Abstracts of the 31st Bárány Society Meeting, Madrid, Spain, May 9-11, 20221
SATELLITE - 7-SATURDAY
9:00:00 AM Scientific Session
ST0136So You Think All Hair Cell Mitochondria are The Same...?
Anna Lysakowski1, Ameena Patel2, Vidya Babu2, Zahid Abdul3, Suhitha Irukulla2, Dua Ruyyashi2, Basil Zakkar4, Ahmad Al-Najjar2, Abd-al-Rahman Al-Rafai2, Priya Satani2, Ishita Bhuptani2, Matthew Mefferd2, Meaghan Smith2, Rose Bahari2, Nora Laban2, Joseph Lesus2, Jacob Kulaga3, Steven D. Price1, Guy Perkins5
1Department of Anatomy and Cell Biology, University of Illinois at Chicago (UIC), IL, USA, 2Department of Biological Sciences, University of Illinois at Chicago, IL, 3Department of Chemistry, University of Illinois at Chicago, Chicago, IL, 4Department of Economics, University of Illinois at Chicago, Chicago, IL, 5National Center for Microscopy & Imaging Research, Univ. of California at San Diego, CA
The theme is vestibular hair cells and the target audience is neuroscientists and vestibular scientists.
ST0082From the Calyx to the Clinic – a Review of the Neural Evidence of Vestibular Activation by Sound and Vibration that Underpins Clinical Otolithic Testing
Ian Curthoys
University of Sydney, NSW, Australia
Sound and vibration are the stimuli in the most widely used clinical tests of otolith function - vestibular evoked myogenic potentials (VEMPs). But sounds and vibration are so dissimilar from the classical vestibular stimuli - linear and angular accelerations - the question becomes how do they stimulate vestibular receptors whose transduction mechanisms are so different to cochlear transduction mechanisms? In this review I show that sounds and vibration really do stimulate vestibular receptors. Aspects of the results cast light on the mechanism of hair cell transduction by vestibular receptors and raise questions about the evolutionary origin of these sensory systems.
The classical paper by Young et al (1977) showed that mammalian primary vestibular afferents with irregular resting discharge are activated by sound and vibration with surprisingly precise phase-locking, similar to the phase-locking of auditory afferents. Phase-locking is key because it shows that every single cycle of the auditory stimulus can effectively stimulate irregular vestibular afferent neurons.
Goldberg et al (1990) showed that the regularity of resting discharge was related to the utricular innervation pattern of the afferent. Afferents with irregular resting discharge derived from calyx synapses on type I receptors at the striola. Other afferent neurons contacting many type II receptors as well as a few type I receptors are dimorphic and mostly have regular resting discharge.
Irregular otolithic afferents are large diameter, fast neurons with, on average, low resting rate and very low gain to low frequency linear accelerations but a high gain at high frequencies. They are excited by low intensity vibration and show very tight phase-locking even at frequencies greater than 1000 Hz with a precision of phase-locking comparable to, or even superior to, that of cochlear afferents.
Recently the work of Lim et al (2011) and Contini et al (2020) has shown the probable mechanisms of this temporal precision: transmission at the type 1-calyx synapse has three elements – quantal release of glutamate, and two non-quantal mechanisms -potassium ion accumulation and the ultrafast (microsecond) resistive coupling between the type I receptor and the calyx.
Why has this system of type 1 receptors and irregular calyx afferents evolved? It may be due to the behavioural demands of species with mobile heads during the evolutionary transition from ocean living to terrestrial environments and the demands that transition places for a fast, temporally precise system for signalling head movements and generating appropriate fast corrective responses.
ST0107A Brave New World: Hair cells of mice, humans, and inner ear organoids
Cristiana Mattei1,2, Hannah R Drury3, Babak Nasr1,4,5, Zihui Li2, Melissa A Tadros3, Giovanna M. D’Abaco2, Kathryn S Stok2, Bryony A Nayagam6, Mirella Dottori1,2,7, Rebecca Lim3
1Centre for Neural Engineering, Melbourne School of Engineering, The University of Melbourne, Melbourne, VIC, Australia, 2Department of Biomedical Engineering, Melbourne School of Engineering, The University of Melbourne, Melbourne, VIC, Australia, 3School of Biomedical Sciences and Pharmacy, Faculty of Health and Medicine, University of Newcastle, Callaghan, NSW, Australia, 4Department of Electrical and Electronic Engineering, Melbourne School of Engineering, The University of Melbourne, Melbourne, VIC, Australia, 5ARC Centre of Excellence for Integrative Brain Function, The University of Melbourne, Melbourne, VIC, Australia, 6Departments of Audiology and Speech Pathology and Department of Medical Bionics, The University of Melbourne, Melbourne, VIC, Australia, 7Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW, Australia
Background: The vast majority of studies investigating the anatomy and function of the inner ear arise from animal studies and in particular from mice. While these results have provided us with a foundation of knowledge, it is still unknown whether these animal models are a true representation of the human form. Similarly, stem cell research has typically relied upon animal models to inform regenerative pathways. It is the aim of this research to describe the similarities and differences in the vestibular neuroepithelium between mice and humans and compare these data to that from hair cell-like cells from inner ear organoids.
Methods: The vestibular neuroepithelium was isolated from mice or human foetal inner ears (aged 10-16 weeks gestation) and were used for anatomical and physiological studies. Human ES cell lines H3 and H9, and human iPS cell line 007 were used to generate inner ear organoids using a rotary cell culture system (RCCS). Neuroepithelia were scanned using helium ion microscopy and micro-computed tomography. Hair cells from mouse, human, and inner ear organoids were immunofluorescently labelled with markers against hair cell specific markers including; Myo7a, ATOH1, and CtBP2. Physiological function of hair cells was compared using whole cell patch clamp recordings using a KCl – gluconate internal solution and Liebovitz’s L15 media as external solution.
Results: The formation of organoids using the RCCS generated cells in vesicle-like structures. Using helium ion microscopy, the surface of orgnoids showed ciliated cells, some with longer bundle that resembled a vestibular hair cell specific kinocilium. Consistent with these observations, these cells expressed hair cell specific marker Myo7A and kinocilia marker alpha acetylated tubulin. These hair cell-like cells also expressed CtBP2, a marker of ribbon synapses. Calcium carbonate crystals, an accessory structure consistent with a vestibular hair cell phenotype was also observed using micro-CT. Whole-cell patch-clamp recordings from organoid hair cell-like cells showed voltage activated currents that are consistent with developing human foetal vestibular hair cells. A subset of these cells also had an inward sodium current, typically only observed during early inner ear development.
Discussion: Inner ear organoids can be generated from hPSC using a RCCS. Inner ear organoid hair cells have structural and functional properties that resemble immature human foetal vestibular hair cells. The capacity to develop organoids that resemble vestibular inner ear hair cells is a valuable resource for examining development of hair cells, the effects of drugs on inner ear function.
11:30 Scientific Session
Vestibular hair cells in mammals include an unusual type (I) with two major specializations relative to the more typical type II hair cells that co-exist in the sensory epithelium. Type I hair cells have a large number of voltage-gated (Kv) potassium channels that are open at resting potential, forming a conductance called gK,L, and receive a large calyceal synaptic contact from primary vestibular afferents. In murids, gK,L ion channels and synaptic calyces are acquired mid-way through hair cell development, in the first postnatal week, before eye and ear opening. Recent work has shown that these specializations both serve an unusual, non-quantal synaptic transmission from the hair cell to the calyx terminal. Previous physiological data from us and others and recent computational work from our collaborators (Govindaraju et al. 2021 BioRxiv doi: https://doi.org/10.1101/2021.11.18.469197), led us to speculate that the specializations increase the speed and linearity of afferent transmission, enhancing the rapid and accurate stabilization of posture and gaze by vestibular reflexes.
Since gK,L was first described (Correia and Lang 1990, Neurosci Lett 116:106) there have been multiple suggestions about its molecular identity, including Kv7 and Kv11 channels. Kv1 is another channel family with low-voltage-activated members. Kv1.8 is expressed in vestibular epithelia, and the Kv1.8-null mouse lacks vestibular evoked potentials (VsEPs) during rapid head motions (Lee et al. 2013, Hearing Res 300:1). Since VsEPs arise from synchronized activity of afferents that contact type I hair cells in otolith organs, we hypothesized that Kv1.8 subunits contribute to gK,L channels. Consistent with our hypothesis, our whole-cell patch clamp recordings showed that in Kv1.8-null mice, gK,L was absent from type I hair cells, and Kv1.8 immunoreactivity was specifically absent in hair cell membranes.
We did not expect a major loss of Kv current in Kv1.8-null type II hair cells because their major Kv conductance, gA, is an inactivating conductance that differs markedly from gK,L. To our surprise, gA was also absent in Kv1.8-null mice. The residual Kv conductance in both type I and II hair cells in Kv1.8-null mice was consistent with a single conductance in the Kv7 family.
Thus, both hair cell types depend on Kv1.8 for their dominant Kv conductances and express an additional Kv7 conductance. The great differences in gK,L and gA must arise from hair cell type-specific expression of molecules that partner with Kv1.8 subunits to form channels or regulate channel properties in other ways.
Supported by NIH R01DC012347
ST0100Activation of the Semicircular Canals and Otolith Organs by Atypical Forms of Energy: Microwaves, Laser Light and Focused Ultrasound
Richard D. Rabbitt
University of Utah
Background: The semicircular canals and otolith organs evolved hundreds of millions of years ago to sense motion and orientation relative to gravity in an environment free from high-power electromagnetic and/or ultrasonic sources of energy. The discovery that pulsed microwaves generate auditory percepts by Alan Frey in the 1960s revealed that the inner ear can be stimulated remotely by a beam of electromagnetic energy. Ultrasonic vibrations well above the normal range of hearing have also been shown to evoke auditory percepts, and strong magnetic fields have been shown to evoke nystagmus. Remote stimulation of the inner ear by atypical forms of energy led to the speculation that auditory and vestibular symptoms associated with “Havana Syndrome” might be triggered by a focused beam of energy. Here, I review several biophysical mechanisms responsible for vestibular afferent sensitivity to microwaves, magnetic fields, laser light and focused ultrasound.
Methods: All experiments were performed with approval by the Institutional Animal Care and Use Committee at the University of Utah and partner institutions. Single unit vestibular afferent neurons were recorded using conventional borosilicate electrodes. Sensitivities to atypical stimuli were characterized in terms discharge rate modulation, action potential timing, and phase-locking vector strength. Biophysical origins of sensitivity were examined by combining multiple forms of stimulation, mechanical measurements, pharmacology and biophysical modeling.
