Comparative effects of community-based family-child-centered care and conventional pediatric rehabilitation for cerebral palsy
Abstract
BACKGROUND:
While the transdisciplinary-based rehabilitation provided ample evidence on improving impairment (body structure and functions) levels, the therapeutic effects on the international classification of functioning, disability, and health (ICF) domains are unknown in cerebral palsy (CP).
OBJECTIVE:
To compare the effects of the community-based family-child-centered care (CFC) and conventional pediatric rehabilitation (CPR) on the physical, cognitive, sensory, and social integration domains in children and adolescents with CP.
METHODS:
Twenty-six participants with CP (mean age = 9.37±5.24, 14 females) were assigned into either CPR or CFC groups. Clinical outcomes included gross motor function measure (GMFM-66), Pediatric Balance Scale (PBS), fine motor area of Bruininks-Oseretsky Test of Motor Proficiency-2 (BOT-2), Functional Independence Measure (FIM) cognition area, Short Sensory Profile (sSP), COPM, Pediatrics Quality of Life (PedsQL) questionnaire, Short Falls Efficacy Scale (sFES), and Dynamic Postural Instability (DPI). An analysis of variance (ANOVA) and an analysis of covariance (ANCOVA) was conducted at P < 0.05.
RESULTS:
ANOVA revealed the superior effects of CFC in GMFM-66, PBS, BOT-2, FIM, and PedsQL compared to CPR (P < 0.05). ANCOVA showed the superior effects of CFC in Z-axis of DPI than CPR (P < 0.05).
CONCLUSIONS:
Our results provide novel, promising clinical evidence that CFC was more effective than CPR at improving impairment, activity, as well as participation levels in participants with CP.
1Introduction
In pediatric rehabilitation, cerebral palsy (CP) is the most common neuromuscular system conditions that present with multiple levels of impairments, activity limitations and associated participation restrictions. Epidemiological evidence reports relatively high prevalence of CP diagnosed (2–3 per 1,000 children) worldwide (Oskoui et al., 2013). CP is classically defined as a non-progressive neurodevelopmental disorder resulting from a brain lesion, which exhibits as spasticity, lack of coordination, muscle weakness, poor balance, and cognitive impairment (Sellier et al., 2016). The associated functional activity limitations include reaching, dressing, walking, and stair climbing. In addition, it is associated with restrictions of participation in social activities, including school, participating in presentations in class, and community leisure activities or sports (Rosenbaum et al., 2007).
Specifically, spastic CP is often related to cortical motor areas and white matter damage due to hypoxia-ischemia, and it manifests as hemiplegic, diplegic, and quadriplegic types (Serdaroglu et al., 2004). Depending on the severity of the sensory-motor impairment and the limb (s) involved, children with spastic CP present with myriad balance and locomotor dysfunctions (asymmetric gait or stiff or scissor-like gait), which in turn, predispose them to a high risk of falls, resulting in their restriction from participation in age-appropriate peer activities at school and in community sports and leisure clubs (Calley et al., 2012; Østensjø et al., 2003).
Dyskinetic CP is the second most common type of CP and is associated with damage to the subcortical gray matter, such as basal ganglia and thalamus, caused by hypoxia-ischemia, as well as by birth asphyxia and hyperbilirubinemia (Sellier et al., 2016). Commonly, maldevelopment due to brain damage and cortical/subcortical and basal ganglia lesions are accompanied by severe cognitive and language impairments (Himmelmann & Uvebrant, 2011). Children with dyskinetic CP present with involuntary, uncontrolled, repetitive, frequently stereotypical movements, muscle tone variations, and primitive reflex patterns, which in turn, predispose them to a high risk of falls, resulting in restrictions in their participation in age-appropriate peer activities at school and in community sports and leisure clubs (Østensjø et al., 2003).
Ataxic CP is the least common type of CP and is related to cerebellar malformations, vermis injury, and genetic mutations. Ataxic CP is mainly characterized by impairment in the coordination processes, indicated by problems in balance and walking, which lead to significant disability (Buckley et al., 2018). The decline in coordination and the decrease in stability with balance impairments limit throwing, kicking, and gait and later affect activities and independent participation in school or community (Michielsen et al., 2019; Parolin Schnekenberg et al., 2015).
To mitigate the neuromuscular and psychiatric-behavioral system conditions in both CP, a variety of interventional approaches including multidisciplinary-based rehabilitation, and transdisciplinary-based rehabilitation have been used.
Multidisciplinary-based rehabilitation is considered the key approach in rehabilitation and health care paradigms for children and adolescents with disabilities. Multidisciplinary-based rehabilitation is a complex process aimed at ensuring that children and their families achieve the best possible quality of life, and it considers the individual in relation to the physical, mental, emotional, communicative, and relational domains, and it involves their familial, social, and environmental context. A multidisciplinary-based pediatric rehabilitation study demonstrated positive effects on gross motor skills but no improvement in the participation domain. Such a lack of improvement in the participation domain may result from an inherent limitation in multidisciplinary-based pediatric rehabilitation, where the rehabilitation relies on the knowledge of practitioners from various specialties, including physical therapists, occupational therapists, speech therapists, social workers, pediatricians, physiatrists, ophthalmologists, neurologists, special educators, and psychologists, who operate only within their own professional fields rather than integrating the patient’s own goals and needs (Trabacca et al., 2012).
Transdisciplinary-based rehabilitation involves a team effort and cooperation to enhance patient outcomes through the synergy effects of teamwork, where the rehabilitation emphasizes the patient’s goals rather than the expert knowledge of individuals. The ultimate goal is to perform integrated assessment and to develop an integrated treatment plan based on patients’ goals (Hartwig & Landis, 1999). The rehabilitation team develops further assessment and intervention strategies, implements them with the help of family members, and the ability to swallow is improved through collaboration. Such improved results can be achieved by accommodating the patients’ own needs and goals and by providing rehabilitation that is focused on satisfying their immediate needs based on the expertise of the professionals (Walker & Avant, 2005).
In general, previous research on the proposed rehabilitation models (multidisciplinary-, and transdisciplinary-based rehabilitation) has laid a solid conceptual foundation for basic function implementation, and tremendous effort had been spent on improving impairment (body structure and functions) levels. However, very little focus has been devoted to optimizing all aspects of the ICF domains embracing the impairment, activity, and participation levels in the family environment, which is an essential part of pediatric rehabilitation care in community-dwelling children with chronic developmental disabilities. Building on the transdisciplinary approach, we developed “the community-based family-child-centered care (CFC) model.”
The purpose of the present study was to compare the effects of community-based family-child-centered care (CFC) and conventional pediatric rehabilitation (CPR). We hypothesized that CFC would show greater improvements in the physical, cognitive, sensory, and social integration domains than CPR in children and adolescents with CP.
2Methods
2.1Participants
A total of 26 children and adolescents with CP (mean age = 9.37±5.24, 14 females) were recruited from the community rehabilitation centers and from the Dongtan Aridm Welfare Center. The study was approved by the Research Ethics Committee of Yonsei University Mirae Campus (1041849-202009-BM-140-04) Institutional Review Board of the Republic of Korea. Written informed consent was obtained from parents or guardian. Inclusion criteria entailed: (1) diagnosed with CP, (2) aged between 1 and 21 years old, (4) GMFCS I–III for CP, and (6) able to follow instructions. Exclusion criteria included the following: (1) having epilepsy or taking epileptic drugs, (2) history of trauma or surgery within the last six months, (3) severe cognitive or visual impairments, and (4) cardiopulmonary system impairments.
