Returning to education after childhood acquired brain injury: Learning from lived parental experience
Abstract
BACKGROUND:
Returning to education (RtE) after an acquired brain injury (ABI) can be stressful for children/young people (CYP) and families. While much can be done to support RtE, there has been limited exploration of the lived experience of parents/carers about what can both help and hinder the process.
OBJECTIVE:
The aim was to understand more about RtE from parents’ perspectives to inform best practice and facilitate improvements in service delivery.
METHODS:
A service evaluation explored parent/carer views about the RtE process and the support received from healthcare professionals at a regional centre in the UK. Questionnaires (n = 59) were sent to parents of patients treated for an ABI in the last two years.
RESULTS:
31 parents (response rate = 51%) completed the survey. Results highlight the many challenges of RtE. Thematic analysis of responses revealed six key themes: Parental mindset and growth; What do they need now?; Specialist support and information; Talk and share; Challenges of new and hidden needs; and Don’t forget them!
CONCLUSION:
Parents offer crucial insight into the challenges of the RtE process. Their feedback highlights important factors for service development and reminds professionals of the key components of an effective return.
1Introduction
Acquired brain injury (ABI) is a major cause of childhood disability, with around 40,000 new ABIs sustained by children and young people (CYP) in the United Kingdom (UK) annually (National Health Service England, 2013). Effects can potentially impact all aspects of a CYP’s functioning (Braga et al., 2005; McKinlay et al., 2016), and even mild injuries can affect CYP participation in usual activities (DeMatteo et al., 2015). Attending school is their primary occupation, and educational settings provide important contexts for ongoing neurorehabilitation after ABI (Glang et al., 2013), immersing CYP in natural, experience-rich environments to help them relearn skills and compensate for acquired difficulties. Furthermore, when asked about key rehabilitation goals after ABI, the majority of CYP highlight reintegration to school and regaining a sense of belonging to school and peer groups as their primary focus (McCarron et al., 2019). Returning to education (RtE) after ABI should, therefore, be an important focus for hospital discharge planning and support.
As childhood ABI is often a sudden event, a timely and proportionate response is required from education settings to ensure successful reintegration, accommodating changed or acquired needs. Despite this, both clinical and research evidence suggests that teacher and Special Educational Needs Coordinator (SENCo) knowledge and understanding of ABI is limited (Bennett et al., 2022; Ettel et al., 2016; Howe & Ball, 2017; Linden et al., 2013). Few, if any, receive training about ABI, and many report being unaware of a pupil’s ABI history (Davies et al., 2013; Hawley et al., 2004). Many teachers describe limited communication with hospital teams (Hartman et al., 2015), a focus on community rather than school interventions (Lindsay et al., 2015), and feeling ill-prepared in supporting RtE (Hartman et al., 2015). They also commented on limited information on possible long-term sequelae (Hawley et al., 2004). Recent research with teachers emphasized a need for both basic training about ABI and child-specific professional development with specialist input (Bate et al., 2021). A report to the UK parliament highlighted gaps in training and knowledge within education, identifying the need for clearer pathways supporting RtE after ABI (Barnes et al., 2018).
This lack of awareness and appropriate support can have a dramatic effect on RtE, and subsequent attendance, integration, engagement and achievement (Leo et al., 2017). Without effective support, CYP with ABI are at risk of adverse outcomes including mental health difficulties, poor educational outcomes and career prospects, and increased likelihood of welfare recipiency (Sariaslan et al., 2016). As the impact of ABI can present differently across development with emerging difficulties in executive function, attention and behaviour common (Anderson et al., 2011), teachers are often faced with an evolving picture of need. There is a risk the ABI is therefore forgotten, unrecognised or misinterpreted, particularly where behaviour that challenges becomes an issue. Inevitably, these CYP are in turn more likely to be seen in child and adolescent mental health services (CAMHS), alternative educational provision settings and the youth justice system, where rates of ABI are reported to be high (Williams et al., 2015).
Given the importance of effective RtE, it is crucial that experiences of those encountering the process are explored and their views considered within service planning and development. While research shows that schools rely on parents to inform them about a brain injury (Hawley et al., 2004), there has been very limited exploration to date of the lived experiences of parents supporting CYP back into education after ABI, particularly regarding the nature of support they needed and received (Andersson et al., 2016).
1.1Study context
The Brain Injury Living Life (BRILL) team at Nottingham Children’s Hospital works with CYP admitted with ABI, providing an evidence-based model of inpatient intensive neurorehabilitation and early supported discharge to smooth transitions to home and local community services (Keetley et al., 2020). CYP are supported by Paediatric Neuropsychology and a Brain Injury Specialist (BIS) or a Neuro-oncology Outreach Nurse Specialist (NOONS). Schools are proactively involved in this transitional process with flexible support offered to help them receive a CYP back at school, including staff training specific to the CYP’s injury, stage of development and rehabilitation progress to date. While this process is largely successful, team observations and anecdotal feedback from families suggest not every return goes as smoothly as hoped. This study therefore sought to understand factors which may help or hinder RtE, from the parental perspective.
1.2Study purpose
A service evaluation was devised to explore lived experiences of parents and carers supporting their CYP’s RtE after ABI, and to provide information for future service development and improvement. The study aimed to gather information about the RtE process, and seek qualitative views on the following questions:
a. What do parents feel have been the main challenges in supporting their CYP to return to education post-ABI?
b. What do parents believe helped?
c. What advice would parents offer other families?
d. What key points would parents want people in education (e.g. teachers and SENCos) to remember when working with pupil with an ABI?
2Method
2.1Participants and procedure
Parents of CYP seen by the neurorehabilitation service within the previous 2.5 years (October 2017 to March 2020) were contacted by email or text (n = 60). A link was provided to a 42-item questionnaire devised by the Paediatric Neuropsychology Service, BIS and NOONS, and administered via Survey Monkey. Questions requested demographic and brain injury information, and explored the experience of RtE from the parent’s perspective, asking them to reflect on what felt challenging and helpful within this phase of their child’s rehabilitation (Table 1).
Table 1
Examples of Question Types and Methods of Analysis
| Question type | Category | Question examples | Method of analysis |
| Closed questions | Demographics and injury/illness characteristics | What is your child’s gender? | Quantitative (descriptive statistics) |
| How old was your child when they had their ABI? | |||
| How long was their stay in hospital? | |||
| Impact of ABI | What has changed for your child because of their ABI? | Quantitative (descriptive statistics) | |
| Select all that apply (e.g. thinking and learning; levels of fatigue; friendships and relationships with teachers, friends and family) | |||
| Is your child classed as having special educational needs? | |||
| Is this the result of their ABI? | |||
| RtE information | Did your child return to their original education setting after their ABI? | Quantitative (descriptive statistics) | |
| How long after your child’s ABI did they return to school? | |||
| On return to school did they return a. full time or b. part time? | |||
| Open questions | Experience of the RtE process from the parent’s perspective | What have been the main challenges in supporting your child to RtE post ABI? | Qualitative (thematic analysis) |
| What are the things that helped? | |||
| What advice would you offer to other parents? | |||
| What is the one thing you want people in education (e.g. teachers and SENCos) to remember when working with a pupil with an ABI? | |||
| Please use this space to add any other comments relevant to your experience of your child RtE |
2.2Data analysis
Descriptive, exploratory analysis of quantitative data was conducted with statistics including mean, standard deviation, and percentages. Thematic analysis was used to analyse qualitative responses to study questions flexibly and inductively, describing this information in rich detail and searching it for patterns (Braun & Clarke, 2006). Thematic analysis followed Braun and Clarke’s (2006) framework. After data immersion by all authors, EB and AF generated initial codes and text exemplars manually to organise data with items of similar meaning. All authors re-read data to check codes were meaningful, generating additional codes and regrouping where relevant until consensus was reached. Codes were then collated into themes and subthemes through discussion and mapping, identifying relevant data extracts (Table 3). Themes were reviewed and refined to ensure coherence between data and agreement between authors, then defined and named before finally preparing the written evaluation. At all stages, study questions were used as a reference point and the thematic analysis framework was used to respond to these dynamically.
