Assessing and addressing footwear needs in Parkinson’s disease—design thinking in neurology
Abstract
BACKGROUND:
Parkinson’s disease (PD) is a neurodegenerative movement disorder that results in a variety of motor deficits such as unsteady gait, bradykinesia, resting tremor, and rigidity.
OBJECTIVE:
The objective of this study was to quantify and assess the challenges and preferences Parkinson’s disease patients have regarding footwear.
METHODS:
A 13-question survey was designed to assess footwear challenges and preferences among PD patients. A total of 89 PD patients, both male and female, were surveyed in the outpatient setting at UC Irvine during their appointments with the senior author.
RESULTS:
A majority of the PD patients in our cohort (64%) reported experiencing difficulties wearing shoes on their own. Patients who experienced difficulties wearing shoes were significantly more likely to report having been forced to make changes to their desired outfits (p = 0.0011), choosing not to wear dress shoes due to their discomfort (p = 0.0175), and preferring shoes without laces (p = 0.0 048).
CONCLUSIONS:
The present study is the first attempt to use a survey to quantify the challenges and preferences reported by PD patients in regard to their usage of footwear. Inspired by our findings, the study team designed a novel dress shoe prototype that may address some of the difficulties and concerns gathered through our survey.
1Introduction
Parkinson’s disease (PD) is a chronic neurodegenerative condition that currently afflicts more than 10 million individuals over the age of 50 (Dorsey et al., 2007). Clinically, PD is characterized by a host of motor symptoms including resting tremor, bradykinesia, rigidity, and postural instability (Jankovic, 2008). Patients can also suffer from non-motor symptoms ranging from cognitive impairment to gastrointestinal dysfunction (Poewe, 2008). Due to the progressive nature of the disease, these clinical features may grow more severe with time and further decrease quality of life (Cheng, Ulane, & Burke, 2010). While pharmacologic and surgical treatments are available, patients may also benefit from technological and wearable innovations that facilitate activities of daily living (ADLs) (Jankovic & Aguilar, 2008). Such assistive devices (ADs) can help patients carry out day-to-day tasks such as walking, turning in bed, wearing clothing, and eating meals (Constantinescu, Leonard, Deeley, & Kurlan, 2007; Cunningham, Nugent, Finlay, Moore, & Craig, 2009).
A number of ADs that may benefit PD patients currently exist and have been studied in the medical literature. Pathak et al., for instance, designed a biomechanical spoon that incorporates Active Cancellation of Tremor (ACT) technology to assist movement disorder patients with the process of eating (Pathak, Redmond, Allen, & Chou, 2014). Moreover, Barthel et al. addressed walking issues in PD by designing an ambulatory visual cueing device that can be strapped to one’s shoes to alleviate freezing of gait (FOG), a common PD symptom in which patients are momentarily unable to take a step forward despite having the intention to walk (Barthel et al., 2018). In addition, a host of simpler ADs exist on the market that may benefit patients, including dress shirts with magnetic buttons (“Magna Ready”), zipper pulls, and shoes with velcro (“Michael J. Fox Foundation for Parkinson’s Research”).
Despite the growing number of ADs aimed at helping individuals with movement disorders, few have attempted to facilitate the process of wearing shoes, an everyday activity that requires dexterity and motor control. Indeed, putting on footwear and tying one’s shoelaces is a daily undertaking that many disabled patients may find difficult to complete, potentially leading to significant compromises in their day-to-day routines and wardrobes. Moreover, while some accessible shoes designed for those with disabilities exist on the market, it is unclear how their aesthetic design factors into patients’ decision to wear these ADs. Herein, we surveyed patients with PD to better understand the challenges and preferences they have regarding their footwear. Based on our results, we prototyped a simple shoe innovation that takes into account the feedback we received from our cohort of PD patients. By presenting this information, we hope to not only contribute to the growing body of literature on ADs for PD patients, but also demonstrate the utility of incorporating design thinking principles into medical education as well as the clinical practice of neurology.
