Utility of in-session assessments during cognitive behavioral therapy for depression after traumatic brain injury: Results from a randomized controlled trial
Abstract
BACKGROUND:
The development of depression after moderate to severe traumatic brain injury (TBI) is common. Cognitive-behavioral therapy (CBT) can be used to treat post-TBI depression, but the symptoms response is poorly described.
OBJECTIVE:
This secondary analysis assessed: (1) the trajectory of depression symptoms up to 12 sessions of CBT, (2) which depressive symptom clusters were responsive to in-person and phone CBT, and (3) whether interim depression thresholds predict 16-week treatment response.
METHOD:
This secondary analysis of the IRB-approved Life Improvement Following Traumatic Brain Injury trial included 100 adults with major depressive disorder (MDD) within ten years of moderate to severe traumatic brain injury from throughout the US. We used a combination of descriptive, graphical, and diagnostic accuracy methods.
RESULTS:
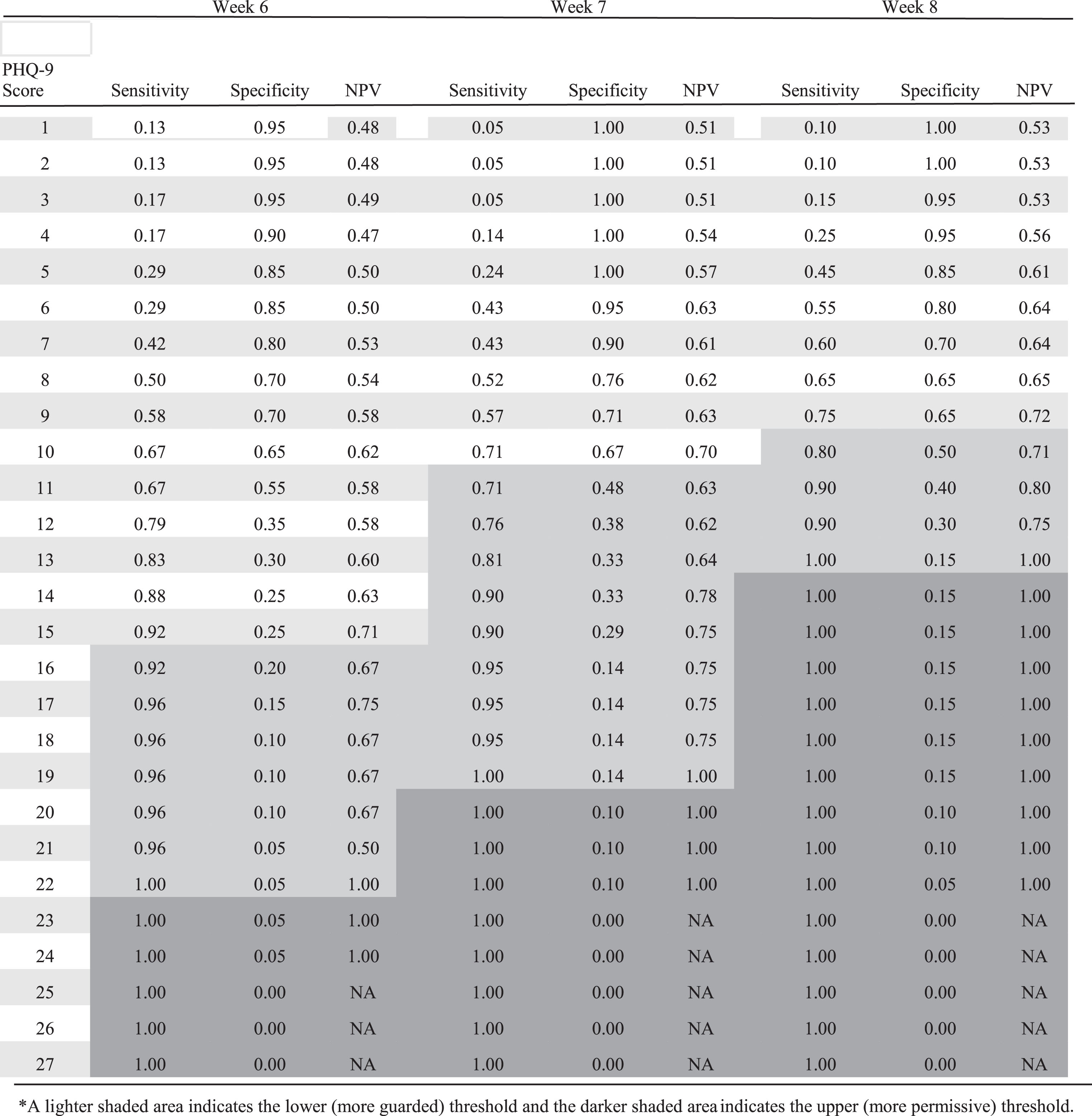
Cardinal and cognitive-affective symptom clusters improved most from CBT over 16 weeks. At 8 and 16 weeks, the most responsive individual symptoms were anhedonia, depressed mood, and fatigue; the least responsive were sleep and appetite. PHQ-9 thresholds with a Negative Predictive Value greater than 0.7 for sessions 6, 7, and 8 were, respectively: >15, >10, and >9.
CONCLUSION:
In-person and phone CBT led to similar symptom responses during treatment. Additionally, using PHQ-9 thresholds for predicting intervention response within eight sessions may help identify the need for treatment adjustments.
1Introduction
Up to half of the persons with moderate to severe traumatic brain injury (TBI) will meet the criteria for major depressive disorder (MDD) within a year after hospitalization (Bombardier, 2010). Over the past 15 years, clinical researchers have experimented with adaptations of cognitive-behavioral therapy (CBT) to treat MDD in people with TBI (Anson, 2006). CBT is based on the theory that negative thinking patterns and lack of engagement in enjoyable and meaningful activities contribute to MDD (Beck, 1979). Investigators have experimented with CBT for TBI-related depression because it has strong evidence for efficacy in people with primary major depression (Cuijper, 2008). Several studies have shown that CBT can effectively treat MDD in persons with TBI (Fann, 2015; Ponsford, 2016). Furthermore, studies across various medical settings show that CBT is equally effective when delivered over the telephone vs. in person (Stiles-Shields, 2015; Mohr, 2008). However, as many as 65% of people with TBI receiving CBT for depression will not respond to treatment (Ashman, 2014, Ponsford 2016).
