A national survey of evidence-based stroke rehabilitation intervention use in clinical practice among Canadian occupational therapists
Abstract
BACKGROUND:
More than 1,000 randomized controlled trials have been published examining the effectiveness of stroke rehabilitation interventions.
OBJECTIVE:
The objective of this study was to explore the use and non-use of evidence-based stroke rehabilitation interventions in clinical practice among Occupational Therapists across various stroke rehabilitation settings in Canada.
METHODS:
Participants were recruited from medical centres providing rehabilitation to stroke patients in each of the ten provinces across Canada (January-July 2021). Adult (18 + years) Occupational Therapists who provide direct rehabilitative care to individuals after a stroke completed a survey in either English or French. Therapists rated their awareness, use, and reasons for non-use of stroke rehabilitation interventions.
RESULTS:
127 therapists (female = 89.8%), largely from Ontario or Quebec (62.2%) were included; most worked full-time (80.3%) in moderate-large (86.1%) cities. The greatest use of interventions were those applied to the body peripherally, without a technological component. Few individuals were aware of interventions applied to the brain (priming or stimulating) with a technological component, and they were rarely, if ever, used.
CONCLUSION:
Significant efforts should be made to increase the awareness of interventions which are supported by strong evidence through knowledge translation and implementation initiatives, particularly for those with a technological component.
1Introduction
Stroke remains a leading cause of long-term disability in Canada (Canadian Institutes of Health Information, 2021). Occupational Therapists provide critical rehabilitative care to individuals after stroke (Legg et al., 2007) and are key members of the interdisciplinary stroke rehabilitation team. Broadly speaking, occupational therapy enables individuals across the life span to develop or restore their maximal performance of valued tasks through the therapeutic use of everyday activities (i.e., occupations) (American Occupational Therapy Association, 2021; Legg et al., 2007). Within the context of stroke rehabilitation, Occupational Therapists primarily focus on sitting and ambulatory exercises (De Wit et al., 2006), sensory, perceptual, and cognitive training (De Wit et al., 2006), as well as remediation of upper and lower extremity impairments, and functional task retraining (e.g., dressing) (Richards et al., 2005).
Occupational therapy is a client-centered profession where physical and mental activities are used to overcome limitations induced by post stroke sequela (Govender & Kalra, 2007). In instances where remediation is impossible, Occupational Therapists work with patients to develop compensatory strategies to promote independence (Govender & Kalra, 2007). Beyond patients’ clinical characteristics, Occupational Therapists’ choice of therapy or intervention to use in clinical practice may be influenced by therapists’ knowledge and expertise, logistical factors (e.g., time and cost), organizational factors (e.g., setting, specialization, expectations), clinical practice guidelines (e.g., Canadian Best Practice Guidelines for Stroke Rehabilitation (Teasell et al., 2020), and established research evidence.
An extensive number of unique therapies for use among Occupational Therapists have been studied with randomized controlled trials (RCTs) (McIntyre et al., 2014; Stroke Rehabilitation Evidence Based Review, 2020). The use of interventions with high quality, research evidence should be used in clinical practice to improve upper and lower extremity impairment, and cognitive impairment, in the post stroke population. However, despite significant advancements in stroke rehabilitation research, professionals including Occupational Therapists face continued challenges in amassing this evidence and translating it into clinical practice (Wressle & Samuelsson, 2014). The degree to which Occupational Therapists use diverse evidence-based interventions in stroke rehabilitation clinical practice is currently unknown in the empirical literature. There are longstanding calls for purposeful efforts to identify effective strategies for implementing research into practice (Juckett et al., 2019). An exploration of factors impeding intervention use in Occupational Therapy practice would be beneficial in informing this initiative. Thus, the purpose of this study was to explore the use and non-use of evidence-based stroke rehabilitation interventions in clinical practice among Occupational Therapists across various stroke rehabilitation settings in Canada.
2Methods
2.1Ethics, study design, reporting guidelines
This study received ethics approval by the Health Sciences Research Ethics Board at Western University (ID115889; January-July 2021). This study employed a cross-sectional, observational (non-experimental) design using a quantitative survey. This study has been reported using the STROBE guidelines for cross-sectional studies (Elm et al., 2007).
2.2Sample
Participants were recruited from medical centres providing rehabilitation to stroke patients in each of the ten provinces across Canada. Individuals could participate if they met the following inclusion criteria: 1) provided direct stroke rehabilitative care to individuals who have experienced a stroke; 2) held one of the following professional clinical roles: physiotherapist, occupational therapist, recreation therapist, therapeutic rehabilitation specialist, or speech language pathologist; 3) were 18 + years old; and 4) could read and write in English or French. For the purposes of the study described herein, only the data collected from Occupational Therapists were included for this analysis.
2.3Recruitment
Recruitment was conducted in two ways. First, contact was made with the regulated colleges for each discipline, in each province, and their general membership was invited to participate in the study (N = 62 organizations). Second, an exhaustive list was generated of all stroke rehabilitation medical centers in Canadian provinces (i.e., acute care, specialized rehabilitation, outpatient, community, etc.) (N = 212 centres); staff were invited to participate in the study via an email from the director or manager of each center. Individuals provided informed (written) consent to participate in the study.
2.4Data collection
Data were collected electronically via an online survey using the REDCap (Research Electronic Data Capture) platform. An electronic survey (Appendix A) captured participants’ demographic information (e.g., professional role, employment status and the medical setting in which they worked), clinical caseload (e.g., type of patients they typically work with and how often) and knowledge uptake (how they stay up to date with respect to rehabilitation interventions). Respondents were asked to review a list of interventions and select which ones they used and how frequently. For interventions that they did not use, respondents were asked to select the reasons for non-use (multiple selections were allowed). The list of interventions selected for inclusion in the survey have previously been studied in stroke rehabilitation RCTs involving subjects post stroke. They are interventions that target functional participation in self-care activities, including functional mobility and equipment use, upper and lower extremity rehabilitation, apraxia, and cognitive rehabilitation. The decision to include these interventions was based on, and supported by, a comprehensive review of the existing literature on Occupational Therapy rehabilitation post stroke (Saikaley & Pauli, 2022; Saikaley, 2022), as well as the Canadian Stroke Best Practice Recommendations (Teasell et al., 2020). Answers were mostly closed-ended, and the survey took approximately 10 minutes to complete.