2Materials & methods
A 13-question survey was written by the study team to assess footwear challenges and preferences among PD patients. In particular, questions were designed to gauge demographic characteristics of the study population as well as specific preferences and concerns they held with regard to their footwear. Moreover, questions were also included to assess challenges with regard to dress shoes in particular. The survey and study received approval from the UC Irvine Institutional Review Board (IRB HS#2018–4428). A total of 89 PD patients, both male and female, were surveyed in the outpatient setting at UC Irvine during their appointments with the senior author. Summary statistics using Student t-test and Chi-squared were used where appropriate to evaluate outcomes across variables. Statistical significance was set with p-value <0.05, with all tests 2-sided. The results informed the design of a novel dress shoe prototype that addresses some of the footwear concerns identified through the survey.
3Results
The population of PD patients surveyed had a mean age of 68.1 years (SD = 9.0 years) and were 70% male. On average, the patients reported having been diagnosed with PD for 8.9 years. When asked whether or not they experience difficulties wearing their shoes on a daily basis, 64% of the patient population reported having at least some problems putting on their footwear (Fig. 1). Median responses for questions pertaining to specific challenges associated with wearing shoes as well as the importance of various aspects of footwear are also reported (Table 1).
Fig. 1
Frequency of difficulties with wearing shoes with level of severity. Study population responses to the degree of difficulty they associated with putting on shoes.
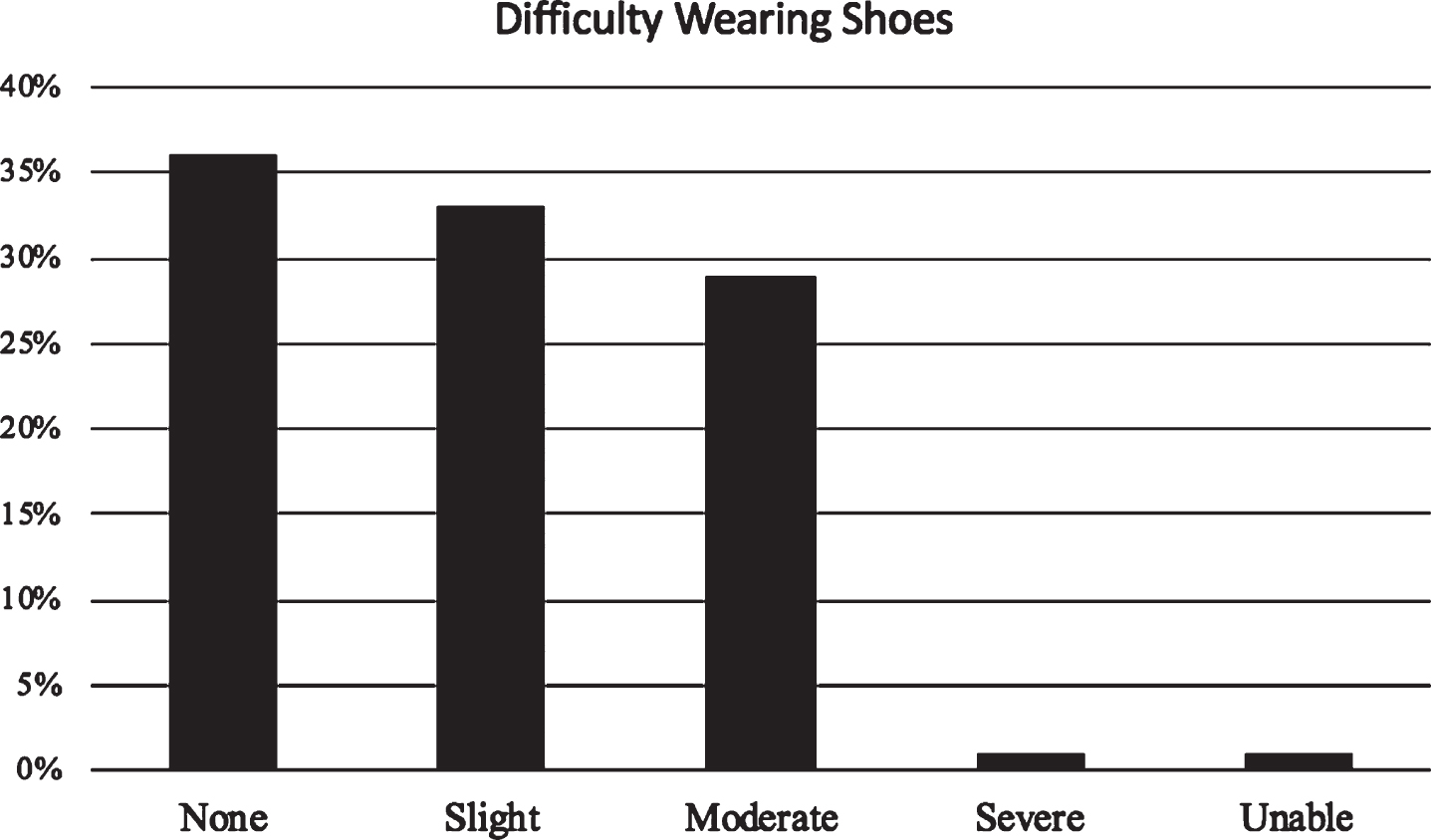
Table 1
Population characteristics
| Male | 70% |
| Female | 30% |
| Mean age (years) | 68.1 (SD = 9.0) |
| Mean years since diagnosis | 8.9 (SD = 6.3) |
| Reported some difficulty wearing shoes | 64% |
| Median difficulty bending down (1–5) | 2 |
