Health coaching for healthcare employees with chronic disease: A pilot study
Abstract
BACKGROUND:
Health coaching promotes healthy lifestyles and may be particularly helpful for employees with chronic disease.
OBJECTIVE:
Evaluate the effects of a health coaching program that targeted health-system employees with at least one cardiovascular disease (CVD) risk factor.
METHODS:
Fifty-four employees volunteered for a health coaching program (6-session, 12-week program, at least one cycle). 40 (74%) completed (mean age [SD] = 53.3 [10.3] years, Female = 95%, Caucasian = 83%). A certified and integrative health coach/nutritionist provided coaching. Self-reported outcomes were collected using a pre-post design.
RESULTS:
Participants reported high rates of obesity (75%), hypertension (52.5%), diabetes/prediabetes (47.5%), and hyperlipidemia (40%). In addition, 20% reported chronic pain/rehabilitation needs, 17.5% seasonal depression, and 30% other significant co-morbidities. Following coaching, participants reported significant weight loss (mean [SD] 7.2 [6.6] pounds, p < 0.0001, d = 1.11), increased exercise (from 0.8 to 2.3 sessions/week, p < 0.001, d = .89), reduced perceived stress (p < 0.04, d = .42), and a trend for improved sleep (p = 0.06, d = .38). Reduced stress correlated with both increased exercise (r = –.39, p < 0.05) and decreased fatigue (r = .36, p = 0.07).
CONCLUSION:
Health coaching for healthcare employees with obesity and other CVD risk factors is a promising approach to losing weight, reducing stress, making healthy lifestyle changes, and improving health and well-being.
1Introduction
Health coaching promotes healthy nutrition, movement, exercise and fitness, and effective stress management. These approaches may optimize health and well-being in the workplace [1]. During this process health coaches partner with clients to identify and support sustainable change in behaviors to achieve self-identified health goals. This can also be beneficial for productivity, absenteeism/presenteeism and susceptibility to injury or lost time due to short-term disability [2]. Health coaching may be particularly helpful for employees with chronic and/or complex health profiles because it can support disease management, and it can help break the common cycle of chronic disease and high stress that many employees experience.
One important area in which health coaching has potential for improving health outcomes is with employees with cardiovascular disease (CVD) and related co-morbidities, since CVD is the leading cause of death in the U.S. and a leading cause of disability [3, 4]. Work related factors that may increase CVD risk include low decision latitude, stress, noise, night work and others [4].
While there has been some research on health coaching for chronic and/or complex disease, there have been many challenges including the range of different health coaching approaches that may be used, the variety of patient populations investigated, and the different study designs and outcome measures used. One study of telephonic health coaching found significantly improved quality of life (QOL) and two-year mortality in employees with Type 2 Diabetes Mellitus, hypertension and/or asthma [5]. A review article also found that health coaching improves the management of chronic diseases because it specifically improves weight management, physical activity, and physical and mental health status [6].
Another challenge is presented by health coaching studies and research designs that may produce inconsistent results. For example, one telemedicine program, utilizing registered dietitian nutritionists and registered nurses to deliver health coaching, found significant improvement in some CVD risk factors (cholesterol reduction and smoking cessation) but not all CVD risks over a 6 month interval [7]. A second health coaching study of the COACH program (Coaching patients On Achieving Cardiovascular Health), using telephonic coaching provided by trained registered nurses, found significant improvement for most CVD risk factors (lipids, blood pressure, blood sugar, weight and exercise) in 1,962 patients with CVD and 707 patients with Type 2 Diabetes [8]. Since these prior studies on telephonic health coaching have shown potential for reducing cardiovascular risk factors, additional studies on at-risk employees are needed to explore potential influences that contribute to inconsistent results and to inform health coaching best practices in worksettings.
A final potentially important impact that health coaching may have in the workplace is that it may help to reduce healthcare costs, since 70–80% of these costs are accounted for by approximately 20% of the population with chronic and comorbid diseases [9, 10]. It has also been estimated that employees with CVD risk factors more than double their per person, per year healthcare expenditures [11]. Health coaching may be helpful for employees with chronic disease(s) such as CVD because it focuses on behavioral change, is employee or client centered, and provides individualized support and education, all of which may increase exercise and weight loss, and improve physical and emotional wellbeing [6].