2.2Experimental procedure
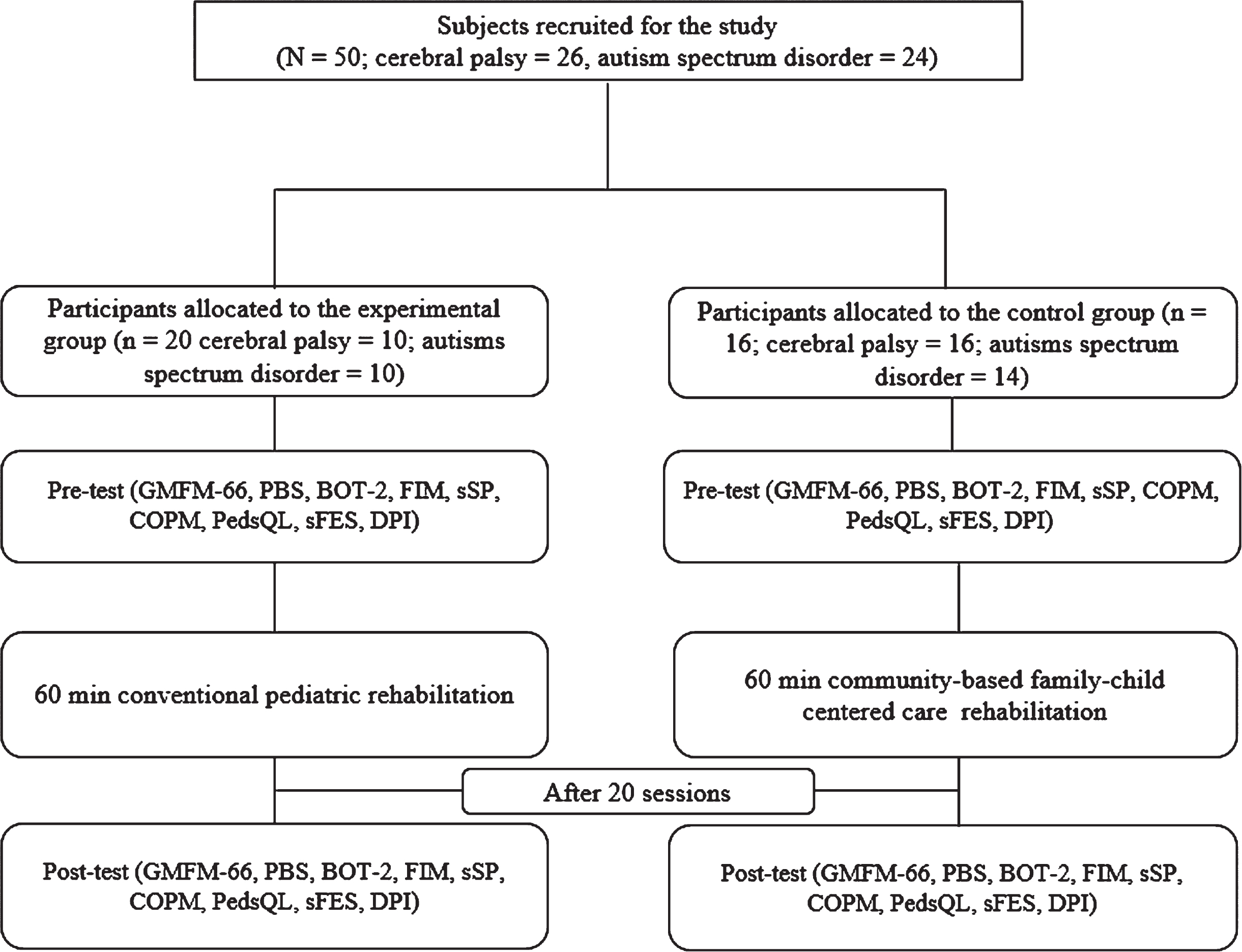
The present study comprised a two-group pretest-posttest design where the 26 participants were randomly assigned either to the CFC or the CPR group via a computer randomization program. A procedural checklist was followed to ensure consistent experimental protocols were observed prior to any data acquisition and throughout the entire test period. Standardized clinical testing procedures included the GMFM-66, Pediatric Balance Scale (PBS), fine motor area of BOT-2, Functional Independence Measure (FIM) cognition area, Short Sensory Profile (sSP), COPM, Pediatrics Quality of Life (PedsQL) questionnaire, Short Falls Efficacy Scale (sFES), and Dynamic Postural Instability (DPI) using a wearable device. These tests were consistently implemented at the pretest and posttest. The flowchart of the study is shown in Fig. 1.
Fig. 1
Flowchart of the study.
2.3Clinical function tests
All clinical functional tests were consistently performed three times with each child in the pretest and posttest by the same tester who was blind to the group assignment and to the results at each center.
2.3.1Gross motor function measure 66 (GMFM-66)
The GMFM-66 was used to evaluate changes in gross motor function in children and adolescents with CP in the activity domain of the ICF, which comprises five major testing sub-items: (A) lying and rolling, (B) sitting, (C) crawling and kneeling, (D) standing, and (E) walking, running, and jumping (Kenyon, 2014). The scoring system entails a 4-point scale, which ranges from 0 to 3, where 0 (‘No initiation’), 1 (‘Initiation’), 2 (‘Partial completion’), and 3 (‘completion’). The intra- and intertester reliability for GMFM-66 is well established with intraclass correlation coefficient (ICC) = 0.96 and 0.97, respectively (Wei et al., 2006).
2.3.2Pediatric balance scale (PBS)
The PBS was used to assess functional balance ability for children with neuromuscular motor impairments in the body function and structure domain of the ICF model (Franjoine et al., 2003). Fourteen test items include seated position to standing position, standing position to sitting position, transfer, standing without support, sitting without support, standing with eyes closed, standing with feet together, standing with one foot in front, standing on one foot, rotating 360 degrees, turning to look back, picking up an object off the floor, placing alternate foot on step or footrest, and reaching forward with extended arm. The test scores range from 0 (‘low function’) to 4 (‘the highest function’), with a potential total score of 56 points. The intra- and intertester reliability of PBS is well established with ICC = 0.97 and 0.98, respectively (Her et al., 2012).
2.3.3Short sensory profile (sSP)
The sSP questionnaire was used to evaluate children’s sensory processing dysfunction in daily life in the body function and structure domain of the ICF model (Tomchek & Dunn, 2007). The questionnaire is comprised of 38 items including the seven functions of sensory processing (tactile sensitivity, taste/smell sensitivity, movement sensitivity, under-responsiveness/seek sensation, auditory filtering, low energy/weak, visual/auditory sensitivity). The questionnaire responses range from 1 (‘always’) to 5 (‘never’) as associated with the child behaviors (Tomchek & Dunn, 2007). The validity and reliability of the sSP is well established with r = 0.87 and ICC = 0.88, respectively (O’Brien et al., 2009).
2.3.4Bruininks-oseretsky test of motor proficiency (BOT-2)
The BOT-2 test was used to assess gross and fine motor skills in children with disabilities in the activity domain of the ICF model. The testing items includes body coordination, manual coordination, motor performance, and fine manual control, which examines motor skills connecting coordination and control of the distal part of the hands and fingers (Deitz et al., 2007). The validity and reliability of BOT-2 are well established with Cronbach’s α= 0.92 and ICC = 0.99, respectively (Wuang & Su, 2009).
2.3.5Functional independence measure (FIM)
The FIM was used to determine basic quality of daily living activities in people with disabilities in the activity domain of the ICF model. The FIM consists of 18-items, with subscales for self-care (6-items), sphincter control (2-items), transfers (3-items), locomotion (2-items), communication (2-items), and social cognition (3-items). Each item is answered on a 7-point scale, where 1 (‘total assistance with helper’) to 7 (‘complete independence with no helper’) (Linacre et al., 1994). The validity and reliability of FIM are well established with Kappa coefficient = 0.92 and ICC = 0.99, respectively (Kidd et al., 1995).