| Median difficulty placing forefoot into shoe (1–5) | 2 |
| Median difficulty slipping heel into shoe (1–5) | 2 |
| Median difficulty tying shoelaces (1–5) | 2 |
| Median importance of shoe weight (1–5) | 4 |
| Median importance of breathability (1–5) | 3 |
| Median importance of aesthetic design (1–5) | 3 |
| Median importance of no lace/slip-on design (1–5) | 3 |
| Median importance of insole comfort (1–5) | 4 |
| Difficulties wearing dress shoes have deterred you from attending an event | 12% |
| Difficulties wearing dress shoes have forced changes to desired outfit | 38% |
| Have chosen not to wear dress shoes due to their discomfort | 65% |
Study population demographics and median responses/proportions gathered from survey analysis.
The patients were also surveyed in regards to the frequency with which they wear specific types of footwear, ranging from athletic to dress shoes (Appendix). When asked specific questions about their usage of dress shoes, 12% indicated that difficulties wearing dress shoes have deterred them from attending an event in the past, while 38% stated that these difficulties have forced them to make changes to their desired outfits. Furthermore, 65% reported having chosen to not wear dress shoes at all due to their discomfort (Table 1).
We then assessed differences in survey responses between patients who reported no difficulties and any difficulty wearing shoes. There was no significant difference in the mean age (p = 0.5840) or gender distribution (p = 0.6959) of these two groups. In contrast, the reported years since diagnosis with PD differed significantly between those who experienced no difficulties and some difficulties wearing shoes, with the latter group reporting longer time since diagnosis (p = 0.0174). Patients who experienced difficulties wearing shoes were significantly more likely to report having been forced to make changes to their desired outfits (p = 0.0011), choosing not to wear dress shoes due to their discomfort (p = 0.0175), and preferring shoes without laces (p = 0.0048) (Table 2).
