Building the bond: Predictors of the alliance in neurorehabilitation
Abstract
BACKGROUND:
Neurorehabilitation services are often delivered through group psycho-education programmes. However, little is known about the therapeutic process at work during such sessions. The present study is the first to gain insight into the therapeutic alliance, during a seven-session group programme. In addition, cognitive, emotional, and demographic predictors of the alliance, and participants’ feelings towards their group members, were investigated, together with predictors of patient engagement.
METHODS:
Forty-five participants with an acquired brain injury completed a series of questionnaires, and neuropsychological assessment, following group psycho-education. The group facilitator completed a parallel therapeutic alliance questionnaire, and rated participants’ engagement.
RESULTS:
Results demonstrated that a strong alliance can be formed in seven group sessions. Notably, no demographic or cognitive factors appear to pose a barrier to developing a therapeutic alliance, nor to group attraction.
CONCLUSION:
High levels of depression, however, may be a challenge, and clinicians may need to tailor their clinical skills to ensure a good therapeutic relationship with such patients. To promote engagement, clinicians may also need to provide additional support to patients with lower levels of education, working memory, and episodic memory impairment.
1Introduction
Acquired brain injury (ABI) is a leading cause of disability worldwide (WHO, 2000-2012), with survivors experiencing a range of complex cognitive and psycho-social changes that can last a lifetime (Draper, Ponsford & Schönberger, 2007; Ponsford, Draper, & Schönberger, 2008). Post-injury impairments often represent a dramatic change in functioning (Colantonio, Ratcliff, Chase, Kelsey, et al., 2004; Ponsford et al., 2008), highlighting the importance of neurorehabilitation services in adjustment to the long-term consequences (Coetzer, 2008). Indeed, the chronic nature of impairment is acknowledged by the National Service for Long Term Conditions (Coetzer, Roberts, Turnbull, & Vaughan, 2018; Department of Health, 2005). Successful rehabilitation inevitably depends on the multi-disciplinary professionals within services, with whom survivors interact (Bright, Kayes, Worrall, & McPherson, 2015; Stagg, Douglas, & Iacono, 2019). The collaborative nature of the client-therapist relationship, more commonly described as the therapeutic or working alliance, appears to act as a vehicle to promote positive rehabilitation outcomes (Stagg et al., 2019). Within the literature on ABI, it is poorly understood how specific features of the population might pose unique challenges to developing a strong alliance (Stagg et al., 2019).
The therapeutic alliance (TA) is a term describing the relational processes which unfold during clinical interactions, and its roots are well-established in the psychotherapy literature (Horvath & Luborsky, 1993; Horvath & Symonds, 1991). Bordin (1979) provides the most influential theoretical framework to follow, consisting of three underlying dimensions, which are important for the TA. These are: 1) the client and therapist agreement on the tasks to be completed as part of therapy; 2) agreement on the goals and expected outcomes; and 3) the interpersonal and emotional bond between client and therapist (Bordin, 1979). Within psychotherapy, the TA has been shown to be a reliable and moderate predictor of outcome (Hovarth & Symonds, 1991; Martin, Garske, & Davis, 2000, for meta-analyses). However, the current literature in the field of neurorehabilitation provides only limited insight into this issue.
1.1The therapeutic alliance in brain injury rehabilitation
More recently, the TA has been identified as having an enhancing effect on outcomes across rehabilitation and medical contexts (Hall, Ferreira, Maher, Latimer, & Ferreira, 2010, for a review): For example, improving symptoms in multiple sclerosis (Rosti-Otajärvi, Mäntynen, Koivisto, Huhtala, & Hämäläinen, 2014), a range of outcomes in the physical rehabilitation of cardiac and musculoskeletal conditions (Hall et al., 2010), and in the treatment of chronic pain (Ferreira, Ferreira, Maher, Refshauge, Latimer, & Adams, 2013). In stroke rehabilitation, some patients perceive the quality of the client-therapist partnership to be of primary importance, above that of the therapy’s content or duration (Peris, Taylor, & Shields, 2012). Despite only limited research into the role of the TA in ABI rehabilitation, the emerging idea is that it shapes outcomes, and is influenced by several factors present in the rehabilitation environment (Stagg et al., 2019, for a review).
The majority of empirical investigations of the role of the TA in rehabilitation outcomes have focused on vocational issues (work, work prospects, school), and have demonstrated positive associations (Evans, Sherer, Nakase-Richardson, Mani, & Irby, 2008; Klonoff, Lamb, & Henderson, 2001; Lustig, Strauser, Weems, Donnell, & Smith, 2003; Schönberger, Humle, Zeeman, & Teasdale, 2006a; Stagg et al., 2019, for a review). Important clinical outcomes include improved independence and social interactions, and reduced communication difficulties and somatic problems (on the European Brain Injury Questionnaire) (Schönberger, Humle, & Teasdale, 2006b).
Finally, it has been demonstrated that the TA promotes patient compliance with a holistic rehabilitation programme, through its impact on self-awareness (Schönberger, Humle, & Teasdale, 2006c). That is, the TA enhances patient awareness, and those who are aware of their difficulties comply and engage in rehabilitation (Schönberger et al., 2006c). Patient engagement with the rehabilitation process is thought to play an important role in its success and adherence (Bright, Kayes, Worrall, & McPherson, 2015, for a review; Lenze, Munin, Quear, Dew, et al., 2004). The patient-therapist relationship is a potential mechanism to enhance engagement, with the majority of evidence from qualitative accounts (Bishop, Kayes, & McPherson, 2019; Bright, Kayes, Cummins, Worrall, & McPherson, 2017; Lawton, Haddock, Conroy, & Sage, 2016). The direct role of the TA on engagement, however, remains unclear.
1.2Predictors of the therapeutic alliance
If the TA is considered a crucial component of rehabilitation by patients and professionals (Lawton et al., 2016), careful attention needs to be paid to the factors which might impede (or facilitate) the development of this process. This is especially relevant in the context of ABI, where the nature of impairment may place unique demands on the TA. For example, a number of interesting interpersonal factors have been identified through qualitative work, including a genuine bond within the therapeutic rapport, and professional collaboration (Bishop, Kayes, & McPherson, 2019; Lawton et al., 2016). Additional insights from qualitative research identify a range of cognitive consequences as the most frequently reported challenges in developing an alliance, followed by emotional factors, and behavioural disinhibition (Judd & Wilson, 2005).
Quantitative research provides modest insight into the factors which promote positive perceptions of the TA, for both patients and professionals (Stagg et al., 2019). For example, studies have demonstrated that younger patient age (Schönberger et al., 2006c) and greater years in education (Sherer, Evans, Leverenz, Stouter, Irby, et al., 2007) positively influenced the strength of the alliance. In terms of injury-specific factors, the influence of cognitive difficulties has been reported to be weak in nature, and differentially associated to therapist and client perceptions (Schönberger, Humle, & Teasdale, 2007). For instance, poor attentional impairment may influence the strength of the alliance negatively, whereas poorer performance on a memory task may have a positive influence, albeit weakly (Schönberger et al., 2007). The authors reported that, out of the several higher cognitive functions explored, verbal fluency and IQ (Information sub-test of the Wechsler Adult Intelligence Scale) was found to be positively related to aspects of the TA. It is noteworthy, however, that the findings of these correlational analyses were not subject to an alpha adjustment, and should be interpreted with caution.
Most of the work investigating the TA in neurorehabilitation has focused on holistic (and intense) programmes, and are correlational in nature (Stagg et al., 2019). However, in a recent study Zelencich and colleagues (2019) aimed to address these gaps by using regression analyses to explore the predictors of the TA in the context of cognitive behaviour therapy (CBT) for people with brain injury. In contrast to previous work (Schönberger et al., 2006c Sherer, Evans, Leverenz, Stouter, et al., 2007) no demographic factors were found to have an influence, however greater time since injury was predictive of a stronger TA. Interestingly, no measure of memory or executive function was predictive of the strength of the therapeutic relationship (Zelencich, Kazantzis, Wong, McKenzie, et al., 2019). This robust empirical finding is suggestive that an ABI, and related cognitive impairment, does not necessarily pose a barrier to developing an effective TA, at least in the context of CBT.