2.3.6Short falls efficacy scale (sFES)
The sFES questionnaire was used to measure the participant’s fear of falling during a range of activities of daily living in the activity domain of the ICF model. The sFES was comprised of seven items. Each daily living activity has a 4-point scale, where 1(‘not at all concerned’), 2(‘somewhat concerned’), 3(‘fairly concerned’), 4(‘very concerned’). Total scores range from 7 (‘low concern’) to 28 (‘high concern’) (Kempen et al., 2008). The validity and reliability of sFES are well established as Cronbach’s α= 0.94 and ICC = 0.99, respectively (Azad et al., 2014).
2.3.7Canadian occupational performance measure (COPM)
The COPM is an individualized criterion-referenced measurement tool designed for assessing changes in occupational performance and the satisfaction of clients receiving occupational therapy in the participation domain of the ICF model. In the COPM process, the client considers the five problems in four domains and evaluates the importance of each problem on a range of 1 to 10. They then, prioritize the five problems and evaluate their performance and satisfaction in the range of 1 to 10 for each of the problems. The higher the scores, the higher importance and the higher the performance and satisfaction (McColl et al., 2000). The validity and reliability of COPM are well established as Cronbach’s α= 0.89 and ICC = 0.99, respectively (Berardi et al., 2019).
2.3.8Pediatrics quality of life (PedsQL) questionnaire
The PedsQL questionnaire was used to measure quality of life in children and adolescents in the participation domain of the ICF model. The questionnaire consists of 23 items, made up of physical functioning (8-items), emotional functioning (5-items), social functioning (5-items), and school functioning (5-items). Each item is answered on a 5-point scale, where 0(‘never a problem’), 1(‘almost never a problem’), 2(‘sometimes a problem’), 3(‘often a problem’), 4(‘almost always a problem’) (Varni et al., 1999). The validity and reliability of COPM are well established as Cronbach’s α= 0.93 and ICC = 0.89, respectively (Desai et al., 2014; Varni et al., 2003).
2.4Body sway measurement
2.4.1Instrument
The PostureRite DPI (PostureRite DPI, Mezoo, Wonju, South Korea) is a wearable device used to measure body sway during functional and social participation environmental tasks. The PostureRite DPI system comprises three axis accelerometers (X, Y, Z axis) a gyro-accelerometer sensor and a portable data receiver, which transmits data via Bluetooth to a laptop. The 3-axis gyro-accelerometer sensor is capable of recording AP, ML, and Vertical acceleration sway signals, which were used to compute DPI.
2.4.2Data collection
The participant was positioned sitting on a supported chair. The targeted skin area was prepared by abrading with rubbing alcohol prior to placement of the DPI sensor. The DPI sensor was attached to at the 1/3 on the line between the jugular notch and the xiphoid process of the sternum where the signals can be best detected (Fazio et al., 2013). All participants were first familiarized with the DPI testing procedure. The DPI data were collected during self-preferred overground walking, as indicated in the GMFM subtest, in all participant with CP, at a sample rate of 30 Hz. The DPI data were recorded three consecutive times for 60 seconds and the acquired DPI data were processed with root mean square (RMS) and saved for further statistical analysis.
2.4.3Data analysis
The processed DPI data were exported to MatLab v2010a to calculate the AP, ML, and Vertical coefficient of variations (CVs), which are expressed as
Specifically, the DPI (acceleration sway signals) were divided into three 10s windows and the standard deviation (SD) was computed for each window. If the SD of at least one of the three windows exceeded five times the SD of one of the other windows, the trial was discarded. A larger CVs represents greater dynamic postural instability during walking.
Fig. 2
The PostureRite DPI.

2.5Intervention
All participants were assigned the standard CPR or CFC interventions, which comprised 60 min/day, 2 days/week with an average of 20 sessions over 10 weeks. CPR rehabilitation was based on the neurodevelopmental treatment (NDT) framework and clinical evidence. CPR rehabilitation in children with CP included mobility exercises, stability exercises according to muscle stretching and strengthening and dynamic or static balance, with gradual progression to overground gait training with or without assistive devices, sensory integration approach and fine motor control. For the intervention strategies in the physical domain, a licensed physical therapist provided the interventions based on the evaluation of selected clinical evidence. The corresponding interventions included stretching (Katalinic et al., 2010), strengthening (Effgen & McEwen, 2008), hippotherapy (Park & You, 2018; Park et al., 2014), treadmill training (Damiano & DeJong, 2009), NDT (Gündüz et al., 2019), robotic assisted gait training (RAGT)(Jin et al., 2020; Park et al., 2020). RAGT (Walkbot, P&S mechanics, Seoul, Korea) was provided to improve gait function. RAGT can provide systemic assistance or resistance interactively in response to the participant’s muscle strength, movement, and fatigue conditions during gait training. The Walkbot system interactively adjusted the walking speed and resistive torque parameters while attempting to minimize kinematic trajectory errors. The assistance guidance force was systematically reduced from 100%(passive mode) to 0%(active mode), where the Walkbot system automatically adjusted the body weight bearing load, resistance, and inertia to accomplish the symmetrical, optimal gait pattern, as it can apply a differential mode to each lower extremity for individuals with hemiparetic CP (Jin et al., 2020). For the intervention strategies of the cognitive domain, a licensed occupational therapist provided the interventions based on the evaluation and selected clinical evidence. The corresponding interventions included fine motor function training, and activities for daily living training (Ko et al., 2020). For the intervention strategies of the sensory domain; and for the intervention strategies of the cognitive domain, an occupational therapist with a sensory integration license provided interventions based on the evaluation and selected clinical evidence. The corresponding interventions included sensory integration (Novakovic et al., 2019). For the intervention strategies of the social integration domain were not carried out in the CPR group.
The CFC rehabilitation for children with CP utilized COPM to identify the important goals of individual children and to develop specific interventional strategies customized for the gross and fine motor of needs of the children with disabilities and customized for the sensory and emotional development goals of the children so as to cover four domains including physical, cognitive, sensory, and social integration. The CFC rehabilitation was derived from the NDT framework based on evidence and the detailed treatment protocol is outlined in Supplementary Table 1. The CFC rehabilitation in children with CP included mobility exercises, stability exercises, controlled mobility exercises, and skilled mobility exercises according to muscle stretching and strengthening and dynamic or static balance, and gradual progression to overground gait training with or without assistive devices, sensory integration approach, fine motor control and counselling for parents and children with CP. For the intervention strategies of the physical domain, a licensed physical therapist provided the interventions based on the evaluation and selected clinical evidence. The corresponding interventions included stretching (Katalinic et al., 2010), strengthening (Effgen & McEwen, 2008), hippotherapy (Park & You, 2018; Park et al., 2014), treadmill training (Damiano & DeJong, 2009), NDT (Gündüz et al., 2019), and RAGT (Jin et al., 2020; Park et al., 2020). For the intervention strategies of the cognitive domain, a licensed occupational therapist provided the interventions based on the evaluation and selected clinical evidence. The corresponding interventions included fine motor function training, and activities for daily living training (Ko et al., 2020). For the intervention strategies of the sensory domain, For the intervention strategies of the cognitive domain, an occupational therapist with a sensory integration license provided the interventions based on the evaluation and selected clinical evidence. The corresponding interventions included sensory integration (Novakovic et al., 2019). For the intervention strategies of the social integration domain, a licensed occupational therapist evaluated COPM and worked with the physical therapist, occupational therapist, and social worker to diagnoses and set goals for the interventions through a team approach. Based on the evaluation and clinical evidence, the corresponding interventions included counselling for parents and children with CP, a social integration program according to a focus group interview (FGI) (Vaughn et al., 1996). The established COPM goals and specific intervention strategies were implemented at the local pediatric community rehabilitation center, and consistently integrated at child’s school or community activity centers as well as in the home environment to maximize the physical-cognitive-sensory-social integration.