2.5Data analysis
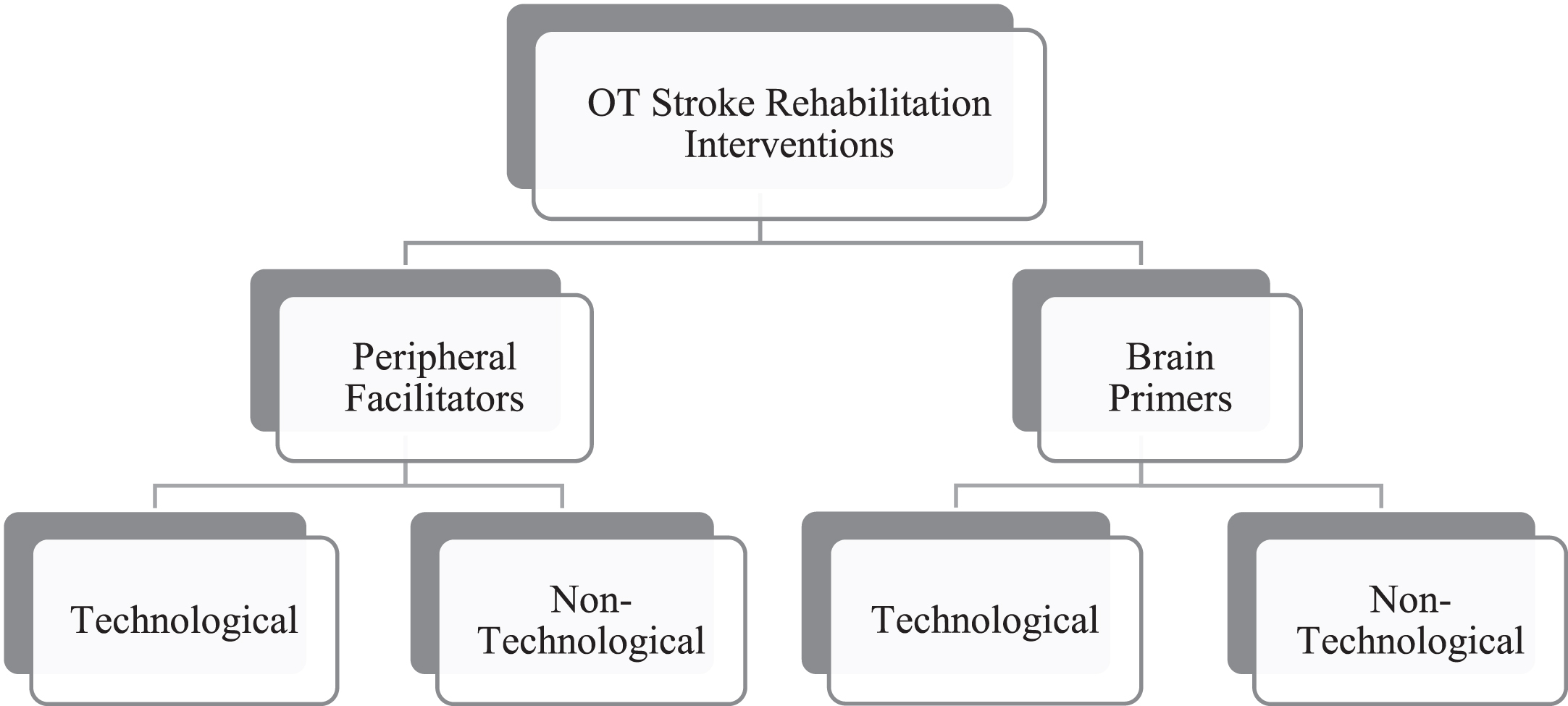
Study data was exported from REDCap to Microsoft Excel for analysis. Categorical data were grouped and reported as counts and percentages. Use and non-use of interventions were compared within and across four major intervention categories (Fig. 1), and with respect to rehabilitation setting (i.e., inpatient versus outpatient), degree of specialization (general versus specialized), and years of employment experience. There were four major categories: (a) technological peripheral facilitators; (b) technological brain primers; (c) non-technological peripheral facilitators; and (d) non-technological brain primers. Technological interventions were those which depended on electrical or mechanical devices designed to help people recover upper or lower limb movement or cognitive function (Naudé & Hughes, 2005). Peripheral facilitators referred to therapeutic interventions that facilitate motor activities physically at a peripheral level (e.g., robotics, functional electrical stimulation, constraint-induced movement therapy [CIMT]). Conversely, brain primers referred to treatments that specifically prime or stimulate the brain (e.g., action observation, mirror therapy, virtual reality, rTMS) (Teasell et al., 2022).
Fig. 1
Framework of OT Stroke Rehabilitation Interventions.
3Results
3.1Demographics and employment
A total of 301 survey participants responded (61.7% response rate), and a total of 127 (35.0%) respondents identified as Occupational Therapists which was the second largest group of respondents for this survey (Table 1). The majority of Occupational Therapists were females (89.8%) from the provinces of Ontario (40.2%), Quebec (22.0%) and Alberta (17.3%). Therapists worked predominately full-time (80.3%) in moderate (22.0%) to large (66.1%) urban centers. Institutional employment settings were largely balanced across acute care hospitals (30.7%), academic rehabilitation centers (26.0%), and community hospitals (20.5%). Nearly one third of Occupational Therapists worked on specialized rehabilitation units (29.9%). Most therapists worked in a rehabilitation environment with fewer than ten other therapists (80.3%), saw less than ten patients per week (66.9%), and delivered less than ten visits per patient per week (78.7%). Occupational Therapists reported staying up to date primarily monthly (48.8%) or yearly (27.6%) using a variety of methods; most often, they sought information from other therapists (85.8%), attending conferences (81.3%), reviewing guidelines (75.6%), or obtaining updates from a local practice leader (50.4%).
