed to bullying yet now awaiting treatment, and other patients not exposed to bullying.
METHODS:
The sample comprised of 405 patients from an outpatient clinic in Norway. The study used a naturalistic observational design and data was collected pre-treatment and post-treatment.
RESULTS:
The results showed the treatment to be effective in symptom reduction for victims of bullying to a similar degree as patients otherwise not exposed to bullying. Even more, victims receiving treatment had a larger improvement compared to the wait-list control group (p < 0.001). Yet, among patients on sick leave pre-treatment, fewer victims of bullying were fully working by the end of treatment compared to the patients not exposed to workplace bullying.
CONCLUSION:
The findings provide ground for optimism for this treatment as an efficient way of dealing with the aftermath of workplace bullying.
1Introduction
Over the last three decades, workplace bullying is firmly documented as a severe and even traumatic social stressor facing employees in all professions and industries all around the globe [1], and with devasting effects on the mental health and well-being of those targeted [2]. It comes in many forms and may be of a personal or a work-related nature. It may be verbal or non-verbal, direct or indirect. Yet, it is often of a subtle and indirect nature and often with elements of social exclusion. Workplace bullying is however mainly characterised by the systematic exposure to unwanted negative behaviour, often taking place over a prolonged period of time [3]. Bullying is generally a gradually escalating process, and the duration and intensity of these negative behaviours may therefore vary. Central in the concept is the imbalance of power involved, with the victim being in or gradually being moved into an inferior position, and consequently having difficulty in defending themself in the actual situations [4, 5].
Hence, victims of ongoing and long-term workplace bullying represent a group characterised with severe negative health complaints, such as musculoskeletal complaints [6], common mental disorders (CMD) in the form of anxiety and depression [2, 7], and even symptoms of post-traumatic stress [8, 9]. The negative health effects may become long-lasting, and some longitudinal studies have confirmed that these negative outcomes may persist over several years [10, 11], and long after the bullying may have ceased [12].
In a recent study, we identified that almost 26% of patients seeking treatment for CMD reported to be victims of workplace bullying [13]. In Norway, where the study was conducted, studies have typically shown the prevalence of bullying in working life to be in the area of 4 to 12% depending on estimation method [14]. By comparison, patients who reported to be victims of bullying were twice as likely to be on full-time sick leave and reported significantly more severe health complaints than patients not exposed to bullying [13]. Thus, these individuals represent a vulnerable group, in need of treatment and in danger of losing their foothold in working life [15]. Hence, the development and evaluation of possible clinical treatment procedures for the aftermath of exposure to bullying is of utmost importance [see also 16, 17]. In this regard, it is important to investigate whether they benefit from psychological therapy to the same extent as other patients with CMD. Alternatively, more specialised treatment procedures need to be developed to address this patient group [see 17, 18]. To date, very few studies have investigated the effect of psychological treatment on the health-related problems often facing victims of workplace bullying, as is the focus of the present study.
However, in Germany an inpatient clinic, dedicated to the treatment of victims of workplace bullying, was established over 20 years ago [16]. The treatment requires the patients to be admitted to the clinic for six to eight weeks and aims to reduce symptoms and help patients either secure or re-establish their work ability and their employee role [16]. The therapy offered is based on Cognitive Behavioural Therapy (CBT) and the treatment programme has been formulated in accordance with well-established, clinical concepts, and linked to findings from workplace bullying research. Thereby, creating a tailor-made therapy for this patient group. The therapy has been shown to have a good effect on this patient group in terms of helping reduce symptoms and increasing their rate of employability [16]. Thus, CBT appears to be effective for this patient group. Nevertheless, this treatment is very time consuming, expensive, and demanding, requiring a significant number of financial and clinical resources [16]. Knowledge of effective treatment programmes to be offered in outpatient clinics is therefore warranted for this patient group.
One of the most established therapies to treat CMD is CBT and is often considered best practise, when treating depression and anxiety [19, 20]. Metacognitive Therapy (MCT) is a more recent therapy, that has greatly benefited patients with CMD [21]. CBT focuses mainly on challenging the validity and content of negative thoughts and attempts to change negative thoughts, and behavioural interventions [22, 23]. In contrast, MCT focuses on aspects of information processing based on the Self-Regulatory Executive Function (S-REF) model [24, 25]. This model postulates that for patients’ metacognitions form the basis of a cognitive attentional syndrome (CAS) which involve thought processes like rumination, worry, threat monitoring as well as maladaptive coping strategies. Challenging the metacognitions and the CAS is the basis for change in MCT [21]. Both CBT and MCT have been proven to be effective when treating CMD, however, some comparative studies have indicated that MCT might be superior to CBT [26].
Although CBT has shown effects on symptom reduction, there have been mixed results when examining whether reduction of symptoms alone, can in turn, reduce the duration of sick leave [e.g., 27, 28]. When combining standard CBT and a work-focused component, several studies have found that this treatment appears to reduce sick leave for patients with CMD more efficiently than CBT alone [29, 30]. These findings have been supported by several meta-analyses, indicating that CBT with a work-focus can help reduce symptoms and the duration of patients’ sick leave [e.g., 31]. Similar results have also been found in a study by Gjengedal et al. [32], with a similar patient population as the present study, when combining a work-focused component with MCT and CBT. The results indicated that the treatment was effective in terms of both symptom reduction and return to work among patients with CMD [32]. However, it is still unknown whether this treatment will be as effective for patients with CMD and a history of workplace bullying, as the mental health problems they are experiencing may be both an outcome of their work and a hinderance in holding onto an employee role. Thus, based on the promising results from combining MCT or CBT with a work-focus, there is a need for effectiveness studies of this approach for individuals struggling with the aftermath of workplace bullying. A vast amount of research has documented exclusion from working life following sick leave to be a major risk for victims of bullying suffering mental health problems [e.g., 33]. Hence, treatment should also focus on this aspect. By focusing on the return to work process in combination with therapy for CMD, it is possible to enhance not only symptom recovery, but also functional recovery by increasing the patient’s self-efficacy [34]. Return to work self-efficacy (RTW-SE) has become a valuable concept in the return to work research and refers to the individuals’ confidence in their own ability to function well at work, despite suffering from CMD [35]. The concept has been found to be a robust predictor of the capability to return to work among individuals with CMD [29, 36], with results suggesting that it can predict a full return to work at follow up three, six, and 12-months post-treatment [37]. In a recent study on a similar patient population to the present study, we found that patients exposed to workplace bullying pre-treatment had significantly lower RTW-SE scores, compared to patients who were not bullied [13].
Considering this and the detrimental effects resulting from the aftermath of workplace bullying, it is likely that victims of bullying will require treatment to help reduce the severe health problems they are experiencing including building a stronger RTW-SE to secure a firm foothold in working life. It is also worth noting that there is little known about age and gender differences in who seeks mental health care services among victims of workplace bullying. It is however well documented in the research literature that women are more likely than men to seek mental health care services in the general population [38–40], but it is less clear when it comes to age differences [39–41].