Results: Results demonstrate microwaves and laser light modulate vestibular afferent discharge rate primarily through rapid changes in temperature. Thermo-mechanical strain and temperature both modulate ion channel open probability and synaptic release, leading to diverse responses in vestibular afferents depending on hair cell/afferent type and channel expression. In addition, high rates of temperature change induce thermo-striction of the lipid bilayer, which drives an excitatory capacitive current capable of evoking an action potential. Thermal effects act on both sensory hair cells and neurons, with hair cells exhibiting highly sensitive excitatory and inhibitory responses. In contrast, focused ultrasound modulates vestibular afferent discharge primarily through the acoustic radiation force deflecting hair bundles. The acoustic radiation force acts in the direction of the ultrasound beam and can be excitatory or inhibitory depending on the orientation of the hair bundles relative to the beam.
Conclusions: Evidence supports the hypothesis that sensitivity of the semicircular canal and otolith afferent neurons to microwaves, laser light and focused ultrasound occurs through conventional thermo-electro-mechanical biophysical mechanisms. Results raise the possibility of using atypical forms of controlled energy for targeted vestibular diagnostic and therapeutic applications.
Supported by NIH: R01DC006685
13.30 Scientific Session
ST0122The efferent vestibular system: connecting synaptic mechanisms to function
Joseph C. Holt1,2,3
1Department of Otolaryngology, University of Rochester, Rochester, NY, United States, 2Department of Neuroscience,University of Rochester, Rochester, NY, United States, 3Department of Pharmacology & Physiology, University of Rochester, Rochester, NY, United States
The efferent vestibular system (EVS) in mammals originates as bilateral clusters of predominantly cholinergic, multipolar neurons in the dorsal brainstem whose axons, after extensive branching, produce a dense deposition of vesiculated varicosities on afferent endings and hair cells in the vestibular periphery. This anatomy alone reveals that the EVS provides the CNS with the direct hardwiring to modulate both sides of the first synapse in vestibular transduction. To this end, activation of EVS pathways can significantly alter the discharge properties and sensitivity of vestibular afferents along multiple time scales, suggesting that the EVS is fundamentally important and that its dysregulation could ultimately contribute to vestibular dysfunction. However, a more thorough understanding regarding the functional framework of this centrifugal pathway in mammals remains rather elusive. We have repeatedly insisted that pharmacological identification of the synaptic mechanisms governing EVS actions in mammals and other vertebrate models are indispensable for characterizing the functional role of the EVS within the constraints of normal vestibular physiology. Furthermore, the same pharmacological interrogation will be instrumental in evaluating EVS function in behaving animal models, provided we can selectively target those synaptic mechanisms in the inner ear. It has been shown that the activation of several distinct acetylcholine (ACh) receptors on vestibular hair cells and afferents can explain the bulk of EVS actions across multiple vertebrate vestibular preparations. However, comparable characterization of synaptic mechanisms underlying afferent responses to EVS stimulation in mammals have only recently been performed. This talk will provide an overview of our recent work in a novel in vivo mouse preparation where we have recorded primary afferent activity from the superior vestibular nerve while stimulating EVS neurons in the brainstem before and after administration of selective pharmacological agents. Consistent with previously-reported EVS pharmacology in other vestibular models, we will show that the EVS in mice also utilizes at least three distinct ACh receptors to modulate the resting discharge of vestibular afferents including alpha9-nicotinic AChRs, alpha4/beta2-containing nicotinic AChRs, and muscarinic AChRs. The implications of these data and thoughts about how we might use select transgenic mouse models, in tandem with the aforementioned pharmacological manipulations, to both specify transmitter receptors and their downstream effectors as well as probe vestibular behaviors will be discussed.
ST0139Bárány Satellite 2022 Peripheral vestibular hypofunction and correlates to labyrinthine synaptopathy
Larry F. Hoffman
Department of Head & Neck Surgery and Brain Research Institute
David Geffen School of Medicine at UCLA
Peripheral vestibular hypofunction is a heterogeneous condition that is recognized to have broad penetrance in adult populations within the United States and Europe. It is characterized by attenuation in various functional measures of the labyrinth, such as the gain of the vestibuloocular reflex or the head impulse test. Despite the apparent broad penetrance of the condition, an understanding of specific cellular and physiologic substrates has yet to be achieved. It might be imagined that the condition’s etiology could be explained by dysfunction at any or multiple components of the peripheral signaling pathway from stimulus transduction to generation of afferent neuron spiketrains. Nonetheless, a reliable model of vestibular hypofunction would not only illuminate sources of dysfunction but also establish targets for potential therapies. Our laboratory has established such a model through which detailed cellular and electrophysiologic correlates of dysfunction can be investigated in detail. The model is based upon the direct intraperilymphatic administration of gentamicin enabling a strategy through which precise dosing is accomplished. This produces preparations in which graded lesions in the neuroepithelia can also be achieved, leading to associated graded levels of dysfunction. Electrophysiologic measures of afferent neuron discharge indicate that aminoglycoside-induced hypofunction may be harbored in compromise of the output spiketrain coherence to the input stimulus. This essentially represents an attenuation in signal-to-noise ratio, which may be interpreted by central nervous system circuits as a degradation in reliability of the sensory afferent signal. In these preparations, response magnitude (the electrophysiologic analog of gain), was unchanged.
These findings are reminiscent of similar conditions underlying cochlear synaptopathy, which is associated with hidden-hearing loss, reflecting compromised ability to extract acoustic stimuli from noise. Comprehensive investigations are currently underway to determine whether a corollary labyrinthine synaptopathy represents an underlying etiology of peripheral vestibular hypofunction.
If in-progress research supports this notion, it may be possible to recruit natural mechanisms for peripheral vestibular plasticity for rehabilitation strategies to drive synaptic recovery within the labyrinth.
14.30 Oral Presentation 04
ST0128DTNA and FAM136A Expression in a 3D inner ear organoid model of Meniere disease
Lidia Frejo1,2,3, Francisca E. Cara1,3, Alvaro Gallego-Martinez1,2,3, Jose A. Lopez-Escamez1,2,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain. 2Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en Enfermedades Raras, CIBERER, 28029 Madrid, Spain. 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, Hospital Universitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain. 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain.
Background: Familial Meniere’s disease (FMD) is an inner ear disorder defined by sensorineural hearing loss, episodic vertigo and tinnitus and it is observed in 5–15% of MD cases. By whole-exome sequencing, we identified two heterozygous single-nucleotide variants in FAM136A and DTNA genes in a Spanish family with three affected cases in consecutive generations, highly suggestive of autosomal-dominant inheritance.
We have generated an induced pluripotent stem cell line (hPSC; GENYOi007-A) from a FMD patient with both mutations and differentiated them into 3D inner ear organoids (IEO).
Methods: CytoTune 2.0 Reprogramming kit was used to reprogram peripheral blood mononuclear cells from this FMD patient. Characterization of the cell line GENYOi007-A included genetic analysis of DTNA and FAM136A variants, Short Tandem Repeats profiling (STR), expression of pluripotency-associated factors and differentiation studies in vitro. To begin the differentiation to IEO, hPSC were aggregated and treated with extracellular matrix proteins to promote epithelialization. Then, by recapitulating signaling pathway activation and attenuation during inner ear development we modulated signaling pathways inducing sequential formation and subsequent self-guided morphogenesis to form sensory epithelia containing hair cells and supporting cells, as well as neurons forming synapses with the hair cells.
Results: First, we confirmed the presence of DTNA and FAM136A variants by Sanger sequencing. GENYOi007-A silenced the expression of exogenous transgenes and activated the expression of the endogenous pluripotent transcription factors (SOX2, REX1, NANOG and OCT4). Importantly, GENYOi07-A cells showed normal karyotype (46, XX). Furthermore, the expression of the pluripotent markers SSEA4, Tra1-60 and Tra1-81 was confirmed by flow cytometry analysis and Confocal imaging. Finally, to demonstrate its capacity to differentiate into the three germ layers we performed an embryoid bodies (EBs) formation assay. EBs derived from this cell line showed specific expression of representative markers of the three germ layers: ectoderm (β3-Tubulin), mesoderm (Vimentin) and endoderm (Cytokeratin CKAE1-AE). IEO showed high levels of MYO7a (FC= 4.3); ATOH1 (FC=54.1) and TUBB3 (FC=13.4) when compared to the hPSC, demonstrating their capacity to differentiate into inner ear tissue. Likewise, DTNA and FAM136A had higher expression in the IEO (FC= 15.1 and 1.6, respectively). Western blot supported the above results.
Conclusion: Both DTNA and FAM136A are expressed in inner ear tissue-like organoids. Further experiments are needed to define the cell types involved in FAM136A and DTNA expression in human inner ear tissue.
Funding: This study was supported by a Sara Borrell Fellowship (ISCIII, CD20/00153) and CTEICU fellowship (Junta de Andalucia, DOC_01677).
ST0121Molecular subtypes of Sporadic Meniere Disease may be defined by DNA methylation signature in mononuclear cells
Marisa Flook1,2,3; Alba Escalera-Balsera1,2,3; Alvaro Gallego-Martinez1,2,3; Juan Manuel Espinosa-Sanchez1,2,3; Ismael Aran4; Andres Soto-Varela5; Jose Antonio Lopez-Escamez1,2,3,6
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain; 2Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en Enfermedades Raras, CIBERER, 28029 Madrid, Spain; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, Hospital Universitario, Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4Department of Otolaryngology, Complexo Hospitalario de Pontevedra, 36071 Pontevedra, Spain; 5Division of Otoneurology, Department of Otorhinolaryngology, Complexo Hospitalario Universitario, 15706 Santiago de Compostela, Spain; 6Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: DNA methylation is a stable epigenetic mechanism required for gene expression regulation and cell phenotype definition. Nevertheless, little research has been done to evaluate the role of epigenetics in hearing. In this study, we conducted whole genome bisulfite sequencing (WGBS) in Meniere Disease (MD) patients and healthy controls to identify a MD methylation signature and potential disease mechanisms.
Methods: WGBS was carried out on fourteen MD patients and six healthy controls. Differentially methylated cytosines (DMC) were mapped with methylKit R package; differentially methylated regions (DMR) were identified with Methpipe software and Undermethylated regions (UMR) were identified with methylSeekR R package. To identify biological pathways, processes and function, functional analyses were conducted using Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG) databases, and Genomic Regions Enrichment of Annotations Tool (GREAT).
Results: We observed two UMRs in PHB gene exclusive to MD patients. We observed a higher number of DMC in MD patients when compared to controls (n= 9545), various mapped to hearing loss genes, such as PCDH15, ADGRV1 and CDH23, which encode proteins forming ankle links in the stereocilia bundle. IL32 gene presented a DMR (DM = -0.35) and a DMC (DM = -0.41) in the promoter region when comparing MD patients with high levels of cytokines (MDH) to controls. IL-1β is increased in MDH patients, which could induce IL-32. Cis-regulatory sites function was predicted with GREAT revealing that the identified DMCs have predicted phenotypes associated with cochlear and organ of Corti degeneration, and abnormal synaptic current.