2.6Statistical analysis
The descriptive statistics included mean and standard deviation. An analysis of variance (ANOVA) was used to determine the intervention-related changes in the outcome variables: (1) GMFM-66, (2) PBS, (3) BOT-2, (4) FIM, (5) sSP, (6) COPM, (7) PedsQL, and (8) sFES and reflecting differences between the CFC and CPR groups. An analysis of covariance (ANCOVA) was used for between-group comparisons because the baseline (pretest) DPI outcome measurement data were statistically different between the CFC and CPR groups. If the interaction effect was observed, Tukey’s HSD (honest significant difference) post hoc test was implemented. We used the G-Power software (G-Power version 3.1.5) to assess the sample size based on our previous study which yielded 46 participants, computing from the effect size (Eta squared, η2 = 0.6) and power (1–β= 0.8) for the GMFM-66, PBS, and BOT-2 variables (Kim et al., 2016; Ko et al., 2020). An independent t-test or chi-square was used to compare general participant characteristics between the CFC and CPR groups, depending on the interval and nominal scale, respectively. A paired t-test was used to compare the following measurements for the pre-test and post-test: (1) GMFM-66, (2) PBS, (3) BOT-2, (4) FIM, (5) sSP, (6) COPM, (7) PedsQL, (8) sFES and (9) DPI. Tukey’s post-hoc test was used to calculate significance between groups. All statistical analyses were performed via the Statistical Package for the Social Sciences (SPSS) version 25, software (SPSS Inc., Chicago, IL, US). The statistical significance level was set at 0.05 for all tests.
3Results
3.1Demographic characteristics of participants
The demographic characteristics of participants are presented in Table 1. No significant differences were observed between the two groups in baseline characteristics, including gender, age, height, weight, and body mass index (BMI).
Table 1
Baseline characteristics of the participants
| CPR group (n = 10) | CFC group (n = 16) | p | |
| Gender (male/female) | 5/5 | 9/7 | 0.84 |
| Age | 10.00±4.41 | 8.73±6.06 | 0.93 |
| Body height (cm) | 129.88±15.14 | 119.07±30.39 | 0.14 |
| Body mass (kg) | 29.06±12.12 | 28.35±19.14 | 0.10 |
| aBMI (kg/m2) | 16.72±4.40 | 17.82±3.44 | 0.30 |
| bCP sort | |||
| Spastic/Hemiplegic/Ataxic/Athetosis | 8/1/0/1 | 9/2/2/3 | 0.67 |
aBMI: Body Mass Index. bCP: Cerebral palsy.
3.2Clinical function tests
3.2.1Physical domains
3.2.1.1GMFM ANOVA analysis showed significant changes in the A, C, and total score of GMFM-66 between the CPR group and CFC group of children with CP. In addition, post-hoc analysis using the Tukey’s post hoc confirmed more significant gross motor movement and function after treatment in the CFC group compared to CPR group (Table 2).
Table 2
Comparison of change in GMFM and BOT-2
| aGMFM | bCPR group | cCFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| A | 98.72±3.52 | 98.72±3.52 | 1.00 | 72.03±33.16 | 89.21±17.50 | 0.00* | 0.01* | 0.59 |
| B | 89.82±18.30 | 89.82±18.30 | 1.00 | 63.49±34.25 | 78.33±27.75 | 0.37 | 0.24 | 0.03 |
| C | 89.03±15.77 | 88.99±15.77 | 0.33 | 51.48±36.66 | 66.62±34.07 | 0.01* | 0.23 | 0.59 |
| D | 73.02±35.10 | 73.02±35.10 | 1.00 | 32.67±32.56 | 46.62±36.85 | 0.14 | 0.18 | 0.48 |
| E | 71.49±33.48 | 71.52±33.49 | 0.81 | 22.57±25.75 | 35.94±35.92 | 0.04* | 0.05* | 0.49 |
| Total | 72.48±22.49 | 72.46±22.48 | 0.66 | 48.29±30.17 | 63.96±28.73 | 0.04* | 0.05* | 0.49 |
| dBOT-2 | CPR group | CFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| 56.25±15.58 | 59.00±15.49 | 0.00* | 34.25±23.51 | 50.73±20.50 | 0.00* | 0.04* | 0.63 | |
aGMFM, Gross motor function measure; bCPR, Conventional pediatric rehabilitation; cCFC, Community-based family-child centered care; dBOT-2, Bruininks-Oseretsky test of motor proficiency-2; *P < 0.05.
3.2.1.2BOT-2 ANOVA showed significant changes in the BOT-2 score between the CFC group and CPR group. Moreover, Tukey’s post-hoc analysis revealed that the CFC group showed greater increase in the BOT-2 score than the CPR groups (Table 2).
3.2.1.3PBS NOVA showed significant changes in the PBS score between the CPR group and CFC group. Moreover, produced a significant time x group interaction effect in the CFC group (P = 0.00). Tukey’s post-hoc analysis revealed that the CFC group showed greater increase in the PBS score than the CPR groups (Table 3).
Table 3
Comparison of change in PBS and DPI
| aPBS | bCPR group | cCFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| 28.88±13.56 | 28.88±13.56 | 1.00 | 16.69±17.06 | 23.13±20.99 | 0.00* | 0.04* | 0.65 | |
| dDPI | CPR group | CFC group | Between | Effect | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | P-value | size | |
| X-axis | 21.67±8.56 | 23.98±11.82 | 0.04* | 74.66±41.23 | 51.40±22.76 | 0.12 | 0.57 | 0.57 |
| Y-axis | 24.39±10.04 | 29.51±13.00 | 0.61 | 66.84±31.12 | 71.55±27.01 | 0.06 | 0.54 | 0.67 |
| Z-axis | 32.86±13.09 | 22.23±7.86 | 0.33 | 77.53±37.84 | 59.52±27.01 | 0.02* | 0.68 | 0.38 |
aPBS, Pediatric balance scale; bCPR, Conventional pediatric rehabilitation; cCFC, Community-based family-child centered care; dDPI, Dynamic postural instability; *P < 0.05.
3.2.1.4DPI ANCOVA did not show significant differences in the DPI between CPR and CFC group, but it demonstrated a significant time main effect in the CFC group (P = 0.02) on the Z-axis. Our effect size analysis indicates a medium effect (Eta squared, η2 = 0.38–0.67), suggesting a greater decrease in body sway after in the CFC group than in the CPR group (Table 3).
3.2.2Cognitive domains
3.2.2.1FIM ANOVA demonstrated a significant difference in the FIM score of the CPR group and CFC group. Moreover, our effect size analysis indicated a small effect (Eta squared, η2 = 0.15). Tukey’s post-hoc analysis revealed that the CFC group showed greater increase in the FIM score than the CPR groups (Table 4).
Table 4
Comparison of change in FIM
| aFIM | bCPR group | cCFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| 20.90±11.71 | 20.90±11.71 | 1.00 | 28.50±5.39 | 29.58±4.96 | 0.00* | 0.04* | 0.15 | |
aFIM, Functional independence measure; bCPR, Conventional pediatric rehabilitation; cCFC, Community-based family-child centered care; *P < 0.05.
3.2.3Sensory domain
3.2.3.1sSP ANOVA did not show significant a difference in the sSP score between the CPR group and the CFC group, but it produced a significant time main effect in the CFC group (P = 0.00). Moreover, our effect size analysis indicates medium effect (Eta squared, η2 = 0.27) (Table 5).
Table 5
Comparison of change in sSP
| asSP | bCPR group | cCFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| 157.20±14.49 | 153.40±20.67 | 0.22 | 141.31±24.54 | 147.25±25.34 | 0.00* | 0.53 | 0.27 | |
asSP, Short sensory profile; bCPR, Conventional pediatric rehabilitation; cCFC, Community-based family-child centered care; *P < 0.05.