This pilot project investigates two primary aims: (1) describe the health status and challenges of employees with chronic and/or complex health concerns willing to engage in health coaching; and (2) assess how effectively a health coaching program can improve lifestyle, physical and emotional well-being, and health outcomes in these employees. We present pilot data from a health coaching program that targeted employees who had at least one CVD risk factor.
2Methods
2.1Participants and enrollment
Participants enrolled in a health coaching corporate wellness program in which lifestyle and health data was collected to help monitor participant progress with the program and to provide general feedback for the healthcare system. We assessed health coaching outcomes in 54 healthcare system employees who volunteered for this pilot program from October 2015 - May 2016. Data were collected through the end of July, 2016. Inclusion criteria were to recruit participants who reported at least one CVD risk factor and agreed to participate in at least 6 health coaching sessions over 12 weeks (one cycle of health coaching) Exclusion criteria were those without known CVD risk factors. Participants represented a range of health system roles including clinical, administrative and other functions.
Recruitment of healthcare system employees included an e-mail invitation to inform them that the health coaching program was available free of charge. Two additional email reminders were sent and employees were not otherwise incentivized or compensated. Flyers were posted in various locations in the main hospital including the cafeteria and in satellite office locations. The coaching sessions, both in person and telephonic, were conducted from a private office in the main hospital.
2.2Variables and measures
The intervention was the health coaching program which supports health-promoting dietary practices, exercise and fitness, stress management techniques, as well as other influences such as accessing resources, overall support and effective organization. The dependent variables specifically assessed included lifestyle (exercise levels), physical and emotional well-being (physical – self-reported symptoms of fatigue, gastrointestinal (GI) symptoms and headaches or migraines; and emotional – perceived stress). In addition, self-reported health outcomes included measures of weight, sleep quality, fatigue and pain, as well as anecdotal changes in blood glucose and/or blood pressure levels and/or medications for diabetes and/or hypertension.
During the initial intake and coaching session, participants self-reported health status information (weight, medical diagnoses, medications taken, and any symptoms such as GI symptoms, fatigue, or headaches). Participants also completed a brief lifestyle survey that included: (a) the 4-item Perceived Stress Scale [12–15] a commonly used 4 question tool that asks the degree to which life over the last month has been perceived as unstable, uncontrollable or overwhelming; (b) Numerical Rating Scales (NRSs) for fatigue, sleep quality and pain [15–18]. Participants were asked to reflect on the last 4 weeks and checked a box between 0 (no pain, no fatigue, or not at all rested) and 10 (meaning highest degree of pain, fatigue and feeling refreshed); and (c) a two question exercise measure with reflection over the last six months: (1) On average, how many times did you exercise aerobically for a minimum of 20 minutes (checking a box for less than once/week, 1-2 times/week, 3-4 times/week or 5 or more times/week for each question); and (2) How often did you perform strengthening exercises for a minimum of 20 minutes (with similar timeframes and responses as in question #1) [15].
These procedures were approved under expedited review guidelines as a chart review study by the Holy Redeemer Health System Institutional Review Board, Meadowbrook, PA.
2.3Health coaching intervention
Health coaches, as defined by the International Consortium for Health and Wellness Coaching (ICHWC), the national certifying body for health coaches as of 2017, “ ... partner with clients seeking self-directed, lasting changes, aligned with their values, which promote health and wellness and, thereby, enhance well-being. In the course of their work, health and wellness coaches display unconditional positive regard for their clients and a belief in their capacity for change, and honoring that each client is an expert on his or her life, while ensuring that all interactions are respectful and non-judgmental.” [19].
The program health coach was the lead author (JSE), a doctorate level and certified clinical nutritionist with 27 years of experience providing nutritional counseling in integrative health and medicine clinical practices. This facilitator is also a certified health coach (NBC-HWC) with 4 years of health coaching experience.