Conclusions: DNA methylation allows to differentiate MD patients from controls. Our study support previous findings of a chronic inflammatory process underlying MD. We identified various DMCs in genes that have been previously associated with cochleovestibular phenotypes in mice.
Funding: PI17/1644, F18/00228 and PI20/1126 Grants from ISCIII by FEDER Funds from EU; Andalusian Government EPIVERT PI-0027-2020 Grant; Horizon 2020, Grant Agreement Number 848261
ST0105Variants in MYO7A and other genes involved in the stereocilia links mediate digenic inheritance in familial Meniere disease
Pablo Roman-Naranjo1,2,3,4, Alba Escalera1,2,3, Alberto Parra-Perez1,2,3, Paula Robles-Bolivar1,2,3, Lidia Frejo1,2,3, José A. Lopez-Escamez1,2,3,4
1 Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre forGenomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain. 2 Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en EnfermedadesRaras, CIBERER, 28029 Madrid, Spain. 3 Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, HospitalUniversitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain. 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain
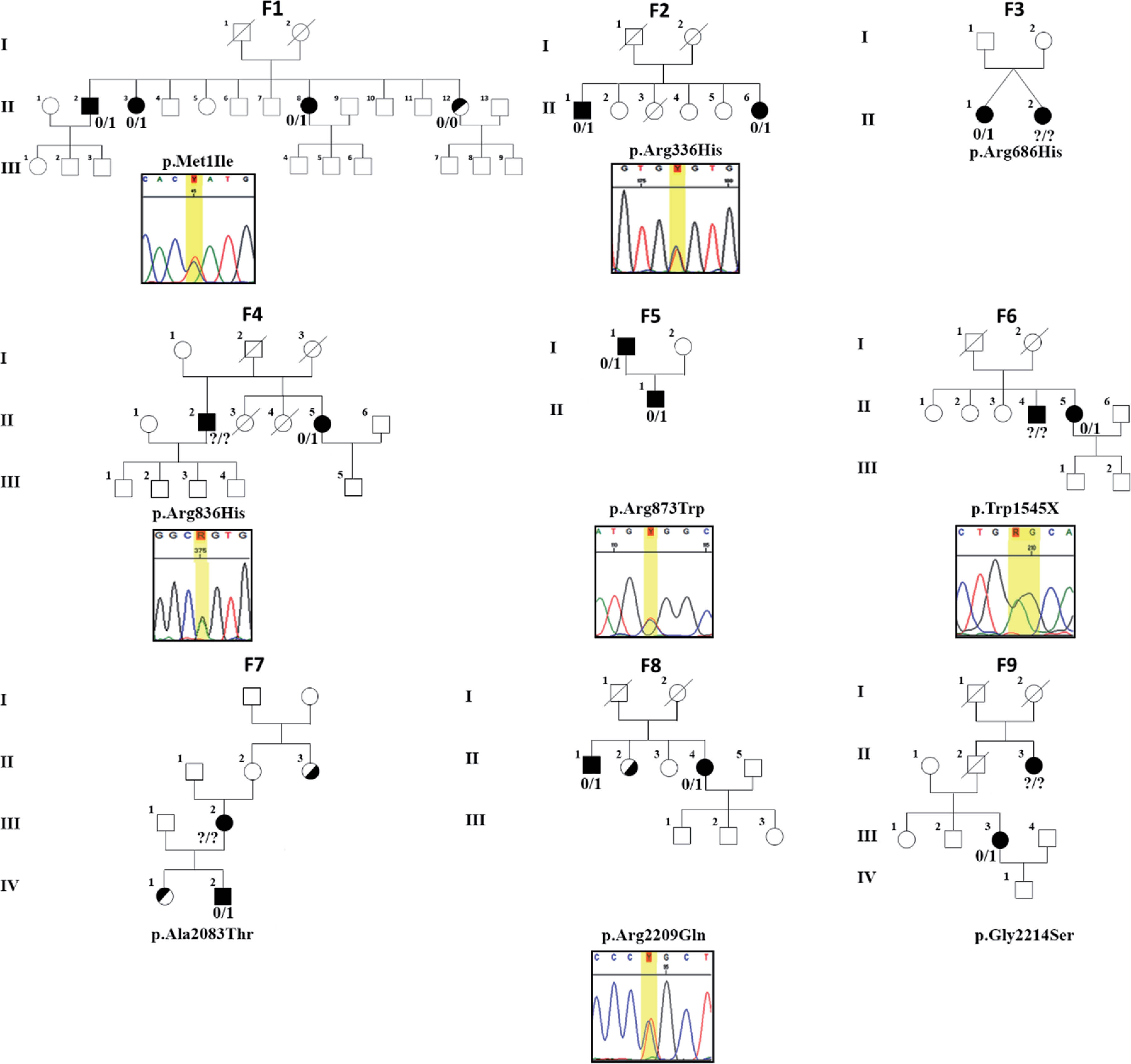
The MYO7A gene (myosin VIIA) encodes a motor protein with a key role in the organization of stereocilia in auditory and vestibular hair cells. Rare variants in this gene are involved in several types of sensorineural hearing loss (SNHL) with variable vestibular dysfunction, including autosomal dominant (DFNA11) or autosomal recessive (DFNB2) SNHL, and Usher syndrome type 1B (USH1B). Familial Meniere’s disease (MD) is a rare inner ear syndrome characterized by lowfrequency sensorineural hearing loss and episodic vertigo associated with tinnitus and aural fullness. Familial aggregation has been found in 6-8% of sporadic cases, and most of the reported genes were involved in single families, supporting genetic heterogeneity. Thus, this study aimed to search for relevant genes not previously linked to this condition. Through exome sequencing and segregation analysis in 62 MD families, we have found a total of 9 rare or novel heterozygous variants in the MYO7A gene in 9 non-related families (Figure 1). Of note, we found two loss of function variants: a start loss variant segregated in three affected individuals of the same family; and a novel stop gain variant (p.Trp1545Ter). Additionally, some novel and rare variants in other genes involved in the organization of the stereocilia links such as CDH23, PCDH15 or ADGRV1 cosegregated in the same patients. Seven of the 9 families carrying rare variants in the MYO7A gene also carried rare variants these genes. Our findings reveal a co-segregation of rare variants in the MYO7A gene and other structural myosin VIIA binding proteins involved in the tip and ankle links of the hair cell stereocilia. We suggest that recessive digenic inheritance involving these genes could affect the ultrastructure of the stereocilia links in familial MD.
Fig. 1
Nine MD families carrying rare variants in the MYO7A gene. Variants in MYO7A found in this study indicated by protein nomenclature and Sanger sequencing chromatograms are displayed under each family. Solid squares (male) and circles (female) indicate patients with definite MD. Those patients with only vertigo or hearing loss are indicated, respectively, with the upper or the lower half of their symbols filled. “0/1”: heterozygous variant. “0/0”: homozygous for the reference allele. “?/?”: Sample not available.
Funding: This project was partially funded by H2020-SC1-2019-848261 (UNITI) and Andalusian Regional Government CECEU PY20-00303 (EPIMEN).
ST0126Abstract
Ménière’s disease (MD) is a debilitating disorder characterized by episodic vertigo, fluctuating low-frequency hearing loss, ear fullness, and tinnitus. A dissociation between two vestibular function tests that are used in the diagnosis of MD and examine the same end-organ—the caloric response test and video head impulse testing (vHIT)—has recently emerged. Caloric responses are often abnormal, while vHIT results remain normal. Here, we conduct a histopathological study using temporal bone specimens (N = 58) to examine the nature of this dissociation. We find otolith membrane herniation into the lateral semicircular canal in 61% of MD ears. Notably, 90% of ears with this herniation also had a diminished caloric response, while no ear with a normal response had this herniation. This represents the first time that herniation seen on temporal bone histopathology has been associated with abnormal caloric responses. Moreover, we evaluated the semicircular canals for endolymphatic hydrops, which has been hypothesized to contribute to the testing dissociation. We found no evidence of duct dilation but did note a novel morphological finding—smaller bony labyrinth cross-sectional dimensions in two of the three canals. The resulting membranous duct-to-canal ratio was larger in MD ears compared to controls. Examining this vestibular testing dissociation and further describing histologic characteristics in MD has implications for diagnosis and paves the way for future studies in further elucidating the pathophysiology of Ménière’s disease.
ST0069Cortical Regions Activated by Galvanic Vestibular Stimulation in Humans
Enrique Soto1, Joaquin Hernández1, Samuel Montero2, Felipe Orihuela-Espina2,3, Rosario Vega1
1Benemérita Universidad Autónoma de Puebla. 2Instituto Nacional de Óptica Electrónica y Astrofísica. 3University of Birmingham (UK)
Vestibular Galvanic Stimulation (GVS) has been used in devices to stabilize subjects when balance and posture are compromised. The cortex uses vestibular system input integrated with visual and proprioceptive input, to generate a subjective percept of self-movement. In this work, we intend to define the cortical regions that are activated by GVS in normal subjects. For this, the Functional Near-Infrared Spectroscopy (fNIRS) technique was used to study the action of GVS on the cerebral hemodynamic response. 18 clinically healthy volunteers were included. Every subject participated in four sessions (72 recording sessions in total) in a crossover experimental design. Participants’ heart rate, blood pressure, body temperature, head capacitance, and resistance were measured before and after each session. Subjects were subject to GVS with the cathode located in the right mastoid and the anode in the fronto-polar point. The GVS consisted of 2 mA DC-current amplitude and a duration of 10 s. False GVS (sham), hand vibration (neutral stimuli), and passive movement (positive control) were also used to compare the hemodynamic response to GVS with those other conditions, all of them presented in a randomized manner within the study. The hemodynamic recording of the cerebral cortex was performed with fNIRS over an arrangement of 26 channels, grouped into four regions: primary somatosensory cortex, associative somatosensory, upper and middle temporal of the left cerebral hemisphere, and upper and middle temporal of the right cerebral hemisphere. A ROI-level analysis was performed.
From subject- and group-level analyses, we determined the extent of HbO2 and HbR responses. Through the ROI analysis, the left temporal and posterior parietal regions were the less and most active areas during the experiments. Similar significant responses for positive control and GVS stimuli were found on the right temporal, anterior and posterior parietal regions. Sham and vibrational conditions did not generate significant changes ROI-wise. Regarding physiological parameters (blood pressure, heart rate, and temperature), no significant variations were found to be produced by GVS, corroborating that its use is safe, and can be used in prosthetic devices.
For the first time, we report that hemodynamic response in the cerebral cortex is similar when GVS and back and forth movement is applied. Our results lend further support to the possibility of using GVS in vestibular prosthetic devices.
ST0070Effect of Electric Field Stimulation (EEC) on the Activation Potential Discharge of Vestibular Primary Afferent Neurons in the Rat.
