Does objectively measured prolonged standing for desk work result in lower ratings of perceived low back pain than sitting? A systematic review and meta-analysis
Abstract
BACKGROUND:
Prolonged sitting has been shown to induce transient low back pain (LBP). Height adjustable office desks now present the opportunity to replace sitting with standing in the workplace. Since standing has also been associated with LBP, this may not be an advisable alternative.
OBJECTIVE:
To determine if objectively measured prolonged exposures to desk work while standing, compared to sitting, results in lower perceived LBP in healthy adults.
METHODS:
A systematic search of several databases was conducted. Two independent reviewers screened titles/abstracts and conducted a quality assessment. The results of three studies were pooled using an inverse variance random-effects meta-analysis. Heterogeneity was tested using the Chi-squared test and I2 statistic.
RESULTS:
Objectively measured prolonged standing postures during desk work did not induce significantly less perceived LBP compared to seated postures (standardized mean difference 0.60, 95% CI –0.68 to 1.87, p = 0.36.) There was significant heterogeneity, I2 = 90%).
CONCLUSIONS:
It appears that replacing seated desk work postures with standing for prolonged periods of time would not be recommended. Larger studies, including a wider age range and health history, conducted in the field with objective measures is recommended to obtain more generalizable data on which to base ergonomic standards for work postures.
1Introduction
Globally, low back pain (LBP) is the leading cause of years lost to disability [1]; is responsible for billions of health care dollars annually [2, 3]; and is not easily resolved, with a significant number of cases progressing to chronicity [4, 5]. In vivo basic science research has demonstrated that prolonged sitting can induce transient perceived back pain in young, healthy populations [6–10]. Considering 40% of the workforce in developed countries [11] are seated for more than two thirds of the workday [12–14] solutions for those who develop pain in sitting are important. To this end, the introduction of height adjustable office desks to workplaces has provided an option to replace seated postures with standing. However, prolonged standing has also been shown to be associated with LBP [15] and may not be a helpful alternative.
To date, there has been a number of epidemio-logical studies that have looked at the association of either standing or sitting postures with LBP [16–20]. However, there has been no systematic evaluation of the literature that directly compared seated and standing desk work postures in terms of immediate LBP development. Further, the studies that have examined the association of either sitting or standing postures with back pain have relied on self-report exposure time or have assumed posture duration based on an occupation title. There is evidence from the literature to suggest that these methods of time determination far underestimate actual durations [21]. The objective measure of sitting and standing time, either by direct observation, timed laboratory trial or wearable sensor would provide a more robust dose/response picture of exposure to postures with back pain. Therefore, the purpose of this study is to conduct a systematic review and meta-analysis to determine whether objectively measured prolonged standing results in less perceived low back pain compared to prolonged sitting.
1.1Research question
Does objectively measured (by laboratory controlled time trial, direct observation or wearable sensor) exposures of prolonged (≥one hour) desk work while standing result in lower perceived back pain (upper or lower back determined by pain scale rating) compared to sitting in adults (>18 years of age) with no history of low back pain?
2Methods
2.1Identification of studies
A systematic review of the literature was conducted, with the support of a health services librarian (MS), in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22]. The electronic databases PubMed (MEDLINE), EMBASE, SPORTDiscus and CINAHL were searched on October 20, 2017 and updated on November 14, 2017 and September 2, 2018. No language restrictions were used and all articles published from database inception to the search date were included. Both observational studies (cross-sectional, cohort, case control) and randomized control trials were sought. The search strategy included all possible versions and combinations of the terms “back pain”, “discomfort”, “upper back”, “lower back”, “objective measure”, “sensor”, “laboratory”, “sitting”, “standing”, “motion analysis” and “video” in either the title or abstract. The specific search strategies for each database are included in the appendix. The reference lists of included articles were also screened to locate additional papers missed by the initial search. We considered sitting and standing in any context (i.e. occupational space, laboratory, leisure time etc.) in any country so long as the criteria of “objectively measured time” was met and the outcome of perceived back pain could be directly related to the exposure.
2.2Title and abstract screen
Exact duplicates of article were identified and removed using RefWorks by the health sciences librarian (MS). Two authors (DD and RG) reviewed the titles and abstracts of the remaining articles and compiled a list of papers that appeared to fit the inclusion criteria. If there was any question of acceptability at this point, the full paper was accessed in order to confirm study details. Reasons for exclusion were documented. The reviewers met to discuss their findings. Discrepancies were resolved through discussion and with consultation of a third reviewer (MG) to reach a final decision when necessary.
Two independent reviewers (DD and RG) extracted data for each for the included studies using a standardized form including the following information: study setting, population demographics and baseline characteristics, details of intervention and control conditions, methodology, recruitment rates and study dropout numbers, outcome measures (including units and variance).
2.3Assessment of quality
Following data extraction for each paper, two independent reviewers (DD and RG) completed a quality assessment of all included articles. Specifically, a critical appraisal checklist from the Joanna Briggs Institute was used to assess these quasi-experimental studies [23]. The reviewers met to discuss their findings. Discrepancies were resolved through discussion and with consultation of a third reviewer (MG) to reach a final decision.