3.2.4Social integration domains
3.2.4.1COPM ANOVA did not show significant differences in the COPM score between the CPR group and the CFC group (P = 0.04), but it produced a significant time main effect in the CFC group (P = 0.00) in performance and satisfaction. Moreover, our effect size analysis indicates a medium effect (Eta squared, η2 = 0.34–0.56), indicating a slightly increase performance and satisfaction score in the CFC group compared to the CPR group (Table 6).
Table 6
Comparison of change in social integration domains
| aCOPM | bCPR group | cCFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| Performance | 4.31±2.15 | 3.94±2.46 | 0.35 | 3.66±1.69 | 5.01±1.82 | 0.00* | 0.24 | 0.34 |
| Satisfaction | 4.00±1.65 | 3.56±1.94 | 0.35 | 3.96±1.76 | 5.22±1.93 | 0.00* | 0.06 | 0.56 |
| dsFES | CPR group | CFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| 17.00±7.54 | 17.00±7.54 | 1.00 | 20.13±6.21 | 18.06±6.76 | 0.00* | 0.73 | 0.19 | |
| ePedsQL | CPR group | CFC group | Between P-value | Effect size | ||||
| Pre-test | Post-test | P-value | Pre-test | Post-test | P-value | |||
| Problem with physical function | 25.00±10.14 | 22.50±9.92 | 0.55 | 18.81±8.29 | 9.63±7.74 | 0.00* | 0.00* | 0.93 |
| Problem with emotional function | 9.00±6.09 | 7.90±7.13 | 0.25 | 7.25±4.64 | 5.63±3.96 | 0.014 | 0.22 | 0.59 |
| Problem with social function | 13.40±6.50 | 11.00±6.58 | 0.33 | 10.53±6.76 | 8.50±5.97 | 0.25 | 0.16 | 0.43 |
| Problem with school function | 10.00±6.25 | 10.80±5.35 | 0.26 | 8.69±4.98 | 6.25±5.11 | 0.06 | 0.06 | 0.61 |
| total | 57.60±18.52 | 55.20±22.54 | 0.47 | 43.25±16.22 | 28.63±17.65 | 0.00* | 0.01* | 0.84 |
aCOPM, Canadian occupational performance measure; bCPR, Conventional pediatric rehabilitation; cCFC, Community-based family-child centered care; dsFES, Short falls efficacy scale; ePedsQL, Pediatric quality of life inventory; P < 0.05.
3.2.4.2sFES ANOVA did not show a significant difference in the sFES score between the CPR group and the CFC group, but it produced a significant time main effect in the CFC group (P = 0.00). However, our effect size analysis indicates a small effect (Eta squared, η2 = 0.19), indicating a slightly decrease fear of falling in the CFC group compared to the CPR group (Table 6).
3.2.4.3PedsQL ANOVA demonstrated significant differences in the PedsQL scores between the CPR group and the CFC group. Moreover, Tukey’s post-hoc analysis revealed that the CFC group showed greater increase in the PedsQL scores than the CPR groups (Table 6).
4Discussion
The present study is the first clinical study to highlight the superior effects of CFC rehabilitation compared to CPR rehabilitation in the physical domain (GMFM-66, PBS, BOT-2, DPI), the cognitive domain (FIM), the sensory domain (sSP), and the social integration domain (COPM, PedsQL, sFES) in children with CP. Consistent with our hypothesis, the CFC group demonstrated a significantly greater improvement than the CPR group, in certain outcomes in the physical, cognitive, sensory, and social integration domains, which included improved gross and fine motor function, balance, body sway, cognitive function, sensory motor function, and quality of life. The CFC rehabilitation emphasizes the importance of providing opportunities to practice relevant personal community individualized-skills and gives time to parent education regarding how they may best assist their child and how one can progress to return the level of community including the school and social welfare center (Mayston, 2001). Bhatia and Joseph (2000) highlighted the need for comprehensive evaluation and comprehensive treatment of children with CP to identify all their related problems so as to perform appropriate its intervention (Bhatia & Joseph, 2000). However, no previous clinical study has been performed with CFC rehabilitation and associated recovery in the physical, cognitive, sensory, and social integration domains recovery in children with CP, which made difficult to compare the effects of CFC with previous evidence in the current literature.
Clinical data analyses from the physical domain revealed more significant improvements in the CFC group relative to the CPR group in the following areas: BOT-2 (between-group mean difference = 27.83%), PBS (between-group mean difference = 26.02%), DPI (between-group mean difference = 14.11%on the X-axis, between-group mean difference = 15.41%on the Y-axis, between-group mean differences = 28.18%on the Z-axis) in the CFC group compared to the CPR group. Further, clinical data analyses from the physical domain also showed improvements in total score in the CFC group compared to the CPR group. This finding was consistent with the results of Champagne and colleagues (2017) who reported a 6.28%increase in GMFM-66 score and a 34.45%increase in BOT-2 score after applying hippotherapy in children with CP. A study assessed the effect of the NDT on gross motor and balance in children with CP. This study demonstrated further improvements in the GMFM-66 score (4.7%) and the PBS score (10.87%) (Kavlak et al., 2018). A possible underlying mechanism for such positive improvements is that the CFC rehabilitation increases postural muscle size, which maintain equilibrium, while at the same time child with CP may have resisted using the subconscious feedforward mechanism by which the transverse abdominis (TrA) and multifidus are synergistically co-activated for upright spinal postural stability (Bordoloi & Sharma, 2012). That stabilizers muscles such as the TrA and multifidus contribute to static postural control is supported by Elshafey (2014), who report a significant improvement in trunk alignment morphology and balance after hippotherapy simulator treatment in children with hemiplegic CP (Elshafey, 2014). The CFC rehabilitation is facilitated by a realigning the uprighting movement and the positioning of the pelvic girdle, which helps normalize the proprioceptive inputs of the cervical-lumbo-pelvic region. This facilitates the selective concentric activation of the deep core muscles. The CFC rehabilitation was designed to activate and strengthen the underactive or weak abdominal musculature and, as a result, cortically or consciously increases cutaneous awareness of using vibration. Damiano and colleagues (1995) showed that a six-week progressive quadriceps resistance muscle strength program involving the performance of exercises with a load intensity of 65%three times a week significantly enhanced the degree of crouch pattern, gait speed, and stride length in spastic diplegic CP (Damiano et al., 1995). Similarly, Eagleton and colleagues (2004) found that a generalized progressive strengthening exercise of the trunk and lower extremity muscles performed with an intensity of 80%three times a week for six weeks improved gait velocity, cadence, step length, distance, and energy expenditure (Eagleton et al., 2004). In particular, strengthening the knee extensors reduced abnormal co-contraction between the knee extensors and flexors during the stance phases and improved stride length during gait. These findings suggest that improved balance between the agonist-antagonist muscles may account for the decreased crouched and stiff hip-knee-ankle with strengthened quadriceps while relatively decreasing hamstring co-activation during gait.
Clinical data analyses for the cognitive domain revealed more significant improvements in FIM in the CFC group compared to the CPR group (between-group mean difference = 14.71%). Further, clinical data analyses from the cognitive domain also showed improvements in CARS in the CFC group compared to the CPR group. This finding was consistent with the results of Song (2014), who reported a 6.86%increase in functional independence measure for children (WeeFIM) score after applying fine motor training in children with CP (Song, 2014).
A possible underlying mechanism for such positive cognitive function improvement is that CFC rehabilitation provides KR and KP feedback, in which visual motor learning strategy (motor and clinical) improvements were related to better memory, mental flexibility, and planning abilities. Presumably, these cognitive processes are more involved in making use of critical information about moving and adapting motor behavior to improve efficiency. The role of augmented feedback in facilitating skills acquisition and learning is a widely accepted reality. The findings of a descriptive study on augmented feedback conducted by Hebert and Landin (1994) revealed that instructors delivered feedback including knowledge of performance (KP), knowledge of results (KR), and behavioral at a rate of 1.5 per minute (Hebert & Landin, 1994). In addition, Hebert and Landin (1994) reported that over half (53%) of all feedback delivered to participants was evaluative in nature and addressed performance outcome (KR), leaving a smaller percentage (42%) of feedback dedicated to information or the execution of a movement pattern (KP) (Hebert & Landin, 1994). Primarily, these researchers have utilized KP to inform participant about performance errors in their movement pattern (s) while the participants practiced a motor task in a laboratory setting.
