Physical therapists’ knowledge and implementation of best practices in the outpatient physiotherapy department during the COVID-19 pandemic: A cross-sectional study
Abstract
BACKGROUND:
Physiotherapists (PTs) play an important role in the well-being and physical rehabilitation of patients with long term health problems. It is important that PTs follow recommended practices that minimize the transmission of SARS-CoV-2 infection in providing Outpatient Physiotherapy services.
OBJECTIVE:
The aim of this study was to assess the knowledge of COVID-19 among the PTs and evaluate the state of implementation of best practices in Outpatient Physiotherapy to prevent SARS-CoV-2 infections during the ongoing pandemic.
METHODS:
A self-administered online questionnaire consisting of three sections, including section one on demographic information, section two on evaluating knowledge about SARS-CoV-2 and section three on implementing best practices as a survey tool for collecting data from PTs working in Lahore and Faisalabad in Punjab, Pakistan.
RESULTS:
A total of 216 completed surveys were received. Correct responses to different questions devised to test the participants’ knowledge of SARS-CoV-2 varied from 58.3% to 99%. The implementation of best practices to prevent the infection transmission in the Outpatient Physiotherapy ranged from 22.7% to 92.1% for different domains. The age of the PTs and OPD setting were associated significantly with the PTs’ knowledge of COVID-19 and also with the state of implementation of recommended practices to prevent SARS-CoV-2 infections in the Outpatient Physiotherapy (p < .05).
CONCLUSION:
The majority of the PTs, particularly those working in the clinic setting, possessed a good knowledge of COVID-19 and implemented best practices in their Outpatient Physiotherapy at a good level. However, efforts should be directed towards further improving the knowledge of PTs and ensuring implementation of best practices in Outpatient Physiotherapy, particularly in government and private hospitals.
1Introduction
Wuhan, China, witnessed a mysterious pneumonia outbreak in December 2019 that was identified as a novel coronavirus strain in December 31, 2019, and named 2019-nCoV by the World Health Organization (WHO) and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) by the International Committee for Virus Taxonomy [1]. The coronavirus infections spread rapidly across the globe and the outbreak was declared a public health emergency of international concern by WHO on 30 January 2020. WHO named the disease as COVID-19 (Coronavirus Disease of 2019) and declared the disease a global pandemic on 11 February 2020 [1]. Unfortunately, the COVID-19 pandemic is still far from being under control and continues to be a major concern worldwide, including in Pakistan. As of 16th September, 2021, 1,215,821 cases have been reported in Pakistan, of which 76,581 are active cases, 1,112,236 have recovered and 27,004 have died [2].
Healthcare workers (HCWs) of different categories and levels are involved in the treatment of COVID-19 patients and this easily transmissible disease has emerged as a serious workplace health hazard for HCWs due to their close contact with the infected patients. The lack of knowledge of effective infection control measures among healthcare workers can be a significant factor contributing to the spread of SARS-CoV-2 in the hospitals and the clinics. Till now hundreds of thousands of the healthcare workers have been infected worldwide with the virus and thousands have died [3]. Therefore it is important to understand the factors contributing to the spread of SARS-CoV-2 infections among healthcare workers [4].
Allied Health Care Professionals (AHCPs) are an indispensable part of the healthcare system and play an important role in the fight against the pandemic by providing a constant support to frontline health care professionals and patients. AHCPs play an important role in all aspect of patient care, such as managing emergencies, disease diagnosis, in-patient care, and rehabilitation services [5]. The millions of healthcare workers including doctors, nurses, technicians, physiotherapists, AHCPs and medical support staff, who risk their lives to save the lives of others suffering from COVID-19 are often ill-equipped and ill-prepared to protect themselves from the infection [6]. Hence, there is an urgent need to assess the knowledge of SARS-CoV-2 COVID-19 among the HCWs and addressing the weak areas.
WHO has issued several guidelines and launched various online courses and training programs geared towards raising the awareness of HCWs for understanding the importance of COVID-19 in containing the pandemic. These programs increase the capabilities of HCWs to prevent SARS-CoV-2 infections in clinics and hospitals [7]. Physiotherapists are a distinct group of healthcare professionals that are playing an important role in the conservative care and management of COVID-19 patients. They provide support to the patients during weaning off from intrusive mechanical ventilation, and also help the survivors of the critical illness associated with the infection with exercise, and mobilisation and rehabilitation interventions [8]. Rehabilitation staff like cardiopulmonary physiotherapists are at an increased risk of contracting SARS-CoV-2 infections as they come in close contact with patients and are exposed directly to respiratory droplets from them. Therefore, physiotherapy staff should have good knowledge of COVID-19 and sincerely implement best practices to ensure their own and patient’s safety during this COVID-19 pandemic [9]. Guidelines have been issued by organizations such as the World Confederation of Physical Therapy and Associations of Physical Therapy in various countries, advocating to minimize the risk of SARS-CoV-2 exposure to the PTs [10, 11]. Unlike many other professionals it is not feasible for the PTs to work from remote locations as physiotherapy requires close contact with the patients. There is a shortage of studies that investigate how PTs and rehabilitation therapists are adapting to work during the COVID-19 pandemic. The current study was conducted to assess the knowledge of Pakistani PTs about SARS-CoV-2 and evaluate the state of implementation of best practices to prevent SARS-CoV-2 infection transmission in Outpatient Physiotherapy in Pakistan. PTs may take precautions in their clinical practice to protect the patients and other colleagues from COVID-19 reported during this study. In addition, the questionnaire developed during this study can be used as recommendations for outpatient physiotherapy management. Moreover, this study can help health authorities take the steps necessary to improve the safety of PTs in Pakistan and around the world.