1.3Emotional predictors of the therapeutic alliance
One aspect of brain injury that may pose a barrier to the TA, but has not received much attention in the literature, are the emotional consequences. It is widely acknowledged that a brain injury often results in a range of emotional difficulties, most commonly depression and anxiety (Hiott & Labbate, 2002; Jorge, Robinson, Moser, Tateno, et al., 2004; Kreutzer, Seel, & Gourley, 2001). Such difficulties can impact upon many aspects of life (Ponsford et al., 2008), are a significant source of care-giver burden (Ergh, Rapport, Coleman, & Hanks, 2002), and compromise socio-emotional functioning (Ownsworth & Fleming, 2005). It seems, therefore, possible that emotional factors may also play a role in rehabilitation engagement and the therapeutic relationship, especially given that the establishment of an emotional bond is a core component of the TA (Bordin, 1979). Additionally, emotional factors such as depression are known to effect motivation (Smith, 2013), which may in turn influence task and goal agreement (additional dimensions of the TA). Indeed, qualitative evidence points to the limiting effect of emotional consequences on developing a strong patient-therapist bond (Judd & Wilson, 2005). Only two studies have directly explored the influence of emotional distress (Evans et al., 2008; Sherer et al., 2007), with one demonstrating a significant association between higher alliance ratings and lower levels of depression (Evans et al., 2008). The other, however, found no significant role (Sherer et al., 2007). Both studies were limited, in that all measures were collected within the first two weeks of therapy, when sufficient time had not passed to develop the alliance (Schönberger et al., 2006c)
1.4Therapeutic alliance across rehabilitation settings
Another issue which has not been previously investigated is how the TA, and factors affecting it, might play out in various rehabilitation settings. As previously mentioned, the existing studies have predominantly focused on holistic post-acute services, which are typically intense in nature (e.g. a number of sessions a week for several months). Intensive rehabilitation is not available for everyone, and service provision remains under-developed in many locations (Krug & Cieza, 2019). Many community services, therefore, seek out cost-effective theoretically driven models to rehabilitate their patients (Coetzer, et al., 2018). One such component of community services includes group psycho-education, to improve ABI consequences and understanding of injury (Backhaus, Ibarra, Klyce, Trexler, & Malec, 2010; Coetzer, 2008; Couchman, McMahon, Kelly, & Ponsford, 2014). Such programmes are common across services (Tyerman & Hucker, 2006), but to our knowledge there has been no previous investigation of the TA (and influencing factors) with the facilitators of group psycho-education programmes.
According to Bordin (1979) the TA is relevant across all settings which involve a process of change, and that each new environment may bring to light factors which could shape its strength. Given the role of the alliance in rehabilitation outcomes (Stagg et al., 2019), and the benefit of group psycho-education programmes within services, it is important to develop an understanding of influencing factors within this context. Additionally, one of the biggest values of group programmes for patients is the quality of the group interaction, and the informal learning which stems from it (Anson & Ponsford, 2006; Lundqvist, Linnros, Orlenius, & Samuelsson, 2010). A member’s feelings towards their group contributes to a number of important processes (Yalom & Rand, 1966), including outcome (Crowe & Grenyer, 2008; Marziali, Munroe-Blum, & McCleary, 1997). Factors affecting the strength of the group attitude may, therefore, be additional components worthy of investigation.
The present study, to our knowledge, is the first to investigate facilitator and patient perceptions of the strength of the alliance, from a short-term group psycho-education programme. Uniquely, it also aimed to investigate how emotional factors, as well as cognitive and demographic factors1, might influence the formation of both the therapeutic relationship and the group attitude. Finally, the present study aimed to investigate whether the factors of TA, group attitude, and emotional, cognitive, and demographic variables (age and education) were predictive of patient engagement within the group programme. Such data would allow clinicians to identify which patients may be vulnerable to experiencing challenges in forming a strong TA or poor programme engagement, allowing them to tailor their clinical and interpersonal skills accordingly (Bishop et al., 2019).
2Methods
2.1Participants
Forty-five participants with an ABI were included in the present study. Each had successfully completed of a seven-week group psycho-education programme (The Brain Injury Solutions and Emotions Programme, BISEP) at a community outpatient rehabilitation unit, the North Wales Brain Injury Service, Betsi Cadwaladr University Health Board (NWBIS, BCUHB). The sample consisted of 11 women and 34 men, ranging from 26 to 86 years old (M = 52, SD = 12), with mixed pathology, reflective of the rehabilitation environment. It included 21 people who had suffered a cerebrovascular accident (CVA), 17 who had suffered a traumatic brain injury (TBI), four who had an ABI following encephalitis, one following hypoxia during cardiac arrest, one following tumour recession, and one from the effects of radiation therapy. Participants ranged from nine-months following injury to 32 years (M = 5 years, SD = 8 years, MDN = 2 years). Participants were referred to BISEP by a NWBIS clinician, and consisted of those with confirmed ABI (as per NWBIS criteria, Coetzer, Vaughan, Roberts, & Rafal, 2003), duration of at least nine months or greater since injury, and sufficient language ability to benefit from a language-based intervention. Exclusion criteria were inability to give informed consent, and the presence of a neurodegenerative condition (one participant excluded based on this criterion), learning disability, or psychiatric disorder in need of acute care.
2.2Measures
2.2.1Therapeutic alliance
The present study used the shortened version of the Working Alliance Inventory (WAI-S) (Tracey & Kokotovic, 1989), originally developed by Horvath and Greenberg (1989). This measure is based upon Bordin’s pantheoretical model (1979) of TA and is widely used, including in studies on brain injury (Schönberger et al., 2006c). The measure includes parallel client and therapist versions, with reports of high reliability (α= 0.95 for therapist ratings, α= 0.97 for therapist ratings) (Tracey & Kokotovic, 1989). The WAI-S scale ranges from 12 (lowest alliance) to 84 (highest alliance), and includes 12 items which are responded to on a seven-point scale. Although this measure includes subscales capturing the three dimensions of the alliance, the aim of the present study was to investigate the overall alliance score (considered the most valid way to represent the measure, Tracey & Kokotovic, 1989). Patient and therapist versions were administered, to capture both perceptions. These were completed by all patients, and by the programme facilitator, immediately after the last session of BISEP, to allow sufficient time to develop the alliance over the seven session programme (Schönberger et al., 2006c). It was explained that participants and facilitator ratings would remain confidential, and data were anonymised by a research intern, prior to the analyses. If needed, participants were assisted in completing the form by a member of the NWBIS clinical team. Participants especially benefitted for an awareness of the two items on the scale that were reverse-scored.
2.2.2Group attraction
Within psychotherapy, aspects of the group dynamic (e.g. conflict and collaboration) have been shown to predict outcome within group programmes (Crowe & Grenyer, 2008). The present study, therefore aimed to capture members’ perceptions and attraction towards their group, and investigate potential barriers. To do this, the Group Attitude Scale was used (Evans & Jarvis, 1986). The Group Attitude Scale is a 20 item measure, scored on a 9-point Likert scale, where higher scores indicate more positive attitude towards their group. It reports high validity and reliability (α= 0.90–.97), and is considered reliable within the present sample (α= 0.81). This measure was chosen as it captures members’ desire to identify with, and be accepted by, their group. This element, relating to other survivors, is perceived as an important component by brain injury groups (Couchman et al., 2014; Levack, Kayes, & Fadyl, 2010; Salas, Casassus, Rowlands, Pimm, & Flanagan, 2018).
2.2.3Engagement
Patient engagement with the programme was defined as “deliberate effort and commitment” to partake in the goals and activities of the programme, demonstrated through active participation in the learning process, intervention activities, and group discussions (Lequerica & Kortte, 2010). Similar to Schönberger et al (2006a), engagement was rated by the BISEP facilitator on a five-point scale: 1) little or no activity, 2) activity when supported, 3) active without participation, 4) active and prepared, and 5) active, independent and spontaneous input.
2.2.4Emotion symptomology
To measure anxiety and depression symptomology the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) was used, which includes two sub-scales. The HADS and has been validated in people with ABI (Dawkins, Cloherty, Gracey, & Evans, 2006; Schönberger & Ponsford, 2010). Participants indicate, on a 4-point scale, agreement with statements such as “I still enjoy the things I used to enjoy”.
2.2.5Cognitive measures
Three tasks were chosen to measure higher cognitive functions. These include: 1) Inhibition, which was measured with the Hayling sentence completion task from the Hayling and Brixton tests (Burgess & Shallice, 1997). This reports high sensitivity (Burgess & Shallice, 1997), and validity in a sample of brain-injured patients (Odhuba, van den Broek, & Johns, 2005). 2) Working Memory was assessed using the Digit Span sub-task from the Wechsler Adult Intelligence Scale (WAIS IV) (Wechsler, 2008), widely used in individuals with ABI (Millis, Rosenthal, Novack, Sherer, et al., 2001). 3) Verbal Ability was measured using the Letter Fluency sub-task from the Delis-Kaplan Executive Function system (D-KEFS) (Delis, Kaplan, & Kramer, 2001), which is thought to be one of the strongest predictors of cognitive control (Henry & Crawford, 2004). Finally, memory was assessed using the Logical Memory sub-tasks from the Wechsler Memory Scale (immediate and delayed recall) (WMS-IV, Wechsler, 2009). This is an “industry standard” test of memory widely used in clinical practice and research within the context of ABI.
2.3Procedure
The study was granted ethical approval by the School of Psychology, Bangor University (2017-16048), and BCUHB (224613). Participants were referred to BISEP by their clinician, and attended the programme in addition to their usual care at the community outpatient service. Approximately two weeks before programme commencement, participants completed the HADS and neuropsychological assessment in random order, as part of a larger research project, and had the opportunity to ask questions about the BISEP. This was done by the first author (LR) at the NWBIS, Bangor University, or patients’ homes. Group members had no therapeutic contact with the programme facilitator outside BISEP. The psycho-education and skills-based intervention forms a seven session programme, where members meet once a week for two hours. It is run by a main facilitator (the first author, LR) and a co-facilitator (an additional member of the clinical team, which was held constant as much as possible). BISEP topics include an introductory session, and sessions on anatomy and mechanisms of injury, emotional changes, emotion regulation, memory, problem solving, and fatigue. Patients receive handouts to provide structure, and each session involves a mixture of formal learning, compensatory strategies, skill building, and group discussions. The BISEP ends with a party and certificates, which the members help to organise.