2.4Quantitative analysis
Perceived pain data (continuous data) from in-cluded studies were then pooled using an inverse variance random-effects meta-analysis calculating the 95% confidence intervals and two-sided p-values accordingly. Heterogeneity was tested using the Chi-squared test and I2 statistic and we considered 0.25, 0.5 and 0.75 as low, moderate and high levels of heterogeneity respectively for the I2. To visually assess publication bias, a funnel plot was generated. Review Manager 5.3 was used to calculate the analysis and generate the resulting tables and figures an online version of R was used to calculate the Fail-Safe N and Kendall’s tau for the funnel plot.
3Results
The search was performed on October 20, 2017 and re-run on November 14, 2017 and September 2, 2018. Figure 1 presents the PRISMA flowchart for this process. A total of 208 articles were found from all databases and 93 were identified and removed as exact duplicates. One new article was identified through a search of reference lists. Of these 116 articles, four [24–27] were identified as satisfying the inclusion with no exclusions and a full text review was completed to extract data (Table 1) and perform the quality assessment (Table 2). All studies were laboratory-controlled cross-sectional experiments that used each participant as an internal control in order to examine outome variables between three work posture conditions for one or more hours: standing, sitting and either sit/stand protocol or a perching-type sit/stand chair. For the purpose of this analysis, only the sitting and standing conditions were used. All studies had measures of perceived back pain discomfort that could be directly related to the posture exposure. Sample sizes of all studies were small, ranging from 12 to 24 participants and only one, Karakolis et al., balanced the population with respect to gender. While all studies included young, healthy individuals, only Karakolis et al. presented detailed exclusion criteria.
Fig. 1
PRISMA flow diagram for search results and selection of included articles for qualitative and quantitative analysis.
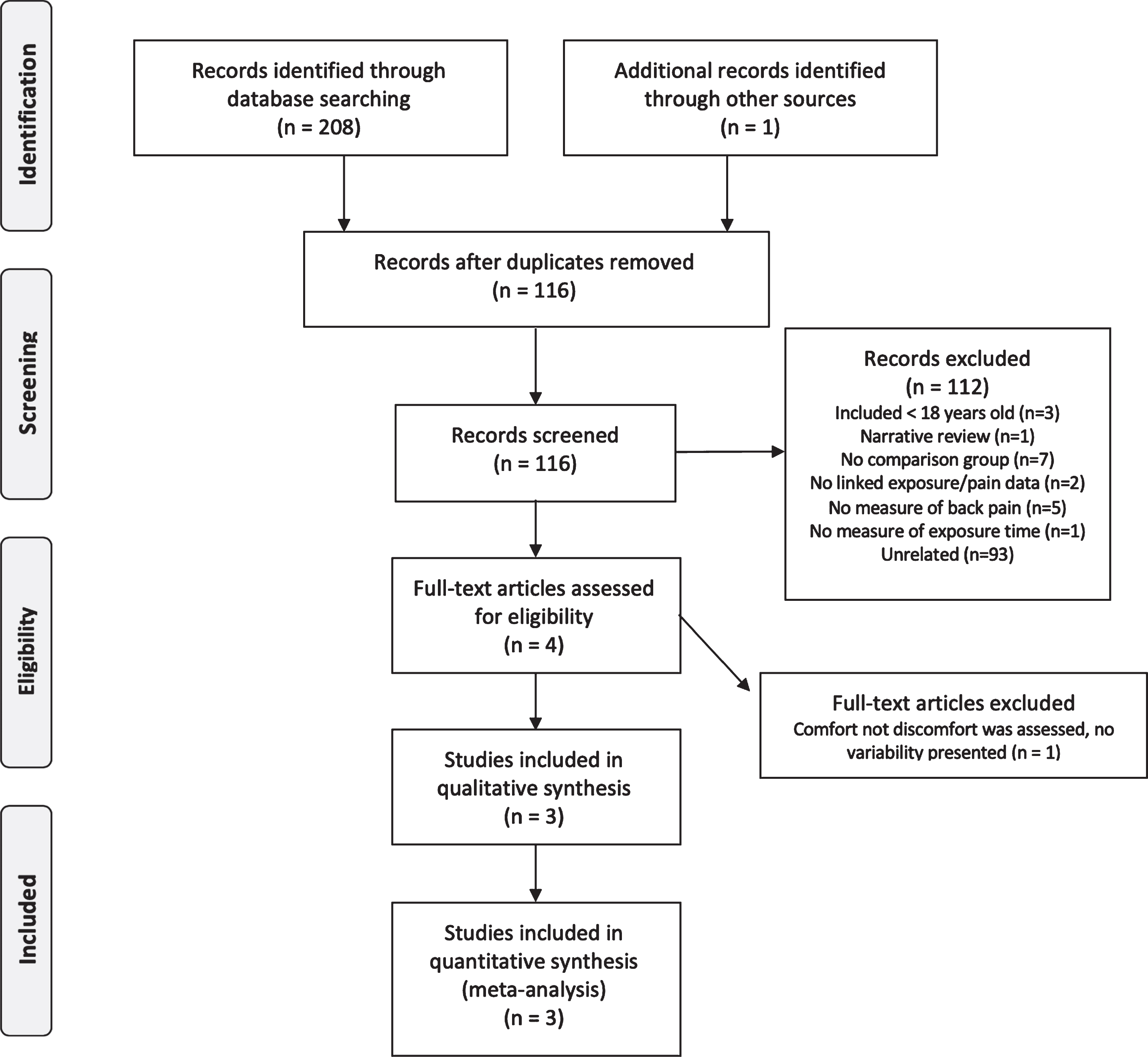
Table 1
Details of each study included for qualitative analysis
| Article | Study type | Population | Intervention | Outcome | Results and conclusions |
| Seo et al. 1996, Japan | Cross-sectional | 12 healthy subjects (8 males | Participants were exposed to 3 | Lower limb swelling | Subjective complaints increased |
| and 4 females), average | laboratory-controlled posture | (bioelectric impedence) | for all conditions. Higher rates | ||
| age 24.1±1.2 years with | exposures in a random order, | and subjective ratings of | of back pain were found for the | ||
| no current edematous | standing sitting (stool type | leg dullness, back pain | buttock chair (5 SD 1) condition | ||
| disease or lower leg injury. | chair with no backrest) | (discrete scale from 1-10) and whole body fatigue. | and was similar for both standing | ||
| and buttock chair sitting while | (3 SD 1) and ordinary chair sitting | ||||
| completing desk work (completing | (3 SD 1). | ||||
| jigsaw puzzles) for 1 hour | |||||
| on three different days. | |||||
| Karakolis et al. 2016, Canada | Cross-sectional | 24 healthy participants (12 male | Participants were exposed to 3, | Spine posture, perceived | All conditions resulted in increasing |
| and 12 female) average age | 1 hour, laboratory-controlled | low back discomfort (rated | levels of discomfort. Overall, there was | ||
| 22.6±1.7 (male) and 23.8±3.0 (female). | posture exposures while | on a 100 mm visual analog | higher discomfort during sitting | ||
| Participants were excluded | completing a standardized | scale with anchors of | (27.66 SD 15.77) compared to standing | ||
| if they had experienced an | desk work task (typing | 0 = no pain and 100 = worst | (25.79, SD 14.70) with the least discomfort | ||
| episode of severe non-specific | and mousing) on three different days | pain), L4–L5 joint loading, | perceived in the sit/stand condition | ||
| low back pain with in the | in three postures in a random order: | work productivity. | (17.15 SD 13.39). A significant interaction | ||
| last 6 months that caused | standing, sitting (office chair | between gender and posture was found | |||
| them to miss at least one day | with backrest removed and | (males more discomfort in standing | |||