Clinical data analyses from the sensory domain showed significant improvements in sSP (between-group mean difference = 2.01%) in the CFC group compared to the CPR group. The neurological impairments of CP children affect sensory information processing, such as the tactile, vestibular, and proprioceptive systems, during their daily activities. The present results indicate that CFC can assist in the activation of nerve (thermal receptor, pain receptor, location receptor) signals to induce cortical reorganization and improve sensorimotor function during sensory integration. This finding is consistent with the results of Papavasiliou and colleagues (2011), who reported that changes in sSP scores (2.05%) after applying sensory integration in children with disabilities were not significant (Papavasiliou et al., 2011). In a previous study, a sensory integration intervention was applied only to children with disabilities, and not to children with CP (Parham et al., 2007). However, it is difficult to compare the present findings with data from a previous study because no appropriate evidence is available in the literature. Our findings support prior evidence that demonstrated more enhanced motor control in the diaphragm and transversus abdominis (TrA)/ internal obilique (IO) muscle after dynamic neuromuscular stabilization (11–18%) than after the abdominal drawing-in maneuver (Son et al., 2017). Such CFC therapeutic effects may offer an explanation of the specific sensory neural adaptations that accompany a vibration treatment. Sound based vibration resonates throughout the body and facilitates the ability to sense the position, location, and orientation (King et al., 2009). Vibration might also alter the connectivity between corticospinal cells and spinal motoneurons (Delecluse et al., 2003). The stimulation of proprioceptive pathways via vibration treatment seems therefore crucial. It is assumed that this repetitive stimulation rearranges motor control strategies and may result in improved postural stability (Schuhfried et al., 2005). One should also consider the influence of vibration stimuli on central motor structures, as it is shown that vibration activates the primary sensorimotor cortices, supplementary motor area (SMA) and cingulate motor area (CMA). All these areas are active when executing limb movements (Naito & Ehrsson, 2001). A possible underlying mechanism for such positive improvement is that CFC rehabilitation responds to emotions with immediacy, accompanied by involuntary physiological responses, in which changes in heart rate, respiration rate, body temperature, and hormone excretion are related to sensory function (Chanda & Levitin, 2013). Furthermore, Bhattacharya’s neuroimaging studies (2001) have shown that music perception engages a widespread bilateral network of frontal, temporal, and parietal areas, and the cerebellum, as well as sub-cortical regions related to attention, working and semantic memory, motor functions, and information processing speed (Bhattacharya et al., 2001). Such CFC rehabilitation thus includes tactile, vestibular, and proprioceptive system stimulation activities (thermal receptors, pain receptors, location receptors) such that therapeutic effects may induce cortical reorganization, stimulate the limbic system, and improve sensorimotor function to calm down or awaken hypersensitive or hyposensitive children to their surroundings. This results in children increasing their balance function, which improves their gait ability and attention.
Clinical data analyses from the social integration domain showed more significant improvements in the CFC group compared to the CPR group: in COPM (between-group mean difference = 43.06%in performance, between-group mean difference = 31.67%in satisfaction), sFES (between-group mean difference = 10.53%), and in PedsQL (between-group mean difference = 18.24%). This finding was consistent with the results of Lin and colleagues (2011) who demonstrated a 13.62%increase in PedsQL score after applying comprehensive rehabilitation in children with CP (Lin et al., 2011). In another study, Novak and colleagues (2009) demonstrated improvements in the COPM performance score (13.66%) and the COPM satisfaction score (2.49%) (Novak et al., 2009). Additionally, Shamy and Kafy (2014) reported that the fear of falling score decreased by 34.42%after applying comprehensive rehabilitation that included balance training and postural balance control to children with CP (El-Shamy & Abd El Kafy, 2014).
The present results indicate that CFC can determine which therapeutic approach is most effective for specific clients and to ensure the effectiveness of the intervention through client-centered individual goal setting and by developing individualized intervention programs that meet the specific therapeutic needs of the clients.
In summation, we have been the first to developed CFC rehabilitation for children with CP, and this has opened new possibilities in terms of an integrated approach to rehabilitation, which includes the physical, cognitive, sensory, and social integration domains. A couple of limitations in the present study should be considered in the future. The first limitation is that the sample size for the control group was weak due to difficulties in recruiting participants due to COVID-19. Clinicians should therefore interpret these results cautiously. The second limitation is that the intervention was temporarily stopped due to COVID-19. If the intervention had been continued, the results would probably have been different. Future studies need to increase the size of the control group and clarify the specific contributions of CFC rehabilitation to children with CP through follow-up. Our study suggests that a transdisciplinary and comprehensive approach to rehabilitation, initiated in well-equipped centers with various specialties, can improve the diagnosis and help formulate appropriate interventions for children with CP and thereby ensure improved long-term results. Efforts should be made worldwide to support public-private collaboration and to make such centers accessible and sustained.
5Conclusion
The present investigation compared the effects of CFC rehabilitation and CPR rehabilitation with children with CP demonstrated that CFC rehabilitation was effective in the physical, cognitive, sensory, and social integration domains. Clinically, the results offer encouraging evidence that CFC rehabilitation is more effective than CPR rehabilitation when managing children with CP. Our findings provide important insights for clinicians when designing an effective pediatric rehabilitation model to manage comprehensive domains (physical, cognitive, sensory, and social integration domains) for children with CP.
Acknowledgments
This research received financial and administrative support from the Korea Health Industry Development Institute (grant no. HI18C1687000020) and Brain Korea 21 PLUS Project (grant no. 2019-51-0018) for the Department of Physical Therapy in Graduate School, Yonsei University.
Conflict of interest
None to report.
Supplementary materials
[1] Supplementary Table 1 is available from https://dx.doi.org/10.3233/NRE-210219.