Group members and the programme facilitator completed the TA questionnaires (WAI-S) following the last session, and the facilitator rated group members on their overall engagement. To encourage group members to answer honestly, they were informed that the facilitator would not see the data. A research intern anonymised data prior to analysis. Participants completed the Group Attitude Scale independently of their group members soon after (within two-weeks) programme completion.
2.4Design and data analysis
This non-experimental correlational design study used a series of robust multiple linear regressions, given the assumption of residual normality was not met. This was done using ‘R’ software, with the additional packages ‘Robustbse’, ‘Complmrob’, and ‘Stats’. Robust regressions were performed with ‘MM’ method (Salibián-Barrera, Aelst, & Willems, 2008), and bootstrapped coefficients from 999 bootstrapped samples (as a form of model validation) (Babyak, 2004; Efron, 2003). A number of separate regression models were carried out, with 1) demographic predictor variables (age and education), with 2) cognitive predictors (logical memory immediate recall, delayed memory recall, working memory, verbal ability, and inhibition), and with 3) emotional predictors (anxiety and depression scores). These were entered into regression models for 1) patient TA ratings, 2) programme facilitator (therapist) alliance ratings, and 3) group attitude scores as separate outcome variables. Additionally, a number of regression analyses were carried out for the outcome variable of patient engagement, with demographic, cognitive, and emotional predictors (as above), and an additional regression for alliance as predictors (patient ratings, therapist ratings, and group attitude). Missing data for one participant on the Group Attitude Scale was omitted.
3Results
The present study aimed to increase understanding of patient and facilitator perceptions of the strength of the alliance, in a short-term (seven week) psycho-education group programme, carried out at a community neurorehabilitation service (analysed under “The therapeutic alliance for group psycho-education”). A second aim was to investigate demographic, emotional, and cognitive predictors of the alliance and group attitude, as a way to identify potential barriers or facilitating factors (see “Predictors of the therapeutic alliance and group attitude”). A final aim was to explore potential predictors of patient engagement with the programme (demographic, emotional, cognitive, and alliance) (see “Predictors of patient engagement”). For descriptive statistics see Table 1.
Table 1
Descriptive Statistics
| Variable | M | SD | Mdn | Range |
| Age | 52.34 | 11.98 | 54.00 | 26–86 |
| Education | 13.57 | 2.14 | 13.00 | 10–20 |
| Anxiety (HADS) | 11.20 | 3.46 | 11.00 | 4–18 |
| Depression (HADS) | 9.14 | 3.79 | 8.50 | 2–16 |
| Inhibition (Hayling task) | 4.70 | 1.83 | 5.00 | 1–8 |
| Verbal fluency (D-KEFS) | 6.82 | 3.62 | 6.00 | 1–19 |
| Working memory (Digits WAIS) | 7.18 | 2.62 | 7.50 | 3–13 |
| Logical memory 1 (WMS) | 6.18 | 2.81 | 5.00 | 1–11 |
| Logical memory 2 (WMS) | 5.68 | 2.84 | 6.00 | 1–11 |
| Patient TA ratings | 73.30 | 9.36 | 74.50 | 52–84 |
| Therapist alliance ratings | 67.45 | 7.63 | 69.00 | 46–82 |
| Group attitude ratings | 156.05 | 16.27 | 157.50 | 120–180 |
| Engagement | 3.41 | 1.25 | 4.00 | 1–5 |
3.1The therapeutic alliance for group psycho-education
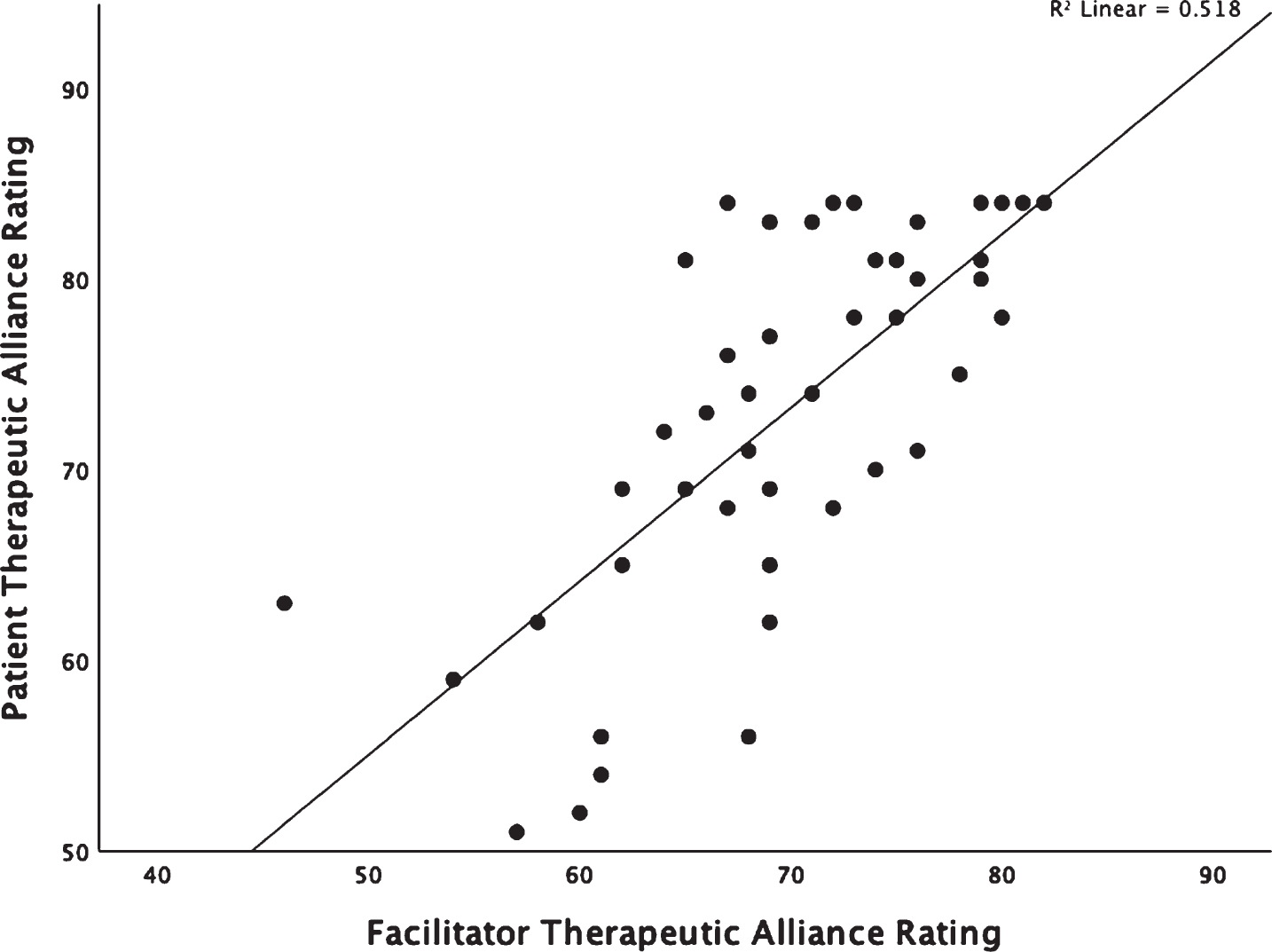
Patient and facilitator perceptions of the strength of the alliance was high overall, with a median rating of 74.50 for patients, and 69 for facilitators (from a maximum of 84). No rating was below 52 (patient ratings) and 46 (facilitator ratings). Importantly, 36% of the patients rated the alliance as 80 or above, with 16% of those as rating the alliance as the highest possible (84/84). The percentage of facilitator ratings above 80 was less high (9%). For patient ratings, over 50% of the sample reported their perceptions of the strength of the alliance to be over 74, and for the facilitator ratings over 50% were higher than 69. Patient ratings of the strength of the TA were significantly higher than facilitator ratings (Z = –2.787, p = .005). Importantly, patient and facilitator ratings were strongly correlated (r = .71, p < .001, see Fig. 1). The results indicate that a strong alliance can be achieved within the context of a short-term group rehabilitation programme.
Fig. 1
Scatter plot demonstrating the correlation between patient and facilitator perceptions of the strength of the alliance.
3.2Predictors of the therapeutic alliance and group attitude
3.2.1Patient perceptions of the alliance
Three robust regression models were carried out (for demographic, cognitive, and emotional predictors), see Table 2 for details. According to these models, demographic variables (age and education), cognitive (inhibition, working memory, verbal fluency, memory 1 and 2), and emotional (anxiety and depression) predictor variables provide a very low explanation of variance of the patient TA ratings, and none significantly improve prediction.