Several factors that impact CBT response in TBI have been described, including older age, more extended post-TBI recovery period, better executive function, client homework engagement, and therapist consistency in using homework (Zelencich, 2020). To add to this literature, we examined whether within-treatment indicators such as overall symptom improvement, improvement within specific symptom clusters, or symptom severity cut-points help predict treatment outcomes and guide interim treatment decisions. It would be helpful to know whether individual symptoms or symptom clusters are more or less responsive during treatment. Furthermore, knowing that not meeting interim treatment progress benchmarks predicts poor treatment outcomes could allow clinicians to intensify or supplement CBT before the course of CBT is completed to improve treatment outcomes. A recent study of behavioral activation examined using a single variable Likert scale during treatment sessions to characterize response (Brenner, 2018). Other therapies have been described in the literature as treating post-TBI depression, including supportive psychotherapy, behavioral activation, CBT, and mindfulness-based cognitive therapy (Beedham, 2020, Ponsford 2016). However, PHQ-9 scores were not described as an in-session measurement during CBT.
As a result of the COVID-19 pandemic, interventions such as CBT have been increasingly delivered remotely (Tajan, 2023). When treatments can be provided in different ways (e.g., in-person versus telephone), knowing whether individual symptoms or symptom clusters respond differently depending on the delivery mode could facilitate treatment decisions. Creating additional literature that explores the potential difference between phone and in-person interventions will be important as healthcare assesses how best to conduct CBT and other interventions post-pandemic. Finally, it would be clinically helpful to determine whether interim measures of depression severity could be used to predict who will likely not respond to treatment, thus guiding timely treatment adjustment, augmentation, or switching.
A study by Schueller et al. (2015) of general adult outpatients in a primary care clinic with MDD demonstrated that there are Patient Health Questionnaire-9 (PHQ-9) depression score cut-off thresholds during 18-session CBT that predict which patients would respond to treatment. They found that a score of <17 at four sessions, <13 at nine sessions, and <9 at 14 sessions predicted eventual treatment response at 18 weeks.
While the PHQ-9 is a valid tool for screening and monitoring depressive symptoms in people with TBI, studies have not examined how the individual PHQ-9 items respond to treatment and whether the symptom courses differ in those receiving in-person or telephone-delivered CBT (Fann, 2005). Furthermore, PHQ-9 items have been categorized into symptom clusters, for example, cardinal symptoms (anhedonia and depressed mood), cognitive-affective symptoms (guilt, concentration, and suicidal thoughts), and somatic symptoms (sleep, fatigue, appetite, and psychomotor changes) (Vrany, 2016; Beard, 2016). These clusters may respond differently to in-person vs. telephone CBT.
The aims of this secondary analysis of the Life Improvement Following Traumatic Brain Injury (LIFT) study (Fann 2015) were to: (1) examine the trajectory of depression symptoms as measured by in-session PHQ-9 scores throughout the 12-session CBT treatment for depression, (2) determine which depression symptom clusters are most responsive to treatment with in-person and phone-delivered CBT, and (3) determine whether in-session depression assessments at different stages of treatment can predict eventual treatment response. While the LIFT study assessed CBT outcomes, it did not evaluate these in-session factors. The small sample size of these groups only allows for descriptive assessments. We are completing this secondary analysis to generate hypotheses around potential new research areas.
2Methods
The study data was collected under an approved Institutional Review Board protocol at the University of Washington before the original study in 2015. The trial was registered with ClinicalTrials.gov and issued identifier NCT00878150. We conducted a secondary analysis of data collected during the LIFT trial, a randomized, choice-stratified controlled trial of up to 12 sessions of telephone-delivered or in-person CBT vs. usual care for MDD within ten years of moderate to severe TBI (Fann, 2015). MDD was confirmed using the Structured Clinical Interview for DSM-IV (SCID) (Beard, 2016). Full descriptions of the study sample and protocol can be found elsewhere (Fann, 2015). In brief, the LIFT study compared CBT administered over the phone (CBT-T) (n = 40) or in-person (CBT-IP) (n = 18) compared with usual care (UC) (n = 42) over 16 weeks (Fann, 2015). The intervention used in this study was CBT-TBI adapted from structured telephone management and CBT protocol. It occurred over 16 weeks (Fann, 2015). Components of care management, motivational interviewing, psychoeducation, and accommodations for cognitive impairment were part of the protocol.
2.1Measures
The Patient Health Questionnaire-9 (PHQ-9) was used to measure response to treatment regarding the trajectories of individual symptoms and symptom clusters (cardinal, cognitive-affective, and somatic). The PHQ-9 is a widely used depression screening and symptom severity measure in psychiatric patients (First, 1997). The PHQ-9 is reliable, valid as a screener, and sensitive to treatment effects in people with TBI (Fann, 2005; Kroenke, 2001). The study therapist administered the PHQ-9 by interview to assess interim response to treatment during each CBT session.
The Hopkins Symptom Checklist-20 (SCL-20) version B was used as an independent measure of response to treatment (Dyer, 2016). The SCL-20 has good construct validity and sensitivity to change compared to other valid measures of depression in people with TBI (Dyer, 2016). A blinded rater not involved in depression treatment administered the SCL-20 in an interview format to all subjects at 8, 16, and 24 weeks. Responders were defined as those who demonstrated at least a 50% reduction in the SCL-20 from baseline to the end of treatment (week 16).
2.2Statistical analysis
A combination of descriptive, graphical, and diagnostic accuracy methods was used to evaluate longitudinal variation in symptom patterns and optimal cutoff scores on the PHQ-9 for predicting response outcomes. Descriptive and visual analyses disaggregate item improvement probabilities on the PHQ-9 individual items and symptom clusters (cardinal, cognitive-affective, and somatic). These item-improvement patterns were presented to provide a descriptive illustration of trajectory profiles throughout the intervention.