References
1 | Azad, A. , Mehraban, A. H. , Mehrpour, M. , & Mohammadi, B. ((2014) ). Clinical assessment of fear of falling after stroke: validity, reliability and responsiveness of the Persian version of the Fall Efficacy Scale-International, Medical journal of the Islamic Republic of Iran, 28: , 131. |
2 | Berardi, A. , Galeoto, G. , Guarino, D. , Marquez, M. A. , De Santis, R. , Valente, D. , Caporale, G. , & Tofani, M. ((2019) ). Construct validity, test-retest reliability, and the ability to detect change of the Canadian Occupational Performance Measure in a spinal cord injury population. Spinal Cord Series and Cases, 5: , (1), 1–8. |
3 | Bhatia, M. , & Joseph, B. ((2000) ). Rehabilitation of cerebral palsy in a developing country: the need for comprehensive assessment. Pediatric Rehabilitation, 4: , (2), 83–86. |
4 | Bhattacharya, J. , Petsche, H. , & Pereda, E. ((2001) ). Long-range synchrony in the γ band: role in music perception. Journal of Neuroscience, 21: , (16), 6329–6337. |
5 | Bordoloi, K. , & Sharma, N. ((2012) ). Effectiveness of proprioceptive training over strength training in improving the balance of cerebral palsy children with impaired balance. Scientific Research Journal of India, 1: , (1), 23–36. |
6 | Buckley, E. , Mazzà, C. , & McNeill, A. ((2018) ). A systematicreview of the gait characteristics associated with CerebellarAtaxia. Gait and Posture, 60: , 154–163. |
7 | Calley, A. , Williams, S. , Reid, S. , Blair, E. , Valentine, J. , Girdler, S. , & Elliott, C. ((2012) ). A comparison of activity, participation and quality of life in children with and without spastic diplegia cerebral palsy. Disability and Rehabilitation, 34: , (15), 1306–1310. |
8 | Chanda, M.L. , & Levitin, D.J. ((2013) ). The neurochemistry of music. Trends in Cognitive Sciences, 17: , (4), 179–193. |
9 | Damiano, D.L. , & DeJong, S.L. ((2009) ). A systematic review of the effectiveness of treadmill training and body weight support in pediatric rehabilitation. Journal of Neurologic Physical 896 Therapy: JNPT, 33: , (1), 27. |
10 | Damiano, D.L. , Kelly, L.E. , & Vaughn, C.L. ((1995) ). Effects of quadriceps femoris muscle strengthening on crouch gait in children with spastic diplegia. Physical Therapy, 75: , (8), 658–667. |
11 | Deitz, J.C. , Kartin, D. , & Kopp, K. ((2007) ). Review of the Bruininks-Oseretsky test of motor proficiency, (BOT-2). Physical and Occupational Therapy in Pediatrics, 27: , (4), 87–102. |
12 | Delecluse, C. , Roelants, M. , & Verschueren, S. ((2003) ). Strength increase after whole-body vibration compared with resistance training. Medicine and Science in Sports and Exercise, 35: , (6), 1033–1041. |
13 | Desai, A.D. , Zhou, C. , Stanford, S. , Haaland, W. , Varni, J.W. , & Mangione-Smith, R.M. ((2014) ). Validity and responsiveness of the pediatric quality of life inventory (PedsQL). generic core scales in the pediatric inpatient setting. JAMA pediatrics, 168: , (12), 1114–1121. |
14 | Eagleton, M. , Iams, A. , McDowell, J. , Morrison, R. , & Evans, C.L. ((2004) ). The effects of strength training on gait in adolescents with cerebral palsy. Pediatric Physical Ttherapy, 16: , (1), 22–30. |
15 | Effgen, S.K. , & McEwen, I.R. ((2008) ). Review of selected physical therapy interventions for school age children with disabilities. Physical Therapy Reviews, 13: , (5), 297–312. |
16 | El-Shamy, S.M. , & Abd El Kafy, E.M. ((2014) ). Effect of balance training on postural balance control and risk of fall in children with diplegic cerebral palsy. Disability and Rehabilitation, 36: , (14), 1176–1183. |
17 | Elshafey, M.A. ((2014) ). Hippotherapy simulator as alternative method for hippotherapy treatment in hemiplegic children. International Journal of Physiotherapy and Research, 2: , (2), 435–441. |
18 | Fazio, P. , Granieri, G. , Casetta, I. , Cesnik, E. , Mazzacane, S. , Caliandro, P. , Pedrielli, F. , & Granieri, E. ((2013) ). Gait measures with a triaxial accelerometer among patients with neurological impairment. Neurological Sciences, 34: , (4), 435–440. |
19 | Franjoine, M.R. , Gunther, J.S. , & Taylor, M.J. ((2003) ). Pediatric balance scale: a modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatric Physical Therapy, 15: , (2), 114–128. |
20 | Gündüz, A.G. , YAZICI, G. , Özkul, Ç. , Küçük, H. , Çablayan, Ca. , & Nazliel, B. ((2019) ). The effects of early neurodevelopmental Bobath approachand mobilization on quadriceps muscle thickness in stroke patients. Turkish Journal of Medical Sciences, 49: , (1), 318–326. |
21 | Hartwig, M.S. , & Landis, B.J. ((1999) ). The Arkansas AHEC model ofcommunity-oriented primary care. Holistic Nursing Practice, 13: , (4), 28–37. https://doi.org/10.1097/00004650-199907000-00006 |
22 | Hebert, E.P. , & Landin, D. ((1994) ). Effects of a learning model and augmented feedback on tennis skill acquisition. Quarterly for Exercise and Sport, 65: , (3), 250–257. |
23 | Her, J.G. , Woo, J.H. , & Ko, J. ((2012) ). Reliability of the pediatric balance scale in the assessment of the children with cerebral palsy. Journal of Physical Therapy Science, 24: , (4), 301–305. |
24 | Himmelmann, K. , & Uvebrant, P. ((2011) ). Function and neuroimaging incerebral palsy: a population-based study. Developmental Medicine and Child Neurology, 53: , (6), 516–521. |
25 | Jin, L.H. , Yang, S.S. , Choi, J.Y. , & Sohn, M.K. ((2020) ). The effect of robot-assisted gait training on locomotor function and functional capability for daily activities in children with cerebral palsy: a single-blinded, randomized cross-over trial. Brain Sciences, 10: , (11), 801. |
26 | Katalinic, O.M. , Harvey, L.A. , Herbert, R.D. , Moseley, A.M. , Lannin, N.A. , & Schurr, K. ((2010) ). Stretch for the treatment and prevention of contractures. Cochrane Database of Systematic Reviews(9). |
27 | Kavlak, E. , Ünal, A. , Tekin, F. , & Altub F. ((2018) ). Effectiveness of Bobath therapy on balance in cerebralpalsy. Cukurova Medical Journal, 43: , (4), 975–981. |
28 | Kempen, G. I. , Yardley, L. , Van Haastregt, J. C. , Zijlstra, G. R. , Beyer, N. , Hauer, K. , & Todd, C. ((2008) ). The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age and Ageing, 37: , (1), 45–50. |
29 | Kenyon, L.K. ((2014) ). Gross otor function measure (GMFM- and GMFM-) users’ manual. Physical and Occupational Therapy in Pediatrics, 34: , (3), 341–342. |
30 | Kidd, D. , Stewart, G. , Baldry, J. , Johnson, J. , Rossiter, D. , Petruckevitch, A. , & Thompson, A. ((1995) ). The Functional Independence Measure: a comparative validity and reliability study. Disability and Rehabilitation, 17: , (1), 10–14. |
31 | Kim, M.R. , Lee, B.H. , & Park, D.S. ((2016) ). Effects of combined Adeli suit and neurodevelopmental treatment in children with spastic cerebral palsy with gross motor function classification system levels I and II. Hong Kong Physiotherapy Journal, 34: , 10–18. |
32 | King, L.K. , Almeida, Q.J. , & Ahonen, H. ((2009) ). Short-term effects of vibration therapy on motor impairments in Parkinson’s disease. NeuroRehabilitation, 25: , (4), 297–306. |
33 | Ko, E.J. , Sung, I.Y. , Moon, H.J. , Yuk, J.S. , Kim, H.S. , & Lee, N.H. ((2020) ). Effect of group-task-oriented training on gross and fine motor function, and activities of daily living in children with spastic cerebral palsy. Physical and Occupational Therapy in Pediatrics, 40: , (1), 18–30. |