Table 2
Robust Multiple Linear Regression results for the patient therapeutic alliance ratings (outcome variable)
| Model | R2 | F | p (sig.) | β coefficients (bootstrapped) | p (sig.) | 95% CIs |
| Demographic predictor variables | 0.05 | 2.28 | 0.321 | |||
| Age | –0.01 | 0.475 | –0.25 –0.24 | |||
| Education | 1.07 | 0.083 | –0.63 –2.49 | |||
| Cognitive predictor variables | 0.14 | 5.96 | 0.310 | |||
| Inhibition | –0.83 | 0.174 | –2.59 –1.05 | |||
| Working memory | –0.42 | 0.313 | –1.82 –1.17 | |||
| Verbal fluency | –0.44 | 0.167 | –1.38 –0.56 | |||
| Memory 1 | –1.58 | 0.153 | –3.91 –1.55 | |||
| Memory 2 | 1.77 | 0.144 | –1.44 –4.30 | |||
| Emotional predictor variables | 0.06 | 2.42 | 0.300 | |||
| Anxiety | –0.02 | 0.501 | –1.01 –1.04 | |||
| Depression | –0.65 | 0.076 | –1.63 –0.23 |
Data is presented for three regression models containing 1) demographic predictor variables, 2) cognitive predictor variables, and 3) emotional predictor variables. * < .05 ** < .001.
3.2.2Therapist perceptions of the alliance
For the facilitator’s ratings, the model containing emotional predictor variables (anxiety and depression) explained 16% of the variance, and significantly improved prediction of the facilitator’s perceptions of the strength of the TA (R2 = 0.16, F(2,44) = 17.11, p < 0.001). Bootstrapped coefficients demonstrated that depression scores (HADS) were the only significant predictor within the model (β= –0.83, p = 0.002), and that a unit increase in depression scores would result in a 0.83 decrease in facilitator TA ratings.
The models with demographic, and cognitive, predictor variables did not significantly improve prediction of TA compared to using the mean alone. See Table 3 for further details. The results indicate that cognitive impairment is no barrier to developing a working alliance. This important issue is addressed in the Discussion.
Table 3
Robust Multiple Linear Regression results for the facilitator therapeutic alliance ratings (outcome variable)
| Model | R2 | F | p (sig.) | β coefficients (bootstrapped) | p (sig.) | 95% CIs |
| Demographic predictor variables | 0.00 | 0.17 | 0.921 | |||
| Age | –0.02 | 0.413 | –0.19 –0.22 | |||
| Education | 0.24 | 0.381 | –0.09 –1.38 | |||
| Cognitive predictor variables | 0.11 | 4.16 | 0.526 | |||
| Inhibition | 0.22 | 0.442 | –1.18 –1.47 | |||
| Working memory | –0.76 | 0.074 | –1.29 –0.37 | |||
| Verbal fluency | –0.27 | 0.261 | –0.27 –0.64 | |||
| Memory 1 | –0.53 | 0.285 | –0.53 –1.39 | |||
| Memory 2 | 0.58 | 0.284 | 0.58 –2.24 | |||
| Emotional predictor variables | 0.16 | 17.11 | <.001** | |||
| Anxiety | 0.24 | 0.176 | 0.24 –0.82 | |||
| Depression | –0.83 | 0.002* | –0.83 ––0.33 |
Data is presented for three regression models containing 1) demographic predictor variables, 2) cognitive predictor variables, and 3) emotional predictor variables. * < .05 ** < .001.
3.2.3Group attitude
The regression model which explained most variance was that containing the emotional predictor variables (anxiety and depression). This model explained 14% of the variance, and significantly improved prediction of group attraction, compared to using the mean alone (R2 = 0.14, F(2,44) = 9.48, p = 0.008). The results suggest that depression scores were the only significant predictor within the model (β= –1.61, p = 0.006), suggesting that a unit increase in depression scores would result in a 1.61 decrease in participants’ ‘attraction’ to their group (group attitude scale).
No other regression model significantly improved prediction of participants’ scores on the group attitude scale (demographic predictor model: p = 0.249; cognitive predictor model: p = 0.340). Verbal fluency was, however, a marginally significant predictor within the cognitive model (β= –1.57, p = 0.049), suggesting it may play a small role (See Table 4 for details). No demographic predictors and most cognitive factors did not predict group attitude; however, depression was a substantial contributor. Again, this issue is raised in the Discussion.
Table 4
Robust Multiple Linear Regression results for patients’ scores on the Group Attitude Scale (outcome variable)
| Model | R2 | F | p (sig.) | β coefficients (bootstrapped) | p (sig.) | 95% CIs |
| Demographic predictor variables | 0.03 | 2.78 | 0.249 | |||
| Age | 0.26 | 0.269 | –0.50 –0.26 | |||
| Education | 1.43 | 0.061 | –0.65 –3.21 | |||
| Cognitive predictor variables | 0.11 | 5.66 | 0.340 | |||
| Inhibition | –0.03 | 0.425 | –4.40 –3.57 | |||
| Working memory | 0.27 | 0.456 | –2.79 –4.30 | |||
| Verbal fluency | –1.57 | 0.049* | –3.25 –0.33 | |||
| Memory 1 | –0.44 | 0.428 | –5.16 –5.00 | |||
| Memory 2 | 1.31 | 0.344 | –5.34 –6.93 | |||
| Emotional predictor variables | 0.14 | 9.48 | 0.008* | |||
| Anxiety | –0.06 | 0.515 | –1.14 –1.31 | |||
| Depression | –1.61 | 0.006* | –2.76 ––0.54 |
Data is presented for three regression models containing 1) demographic predictor variables, 2) cognitive predictor variables, and 3) emotional predictor variables. * < .05 ** < .001.
3.3Predictors of patient engagement
Four robust regression models were carried out to investigate demographic, cognitive, emotional, and alliance predictors of patient engagement with the programme. The results demonstrated that the demographic predictor model (containing age and education) explained 14% of the variance (as rated by the facilitator), and significantly improved prediction of patient engagement (R2 = 0.14, F(2,44) = 7.84, p = 0.020). Patients’ years in education was the only significant predictor within the model (β= 0.22, p = 0.005), suggesting that a 1 year increase in education would result in a 0.22 increase in (the 5-point) engagement scores.
The regression model containing the cognitive predictors (inhibition, working memory, verbal fluency, immediate memory recall, and delayed memory recall) explained 19% of the variance, and significantly improved prediction of patient engagement (R2 = 0.19, F(5,44) = 13.49, p = 0.019). Working memory was a significant predictor within the model (β= 0.18, p = 0.018), suggesting that a unit increase in working memory would again result in a substantial 0.18 increase in engagement. Interestingly, immediate memory recall was a significant positive predictor of engagement (β= 0.29, p = 0.033), whereas delayed recall was a significant negative predictor (β= –0.26, p = 0.037). This suggests that a unit increase in immediate memory recall would result in a 0.29 increase in engagement, but a unit increase in delayed memory recall would result in a 0.26 decrease in engagement.
The model containing emotional and alliance predictors did not significantly improve prediction of engagement, and had low explanation of variance (See Table 5). These results are clearly both clinically useful and complex, and are interpreted in the Discussion.
Table 5
Robust Multiple Linear Regression results for patient engagement (outcome variable)
| Model | R2 | F | p (sig.) | β coefficients (bootstrapped) | p (sig.) | 95% CIs |
| Demographic predictor variables | 0.14 | 7.84 | 0.020* | |||
| Age | –0.02 | 0.189 | –0.05 –0.02 | |||
| Education | 0.22 | 0.005* | 0.06 –0.39 | |||
| Cognitive predictor variables | 0.19 | 13.49 | 0.019* | |||
| Inhibition | –0.11 | 0.127 | 1.42 –4.36 | |||
| Working memory | 0.18 | 0.018* | 0.02 –0.33 | |||
| Verbal fluency | –0.07 | 0.121 | –0.20 –0.05 | |||
| Memory 1 | 0.29 | 0.033* | –0.01 –0.49 | |||
| Memory 2 | –0.26 | 0.037* | –0.48 –0.03 | |||
| Emotional predictor variables | 0.02 | 1.00 | 0.610 | |||
| Anxiety | 0.04 | 0.302 | –0.09 –0.16 | |||
| Depression | –0.04 | 0.196 | –0.16 –0.06 | |||
| Alliance and group attitude predictor variables | 0.21 | 5.90 | 0.116 | |||
| Patient alliance ratings | 0.01 | 0.407 | –0.07 –0.08 | |||
| Facilitator alliance ratings | 0.05 | 0.108 | –0.03 –0.12 | |||
| Group attitude scores | 0.01 | 0.206 | –0.02 –0.04 |
Data is presented for four regression models containing 1) demographic predictor variables, 2) cognitive predictor variables, 3) emotional predictor variables, and 4) therapeutic alliance and group attitude predictor variables. * < .05 ** < .001.
4Discussion
4.1A strong alliance can be developed surprisingly quickly
Importantly, these findings suggest that a strong TA can be achieved in a short-term group psycho-education programme. This conclusion stems from the observation that 50% of alliance ratings were over 74 (patient ratings) and 69 (therapist ratings). As discussed above, previous work has focused mainly on intense holistic rehabilitation (Stagg et al., 2019, for a review). This finding, in a short-term group programme, is consistent with the idea that the alliance is relevant across settings involving a process of change (Bordin, 1979), especially for patient perceptions.