Rosario Vega, Sergio Benavides y Enrique Soto
Instituto de Fisiología, Benemérita Universidad Autónoma de Puebla, México
Galvanic Vestibular Stimulation (GVS) has aroused interest due to its potential use in auxiliary devices to correct posture, also in virtual reality systems, and in the correction of motor responses under microgravity (Soto et al., 2020). We studied the effects of electric field stimulation in the isolated vestibule of the rat to define the cellular mechanisms and parameters of stimuli that were relevant for GVS. For the experiments, Long-Evans C2 rats of 14-17 postnatal days were used. The isolated vestibule was maintained with constant perfusion with oxygenated Tyrode, maintained at 37.5 °C. The multiunit activity of the fibers from the anterior semicircular canal were recorded by means of a suction electrode. For the electrical stimulation, an arbitrary function generator and constant current linear isolation unit were used. Electrodes consisted of two platinum plates placed at the recording chamber with about 3 cm between them. Kruskal-Wallis and Mann-Whitney U-test were used to determine statistical differences. Shapiro-Wilk normality test were used for statistical analysis.
Initially, we studied the influence of the stimulus waveform (DC, sinusoidal, and white noise), on the discharge of vestibular afferent neurons. DC stimuli (20 s) elicited an initial discharge rate increase whose amplitude depends in a sinusoidal form on the intensity of the stimulus (half excitatory at 30 µA) and is followed by an adaptation process that decreases discharge rate towards basal level, at the end of stimulus an inhibitory period was produced. Sinusoidal stimulation produced a phase-locked increase in discharge rate which reached a maximal at 1 Hz, decays towards higher frequencies of stimulation, and shows no adaptation. By maintaining a constant frequency of stimulation (1 Hz) and increasing amplitude from 10 to 100 µA, the response shows a sigmoidal growth which is significant above 30 µA. Notably, white noise stimulation a sustained discharge throughout the stimulation period (20 s) was elicited, with an increase in the spike activity which shows a sigmoidal dependence on the stimulus amplitude (half excitation reached at 160 µA) and saturated at above 250 µA.
These results show that waveform and amplitude have a significant influence on the discharge rate and in the characteristics of the response of the vestibular afferent neurons to electrical field stimulation. This indicates that GVS used in subjects may critically depend on waveform, frequency, and amplitude of the stimuli thus offering an ample opportunity for vestibular system modulation by GVS.
16.00 Selected Poster presentation
ST0065Visual-inertial heading perception: Effect of heading direction, offset, and visual field size on multisensory integration and perception of common causation
Benjamin T. Crane1,2,3, Raul Rodriguez3
University of Rochester. Departments of Otolaryngology1, Neuroscience2, and Bioengineering3
Visual and inertial cues are the sensory modalities for heading determination. The visual cue is ambiguous as it can represent either self-motion through a fixed environment or environmental motion. When there are offsets between visual and inertial headings, it is only appropriate to integrate them when they are both due to motion through a fixed environment, a situation known as common causation. Difference in heading direction is one factor that makes common causation less likely to be perceived, although surprisingly large differences can be perceived as common causation. We looked at the effects of visual field size, heading offset and direction on common causation and integration. Experiments were done using 102° of the horizontal visual field and 70° of the vertical visual field and these were compared with a visual field of 38° in both directions (11% size). Both inertial and visual stimuli consisted of 2s of synchronized motion. The visual stimulus consisted of a 70% coherence star field. Trial blocks included 12 possible visual and inertial headings which covered the full 360° range in the horizontal plane in 30° increments. Every heading combination was presented in random order with 144 stimuli per block. A dial was used to report the perceived direction of the visual or inertial heading and buttons were pressed to report if the headings were the same or different. Six trial blocks were performed per subject, in 3 blocks inertial heading was reported and in 3 visual heading was reported. In all 6 blocks subjects reported if headings were the same or different. Greatly diminishing the visual field size and removing peripheral vision had a surprisingly small effect on visual direction determination or common causation perception. The lateral component of non-cardinal visual headings (e.g. 30°, 60°) was over-estimated by about 20°. Perception of common causation was also very similar to a full field with common causation which was highest when stimuli were aligned in cardinal directions and very low when stimuli were separated by 90° or more. When offset, visual headings continued to have a large influence on inertial heading perception – 10° with a 30° offset, 8° with 60-90° offsets, and 3° with a 120-150° offset. These were smaller than the offsets seen with the full visual field (13° with a 30° offset, and 13-19° with 60-120° offsets. The inertial stimulus influence on the visual stimulus was minimal (<2°) in both conditions.
ST0066Diagnosis of inner ear disorders using MRI -from animal study to clinical application
Maoli Duan1, Jun Yang2
1Department of Otolaryngology Head and Neck Surgery & Audiology and Neurotology and Department of Clinical Science, Intervention and Technology, Karolinska Institute, Stockholm, Sweden, 2Department of Otolarynggology Head and Neck Surgery, Shanghai Xinhua Hospital, Shanghai Jiaotong University, China
We have performed MRI scanning from in vitro to in vivo animal study and found that the method is useful mean to diagnose inner ear disorders using 4.7 Tesla MRI. The important findings are that Gd cannot enter endolymph but perilymph. We further expanded the findings to patient study using 3.0 Tesla MRI and found that Gd cannot enter endolymph but enter easily in perilymph. Thus, the findings provide critical means to diagnose inner ear diseases.
ST0089The effect of a customized vestibular rehabilitation programme with and without additional dual-task training on treatment outcome in persons with a chronic vestibular disorder. A randomised controlled trial.
Viktoria Azoidou1, Doris-Eva Bamiou2, Louisa Murdin3, Marousa Pavlou1
1Centre for Human and Applied Physiological Sciences, King’s College London, London, United Kingdom, ; 2Neuro-otology Department, National Hospital for Neurology and Neurosurgery, and Ear Institute, University College London, London, United Kingdom, ; 3Audiovestibular Medicine Department, Guy’s Hospital, Guy’s and St Thomas NHS Foundation Trust, London, United Kingdom, ; 1Centre for Human and Applied Physiological Sciences, King’s College London, London, United Kingdom, .
Background: Dual-tasking (DT) training (e.g. incorporating various balance and/or gait exercises with a secondary cognitive or auditory task) has been used in balance programmes for older adults at risk of falling, stroke patients and persons with Parkinson’s disease and multiple sclerosis. No studies up to date, have investigated the efficacy of DT training in persons with a chronic vestibular disorder.
Methods: A single-blinded randomized controlled trial investigated the effect of a 12-week customized vestibular rehabilitation (VR) programme incorporating cognitive and auditory DT exercises in 39 persons with chronic vestibular symptoms, aged 18-80 years old, who were randomly allocated to VR without (Group A) or with cognitive DT exercises (Group B). Treatment response was assessed at baseline and end of treatment. Primary outcome measure was Functional Gait Assessment (FGA) and FGA DT with Numeracy, Literacy and Auditory tasks. Secondary outcome measures included physical activity levels and cognitive function assessed with Axivity Wrist Band 3Axis logging accelerometer and Cambridge Neuropsychological Test Automated Battery, respectively, MiniBESTest, and questionnaires for vestibular symptoms and symptom triggers, balance confidence, self-perceived beliefs about health-state and illness, sleep and psychological state. Statistical significance was set at p<0.05.
Results: This study is ongoing. Group A included 19 participants (9 females, mean age ±SD= 53.05±12.51 years) while Group B included 20 participants (14 females, mean age ±SD= 43.70±15.08 years). Significant within-group improvements were noted in Group A for FGA Literacy and Numeracy (17.78±5.48 versus 23.89±7.64, 19.00±5.22 versus 23.22±6.12, respectively) and Group B for FGA Auditory, Numeracy and Literacy (22.44±5.10 versus 26.11±5.88; 16.33±4.87 versus 23.22±6.06; 18.67±5.03 versus 24.44±5.48, respectively). Group B showed significant improvement for patients’ perceived dizziness (47.25±13.90 versus 26.75±18.20), vertigo (0.81±0.59 versus 0.55±0.50), and visually induced dizziness (1.55±0.93 versus 1.12±1.09). Group B showed trends for improvement in cognitive domains examining visual memory and new learning (79.30±26.13 versus 82.1±8.95; 24.60±18.39 versus 16.50±15.28, respectively).
Conclusions: Preliminary data suggests that the addition of DT exercises to a VRT programme may be useful for improving specific cognitive domains associated with visual memory and new learning in people with a vestibular disorder. Practising DT exercises may provide a greater change in patients’ perceived handicap from dizziness, vertigo symptoms and visually induced dizziness. Numeracy and Literacy cognitive DT FGA performance does not appear to require additional DT exercises to improve.
ST0090Enrichment of Missense Variants in Axonal Guidance Signalling-related genes in Sporadic Meniere’s Disease cases
Alvaro Gallego-Martinez1, Teresa Requena1, Pablo Roman-Naranjo1, Patrick May2, Jose A Lopez-Escamez1,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain; 2Bioinformatics core, Luxembourg Centre for Systems Biomedicine, University of Luxembourg, Esch-Sur-Alzette, Luxembourg; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, Hospital Universitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain
Introduction: Meniere’s disease (MD) is a rare inner ear disorder defined by episodic vertigo, sensorineural hearing loss and tinnitus. MD is suspected to have an important genetic background. Although it has been mostly described in sporadic cases, around 10% of the observed individuals reports familial cases. It is associated with an accumulation of endolymph in the inner ear and the formation of endolymphatic hydrops, but the molecular mechanisms remain still unknown. However, it is suspected that supporting cells of the inner ear may be an important biological target for the disease. Previous studies detected that the main molecular pathways showing higher differentially expressed genes in the supporting cells are related to cochlea-vestibular neuronal innervation, cell-cell adhesion and leucocyte extravasation. In this study, our objective is to analyse a possible burden of rare variants in genes that interact with the main signalling pathways in supporting cells of the inner ear in patients with sporadic MD.
Methods: We designed a targeted-sequencing panel including genes related with the main molecular pathways in supporting cells and sequenced 860 Spanish patients with sporadic MD. We selected variants with minor allele frequencies <0.1 in the gene panel and were compared with three independent population reference datasets (CSVS for spanish population, GnomAD NFE for non-finnish european population and GnomAD ALL for global population). Variants were classified as loss of function, missense and synonymous. Missense variants with a combined annotation dependent depletion score (CADD) of >20 were classified as damaging missense variants. We calculated odds ratio for each gene in the panel for every group of variants in every population frequency dataset. Genes significantly enriched in our cohort for the different comparisons were ranked, pointing to which pathway was more represented by missense variant-enriched genes.
Results: We have observed a significant burden of damaging missense variants in few key genes, including the NTN4 and NOX3 genes, associated with axon guidance signalling pathways in patients with sporadic MD. We have also identified active subnetworks having an enrichment of rare variants in sporadic MD.