34 | Lin, K.Y. , Hu, Y.T. , Chang, K.J. , Lin, H.F. , & Tsauo, J.Y. (2011). Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2011. |
35 | Linacre, J.M. , Heinemann, A.W. , Wright, B.D. , Granger, C.V. , & Hamilton, B.B. ((1994) ). The structure and stability of the Functional Independence Measure. Archives of physical medicine and rehabilitation, 75: , (2), 127–132. |
36 | Mayston, M.J. ((2001) ). People with cerebral palsy: effects of and perspectives for therapy. Neural Plasticity,, 8: , (1-2), 51–69. |
37 | McColl, M.A. , Paterson, M. , Davies, D. , Doubt, L. , & Law, M. ((2000) ). Validity and community utility of the Canadian Occupational Performance Measure. Canadian Journal of Occupational Therapy, 67: , (1), 22–30. |
38 | Michielsen, M. , Vaughan-Graham, J.A. , Holland, A. , Magri, A. , & Suzuki, M. ((2019) ). The Bobath concept-a model to illustrate clinical practice: responding to comments on Michielsen et al. Disability and Rehabilitation, 41: , (17), 2109–2110. |
39 | Naito, E. , & Ehrsson, H.H. ((2001) ). Kinesthetic illusion of wrist movement activates motor-related areas. Neuroreport, 12: , (17), 3805–3809. |
40 | Novak, I. , Cusick, A. , & Lannin, N. ((2009) ). Occupational therapy home programs for cerebral palsy: double-blind, randomized, controlled trial. Pediatrics, 124: , (4), e606–e614. |
41 | Novakovic, N. , Milovancevic, M.P. , Dejanovic, S.D. , & Aleksic, B. ((2019) ). Effects of Snoezelen—Multisensory environment on CARS scale in adolescents and adults with autism spectrum disorder. Research in Developmental Disabilities, 89: , 51–58. |
42 | O’Brien, J. , Tsermentseli, S. , Cummins, O. , Happä F. , Heaton, P. , & Spencer, J. ((2009) ). Discriminating children with autism from children with learning difficulties with an adaptation of the Short Sensory Profile. Early Child Development and Care, 179: , (4), 383–394. |
43 | Oskoui, M. , Coutinho, F. , Dykeman, J. , Jettä N. , & Pringsheim, T. ((2013) ). An update on the prevalence of cerebralpalsy: a systematic review and meta-analysis. Developmental Medicine and Child Neurology, 55: , (6), 509–519. |
44 | Østensjø, S. , Carlberg, E.B. , & Vøllestad, N.K. ((2003) ). Everyday functioning in young children with cerebral palsy: functional skills, caregiver assistance, and modifications of the environment. Developmental Medicine and Child Neurology, 45: , (9), 603–612. |
45 | Papavasiliou, A.S. , Nikaina, I. , Rizou, J. , & Alexandrou, S. ((2011) ). The effect of a psycho-educational program on CARS scores and short sensory profile in autistic children. European Journal of Paediatric Neurology, 15: , (4), 338–344. |
46 | Parham, L.D. , Cohn, E.S. , Spitzer, S. , Koomar, J.A. , Miller, L.J. , Burke, J.P. , Brett-Green, B. , Mailloux, Z. , May-Benson, T.A. , & Roley, S.S. ((2007) ). Fidelity in sensory integration intervention research. American Journal of Occupational Therapy, 61: , (2), 216–227. |
47 | Park, C.H. , Oh-Park, M. , Dohle, C. , Bialek, A. , Friel, K. , Edwards, D. , Krebs, H.I. , & You, J.S.H. ((2020) ). Effects of innovative hip-knee-ankle interlimb coordinated robot training on ambulation, cardiopulmonary function, depression, and fall confidence in acute hemiplegia. NeuroRehabilitation, 46: , (4), 577–587. |
48 | Park, J.H. , & You, J.S.H. ((2018) ). Innovative robotic hippotherapy improves postural muscle size and postural stability during the quiet stance and gait initiation in a child with cerebral palsy: A single case study. NeuroRehabilitation, 42: , (2), 247–253. |
49 | Park, J.H. , Shurtleff, T. , Engsberg, J. , Rafferty, S. , You, J.Y. , You, I.Y. , & You, S.H. ((2014) ). Comparison between the robo-horse and real horse movements for hippotherapy. Bio-medical Materials and Engineering, 24: , (6), 2603–2610. |
50 | Parolin S. R. , Perkins, E. M. , Miller, J. W. , Davies, W. I. , D’Adamo, M. C. , Pessia, M. , Fawcett, K. A. , Sims, D. , Gillard, E. , Hudspith, K. , Skehel, P. , Williams, J. , O’Regan, M. , Jayawant, S. , Jefferson, R. , Hughes, S. , Lustenberger, A. , Ragoussis, J. , Jackson, M. , Tucker, S. J. , & Nämeth, A. H. ((2015) ). De novopoint mutations in patients diagnosed with ataxic cerebral palsy. Brain, 138: , (Pt 7), 1817–1832. https://doi.org/10.1093/brain/awv117 |
51 | Rosenbaum, P. , Paneth, N. , Leviton, A. , Goldstein, M. , Bax, M. , Damiano, D. , Dan, B. , & Jacobsson, B. ((2007) ). A report: the definition and classification of cerebral palsy April 2006. Developmental Medicine and Child Neurolology, 109: , (suppl 109)), 8–14. |
52 | Schuhfried, O. , Mittermaier, C. , Jovanovic, T. , Pieber, K. , & Paternostro-Sluga, T. ((2005) ). Effects of whole-body vibration in patients with multiple sclerosis: a pilot study. Clinical Rehabilitation, 19: , (8), 834–842. |
53 | Sellier, E. , Platt, M. J. , Andersen, G. L. , Krägeloh-Mann, I. , De La Cruz, J. , Cans, C. , Network S. o. C. P., Van Bakel, M. , Arnaud, C. , & Delobel, M. ((2016) ). Decreasing prevalence in cerebralpalsy: a multi-site European population-based study, 1980 to 2003. Developmental Medicine and Child Neurology, 58: , (1), 85–92. |
54 | Serdaroglu, G. , Tekgul, H. , Kitis, O. , Serdaroglu, E. , & Gökben, S. ((2004) ). Correlative value of magnetic resonance imaging for neurodevelopmental outcome in periventricular leukomalacia. Developmental Medicine and Child Neurology, 46: , (11), 733–739. |
55 | Son, M.S. , Jung, D.H. , You, J.S.H. , Yi, C.H. , Jeon, H.S. , & Cha, Y.J. ((2017) ). Effects of dynamic neuromuscular stabilization on diaphragm movement, postural control, balance and gait performance in cerebral palsy. NeuroRehabilitation, 41: , (4), 739–746. |
56 | Song, C.S. ((2014) ). Effects of task-oriented approach on affected arm function in children with spastic hemiplegia due to cerebral palsy. Journal of Physical Therapy Science, 26: , (6), 797–800. |
57 | Tomchek, S.D. , & Dunn, W. ((2007) ). Sensory processing in children with and without autism: a comparative study using the short sensory profile. American Journal of Occupational Therapy, 61: , (2), 190–200. |
58 | Trabacca, A. , Russo, L. , Losito, L. , Rinaldis, M. D. , Moro, G. , Cacudi, M. , & Gennaro, L. ((2012) ). The ICF-CY perspective on theneurorehabilitation of cerebral palsy: a single case study. Journal of Child Neurology, 27: , (2), 183–190. https://doi.org/10.1177/0883073811415852 |
59 | Varni, J.W. , Burwinkle, T.M. , Seid, M. , & Skarr, D. ((2003) ). The PedsQL™*. as a pediatric population health measure: feasibility, reliability, and validity. Ambulatory pediatrics, 3: , (6), 329–341. |
60 | Varni, J. W. , Seid, M. , & Rode, C. A. (1999). The PedsQL™: measurement model for the pediatric quality of life inventory. Medical Care, 126-139. |
61 | Vaughn, S. , Schumm, J. S. , & Sinagub, J. M. ((1996) ). Focus group interviews in education and psychology. Sage. |
62 | Walker, L. O. , & Avant, K. C. ((2005) ). Strategies for theory construction in nursing (Vol. 4). Pearson/Prentice Hall Upper Saddle River, NJ. |
63 | Wei, S. , Su-Juan, W. , Yuan-Gui, L. , Hong, Y. , Xiu-Juan, X. , & Xiao-Mei, S. ((2006) ). Reliability and validity of the GMFM- in -to -year-old children with cerebral palsy. Journal of Physical Medicine and Rehabilitation, 85: , (2), 141–147. |
64 | Wuang, Y.P. , & Su, C,Y. ((2009) ). Reliability and responsiveness of the Bruininks–Oseretsky Test of Motor Proficiency-in children with intellectual disability. Research in Developmental Disabilities, 30: , (5), 847–855. |