For the participants in the in-person or phone CBT conditions and each follow-up during the intervention, the optimal treatment thresholds on PHQ-9 for predicting a 16-week response were calculated. The negative predictive value (NPV), or the probability of not responding to intervention among those anticipated not to respond, to determine optimal cutoff scores for each session were used; also, the sensitivity (probability of response prediction among those who responded) and specificity (probability of non-response among those who did not respond) for each possible optimal threshold score were provided.
3Results
The primary study findings can be described elsewhere (Fann, 2015). Briefly, 100 participants with MDD met the entrance criteria, consented, and were randomized to telephone-delivered CBT (CBT-T: n = 40), in-person CBT (CBT-IP, n = 18), or usual care (UC, n = 42). Meantime, since injury was 3.33 (SD 2.72) years and 31% had severe TBI. 12% did not provide 16-week outcome data, and 14% did not offer 24-week outcome data. The mean number of sessions was 9.6 (SD 3.3) for the CBT-T group and 8.6 (SD 4.6) for the CBT-IP group. All study groups’ demographic and injury characteristics can be found in the original study description (Fann, 2015).
3.1Symptom trajectories
Our secondary analysis found no significant difference between the combined CBT and UC groups over 16 weeks on the SCL-20. In follow-up comparisons, the CBT-T group had significantly more improvement on the SCL-20 than the UC group (p = 0.043), and those who completed eight or more CBT sessions (CBT-T = 73% and CBT-IP = 61%) had significantly improved SCL-20 scores compared with the UC group (p = 0.011). CBT participants reported substantially more symptom improvement (p = 0.010) and greater satisfaction with depression care (p < 0.001) than did the UC group (Fann, 2015).
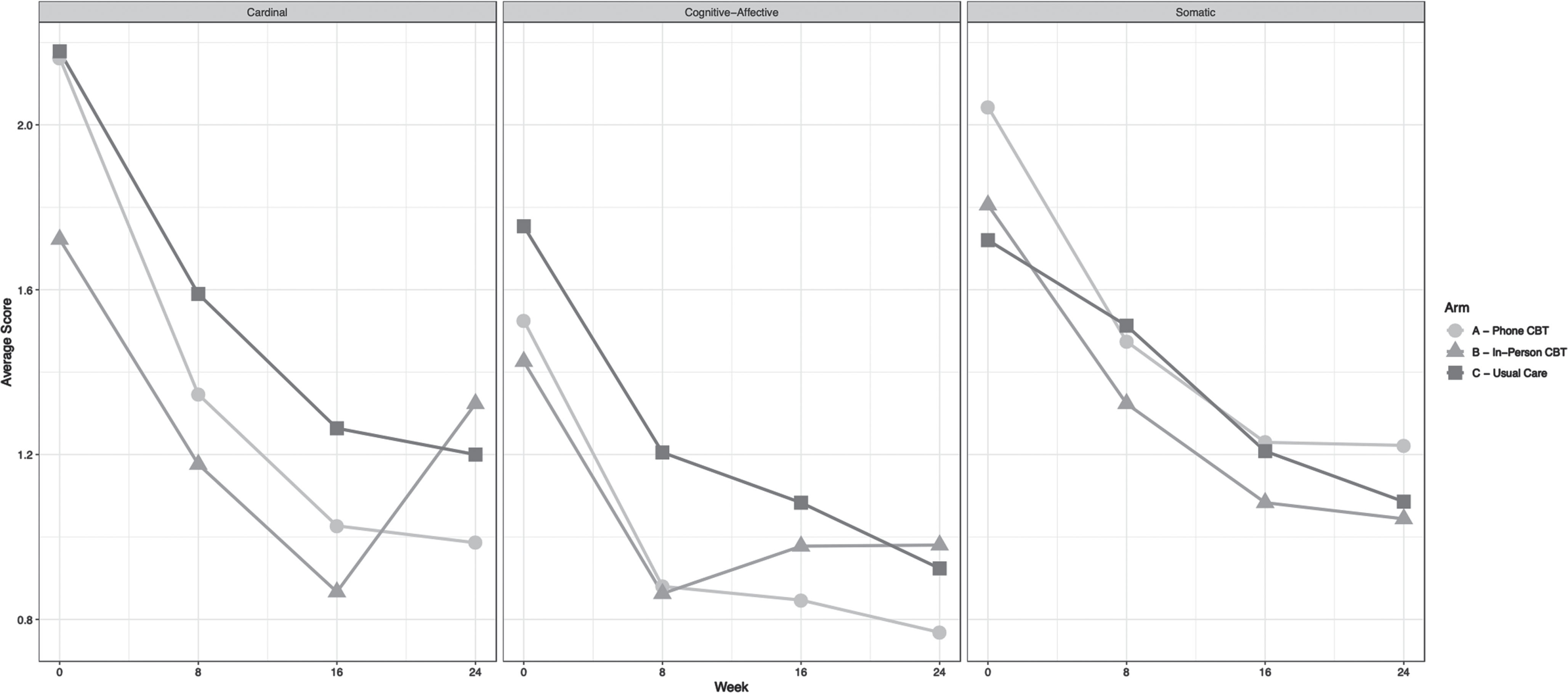
Figure 1a shows the trajectory of individual symptoms, and Fig. 1b shows the course of symptom clusters for the three treatment groups at baseline and the 8, 16, and 24-week outcome assessments. The CBT groups showed more rapid interest, energy, and guilt improvement than the UC group. However, symptoms of somatic motor, appetite, and sleep disturbance showed a minimal difference between CBT and UC groups. There was more remarkable improvement in cardinal and cognitive-affective clusters than UC over 16 weeks, with the somatic cluster’s trajectory similar to UC. Many of the symptoms and clusters in the CBT groups were similar to those in the UC group, with the in-person CBT group generally showing more significant symptom regression than the phone CBT group, particularly for the cardinal and cognitive-affective clusters by 24 weeks.
Fig. 1a
Graphic display of depression symptom trajectories.
