Development of an inpatient rehabilitation pathway for motor functional neurological disorders: Initial reflections
Abstract
BACKGROUND:
Emerging research supports a primary role for rehabilitation therapy alongside psychoeducation and psychotherapy in the treatment of functional neurological disorder (FND).
OBJECTIVE:
While consensus recommendations for physical therapists, occupational therapists, and speech and language pathologists treating FND have been published, specific recommendations for multidisciplinary FND care delivered on an inpatient rehabilitation unit are yet to be established.
METHODS:
This report describes one inpatient rehabilitation facility’s efforts to design and implement a clinical pathway for patients with acute-onset motor FND—patients recently hospitalized for work-up of new neurological symptoms subsequently deemed functional.
RESULTS:
Detailed descriptions on defining admission criteria and delivering consensus- and evidence-based multidisciplinary inpatient rehabilitation are provided.
CONCLUSIONS:
In the context of prospective research studies, considerably more work is needed to delineate the optimal duration and intensity of inpatient rehabilitation treatment for the management of patients with motor FND.
1Introduction
In this article, we describe the development and initial implementation of a clinical pathway for treating functional neurological disorder (FND) at an acute inpatient rehabilitation facility. FND is a condition in which sensorimotor neurological symptoms are inconsistent and incongruent with other known neurological conditions, and ranks among the most common diagnoses seen in neurology clinics (Espay et al., 2018; Stone et al., 2010). FND can be associated with a range of disabling motor (e.g. limb weakness/paralysis, hyperkinetic movements, atypical gait, seizures), sensory (e.g. vision), or cognitive symptoms (Stone et al., 2009). FND may also be accompanied by a range of comorbid symptoms including pain, fatigue, cognitive difficulties and/or urinary and bowel concerns; and while not found in all patients, many individuals with FND also have prominent depression, anxiety and trauma-related symptoms (Baslet et al., 2021; Nicholson et al., 2020; Perez et al., 2021). Our inpatient rehabilitation pathway specifically targeted patients with motor FND, including functional limb weakness, movement and gait disorders.
For much of the 20th century, FND, also known as conversion disorder, received relatively little attention from the medical establishment, and treatment was often relegated to mental health professionals alone (Fend et al., 2020). Renewed academic interest has since identified functional and structural abnormalities in several underlying neural networks, including those involved in self-focused attention, emotional processing, and motor planning (Baizabal-Carvallo et al., 2019; Bègue et al., 2019). In parallel, emerging treatment-focused research has begun to support a primary role for rehabilitation therapy (Nielsen et al., 2013) alongside skills-based psychotherapy (Baslet et al., 2020; Espay et al., 2019; Goldstein et al., 2020; Sharpe et al., 2011).
Recently, a series of rehabilitation consensus recommendations and reviews has been published, outlining specific strategies for physical therapists (PT), occupational therapists (OT), and speech language pathologists (SLP) treating FND (Baker et al., 2021; Nicholson et al., 2020; Nielsen et al, 2015). Many recommended FND strategies are unique and not traditionally employed elsewhere in rehabilitation protocols —for example use of distraction during motor tasks (counting backwards, snapping fingers, listening to music) or approaching a motor task in a novel way (walking backwards or sideways rather than forwards).
The majority of FND-related rehabilitation care currently involves individuals with motor symptoms and takes place in the outpatient setting. Literature here supports the role of physical therapy delivered as part of an outpatient FND clinic (Maggio et al., 2020) or multidisciplinary day program (Czarnecki et al., 2012; Nielsen et al., 2017; Petrochilos et al., 2020). FND patients may also present for inpatient rehabilitation following an acute hospital admission. In fact, a recent study indicates that nearly 20% of individuals presenting to the hospital with acute onset FND will require inpatient rehabilitation (Stephen et al., 2021). Several aspects of inpatient rehabilitation may be of particular benefit for this population experiencing new, marked functional deficits. Compared with standard outpatient care, inpatient rehabilitation can offer a higher frequency of therapies, coordinated delivery of both rehabilitation and psychological therapies, and provision of a sheltered setting that may temporarily limit exposure to detrimental social and environmental conditions (Gilmour et al., 2020).
Research into outcomes following inpatient rehabilitation is growing. For example, one recent study evaluated the impact of a five day intensive multidisciplinary inpatient program for functional movement disorders, involving daily PT, OT, SLP, and psychotherapy (Jacob, Kaelin, et al., 2018). At discharge, more than 85% of participants self-reported improvement on the clinical global impressions scale which was maintained in nearly 70% at 6-month follow-up; nearly 60% also showed improvement between admission and discharge on a physician-rated psychogenic motor disorder scale. Further research on inpatient rehabilitation for motor FND includes several case series and cohort studies (Demartini et al., 2014; Hebert et al., 2021; Heruti et al., 2002; Jacob, Kaelin, et al., 2018; Saifee et al., 2012; Shapiro, 1997; Shapiro & Teasell, 2004) as well as a randomized controlled trial (Jordbru et al., 2014). On the whole, this literature suggests a benefit from inpatient rehabilitation for a majority of patients (Williams et al., 2016), showing at least a short term functional benefit that persists for the longer-term (Jacob, Smith, et al., 2018; Saifee et al., 2012) in many cases.
While inpatient rehabilitation for motor FND is delivered in many health care facilities across the world, recommendations to direct inpatient teams are not currently available. The present report outlines one facility’s efforts to adapt its services to more specifically address the needs of individuals presenting with motor FND. Importantly, the present initiative did not aim to create a novel motor FND rehabilitation program, but rather sought to systematically apply specialized strategies—guided by existing evidence whenever possible—to more effectively treat motor FND in a coordinated way. As a matter of fact, patients with motor FND had already been treated at the present institution for many years. In designing and implementing the motor FND pathway, efforts were made to minimize the need for major structural changes to the general delivery of care, so that this pathway would not place further economic or time burden on the institution or on individual staff members. By sharing our experiences, we hope that others in the future will continue to build upon this work and help develop future practice recommendations for multidisciplinary inpatient care.