Conclusion: The enrichment of missense variants genes such as NTN4 and NOX3 suggests that axonal guidance signalling gene network could be a novel pathway involved in sporadic MD.
Acknowledgments: This study was funded by the Luxembourg National Research Fund Inter/Mobility/17/11772209 grant and EF-0247-2017 from Andalusian Health Government.
ST0131An explanation for individual variations in three-dimensional vestibular behavior
Chengqi Wang (a), Amsal Madhani (a), Faisal Karmali (a)
(a) Harvard Medical School / Massachusetts Eye and Ear, Boston, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Many vestibular patients complain of inappropriate perceptions of three-dimensional motion, and subjectively there are differences even amongst vestibular-normal individuals. In this study, we used computational models to begin to develop hypotheses for the physiologic reasons for these variations. It is well accepted that the vestibular organs are imperfect, yet the brain is able to synthesizes a robust estimate of three-dimensional motion and orientation in most individuals. Computational models accurately describe these central processes. A growing body of computational and experimental evidence suggests that these central processes are adaptatively adjusted to minimize error – i.e., optimize in a Bayesian sense - based on the statistics of vestibular neural noise (i.e., variability) and experienced motion. For example, we have previously used this approach to study changes with aging and peripheral damage that occur in the yaw angular velocity. In this case, while a longer time constant would be advantageous because this would make the VOR accurate over a longer period of time, it has been argued that this would result in the accumulation of noise by the velocity storage mechanism, which would result in drift and make the VOR less precise. In this study, we extended these results to three-dimensional processing. The first behavior we studied was post-rotatory tilts - 45 deg tilts of the body following the cessation of constant-velocity upright yaw rotation. As in previous studies, we used perceptual thresholds and signal detection theory to estimate vestibular noise. We predicted responses that cover the normal range of human vestibular noise by using published data on the range of human thresholds. These predictions showed that changing only SCC noise resulted in substantial variations in estimates of angular velocity, linear acceleration and the direction of gravity. These inappropriate estimates of motion persisted for many seconds. The second behavior we studied was off-vertical axis rotation – constant-velocity rotation about an axis tilted relative to the vertical. These predictions showed that changing only SCC noise resulted in notable variations in estimates of angular velocity, minor variations in estimates of linear acceleration, and no variations in the estimates of gravity. These results provide a first step in explaining interindividual variations in three-dimensional vestibular responses and could lead to a better understanding of dizziness and vertigo.
Acknowledgements: Funded by NIH/NIDCD R01-DC018287.
SATELLITE - 8-SUNDAY
9:00:00 AM Scientific Session
ST0099Predictive Coding of Natural Self-Motion: Implications for Perception & Action
Click here to write
The Johns Hopkins University
A fundamental question in neuroscience is: How does the brain compute accurate estimates of our self-motion and orientation relative to the world to ensure accurate behavior and stabile perception in everyday life. In this talk, I will describe my laboratory’s recent research addressing this question. First, we have explored the statistics of natural self-motion signals experienced by mice, monkeys, and humans, and established the neural coding strategies used by early vestibular pathways to encode these natural stimuli. Next, I will explain how neurons at the first central stage of vestibular processing respond robustly to unexpected (externally applied) motion but not actively generated motion, as well our unpublished evidence that a cerebellar-based mechanism underlies this distinction. Importantly, our experiments have demonstrated that when unexpected vestibular inputs become persistent during active motion, this mechanism is rapidly updated to re-enable the vital distinction between active and passive motion. Taken together, our findings have important implications for our understanding of the brain mechanisms that ensure accurate perception and behaviour during everyday activities, including how motor-based predictions are dynamically updated as the relationship between a voluntary motor command and its sensory consequences changes.
Target audience - both Basic and Clincal Scientists
Satellite Symposium in Granada
entitled The Vestibular System: Beyond the Synapse
re-scheduled on May 7-8th 2022
Invited speaker
Abstract oral presentation (duration: 20 min):
Title: Robust repair process at primary vestibular synapses must not be omitted when considering the restauration of vestibular function following acute peripheral vestibulopathy
Aix Marseille University, CNRS, UMR 7260, Laboratory of Cognitive Neurosciences
State of art, state of the question: The question of the self-repair abilities of primary auditory synapses has long been the subject of debate in the hearing community, to determine whether and how far these synapses were able to repair following SHL or SNHL. This question is just as important for the vestibular sphere in a situation of acute peripheral vestibulopathy(APV) and beyond, with regard to vestibular aging which we know, may particularly affect these primary synapses.
To thoroughly study this phenomenon of spontaneous synaptic repair which takes place within the inner ear vestibular sensory epithelia, we selectively damaged the synaptic contacts between hair cells and primary vestibular neurons unilaterally in the adult mouse, and studied on the one hand, the functional consequences (through behavioral studies of equilibration and locomotion, and VOR monitoring), as well as its histological correlates (immunohistochemistry; Cassel et al. 2019).
Results: We demonstrate that i) selective vestibular synapse deafferentation of hair cells is sufficient to generate acute vestibular syndrome with characteristics similar to those reported in APV patients; ii) both the posturo-locomotor and VOR deficits recover within the first few days after the insult, while iii) a spontaneous repair process involving resynthesis and adressage of pre and post synaptic proteins, starts after a week, and allows the full reformation of primary synapses.
Conclusion: These observations i) confirm the ability of primary synapses to repair spontaneously following selective deafferentation, if hair cells are preserved, ii) raise questions about the role of the peripheral repair when vestibular compensation has occurred, and iii) on the pattern of the repaired network; iii) opens new avenues to preserve the primary vestibular synapses and stimulate their repair when damaged.
Cassel R, Bordiga P, Carcaud J, Simon F, Beraneck M, Le Gall A, Benoit A, Bouet V, Philoxene B, Besnard S, Watabe I, Pericat D, Hautefort C, Assie A, Tonetto A, Dyhrfjeld-Johnsen J, Llorens J, Tighilet B, Chabbert C. Morphological and functional correlates of vestibular synaptic deafferentation and repair in a mouse model of acute-onset vertigo. Dis Model Mech. 2019 Jul 15;12(7):dmm039115. doi: 10.1242/dmm.039115. PMID: 31213478; PMCID: PMC6679379.
ST0141Loss of stereocilia rootlet structure by TRIOBP deficiency causes progressive vestibular dysfunction
Shin-ichiro Kitajiri
Kitajiri Ear, Nose and Throat Clinic, Japan
Abstract
The actin filaments at the lower tapering end of stereocilia become densely packed to form rootlets that extend into the hair cell body. We previously reported that TRIOBP is an actin bundling protein required for the development of the stereocilia rootlet in cochlear hair cells. Triobp-4/5 deficient cochlear stereocilia lack rootlets and degenerate, causing deafness both in human and mice. In this study, we examined vestibular function for Triobp-4/5 deficient mice. In wild type mice, TRIOBP is also localized in the rootlet of vestibular hair cell stereocilia. In Triobp-4/5 deficient mice, rootlets of vestibular stereocilia do not develop, just as in cochlear hair cells, and yet Triobp-4/5 deficient mice appear to have normal balance behavior. Nevertheless, these mice have impaired gravity receptor function as measured by vestibular evoked potentials (VsEPs), a quantitative and direct measure of gravity receptor organs. VsEP response threshold, P1 latencies and P1-N1 amplitudes were quantified. At all examined ages, TRIOBP heterozygous mice had normal VsEP response. Despite profound hearing loss at an early age, TRIOBP homozygous mutant mice had measurable VsEPs until at least 80 days of age (P80). At 40 days (P40), these mice had significantly elevated thresholds, prolonged P1 latencies and smaller P1-N1 amplitudes. By P80, thresholds remained elevated, while P1 latencies become more prolonged than at P40. At 8 months and older, all homozygous mutant mice had no VsEPs. Scanning electron microscopy (SEM) showed a slowly progressing degeneration that was likely to be the cause of VsEP deficiency. Measurable VsEPs at P40 and P80 were consistent with normal behaviors for the mutant mice. Since the VsEPs do not disappear until sometime after 80 days of age, balance behaviors remained normal well into adulthood.
11.30 Scientific Session
ST0140Molecular Genetics in Familial Meniere disease in Spain
Jose Antonio Lopez-Escamez, Pablo Roman-Naranjo, Alvaro Gallego-Martinez, Lidia Frejo
Division of Otolaryngology, Department of Surgery, Universidad de Granada, Spain Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain
Objective: Familial Meniere Disease (FMD) is a polygenic disorder of the inner ear characterized by episodes of vertigo associated with sensorineural hearing loss, tinnitus and/or aural fullness. Segregation analyses and exome sequencing studies have identified ultrarare single nucleotide variants (SNVs) in 9 genes (FAM136A, DTNA, PRKCB, COCH, DPT, SEMA3D, OTOG, MYO7A and TECTA). Most of these genes have been reported in singular families—the exception being OTOG, MYO7A and TECTA genes.
Methods: We performed exome sequencing and bioinformatic analyses in 77 families with MD to evaluate the pathogenicity of each SNV and compared its allelic frequency with reference datasets to evaluate its role in the pathogenesis of FMD. By retrieving gene expression data in these genes from different databases, we could classify them according to their gene expression in neural or inner ear tissues. Finally, we evaluated the pattern of inheritance to conclude which genes show an autosomal dominant (AD) or autosomal recessive (AR) inheritance in FMD.
Results and conclusions: Our data suggest that rare missense SNVs in OTOG is the most common finding in Spanish families with MD. There are different models of inheritance including AD for FAM136A, DTNA, PRKCB, COCH, DPT, SEMA3D genes; compound recessive inheritance for the OTOG gene and digenic inheritance involving MYO7A and in the organization of the stereocilia links such as CDH23, PCDH15 or ADGRV1. The burden of rare variation in genes encoding proteins involved in the stereocilia or tectorial membrane structure (TM) suggests that changes in the TM micromechanics could influence the sound-evoked motion of stereocilia in familial MD.
Funding by CECEU P20_00303 (EPIMEN), B-CTS-68-UGR20 and CIBERER (CLASSIFI_ER)
FREE PAPER FORM
FP0936Drosophila Dyb Mutants show Meniere Phenotype with Hearing and Proprioception Defects
Teresa Requena1, Alyona Keder2, Joerg T. Albert2, Andrew P. Jarman1
1Centre for Discovery Brain Sciences, Edinburgh Medical School: Biomedical Sciences, University of Edinburgh, Edinburgh EH8 9XD, UK. 2Ear Institute, University College London, 332 Gray’s Inn Road, London, WC1X 8EE, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Introduction: Evidence from epidemiology suggests that Meniere’s disease (MD), an inner ear disorder defined by recurrent vertigo attacks, sensorineural hearing loss and tinnitus, present genetic susceptibility involving multiple genes. Although Dystobrevin (DTNA) appeared as the best candidate, there is no animal model to study the disease mechanisms. The fly’s ‘inner ear’, called Johnston’s organ (JO), is a chordotonal organ localized in the 2nd antennal segment, which mediates the sensation of hearing, gravity and wind. In Drosophila, DTNA orthologue Dyb is predicted to be part of the dystrophin-associated glycoprotein complex and is expressed in the auditory/proprioceptive chordotonal sensory organs.