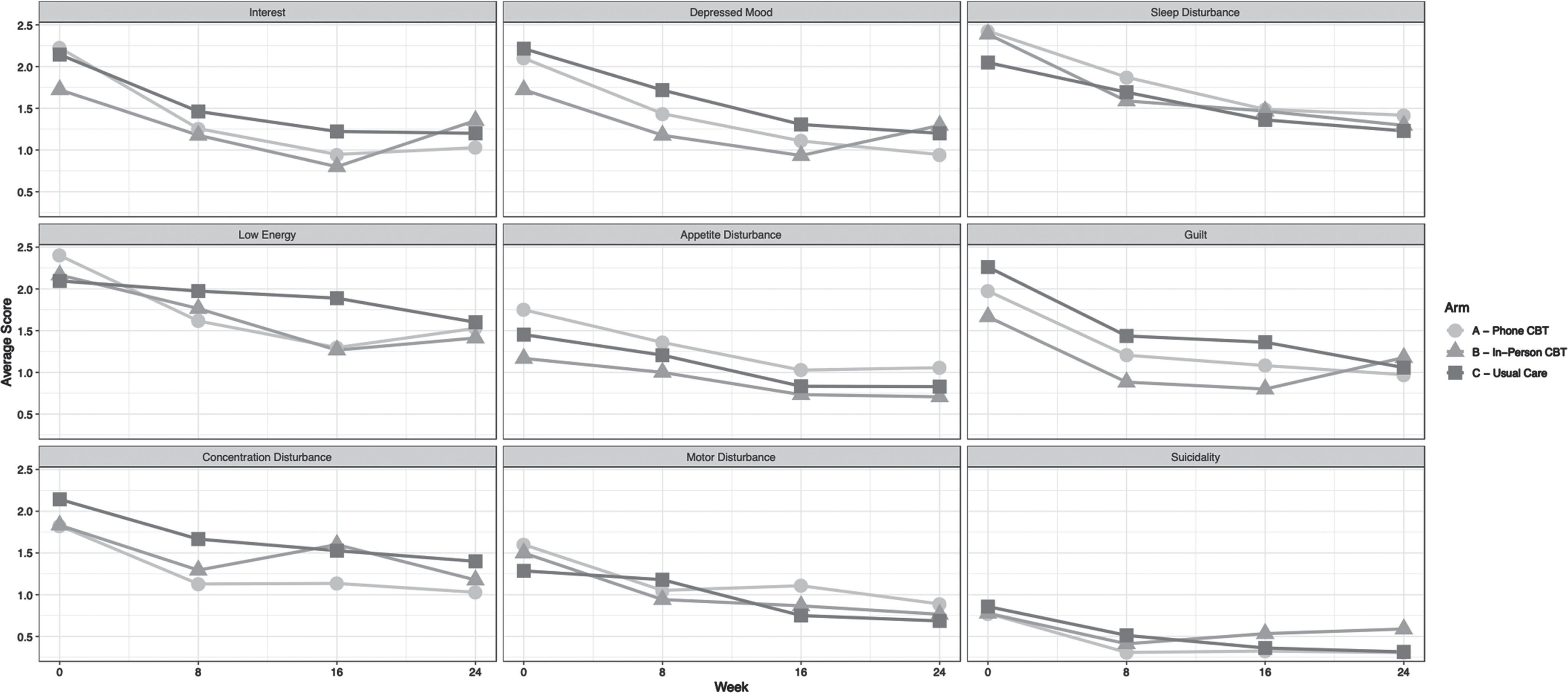
Fig. 1b
Graphic display of symptom cluster trajectories.
3.2Symptom improvement
Figure 2a shows in-session symptom severity data on individual symptoms for CBT-T responders and non-responders. Overall, the PHQ-9 scores obtained by the therapist appear to track progress exceptionally well compared to outcomes on the SCL-20 measured by an independent blinded observer. There is a visible difference between CBT-T and UC symptom severity after the first assessment. As the sessions progressed, more non-responding participants stayed in severity categories of ‘more than half the days’ or higher, with responders progressing into scores of ‘several days’ or ‘not at all.’
Fig. 2a
Graphic display of symptom severity over time of CBT-T responders and non-responders.
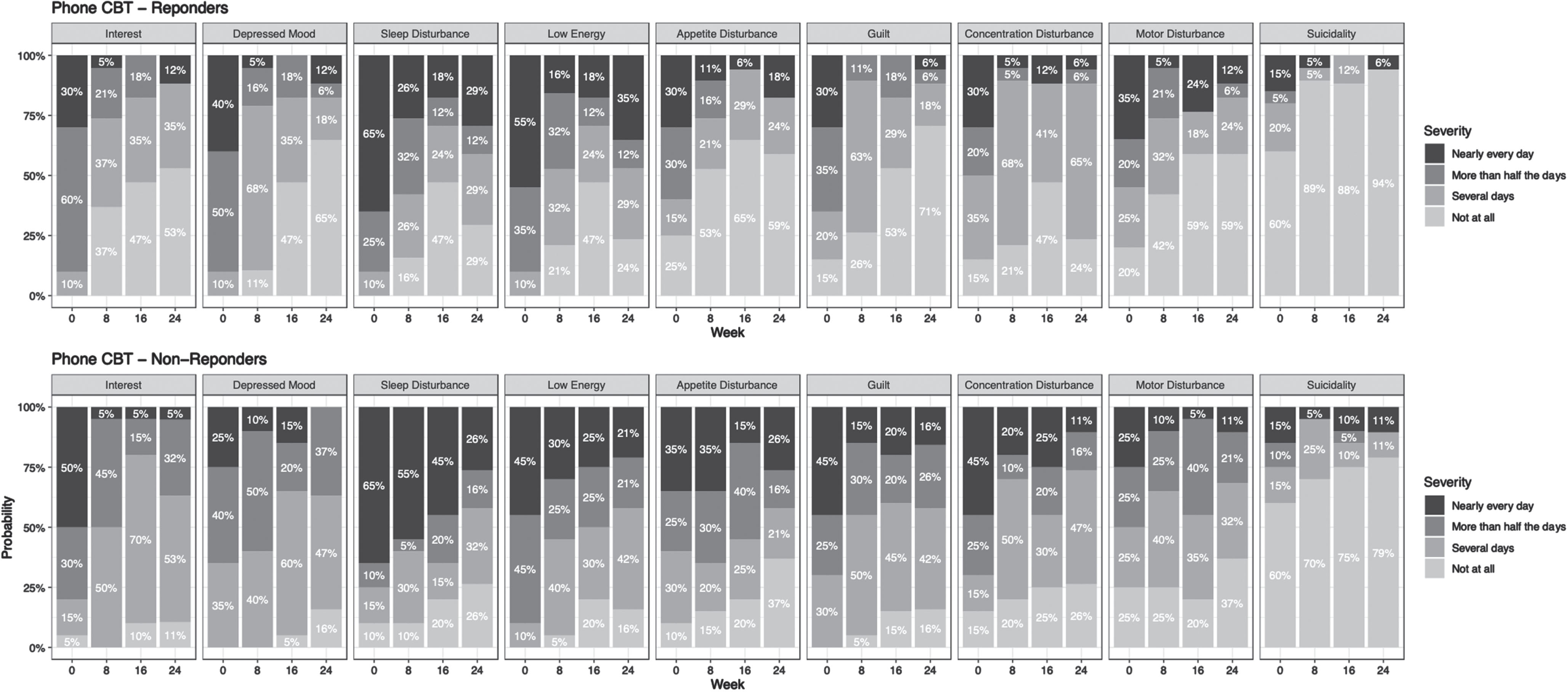
Visually, responders have consistently better reported scores in interest, depressed mood, appetite disturbance, guilt, and suicidality. Over time, concentration also improves but is slower. Sleep disturbance and low energy also decrease over time but not robustly.