2Methods
2.1Participant recruitment
The PTs practicing in the cities of Lahore and Faisalabad, Punjab, Pakistan were recruited for this study. The PTs of either genders with at least a bachelor’s degree in physiotherapy, working in private or government sector hospitals or clinics and with at least 1 year of clinical experience were included in the study. PT students, PT technicians, interns and non-practicing PTs were excluded from the study. Informed consent was obtained from all participating PTs and ethical approval for the study was obtained from the Research Ethics Committee of the Riphah International University (RCRAHS/REC/COVID/101).
2.2Data collection
The PTs’ knowledge of COVID-19 and the state of implementation of best practices in the physiotherapy Outpatient Physiotherapy were assessed using a self-administered questionnaire prepared using previously published literature and the guidelines published by various physiotherapy societies [10, 12, 13]. The suitability of the questionnaire in meeting the objectives of the study was checked by a panel of experts and the changes proposed by the expert panel were incorporated in the questionnaire. Before the survey began, pilot study was conducted to assess the content validity of each question.
2.3Questionnaire
The questionnaire was divided into three parts. The participating PTs provided the demographic information (name, age, gender, qualification, experience, specialty, type of job) in the first part and answered the 15 questions devised to evaluate their knowledge of SARS-CoV-2. The third part of the questionnaire evaluated the state of implementation of best practices to prevent SARS-CoV-2 infection transmission in the Outpatient Physiotherapy. The questions in this part covered the following 10 domains associated with the prevention of transmission of infections in physiotherapy Outpatient Physiotherapy: 1) before the patient arrives for PT treatment, 2) first appointment, 3) arrangements in the waiting room areas, 4) Sanitary facilities 5) use of personal Protection equipment (PPE) 6) sanitary provisions in the treatment area 7) time gap between appointments, 8) patient departure after PT treatment, 9) follow-up care and 10) payment methods. The questions included under different domains in the third of the questionnaire were as below:
2.3.1Before arriving for PT treatment
(i) Do you recommend to patients that they arrive in clinic as close to treatment time as possible and wait in a waiting area outside the practice space?
(ii) Do you place signboards in your waiting area instructing patients to stay outside of the treatment area until called for the treatment?
(iii) Do you emphasize to your patient that they disinfect hands and wear a face mask prior to entering the treatment room?
2.3.2First appointment
(i) Do you prefer first appointment with your patient over the phone?
(ii) Do you set your appointment according to the concept of triage, i.e., according to urgency of treatment and postpone all non-urgent appointments?
(iii) Do you check for COVID-19 symptoms in patients at your urgent appointments?
(iv) Do you take history of the patients suspected to have SARS-CoV-2 infection? This may include questions such as from where the patient belongs, where he/she has been in the last one month, whether he/she has been to an area affected by COVID-19 in the last 14 days and if he/she came in contact with someone who have had symptoms of COVID-19 within last 14 days.
(v) Do you educate your patients on the appropriate way of arriving and leaving the physical therapy OPD, such as adhering strictly to schedule, wearing a face mask, observing hand hygiene, and the need to call the therapist immediately if any symptoms of COVID-19 are experienced?
(vi) Do you check again for compliance with the instructions for maintaining hand hygiene and wearing of a face mask after the patient enters the treatment room?
(vii) Are you providing face masks to the patients arriving without one?
(viii) Do you recommend a social distance of at least 1 meter between you and your patient whenever possible?
(ix) Are you taking steps to minimize contact with patients during treatment sessions?
(x) Do you change your gloves after treatment?
2.3.3Waiting areas
(i) Is your waiting area well-disinfected?
(ii) Does your waiting room area has disinfectant braces?
(iii) Are there information displays on the walls of your waiting room describing correct procedures for hand disinfection?
(iv) Are there information displays on the walls of your waiting room area describing important precautionary measures for preventing the spread of SARS-CoV-2 infection (hand and respiratory hygiene, no handshaking)?
(v) Do you apply measures to minimize the number of patients present in the waiting room at a particular time?
(vi) Do you instruct your patients to maintain a distance of at least 1 meter from other patients in your waiting room?
2.3.4Sanitary facilities
(i) Do you have separate sanitary areas or sanitary facilities for physical therapists and patients?
(ii) Are toilets equipped with wash basins and disinfecting agents?
(iii) Are informative posters describing the correct way of hand washing, and the importance of hand hygiene displayed?
(iv) Are dustbins in the toilet closed and equipped with a treadle to open and dispose paper towels?
2.3.5Personal protection equipment
(i) Do you use WHO recommended PPE, i.e., medical mask (FFP2 or equivalent), clean non-sterile medical gowns, and gloves?
(ii) Do you dispose of PPE after every session?
2.3.6Treatment areas
(i) Is the treatment area well-disinfected?
(ii) Is the treatment area well-ventilated?
(iii) Does your clinic has a separate treatment room?
(iv) Are therapeutic equipment sanitized or disinfected after every use?
(v) Do you minimize equipment in your treatment room as a precautionary measure to prevent transmission of infection?
(vi) Do you maintain a social distancing of at least 1 meter with your patient in the treatment area whenever possible?
(vii) Does your treatment room has a washbasin, suspender for soap, disinfectant, and closed bin with treadle to open and close the lid?
(viii) Do you use disposable paper towels in the treatment area?
2.3.7Payment methods
(i) During the ongoing pandemic, do you emphasize on online payments?
(ii) Leaving after PT Treatment
(iii) Do you ask your patients to disinfect their hands before leaving the treatment room?
(iv) Do you request your patient to limit the time spent in the waiting area after the treatment?
2.3.8Follow up care
(i) Do you prescribe a written exercise program to your patients for follow-up?
(ii) Do you offer tele-rehabilitation services for follow up?
(iii) Before follow up visit do you ask the patient if he/she has any signs and symptoms of an infection?
2.3.9Time gap between appointments
(i) Do you keep enough time gap between two appointments?
Criteria were established for grading the response of the PTs as ‘poor level of knowledge’, ‘moderate level of knowledge’ and ‘good level of knowledge’. Criteria were also established for grading of implementation of best practices for prevention of transmission of SARS-CoV-2 infection as ‘poor level of implementation’, ‘moderate level of implementation’ and ‘good level of implementation’.