Previous work has suggested that the strength of alliance is dependent upon the quantity of therapeutic contact, and develops over time (Schönberger et al., 2006c). The present study’s findings suggest that a strong TA can be developed over 7 short sessions. It may, therefore, be the quality of the therapeutic contact that is most important (Bishop et al., 2019; Lawton et al., 2016). In addition, an essential component of the therapeutic relationship is person-centredness (Bishop et al., 2019; Lawton et al., 2016), something which may have been considered difficult to achieve in a group setting. These findings suggest that this is not the case, and providing rehabilitation in a group setting is not necessarily a barrier to developing an alliance with the members. It has been suggested that this effect is due to a clinician’s skill in recognising variability among patients, and tailoring their approach accordingly (Bishop et al., 2019; McCormack, Karlsson, Dewing, & Lerdal, 2010). These results should be encouraging for all those who engage in short-term group rehabilitation programmes.
4.2Cognitive and demographic variables are not predictors of alliance
Another important finding is that demographic and cognitive variables do not appear to influence the strength of the alliance (for facilitator or patient perceptions), or the patients’ ‘attraction’ towards their group. Similar to previous studies, this finding suggests that age (Sherer et al., 2007) and education (Zelencich et al., 2019), do not pose a barrier to developing a strong therapeutic relationship with ABI survivors. This can only be seen as a positive for rehabilitation, because of the wide range of brain injury demography: young adults and the elderly, and all levels of education.
Surprisingly, no cognitive factors were identified as having an influence on patient or therapist perceptions of the TA, in contrast to qualitative accounts (Judd & Wilson, 2005). This particular finding contributes to an emerging picture in the quantitative literature, that cognitive impairments in the ABI population do not necessarily pose a challenge in developing a therapeutic relationship (Stagg et al., 2019; Zelencich et al., 2019). Of particular relevance for this idea is a recent detailed description of the inter-personal psychotherapeutic process, which remains intact with a profoundly amnesic patient (Moore, Salas, Dockree, & Turnbull, 2017). The facilitator’s skills in circumventing cognitive difficulties (Judd & Wilson, 2005; Schönberger et al., 2007), and specific elements of BISEP (e.g. handouts and prompts) (Judd & Wilson, 2005), may also play a part.
Additionally, no cognitive factor was found to play a role in participants’ ‘attraction’ towards their group. It is important to note that this specific measure captures important elements of the group interaction, such as relating to the experiences of other group members, and a feeling of unity (Evans & Jarvis, 1986). One may have expected cognitive difficulties to negatively impact this group element, given their substantial role in social skills (Muscara, Catroppa, & Anderson, 2008; Salas, Casassus, Rowlands, Pimm, & Flanagan, 2018), and psycho-social outcomes (Draper, Ponsford, & Schönberger, 2007). However, given that cognitive impairment is often a feature of a brain injury, and an element which unites the group members, participants likely did not see this as a barrier (Salas et al., 2018). The high scores on this measure indicate that participants are not only able to relate to one another, but that they also enjoyed the group experience, regardless of age, education, and cognitive abilities.
It is noteworthy that a number of qualitative factors, not investigated in the present study, might play a part in the alliance (Lawton et al., 2016 for review), and group ‘attraction’. For example, the fostering of a personal connection, humour, empathy (Bishop et al., 2019), trust, and being treated as an individual (Lawton et al., 2016 for review). Considered together, it is possible that a number of personal and professional characteristics, independent of injury-related factors, underlie these complex therapeutic processes. Again, these findings are encouraging for those who work with patients from a range of demographic backgrounds, with cognitive impairment.
4.3Depression is a significant predictor, but not in all cases
A key finding is that depression scores negatively predicted firstly, the facilitator perceptions of the alliance, and may, therefore, be a barrier to developing a strong therapeutic relationship. This idea is consistent with previous findings (Evans et al., 2008), and qualitative evidence, which suggests that ‘emotional difficulties’ are often a challenge to developing an alliance (Judd & Wilson, 2005). It is widely acknowledged that emotional distress can impact on processes important in rehabilitation (Coetzer et al., 2018), such as motivation (Siegert & Taylor, 2004) and appraisals of impairment (Byrne, Coetzer, & Addy, 2017). The present study’s findings extend this idea, by providing direct evidence that depression also negatively impacts the development of the TA.
What might explain this effect? Referring back to Bordin’s pantheoretical framework (1979), it is possible that depression may have affected the dimensions of the TA differentially. For instance, depression may have influenced the more active components of the TA, such as agreement on tasks and goals. Notably, depression symptomology may decrease motivation and self-efficacy (Maddux & Meier, 1995; Smith, 2013), and in turn may make participants more passive in task agreement (Gibbon, 2004; Lawton et al., 2016 for a review; Rhode, Townley-O’Neill, Trendall, Worrall, & Cornwell, 2012). Interestingly, depression was not predictive of patients’ perceptions of the alliance, possibly due to poor awareness (Prigatano, 2005), or general positive perceptions leading to high ratings within a narrow range.
A second finding on this topic is that depression also negatively predicted participants’ ‘attraction’ towards their group. It has been long acknowledged that emotional distress can play a role in social functioning (Gainotti, 1993; Morton & Wehman, 1995; Weddel, Oddy, & Jenkins, 1980). Within the context of rehabilitation programmes, depression may impact upon the group dynamic in a number of ways. Firstly, high depression symptomology may lead to a negative bias (Peckham, McHugh, & Otto, 2010; Watkins, Vache, Verney, Muller, & Mathews, 1996), whereby participants’ overall views of the group experience may be influenced by a preoccupation with instances of negative interactions. Secondly, as previously mentioned, depression may lead to poor motivation (Smith, 2013) to connect with the group. A final issue is how depression might compromise a person’s sense of identity (Cruwys, Haslam, Dingle, Haslam, & Jetten, 2014). Due to a sense of threat to the self, a person might use maladaptive strategies, such as avoidance, as a way of coping (Riley, Brennan, & Powell, 2004). That is, they may stay on the outskirts of the group, and avoid becoming actively involved in relational elements that are important for developing a strong group bond (e.g. discussions, activities, sharing their own stories). This has important clinical implications as discussed below.
4.4Education is the biggest predictor of engagement
Within neurorehabilitation, a person’s level of education has been identified as a factor which positively influences outcome (Ponsford, Draper, & Schönberger 2008), including employment and fewer depressive symptoms (Whelan-Goodinson, Ponsford, Schönberger, & Johnston, 2010). It is, therefore, not surprising that the findings suggest that higher levels of education are also predictive of engagement, consistent with previous research in acute inpatient rehabilitation (Ramanathan-Elion, McWhorter, Wegener, & Bechtold, 2016).
The majority of studies of rehabilitation engagement have investigated the role of psychological variables, such as hope and denial (Ramanathan-Elion et al., 2016), but factors contributing to this process remain poorly understood. Lequerica and Kortte (2010) provide a useful model, whereby engagement is dependent upon interacting personal and environmental factors. The present study’s findings suggest that the level of education may also play a part in the underlying factors, possibly through perceived self-efficacy (Lequerica & Kortte, 2010). It is, therefore, important for clinicians to actively promote engagement in group members with lower levels of education.
4.5Some cognitive abilities are important for engagement
Another key finding is that aspects of cognition are important for engagement. Though this area of research is in its infancy, these findings are in line with previous research on participation in rehabilitation, a related and overlapping construct to engagement (Skidmore, Whyte, Holm, Becker, et al., 2010). This presumably relates to the idea that cognitive impairment presents a hindrance to engaging in every-day life, and in social adjustment (Salas et al., 2018).
Of the cognitive factors explored, the present study is the first to demonstrate that good working memory significantly predicted higher levels of engagement (c.f. Skidmore et al., 2010). One can see why intact levels of this limited-capacity ability would be beneficial within the context of a group psycho-education programme, where one must follow the content, listen to the group members’ accounts, take part in programme activities, all the while keeping track of the overall narrative of each session (Mcallister, Flashman, Sparling, & Saykin, 2004, for a review). When this system becomes overloaded, participants may well disengage from the sessions, as a way to avoid a catastrophic reaction (Goldstein, 1965; Salas, 2012). The findings suggest that those with marked working memory difficulties might need additional support to maintain engagement.
A peculiar finding is related to episodic memory (Logical Memory, WAIS). The present study suggests that poorer immediate memory recall is predictive of lower engagement, but poorer delayed memory recall is predictive of higher engagement. For the former, it is likely that those who cannot remember the content as it progresses during each session may disengage. A possible explanation for the latter is that patients who are aware of delayed memory impairment may engage more during future sessions in an attempt to compensate. Previous work by Schönberger et al (2007) found that poorer memory was associated with better patient perceptions of the alliance. It is possible that this too was due to increased engagement with the therapeutic process. It is not easy to interpret these complex findings, but encouraging patients to take notes, and providing information in ‘bite sized’ chunks, would be practical suggestions to promote engagement.