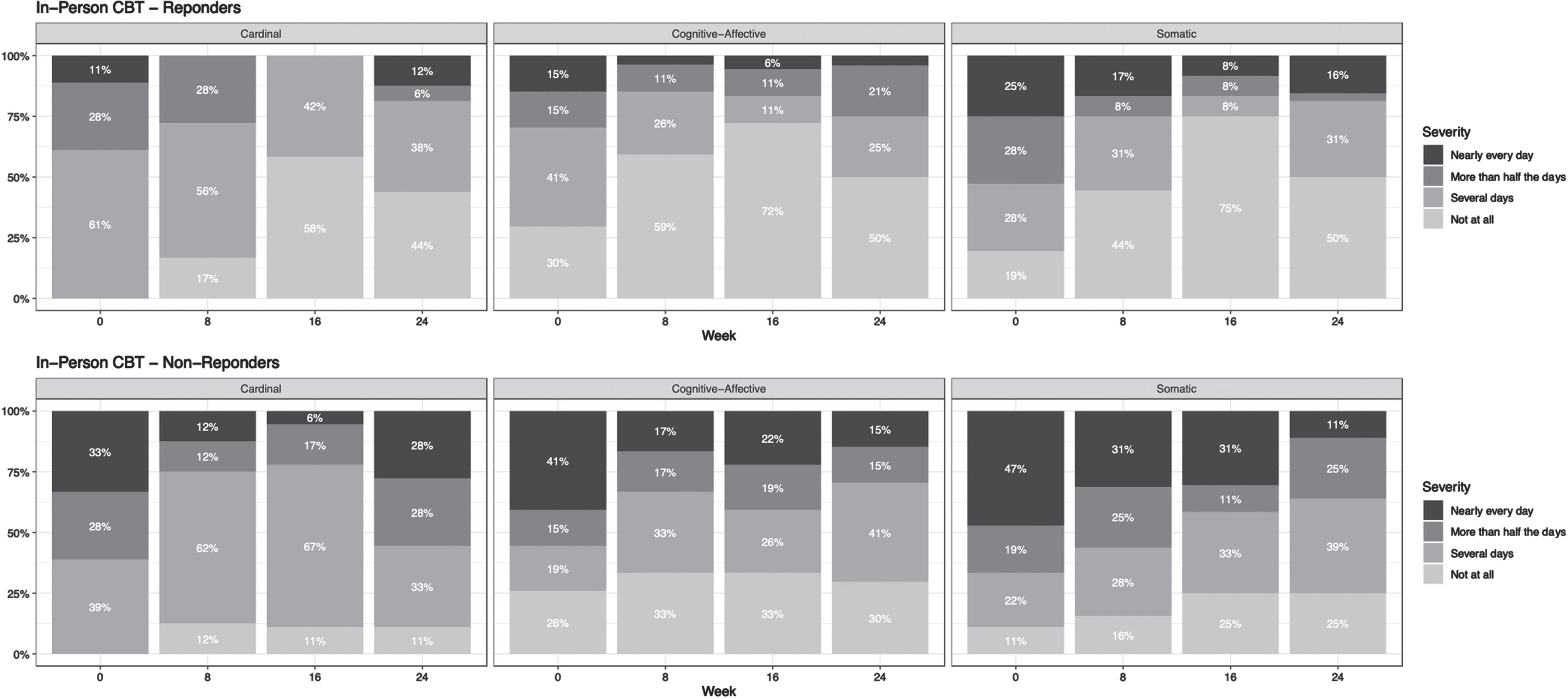
Figure 2b shows the percentage of patients with a combined score on the symptom clusters over time for CBT-T responders and non-responders. The cardinal and cognitive-affective clusters improve rapidly in eventual treatment responders, while the somatic cluster shows similar changes between responders and non-responders over time.
Fig. 2b
Graphic display of symptom cluster severity over time of CBT-T responders and non-responders.
