Impact of workplace yoga on pain measures, mental health, sleep quality, and quality of life in female teachers with chronic musculoskeletal pain: A randomized controlled study
Abstract
BACKGROUND:
Chronic pain conditions such as low back pain, knee pain and cervical pain are highly prevalent among female teachers. Chronic pain significantly affects the mental health, sleep and quality of life among teachers.
OBJECTIVE:
This study is intended to investigate the impact of a workplace yoga intervention on musculoskeletal pain, anxiety, depression, sleep, and quality of life (QoL) among female teachers who had chronic musculoskeletal pain.
METHOD:
Fifty female teachers aged between 25–55 years with chronic musculoskeletal pain were randomized to either the yoga group (n = 25) or the control group (n = 25). The yoga group received a 60-minute structured Integrated Yoga intervention (IY) four days a week for six consecutive weeks at school. The control group received no intervention. Outcome measures: Pain intensity, anxiety, depression, stress, fatigue, self-compassion, sleep quality, and quality of life were assessed at the baseline and six weeks.
RESULTS:
A significant (p < 0.05) reduction in pain intensity and pain disability in the yoga group was observed after 6-week compared to baseline. Anxiety, depression, stress, sleep scores and fatigues also improved in the yoga group after six weeks. The control group showed no change. Post score comparison showed a significant difference between the groups for all the measures.
CONCLUSION:
Workplace yoga intervention is found to be effective in improving pain, pain disability, mental health, sleep quality among female teachers with chronic musculoskeletal pain. This study strongly recommends yoga for the prevention of work-related health issues and for the promotion of wellbeing among teachers.
1Introduction
Teachers help to shape young minds and turn them into responsible citizens of society. In addition to teaching, teachers are involved in various other activities such as participating in meetings, committees, assignments, assessments, and counseling in the school which contributes to increased burden. Evidence indicates that a significant number of teachers experience stress and burnout. Particularly female teachers find it more challenging compared to male teachers as they have added responsibilities of household activities, including caring for children and/or the elderly at home. Such stressors often contribute to increased burnout, stress and poor mental health, contributing to chronic musculoskeletal problems (cMSP) [1, 2].
The pain related to muscles, bones, ligaments, tendons, and nerves is called musculoskeletal pain. cMSP is one of the frequently reported health issues among teachers contributing to significant disability and distress [3]. Teaching involves task such as standing for long hours, blackboard activities, talking, monitoring, and mentoring, and teachers are expected to stand for a long time [4, 5]. Such activities often lead to pain in the wrist, low back pain, neck pain, shoulder pain, and pain in the knees and hip, which are common cMSP sites among teachers [6].
The prevalence of cMSP among teachers varies between 50–84% and and it ranges from 50–70% among Indian teachers [7, 8]. In a survey study of 525 Brazilian teachers (452 females teachers), a 73% prevalence of cMSP was reported [9]. In another study, teachers from 15 primary schools were followed up for six months. The study revealed that 80% of teachers had musculoskeletal disorders during the study period, and the musculoskeletal problem was associated with increased depression [10]. In another study among 1482 teachers in Malaysia, 40% teachers had low back pain, and 60% had neck pain in the past 12 months [11].
cMSP among teachers is found to be multifactorial in origin. Factors such as mental health, social factors, individual habits and lifestyle, physical activity, and gender (females are more prone) are found to be common causes. Evidence suggests that female teachers have a heightened risk of cMSP compared to their male colleagues; this could be due to lower pain thresholds and pain tolerance among females [12–14]. Furthermore, teachers are often paid less compared to the amount work load they have. cMSP has a negative impact on sleep quality. A study among 242 teachers reported that teachers who had poor sleep quality have two times greater pain compared to teachers who had better sleep quality [15].
Evidence suggests that psychological factors contribute to increased incidences of exacerbation of cMSP [16, 17]. Psychosocial factors such as increased stress, poor social support, low job satisfaction, and increased workload are found to be associated with an increased risk of cMSP among teachers [18–20]. Depression and anxiety are highly prevalent psychopathologies among individuals with chronic pain [21]. Both contribute to increased pain and pain-related disability among such individuals [22]. Evidence also suggests that female teachers have higher anxiety and depression compared to male teachers [23]. In a study, self-reported low back pain was found to be associated with anxiety, depression and stress among teachers, and in the same study, self-reported neck pain was associated with anxiety, depression, and poor mental health [24]. Teachers with cMSP tend to opt for more sick leaves, absenteeism, and early retirement more often than controls [25]. cMSP affects work efficacy, enthusiasm, and concentration. Disability due to chronic pain also has a negative impact on the quality of life [26].
Yoga is a traditional system of mind-body practice that aims to correct bio-rhythms through a harmonious connection between mind, body, and breath. Yoga practice reduces stress and relaxes the mind and body. It also enhances autonomic balance, metabolism, and endocrine functions [27–29]. Studies have demonstrated that yoga improves pain, spinal flexibility, and quality of life in patients with chronic musculoskeletal pain, such as low back pain [30]. Previous studies have demonstrated the feasibility and efficacy of workplace yoga among different working professionals. Workplace yoga is found to be effective in improving the physical and mental health of employees [31, 32]. Studies have reported a positive impact of spiritual practices and prayers among teacher with stress and burnout [33, 34]. Literature suggests a lack of yoga studies on cMSP among teachers.
Thus, the current study intended to investigate the effect of 6-week workplace yoga intervention on pain intensity, severity, and sleep quality, and mental health measures among female teachers with chronic musculoskeletal pain.
2Methods
2.1Participants
Participants in this study were female teachers with cMSP working in secondary schools.
2.1.1Ethics compliance
The study was approved by the Institutional Ethics Committee (IEC) of Swami Vivekananda Yoga Anusandhana Samsthana (SVYASA University) (IEC No. RES/IEC-SVYASA/135/2019).
2.2Inclusion and exclusion criteria
Consenting female teachers within the age group 20–50 years with pain disability index score > 30 were recruited into the study. We chose only female teachers because we intended to study the impact of yoga exclusively among female teachers as their there stress levels are completely different and they are more vulnerable for cMSP compared to male teachers.
