A narrative review of the use of a cutting-edge virtual reality rehabilitation technology in neurological and neuropsychological rehabilitation
Abstract
BACKGROUND:
Virtual reality (VR) interventions have been increasingly used in the rehabilitation of a wide range of neurological and neuropsychological dysfunctions. Findings of previous reviews showed positive and promising effects of VR-based interventions. However, they summarized findings on VR-based intervention carried out through different VR systems and tasks.
OBJECTIVE:
We carried out a narrative review with the aim of qualitatively synthesising the results of previous studies that used specific VR systems, i.e. the Khymeia –Virtual Reality Rehabilitation System, for treatment purposes.
METHODS:
We searched the literature in various databases (i.e. EMBASE, Web of Science, SCOPUS, PubMed and PubMed Central) for studies published until November 23, 2023.
RESULTS:
30 studies were selected. The VRRS was used for neuromotor rehabilitation only in 13 studies, for cognitive rehabilitation in 11 studies, and for both neuromotor and cognitive rehabilitation in six studies. The study design was heterogeneous including 15 randomised controlled trials.
CONCLUSION:
After discussing each study according to the type of rehabilitation we concluded that the use and efficacy of VRRS rehabilitative intervention for increasing the neurological and neuropsychological functioning of patients are promising but more evidence is needed to make a comparison with conventional treatment. Future studies should also include long-term follow-up as well as cost-effectiveness analysis.
1Background
Virtual reality (VR) artificially simulates life-like environments providing a sensation of being inside an artificial world (Riva et al., 2020). It has been conceptualized as “an advanced form of human-computer interface that allows the user to interact with and become immersed in a computer-generated environment in a naturalistic fashion” (Rizzo et al., 2002; Schultheis & Rizzo, 2001). VR technology may be used as a tool for the study, assessment, diagnosis, and treatment of several neurological and neuropsychological disorders (Rizzo et al., 2002; Weiss et al., 2006). The use of VR makes it also possible to implement interventions of telerehabilitation (TR), i.e. an application of telemedicine that concerns the remote delivery of a variety of rehabilitative services through telecommunication technology (Piron et al., 2009).
VR-based treatment may provide several advantages compared with traditional rehabilitation methods in neurological and neuropsychological rehabilitation (Morganti, 2004; Rizzo et al., 2002; Schultheis & Rizzo, 2001). One assumption for its use in rehabilitation is that VR treatment provides multisensory feedback that could enhance the neural plasticity underlying neurological and neuropsychological recovery (Hao et al., 2021; Leonardi et al., 2021). In addition, skills learned during VR intervention might transfer or generalize to the real world (Schultheis & Rizzo, 2001; Wang & Reid, 2011).
As a consequence,VR interventions have been applied in the treatment of a wide range of neurological and neuropsychological dysfunctions associated with several conditions, such as neurodegenerative disease (Oliveira et al., 2021; Serino et al., 2017), cerebral palsy (Bryanton et al., 2006; Golomb et al., 2010; Park et al., 2021), stroke (Gamito et al., 2017; Kim et al., 2019; You et al., 2005), and neurodevelopmental disorders (Rodrigo-Yanguas et al., 2021; Wang & Reid, 2011; Zhao et al., 2021). Recently, several research groups synthesised the available evidence on the efficacy of VR-based intervention(s) for neurological and neuropsychological rehabilitation in different conditions, for example, in post-stroke (Maier et al., 2019; Rintala et al., 2019; Tchero et al., 2018), multiple sclerosis (Nascimento et al., 2021), and aphasia (Cacciante et al., 2021).
The available reviews and meta-analyses mainly summarized findings on VR-based intervention carried out through different VR systems (i.e., different hardware, software, and devices) and tasks. From both clinical and research perspectives, it is also essential to address the use and the efficacy of specific VR system. Thus, we carried out a narrative review with the aim of qualitatively synthesising the results of previous studies that used a specific virtual reality system: the Khymeia –Virtual Reality Rehabilitation System (VRRS). The VRRS allows the implementation (also via TR) of both neuropsychological and neurological rehabilitation treatments based on immersive or non-immersive virtual reality (for a detailed description of the K-VRRS see https://khymeia.com). The aim of this work was to review how the VRRS has been used in previous studies summarizing the features (e.g., tasks, duration) of the VRRS treatment as well as studies’ findings.
2Methods
The study design was specified as a non-systematic general narrative review on the applications of the VRRS for treatment purposes irrespective of study design. The narrative review was prepared in accordance to previous recommendations on standards for reporting of narrative reviews (Baethge et al., 2019; Byrne, 2016; Gasparyan et al., 2011; Green et al., 2006; Kable et al., 2012; Pautasso, 2013).
2.1Literature search
Initially, we searched EMBASE, Web of Science, SCOPUS, PubMed and PubMed Central for studies published until January 31, 2022 using the following keywords: Khymeia or VRRS or “virtual reality rehabilitation system”. Moreover, we searched for other potential references the following: bibliographies and citations of included studies, bibliographies of recent systematic-reviews and meta-analyses. Finally, other resources (i.e., Khymeia website, Google and Google Scholar) were searched for gray literature. No language restriction was applied. To ensure timeliness, we carried out an update of the literature search on November 23, 2023, using the same procedure specified above.
2.2Study selection and data extraction
Firstly, we examined the presence of possible duplicates in the obtained pool of records using Zotero 5.0 for Windows. Secondly, two investigators independently screened titles and abstracts. Subsequently, the same two investigators conducted the full-texts assessment. The screening occurred during February 2022. Any discrepancies were resolved by consensus and, if necessary, through arbitration by the lead investigator.
The eligibility criteria were single case and analytical studies that reported information on patients functioning assessed at both pre- and post-treatment and in which the VRRS was used as treatment intervention. We excluded review and studies in which the VRRS was not used for treatment (e.g., as a tool for the assessment of patients).
Two investigators performed the data extraction. A data extraction form was filled with all the relevant data, i.e., authors and year of publication, condition under treatment, study design, blinding procedure, total number of patients and their mean age in years, intervention aim, and treatment duration (with a focus on the VRRS).
2.3Outcomes
The VRRS provides both neuromotor and cognitive modules (and tasks) for rehabilitation. Consequently, the main outcome(s) of this review was to analyze the improvement in the neuromotor and cognitive domains. We focused on primary outcome(s) of each original study that the use of VRRS was intended to treat/improve and, specifically, on results of randomized controlled trials when available. For easy of reporting, we grouped studies according to the outcome for which the VRRS module was used. Further, we structured the presentation and discussion of the studies’ findings according to study design.
3Results
3.1Search results and included studies
The literature search yielded 456 records. After the removal of 201 duplicates, 255 titles and abstracts were screened. Then, 168 records were excluded and 87 full text were assessed for eligibility. Sixty-eight articles were further excluded because they did not address the VRRS or its use for treatment purposes. Nineteen studies were retained. After screening references of published review, included studies, and other resources two additional studies were retrieved. During the literature search update, nine additional studies were found endorsing criteria for inclusion out of a total of 81 records. A final number of 30 studies were retained. The study selection process is shown in Fig. 1 whereas the studies characteristics are summarized in Table 1 and other features of VRRS treatments, i.e., specific tasks when reported, in Table 2.
Fig. 1
Adapted PRISMA flow diagram from Page et al. (2021).