Table 3
Samples of Text Used to Develop Codes and Build Themes
| Codes | Sample of coded text | Theme |
| •Parental need to build resilience | “My determination to not give up” | Parental mindset and growth |
| •Parent learning to become an advocate for their child | “Don’t give up, keep pestering the system until you are happy your child’s needs are being met” | |
| •Perseverance in the face of challenges an knowledge gaps | “To persevere with getting things put in place for their child. Seek advice on what’s available” | |
| •Parents needing to be patient/kind to themselves, their child and school | “Don’t expect too much too soon, and just accept one day at a time” | |
| •The essential role of specialists | “The Brain Injury Specialist gave us that knowledge and was very helpful about how to handle behavioural changes” | |
| •Utilising the available ABI networks and information | “Get a list of support groups, charities, websites and contact details and most importantly a contact for help and advice” | |
| •Liaison between ABI professionals and school | “The links between the medical and ABI teams and school are essential to ensure a successful return to education” | |
| •Need for new types of support from school | “Be patient with the school as this may be new for them too” | |
| •Need for adjustments within school/the classroom | “Reduced hours, regular breaks” | |
| •The need for bespoke support | “the school have used visual aides for maths and have recently tried short bursts of work” | |
| •Need for schools to give time and display patience/empathy towards the child | “be more empathetic as this could easily be your child so treat and support these pupils how you would want your own child to be treated and supported” | |
| •School’s knowledge & understanding of ABI | “School taking time to understand the holistic nature and impact of the ABI was important” | |
| •Communication between everyone playing a part in the RtE | “He has up to 10 teachers per day and no one seems to communicate with each other to understand him” | Talk and share |
| •Liaison with family & child –holding them at the centre | “Involve the child in the planning process to support their understanding . . . the ‘done to them’ approach does not help” | |
| •Liaison with professionals to understand new needs | “Try to get behavioural advise as soon as possible. It is not only about the physical effects but also longer term recovery of personality” | |
| •ABI as a hidden disability | “Just because they look like every one else doesn’t mean they think/react like everyone else” | |
| •Consideration of longer-term needs | “take note and implement recommendations from the BIS and parents, and to maintain these over the long term of recovery not to forget them after the first few weeks” | |
| •Child’s new needs post-ABI | “He shouts and swears at times which is all post ABI” | |
| •Anxiety within the child and their system | “The worries and fears of how school will be with them and getting them into school when they are so nervous” | |
| •Changes to inclusion and participation | “Dealing with his exclusions from activities whilst his blood clot dispersed” | |
| •Difficulties with peers | “the effect on her friendships because of her apparent bluntness, and lack of consideration of other people’s feelings” | |
| •The need for others to help facilitate friendships | “Seek out and find special friends who your child can connect with who will support them” | |
| •Challenges associated with the amount of school missed | “Completing the education to the best of their ability whilst acknowledging the work he missed is so vast” |
3Results
3.1Demographics
Thirty-one parents/carers (response rate = 52%) completed the survey. 61% of their children were male (n = 19) with CYP age ranging from five years to 18 years-old at the time of survey completion. All were at least six months post-injury or illness and had returned to education. Prior to their ABI, 90% of children had been in mainstream education (n = 27). Two children attended independent schools (7%), one CYP was in a special school setting, and one parent did not provide an answer. Further demographic and injury details are outlined in Table 2.
Table 2
Demographic Information and Injury Details
| Demographic variables | Number |
| Gender: boys; no. (%) | 19 (61%) |
| Age at injury (years): mean SD (range) | 10 5.6 (2–17) |
| Age at injury | |
| 0–4 | 2 |
| 5–8 | 7 |
| 9–11 | 9 |
| 12–15 | 11 |
| 16–18 | 2 |
| Injury/illness characteristics | |
| Length of stay in hospital (days): mean Mode (range) | 16 14 (0–64 days) |
| Cause of brain injury | |
| Concussion/mild TBI | 3 |
| Mod/severe TBI | 12 |
| Stroke/AVM | 3 |
| Brain tumour | 6 |
| Infection | 4 |
| Hypoxia | 1 |
| Unsure | 1 |
| No response | 1 |
3.2RtE information
All CYP except one returned to their previous education setting after their ABI (97%). RtE took between 0 and 40 weeks, with a mean re-entry time of 9 weeks; only one CYP returned immediately after discharge. Fifteen (48%) children missed more than seven weeks of schooling, while 9 of these (29%) missed more than 12 weeks. Twenty-nine percent required home education before returning to school, and 77% of children returned part-time (N = 24) on school re-entry; eleven parents said their CYP only attended for half days in the first stages, 6 reported they attended for just a few hours, and some children did as little as an hour. With regard to re-joining lessons, 58% joined their previous lessons, 6% completed their lessons separately to peers (e.g. in the learning support area) and 23% learned across both environments; 13% transitioned into new settings (e.g. moving from primary to secondary school) so could not answer this question.
3.3Impact of ABI and support needed
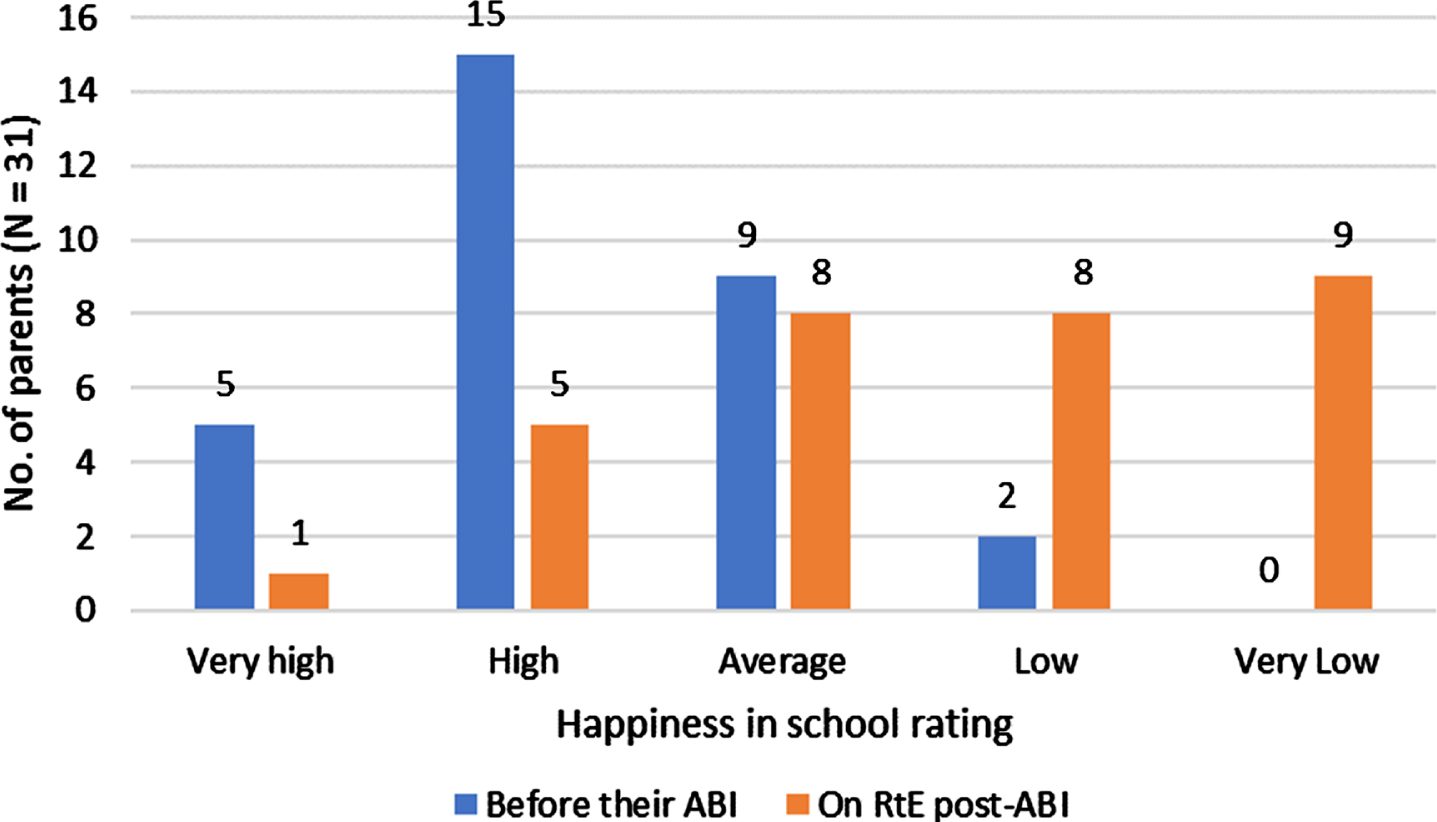
Parents (n = 29) reported a high number of chan-ges in their child’s abilities and needs post-ABI, illustrated in Fig. 1. The five highest rated changes included levels of fatigue (86%, n = 24), ways of behaving (76%, n = 22), thinking and learning (72%, n = 21), feelings about things (emotions) (72%, n = 21) and communication (59%, n = 17). Changes in at least three areas were reported for 24 (83%) CYP, and in at least five areas for 17 (59%). As a result of these changes, 48% of CYP were described by parents as having special educational needs (SEN), although only 29% had an Education, Health and Care Plan (EHCP) and only 16% of parents reported the school had applied for additional funding to support their child. Two young people were reported to have been excluded from school since their ABI. Parents frequently reported changes in their child’s levels of happiness in school pre and post-ABI (see Fig. 2).