Table 2
Comparison of survey results between patients with and without self-reported problems wearing shoes
| Reported no problems | Reported problems | |
| (n = 32) | (n = 57) | |
| Age (years) | 67.4 (SD = 9.95) | 68.5 (SD = 8.53) |
| Male | 72% | 68% |
| Female | 28% | 32% |
| Mean years since diagnosis | 6.8 (SD = 6.1, n = 32) | 10.1 (SD = 6.2, n = 57) |
| Median difficulty bending down (1–5) | 1 | 3 |
| Median difficulty placing forefoot into shoe (1–5) | 1 | 2 |
| Median difficulty slipping heel into shoe (1–5) | 1 | 3 |
| Median difficulty tying shoelaces (1–5) | 1 | 2 |
| Median importance of shoe weight (1–5) | 3 | 4 |
| Median importance of breathability (1–5) | 3 | 3 |
| Median importance of aesthetic design (1–5) | 2.5 | 3 |
| Median importance of no lace/slip-on design (1–5) | 2 | 4 |
| Median importance of insole comfort (1–5) | 4 | 5 |
| Difficulties wearing dress shoes have deterred you from attending an event | 6% | 14% |
| Difficulties wearing dress shoes have forced changes to desired outfit | 15% | 50% |
| Have chosen not to wear dress shoes due to their discomfort | 50% | 75% |
| No-lace preference | 45% | 75% |
Comparison of survey responses between patients who reported some difficulty putting on shoes versus those who reported no difficulty putting on shoes, as determined by Question 4 on the PD Shoe Questionnaire.
4Discussion
While the notion that individuals with disabilities may struggle to wear their shoes on a daily basis may appear self-evident, the current study is the first to quantify and characterize specific challenges and concerns among PD patients. In particular, a majority (64%) of the PD patients in our cohort reported experiencing some difficulties wearing shoes on their own. Moreover, while only 12% stated that difficulties with dress shoes in particular have deterred them from attending an event in the past, 38% reported having changed their desired outfit as a result while 65% abandoned dress shoes altogether.
In effort to better understand the factors underlying these results, we then analyzed differences between PD patients in our cohort who reported having difficulties wearing shoes and those who did not. Our analysis indicated that individuals who experienced difficulties reported a higher mean difficulty with every aspect of the shoe-wearing process mentioned in our survey, ranging from bending down to slipping their heels into shoes. Moreover, this subgroup also reported higher median preferences for shoes that are lightweight, breathable, laceless, able to be slipped on, equipped with comfortable insoles, and aesthetically pleasing. In regard to dress shoes in particular, they reported significantly higher rates of choosing not to attend an event, making changes to their desired outfit, and abandoning dress shoes altogether due to discomfort.
Interestingly, gender distribution and mean age of the two groups were approximately the same. The mean reported years since diagnosis, in contrast, was significantly greater in the subgroup that reported difficulties putting on footwear. These results suggest that disease stage, rather than patients’ age, may be a key factor behind our results.
Another notable result is the higher mean preference of a shoe’s aesthetic design for individuals who experience difficulty wearing footwear. This finding perhaps implies that although comfortable and easy to wear shoes exist on the market, these options may not meet the aesthetic preferences of our patients. One example of this notion is demonstrated by dress shoes: individuals with PD who desire to continue wearing formal, yet handicap-accessible footwear for their personal lives or profession have limited options on the current market.
Inspired by the results in this study, our team of medical students and physicians designed a novel dress shoe prototype in effort to meet this need (Fig. 2 and Appendix). While appearing as a dress shoe accompanied with laces, this shoe is able to be slipped on easily and secured over the foot using a magnetic system that runs down the upper. With this innovation, patients can pull open the shoe, step into it, and utilize a magnetic system to close the forefoot. By eliminating the need to tie one’s shoelaces, this prototype reduces the need for fine motor control while preserving the aesthetic appeal of the original dress shoe design. We believe that simple, inexpensive innovations such as ours may provide meaningful and immediate benefit to many patients’ lives.
Fig. 2
Novel dress shoe prototype. A novel dress shoe prototype developed by medical students in light of survey findings. While disguised as an elegant dress shoe accompanied with laces, this shoe is able to be slipped on easily and secured over patients’ feet using a magnetic system that runs down the upper. With this innovation, patients can pull open the shoe, step into it, and utilize a magnetic system to close the upper.