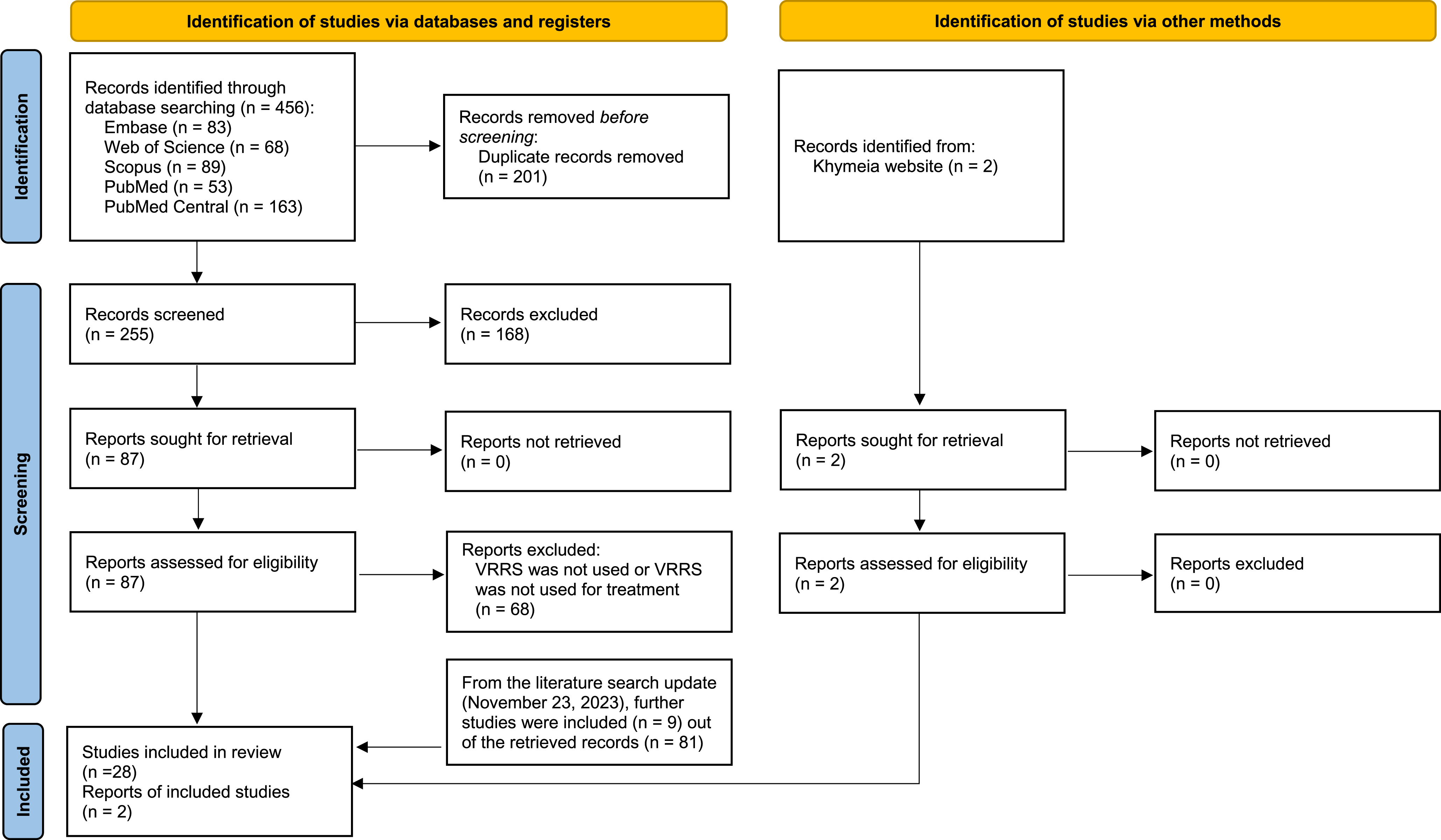
Table 1
Characteristics of included studies
| Study | Study design | Condition | Blinding | Total no. of patients | Mean age in years (SD) | Intervention aim | Duration |
| Neurological Rehabilitation | |||||||
| Chillura et al. 2020 | Case study | Intensive care unit acquired weakness | ns | 1 | 56 | Improvement of muscle strength, overall mobility, and disability burden | 360 h+daily sessions of VR for two months (additional information on VR sessions duration was not reported) |
| Luque-Moreno et al. 2016 | Case study | Poststroke hemiparesis | ns | 2 | 58 (participant 1), 49 (participant 2) | Lower extremity motor rehabilitation | 30 h VR+CT (15 h VR: 60 min x 5d x 3 w) |
| Menici et al. 2021 | Case study | Motor disorder | Rater-blinded | 1 | 17 | Postural control and balance improvement | 24 h (VR HomeKit: 30 min x 48 sessions in 12 w) |
| Contrada et al. 2022 | Uncontrolled trial | Poststroke | Rater-blinded | 19 | 61.1 (8.3) | Motor rehabilitation | 60 h (60 min x 5d x 12 w) |
| Maistrello et al. 2021 | Uncontrolled trial | Poststroke | ns | 50 | 63.62 (12.29) | Upper limb treatment | 20 h (60 min x 5d x 4 w) |
| Olivieri et al. 2013 | Uncontrolled trial | Hemiparesis | ns | 6 | 8.6 (4.5) | Upper limb rehabilitation | 15 h CT+VR (7.5 h VR: 45 min x 1d x 10 w) |
| Luque-Moreno et al. 2021 | Non-randomized controlled trial | Poststroke | Rater-blinded | 10 (VR+CT), 10 (CT) | 62.45 (12.01) | Re-education of the lower extremity | 30 h VR+CT (15 h VR: 60 min x 5d x 3 w), 30 h CT |
| Turolla et al. 2013 | Non-randomized controlled trial | Poststroke | Rater-blinded | 263 (VR+CT), 113 (CT) | 60.2 (14.3) (VR+CT), 65.4 (12.5) (CT) | Upper limb rehabilitation | 40 h VR+CT (20 h VR: 60 min x 5d x 4 w), 40 h CT |
| Fascio et al. 2022 | Randomized controlled trial | Total knee arthroplasty | Rater-blinded | 21 (VR telerehabilitation), 22 (CT) | 61.5 (6.21) (VR), 60.9 (7.52) (CT) | Improving functional outcomes after surgery | ns |
| Gianola et al. 2020 | Randomized controlled trial | Total knee arthroplasty | Rater-blinded | 35 (VR), 39 (CT) | 68.6 (8.8) | Improving functional outcomes after surgery | 5 h (60 min x 5d) |
| Kiper et al. 2011 | Randomized controlled trial | Poststroke | ns | 40 (VR+CT), 40 (CT) | 64 (16.4) | Upper extremity rehabilitation | 40 h VR+CT (20 h VR: 60 min x 5d x 4 w), 40 h CT |
| Kiper et al. 2014 | Randomized controlled trial | Poststroke | Single-blind | 23 (VR+CT), 21 (CT) | 64.3 (12.6) | Upper limb rehabilitation | 40 h VR+CT (20 h VR: 60 min x 5d x 4 w), 40 h CT |
| Piron et al. 2009 | Randomized controlled trial | Poststroke | Rater-blinded | 18 (VR telerehabilitation), 18 (CT) | 65.2 (7.8) | Upper extremity rehabilitation | 20 h (60 min x 5d x 4 w) |
| Neuropsychological Rehabilitation | |||||||
| Emedoli et al. 2021 | Case study | Buccofacial apraxia | ns | 1 | 58 | Treatment of apraxia | 15 h (60 min x 5d x 3 w) |
| Tartamella et al. 2020 | Case study | Brainstem radionecrosis | ns | 1 | 57 | Cognitive rehabilitation | 240 h (24 h VR: 30 min x 6d x 8 w) |
| Maresca et al. 2020 | Uncontrolled trial | Myotonic dystrophy type 1 | Not blinded | 11 | 38.4 (15) | Cognitive rehabilitation | 80 h CT+VR (40 h VR: 1 h x 5d x 8 w) |
| Torrisi et al. 2019 | Quasi-randomized controlled trial | Poststroke | Rater-blinded | 20 (VR+telerehabilitation), 20 (CT) | 55.17 (18.37) | Cognitive rehabilitation | 60 h (VR+telerehabilitation vs CT+CT: 50 min x 3d x 12 w+50 min x 3d x 12 w) |
| Cappadona et al. 2023 | Randomized controlled trial | Developmental language disorder | Rater-blinded | 16 (VR), 16 (CT) | 4.8 (1.1) | Speech therapy | 48 h (60 min x 2d x 24 w) |
| Maresca et al. 2022 | Randomized controlled trial | Dyslexia | Rater-blinded | 14 (VR), 14 (CG) | 10.3 (2) | Improvement of reading, writing, and cognitive level | 72 h (60 min x 3d x 24 w) |
| De Luca et al. 2022b | Randomized controlled trial | Traumatic brain injury | Rater-blinded | 15 (VR), 15 (CT) | 43.53 (16.04) | Attention rehabilitation | 24 h (60 min x 3d x 8 w) |
| De Luca et al. 2023 | Randomized controlled trial | Traumatic brain injury | Rater-blinded | 10 (VR), 10 (CT) | 44.6 (16.13) | Executive functions | 24 h (60 min x 3d x 8 w) |
| Leonardi et al. 2021 | Randomized controlled trial | Multiple sclerosis | ns | 15 (VR), 15 (CT) | 54.6 (1) | Cognitive rehabilitation | 18 h (45 min X 3d x 8 w) |
| Manenti et al. 2020 | Randomized controlled trial | Mild cognitive impairment | Rater- and researcher-blinded | 18 (VR+telerehabilitation), 14 (VR+unstructured), 10 (CT) | 76.5 (4.2) | Cognitive rehabilitation | 48 h VR+telerehabilitation (60 min x 12d in 4 w+60 min x 3d x 12 w); 48 h VR+unstructured (60 min x 3d in 12 w+60 min x 3d x 12 w); 12 CT (60 min x 3d x 4 w) |
| Maresca et al. 2019 | Randomized controlled trial | Poststroke aphasia | ns | 15 (VR+telerehabilitation), 15 (CT+territorial services) | 51.2 (11.3) | Aphasia rehabilitation | 100 h (VR+telerehabilitation vs CT+territorial service: 50 min x 5d x 12 w+50 min x 5d x 12 w) |
| Neuropsychological and Neurological Rehabilitation | |||||||
| De Luca et al. 2022a | Case study | Nasu-Hakola disease | Rater-blinded | 1 | 41 | Treatment of cognitive, behavioral, and motor symptoms | 288 h (72 h VR physical/motor and cognitive modules: 60 min x 3d x 12 w+60 min x 3d x 12 w) |
| Maresca et al. 2018 | Case study | Spinal cord injury with moderate tetraparesis | Rater-blinded | 1 | 60 | Treatment of cognitive and behavioral alterations | 336 h (72 h VR cognitive and sensory-motor modules: 60 min x 3d x 12 w+60 min x 3d x 12 w) |
| Alemanno et al. 2019 | Uncontrolled trial | Chronic low back pain | ns | 20 | 47.5 (15.3) | Treatment of chronic low-back pain | 12 h (60 min x 12d in 4/6 w) |
| Calabrò et al. 2023 | Multicenter randomized controlled trial | Severe acquired brain injury | Rater-blinded | 20 (VR) 20 (CT) | 48.12 (16.84) | Motor and cognitive rehabilitation | 60 h (60 min x 5d x 12 w) |
| Goffredo et al. 2023 | Randomized controlled trial | Multiple sclerosis and Parkinson’s disease | Rater-blinded | 65 (VR), 67 (CT) | 58.12 (12.43) (VR), 61.12 (11.06) (CT) | Motor and cognitive rehabilitation | 22.5–30 h (45 min x 5d x 6–8 w) |
| Pagliari et al. 2021 | Randomized controlled trial | Multiple sclerosis | Rater-blinded | 35 (VR), 35 (CT) | 48.33 (9.66) (VR), 52.23 (9.34) (CT) | Motor and cognitive rehabilitation | 22.5 h (45 min x 5d x 6 w) |
Note. Randomization was considered “present” if the authors of the study specified the randomization procedure. VR: virtual reality treatment, CT: conventional therapy, w: weeks, d: days, h: hours, m: minutes, na: not applicable, ns: not specified.