Fig. 1
Areas of Function that have Changed for CYP as a Result of ABI.
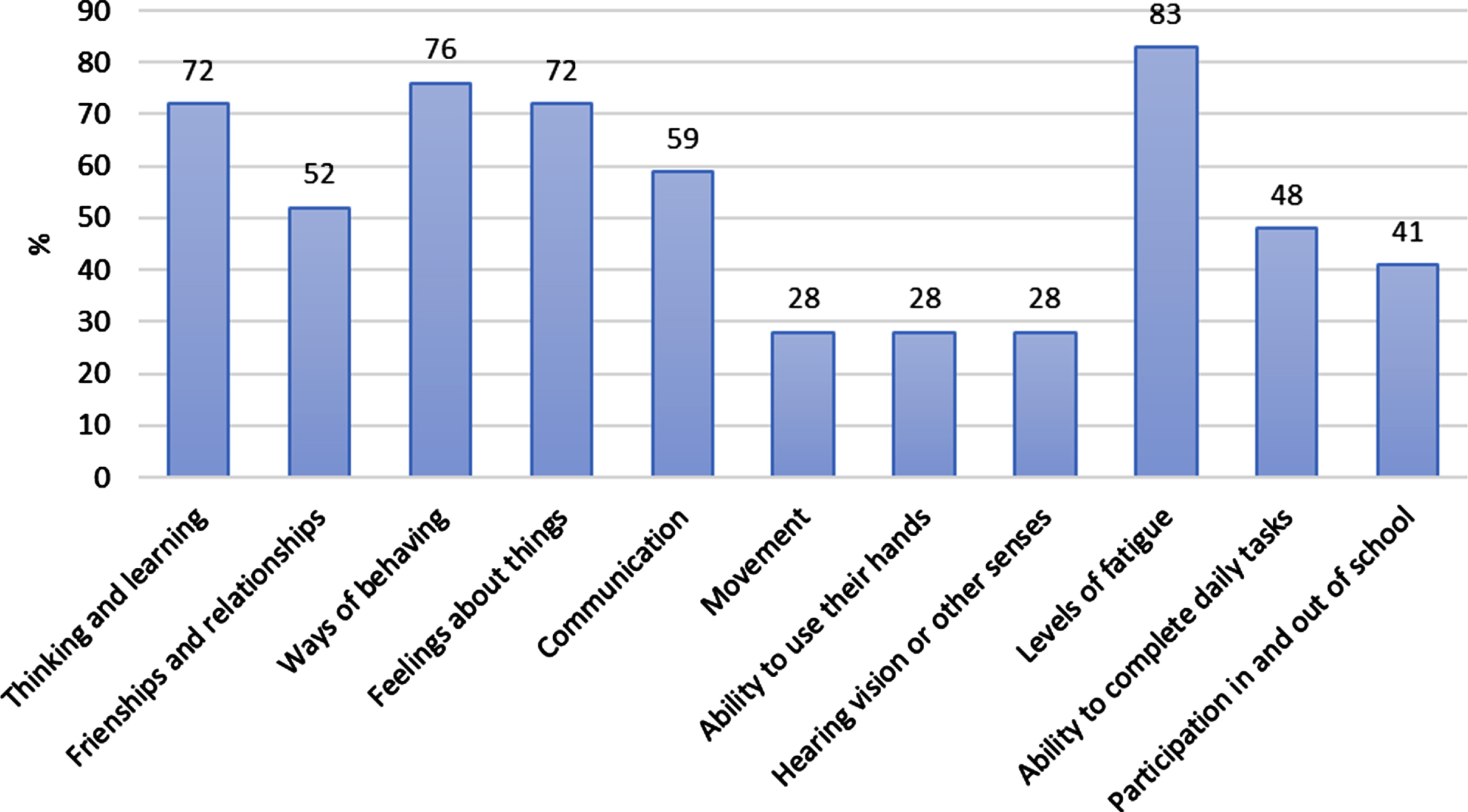
Fig. 2
Parental Ratings of their Child’s Happiness in School Pre-ABI and on Return to Education Post-ABI.
3.4Thematic analysis
Six main themes were identified, summarised in Fig. 3. Themes and subthemes are described and illustrated below; parents are identified by their response number to the survey (e.g. P1).
Fig. 3
Subthemes and Themes Emerging from Parental Qualitative Responses.
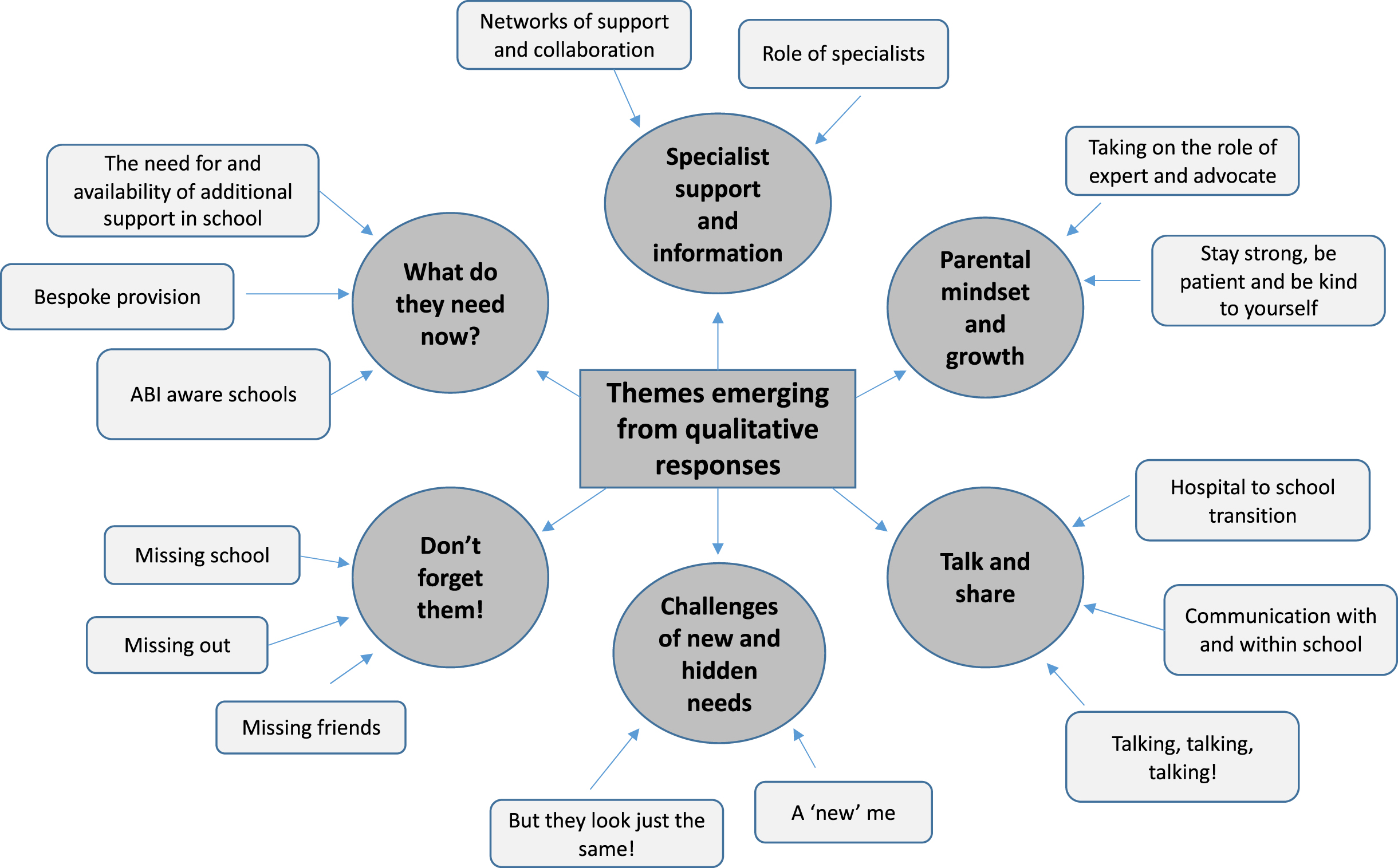
3.4.1Parental mindset and growth
One of the key emerging themes addressed the changed role and mindset parents felt they had to ‘grow into’ after their CYP’s ABI, developing resilience, patience and perseverance to manage the many challenges presented throughout RtE. Parents also spoke of their role in advocating for their child, particularly in the absence of knowledge about ABI within the education setting. The need for self-kindness in taking on this ‘new’ role was widely described and supports themes in previous research about learning to be a ’new parent to a different child’ (Tyerman et al., 2017).