With the rapid progression and accessibility of assistive technology, findings like ours can help inform engineers and medical innovators on the day-to-day difficulties our patients face which cannot currently be addressed through clinical means. Recently, medical school curriculums around the nation have begun to incorporate design thinking to encourage future physicians to think beyond the confines of pharmaceutical and surgical treatments in solving patients’ concerns. Popularized by founder of the international design firm IDEO Tim Brown and further developed by institutions such as Stanford’s Hasso Plattner Institute of Design, design thinking is a systematic process that fosters human-centered innovations through a cycle of empathizing, defining, ideating, prototyping, and testing (Brown, 2008; Gottlieb, Wagner, Wagner, & Chan, 2017). Our methodology in this study fit well within this framework, as we initially attempted to define the specific challenges PD patients face in regard to their daily use of footwear. Based on our results, we then ideated several shoe designs using the feedback we received from our cohort. Here, we present the final working dress shoe prototype in Fig. 2. This dress shoe is an innovation that was developed by medical students that may inspire further innovations by medical professionals of all stages, ranging from current trainees to established clinicians.
The current study is not without limitations. Foremost, our cohort was relatively small, consisting of 89 PD patients. Moreover, many of these patients resided within the greater Orange County area, which is generally comprised of communities from a higher-than-average socioeconomic status. The survey used in this study was also non-exhaustive and did not include many potential questions that could have benefited our analyses. In addition, no objective physical assessments or recordings were performed to quantify difficulties experienced by patients as they wore different types of shoes; rather, all results in this study were self-reported to us by the surveyed patients.
5Conclusion
The present study is the first attempt to use a survey to quantify the challenges and preferences reported by PD patients in regard to their usage of footwear. It was found that 64% of patients expressed some degree of difficulty wearing shoes on a daily basis. Moreover, while only 12% stated that difficulties with dress shoes in particular have deterred them from attending an event in the past, 38% reported having changed their desired outfit as a result while 65% abandoned dress shoes altogether. Inspired by our findings, the study team designed a novel dress shoe prototype that may address some of the difficulties and concerns gathered through our survey. In turn, we hope to inspire further innovations that may help PD patients with activities of daily living through non-invasive, non-pharmaceutical means.