Table 2
Features of VRRS treatments (i.e., specific tasks)
| Study | Condition | VRRS treatment |
| Neurological Rehabilitation | ||
| Olivieri et al. 2013 | Hemiparesis | Exercises administered to improve reaching and tracking movements of the paretic arm included: grasping objects and stacking them up according to a specific sequence, moving objects according to a reference trajectory or in different directions, hitting a frog appearing in random places on the screen, grasping a quickly moving fish on the screen, and tiding up a sort of virtual bedroom. (pp. 2-3) |
| Chillura et al. 2020 | Intensive care unit acquired weakness | The virtual reality rehabilitation system Evo workstation was equipped with a high-resolution LCD projector displaying the virtual scenarios on a large wall screen and a stabilometric and a proprioceptive/dynamic platform was used. Virtual sensory-motor tasks aimed at stimulating muscle strength, joint range of movement, posture stability, balance reactions, and pelvis movements were performed. Each session consisted of different types of motor tasks, including manipulating objects while interacting with a virtual scenario, static balance training, supine mobilization, assisted and active exercises for trunk control and balance in a sitting position, exercises for weight shift and stepping in static and dynamic equilibrium using a stabilometric and a proprioceptive/dynamic platform. (p. 3) |
| Menici et al. 2021 | Motor disorder | The patient performed the exercises standing on the balance board. The training exercises included postural tasks, starting from unidirectional load shifts up to moving in all directions and three-dimensional environments. The therapists selected exercises that remained unchanged throughout the entire training period (i.e., “Reaching points” exercise where the patient had to move her COP to reach one target along a visible path on the screen), while others (i.e., “Reaching” exercise where the patient had to reach an increased number of targets, placed around her COP in different directions, trying to take the most direct path possible) were modified periodically. (p. 3) |
| Contrada et al. 2022 | Poststroke | The intervention was performed via the TR (online and offline) modality. Exercises were tailored to the clinical status of stroke patients. In the article, the authors described VRRS exercises in general rather than specifying the ones that were administered as follows: the software contains specific exercises for the trunk (flexion and extension, rotation, lateral inclination, and dorsal mobilization), for the singular right or left upper limb (shoulder adduction and abduction, shoulder flexion and extension, shoulder intra- and extra rotation, elbow flexion and extension, and forearm pronation and supination), and for singular (hip abduction, adduction, flexion and extension, knee flexion and extension, and ankle flexion and extension) or both lower limbs (squats, get up on the tips, and march on the spot). Other exercises, namely, “functional exercises” reproduced activities of daily living (ADLs) such as ironing, opening a jar, and bringing a glass to the mouth. (p. 3) |
| Kiper et al. 2014 | Poststroke | During the virtual reality treatment, the subject was seated in front of the wall screen grasping a sensorized real object (i.e., ball, disc, or glass) with the paretic hand; in case of severe impairment of grasping the sensor was fixed to a glove worn by the patient. The real object, held by the subject, was matched to the virtual object displayed on the wall screen through an electromagnetic sensor placed onto the dorsal face of the hand (i.e., end-effector). The therapist created the virtual scenarios consisting of a sequence of motor tasks that the patient was asked to perform on his workstation during the therapy session. (p. 2) |
| Kiper et al. 2011 | Poststroke | During the virtual therapy, the subject was seated in front of the wall screen grasping a sensorized real object with the affected hand. If the grasp was not possible the sensors were fixed on a glove worn by the patient. The patient moved the real object (envelope, carafe, hammer) following the trajectory of the corresponding virtual object displayed on the computer screen under the requested virtual task. Virtual tasks consisted mainly of simple movements, e.g., pouring water from a glass, using a hammer, turning around the center of a doughnut, etc. (p. 438) |
| Luque-Moreno et al. 2021 | Poststroke | Different types of motor tasks in which the patient had real objects as references (staircase steps, objects in high places, signs on the floor, etc.). The proprioceptive activity was also performed. The virtual scenario showed the correct movement trajectory of the foot climbing up the staircase step (red), previously recorded by the physiotherapist. Thus, the patient was asked to emulate (yellow) the correct movement trajectory shown on the screen, facilitating the perception of the patient and the correction of his/her movement errors through auditory/visual feedback, both during the realization of the task and once it was finished, to visualize the obtained results (feedback of the performance and outcomes, respectively). The physiotherapist selected the characteristics and complexity of the motor tasks, modified the parameters of the software related to feedback (types of objects, trajectories, sounds, etc.), and applied a progression of difficulty based on the individual capacities of each patient. (p. 5) |
| Maistrello et al. 2021 | Poststroke | Subjects executed seven standardized motor tasks including shoulder flexion–extension, abduction–adduction, internal–external rotation, circumduction, elbow flexion–extension, forearm pronation–supination, and hand–digit motion. (p. 4) |
| Piron et al. 2009 | Poststroke | Five virtual tasks, comprising simple arm movements, were devised for training the patient’s left or right arm deficits. During the rehabilitation session, the patient moved the real object following the trajectory of the corresponding virtual object displayed on the computer screen under the requested virtual task. (p. 1017) |
| Turolla et al. 2013 | Poststroke | Therapy involved performing different kinds of motor tasks during which the patient was required to emulate the correct movement trajectory displayed in the background of the virtual scene. (p. 3) |
| Luque-Moreno et al. 2016 | Poststroke hemiparesis | The equipment included a high-resolution LCD projector which displayed the virtual scenarios on a large wall screen and a computer workstation connected to a 3D motion-tracking system (Polhemus FASTRAK® 3Space, Vermont, USA). The subject was asked to perform different tasks, for example, moving virtual objects following specific trajectories or using the healthy foot to reach reference points on the ground to work on the proprioception of the supporting plegic foot. (p. 90) |
| Fascio et al. 2022 | Total knee arthroplasty | The core exercise program involved active mobilization of the operated hip in the sagittal plane avoiding rotation and extension, strengthening of gluteal and tight muscles, and load and balance management (p. 3). Exercises are reported in detail in Table 1 of the original article. (p. 4) |
| Gianola et al. 2020 | Total knee arthroplasty | First three sessions: knee extension; ball compression, knee flexed; hip abduction on one side; active flexion-extension on the bed; hip flexion with the knee extended; gluteal bridge exercise; active knee extension; active triple flexion; supine target proprioception. After the first three sessions (from the fourth to discharge on day 10): hip flexion with knee extended; in sitting position, active knee flexion and extension; in standing, active bilateral squat; in standing position, hip extension; in standing position, knee flexion; in standing position, active hip abduction; in standing position, proprioception; standing on the balance board, target proprioception; balance between lower extremity limbs; reaching targets by lower extremity limbs. (supplementary material) |
| Neuropsychological Rehabilitation | ||
| Emedoli et al. 2021 | Buccofacial apraxia | During the first 20 minutes, the subject paid specific attention to video sequences of facial movements (smile, kiss, lateral angle of mouth displacement, raise eyebrows, and wrinkle forehead). During the other 40 minutes of treatment. The participant performed voluntary facial movements with augmented feedback, consisting of the reflection of avatar movements projected on a virtual reality screen. (p. 3) |
| Tartamella et al. 2020 | Brainstem radionecrosis | A series of exercises involving attention, memory (verbal and visuospatial), spatial cognition, ocular-manual coordination, gnosis abilities, problem-solving, executive function, and constructive praxis were included. (p. 3) |
| Cappadona et al. 2023 | Developmental language disorder | VRRS tasks were the same for all children, but the difficulty and duration varied according to the needs and goals to be achieved. Different language domains (i.e., comprehension, repetition, denomination, verbal production) were treated via several exercises, such as: recognizing the object among the images depicted (to intervene in comprehension), repeating the words represented in a period of a few seconds (to intervene on repetition), name the images depicted in a period of a few seconds (to intervene on denomination), and write the completed sentence in the video (to intervene on Verbal Production). (p. 4) |
| Maresca et al. 2022 | Dyslexia | The VRRS cognitive module used consists of a wide range of rehabilitative activities. All activities are organized to stimulate the different cognitive domains: memory, attention, language, spatial–temporal orientation, executive functions, calculation, and practice. (p. 4) |
| Manenti et al. 2020 | Mild cognitive impairment | Face-to-face cognitive VRRS treatment included twelve exercises designed to enhance memory, visuospatial abilities, attention, and executive functions. Memory exercises: safe opening –forward (list of numbers), visual memory (geometric shapes or animals’ cards), safe opening- backward (sequence of numbers in the reverse order), verbal memory (list of words). Attention and Executive functions: complete the sequence of shapes, change colour, and rotation, and complete the logical relationship. Visuospatial abilities: spatial orientation, road route, finding the symmetrical, recognizing farm animals.Home-Based Cognitive VRRS Treatment (VRRSHomeKit) included twelve exercises designed to enhance memory, visuospatial abilities, attention, and executive functions, different from those used in face-to-face VRRS training. Memory: recognize banknotes and coins, collect money up to 10 euros, recognize banknotes and coins –back, collect money up to 100 euros. Attention and Executive functions: change of shape, find the missing Cuisenaire rod, change all, and complete the sequence following the rule. Visuospatial abilities: spatial orientation- front or rear, indicates the rotation, puzzle, and connections of points. (pp. 5-6) |
| Leonardi et al. 2021 | Multiple sclerosis | The cognitive rehabilitative program using the VRRS included attention (immediate and recall feedback exercises), memory (remembering previously observed objects), and executive and visuospatial functions (movements finalized to virtual touch, objects manipulation, realization of specific associations) training. (p. 3) |
| Torrisi et al. 2019 | Poststroke | The exercises performed by the patients included reasoning and executive tasks (movements finalized to virtual- interactive touch, to move or manipulate specific objects, in different directions of the virtual space; or to realize specific associations), memory tasks (elements observation and recall; fluency exercises, semantic associations and access to vocabulary) and attention processes and spatial cognition tasks (elements selection/exploration, with an immediate and recall feedback). (pp. 346-347) |
| Maresca et al. 2019 | Poststroke aphasia | The VRRS was used for the following linguistic exercise: compose the word- acoustic, textual, and virtual item; compose the complex words; rewrite the word- acoustic, textual, visual item; write the word- acoustic, textual, visual item; complete the logical relation; match the coloured stick to the number; collect the money up to 1, 10, 100, and 1000. (p. 4) |