The questionnaire was posted online, and the web link was sent to 300 registered members of the Pakistan Physical Therapy Association (PPTA) in Lahore and Faisalabad cities located in Punjab, Pakistan. The participants were assured of confidentiality and a reminder email was sent two weeks after the first request to participate in the survey.
2.4Data analysis
Data entry and statistical analysis was carried out using the SPSS software version 22 (IBM Corp, Armonk, NY, USA). Univariate analysis using a Chi-square test was performed to determine the association between the demographic variables and the PTs’ level of knowledge of SARS-CoV-2 and also the implementation of best practices for prevention of SARS-CoV-2 infection transmission in outpatient physiotherapy setting. Multivariate logistic regression was performed to assess the factors associated with moderate/good level of knowledge of COVID-19 and moderate/good level of implementation of best practices for in Outpatient Physiotherapy.
3Results
Out of 300 surveys sent, only 216 were received completely filled and 84 had missing information and were not considered for the study. Out of 216 completed surveys, 120 (55.6%) were from male PTs and 96 (44.4%) were from female PTs. City-wise distribution of the completed surveys was–111 (51.4%) from Lahore and 105 (48.6%) from Faisalabad. The major specialization of PTs that participated in the survey was musculoskeletal physiotherapy (Table 1).
Table 1
Demographic information of the participating PTs (N = 216)
| Variables | Frequency | Percentage |
| Gender | ||
| Male | 120 | 55.6 |
| Female | 96 | 44.4 |
| Age (years) | ||
| 21–25 | 48 | 22 |
| 26–30 | 46 | 21.3 |
| 30–35 | 34 | 15.7 |
| 35–40 | 42 | 19.4 |
| >40 | 46 | 21.3 |
| Qualification | ||
| DPT | 33 | 15.3 |
| MS/M.Phil | 175 | 81 |
| PhD | 8 | 4 |
| Clinical experience | ||
| 01–05 | 135 | 62.5 |
| 06–09 | 67 | 31 |
| >10 | 14 | 6.5 |
| Employment status | ||
| Part Time | 105 | 48.6 |
| Full Time | 111 | 51.4 |
| Specialization | ||
| Cardiopulmonary PT | 20 | 9.3 |
| Gynaecology PT | 17 | 7.9 |
| Musculoskeletal PT | 56 | 26 |
| Neurological PT | 46 | 21.3 |
| Orthopaedic PT | 42 | 19.4 |
| Sport PT | 35 | 16.2 |
| Working setting | ||
| Clinic | 57 | 26.4 |
| Govt. hospital | 36 | 16.7 |
| Private hospital | 123 | 56.9 |
| City | ||
| Lahore | 111 | 51.4 |
| Faisalabad | 105 | 48.6 |
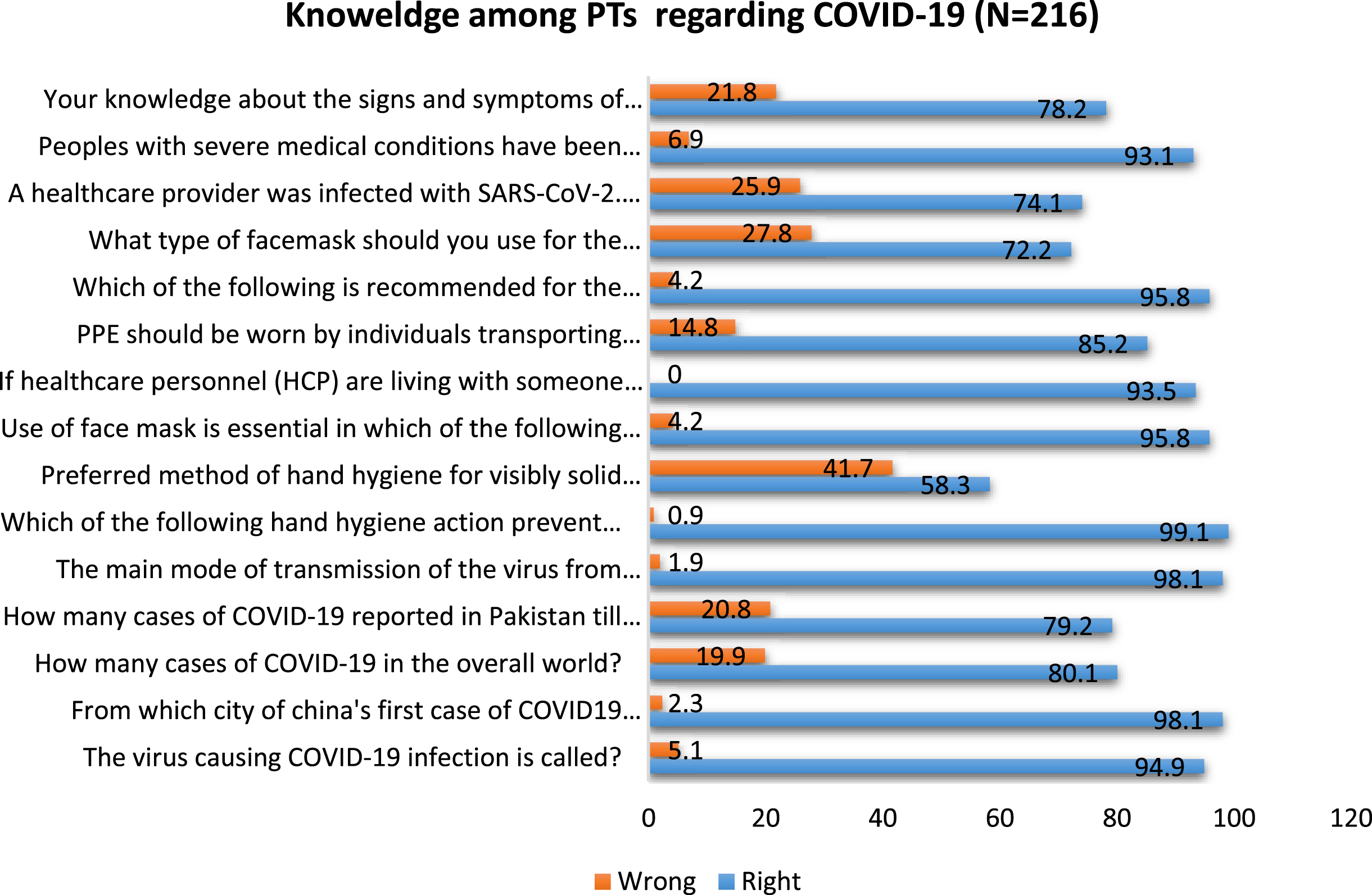
The correct answers to the 15 questions devised to test the participants’ knowledge on the SARS-CoV-2 COVID-19, in the first part of the survey varied from 58% to 99% for individual questions. This indicates that the PTs have adequate knowledge of SARS-CoV-2 infection control measures. The highest number (99%) of participants answered correctly the question on the importance of hand hygiene in prevention of transmission of the virus. The lowest number of PTs (58%) answered correctly the question on the best method to disinfect visibly soiled hands (Fig. 1).