Methods: In order to investigate whether Dyb causes an MD-like phenotype, we analysed Dyb null and RNAi knockdown flies. We collected F1 knockdown, KO and control flies. We evaluated proprioception through locomotory coordination using climbing assays in light and dark. We assessed JO auditory function in vivo using Laser Doppler Vibrometry. Immunohistochemistry confocal was performed to confirm the expression in antennae and to define the effect of the mutant allele.
Results: Dyb null mutants and RNAi knockdown flies showed normal mechanosensory (proprioception) under white light but they exhibited climbing defects when assayed in effective darkness (i.e. under red light conditions). In fact the climbing defect persists over time. The flies thus present a mild proprioception defect that can be compensated by visual input. In addition, Dyb mutant flies show a decrease in auditory active amplification in both males and females. Preliminary analyses of Dyb RNAi knockdowns using specific lines, narrow the cells involve in the MD-like phenotype to ligament and scolopale cells.
Conclusions: Our results support that disruption in Dyb mutant flies generates an MD-like phenotype with hearing and proprioception defects. Additionally, our results show that the flies’ sense of balance integrates both proprioceptive and visual information: the proprioceptive deficits that arise from a loss of Dyb function can be compensated by visual cues. However further analyses are needed to be carried out to understand the function and mechanisms of Dyb JO hearing and proprioception.
Funding: Funded by Marie Curie Intra-European Fellowship (H2020-MSCA-IF-2017-794651) and EMBO travel fellowship (EMBO-STF_6917).
13:30 Oral Presentation
SATELLITE FREE PAPERS FORM
ST0072Contralateral spreading of substances following intratympanic nanoparticle-conjugated gentamicin injection in a rat model
Sang-Yeon Lee1, Jeonghyo Kim2, Sangjin Oh2, Gaon Jung1, Jaebeom Lee2 and Ja-Won Koo1
1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea, 2Department of Chemistry and Department of Chemical Enginnering and Applied Chemistry, Chungnam National University, Daejeon, Korea
This study was performed to investigate the Eustachian tube as a potential route for contralateral spreading following intratympanic nanoparticle (NP)-conjugated gentamicin injection in a rat model. Sprague-Dawley rats were divided into three groups and substances were injected in the right ear: group 1 (fluorescent magnetic nanoparticles [F-MNPs], n = 4), group 2 (F-MNP-conjugated gentamicin [F-MNP@GM], n = 2), and control group (no injections, n = 2). T2-weighted sequences corresponding to the regions of interest at 1, 2, and 3 hours after intratympanic injection were evaluated, along with immunostaining fluorescence of both side cochlea. The heterogeneous signal intensity of F-MNPs and F-MNP@GM on T2-weighted images, observed in the ipsilateral tympanum, was also detected in the contralateral tympanum in 4 out of 6 rats, recapitulating fluorescent nanoparticles in the contralateral cochlear hair cells. Computational simulations demonstrate the contralateral spreading of particles by gravity force following intratympanic injection in a rat model. The diffusion rate of the contralateral spreading relies on the sizes and surface charges of particles. Collectively, the Eustachian tube could be a route for contralateral spreading following intratympanic injection. Caution should be taken when using the contralateral ear as a control study investigating inner-ear drug delivery through the transtympanic approach.
ST0112The effect of Galvanic vestibular stimulation on visuospatial cognition in bilateral vestibular deafferentation mouse model
Thanh Tin Nguyen1,3,6, Gi-Sung Nam2,3, Jin-Ju Kang3,4, Gyu Cheol Han5, Sun-Young Oh1,3,4
1Jeonbuk National University College of Medicine, Jeonju, South Korea. 2Department of Otorhinolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Kwangju, South Korea. 3Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea. 4Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, South Korea. 5Department of Otolaryngology-Head and Neck Surgery, Gachon University of Medicine and Science, Graduate School of Medicine, Incheon, South Korea. 6Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam.
Objectives: To investigate the efficacy of galvanic vestibular stimulation (GVS) for recovery from the deficits of locomotor and spatial memory functions in bilateral vestibular deafferentation (BVD) mouse model.
Methods: Thirty-six male C57BL/6 mice were allocated into two experimental groups of BVD with (BVD_GVS group) and without GVS intervention (BVD_non-GVS group), and a control group. We assessed the locomotor and cognitive behavioral function before (baseline) and 3, 7 and 14 days after surgical bilateral labyrinthectomy, using the open field (OF), Y maze, and Morris water maze (MWM) tests. For the GVS group, a sinusoidal current at the frequency at 1 Hz and amplitude 0.1 mA was delivered for 30 minutes daily from the postoperative day (POD) 0 to 4 via the electrodes inserted subcutaneously close to both bony labyrinths.
Results: Short-term spatial memory were significantly impaired in the bilaterally labyrinthectomized mice (BVD_non-GVS group) reflected by decreased spontaneous alternation performance (SAP), place recognition test (PRT) and time-spent in novel arm as well as by increased same arm return (SAR) compared to the control. The long-term spatial memory was also impaired during the MWM indicated by longer escape latency in hidden platform trial and lower percentage of time spent in target quadrant in probe trial. GVS application significantly accelerated recovery of locomotion, and the short-term and long-term spatial memory deficits in bilateral vestibular deafferentation (BVD) mice.
Conclusions: Our data demonstrated that locomotion, short-term and long-term spatial memory were impaired in BVD mice last longer than 2 weeks. Early administration of sinusoidal GVS could partially accelerate recoveries of locomotion and spatial memory deficiencies. GVS may be applied in the patients with BVD to improve their locomotion and vestibular cognitive functions.
ST0120Isolated Otolith Dysfunction in Persistent Postural-Perceptual Dizziness
Toshihisa Murofushi, Koji Nishimura, Masahito Tsubota
Department of Otolaryngology, Teikyo University, School of Medicine, Mizonokuchi Hospital
Background: There are many patients suffering from chronic floating dizziness. Most of them have been remained undiagnosed. Recently, assessment tools of vestibular function such as vestibular evoked myogenic potential test (VEMP) and video head-impulse test (vHIT) have been developed. Also, a new clinical entity, postural-perceptual dizziness (PPPD), has been proposed with its diagnostic criteria (2017). Because the main symptom of PPPD is non-spinning dizziness, association between PPPD and otolith organ dysfunction is likely. However, otolith organ function in PPPD has not been extensively studied.
Objectives: The aim of this study is to clarify otolith organ dysfunction in PPPD patients, especially isolated otolith organ dysfunction (with preserved semicircular canal function).
Methods: Twenty-one patients diagnosed with having PPPD were enrolled into this study. Subjects filled questionnaire (DHI, Niigata PPPD questionnaire = NPQ) and underwent pure-tone audiometry, VEMP testing, vHIT and stabilometry.
Results: Majority of subjects had vestibular dysfunction. Nine of the 21 subjects showed isolated otolith organ dysfunction (decreased otolith organ function with preserved semicircular canal function). Two patients had isolated canal dysfunction while 4 did both of otolith organ and canal dysfunction. Six patients did not show dysfunction of otolith organ or canal.
Conclusions: PPPD seems to have close relationship with otolith dysfunction.
ST0079Simulations of BPPV Maneuvers: Three Dimensional Visualization to Understand and Improve Management
Anita Bhandari1, Rajneesh Bhandari2, Herman Kingma3,4,5, Michael Strupp6
1(ENT) Vertigo and Ear Clinic, India2 NeuroEquilibrium Diagnostics, Jaipur, India3 Department of Ear Nose Throat, Maastricht University, Maastricht, Netherlands
4Faculty of Physics, Tomsk State National Research University, Tomsk, Russia, 5Department of Ear Nose Throat, Aalborg University, Aalborg, Denmark, 6Department of Neurology and German Center for Vertigo and Balance Disorders, Hospital of the Ludwig Maximilians University Munich, Germany
Background and Objectives: BPPV is a mechanical disorder of the inner ear. This study aims to show how 3D dynamic simulation models of BPPV can help to visualize the movement of the debris within the canals during head movement. This can be used for a better understanding of the theoretical efficacy of maneuvers and help in development of new maneuvers to treat different BPPV variants.
Methods: Based on reconstructed MRI images and fluid dynamics, a 3D dynamic simulation model (as a function of time) was developed and applied. Maneuvers used to treat canalithiasis affecting the posterior, horizontal and anterior canals were studied.
Results: 3D visualization of the canals linked to head movement displays the importance of each step of various maneuvers to bring the affected canal at an angle at which gravity can act best. The simulations have shown how the Semont’s Plus maneuver and Modified Yacovino maneuver improve the efficacy of the previously described maneuvers. Some maneuvers, like the Gufoni maneuver for apogeotropic ampullary arm Horizontal canal BPPV, have been shown to be less effective in particle repositioning while the 3600 roll and Zuma maneuver were seen to be effective for all hc-BPPV variants.
Conclusions: The 3D simulations for movement of the otoconia debris can be used to test the mechanism of action and the theoretical efficacy of existing maneuvers for the different BPPV variants. It can provide a visual explanation for the need of specific maneuvers for each type of BPPV. The simulator software can help in optimizing maneuvers along with eliminating incorrect and unnecessary steps.
ST0087Meniere’s disease: different mechanisms for hydrops and implication of treatments – an update
Anki Pålbrink2, René in t’Zandt3, Mikael Karlberg1, Fredrik Tjernström1, Eva Degerman2
1Dept of clinical Sience, Section of Otorhinolaryngology 2Dept of Experimental Medical Science.3Lund University Biomedical Imaging Center.Lund University, Skane University Hospital, Lund, Sweden
The course and symptoms in Meniere’s disease is highly variable. While some patients have a high frequency of attacks and continuous symptoms, other have sporadic attacks and others again go into remissions that last for years. The responses to different treatments are similar. While one patient may respond to a certain treatment, this may not help another. This holds true for most non-destructive approaches. Actually, the literature report most treatments seems to have a success rate of about 2/3rd. which, resembles the number going into spontaneous remission when observed for several months. We can thus suggest the “two-third problem” in Meniere’s disease. The heterogenicity of treatment responses, the number of different treatments suggested and the variety in the spontaneous course and in symptoms, may lead to a suspicion that there is either more than one etiology causing similar symptoms and/or that this is actually more than one disorder.
Meniere’s disease is suggested to be related to endolymphatic hydrops, and it is now possible to visualize the endolymphatic compartment with MRI after either an i.v. or intratympanical administration of gadolinium.