4.6Therapeutic alliance may not predict engagement
The therapeutic alliance was not a predictor of engagement in the present study. However, this stands in sharp contrast to previous qualitative work, which have described the therapists as having a ‘pivotal’ role in encouraging patient engagement, and that the alliance might be a mechanism by which to promote participation (Bright et al., 2015; Lawton et al., 2016, for reviews). It is likely that, in a group setting, engagement is dependent on personal characteristics (e.g. education), psychological factors, and the programme itself, more so than the therapeutic relationship. Engagement is a complex phenomenon. To better understand the process it is important to use both quantitative and qualitative approaches from the same data set. This seems to be the most sensible way forwards, because at the moment these methods seem to be producing different results. In addition, future work may benefit from following more closely a model of therapeutic engagement (e.g. Lequerica & Kortte, 2010).
4.7Future directions
A possible limitation of the present study is that the focus upon the overall alliance prevents more detailed analysis of the three underlying dimensions, especially as these develop over multiple time points. As regards cognitive skills, a variable which may be important to consider in future studies is sustained attention (Leclercq, Deloche, & Rousseaux, 2002). This impairment, commonly described as distractibility, might play a role in participants’ engagement with rehabilitation programmes and with the therapeutic relationship (Schönberger et al., 2007). Finally, future work will benefit from investigating the importance of the alliance for the outcomes of group rehabilitation programmes.
4.8Implications for neurorehabilitation
The present study has several implications for rehabilitation professionals, of which the most important may be that cognitive impairment following ABI does not pose a barrier to developing an alliance with their clients. The relevance of depression symptomology is also a clinically important finding, and suggests that rehabilitation professionals should identify those vulnerable to poorer alliance and group connection. Facilitators can then pay extra attention to participants with high levels of depression, and provide scaffolding and encouragement to help them with tasks and activities. Additionally, clinicians may need to actively help such patients to bond with the group, by drawing them into group discussions, and help them move past maladaptive ways of coping (e.g. avoidance, as discussed above) (Riley et al., 2004). Professionals may wish to tailor their approach according to known factors contributing to engagement, especially lower levels of education, poorer working memory skills, and poorer episodic memory.
4.9Conclusion
The findings demonstrate that a good alliance can be achieved despite short duration, demographic variation, and cognitive impairment. Some barriers to the alliance, patient engagement, and group ‘attraction’ have, however, been identified. The present study provides direct evidence that depression negatively influences the strength of the alliance, and participants’ ‘attraction’ towards their group. To promote engagement, clinicians may need to provide additional support to patients with lower levels of education, working memory, and episodic memory impairment. We have suggested practical solutions which can address these challenges. Given the financial and workload advantages of short-term group interventions, these positive findings encourage the continued use of group programmes for neurorehabilitation services.
Conflict of interest
The authors have no conflict of interest to disclose.
Acknowledgments
This study was supported by EU Social Fund through the Welsh Government. We would like to thank all the participants and staff at the North Wales Brain Injury Service. Our gratitude also goes to patients’ friends and family, and the Welsh Ambulance Service Non-Emergency Transport, for driving the participants to the psycho-education sessions.
References
1 | Anson, K. , & Ponsford, J. ((2006) ). Evaluation of a coping skills group following traumatic brain injury. Brain Injury 20: (2), 167–178. DOI: 10.1080/02699050500442956 |
2 | Babyak, M. A. ((2004) ). What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosomatic medicine 66: (3), 411–421. |
3 | Backhaus, S. L. , Ibarra, S. L. , Klyce, D. , Trexler, L. E. , & Malec, J. F. ((2010) ). Brain injury coping skills group: a preventative intervention for patients with brain injury and their caregivers. Archives of physical medicine and rehabilitation 91: (6), 840–848. DOI: 10.1016/j.apmr.2010.03.015 |
4 | Bishop, M. , Kayes, N. , & McPherson, K. ((2019) ). Understanding the therapeutic alliance in stroke rehabilitation. Disability and rehabilitation 1–10. DOI: 10.1080/09638288.2019.1651909 |
5 | Bordin, E. S. ((1979) ). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, research & practice 16: (3), 252. DOI: 10.1037/h0085885 |
6 | Bright, F. A. , Kayes, N. M. , Cummins, C. , Worrall, L. M. , & McPherson, K. M. ((2017) ). Co-constructing engagement in stroke rehabilitation: a qualitative study exploring how practitioner engagement can influence patient engagement. Clinical rehabilitation 31: (10), 1396–1405. DOI: 10.1177/0269215517694678 |
7 | Bright, F. A. , Kayes, N. M. , Worrall, L. , & McPherson, K. M. ((2015) ). A conceptual review of engagement in healthcare and rehabilitation. Disability and rehabilitation 37: (8), 643–654. DOI: 10.3109/09638288.2014.933899 |
8 | Burgess, P. W. , & Shallice, T. ((1997) ). The Hayling and Brixton tests. Thurston, Suffolk: Thames Valley Test Company. |
9 | Byrne, C. , Coetzer, R. , & Addy, K. ((2017) ). Investigating the discrepancy between subjective and objective cognitive impairment following acquired brain injury: The role of psychological affect. NeuroRehabilitation 41: (2), 501–512. DOI: |
10 | Coetzer, B. R. , Vaughan, F. L. , Roberts, C. B. , & Rafal, R. ((2003) ). The development of a holistic, community-based neurorehabilitation service in a rural area. Journal of Cognitive Rehabilitation 21: (1), 4–15. |
11 | Coetzer, R. ((2008) ). Holistic neuro-rehabilitation in the community: Is identity a key issue? Neuropsychological Rehabilitation 18: (5-6), 766–783. DOI: 10.1080/09602010701860266 |
12 | Coetzer, R. , Roberts, C. , Turnbull, O. H. , & Vaughan, F. L. ((2018) ). Neuropsychoanalytically informed psychotherapy approaches to rehabilitation: The North Wales Brain Injury Service–Bangor University experience 1998–2018. Neuropsychoanalysis 20: (1), 3–13. DOI: 10.1080/15294145.2018.1478747 |
13 | Colantonio, A. , Ratcliff, G. , Chase, S. , Kelsey, S. , Escobar, M. , & Vernich, L. ((2004) ). Long term outcomes after moderate to severe traumatic brain injury. Disability and Rehabilitation 26: (5), 253–261. DOI: 10.1080/09638280310001639722 |
14 | Comper, P. , Bisschop, S. M. , Carnide, N. , & Tricco, A. ((2005) ). A systematic review of treatments for mild traumatic brain injury. Brain injury 19: (11), 863–880. |
15 | Couchman, G. , McMahon, G. , Kelly, A. , & Ponsford, J. ((2014) ). A new kind of normal: qualitative accounts of multifamily group therapy for acquired brain injury. Neuropsychological rehabilitation 24: (6), 809–832. DOI: 10.1080/09602011.2014.912957 |
16 | Crowe, T. P. , & Grenyer, B. F. ((2008) ). Is therapist alliance or whole group cohesion more influential in group psychotherapy outcomes? Clinical Psychology & Psychotherapy 15: (4), 239–246. DOI: 10.1002/cpp.583 |
17 | Cruwys, T. , Haslam, S. A. , Dingle, G. A. , Haslam, C. , & Jetten, J. ((2014) ). Depression and social identity: An integrative review. Personality and Social Psychology Review 18: (3), 215–238. DOI: 10.1177/1088868314523839 |
18 | Dawkins, N. , Cloherty, M. E. , Gracey, F. , & Evans, J. J. ((2006) ). The factor structure of the Hospital Anxiety and Depression Scale in acquired brain injury. Brain injury 20: (12), 1235–1239. DOI: 10.1080/02699050601076414 |
19 | Delis, D. C. , Kaplan, E. , & Kramer, J. H. ((2001) ). Delis-Kaplan Executive function system: examiners manual. Psychological Corporation. |
20 | Department of Health. ((2005) ). National service framework for long term conditions. London: Fact Department of Health. |