Fig. 1
Knowledge of SARS-CoV-2 among the Pakistani physiotherapists.
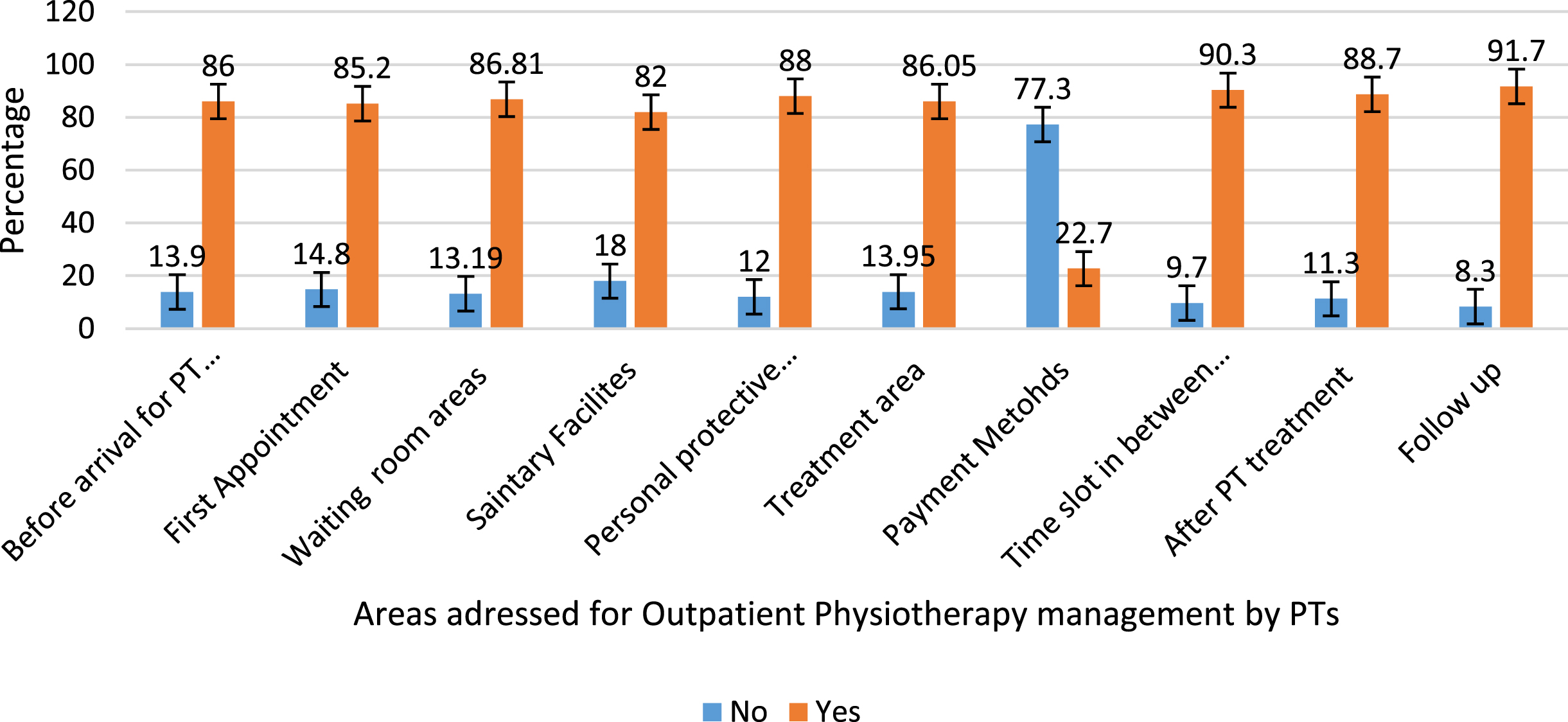
The implementation of best practices, based on the recently published literatures and the guidelines to prevent the SARS-CoV-2 infection transmission in the Outpatient Physiotherapy was found to be adequate. An average of the correct responses in a particular domain of best practices was calculated for the domains with multiple questions. It was found that the level of implementation of best practices for handling of patients in the waiting area was 86.81% while that of maintaining sanitation was 82.0%. Similarly, implementation of the practice of informing patients beforehand about the precautionary measures to be followed in the OPD was 86% and that of booking the first appointment as per the principle of triage was 85.2%. An implementation level of 88% was observed for the use of personal protective equipment. A high level of implementation of 86.05% was also reported for the precautionary measures meant for preventing the spread of SARS-CoV-2 infection in the treatment area. A suitable time gap between two appointments was kept by 90.3% of the PTs, and 88.7% of the PTs instructed their patients to sanitize hands before leaving the treatment area and minimize their time in the waiting area post-treatment. The average implementation of the practice of providing proper follow-up instructions to patients was 91.7%. The best practice of asking for online payments was, however, implemented by only 22.7% of the PTs (Fig. 2 & 3).