As we have encountered, developing an experimental model creating a hydrops in mice, visualizing it with a 9,4T animal MRI system with specially developed sequences, there seem to be different mechanisms to develop hydrops. Even on a cellular level. This has implication on the treatment regime.
Here, we will present an overview on treatments relative etiology of Meniere’s disease or hydropic inner ear disease, as based on present knowledge and experience. We will suggest that the new data seems ro suggests an open minded approach to the patients and and a multii modal therapeutic approach.
14.30 Selected Poster presentation
ST0103Sensitivity and Stimulation Characteristics of the Mammalian Vestibular short-latency Evoked Potential
Christopher J. Pastras1, Ian S. Curthoys2, Daniel J. Brown3
1School of Medical Sciences. The University of Sydney. 2Vestibular Research Laboratory, The University of Sydney. 3School of Pharmacy and Biomedical Science, Curtin University
The Vestibular short-latency Evoked Potential (VsEP) has been used as an objective measure of vestibular nerve function and represents the synchronous firing of vestibular primary afferents to the onset of motion. It was first termed the short latency vestibular evoked potential by Elidan et al. in 1982 due to its similarity to the auditory brainstem evoked potential. Since then, the VsEP has been measured in various vertebrate models and preparations; the most common being a non-invasive, scalp recording to linear-jerk pulses. This approach is attractive for several reasons, such as the ability to measure vestibular nerve function in chronic recovery animal models without disturbance of the labyrinth. However, with the cochlea intact, this approach is prone to auditory contamination, making interpretation difficult. Given the increased popularity of the VsEP in recent years, it’s important to validate key features of the response for future interpretation and use. This work aimed to characterise the near-field VsEP recorded close to the vestibular afferents from facial nerve canal in anaesthetized guinea pigs. Linear-jerk pulses of varying widths (~0.1-3ms) were used to evoke the VsEP and were compared to responses with the cochlea intact, before and after controlled experimental manipulations, such as acoustic-masking, changes in stimulation rate, and cochlear ablation. Responses from the facial nerve canal were also compared to the vertex. Responses evoked by a 2ms jerk pulse were not suppressed by acoustic forward-masking but were significantly masked using continuous broadband noise. Changing the stimulation rate was used to characterise differences in cochlear and vestibular neuronal forward masking. With the cochlea intact, 50% of the response was forward-masked with a stimulation rate of 60Hz, whereas the response after cochlear ablation did not forward-mask. Overall, surgical ablation of the cochlea revealed significant cochlear contribution of the response across all linear-jerk pulse widths. An iso-acceleration, iso-jerk, and iso-VsEP paradigm was used to probe the kinematic vector sensitivity of the VsEP. Surprisingly, results indicate that the VsEP scales with linear acceleration of the earbar, rather than kinematic jerk. Interestingly, responses with the cochlea intact from both the facial nerve canal and vertex, scaled with kinematic jerk, rather than acceleration. This work reveals new findings that call into question the original interpretation of the sensitivity and stimulation characteristics of the mammalian VsEP.
The target audience is basic vestibular researchers; however, we believe this work will be of interest to a wide readership such as clinicians.
ST0108Galvanic Vestibular Stimulation Improves Spatial Cognition After Unilateral Labyrinthectomy in Mice
Thanh Tin Nguyen1,2,3†, Gi-Sung Nam2,4†, Jin-Ju Kang2,5, Gyu Cheol Han6*, Ji-Soo Kim7, Marianne Dieterich8,9,10 and Sun-Young Oh1,2,5*
1Jeonbuk National University College of Medicine, Jeonju, South Korea. 2Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea. 3Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam. 4Department of Otorhinolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Kwangju, South Korea. 5Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, South Korea. 6Department of Otolaryngology-Head and Neck Surgery, Graduate School of Medicine, Gachon University of Medicine and Science, Incheon, South Korea. 7Department of Neurology, Seoul National University Hospital & School of Medicine, Seoul, South Korea. 8Department of Neurology, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany. 9German Center for Vertigo and Balance Disorders-IFB, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany. 10Munich Cluster for Systems Neurology (SyNergy), Munich, Germany.
Objectives: To investigate the deficits of spatial memory and navigation from unilateral vestibular deafferentation (UVD) and to determine the efficacy of galvanic vestibular stimulation (GVS) for recovery from these deficits using a mouse model of unilateral labyrinthectomy (UL).
Methods: Thirty-six male C57BL/6 mice were allocated into three groups that comprise a control group and two experimental groups, UVD with (GVS group) and without GVS intervention (non-GVS group). In the experimental groups, we assessed the locomotor and cognitive behavioral function before (baseline) and 3, 7, and 14 days after surgical UL, using the open field (OF), Y maze, and Morris water maze (MWM) tests. In the GVS group, the stimulations were applied for 30 min daily from postoperative day (POD) 0–4 via the electrodes inserted subcutaneously close to both bony labyrinths.
Results: Locomotion and spatial cognition were significantly impaired in the mice with UVD non-GVS group compared to the control group. GVS significantly accelerated recovery of locomotion compared to the control and non-GVS groups on PODs 3 (p < 0.001) and 7 (p < 0.05, Kruskal–Wallis and Mann–Whitney U tests) in the OF and Y maze tests. The mice in the GVS group were better in spatial working memory assessed with spontaneous alternation performance and spatial reference memory assessed with place recognition during the Y maze test than those in the non-GVS group on POD 3 (p < 0.001). In addition, the recovery of long-term spatial navigation deficits during the MWM, as indicated by the escape latency and the probe trial, was significantly better in the GVS group than in the non-GVS group 2 weeks after UVD (p < 0.01).
Conclusions: UVD impairs spatial memory, navigation, and motor coordination. GVS accelerated recoveries in short- and long-term spatial memory and navigation, as well as locomotor function in mice with UVD, and may be applied to the patients with acute unilateral vestibular failure.
ST0114Using Mouse Behavioral Models for Assaying Vestibular Efferent Function
Anjali Sinha1,2, Natalie B. Dang1, Choongheon Lee1, Joseph C. Holt1,2,3
1Department of Otolaryngology, University of Rochester, Rochester, NY, United States, 2Department of Neuroscience,University of Rochester, Rochester, NY, United States, 3Department of Pharmacology & Physiology,University of Rochester, Rochester, NY, United States
The efferent vestibular system (EVS) in mammals starts as a small number of bilateral, multipolar neurons in the dorsal brainstem. Axons of contralateral and ipsilateral vestibular efferent neurons (VENs) travel to multiple vestibular end organs on each side and extensively branch to give rise to an abundance of synaptic varicosities on hair cells and afferent terminals. While electrical stimulation of mammalian VENs in the laboratory setting profoundly modulates both the resting discharge and sensitivity of vestibular afferents, the functional framework, for how and when the mammalian EVS is employed under normal physiological conditions, is poorly understood. Pharmacological data regarding EVS actions in mice from our lab have characterized a number of cholinergic synaptic mechanisms that underlie the responses of vestibular afferents to efferent stimulation, including multiple muscarinic and nicotinic acetylcholine receptors. Some of our interest in performing vestibular studies in mice was having access to transgenic animals where these specific EVS synaptic mechanisms, implicated by our pharmacological data, have been disrupted. These mice are likely to present with distinct vestibular phenotypes that can be characterized in both electrophysiological and behavioral assays.
The utility of such an approach is highlighted by a number of recent observations made in mice where the alpha9 nicotinic acetylcholine receptor subunit (α9nAChR-KO) has been altered. Loss of functional α9nAChRs in α9nAChR-KO animals is associated with modifications in the response properties of vestibular afferents that likely give rise to changes in the vestibulo-ocular reflex (VOR), vestibular sensory evoked potential (VsEP), and vestibulo-autonomic pathways. For further insight into EVS function, we have recently employed a suite of behavioral assays that might reveal vestibular deficits in transgenic mice missing critical EVS signaling components. As our first test, we probed if α9nAChR-KO animals, relative to their controls (α9nAChR-WT), behave differently before and/or after being subjected to a provocative vestibular stimulus. Postural sway and center of pressure (COP) measurements were made on a miniature force plate from α9nAChR-WT and α9nAChR-KO mice before and after a 5-min rotation at 125 RPMs on an orbital shaker. Before stimulation, both groups of mice readily explored the confines of the force plate and exhibited comparable COP metrics. In the poststimulus period, however, α9AChR-KO mice displayed a striking reduction in their movement on the force plate which was often associated with a significant compression of postural sway space, bouts of immobilization along the corners and walls of the plate enclosure, and reduced point-to-point movements. Interestingly, older α9nAChR-KO, but not WT, animals exhibited similiar mobility phenotypes during the prestimulus period which may point to interactions among aging, stress, and vestibular function.
ST0118How peripheral vestibular damage affects velocity storage
Amsal Madhani1, Richard F. Lewis1,2,3, Faisal Karmali1,3
1Jenks Vestibular Physiology Laboratory, Massachusetts Eye and Ear Infirmary, Boston, MA. 2Department of Neurology, Harvard Medical School, Boston, MA. 3Department of Otolaryngology, Harvard Medical School, Boston, MA.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Velocity storage is a centrally-mediated mechanism that processes peripheral vestibular inputs. One prominent aspect of velocity storage is its effect on dynamic responses to yaw rotation. Specifically, when normal human subjects are accelerated to constant angular yaw velocity, horizontal eye movements and perceived angular velocity decay exponentially with a time constant circa 15-30 s, even though the input from the vestibular periphery decays much faster (~ 6 s). Peripheral vestibular damage causes a time constant reduction, which is useful for clinical diagnoses, but a mechanistic explanation for the relationship between vestibular damage and changes in these behavioral dynamics is lacking. It has been hypothesized that Bayesian optimization determines ideal velocity storage dynamics based on statistics of vestibular noise and experienced motion. Specifically, while a longer time constant would make the central estimate of angular head velocity closer to actual head motion, it may also result in the accumulation of neural noise which simultaneously degrades precision. Thus, the brain may balance these two effects by determining the time constant that optimizes behavior. We applied a Bayesian optimal Kalman filter to determine the ideal velocity storage time constant for unilateral damage. Predicted time constants were substantially lower than normal, similar to patients, and modeled interactions between age-related hair cell loss and peripheral damage. These results provide a mechanistic explanation for changes in velocity storage after peripheral damage. Results also suggested that even after peripheral damage, ipsilateral noise originating in the periphery or early central processing remains relevant in neurocomputations. Overall, our findings support the hypothesis that the brain optimizes velocity storage based on the vestibular signal-to-noise ratio.