Table 1
Sample and setting characteristics for total sample (N = 363) and occupational therapists only (N = 127)
| Subject characteristics | Total sample (N = 363) | Occupational therapists (N = 127) | ||
| # | % | # | % | |
| Sex | ||||
| Female | 314 | 86.5% | 114 | 89.8% |
| Male | 34 | 9.4% | 8 | 6.3% |
| Blank | 15 | 4.1% | 5 | 3.9% |
| Province | ||||
| Alberta | 60 | 16.5% | 22 | 17.3% |
| British Columbia | 24 | 6.6% | 7 | 5.5% |
| Manitoba | 3 | 0.8% | 0 | 0.0% |
| New Brunswick | 13 | 3.6% | 1 | 0.8% |
| Newfoundland & Labrador | 20 | 5.5% | 3 | 2.4% |
| Nova Scotia | 20 | 5.5% | 10 | 7.9% |
| Ontario | 141 | 38.8% | 51 | 40.2% |
| Quebec | 62 | 17.1% | 28 | 22.0% |
| Saskatchewan | 19 | 5.2% | 5 | 3.9% |
| Blank | 1 | 0.3% | 0 | 0.0% |
| Current employment status | ||||
| Full-Time | 279 | 76.9% | 102 | 80.3% |
| Part-Time | 78 | 21.5% | 22 | 17.3% |
| Casual | 5 | 1.4% | 2 | 1.6% |
| Blank | 1 | 0.3% | 1 | 0.8% |
| Length of time employed | ||||
| 0–5 years | 69 | 19.0% | 22 | 17.3% |
| 6–10 years | 72 | 19.8% | 27 | 21.3% |
| 11–20 years | 116 | 32.0% | 43 | 33.9% |
| 20 + years | 105 | 28.9% | 35 | 27.6% |
| Blank | 1 | 0.3% | 0 | 0.0% |
| Institution type | ||||
| Academic rehabilitation centre | 76 | 20.9% | 33 | 26.0% |
| Acute care hospital | 123 | 33.9% | 39 | 30.7% |
| Community hospital | 74 | 20.4% | 26 | 20.5% |
| Independent community rehabilitation clinic | 12 | 3.3% | 4 | 3.1% |
| Other | 49 | 13.5% | 16 | 12.6% |
| Rehab service linked to a community medical practice | 48 | 13.2% | 9 | 7.1% |
| Rehab setting | ||||
| Acute care stroke rehab team (dedicated unit) | 65 | 17.9% | 23 | 18.1% |
| Acute care stroke rehab team (no dedicated unit/mobile team) | 32 | 8.8% | 12 | 9.4% |
| General outpatient rehab service (hos/com) | 35 | 9.6% | 11 | 8.7% |
| General rehab unit (< 50% caseload is stroke) | 40 | 11.0% | 13 | 10.2% |
| General rehab unit (> 50% caseload is stroke) | 51 | 14.0% | 15 | 11.8% |
| Specialized neurorehab outpatient (hospital/community) | 43 | 11.8% | 15 | 11.8% |
| Specialized rehab unit (> 80% caseload is stroke) | 93 | 25.6% | 38 | 29.9% |
| Blank | 4 | 1.1% | 0 | 0.0% |
| Community size | ||||
| ≤999 | 3 | 0.8% | 1 | 0.8% |
| 1,000–29,000 | 41 | 11.3% | 11 | 8.7% |
| 30,000–99,999 | 71 | 19.6% | 28 | 22.0% |
| ≥100,000 | 241 | 66.4% | 84 | 66.1% |
| Blank | 6 | 1.7% | 3 | 2.4% |
| # Therapists | ||||
| 1–9 | 312 | 86.0% | 102 | 80.3% |
| 10–19 | 29 | 8.0% | 14 | 11.0% |
| 20–49 | 13 | 3.6% | 9 | 7.1% |
| 50+ | 4 | 1.1% | 1 | 0.8% |
| Blank | 5 | 1.4% | 1 | 0.8% |
| # Beds | ||||
| 0 | 15 | 4.1% | 5 | 3.9% |
| 1–9 | 16 | 4.4% | 7 | 5.5% |
| 10–29 | 108 | 29.8% | 36 | 28.3% |
| 30–49 | 116 | 32.0% | 40 | 31.5% |
| 50+ | 47 | 12.9% | 20 | 15.7% |
| Blank | 62 | 17.1% | 19 | 15.0% |
| # Stroke pts seen | ||||
| 0 | 2 | 0.6% | 1 | 0.8% |
| 1–4 | 114 | 31.4% | 33 | 26.0% |
| 5–9 | 143 | 39.4% | 52 | 40.9% |
| 10–14 | 50 | 13.8% | 20 | 15.7% |
| 15+ | 44 | 12.1% | 19 | 15.0% |
| Blank | 11 | 3.0% | 3 | 2.4% |
| # Visits | ||||
| 0 | 1 | 0.3% | 1 | 0.8% |
| 1 | 34 | 9.4% | 10 | 7.9% |
| 2–4 | 135 | 37.2% | 45 | 35.4% |
| 5–9 | 155 | 42.7% | 55 | 43.3% |
| 10+ | 24 | 6.6% | 10 | 7.9% |
| Blank | 14 | 3.9% | 6 | 4.7% |
| How do you stay up to date? | ||||
| Research involvement | 61 | 16.8% | 22 | 17.3% |
| Journal club | 36 | 9.9% | 8 | 6.3% |
| Special interest group w/ college | 48 | 13.2% | 14 | 11.0% |
| Review of guidelines (independent or group) | 247 | 68.0% | 96 | 75.6% |
| Local update from practice leader | 151 | 41.6% | 64 | 50.4% |
| Conference attendance | 248 | 68.3% | 102 | 80.3% |
| Other therapists | 291 | 80.2% | 109 | 85.8% |
| Other | 59 | 16.3% | 19 | 15.0% |
| I have not stayed up-to-date | 3 | 0.8% | 0 | 0.0% |
| How often do they stay up-to-date? | ||||
| Daily | 8 | 2.2% | 1 | 0.8% |
| Weekly | 59 | 16.3% | 22 | 17.3% |
| Monthly | 172 | 47.4% | 62 | 48.8% |
| Yearly | 113 | 31.1% | 35 | 27.6% |
| >Yearly | 9 | 2.5% | 6 | 4.7% |
3.2Use and frequency of use
Table 2 shows the number of Occupational Therapists who reported using each intervention (categorized by the four therapy types) and the frequency with which the intervention was used. Among 15 non-technological peripheral facilitators, just 5 interventions were reportedly used by more than half of the sample (52.0–72.4%): wheelchairs, strength training, task-specific training, trunk training, and neurodevelopmental techniques. These interventions were used most often on a weekly basis. Conversely, the remaining 10 non-technological peripheral facilitators were hardly used by therapists and were applied with highly variable frequency.