In the present study we investigate the effects of a MCT or CBT with a work-focus in terms of symptoms reduction and the patients’ belief in their ability to return to work. In this regard a comparison was made between the victims of workplace bullying with CMD with the majority of patients who had not been exposed to bullying. Furthermore, we used a wait-list control group consisting of patients who had also been exposed to bullying awaiting treatment. The following Research Questions (RQ) will be examined:
RQ 1a) Will victims of bullying have a decrease in depressive symptoms, symptoms of anxiety, and subjective health complaints, after MCT or CBT with work-focus, compared with a wait-list control group consisting of patients who had been exposed to bullying but were awaiting treatment? 1b) Will the victims of bullying have a similar change in symptoms as the patients not exposed to bullying after treatment?
RQ 2a) Will victims of bullying have an increase in RTW-SE, after MCT or CBT with work-focus, compared with a wait-list control group consisting of patients who had been exposed to bullying but were awaiting treatment? 2b) Will the victims of bullying have a similar change in RTW-SE as the patients not exposed to bullying after treatment?
In addition, we will investigate the effect of the treatment among the patients that were on sick leave during the intake process pre-treatment to see if there is a difference between the victims of bullying and patients not exposed to bullying regarding actual return to work. The following RQ will be examined:
RQ 3) Will MCT or CBT with work-focus be as effective among victims of bullying in respect to actual return to work after sick leave compared with patients not exposed to bullying?
2Material and methods
2.1Participants
The sample consisted of 423 patients with all data obtained between May 2017 and June 2020 from a mental health outpatient clinic at Diakonhjemmet Hospital in Oslo, Norway. Out of the 423 patients 405 patients had completed the Short Negative Acts Questionnaire which was a requirement for being included in the analyses. The data used originated from a naturalistic observational study in the project “The Norwegian studies of psychological treatments and work (NOR-WORK)” at the aforementioned clinic. The patients included, had been referred to the clinic by their general practitioner (GP) due to depression and/or anxiety disorders, and were all either on sick leave or at risk of sick leave, as determined by their GP. All patients were over the age of 18. Patients presenting with severe mental disorders (e.g., schizophrenia or bipolar), substance abuse or a high risk of suicide were not included and were instead referred to more appropriate treatment better suited to their needs.
2.2Intervention
Participants received either MCT or CBT, both integrated with work-focused interventions. In doing so it was essential that work-related issues were addressed in the assessment and that the patient’s workplace was used actively through the course of treatment. This was accomplished by integrating work-related aspects and issues into the standard treatment content for MCT or CBT, thereby assuring that work-focused interventions were implemented in every treatment session. The treatment manuals were not designed to address bullying explicitly. Patients victimised by bullying received the same treatment procedure as all the included patients, however the work-interventions were flexibly tailored to each person. In this model it is central that treatment starts with a workplace analysis including an assessment of both benefits and problems of the patient’s workplace. If work-related risk factors such as bullying were identified a permanent job change may be an important goal during treatment [42].
The patient’s work situation and their assumptions regarding sick leave, their own health, and work were examined in collaboration with the therapist, and the patients were provided with psychoeducation about mental health and work. A return to work plan was drafted and communicated to the patient’s GP, facilitating a gradual return or a job change over the course of the treatment. Further, barriers for return to work and the need for adjustments at work were explored. As many patients might fear that going back to work might worsen their health condition this was meant to help enhance self-efficacy for the patient and to help them cope with setbacks that may arise during the return to work process. The patients were also encouraged to use their own workplace, or to roleplay work-related scenarios, to implement what they had learned during the intervention. Together with the therapist they reflected on what could be appropriate job-related context that have high feasibility and were relevant to the goals set during therapy. Examples may be related to worrying about work-related situations. Some patients may worry about asking a question in a meeting, eating lunch with their colleagues or other kinds of situations. In MCT it is the worry process that maintains the disorder, not the situation in itself. The task would then be to postpone worries related to such a situation until after the work-related situation has taken place. Not engaging with the anticipatory worry process will change how the patient relates to their thinking process and thus break the mental strategy that maintains the disorder. The therapist encouraged patients to establish dialogue with the workplace by generating an information strategy. The therapist did not as part of the work-interventions have regular communication with the employer.
The therapists in the study were trained at addressing workplace issues. They received regular supervision in applying work-interventions in parallel with MCT and CBT protocols. The supervision was conducted weekly in teams where psychologists specialised in work and rehabilitation secured a work-related focus. The treatment integrity was however not recorded as this study was a naturalistic observational study. Therapists were free to integrate the work-interventions according to the patient’s work situation and needs. For a more detailed explanation of the intervention please see Gjengedal et al. [32].
2.3Procedure
The patients in the study completed the same set of questionnaires pre-treatment (during intake and before first session) and post-treatment. Prior to the statistical analyses, the patients were categorised into two groups: patients who reported being victims of bullying and patients not exposed to workplace bullying. Patients categorised as victims of bullying, attended a mean of 10.8 sessions, while the patients not exposed to bullying attended a mean of 10.0 sessions. The victims of bullying were further divided into two groups, a treatment group and a wait-list control group. This to compare the changes during the treatment period in the treatment group to the changes during the waiting period in the wait-list control group. The treatment group had a delay 0–30 days after the intake assessment before their first treatment session, while the wait-list control group had waited for≥60 days before receiving treatment. The reasoning behind using 60 days as a cut-off, was due to 10 sessions of therapy could be delivered within 60 days. The waiting time in the treatment group was, on average, 20 days from assessment to start of treatment, while the waiting time for the wait-list control group was 80 days on average. As this study constituted a naturalistic study design, a waiting time of 30 or less days from the intake assessment session to the start of treatment could be considered minimal or no delay.
2.4Instruments
Background variables (age, gender, marital status, education, workplace participation, and psychiatric disorders), in addition to a range of standardised instruments were completed pre-treatment (during intake and before first session) and post-treatment.
2.4.1Workplace bullying
Exposure to workplace bullying was measured with the Short version of the Negative Acts Questionnaire (S-NAQ) [43]. This scale comprises nine items including typical negative acts experienced by victims of workplace bullying. These negative acts include acts of a work-related (e.g., “repeated reminders of errors or mistakes”) or a personal-related nature (e.g., “being ignored or excluded”) and were scored from 1 (never) to 5 (daily) based on the last six months that the individual had been at work. The cut-off values for the S-NAQ (sum scores ranging from 9–45) were calculated based on the validated cut-off values for the Negative Acts Questionnaire-Revised (NAQ-R) [44, 45]. The number of items in the NAQ-R were divided with itself and then multiplied by the number of items included in the S-NAQ. The patients were then categorised into two groups; victims of workplace bullying (S-NAQ score of≥14) and patients not exposed to workplace bullying (S-NAQ score of≤13). The scale showed satisfactory reliability in the form of internal stability (Cronbach’s α= 0.87).