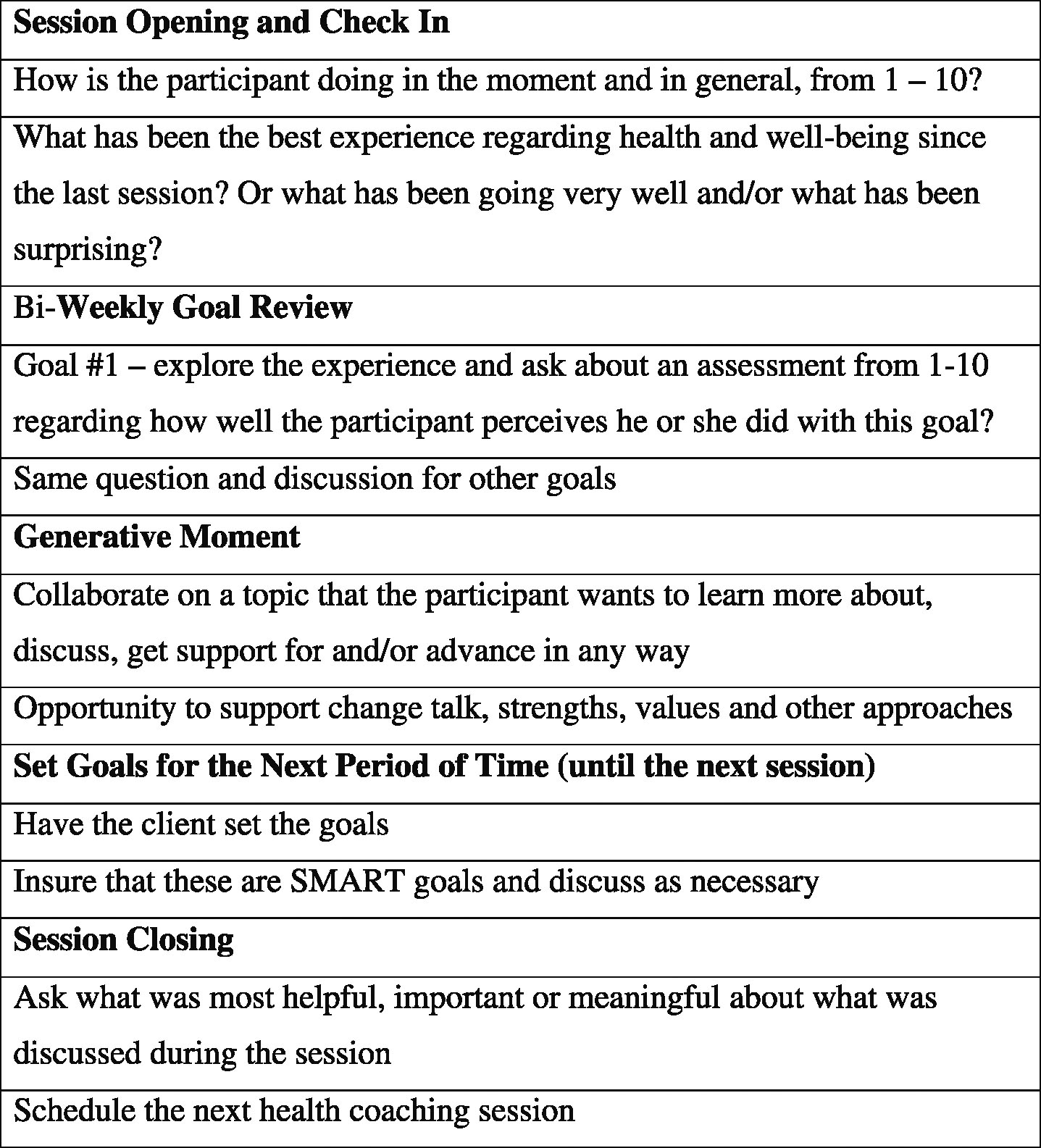
The integrative health coaching intervention focused on supporting nutrition, movement/exercise, stress management, and resources/support using a framework of a health vision (created by the participant), and three-month goals and two-week goals, which were developed by the participant with the coach’s support. This is a standard framework for most health coaching programs. Figure 1 presents an outline for the content of typical follow-up health coaching sessions [20]. In general, follow up sessions included: (a) a “check in” to connect with the client and appreciate how they are doing at the moment; (b) a review of their experience with their stated goals from the previous session; (c) a generative moment to discuss any area or topic that the client would like to talk about or get support for; (d) state goals to work on until the next session; and (e) session closing to reflect on what was most helpful or meaningful from the session and to schedule a time for the next session.
