Physical performance outcome measures used in exercise interventions for adults with childhood-onset disabilities: A scoping review
Abstract
BACKGROUND:
People with childhood-onset disabilities face unique physical and social challenges in adulthood. Exercise interventions may improve physical performance in children, but there is a lack of research on adults.
OBJECTIVE:
To describe studies that investigate exercise interventions and to evaluate the quality of physical performance outcome measures for adults with childhood-onset disabilities.
METHODS:
Eligible studies reported on exercise interventions for adults (ages 16+) with cerebral palsy, spina bifida, or acquired brain injuries. Only randomized controlled trials published in English from 2008 to 2019 were included. MEDLINE, CINAHL, PEDro, EMBASE, and Cochrane Central Register of Controlled Trials were searched. Two reviewers independently screened studies and abstracted data.
RESULTS:
This scoping review included 4 trials reporting on cerebral palsy only. Three strength training programs found significant improvements in gait, and one mixed training program found significant improvements in strength and fitness. Only two outcome measures used are valid/reliable for adults (6 Minute Walk Test and Borg-20 Grades).
CONCLUSION:
Certain interventions may improve physical performance, but there is a lack of research on appropriate exercise interventions and physical performance outcome measures for adults with childhood-onset disabilities. Different exercise interventions should be investigated using larger sample sizes and outcome measures should be standardized.
1Introduction
Previously, most children living with chronic disabling neurological conditions including cerebral palsy (CP), spina bifida (SB), and acquired brain injuries (ABI) were not expected to survive past childhood. However, medical innovations have led to significant improvements in survival rates over the past several decades; more than 90% of those with childhood-onset disabilities such as SB are now expected to live past the age of 20, with over 500,000 individuals reaching adulthood (age 18) each year based on estimates from the United States (Hunt & Sharma, 2013). Sixty percent of individuals with SB are now expected to survive well into their 20s, which is a 20–30% improvement from rates seen just 40 years ago (Betz et al., 2018; Timberlake et al., 2015). Across the globe, over 17 million people live with CP, and 1 in 1000 babies are born with SB each year (Foster, 2019; “Key Facts”, n.d.). Additionally, over 1.5 million Canadians currently live with ABIs, with hundreds of thousands of new cases arising each year (“About Acquired Brain Injury”, n.d.). Individuals with childhood-onset disabilities experience significant health-related problems such as chronic pain and fatigue, as well as severe deterioration in physical function as they age compared to able-bodied peers (Roebroeck et al., 2009).
For those with childhood-onset disabilities, achieving a good quality of life is often hindered by issues arising from lack of mobility. Most of these individuals are less physically active due to unique personal, institutional, social, and/or environmental barriers. These barriers include, but are not limited to, lack of motivation to engage in physical activity, poor gross motor function of the individual, lack of staff knowledge about appropriate physical activity programs, and inaccessible built environments (e.g., lack of wheelchair accessible areas) (Acharya, Meza, & Msall, 2017). Furthermore, studies have reported significant age-related declines in physical activity for adolescents with conditions such as CP (Imms & Adair, 2016). The inactive lifestyles of individuals with disabilities can lead to a cycle of deconditioning that often results in further reduction in physical activity and physical deterioration (Hombergen et al., 2012). For example, many adults with CP experience decreased physical activity and participation in fitness programs, which are coupled with loss of strength and development of musculoskeletal pain (Blackman & Conaway, 2013). These physical health issues ultimately lead to difficulties in daily performance, self-care, and mobility (Blackman & Conaway, 2013).
Due to the added challenges of maintaining adequate physical activity levels, adults with childhood-onset conditions have a greater risk of developing preventable age- or lifestyle-related secondary health issues and complications such as obesity, cardiovascular disease, hypertension, pain, deformities, and bladder/bowel problems (LaPlante, 2015; Roebroeck et al., 2009). Subsequently, individuals with chronic health issues have an increased need for healthcare services over time. Population data from the Ontario Health Insurance Plan and Canadian Institute for Health Information databases show that adults with CP, SB, and ABI were admitted to the hospital, on average, once every 6.8 years and visited physicians 11.5 times per year or about 5–10 times more frequently than peers. Annual admission rates to healthcare services for adults with childhood-onset disabilities were nine times that of the general population (Young et al., 2009). A recent retrospective cohort study revealed that hospital readmission rates in the U.S. are rising in adults with childhood-onset disabilities, most likely due to age- and condition-related comorbidities (Goodman et al., 2011).
In addition to hospitalizations comorbidities-related, adults with childhood-onset conditions are often hospitalized due to fall-related injuries that can occur up to several times a week (Morgan, Mcdonald, & Mcginley, 2015). The high frequency of falls can incite feelings of embarrassment, powerlessness, and fear (Morgan, Mcdonald, & Mcginley, 2015). Furthermore, falls may cause dislocations, fractures, and other severe health complications requiring extensive treatment and further impeding an individual’s ability to undertake daily tasks (Morgan, Mcdonald, & Mcginley, 2015). Mental health issues are also prevalent in adolescents with chronic physical health conditions (Erickson et al., 2005). Significantly higher instances of substance abuse, suicidal thoughts, low self-esteem, and depression (compared to healthy peers) have also been reported (Erickson et al., 2005). Since advancements in care have dramatically extended the life expectancy of adolescents and young adults with childhood-onset disabilities, it has become increasingly imperative to investigate and reinforce appropriate interventions to improve quality of life both socially and physically as adolescents with disabilities transition into adulthood (Roebroeck et al., 2009).
Exercise is one type of intervention that is com-monly prescribed to children, adolescents, and adults with childhood-onset conditions. Examples of such interventions include combined progressive resistance and anaerobic training sessions, progressive weight machine training sessions, and upper extremity strength-training programs, administered at varying intensities for varying durations (Bania et al., 2015; Gillett et al., 2018; Hutzler et al., 2013). Studies have reported that these types of exercise training programs have the potential to increase hand, wrist, and leg strength and functional capacity, allowing for greater independence and quality of life throughout the lifespan, while decreasing the risk of developing health complications resulting from inactivity (de Groot et al., 2015; Gillett et al., 2018; Hutzler et al., 2013). Some exercise interventions may also increase daily physical activity levels, in turn providing a variety of emotional, cognitive, and social benefits (Acharya, Meza, & Msall, 2017). A recent review by Ryan et al. (2017) explored the effects of aerobic training (i.e., walking, running, cycling, arm ergometry), resistance training (i.e., muscles working against free weights, body weight, machine weights, elastic bands), and mixed training (i.e., a mix of aerobic, anaerobic, and resistance training) interventions on children, adolescents, and adults with CP in terms of physical activity, social participation, and quality of life. This systematic review included 29 trials with 926 total participants. The review found that while aerobic exercise may improve short-term motor function activity, it may not improve gait speed, walking endurance, or aerobic fitness of children with CP. Meanwhile, resistance training may improve short-term muscle strength, but may not improve gait speed, participation, or motor function in children, adolescents, and young adults with CP. Furthermore, mixed training may improve participation of children and adolescents with CP in the short term, but it may not improve their motor function or gait speed. These conclusions were described as tentative as there was low-quality evidence to support them due to the small sample sizes (i.e. range of 12 to 102 participants per trial, n < 50 for 24 of the 29 trials) of the studies in question.
The review by Ryan and colleagues (2017) summarized exercise interventions for children and adolescents with CP, as well as physical activity outcome measures that assess two domains: activity and changes in body structure/functions. Ryan et al. also identified several gaps in research, one being that there exist very few trials involving adults with CP. There is also a lack of literature assessing outcome measures in terms of their reliability and validity, which is crucial to appropriately monitor intervention effects. Only four out of the 29 (14%) trials included in the review by Ryan et al. (2017) included adolescents/young adults (ages 10 to 22) or adults over the age of 20.
For those with childhood-onset disabilities, the transition into adulthood is accompanied by additional deterioration in physical function and health due to reduced respiratory fitness, pain, fatigue, and secondary age-related disabilities (Jahnsen et al., 2004; Opheim et al., 2009; Sandström, Alinder, & Oberg, 2004). The outcome measures and exercise interventions prescribed to adults must be tailored to their specific needs and physical changes as they age past adolescence. Since the samples in the review by Ryan et al. (2017) consisted primarily of children, we cannot extrapolate the findings from this review to young or older adults with childhood-onset disabilities.
The current scoping review aims to identify val-idated physical performance outcome measures used in exercise intervention studies targeting adults with childhood-onset disabilities including CP, SB, and ABI. This review will: (1) describe exercise interventions used for adults with childhood-onset disabilities, and (2) identify gaps in the quality (in terms of reliability and validity) of physical performance outcome measures being used to assess the efficacy of these exercise interventions.
2Methods
We applied Arksey and O’Malley’s (2005) metho-dological framework for the current review, which includes the following five stages: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing, and reporting the results. The Joanna Briggs Institute guidance for scoping reviews was referenced as well (Peters et al., 2017). This review was written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist (Tricco et al., 2018). No protocol has been published for this review.
2.1Eligibility criteria
Studies were included in this review if they met the following criteria: (1) published between January 2008 and July 2019 to ensure the inclusion of interventions and outcome measures that are consistent with the current healthcare system; (2) randomized controlled trials (RCTs), as they are the gold standard for effectiveness research; (3) written in English; (4) sampled adults (16 years to 65 years to account for studies with populations starting at 16 years old) with childhood-onset disabilities; and (5) included at least one outcome measure of physical performance (categorized into five domains: fitness, functional mobility, strength, balance, and gait as per McGough et al.’s (2019) review).