Participants who had uncontrolled diabetes, thyroid function disorders, uncontrolled hypertension, heart disease, psychiatric medications, morbid obesity, pregnancy, or abdominal surgery within the past 1-month were excluded from the study. In addition, participants who had previous exposure to any form of yoga in the past one year (with regular practice for more than one month in the past one year) were also excluded from the study.
2.3Procedure
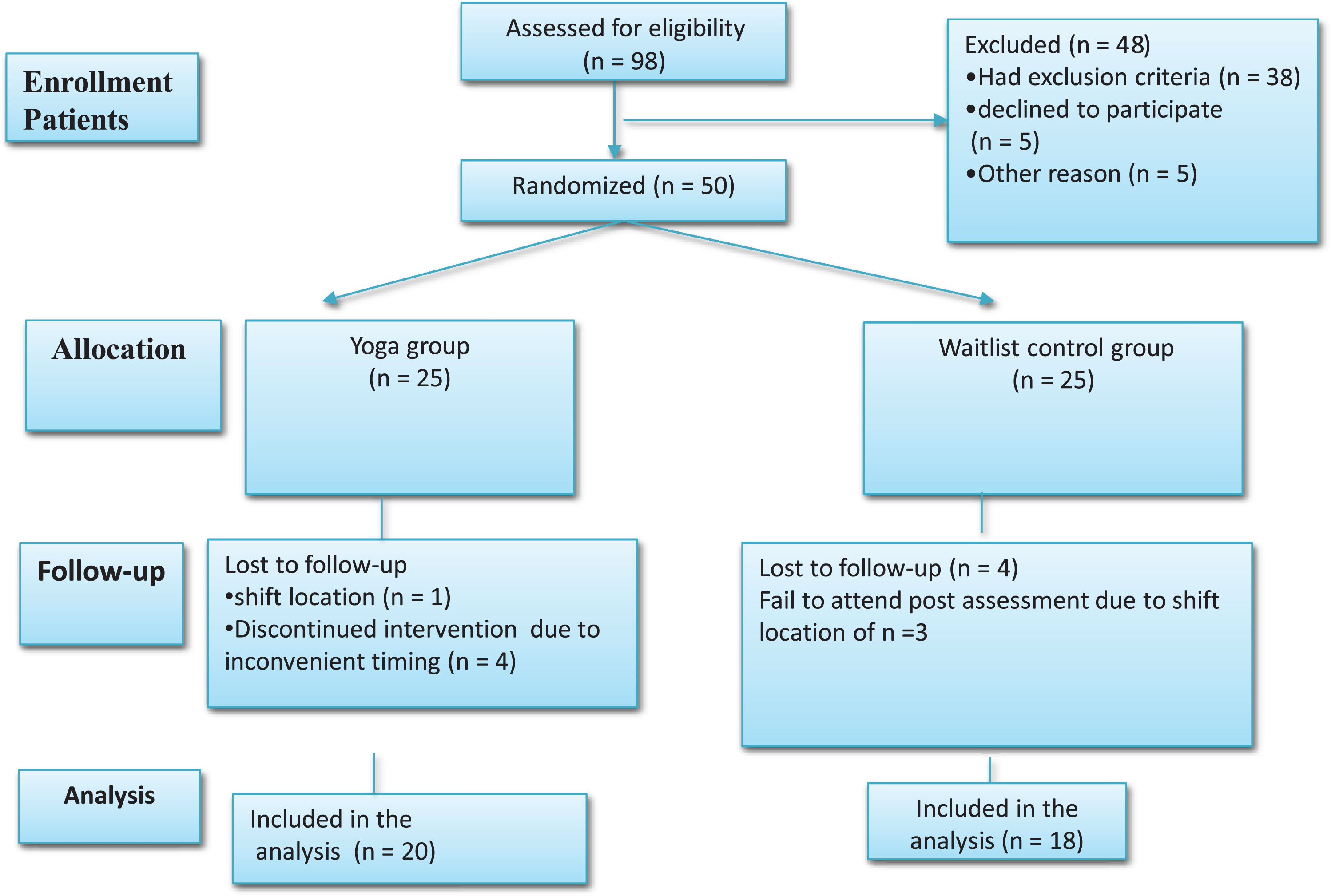
Two private English-medium schools were selected for the study. An advertisement about the study was published on the notice board of the two schools and interested participants were interviewed for eligibility. A total of 98 teachers were screened for eligibility criteria. Forty-eight participants were excluded; of these, 38 had exclusion criteria, five refused to participate, and five were not convinced with intervention. Fifty were randomized into either yoga group or control group.
2.4Randomization
Randomization was done in two stages using a computer-based random number generator (https://www.google.com/search?q=random+number). All participants’ names were arranged in alphabetical order, and then they were numbered from 1– 50. Two groups were formed (consisting of 25 members in each group); group A and group B were obtained using a computer-based random number generated. The toss method was used to assign one set for intervention and the other for the controlgroup.
Randomization was done by an independent computer expert who was not associated with the study and was blind to the groups. Allocation concealment was followed during randomization.
2.5Intervention
Participants in the yoga group received a 60-minute integrated yoga session each day, four days a week, for six continuous weeks. Participants in the yoga groups were advised to attend either enter every day’s or daily yoga session between 4:30–5:30 PM at the school. Participants were advised to come for a yoga session on an empty stomach/minimum of 2 hours after the meal. They were encouraged to wear stretchable and comfortable clothes for yoga practice. After yoga sessions, participants were encouraged to ask the yoga expert to address their yoga practice queries. A certified trained yoga expert administered yoga sessions. A structured yoga module consisting of loosening practices, yoga poses, breathing practices, relaxation techniques, and meditation was used (Table 1).