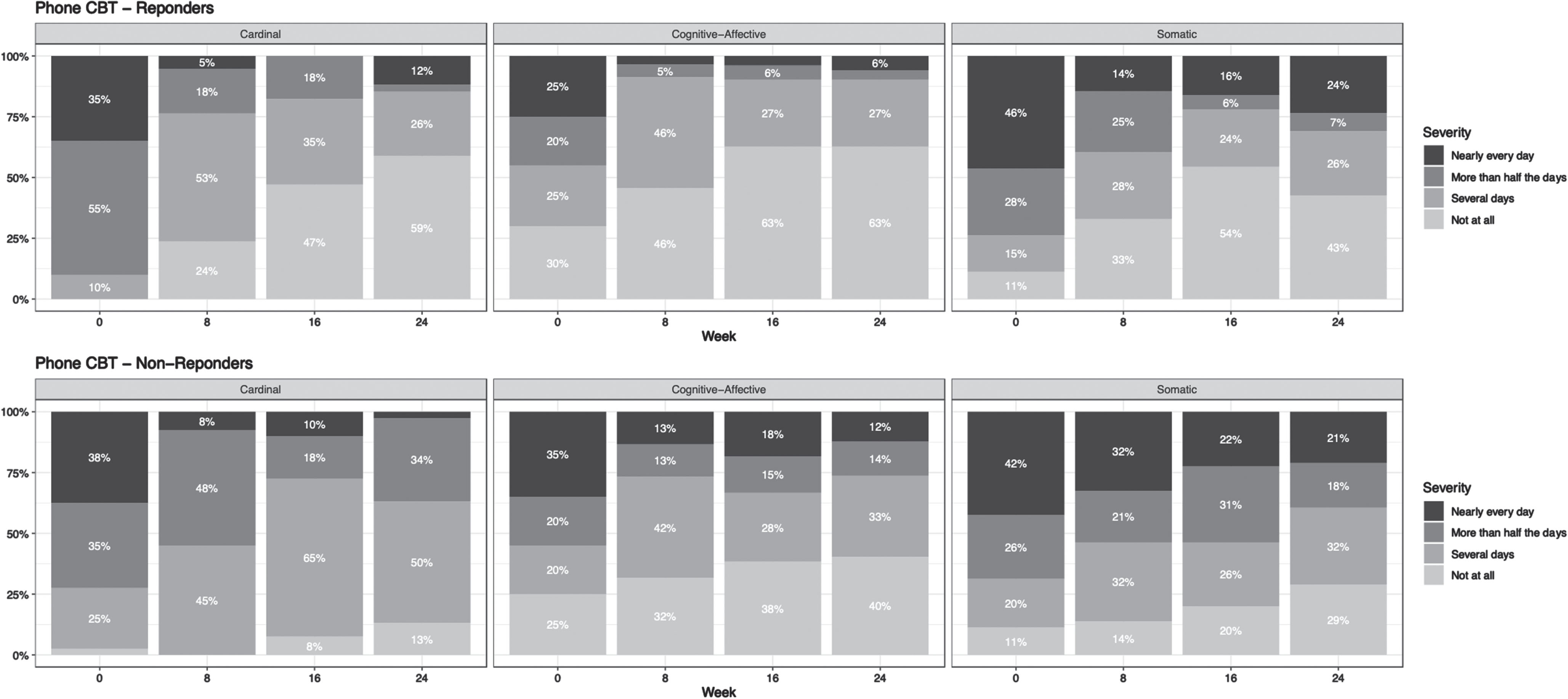
Figure 3a shows in-session symptom severity data for CBT-IP responders and non-responders. Overall, the week-to-week scores appear less consistent than the CBT-T group. However, responders consistently reported lower scores in interest, depressed mood, appetite disturbance, guilt, and suicidality. Eventually, concentration also improves, but not as quickly or consistently. Sleep disturbance and low energy also improve over time but not as robustly.
Fig. 3a
Graphic display of symptom severity over time of CBT-IP responders and non-responders.
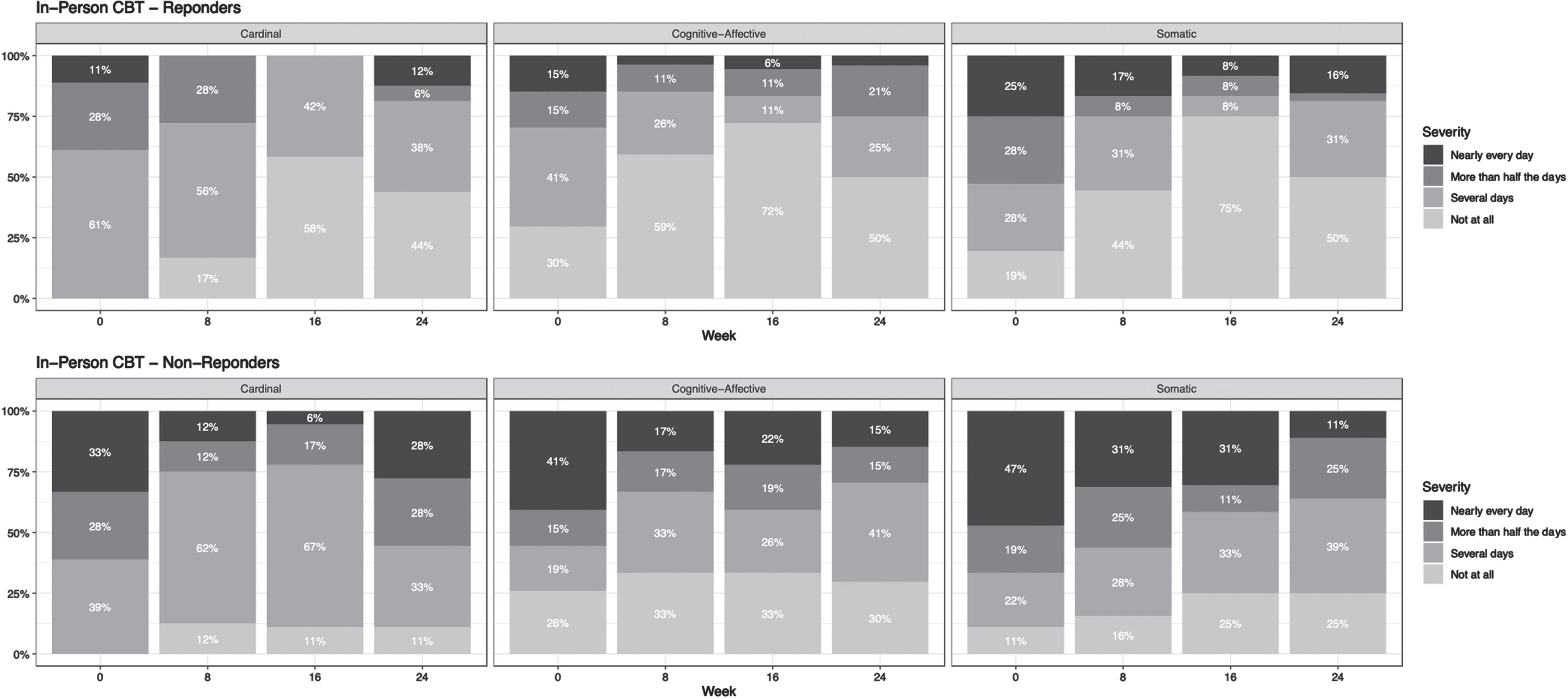
Figure 3b shows in-session severity data on symptom clusters for CBT-IP responders and non-responders. Both the cardinal and cognitive-affective scores improve quickly. The somatic cluster shows the least improvement over time.