2.2Search strategy and information sources
A comprehensive literature search was conducted by an experienced librarian (LP) with input from the investigators. Search terms were derived from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the Merck Manual, and the ICD-11 (American Psychiatric Association, 2013; Porter et al., 2018; World Health Organization, 2019). The strategies were peer-reviewed by another information specialist prior to execution using the PRESS Checklist (McGowan et al., 2016). A comprehensive literature search was initially run on June 1, 2018 and rerun on July 5, 2019. The following literature databases were searched: MEDLINE (OVID), MEDLINE In-Process & Other Non-Indexed Citations (OVID), MEDLINE Epub Ahead of Print (OVID), EMBASE (OVID), CINAHL (EBSCOhost), PEDro (www.pedro.org.au), and the Cochrane Central Register of Controlled Trials (Wiley). A validated search filter was added to the MEDLINE, EMBASE, and CINAHL databases searches for identifying randomized trials that was developed by the Health Information Research Unit at McMaster University (Health Information Research Unit 2019). Duplicates were removed by using EndNote’s duplicate identification feature and by reviewing records manually.
MEDLINE, EMBASE, PEDro (Physiotherapy Evidence Database), CINAHL, and Cochrane Central Register of Controlled Trials were searched originally on June 1, 2018 and retrieved 1,259, 2,937, 78, 391, and 2,193 studies, respectively. Searches were limited to the last 10 years (i.e., 2008–2018) and the English language. Appropriate wildcards were used in the searching to account for plurals and variations in spelling.
An update of the search was performed on July 5, 2019 by an experienced librarian (LP). MEDLINE, EMBASE, PEDro (Physiotherapy Evidence Database), CINAHL, and Cochrane Central Register of Controlled Trials were searched and retrieved 194, 654, 10, 0, and 710 studies, respectively. The identical search strategy with the same search terms was used from the original search. Searches were limited to articles published between June 2, 2018 and July 5, 2019 and to English language articles. Appropriate wildcards were again used in the searching to account for plurals and variations in spelling.
2.3Selection of articles and data abstraction
Two independent reviewers (initials removed for blinding purposes) performed level 1 screening of article titles and abstracts from the initial results. Reviewers then met to discuss and reach consensus on any disagreements regarding eligibility criteria. Following this, full-text articles were obtained and screened by two independent reviewers. Disagreements about the inclusion or exclusion of articles for level 2 screening were also resolved via discussion. No third reviewer was required. Abstraction was completed on the remaining articles by two independent reviewers. Following the independent abstraction, results were compared and consolidated after resolution of any issues. The following data were abstracted from the included studies: country of study, year of publication, study design, study setting, study objective, participant sample, key characteristics of the study intervention (see Table 1), outcome measures used (including psychometric characteristics; see Table 2), and results.
Table 1
Study characteristics
| Author | Study Design | Conditions of Participants | Country | Intervention and Outcome Testing Setting | N | Age range (years) | Duration | Frequency | Intervention Description | Goal of the Intervention | Measurement Time Points | Results |
| Maeland et al., 2009 | Single-blind randomized controlled trial | Spastic diplegic CP, GMFCS II or III | Norway | Community physiotherapy clinics (intervention and outcome testing) | 12 | 27–69 | 8 weeks | 3x/week | Intervention Group: The high-intensity PRE program consisted of a 10-minute low intensity warm-up on a bike or treadmill followed by seated leg press (SLP) 2–14RM in 4 sets for 2 weeks. A progression to 4–6RM in 4 sets was achieved in the next 6 weeks. When these were done, resistance was increased by 5–10 kg. Participants were asked not to start new treatments or activities during the 8 weeks. | To observe changes in walking and functional lower limb strength in adults with spastic diplegic CP. | Baseline and post intervention | No significant differences between groups or within the intervention and control groups for any measures.Walking ability and functional lower limb strength/isokinetic quadricep muscle strength did not improve significantly. |
| Control Group: Participants were not offered any type of exercise regime during the 8 weeks. Participants were asked not to start new treatments or activities during the 8 weeks. | ||||||||||||
| Bania et al., 2015 | Single-blind randomized controlled trial | Bilateral spastic CP, GMFCS II or III | Australia | Community gymnasiums (intervention and outcome testing) | 49 | 14–22 | 12 weeks | 2x/week | Intervention Group: The PRT program consisted of 2–3 sets of 10–12 repetitions of each given exercise specifically prescribed to each person based on gait analysis (e.g., leg press, calf raise, hip abduction/extension, reverse leg press). The load was the weight participants could lift for 10–12 repetitions before experiencing muscle fatigue. Amount of weight lifted was increased whenever participants completed 3 sets of 12 repetitions of an exercise without muscle fatigue. | To observe changes in daily physical activity levels and muscle strength of adolescents and young adults with CP with walking difficulties. | Baseline, post intervention, and follow-up 12 weeks after intervention | No significant differences between groups from baseline to post intervention or follow-up for any of the measures, but there was a greater observed increase in 1RM leg press strength within the intervention group vs. control (20% larger in intervention group).Lower limb muscle strength might be increased by the PRT, but it did not increase daily physical activity. |
| Control Group: Participants continued their usual care (recreation and physiotherapy) that did not include progressive resistance training. | ||||||||||||
| Taylor et al., 2013 | Single-blind randomized controlled trial | Spastic diplegic CP, GMFCS II or III | Australia | Community gymnasium (intervention testing), hospital gait laboratory (outcome testing) | 48 | 14–22 | 12 weeks | 2x/week | Intervention Group: The PRT program consisted of three sets of 10–12 repetitions of each individualized exercise (e.g., leg press, hip extensors/abductors) with a 2-minute break between sets (participants lifted enough weight to have muscle fatigue after each set). When sets were complete, the weight to be lifted was increased. Exercises were individualized and targeted deficits in gait and strength. After 12 weeks, participants were asked not to train but to resume with usual activities until testing at 24 weeks.Control Group: Participants continued with usual care (recreation and physiotherapy) that did not include progressive resistance training. | To observe changes in mobility-related function of adolescents and young adults with CP with walking difficulties. | Baseline, post intervention, and follow-up 12 weeks after intervention. | No significant differences between or within groups in gait kinematics (GPS), gross motor function (GMFM-D, GMFM-E), or walking distance (6MWT) post intervention or at follow-up.Intervention group had significant improvements in participant-rated measures of mobility including the FMS at 5 metres (p = 0.04) as well as the FAQ (p = 0.02) post intervention. Intervention group also showed improvement in the FMS scale at 5 metres (p = 0.04) compared to the control group at follow up.Muscle strength in the intervention group increased by 27% and strength of leg press increased by 17% compared to the control group post intervention.Leg muscle strength did improve. Objective measures of mobility did not improve from this PRT program, but the intervention may provide psychological benefits that assist mobility (e.g. improved confidence in mobility). |
| Gillett et al., 2018 | Waitlist randomized controlled trial | Spastic CP, GMFCS I or II | Australia | Fully equipped tertiary institution gymnasium (intervention and outcome testing) | 17 | 15–28 | 12 weeks | 3x/week | Intervention Group: The program consisted of a PRT component and a functional anaerobic training component. The PRT consisted of five lower limb resistance exercise stations (e.g., leg press, seated bent knee calf raise, standing calf raise). It included multiple sets of 6 to 12 repetitions, which progressed every 4 weeks. Training load was adjusted during sessions based on the participants’ abilities. The functional anaerobic training consisted of 2–3 functional anaerobic exercises (e.g., activities related to stair climbing, bending, changing direction, stepping over obstacles) completed at maximal intensity. The number of exercises per session, repetitions performed, and work-to-rest ratio progressed every 4 weeks. | To observe changes in lower limb neuromuscular properties and functional capacity in young adults with spastic-type CP. | Baseline and within 3 days post- intervention. | Walking ability (distance as measured by the 6MWT) was higher in the intervention group compared with the control group post-test (6.1% improvement in training group; p = 0.006). Functional strength (30-Repetition Maximum), agility (10×5-m Sprint Test), and anaerobic capacity (MPST peak power) all improved in the intervention group as well (50.2%, 13.4%, and 8.3%, respectively).Muscle volumes, strength, and functional capacity increased from this combined exercise program. |
| Control Group: Participants did not receive resistance or anaerobic training and continued with daily activities. |
Table 2
Outcome characteristics1
| Validated Physical Fitness Outcome Measures | Studies That Used the Measure (Author) | Purpose of Measure | Administration of Measure | Validity and/or Reliability |
| Fitness | ||||
| 6 Minute Walk Test (6MWT) | Gillett et al., 2018; Taylor et al., 2013; Maeland et al., 2009 | Evaluates an individual’s submaximal aerobic capacity and endurance (Andersson et al., 2003). | Measures the maximum distance a participant can walk over the course of six minutes (“6 Minute Walk Test”, n.d.). | Excellent reliability and responsiveness in adults with CP, with ICC values between 0.94–0.99 (Andersson et al., 2006). |
| Borg-20 Grades | Maeland et al., 2009 | Monitors and guides exercise intensity using subjective levels of exertion during exercises (Borg, 1970). | Measures total perceived exertion right after completing the 6MWT (Borg, 1970). | Moderate criterion validity in healthy adults and content validity (τ= 0.70) in adolescents and adults with SB (Borg, 1970; Chen, Fan, &Moe, 2002; Crytzer et al., 2015). |