Table 2
Rate of use and frequency of use of stroke rehabilitation interventions among occupational therapists (N = 127)
| Occupational therapist stroke rehabilitation interventions | Use of intervention | Frequency of use | |||
| Weekly | Monthly | Yearly | |||
| # | % | # | # | # | |
| Non-technological – Peripheral facilitators | |||||
| Wheelchair use | 92 | 72.4% | 73 | 11 | 7 |
| Strength training | 88 | 69.3% | 79 | 7 | 2 |
| Task-specific training | 88 | 69.3% | 81 | 7 | 0 |
| Trunk training | 75 | 59.1% | 61 | 11 | 3 |
| Neurodevelopmental techniques | 66 | 52.0% | 55 | 7 | 4 |
| Constraint induced movement therapy | 61 | 48.0% | 17 | 19 | 25 |
| Orthotics | 50 | 39.4% | 11 | 28 | 10 |
| Cycle ergometer | 39 | 30.7% | 22 | 11 | 5 |
| Thermal stimulation | 17 | 13.4% | 9 | 5 | 3 |
| Massage therapy | 16 | 12.6% | 9 | 6 | 1 |
| Yoga | 9 | 7.1% | 2 | 5 | 2 |
| Tai chi | 9 | 7.1% | 4 | 1 | 4 |
| Pilates | 4 | 3.1% | 0 | 3 | 1 |
| Aquatic therapy | 4 | 3.1% | 0 | 2 | 2 |
| Acupuncture | 0 | 0.0% | 0 | 0 | 0 |
| Non-technological – brain primers | |||||
| Bilateral arm training | 86 | 67.7% | 59 | 17 | 2 |
| Mirror therapy | 76 | 59.8% | 27 | 29 | 20 |
| Mental practice | 62 | 48.8% | 34 | 22 | 6 |
| Dual task training (cognitive motor interference) | 50 | 39.4% | 37 | 11 | 2 |
| Ideomotor apraxia training | 48 | 37.8% | 18 | 23 | 7 |
| Action observation | 46 | 36.2% | 42 | 3 | 1 |
| Music-based therapy | 16 | 12.6% | 3 | 6 | 6 |
| Rhythmic auditory stimulation | 4 | 3.1% | 0 | 1 | 3 |
| Technological – peripheral facilitators | |||||
| Functional electrical stimulation | 66 | 52.0% | 33 | 19 | 14 |
| Neuromuscular electrical stimulation | 33 | 26.0% | 21 | 14 | 8 |
| Muscle vibration | 33 | 26.0% | 18 | 4 | 11 |
| Transcutaneous electrical nerve stimulation | 14 | 11.0% | 2 | 7 | 5 |
| Robotics/electromechanical devices | 5 | 3.9% | 0 | 2 | 3 |
| Interferential current therapy | 3 | 2.4% | 1 | 1 | 1 |
| Functional magnetic neuromuscular stimulation | 2 | 1.6% | 0 | 1 | 1 |
| Electroacupuncture | 0 | 0.0% | 0 | 0 | 0 |
| Extracorporeal shockwave therapy | 0 | 0.0% | 0 | 0 | 0 |
| Repetitive peripheral magnetic stimulation | 0 | 0.0% | 0 | 0 | 0 |
| Technological – brain primers | |||||
| Biofeedback | 86 | 67.7% | 26 | 12 | 2 |
| Computer-based cognitive therapy | 45 | 35.4% | 21 | 19 | 5 |
| Virtual reality | 10 | 7.9% | 4 | 3 | 3 |
| Galvanic vestibular stimulation | 1 | 0.8% | 0 | 0 | 1 |
| Transcranial direct current stimulation | 0 | 0.0% | 0 | 0 | 0 |
| Repetitive transcranial magnetic stimulation | 0 | 0.0% | 0 | 0 | 0 |
| Theta burst stimulation | 0 | 0.0% | 0 | 0 | 0 |
Only two of the eight non-technological brain primers were reportedly used by more than half of all therapists (i.e., bilateral arm training, 67.7% and mirror therapy, 59.8%), primarily on a weekly basis. Of note, although dual task training (39.4%) and action observation (36.2%) were used by a modest proportion of respondents, these therapists reported using them weekly.
Among all the technological interventions, just two were used by more than half of the sample: functional electrical stimulation (peripheral facilitator, 52.0%) and biofeedback (brain primer, 37.7%). The remaining technological interventions were rarely used by therapists. Of note, six interventions were reportedly not used by any therapist: electroacupuncture, extracorporeal shockwave therapy, repetitive peripheral magnetic stimulation, transcranial direct current stimulation, repetitive transcranial magnetic stimulation, theta burst stimulation.
The use of stroke rehabilitation interventions was stratified by therapists’ respective rehabilitation settings and degree of specialization (Supplementary Table 1), as well as their number of years employed (Supplementary Table 2). Except for the following trends, there were no major differences between therapists from different rehabilitation settings in their use of interventions. Constraint induced movement therapy and cycle ergometry were used by a greater number of therapists in specialized outpatient settings compared to specialized inpatient settings or general rehabilitation settings. Fewer therapists from specialized inpatient settings reported using wheelchairs, strength training, task-specific training, and neurodevelopmental techniques compared to specialized outpatient setting or general rehabilitation settings. In general, a greater number of therapists with long employment experiences (10 + years) tended to use a greater number and variety of stroke rehabilitation interventions.
3.3Non-use and reasons for non-use
Table 3 shows the number of Occupational Therapists who did not use each intervention (categorized by the four therapy types) and the reason(s) for non-use. Except for awareness, respondents were able to select multiple reasons for not using an intervention.