Conflict of interest
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Appendices
Appendix
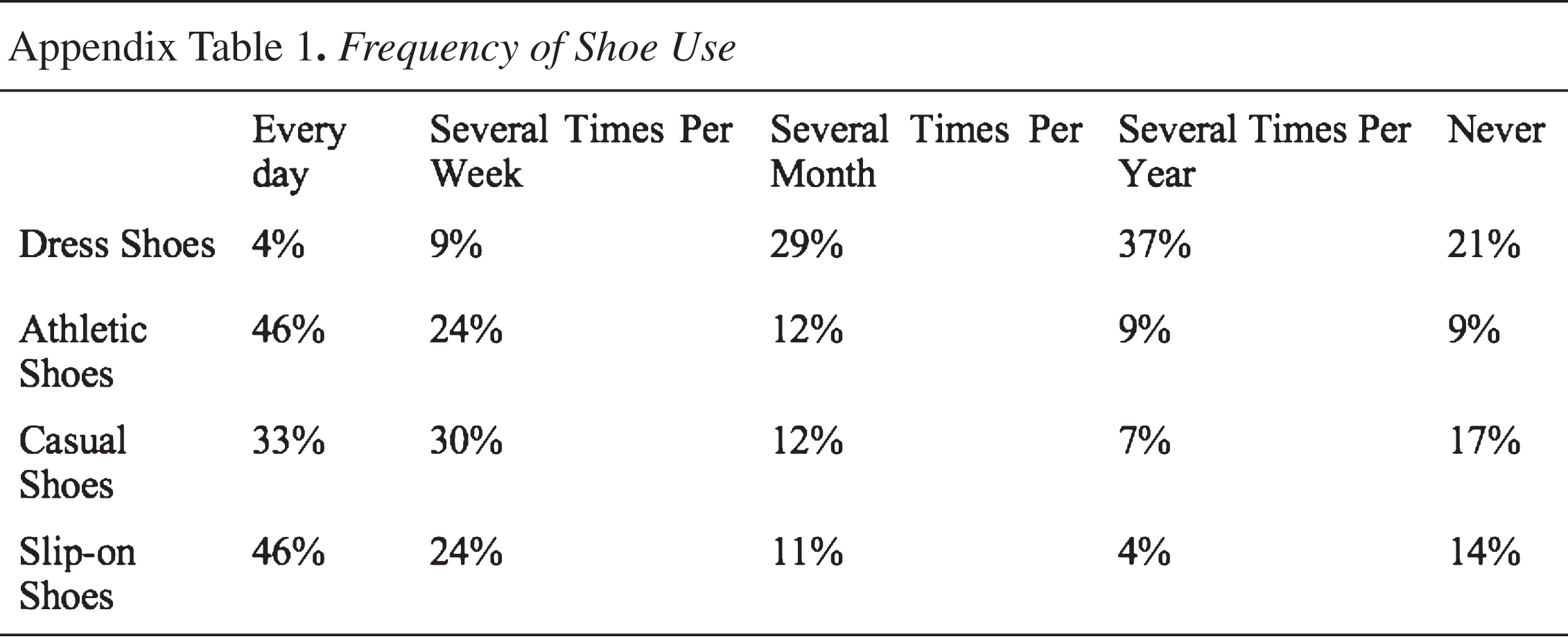 |
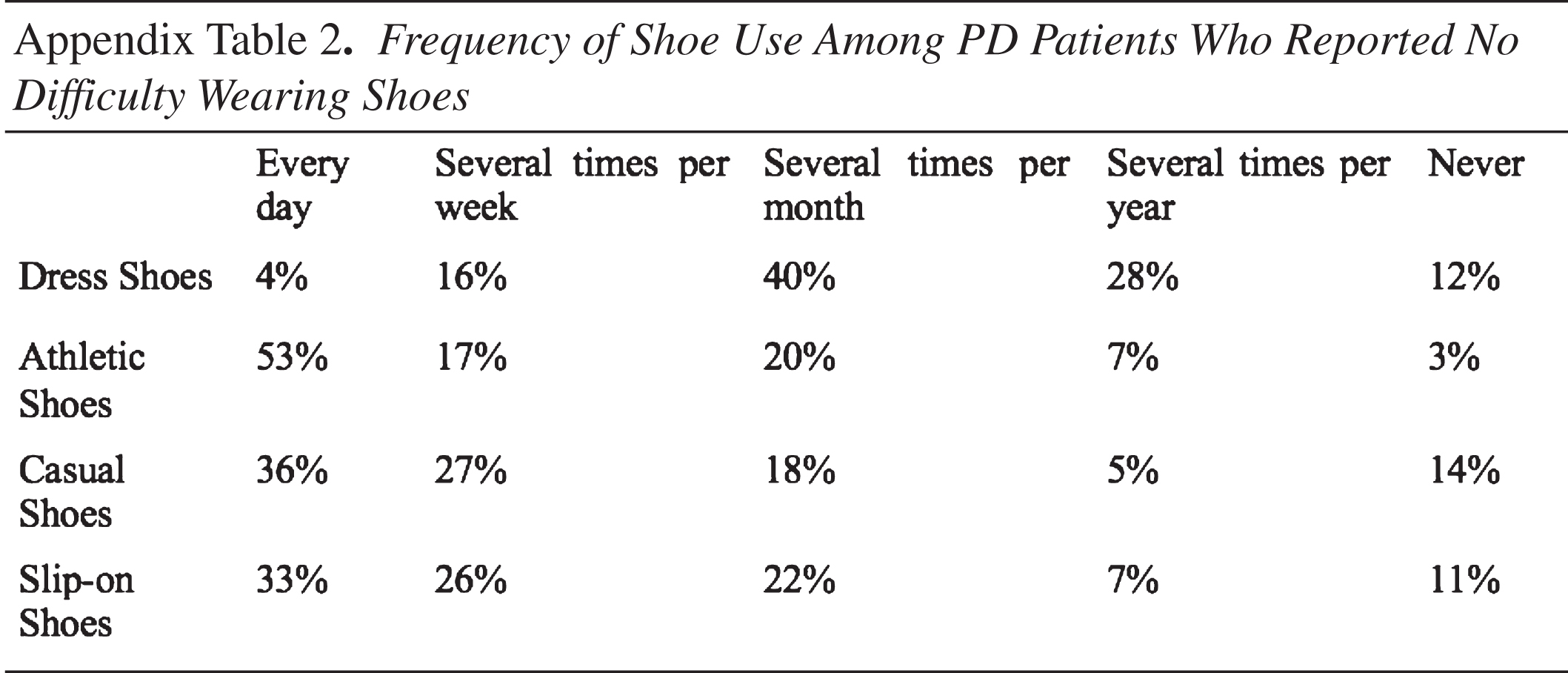 |
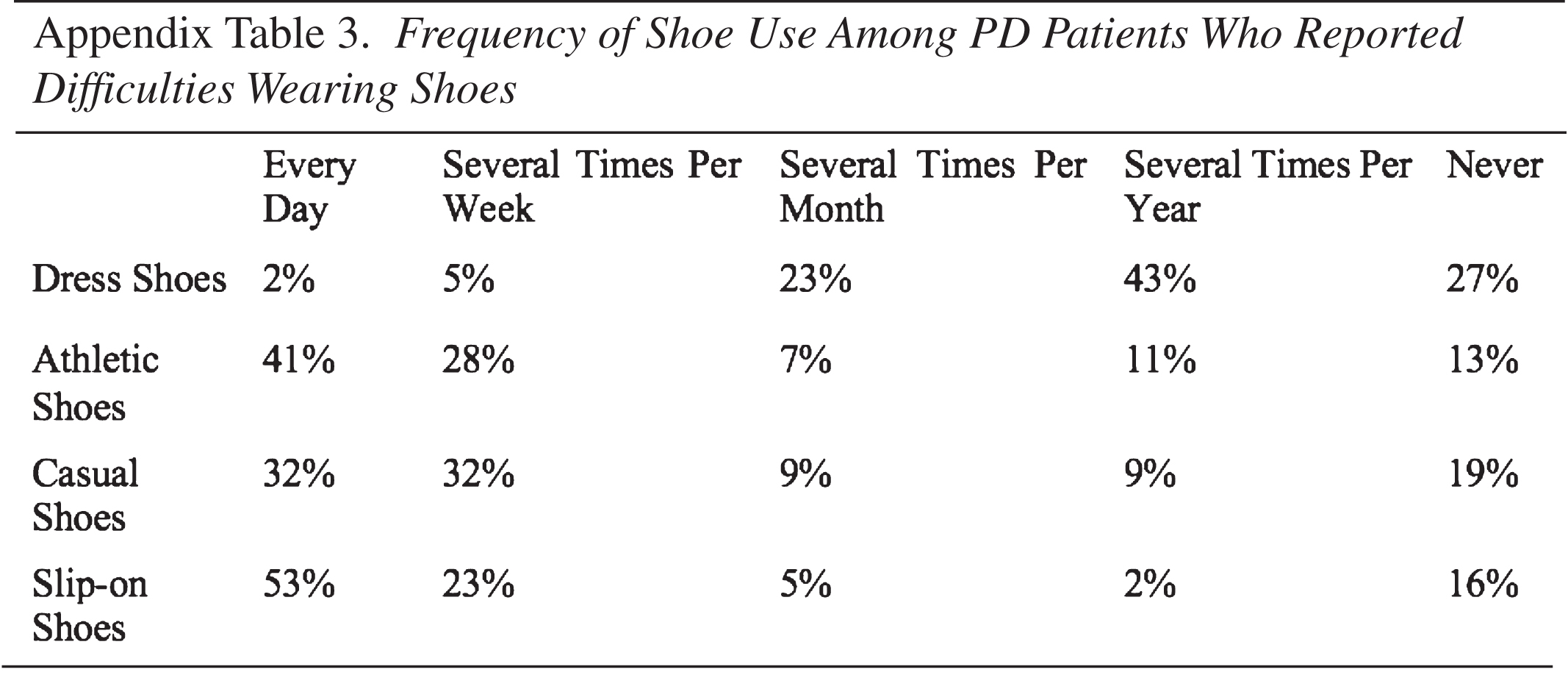 |
References
1 | Barthel, C , Nonnekes, J , van Helvert, M , Haan, R , Janssen, A , Delval, A , & Ferraye, M. U. ((2018) ). The laser shoes: A new ambulatory device to alleviate freezing of gait in Parkinson disease. Neurology, 90: (2), e164–e171. doi: 10.1212/wnl.0000000000004795 |
2 | Brown, T. ((2008) ). Design thinking. Harvard Business Review, 86: (6), 84–92. |
3 | Cheng, H. C , Ulane, C. M , & Burke, R. E. ((2010) ). Clinical progression in Parkinson disease and the neurobiology of axons. Ann Neurol, 67: (6), 715–725. doi: 10.1002/ana.21995. |
4 | Constantinescu, R , Leonard, C , Deeley, C , & Kurlan, R. ((2007) ). Assistive devices for gait in Parkinson’s disease. Parkinsonism Relat Disord, 13: (3), 133–138. doi: 10.1016/j.parkreldis.2006.05.034 |
5 | Cunningham, L. M , Nugent, C. D , Finlay, D. D , Moore, G , & Craig, D. ((2009) ). A review of assistive technologies for people with Parkinson’s disease. Technol Health Care, 17: (3), 269–279. doi: 10.3233/thc-2009-0547 |