| Muscle Power Sprint Test (MPST) | Gillett et al., 2018 | Evaluates anaerobic muscle power in children with CP (Verschuren et al., 2007). | Participants sprint a specific distance six times at maximum speed, and the highest and average power scores are assigned as measures of peak and mean power, respectively (Verschuren et al., 2007). | Excellent inter and intra-rater reliability (ICC > 0.97) and test-retest reliability (ICC > 0.97) for both peak and mean power in children with CP and SB (Bloemen et al., 2017; Verschuren et al., 2007; Verschuren et al., 2013b). Excellent criterion validity for peak and mean power scores when compared with WAnT (r > 0.70) for children with CP (GMFCS I-II and III-IV) (Verschuren et al., 2013a; Verschuren et al., 2013b). Excellent discriminant validity (significant differences in peak and mean power scores (p = 0.007 and 0.006) between children on GMFCS levels I and II in children with CP (Verschuren et al., 2007). Excellent criterion validity when compared with WAnT (r > 0.70) and excellent convergent validity between MPST and 10×5MST (r = –0.70), between slalom test and MPST (r = –0.67), and between One Stroke Push Test and MPST (r = 0.56) in children and adolescents with SB (Bloemen et al., 2017). |
| 10×5-m Sprint Test | Gillett et al., 2018 | Evaluates an individual’s ability to complete difficult tasks that require agility and coordination (Verschuren et al., 2007). | Measures the amount of time it takes for the participant to perform ten 5-meter sprints around two sets of cones (Verschuren et al., 2007). | Excellent test-retest reliability (ICC = 0.97), interrater reliability (ICC = 1.00), and construct validity (significant difference was found for children on GMFCS levels I and II, p = 0.002) in children and adolescents with CP (Verschuren et al., 2007). |
| Functional Mobility | ||||
| Gross Motor Function Measure (GMFM) | Taylor et al., 2013; Maeland et al., 2009 | Identifies changes in gross motor function with an intervention or over time in children with CP (“Gross Motor Function Measure (GMFM)”, n.d., para. 1). | Measures either 66 or 88 items in five dimensions of gross motor activities: A (lying and rolling), B (sitting), C (crawling and kneeling), D (standing), and E (walking, running, and jumping) (“Gross Motor Function Measure (GMFM)”, n.d., para. 2)Note: Taylor et al.’s study used an abbreviated 66-item version which included dimensions D and E. Maeland et al.’s study only evaluated stair climbing, based on items 84 and 87 of the 88-item version. | Excellent inter- and intra-rater reliability (ICC = 0.99), test-retest reliability (ICC = 0.99) (Brunton &Bartlett, 2011). Excellent concurrent validity (comparing two abbreviated versions of the GMFM-66 –ICC = 0.99) and construct validity (significant relationships were observed between gait speed and dimensions D and E of GMFM-88 –r > 90) for children with CP (Brunton &Bartlett, 2011; Russell et al., 2000). |
| Timed Up and Down Stairs Test (TUDS) | Gillett et al., 2018 | Evaluates improvements in musculoskeletal and neuromuscular systems of individuals that lead to greater functional mobility (Zaino, Marchese, &Westcott, 2004). | Measures the amount of time taken to ascend then descend a set of stairs (five steps in Gillett’s study) when done as quickly as possible without running (Zaino, Marchese, &Westcott, 2004). | This measure has shown excellent inter-rater, intra-rater, and test-retest reliability (ICC > 0.93 for all) in children with CP (Zaino, Marchese, &Westcott, 2004). It has moderate concurrent validity when compared with other tests of balance and functional mobility (rs = 0.68 between TUDS and TUG) for children with CP (Zaino, Marchese, &Westcott, 2004). It has moderate construct validity (rs = –0.61 and –0.41 for typically developing children and children with CP, respectively) when assessing the relationship between TUDS and age (Zaino, Marchese, &Westcott, 2004). |
| Strength Measures | ||||
| Timed Stands Test (TST) | Maeland et al., 2009; Taylor et al., 2013 | Evaluates general muscle strength impairment in the lower extremities (Csuka &McCarty, 1985). | Measures the time it takes for an individual to complete ten full stands from a sitting position, in a standardized chair without armrests. | This measure has demonstrated test-retest reliability (r = 0.882) when tested in adults with rheumatoid arthritis, and healthy adults (Csuka &McCarty, 1985; Newcomer, Krug, &Mahowald, 1993). |
| One Repetition Maximum (1RM) | Bania et al., 2015; Taylor et al., 2013 | Evaluates muscle strength (gold standard) (Seo et al., 2012). | Measures the maximum amount of weight that an individual can lift one time with the correct technique and can involve several different exercises (Seo et al., 2012). | Excellent test-retest reliability (ICC > 0.91 for all exercise types) and excellent concurrent validity (as indicated by high correlations between the plate-loaded and the chain-loaded free-weight bench press exercises), r = 0.99 for healthy adults (McCurdy et al., 2008; Seo et al., 2012). |
| 30-s Repetition Maximum Test | Gillett et al., 2018 | Evaluates functional strength of individuals with CP (Verschuren et al., 2008). | Measures the maximum number of repetitions of three exercises that a participant can complete in 30 seconds. Includes the lateral step-up, sit-to-stand, and stand from half kneel (Verschuren et al., 2008). | Excellent interrater reliability (ICC between 0.91 and 0.96 for each exercise) in children and adolescents with CP (Verschuren et al., 2008). |
| Gait Measures | ||||
| Gait Profile Score (GPS) | Taylor et al., 2013 | It evaluates the quality of walking ability in an individual (Baker et al., 2009). | Measures kinematic deviation by quantifying gait deviation from normal walking in degrees (Baker et al., 2009). | Strong criterion-related validity relative to clinician judgements when administered to children with CP, SB and ABI (rs between 0.89 to 0.97) (Beynon et al., 2010). The measure also has high test-retest reliability (ICC > 0.77) in adults with spinal cord injuries (Wedege et al., 2017). |
| Functional Mobility Scale (FMS) | Taylor et al., 2013 | Evaluates the walking performance of children with CP. | Measures the walking ability of individuals with CP at 5, 50, and 500 meters, which represents their mobility ability at home, at school, or in the community. Based on parental responses, this scale considers any assistive devices that the individual uses and documents any changes in use over time or following interventions (Harvey et al., 2007). | This measure is shown to have excellent inter and intra-rater reliability (ICC > 0.93), criterion validity, construct validity, and content validity (r = 0.51–0.89 when compared to different outcome tools) in children with CP (Graham et al., 2004; Harvey et al., 2009; Harvey et al., 2010). |
| 10-Meter Walk Test (10MWT) | Maeland et al., 2009 | It evaluates the gait of children or adults with CP, TBI, spinal cord injuries, multiple sclerosis, Parkinson’s, and stroke (Wade, 1992). | Measures walking speed in meters per second on a 10-meter indoor track (Wade, 1992). | This measure has excellent test-retest reliability in children with neuromuscular disease and adults with TBI (ICC > 0.90), and excellent inter-rater/intra-rater reliability for adults with TBI (ICC = 0.99) and stroke (ICC = 0.998) (Collen, Wade, &Bradshaw, 1990; Pirpiris et al., 2003; Tyson &Connell, 2009; Watson, 2002). It has good to excellent test-retest reliability (ICC from 0.70 to 0.90) in children with neurological gait disorders including CP (Graser, Letsch, &van Hedel, 2016). It also has excellent criterion and convergent validity for stroke patients (r and ICC > 0.60 when compared against various other tests) (Flansbjer et al., 2005; Tyson &Connell, 2009). |
| Gillette Functional Assessment Questionnaire –Walking Scale (FAQ) | Taylor et al., 2013 | Evaluates locomotor skills in children with neuromusculoskeletal conditions (Gorton et al., 2010). | Measures walking ability using a 10-level, parent or self-report walking scale (Novacheck, Stout, &Tervo, 2000). | Good test-retest reliability (ICC > 0.80), and high content and concurrent validity as assessed by FAQ’s correlation to other standardized mobility outcome measures such as POSNA Transfers and Basic Mobility Scale (r > 0.70) in children with chronic neuromuscular conditions (Novacheck, Stout, &Tervo, 2000). |
1Description of measures (purpose and administration) and assessments of reliability/validity are taken from the original sources which assessed and described these measures, not from the four studies in our review.
All outcome measures identified in the abstraction process were categorized into five domains of physical performance: fitness, functional mobility, gait, balance, and strength, all of which were derived from a review by McGough et al. (2019). Fitness measures assess cardiorespiratory and muscle endurance required for cardiopulmonary, biomechanical, and neuromuscular function (McGough et al., 2019; Rydwik, Frändin, & Akner, 2004). Functional mobility measures assess one’s ability to perform everyday physical tasks such as stair climbing (McGough et al., 2019; Rydwik, Frändin, & Akner, 2004). Gait measures assess spatial and temporal aspects of gait (e.g., speed and stride length) (McGough et al., 2019), and overall performance of gait. For the purpose of categorization, when a measure examined walking performance, we considered it a measure of gait rather than functional mobility. Balance measures assess the ability to remain upright during balance assessments (McGough et al., 2019; Rydwik, Frändin, & Akner, 2004). Strength measures assess muscle capacity for force generation in various muscles (McGough et al., 2019; Rydwik, Frändin, & Akner, 2004). Gross motor tests were included while fine motor tests were excluded because they do not directly assess performance in terms of our physical performance outcome measures (i.e., fine motor tests are not directly indicative of improvements in fitness). Variations of these five domains have also been used across various studies, including a systematic review on physical performance in elderly patients by Rydwik, Frändin, & Akner (2004), a validation study on items in the National Institutes of Health (NIH) toolbox by Reuben et al. (2013), and a position statement on exercise interventions for healthy adults by Garber et al. (2011). Critical appraisal of the four RCTs was performed according to the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
3Results
3.1Study selection
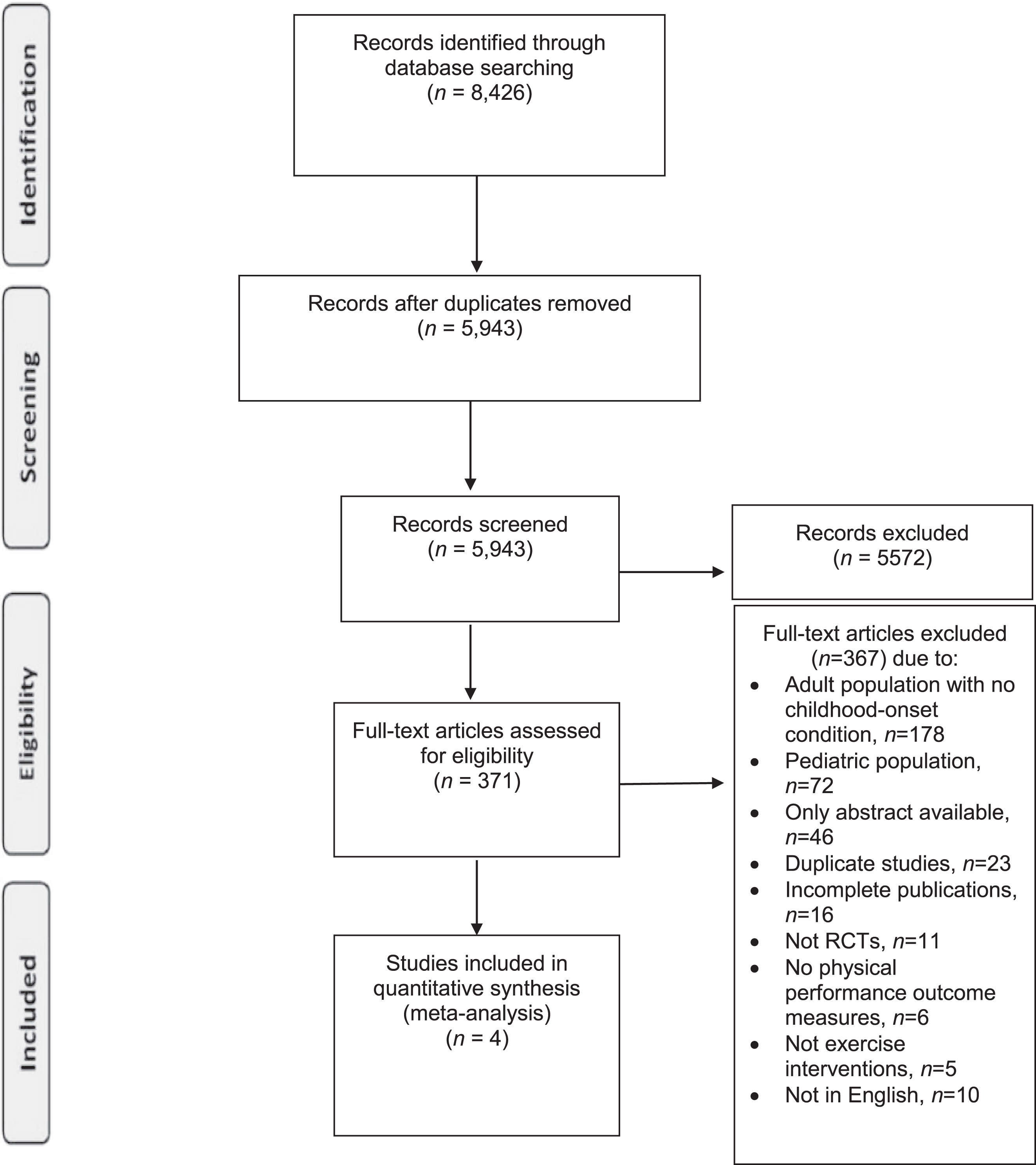
A flowchart of the results of the study selection process is displayed in Fig. 1. The initial search yielded a total of 6,858 articles; the update on the search yielded another 1,568 articles. After duplicates were removed, 5,943 articles underwent initial screening. Subsequent to the level 1 screening, 371 articles were included for full-text screening. Of these 371 articles, 367 were excluded, leaving four studies for data abstraction.