Fig. 3b
Graphic display of symptom cluster severity over time of CBT-IP responders and non-responders.
3.3Symptom predictors of response
Using the 58 CBT participants, we calculated the sensitivity, specificity, and negative predictive value (NPV) of the PHQ-9 scores at sessions 6, 7, and 8. In setting thresholds, we prioritized the NPV as a practical criterion: the probability of non-response for a given score. High NPVs could indicate that the active treatment regimen needs modification. The 6–8-week period often corresponds to a near midpoint in many CBT interventions, so we focused on these time points.
Our team identified two thresholds of potential interest to clinicians as part of this analysis. The first is an ‘upper’ (more permissive) threshold, corresponding to the lowest PHQ-9 scores that maximize the NPV. These thresholds are higher, meaning that the active treatment intervention would be more likely to be permitted to continue until further evaluation, and they may miss as many eventual non-responders. The following upper treatment thresholds were identified for sessions 6, 7, and 8, respectively: >22, >19, and >13. The second threshold of potential interest to clinicians is a ‘lower’ (more guarded) threshold, corresponding to the lowest PHQ-9 scores that indicate an NPV of at least.70 (i.e., a non-response probability of 70%). These thresholds are lower and would more likely trigger an early modification to the clinical regimen. The following lower thresholds were identified for sessions 6, 7, and 8, respectively: >15, >10, and >9.
Table 1
Optimal treatment thresholds on the PHQ-9 at sessions 6, 7, and 8*
 |
4Discussion
This is the first study to examine the trajectory and predictive value of depression symptoms during CBT among individuals with TBI. While a previous study provided a single variable visual report of depression in a behavioral activation intervention, this study offers visual reports of all PHQ-9 symptoms and depression clusters (Brenner, 2018). At 8 and 16 weeks, the most treatment-responsive symptoms were anhedonia, depressed mood, and fatigue. The least responsive symptoms were sleep and appetite disturbance. Furthermore, most symptoms that seemed to respond to CBT showed some regression at the 24-week follow-up. While it is unclear what is causing this phenomenon, it suggests that patients may benefit from some follow-up after a course of CBT to provide relapse prevention strategies to maintain symptomatic gains.
The cardinal, cognitive, and affective symptoms improve more with CBT than somatic symptom clusters. Since the intervention focuses on cognitive and behavioral strategies, it is unsurprising that these clusters responded more strongly to treatment than somatic symptoms. Some somatic symptoms, such as insomnia, appear nonresponsive to CBT for depression. Increasing evidence shows that sleep disorders require specialized diagnostic and treatment efforts after TBI (Wolfe, 2018). In contrast, another somatic symptom, fatigue, did improve in response to CBT for depression, likely due to the early emphasis on behavioral activation in the treatment protocol.
Overall, there is a consistent symptom pattern present between responders and non-responders. Our findings of how symptoms respond over time to CBT support the importance of measurement-based care for depression in this population. These results can assist clinicians and patients in shared decision-making about depression treatment and help clinicians provide psychoeducation to patients about what improvements to anticipate during CBT.
We found no difference in response between phone and in-person CBT. This suggests that how CBT is accessed may not matter significantly regarding who will respond to the modality. COVID-19 has dramatically changed how many providers practice, and this finding provides some optimism for assisting this vulnerable population during the pandemic.
5Conclusion
Our findings suggest that even during treatment, responders and non-responders begin to look different on PHQ-9 scores and that probable non-responders may be identified before an entire course of treatment. Like Schueller et al., we found consistent PHQ-9 response thresholds predictive of subsequent treatment response. Our analysis suggests that patients who score above this threshold during sessions 6, 7, and 8 are not likely to progress toward a complete treatment response. While replication of these findings will be needed, this analysis suggests that patients likely to be non-responsive to CBT can be identified during treatment. This may allow for more timely identification and initiation of alternate treatment protocols such as antidepressant medications or an adjustment in the psychotherapeutic approach.
Limitations
There are several limitations to this study. The symptomatic comparisons are phenomenological and not conducive to statistical comparisons. Our sample is relatively small; therefore, the optimal thresholds identified in this study need to be replicated. Due to these limitations, these findings are hypothesis-generating rather than hypothesis-testing. Clinicians should not consider these as strict thresholds but somewhat approximate indications of likely non-response under the current clinical regimen.
Future directions
This study demonstrates that among patients with TBI and MDD, the cardinal and cognitive-affective symptoms of depression respond better to CBT than somatic symptoms. These symptom patterns do not differ markedly between those receiving CBT in person or via telephone. CBT treatment responders and non-responders may potentially be identified as early as the sixth treatment session, providing clinicians an early indication that a patient needs to be ‘stepped up’ to a different or increased treatment intensity. More extensive studies are required to confirm and further explore these findings. In addition, repeating this study to assess symptom response and thresholds by characteristics such as gender, age, and education level may identify further factors that could predict response to CBT. Finally, a study examining the outcome of early treatment adjustments guided by in-session assessments is warranted.
Acknowledgments
None to report.
Conflicts of interest
None of the authors report conflicts of interest.
Data availability statement
The data sets generated and analyzed during the current study are available from the senior author upon reasonable request.