| of school or work, had backpain | alternating standing/ | and females more discomfort in sitting). | |||
| at the time of the study, | sitting in a 3:1 ratio. | ||||
| self-identified as developing | |||||
| low back pain from sitting | |||||
| that would lead them to | |||||
| avoid prolonged seated | |||||
| exposures (i.e. a long drive), | |||||
| held a job that involved | |||||
| prolonged standing exposures | |||||
| for more than 10 hours per week | |||||
| or had upper extremity pain that | |||||
| limited their ability to | |||||
| perform typing/mousing tasks. | |||||
| Le and Marras 2016, USA | Cross-sectional | 20 healthy participants | Participants exposed to 3 | Postural transitions, spinal | Standing had the highest reports |
| (10 men and 10 women), | conditions, in a counter-balanced | loads, discomfort for | of discomfort (23 SD 8), | ||
| average age 26.5±8.5 years, | presentation, of sitting (office chair | various body regions | followed by perching | ||
| with no history of previous | with backrest), standing and perching | (measured with a 10 cm | (8 SD 5) and sitting | ||
| or current low back pain | while completing a standardized desk | visual analog scale) and | (9 SD 6). | ||
| in the past 6 months. | work task in a laboratory-controlled | task performance. | |||
| study. All conditions were completed | |||||
| on the same testing day, for 1 hour | |||||
| duration each, with a 20 minute | |||||
| washout period in between | |||||
| (duration of washout | |||||
| based on pilot work). |
Table 2
The checklist for quasi-experimental studies (non-randomized experimental studies) from the Joanna Briggs Institute was used to assess quality for the four articles identified as satisfying the inclusion/exclusion criteria of this study. Final results, following review and consultation by two independent researchers, are presented. Based on these findings one study, Chester et al. 2002, was excluded with justification provided
| Articles | |||||
| Joanna Briggs Institute | Chester et al. 2002 | Seo et al. 1996 | Karakolis et al. 2016 | Le and Marras 2016 | |
| Critical Appraisal Checklist | |||||
| for Quasi-Experimental Studies | |||||
| Leg swelling, comfort and fatigue when sitting, standing and sit/standing | Leg swelling during continuous standing and sitting work without restricting leg movement. | A comparison of trunk biomechanics, musculoskeletal discomfort and productivity during simulated sit-stand office work. | Evaluating the low back biomechanics of three different office workstations: seated, standing, and perching. | ||
| 1 Is it clear in the study what is the “cause” and what is the “effect” (i.e. there is no confusion about what variable comes first)? | yes | yes | yes | yes | |
| 2 Were the participants included in any comparisons similar? | yes | yes | yes | yes | |
| 3 Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest? | yes | yes | yes | yes | |
| 4 Was there a control group? | not applicable | not applicable | not applicable | not applicable | |
| 5 Were there multiple measurements of the outcome both pre and post the intervention/exposure? | yes | yes | yes | yes | |
| 6 Was follow up complete, and if not, were differences between groups in terms of their follow up adequately described and analyzed? | yes | yes | yes | yes | |
| 7 Were the outcomes of participants included in any comparisons measured in the same way? | yes | yes | yes | yes | |
| 8 Were outcomes measured in a reliable way? | yes | yes | yes | yes | |
| 9 Was appropriate statistical analysis used? | yes | yes | yes | yes | |
| Overall appraisal | |||||
| Include | ✓ | ✓ | ✓ | ||
| Exclude | ✓ | ||||
| Seek further info | |||||
| Reasons for exclusion | (1) Perceived comfort | ||||
| is presented, not a direct | |||||
| opposite of discomfort/pain. | |||||
| (2) No standard deviations | |||||
| are given for mean values. | |||||
All included studies were found to have acceptable quality. At this stage Chester et al., 2002, was excluded from the qualitative and quantitative analyses. This decision was made based on the fact that perceived ratings of comfort were used instead of discomfort and the assumption could not be made that inverting comfort values would approximate discomfort. Further, no standard deviations or p-values for the mean results were provided which direcly limits inclusion into the quantitative analysis.