Fig. 1
Articles yielded from the literature search, title and abstract screening, full-text screening. Diagram adopted from PRISMA.
3.2Study characteristics
The study characteristics and results of the four studies included in the review can be found in Table 1. The four studies were published between 2009 and 2018. Three were conducted in Australia and one was conducted in Norway. The studies took place in community settings (n = 3) and a physiotherapy clinic (n = 1). Sample sizes ranged from 17 to 49 participants, with participants ranging in age from 14 to 69 years. All four trials only involved individuals with CP. Three trials used a progressive resistance training/exercise (PRT/PRE) intervention and one used a PRT/functional anaerobic mixed training intervention. The interventions varied in terms of duration (one was 8 weeks and three were 12 weeks), intensity (two were twice a week and two were three times a week), and intervention goal (i.e., increasing general physical activity levels, muscle strength, and functional mobility). All trials included a pre- and post-assessment, with two of the four studies also including a follow-up (12 weeks post-treatment) assessment.
3.3Critical appraisal of evidence
All four RCTs included in our review had a well-structured abstract and introduction describing CP as well as specific issues that adults with CP struggle with (i.e., muscle deterioration, lack of physical activity). Each clearly stated their objective. In the methods section, each RCT described the study design, eligibility criteria, intervention, and intervention setting in detail. Both primary and secondary outcome measures were stated clearly in all four RCTs. Only one RCT (Taylor et al., 2013) used a different outcome measure for gait than the one they had originally planned, and the study authors provided reasons for this change. All four RCTs provided a justification for how the (minimum) sample size was determined and included the method of randomization. In one RCT (Bania et al., 2015), the method of concealment was not described in detail. Statistical methods were described in all four RCTs. In the results section, each RCT provided a participant flow diagram, a baseline data table, and the results for each group. Three RCTs (Bania et al., 2015, Gillett et al., 2018, and Taylor et al., 2013) indicated the effect size (i.e., mean difference) as well as its precision (i.e., 95% confidence interval), while only one RCT (Maeland et al., 2009) included the p-values for between-group changes. No harms were reported for any of the RCTs. In the discussion sections, generalizability of the results and other interpretations of data were stated. Limitations were discussed in three RCTs (Bania et al., 2015, Gillett et al., 2018, and Taylor et al., 2013). Information regarding funding was provided in all four RCTs.
3.4Outcome measures
A total of 13 validated outcome measures were extracted and organized into four of the five domains of physical performance: fitness (four measures; 6-Minute Walk Test (6MWT), Borg-20 Grades, Muscle Power Sprint Test (MPST), 10×5 m Sprint Test), functional mobility (two measures; Timed Up and Down Stairs Test (TUDS), Gross Motor Function Measure (GMFM)), strength (three measures; Timed Stands Test (TST), One Repetition Maximum (1RM), 30-s Repetition Maximum), and gait (four measures; Gait Profile Score (GPS), Functional Mobility Scale (FMS), 10-Meter Walk Test (10MWT), Gillette Functional Assessment Questionnaire (FAQ –Walking Scale)). No outcome measures pertaining to balance were used in any of the studies. Table 2 summarizes the outcome measures and their psychometric characteristics (as cited within the included studies and/or from original sources which assessed the outcome measures specifically).
3.4.1Fitness measures
Three of the four studies used fitness outcome measures, with four different validated fitness measures found across the four studies. Gillett et al. (2018), Taylor et al. (2013), and Maeland et al. (2009) used the 6MWT. This test measures the maximum distance a participant can walk over the course of six minutes to assess an individual’s submaximal aerobic capacity and endurance (“6 Minute Walk Test”, n.d.). The 6MWT has demonstrated excellent reliability and responsiveness in adults with CP, with intraclass correlation (ICC) values between 0.94–0.99 (Andersson et al., 2006). Two of the three studies (Maeland et al., 2009; Taylor et al., 2013) did not find any significant differences with this measure between or within the intervention groups; however, Gillett et al. (2018) determined that distances reached improved by 6.1% in the intervention group, which was significantly higher compared to the control group (p = 0.006) when measured within 3 days following their 12-week intervention.
Maeland et al. (2009) also included the Borg –20 Grades Rating Scale of Perceived Exertion (Borg, 1970) as a fitness outcome measure. The Borg –20 Grades Rating Scale of Perceived Exertion measures total perceived exertion right after completing the 6MWT (Borg, 1970). It monitors and guides exercise intensity using subjective levels of exertion during exercises. This measure has moderate criterion validity when evaluating exercise intensity in healthy adults, and content validity (τ= 0.70) in adolescents and adults with SB (Borg, 1970; Chen, Fan, & Moe, 2002; Crytzer et al., 2015). In Maeland et al.’s study, no significant differences were found between the intervention and control groups on this measure of fitness.
Gillett et al. (2018) included two additional fitness tests: MPST and the 10×5-m Sprint Test. The MPST is a variation of the Wingate Anaerobic Cycling Test (WAnT) which is considered the gold standard for anaerobic muscle power testing (Verschuren et al., 2007). Instead of cycling (which may be difficult for those with CP), MPST participants must sprint a specific distance six times at maximum speed, and the highest and average power scores are assigned as measures of peak and mean power, respectively (Verschuren et al., 2007). The purpose of MPST is to evaluate anaerobic muscle power in children with CP, which reflects the child’s capacity for short-duration maximal exercise (Verschuren et al., 2007). This measure has shown consistently excellent inter- and intra-rater reliability (ICC >0.97) and test-retest reliability (ICC >0.97) for both peak and mean power, as well as excellent criterion validity and convergent/discriminant validity in children and adolescents with CP and SB (r >0.70; see Table 2) (Verschuren et al., 2007; Verschuren et al., 2013a; Verschuren et al., 2013b; Bloemen et al., 2017). Gillett et al. found that young adults in the training group showed an improvement of 8.3% in anaerobic capacity in terms of peak power, which was significant compared to the control group (p = 0.026).
The 10×5-m Sprint Test measures the amount of time it takes for the participant to perform ten 5-meter sprints around two sets of cones. This evaluates a child’s ability to complete difficult tasks that require agility and coordination (Verschuren et al., 2007). This measure has shown excellent test-retest reliability (ICC = 0.97), inter-rater reliability (ICC = 1.00), and construct validity in children and adolesents with CP (Verschuren et al., 2007). Gillett et al. found that young adults in the training group had a 13.4% improvement in agility, which was significant compared to the control group (p = 0.016).
3.4.2Functional mobility measures
Three of the four studies used functional mobility outcome measures, with two validated functional mobility measures found across the four studies. Taylor et al. (2013) and Maeland et al. (2009) used the GMFM. This measure evaluates either 66 or 88 items in five dimensions of gross motor activities: A (lying and rolling), B (sitting), C (crawling and kneeling), D (standing), and E (walking, running, and jumping) (Russell, 2002). The purpose of this tool is to identify changes in gross motor function with an intervention or over time in children with CP (“Gross Motor Function Measure (GMFM)”, n.d., para. 1). Taylor et al.’s study used an abbreviated 66-item version which included dimensions D and E. Maeland et al.’s study only evaluated stair climbing, based on items 84 and 87 of the 88-item version. Both assessments used items that have been found to be unidimensional with the Rasch analysis. This measure has demonstrated consistently excellent inter- and intra-rater reliability (ICC = 0.99), test-retest reliability (ICC = 0.99), and concurrent and construct validity (ICC = 0.99 and r > 90, respectively) for children with CP (Brunton & Bartlett, 2011; Russell et al., 2000). However, it has not been evaluated in adults with CP. Neither study using GMFM found significant differences between the control and intervention groups.