3.4.1.1Taking on the role of expert and advocate Many parents described feeling a need to help school understand their child’s new needs and push for appropriate support, including requesting meetings, making judgements about when the CYP should return to certain activities, and challenging schools when provision was not forthcoming. Parents highlighted difficulties “getting enough help for him in school and getting his EHCP” (P30), and sometimes required a strong stance to challenge the school, reflecting previous research of the stressful nature of parenting a CYP with a brain injury (Brown et al., 2013): “it took time, determination and sometimes confrontation to get what we believed our daughter needed” (P10).
P10’s comment that “it has been a very difficult journey of two and half years to get to our current situation of having an EHCP and support in place. It’s taken too long”, highlights the need to persevere. This was also illustrated by the 56% of respondents who advised other parents to have perseverance when advocating for their child: “It’s a long fight to get help but don’t give up, even when it seems no one is listening” (P25).
Additionally, the process of becoming an expert advocate in their CYP’s ABI was highlighted as a challenge, with parents describing needing time “for me to get to know and understand the ‘new X’ and be able to explain this to others” (P27), while also “Having to ask for support to be put in place but not knowing what can be offered and not being given a choice of different options” (P18).
3.4.1.2. Stay strong, be patient and be kind to yourself In response to the many challenges acknowledged in supporting their child’s RtE after ABI, 52% highlighted the importance of self-kindness. Parents emphasized that patience was key, advising other parents that having an understanding that RtE may not be sorted immediately was crucial to looking after themselves and their child:
Don’t expect too much too soon, and just accept one day at a time, and then make sure you communicate with school and keep checking in with your child that they feel they are being listened to and adequately supported. (P27)
Be patient with your child and yourself. Take it one day at a time. Be kind to yourself as you will be learning new things along with your child. (P2)
Finally, many parents reported the need for resilience, with one feeling the eventual progress in gaining support for her CYP was down to “my determination to not give up” (P16). Parents were able to recognise how their own strength and growth had been important, but also spoke about the “battle” (P10) to get the right help for their CYP while still processing the trauma of what had happened.
3.4.2Specialist support and information
Parents reflected on the role of collaboration with health and education professional networks, and the value ABI-specific support could add to education staff during RtE and beyond. This reflects recommended best practice of seamless care, with education staff understanding their role in the CYP’s rehabilitation (Andersson et al., 2016; McKinlay et al., 2016) to enable appropriate support for both CYP and family (Hartman et al., 2015).
3.4.2.1. Role of specialists Specialists from multiple acute care and neurorehabilitation disciplines were highlighted as “knowledgeable sources” (Hartman et al., 2015) for education staff to tap into, with P23 advising schools “take note and implement recommendations from the Brain Injury Specialist and parents and maintain these over the long term of recovery not forge[t] them after the first few weeks”. P10 noted “The epilepsy nurse was amazing. She became our voice at school”, supporting their attempts to advocate for their CYP, while other parents noted the crucial roles of the neuropsychologist (P19), and BRILL/hospital team (P14, P21). Some parents, however, noted that specialist advice was not followed, and exhorted education staff to take on specialist advice offered:
I would’ve liked teachers to follow the advice of the clinical psychologist report, by giving him time to process the subject matter prior to each lesson and understand how fatigued he would be. (P22)
3.4.2.2. Networks of support and collaboration In addition to advising education staff to “work with and seek advice from the family to learn what the child’s capabilities are and what support they can put in place individually for them” (P22), parents noted the value of having networks of support around them and their child: “the links between the medical and ABI teams and school are essential to ensure a successful return to education” (P20). Parental views echo recommendations for education staff to be proactive in working alongside health professionals from an early stage after the child’s injury (Savage et al., 2005), and reflect national recommendations encouraging professional network support (for example, Paediatric Stroke Working Group, 2004).
When asked what advice they would offer other parents, survey respondents emphasised the importance of building and using the available network, including third-sector organisations: “Work with the ABI support teams to deliver advice to school. Be informed and draw on the information . . . available through The Children’s Trust and other sources” (P20). Having “a list of support groups, charities, websites and contact details and most importantly a contact for help and advice” was also advised (P10), and in reflecting back on their experience over time, parents noted the importance of drawing on networks, even if support does not seem essential initially:
In the beginning agree to all help and support offered by children’s trust for support groups and a support worker or whatever else they offer, even if you think you won’t need it . . . you will need to be sure you have support long-term. (P16)
3.4.3What do they need now?
The need for schools to be responsive in meeting a CYP’s new needs after ABI in appropriate and timely ways was raised by all parents, encompassing wide-ranging aspects including adjustments and bespoke approaches for supporting changed educational needs, recognition of the additional time, patience and empathy CYP may require, and the importance of underpinning these by ensuring schools have comprehensive knowledge and understanding of ABI. These subthemes reflect previous recommendations exploring the experiences of individuals with ABI and their families (Norman et al., 2022) and current practice recommendations (McKinlay et al., 2016).
3.4.3.1. The need for and availability of additional support in school For many parents, getting enough support from school for their CYP following their ABI was a challenge, with P10 noting that, “initially, it was just awful . . . Having no support and being totally ignorant of what we were dealing with”. The relationship with the previous theme of network collaboration was highlighted in this subtheme, noting that where this was dysfunctional, “the battles with funding and lack of cohesive support from all the experts together, initially made getting support in place very difficult” (P10). Underlining the need for parental resilience noted earlier, several parents described feeling let down when the school did not action agreed provision:
. . . School staff gave promises and agreed to give support to my daughter on return to school when in meetings with myself and Brill team, but never followed through with agreed support when my daughter actually returned to school . . . the whole experience was disheartening. (P16)
Another parent discussed challenges faced when progressing through the education system where there was “a lack of records from her time in Year 5 . . . [and the challenge of] making sure that the right information is handed over from primary school” (P18).
Conversely, parents also discussed wider aspects of school culture deemed helpful when accessing support for their CYP in school, with positive experiences including “school involvement, meeting his friends, meeting head teacher” (P1) and “feeling safe and supported in school, by staff who are informed and understanding” (P20), and recognising the benefit when an “EHCP was sorted very quickly” (P30). Where schools were viewed as meeting needs well, parents were very positive, with P9 saying “the school were superb and I don’t feel I could have asked for more” and P10 describing a good transition to secondary education where “the secondary school . . . have done everything in their power to support us and our daughter”.
3.4.3.2. Bespoke provision Support packages were considered more effective when they were “suitable for the child, and agreeable with them” (P11). Such adjustments included, “visual aids for maths and . . . short bursts of work, repeating what he has already done to help him retain the information” (P13), “rest and not too many expectations” (P7), “reduced hours, regular breaks” (P29), “brain breaks, completing revision work and then minimal work” (P3), adjustments to managing “behavioural changes” (P23), and a holistic approach to “managing the day” (P24). This was reinforced by P20’s documentation of beneficial bespoke arrangements:
Teaching staff support –reassurance and guidance, weekly meetings with head of year, re-starting the school year, 1 : 1 subject teaching, new friendship group, counselling, exam access arrangements, and school taking the time to understand the holistic nature and impact of ABI. (P20)
Some parents highlighted the role of one-to-one support: “having a TA (teaching assistant) . . . work solely with him . . . helped with communication and they know what signs to look for when he becomes fatigued or losing concentration” (P22).