2.4.2Health
Depressive symptoms were self-reported using the Beck Depression Inventory–II (BDI-II) [46]. This is a scale comprising of 21 self-report items to measure various affective and cognitive symptoms (e.g., sadness, tiredness or fatigue) experienced by the patients over the last 14 days and scored on a scale from 0 to 3. The scale showed satisfactory reliability in the form of internal stability (Cronbach’s α= 0.86).
Symptoms of anxiety were measured with the Beck Anxiety Inventory (BAI) [47]. This scale comprises 21 items, using self-report to measure various symptoms of anxiety (e.g., nervousness, heart racing), experienced by the patients over the last seven days and was scored on a scale from 0 to 3. The scale showed satisfactory reliability in the form of internal stability (Cronbach’s α= 0.90).
Subjective somatic and psychological complaints, experienced over the last 30 days, were measured using the Subjective Health Complaints inventory (SHC) [48]. The inventory is a self-report measure comprising 29 items, with each item describing various common health complaints (e.g., headache) for the patients to score from 0 (no complaints) to 3 (serious complaints). The scale showed satisfactory reliability in the form of internal stability (Cronbach’s α= 0.83).
The Mini-International Neuropsychiatric Interview (MINI) [49] is a structured diagnostic interview based on “yes/no” answers. It was used to assess psychiatric disorders based on criteria from DSM-IV [50] and ICD-10 [51] for all the patients in the present study. The MINI covers 15 axis I disorders (e.g., mood disorders, anxiety disorders, eating disorders, substance related disorders, and psychotic disorders) and 1 axis II disorder (antisocial personality disorders). For the present study the Norwegian version of MINI 6.0.0 was used [52].
2.4.3Workplace participation and return to work
The validate Norwegian version [37] of the Return to Work Self-Efficacy scale (RTW-SE) [35] was used to measure expectations and perceived ability to function well at work. This scale was developed to measure work-related self-efficacy among individuals suffering from CMD, either as a return to work process, or to enable the patient to evaluate their current work function if they are currently working [35]. As this scale can be used for both patients on sick leave and for patients in a working role, we did not refer to the scale as RTW-SE, so as to not cause any confusion among the patients. The scale comprises 11 items (e.g., “I will be able to set my personal boundaries at work”) scored from 1 (totally disagree) to 6 (totally agree). A higher score would indicate the patient having a higher level of self-efficacy. The scale showed satisfactory reliability in the form of internal stability (Cronbach’s α= 0.89).
Workplace participation was measured using a single self-report item, dividing the patients into “work with no benefits”, “combined work and sick leave”, and “full-time sick leave”.
2.5Statistical analysis
Statistical analyses were conducted using SPSS version 25.0 [53]. ANCOVAs were used to compare the change in symptoms with regard to depressive symptoms (BDI-II), symptoms of anxiety (BAI), subjective health complaints (SHC), and return to work self-efficacy (RTW-SE) between the victims in the treatment group (delay of 0–30 days before their first treatment session) and the wait-list control group (delay of≥60 days), controlling for baseline scores on the respective scales, age, and gender. Paired sample t-tests were used to compare pre- and post-scores within both groups. The same analyses were repeated to compare changes between victims of bullying and the patients not exposed to bullying.
A Fisher’s exact test, using categorical variables, were used to measure change in workplace participation among the patients that were either on full sick leave or combined work and sick leave pre-treatment by comparing how many were fully working post-treatment among the victims of bullying and the patients not exposed to bullying.
To correct for missing values, total scores were calculated for S-NAQ, BDI-II, BAI, SHC, and RTW-SE where we allowed for up to 30% missing. The number of patients in each group might vary slightly in the different analyses, due to missing on single items needed to calculate the sum score on the different instruments.
2.6Ethical considerations
The present study was conducted in accordance with the Helsinki Declaration and was approved by the Data Protection Office at Oslo University Hospital (ref. nr.: 2015/15606). Patients provided written informed consent.
3Results
3.1Background
The sample consisted of 71.9% women (n = 304) and a mean age of 37.6 years (SD = 10.6; age ranging from 18 to 65 years). As many as 27.9% of the patients was classified as victims of bullying based on the scores on the S-NAQ. The most common diagnosis among the victims of bullying were major depressive disorder and generalised anxiety disorder (see Table 1 for patient characteristics).
Table 1
Patient characteristics for both groups at baseline
| Victims of bullying (n = 118) | Not bullied (n = 287) | |||||||
| % | (n) | Mean | SD | % | (n) | Mean | SD | |
| Age | 39.8 | 10.9 | 36.5 | 10.2 | ||||
| Gender | ||||||||
| Female | 66.1 | (78) | 75.6 | (217) | ||||
| Marital status | ||||||||
| Living with partner | 64.4 | (76) | 56.8 | (163) | ||||
| Education | ||||||||
| Primary school | 0.8 | (1) | 1.7 | (5) | ||||
| Upper secondary school | 18.6 | (22) | 13.9 | (40) | ||||
| Higher education 1-4 years | 32.2 | (38) | 38.3 | (110) | ||||
| Higher education > 4 years | 46.6 | (55) | 44.3 | (127) | ||||
| Employment status | ||||||||
| Work with no benefits | 47.5 | (56) | 58.5 | (168) | ||||
| Combined work and sick leave | 18.6 | (22) | 22.0 | (63) | ||||
| Full sick leave | 28.8 | (34) | 15.3 | (44) | ||||
| Diagnosis assessment (MINI) | ||||||||
| Major depressive disorder (ongoing) | 72.9 | (86) | 58.2 | (167) | ||||
| Major depressive disorder (previous) | 22.0 | (26) | 28.9 | (83) | ||||
| Major depressive disorder (reoccurring) | 18.6 | (22) | 13.9 | (40) | ||||
| Agoraphobia | 14.4 | (17) | 9.8 | (28) | ||||
| Generalized anxiety disorder | 44.1 | (52) | 47.4 | (136) | ||||
| Panic disorder | 22.0 | (26) | 20.6 | (59) | ||||
| Post-traumatic stress disorder | 2.5 | (3) | 4.2 | (12) | ||||
| Social phobia | 18.6 | (22) | 15.7 | (45) | ||||
3.2Treatment group compared to a wait-list control group among the victims
Paired sample t-tests showed significant improvements in the treatment group for BDI-II, BAI, and SHC, and significant improvements in the wait-list control group for BDI-II and BAI. However, the observed improvement from intake to the first treatment session for the victims in the wait-list control group were minimal and of no clinical relevance. Results from ANCOVA analyses showed a significant difference between baseline and follow-up scores between the victims in the treatment group and the wait-list control group for BDI-II, BAI, and SHC, controlling for baseline scores on the respective scales, age, and gender, indicating that the victims in the treatment group had a significant larger decline in scores for all the three health outcomes, compared to the wait-list control group (Table 2; Fig. 1). The covariates age and gender did not have a significant effect on any of the outcomes (BDI-II, BAI, and SHC).