3.1Qualitative synthesis
With the exception of the study by Le and Marras, which found higher rates of perceived pain in the prolonged standing condition, the majority of included studies [25–27] found little difference in pain ratings between postures.
3.2Quantitative synthesis
Data from the three included studies [25–27], in-cluding a total 56 participants, were pooled for the outcome measure of perceived low back pain using standardized mean differences (Fig. 2). Prolonged standing postures during the completion of a standar-dized work task in a laboratory controlled environment did not induce significantly less perceived low back pain compared to seated postures (standardized mean difference 0.60, 95% CI –0.68 to 1.87, p = 0.36). There was significant heterogeneity observed in this analysis. Specifically, I2 was 90% which indicates a large amount of heterogeneity not attributable to random error.
Fig. 2
Top: Forest plot and measures of heterogeneity for perceived ratings of low back discomfort in laboratory-controlled and objectively measured conditions of prolonged standing versus prolonged sitting desk work postures in healthy adults for all three incldued studies. Bottom: Forest plot and measures of heterogeneity for perceived ratings of low back discomfort in laboratory-controlled and objectively measured conditions of prolonged standing versus prolonged sitting desk work postures in healthy adults with data for Le and Marras (2016) removed.
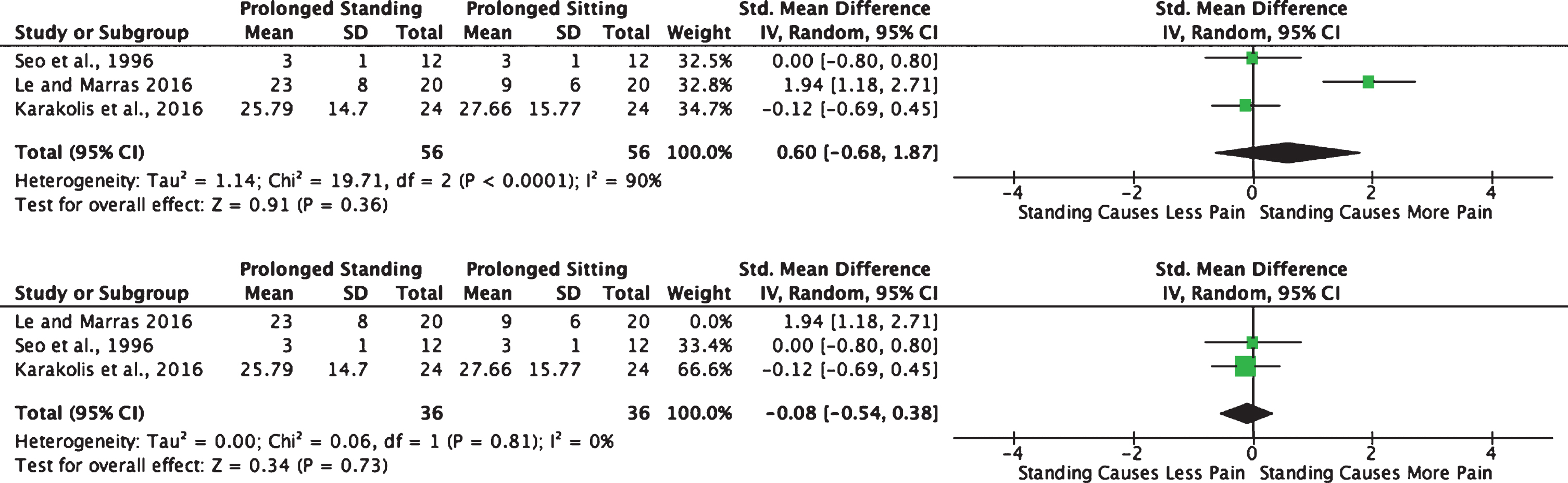
A visual analysis of the Forrest Plot (Fig. 2) highlighted Le and Marras (2016) as potentially driving this heterogeneity, perhaps due to the presence of a backrest in the seated condition compared to no back-rest in the remaining two studies. Considering this, there was a question of whether this methodologi-cal difference impacted the results. Therefore, a secondary analysis was done removing the Le and Marras study. Doing this removed the heterogeneity previously seen (I2 = 0%), however, did not change the overall result. No statistical difference was found between prolonged standing and sitting in terms of the outcome perceived ratings of low back pain (p = 0.73).