Fig.1
Sample health coaching follow-up session framework (20–30 minutes; adapted from Moore M, Tschannen-Moran B, coaching psychology manual, Lippincott Williams & Wilkins, Philadelphia, 2010).
For participants who reported symptoms such as fatigue, GI symptoms and/or headaches or migraines, the coach asked if the participant desired information about nutrition, exercise and stress management approaches that could be helpful for these specific symptoms. In addition, the coach provided handouts and resources available that were then offered to participants if interested in considering these options.
Other health coaching approaches were discussed and/or implemented on an individual basis such as motivational interviewing, food and exercise logs, health education, targeted use of nutritional supplements, healthcare utilization, organization, resource utilization, and other specific activities or topic discussions. Most health coaching sessions were in person meetings; however, the health system has many satellite offices at a distance from the main hospital, so some participants had some or all sessions conducted by phone. Because building rapport and trusting relationships is essential in health coaching, effort was made to meet in person for at least the first session.
During the initial coaching session participants signed a health coaching agreement to complete the free 6-session, 12-week cycle of coaching with an option to continue. Depending upon the needs and desires of the participant, session intervals at the end of the initial coaching cycle continued every other week but more often it increased to every three or four weeks. Initial coaching sessions were 50–60 minutes and follow-up sessions were 20–30 minutes.
2.4Data collection
The brief data survey was completed by participants at their initial health coaching session and at the sixth session, which defined the first cycle of health coaching and was approximately 3-4 months after initiation of the program. This brief survey included the perceived stress scale, numerical rating scales for fatigue, sleep quality and pain, and the exercise measure for aerobic and strengthening exercises. The brief survey assessment took about five minutes to complete, and was designed as a short but useful indicator of program effectiveness.
Thirty percent (12/40) of participants discontinued involvement in the program at the end of the first cycle of health coaching (6 sessions). Self-reported measures of weight and other program effects such as change in symptoms were collected at this time for these participants. For those participants who continued with the health coaching program, weight and other information was collected when they withdrew from the health coaching program or at the end of July 2016 when data collection for this project ended.
2.5Statistical analyses
SPSS 22.0 was used for statistical analyses, with descriptive summaries presented as means and standard deviations for continuous variables, and as frequencies and percentages for categorical variables. Pre and post intervention scores were compared using paired t-tests.
Cohen’s d for paired samples was used to derive effect sizes [21]. Calculated as the pre-post mean difference divided by the SD of the mean difference, Cohen’s d can be interpreted as d = 0.20 (small), d = 0.50 (medium), and d = 0.80 or higher (large). Pearson’s correlation coefficient (r) was used to test for bivariate correlations between changes in outcome measures including weight, exercise, perceived stress, pain, sleep and fatigue.
3Results
3.1Participant and program characteristics
Seventy-four percent of participants (40/54) completed at least the initial 6-session, 12-week program. For completers, average age was 53.3 years (SD = 10.3; range 27–68 years); 95% were female, and 82.5% were Caucasian, 15% were African American and 2.5% Asian.
For CVD and metabolic syndrome risk factors, 75% of participants (30/40) were obese or morbidly obese (average BMI = 34.7, SD = 8.3) (Table 1), 52.5% (21/40) reported hypertension, 47.5% (19/40) reported diabetes/prediabetes, and 40% (16/40) reported hyperlipidemia. Various co-morbidities were also reported by 30% (12/40) of participants. This included osteoporosis/osteopenia (three), self-reported depression (two), hypothyroidism (two), celiac disease, asthma, psoriasis, narcolepsy, rheumatoid arthritis and a history of cancer. Twenty percent (8/40) reported chronic pain and/or rehabilitation needs, and 17.5% (7/20) reported seasonal depression or winter blues. With respect to ongoing symptoms (and possible disorders), 37.5% of participants (15/40) reported gastrointestinal symptoms (10 heartburn or gastroesophageal refluxdisease symptoms and 5 with irritable bowel syndrome (IBS) symptoms including bloating, flatulence, diarrhea and/or constipation), 37.5% (15/40) reported fatigue, and 20% (8/40) reported headaches or migraines.