Table 3
Rate of non-use and reasons for non-use of stroke rehabilitation interventions among occupational therapists
| Occupational therapist stroke rehabilitation interventions | Non-use of the intervention | Internal factors* | External factors* | ||||||
| Unaware of the intervention | Unsure where to learn | Outside role/scope | Lack of evidence | Time | Cost | No access | |||
| # | % | # | # | # | # | # | # | # | |
| Non-technological – peripheral facilitators | |||||||||
| Acupuncture | 127 | 100.0 | 43 | 6 | 62 | 3 | 1 | 3 | 8 |
| Aquatic therapy | 123 | 96.9 | 50 | 1 | 4 | 0 | 6 | 3 | 43 |
| Pilates | 123 | 96.9 | 66 | 8 | 31 | 4 | 2 | 0 | 1 |
| Yoga | 118 | 92.9 | 51 | 10 | 35 | 1 | 10 | 2 | 6 |
| Tai chi | 118 | 92.9 | 53 | 9 | 31 | 6 | 9 | 1 | 7 |
| Massage therapy | 111 | 87.4 | 47 | 1 | 57 | 1 | 0 | 0 | 2 |
| Thermal stimulation | 110 | 86.6 | 91 | 3 | 4 | 2 | 2 | 1 | 2 |
| Cycle ergometer | 88 | 69.3 | 65 | 0 | 10 | 2 | 0 | 0 | 6 |
| Orthotics | 77 | 60.6 | 39 | 1 | 30 | 0 | 0 | 0 | 2 |
| Constraint induced movement therapy | 66 | 52.0 | 31 | 1 | 6 | 4 | 10 | 1 | 1 |
| Neurodevelopmental techniques | 61 | 48.0 | 45 | 6 | 2 | 2 | 1 | 1 | 0 |
| Trunk training | 52 | 40.9 | 45 | 0 | 4 | 0 | 1 | 0 | 0 |
| Strength training | 39 | 30.7 | 34 | 0 | 5 | 0 | 0 | 0 | 0 |
| Task-specific training | 39 | 30.7 | 36 | 1 | 1 | 0 | 1 | 0 | 0 |
| Wheelchair use | 35 | 27.6 | 32 | 0 | 3 | 0 | 0 | 0 | 0 |
| Non-technological – brain primers | |||||||||
| Rhythmic auditory stimulation | 123 | 96.9 | 120 | 1 | 1 | 1 | 0 | 0 | 0 |
| Music-based therapy | 111 | 87.4 | 57 | 6 | 24 | 1 | 8 | 1 | 7 |
| Action observation | 81 | 63.8 | 71 | 1 | 0 | 0 | 2 | 2 | 3 |
| Ideomotor apraxia training | 79 | 62.2 | 68 | 3 | 2 | 1 | 0 | 1 | 2 |
| Dual task training (cognitive motor interference) | 77 | 60.6 | 64 | 5 | 0 | 2 | 4 | 0 | 0 |
| Mental practice | 65 | 51.2 | 58 | 3 | 1 | 1 | 0 | 0 | 0 |
| Mirror therapy | 51 | 40.2 | 33 | 3 | 3 | 4 | 2 | 0 | 5 |
| Bilateral arm training | 41 | 32.3 | 28 | 1 | 3 | 1 | 1 | 0 | 1 |
| Technological - peripheral facilitators | |||||||||
| Electroacupuncture | 127 | 100.0 | 111 | 0 | 13 | 0 | 1 | 2 | 1 |
| Extracorporeal shockwave therapy | 127 | 100.0 | 115 | 3 | 6 | 1 | 0 | 1 | 3 |
| Repetitive peripheral magnetic stimulation | 127 | 100.0 | 123 | 1 | 2 | 3 | 0 | 0 | 1 |
| Functional magnetic neuromuscular stimulation | 125 | 98.4 | 99 | 2 | 15 | 0 | 1 | 3 | 12 |
| Interferential current therapy | 124 | 97.6 | 107 | 0 | 8 | 3 | 0 | 0 | 3 |
| Robotics/electromechanical devices | 122 | 96.1 | 79 | 4 | 4 | 1 | 5 | 14 | 27 |
| Transcutaneous electrical nerve stimulation | 113 | 89.0 | 85 | 2 | 20 | 0 | 1 | 2 | 6 |
| Neuromuscular electrical stimulation | 94 | 74.0 | 53 | 2 | 8 | 0 | 2 | 2 | 5 |
| Muscle vibration | 94 | 74.0 | 81 | 0 | 2 | 3 | 0 | 0 | 6 |
| Functional electrical stimulation | 61 | 48.0 | 39 | 2 | 13 | 0 | 0 | 0 | 7 |
| Technological - brain primers | |||||||||
| Repetitive transcranial magnetic stimulation | 127 | 100.0 | 102 | 2 | 17 | 1 | 1 | 0 | 10 |
| Theta burst stimulation | 127 | 100.0 | 127 | 0 | 0 | 0 | 0 | 0 | 0 |
| Transcranial direct current stimulation | 127 | 100.0 | 106 | 4 | 13 | 1 | 0 | 1 | 11 |
| Galvanic vestibular stimulation | 126 | 99.2 | 115 | 1 | 7 | 1 | 0 | 1 | 3 |
| Virtual reality | 117 | 92.1 | 47 | 6 | 3 | 4 | 13 | 16 | 56 |
| Computer-based cognitive therapy | 82 | 64.6 | 46 | 6 | 1 | 4 | 4 | 7 | 23 |
| Biofeedback | 41 | 32.3 | 37 | 12 | 5 | 0 | 6 | 5 | 28 |
Note: Survey respondents were able to select multiple options.
A significant proportion of therapists reported not using 9 of the 15 non-technological peripheral facilitators (60.6–100.0%). Other than lack of awareness (primary reason for non-use), many therapists reported that acupuncture, massage therapy Pilates, yoga, Tai Chi, thermal stimulation, cycle ergometry and orthotics were outside of their role or professional scope of practice. Conversely, respondents indicated that lack of access was a secondary reason for not using aquatic therapy.
Among eight non-technological brain primers, five interventions were reportedly unused by 60.6–96.9% of Occupational Therapists, with most of them indicating a lack of awareness of these stroke rehabilitation interventions as their primary reason for non-use. A modest proportion of therapists (21.6%) alternatively reported that music-based therapy was outside of their scope of practice.
Most respondents indicated they did not use any of the ten technological peripheral facilitators (48.0–100.0%) nor six of the seven technological brain primers (64.6–100.0%). When prompted for reasons for non-use, respondents overwhelmingly stated that they were unaware of technological interventions whether they were peripheral facilitators (80.1%) or brain primers (77.6%). For therapists that were aware of these technologies, cited reasons for non-use included a lack of access (10.9%) or the perception that it was outside of their professional scope of practice (7.4%).