2Methods
2.1Program development
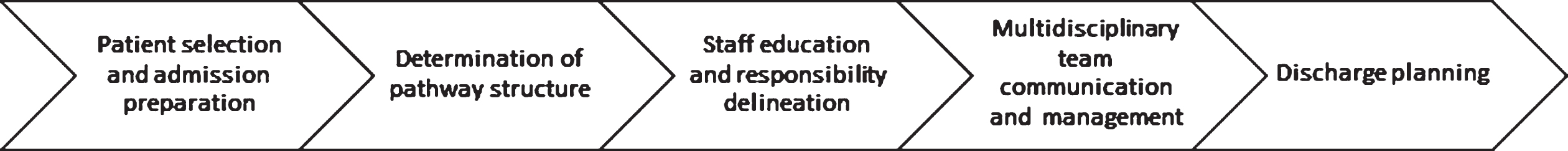
Over several months, a multidisciplinary FND taskforce at Spaulding Rehabilitation Hospital, a freestanding inpatient rehabilitation facility (IRF) in the Boston-area, assembled and participated in a series of meetings. Participants included the local admissions director, representative attending physiatrists, rehabilitation therapists, nurses, psychologists, social workers, and case managers. The taskforce worked to identify several key areas (Fig. 1) in need of development: 1) patient selection and admission preparation, 2) determination of pathway structure, 3) staff education and responsibility designation, 4) multidisciplinary team communication and management, and 5) discharge planning.
Fig. 1
Steps in developing a motor FND inpatient rehabilitation pathway.
2.2Patient selection and admission preparation
Admission criteria (Table 1) were developed with specific goals in mind: 1) minimizing ambiguity regarding the motor FND diagnosis which had been a source of confusion for patients and clinicians on the inpatient rehabilitation unit in the past, 2) screening out patients who were not willing or able to participate fully in a multidisciplinary mind-body treatment, and 3) minimizing risk of prolonged, futile rehabilitation stays.
Table 1
Admission criteria for motor FND inpatient rehabilitation
| 1. A motor FND diagnosis is made and delivered by a neurologist and clearly documented in the medical record |
| 2. Neurology team confirms completion of all diagnostic testing |
| 3. Patient affirms openness to diagnosis and motivation for multidisciplinary motor FND rehabilitation |
| 4. Patient understands 2-week pathway duration and can identify a reasonable post-rehabilitation community discharge plan if improvements are not seen |
| 5. All other criteria for acute inpatient rehabilitation level of care are met |
Referrals for inpatient rehabilitation came almost exclusively from inpatient neurology or medicine teams at affiliated hospitals. Referrals for inpatient rehabilitation coming from the Emergency Department were not accepted; motor FND patients were required to have been formally admitted to the acute care hospital. To meet the first aim, prior to transfer, referring neurology teams must have formally established the motor FND diagnosis based on history, examination, diagnostic testing and “rule-in” signs establishing inconsistency in motor symptoms (American Psychiatric Association, 2013). Referring teams must have also documented the diagnosis in the medical record, confirmed that all diagnostic testing was completed, and delivered the diagnosis to the patient. In simultaneous support of this effort, additional training was delivered by experienced neurology faculty to the broader neurology inpatient service at affiliated hospitals, regarding making and communicating the diagnosis of FND (Carson et al., 2016; McKee et al., 2018).
The neurology team or a consulting physiatrist were then further required to confirm that the patient expressed openness to participate fully in both physical rehabilitation therapies and psychotherapy for FND (Saifee et al., 2012). Patients were to have been informed that their stay at the acute rehabilitation facility would be approximately two weeks (as will be described further below), and case managers at referring hospitals were asked to begin discussions with patients regarding options for a community discharge with supports following an inpatient rehabilitation stay.
Typical criteria for admission to an acute rehabilitation hospital were also maintained: need for inpatient rehabilitation level of care based on functional impairment and medical need, ability to participate in at least three hours of rehabilitation therapy a day, and insurance pre-authorization approval. If any of these criteria were not met—e.g. severe pain or fatigue prevented full participation in rehabilitation therapy, or a patient strongly disagreed with the diagnosis and desired further neurologic work-up to uncover an alternative cause—that individual would not be accepted into the pathway. Individuals with comorbid neurological conditions such as a prior stroke, along with motor FND were allowed to participate in the pathway, as long as they met all other above criteria.
2.3Pathway structure
The motor FND pathway was designed to have a fixed two-week endpoint. Other facilities have reported widely variable length of stays (LOS) for inpatient rehabilitation, ranging from a few days to several months (Demartini et al., 2014; Gilmour et. al, 2021; Jacob, Kaelin, et al., 2018). Taskforce members agreed upon a two-week duration as this approximated the average LOS for an acute rehabilitation admission and was considered appropriately long enough to allow for full multidisciplinary assessment and treatment. A fixed, rather than open endpoint was selected based on discussions with other experts in the field. The intention here was to mitigate regression of symptoms as a flexible discharge date neared and to avoid prolonging rehabilitation stays when or if treatment was not proving to be beneficial. As such, prior to admission, a plan for discharge was established with the intent to be upheld regardless of whether or not the patient improved by the end of two weeks. In cases where a patient improved substantially in terms of mobility and self-care prior to the end of two weeks, an early return home was considered. A plan was also made to allow for occasional length of stay extensions for select cases in which the multidisciplinary team agreed that a few additional days of inpatient rehabilitation had a high likelihood of further improving functional capabilities.
During the two-week stay, individuals participated in three hours of PT/OT/SLP a day, 5-6 days a week, depending on their identified domains of impairment. They also participated at minimum, in twice weekly Cognitive Behavior Therapy (CBT) sessions with a clinical psychologist.1 Psychological interventions were adapted to individual needs considering factors such as readiness for change, engagement, self-awareness, symptom presentation and strengths. Consulting psychiatrists were involved in cases in which there were questions regarding psychopharmacology for comorbid mood and anxiety disorders. Ancillary services including social work, therapeutic recreation, music therapy, and aquatic therapy were also included on a case by case basis.
2.4Staff education and responsibilities of the multidisciplinary team
Members of the multidisciplinary team fulfilled both distinct and overlapping roles (Table 2). Education regarding motor FND was provided to each individual discipline through lectures, sharing of journal articles, and/or direction to FND educational websites such as www.neurosymptoms.org (Stone, 2018). Several clinicians working at the present acute inpatient rehabilitation facility also participated in or attended a large interprofessional psychoeducational symposium on FND hosted by Spaulding Rehabilitation Hospital several months prior, which likely helped facilitate global institutional knowledge regarding treatment of the disorder.