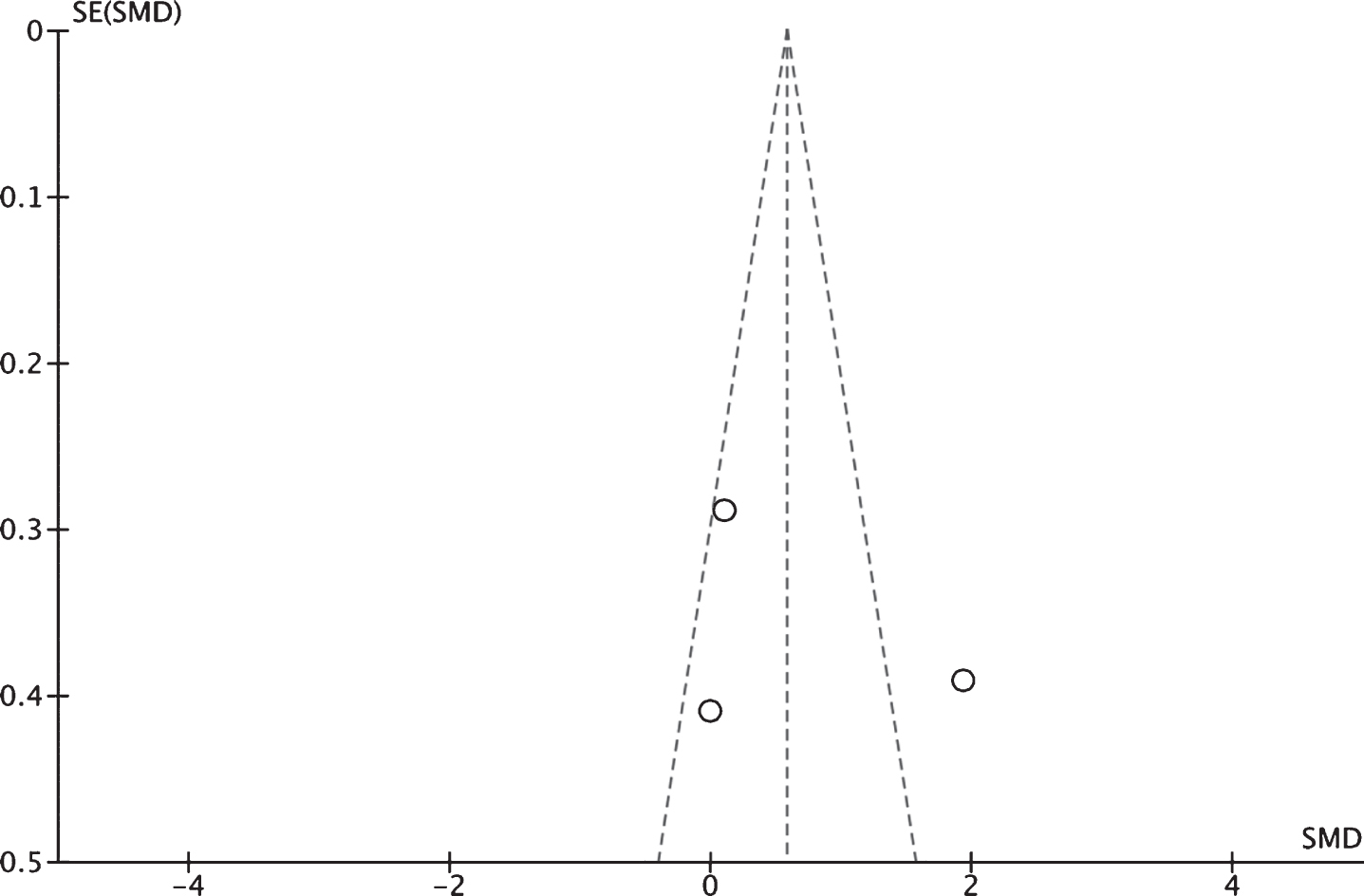
The potential for publication bias was assessed visually to be low using a funnel plot (Fig. 3). The plot is symetrical and covers a fair range of standardized mean differences. Further, a rank correlation test, Kendall’s tau, was found to be low (tau = 0.3333, p = 1.0000). The Fail-Safe N calculation using the Rosenthal Approach found that 8 studies would be needed to change the result from insignificant to significant.
Fig. 3
To visually assess for publication bias, a funnel plot of the three studies included in the quantatitve analysis has been prepared. Since the plot is balanced (Kendell’s Tau = 0.3333, p = 1.0000), it appears that the risk of publication bias in this case is small. The Fail-Safe N was calculated to be 8 using the Rosenthal approach.
4Discussion
The results of this study suggest that prolonged standing for desk work does not translate into lower rates of perceived low back pain compared to sitting. Both postures induce low back pain that appear to be directly linked to the exposure. Furthermore, it appears that the perceived pain induced in all studies is large enough to be clinically meaningful: having a change of more than two points on a discrete scale and more than 2 cm or 20 mm on a 10 cm or 100 mm visual analog scale. Therefore, this suggests that neither posture would be recommended for prolonged periods of deskwork. To be prudent, however, the results of this study should be interpreted with caution, given the cross-sectional study design, small number of included studies, and small sample size of the included studies.