Table 2
Descriptive results and comparisons for the BDI-II, BAI, SHC, and RTW-SE between and within the groups (victims of bullying; treatment period in the treatment group and the waiting period in the wait-list control group)
| Baseline | Follow-up | Within groups | Between groups | ||||||
| n | Mean | SD | Mean | SD | t | Cohens d | F | ηp2 | |
| BDI-II score | 59.94*** | 0.47 | |||||||
| Treatment | 38 | 32.89 | 11.40 | 12.39 | 10.24 | 10.79*** | 1.75 | ||
| Wait-list control | 35 | 29.66 | 7.24 | 26.24 | 9.03 | 3.47** | 0.59 | ||
| BAI score | 43.20*** | 0.39 | |||||||
| Treatment | 38 | 20.25 | 13.45 | 7.32 | 8.60 | 8.63*** | 1.40 | ||
| Wait-list control | 35 | 21.34 | 11.57 | 17.90 | 10.28 | 2.78** | 0.47 | ||
| SHC score | 32.21*** | 0.33 | |||||||
| Treatment | 37 | 25.79 | 13.03 | 13.10 | 9.83 | 7.85*** | 1.29 | ||
| Wait-list control | 33 | 24.75 | 7.50 | 24.70 | 12.73 | 0.03 | 0.01 | ||
| RTW-SE score | 33.18*** | 0.33 | |||||||
| Treatment | 38 | 2.96 | 1.07 | 4.31 | 0.99 | –7.01*** | –1.14 | ||
| Wait-list control | 34 | 2.95 | 0.88 | 3.11 | 0.98 | –1.57 | –0.27 | ||
Note. BDI-II = Beck Depression Inventory-II; BAI = Beck Anxiety Inventory; SHC = Subjective Health Complaints; RTW-SE = Return to Work Self-Efficacy. Between group differences measured with ANCOVA controlling for baseline scores on the respective scales, age, and gender. Within group differences measured with paired sample t-tests. ***p < 0.001, **p < 0.01.
Fig. 1
Differences in depressive symptoms (a), symptoms of anxiety (b), subjective health complaints (c), and return to work self-efficacy (d) from baseline to follow-up for the victims of bullying; treatment group compared to the wait-list control group.
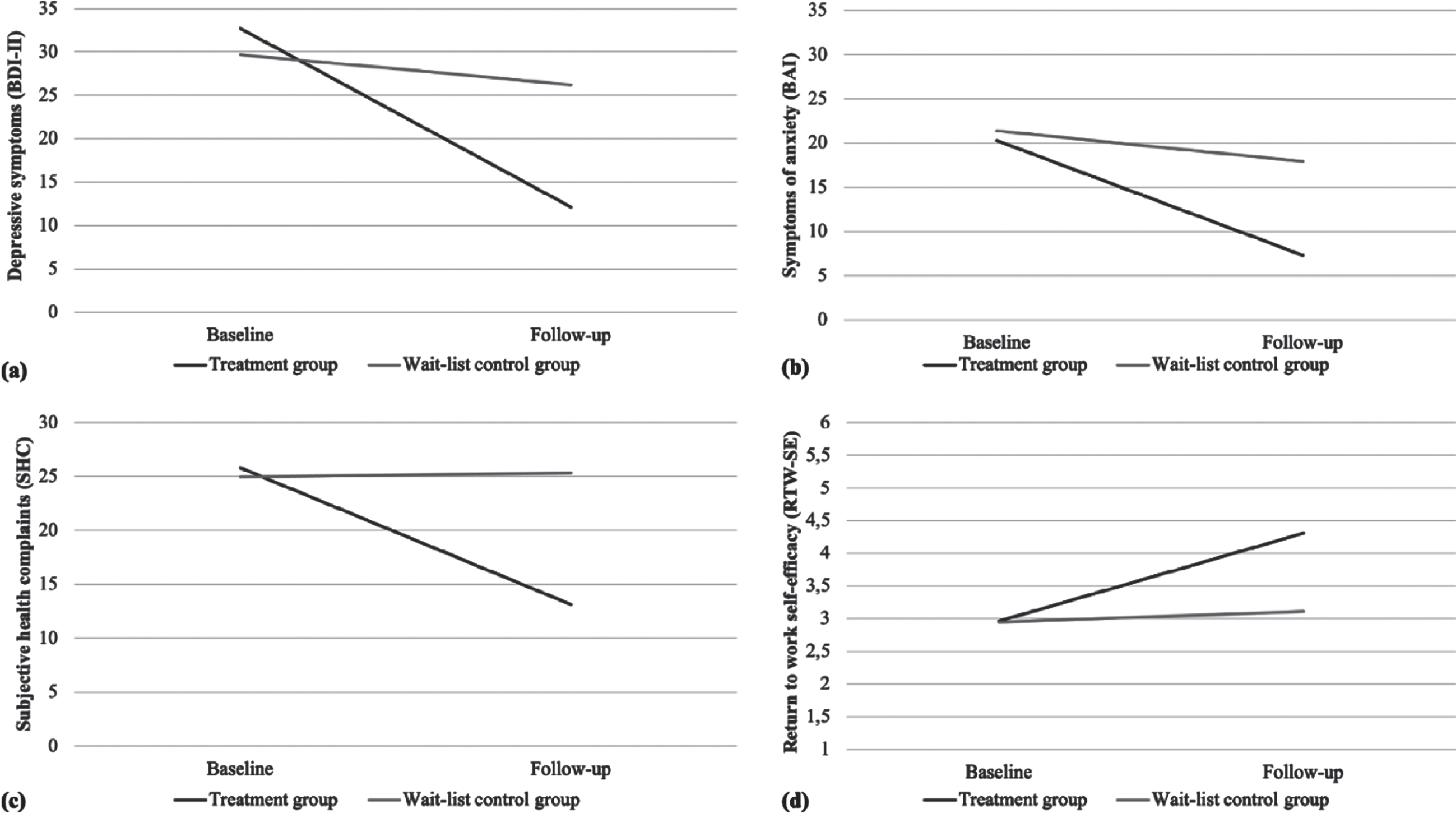
Paired sample t-tests showed significant improvement in RTW-SE scores in the treatment group, but not the wait-list control group. Results from the ANCOVA analysis showed a significant difference between baseline and follow-up scores between the victims in the treatment group and the wait-list control group, controlling for baseline, age, and gender, with the treatment group having a significant improvement in RTW-SE scores. The covariates age and gender did not have a significant effect on RTW-SE.
3.3Victims of bullying compared to patients not exposed to workplace bullying
Paired sample t-tests showed that patients in both groups, achieved significant improvements in their BDI-II, BAI, and SHC scores from pre- to post-treatment. Results from ANCOVA analyses showed that there were no significant differences between pre- and post-treatment scores between the victims of bullying compared to the patients not exposed to bullying for BDI-II, BAI, and SHC, controlling for baseline scores on the respective scales, age, and gender (Table 3; Fig. 2). Thus, the treatment did not seem to affect the two groups differently as both benefitted equally. The covariates age and gender did not have a significant effect on any of the outcomes (BDI-II, BAI, and SHC).