Table 1
Yoga module
| Type of practice | Name of the practices |
| Loosening practices | Loosening of all small joints, drill walking, spinal twisting, hip rotation, padasanchalana, kartal shaktivikasaka |
| Breathing practices | Hands in and out breathing, hands stretch breathing, ankle stretch breathing, tiger breathing, setubandhasana breathing, bhujangasana breathing |
| Asana | Halh-wheel pose (ardhachakrasana), half-waist pose (ardhakatichakrasana), camel pose (ustrasana), bhunamanasana, bridge pose (setubandhasana), bhujangasana (snake pose), pavanamuktasana, lumbar stretches in supine (jatharpeedan kriya) |
| Pranayama | Alternate nostril breathing (nadishodhana pranayama), bhramari (humming), cooling pranayama, vibhagiya pranayama |
| Meditation | Mindfulness meditation and om meditation |
| Relaxation | Deep relaxation, quick relaxation, and yoga nidra |
The control group participants did not receive yoga intervention, and they were advised to follow their routine activities. No major change in diet and physical activity were noted in the control group during the study period.
2.6Assessments
The assessments were performed by a team consisting of a psychologist and two assistants. This team was blinded to the groups. All the assessments were performed twice: at baseline and after 6-weeks. Baseline assessments were performed prior to randomization. Scoring and data entry were done by the assessment team.
2.7Primary outcome measures
2.7.1Pain disability
Pain Disability Questionnaire (PDQ): It is considered a valid and reliable tool to assess pain-related disability in patients with chronic musculoskeletal pain [35] with Cronbach’s alpha 0.96 [36]. This is a self-reported questionnaire that evaluates a patient’s perceived disability due to pain. The patient is asked to rate how pain has restricted their routine activity on a 0–10 scale; the higher the score, the greater the perceived disability. PDQ scores between 0–70 indicate mild/moderate disability; 71–100 indicate severe disability, and 101 and above indicate extreme disability. Also, PDQ measures both physical and psychosocial factors indecently.
2.7.2Pain assessments
a) Numerical Pain Rating Scale (NPRS)
It assesses the pain severity in various pain conditions including cMSP. The patient is expected to rate their subjective pain feeling on a 0 to 10 scale, with 0 being no pain and 10 being extreme pain. NPRS is recognized as a valid tool to assess pain severity in musculoskeletal pain patients. It is a valid tool to measure pain intensity [37]. Its test– retest reliability was found to be varying from 0.67 to 0.96, with convergent validity from 0.79 to 0.95 [38].
b) Sleep quality
PSQI is considered a valid and reliable tool with a test-retest reliability of 0.87. It is a widely used tool to assess subjective sleep quality in both clinical and non-clinical populations. It consists of six aspects of sleep: sleep quality, sleep latency, sleep duration, sleep disturbance, daytime dysfunction, and medication use. A global score of 0– 21 is possible, wherein a score over five is considered sleep impairment [39].
c) Secondary outcome measures
2.7.3Psychological measures
Stress, anxiety, and depression were measured using the Depression, Anxiety, and Stress Scale 21 (DASS 21).
a) DASS 21
DASS 21 is a valid and reliable questionnaire that assesses subjective depression, anxiety, and stress in both clinical and non-clinical populations. This scale consists of 3 subscales of 7 items; each subscale measures depression, stress, and anxiety. The depression scale measures dysphoric mood states, a feeling of hopelessness, and low interest. The anxiety scale assesses anxious mood, autonomic arousal, and muscle tension. The stress scale assesses emotional vulnerability to stressor and tension [40]. Its Cronbach’s alpha was found to be 0.83 [41].
b) Quality of life was assessed using WHO-QoL-BRIEF
WHO-QoL-BRIEF is considered a valid tool to assess subjective quality of life. It consists of 26 questions, wherein participants rated on a 5-point Likert scale their perception about the quality of life in the past four weeks. WHO-QoL-BRIEF consists of four domains. These domains assess four aspects of life: physical health, psychological health, social relationship, and environment [42].
c) Physiological assessments
Systolic and diastolic blood pressure and pulse rate were also assessed in the morning session between 9– 10 am. Participants asked to relax for 10 minutes before assessment. OMRAN electric BP measuring device was used. Body Mass Index was calculated using height and weight. Formula: BMI = Weight (kg)/Height (M)2.
2.8Ethical comply
The institutional Ethics Committee approved the study (Approval no. RES/IEC/SVYASA/135/2019). The study was conducted in accordance with the Declaration of Helsinki for research that includes human subjects. The study was conducted between August 2019 and January 2020. All participants signed a written consent form, which was explained orally. Participants were explained that they could walk out of the study at any point during the study if they wished, and patients’ information was kept confidential. The group was offered yoga sessions after the study period was over.
2.9Statistical analysis
Continuous variables were represented as mean±S.D., whereas; categorical variables were represented as numbers (percentage). ANOVA model was run to assess the treatment effect across the two study groups. The between-subjects model factor was group, and within-subjects factors were time (pre and post) and interaction of group by time. Paired sample t test was used to ascertain the within-group treatment effect from baseline to follow-up. p < 0.05 was considered as statistically significant throughout the analysis. Stata ver. 13.1 was used for statistical analysis. Independent variable was yoga interventional and pain measures, anxiety, depression stress and quality life were the dependent variables.
3Results
Five teachers in the yoga group and seven teachers in the control group dropped out due to personal reasons (See Fig. 1). Twenty teachers in the yoga group and eighteen in the control group completed the study.
Fig. 1
CONSORT flowchart.
The average age and baseline score for all the assessments are depicted in Table 2. Both groups were comparable at the baseline in terms of BMI, years of experience, age, duration of the pain, and working hours in the school (Table 2).