Table 1
Baseline health status profile reported by participants (n = 40)
| Diagnoses, health issues and symptoms | Percentage (%) of participants | Number of participants |
| Metabolic syndrome characteristics | ||
| Weight (BMI): Obese or morbid obesity | 75 | 30 |
| Hypertension | 52.5 | 21 |
| Type 2 Diabetes Mellitus or Prediabetes | 47.5 | 19 |
| Hyperlipidemia | 40 | 16 |
| Other diagnoses or health issues | ||
| Chronic pain and/or rehabilitation issues | 20 | 8 |
| Seasonal depression or seasonal blues | 17.5 | 7 |
| Other significant diagnoses* | 30 | 12 |
| Other reported symptoms (ongoing) | ||
| Gastrointestinal symptoms | 37.5 | 15 |
| Fatigue | 35 | 14 |
| Headaches or migraines | 20 | 8 |
*Osteoporosis/osteopenia (3), depression (2), hypothyroidism (2), celiac disease, asthma, narcolepsy, rheumatoid arthritis, history of cancer.
Participants averaged 7.8 health coaching sessions (range 6–12) over 5.5 months (range 3.0–10.0). Fifty seven percent received in-person coaching, 26% in-person and telephonic coaching (telephonic sessions were sometimes included when unexpected work or family circumstances emerged), and 17% had telephonic coaching only.
At baseline, prior to health coaching, few participants exercised regularly (average of 0.8 times per week). Perceived stress fell in the normal range (mean = 5.4, SD = 3.4), and higher PSS scores significantly correlated with poorer sleep quality (r = –.51, p = 0.01, n = 39). The PSS was not correlated with pain or fatigue.
3.2Lifestyle, physical and emotional well-being, health outcome changes and correlations
Significant and positive outcomes were found in each health-related category. For example, the primary lifestyle change was a tripling of exercise from 0.8 times per week [SD = 1.1] to 2.3 times per week (SD = 1.3, p < 0.0001). Regarding changes in physical well-being, self-reported symptom improvements included 12/15 who reported less GI symptoms and 8/8 reported less frequent and/or less severe headaches or migraines. Interestingly, only 15/40 reported fatigue initially, yet 25/40 employees who completed the health coaching program reported improved energy or less fatigue. Emotional well-being had a significant decrease of 22% in perceived stress (pre = 5.4 [3.4], post = 4.2 [2.7], p < 0.04). Finally, the most important change in health outcomes was the significant average weight loss of 7.2 pounds (SD = 6.6, p < 0.0001).
Large effects were found for both self-reported weight loss (d = 1.11) and aerobic and/or weight training exercise (d = .89). Eighty-five percent (34/40) lost weight, with an average weight loss of 8.5 pounds (range 1–27 pounds; p < 0.0001). Four participants also reported improvements in hemoglobin A1c (with 2 taking less medication) and three participants reduced blood pressure medication.
There were small-to-medium-sized effects for reduced perceived stress (d = 0.42) and improved sleep quality (d = 0.38). No significant changes were found for fatigue (d = 0.28) or pain (d = 0.04). Correlational analyses revealed that decreased perceived stress correlated with increased exercise (r = – 0.39, p < 0.05, n = 26) and decreased fatigue (r = 0.36, p = 0.07, n = 26).
4Discussion
This pilot study of a workplace health coaching program had two important primary findings: (1) this health coaching population was characterized by multiple chronic disorders and symptoms; and (2) it supported limited previous research suggesting that health coaching can significantly reduce CVD risks including weight, exercise, stress and sleep, in employees with chronic disease working in a healthcare system [3, 4]. We found that in addition to the common and important focus on metabolic syndrome characteristics and insulin resistance, other co-morbidities may include chronic pain and/or orthopedic needs and depression. In addition, other significant self-reported medical diagnoses were often present, as well as significant stress and a range of other potential symptoms such as fatigue, headaches and poor sleep.