Gillett et al. (2018) included the Timed up and Down Stairs (TUDS) test. The TUDS test measures the amount of time taken to ascend then descend a set of stairs (five steps in Gillett’s study) when done as quickly as possible without running (Zaino, Marchese, & Westcott, 2004). This evaluates improvements in musculoskeletal and neuromuscular systems of children that lead to greater functional mobility. This measure has shown excellent inter-rater, intra-rater, and test-retest reliability (ICC >0.93 for all) in children with CP, as well as moderate concurrent (rs = 0.68) and construct validity (rs = –0.61 and –0.41 in children with typical development and CP, respectively) (Zaino, Marchese, & Westcott, 2004). It has not been found to be reliable or valid in adults with childhood-onset disabilities. Gillett et al. found that young adults in the training group did not have significant improvements on the TUDS test compared to the control group.
3.4.3Strength measures
Each study used at least one outcome measure of strength, with three different validated outcome measures found across the four studies. Two studies in this review, Maeland et al. (2009) and Taylor et al. (2013), included the Timed Stand Test (TST). This test measures the time it takes for an individual to complete ten full stands from a sitting position in a standardized chair without armrests. It evaluates general muscle strength impairment in the lower extremities (Csuka & McCarty, 1985). This measure has demonstrated good test-retest reliability (r = 0.882) when tested in adults with rheumatoid arthritis and healthy adults (Csuka & McCarty, 1985; Newcomer, Krug, & Mahowald, 1993). Neither study found significant improvements on the TST between or within groups at post-intervention.
Both Bania et al. (2015) and Taylor et al. (2013) used the 1 Repetitive Max (1RM) test. This test measures the maximum amount of weight that an individual can lift one time with the correct technique and can involve several different exercises (e.g., leg press, hip extension) (Seo et al., 2012). It is the gold standard for evaluating muscle strength. This measure has high test-retest reliability (ICC >0.91 for all types of test exercises) and excellent concurrent validity (r = 0.99) for healthy adults (McCurdy et al., 2008; Seo et al., 2012). It has not been validated or found to be reliable in adults with childhood-onset disabilities. Both Bania et al. and Taylor et al. used this measure to assess lower limb muscle strength using leg press and reverse leg press. Bania et al. found no significant differences between the intervention and control groups from baseline to 12 weeks (post intervention), but they did observe an increase in 1RM leg press strength in the intervention group compared to the control group at post-intervention (mean difference of 11.8 kg or 20%). Taylor et al. found that the strength of leg press had increased significantly by a mean of 14.8 kg (17% increase) in the intervention group compared to the control group immediately post-intervention, but this change was not retained at 24-week follow-up. No between group differences were found in reverse leg press strength.
Gillett et al. (2018) included the 30-s Repetition Maximum test. The 30-s Repetition Maximum measures the maximum number of repetitions of three exercises that a participant can complete in 30 seconds. It includes the lateral step-up, sit-to-stand, and stand from half kneel (Verschuren et al., 2008) and evaluates the functional strength of children with CP. This measure has excellent inter-rater reliability (ICC between 0.91 and 0.96 for each of the three exercises) in children and adolescents with CP (Verschuren et al., 2008). However, it has not been evaluated for use in adults over 18. Gillett et al. found that young adults in the training group showed an improvement of 50.2%, which was significant compared to the control group (p < 0.001).
3.4.4Gait measures
Two out of the four studies used gait outcome measures, with four different validated outcome measures found across the four studies. Only Taylor and colleagues (2013) used the Gait Profile Score (GPS). This test measures kinematic deviation by quantifying gait deviation from normal walking in degrees (Baker et al., 2009). It evaluates the quality of walking ability in individuals with gait disorders. This measure has strong criterion validity relative to clinician judgements (rs from 0.89 to 0.97) when administered to children with CP, SB and ABI (Beynon et al., 2010). The measure also has high test-retest reliability (ICC > 0.77) in adults with spinal cord injuries (Wedege et al., 2017). It has not been found to be reliable or valid in adults with childhood-onset disabilities. Taylor et al. found no significant differences on this measure between or within groups.
Taylor et al. (2013) used an additional gait outcome measure in their study: the Functional Mobility Scale (FMS). While “functional mobility” is in the title, the measure falls under gait because it is primarily an assessment of walking performance. The FMS rates the walking ability of children with CP at 5, 50, and 500 meters, which represents their mobility at home, at school, or in the community, respectively. Based on parent responses, this scale considers any assistive devices that the individual uses and documents any changes in walking ability use over time or following interventions (Harvey et al., 2007). This measure is shown to have excellent inter- and intra-rater reliability (ICC >0.93), criterion validity, construct validity, and content validity (r = 0.51–0.89 when compared to different outcome tools) in children with CP (Graham et al., 2004; Harvey et al., 2009; Harvey et al., 2010). It has not been found to be reliable or valid in adults with childhood-onset disabilities. In Taylor et al.’s study, participants in the intervention group demonstrated significant improvements at 5-metres (mean difference of 0.06 units, p = 0.04) compared to the control group post-intervention. Significant improvements were also seen on the FMS follow-up for the intervention group.
Maeland et al. (2009) included the 10-metre Walk Test (10MWT). The 10MWT measures walking speed in meters per second on a 10-meter indoor track (Wade, 1992). It evaluates the gait of children or adults with CP, traumatic brain injury (TBI), spinal cord injuries, multiple sclerosis, Parkinson’s, and stroke. This measure has excellent test-retest reliability in children with neuromuscular disease and adults with TBI (ICC >0.90), as well as excellent inter- and intra-rater reliability for adults with TBI (ICC = 0.99) and stroke (ICC = 0.998) (Collen, Wade, & Bradshaw, 1990; Watson, 2002; Pirpiris et al., 2003; Tyson & Connell, 2009). It has good to excellent test-retest reliability (ICC from 0.70 to 0.90) in children with neurological gait disorders including CP (Graser, Letsch, & van Hedel, 2016). It also has excellent criterion and convergent validity for stroke patients (r and ICC > 0.60 when compared against various other tests) (Flansbjer et al., 2005; Tyson & Connell, 2009). In Maeland et al.’s study, no significant differences were found between groups on this measure post-intervention.
Taylor et al. (2013) also used FAQ –Walking Scale. This measure evaluates walking ability in individuals using a 10-level parent or self-report walking scale (Novacheck, Stout, & Tervo, 2000). The purpose of this measure is to assess locomotor skills in children with neuromusculoskeletal conditions and evaluate independent walking ability of the individual with the use of assistive devices (Gorton et al., 2010). This measure has good test-retest reliability (ICC >0.80) and high content and concurrent validity (r > 0.70 when compared to other standardized mobility outcome measures; see Table 2) in children with chronic neuromuscular conditions including CP (Novacheck, Stout, & Tervo, 2000). In Taylor et al.’s study, 43% of the training group rated their perceived walking ability one unit higher on the scale post-intervention, and there was a mean between-group difference of 0.8 units (p = 0.02), both of which indicated significant improvements in the training group compared to the control group.
4Discussion
4.1Summary of findings
This scoping review identified exercise interventions and valid and reliable physical performance outcome measures commonly used for adults with childhood-onset disabilities. Only four RCTs met the eligibility criteria, and all four RCTs included adults with CP only. Three of the RCTs (Bania et al., 2015, Maeland et al., 2009; Taylor et al., 2013) used a PRE/PRT intervention, and one RCT (Gillett et al., 2018) used a combination of PRT and functional anaerobic training. Their combined results indicate that PRE/PRT interventions may improve gait in the short term, but it may not improve fitness, strength, or functional mobility in adults with CP. In some cases, there was some observed improvement in these domains post intervention (notably in strength), but the improvements were not significant within or between groups. Furthermore, PRT and functional anaerobic mixed training may improve fitness and strength in the short term, but it may not improve functional mobility in adults with CP. These conclusions are tentative as the data is drawn from only four RCTs, all of which had very small sample sizes (n < 50). Moreover, the RCTs only included adults in Gross Motor Function Classification System (GMFCS) levels I, II, or III, so these conclusions may not translate to adults classified as GMFCS IV or V. In terms of outcome measures, the 6MWT is valid and/or reliable for adults with CP, while Borg-20 Grades is valid and/or reliable for adults with SB. All other outcome measures used in the RCTs are validated in populations other than our target population. Overall, this review highlights a lack of high-quality research focused on exercise interventions/outcome measures for adults with childhood-onset disabilities. We identify a few valid/reliable outcome measures, but our focus is to provide specific recommendations for future research as a step to improving clinical care for adults with childhood-onset disabilities.
4.2Gaps in research
4.2.1Exercise interventions
Fitness, functional mobility, gait, balance, and strength are all important indicators of physical function in adults with childhood-onset disabilities. These five domains can deteriorate over time without regular, targeted training, but with appropriate interventions, improvements to physical function, mobility, and overall fitness are possible (Lawrence et al., 2016). However, there exists very minimal research on exercise interventions for adults with childhood-onset disabilities; this review found only four published RCTs that target this population. Because adults with childhood-onset disabilities are now living well into adulthood, it is critical to prevent deconditioning and physical deterioration with appropriate interventions. Exercise interventions and outcome measures used for children differ from those used for adults, since children undergo physical changes as they enter adulthood. Thus, we cannot extrapolate findings from RCTs of exercise interventions that use samples of children. In the future, more RCTs are needed to evaluate exercise interventions that are appropriate for adults with childhood-onset disabilities. RCT samples should include adults with chronic physical impairments as a result of SB, childhood-onset ABIs, and other childhood-onset conditions in addition to CP.