21 | Draper, K. , Ponsford, J. , & Schönberger, M. ((2007) ). Psychosocial and emotional outcomes 10 years following traumatic brain injury. The Journal of head trauma rehabilitation 22: (5), 278–287. DOI: 10.1097/01.HTR.0000290972.63753.a7 |
22 | Draper, K. , Ponsford, J. , & Schönberger, M. ((2007) ). Psychosocial and emotional outcomes 10 years following traumatic brain injury. The Journal of head trauma rehabilitation 22: (5), 278–287. DOI: 10.1097/01.HTR.0000290972.63753.a7 |
23 | Efron, B. ((2003) ). Second thoughts on the bootstra. Statistical Science 18: (2), 135–140. |
24 | Ergh, T. C. , Rapport, L. J. , Coleman, R. D. , & Hanks, R. A. ((2002) ). Predictors of caregiver and family functioning following traumatic brain injury: Social support moderates caregiver distress. The Journal of head trauma rehabilitation 17: (2), 155–174. |
25 | Evans, C. C. , Sherer, M. , Nakase-Richardson, R. , Mani, T. , & Irby J. W. Jr, ((2008) ). Evaluation of an Interdisciplinary Team Intervention to Improve Therapeutic Alliance in Post–acute Brain Injury Rehabilitation. The Journal of head trauma rehabilitation 23: (5), 329–338. DOI: 10.1097/01.HTR.0000336845.06704.bc |
26 | Evans, N. J. , & Jarvis, P. A. ((1986) ). The group attitude scale: A measure of attraction to group. Small Group Behavior 17: (2), 203–216. DOI: 10.1177/104649648601700205 |
27 | Ferreira, P. H. , Ferreira, M. L. , Maher, C. G. , Refshauge, K. M. , Latimer, J. , & Adams, R. D. ((2013) ). The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Physical therapy 93: (4), 470–478. DOI: 10.2522/ptj.20120137 |
28 | Gainotti, G. ((1993) ). Emotional and psychosocial problems after brain injury. Neuropsychological rehabilitation 3: (3), 259–277. DOI: 10.1080/09602019308401440 |
29 | Gibbon, B. ((2004) ). Service User Involvement: The impact of stroke and the meaning of rehabilitation (part 1) Service User Involvement: Key Contributors, Goal Setting and Discharge Home (part 2). JARNA 7: (2), 8–12. |
30 | Goldstein, K. ((1965) ). The Organism. NewYork: Zone Books, (1995) |
31 | Hall, A. M. , Ferreira, P. H. , Maher, C. G. , Latimer, J. , & Ferreira, M. L. ((2010) ). The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Physical therapy 90: (8), 1099–1110. DOI: 10.2522/ptj.20090245 |
32 | Henry, J. D. , & Crawford, J. R. ((2004) ). A meta-analytic review of verbal fluency performance in patients with traumatic brain injury. Neuropsychology 18: (4), 621. DOI: 10.1037/0894-4105.18.4.621 |
33 | Hiott, D. W. , & Labbate, L. ((2002) ). Anxiety disorders associated with traumatic brain injuries. NeuroRehabilitation 17: (4), 345–355. DOI: |
34 | Horvath, A. O. , & Greenberg, L. S. ((1989) ). Development and validation of the Working Alliance Inventory. Journal of counseling psychology 36: (2), 223. DOI: 10.1037/0022-0167.36.2.223 |
35 | Horvath, A. O. , & Luborsky, L. ((1993) ). The role of the therapeutic alliance in psychotherapy. Journal of consulting and clinical psychology 61: (4), 561. DOI: 10.1037/0022-006X.61.4.561 |
36 | Horvath, A. O. , & Symonds, B. D. ((1991) ). Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of counseling psychology 38: (2), 139. DOI: 10.1037/0022-0167.38.2.139 |
37 | Jorge, R. E. , Robinson, R. G. , Moser, D. , Tateno, A. , Crespo-Facorro, B. , & Arndt, S. ((2004) ). Major depression following traumatic brain injury. Archives of general psychiatry 61: (1), 42–50. DOI: 10.1001/archpsyc.61.1.42 |
38 | Judd, D. , & Wilson, S. L. ((2005) ). Psychotherapy with brain injury survivors: An investigation of the challenges encountered by clinicians and their modifications to therapeutic practice. Brain Injury 19: (6), 437–449. DOI: 10.1080/02699050400010994 |
39 | Klonoff, P. S. , Lamb, D. G. , & Henderson, S. W. ((2001) ). Outcomes from milieu-based neurorehabilitation at up to 11 years post-discharge. Brain Injury 15: (5), 413–428. DOI: 10.1080/02699050116744 |
40 | Kreutzer, J. S. , Seel, R. T. , & Gourley, E. ((2001) ). The prevalence and symptom rates of depression after traumatic brain injury: a comprehensive examination. Brain injury 15: (7), 563–576. DOI: 10.1080/02699050116884 |
41 | Krug, E. , & Cieza, A. ((2019) ). Strengthening health systems to provide rehabilitation services. Neuropsychological rehabilitation 29: (5), 672–674. DOI: 10.1080/09602011.2017.1319391 |
42 | Lawton, M. , Haddock, G. , Conroy, P. , & Sage, K. ((2016) ). Therapeutic alliances in stroke rehabilitation: A meta-ethnography. Archives of Physical Medicine and Rehabilitation 97: (11), 1979–1993. DOI: 10.1016/j.apmr.2016.03.031 |
43 | Leclercq, M. , Deloche, G. , and Rousseaux, M. ((2002) ). “Attentional complaints evoked by traumatic brain injured and stroke patients: frequency and importancy,” in Applied Neuropsychology of Attention: Theory, Diagnosis and Rehabilitation, eds M. Leclercq and P. Zimmermann (London: Psychology Press), 89–109 |
44 | Lenze, E. J. , Munin, M. C. , Quear, T. , Dew, M. A. , Rogers, J. C. , Begley, A. E. , & Reynolds C. F. III, ((2004) ). Significance of poor patient participation in physical and occupational therapy for functional outcome and length of stay. Archives of physical medicine and rehabilitation 85: (10), 1599–1601.DOI: 10.1016/j.apmr.2004.03.027 |
45 | Lequerica, A. H. , & Kortte, K. ((2010) ). Therapeutic engagement: a proposed model of engagement in medical rehabilitation. American journal of physical medicine & rehabilitation 89: (5), 415–422. DOI: 10.1097/PHM.0b013e3181d8ceb2 |
46 | Levack, W. M. , Kayes, N. M. , & Fadyl, J. K. ((2010) ). Experience of recovery and outcome following traumatic brain injury: a metasynthesis of qualitative research. Disability and rehabilitation 32: (12), 986–999. DOI: 10.3109/09638281003775394 |
47 | Lundqvist, A. , Linnros, H. , Orlenius, H. , & Samuelsson, K. ((2010) ). Improved self-awareness and coping strategies for patients with acquired brain injury—A group therapy programme. Brain injury 24: (6), 823–832. DOI: 10.3109/02699051003724986 |
48 | Lustig, D. C. , Strauser, D. R. , Weems, G. H. , Donnell, C. M. , & Smith, L. D. ((2003) ). Traumatic brain injury and rehabilitation outcomes: does the working alliance make a difference? Journal of Applied Rehabilitation Counseling 34: (4), 30. Retrieved from https://search.proquest.com/docview/216473171?accountid=14874 |
49 | Maddux, J. E. , & Meier, L. J. ((1995) ). Self-efficacy and depression. In Self-Efficacy, adaptation, and adjustment (pp. 143-169). Springer, Boston, MA. |
50 | Martin, D. J. , Garske, J. P. , & Davis, M. K. ((2000) ). Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. Journal of consulting and clinical psychology 68: (3), 438. DOI: 10.1037/0022-006X.68.3.438 |
51 | Marziali, E. , Munroe-Blum, H. , & McCleary, L. ((1997) ). The contribution of group cohesion and group alliance to the outcome of group psychotherapy. International Journal of Group Psychotherapy 47: (4), 475–497. DOI: 10.1080/00207284.1997.11490846 |
52 | Mcallister, T. W. , Flashman, L. A. , Sparling, M. B. , & Saykin, A. J. ((2004) ). Working memory deficits after traumatic brain injury: catecholaminergic mechanisms and prospects for treatment—a review. Brain Injury 18: (4), 331–350. DOI: 10.1080/02699050310001617370 |
53 | McCormack, B. , Karlsson, B. , Dewing, J. , & Lerdal, A. ((2010) ). Exploring person-centredness: a qualitative meta-synthesis of four studies. Scandinavian Journal of Caring Sciences 24: (3), 620–634. DOI: 10.1111/j.1471-6712.2010.00814.x |
54 | Millis, S. R. , Rosenthal, M. , Novack, T. A. , Sherer, M. , Nick, T. G. , Kreutzer, J. S. ,... Ricker, J. H. ((2001) ). Long-term neuropsychological outcome after traumatic brain injury. The Journal of head trauma rehabilitation 16: (4), 343–355. |
55 | Moore, P. A. , Salas, C. E. , Dockree, S. , & Turnbull, O. H. ((2017) ). Observations on working psychoanalytically with a profoundly amnesic patient. Frontiers in psychology 8: , 1418. DOI: 10.3389/fpsyg.2017.01418 |
56 | Morton, M. V. , & Wehman, P. ((1995) ). Psychosocial and emotional sequelae of individuals with traumatic brain injury: a literature review and recommendations. Brain injury 9: (1), 81–92. DOI: 10.3109/02699059509004574 |
57 | Muscara, F. , Catroppa, C. , & Anderson, V. ((2008) ). Social problem-solving skills as a mediator between executive function and long-term social outcome following paediatric traumatic brain injury. Journal of neuropsychology 2: (2), 445–461.DOI: 10.1348/174866407X250820 |