6 | Dorsey, E. R , Constantinescu, R , Thompson, J. P , Biglan, K. M , Holloway, R. G , Kieburtz, K , & Tanner, C. M. ((2007) ). Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology, 68: (5), 384–386. doi: 10.1212/01.wnl.0000247740.47667.03 |
7 | Gottlieb, M , Wagner, E , Wagner, A , & Chan, T. ((2017) ). Applying Design Thinking Principles to Curricular Development in Medical Education. AEM Education and Training, 1: (1), 21–26. |
8 | Jankovic, J. ((2008) ). Parkinson’s disease: Clinical features and diagnosis. J Neurol Neurosurg Psychiatry, 79: (4), 368–376. doi: 10.1136/jnn2007.131045 |
9 | Jankovic, J , & Aguilar, L. G. ((2008) ). Current approaches to the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat, 4: (4), 743–757. |
10 | MagnaReady. Retrieved from https://www.magnaready.com/shop |
11 | Michael, J . Fox Foundation for Parkinson’s Research. Retrieved from https://www.michaeljfox.org/foundation/news-detail.php?assistance-products-for-parkinson-disease-community-recommendations |
12 | Pathak, A , Redmond, J. A , Allen, M , & Chou, K. L. ((2014) ). A noninvasive handheld assistive device to accommodate essential tremor: a pilot study. Mov Disord, 29: (6), 838–842. doi: 10.1002/mds.25796 |
13 | Poewe, W. ((2008) ). Non-motor symptoms in Parkinson’s disease. Eur J Neurol, 15: (Suppl 1), 14–20. doi: 10.1111/j.1468-1331.2008.02056.x |