All four studies included in this review aimed to evaluate the effects of the exercise interventions on functional ability, mobility, and/or strength. The findings of these studies suggest that PRE/PRT alone cannot improve mobility but can improve strength. This assumption is consistent with results from other RCTs on exercise interventions targeting children with CP, as well as the review by Ryan et al. (2017). Scholtes et al. (2011) reported that while muscle strength improved from a 12-week PRE program for children with CP, walking ability did not. However, mobility and running ability did improve in children with CP using a running intervention conducted by Gibson et al. (2018). Therefore, different types of exercise interventions yield improvements in different domains of physical function. Exercise interventions aimed at exploring other aspects of physical performance (i.e. functional mobility, gait, balance) also should be studied in adults with childhood-onset disabilities.
Notably, none of the studies evaluated the effects of the exercise interventions on balance. This is possibly attributable to the fact that the types of exercise interventions administered in the RCTs did not target balance (PRE/PRTs train specific muscle groups to improve strength and some aspects of gait or functional mobility). A RCT by Grecco et al. (2013) found that treadmill gait training has the potential to improve functional balance in children with CP. Such exercise interventions should be investigated further to observe their effects on the balance of adults with CP and other childhood-onset disabilities.
4.2.2Outcome measures
Outcome measures used to assess fitness across the four studies were 6MWT, Borg-20 grades, MPST, and 10×5 m Sprint Test; measures to assess functional mobility were TUDS and GMFM; measures to assess strength were TST, 1RM, and 30-s Repetition Maximum; and measures to assess gait were GPS, FMS, 10MWT, and FAQ. Of these measures, good to excellent reliability and validity were shown in children with CP or other neuromuscular conditions (GPS, FMS, FAQ, 10MWT, MPST, 10×5-m Sprint Test, 30-s Repetition Maximum, GMFM, TUDS). This is also true for typically developing children and adults (Borg-20 Grades, TUDS, TST, 1RM), and adults with other disabilities (i.e., not childhood-onset) (TST, 10MWT). However, few of the measures have been validated for adolescents (MPST, 30-s Repetition Maximum) or adults (6MWT, Borg-20 Grades) with childhood-onset disabilities such as CP and SB. The 10MWT has been validated for adults with TBI but not specifically for adults with childhood-onset ABI; in fact, none of the measures were validated for adults with childhood-onset ABI. We recommend more research on validating physical performance outcome measures for adolescents and adults with CP, SB, and childhood-onset ABI.
Furthermore, there are very few valid and reliable balance outcome measures for adults with CP or other childhood-onset disabilities. A systematic review by Saether et al. (2013) found that only 2 out of 22 balance assessment tools used in clinical practice (Posture and Posture Ability Scale (PPAS), Seated Posture Control Measurement (SPCM)) were validated in adults with CP; the rest were only validated in children with CP. These tools both focus on postural balance and are more commonly used for evaluating individuals with more significant motor impairment. Another clinical practice outcome measure that can potentially be used for ambulatory adults with CP or childhood-onset ABIs is the Community Balance and Mobility Scale (CB&M), which evaluates balance during more challenging tasks commonly encountered in the community (Howe et al., 2011). The CB&M has excellent inter- and intra-rater (ICC = 0.977) and test-retest reliability (ICC = 0.975) in adults with TBI, and good responsiveness when tested on adolescents with CP (Brien & Sveistrup, 2011; Howe et al., 2006). Given that the CB&M is intended for adults with only minor motor impairment who can ambulate without a mobility device, it would capture only a small subset of our target population. We recommend that more balance outcome measures be studied for validity and reliability in ambulatory adults with CP and other childhood-onset disabilities (in particular, in those who have moderate motor impairment and rely on a handheld mobility device, or in those who have difficulty walking long distances).
A commonly used measure of strength in cli-nical practice is dynamometry, which involves devices such as the Pinchmeter-P100 and Grip Dynamometer-G100 to evaluate strength in the extremities. None of the studies that were included used dynamometry outcome measures, even though each study used at least one measure of strength. This is likely because the exercise interventions administered in the studies did not target the upper extremities. Both the Pinchmeter-P100 and Grip Dynamometer-G100 demonstrate excellent test-retest reliability (ICC = 0.830–0.998) for measuring grip and hand strength in adults with CP (Hutzler et al., 2013). Notably, a recent literature review revealed that grip strength may be an evaluative or predictive biomarker of current and future health status (e.g., disease status, depression, cancer mortality) in adults (Bohannon, 2019). If these properties of grip strength apply to adults with CP, SB, and ABI, dynamometry would be a useful tool for health maintenance as they age. We recommend that grip strength be investigated as a biomarker for adults with childhood-onset disabilities. The Pinchmeter-P100 and Grip Dynamometer-G100 are both reliable tools of dynamometry that can be used in future studies for adults with CP.
The Timed Stands Test, which requires participants to complete ten full stands from a sitting position, was used in two of the four studies; however, this test may be too demanding or difficult for individuals who are deconditioned or have significant impairment. The Five Times Sit to Stand Test (5xSTS) and the 30 Second Sit to Stand/Chair Test (30CST) are both variations of the TST used in clinical practice that may be better suited for adults with CP, SB, and ABI. The 5xSTS is an abbreviated version of the TST that requires the participant to complete five full stands, rather than the original ten (Wang, Liao, & Peng, 2011). It has excellent test-retest reliability (ICC =0.99) and moderate to high reliability when compared to other tests (r values ranged from 0.30 to 0.78) for children with CP (Wang, Liao, & Peng, 2011). The 30CST is another variation of the TST that was developed to overcome the floor effect of the TST (Jones, Rikli, & Beam, 1999). It measures how many repetitions the participant is able to complete in 30 seconds, which is ideal for those who struggle to complete even one repetition (e.g., individuals with CP, GMFCS III and IV) (Jones, Rikli, & Beam, 1999). This test has excellent test-retest reliability (r = 0.89), inter- and intra-rater reliability (r = 0.95), and criterion validity (r > 0.70) in community dwelling elderly (Jones, Rikli, & Beam, 1999). Both tests should be investigated for adults with childhood-onset disabilities.
4.3Clinical considerations
This review also identifies a discrepancy between measures that are used in RCTs and measures that are used in clinical practice. For example, measures that are commonly used in clinical practice (e.g., CB&M, 30CST, dynamometry) were not used in the RCTs. Similarly, the measures found across the four RCTs are not consistently used in clinical practice; since there is currently no gold standard for physical performance evaluation in our target population, clinicians often select outcome measures based on preferences or clinical setting instead. Additionally, some tests that are only validated for children (e.g., Dynamic Gait Index) are often used in clinical practice with adults as the best option available. No recommendations can yet be made, based on our review, for the clinical use of the measures used in RCTs, but we propose that clinicians and researchers collaborate to validate measures used in RCTs for clinical practice and vice versa. While our review cannot aid clinicians and researchers in selecting appropriate measures to evaluate physical performance outcomes in response to exercise interventions, it does identify many gaps in research as well as future research opportunities.
5Strengths and limitations
This is the only existing scoping review that examines the outcome measures used in exercise interventions specifically for adults with childhood-onset disabilities and identifies various gaps in the quality (via validity and reliability) of the measures. Our review is strengthened by the use of an experienced information specialist to conduct an exhaustive literature search, as well as multiple reviewers to conduct screening and data extraction independently, in duplicate. The multidisciplinary expertise of our coauthors (which includes researchers and clinicians who specialize in the areas of physical rehabilitation, physical activity promotion, and young adulthood and disability) helps to strengthen the review. We also acknowledge some limitations. While the literature search was thorough and the search criteria included participants with CP, SB or ABIs, the studies that qualified for inclusion in this scoping review were focused on adults with CP only. Therefore, the validity and reliability of the outcome measures as well as the results of the exercise interventions may not apply to the other populations of interest (i.e., adults with childhood-onset ABI and adults with SB). Furthermore, it was challenging to identify ABIs (e.g., stroke) as ‘childhood-onset’ because this was not explicitly stated in studies. We used mean participant age and time of stroke onset to determine whether the ABI first developed in childhood. Moreover, since this review included English-language studies only, there may have been bias toward the inclusion of studies from English-speaking countries. Since the search was limited to the last 11 years, we may have also excluded important and relevant studies from before the year 2008. Another possible limitation is the inclusion of only RCTs, since a broader range of study designs may have included more outcome measures or studies involving individuals with SB and ABI. We plan to use the results from this review to begin fitness testing research which is a step towards validation work.
6Conclusion
Our scoping review on validated outcome measures and exercise interventions for adults with childhood-onset disabilities revealed several gaps in the existing research on exercise interventions as well as the validity of the outcome measures. We recommend that future studies evaluate the effects of exercise interventions on adults with childhood-onset disabilities, as most existing studies only sample children. Larger sample sizes should be used in these studies. Adults with childhood-onset disabilities other than CP should be sampled as well. It would also be useful to investigate the effectiveness of different exercise interventions (e.g., treadmill training, balance exercises) on different domains of physical performance (e.g., gait, mobility, balance), since existing RCTs with adults focus on PRE/PRT interventions that target strength. There is a lack of research identifying appropriate exercise interventions and validated outcome measures especially for the balance domain. Furthermore, the outcome measures across the included studies were often validated in a population different from the one being studied (i.e., in children with CP and healthy adults rather than adults with childhood-onset disabilities). We recommend that clinicians and researchers collaborate to examine the reliability and validity of outcome measures specifically for adults with childhood-onset disabilities to ensure their usefulness and accuracy in future clinical practice.
Conflict of interest
None to report.
Funding
This research was supported by Toronto Rehab Foundation.