Table 3
Descriptive results and comparisons for the BDI-II, BAI, SHC, and RTW-SE between and within the groups (victims of bullying, and patients not exposed to bullying)
| Pre-treatment | Post-treatment | Within groups | Between groups | ||||||
| n | Mean | SD | Mean | SD | t | Cohens d | F | ηp2 | |
| BDI-II score | 0.12 | 0.00 | |||||||
| Victims of bullying | 117 | 30.02 | 9.27 | 12.20 | 10.23 | 18.00*** | 1.66 | ||
| Not bullied | 278 | 24.86 | 8.18 | 9.80 | 8.45 | 26.72*** | 1.60 | ||
| BAI score | 0.00 | 0.00 | |||||||
| Victims of bullying | 117 | 20.98 | 11.67 | 7.57 | 7.68 | 15.30*** | 1.41 | ||
| Not bullied | 279 | 17.21 | 9.32 | 6.19 | 5.97 | 22.43*** | 1.34 | ||
| SHC score | 0.03 | 0.00 | |||||||
| Victims of bullying | 112 | 25.85 | 10.96 | 14.46 | 10.50 | 13.30*** | 1.26 | ||
| Not bullied | 280 | 22.05 | 9.51 | 12.61 | 8.33 | 18.55*** | 1.11 | ||
| RTW-SE score | 3.10 | 0.01 | |||||||
| Victims of bullying | 114 | 3.03 | 0.95 | 4.34 | 1.08 | –11.78*** | –1.10 | ||
| Not bullied | 281 | 3.32 | 0.93 | 4.65 | 0.90 | –21.65*** | –1.29 | ||
Note. BDI-II = Beck Depression Inventory-II; BAI = Beck Anxiety Inventory; SHC = Subjective Health Complaints; RTW-SE = Return to Work Self-Efficacy. Between group differences measured with ANCOVA controlling for baseline scores on the respective scales, age, and gender. Within group differences measured with paired sample t-tests. ***p < 0.001.
Fig. 2
Differences in depressive symptoms (a), symptoms of anxiety (b), subjective health complaints (c), and return to work self-efficacy (d) from baseline to follow-up for the victims of bullying compared to the patients not exposed to bullying.
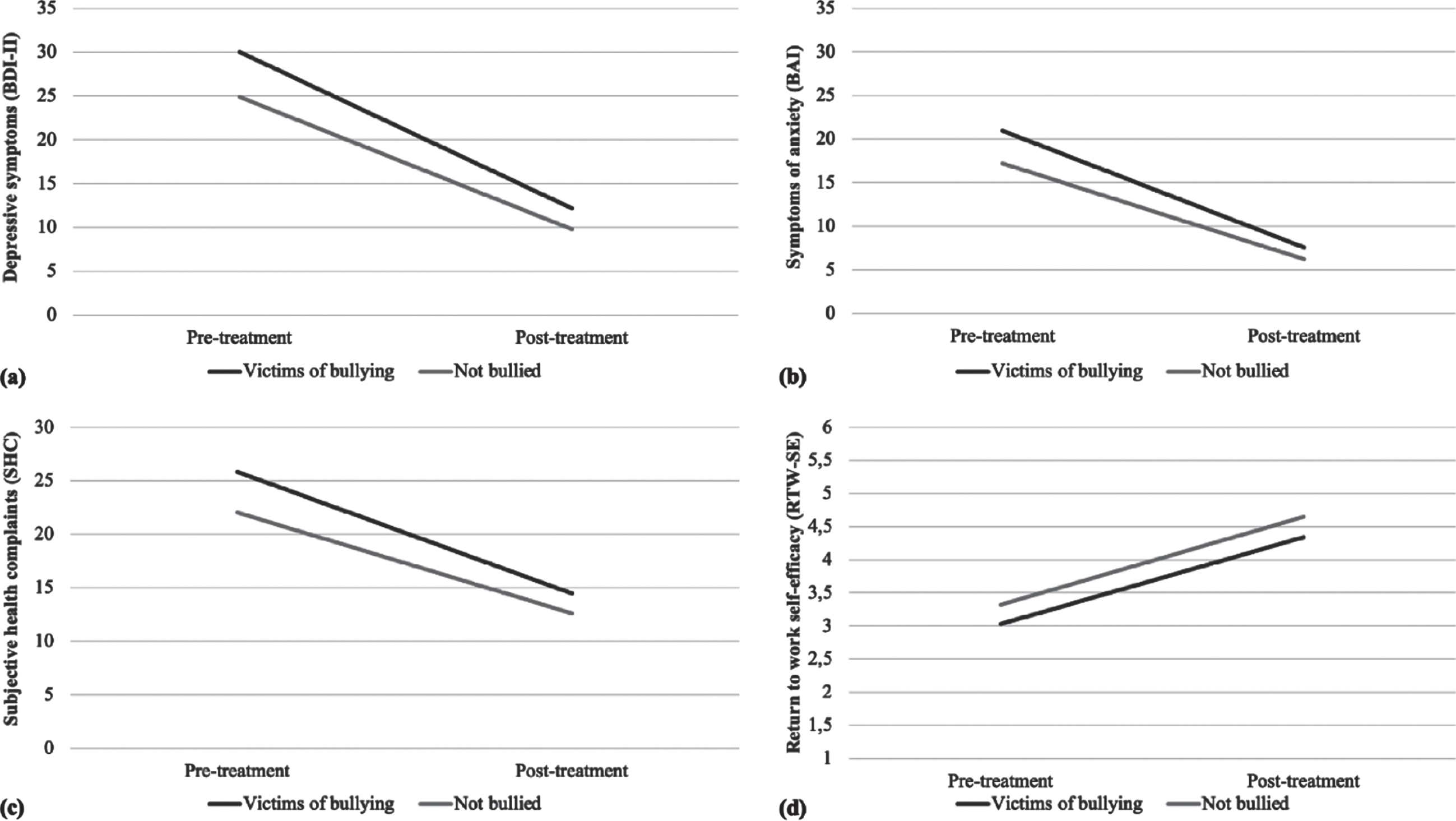
Paired sample t-tests showed significant improvement in RTW-SE scores from pre- to post-treatment in both groups (Table 3; Fig. 2). Results from the ANCOVA analysis showed that there was no significant difference between pre- and post-treatment scores between the victims of bullying compared to the patients not exposed to bullying for RTW-SE, controlling for baseline, age, and gender. Gender did not have a significant effect on RTW-SE, while age was borderline (p = 0.05). A secondary analysis showed that there was a significant interaction effect between S-NAQ and age on RTW-SE (F (1, 388) = 5.74, p < 0.05, ηp2 = 0.02). The results indicated that victims of bullying with a higher age reported a smaller change in RTW-SE scores from pre- to post-treatment compared to patients with a higher age who were not victims of bullying, while younger patients had the same change in RTW-SE scores regardless of being a victim of workplace bullying or not. Thus, suggesting that among victims of bullying, younger patients had a higher belief in their own ability to return to work after treatment than older patients.