The result that prolonged standing for desk work is no better than sitting in terms of perceived back pain supports opinons that have been expressed in the literature, namely that both standing and sitting, statically sustained for prolonged periods of time can lead to pain [28]. To date, no meta-analyses of perceived low back pain in res-ponse to sitting and/or standing have been conduc-ted. However, previous systematic reviews, have reached conflicting conclusions about the relationship between posture and pain during desk work. A number of reports have concluded there is a relationship between sitting [18, 29, 30] and low back pain as well as standing [15, 31] and low back pain while others have found conflicting results for these postures [16, 17, 19, 32]. The relationship with back pain is indeed complex, with many confounding variables such as health history, previous back injury, psychological, social, economic and occupational factors playing a role. While this work highlights that prolonged standing may not be a suitable replacement for prolonged sitting at work, more studies, using higher level designs, are needed to generate high quality evidence upon which to base occupational standards and recommendations.
The heterogeneity in the main analysis was high (I2 = 90%). While the included studies were very similar in terms of experimental setting, health status, age range and objective measures there were some key differences that could have contributed to this finding. For instance, Karakolis et al. found significant differences in perceived discomfort ratings between men and women: with men perceiving higher rates of back pain in standing and women perceiving higher rates in sitting. Since most articles included in this analysis contained datasets with unbalanced genders and did not present data separately for males and females, there is the possibility that these differences contributed to the observed heterogeneity. However, considering the heterogeneity dropped to 0% with the removal of the Le and Marras study, it is reasonable to conclude that the factor driving the large heterogenity was the presence of a backrest. The sensi-tivity of the results to the presence/absence of a backrest during sitting was tested during the analysis by removing the study by Le and Marras and re-analy-zing the data. While the result was unaffected in this case, it can be argued that this factor needs to be better addressed with more research before drawing a firm conclusion; especially since logically the ability to recline back and unload body stress on a support would result in lower amounts of perceived back pain.
This study was strengthened by using data from studies in which the exposure was objectively measured. This is particularly important as recent evidence suggests that self-recall for posture exposure, beyond TV viewing, is poor [33]. However, this study was limited by a several factors. First, there were a small number of (small) cross-sectional studies that fit the inclusion criteria (total participant sample = 56) and, while a within-control design was used, there were no true control groups in the design of any of these studies. Secondly, the data extracted from two papers (Le and Marras 2016 and Seo et al. 1996) were estimated from graphs, as tabulated data were not provided. Further, since only Karakolis et al. presented data separately by gender, a subgroup analysis could not be performed in this meta-analysis. Future work should take care to study and present data for males and females since Karakolis et al. found a significant interaction for gender and posture and these underlying differences can contribute to heterogeneity and may warrant gender-specific recommendations for guidelines.
5Conclusion
Replacing sitting with standing for deskwork would not be recommended based on the results of this study; indeed both postures appear to be a problem. However, this interpretation must be accepted with caution due to the study type, number and size or the studies included in this analysis. To best answer this question, larger studies, with objective measures conducted preferably in a field setting and including a wider age range and sub-grouped by gender and health history should be performed to generate high quality evidence upon which to base ergonomic guidelines.
Conflict of interest
The authors have no conflicts of interest or funding to declare for this project.
Appendices
Appendix
PubMed (Medline)