| De Luca et al. 2022b | Traumatic brain injury | The Virtual Reality Based-Attention Processes Training involved several exercises concerning (1) sustained attention, (2) selective attention, (3) alternating attention, and (4) divided attention. For example, 1) scanning the entire screen to locate target symbols (to act on selective attention); 2) observing from 3 to 5 targets-stimuli for a variable and progressive time (10–15 min), with an attentional focus on virtual tasks (to act on sustained attention); 3) double task such as selecting/associating the colour to the shape and at the same time eliminating the different shapes/virtual stimuli (to act on divided attention); 4) specific virtual activities, involving the mental flexibility for moving between tasks with different cognitive requirements, which use computer games/software dedicated (such as to make simple sequences of animals, fruit, objects-colours-pictures). (p. 5) |
| De Luca et al. 2023 | Traumatic brain injury | To promote the recovery of executive functioning, the psychiatric therapist asks the patients to realize specific activities to stimulate categorization skills, semantic and phonemic categorization; activities planning and logical association; tasks of analogical reasoning using a pc-based approach, and virtual 2D and 3D activities. To promote coping strategies and problem-solving, the therapist invited the patients to build sequential logical sequences using virtual game cards with colourful images representing animals, money, and objects and to order them according to variable criteria. The therapist asked the patients to find a solution to a problem of daily life using a virtual tool. (pp. 4-8 and Table 3) |
| Neuropsychological and Neurological Rehabilitation | ||
| Alemanno et al. 2019 | Chronic low back pain | Patients underwent a series of exercises consisting mainly of trunk rotation, flexion, and extension realized in various positions (standing, sitting, and kneeling). (p. 5) |
| Pagliari et al. 2021 | Multiple sclerosis | The VRRSHomeKit was used. The treatment included motor and cognitive rehabilitation activities. Each session was planned by alternating 30 minutes of motor activities and 15 minutes of cognitive activities. The motor section included ten motor tasks of not less than 3 minutes, and they were aimed at training the trunk and both upper and lower limbs (example of exercises: trunk catching forward, inclination right and left, reaching rotation right and left, right/left hip catching, right/left knee extension, right/left hip abduction reaching, march in place). In the cognitive section, the tasks were selected to enhance visuospatial abilities, attention, memory, and executive functions (examples of exercises: memorization of a list of words or numbers, indication of the rotation, and puzzle completion). (p. 3 and appendix 1) |
| Goffredo et al. 2023 | Multiple sclerosis and Parkinson’s disease | The motor exercises were performed using inertial sensors for the acquisition and processing of the movement performed by the patient. These data were shown to the patient with visual and auditory feedback in a serious game environment. The exercises covered the rehabilitation of balance and lower limbs (e.g., maintaining balance on one leg, marching in place, standing on tiptoe, squatting, etc.). (p. 3) |
| De Luca et al. 2022a | Nasu-Hokola disease | The VRRS cognitive training involved tasks that stimulate specific domains such as orientation (personal, temporal, spatial orientation), memory and attention processes, and verbal and not executive functions. The VRRS motor program included specific tasks to stimulate muscle strengthening, strengthen leg tendons and ligaments, improve posture, pelvis movements, and balance reactions. |
| Calabrò et al. 2023 | Severe acquired brain injury | The VRRSHomeKit was used. The motor program included exercises concerning Eye-hand coordination (visual achievement of coloured targets (e.g., balls, machines, asteroids) to select or collect them by moving the upper limbs using a K-wand sensor), Trunk control (sitting activities with latero-lateral and anteroposterior movements of the trunk and standing activities with the support of the caregiver), and Bimanual coordination (exercises for carrying out bimanual coordination activities are based on trying to catch targets in motion and all directions). Cognitive treatment included several exercises that stimulated selective attention (selecting and immediately recalling the same feedback of various elements observed in the virtual environment), sustained attention (the patient observes 3–5 target stimuli for a variable and progressive amount of time, with an attentional focus on the virtual task), memory (the patient is asked to observe at first particular elements and then (in the immediate and recall time) to remember those (e.g., eggs, seasons, colours, balls, numbers, environments, animals, geometric forms or not, fruits, jobs) with a dynamic interaction in a semi-immersive virtual environment (using sprites tasks). The patient must remember the place (the position; visuospatial memory) and name (verbal information) of the element observed), and visuospatial skills (the goal is to process visual stimuli to comprehend spatial relationships between virtual objects and to visualize different virtual scenarios or computer-based images, to record and recover information needed to plan a course to a location, and to recall the virtual location/position of an object or the occurrence of an event). (pp. 6-7 and Tables 4 and 5) |
| Maresca et al. 2018 | Spinal cord injury with moderate tetraparesis | The cognitive exercises included reality orientation, attention process (selection of elements with immediate and recall feedback), memory, and problem-solving training, whereas sensory-motor exercises included trunk control training, static and dynamic balance, symmetrical load, and weight shifting. In the first training phase, the therapist used the stabilometric platform to increase the static balance. Supine mobilization and assisted and free exercises for trunk control and balance in a sitting position, along with exercises with weight shift and walking, were carried out. At a later stage, the therapist used a proprioceptive/dynamic platform, characterized by greater instability and greater executive difficulty, with training of the trunk control, in static and dynamic equilibrium and weight displacement. (pp. 3-5) |
Note. We report intervention and/or exercise descriptions provided in the original study. We had no access to the supplementary material from Maresca et al. (2020) that describes VRRS exercises.
The VRRS was used for neuromotor rehabilitation in 13 studies, for cognitive rehabilitation in 11 studies, and for both neuromotor and cognitive rehabilitation in six studies. Of all 30 studies, seven were single case reports, five uncontrolled trials, two non-randomised controlled trials, one quasi-randomised controlled trial, and 15 randomised controlled trials.
3.2Neurological rehabilitation
The VRRS was used for neuromotor rehabilitation in 19 studies: five case reports, four uncontrolled trials, two non-randomised controlled trials, and eight randomised controlled trials.
3.2.1Nonexperimental design
Several studies examined whether neuromotor recovery may take advantage from adding VRRS training to standard treatments. Some case reports suggested the possibility of using the VRRS in combination with physiotherapy and/or other treatment to improve motor functions (Chillura et al., 2020; Luque-Moreno et al., 2016; Maresca et al., 2018). Luque-Moreno and colleagues (Luque-Moreno et al., 2016) described the use of the VRRS in addition to conventional physiotherapy programs in the treatment of post-stroke gait disorders in two patients. Menici and colleagues (Menici et al., 2021) reported on the VRRS based motor intervention via TR to improve posture and balance abilities in a 17-years-old female with a diagnosis of myopathy and moderate intellectual disability. Whereas Maresca et al. (2018) used both the VRRS based neuromotor and cognitive trainings to improve motor and cognitive functioning of a 60-years-old man with spinal cord injury showing good outcomes overall. Chillura et al. (2020) have described an intensive neuro-rehabilitation program lasting 6 months, carried out under hospitalization, aimed at the improving motor and muscle deficits in a patient with intensive care unit acquired weakness. The authors (Chillura et al., 2020) stressed that combining different rehabilitation strategy including conventional treatment (i.e. physiotherapy and occupational therapy), robotic-aided training, and sessions of neuromotor training based on VRRS, could provide more advantages than conventional treatment alone in improving motor functions. De Luca et al. (2022a) reported an improvement in head and trunk control in a patient with Nasu-Hakola disease (i.e., a rare neurodegenerative disorder) after a multimodal treatment including both VRRS and standard physiotherapy.
With respect to uncontrolled studies, Olivieri et al. (2013) showed a reduction of upper limb motor impairment in a group of children with congenital hemiplegia after traditional physiotherapy and VRRS interventions. Alemanno et al. (2019) conducted a 6 week-neurorehabilitative treatment using the VRRS with patients with chronic low-back pain. The treatment consisted on teaching patients to execute correct movements with the painful body part in order to reduce pain and to regain a correct body image. The results of the study showed a significant reduction in pain and improvement in quality of life. Another study (Maistrello et al., 2021) showed that, concomitantly to the use of the VRRS, post-stroke patients’ motor impairment of upper extremities improved. Finally, Contrada et al. (2022) assessed motor recovery after a TR intervention performed using VRRS in a group of chronic post-stroke patients. The authors found an improvement in motor functions of the upper paretic limb whereas no pre- post-difference was found in motor functions of the lower paretic limb.
All these findings certainly encourage further studies testing the efficacy of VRRS in neurological and neuromotor rehabilitation. Despite promising, as generally noted by the authors, evidence arise from single case and single group pre-and post-test research designs. As a consequence, findings suffer from low internal validity due to absence of comparison groups and implementation of other treatments in the original studies. For example, Olivieri and colleagues (2013) stressed that their study doesn’t provide evidence that the VRRS alone improves motor functions in children since physiotherapy was also provided. The authors highlighted the need of randomized controlled studies to adequately test the efficacy of VRRS based motor treatment.
3.2.2Experimental design
Besides case reports and single-arm studies discussed above, ten studies adopted a controlled experimental approach with eight of these studies using randomization procedures. Four studies (Kiper et al., 2011, 2014; Luque-Moreno et al., 2021; Turolla et al., 2013) compared the VRRS based motor training, combined with conventional treatment (e.g., physiotherapy), with conventional treatment alone in improving motor impairment of upper or lower extremities in post-stroke patients. All these studies used the Fugl-Meyer Upper/Lower Extremity (FM) and the Functional Independence Measure (FIM) scales as outcome measures. Overall, these studies demonstrated that combined treatment (i.e., VRRS based training combined with conventional treatment) was associated with a larger improvement in motor functioning compared to the conventional treatment alone. In another randomized controlled trial, the efficacy of the VRRS based motor training and traditional rehabilitation (i.e., physiotherapy) in reducing pain intensity and knee disability, and improving quality of life, FIM scores and others measures, in patients with knee osteoarthritis after undergone orthopaedic surgery were tested (Gianola et al., 2020). The authors showed that the VRRS treatment was not superior to traditional rehabilitation in terms of pain relief and other functional outcomes. However, they concluded that it seems to improve the global proprioception despite this outcome was measured only after treatment and, as such, the difference could have been due to baseline differences between groups rather than to treatment itself.