3.4Change in workplace participation
Among the patients that were either on full or combined sick leave pre-treatment, Fisher’s exact test revealed that there were significantly fewer patients that were fully working after treatment among the victims of bullying (45.7%, n = 21) compared to the patients not exposed to bullying (66.0%, n = 66), X2(1) = 4.61 p < 0.05, phi = –0.19.
4Discussion
Testing clinical treatment procedures for the mental health problems victims of workplace bullying tend to suffer from, and securing their safe return to work, is of utmost importance. The results of this study showed MCT or CBT with a work-related focus to be an effective treatment procedure when it comes to symptom reduction and facilitating return to work for victims of bullying. The victims of bullying showed a large improvement in depressive symptoms, symptom of anxiety, and subjective health complaints compared to the wait-list control group, with the wait-list control group still having high scores at the end of the waiting period. The same could be seen for RTW-SE with the victims in the treatment group showing large improvements compared to the wait-list control group showing little to no improvement. This indicates that the detrimental effects following workplace bullying do not disappear without treatment. The treatment did not seem to affect the victims of bullying differently from the patients not exposed to bullying. Furthermore, among the patients that were on sick leave pre-treatment, there were significantly fewer that were fully working post-treatment among the victims of bullying compared to the patients not exposed to bullying.
The symptom reduction found in this study is similar to findings reported by Schwickerath and Zapf [16], who also found a significant reduction in health symptoms, depressive moods, and psychosomatic complaints after treatment. Yet in the present study we were able to find this with far less use of resources by treating the patients in an outpatient clinic with an average of 10.8 sessions compared to being admitted for six to eight weeks for inpatient care. The results are in line with previous research showing a strong association between workplace bullying and both psychological and physiological health complaints [e.g., 7, 13]. In this respect it is noteworthy that patients who are victims of workplace bullying reported more mental health problems than the other patients not exposed to bullying in the present study sample. Several studies have also indicated that mental health complaints, caused by workplace bullying, could withstand for years, even after the bullying have subsided [10]. This further highlights the importance of low-cost effective treatment programmes for this patient group.
The MCT or CBT with work-focus also showed a good effect on the victims’ beliefs in their ability to return to work, when measured with the RTW-SE scale. Recent findings have indicated that having an RTW-SE score below 3.7 was associated with no return to work, a score between 3.7 and 4.6 was associated with partial return, and scoring above 4.6 was associated with a full return to work [37]. Our results indicated that the victims in the treatment group went from a score associated with no return to work (2.96) to a score associated with partial return to work (4.31) post-treatment, while the victims in the wait-list control group did not improve from a score associated with no return to work (2.95) during the waiting period (3.11). Thus, emphasising the great risk of exclusion from work and working life suffered by victims of workplace bullying not receiving proper treatment [15, 33]. Although there was no significant difference in the change in RTW-SE between the victims of workplace bullying and the patients not exposed to bullying, there was a significant interaction effect between workplace bullying and age. The results suggested that younger patients had a higher belief in their own ability to return to work after treatment regardless of being a victim of workplace bullying or not, while the older patients had a smaller improvement when being a victim of bullying. As it is often not an option for victims of bullying to return to their previous workplace many change their workplace to escape the situation [15]. However, it might be more challenging to find a new workplace for older workers [54], which could be a possible explanation for our findings. Nevertheless, it should be noted that these findings are based on secondary analysis and further studies are needed.
Among the patients on either full or combined sick leave pre-treatment, there were a significantly lower percentage among the victims of bullying fully working post-treatment (45.7%) compared to the patients not exposed to bullying (66.0%). These results indicate that the victims of bullying improve during treatment, but not quite as well as those not exposed to bullying. Hence, treatment for mental health problems seem to be relatively easier to accomplish than actual return to work for this group.
A possible explanation for these results could be that the victims of bullying might be in need of more work-focus than the average patient in such clinics, and some may need a tailored component to their treatment plan to feel able to and to achieve actual return to work, perhaps addressing the actual bullying scenario to a greater extent or focusing even more on a change of workplace. The few studies that exist examining treatment of victims of workplace bullying have suggested that those who changed workplaces, thus not confronted with the bullies anymore, seemed to be the ones that benefited the most from treatment [16]. Thereby suggesting that even if the treatment is able to reduce symptoms significantly, it does not necessarily help if the patient is returning to the same untreated work situation. Alternatively, the present treatment procedure may have to be complemented with actual interventions at the workplace, e.g., in a collaboration with the employer and/or the organisations occupational health service. The treatment could potentially benefit from being combined with individual job support in line with the “Individual Placement and Support model” (IPS) since patients with bullying experience often needs support to identify a new appropriate job situation. However, changing workplace is often a long-lasting process which underscores the need for future studies with a long follow-up time.
4.1Implications
Given the detrimental effects associated with workplace bullying, and the lack of research on this topic, the results from the present study provide novel findings indicating that MCT or CBT with work-focus can be an efficient treatment option for this patient group. The results showed symptom reduction that were close to the same level as other patients with CMD not exposed to bullying, but if left untreated the symptoms will remain high. While the treatment also showed effective results regarding full return to work among patients on sick leave at baseline, the results were not quite as good as for the non-exposed patients. The results from the present study highlights that it might be of value for clinicians to try to identify patients exposed to workplace bullying early on in therapy, for example through the use of questionnaires. This to identify if it is an option for the patient to successfully return to their current working situation, or if the situation has reached a point where there is no chance of new beginnings and the aim should be returning to a new workplace as previously suggested by Schwickerath [55]. Thus, it is important to map this situation early on in the treatment process so this can be integrated and worked with through the whole return to work process.
Another implication of the present study is that the targets of bullying will benefit from a treatment procedure of approximately 10 sessions, even if it is not tailor-made to this group. This treatment requires less time and resources as compared to an inpatient clinic and will be a cost saving option, not at least compared to the societal cost if this group is left untreated with a high risk of them losing their foothold in working life completely.
4.2Strengths and limitations
Some of the main strengths with the present study were the large sample size and its design where we were able to compare the effect of treatment for the patients that were victims of workplace bullying both to a similar group of patients not exposed to bullying and to a wait-list control group consisting of bullied patients awaiting treatment. Furthermore, the present study was implemented in a naturalistic health care setting, providing high ecological validity. Furthermore, to measure mental health-related complaints we used a well-known clinical interview and frequently used self-report questionnaire to assess levels of symptoms (MINI, BDI-II, BAI, and SHC) and to assess victimisation from bullying (S-NAQ).
However, even though the study is implemented in a naturalistic health care setting the lack of a randomised control trial (RCT) design can still be seen as a limitation with the study, as RCT is regarded the gold standard for evaluating the effectiveness of interventions. Another possible limitation is the lack of information regarding the degree that the therapists adhere to the treatment protocols. Hence, we are not able to assess how frequently different components of the work-focused intervention was implemented during the course of treatment.
Further, workplace participation was measured using a single self-report item and could not control for if the patients changed job or had intention of changing jobs during the course of treatment, which is something that in particular may be important for the victim group. It is also worth noting that due to a large number of comparisons with a number of different outcome variables, the analyses should be interpreted with caution.