The prevalence of chronic and/or complex disease and symptoms is common, and is rising significantly [10, 22]. Chronic diseases are defined as conditions that last 1 year or more and require ongoing medical attention or limit function, activities of daily living or both. In this specific population the question needs to be raised about the extent to which optimal health outcomes require effective and individualized health approaches and support, addressing the full range of health-related issues present, while being able to prioritize the most important influences on daily functioning and well-being. For example, our finding that greater reduction of stress was directly correlated with a greater increase in exercise suggests that tailoring health coaching to focus on stress reduction could aid in making other healthy lifestyle changes. Similarly, greater reduction in stress levels was directly correlated with reduced fatigue, which, in turn, is linked to presenteeism and workplace productivity [23].
These primary findings suggest that employees may often present with multiple chronic diseases, impacting their health, lives (personal and professional) and healthcare costs, and that a well designed and implemented health coaching program or corporate wellness program that includes health coaching, may effectively encourage sustainable behavioral and lifestyle changes. This ultimately leads to significantly improved physical and emotional well-being, and improved health outcomes [6]. As described elsewhere, this illustrates the important movement toward personalized and precision lifestyle medicine for best practices in healthcare and optimal health outcomes [24–27].
Experienced health coaching, as illustrated in this program, may be essential because of its focus on developing rapport with clients/patients and its client centered focus, as well as the ability to support an integrative or comprehensive program in partnership with the client/patient. Experienced and well-trained health coaches are also needed for employees with complex high-risk chronic disease because of the range of health issues present, and their understanding and ability to apply a range of coaching skills. More effective may be a team of coaches that have expertise in psychological/emotional health, nutrition, and integrative health and medicine who can lead corporate wellness health coaching programs. They in turn can collaborate on yearly modifications or improvements in a program producing effective and sustainable health outcomes and health coaching best practices. Although there would be similar approaches to various disease specific programs, health coaching best practices would need to be developed for CVD and type 2 diabetes mellitus, neuropsychological disorders, chronic pain, GI disorders, cancer, and other categories based on their prevalence and cost to the healthcare system.
Some observations from this health coaching intervention for employees with chronic and/or complex disorders that may support chronic disease health coaching include: (1) the initial 3 month health coaching cycle (6 sessions and approximately 12 weeks) may focus an individualized and potentially effective approach to participant nutrition, movement and exercise, stress management, and resources/support, instead of attaining significant progress toward their goals. This was based on a subset of participants that needed time to try various approaches in order to find what worked best for them; (2) self-care and positive psychology are foundational and appreciated aspects of health coaching – many participants discussed difficulty in finding time for self-care and many voiced their appreciation for not being judged or criticized about how well or poorly they were able achieve their between session goals; (3) for many employees flexible goal setting or ‘maintenance phases’ can be important – these are often needed during times of potentially higher stresses and/or more social activities (e.g. a family illness or crisis, or from Thanksgiving to New Year’s Day or during the summer); this is also an opportunity to evaluate participant program resilience, practicing the ability to make modifications in their lifestyle program that allows them to maintain progress; and (4) these participants often reported feeling overwhelmed so significant consideration is required for the overall support of these employees who need an effective individualized, multifaceted, long-term and ‘local’ support system and program, that encourages their engagement as the path of least resistance.
There were several limitations of this pilot study including: (1) a small sample size with no control group; (2) a self-selected sample, mostly female, conducted in a healthcare setting; and (3) no specific QOL or depression scales. The small sample likely contributed to the lack of statistically significant improvement in the fatigue NRS, as we observed a non-negligible effect size (d = 0.28) for fatigue, and nearly 2/3 of the program participants (25/40) self-reported improved energy/fatigue after taking part in health coaching. Improved fatigue appeared to be linked to several other key outcomes, including lower perceived stress, increased exercise, improved nutrition (based on significant weight loss), and the trend for improved sleep.