Five studies evaluated the efficacy of VRRS based motor training deliver via TR. Like findings from Gianola et al. (2020), Fascio et al. (2022) found no difference between TR and traditional rehabilitation interventions for hip disability and functional independence in patients who underwent total hip arthroplasty. A multicenter randomized controlled study did not find any statistical differences in motor outcome between a group of patients with severe acquired brain injury that underwent a VRRS motor treatment delivered via TR and a group of patients with severe acquired brain injury that underwent a conventional face-to-face motor treatment performed at patients’ homes (Calabrò et al., 2023). Rather, both groups of patients showed improvements in global functional status and gross motor functions whereas no difference between baseline and follow-up measurements were noted for spasticity (Calabrò et al., 2023).
Piron et al. (2009) examined improvement in motor impairment of upper limb directly comparing VRRS based motor training delivered via TR, with conventional treatment, in post-stroke patients. The authors demonstrated significant improvement (as measured by FM and Ashworth Assessment Scale) in both groups. However, the VRRS treatment via TR group showed a higher score at the FM compared with that of the control group. Pagliari et al. (2021) showed that VRRS based motor training delivered via TR was more effective than conventional treatment carried out at home in improving balance (as measured by the Mini-BES Test) whereas no difference between interventions was demonstrated for unilateral gross manual dexterity (as measured by the Box and Block Test) in patients with multiple sclerosis. Finally, Goffredo et al. (2023) showed that VRRS treatment via TR improves static and dynamic balance and gait (as measured by the Mini-BES Test) more compared to at-home treatment without the use of any technological devices in patients with multiple sclerosis and Parkinson’s disease.
3.3Neuropsychological rehabilitation
The VRRS was used for neuropsychological rehabilitation in 17 studies: four case reports, two uncontrolled trials, one quasi-randomised controlled trial, and ten randomised controlled trials.
3.3.1Non-experimental design
Regarding case reports, no improvement in cognitive impairment (as indicated by a reliable change index equal to 1.3) after two months of VRRS based cognitive training was observed in an adult patient with neurocognitive and motor dysfunctions due to brain alterations linked to brain-stem radionecrosis (Tartamella et al., 2020). Similarly, no improvement in global cognition and executive functions was observed in a patient with neurodegenerative disease after VRRS training (De Luca et al., 2022a).
Maresca et al. (2018) reported improvement in general cognitive status, attention process and prefrontal cortex related executive functioning of a patient with spinal cord injury that underwent combined treatment including both standard treatment (i.e., psychological counselling, standard cognitive training, and physiotherapy) and VRRS cognitive training. Emedoli et al. (2021) implemented the “Action Observation Therapy” (AOT) via VRRS for the rehabilitation of buccofacial apraxia in an adult patient that underwent a neurosurgery resection of a right frontoparietal atypical meningioma. AOT is a relatively new rehabilitation approach that exploits mirror neuron mechanisms to treat neuromotor disorders (Buccino, 2014; De Stefani et al., 2021; Ertelt et al., 2007; Sgandurra et al., 2013). The patient was required to observe and subsequently reproduce different voluntary facial movements of an avatar projected on the VRRS. After the treatment, the patient showed an improvement in the quality and range of voluntary facial movements and gestures. This case report suggests that the application of AOT through VRRS could be a promising application of VRRS in the rehabilitation of buccofacial apraxia. Clearly, randomized controlled studies are needed to show the efficacy of AOT in combination with VRRS in the recovery of buccofacial apraxia.
Three single-arm studies were conducted with samples of patients with chronic low back pain (Alemanno et al., 2018, 2019) and myotonic dystrophy type 1 (Maresca et al., 2020). In patients with chronic low back pain, pain and cognitive functions improved during the VRRS based cognitive training (Alemanno et al., 2018, 2019). Similarly, patients with myotonic dystrophy type 1 showed improvement in neuropsychological functioning (Maresca et al., 2020). However, the absence of a control group is a relevant limitation of these studies since observed changes may be related to factors other than the VRRS treatment.
3.3.2Experimental design
Eleven studies adopted a controlled experimental design with ten of these studies using randomization procedures. Two studies (Maresca et al., 2019; Torrisi et al., 2019) involved samples of post-stroke patients. Torrisi et al. (2019) evaluated the efficacy of VRRS cognitive training based on improving neuropsychological functions (including attention, memory, executive functions, and language skills) in post-stroke patients. The study lasted six months and included two phases: during the first one VRRS and standard cognitive treatments, respectively, were carried out at a rehabilitation centre; during the second phase the experimental group was treated with VRRS via TR modality, whereas the control group continued the traditional (paper and pencil) training at home. Before and after each phase, all participants underwent an extensive neuropsychological assessment. The authors observed significant improvement in the global cognitive level, as well as in the attentive, memory and linguistic skills in the VRRS. Moreover, significant differences between the VRRS group and the control group were shown in phonemic fluency, and learning and memory functioning, favouring the VRRS group only after the second phase (VRRS via TR) of the study. In another study, Maresca et al. (2019) investigated the efficacy of a linguistic treatment performed using VRRS and traditional linguistic treatment to treat language deficit in post-stroke patients with aphasia. The study lasted six months and included two phases: during the first one (implemented during hospitalization), the experimental group underwent linguistic treatment performed using VRRS, while the control group underwent the conventional speech therapy based on the same exercises as the experimental group, but using paper-pencil tools. In the second phase of the study, the experimental group continued linguistic treatment by means of VRRS via TR, while the control group continued the conventional speech therapy, which were provided by territorial services. The patients underwent an expansive neuropsychological assessment to assess several language skills, including naming, comprehension, repetition, reading, and calculation. The authors reported no between groups difference in comprehension, reading and calculation at baseline whereas at the end of the study (at the end of the TR) there were significant differences favouring the VRRS group. No differences were shown in repetition and naming.
The VRRS was used to improve language functions also in children with developmental language disorders (Cappadonna et al., 2023). The control group underwent conventional speech therapy, while the experimental group underwent a speech therapy program implemented via VRRS. Both groups improved in language functions after treatment. However, despite the authors stressed that the experimental group showed larger improvements compared to the control group, direct statistical comparisons between the two groups were not performed.
The VRRS was also used with children with dyslexia (Maresca et al., 2022). Maresca et al. (2022) found that VRRS cognitive intervention improved word-reading, homophonic writing and some index of the Wechsler Intelligence Scale for Children-IV (i.e., Full Scale IQ, Perceptual Reasoning Index, and Processing Speed Index) compared to conventional neuropsychological treatment in children with dyslexia.
Three studies, conducted from the same research group, involved patients with acquired/traumatic brain injury. De Luca and collaborators (De Luca et al., 2022b) showed that a neuropsychological attention training (i.e., Attention Process Training) implemented through VRRS is more effective than the same treatment based on paper and pencil exercises in improving attentive processes in patients with traumatic brain injury. In a further study, De Luca et al. (2023) evaluated the efficacy of VRRS cognitive training in improving executive functions of patients with traumatic brain injury. The experimental group underwent VRRS training for executive functions while the control group was provided with a conventional cognitive treatment. Comparing pre- and post-treatments scores, both the experimental and the control group improved. However, between-group post-treatment analysis showed significant differences only in some but not all measure of executive functions. Additionally, a multicenter study evaluated the efficacy of the VRRS based cognitive training implemented via TR in improving global cognitive functioning and executive functions in patients with severe acquire brain injury (Calabrò et al., 2023). Neuropsychological effects of the VRRS based treatment implemented via TR were compared with those of the conventional treatment performed at patients’ homes by a physiotherapist or a speech therapist. Again, between-group statistical analysis did not indicate any difference in cognitive outcomes between patients that underwent VRRS based treatment implemented via TR and patients that underwent the conventional treatment. Regarding these three studies with patients with acquired/traumatic brain injury, it is not clear whether they analysed independent data (participants were included only in one study) or dependent data (participants were included in more than one study).
Manenti et al. (2020) conducted a multicenter rater-blinded, controlled and randomized study to evaluate the efficacy of the VRRS based cognitive treatment compared to usual care treatment in enhancing cognitive functioning in patients with mild cognitive impairment. This study also tested the hypothesis that continuing the VRRS based cognitive treatment at home via TR may induce maintenance of the cognitive benefits obtained. Participants were assigned to one of three groups: 1) face to face cognitive VRRS treatment followed by VRRS via TR; 2) face to face cognitive VRRS treatment followed by at-home unstructured cognitive stimulation; and 3) those who received several conventional treatments in the clinical setting (e.g., reminiscence therapy and paper and pencil exercise) followed from no other treatment at home. The primary outcome was verbal episodic memory as measured by two different tasks (i.e., Free and Cued Selective Reminding Test and Rey Auditory Verbal Learning Test). Further, all participants underwent an extensive neuropsychological evaluation to assess other cognitive domains (i.e., language, attention, and visuoconstructional skills). Comparing the effects of face to face cognitive VRRS treatment with the conventional treatment on measures of verbal episodic memory (primary outcome) in the clinical setting, the authors showed that the VRRS treatment was more effective than the conventional treatment in improving some (but not all) sub-scores of verbal episodic memory as measure by the Free and Cued Selective Reminding Test, whereas no difference between treatments were observed for other measures of memory (i.e. Rey Auditory Verbal Learning Test). In addition, the VRRS treatment outperformed the conventional one on some secondary outcome measures (i.e., verbal fluency and visuoconstructional functions) whereas no between group difference was observed for others. Overall, these results support the efficacy of face-to-face VRRS treatment. Considering outcome measures at follow-up (after home treatment), overall the authors showed that cognitive VRRS-TR has comparable effects to the conventional rehabilitation treatment.