5Conclusion
The present study provides support for the effectiveness of MCT or CBT with work-focus when treating patients exposed to workplace bullying and is one of very few studies to investigate the treatment of the mental health aftermath of workplace bullying. These findings provide grounds for optimism for MCT or CBT with work-focus as an efficient way of treating the detrimental effects following being victimised by workplace bullying. The results indicate that such a treatment protocol is effective in reducing symptoms and increasing the victims of bullying belief in their ability to being able to return to or hold on to work and increasing their workplace participation. The treatment increased RTW-SE among the victims of workplace bullying. Additionally, return to work among bullied patients on sick leave were increased, although not quite as efficiently as for patients not exposed to workplace bullying. There is little knowledge about the long-term effect of this treatment for patients that have experienced bullying. Thus, future studies should investigate this further to see if these effects can withstand over time, and if maybe this patient group needs longer treatment in order to return to work to the same degree as patients not exposed to bullying. Future studies should also try to implement a component to the treatment targeting return to work explicitly among the bullied patients.
Acknowledgments
The authors would like to thank all patients and therapists who participated in the study.
Availability of data materials
The dataset from the present study is not available for public access or sharing. This is because the participants have not consented to distribution of data outside the studies conducted at the clinic and its specific conditions regarding confidentiality, privacy protection and data handling, which have been approved by the Data Protection Office at Oslo University Hospital and described to the participants.
Conflict of interest
The authors declare that they have no competing interests.
Funding
This paper was supported by a joint grant (Toppforsk) from the University of Bergen and the Norwegian Research Council (NFR) (grant number 250127).
References
[1] | Zapf D , Escartín J , Scheppa-Lahyani M , Einarsen SV , Hoel H , Vartia M . Empirical findings on the prevalence and risk groups of bullying in the workplace. In: EinarsenSV, HoelH, ZapfD, CooperCL, editors. Bullying and harassment in the workplace: Theory, research, and practice. 3rd ed. Boca Raton: CRC Press; (2020) . pp. 105–162. |
[2] | Mikkelsen EG , Hansen ÅM , Persson R , Byrgesen MF , Hogh A . Individual consequences of being exposed to workplace bullying. In: EinarsenSV, HoelH, ZapfD, CooperCL, editors. Bullying and Harassment in the Workplace: Developments in Theory, Research and Practice. 3rd ed. Boca Raton: CRC Press; (2020) . pp. 163–208. |
[3] | Einarsen SV , Hoel H , Zapf D , Cooper CL . The concept of bullying and harassment at work: The European tradition. In: EinarsenS, HoelH, ZapfD, CooperCL, editors. Bullying and harassment in the workplace: Developments in theory, research, and practice. 3rd ed. Boca Raton, Fla: CRC Press; (2020) . pp. 3–41. |
[4] | Einarsen S , Skogstad A . Bullying at work: Epidemiological findings in public and private organizations. Eur J Work Organ Psychol. (1996) ;5: (2):185–201. |
[5] | Harvey M , Treadway D , Heames JT , Duke A . Bullying in the 21st century global organization: An ethical perspective. J Bus Ethics. (2009) ;85: (1):27. |
[6] | Buhaug K , Magerøy N , Einarsen SV , Assmus J , Kvåle A . A clinical study of musculoskeletal dysfunction in targets of workplace bullying. Eur J Physiother. (2021) : doi: 10.1080/21679169.2020.1865451. |
[7] | Boudrias V , Trépanier S-G , Salin D . A systematic review of research on the longitudinal consequences of workplace bullying and the mechanisms involved. Aggress Violent Behav. (2021) ;56: :1–17. |
[8] | Tatar ZB , Yüksel S . Mobbing at Workplace - Psychological Trauma and Documentation of Psychiatric Symptoms. Arch Neuropsychiatry. (2019) ;56: (1):57–62. |
[9] | Mikkelsen EG , Einarsen S . Basic assumptions and symptoms of post-traumatic stress among victims of bullying at work. Eur J Work Organ Psychol. (2002) ;11: (1):87–111. |
[10] | Bonde JP , Gullander M , Hansen ÅM , Grynderup M , Persson R , Hogh A , et al. Health correlates of workplace bullying: a 3-wave prospective follow-up study. Scand J Work Environ Health. (2016) ;42: (1):17–25. |
[11] | Einarsen S , Nielsen MB . Workplace bullying as an antecedent of mental health problems: a five-year prospective and representative study. Int Arch Occup Environ Health. (2015) ;88: (2):131–42. |
[12] | Hoprekstad ØL , Hetland J , Bakker AB , Olsen OK , Espevik R , Wessel M , et al. How long does it last? Prior victimization from workplace bullying moderates the relationship between daily exposure to negative acts and subsequent depressed mood. Eur J Work Organ Psychol. (2019) ;28: (2):164–78. |
[13] | Aarestad SH , Einarsen SV , Hjemdal O , Gjengedal RGH , Osnes K , Sandin K , et al. Clinical Characteristics of Patients Seeking Treatment for Common Mental Disorders Presenting With Workplace Bullying Experiences. Front Psychol. (2020) ;11: :1–12. |
[14] | Nielsen MB , Skogstad A , Matthiesen SB , Glasø L , Aasland MS , Notelaers G , et al. Prevalence of workplace bullying in Norway: Comparisons across time and estimation methods. Eur J Work Organ Psychol. (2009) ;18: (1):81–101. |
[15] | Glambek M , Skogstad A , Einarsen S . Take it or leave: a five-year prospective study of workplace bullying and indicators of expulsion in working life. Ind Health. (2015) ;53: (2):160–70. |
[16] | Schwickerath J , Zapf D . Inpatient Psychotherapy of Bullying Victims. In: EinarsenSV, HoelH, ZapfD, CooperCL, editors. Bullying and harassment in the workplace: Theory, research, and practice. Boca Raton: CRC Press; (2020) . pp. 593–619. |
[17] | Schwickerath J , Zapf D . Inpatient treatment of bullying victims. In: EinarsenSV, HoelH, ZapfD, CooperCL, editors. Bullying and harassment in the workplace: Theory, research, and practice. Boca Raton: CRC Press; (2011) . pp. 397–421. |
[18] | Buhaug K , Aasen TB , Einarsen S , Magerøy N . Health care related to workplace bullying. Tidsskr Nor Legeforen. (2013) ;133: (20):2129–30. |
[19] | National Institute of Health and Care Excellence. Generalised anxiety disorder and panic disorder in adults: management. NICE Clinical guidelines. 2011. https://www.nice.org.uk/guidance/cg113. Accessed 19 May 2021. |
[20] | National Institute of Health and Care Excellence. Depression in adults: recognition and management. NICE Clinical guidelines. 2009. https://www.nice.org.uk/guidance/cg90. Accessed 19 May 2021. |
