Ultrasonographic approach for a foot ganglion after sewing masks in the COVID-19 pandemic: Blessing in disguise
Abstract
BACKGROUND:
During the coronavirus disease (COVID-19) pandemic, people volunteered for sewing hand-made face masks. However, sewing-machine operating might be associated with high ergonomic risk and a negative impact on musculoskeletal health.
OBJECTIVE AND METHODS:
This paper describes an ultrasonographic diagnosis of a foot ganglion - after sewing 300 face masks within two months using a foot-operated sewing machine.
RESULTS:
The patient significantly improved after an ultrasound-guided aspiration and corticosteroid injection.
CONCLUSION:
In short, we highlight the importance of ultrasound examination in the management of work (overuse)-related disorders in occupational medicine practice.
1Introduction
In 2020, the coronavirus disease (COVID-19) pandemic significantly impacted the whole world/ society. In order to slow down the spread of the coronavirus, official authorities recommended social distancing, adherence to strict hygiene rules, and personal protective equipment (PPE) (i.e., gloves, face shield, or face mask). Further, face-covering became necessary and mandatory in some situations [1]. Since the pandemic appeared ‘out of the blue‘, PPE was not widely/immediately available in March 2020. As such, people commonly volunteered for sewing hand-made face masks. Herein, we report a case of foot ganglion after sewing plenty of face masks in a short period.
2Case presentation
A 55-year-old woman (otherwise healthy janitor in preschool) presented with a 3-month history of painless mass on her right foot’s dorsum. She also described cramping along her foot’s medial side three times a day, regardless of rest or physical activity. She declared that she had volunteered to tailor approximately 300 hand-made face masks on a foot-controlled sewing machine in the 1st two months of the COVID-19 pandemic lockdown.
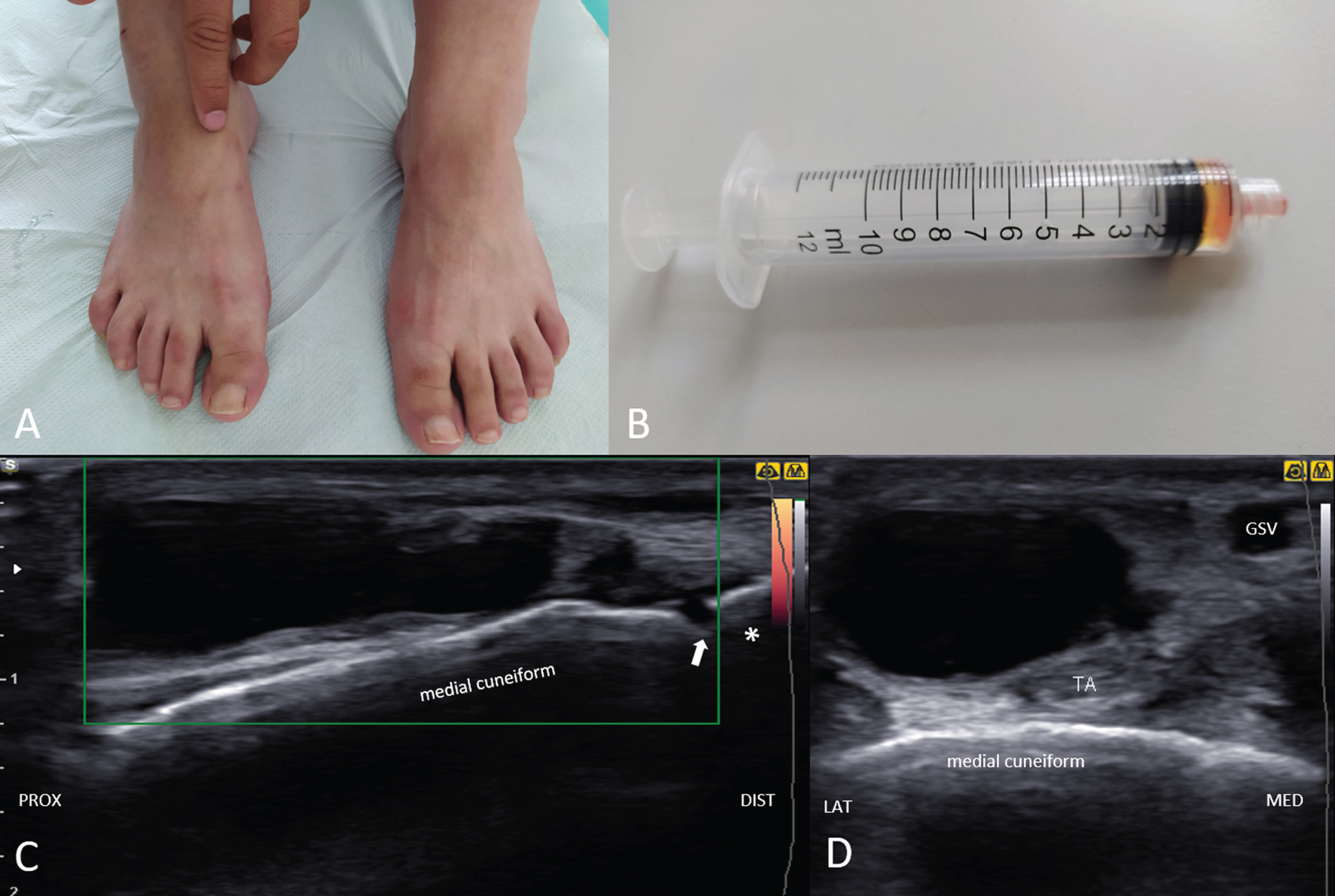
Her current neuromusculoskeletal examination was normal, except for a 1.5 cm palpable mass on the dorsomedial aspect of her right foot (Fig. 1A). Ultrasound (US) examination (Samsung UGEO HM70A, Seoul, South Korea) demonstrated a ganglion cyst originating from the 1st metatarsal-cuneiform joint (Fig. 1C), next to the tibialis anterior tendon (Fig. 1D). Doppler imaging did not reveal any hypervascular signal (Fig. 1C). Under US guidance, 1 mL of viscous, yellowish content was aspirated (Fig. 1B); and intralesional injection of 0.5 mL of methylprednisolone acetate and 0.5 mL of trimecaine hydrochloride was performed. The patient was free of any complaints on the 4th-week follow-up.