Table 2
Baseline characteristics of the participants
| Characteristics | Total | Yoga group | Control group | p |
| (n = 38) | (n = 20) | (n = 18) | value | |
| Age (years) | 39.37±6.97 | 39.8±7.37 | 38.88±6.67 | >0.05 |
| BMI | 26.69±4.63 | 27.36±4.80 | 25.93±4.45 | >0.05 |
| Mean duration of pain | 4.6±2.5 | 4.3±2.8 | 4.9±3.2 | >0.05 |
| Mean workload (hrs)/day | 5.2±2.1 | 5.1±1.9 | 5.3±2.2 | >0.05 |
| SBP (mmHg) | 126.84±12.79 | 127.6±12.63 | 126±13.27 | >0.05 |
| DBP (mmHg) | 79.60±6.65 | 81.1±7.13 | 77.94±5.81 | >0.05 |
| Pulse rate (bpm) | 81.21±9.91 | 84.7±9.10 | 77.33±9.53 | >0.05 |
| QoL_D1 | 23.52±2.85 | 22.55±2.91 | 24.61±2.42 | >0.05 |
| QoL_D2 | 21.26±2.72 | 21.05±2.94 | 21.5±2.52 | >0.05 |
| QoL_D3 | 12.15±1.96 | 12.45±1.93 | 11.83±2.00 | >0.05 |
| QoL_D4 | 29.86±4.39 | 30±5.11 | 29.72±3.56 | >0.05 |
| QoL_Total scores | 97.92±11.39 | 97.95±12.75 | 97.88±10.04 | >0.05 |
| PSQI score | 5.81±3.16 | 5.7±3.52 | 5.94±2.81 | >0.05 |
| FSS scores | 31.86±11.33 | 32.95±11.32 | 30.66±11.54 | >0.05 |
| PDI_D1 | 24.65±15.63 | 22.9±16.44 | 26.61±14.90 | >0.05 |
| PDI_D2 | 13.60±12.27 | 14.2±14.70 | 12.94±9.25 | >0.05 |
| PDI_Total score | 38.26±26.73 | 37.1±30.38 | 39.55±22.82 | >0.05 |
| NPAS | 4.07±2.04 | 3.85±2.15 | 4.33±1.94 | >0.05 |
| VPAS | 1.71±0.83 | 1.7±0.86 | 1.72±0.82 | >0.05 |
| Anxiety | 11.42±8.34 | 11.5±9.83 | 11.33±6.57 | >0.05 |
| Depression | 8.57±7.08 | 8.9±8.57 | 8.22±5.17 | >0.05 |
| Stress | 11.26±7.19 | 10.6±8.53 | 12±5.48 | >0.05 |
| SC | 39.94±7.36 | 39.4±7.59 | 40.55±7.26 | >0.05 |
Abbreviations: BMI-Body Mass Index, SBP-Systolic Blood Pressure, DBP-Diastolic Blood Pressure, QoL - Quality of life, PSQI-Pittsburgh’s Sleep Quality Index, FSS-Fatigue Severity Index, PDI-Pain Disability Index, NPRS-Numerical Pain Rating Scale, VPRS-Visual Pain Rating Scale, SC-Self compassion. No significant difference was observed on baseline comparison.
3.1Changes in the outcome measures
A statistically significant decrease in the SBP, DP, and heart rate was noticed in the yoga group post-intervention compared to the baseline.
At 6-week, in the between groups comparison there was a significant difference in all the variables except pulse, physical domain of QoL, and stress. This suggests a positive impact of 6-week yoga intervention on cardiac parameters, mental health measures, QoL, and sleep quality measures (Table 3).
Table 3
Physiological measures
| Measures | Assessments | Yoga group | Control group | f-value | @p-value | Effect size (95% CI) |
| BMI | Baseline | 27.36±4.80 | 25.93±4.45 | 7.60 | 0.0093 | 0.18(0.012, 0.39) |
| 6-week | 27.19±4.81 | 26.02±4.59 | ||||
| p value$ | 0.0295 | 0.1868 | ||||
| SBP | Baseline | 127.6±12.63 | 126±13.27 | 18.0 | 0.0002 | 0.34(0.10–0.53) |
| 6-week | 117.85±11.31 | 129.44±11.79 | ||||
| p value$ | 0.0014 | 0.055 | ||||
| DBP | Baseline | 81.1±7.13 | 77.94±5.81 | 13.34 | 0.0009 | 0.28(0.05, 0.48) |
| 6-week | 76.3±7.88 | 81.33±4.43 | ||||
| p value$ | 0.068 | 0.001 | ||||
| Heart rate | Baseline | 84.7±9.10 | 77.33±9.53 | 7.02 | 0.0121 | 0.17(0.008, 0.37) |
| 6-week | 77.65±8.49 | 80.44±8.88 | ||||
| p value$ | 0.0072 | 0.0145 |
Abbreviations: BMI-Body Mass Index, SBP-Systolic Blood Pressure, DBP-Diastolic Blood Pressure.$Within group pre-post comparison. @Between group post intervention comparison.
A significant decrease in the pain disability and pain intensity in the yoga group compared to the control group was noticed (Table 4) at 6 weeks.
Table 4
Changes in pain measures
| PDI scores | ANOVA | |||||
| Measures | Assessments | Yoga group | Control group | F value | @p-value | Effect size (95% CI) |
| D1 | Baseline | 22.9±16.44 | 26.61±14.90 | 15.22 | 0.0004 | 0.30 (0.07, 0.50) |
| 6-week | 14.95±14.23 | 33.27±14.27 | ||||
| $P value | 0.0638 | 0.051 | ||||
| D2 | Baseline | 21.05±2.94 | 21.5±2.52 | 15.51 | 0.0004 | 0.31 (0.07, 0.50) |
| 6-week | 5.9±6.58 | 14±6.91 | ||||
| $P value | 0.016 | 0.6147 | ||||
| Total | Baseline | 37.1±30.38 | 39.55±22.82 | 18.08 | 0.0002 | 0.34 (0.10, 0.53) |
| 6-week | 20.85±20.26 | 47.27±19.21 | ||||
| $P value | 0.0278 | 0.605 | ||||
| PAS numerical | ||||||
| NPRS | Baseline | 3.85±2.15 | 4.33±1.94 | 22.31 | P < 0.001 | 0.39(0.14, 0.57) |
| 6-week | 2.1±1.77 | 4.33±1.23 | ||||
| $P value | 0.0005 | 1 | ||||
| VPAS | Baseline | 1.7±0.86 | 1.72±0.82 | 42.17 | P < 0.001 | 0.55(0.30, 0.69) |
| 6-week | 0.75±0.55 | 1.94±0.63 | ||||
| $P value | 0.0001 | 0.298 | ||||
Abbreviations: PDI- Pain Disability Index, D1-, D2-, NPRS-Numerical Pain Rating Scale, VPAS-Visual Pain Assessment Scale. $Within group pre-post comparison. @Between group post intervention comparison.