[21] | Wells A , Fisher P , Myers S , Wheatley J , Patel T , Brewin CR . Metacognitive therapy in recurrent and persistent depression: A multiple-baseline study of a new treatment. Cognit Ther Res. (2009) ;33: (3):291–300. |
[22] | Hofmann SG , Asnaani A , Vonk IJJ , Sawyer AT , Fang A . The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res. (2012) ;36: (5):427–40. |
[23] | Nordahl HM , Borkovec TD , Hagen R , Kennair LEO , Hjemdal O , Solem S , et al. Metacognitive therapy versus cognitive–behavioural therapy in adults with generalised anxiety disorder. BJPsych Open. (2018) ;4: (5):393–400. |
[24] | Wells A , Matthews G . Modelling cognition in emotional disorder: The S-REF model. Behav Res Ther. (1996) ;34: (11):881–8. |
[25] | Wells A , Matthews G . Self-consciousness and cognitive failures as predictors of coping in stressful episodes. Cogn Emot. (1994) ;8: (3):279–95. |
[26] | Normann N , Morina N . The Efficacy of Metacognitive Therapy: A Systematic Review and Meta-Analysis. Front Psychol. (2018) ;9: :1–14. |
[27] | Ejeby K , Savitskij R , Öst L-G , Ekbom A , Brandt L , Ramnerö J , et al. Symptom reduction due to psychosocial interventions is not accompanied by a reduction in sick leave: Results from a randomized controlled trial in primary care. Scand J Prim Health Care. (2014) ;32: (2):67–72. |
[28] | Marco JH , Alonso S , Andani J . Early intervention with cognitive behavioral therapy reduces sick leave duration in people with adjustment, anxiety and depressive disorders. J Ment Health. (2018) ;29: (3):247–55. |
[29] | Lagerveld SE , Blonk RWB , Brenninkmeijer V , Wijngaards-de Meij L , Schaufeli WB . Work-focused treatment of common mental disorders and return to work: A comparative outcome study. J Occup Health Psychol. (2012) ;17: (2):220–34. |
[30] | Kröger C , Bode K , Wunsch E-M , Kliem S , Grocholewski A , Finger F . Work-related treatment for major depressive disorder and incapacity to work: Preliminary findings of a controlled, matched study. J Occup Health Psychol. (2015) ;20: (2):248–58. |
[31] | Cullen KL , Irvin E , Collie A , Clay F , Gensby U , Jennings PA , et al. Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners. J Occup Rehabil. (2018) ;28: (1):1–15. |
[32] | Gjengedal RGH , Reme SE , Osnes K , Lagerfeld SE , Blonk RWB , Sandin K , et al. Work-focused therapy for common mental disorders: A naturalistic study comparing an intervention group with a waitlist control grouWork ((2020) ;66: (3):657–67. |
[33] | Berthelsen M , Skogstad A , Lau B , Einarsen S . Do they stay or do they go? Int J Manpow. (2011) ;32: (2):178–93. |
[34] | Lagerveld SE . MasteryMatters: The impact of self-efficacy andwork-focused therapy on return towork among employees with common mental disorders [Doctorial dissertation]: Utrecht University; 2017. |
[35] | Lagerveld SE , Blonk RWB , Brenninkmeijer V , Schaufeli WB . Return to work among employees with mental health problems: development and validation of a self-efficacy questionnaire. Work Stress. (2010) ;24: (4):359–75. |
[36] | Nieuwenhuijsen K , Noordik E , van Dijk FJ , van der Klink JJ . Return to work perceptions and actual return to work in workers with common mental disorders. J Occup Rehabil. (2013) ;23: (2):290–9. |
[37] | Gjengedal RGH , Lagerveld SE , Reme SE , Osnes K , Sandin K , Hjemdal O . The Return-to-Work Self-efficacy Questionnaire (RTW-SE): A Validation Study of Predictive Abilities and Cut-off Values for Patients on Sick Leave Due to Anxiety or Depression. J Occup Rehabil. (2021) ; doi: 10.1007/s10926-021-09957-8. |
[38] | Liddon L , Kingerlee R , Barry JA . Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. Br J Clin Psychol. (2018) ;57: (1):42–58. |
[39] | Hansen AH , Høye A . Gender differences in the use of psychiatric outpatient specialist services in Tromsø, Norway are dependent on age: a population-based cross-sectional survey. BMC Health Serv Res. (2015) ;15: (1):477. |
[40] | Thompson AE , Anisimowicz Y , Miedema B , Hogg W , Wodchis WP , Aubrey-Bassler K . The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. (2016) ;17: (1):38. |
[41] | Mackenzie CS , Gekoski WL , Knox VJ . Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Health. (2006) ;10: (6):574–82. |
[42] | Harvey SB , Modini M , Joyce S , Milligan-Saville JS , Tan L , Mykletun A , et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. (2017) ;74: (4):301–10. |
[43] | Notelaers G , Van der Heijden B , Hoel H , Einarsen S . Measuring bullying at work with the short-negative acts questionnaire: identification of targets and criterion validity. Work Stress. (2019) ;33: (1):58–75. |
[44] | Einarsen S , Hoel H , Notelaers G . Measuring exposure to bullying and harassment at work: Validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work Stress. (2009) ;23: (1):24–44. |
[45] | Notelaers G , Einarsen S . The world turns at 33 and Defining simple cutoff scores for the Negative Acts Questionnaire–Revised in a representative sample. European Journal of Work and Organizational Psychology. (2013) ;22: (6):670–82. |
[46] | Beck AT , Brown GK , Steer RA . BDI-II, Beck depression inventory: manual. 2nd ed. San Antonio, Texas: Psychological Corporation; (1996) . |
[47] | Beck AT , Steer RA . Manual for the Beck anxiety inventory. San Antonio, Texas: Psychological Corporation; (1990) . |
[48] | Eriksen HR , Ihlebaek C , Ursin H . A scoring system for subjective health complaints (SHC). Scand J Public Health. (1999) ;27: (1):63–72. |
[49] | Sheehan DV , Lecrubier Y , Sheehan KH , Amorim P , Janavs J , Weiller E , et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) ;59: (20):22–33. |
[50] | American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. Washington, D.C: American Psychiatric Association; 1994. |
[51] | World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. |
[52] | Leiknes KA , Leganger S , Malt EA , Malt UF . MINI International Neuropsychiatric Interview, Norwegian version 6.0.0. Oslo, Norway: Norwegian - Mapi Research Institute; (2009) . |
[53] | IBM Corp. IBM SPSS Statistics for Windows,Version 25.0. Armonk, NY: IBM Corporation; 2017. |
[54] | Mykletun RJ . Aldersriktig ledelse - ivaretakelse og motivering av eldre arbeidstakere [Age-appropriate management - taking care of and motivating older employees]. In: EinarsenS, SkogstadA, editors. Den dyktige medarbeider: behov og forventninger. 2nd ed. Bergen: Fagbokforlaget; (2016) . pp. 441–69. |
[55] | Schwickerath J . Mobbing am Arbeitsplatz: Aktuelle Konzepte zu Theorie, Diagnostik und Verhaltenstherapie [Mobbing in the workplace: Current concepts of theory, diagnosis and behavioral therapy]. Psychotherapeut. (2001) ;46: (3):199–213. |