In addition to receiving the best health outcomes and most effective disease management possible, another important result of a comprehensive and effective health coaching and corporate wellness program is decreasing healthcare costs. Employees with chronic, multiple chronic and/or complex disease(s) account for a large percentage of these costs [9, 10], and cost-effectiveness and work productivity research is needed. Although a discussion of healthcare costs is beyond the scope of this health coaching pilot, one such study found that health coaching for chronic diseases such as type II diabetes and coronary artery disease were cost effective, while it was not cost effective for the management of congestive heart failure (CHF) [28]. This suggests that health coaching cost effectiveness may vary across subgroups of chronically ill clients or patients.
4.1Future research
Significant future research is required to clarify and confirm a range of issues addressed in this article. First, research is needed to confirm our findings in a larger, more demographically diverse sample, and to see if similar outcomes and associations emerge among employees with chronic diseases, higher or persistent levels of stress, and co-morbid disorders such as depression. Additional studies are also needed to further characterize what specific types and combinations of chronic diseases and co-morbid conditions are present in employees, that are associated with the highest healthcare costs.
Methodological designs should also ensure that health coaching studies more clearly describe the health coach characteristics and health coaching approaches used. Sound psychometric outcome measures should be disease specific and be easily completed. This will help other researchers to replicate research findings and to evaluate potentially inconsistent study results in similar populations. Finally, this important research will help to identify chronic disease specific health coaching and corporate wellness best practices that are most likely to engage employees, produce behavioral and lifestyle changes, and ultimately achieve optimal health outcomes and lower healthcare costs.
5Conclusions
Health coaching for healthcare employees with obesity and other co-morbidities can improve weight and other important CVD risk factors, including exercise, stress, and sleep. This may be particularly helpful for employees with chronic or complex disorders who may have a vicious cycle of chronic disease and symptoms, and significant stress. Given chronic disease influences on healthcare costs, ongoing research of chronic disease health profiles, health coaching best practices, and health outcomes is warranted.
Conflict of interest
None to report.
References
[1] | Munoz Obino KF , Aguiar Pereira C , Caron-Lienert RS . Coaching and barriers to weight loss: An integrative review. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy (2016) ;10: :1–11. |
[2] | Lerner D , Adler DA , Rogers WH , Chang H , Greenhill A , Cymerman E , Azocar F . A randomized clinical trial of a telephone depression intervention to reduce employee presenteeism and absenteeism. Psychiatr Serv (2015) ;66: :570–7. |
[3] | Foy AJ , Mandrola JM . Heavy heart: The economic burden of heart disease in the United States now and in the future. Prim Care (2018) ;45: :17–24. |
[4] | Theorell Jood K , Jarvholm LS , Vingard E , Perk J , Ostergren PO , Hall C . A systematic reviw of the studies in the contributions of the work environment to ischaemic heart disease development. Eur J Public Health (2016) ;26: :470–77. |
[5] | Harter M , Dirmaier J , Dwinger S , Kriston L , Herbarth L , Siegmund-Schultze E , Bermejo I , Matschinger H , Heider D , Konig HH . Effectiveness of telephone-based health coaching for patients with chronic conditions: A randomized controlled trial. PLOS One (2016) ; September 15, 2016. |
[6] | Kivela K , Elo S , Kyngas H , Kaariainen M . The effects of health coaching on adult patients with chronic diseases: A systematic review. Patient Educ Couns (2014) ;97: :147–57. |