Anxiety, depression, stress, and fatigue decreased after 6 weeks compared to the yoga group’s baseline compared to the control group (Table 5).
Table 5
Changes in the psychological measures
| Measures | Assessments | Yoga group | Control group | F-value | @p-value | Effect size (95% CI) |
| Anxiety | Baseline | 11.5±9.83 | 11.33±6.57 | 6.78 | 0.0136 | 0.16 (0, 0.37) |
| 6-week | 4.9±6.30 | 10.22±6.68 | ||||
| $P value | 0.0024 | 0.6073 | ||||
| Depression | Baseline | 8.9±8.57 | 8.22±5.17 | 5.81 | 0.0293 | 0.13 (0, 0.13) |
| 6-week | 4.5±5.42 | 9.88±8.66 | ||||
| $P value | 0.0543 | 0.4858 | ||||
| Stress | Baseline | 10.6±8.53 | 12±5.48 | 2.66 | 0.1122 | 0.07 (0, 0.266) |
| 6-week | 6.7±6.06 | 10.88±8.20 | ||||
| $P value | 0.0295 | 0.6392 | ||||
| SC | Baseline | 39.4±7.59 | 40.55±7.26 | 17.03 | 0.0002 | 0.33 (0.09, 0.52) |
| 6-week | 45.7±6.82 | 38.55±6.30 | ||||
| $P value | 0.002 | 0.1175 | ||||
| PSQI score | Baseline | 5.7±3.52 | 5.94±2.81 | 8.49 | 0.0063 | 0.19 (0.18, 0.40) |
| 6-week | 3.9±1.74 | 5.33±2.19 | ||||
| $P value | 0.013 | 0.0445 |
Abbreviations: SC- Self Compassion, PSQI- Pittsebrg’s Sleep Quality Index. $Within group pre-post comparison. @Between group post intervention comparison.
In the yoga group, there was a significant decrease in the score of anxiety (–54%, d = 0.78), depression (–54%, d = 0.7), and stress (–34.5%, d = 0.5) of DASS-21 after 6 weeks compared to baseline. Similarly, global sleep quality improved significantly (–32.3%, d = 0.72), among sleep measure daytime dysfunction (–35%, d = 0.44) and habitual sleep efficiency (–88%, d = 0.8) improved significantly.
Significant improvement in all domains of the QoL was found in the yoga group at 6 weeks compared to baseline. No change was noticed in the control group. There was a significant difference in the between-group comparison (Table 6).
Table 6
Changes in the quality of life measures
| Quality of life | ANOVA | |||||
| Measures | Assessments | Yoga group | Control group | F-value | p-value | Effect size (95% CI) |
| Physical | Baseline | 22.55±2.91 | 24.61±2.42 | 2.79 | 0.018 | 0.07 (0, 0.27) |
| 6-week | 25.2±2.44 | 24.05±1.95 | ||||
| P value | 0.0119 | 0.172 | ||||
| Psychological | Baseline | 21.05±2.94 | 21.5±2.52 | 15.2 | 0.0004 | 0.30 (0.74, 0.50) |
| 6-week | 23.4±2.39 | 20.72±1.96 | ||||
| P value | 0.0115 | 0.1397 | ||||
| Social | Baseline | 12.45±1.93 | 11.83±2.00 | 0.68 | 0.4139 | 0.019 (0, 0.17) |
| 6-week | 13±1.48 | 6.44±1.42 | ||||
| P value | 0.2645 | 0.666 | ||||
| Environmental | Baseline | 30±5.11 | 29.72±3.56 | 16.14 | 0.0003 | 0.32 (0.08, 0.51) |
| 6-week | 33.75±3.82 | 29.16±2.99 | ||||
| P value | 0.021 | 0.5288 | ||||
| Total scores | Baseline | 97.95±6.75 | 97.88±10.04 | 19.34 | 0.0001 | 0.36 (0.11, 0.54) |
| 6-week | 111.4±10.67 | 97.61±7.81 | ||||
| P value | 0.0024 | 0.8994 | ||||
$Within group pre-post comparison. @Between group post intervention comparison.
In the yoga group in the first week of the intervention, 5 teachers reported an increase in body ache. This could be in response to stretches during asanas practice, which got resolved after the 2nd week of the intervention. Overall, no serious symptoms due to yoga practice were reported during the 6-week yoga intervention.
4Discussion
This study reports a positive impact of a 6-week yoga intervention on pain measures, anxiety, depression, stress, fatigue, sleep quality, and quality of life among female teachers with cMSP pain. Musculoskeletal problems are the most common problems among teachers that significantly affect the mental health and quality of life of the teachers. This study suggests the usefulness of yoga intervention at school in the prevention and management of cMSP among female teachers.
We observed improvement in physiological measures and anxiety in the yoga group, which is suggestive of improvement in autonomic balance following yoga intervention, as reported in several studies [43].
Previous studies on yoga have reported improved chronic pain [44, 45], mental health domains, sleep quality, and quality of life [46–48] following yoga intervention.
Previously, in an randomized controlled study, Karen et al. compared the impact of a 6-week yoga, exercise, and self-care book intervention on back-related functional status and bothersome among 110 chronic low back pain patients. Thirty-four patients received yoga, 32 accepted activities, and 29 followed self-care [49]. This study reported that yoga intervention was superior to exercise and self-care books regarding back-related functions at 6 weeks. Another study by Cramer et al. reported significant improvement in pain functional disability and quality of life following a 9-week yoga intervention as compared to home-based exercise among patients with chronic neck pain [50]. The findings of the present study also align with the observations of Cramer and Karen. However, neither included teachers.