3.4.3.3. ABI aware schools 57% of parents highlighted the impact of a school’s depth of knowledge and understanding of ABI on the nature and efficacy of educational support, noting a link between a “lack of understanding in handling change of behaviour and . . . of support / interest / action by the school” (P23). While the role of specialists in giving detailed information about a CYP’s neurorehabilitation progress and new needs is identified in a previous theme, this subtheme of ABI aware schools acknowledges the responsibilities schools have to proactively deepen their knowledge of ABI to support RtE. P29 requested staff to:
. . . please research as much as you can to provide the best support and not to be afraid of being honest about particular doubts and concerns . . . I would have preferred honesty instead of avoidance and putting obstacles in my child’s way to return to school. (P29)
P22 wished all educators working with students with ABI would “gain knowledge and understanding of how an ABI can affect a child’s learning and the day to day struggles for them and their whole family”, and P19 noted inconsistencies in awareness between those who had received training and those who had not: “some [staff] are brilliant, some think he is just being naughty like others in the class”. Parents felt a deeper understanding of ABI would help teachers appreciate the need to “give them time” (P3), with “an abundance of patience and not always adhering to social norms” (P22). The need for this empathetic approach towards CYP with ABI during RtE was eloquently described:
This is very confusing for the pupil, more challenging than they let on. So be more empathic as this could easily be your child so treat and support these pupils how you would want your own child to be treated and supported. (P16)
3.4.4Talk and share
Parents emphasized the importance of communication between hospitals, parents, and schools as well as amongst teaching staff, with this theme acting as a foundation to all other identified themes.
3.4.4.1. Hospital to school transition The impact of poor communication during RtE was highlighted starkly by one parent, whose CYP was not initially referred to BIS or BRILL:
. . . there should have been some direct communication between hospital and school. School knew nothing about what had happened or what should be in place and simply relied on asking us what they needed to do. (P10)
Others, however, felt well supported, encouraging educators to communicate with “hospital staff to find out what help is available within the NHS, they are amazing and offer support beyond diagnosis” (P14).
3.4.4.2. Communication with and within school The need for strong, open communication between parents and schools was also important, with P10 commenting that “lots of contact and communication is vital”; conversely, parents found RtE extremely stressful when there was “little communication from school” (P15). Where possible, many parents recommended keeping channels of communication open and working alongside the school to ensure their child’s needs were being met: “Make sure you communicate with school and keep checking in with your child that they feel they are being listened to and adequately supported” (P27); “Keep communication open with the school and don’t be afraid to speak up for your child remember...you know them best” (P2). One parent also believed:
Communication and cooperation with school is key. Be brave and don’t let your anxiety transfer to your child. Work with the ABI support teams to deliver advice to school. Be informed and draw on the information about ABI . . . Look after yourself! (P20).
One particular challenge highlighted was internal school communication, with one parent describing how, “he has up to 10 teachers per day and no one seems to communicate with each other to understand him” (P7). Reflecting on the time since their CYP’s ABI, parents emphasised the fundamental importance of communication on transition between schools, with some parents noting risks:
For secondary school –making sure the right information is handed over from primary school but again I had to request a meeting with safeguarding lead to make sure they were aware of my child’s difficulties. (P18)
3.4.4.3. Talking, talking, talking! Several parents also acknowledged the importance of communication in supporting their own and the CYP’s adjustment following ABI, including during RtE. One recommended, “Talk (find safe people to talk to) about how you feel and what you are going through. Allow your child to do the same” (P2). Parents recognised the importance of “Talking, talking, talking. Letting him know it’s OK to feel the way he feels” (P2), and of using this to “still have some banter in order to make them realise they are still the same child as they were before” (P15).
3.4.5Challenges of new and hidden needs
Foundational to RtE approaches, the often ‘hidden’ nature of new needs linked to ABI was a clear theme within parent responses, and the challenges these needs created when not always evident to others.
3.4.5.1. But they look just the same! When asked what they wished SENCos/teachers would remember about ABI, 43% of survey respondents highlighted its ‘hidden disability.’ P25 wished to remind teachers that “just because they look like everyone else doesn’t mean they think/react like everyone else,” while P24 wrote, “they look ok on the outside, but often there are still many challenges happening internally.” Others commented, “it’s a hidden disability. The child may look fine, but they don’t always feel fine. They may not have the capacity to say . . . ” (P20), “they may look physically fit but are maybe struggling with the way they now think” (P19) and:
Just because my son looks fine, his brain gets tired and he needs breaks. He needs more time to finish tasks and he needs more time to recall. Just because they are back at school doesn’t mean they are back to normal. The trauma has an impact and they need support and kindness (P17).
One parent emphasised the conflict this caused with school, “until the brain injury specialist went into school they were clueless and I think it’s easy for them to forget that because he looks ok doesn’t mean the ABI isn’t there (P13).
3.4.5.2. A ‘new’ me The specific impact and challenges of a CYP’s new ABI-linked needs on settling back into an education system were strongly and eloquently illustrated by parents within this subtheme:
Getting teachers to understand his behaviour, some are brilliant, some think he is being naughty like others in the class. He is easily led and makes poor decisions, some teachers think it’s his choice. He shouts and swears at times which is all post-ABI. (P19)
Expanding on changes listed in Fig. 1 above, and reflecting other studies reporting numerous post-ABI difficulties across a range of domains (Babikian & Asarnow, 2009; Keenan et al., 2018; Wilkinson et al., 2018), parents noted their CYP’s new needs included “reading books” (P28); anxiety, low mood, emotions and confidence, (P31, P17, P2, P1); behaviour (P23, P19); memory (P26); concentration (P4) and fatigue (P24, P29, P27, P7, P9, P4, P3). One parent described changes in more detail, highlighting “fatigue, anxiety –in particular in relation to keeping up with the workload and perceived teachers’ expectations. Pacing –learning to manage fatigue” (P20), while another said, “the fatigue and memory loss has been very difficult. He struggles to retain information in all subjects . . . maths especially” (P13). P1 described changes to her son’s “confidence, his appearance, his independence”, while others described changes in personality: “they are not the person they were, they’ve changed . . . they quite often lack insight . . . they may react differently in certain situations and seem ‘odd”’ (P10); “It is not only about physical effects but also the long-term recovery of personality” (P23).
3.4.6Don’t forget them!
The final theme emerging from the qualitative data related to the challenges encountered by parents while supporting their CYP’s participation and inclusion. As highlighted in recent research (Keetley et al., 2021; Wales et al., 2021), parents reported changes in participation relating to school engagement, maintaining friendships and peer relationships, and involvement in extra-curricular/community activities.
3.4.6.1. Missing school Missed school was noted by some parents as a current and ongoing challenge in supporting their child’s RtE, reflecting that learning has continued for other students while the CYP with ABI has been unable to attend:
Completing the education to the best of their ability whilst acknowledging the work he missed is so vast that he will not be able to catch up. Having to encourage him to complete homework whilst fatigued from being at school all day and fitting in extra-curricular activities and health appointments. (P22)
Another parent faced challenges with their CYP’s attendance after ABI as “she does not want to go to school” (P12), and P26 described how her son continued to “miss a day here and there . . . as he was exhausted”. While adjusted hours were valued by some parents (see bespoke provision subtheme above), P2 saw this less positively, commenting that the need for a phased return meant her child struggled to “attend school for longer.”
3.4.6.2. Missing out Many parents felt participation had changed for their CYP post-ABI, and several linked this to fatigue. P2 stated, “fatigue can play a huge part in obstacles”, and P22 noted the impact of this on leisure time and learning (see P22 quote above). P17 described the challenges “dealing with exclusions from outdoor activities whilst his blood clot dispersed and . . . judging the timing of return to activities . . . anxiety of certain sports means he does not want to take part”. Others highlighted problems “resuming sport activities (P20), “requiring surgery before he can participate” (P19), and being “unable to go in the playground” (P13). In addition to physical restrictions due to medical needs, one parent spoke honestly of the parental impact on participation by encouraging parents to “let go a little, as difficult as it is . . . let them do things for themselves to make them feel normal” (P15).