Fig. 1
The physician’s finger indicates a mass on the patient’s right foot (dorsomedial aspect) (A). The syringe contains 1 mL of gelatinous and yellowish fluid aspirated from the ganglion (B). Ultrasonography (long-axis view) shows an irregular, septated, and hypoechoic mass in continuity with the 1st metatarsal-cuneiform joint with no hypervascularisation under power Doppler imaging (C). Adjacent tibialis anterior tendon (TA) is seen in the short axis-view (D). Asterisk; 1st metatarsal bone; arrow; 1st metatarsal-cuneiform joint, GSV; greater saphenous vein.
3Discussion
The pertinent literature of musculoskeletal disorders in sewing-machine operators generally encompasses neck, back, and upper limb problems, e.g., awkward posture, overuse injuries, Heberden’s nodules and trigger finger [2–4]. Herewith, many sewing machines are still foot-operated, and the pedal’s repetitive movements might pose ergonomic risk to the feet. For instance, foot dystonia (similar to the writer’s cramp) has been reported after long-term pedaling in a seamstress [5].
Ganglion cysts are benign lesions that usually arise near joints or tendon sheaths [6]. They are believed to occur after repetitive microtrauma to the joint capsule, tendinous and ligamentous structures [7]. A possible explanation is the stimulation of fibroblasts to produce hyaluronic acid, which, together with other mucopolysaccharides, pools as a cyst [8]. These lesions are most commonly found in the wrist and hand [9], less in the ankle and foot (being 11% of all cases) [10]. While conservative approach is usually preferred in their management, recalcitrant cases are treated with aspiration/injection or, less rarely, with excision - mainly in the presence of painful complaints or cosmetic concerns [11].
4Conclusion
In short, presenting this otherwise trivial case of a ganglion, we would like to emphasize the paramount/convenient role of US imaging in the diagnosis and treatment of work-related occupational problems [6, 7]. Owing to its several advantages [12], US imaging/guidance can surely be implemented in the daily clinical practice of physicians dealing with a great spectrum of musculoskeletal disorders.
Conflict of interest
None.
Funding
None.
Informed consent
The patient consented to be presented in this case report.
References
[1] | World Health Organization [homepage on the Internet]. Advice on the use of masks in the context of COVID-19: interim guidance, 6 April 2020. World Health Organization 2020. Available from: https://apps.who.int/iris/handle/10665/331693 |
[2] | Habib MM . Ergonomic risk factor identification for sewing machine operators through supervised occupational therapy fieldwork in Bangladesh: A case study. Work. (2015) ;50: (3):357–62. |
[3] | Poole CJ . Seamstress’s finger. Br J Ind Med. (1993) ;50: (7):668–9. |
[4] | De la Parra-Márquez ML , Tamez-Cavazos R , Zertuche-Cedillo L , Martínez-Pérez JJ , Velasco-Rodríguez V , Cisneros-Pérez V . Factores de riesgo asociados a tenosinovitisestenosante. Estudio de casos y controles [Risk factors associated with trigger finger. Case-control study]. Cir Cir. (2008) ;76: (4):323–7. |
[5] | Lee D , Lee JS , Ahn TB . Moving foot dystonia in a seamstress. Neurol Sci. (2015) ;36: (8):1495–6. doi: 10.1007/s10072-015-2109-1 |
[6] | Casal D , Bilhim T , Pais D , Almeida MA , O’Neill JG . Paresthesia and hypesthesia in the dorsum of the foot as the presenting complaints of a ganglion cyst of the foot. Clin Anat. (2010) ;23: (5):606–10. |
[7] | Kannus P , Józsa L . Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. (1991) ;73: (10):1507–25. |
[8] | Minotti P , Taras JS . Ganglion cysts of the wrist. J Am Soc Surg Hand. (2002) ;2: :102–7. |
[9] | Angelides A , Wallace P . The dorsal ganglia of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am. (1976) ;1: (3):228e235. |
[10] | McEvedy BV . Simple ganglia. Br J Surg. (1962) ;49: :585–94. |
[11] | Head L , Gencarelli JR , Allen M , Boyd KU . Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am. (2015) ;40: (3):546–53.e8. |
[12] | Özçakar L , Kara M , Chang KV , Çarl AB , Akkaya N , Tok F , Chen WS , Wang TG , Tekin L , Ulaşl AM , Chen CPC , Çapkn E , Muynck MD . Nineteen reasons why physiatrists should do musculoskeletal ultrasound: EURO-MUSCULUS/USPRM recommendations. Am J Phys Med Rehabil. (2015) ;94: (6):e45–e49. |