Fig. 2
The physiotherapists’ response to questions related to implementation of the best practices for prevention of SARS-CoV-2 infection transmission in physiotherapy Outpatient Physiotherapy during the COVID-19 pandemic.
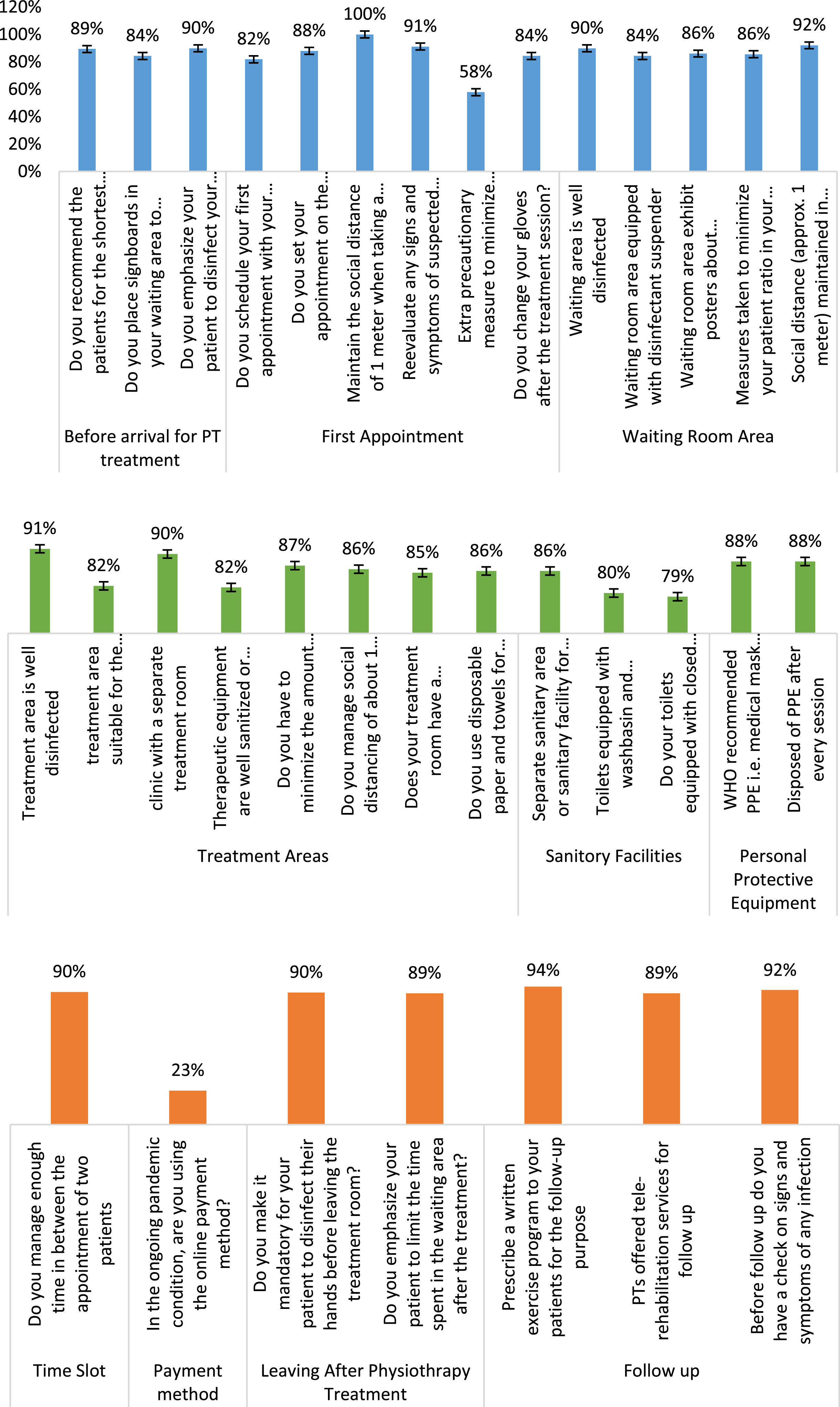
Fig. 3
Overall response of the physiotherapists in 10 different domains of the best practices for prevention of SARS-CoV-2 in Outpatient Physiotherapy during the COVID-19 pandemic.
Univariate analysis using a Chi-square test showed a statistically significant association of age of the PTs and the setting of physiotherapy Outpatient Physiotherapy, with the PTs’ Knowledge of SARS-CoV-2 COVID-19 and the implementation of best practices for prevention of transmission of infection (p < 0.05). The PTs in the age group 21–25 year were found to have ‘good knowledge’ of the measures effective in controlling transmission of SARS-CoV-2 infection and also implemented best practices in the physiotherapy Outpatient Physiotherapy at a‘good level’. Similarly, PTs practicing in clinics showed ‘good knowledge of the measures for preventing transmission of SARS-CoV-2 infection and also implemented best practices in Outpatient Physiotherapy at a ‘good level’ (Table 2). A multivariate logistic regression analysis showed that the PTs working in clinic setting had 4.8 times greater odds of having ‘good knowledge’ of SARS-CoV-2 infection control measures and 5.3 times greater odds of ‘good level’ of implementation of best practices in the OPD (Tables 3 & 4).