Two other studies (Leonardi et al., 2021; Pagliari et al., 2021) involved samples of patients with multiple sclerosis and compared the efficacy of conventional treatment rehabilitation with the VRRS rehabilitation in the clinical setting (Leonardi et al., 2021) and via TR (Pagliari et al., 2021). Leonardi et al. (2021) found that the VRRS based cognitive training improved global cognition, long term verbal memory, semantic verbal fluency and mental quality of life more than the conventional treatment. On the other hand, both treatments increased long term visuospatial memory and attention. Pagliari et al. (2021) found that VRRS cognitive training administered through TR had comparable effects to the conventional cognitive intervention. Finally, Goffredo et al. (2023) found that VRRS cognitive training administered through TR had comparable effects to an at-home self-administered treatment in improving global cognition of patients with multiple sclerosis and Parkinson’s disease.
4Discussion
Overall, we found 30 studies using the VRRS in neuromotor and neuropsychological rehabilitation. Below we discuss only those studies that adopted an experimental approach.
We found 19 studies that report information on the use of the VRRS for neurological rehabilitation with ten studies including control group condition and/or randomization procedure (Kiper et al., 2011, 2014; Luque-Moreno et al., 2021; Pagliari et al., 2021; Piron et al., 2009; Gianola et al., 2020; Turolla et al., 2013; Calabrò et al., 2023; Goffredo et al., 2023; Fascio et al., 2022). Most of the studies suggest that VRRS based neuromotor training (alone or in combination with conventional interventions) may be more effective than the conventional treatment (Kiper et al., 2011, 2014; Luque-Moreno et al., 2021; Pagliari et al., 2021; Piron et al., 2009; Turolla et al., 2013; Goffredo et al., 2023).
Seventeen studies examined the use of the VRRS for neuropsychological rehabilitation with 11 studies including control group condition and/or randomization procedure (Maresca et al., 2019; 2022; Manenti et al., 2020; Torrisi et al., 2019; Cappadonna et al., 2023; De Luca et al., 2022b; 2023; Calabrò et al., 2023; Goffredo et al., 2023; Leonardi et al., 2021; Pagliari et al., 2021). Concerning face-to-face VRRS based cognitive training, most of the studies demonstrated the efficacy of the VRRS based cognitive in improving neuropsychological functions (Leonardi et al., 2021; Maresca et al., 2022; Manetti et al., 2020; De Luca et al., 2022b; 2023). Concerning the efficacy of the VRRS intervention via TR the majority of studies suggests that VRRS via TR could have a comparable effect to the conventional/control treatment (Calabrò et al., 2023; Manenti et al., 2020; Pagliari et al., 2021; Goffredo et al., 2023). However, two studies found that VRRS intervention via TR outperformed traditional treatment administered at home (Maresca et al., 2019; Torrisi et al., 2019).
It is important to consider a relevant aspect that might question the efficacy of the VRRS in the treatment of specific neuropsychological deficits. In some cases, there are inconsistent results of treatment effect on the same cognitive function both within the same study and between different studies. For example, the same study finds an improvement in some but not all measures of the same neuropsychological function (see e.g. memory measures in Manenti et al., 2020). Additionally, other studies report discordant results about the efficacy of VRRS in improving some cognitive functions (see for example phonetic fluency in Manenti et al., 2020; Torrisi et al., 2019; and TMT in De Luca et al., 2022b; 2023). Therefore, although studies generally agree in indicating the efficacy of VRRS in neuropsychological rehabilitation overall, the conflicting results concerning specific cognitive functions and tasks limit in some case the possibility of drawing firm conclusions on the efficacy of VRRS in addressing them. Therefore, future research needs to evaluate the efficacy of VRRS in the rehabilitation of specific neuropsychological functions in specific conditions and outcomes measures.
4.1Recommendations for future research
Studies concerning the neurological and neuropsychological treatment using the VRRS in-person provide some evidence on its efficacy. However, VRRS was used for treating different dysfunctions and diseases for which a consistent body of evidence is lacking except for post-stroke conditions. Therefore, it is important to acknowledge that the discussed findings on the use of the VRRS for treatment are not generalizable across different populations of patients. Further studies are needed to examine and confirm the efficacy of the VRRS in specific populations. It is reasonable to assume that, based on quality of scientific evidence, the VRRS and VRRS via TR could be recommended for specific group of patients, and not others.
TR is particularly important for subjects with limited access to therapy due to geographical distance, transport difficulties or a lack of local services (Manenti et al., 2020). Our findings thus encourage future research to further test applications and efficacy of VRRS via TR.
VRRS was used for treating several dysfunctions and diseases. However, few studies investigated the use of the VRRS for neurological and neuropsychological rehabilitation of children and adolescents (Menici et al., 2021; Olivieri et al., 2013; Cappadonna et al., 2023; Maresca et al., 2022). Thus, controlled randomized studies are needed to test the efficacy of the VRRS and its TR application in the young population. Further, the analysed studies generally included short term follow-ups (i.e., evaluations soon after treatment).
Finally, detailed cost effectiveness and economic analyses should be performed to examine whether rehabilitation using the VRRS, during hospitalization and/or via the TR modality, reduces health care providers’ and patients’ costs compared with conventional (face to face) treatments or not.
4.2Study limitations
The present study provides a recent and exhaustive literature review on research studies using the VRRS for rehabilitation. However, it has some limitations that should be kept in mind when interpreting its findings. First, as for all narrative/literature reviews, we did not provide an empirical synthesis of the findings of included studies. Second, as for all reviews, the quality of reported findings relies on the quality of statistical analysis of original studies and, as such, reported evidence are limited by original studies limitations (e.g., lack of control group and long-term follow-up, poor description and/or reporting of statistical analysis, lack of testing between group differences and between group analysis not controlling for important baseline covariates, multiple testing increasing the risk of false-positive findings, small sample size). Despite important initial efforts, more needs to be done to improve scientific evidence. Future systematic reviews with meta-analysis should address VRRS rehabilitation efficacy.
5Conclusion
VRRS was widely used for treated several dysfunctions and diseases. The present study after narratively reviewing scientific evidence suggests that the use and efficacy of VRRS rehabilitative intervention for increasing neurological and neuropsychological functioning of patients is promising. However, further studies are needed in order to evaluate the efficacy of VRRS in the rehabilitation of specific neurological and neuropsychological functions. Moreover, the evidence is very limited for young patients. Future studies should also plan and analyse long-term follow-up as well as provide cost-effectiveness analyses.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
This research was funded by the “5 per mille” 2021 – funds for biomedical research by Antonio Trabacca and by the Italian Ministry of Health (Ricerca Corrente funds).
Ethics statement
All procedures followed were in accordance with the ethical standards on human experimentation of the institutional Ethical and Scientific Committees and with the Helsinki Declaration of 1975.
References
1 | Alemanno, F. , Houdayer, E. , Emedoli, D. , Locatelli, M. , Iannaconne, S. (2018). Telemedicine to set new frontiers in neurorehabilitation: A cognitive home-based solution [Conference Abstract]. Neurorehabilitation and Neural Repair, 32. https://doi.org/10.1177/1545968318765498 |
2 | Alemanno, F. , Houdayer, E. , Emedoli, D. , Locatelli, M. , Mortini, P. , Mandelli, C. , Raggi, A. , Iannaccone, S. ((2019) ) Efficacy of virtual reality to reduce chronic low back pain: Proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome, PLOS ONE 14: (5) e0216858. https://doi.org/10.1371/journal.pone.0216858 |
3 | Baethge, C. , Goldbeck-Wood, S. , Mertens, S. ((2019) ) SANRA—a scale for the quality assessment of narrative review articles, Research Integrity and Peer Review 4: (1) 5. https://doi.org/10.1186/s41073-019-0064-8 |
4 | Bryanton, C. , Bossé, J. , Brien, M. , McLean, J. , McCormick, A. , Sveistrup, H. ((2006) ) Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy, Cyberpsychology & Behavior: The Impact of the Internet, Multimedia and Virtual Reality on Behavior and Society 9: (2) 123–128. https://doi.org/10.1089/cpb.2006.9.123 |