Table 2
Roles and responsibilities of multidisciplinary team members
| Discipline | Role description |
| Neurorehabilitation physician | Reconfirm and explain the diagnosis, validate patient experience, provide psychoeducation, define overarching multidisciplinary treatment plan, manage medical issues, treat pain, monitor progress. |
| Nursing | Provide psychoeducation, emphasize carryover strategies learned in therapy, minimize sick role, encourage independence, execute behavioral plan for functional seizures. |
| PT, OT, and SLP | Collaborate with patients on setting specific functional goals. Develop and implement a stepwise progressive approach to meet goals, utilizing activity logs and goal sheets when needed. Develop and reinforce self-management strategies. Communicate with entire team regarding mobility, self-care, and motor speech strategies to help with consistent carryover throughout the patient’s stay. |
| PT: targeted mobility training. | |
| OT: targeted self-care, ADL, and IADL training. | |
| SLP: Targeted IADL training, speech/voice, language, swallowing, and cognition. | |
| Mental health | Initial assessment: biopsychosocial assessment, address predisposing, precipitating, and perpetuating factors, assess “buy-in” to the diagnosis and readiness for change, identify rehab goals. |
| Subsequent sessions: psychoeducation, exploring contextual factors that may influence symptoms, stress management techniques, introduction to mindfulness. | |
| Case management | Discharge planning |
| Ancillary services | Therapeutic recreation: practice motor skills during leisure activities. |
| Neurologic music therapy: use music as a tool for distraction and use rhythm to normalize gait patterns (delivered in conjunction with PT, OT, or SLP). | |
| Aquatic therapy: practice movement patterns in a novel, buoyant environment (provided by OT or PT). |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living; OT, occupational therapy, PT, physical therapy; SLP, speech and language pathology.
2.5Physicians
Attending physiatrists helped set expectations for motor FND patients as they entered the inpatient rehabilitation facility. Inpatient rehabilitation was presented as a “bootcamp” with the goal to “learn self-management skills for the body and mind.” To help streamline the work of physicians without prior experience with FND, a physician checklist was created, outlining the following steps of initiating care: confirming and reiterating the diagnosis (your brain has difficulty “functioning” or “sending signals” despite being structurally intact), setting positive expectations for recovery, affirming the role of both rehabilitation work (“motor re-programming”) and psychotherapy (skills-based “brain-retraining”), and explaining the structure of the two week clinical pathway. A physician communication table of key psychoeducational points (Table 3) based in part on prior published work (Stone & Edwards, 2012) was also included in the physician checklist.
Table 3
Physician-patient communication points
| Topic | Communication point |
| Explanatory model (positive diagnosis) | The brain is unable to effectively “function” or “send signals” despite structural integrity. “This is like a software problem rather than a hardware problem.” |
| This condition is very common. | |
| Addressing other diagnostic concerns | What you don’t have (stroke, tumor, multiple sclerosis, etc.). |
| Review rationale for diagnosis | How the diagnosis was made (e.g. no changes on brain MRI). |
| Positive functional signs on exam (e.g. distractibility, Hoover’s, tremor entrainment) can be demonstrated to patients and used as a teaching device. | |
| Validation | These symptoms are genuine and not “all in the mind.” |
| Creating a positive expectation | With treatment, these symptoms are potentially reversible. |
| Treatment | There are effective treatments that require training. |
| PT/OT/SLP work through “motor-reprogramming.” | |
| Psychotherapy works through skills-based “brain-retraining” |
Abbreviations: MRI, magnetic resonance imaging; OT, occupational therapy, PT, physical therapy; SLP, speech and language pathology. Several elements of this table were extracted from Stone and Edwards (2012).
For maintaining consistency of patient buy-in to the diagnosis, if or when new neurological symptoms arose during a patient’s inpatient stay, physicians were advised to perform a physical examination, document any present “rule-in” functional signs, and try to minimize further diagnostic assessments unless clearly necessary. Exceptions to this general recommendation included a high degree of concern for a new neurologic diagnosis or progressive functional regression that did not appear to be impacted by any known FND trigger such as worsening stress or pain.
Education and training of physicians took place during a monthly inpatient attending meeting. The physicians were informed of the pathway development and the goals in terms of eliminating ambiguity of the diagnosis, providing continuity of the education and treatment started within the acute care hospital for the patient, and developing optimal rehabilitation strategies based on current evidenced-based literature. Attending physiatrists were also asked to review further literature on the topic (Stone & Carson, 2015). Given limited interest by this pool of physiatrists, efforts were subsequently made to identify a single physiatrist who would oversee the majority of motor FND admissions.
2.6Physical therapy, occupational therapy, and speech language pathology
Rehabilitation therapists played an essential role in the motor FND pathway. PTs, OTs, and SLPs used strategies from published consensus recommendations (Baker et al., 2021; Nicholson et al., 2020; Nielsen et al, 2015) whenever possible. All rehabilitation disciplines reinforced psychoeducation on FND. Rehabilitation therapists applied prior knowledge in progressive motor re-training to those with FND and also practiced behavioral strategies, recognizing and praising improvements, while minimizing attention paid to symptom exacerbations.
Lead therapists involved in the FND taskforce additionally delivered department-wide FND presentations to PTs, OTs, and SLPs regarding treatment and the structure of the multidisciplinary FND pathway.
FND taskforce members did not work directly with all motor FND admissions, and thus to support all rehabilitation staff when working with motor FND, rehabilitation consultations were sometimes employed. In these cases, the primary therapist assigned to a case would initially meet with a patient and perform an intake assessment, then request an in-person rehabilitation consultation with a provider more experienced in motor FND. The consulting rehabilitation therapist would thereafter coach the primary therapist regarding psychoeducation and treatment planning.
Family members and/or caregivers were encouraged throughout the admission to attend and participate in therapies assuming they were not a barrier to care. During family training, family was further educated by the rehabilitation team on the diagnosis and treatment of motor FND. This educational process helped ensure a commitment by family members to continue treatment upon discharge and help support gains made during the inpatient stay. Family members were also trained to help reinforce self-management strategies and functional independence recovery.
Therapists were lastly tasked with critically thinking about when or if to remove standard medical equipment or assistive devices from a patient’s room, such as a bedside commode or walker. Therapists optimized the room set-up to promote less reliance on equipment when it was safe to do so.
2.7Nursing
Nursing and personal care assistants (PCAs) played an active role in rehabilitation of motor FND patients. Education on FND was provided through in-service meetings for day and evening shift nurses. For education of PCAs, FND presentations were further simplified from a medical jargon standpoint, and emphasis was placed on the importance of being the discipline with the most patient contact throughout the day. Nursing and PCA educational materials were printed and left on the unit for ease of access.
Nurses and PCAs were encouraged to reinforce behavioral interventions by minimizing attention paid to functional impairments to only what was necessary for safety, encouraging functional independence and promoting self-efficacy (Delargy et al., 1986). Emphasis was placed on all shifts providing the same message and education to patients to avoid miscommunication and inconsistency in care. Communication on functional status remained consistent with usual hospital procedure, including use of dry-erase communication boards in each patient’s room as well as handoffs between nursing and therapy staff regarding any status changes.
Nurse and PCA training also included a discussion on functional seizures with the intent to limit unnecessary escalation of medical care. For patients with comorbid functional seizures, typical characteristics (e.g., full body rhythmic shaking) were documented in the medical record. If a patient exhibited his or her typical pattern of functional seizure while at inpatient rehabilitation, nurses and PCAs were instructed to alert responding clinicians by page rather than calling a rapid response or medical code.