Table 2
Univariate analysis of demographic parameters associated with the PTs knowledge of SARS-CoV-2 and the implementation of the best practices to prevent SARS-CoV-2 infection transmission in the Outpatient Physiotherapy
| Variables | Knowledge of COVID-19 | Total | p-value | Implementation of the best practices | Total | p-value | ||
| Gender | Moderate | Good | 216 | Moderate | Good | 216 | ||
| n = 51 | n = 165 | n = 40 | n = 176 | |||||
| Male | 30(25.0) | 90(75.0) | 120 | 0.631 | 22(18.3) | 98(81.7) | 120 | 1 |
| Female | 21(21.9) | 75(78.1) | 96 | 18(18.8) | 78(81.3) | 96 | ||
| Age (years) | ||||||||
| 21– 25 | 8(13) | 40(87) | 48 | .001** | 4(8.3) | 44(91.7) | 48 | .006** |
| 26– 30 | 6(13) | 40(87) | 46 | 5(10.9) | 41(89.1) | 46 | ||
| 30– 35 | 16(47.1) | 18(52.9) | 34 | 12(35.3) | 22(64.7) | 34 | ||
| 35– 40 | 9(21.4) | 33(78.6) | 42 | 12(28.6) | 30(71.4) | 42 | ||
| >40 | 14(30.4) | 32(69.6) | 46 | 7(15.2) | 39(84.8) | 46 | ||
| Qualification | ||||||||
| DPT | 13(39.4) | 20(60.6) | 33 | 0.065 | 9(27.3) | 24(72.7) | 33 | 0.115 |
| MS/M.Phil. | 36(20.6) | 139(79.4) | 175 | 28(16.0) | 147(84.0) | 175 | ||
| PhD | 2(25.0) | 6(75.0) | 8 | 3(37.5) | 5(62.5) | 8 | ||
| Clinical experience | ||||||||
| 01– 05 | 30(22.2) | 105(77.8) | 135 | 0.75 | 26(19.3) | 109(80.7) | 135 | 0.891 |
| 06– 09 | 18(26.9) | 49(73.1) | 67 | 12(17.9) | 55(82.1) | 67 | ||
| >10 | 3(21.4) | 11(78.6) | 14 | 2(14.3) | 12(85.7) | 14 | ||
| Employment status | ||||||||
| Part time | 27(25.7) | 78(74.3) | 105 | 0.523 | 22(21) | 83(79.0) | 105 | 0.387 |
| Full time | 24(21.6) | 87(78.4) | 111 | 18(16.2) | 96(83.8) | 111 | ||
| Specialization | ||||||||
| Cardiopulmonary PT | 7(35.0) | 13(65.0) | 20 | 0.11 | 6(30.0) | 14(70.00) | 20 | 0.134 |
| Gynaecology PT | 2(11.8) | 15(88.2) | 17 | 2(11) | 15(88.2) | 17 | ||
| Musculoskeletal PT | 17(30.4) | 39(69.6) | 56 | 10(17.9) | 46(82.1) | 56 | ||
| Neurological PT | 9(19.6) | 37(80.4.) | 46 | 5(10.9) | 41(89.1) | 46 | ||
| Orthopaedic PT | 5(11.9) | 37(88.1) | 42 | 6(14.3) | 36(85.7) | 42 | ||
| Sport PT | 11(31.4) | 24(68.6) | 35 | 11(31.4) | 24(68.6) | 35 | ||
| Working setting | ||||||||
| Clinic | 4(7.0) | 53(93) | 57 | .002** | 3(5.3) | 54(94.7) | 57 | .008** |
| Govt. hospital | 13(36.1) | 23(63.9) | 36 | 10(27.8) | 26(72.2) | 36 | ||
| Private hospital | 34(27.6) | 89(72.4) | 123 | 27(22) | 96(78.0) | 123 | ||
Chi-square test significant at *P < 0.05, **P < 0.01.
Table 3
Multivariate logistic regression analysis to assess moderate/good knowledge of the SARS-CoV-2 infection control measures
| Parameters | Odds | 95% CI | P-value ratio | |
| Lower upper | Upper | |||
| Work setting | 0.013 | |||
| Clinic | 4.822 | 1.613 | 14.414 | 0.005 |
| Govt. hospital | –0.812 | 0.337 | 1.954 | 0.641 |
| Private hospital | ref |
P < 0.01; Ref –Ref- reference category; CI: Confidence Interval.
Table 4
Multivariate logistic regression analysis to assess moderate/good level of implementation of best practices for preventing SARS-CoV-2 infection transmission
| Parameters | Odds | 95% CI | P-value ratio | |
| Lower Upper | Upper | |||
| Work setting | 0.014 | |||
| Clinic | 5.321 | 1.529 | 18.518 | 0.009 |
| Govt. hospital | –0.626 | 0.244 | 1.608 | 0.331 |
| Private hospital | ref |
P < 0.01; Ref –Ref- reference category; CI: Confidence Interval.
4Discussion
Physiotherapists are playing an important role in functional and respiratory rehabilitation of patients affected with COVID-19 by providing tele-rehabilitation services and carrying out outpatient physiotherapy during the pandemic [14]. The current study was conducted to assess the knowledge of SARS-CoV-2 COVID-19 of Pakistani PTs and evaluation of implementation of best practices for prevention of SARS-CoV-2 infection in the Pakistani physiotherapy Outpatient Physiotherapy during the COVID-19 pandemic.
4.1PT’s knowledge of hand hygiene
A surprising finding of the study was that only 58.3% of the PTs enrolled in the study knew about the correct method of disinfecting visibly soiled hands. The finding that coronavirus can spread by contaminated hands has spurred a global interest in the importance of knowledge of correct methods of hand hygiene in preventing SARS-CoV-2 infection. A reduction in the speed of transmission of SARS-CoV-2 infection has been observed with increasing awareness of importance of hand washing [15]. In the wake of a rapid spread of SARS-CoV-2, it has also been stressed to use innovative technologies to monitor the compliance with the hand hygiene guidelines, [16], and use creative means to increase the hand hygiene compliance [17]. At the same time it is important to devise strategies and put them in place to prevent the recontamination of clean hands [18]. The CDC recommends washing hands regularly with soap and water for 20 seconds to prevent virus transmission. However, if soap and water are not available, a hand sanitizer containing at least 60% alcohol can be used [19]. WHO has proposed two alcohol-based formulations for hand hygiene in healthcare to minimize the spread of SARS-CoV-2 [20, 21]. It is important to increase the awareness of the correct procedures for hand hygiene among Pakistani PTs in controlling the SARS-CoV-2 infections in Outpatient Physiotherapy. The policy makers should focus their attention on the issue of low level of awareness of correct hand hygiene procedures in physiotherapy Outpatient Physiotherapy in Pakistan.