4Discussion
Based on a Canadian national survey, the findings from this study showed that Occupational Therapists were largely unaware of evidence-based stroke rehabilitation interventions, and that this is a primary reason for not using them in clinical practice (71.2%). A significant proportion of therapists held the perception that the use of these interventions was outside of their professional role or scope of practice. Infrequently cited reasons for non-use included lack of access (7.9%), being unsure where to learn (3.1%), lack of time (2.5%), cost (1.8%), and insufficient scientific evidence (1.5%). The findings also showed that therapists with more knowledge of evidence-based interventions used them more often in clinical practice, particularly among those working in specialized outpatient rehabilitation settings and with long-term employment.
Non-technological, peripheral facilitators were well-known and used by Occupational Therapists. These interventions are, for the most part, well aligned with conventional Occupational Therapy rehabilitation therapies and training where the focus is on the use of meaningful activities and exercises targeting individualized goals, including functional independence (Canadian Association of Occupational Therapists, 2016). This approach is shaped by pragmatic recovery needs and increasingly governed by standardized guidelines and principles. A notable outlier among this group was constraint induced movement therapy which had low-moderate use, despite being well known among therapists. This may be explained by its time-intensive protocol relative to other conventional therapies. Traditional CIMT requires approximately 6 hours of direct patient interaction per day (Uswatte et al., 2006; Viana & Teasell, 2012) while modified CIMT is less time-intensive but can still be difficult for patients.
Among non-technological, brain priming interventions, awareness and use was greatest for mirror therapy and BAT. There is strong evidence for these two particular interventions in the research literature (Saikaley, 2022), and in combination with the limited resources required to perform them, may help to explain their high uptake in clinical practice. Of note, for all non-technological interventions, Occupational Therapists from specialized outpatient settings reported the greatest awareness and use relative to the other rehabilitation settings. Patients attending outpatient therapy tend to be later post stroke at a time when recovery is more likely to be plateauing (Cassidy & Cramer, 2017; Kwakkel et al., 2003; Langhorne et al., 2011). We speculate that outpatient Occupational Therapists may seek out new or alternative therapies to prolong recovery, overcome persistent impairments, or address new considerations in the chronic phase of stroke.
Overall, Occupational Therapists had severely limited awareness and almost complete lack of use of technological stroke rehabilitation interventions. Notable exceptions were for functional electrical stimulation and neuromuscular stimulation which was highest in specialized inpatient and outpatient settings. Research shows that these two interventions, in particular, are superior for improving activities of daily living compared to conventional therapy alone (Howlett et al., 2015; Kristensen et al., 2022). The remaining interventions represent more recent, emerging technology in stroke rehabilitation with mounting scientific evidence (Aprile et al., 2020; Laver et al., 2017). Therapists in our study indicated that, other than lack of awareness, they did not use technological interventions because they felt that it was outside of their role or scope (lack of exposure), were unsure how to use the therapy (inadequate training) or did not have access. Regarding exposure, this survey highlighted that Occupational Therapists keep up to date primarily through attendance at conferences, journal club participation and discussion with other therapists. While research in this area is not exactly novel, it is still emerging and may not yet be considered relevant or practical enough to be part of, or have a significant presence at, a conference or topic list for journal discussion. This survey also identified that the foundational skills, tools used, and clinician awareness is shaped by what is learned initially in Occupational Therapy training. Early career participants in our study had similar practice and level of awareness to those later in their career which may suggest that discussion of, or training in, the use of these technologies has not yet been accentuated. Finally, with respect to access, despite encouraging research, regional health regulatory agencies may be at variable stages of approval which directly impacts therapists’ access to these devices. For example, repetitive transcranial stimulation has only received Health Canada approval for the treatment of depression and experimental research, irrespective of the evidence supporting its use in treating subacute and chronic motor recovery, coordination, swallowing, aphasia, and neglect (Lefaucheur et al., 2020). Newer technologies also tend to have higher equipment costs. Costs are expected to decrease with general adoption; however, current costs may be prohibitive particularly in a publicly funded system with competing priorities. It is also important to consider the cost and availability of training which can be difficult to obtain as devices are highly specialized tools that are not generally available. Training requires time, both personal and away from clinical work, as well as costs associated with travel and education.
4.1Implications to practice and research
Using interventions with the highest evidence is critical to the recovery of patients after stroke. Each intervention included in our survey has been extensively studied in the scientific literature via RCTs; some interventions have been studied in over 100 RCTs. If therapists are to consider and incorporate new interventions in the treatment of their patients, they must have some awareness of the literature and the ability to critically appraise the evidence. To date, clinicians have been expected to independently evaluate the literature. Unfortunately, the findings from this study demonstrated a significant lack of awareness of stroke rehabilitation interventions from the literature among Occupational Therapists. Awareness is a precursor for intervention use in clinical practice although it is not always a guarantee. The literature on knowledge translation (KT) and implementation science for health professionals has found that uptake of evidence in clinical practice is limited (Thomas & Bussières, 2021). In a recent survey, Barrimore et al. (2020) found that therapists had moderate confidence in identifying evidence-practice gaps and were even less confident in implementing practice changes.
We found that early career clinicians had the lowest awareness and use across all stroke rehabilitation intervention categories. This is concerning given that Canadian university programs in rehabilitation, including occupational therapy, physiotherapy and speech language pathology focus on evidence-based practice (EBP), and define essential competencies for practice based upon the scientific literature (Hallé et al., 2021). Despite interest by clinicians in KT (Barrimore et al., 2020), and the academic commitment by Canadian post-secondary institutions to teach competencies associated with EBP (Hallé et al., 2021), KT has primarily focused on how to expose the end-user to the evidence and not how to integrate the evidence (Thomas & Ellaway, 2021). There is currently a drive in post-secondary institutions to instruct learners on how to use scientific evidence to address key clinical questions (Hallé et al., 2021). Unfortunately, most learners report a lack of time to apply EBP, as well as limited modeling of EBP by clinicians as two of several barriers to developing this skill (Hallé et al., 2021). Linking EBP to clinical rotations is an important strategy to learn how to gain technical and clinical reasoning skills and implement EBP (Hallé et al., 2021).
Future research should explore the clinical implementation of key stroke rehabilitation interventions directly into occupational therapy clinical practice and identify solutions to overcome barriers as identified in this study. Additionally, studies should compare adjunct interventions alone and in combination with conventional therapies or other adjunct therapies to explore their impact on stroke recovery. This would assist clinicians in combining interventions to best meet individualized patient needs (i.e., personalized care) in the context of the physical or fiscal restrictions of their practice environments. As therapists gain experience with technological and non-technological brain primers or peripheral facilitators, new research questions will arise as to their optimal clinical application. Finally, clinical practice guidelines could more explicitly consider the role of adjuvants, where they are best applied, and the potential synergies with standardized or conventional care.