References
1 | About Acquired Brain Injury. (n.d.). https://www.braininjurycanada.ca/acquired-brain-injury/ |
2 | Acharya, K. , Meza, R. , Msall, M. E. ((2017) ). Disparities in Life Course Outcomes for Transition-Aged Youth with Disabilities. Pediatric Annals, 46: (10), e371–e376. |
3 | American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596 |
4 | Andersson, C. , Asztalos, L. , Mattsson, E. ((2006) ). Six-minute walk test in adults with cerebral palsy. A study of reliability. Clinical Rehabilitation, 20: (6), 488–495. |
5 | Andersson, C. , Grooten, W. , Hellsten, M. , Kaping, K. , Mattsson, E. ((2003) ). Adults with cerebral palsy: Walking ability after progressive strength training. Developmental Medicine & Child Neurology, 45: (4), 220–228. |
6 | Arksey, H. , O’Malley L. ((2005) ). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8: (1), 19–32. |
7 | Baker, R. , McGinley, J. L. , Schwartz, M. H. , Beynon, S. , Rozumalski, A. , Graham, H. K. , Tirosh, O. ((2009) ). The gait profile score and movement analysis profile. Gait & Posture, 30: (3), 265–269. |
8 | Bania, T. A. , Dodd, K. J. , Baker, R. J. , Graham, H. K. , Taylor, N. F. ((2016) ). The effects of progressive resistance training on daily physical activity in young people with cerebral palsy: a randomised controlled trial. Disability and Rehabilitation, 38: (7), 620–626. |
9 | Betz, C. L. , Smith, K. , Van Speybroeck, A. , Jacobs, R. A. , Rivera, N. , Lee, J. , Saghhafi, S. , Nguyen, B. , Tu, H. ((2018) ). Descriptive Analysis and Profile of Health Care Transition Services Provided to Adolescents and Emerging Adults in the Movin’ On Up Health Care Transition Program. Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners, 32: (3), 273–284. |
10 | Beynon, S. , McGinley, J. L. , Dobson, F. , Baker, R. ((2010) ). Correlations of the Gait Profile Score and the Movement Analysis Profile relative to clinical judgments. Gait Posture, 32: (1), 129–132. |
11 | Blackman, J. A. , Conaway, M. R. ((2013) ). Adolescents with Cerebral Palsy. Clinical Pediatrics, 53: (4), 356–363. |
12 | Bloemen, M. A. , Takken, T. , Backx, F. J. , Vos, M. , Kruitwagen, C. L. , de Groot, J. F. ((2017) ). Validity and Reliability of Skill-Related Fitness Tests for Wheelchair-Using Youth With Spina Bifida. Archives of Physical Medicine and Rehabilitation, 98: (6), 1097–1103. |
13 | Bohannon, R. W. ((2019) ). Grip Strength: An Indispensable Biomarker for Older Adults. Clinical Interventions in Aging, 14: , 1681–1691. |
14 | Borg, G. ((1970) ). Perceived exertion as an indicator of somatic stress. Scandinavian Journal of Rehabilitation Medicine, 2: (2), 92–98. |
15 | Brien, M. , Sveistrup, H. ((2011) ). An intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsy. Pediatric Physical Therapy: The Official Publication of the Section on Pediatrics of the American Physical Therapy Association, 23: (3), 258–266. |
16 | Brunton, L. K. , Bartlett, D. J. ((2011) ). Validity and reliability of two abbreviated versions of the Gross Motor Function Measure. Physical Therapy, 91: (4), 577–588. |
17 | Chen, M. J. , Fan, X. , Moe, S. T. ((2002) ). Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. Journal of Sports Sciences, 20: (11), 873–899. |
18 | Collen, F. M. , Wade, D. T. , Bradshaw, C. M. ((1990) ). Mobility after stroke: reliability of measures of impairment and disability. International Disability Studies, 12: (1), 6–9. |
19 | Crytzer, T. M. , Dicianno, B. E. , Robertson, R. J. , Cheng, Y. T. ((2015) ). Validity of a wheelchair perceived exertion scale (wheel scale) for arm ergometry exercise in people with spina bifida. Perceptual and Motor Skills, 120: (1), 304–322. |
20 | Csuka, M. , McCarty, D. J. ((1985) ). Simple method for measurement of lower extremity muscle strength. The American Journal of Medicine, 78: (1), 77–81. |
21 | de Groot, J. , Takken, T. , Verschuren, O. , Maher, L. , Wiart, C. ((2015) ). In)activity and health in childhood onset disability across the lifespan. Physiotherapy, 101: (1), eS1–eS25. |
22 | Erickson, J. D. , Patterson, J. M. , Wall, M. , Neumark-Sztainer, D. ((2005) ). Risk behaviors and emotional well-being in youth with chronic health conditions. Children’s Health Care, 34: (3), 181–192. |
23 | Flansbjer, U. B. , Holmbäck, A. M. , Downham, D. , Patten, C. , Lexell, J. ((2005) ). Reliability of gait performance tests in men and women with hemiparesis after stroke. Journal of Rehabilitation Medicine, 37: (2), 75–82. |
24 | Foster, M. R. ((2019) ). Spina Bifida. https://emedicine.medscape.com/article/311113-overview |
25 | Garber, C. E. , Blissmer, B. , Deschenes, M. R. , Franklin, B. A. , Lamonte, M. J. , Lee, I. M. , Nieman, D. C. , Swain, D. P. , American College of Sports Medicine. ((2011) ). American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine and Science in Sports and Exercise, 43: (7), 1334–1359. |
26 | Gibson, N. , Chappell, A. , Blackmore, M. , Morris, S. , Williams, G. , Bear, N. , Allison, G. ((2018) ). The effect of a running intervention on running ability and participation in children with cerebral palsy: a randomized controlled trial. Disability and Rehabilitation, 40: , 1–9. |
27 | Gillett, J. G. , Lichtwark, G. A. , Boyd, R. N. , Barber, L. A. ((2018) ). Functional Anaerobic and Strength Training in Young Adults with Cerebral Palsy. Medicine and Science in Sports and Exercise, 50: (8), 1549–1557. |
28 | Goodman, D. M. , Hall, M. , Levin, A. , Watson, R. S. , Williams, R. G. , Shah, S. S. , Slonim, A. D. ((2011) ). Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics, 128: (1), 5–13. |
29 | Gorton, G. E. , 3rd, Stout, J. L. , Bagley, A. M. , Bevans, K. , Novacheck, T. F. , Tucker, C. A. ((2011) ). Gillette Functional Assessment Questionnaire -item skill set: factor and Rasch analyses. Developmental Medicine and Child Neurology, 53: (3), 250–255. |
30 | Graham, H. K. , Harvey, A. , Rodda, J. , Nattrass, G. R. , Pirpiris, M. ((2004) ). The Functional Mobility Scale (FMS). Journal of Pediatric Orthopedics, 24: (5), 514–520. |
31 | Graser, J. , Letsch, C. , van Hedel, H. ((2016) ). Reliability of timed walking tests and temporo-spatial gait parameters in youths with neurological gait disorders. BMC Neurology, 16: . |
32 | Grecco, L. A. , Tomita, S. M. , Christovão, T. C. , Pasini, H. , Sampaio, L. M. , Oliveira, C. S. ((2013) ). Effect of treadmill gait training on static and functional balance in children with cerebral palsy: a randomized controlled trial. Brazilian Journal of Physical Therapy, 17: (1), 17–23. |
33 | Gross Motor Function Measure (GMFM). (n.d.). https://canchild.ca/en/resources/44-gross-motor-function-measure-gmfm# |
34 | Harvey, A. , Baker, R. , Morris, M. E. , Hough, J. , Hughes, M. , Graham, H. K. ((2010) ). Does parent report measure performance? A study of the construct validity of the Functional Mobility Scale. Developmental Medicine and Child Neurology, 52: (2), 181–185. |
35 | Harvey, A. , Graham, H. K. , Morris, M. E. , Baker, R. , Wolfe, R. ((2007) ). The Functional Mobility Scale: ability to detect change following single event multilevel surgery. Developmental Medicine and Child Neurology, 49: (8), 603–607. |
36 | Harvey, A. R. , Morris, M. E. , Graham, H. K. , Wolfe, R. , Baker, R. ((2010) ). Reliability of the functional mobility scale for children with cerebral palsy. Physical & Occupational Therapy in Pediatrics, 30: (2), 139–149. |
37 | Hombergen, S. P. , Huisstede, B. M. , Streur, M. F. , Stam, H. J. , Slaman, J. , Bussmann, J. B. , van den Berg-Emons, R. J. ((2012) ). Impact of cerebral palsy on health-related physical fitness in adults: systematic review. Archives of Physical Medicine and Rehabilitation, 93: (5), 871–881. |
38 | Howe, J. A. , Inness, E. L. , Venturini, A. , Williams, J. I. , Verrier, M. C. ((2006) ). The Community Balance and Mobility Scale–a balance measure for individuals with traumatic brain injury. Clinical Rehabilitation, 20: (10), 885–895. |
39 | Hunt, S. , Sharma, N. ((2013) ). Pediatric to adult-care transitions in childhood-onset chronic disease: hospitalist perspectives. Journal of Hospital Medicine, 8: (11), 627–630. |
40 | Hutzler, Y. , Lamela Rodríguez, B. , Mendoza Laiz, N. , Díez, I. , Barak, S. ((2013) ). The effects of an exercise training program on hand and wrist strength, and function, and activities of daily living, in adults with severe cerebral palsy. Research in Developmental Disabilities, 34: (12), 4343–4354. |
41 | Imms, C. , Adair, B. ((2017) ). Participation trajectories: impact of school transitions on children and adolescents with cerebral palsy. Developmental Medicine and Child Neurology, 59: (2), 174–182. |
42 | Jahnsen, R. , Villien, L. , Egeland, T. , Stanghelle, J. K. , Holm, I. ((2004) ). Locomotion skills in adults with cerebral palsy. Clinical Rehabilitation, 18: (3), 309–316. |
43 | Jones, C. J. , Rikli, R. E. , Beam, W. C. ((1999) ). A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport, 70: (2), 113–119. |
44 | Key Facts. (n.d.). Retrieved from https://www.yourcpf.org/statistics/ |
45 | LaPlante, M. P. ((2014) ). Key goals and indicators for successful aging of adults with early-onset disability. Disability and Health Journal, 7: (1 Suppl), S44–S50. |