2.8Mental health
A clinical psychologist met with motor FND patients at least twice a week for FND-focused skills-based psychotherapy. These sessions began to lay a groundwork for FND-focused psychotherapy to be expanded upon discharge in the outpatient setting. The initial clinical mental health assessment explored specific FND related elements and was informed by a Transtheoretical Model of Behavior Change (Prochaska et al., 2009). The patient’s “readiness for change” was considered in terms of the degree of engagement in the diagnosis and willingness to commit to behavior change. Subsequent sessions utilized motivational interviewing strategies to elicit reasons for change and help move patients toward healthy behaviors at their own pace. Patients were asked about specific symptoms; predisposing, precipitating and perpetuating factors; the impact of these symptoms on their life; attribution of their illness, buy-in, readiness for change, and goals for rehabilitation.
The following sessions were structured around the goals identified during the initial assessment. Some common elements covered in these subsequent sessions included psychoeducation, stress management strategies, and an introduction to mindfulness. Patients were frequently assigned “homework” to be completed between sessions that included education and symptom tracking (e.g. in relation to activities, time of day and mood) to help facilitate more targeted interventions. These specific interventions were modeled in part after prior CBT and mindfulness based interventions applied within the field of FND, though a specific manualized approach was not implemented (Baslet et al., 2020; Sharpe et al., 2011; Williams et al., 2017). Other disciplines helped reinforce participation in the homework assignment by reminding patients of their need to log their symptoms and/or practice certain skills. By the time of discharge, patients were expected to have developed a concrete set of skills with a plan to connect with an outpatient psychotherapist who could build upon this groundwork.
2.9Multidisciplinary team management
Efforts were made to provide education to the primary team just before a motor FND admission. Once the admissions department confirmed a motor FND admission, a taskforce email that included key resources (departmental clinical resources and FND education resources) was sent out to a unit’s multidisciplinary team.
As is customary in acute rehabilitation settings, multidisciplinary teams of physicians, PT, OT, SLP, nursing, psychology, and case management often meet weekly for Interdisciplinary Team Conference (ITC). In addition to this standard meeting that covers all admissions across diagnoses, several members of this multidisciplinary team met separately to discuss motor FND patients within a day after admission. See Table 4 for details on this team huddle. This additional meeting enabled team members to discuss initial evaluations and address potential barriers (e.g., pain) to ensure there were no unnecessary delays or disruptions to the rehabilitation pathway. There was open dialogue throughout the first week to determine if a second huddle was necessary to address concerns for optimal clinical progress, including identifying perpetuating factors, and discharge expectations.
Table 4
Team huddle checklist
| Topic | Discussion item |
| Management plan | What needs to be discussed to ensure interdisciplinary consistency of our management plan (toileting, transfers, medical equipment, splints, etc)? |
| Do we need a written contract or behavior plan? | |
| What self-management strategies have been initiated with the patient by psychology? | |
| Safety concerns | Any concerns for falls? If so, how can we reduce risk of injury should a fall occur? |
| Any other safety concerns (vitals, medication management, behaviors, etc)? | |
| Functional seizures | Does the patient experience functional seizures? What is the semiology? |
| Are there any known triggers? | |
| How should we help to manage functional seizures? | |
| Does a “rapid response” (emergency response) need to be called? | |
| Consults | Therapeutic Recreation consult? |
| Music Therapy consult? | |
| Aquatic Therapy consult? | |
| Caregiver presence | Any concerns regarding caregivers providing support? |
| Should we encourage caregivers to be present at sessions? | |
| How should we plan for caregiver training prior to discharge? | |
| Discharge planning | Any red flags or concerns for discharge within 2 weeks? |
2.10Preparation for discharge
In preparation for discharge, multidisciplinary team members including psychology, rehabilitation PT/OT/SLP, nursing, and physicians collectively helped prepare a customized summary document to encourage further understanding of motor FND and reinforcement of self-management strategies. The document listed the patient’s functional symptoms, described identified triggers and warnings signs, situations/events/experiences associated with symptom worsening, and interventions (e.g., breathing exercises, relaxation, music, distraction) that helped with symptom improvement. Thoughts and beliefs negatively impacting symptoms were also listed. This editable document was maintained on the electronic medical record so that multidisciplinary team members could collectively co-create the document. The document was then provided to the patient at the time of discharge as part of the after-visit summary paperwork. The patient was encouraged to share the document with members of his or her subsequent clinical outpatient aftercare team.
Case management helped with discharge planning, including coordinating ongoing follow-up with an outpatient physician with expertise in motor FND as well as home or outpatient PT/OT/SLP as needed. These referrals were kept within network whenever possible, with significant effort made to connect patients with outpatient rehabilitation specialists also known to be versed in motor FND. At times, there was a need for caregivers to supervise (but not provide physical assist) during certain higher-risk activities at discharge, primarily including stairs management, bathing/showering, cooking tasks, and community ambulation. When this was the case, caregivers were instructed in proper supervision techniques.
The inpatient psychologist took responsibility for referrals to outpatient psychotherapy to connect motor FND patients with appropriate providers. Attempts were made to refer to specialists with clinical experience in FND if possible, and at the very least with expertise in skills-based psychotherapies (such as CBT or mindfulness-based psychotherapy) or experience with chronic medical/neurological illnesses. Patients were also provided with specific information to help guide further work, including workbooks and websites (Sharpe et al., 2011; Stone, 2018; Williams et al., 2017), to assist outpatient clinicians. For those patients already followed by a community therapist, efforts were made to reach out and request integration of FND-focused skills into ongoing work. In cases where a pre-existing therapist practiced psychodynamic therapy, discussions regarding referral for short term alternative work on CBT for FND were made, after which the patient would return to his or her pre-existing therapist. Direct conversation between referring and receiving therapist were encouraged in this motor FND pathway keeping in line with the hospital’s general processes utilized in more complex cases. These direct hand-offs between inpatient and outpatient therapists help to smooth the transition to the new therapy provider which should allow for continued patient progress.
2.11Metrics
As is customary for acute inpatient rehabilitation, standardized functional independence measurements for PT and OT were collected within three days of admission and the day before discharge. In the present case, metrics included those already collected on the Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) from the Center for Medicare and Medicaid Service (Inpatient Rehabilitation Facility - Patient Assessment Instrument, 2020), which replaced the Functional Independence Measure (FIM™) in October, 2019. In line with the well-recognized importance for patient-reported measurements in the FND field (Nicholson et al., 2020; Pick et al., 2020), patient self-assessment forms regarding quality of life (36-Item Short Form Survey), somatic symptoms (Patient Health Questionnaire-15), anxiety (Generalized Anxiety Disorder-7), depression (Patient-Health Questionnaire-9), and perceived change in clinical status were also obtained. The use of consented videotaping of the patient’s baseline and discharge functional status was also encouraged whenever possible to provide patients with feedback on their progress.