4.2PT’s Knowledge of sign and symptoms of COVID-19
The results of this study show that 78.2% of PTs enrolled in the study were aware of the signs and the symptoms of COVID-19, which is important for prevention of infection transmission in the Outpatient Physiotherapy. The incubation period of SARS-CoV-2 averages 5 to 6 days, but can be up to 14 days [22, 23]. Pre-symptomatic transmission of coronavirus is also possible by patients who have been infected with the virus but have not yet developed symptoms. On or just before the day on which symptoms are experienced, people tend to have a higher viral load as compared to the later stages of the infection [24]. Symptoms can include fever (83–99 %), cough (59–82 %), fatigue (44–70 %), loss of appetite (40–85 %), shortness of breath (31–40 %), muscle pain (11–35 %) and secretion development (28–33 %). Other non-specific symptoms such as sore throat, nasal congestion, headache, diarrhoea, and vomiting are also noted. Loss of smell and taste is also experienced prior to the onset of respiratory symptoms [24, 25]. About 15% of the patients develop serious symptoms of the disease such as shortness of breath, hypoxia, or > 50% involvement of the lungs as revealed by imaging [24–26]. Atypical symptoms such as fatigue, decreased alertness, decreased mobility, diarrhoea, loss of appetite and a lack of fever in the elderly and immunocompromised patients has also been noted [27, 28]. It is also important to keep in mind that very mild and non-specific symptoms may be present in some patients infected with the virus. A majority of Pakistani PTs understood the importance of recognizing the symptoms of COVID-19 in the early stages of the infection, which can help in preventing the transmission of infection in physiotherapy Outpatient Physiotherapy. However, it is desirable to further increase the awareness of the importance of early detection of the symptoms of SARS-COV-2 infection in the patients among the Pakistani PTs.
4.3PT’s knowledge of personal protective equipment
The importance of using N95 mask in Outpatient Physiotherapy for prevention of SARS-CoV-2 infection was known to 95% of the PTs. Respiratory protective device (N95 mask) is one of the key components of personal protective equipment (PPE) used by the healthcare workers to protect themselves from SARS-CoV-2 infection [29, 30]. The data from the previous studies have shown that a surgical face mask is less than 95 percent effective in protecting healthcare professionals from SARS-CoV-2 infection [31]. There is a general agreement that N95 respirators provide better protection than surgical masks from aerosol generating procedures such as intubation or bronchoscopy. N95 respirators are designed to reduce the leakage of air around the nose and at the edges, thus minimize the breathing-in of small particles present in the air and also the release of unfiltered expired air. Surgical masks though loose fitting are effective due to the barrier protection against large droplets, and by reducing hand-to-face contact [32–34].
4.4Outpatient physiotherapy management
The results indicate that 85.2% of the PTs followed best practice for scheduling first appointment. The SARS-CoV-2 virus is mainly transmitted via large droplets with a range of about 2 meters, and it is known that the rate of infection decreases with social distancing and wearing of at least a surgical mask. The appointment should therefore be planned early with the recommendation of social distancing and avoidance of hospital visits or contact with COVID-19 positive patients before the appointment [36].
In the current study, nearly 87% of PTs reported that outpatient physical therapy management precautions were addressed in relation to waiting areas. It is imperative to create a separate waiting area with a disinfectant holder. Posters explaining how to use disinfectant hand sanitizer effectively would be beneficial. In addition, behaviour-related measures should be indicated, such as hand and respiratory hygiene, a distance of one meter and no handshaking in waiting area to avoid spread of COVID-19 during physiotherapy outpatients’ services[35, 36].
Our study found that 86% of PTs reported implementing best practices for using the treatment areas during COVID-19 while providing physical therapy services. Particular attention should be paid to adequate ventilation of the treatment room. The treatment room should be structurally separated from all other rooms. Therapeutic devices should be kept to a minimum as they have to be disinfected after use. The distance between the patient and the physiotherapist should be at least 1 meter. The room should have a sink, a stand for soap and one for disinfectant, and a closed trash bin and disposable paper towels should be used [35, 36].
Telemedicine is an initiative aimed at reducing contact between people and preventing the spread of SARS-CoV-2 infection by limiting patient contact with other healthy individuals [35, 37]. Our results indicate that overall 91.7% of the PTs advised their patients to perform exercises at home and provided tele-consultation. This can play an important role in preventing the spread of COVID-19 disease.
It was found that 88.0% of physiotherapists were aware of the importance of wearing medical masks, clean non-sterile medical gowns, and gloves during the treatment. Wearing of personal protective equipment to prevent the spread of SARS-CoV-2 infections is strongly recommended [31, 37].
5Conclusions
This study revealed that Pakistani PTs included in the study possessed a good knowledge of SARS-CoV-2 infection and implemented best practices in their Outpatient Physiotherapy at a good level. Convenience sampling was used to conduct a quick survey, keeping in mind the rapidly changing dynamics of the COVID-19 pandemic, which can make any study on COVID-19 quickly lose relevance if stretched for a long period of time. Only the PTs located in two major cities in Punjab, Pakistan were included in this study. Thus, the results may not reflect the true situation in the smaller cities or rural areas of Pakistan. The PTs should continue to strengthen their knowledge and upgrade their OPD management skills to provide rehabilitation support to patients in a safe manner, while ensuring their own safety. Strictly following the guidelines of the local authorities, hospitals, government, WHO, WCPT and the PT associations will help prevent the spread of COVID-19 disease. To the best of our knowledge, this is considered to be the first study of physical therapists’ knowledge of COVID-19 and the implementation of best practices in outpatient physical therapy by physical therapists during the COVID-19 pandemic.