3.4.6.3. Missing friends Facilitating and maintaining peer and social relationships also presented a participatory challenge for many CYP after ABI: “For the first few months the main challenge was [child]’s emotional needs, and the effect on her friendships because of her apparent bluntness, and lack of consideration of other people’s feelings. Total lack of diplomacy” (P27). P2 also described the “change in friendships,” while another mentioned the “impact on former social relationships” and the challenge of having to form a “new friendship group” after old relationships broke down (P20). However, many parents also spoke of how peer relationships had been crucial in assisting the RtE:
Having one close friend who accepted [child] just as she was, and didn’t judge even if [child] said upsetting things. Also time ... time for me to get to know and understand the ‘new [child]’ and be able to explain this to others. (P4)
Many advised other parents to encourage and facilitate friendships in a way they may have not needed to before the ABI. Parents suggested, “seek out and find special friends who your child can connect with who will support them” (P22), “Arrange for them to meet one or two of their closest friends so they get that feeling of care back” (P27).
4Discussion
The findings from this service evaluation highlight the importance of hearing the voices and wisdom of parents supporting their children to RtE post-ABI. Parents of children aged two to 17 years of age at injury described the process of RtE after ABI. The majority returned to their previous education setting but over three quarters of the CYP experienced changes in at least three areas of function, and nearly half were described as having special educational needs. Thematic analysis of the 31 completed questionnaires identified six main themes: parental mindset and growth, specialist support and information, what do they need now, talk and share, challenges of new and hidden needs, and don’t forget them. In line with study purposes and within each of these themes, parents clearly articulated the many challenges they faced when supporting their child’s RtE, and acknowledged these often existed even where health service provision was good. Their reflections illustrated strategies and approaches which were helpful, offered rich advice for other families, and together the themes provide clear key points for schools to remember when supporting RtE after ABI. Implications of these findings for local and wider service provision and planning are discussed below.
4.1Multisystem support
Results highlight the essential role played by professionals with ABI expertise and experience in supporting effective and child-specific information sharing, consultation and guidance during RtE, offering insight into the recovery trajectory and anticipated longer-term difficulties to inform support strategies. Part of this must involve upskilling parents, CYP, and teachers alike via psychoeducation, to ensure they too can be effective advocates for the CYP’s new support needs. It is important, therefore, that health service commissioners are aware of key health services and roles essential for supporting a successful RtE, and the potential personal and economic costs of not facilitating this, including increased risk of parental and CYP mental health difficulties. Indeed, evidence suggests where rehabilitation and school reintegration are successful, CYP are better able to participate in secondary education (Todis & Glang, 2008) and thus occupation in the future, reducing the recognised risk of possible dependency on services and benefits in adulthood (Sariaslan et al., 2016).
As well as ensuring the availability of ABI-specific health service provision to support RtE, teachers, SENCos and the wider education system must be knowledgeable and well-equipped for supporting CYP with ABI. This study showed huge disparity in school awareness of ABI, with negative or positive impact on RtE as perceived by parents: this reflects previous research recognising greater needs for parental advocacy when schools are viewed as lacking in training or refusing services (Burke & Hodapp, 2016). The paucity of training on ABI is recognised by health and education services alike and well-documented in the literature (Andersson et al., 2016; Barnes et al., 2018; Bennett et al., 2022), yet driving change remains challenging, particularly in the UK where SEND systems are increasingly focused on broad areas of need rather than specific conditions (Department for Education (DfE), 2014). However, given the sudden and dramatic changes presented by ABI, the risk of hidden disabilities and the potential for emerging needs across development, ABI training for all teachers is essential, with input from specialists around individual needs as required. This gap is emphasised in the All-Party Parliamentary Group on ABI’s report to the UK Parliament, which states, “All education professionals should have a minimum level of awareness and understanding about ABI” (UKABIF, 2018, p22); this is now reflected in the key aims of the National ABI in Learning and Education Syndicate (N-ABLES, 2018).
4.2Recognising complexity
The issue of hidden and complex needs after ABI, and the challenges associated with fatigue are also emphasised in parental responses. As shown above, many CYP in the study had a range of difficulties and 83% of CYP had at least three areas of deficit post-ABI. Research also demonstrates high levels of pre-existing vulnerabilities/comorbidities in the ABI population including ADHD (Eme, 2014; Hoarea & Beattieb, 2003; Max et al., 2004; Yeates et al., 2021), and many CYP also face ongoing medical complications/treatments which may create additional needs or further RtEs, for example, ongoing oncology treatments, hydrocephalus, arteriovenous malformation and cavernoma management. Parents remind us that it is essential to create child-centered pathways and systems responsive and adaptive to the complexity of individual needs, ensuring CYP can continue to make educational progress at intensities and levels suiting their recovery, progress with neurorehabilitation and emerging development.
Participation should also remain a central focus within support, as CYP are often excluded on many levels post-ABI. This need for participation to be considered within conceptualisations of disability/function and across all rehabilitation contexts is highlighted within the International Classification of Functioning, Disability and Health (World Health Organisation, 2001), and in emerging research addressing outcomes of paediatric ABI (Câmara-Costa et al., 2020; de Kloet et al., 2015; Thompson et al., 2016). Given changes in identity, needs and participation, it is also important pathways into timely mental health support are identified and strengthened.
4.3Supporting parents
The role of parental advocacy in supporting RtE is a clear theme from this study, and reflects research highlighting that rehabilitation understood and delivered by families is often most effective (e.g., Braga et al., 2005). However, given that parents described the effort and time required to embrace and ‘grow’ into this new role, it is crucial that the vulnerabilities of such reliance on parents, and the risk of increased inequity in RtE experiences, are acknowledged. Effective parental advocacy is enhanced, for example, in families with higher socioeconomic and education backgrounds (Burke & Hodapp, 2016; Lalvani, 2012), whereas parents with different cultural and language backgrounds or inexperience of navigating school and special educational needs systems may find advocacy more challenging (Bacon & Causton-Theoharis, 2013; Rosetti et al., 2020; Savage et al., 2005). Hospital teams also recognise that emotional trauma of a child’s ABI (for example, an accident which parents may also have been involved in) may have a negative impact on parental ability to absorb new information and advocate successfully on their child’s behalf. Thus, the system cannot be wholly reliant on parents, particularly in the early stages after injury, but instead needs to support parents to share their learned expertise: it is, therefore, essential that hospital/specialist teams are involved in RtE, education staff receive adequate training, and parental mental health is considered within service provision.