Previous studies on yoga have reported a positive impact of yoga on mental health. A study by Shohani et al. reported a significant improvement in stress, anxiety, and depression following a 4-week yoga intervention of 3 sessions/week [51]. In the present randomized controlled study, we also observed a significant decrease in anxiety, stress, and depression in the yoga group. Further, in our study, we observed that the number of teachers with clinical depression, anxiety, and higher stress at the baseline significantly reduced after an intervention, whereas, in the control group, it significantly increased.
Chronic pain has a significantly negative impact on the quality of life. Yoga has been found to be an effective intervention in improving the quality of life in chronic pain conditions such as chronic low back pain. In a study by Nitin et al., 44 female nurses received a 6-week yoga intervention, and another group of 44 nurses served as a control group. Post-intervention, nurses in the yoga group demonstrated significant improvement in physical, psychological, and social domains of life [52]. Similar results have been found in the present study also.
Similarly, a study by Wieland reported a significant improvement in the quality of life of CLBP patients following one week of residential yoga intervention [53]. There is a negative correlation between pain with sleep quality. Poor sleep quality often worsens the existing pain and contributes to an increase in the need for medication. It contributes to the deterioration of mental well-being.
Yoga has been shown to have beneficial effects on sleep quality in patients with chronic pain. Previously, in a multicenter, randomized controlled trial study, a 4-week yoga intervention produced significant improvement in different sleep domains such as subjective sleep quality, daytime dysfunction, wake after sleep onset, sleep efficiency, and medication in patients with cancer [54]. Further, studies on spiritual practices have reported a positive impact of such practices on the mental health of employees [55].
The present study also confirms yoga’s positive role in stress prevention and the promotion of physical and mental health. To the best of our knowledge, the present study is the first to report yoga’s efficacy among female teachers with cMSP. Previously, Rao et al. reported significant mental health and sleep quality improvements among female teachers following 4-week yoga-based meditation (MSRT) intervention [56]. This study differs from the present study regarding the type of intervention, assessment, and population.
The present study results suggest the potential role of yoga in the prevention of cMSP and associated psychopathology and poor quality of life among female teachers. In addition, yoga may also contribute to enhanced productivity and enthusiasm in teaching.
Improvements in pain following yoga intervention may be attributed to modulation in pain perception, pain tolerance, and reduced muscle ischemia by enhancing micro-circulation. Various yoga postures, breathing practices, and meditation techniques increase the practitioner’s attention to inner sensations and enhance non-reaction to unpleasant sensations such as pain. This contributes to the increased pain tolerance [57]. Further, yoga is known to enhance circulatory endorphins and serotonin levels, which have analgesic effects [58]. It also improves melatonin, GABA levels, reduces sympathetic over activity, and enhances vagal tone; these changes might enhance the quality of sleep and mental health [59]. Improvement in overall activity, mood, and functionality may facilitate improvement in the quality of life. The present study has several limitations, such as small sample size, short-term intervention, and lack of objective assessment methods. Further studies addressing this limitation are warranted. This study lacked the studying of mechanisms of action of yoga.
5Conclusion
cMSP is a commonly reported health issue among teachers. It may have significant negative impact on mental health, sleep and quality life. The present study provides beneficial effects of yoga intervention at school in improving cMSP, mental health, sleep, and QoL measures among female teachers with a pain disability. This study recommends yoga practice at workplace to manage musculoskeletal pain and mental and sleep quality among teachers. Further studies with a larger sample size and long-term intervention using objective assessment methods are warranted.
Ethical approval
The study was approved by the Institutional Ethics Committee (IEC) of Swami Vivekananda Yoga Anusandhana Samsthana (SVYASA University) (IEC No. RES/IEC-SVYASA/135/2019).
Informed consent
All study participants were informed about the study protocol and their duly signed written consent form was obtained prior to the study commencement.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors thank all the administrative staff of the school for their valuable support and cooperation during the study.
Funding
This study was not funded by any government or private funding agency.
References
[1] | Chirico F , Capitanelli I , Bollo M , Ferrari G , Acquadro Maran D . Association between workplace violence and burnout syndrome among schoolteachers: A systematic review. J Health Soc Sci. (2021) ;6: (2):187–208.10.19204/2021/ssct6. |
[2] | Antoniou AS , Ploumpi A , Ntalla M . Occupational stress and professional burnout in teachers of primary and secondary education: The role of coping strategies. Psychology. (2013) ;4: (03):349. |
[3] | Vargas-Prada S , Coggon D . Psychological and psychosocial determinants of musculoskeletal pain and associated disability. Best Practice & Research Clinical Rheumatology. (2015) ;29: (3):374–90. |
[4] | Erick PN , Smith DR . Low back pain among school teachers in Botswana, prevalence, and risk factors. BMC Musculoskelet Disord [Internet]. (2014) Oct 30 [cited 2020 Aug 19]; 15: (1):1–13. Available from. https://link.springer.com/articles/10.1186/1471-2474-15-359. |