5 | Buccino, G. ((2014) ) Action observation treatment: A novel tool in neurorehabilitation, Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences 369: (1644) 20130185. https://doi.org/10.1098/rstb.2013.0185 |
6 | Byrne, J. A. ((2016) ) Improving the peer review of narrative literature reviews, Research Integrity and Peer Review 1: (1) 12. https://doi.org/10.1186/s41073-016-0019-2 |
7 | Cacciante, L. , Kiper, P. , Garzon, M. , Baldan, F. , Federico, S. , Turolla, A. , Agostini, M. ((2021) ) Telerehabilitation for people with aphasia: A systematic review and metaanalysis, Journal of Communication Disorders 92: 106111. https://doi.org/10.1016/j.jcomdis.2021.106111 |
8 | Calabrò, , Rocco Salvatore, et al. ((2023) ). Benefits of Telerehabilitation for Patients With Severe Acquired Brain Injury: Promising Results From a Multicenter Randomized Controlled rial Using Nonimmersive Virtual Reality. Journal of Medical Internet Research, 25: , e45458. |
9 | Cappadona, I. , Ielo, A. , La Fauci, M. , Tresoldi, M. , Settimo, C. , De Cola, M. C. , Muratore, R. , De Domenico, C. , Di Cara, M. , Corallo, F. , Tripoli, E. , Impallomeni, C. , Quartarone, A. , Cucinotta, F. ((2023) ) Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial, Children 10: (8) 1336. https://doi.org/10.3390/children10081336 |
10 | Chillura, A. , Bramanti, A. , Tartamella, F. , Pisano, M. F. , Clemente, E. , Lo Scrudato, M. , Cacciato, G. , Portaro, S. , Calabrò, R. S. , Naro, A. ((2020) ) Advances in the rehabilitation of intensive care unit acquired weakness, Medicine 99: (28) e20939. https://doi.org/10.1097/MD.0000000000020939 |
11 | Contrada, M. , Arcuri, F. , Tonin, P. , Pignolo, L. , Mazza, T. , Nudo, G. , Pignataro, M.L. , Quintieri, M. , Iozzi, A. , Cerasa, A. ((2022) ) Stroke Telerehabilitation in Calabria: A Health Technology Assessment, Frontiers in Neurology 12: 777608. https://doi.org/10.3389/fneur.2021.777608 |
12 | De Luca, R. , Bonanno, M. , Marra, A. , Rifici, C. , Pollicino, P. , Caminiti, A. , Castorina, M.V. , Santamato, A. , Quartarone, A. , Calabrò, R. S. ((2023) ) Can Virtual Reality Cognitive Rehabilitation Improve Executive Functioning and Coping Strategies in Traumatic Brain Injury? A Pilot Study, Brain Sciences 13: (4) 578. https://doi.org/10.3390/brainsci13040578. |
13 | De Luca R. , Marra A. , Pollicino P. , Buda M. , Mucari M. , Bonanno M. , Torregrossa W. , Caminiti A. , Rifici C. , Calabrò R. S. ((2022) )a. Advances in neuroRehabilitation of TREM2-related dementia: A case report on a novel multimodal approach using virtual reality. Medicine, 101: (21). doi: 10.1097/MD.0000000000029470 |
14 | De Luca R. , Bonanno, M. , Rifici, C. , Pollicino, P. , Caminiti, A. , Morone, G.,. , Calabrò R. S. ((2022) )b. Does Non-Immersive Virtual Reality Improve Attention Processes in Severe Traumatic Brain Injury? Encouraging Data from a Pilot Study. Brain Sciences, 12: (9), 1211. https://doi.org/10.3390/brainsci12091211. |
15 | De Stefani, E. , Barbot, A. , Bertolini, C. , Belluardo, M. , Garofalo, G. , Bruno, N. , Bianchi, B. , Ferri, A. , Ferrari, P. F. ((2021) ) A New Neurorehabilitative Postsurgery Intervention for Facial Palsy Based on Smile Observation and Hand-Mouth Motor Synergies, Neural Plasticity 2021: 8890541. https://doi.org/10.1155/2021/8890541 |
16 | Emedoli, D. , Arosio, M. , Tettamanti, A. , Iannaccone, S. ((2021) ) Virtual Reality Augmented Feedback Rehabilitation Associated to Action Observation Therapy in Buccofacial Apraxia: Case Report, Clinical Medicine Insights. Case Reports 14: 1179547621994579. https://doi.org/10.1177/1179547621994579 |
17 | Ertelt, D. , Small, S. , Solodkin, A. , Dettmers, C. , McNamara, A. , Binkofski, F. , Buccino, G. ((2007) ). Action observation has a positive impact on rehabilitation of motor deficits after stroke. NeuroImage, 36 Suppl 2, T164–173. https://doi.org/10.1016/j.neuroimage.2007.03.043 |
18 | Fascio, E. , Vitale, J. A. , Sirtori, P. , Peretti, G. , Banfi, G. , Mangiavini, L. ((2022) ) Early virtual-reality-based home rehabilitation after total hip arthroplasty: a randomized controlled trial, Journal of Clinical Medicine 11: (7) 1766. https://doi.org/10.3390/jcm11071766 |
19 | Gamito, P. , Oliveira, J. , Coelho, C. , Morais, D. , Lopes, P. , Pacheco, J. , Brito, R. , Soares, F. , Santos, N. , Barata, A. F. ((2017) ) Cognitive training on stroke patients via virtual reality-based serious games, Disability and Rehabilitation 39: (4) 385–388. https://doi.org/10.3109/09638288.2014.934925 |
20 | Gasparyan, A. Y. , Ayvazyan, L. , Blackmore, H. , Kitas, G. D. ((2011) ) Writing a narrative biomedical review: Considerations for authors, peer reviewers, and editors, Rheumatology International 31: (11) 1409–1417. https://doi.org/10.1007/s00296-011-1999-3 |
21 | Gianola, S. , Stucovitz, E. , Castellini, G. , Mascali, M. , Vanni, F. , Tramacere, I. , Banfi, G. , Tornese, D. ((2020) ) Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial, Medicine 99: (7) e19136. https://doi.org/10.1097/MD.0000000000019136 |
22 | Goffredo, M. , Pagliari, C. , Turolla, A. , Tassorelli, C. , Di Tella, S. , Federico, S. , Franceschini, M. ((2023) ) Non-Immersive Virtual Reality Telerehabilitation System Improves Postural Balance in People with Chronic Neurological Diseases, Journal of Clinical Medicine 12: (9) 3178. https://doi.org/10.3390/jcm12093178 |
23 | Golomb, M. R. , McDonald, B. C. , Warden, S. J. , Yonkman, J. , Saykin, A. J. , Shirley, B. , Huber, M. , Rabin, B. , Abdelbaky, M. , Nwosu, M. E. , Barkat-Masih, M. , Burdea, G. C. ((2010) ) In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy, Archives of Physical Medicine and Rehabilitation 91: (1) 1–8.e1. https://doi.org/10.1016/j.apmr.2009.08.153 |
24 | Green, B. N. , Johnson, C. D. , Adams, A. ((2006) ) Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade, Journal of Chiropractic Medicine 5: (3) 101–117. https://doi.org/10.1016/S0899-3467(07)60142-6 |
25 | Hao, J. , Xie, H. , Harp, K. , Chen, Z. , Siu, K.-C. ((2021) ) Effects of Virtual Reality Intervention on Neural Plasticity in Stroke Rehabilitation: A Systematic Review, Archives of Physical Medicine and Rehabilitation 103: 523–541. https://doi.org/10.1016/j.apmr.2021.06.024 |
26 | Kable, A. K. , Pich, J. , Maslin-Prothero, S. E. ((2012) ) A structured approach to documenting a search strategy for publication: A 12 step guideline for authors, Nurse Education Today 32: (8) 878–886. https://doi.org/10.1016/j.nedt.2012.02.022 |
27 | Kim, O. , Pang, Y. , Kim, J.-H. ((2019) ) The effectiveness of virtual reality for people with mild cognitive impairment or dementia: A meta-analysis, BMC Psychiatry 19: (1) 219. https://doi.org/10.1186/s12888-019-2180-x |
28 | Kiper, P. , Agostini, M. , Luque-Moreno, C. , Tonin, P. , Turolla, A. ((2014) ) Reinforced Feedback in Virtual Environment for Rehabilitation of Upper Extremity Dysfunction after Stroke: Preliminary Data from a Randomized Controlled Trial, BioMed Research International 2014: 752128. https://doi.org/10.1155/2014/752128 |
29 | Kiper, P. , Piron, L. , Turolla, A. , Stożek, J. , Tonin, P. ((2011) ) The effectiveness of reinforced feedback in virtual environment in the first 12 months after stroke, Neurologia I Neurochirurgia Polska 45: (5) 436–444. https://doi.org/10.1016/s0028-3843(14)60311-x |
30 | Leonardi, S. , Maggio, M. G. , Russo, M. , Bramanti, A. , Arcadi, F. A. , Naro, A. , Calabrò, R. S. , De Luca, R. ((2021) ) Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation, Clinical Neurology and Neurosurgery 208: 106828. https://doi.org/10.1016/j.clineuro.2021.106828 |
31 | Luque-Moreno, C. , Kiper, P. , Solís-Marcos, I. , Agostini, M. , Polli, A. , Turolla, A. , Oliva-Pascual-Vaca, A. ((2021) ) Virtual Reality and Physiotherapy in Post-Stroke Functional Re-Education of the Lower Extremity: A Controlled Clinical Trial on a New Approach, Journal of Personalized Medicine 11: (11) 1210. https://doi.org/10.3390/jpm11111210 |
32 | Luque-Moreno, C. , Oliva-Pascual-Vaca, A. , Kiper, P. , Rodríguez-Blanco, C. , Agostini, M. , Turolla, A. ((2016) ) Virtual Reality to Assess and Treat Lower Extremity Disorders in Post-stroke Patients, Methods of Information in Medicine 55: (1) 89–92. https://doi.org/10.3414/ME14-02-0020 |
33 | Maier, M. , Rubio Ballester, B. , Duff, A. , Duarte Oller, E. , Verschure, P. F. M. J. ((2019) ) Effect of Specific Over Nonspecific VR-Based Rehabilitation on Poststroke Motor Recovery: A Systematic Meta-analysis, Neurorehabilitation and Neural Repair 33: (2) 112–129. https://doi.org/10.1177/1545968318820169 |
34 | Maistrello, L. , Rimini, D. , Cheung, V. C. K. , Pregnolato, G. , Turolla, A. ((2021) ). Muscle Synergies and Clinical Outcome Measures Describe Different Factors of Upper Limb Motor Function in Stroke Survivors Undergoing Rehabilitation in a Virtual Reality Environment. Sensors, 21: (23), Art. 23. https://doi.org/10.3390/s21238002. |
35 | Manenti, R. , Gobbi, E. , Baglio, F. , Macis, A. , Ferrari, C. , Pagnoni, I. , Rossetto, F. , Di Tella, S. , Alemanno, F. , Cimino, V. , Binetti, G. , Iannaccone, S. , Bramanti, P. , Cappa, S. F. , Cotelli, M. ((2020) ) Effectiveness of an Innovative Cognitive Treatment and Telerehabilitation on Subjects With Mild Cognitive Impairment: A Multicenter, Randomized, Active-Controlled Study, Frontiers in Aging Neuroscience 12: 585988. https://doi.org/10.3389/fnagi.2020.585988 |