3Results
A motor FND pathway involving evidence-based treatment strategies was successfully developed and implemented at the present inpatient rehabilitation facility. At the time of this writing, 18 patients with motor FND have participated. Admission criteria were successfully implemented and served as an effective gatekeeper to maintain appropriateness of referrals. All patients participating in the motor FND pathway were formally diagnosed with motor FND from a neurologist at an affiliated hospital and had completed all diagnostic testing for the presenting symptoms. All motor FND patients successfully participated in three hours of rehabilitation therapy a day as well as a minimum of twice weekly psychotherapy. Depending on individual needs, some patients met with psychiatry, social work, therapeutic recreation, music therapy, and/or aquatic therapy as well.
All participants improved in functional measurements as measured by the IRF-PAI between admission and discharge. Quantitative clinical outcome data from these assessments will be presented in a future manuscript. Video recording was encouraged but initially proved difficult for rehabilitation staff who were not accustomed to having this task in their typical workflow.
The involvement of a psychologist as a member of the multidisciplinary treatment team was established as part of the patient’s standard of care and therefore was not questioned or problematic for any of the participants. Although admission criteria sought to help select motivated patients who were receptive to the formal diagnosis of motor FND, this did not necessarily eliminate skepticism or establish full “buy-in” for the diagnosis for all participants. Therefore, the degree of involvement of psychology aligned directly with the assessment of patient’s level of commitment for change. This varied drastically amongst patients and was significantly challenged by the brief anticipated length of stay of two weeks. Although some patients functionally declined as discharge approached, all demonstrated greater self-awareness and understanding of the diagnosis itself and movement towards greater readiness for change. This observation was not formally measured, but rather identified through a final review of skills and education with established discharge plans for ongoing outpatient therapy.
The average length of stay of participants initially completing the pathway was slightly over two weeks. Patients were discharged early if they recovered mobility and self-care capacities prior to the end of their planned 2-week stay. A few patients stayed longer than planned due to an unexpected fall in one case and exacerbation of functional symptoms in another. In both cases, insurance approval to extend the stay was obtained and after the extension, patients continued to progress favorably. For complex cases, the additional FND team huddle led to productive conversations. Following discharge, appropriate referrals were made to outpatient rehabilitation therapies, psychotherapy, and physician follow-up.
There was concern that for patients who quickly returned to near normal baseline function, insurance coverage would be terminated early. However, in such cases, either (1) the patient and/or family members and multidisciplinary team all felt comfortable with an earlier discharge or (2) the team was able to justify the admission and continuing the hospital stay via peer-to-peer review with the insurance company, highlighting the medical necessity and ultimate functional benefit of completing the inpatient stay.
Overall, the vast majority of participating staff were able to fairly quickly learn and integrate strategies for managing patients with motor FND. Many were highly motivated to learn and apply best practices. Some staff, however, continued to express concern that caring for motor FND patients could require excessive effort on their part and questioned whether an inpatient psychiatric hospital would be a more appropriate treatment setting.
4Discussion
Inpatient rehabilitation treats a large range of conditions, including cardiopulmonary conditions, musculoskeletal disorders such as fractures, hip and knee arthroplasty, and neurological conditions such as spinal cord injury, stroke, acquired brain injury and other conditions (Anderson & Taylor, 2014; Khan et al., 2008; Langhorne, 2001; Nordström et al., 2018; Puhan et al., 2011). The common feature among this variety of conditions is that the patient has a body system/structure deficit leading to difficulty in activity or participation in social functioning. The defining characteristic of the inpatient rehabilitation setting is the use of a biopsychosocial framework and the practice of multidisciplinary teamwork focused on achieving functional tasks in an environment that promotes communication, coordination of care, support and teamwork. Our experience suggests the IRF setting represents a feasible model of care for patients with motor FND.
In developing and implementing a motor FND pathway for inpatient rehabilitation, several key findings emerged: 1) the need for a critical group of dedicated, skilled individuals was essential to the successful design and implementation of this pathway, and 2) consensus- and evidence-based strategies for managing motor FND could be incorporated into an inpatient rehabilitation pathway with limited structural change to the overarching infrastructure.
A frequently cited challenge to treating FND in any setting is providers’ limited experience with the diagnosis and lack of confidence in formulating a treatment plan. Clinicians across a range of settings have expressed difficulty due to lack of familiarity with the condition (Hallett, 2006; Lehn et al., 2019; Rommelfanger et al., 2017), formal training in diagnosis or treatment (Rommelfanger et al., 2017), or available therapeutic guidelines (Yam et al., 2015). The same held true for many staff members at the present rehabilitation facility. For this reason, it appeared essential to assemble a group of motivated providers and emphasize facility-wide staff education. That all inpatient rehabilitation disciplines (physician, PT, OT, SLP, psychology, social work, nurse manager, case management) were represented in the taskforce helped expedite efforts, as did having both physician and therapy leaders who could take charge of educating and training the involved broader group of providers and offer ongoing supervision.
Another notable challenge in implementing this pathway was disagreement from a few staff members regarding the appropriateness of inpatient rehabilitation for motor FND. In the treatment of FND at large, displeasure of treating clinicians is not uncommon (Ahern et al., 2009; Stewart, 1983; Yam et al., 2015). Elsewhere, inpatient rehabilitation and neuroscience clinicians have contested that FND—a condition with frequent psychological underpinnings—be treated similarly to those with strictly physical disabilities (Ahern et al., 2009; Stewart, 1983).
Further negative beliefs associated with FND include characterizing this population as being “more difficult to help” than other neurologic conditions (Carson, 2004) and more likely to require inordinate amounts of time for care (Ahern et al., 2009; Rommelfanger et al., 2017). Clinicians have further described the population as attention-seeking or overly demanding (Ahern et al., 2009) and also equated (inaccurately) FND with malingering (Galli et al., 2018). Lack of knowledge and comfort in treating FND, negative beliefs, and disagreement with the appropriateness of rehabilitation for this population can all cause major roadblocks. Here once again involvement of a multidisciplinary group of engaged providers helped enable to pathway to persist despite the initiative’s lack of unanimous popularity.
As stated at the beginning of this report, the intent of this initiative was to incorporate FND-informed strategies into the present structures for IRF-level care delivery, rather than to create an entirely new motor FND rehabilitation program. Ultimately, a IRF level FND pathway was established with limited need for permanent structural change in institutional operations. One of the few structural changes that was implemented and continued to persist even after initial admissions was the inclusion of an additional multidisciplinary team huddle that deviated from the typical ITC format. This meeting was designed to help team members feel informed of the patient narrative and the treatment plan, and to establish consistency of messaging between the multidisciplinary staff and the patient.