Funding
The study was supported by the National Institutes of Health (grant R21HD53736) and the Department of Education, National Institute on Disability and Rehabilitation Research (grant H133G070016).
References
1 | Anson, K. , Ponsford, J. ((2006) ). Who benefits? Outcome following a coping skills group intervention for traumatically brain injured individuals. Brain injury, 20: (1), 1–13. |
2 | Ashman, T. , Cantor, J. B. , Tsaousides, T. , Spielman, L. , Gordon, W. ((2014) ). Comparison of cognitive behavioral therapy and supportive psychotherapy for treating depression following traumatic brain injury: a randomized controlled trial. The Journal of Head Trauma Rehabilitation, 29: (6), 467–478. |
3 | Beard, C. , Hsu, K. J. , Rifkin, L. S. , Busch, A. B. , Björgvinsson, T. ((2016) ). Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders, 193: , 267–273. |
4 | Beck, A. T. (Ed.). (1979). Cognitive therapy of depression. Guilford press. |
5 | Beedham, W. , Belli, A. , Ingaralingam, S. , Haque, S. , Upthegrove, R. ((2020) ). The management of depression following traumatic brain injury: A systematic review with meta-analysis. Brain injury, 34: (10), 1287–1304. |
6 | Bombardier, C. H. , Fann, J. R. , Temkin, N. R. , Esselman, P. C. , Barber, J. , Dikmen, S. S. ((2010) ). Rates of major depressivedisorder and clinical outcomes following traumatic brain injury. JAMA, 303: (19), 1938–1945. doi: 10.1001/jama.2010.599. |
7 | Brenner, L. A. , Forster, J. E. , Hoffberg, A. S. , Matarazzo, B. B. , Hostetter, T. A. , Signoracci, G. , Simpson, G. K. ((2018) ). Windowto Hope: a randomized controlled trial of a psychologicalintervention for treating hopelessness among veterans with moderateto severe traumatic brain injury. Journal of Head TraumaRehabilitation, 33: (2), E64–E73. |
8 | Caplan, B. , Bogner, J. , Brenner, L. , Dyer, J. R. , Williams, R. , Bombardier, C. H. , Fann, J. R. ((2016) ). Evaluating thepsychometric properties of 3 depression measures in a sample ofpersons with traumatic brain injury and major depressive disorder. Journal of head trauma rehabilitation, 31: (3), 225–232. |
9 | Cuijpers, P. , van Straten, A. , Andersson, G. , van Oppen, P. ((2008) ). Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol, 76: (6), 909–922. doi: 10.1037/a0013075. |
10 | Fann, J. R. , Bombardier, C. H. , Vannoy, S. et al. ((2015) ). Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: a randomized controlled trial. J Neurotrauma, 32: (1), 45–57. doi: 10.1089/neu.2014.3423. |
11 | Fann, J. R. , Bombardier, C. H. , Dikmen, S. , Esselman, P. , Warms, C.A. , Pelzer, E. , Temkin, N. ((2005) ). Validity of the PatientHealth Questionnaire-9 in assessing depression following traumaticbrain injury. The Journal of Head Trauma Rehabilitation, 20: (6), 501–511. |
12 | First, M. B. (1997). Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), Clinician Version (Administration Booklet). American Psychiatric Publishing, Inc. |
13 | Kroenke, K. , Spitzer, R. L. , Williams, J. B. ((2001) ). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16: (9), 606–613. |
14 | Mohr, D. C. , Vella, L. , Hart, S. , Heckman, T. , Simon, G. ((2008) ). The effect of telephone-administered psychotherapy on symptoms of depression and attrition: A meta-analysis. Clinical Psychology: Science and Practice, 15: (3), 243. |
15 | Ponsford, J. , Lee, N. , Wong, D. et al. ((2016) ). Efficacy of motivational interviewing and cognitive behavioral therapy for anxiety and depression symptoms following traumatic brain injury. Psychological Medicine, 46: (5), 1079–1090. doi: 10.1017/S0033291715002640. |
16 | Ponsford, J. , Wong, D. , McKay, A. et al. ((2016) ). Depression and anxiety following traumatic brain injury: Can these high prevalence disorders be effectively treated using adapted cognitive behavioral therapy? Innovations and Future Directions in the Behavioural and Cognitive Therapies. 182: . |
17 | Schueller, S. M. , Kwasny, M. J. , Dear, B. F. , Titov, N. , Mohr, D. C. ((2015) ). Cut points on the Patient Health Questionnaire (PHQ-9) that predict response to cognitive–behavioral treatments for depression. General Hospital Psychiatry, 37: (5), 470–475. |
18 | Stiles-Shields, C. , Corden, M. E. , Kwasny, M. J. , Schueller, S. M. , Mohr, D. C. ((2015) ). Predictors of outcome for telephone and face-to-face administered cognitive behavioral therapy for depression. Psychol Med, 45: (15), 3205–3215. doi: 10.1017/S0033291715001208. |
19 | Tajan, N. , Devès, M. , Potier, R. ((2023) ). Tele-psychotherapy during the COVID-19 pandemic: a mini-review. Front Psychiatry, 14: , 1060961. doi: 10.3389/fpsyt.2023.1060961. PMID: 37476543; PMCID: PMC10354254 |
20 | Vrany, E. A. , Berntson, J. M. , Khambaty, T. , Stewart, J. C. ((2016) ). Depressive symptoms clusters and insulin resistance: race/ethnicity as a moderator in 2005–2010 NHANES data. Annals of Behavioral Medicine, 50: (1), 1–11. |
21 | Wolfe, L. F. , Sahni, A. S. , Attarian, H. ((2018) ). Sleep disorders in traumatic brain injury. NeuroRehabilitation, 43: (3), 257–266. |
22 | Zelencich, L. M. , Wong, D. , Kazantzis, N. , McKenzie, D. P. , Downing, M. , Ponsford, J. L. ((2020) ). Predictors of anxiety and depression symptom improvement in cbt adapted for traumatic brain injury: pre/post-injury and therapy process factors. Journal of the International Neuropsychological Society, 26: (1), 97–107. |