(“Back Pain”[Mesh] OR ((discomfort[tw] OR pain*[tw] OR ache*[tw] OR aching[tw]) AND (back OR thoracic[tw] OR thorax[tw] OR lumbar[tw])) OR backache*[tw] OR dorsalgia[tw] OR LBP[tw] OR lumbago[tw] OR “Sciatica” [Mesh] OR sciatica[tw] OR “Radiculopathy” [Mesh] OR radiculopath*[tw]) AND (sitting[tw]) AND (standing[tw]) AND (“Monitoring, Ambulatory” [Mesh] OR “Monitoring, Physiologic” [Mesh] OR “Video Recording” [Mesh] OR “Task Performance and Analysis” [Mesh] OR “Accelerometry” [Mesh] OR “Actigraphy” [Mesh] OR acceleromet*[tw] OR actigraph*[tw] OR gy-roscop*[tw] OR sensor[tw] OR sensors[tw] OR device*[tw] OR wearable[tw] OR inertial[tw] OR “motion capture” [tw] OR “motion analysis” [tw] OR lab[tw] OR laborator*[tw] OR video[tw] OR videorecord*[tw] OR videotap*[tw] OR “objectively measured” [tw])
Embase
(‘backache’/exp OR ((discomfort:ab,ti OR pain*:ab,ti OR ache*:ab,ti OR aching:ab,ti) AND (back:ab,ti OR thoracic:ab,ti OR thorax:ab,ti OR lumbar:ab,ti)) OR backache*:ab,ti OR dorsalgia:ab,ti OR lbp:ab,ti OR lumbago:ab,ti OR ‘sciatica’/de OR sci-atica:ab,ti OR ‘radiculopathy’/exp OR radiculopath*:ab,ti) AND sitting:ab,ti AND standing:ab,ti AND (‘ambulatory monitoring’/de OR ‘physiologic monitoring’/exp OR ‘videorecording’/de OR ‘task perfor-mance’/de OR ‘accelerometry’/de OR ‘actimetry’/de OR acceleromet*:ab,ti OR actigraph*:ab,ti OR gyroscop*:ab,ti OR sensor:ab,ti OR sensors:ab,ti OR de-vice*:ab,ti OR wearable:ab,ti OR inertial:ab,ti OR ‘motion capture’:ab,ti OR ‘motion analysis’:ab,ti OR lab:ab,ti OR laborator*:ab,ti OR video*:ab,ti OR ‘ob-jectively measured’:ab,ti)
Cinahl
(MH “Back Pain” OR ((TI discomfort OR TI pain* OR TI ache* OR TI aching OR AB discomfort OR AB pain* OR AB ache* OR AB aching) AND (TI back OR TI thoracic OR TI thorax OR TI lumbar OR AB back OR AB thoracic OR AB thorax OR AB lumbar)) OR TI backache* OR AB backache* OR TI dorsalgia OR AB dorsalgia OR TI LBP OR AB LBP OR TI lumbago OR AB lumbago OR MH “Sciatica” OR TI sciatica OR AB sciatica OR MH “Radiculopathy” OR TI radiculopath* OR AB radiculopath*) AND (MH “Sitting” OR TI sitting OR AB sitting) AND (MH “Standing” OR TI standing OR AB standing) AND (MH “Monitoring, Physiologic” OR MH “Videorecording” OR MH “Task Performance and Analysis” OR MH “Accelerometry” OR MH “Actigraphy” OR TI acceleromet* OR AB acceleromet* OR TI actigraph* OR AB actigraph* OR TI gyroscop* OR AB gyroscop* OR TI sensor OR AB sensor OR TI sensors OR AB sensors OR TI device* OR AB device* OR TI wearable OR AB wearable OR TI in-ertial OR AB inertial OR TI “motion capture” OR AB “motion capture” OR TI “motion analysis” OR AB “motion analysis” OR TI lab OR AB lab OR TI laborator* OR AB laborator* OR TI video* OR AB video* OR TI “objectively measured” OR AB “objectively measured”)
SPORTDiscus
(DE “BACKACHE” OR DE “LUMBAR pain” OR ((TI discomfort OR TI pain* OR TI ache* OR TI ac-hing OR AB discomfort OR AB pain* OR AB ache* OR AB aching) AND (TI back OR TI thoracic OR TI thorax OR TI lumbar OR AB back OR AB thoracic OR AB thorax OR AB lumbar)) OR TI backache* OR AB backache* OR TI dorsalgia OR AB dorsalgia OR TI LBP OR AB LBP OR TI lumbago OR AB lumbago OR DE “SCIATICA” OR TI sciatica OR AB sciatica OR DE “RADICULOPATHY” OR TI radiculopath* OR AB radiculopath*) AND(DE “SITTING position” OR TI sitting OR AB sitting) AND (DE “STANDING position” OR TI standing OR AB stan-ding) AND (DE “PATIENT monitoring” OR DE “ACCELEROMETERS” OR DE “SPEEDOMETERS” OR TI acceleromet* OR AB acceleromet* OR TI ac-tigraph* OR AB actigraph* OR TI gyroscop* OR AB gyroscop* OR TI sensor OR AB sensor OR TI sensors OR AB sensors OR TI device* OR AB device* OR TI wearable OR AB wearable OR TI inertial OR AB inertial OR TI “motion capture” OR AB “motion capture” OR TI “motion analysis” OR AB “motion analysis” OR TI lab OR AB lab OR TI laborator* OR AB laborator* OR TI video* OR AB video* OR TI “objectively measured” OR AB “objectively measured”)
References
[1] | GBD 2013 DALYs and HALE Collaborators, Murray CJ , Barber RM , Foreman KJ , Abbasoglu Ozgoren A , Abd-Allah F , et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. (2015) ;386: (10009):2145–91. |
[2] | Dagenais S , Caro J , Haldeman S . A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. (2008) ;8: (1):8–20. |
[3] | Luo X , Pietrobon R , Sun SX , Liu GG , Hey L . Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa1976). (2004) ;29: (1):79–86. |
[4] | Pengel LH , Herbert RD , Maher CG , Refshauge KM . Acute low back pain: systematic review of its prognosis. BMJ. (2003) ;327: (7410):323. |
[5] | Von Korff M , Saunders K . The course of back pain in primary care. Spine (Phila Pa1976). (1996) ;21: (24):2833–7; discussion 2838-9. |
[6] | Fenety A , Putnam C , Walker JM . In-chair movement: val-idity, reliability and implications for measuring sitting discomfort. ApplErgon. (2000) ;31: (4):383–93. |
[7] | Beach TA , Parkinson RJ , Stothart JP , Callaghan JP . Effects of prolonged sitting on the passive flexion stiffness of the in vivo lumbar spine. Spine J. (2005) ;5: (2):145–54. |
[8] | De Carvalho DE , Callaghan JP . Passive stiffness changes in the lumbar spine and effect of gender during prolonged simulated driving. IntJIndErgonomics. (2011) ;41: (6):617–24. |