[5] | Kovač M , Leskošek B , Hadžić V , Jurak G . Occupational health problems among Slovenian physical education teachers. Kinesiology. (2013) ;45: (1.):92–100. |
[6] | Rottermund J , Knapik A , Saulicz E , Myśliwiec A , Saulicz M , Rygiel KA , Linek P . Back and neck pain among school teachers in Poland and its correlations with physical activity. Med Pr. (2015) ;66: (6):771–8. |
[7] | Vaghela NP , Parekh SK . Prevalence of the musculoskeletal disorder among school teachers. National Journal of Physiology, Pharmacy and Pharmacology. (2018) ;8: (2):197–201. |
[8] | Damayanti S , Zorem M , Pankaj B . Occurrence of Work Related Musculoskeletal Disorders among School Teachers in Eastern and Northeastern Part of India. International Journal of Musculoskeletal Pain Prevention. (2017) ;2: (1):187–92. |
[9] | Ceballos AG , Santos GB . Fatoresassociados à dormusculoesqueléticaemprofessores: aspectossociodemográficos, saúdegeral e bem-estar no trabalho. RevistaBrasileira de Epidemiologia. (2015) ;18: :702–15. |
[10] | Ng YM , Voo P , Maakip I . Psychosocial factors, depression, and musculoskeletal disorders among teachers. BMC Public Health. (2019) ;19: (1):1–0. |
[11] | Solis-Soto MT , Schön A , Parra M , Radon K . Associations between effort-reward imbalance and health indicators among school teachers in Chuquisaca, Bolivia: a cross-sectional study. BMJ Open. (2019) ;9: (3):e025121. |
[12] | King CD , Mano KE , Barnett KA , Pfeiffer M , Ting TV , Kashikar-Zuck S . Pressure pain threshold and anxiety in adolescent females with and without juvenile fibromyalgia: a pilot study. The Clinical Journal of Pain. (2017) ;33: (7):620. |
[13] | Hirsh AT , Waxenberg LB , Atchison JW , Gremillion HA , Robinson ME . Evidence for Sex Differences in the Relationships of Pain, Mood, and Disability. J Pain. (2006) ;7: (8):592–601. |
[14] | Wijnhoven HAH , de Vet HCW , Picavet HSJ . Explaining sex differences in chronic musculoskeletal pain in a general population. Pain. (2006) ;124: (1–2):158–66. |
[15] | De Souza JM , de A Pinto RZ , Tebar WR , Gil F , Delfino LD , Morelhão PK , Da Silva C , Oliveira C , Christofaro DG . Association of musculoskeletal pain with poor sleep quality in public school teachers. Work, (2020) . (Preprint), pp. 1–8. |
[16] | Darwish MA , Al-Zuhair SZ . Musculoskeletal pain disorders among secondary school Saudi female teachers. Pain Research and Treatment. (2013) ;2013. |
[17] | Erick PN , Smith DR . Low back pain among school teachers in Botswana, prevalence and risk factors. BMC Musculoskeletal Disorders. (2014) ;15: (1):1–13. |
[18] | Herr RM , Bosch JA , Loerbroks A , van Vianen AE , Jarczok MN , Fischer JE , Schmidt B . Three job stress models and their relationship with musculoskeletal pain in blue-and white-collar workers. Journal of Psychosomatic Research. (2015) ;79: (5):340–7. |
[19] | Haghshenas B , Habibi E , Haji Esmaeil Hajar F , GhanbarySartang A , van Wijk L , Khakkar S . The association between musculoskeletal disorders with mental workload and occupational fatigue in the office staff of a communication service company in Tehran, Iran, in 2017. Journal of Occupational Health and Epidemiology. (2018) ;7: (1):20–9. |
[20] | Zamri EN , Moy FM , Hoe VC . Association of psychological distress and work psychosocial factors with self-reported musculoskeletal pain among secondary school teachers in Malaysia. PloS One. (2017) ;12: (2):e0172195. |
[21] | Lerman SF , Rudich Z , Brill S , Shalev H , Shahar G . Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosomatic Medicine. (2015) ;77: (3):333–41. |
[22] | Feingold D , Brill S , Goor-Aryeh I , Delayahu Y , Lev-Ran S . Depression and anxiety among chronic pain patients receiving prescription opioids and medical marijuana. Journal of Affective Disorders. (2017) ;218: :1–7. |
[23] | Georgas J , Giakoumaki E . Psychosocial stress, symptoms, and anxiety of male and female teachers in Greece. Journal of Human Stress. (1984) ;10: (4):191–7. |
[24] | Zamri EN , Moy FM , Hoe VC . Association of psychological distress and work psychosocial factors with self-reported musculoskeletal pain among secondary school teachers in Malaysia. PloS One. (2017) ;12: (2):e0172195. |
[25] | Vaghela NP , Parekh SK . Prevalence of the musculoskeletal disorder among school teachers. National Journal of Physiology, Pharmacy and Pharmacology. (2018) ;8: (2):197–201. |
[26] | Luque-Suarez A , Martinez-Calderon J , Falla D . Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. British Journal of Sports Medicine. (2019) ;53: (9):554–9. |
[27] | Herzog H , Lele VR , Kuwert T , Langen KJ , Kops ER , Feinendegen LE . Changed pattern of regional glucose metabolism during yoga meditative relaxation. Neuropsychobiology. (1990) ;23: (4):182–7. |
[28] | Nidhi R , Padmalatha V , Nagarathna R , Amritanshu R . Effects of a holistic yoga program on endocrine parameters in adolescents with polycystic ovarian syndrome: a randomized controlled trial. The Journal of Alternative and Complementary Medicine. (2013) ;19: (2):153–60. |
[29] | Holtzman S , Beggs RT . Yoga for chronic low back pa:n a meta-analysis of randomized controlled trials. Pain Research and Management. (2013) ;18: (5):267–72. |
[30] | Deepika S , Hemant B . Effect of mind sound resonance technique as an add on to yoga therapy on quality of sleep, pain, stress and state anxiety levels in patients suffering from chronic musculoskeletal pain: matched controlled trial. International Journal of Review in Life Sciences. (2016) ;6: (1):5–11. |
[31] | Puerto Valencia LM , Weber A , Spegel H , Bögle R , Selmani A , Heinze S , Herr C . Yoga in the workplace and health outcomes: a systematic review. Occupational Medicine. (2019) ;69: (3):195–203. |
[32] | Della Valle E , Palermi S , Aloe I , Marcantonio R , Spera R , Montagnani S , Sirico F . Effectiveness of Workplace Yoga Interventions to Reduce Perceived Stress in Employees: A Systematic Review and Meta-Analysis. Journal of Functional Morphology and Kinesiology. (2020) ;5: (2):33. |