58 | Odhuba, R. A. , Van den Broek, M. D. , & Johns, L. C. ((2005) ). Ecological validity of measures of executive functioning. British Journal of Clinical Psychology 44: (2), 269–278. DOI: 10.1348/014466505X29431 |
59 | Ownsworth, T. , & Fleming, J. ((2005) ). The relative importance of metacognitive skills, emotional status, and executive function in psychosocial adjustment following acquired brain injury. The Journal of head trauma rehabilitation 20: (4), 315–332. |
60 | Peckham, A. D. , McHugh, R. K. , & Otto, M. W. ((2010) ). A meta-analysis of the magnitude of biased attention in depression. Depression and anxiety 27: (12), 1135–1142. DOI: 10.1002/da.20755 |
61 | Peiris, C. L. , Taylor, N. F. , & Shields, N. ((2012) ). Patients value patient-therapist interactions more than the amount or content of therapy during inpatient rehabilitation: a qualitative study. Journal of Physiotherapy 58: (4), 261–268. DOI: 10.1016/S1836-9553(12)70128-5 |
62 | Ponsford, J. , Draper, K. , & Schönberger, M. ((2008) ). Functional outcome 10 years after traumatic brain injury: its relationship with demographic, injury severity, and cognitive and emotional status. Journal of the International Neuropsychological Society 14: (2), 233–242. DOI: 10.1017/S1355617708080272 |
63 | Ponsford, J. , Draper, K. , & Schönberger, M. ((2008) ). Functional outcome 10 years after traumatic brain injury: its relationship with demographic, injury severity, and cognitive and emotional status. Journal of the International Neuropsychological Society 14: (2), 233–242. DOI: 10.1017/S1355617708080272 |
64 | Prigatano, G. P. ((2005) ). Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: a 20-year perspective. The Journal of head trauma rehabilitation 20: (1), 19–29. |
65 | Ramanathan-Elion, D. M. , McWhorter, J. W. , Wegener, S. T. , & Bechtold, K. T. ((2016) ). The role of psychological facilitators and barriers to therapeutic engagement in acute, inpatient rehabilitation. Rehabilitation psychology 61: (3), 277. DOI: 10.1037/rep0000095 |
66 | Riley, G. A. , Brennan, A. J. , & Powell, T. ((2004) ). Threat appraisal and avoidance after traumatic brain injury: why and how often are activities avoided? Brain Injury 18: (9), 871–888. DOI: 10.1080/02699050410001671829 |
67 | Rohde, A. , Townley-O’Neill, K. , Trendall, K. , Worrall, L. , & Cornwell, P. ((2012) ). A comon of client and therapist goals for people with aphasia: A qualitative exploratory study. Aphasiology 26: (10), 1298–1315. DOI: 10.1080/02687038.2012.706799 |
68 | Rosti-Otajärvi, E. , Mäntynen, A. , Koivisto, K. , Huhtala, H. , & Hämäläinen, P. ((2014) ). Predictors and impact of the working alliance in the neuropsychological rehabilitation of patients with multiple sclerosis. Journal of the neurological sciences 338: (1-2), 156–161. DOI: 10.1016/j.jns.2013.12.039 |
69 | Salas, C. E. ((2012) ). Surviving catastrophic reaction after brain injury: the use of self-regulation and self-other regulation. Neuropsychoanalysis 14: (1), 77–92. DOI: 10.1080/15294145.2012.10773691 |
70 | Salas, C. E. , Casassus, M. , Rowlands, L. , Pimm, S. , & Flanagan, D. A. ((2018) ). Relating through sameness”: a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychological rehabilitation 28: (7), 1161–1178. DOI: 10.1080/09602011.2016.1247730 |
71 | Salas, C. E. , Casassus, M. , Rowlands, L. , Pimm, S. , & Flanagan, D. A. ((2018) ). Relating through sameness”: a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychological rehabilitation 28: (7), 1161–1178. DOI: 10.1080/09602011.2016.1247730 |
72 | Salibián-Barrera, M. , Van Aelst, S. , & Willems, G. ((2008) ). Fast and robust bootstrap. Statistical Methods and Applications 17: (1), 41–71. |
73 | Schönberger, M. , & Ponsford, J. ((2010) ). The factor structure of the Hospital Anxiety and Depression Scale in individuals with traumatic brain injury. Psychiatry research 179: (3), 342–349. DOI: 10.1016/j.psychres.2009.07.003 |
74 | Schönberger, M. , Humle, F. , Teasdale, T. W. , ((2006) b). Subjective outcome of brain injury rehabilitation in relation to the therapeutic working alliance, client compliance and awareness. Brain Injury 20: (12), 1271–1282. DOI: 10.1080/02699050601049395 |
75 | Schönberger, M. , Humle, F. , Teasdale, T. W. , ((2006) c). The development of the therapeutic working alliance, patients’ awareness and their compliance during the process of brain injury rehabilitation. Brain Injury 20: (4), 445–454. DOI: 10.1080/02699050600664772 |
76 | Schönberger, M. , Humle, F. , & Teasdale, T. W. ((2007) ). The relationship between clients’ cognitive functioning and the therapeutic working alliance in post-acute brain injury rehabilitation. Brain Injury 21: (8), 825–836. DOI: 10.1080/02699050701499433 |
77 | Schönberger, M. , Humle, F. , Zeeman, F. , & Teasdale, T. W. ((2006) a). Working alliance and patient compliance in brain injury rehabilitation and their relation to psychosocial outcome. Neuropsychological Rehabilitation 16: (3), 298–314. DOI: 10.1080/09602010500176476 |
78 | Sherer, M. , Evans, C. C. , Leverenz, J. , Stouter, J. , Irby J. W. Jr , Eun Lee, J. , & Yablon, S. A. ((2007) ). Therapeutic alliance in post-acute brain injury rehabilitation: predictors of strength of alliance and impact of alliance on outcome. Brain Injury 21: (7), 663–672. DOI: 10.1080/02699050701481589 |
79 | Siegert, R. J. , & Taylor, W. J. ((2004) ). Theoretical aspects of goal-setting and motivation in rehabilitation. Disability and rehabilitation 26: (1), 1–8. DOI: 10.1080/09638280410001644932 |
80 | Skidmore, E. R. , Whyte, E. M. , Holm, M. B. , Becker, J. T. , Butters, M. A. , Dew, M. A. ,... Lenze, E. J. ((2010) ). Cognitive and affective predictors of rehabilitation participation after stroke. Archives of physical medicine and rehabilitation 91: (2), 203–207. DOI: 10.1016/j.apmr.2009.10.026 |
81 | Smith, B. ((2013) ). Depression and motivation. Phenomenology and the Cognitive Sciences 12: (4), 615–635. DOI: 10.1007/s11097-012-9264-0 |
82 | Stagg, K. , Douglas, J. , & Iacono, T. ((2017) ). A scoping review of the working alliance in acquired brain injury rehabilitation. Disability and rehabilitation 41: (4), 489–497. DOI: 10.1080/09638288.2017.1396366 |
83 | Tracey, T. J. , & Kokotovic, A. M. ((1989) ). Factor structure of the working alliance inventory. Psychological Assessment: A journal of consulting and clinical psychology 1: (3), 207. DOI: doi:10.1037/1040-3590.1.3.207 |
84 | Tyerman, A. , & Hucker, R. ((2016) ). Community Brain Injury Rehabilitation Services Benchmarking Exercise. Buckinghamshire Healthcare NHS Trust: United Kingdom |
85 | Watkins, P. C. , Vache, K. , Verney, S. P. , Muller. S. , & Mathews, A. ((1996) ). Unconscious mood-congruent memory bias in depression. Journal of Abnormal Psychology 105: (3), 4. |
86 | Wechsler, D. ((2008) ). Wechsler Adult Intelligence Scale–Fourth Edition (WAIS–IV). San Antonio, TX: The Psychological Corporation. |
87 | Wechsler, D. ((2009) ). Wechsler Memory Scale–Fourth Edition, San Antonio, TX: Pearson. |
88 | Weddell, R. , Oddy, M. , & Jenkins, D. ((1980) ). Social adjustment after rehabilitation: a two year follow-up of patients with severe head injury. Psychological Medicine 10: (2), 257–263. DOI: 10.1017/S0033291700044019 |
89 | Whelan-Goodinson, R. , Ponsford, J. L. , Schönberger, M. , & Johnston, L. ((2010) ). Predictors of psychiatric disorders following traumatic brain injury. The Journal of head trauma rehabilitation 25: (5), 320–329. DOI: 10.1097/HTR.0b013e3181c8f8e7 |
90 | World Health Organization. ((2014) ). WHO methods and data sources for country-level causes of death 2000–2012. Geneva, Switzerland: WHO. |
91 | Yalom, I. D. , & Rand, K. ((1966) ). Compatibility and cohesiveness in therapy groups. Archives of General Psychiatry 15: (3), 267–275. DOI: 10.1001/archpsyc.1966.01730150043007 |
92 | Zelencich, L. , Kazantzis, N. , Wong, D. , McKenzie, D. , Downing, M. , & Ponsford, J. ((2019) ). Predictors of working alliance in cognitive behaviour therapy adapted for traumatic brain injury. Neuropsychological rehabilitation, 1-19. DOI: 10.1080/09602011.2019.1600554 |
93 | Zigmond, A. S. , & Snaith, R. P. ((1983) ). The hospital anxiety and depression scale. Acta psychiatrica scandinavica 67: (6), 361–370. DOI: 10.1111/j.1600-0447.1983.tb09716.x. |
Notes
1 Time since injury was not considered due to the highly skewed and bimodal nature of this variable within the sample.