4.4Reducing regional variation
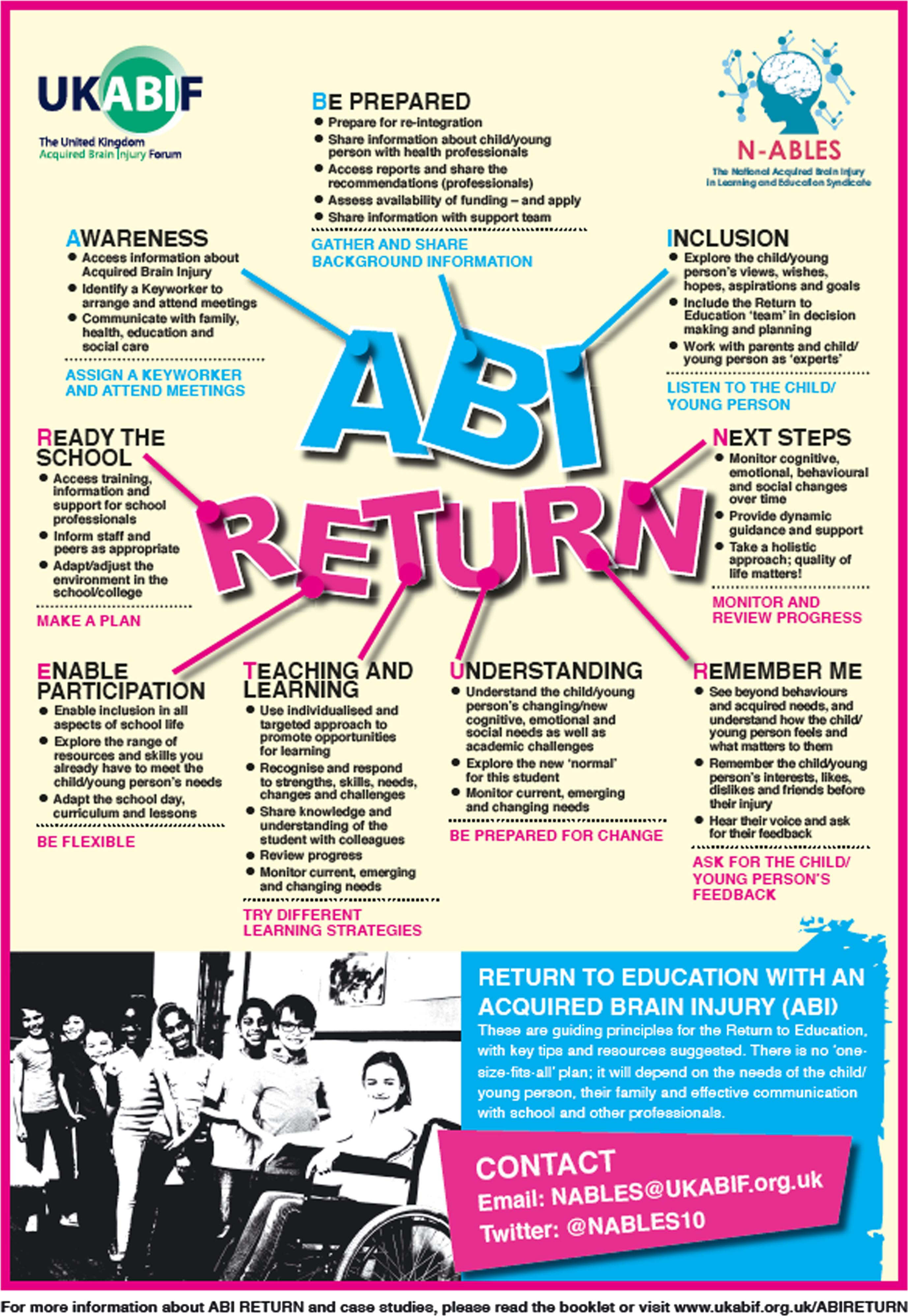
It is important to appreciate parent voices represented in this evaluation are the experiences of parents who had support of ABI professionals, yet RtE was still challenging in most cases. The authors recognise that in some parts of the UK, there would be no neuropsychology/neurorehabilitation team or BIS/NOONS to offer support, and it is likely the RtE process would be additionally stressful and challenging for families. The recent work of N-ABLES attempts to begin addressing this inequity with the production of best practice guidance, ABI RETURN, which informs educators and families about how best to help. ABI RETURN addresses many of the key principles highlighted by this evaluation, outlining nine key ways to support RtE, centered around communication and training, planning and preparation, flexible and dynamic responses within the system, CYP and family-centred working, and participation and inclusion (see Fig. 4) (UKABIF, 2021).
Fig. 4
N-ABLES ABI RETURN Best Practice Guidance.
4.5Strengths, limitations and future research directions
Strengths of this service evaluation include championing the voice of parents with lived experience, within one regional system in the UK. This is helpful for service improvement within the specific system, and for wider learning about the key themes and gaps acknowledged. Limitations of this approach, however, mean that it is representative of this one area only and some findings may not be applicable to all UK contexts, or further afield. Research to explore experiences across other parts of the UK, with and without specific ABI RtE support, would be beneficial to ensure comprehensive understanding of needs and identify good practice more widely. Future research might also explore how hospital or neurorehabilitation teams might best equip families for knowing their rights and advocating within the education system. Research should also be broadened to explore the experience of teachers and education teams and their interaction with RtE pathways. The voice of CYP should also be sought to understand their experiences and understand what is important to them as they RtE after ABI. Next steps would be to investigate how support continues throughout a CYP’s educational career once initial RtE has been completed, the role of neurorehabilitation professionals across hospital and community contexts in supporting this, and the effectiveness of structured pathways in supporting RtE.
5Conclusions
This service evaluation set out to learn from the perspective of parents with lived experience of supporting their CYP’s RtE after ABI. Their comments and insights have highlighted areas of good practice, and deepened understanding of aspects of RtE which are important for health and educational professionals to improve, including communication, network support and awareness of ABI across these, and consideration of parental confidence and wellbeing. Despite better understanding of these issues and positive progress regarding best practice guidance, there remains a challenge as to how to disseminate best practice on a broader, national level to ensure appropriate and timely RtE support for CYP after ABI. Ideally, dissemination and delivery supported on a multisystem level by the UK government, DfE, and local health, education, and social care partnerships would ensure schools are trained and aware of their roles in RtE after ABI. In the longer-term, this evaluation also makes it clear that consistent, well-defined, child- and family-centered pathways for RtE are needed, with involvement and investment from both health and education.
Declaration of interest
The authors have no competing interests to declare.
Funding
The authors report no funding.
Acknowledgments
The authors would like to thank the parents who gave their time to share insights and views on the return to education process.
Ethical considerations
This study, as a service evaluation, was exempt from NHS Ethical Board approval. It was approved by the NHS Trust as a service evaluation.
References
1 | Anderson, V. , Spencer-Smith, M. , & Wood, A. ((2011) ). Do children really recover better? Neurobehavioural plasticity after early brain insult. Brain, 134: (8), 2197–2221. |
2 | Andersson, K. , Bellon, M. , & Walker, R. ((2016) ). Parents’ experiences of their child’s return to school following acquired brain injury (ABI): A systematic review of qualitative studies. Brain Injury, 30: (7), 829–838. |
3 | Babikian, T. , & Asarnow, R. ((2009) ). Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology, 23: (3), 283. |
4 | Bacon, J. K. , & Causton-Theoharis, J. ((2013) ). It should be teamwork’: a critical investigation of school practices and parent advocacy in special education. International Journal of Inclusive Education, 17: (7), 682–699. |
5 | Barnes, M. , Bennet, E. , & Etherington, J. (2018). Acquired brain injury and neurorehabilitation time for change: All party parliamentary group on acquired brain injury report. UKABIF: UK. |
6 | Bate, C. , Turner, K. , & Fricke, S. ((2021) ). Return to school after acquired brain injury in the UK–the educators’ perspectives. Journal of Research in Special Educational Needs, 21: (3), 242–253. |
7 | Bennett, E. , Thomas, S. , & Woolf, E. ((2022) ). Childhood acquired brain injury: the knowledge and training needs of special educational needs coordinators. Support for Learning, 37: (2), 209–224. |
8 | Braga, L. W. , Da Paz Junior, A. C. , & Ylvisaker, M. ((2005) ). Direct clinician-delivered versus indirect family-supported rehabilitation of children with traumatic brain injury: a randomized controlled trial. Brain Injury, 19: (10), 819–831. |
9 | Braun, V. , & Clarke, V. ((2006) ). Using thematic analysis in psychology. Qualitative Research in Psychology, 3: (2), 77–101. |
10 | Brown, F. L. , Whittingham, K. , McKinlay, L. , Boyd, R. , & Sofronoff, K. ((2013) ). Efficacy of Stepping Stones Triple P plus a stress management adjunct for parents of children with an acquired brain injury: The protocol of a randomised controlled trial. Brain Impairment, 14: (2), 253–269. |
11 | Burke, M. M. , & Hodapp, R. M. ((2016) ). The nature, correlates, and conditions of parental advocacy in special education. Exceptionality, 24: (3), 137–150. |
12 | Câmara-Costa, H. , Francillette, L. , Opatowski, M. , Toure, H. , Brugel, D. , Laurent-Vannier, A. ,... & Chevignard, M. ((2020) ). Participation seven years after severe childhood traumatic brain injury. Disability and Rehabilitation, 42: (17), 2402–2411. |
13 | Davies, S. C. , Fox, E. E. , Glang, A. , Ettel, D. , & Thomas, C. ((2013) ). Traumatic brain injury and teacher training: A gap in educator preparation. Physical Disabilities: Education and Related Services, 32: (1). |
14 | de Kloet, A. J. , Gijzen, R. , Braga, L. W. , Meesters, J. J. , Schoones, J. W. , & Vliet Vlieland, T. P. ((2015) ). Determinants of participation of youth with acquired brain injury: a systematic review. Brain Injury, 29: (10), 1135–1145. |
15 | DeMatteo, C. , Stazyk, K. , Giglia, L. , Mahoney, W. , Singh, S. K. , Hollenberg, R. ,... & Randall, S. ((2015) ). A balanced protocol for return to school for children and youth following concussive injury. Clinical Pediatrics, 54: (8), 783–792. |
16 | Department for Education. ((2014) ). Special Educational Needs and Disability Code of Practice: 0–25 Years. London: HMSO. |
17 | Eme, R. ((2014) ). ADHD and the Biological Roots of Violent Crime. The ADHD Report, 22: (7), 1. |