[33] | Chirico F , Sharma M , Zaffina S , Magnavita N . Spirituality and Prayer on Teacher Stress and Burnout in an Italian Cohort: A Pilot, Before-After Controlled Study. Front Psychol. (2020) ;10: :2933. Published 2020 Jan 21. |
[34] | Chirico F . Religious Belief and Mental Health in Lay and Consecrated Italian Teachers. J Relig Health. (2017) ;56: (3):839–51.10.1007/s10943-016-0242-7. |
[35] | Anagnostis C , Gatchel RJ , Mayer TG . The pain disability questionnaire: a new psychometrically sound measure for chronic musculoskeletal disorders. Spine. (2004) ;29: (20):2290–302. |
[36] | Gatchel RJ , Mayer TG , Theodore BR . The pain disability questionnaire: relationship to one-year functional and psychosocial rehabilitation outcomes. Journal of Occupational Rehabilitation. (2006) ;16: (1):72–91. |
[37] | Salaffi F , Stancati A , Silvestri CA , Ciapetti A , Grassi W . Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. European Journal of Pain. (2004) ;8: (4):283–91. |
[38] | Good M , Stiller C , Zauszniewski JA , Anderson GC , StantonHicks M , Grass JA . Sensation and distress of pain scales: reliability, validity, and sensitivity. J Nurs Meas. (2001) ;9: :219–38. |
[39] | Backhaus J , Junghanns K , Broocks A , Riemann D , Hohagen F . Test– retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research. (2002) ;53: (3):737–40. |
[40] | Norton PJ . Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, stress, and Coping. (2007) ;20: (3):253–65. |
[41] | Sahebi A , Asghari A , Salari RS . [Validation of depression anxiety and stress scale for an Iranian population] Journal of Iranian psychologists. (2005) ;1: :299–312. (Persian). |
[42] | Cruz LN , Camey SA , Fleck MP , Polanczyk CA . World Health Organization quality of life instrument-brief and Short Form-36 in patients with coronary artery disease: do they measure the similar quality of life concepts? Psychology, Health & Medicine. (2009) ;14: (5):619–28. |
[43] | Riley KE , Park CL . How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychology Review. (2015) ;9: (3):379–96. |
[44] | Tekur P , Singphow C , Nagendra HR , Raghuram N . Effect of a short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med [Internet]. 2008 Jul 1 [cited 2020 Sep 24]; 14: (6):637–44. |
[45] | Neyaz O , Sumila L , Nanda S , Wadhwa S . Effectiveness of Hatha Yoga Versus Conventional Therapeutic Exercises for Chronic Nonspecific Low-Back Pain. J Altern Complement Med [Internet]. 2019 Sep 1 [cited 2020 Sep 24]; 25: (9):938–45. |
[46] | Herman PM , Yuan AH , Cefalu MS , Chu K , Zeng Q , Marshall N , et al. The use of complementary and integrative health approaches for chronic musculoskeletal pain in younger US Veterans: An economic evaluation. Wilson FA, editor. PLoS One [Internet]. 2019 Jun 5 [cited 2020 Sep 22]; 14: (6):e0217831. |
[47] | Nambi G , Shanmugananth , Devi S , Inbasekaran D , Jagannathan K , Khuman R . Changes in pain intensity and health-related quality of life with Iyengar yoga in nonspecific chronic low back pain: A randomized controlled study Int J Yoga [Internet]. 2014 [cited 2020 Sep 24]; 7: (1):48. |
[48] | Biman S , Maharana S , Metri KG , Nagartna R . Effects of yoga on stress, fatigue, musculoskeletal pain, and the quality of life among employees of diamond industry: A new approach in employee wellness. Work, 1–16. |
[49] | Sherman KJ , Cherkin DC , Erro J , Miglioretti DL , Deyo RA . Comparing Yoga, Exercise, and a Self-Care Book for Chronic Low Back Pain. Ann Intern Med [Internet]. 2005 Dec 20 [cited 2020 Sep 24]; 143: (12):849. |
[50] | Cramer H , Lauche R , Hohmann C , Lüdtke R , Haller H , Michalsen A , et al. Randomized-controlled Trial Comparing Yoga and Home-based Exercise for Chronic Neck Pain. Clin J Pain [Internet]. 2013 Mar [cited 2020 Sep 24]; 29: (3):216–23. |
[51] | Shohani M , Badfar G , Nasirkandy MP , Kaikhavani S , Rahmati S , Modmeli Y , Soleymani A , Azami M . The effect of yoga on stress, anxiety, and depression in women. International Journal of Preventive Medicine. (2018) ;9. |
[52] | Patil N , Nagaratna R , Tekur P , Manohar P , Bhargav H , Patil D . A randomized trial comparing the effect of yoga and exercises on quality of life in among nursing population with chronic low back pain. Int J Yoga [Internet]. 2018 [cited 2020 Sep 24]; 11: (3):208. |
[53] | Wieland LS , Skoetz N , Pilkington K , Vempati R , D’Adamo CR , Berman BM . Yoga treatment for chronic non-specific low back pain. Cochrane Database of Systematic Reviews. (2017) (1). |
[54] | Mustian KM , Sprod LK , Janelsins M , Peppone LJ , Palesh OG , Chandwani K , et al. Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors. J Clin Oncol [Internet]. 2013 Sep 10 [cited 2020 Sep 25]; 31: (26):3233–41. |
[55] | Chirico F , Magnavita N . The Spiritual Dimension of Health for More Spirituality at Workplace. Indian J Occup Environ Med. (2019) ;23: (2):99.10.4103/ijoem.IJOEM_209_18. |
[56] | Rao M , Metri KG , Raghuram N , Hongasandra NR . Effects of Mind Sound Resonance Technique (Yogic Relaxation) on Psychological States, Sleep Quality, and Cognitive Functions in Female Teachers: A Randomized, Controlled Trial. Adv Mind Body Med [Internet]. 2017 Jan 1 [cited 2020 Sep 25]; 31: (1):4–9. |
[57] | Chuntharapat S , Petpichetchian W , Hatthakit U . Yoga during pregnancy: Effects on maternal comfort, labor pain and birth outcomes. Complement Ther Clin Pract [Internet]. 2008 [cited 2020 Sep 25]; 14: :105–15. |
[58] | Karimi M , Safapour F . Effect of a period of selected yoga exercises on serum levels of serotonin and dopamine in non-athlete obese women. Journal of Practical Studies of Biosciences in Sport. (2018) ;6: (11):73–83. |
[59] | Tyagi A , Cohen M . Yoga and heart rate variability: A comprehensive review of the literature. International Journal of Yoga. (2016) ;9: (2):97. |