5Limitations
The applicability of the present institution’s experience to others may be limited by several factors. For instance, prior to developing the motor FND clinical pathway, this institution already had well-developed relationships with case managers, discharge planners, clinical and rehabilitative consultants at referring hospitals who facilitated patient selection. Furthermore, local outpatient motor FND specialists, working within the broader hospital network, allowed for an easy discharge transition. In contrast, in many other settings, discharging planning without a pool of recognized outpatient physicians proficient in the longitudinal management of motor FND would likely result in additional discharge planning challenges.
Finally, this report discusses development and implementation of a clinical pathway for treating motor FND at an inpatient rehabilitation facility, but it does not provide data on the efficacy of our established pathway criteria, whether intensive rehabilitation provides short- or long-term functional or clinical benefits, or maintains a favorable cost-benefit ratio. Many unanswered questions remain, including whether the approach stated here reflects the optimal dose, intensity, and duration of treatment to maximize clinical outcomes, or whether a precision medicine approach, in part informed by the clinical phenotype and clinical formulation, could provide more tailored (and efficacious) treatments. Clinician satisfaction with the initiation was also not assessed beyond noting of anecdotal comments. Given the high level of cost and resources involved, the inpatient rehabilitation setting may ultimately be deemed most suitable for only select cases—e.g., those with the most severe, complex, or disabling motor symptoms who also meet IRF criteria for admission. For now, which precise cases are most appropriate for inpatient rehabilitation remains to be determined.
6Conclusion
A clinical pathway for treating motor FND was designed for an IRF and required relatively little structural change to implement. Further research is needed to evaluate the short- and long-term functional outcomes and cost-benefit ratio of inpatient rehabilitation for patients with motor FND.
Acknowledgments
The authors would like to acknowledge the many additional clinicians, educators, and administrators involved across Mass General Brigham Hospital and Spaulding Rehabilitation Hospital who helped to facilitate this work.
Conflict of interest
B. D. and G. B. receive royalties on the Oxford University Press book, Psychogenic Nonepileptic Seizures: Toward the Integration of Care. D.L.P. has received honoraria for continuing medical education lectures in functional neurological disorders and is on the editorial board of Epilepsy & Behavior. J. M. receives research funding from the Sidney R. Baer Jr. Foundation. M. O. performs consulting work for Best Docs and Crico.
Funding
No funding was received for this publication.
References
1 | Ahern, L. , Stone, J. , & Sharpe, M.C. ((2009) ). Attitudes of neuroscience nurses toward patients with conversion symptoms. Psychosomatics, 50: (4), 336–339. |
2 | American Psychiatric Association. ((2013) ). Diagnostic and Statistical Manual of Mental disorders (5th edition). Washington, USA, American Psychiatric Association. |
3 | Anderson, L.J. , & Taylor, R.S. ((2014) ). Cardiac rehabilitation for people with heart disease: An overview of Cochrane systematic reviews. International Journal of Cardiology, 177: , 348–361. |
4 | Baizabal-Carvallo, J.F. , Hallett, M. , & Jankovic, J. ((2019) ). Pathogenesis and pathophysiology of functional (psychogenic) movement disorders. Neurobiology of Disease, 127: , 32–44. |
5 | Baker , Janet, , Caroline Barnett, , Lesley Cavalli, , Maria Dietrich, , Lorna Dixon, , Joseph R. Duffy, , Annie Elias, , Diane Fraser, E. , Jennifer Freeburn, L. , Catherine Gregory, , Kirsty McKenzie , Nick Miller , Jo Patterson, , Carole Roth, , Nelson Roy, , Jennifer Short, , Rene Utianski, , Miriam Van Mersbergen, , Anne Vertigan, , Alan Carson, , Jon Stone, , & Laura McWhirter, . (2021) . “Management of Functional Communication, Swallowing, Cough and Related Disorders: Consensus Recommendations for Speech and Language Therapy.” Journal of Neurology, Neurosurgery and Psychiatry, 92: (10), 1112–25. |
6 | Baslet, G. , Bajestan, S.N. , Aybek, S. , Modirrousta, M. , Price, J. , Cavanna, A. , Perez, D.L. , Lazarow, S.S. , Raynor, G. , Voon, V. , Ducharme, S. , & LaFrance, W.C. ((2021) ). Evidence-based practice for the clinical assessment of psychogenic nonepileptic seizures: a report from the American Neuropsychiatric Association Committee on Research. Journal of Neuropsychiatry and Clinical Neurosciences, 33: , 27–42. |
7 | Baslet, G. , Ehlert, A. , Oser, M. , & Dworetzky, B.A. ((2020) ). Mindfulness-based therapy for psychogenic nonepileptic seizures. Epilepsy & Behavior,, 103: , 106534. |
8 | Bègue, I. , Adams, C. , Stone, J. , & Perez, D.L. ((2019) ). Structural alterations in functional neurological disorder and related conditions: a software and hardware problem? NeuroImage: Clinical, 22: , 101798. |
9 | Carson, A.J. ((2004) ). Patients whom neurologists find difficult to hel. Journal of Neurology, Neurosurgery & Psychiatry, 75: , 1776–1778. |
10 | Carson, A. , Lehn, A. , Ludwig, L. , & Stone, J. ((2016) ). Explaining functional disorders in the neurology clinic: a photo story. Practical Neurology, 16: , 56–61. |
11 | Czarnecki, K. , Thompson, J.M. , Seime, R. , Geda, Y.E. , Duffy, J.R. , & Ahlskog, J.E. ((2012) ). Functional movement disorders: Successful treatment with a physical therapy rehabilitation protocol. Parkinsonism & Related Disorders, 18: , 247–251. |
12 | Delargy, M.A. , Peatfield, R.C. , & Burt, A.A. ((1986) ). Successful rehabilitation in conversion paralysis. British Medical Journal, 292: , 1730–1731. |