[7] | Benson GA , Sidebottom A , Sillah A , Boucher JL , Miedema MD , Knickelbine T , VanWormer JJ . Reach and effectiveness of the HeartBeat Connections telemedicine pilot program. J Telemed Telecare (2017) , Jan 1 Epub. |
[8] | Ski CF , Vale MJ , Bennett GR , Chalmers VL , McFarlane K , Jelinek VM , Scott IA , Thompson DR . Improving access and equity in reducing cardiovascular risk: The Queensland Health model. Med J Aust (2015) ;202: :148–52. |
[9] | Rieken M , Struckmann V , Melchieone MG , on the behalf of the ICARE4EU partners et al. ICARE 4EU. Improving care for people with multiple chronic conditions in Europe. Eurohealth (2013) ;19: :29–31. |
[10] | Sambamoorthi U , Tan X , Deb A . Multiple chronic conditions and healthcare costs among adults. Expert Rev Pharmacoecon Outcomes Res (2015) ;15: :823–32. |
[11] | Goetzel RZ , Henke RM , Head MA , Benevent R , Calitz C . Workplace programs, policies and Environmental supports to prevent cardiovascular disease. Health Aff (2017) ;36: :229–36. |
[12] | Cohen S , Kamarck T , Mermelstein R . A global measure of perceived stress. J Health Soc Behav (1983) ;24: :385–96. |
[13] | Karam F , Berard A , Sheehy O , Huneau MC , Briggs G , Chambers C , Einarson A , Johnson D , Kao K , Koren G , Martin B , Polifka JE , Riordan SH , Roth M , Lavigne SV , Wolfe L , OTIS Research Committee Reliability and validity of the 4-item perceived stress scale among pregnant women: Results from the OTIS antidepressants study. Res Nurs Health (2012) ;35: :363–75. |
[14] | Lee EH . Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (2012) ;6: :121–7. |
[15] | Wolever RQ , Abrams DI , Kligler B , Dusek JA , Roberts R , Frye J , Edman JS , . Patients seek integrative medicine for preventive approach to optimize health. Explore (2012) ;8: :348–52. |
[16] | Farrar JT , Young Jr JP , LaMoreaux L , Werth JL , Poole RM . Clinical importance of changes in chronic pain intensity measured on an 11 point numerical pain rating scale. Pain (2001) ;94: :149–58. |
[17] | Friedberg F , Naploi A , Coronel J , Adamowicz J , Seva V , Caikauskaite I , Ngan MC , Chang J , Meng H . Chronic fatigue self-assessment in primary care: A randomized trial. Psychosom Med (2013) ;75: :650–7. |
[18] | Edman JS , Greeson JM , Roberts RS , Kaufman AB , Abrams DI , Dolor RJ , Wolever RQ . Perceived stress in patients with common gastrointestinal disorders: Associations with QOL, symptoms and disease management. Explore (2017) ;13: :124–8. |
[19] | Wolever RQ , Jordan M , Lawson K , Moore M . Advancing a new evidence-based profession in healthcare: Job task analysis for health coaches. BMC Health Services Research (2016) ;16: :205. |
[20] | Moore M , Tschannen-Moran B , Coaching Psychology Manual, Lippincott Williams & Wilkins, Philadelphia, PA, (2010) . |
[21] | Cohen J , Statistical Power Analysis for the Behavioral Sciences, Lawrence Erlbaum, Hillsdale, NJ, USA, (1988) . |
[22] | Raghupathi W , Raghupathi V . An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach. Int J Environ Res Public Health (2018) ;15: :431. |
[23] | VanWormer JJ , Fyfe-Johnson AL , Boucher JL , Johnson PJ , Britt HR , Thygeson NM , Dusek JA . Stress and workplace productivity loss in the Heart New Ulm project. J Occup Envir Med (2011) ;53: :1106–9. |
[24] | Leopold JA , Loscalzo J . Emerging role of precision medicine in cardiovascular disease. Circ Res (2018) ;122: :1302–15. |
[25] | van Ommen B , Wopereis S , van Empelen P , van Keulen HM , Otten W , Kasteleyn M , Molema JJW , de Hoogh IM , Chavannes NH , Numans ME , Evers AWM , Pijl H . From diabetes care to diabetes cure – the integration of systems biology, ehealth and behavioral change. Front Endocrinol (2018) ;8: :381. |
[26] | Paguntalan JC , Gregoski M . Physical activity barriers and motivators among high-risk employees. WORK (2016) ;55: :515–24. |
[27] | McEwen BS . Integrative medicine: Breaking down silos of knowledge and practice an epigenetic approach. Metabolism (2017) ;69S: :S21–9. |
[28] | Oksman E , Linna M , Horhammer I , Lammintakanen J , Talja M . Cost-effectiveness analysis for a tele-based health coaching program for chronic disease in primary care. BMC Health Services Research (2017) ;17: :138. |