[9] | Dunk NM , Callaghan JP . Gender-based differences in postural responses to seated exposures. ClinBiomech(Bristol, Avon). (2005) ;20: (10):1101–10. |
[10] | Gregory DE , Dunk NM , Callaghan JP . Stability ball versus office chair: comparison of muscle activation and lumbar spine posture during prolonged sitting. HumFactors. (2006) ;48: (1):142–53. |
[11] | van der Ploeg HP , Moller SV , Hannerz H , van der Beek AJ , Holtermann A . Temporal changes in occupational sit-ting time in the Danish workforce and associations with all-cause mortality: results from the Danish work environment cohort study. IntJBehavNutrPhysAct. (2015) ;12: (Journal Article):71-015-0233-1. |
[12] | Clemes SA , O’Connell SE , Edwardson CL . Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. JOccupEnvironMed. (2014) ;56: (3):298–303. |
[13] | Jans MP , Proper KI , Hildebrandt VH . Sedentary behavior in Dutch workers: differences between occupations and business sectors. AmJPrevMed. (2007) ;33: (6):450–4. |
[14] | Kazi A , Duncan M , Clemes S , Haslam C . A survey of sitting time among UK employees. OccupMed(Lond). (2014) ;64: (7):497–502. |
[15] | Nelson-Wong E , Callaghan JP . Transient low back pain development during standing predicts future clinical low back pain in previously asymptomatic individuals. Spine (Phila Pa1976). (2014) ;39: (6):E379–83. |
[16] | Hartvigsen J , Leboeuf-Yde C , Lings S , Corder EH . Is sitting-while-at-work associated with low back pain? A systematic, critical literature review. ScandJPublic Health. (2000) ;28: (3):230–9. |
[17] | Chen SM , Liu MF , Cook J , Bass S , Lo SK . Sedentary lifestyle as a risk factor for low back pain: a systematic review. IntArchOccupEnvironHealth. (2009) ;82: (7):797–806. |
[18] | Frymoyer JW , Pope MH , Costanza MC , Rosen JC , Goggin JE , Wilder DG . Epidemiologic studies of low-back pain. Spine. (1980) ;5: (5):419–23. |
[19] | Roffey DM , Wai EK , Bishop P , Kwon BK , Dagenais S . Causal assessment of occupational sitting and low back pain: results of a systematic review. Spine J. (2010) ;10: (3):252–61. |
[20] | Magora A . Investigation of the relation between low back pain and occupation. 3. Physical requirements: sitting, standing and weight lifting. IMS IndMedSurg. (1972) ;41: (12):5–9. |
[21] | Foley B , Engelen L , Gale J , Bauman A , Mackey M . Sedentary Behavior and Musculoskeletal Discomfort Are Reduced When Office Workers Trial an Activity-Based Work Environment. JOccupEnvironMed. (2016) ;58: (9):924–31. |
[22] | Moher D , Liberati A , Tetzlaff J , Altman DG , PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. IntJSurg. (2010) ;8: (5):336–41. |
[23] | Aromataris E , Munn Z . Joanna Brigs Institute Reviewer’s Manual [Internet]. 2017. (Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L, editors. Systematic Reviews of effectiveness.).Available from: https://joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Quasi-Experimental_Appraisal_Tool2017.pdf |
[24] | Chester MR , Rys MJ , Konz SA . Leg swelling, comfort and fatigue when sitting, standing, and sit/standing. IntJIndErgon. (2002) ;29: (5):289–96. |
[25] | Karakolis T , Barrett J , Callaghan JP . A comparison of trunk biomechanics, musculoskeletal discomfort and productivity during simulated sit-stand office work. Ergonomics. (2016) ;59: (10):1275–87. |
[26] | Le P , Marras WS . Evaluating the low back biomechanics of three different office workstations: Seated, standing, and perching. Appl Ergon. (2016) ;56: :170–8. |
[27] | Seo A , Kakehashi M , Tsuru S , Yoshinaga F . Leg Swelling during Continuous Standing and Sitting Work without Restricting Leg Movement. Journal of Occupational Health. (1996) ;38: (4):186–9. |
[28] | Callaghan J , De Carvalho D , Gallagher K , Karakolis T , Nelson-Wong E . Is Standing the Solution to Sedentary Office Work? Ergonomics in Design. (2015) ;23: (3):20–4. |
[29] | Damkot DK , Pope MH , Lord J , Frymoyer JW . The relationship between work history, work environment and low-back pain in men. Spine. (1984) ;9: (4):395–9. |
[30] | Wilder DG , Pope MH . Epidemiological and aetiological aspects of low back pain in vibration environments - an update. ClinBiomech(Bristol, Avon). (1996) ;11: (2):61–73. |
[31] | Coenen P , Parry S , Willenberg L , Shi JW , Romero L , Blackwood DM , et al. Associations of prolonged standing with musculoskeletal symptoms-A systematic review of laboratory studies. Gait Posture. (2017) ;58: (Journal Article):310–8. |
[32] | Roffey DM , Wai EK , Bishop P , Kwon BK , Dagenais S . Causal assessment of occupational standing or walking and low back pain: results of a systematic review. Spine J. (2010) ;10: (3):262–72. |
[33] | Clark BK , Thorp AA , Winkler EA , Gardiner PA , Healy GN , Owen N , et al. Validity of self-reported measures of workplace sitting time and breaks in sitting time. MedSciSports Exerc. (2011) ;43: (10):1907–12. |