13 | Demartini, B. , Batla, A. , Petrochilos, P. , Fisher, L. , Edwards, M.J. , & Joyce, E. ((2014) ). Multidisciplinary treatment for functional neurological symptoms: a prospective study. Journal of Neurology, 261: , 2370–2377. |
14 | Espay, A.J. , Aybek, S. , Carson, A. , Edwards, M.J. , Goldstein, L.H. , Hallett, M. , LaFaver, K. , LaFrance, W.C. , Lang, A.E. , Nicholson, T. , Nielsen, G. , Reuber, M. , Voon, V. , Stone, J. , & Morgante, F. ((2018) ). Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurology, 75: , 1132–1141. |
15 | Espay, A.J. , Ries, S. , Maloney, T. , Vannest, J. , Neefus, E. , Dwivedi, A.K. , Allendorfer, J.B. , Wulsin, L.R. , LaFrance, W.C. , Lang, A.E. , & Szaflarski, J.P. ((2019) ). Clinical and neural responses to cognitive behavioral therapy for functional tremor. Neurology, 93: , e1787–e1798. |
16 | Fend, M. , Williams, L. , Carson, A.J. , & Stone, J. ((2020) ). The Arc de Siècle: functional neurological disorder during the ‘forgotten’ years of the th century. Brain, 143: , 1278–1284. |
17 | Galli, S. , Tatu, L. , Bogousslavsky, J. , & Aybek, S. ((2018) ). Conversion, factitious disorder and malingering: a distinct pattern or a continuum? Frontiers of Neurology and Neuroscience, 42,: , 72–80. |
18 | Gilmour, , Gabriela, S. , & Jessica Jenkins. D. (2021) . “Inpatient Treatment of Functional Neurological Disorder: A Scoping Review”. Canadian Journal of Neurological Sciences / Journal Canadien Des Sciences Neurologiques 48: (2), 204–17. |
19 | Gilmour, G.S. , Nielsen, G. , Teodoro, T. , Yogarajah, M. , Coebergh, J.A. , Dilley, M.D. , Martino, D. , & Edwards, M.J. ((2020) ). Management of functional neurological disorder. Journal of Neurology, 267: , 2164–2172. |
20 | Goldstein, L.H. , Robinson, E.J. , Mellers, J.D. , Stone, J. , Carson, A. , & Reuber, M. ((2020) ). Cognitive behavioural therapy for adults with dissociative seizures (CODES): a pragmatic, multicentre, randomised controlled trial. Lancet Psychiatry, 7: , 491–505. |
21 | Hallett, M. ((2006) ). Psychogenic movement disorders: A crisis for neurology. Current Neurology and Neuroscience Reports, 6: , 269–271. |
22 | Hebert, C. , Behel, J.M. , Pal, G. , Kasi, R. , & Kompoliti, K. ((2021) ). Multidisciplinary inpatient rehabilitation for Functional Movement Disorders: A prospective study with long term follow up. Parkinsonism and Related Disorders, 82: , 50–55. |
23 | Heruti, R. , Reznik, J. , Adunski, A. , Levy, A. , Weingarden, H. , & Ohry, A. ((2002) ). Conversion motor paralysis disorder: analysis of consecutive referrals. Spinal Cord, 40: , 335–340. |
24 | Inpatient Rehabilitation Facility - Patient Assessment Instrument. (2020). Baltimore, USA, Centers for Medicare & Medicaid Services. |
25 | Jacob, A.E. , Kaelin, D.L. , Roach, A.R. , Ziegler, C.H. , & LaFaver, K. ((2018) ). Motor Retraining (MoRe) for functional movement disorders: outcomes from a -week multidisciplinary rehabilitation program. PM&R, 10: , 1164–1172. |
26 | Jacob, A.E. , Smith, C.A. , Jablonski, M.E. , Roach, A.R. , Paper, K.M. , Kaelin, D.L. , Stretz-Thurmond, D. , & LaFaver, K. ((2018) ). Multidisciplinary clinic for functional movement disorders (FMD): -year experience from a single centre. Journal of Neurology, Neurosurgery & Psychiatry, 89: , 1011–1012. |
27 | Jordbru, A. , Smedstad, L. , Klungsøyr, O. , & Martinsen, E. ((2014) ). Psychogenic gait disorder: A randomized controlled trial of physical rehabilitation with one-year follow-up. Journal of Rehabilitation Medicine, 46: , 181–187. |
28 | Khan, F. , Ng, L. , Gonzalez, S. , Hale, T. , & Turner-Stokes, L. ((2008) ). Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database of Systematic Reviews, 16: , CD004957. |
29 | Langhorne, P. (Ed.). ((2001) ). Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews, 4: , CD000191. |
30 | Lehn, A. , Bullock-Saxton, J. , Newcombe, P. , Carson, A. , & Stone, J. ((2019) ). Survey of the perceptions of health practitioners regarding Functional Neurological Disorders in Australia. Journal of Clinical Neuroscience, 67: , 114–123. |
31 | Maggio, J.B. , Ospina, J.P. , Callahan, J. , Hunt, A.L , Stephen, C.D. , & Perez, D.L. ((2020) ). Outpatient physical therapy for functional neurological disorder: a preliminary feasibility and naturalistic outcome study in a U.S. cohort. Journal of Neuropsychiatry and Clinical Neurosciences, 32: , 85–89. |
32 | McKee, K. , Glass, S. , Adams, C. , Stephen, C.D , King, F. , Parlman, K. , Perez, D.L. , & Kontos, N. ((2018) ). The Inpatient assessment and management of motor functional neurological disorders: an interdisciplinary perspective. Psychosomatics, 59: , 358–368. |
33 | Nicholson, C. , Edwards, M.J. , Carson, A.J. , Gardiner, P. , Golder, D. , Hayward, K. , Humblestone, S. , Jinadu, H. , Lumsden, C. , MacLean, J , Main, L , Macgregor, L. , Nielsen, G. , Oakley, L. , Price, J. , Ranford, J. , Ranu, J. , Sum, E. , & Stone, J. ((2020) ). Occupational therapy consensus recommendations for functional neurological disorder. Journal of Neurology, Neurosurgery & Psychiatry,, 91: , 1037–1045. |
34 | Nicholson, T.R. , Carson, A. , Edwards, M.J. , Goldstein, L.H. , Hallett, M. , Mildon, B. , Nielsen, G. , Nicholson, C. , Perez, D.L. , Pick, S. , Stone, J. , Anderson, D. , Asadi-Pooya, A. , Aybek, S. , Baslet, G. , Bloem, B.R. , Brown, R.J. , Chalder, T. , Damianova, M. , . . . Tinazzi, M. ((2020) ). Outcome measures for functional neurological disorder: a review of the theoretical complexities. Journal of Neuropsychiatry and Clinical Neurosciences, 32: , 33–42. |
35 | Nielsen, G. , Buszewicz, M. , Stevenson, F. , Hunter, R. , Holt, K. , Dudziec, M. , Ricciardi, L. , Marsden, J. , Joyce, E. , & Edwards, M. ((2017) ). Randomised feasibility study of physiotherapy for patients with functional motor symptoms. Journal of Neurology, Neurosurgery & Psychiatr,, 88: , 484–490. |