4.2Limitations
The goal of the survey was to reach Occupational Therapists across Canada, treating stroke survivors across the continuum of care, in both urban and rural settings. Respondents were from all provinces; however, the sample had a greater representation from Ontario, Quebec, and Alberta. Due to regulatory challenges, the survey was not sent to therapists in the Yukon, Northwest Territories or Nunavut. Also, most respondents were from moderate to large size urban centres. While this is representative of the population of Canada and the distribution of therapists, it is not clear what unique challenges are faced in more rural settings.
5Conclusions
The use of stroke rehabilitation interventions among Occupational Therapists was greatest for those that align best with foundational training for the profession, with most aligning best with peripheral facilitators, which have low or no technological component. For technological interventions, awareness and use among therapists was generally low regardless of its classification as a peripheral facilitator or brain primer. Lack of awareness clearly impacts adoption, as well as cost, and assumed need for training. Keeping up to date with the large evidence base in stroke rehabilitation is an extremely difficult task. This is particularly challenging since the primary means of staying up-to-date for therapists was through colleague discussions, annual conferences, or guideline reviews, which typically are unable to provide a good summary of the available data for individual therapies. There is a need for peer reviews of the different interventions or a similar web-based archive of stroke rehabilitation literature, providing a critical analysis of the available data, such as the Stroke Rehabilitation Evidenced Based Review (2020). With an understanding of available occupational therapy interventions, as well as their impact on a variety of meaningful outcomes, therapists will be able to advocate for additional training as well funding for equipment to positively impact patients in their practice.
Acknowledgments
None to report.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding
None to report.
Supplementary materials
[1] The supplementary tables are available from https://dx.doi.org/10.3233/NRE-220279.
References
1 | American Occupational Therapy Association. (2021). About Occupational Therapy. https://www.aota.org/About-Occupational-Therapy.aspx |
2 | Aprile, I. , Germanotta, M. , Cruciani, A. , Loreti, S. , Pecchioli, C. , Cecchi, F. , Montesano, A. , Galeri, S. , Diverio, M. , Falsini, C. , Speranza, G. , Langone, E. , Papadopoulou, D. , Padua, L. , & Carrozza, M. C. ((2020) ). Upper limb robotic rehabilitation after stroke: A multicenter, randomized clinical trial. Journal of Neurological Physical Therapy 44: (1), 3–14. https://doi.org/10.1097/npt.0000000000000295 |
3 | Barrimore, S. E. , Cameron, A. E. , Young, A. M. , Hickman, I. J. , & Campbell, K. L. ((2020) ). Translating research into practice: How confident are allied health clinicians? Journal of Allied Health 49: (4), 258–262. |
4 | Canadian Association of Occupational Therapists. (2016). What is Occupational Therapy? https://www.caot.ca/site/aboutot/whatisot?nav=sidebar |
5 | Canadian Institutes of Health Information. (2021). Improved stroke data means better care and outcomes for patients. Retrieved October 4 from https://www.cihi.ca/en/improved-stroke-data-means-better-care-and-outcomes-for-patients |
6 | Cassidy, J. M. , & Cramer, S. C. ((2017) ). Spontaneous and therapeutic-induced mechanisms of functional recovery after stroke. Translational Stroke Research 8: (1), 33–46. https://doi.org/10.1007/s12975-016-0467-5 |
7 | De Wit, L. , Putman, K. , Lincoln, N. , Baert, I. , Berman, P. , Beyens, H. , Bogaerts, K. , Brinkmann, N. , Connell, L. , Dejaeger, E. , De Weerdt, W. , Jenni, W. , Lesaffre, E. , Leys, M. , Louckx, F. , Schuback, B. , Schupp, W. , Smith, B. , & Feys, H. ((2006) ). Stroke Rehabilitation in Europe. Stroke 37: (6), 1483–1489. https://doi.org/10.1161/01.STR.0000221709.23293.c2 |
8 | Elm, E. v. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. ((2007) ). Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335: (7624), 806–808. https://doi.org/10.1136/bmj.39335.541782.AD |
9 | Govender, P. , & Kalra, L. ((2007) ). Benefits of occupational therapy in stroke rehabilitation. Expert Review of Neurotherapeutics 7: (8), 1013–1019. https://doi.org/10.1586/14737175.7.8.1013 |
10 | Hallé, M. C. , Bussières, A. , Asseraf-Pasin, L. , Storr, C. , Mak, S. , Root, K. , & Thomas, A. ((2021) ). Building evidence-based practice competencies among rehabilitation students: a qualitative exploration of faculty and preceptors’ perspectives. Advances in Health Science Education Theory Practice 26: (4), 1311–1338. https://doi.org/10.1007/s10459-021-10051-0 |
11 | Howlett, O. A. , Lannin, N. A. , Ada, L. , & McKinstry, C. ((2015) ). Functional electrical stimulation improves activity after stroke: a systematic review with meta-analysis. Archives of Physical Medicine and Rehabilitation 96: (5), 934–943. https://doi.org/10.1016/j.apmr.2015.01.013 |
12 | Juckett, L. A. , Robinson, M. L. , & Wengerd, L. R. ((2019) ). Narrowing the gap: An implementation science research agenda for the occupational therapy profession. American Journal of Occupational Therapy 73: (5), 7305347010p7305347011–7305347010p7305347016. https://doi.org/10.5014/ajot.2019.033902 |
13 | Kristensen, M. G. H. , Busk, H. , & Wienecke, T. ((2022) ). Neuromuscular electrical stimulation improves activities of daily living post stroke: A systematic review and meta-analysis. Archives of Rehabilitation Research Clinical Translation 4: (1), 100167. https://doi.org/10.1016/j.arrct.2021.100167 |