18 | Ettel, D. , Glang, A. E. , Todis, B. , & Davies, S. C. ((2016) ). Traumatic brain injury: Persistent misconceptions and knowledge gaps among educators. Exceptionality Education International, 26: (1). |
19 | Glang, A. , Ettel, D. , Tyler, J. S. , & Todis, B. (2013). Educational issues and school reentry for students with traumatic brain injury. Brain Injury Medicine, 602-620. |
20 | Hartman, L. R. , Duncanson, M. , Farahat, S. M. , & Lindsay, S. ((2015) ). Clinician and educator experiences of facilitating students’ transition back to school following acquired brain injury: A qualitative systematic review. Brain Injury, 29: (12), 1387–1399. |
21 | Hawley, C. A. , Ward, A. B. , Magnay, A. R. , & Mychalkiw, W. ((2004) ). Return to school after brain injury. Archives of Disease in Childhood, 89: (2), 136–142. |
22 | Hoarea, P. , & Beattieb, T. ((2003) ). Children with attention deficit hyperactivity disorder and attendance at hospital. European Journal of Emergency Medicine, 10: (2), 98–100. |
23 | Howe, J. , & Ball, H. ((2017) ). An exploratory study of Special Educational Needs Co-ordinators’ knowledge and experience of working with children who have sustained a brain injury. Support for Learning, 32: (1), 85–100. |
24 | Keenan, H. T. , Clark, A. E. , Holubkov, R. , Cox, C. S. , & Ewing-Cobbs, L. ((2018) ). Psychosocial and executive function recovery trajectories one year after pediatric traumatic brain injury: the influence of age and injury severity. Journal of Neurotrauma, 35: (2), 286–296. |
25 | Keetley, R. , Kelly, L. , Whitehouse, W. P. , Thomas, S. , Bennett, E. , Chow, G. ,... & Williams, J. ((2020) ). Early discharge and rehabilitation in paediatric acquired brain and neurological injury: a transferable model. Archives of Disease in Childhood - Education and Practice, 105: (1), 41–44. |
26 | Keetley, R. , Westwater-Wood, S. , & Manning, J. C. ((2021) ). Exploring participation after paediatric acquired brain injury. Journal of Child Health Care, 25: (1), 81–92. |
27 | Lalvani, P. (2012). Parents’ participation in special education in the context of implicit educational ideologies and socioeconomic status. Education and Training in Autism and Developmental Disabilities, 474-486. |
28 | Leo, G. S. , Macey, J. A. , & Barzi, F. ((2017) ). Educational outcomes for children with moderate to severe acquired brain injury. Australian Medical Student Journal, 8: (1), 46–50. |
29 | Linden, M. A. , Braiden, H. J. , & Miller, S. ((2013) ). Educational professionals’ understanding of childhood traumatic brain injury. Brain Injury, 27: (1), 92–102. |
30 | Lindsay, S. , Hartman, L. R. , Reed, N. , Gan, C. , Thomson, N. , & Solomon, B. ((2015) ). A systematic review of hospital-to-school reintegration interventions for children and youth with acquired brain injury. PLoS one, 10: (4), e0124679. |
31 | Max, J. E. , Lansing, A. E. , Koele, S. L. , Castillo, C. S. , Bokura, H. , Schachar, R. ,... & Williams, K. E. ((2004) ). Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Developmental Neuropsychology, 25: (1-2), 159–177. |
32 | McCarron, R. H. , Watson, S. , & Gracey, F. ((2019) ). What do kids with acquired brain injury want? Mapping neuropsychological rehabilitation goals to the international classification of functioning, disability and health. Journal of the International Neuropsychological Society, 25: (4), 403–412. |
33 | McKinlay, A. , Linden, M. , DePompei, R. , Aaro Jonsson, C. , Anderson, V. , Braga, L. ,... & Wicks, B. ((2016) ). Service provision for children and young people with acquired brain injury: Practice recommendations. Brain Injury, 30: (13-14), 1656–1664. |
34 | National Health Service England ((2013) ). 2013/14 NHS standard contract for paediatric neurosciences: neurorehabilitation. NHS England: London. https://www.england.nhs.uk/wp-content/uploads/2018/09/Paediatric-Neurorehabilitation.pdf |
35 | National Acquired Brain Injury in Learning and Education Syndicate (2018). N-ABLES information sheet. https://cdn.ymaws.com/ukabif.org.uk/resource/resmgr/nables/1671_n-ables_1pp_040320_amen.pdf |
36 | Norman, A. , Curro, V. , Holloway, M. , Percuklievska, N. , & Ferrario, H. (2022). Experiences of individuals with acquired brain injury and their families interacting with community services: a systematic scoping review. Disability and Rehabilitation, 1-13. |
37 | Paediatric Stroke Working Group, Royal College of Physicians of London. Clinical Effectiveness, & Evaluation Unit. (2004). Stroke in childhood: clinical guidelines for diagnosis, management and rehabilitation. Royal College of Physicians. |
38 | Rossetti, Z. , Redash, A. , Sauer, J. S. , Bui, O. , Wen, Y. , & Regensburger, D. ((2020) ). Access, accountability, and advocacy: Culturally and linguistically diverse families’ participation in IEP meetings. Exceptionality, 28: (4), 243–258. |
39 | Sariaslan, A. , Sharp, D. J. , D’Onofrio, B. M. , Larsson, H. , & Fazel, S. ((2016) ). Long-term outcomes associated with traumatic brain injury in childhood and adolescence: a nationwide Swedish cohort study of a wide range of medical and social outcomes. PLoS medicine, 13: (8), e1002103. |
40 | Savage, R. C. , DePompei, R. , Tyler, J. , & Lash, M. ((2005) ). Paediatric traumatic brain injury: A review of pertinent issues. Pediatric Rehabilitation, 8: (2), 92–103. |
41 | Thompson, M. , Elliott, C. , Willis, C. , Ward, R. , Falkmer, M. , Falkmer, T. ,... & Girdler, S. ((2016) ). Can, want and try: parents’ viewpoints regarding the participation of their child with an acquired brain injury. PLoS One, 11: (7), e0157951. |
42 | Todis, B. , & Glang, A. ((2008) ). Redefining success: Results of a qualitative study of postsecondary transition outcomes for youth with traumatic brain injury. The Journal of Head Trauma Rehabilitation, 23: (4), 252–263. |
43 | Tyerman, E. , Eccles, F. J. , & Gray, V. ((2017) ). The experiences of parenting a child with an acquired brain injury: A meta-synthesis of the qualitative literature. Brain Injury, 31: (12), 1553–1563. |
44 | UKABIF (2021). ABI RETURN: Children and young people with acquired Brain Injury – Guiding their Return to Education. UKABIF. https://ukabif.org.uk/page/ABIRETURN |
45 | UKABIF (2018). Time for Change: Acquired Brain Injury and Neurorehabilitation. UKABIF. https://cdn.ymaws.com/ukabif.org.uk/resource/resmgr/appg/1533_40pp_appg_on_abi_report.pdf |
46 | Wales, L. , Davis, K. , Kelly, G. , & Lynott, H. ((2021) ). Long Term Participation Outcomes for Severe Acquired Brain Injury in Childhood –An Expanded Scoping Review. Developmental Neurorehabilitation, 24: (6), 379–387. |
47 | Wilkinson, J. , Marmol, N. L. , Godfrey, C. , Wills, H. , van Eijndhoven, Q. , Botchway, E. N. ,... & Catroppa, C. ((2018) ). Fatigue following paediatric acquired brain injury and its impact on functional outcomes: a systematic review. Neuropsychology Review, 28: (1), 73–87. |
48 | Williams, H. , Chitsabesan, P. , Lennox, C. , Tariq, O. , & Shaw, J. ((2015) ). Traumatic brain injury in juvenile offenders: findings from the comprehensive health assessment tool study and the development of a specialist linkworker service. Journal of Head Trauma Rehabilitation, 30: (2), 106–115. |
49 | World Health Organization. (2001). The International Classification of Functioning, Disability and Health (ICF). Geneva: WHO. |
50 | Yeates, K. O. , Max, J. E. , & Narad, M. E. ((2021) ). Advances in understanding the association between pediatric traumatic brain injury and attention-deficit/hyperactivity disorder. JAMA pediatrics, 175: (10), 1001–1003. |