36 | Nielsen, G. , Stone, J. , & Edwards, M.J. ((2013) ). Physiotherapy for functional (psychogenic) motor symptoms: a systematic review. Journal of Psychosomatic Research, 75: , 93–102. |
37 | Nielsen, G. , Stone, J. , Matthews, A. , Brown, M. , Sparkes, C. , Farmer, R. , Masterton, L. , Duncan, L. , Winters, A. , Daniell, L. , Lumsden, C. , Carson, A. , David, A.S. , & Edwards, M. ((2015) ). Physiotherapy for functional motor disorders: a consensus recommendation. Journal of Neurology, Neurosurgery& Psychiatry, 86: , 1113–1119. |
38 | Nordström, P. , Thorngren, K.-G. , Hommel, A. , Ziden, L. , & Anttila, S. ((2018) ). Effects of Geriatric Team rehabilitation after hip fracture: meta-analysis of randomized controlled trials. Journal of the American Medical Directors Association, 19: , 840–845. |
39 | Perez, D.L. , Aybek, S. , Popkirov, S. , Kozlowska, K. , Stephen, C.D. , Anderson, J. , Shura, R. , Ducharme, S. , Carson, A. , Hallett, M. , Nicholson, T.R. , Stone, J. , LaFrance, W.C. , & Voon, V. ((2021) ). A review and expert opinion on the neuropsychiatric assessment of motor functional neurological disorders. Journal of Neuropsychiatry and Clinical Neurosciences, 33: , 14–26. |
40 | Petrochilos, P. , Elmalem, M.S. , Patel, D. , Louissaint, H. , Hayward, K. , Ranu, J. , & Selai, C. ((2020) ). Outcomes of a -week individualised MDT outpatient (day-patient) treatment programme for functional neurological symptom disorder (FNSD. Journal of Neurology, 267: , 2655–2666. |
41 | Pick, S. , Anderson, D.G. , Asadi-Pooya, A.A. , Aybek, S , Baslet, G. , Bloem, B.R. , Bradley-Westguard, A. , Brown, R.J. , Carson, A.J. , Chalder, T. , Damianova, M. , David, A.S. , Edwards, M.J. , Epstein, S.A. , Espay, A.J. , Garcin, B. , Goldstein, L.H. , Hallett, M. , Jankovic, J. ,. . . Nicholson, T.R. ((2020) ). Outcome measurement in functional neurological disorder: a systematic review and recommendations. Journal of Neurology, Neurosurgery & Psychiatry, 91: , 638–649. |
42 | Prochaska, J.O. , Johnson, S. , & Lee, P. ((2009) ). The transtheoretical model of behavior change. In S.A. Shumaker, J.K. Ockene & K.A. Riekert (Eds.), Handbook of Health Behavior Change, 3rd edition (pp. 59-83). New York, Springer Publishing Company. |
43 | Rommelfanger, K.S. , Factor, S.A. , LaRoche, S. , Rosen, P. , Young, R. , & Rapaport, M.H. ((2017) ). Disentangling stigma from functional neurological disorders: conference report and roadmap for the future. Journal of Neurosurgery, 122: , 106. |
44 | Saifee, T.A. , Kassavetis, P. , Pareés, I. , Kojovic, M. , Fisher, L. , Morton, L. , Foong, J. , Price, G. , Joyce, E.M. , & Edwards, M.J. ((2012) ). Inpatient treatment of functional motor symptoms: a long-term follow-up study. Journal of Neurology,, 259: , 1958–1963. |
45 | Shapiro, A. ((1997) ). Strategic-behavioural intervention in the inpatient rehabilitation of non-organic (factitious/conversion) motor disorders. Neurorehabilitation, 8: , 183–192. |
46 | Shapiro, A.P. , & Teasell, R.W. ((2004) ). Behavioural interventions in the rehabilitation of acute v. chronic non-organic (conversion/factitious) motor disorders. British Journal of Psychiatry, 185: , 140–146. |
47 | Sharpe, M. , Walker, J. , Williams, C. , Stone, J. , Cavanagh, J. , Murray, G. , Butcher, I. , Duncan, R. , Smith, S. , & Carson, A. ((2011) ). Guided self-help for functional (psychogenic) symptoms: A randomized controlled efficacy trial. Neurology, 77: , 564–572. |
48 | Stephen, C. , Fung, V. , Lungu, C. , & Espay, A. ((2021) ). Assessment of emergency department and inpatient use and costs in adult and pediatric functional neurological disorders. JAMA Neurology, 78: , 88–101. |
49 | Stewart, T.D. ((1983) ). Hysterical conversion reactions: Some patient characteristics and treatment team reactions. Archives of Physical Medicine and Rehabilitation, 64: , 308–310. |
50 | Stone, J. , Carson, A. , Duncan, R. , Roberts, R. , Warlow, C. , Hibberd, C. , Coleman, R. , Cull, R. , Murray, G. , Pelosi, A. , Cavanagh, J. , Matthews, K. , Goldbeck, R. , Smyth, R. , Walker, J. , & Sharpe, M. ((2010) ). Who is referred to neurology clinics?—The diagnoses made in new patients. Clinical Neurology and Neurosurgery,, 112: , 747–751. |
51 | Stone, J. (2018). Functional Neurological Disorder (FND): a patient’s guide. https://www.neurosymptoms.org/ |
52 | Stone, J. , & Carson, A. ((2015) ). Functional neurologic disorders. Continuum,, 21: , 818–837. |
53 | Stone, J. , Carson, A. , Aditya, H. , Prescott, R. , Zaubi, M. , Warlow, C. , & Sharpe, M. ((2009) ). The role of physical injury in motor and sensory conversion symptoms: A systematic and narrative review. Journal of Psychosomatic Research, 66: , 383–390. |
54 | Stone, J. , & Edwards, M. ((2012) ). Trick or treat?: Showing patients with functional (psychogenic) motor symptoms their physical signs. Neurology, 79: , 282–284. |
55 | Williams, C. , Carson, A. , Smith, S. , Sharpe, M. , Cavanagh, J. , & Kent, C. ((2017) ). Overcoming Functional Neurological Symptoms: A Five Areas Approach. London, CRC Press. |
56 | Williams, D.T. , Lafaver, K. , Carson, A. , & Fahn, S. ((2016) ). Inpatient treatment for functional neurologic disorders. Handbook of Clinical Neurology, 139: , 631–641. |
57 | Yam, A. , Rickards, T. , Pawlowski, C.A. , Harris, O. , Karandikar, N. , Maya, V. , & Rickards, T. ((2015) ). Interdisciplinary rehabilitation approach for functional neurological symptom (conversion) disorder: a case study. Rehabilitation Psychology, 61: , 102–111. |
Notes
1 At the present institution, psychologists deliver behavioral health care during inpatient rehabilitation. Elsewhere this role may have been appropriate for other allied mental health professionals such as licensed clinical social workers.