36 | Maresca, G. , Maggio, M. G. , Buda, A. , La Rosa, G. , Manuli, A. , Bramanti, P. , De Luca, R. , Calabrò, R. S. ((2018) ) A novel use of virtual reality in the treatment of cognitive and motor deficit in spinal cord injury, Medicine 97: (50) e13559. https://doi.org/10.1097/MD.0000000000013559 |
37 | Maresca, G. , Maggio, M. G. , Latella, D. , Cannavò, A. , De Cola, M. C. , Portaro, S. , Stagnitti, M. C. , Silvestri, G. , Torrisi, M. , Bramanti, A. , De Luca, R. , Calabrò, R. S. ((2019) ) Toward Improving Poststroke Aphasia: A Pilot Study on the Growing Use of Telerehabilitation for the Continuity of Care, Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association 28: (10) 104303. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104303 |
38 | Maresca, G. , Portaro, S. , Naro, A. , Scarcella, I. , Bramanti, P. , Militi, D. , Accorinti, M. , De Luca, R. , Calabrò, R. S. ((2020) ) Look at the cognitive deficits in patients with myotonic dystrophy type 1: An exploratory research on the effects of virtual reality, International Journal of Rehabilitation Research. Internationale Zeitschrift Fur Rehabilitationsforschung. Revue Internationale De Recherches De Readaptation 43: (1) 90–94. https://doi.org/10.1097/MRR.0000000000000384 |
39 | Maresca, G. , Leonardi, S. , De Cola, M. C. , Giliberto, S. , Di Cara, M. , Corallo, F. , Quartarone, A. , Pidalà, A. ((2022) ) Use ofVirtual Reality in Children with Dyslexia, Children 9: (11) 1621. https://doi.org/10.3390/children9111621 |
40 | Menici, V. , Barzacchi, V. , Filogna, S. , Beani, E. , Tinelli, F. , Cioni, G. , Sgandurra, G. (2021). Tele-Rehabilitation for Postural Control by Means of Virtual Reality Rehabilitation System in an Adolescent With Motor Disorder: A Case Study. Frontiers in Psychology, 12. https://www.frontiersin.org/articles/10.3389/fpsyg.2021.720677 |
41 | Morganti, F. ((2004) ). Virtual interaction in cognitive neuropsychology. Studies in Health Technology and Informatics, 99: , 55–70. |
42 | Nascimento, A. S. , Fagundes, C. V. , Mendes, F. A. D. S. , Leal, J. C. ((2021) ) Effectiveness of Virtual Reality Rehabilitation in Persons with Multiple Sclerosis: A Systematic Review and Meta-analysis of Randomized Controlled Trials, Multiple Sclerosis and Related Disorders 54: 103128. https://doi.org/10.1016/j.msard.2021.103128 |
43 | Oliveira, J. , Gamito, P. , Souto, T. , Conde, R. , Ferreira, M. , Corotnean, T. , Fernandes, A. , Silva, H. , Neto, T. ((2021) ) Virtual Reality-Based Cognitive Stimulation on People with Mild to Moderate Dementia due to Alzheimer’s Disease: A Pilot Randomized Controlled Trial, International Journal of Environmental Research and Public Health 18: (10) 5290. https://doi.org/10.3390/ijerph18105290 |
44 | Olivieri, I. , Chiappedi, M. , Meriggi, P. , Mazzola, M. , Grandi, A. , Angelini, L. ((2013) ) Rehabilitation of Children with Hemiparesis: A Pilot Study on the Use of Virtual Reality, BioMed Research International 2013: 695935. https://doi.org/10.1155/2013/695935 |
45 | Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo-Wilson, E. , McDonald, S. , Moher, D. ((2021) ) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, BMJ 372: n71. https://doi.org/10.1136/bmj.n71 |
46 | Pagliari, C. , Di Tella, S. , Jonsdottir, J. , Mendozzi, L. , Rovaris, M. , De Icco, R. , Milanesi, T. , Federico, S. , Agostini, M. , Goffredo, M. , Pellicciari, L. , Franceschini, M. , Cimino, V. , Bramanti, P. , Baglio, F. (2021). Effects of homebased virtual reality telerehabilitation system in people with multiple sclerosis: A randomized controlled trial. Journal of Telemedicine and Telecare, 1357633X211054839. https://doi.org/10.1177/1357633X211054839 |
47 | Park, S.-H. , Son, S.-M. , Choi, J.-Y. ((2021) ) Effect of posture control training using virtual reality program on sitting balance and trunk stability in children with cerebral palsy, NeuroRehabilitation 48: (3) 247–254. https://doi.org/10.3233/NRE-201642 |
48 | Pautasso, M. ((2013) ) Ten Simple Rules for Writing a Literature Review, PLOS Computational Biology 9: (7) e1003149. https://doi.org/10.1371/journal.pcbi.1003149 |
49 | Piron, L. , Turolla, A. , Agostini, M. , Zucconi, C. , Cortese, F. , Zampolini, M. , Zannini, M. , Dam, M. , Ventura, L. , Battauz, M. , Tonin, P. ((2009) ) Exercises for paretic upper limb after stroke: A combined virtual-reality and telemedicine approach, Journal of Rehabilitation Medicine 41: (12) 1016–1102. https://doi.org/10.2340/16501977-0459 |
50 | Rintala, A. , Päivärinne, V. , Hakala, S. , Paltamaa, J. , Heinonen, A. , Karvanen, J. , Sjögren, T. ((2019) ) Effectiveness of Technology-Based Distance Physical Rehabilitation Interventions for Improving Physical Functioning in Stroke: A Systematic Review and Meta-analysis of Randomized Controlled Trials, Archives of Physical Medicine and Rehabilitation 100: (7) 1339–1358. https://doi.org/10.1016/j.apmr.2018.11.007 |
51 | Riva, G. , Mancuso, V. , Cavedoni, S. , Stramba-Badiale, C. ((2020) ) Virtual reality in neurorehabilitation: A review of its effects on multiple cognitive domains, Expert Review of Medical Devices 17: (10) 1035–1061. https://doi.org/10.1080/17434440.2020.1825939 |
52 | Rizzo, A. A. , Buckwalter, J. G. , van der Zaag, C. (2002). Virtual Environment Applications in Clinical Neuropsychology. In Handbook of Virtual Environments. CRC Press. |
53 | Rodrigo-Yanguas, M. , Martin-Moratinos, M. , Menendez-Garcia, A. , Gonzalez-Tardon, C. , Sanchez-Sanchez, F. , Royuela, A. , Blasco-Fontecilla, H. ((2021) ) A Virtual Reality Serious Videogame Versus Online Chess Augmentation in Patients with Attention Deficit Hyperactivity Disorder: A Randomized Clinical Trial, Games for Health Journal 10: (4) 283–292. https://doi.org/10.1089/g4h.2021.0073 |
54 | Schultheis, M. T. , Rizzo, A. A. ((2001) ) The application of virtual reality technology in rehabilitation, Rehabilitation Psychology 46: (3) 296–311. https://doi.org/10.1037/0090-5550.46.3.296 |
55 | Serino, S. , Pedroli, E. , Tuena, C. , De Leo, G. , Stramba-Badiale, M. , Goulene, K. , Mariotti, N. G. , Riva, G. ((2017) ) A Novel Virtual Reality-Based Training Protocol for the Enhancement of the “Mental Frame Syncing” in Individuals with Alzheimer’s Disease: A Development-of-Concept Trial, Frontiers in Aging Neuroscience 9: 240. https://doi.org/10.3389/fnagi.2017.00240 |
56 | Sgandurra, G. , Ferrari, A. , Cossu, G. , Guzzetta, A. , Fogassi, L. , Cioni, G. ((2013) ) Randomized trial of observation and execution of upper extremity actions versus action alone in children with unilateral cerebral palsy, Neurorehabilitation and Neural Repair 27: (9) 808–815. https://doi.org/10.1177/1545968313497101 |
57 | Tartamella, F. , Chillura, A. , Pisano, M. F. , Cacioppo, A. , Licari, S. , Caradonna, D. , Portaro, S. , Calabrò, R. S. , Bramanti, P. , Naro, A. ((2020) ) A case report on intensive, robot-assisted rehabilitation program for brainstem radionecrosis, Medicine 99: (10) e19517. https://doi.org/10.1097/MD.0000000000019517 |
58 | Tchero, H. , Tabue Teguo, M. , Lannuzel, A. , Rusch, E. ((2018) ) Telerehabilitation for Stroke Survivors: Systematic Reviewand Meta-Analysis, Journal of Medical Internet Research 20: (10) e10867. https://doi.org/10.2196/10867 |
59 | Torrisi, M. , Maresca, G. , De Cola, M. C. , Cannavò, A. , Sciarrone, F. , Silvestri, G. , Bramanti, A. , De Luca, R. , Calabrò, R. S. ((2019) ) Using telerehabilitation to improve cognitive function in post-stroke survivors: Is this the time for the continuity of care? International Journal of Rehabilitation Research, Internationale Zeitschrift Fur Rehabilitationsforschung. Revue Internationale De Recherches De Readaptation 42: (4) 344–351. https://doi.org/10.1097/MRR.0000000000000369 |
60 | Turolla, A. , Dam, M. , Ventura, L. , Tonin, P. , Agostini, M. , Zucconi, C. , Kiper, P. , Cagnin, A. , Piron, L. ((2013) ) Virtual reality for the rehabilitation of the upper limb motor function after stroke: A prospective controlled trial, Journal of Neuroengineering and Rehabilitation 10: 85. https://doi.org/10.1186/1743-0003-10-85 |
61 | Wang, M. , Reid, D. ((2011) ) Virtual reality in pediatric neurorehabilitation: Attention deficit hyperactivity disorder, autism and cerebral palsy, Neuroepidemiology 36: (1) 2–18. https://doi.org/10.1159/000320847 |
62 | Weiss, P. , Kizony, R. , Feintuch, U. , Katz, N. (2006). Virtual reality in neurorehabilitation. Textbook of Neural Repair and Rehabilitation, 182-197. https://doi.org/10.1017/CBO9780511545078.015 |
63 | You, S. H. , Jang, S. H. , Kim, Y.-H. , Hallett, M. , Ahn, S. H. , Kwon, Y.-H. , Kim, J. H. , Lee, M. Y. ((2005) ) Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: An experimenter-blind randomized study, Stroke 36: (6) 1166–1171. https://doi.org/10.1161/01.STR.0000162715.43417.91 |
64 | Zhao, J.-Q. , Zhang, X.-X. , Wang, C.-H. , Yang, J. ((2021) ) Effect of cognitive training based on virtual reality on the children with autism spectrum disorder, Current Research in Behavioral Sciences 2: 100013. |