46 | Lawrence, H. , Hills, S. , Kline, N. , Weems, K. , Doty, A. ((2016) ). Effectiveness of Exercise on Functional Mobility in Adults with Cerebral Palsy: A Systematic Review. Physiotherapy Canada. Physiotherapie Canada, 68: (4), 398–407. |
47 | Maeland, S. , Jahnsen, R. , Opheim, A. , Froslie, K. F. , Moe-Nilssen, R. , Stanghelle, J. K. ((2009) ). No effect on gait function of progressive resistance exercise in adults with cerebral palsy –A single-blind randomized controlled trial. Advances in Physiotherapy, 11: (4), 227–233. |
48 | McCurdy, K. , Langford, G. , Jenkerson, D. , Doscher, M. ((2008) ). The validity and reliability of the 1RM bench press using chain-loaded resistance. Journal of Strength and Conditioning Research, 22: (3), 678–683. |
49 | McGough, E. L. , Lin, S. Y. , Belza, B. , Becofsky, K. M. , Jones, D. L. , Liu, M. , Wilcox, S. , Logsdon, R. G. ((2019) ). A Scoping Review of Physical Performance Outcome Measures Used in Exercise Interventions for Older Adults with Alzheimer Disease and Related Dementias. Journal of Geriatric Physical Therapy, 42: (1), 28–47. |
50 | McGowan, J. , Sampson, M. , Salzwedel, D.M. , Cogo, E. , Foerster, V. , Lefebvre, C. ((2016) ). PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. Journal of Clinical Epidemiology, 75: , 40–6. |
51 | Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , PRISMA Group ((2009) ). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed.), 339: , b2535. |
52 | Morgan, P. , Mcdonald, R. , Mcginley, J. ((2015) ). Perceived Cause, Environmental Factors, and Consequences of Falls in Adults with Cerebral Palsy: A Preliminary Mixed Methods Study. Rehabilitation Research and Practice, 196395. |
53 | Newcomer, K. L. , Krug, H. E. , Mahowald, M. L. ((1993) ). Validity and reliability of the timed-stands test for patients with rheumatoid arthritis and other chronic diseases. The Journal of Rheumatology, 20: (1), 21–27. |
54 | Novacheck, T. F. , Stout, J. L. , Tervo, R. ((2000) ). Reliability and validity of the Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. Journal of Pediatric Orthopedics, 20: (1), 75–81. |
55 | Opheim, A. , Jahnsen, R. , Olsson, E. , Stanghelle, J. K. ((2009) ). Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. Developmental Medicine and Child Neurology, 51: (5), 381–388. |
56 | Peters, M. D. J. , Godfrey, C. , McInerney, P. , Baldini, Soares C. , Khalil, H. , Parker, D. ((2017) ). Chapter 11: Scoping Reviews. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute. Available from https://reviewersmanual.joannabriggs.org/ |
57 | Pirpiris, M. , Wilkinson, A. J. , Rodda, J. , Nguyen, T. C. , Baker, R. J. , Nattrass, G. R. , Graham, H. K. ((2003) ). Walking speed in children and young adults with neuromuscular disease: comparison between two assessment methods. Journal of Pediatric Orthopedics, 23: (3), 302–307. |
58 | Porter, R. S. , Kaplan, J. L. , Lynn, R. B. , Reddy, M. T. ((2018) ). The Merck manual of diagnosis and therapy. Kenilworth, NJ: Merck Sharp & Dohme, a subsidiary of Merck. |
59 | Reuben, D. B. , Magasi, S. , McCreath, H. E. , Bohannon, R. W. , Wang, Y. C. , Bubela, D. J. , Rymer, W. Z. , Beaumont, J. , Rine, R. M. , Lai, J. S. , Gershon, R. C. ((2013) ). Motor assessment using the NIH Toolbox. Neurology, 80: (11 Suppl 3), S65–S75. |
60 | Roebroeck, M. E. , Jahnsen, R. , Carona, C. , Kent, R. M. , Chamberlain, M. A. ((2009) ). Adult outcomes and lifespan issues for people with childhood-onset physical disability. Developmental Medicine & Child Neurology, 51: (8), 670–678. |
61 | Russell D. Gross Motor Function Measure (GMFM-66 & GMFM-88). User’s Manual. ((2002) ). Clinics in Developmental Medicine No. 159. London: Mac Keith Press. |
62 | Russell, D. J. , Avery, L. M. , Rosenbaum, P. L. , Raina, P. S. , Walter, S. D. , Palisano, R. J. ((2000) ). Improved scaling of the gross motor function measure for children with cerebral palsy: evidence of reliability and validity. Physical Therapy, 80: (9), 873–885. |
63 | Ryan, J. M. , Cassidy, E. E. , Noorduyn, S. G. , O’Connell, N. E. ((2017) ). Exercise interventions for cerebral palsy. The Cochrane Database of Systematic Reviews, 6: (6), CD011660. |
64 | Rydwik, E. , Frändin, K. , Akner, G. ((2004) ). Effects of physical training on physical performance in institutionalised elderly patients (+) with multiple diagnoses. Age and Ageing, 33: (1), 13–23. |
65 | Saether, R. , Helbostad, J. L. , Riphagen, I. I. , Vik, T. ((2013) ). Clinical tools to assess balance in children and adults with cerebral palsy: a systematic review. Developmental Medicine and Child Neurology, 55: (11), 988–999. |
66 | Sandström, K. , Alinder, J. , Oberg, B. ((2004) ). Descriptions of functioning and health and relations to a gross motor classification in adults with cerebral palsy. Disability and Rehabilitation, 26: (17), 1023–1031. |
67 | Seo, D. I. , Kim, E. , Fahs, C. A. , Rossow, L. , Young, K. , Ferguson, S. L. , Thiebaud, R. , Sherk, V. D. , Loenneke, J. P. , Kim, D. , Lee, M. K. , Choi, K. H. , Bemben, D. A. , Bemben, M. G. , So, W. Y. ((2012) ). Reliability of the one-repetition maximum test based on muscle group and gender. Journal of sports science & Medicine, 11: (2), 221–225. |
68 | Scholtes, V. A. , Becher, J. G. , Janssen-Potten, Y. J. , Dekkers, H. , Smallenbroek, L. , Dallmeijer, A. J. ((2012) ). Effectiveness of functional progressive resistance exercise training on walking ability in children with cerebral palsy: a randomized controlled trial. Research in Developmental Disabilities, 33: (1), 181–188. |
69 | Minute Walk Test. (n.d.). https://www.sralab.org/rehabilitation-measures/6-minute-walk-test |
70 | Taylor, N. F. , Dodd, K. J. , Baker, R. J. , Willoughby, K. , Thomason, P. , Graham, H. K. ((2013) ). Progressive resistance training and mobility-related function in young people with cerebral palsy: a randomized controlled trial. Developmental Medicine and Child Neurology, 55: (9), 806–812. |
71 | Timberlake, M. D. , Corbett, S. T. , Costabile, R. A. , Herndon, C. D. ((2015) ). Identification of adolescent and adult patients receiving pediatric urologic care and establishment of a dedicated transition clinic. Journal of Pediatric Urology, 11: (2), 62.e1–62.e626. |
72 | Tricco, A. C. , Lillie, E. , Zarin, W. , O’Brien, K. K. , Colquhoun, H. , Levac, D. , Moher, D. , Peters, M. D. , Horsley, T. , Weeks, L. , Hempel, S. et al. ((2018) ). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med, 169: (7), 467–473. |
73 | Tyson, S. , Connell, L. ((2009) ). The psychometric properties and clinical utility of measures of walking and mobility in neurological conditions: a systematic review. Clinical Rehabilitation, 23: (11), 1018–1033. |
74 | Verschuren, O. , Bongers, B. C. , Obeid, J. , Ruyten, T. , & Takken, T. , ((2013) a). Validity of the muscle power sprint test in ambulatory youth with cerebral palsy. Pediatric Physical Therapy : The official publication of the Section on Pediatrics of the American Physical Therapy Association, 25: (1), 25–28. |
75 | Verschuren, O. , Ketelaar, M. , Takken, T. , Van Brussel, M. , Helders, P. J. , Gorter, J. W. ((2008) ). Reliability of hand-held dynamometry and functional strength tests for the lower extremity in children with Cerebral Palsy. Disability and Rehabilitation, 30: (18), 1358–1366. |
76 | Verschuren, O. , Takken, T. , Ketelaar, M. , Gorter, J. W. , Helders, P. J. ((2007) ). Reliability for running tests for measuring agility and anaerobic muscle power in children and adolescents with cerebral palsy. Pediatric Physical Therapy: The official publication of the Section on Pediatrics of the American Physical Therapy Association, 19: (2), 108–115. |
77 | Verschuren, O. , Zwinkels, M. , Obeid, J. , Kerkhof, N. , Ketelaar, M. , & Takken, T. ((2013) b). Reliability and validity of short-term performance tests for wheelchair-using children and adolescents with cerebral palsy. Developmental Medicine and Child Neurology, 55: (12), 1129–1135. |
78 | Wade, D. T. ((1992) ). Measurement in neurological rehabilitation. Current Opinion in Neurology and Neurosurgery, 5: (5), 682–686. |
79 | Wang, T. H. , Liao, H. F. , Peng, Y. C. ((2011) ). Reliability and validity of the five-repetition sit-to-stand test for children with cerebral palsy. Clinical Rehabilitation, 26: (7), 664–671. |
80 | Watson, M. ((2002) ). Refining the Ten-metre Walking Test for Use with Neurologically Impaired People. Physiotherapy, 88: , 386–397. |
81 | Wedege, P. , Steffen, K. , Strøm, V. , Opheim, A. I. ((2017) ). Reliability of three-dimensional kinematic gait data in adults with spinal cord injury. Journal of Rehabilitation and Assistive Technologies Engineering, 4: , 2055668317729992. |
82 | World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/ |
83 | Young, N. L. , Steele, C. , Fehlings, D. , Jutai, J. , Olmsted, N. , Williams, J. I. ((2005) ). Use of health care among adults with chronic and complex physical disabilities of childhood. Disability and Rehabilitation, 27: (23), 1455–1460. |
84 | Zaino, C. A. , Marchese, V. G. , Westcott, S. L. ((2004) ). Timed up and down stairs test: preliminary reliability and validity of a new measure of functional mobility. Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association, 16: (2), 90–98. |