Acknowledgments
The authors thank all participants who volunteered to take part in this study.
Conflict of interest
None to report.
References
[1] | Lai C-C , et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-(COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. (2020) ;55: (3):105924. |
[2] | Government P . COVID-19 Health Advisory Platform by Ministry of National Health Services Regulations and Coordination. 2021 [cited 2021 September 16]; Available from: https://covid.gov.pk/. |
[3] | Kursumovic E , Lennane S , Cook T . Deaths in healthcare workers due to COVID-19: the need for robust data and analysis. Anaesthesia, 2020. |
[4] | Saqlain M , et al. Knowledge, attitude and practice among healthcare professionals regarding COVID-19: A cross-sectional survey from Pakistan. Journal of Hospital Infection, 2020. |
[5] | Shrivastava D , et al. Assessment of knowledge and attitude of allied healthcare professionals about COVID-19 across Saudi Arabia. Work. 2021: (Preprint):1–11. |
[6] | Cox CL . ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. Journal of Medical Ethics. (2020) ;46: (8):510–3. |
[7] | Bhagavathula AS , et al. Novel coronavirus (COVID-19) knowledge and perceptions: a survey on healthcareworkers. MedRxiv, 2020. |
[8] | Lazzeri M , et al. , Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Archives for Chest Disease. (2020) ;90: (1). |
[9] | Thomas P , et al. , Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. Journal of Physiotherapy. (2020) ;66: (2):73–82. |
[10] | Wittmeier K , et al. Operational Considerations for Physical Therapy During COVID- A Rapid Review. Physical Therapy. (2020) ;100: (11):1917. |
[11] | Zhu Y , et al. Summary of respiratory rehabilitation and physical therapy guidelines for patients with COVID-19 based on recommendations of World Confederation for Physical Therapy and National Association of Physical Therapy. Journal of Physical Therapy Science. (2020) ;32: (8):545–9. |
[12] | Felten-Barentsz KM , et al. Recommendations for hospital-based physical therapists managing patients with COVID-19. Physical Therapy. (2020) ;100: (9):1444–57. |
[13] | Shanthanna H , et al. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia. (2020) ;75: (7):935–44. |
[14] | Kashif M , et al. The role of the physiotherapist in a pandemic situation: a covid-19 outbreak perspective. RMJ. (2021) ;46: (2):485–87. |
[15] | Lin Y-H , Liu C-H , Chiu Y . -C. Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain, Behavior, and Immunity. (2020) ;87: :30–2. |
[16] | Cawthorne K-R , Cooke RP . Innovative technologies for hand hygiene monitoring are urgently needed in the fight against COVID-19. Journal of Hospital Infection. (2020) ;105: (2):362–3. |
[17] | Thampi N , et al. It’s in our hands: a rapid, international initiative to translate a hand hygiene song during the COVID-19 pandemic. Journal of Hospital Infection. (2020) ;105: (3):574–76. |
[18] | Gon G , et al. Reducing hand recontamination of healthcare workers during COVID-19. Infection Control & Hospital Epidemiology. (2020) ;41: (7):870–1. |
[19] | Rundle CW , et al. Hand hygiene during COVID-19: recommendations from the American contact dermatitis society. Journal of the American Academy of Dermatology. 2020. |
[20] | Mahmood A , et al. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Science of the Total Environment. (2020) ;742: :140561. |
[21] | Director-General’s W . WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020 [cited 2021 31st April 2021]; Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. |
[22] | Chan JF-W , et al. A familial cluster of pneumonia associated with the novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet. (2020) ;1022: (3953)514–23. |
[23] | Yu P , et al. A familial cluster of infection associated with the novel coronavirus indicating possible person-to-person transmission during the incubation period. The Journal of Infectious Diseases. (2020) ;221: (11):1757–61. |
[24] | Bai Y , et al. Presumed asymptomatic carrier transmission of COVID-19. Jama. (2020) ;323: (14):1406–7. |
[25] | Kimball A , et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. Morbidity and Mortality Weekly Report. (2020) ;69: (13):377. |
[26] | Organization WH. Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020. 2020, World Health Organization. |
[27] | Jordan RE , Adab P , Cheng K . Covid-19: risk factors for severe disease and death. (2020) , British Medical Journal Publishing Group. |
[28] | Mo P , et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clinical Infectious Diseases, 2020. |
[29] | O’Dowd K , et al. Face masks and respirators in the fight against the COVID-19 pandemic: a review of current materials, advances and future perspectives. Materials. (2020) ;13: (15):3363. |
[30] | Czubryt M , et al. N95 mask reuse in a major urban hospital: COVID-19 response process and procedure. Journal of Hospital Infection. (2020) ;106: (2):277–82. |
[31] | Sickbert-Bennett EE , et al. Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Internal Medicine. (2020) ;180: (12):1607–12. |
[32] | Isaacs D , et al. Do facemasks protect against COVID-19? Journal of Paediatrics and Child Health. (2020) ;56: (6):976. |
[33] | Radonovich LJ , et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. Jama. (2019) ;322: (9):824–33. |
[34] | Long Y , et al. Effectiveness of N95 respirators versus surgical masks against influenza: a systematic review and meta-analysis. Journal of Evidence-Based Medicine. (2020) ;13: (2):93–101. |
[35] | Al Attar WSA , Husain MA . Physiotherapists’ knowledge and the implementation of COVID-19 infection prevention and control measures. Work. 2021: (Preprint): p. 1–8. |
[36] | Ladner-Nitsche A . Guidelines for COVID-19 adaptations and changes in professional procedures in outpatient physiotherapy private solo practices. |
[37] | Zhao Y , et al. Personal protective equipment protecting healthcare workers in the Chinese epicentre of COVID-19. Clinical Microbiology and Infection. (2020) ;26: (12):1716–8. |