14 | Kwakkel, G. , Kollen, B. J. , van der Grond, J. , & Prevo, A. J. H. ((2003) ). Probability of regaining dexterity in the flaccid upper limb. Stroke 34: (9), 2181–2186. https://doi.org/10.1161/01.STR.0000087172.16305.CD |
15 | Langhorne, P. , Bernhardt, J. , & Kwakkel, G. ((2011) ). Stroke rehabilitation. Lancet 377: (9778), 1693–1702. https://doi.org/10.1016/s0140-6736(11)60325-5 |
16 | Laver, K. E. , Lange, B. , George, S. , Deutsch, J. E. , Saposnik, G. , & Crotty, M. ((2017) ). Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 11: (11), Cd008349. https://doi.org/10.1002/14651858.CD008349.pub4 |
17 | Lefaucheur, J. P. , Aleman, A. , Baeken, C. , Benninger, D. H. , Brunelin, J. , Di Lazzaro, V. , Filipović, S. R. , Grefkes, C. , Hasan, A. , Hummel, F. C. , Jääskeläinen, S. K. , Langguth, B. , Leocani, L. , Londero, A. , Nardone, R. , Nguyen, J. P. , Nyffeler, T. , Oliveira-Maia, A. J. , Oliviero, A. , Padberg, F. , Palm, U. , Paulus, W. , Poulet, E. , Quartarone, A. , Rachid, F. , Rektorová, I. , Rossi, S. , Sahlsten, H. , Schecklmann, M. , Szekely, D. , & Ziemann, U. ((2020) , Feb). Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014). Clinical Neurophysiology 131: (2), 474–528. https://doi.org/10.1016/j.clinph.2019.11.002 |
18 | Legg, L. , Drummond, A. , Leonardi-Bee, J. , Gladman, J. R. F. , Corr, S. , Donkervoort, M. , Edmans, J. , Gilbertson, L. , Jongbloed, L. , Logan, P. , Sackley, C. , Walker, M. , & Langhorne, P. ((2007) ). Occupational therapy for patients with problems in personal activities of daily living after stroke: systematic review of randomised trials. BMJ 335: (7626), 922. https://doi.org/10.1136/bmj.39343.466863.55 |
19 | McIntyre, A. , Richardson, M. , Janzen, S. , Hussein, N. , & Teasell, R. ((2014) ). The evolution of stroke rehabilitation randomized controlled trials. International Journal of Stroke 9: (6), 789–792. https://doi.org/10.1111/ijs.12272 |
20 | Naudé, K. , & Hughes, M. ((2005) ). Considerations for the use of assistive technology in patients with impaired states of consciousness. Neuropsychological Rehabilitation 15: (3-4), 514–521. https://doi.org/10.1080/09602010443000470 |
21 | Richards, L. G. , Latham, N. K. , Jette, D. U. , Rosenberg, L. , Smout, R. J. , & DeJong, G. ((2005) ). Characterizing occupational therapy practice in stroke rehabilitation. Archives of Physical Medicine and Rehabilitation 86: (12, Supplement), 51–60. https://doi.org/10.1016/j.apmr.2005.08.127 |
22 | Saikaley, M. , Pauli G, I. J. , Iliescu N , Foley M , Mirkowski J , Weiner J , Chow A , Cotoi S , Peireira N , Fragis R , Alam A , Dukelow S , Miller T , & Teasell R. (2022). Chapter 9: Lower extremity motor rehabilitation interventions. In Robert Teasell, Stroke Rehabilitation Evidence Based Review (Ed.). Canadian Partnership for Stroke Recovery. |
23 | Saikaley, M. P. G. , Iruthayarajah, J. , Mirkowski, M. , Iliescu, A. , Caughlin, S. , Fragis, N. , Alam, R. , Harris, J. , Dukelow, S. , Chae, J. , Knutson, J. , Miller, T. , & Teasell R. (2022). Chapter 10: Upper extremity motor rehabilitation interventions. In Robert Teasell, Stroke Rehabilitation Evidence Based Review (Ed.). Canadian Partnership for Stroke Recovery. |
24 | Stroke Rehabilitation Evidence Based Review. (2020). Evidence-based review of stroke rehabilitation. Canadian Partnership for Stroke Recovery. www.ebrsr.com |
25 | Teasell, R. , McIntyre, A. , Viana, R. , Bateman, E. A. , Murie-Fernandez, M. , Janzen, S. , & Saikaley, M. (2022). Developing a framework for utilizing adjunct rehabilitation therapies in motor recovery of upper extremity post stroke. Topics in Stroke Rehabilitation, 1-8. https://doi.org/10.1080/10749357.2022.2070364 |
26 | Teasell, R. , Salbach, N. M. , Foley, N. , Mountain, A. , Cameron, J. I. , Jong, A. D. , Acerra, N. E. , Bastasi, D. , Carter, S. L. , Fung, J. , Halabi, M.-L. , Iruthayarajah, J. , Harris, J. , Kim, E. , Noland, A. , Pooyania, S. , Rochette, A. , Stack, B. D. , Symcox, E. , Timpson, D. , Varghese, S. , Verrilli, S. , Gubitz, G. , Casaubon, L. K. , Dowlatshahi, D. , & Lindsay, M. P. ((2020) ). Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part One: Rehabilitation and Recovery Following Stroke; 6th Edition Update 2019. International Journal of Stroke 15: (7), 763–788. https://doi.org/10.1177/1747493019897843 |
27 | Thomas, A. , & Bussières, A. ((2021) ). Leveraging knowledge translation and implementation science in the pursuit of evidence informed health professions education. Advances in Health Science Education, Theory, and Practice 26: (3), 1157–1171. https://doi.org/10.1007/s10459-020-10021-y |
28 | Thomas, A. , & Ellaway, R. H. ((2021) ). Rethinking implementation science for health professions education: A manifesto for change. Perspectives in Medical Education 10: (6), 362–368. https://doi.org/10.1007/s40037-021-00688-3 |
29 | Uswatte, G. , Taub, E. , Morris, D. , Barman, J. , & Crago, J. ((2006) ). Contribution of the shaping and restraint components of Constraint-Induced Movement therapy to treatment outcome. NeuroRehabilitation 21: (2), 147–156. |
30 | Viana, R. , & Teasell, R. ((2012) ). Barriers to the implementation of constraint-induced movement therapy into practice. Topics in Stroke Rehabilitation 19: (2), 104–114. https://doi.org/10.1310/tsr1902-104 |
31 | Wressle, E. , & Samuelsson, K. ((2014) ). High job demands and lack of time: A future challenge in occupational therapy. Scandinavian Journal of Occupational Therapy 21: (6), 421–428. https://doi.org/10.3109/11038128.2014.941929 |