ST0119Proposed Diagnostic Criteria for Definite Isolated Otolith Dysfunction
Myung-Whan Suh1, Toshihisa Murofushi2
1Department of Otolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea; 2Department of Otolaryngology, Teikyo University School of Medicine Mizonokuchi Hospital, Kawasaki, Japan Address for correspondence Myung-Whan Suh, MD, PhD Department of Otorhinolaryngology-Head and Neck
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and objectives: Dizzy patients with abnormal otolith function tests, despite a normal caloric response, are defined as having specific (isolated) otolith organ dysfunction. This study was performed to compare the differences in clinical presentation between isolated otolith dysfunction (iOD) patients with lab- and Sx-based iOD group and lab-based iOD symptoms.
Subject and methods: The medical records of 23 iOD patients with normal caloric response but abnormal cervical vestibular evoked myogenic potential (VEMP), ocular VEMP, or subjective visual vertical were reviewed. Non-spinning vertigo was considered as otolith-related symptoms. The patients’ age, onset of dizziness, Numeric Rating Scale on the severity of dizziness, and concomitant vestibular disorders were analyzed.
Results: Patients in the lab-based iOD group were significantly older than those in the lab- and Sx-based iOD group. Known vestibular disorders were significantly more common in the lab-based iOD group (83.3%) compared to the lab- and Sx-based iOD group (18.2%). Despite the normal caloric response, catch-up saccade was found in the video head impulse test in more than half (54.5%) of the lab-based iOD group patients. There was no catch-up saccade in the lab- and Sx-based iOD group. There were no significant differences in gender ratio, frequency of dizziness attacks, and duration of illness.
Conclusions: We propose new definitions of definite iOD (lab- and Sx-based iOD) and probable iOD (lab- or Sx-based iOD). These new definitions may help researchers to identify patients who are more likely to have true iOD, and facilitate comparisons of results between different studies.
SATELLITE - 09-MONDAY
SY0040Session title: Application of AI & VR for Diagnosis & Management of vestibular disorders
Organizer: Kyu-Sung Kim, Chairman of Korean Balance Society,
(Professor, Department of Otorhinolaryngology-Head and Neck Surgery, Inha University College of Medicine, Korea)
1. Nystagmus classification system using deep learning. Sung Kwang Hong (Professor, Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Anyang, Korea)
2. Automatic algorithm of gait/vestibular function-related fall risk problems in vestibular disease using machine learning. Hwan Ho Lee (Professor, Department of Otorhinolaryngology-Head & Neck Surgery, Kosin University College of Medicine, Korea)
3. Development of Software for Diagnosis and Treatment of Benign Paroxysmal Positional Vertigo. Ji-Soo Kim (Department of Neurology, Seoul National University College of Medicine, Seoul, South Korea)
4. Vestibular rehabilitation with virtual reality: Visual stimulation in PPPD. Seo-Young Choi (Professor, Department of Neurology, College of Medicine, Pusan National University, Pusan National University Hospital)
5. Wearable device for dizziness using AR/VR. Jae Jun Song (Professor, Department of Otorhinolaryngology-Head & Neck Surgery, College of Medicine, Korea University, Korea)
A brief description of the theme & target audience
Recently, a lot of progress has been made in the development of medical devices and diagnosis of diseases using the development of AI and VR. Therefore, this symposium aims to understand the recent trends and development of diagnostic devices and treatments currently being developed using AI and VR.
A 150-word abstract from each of the speakers
Abstract 1
Nystagmus classification system using deep learning.
Sung Kwang Hong (Professor, Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Anyang, Republic of Korea)
Artificial intelligence indicates the simulation of the human’s cognitive abilities using computers or machines, such as learning and problem solving, to perform tasks similar to humans, accomplished by the “machine learning” technology. Machine learning technology has been increasingly used in the medical field with its significant benefits. The paring of neurotologic data and AI might create a new paradigm in diagnosis and treatment in neurotologic fields. We have developed the automatic nystagmus classification algorithm using deep learning. The main focus of this talk is to introduce our system for nystagmus classification and clinical applications in the neurotologic domain.
Abstract 2
Automatic algorithm of gait/vestibular function-related fall risk problems in vestibular disease using machine learning.
Hwan Ho Lee (Department of Otorhinolaryngology-Head & Neck Surgery, Kosin University College of Medicine)
The vestibular disorders can cause several fatal diseases, such as depression and fall. Specifically, patients with balance disorders and dizziness by vestibular disorders are 2.6 times and 12 times more likely to fall, respectively. Falls lead to more than 80% of all elderly deaths. Our main contribution lies in developing the first machine learning framework that predicts vestibular disorders and their types employing gait patterns such as musculoskeletal disorders, Parkinson’s disease. We employed the XGBoost algorithm, which was the most popular gradient boosted decision trees. For developing and evaluating our machine learning model, we collected gait patterns for health and vestibular disorder patients in Kosin hospital. Our machine learning model turns out to offer great performance on our evaluation dataset. Another contribution is that we explain which of the gait features is the most relevant to vestibular disorders. To this end, we exploit the explainable AI techniques such as feature importance and partial dependence plot.
Abstract 3
Development of Software for Diagnosis and Treatment of Benign Paroxysmal Positional Vertigo.
Ji-Soo Kim (Department of Neurology, Seoul National University College of Medicine, Seoul, South Korea)
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo. Appropriate canalith repositioning procedure (CRP) results in immediate resolution of BPPV in about 80% of patients after single application and the success rate increases up to 92% with repetition of the procedure. CRP may be attempted by the patients themselves if instructed appropriately. However, the appropriate CRP should be selected according to the affected canal and subtype (canalolithiactic vs. cupulolithiatic) of BPPV. A few studies have explored the utility of questionnaires in confirming BPPV and determining the subtypes based on the characteristics (positional triggering, duration etc.) of the vertigo and positional changes that mostly induce it. A recent study investigating this questionnaire approach showed an accuracy of 71.2% in diagnosing BPPV and determining the involved canal and type. The questionnaire is comprised of six questions. The first three are designed to diagnose BPPV, and the latter three to determine the subtype and affected ear. Currently, a clinical trial is under way for self-application of CRPs based on the results of web-based questionnaire and online transfer of the video-clip for appropriate CRP (CRIS registry no. KCT00002364).
Abstract 4
Vestibular rehabilitation with virtual reality: Visual stimulation in PPPD
Seo-Young Choi (Department of Neurology, College of Medicine, Pusan National University, Pusan National University Hospital)
Recently, several studies showed significant improvement of subjective symptoms or static posturographic assessment by vestibular exercises using virtual reality programs in patients with persistent postural-perceptual dizziness (PPPD). Especially, habituation program using visual stimuli with optokinetic or complex background is revealed to be effective for improving visual vertigo. Virtual reality may be an optimized tool for promoting habituation, and it can maximize patients’ compliance. I present here the effect of vestibular rehabilitation using visual stimuli in virtual reality.
Abstract 5
Wearable device for dizziness using AR/VR.
Jae Jun Song (Professor, Department of Otorhinolaryngology-Head & Neck Surgery, College of Medicine, Korea University, Korea)
The vestibular system is responsible for detecting and regulating body movements, preventing falls and maintaining vision. For this, coordination of vision, vestibular organs, and proprioceptive systems is required. In order to evaluate the balance system, it is important to evaluate the coordination of those systems.
Virtual reality is a technology that can provide an expanded spatial experience, and the patient can experience virtual space in various environments. We have developed a wearable medical device based on virtual reality and will apply to the diagnosis and rehabilitation of dizziness. Existing vestibular rehabilitation treatment requires a lot of space and expensive equipment, but the wearable medical device developed by us can provide a variety of environments without space restrictions, and can provide real-time feedback to the patient. Through this presentation, the authors will discuss the medical application of virtual reality technology and present the usefulness of the device currently under development.
9:00:00 AM AUDIOVESTIBULAR COGNITION
1.- FP0997How Bilateral Vestibulopathy affects Cognition in Older Adults corrected for Hearing Status
Joyce Bosmans1, Hanne Gommeren1,2, Griet Mertens1,2, Patrick Cras1,2, Sebastiaan Engelborghs1,3, Angelique Van Ombergen1, Luc Vereeck1,2, Annick Gilles1,2,4, Vincent Van Rompaey1,2
1University of Antwerp, 2Antwerp University Hospital, 3Vrije Universiteit Brussel (VUB), 4University College Ghent
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: A growing body of literature suggests a significant impact of the vestibular system on cognitive function, and visuospatial processing in particular. A higher prevalence of vestibular loss has been observed in people with varying degrees of cognitive impairment while hippocampal atrophy, an important biomarker for Alzheimer’s disease, has been associated with vestibular decline. However, the co-occurrence of sensorineural hearing loss in people with vestibular loss has often been overlooked and may have produced unwarranted conclusions.
Objectives: The primary objective is to investigate cognitive function in older adults with bilateral vestibulopathy (BV) taking hearing status into account and compare these results with a healthy control group. The secondary objective is to explore multiple vestibular characteristics (including measurements of the peripheral vestibular end organ, clinical balance testing and questionnaires) and their potential influence on cognition within the BV population.
Materials and Methods: This study included 34 people with a diagnosis of BV according to the Bárány Society criteria. Each control was individually matched based on age, gender and best aided hearing performance. All subjects underwent cognitive, vestibular and hearing assessments. The primary outcome measure was cognition, measured by the Repeatable Battery for the Assessment of Neuropsychological Status for Hearing impaired individuals (RBANS-H).
Results: Overall, people with BV obtained a significantly lower score on the RBANS-H total scale. This decline was most pronounced in the subdomains of immediate memory, visuospatial and attention. Language and delayed memory subdomains remained preserved. Within the BV population, only one vestibular parameter (the Performance-Oriented Mobility Assessment, in particular the balance subscale) was significantly associated with lower cognitive scores. Further vestibular parameters, including measurements of the peripheral vestibular end organ and questionnaires, demonstrated no association.
Conclusions: The older adult BV population demonstrated worse cognitive function in general in comparison with a healthy control group, which was most pronounced in the subdomains of immediate memory, visuospatial and attention. This cognitive loss was found to be independent of concurrent hearing loss. Only one clinical balance assessment was associated with the observed lower cognitive scores in the former population. Other vestibular parameters such as measurements of the peripheral vestibular end organ and questionnaires demonstrated to significant association. These results support and extend evidence on an association between vestibular loss and cognitive impairment, in particular Alzheimer’s disease. Further research on the causal mechanisms underlying this association and the impact of vestibular rehabilitation on cognition is needed.
2.- FP1021The human egomotion network
Ria Maxine Rühl1,2, Leoni Ophey2,Theresa Raiser, Katharina Seiderer, Virginia Flangin, Matthias Ertl2,3, Julian Conrad1,2 and Peter zu Eulenburg2,4
Department of Neurology1 and German Center for Vertigo and Balance Disorders2 IFB-LMU, Ludwig-Maximilians-University, Munich, Institute of Psychology and Inselspital3, University of Bern, Institute for Neuroradiology4, Ludwig-Maximilians-University Munich, Munich, Germany4
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Theme: Volitional movement in a three-dimensional environment requires multisensory integration, in particular of visual and vestibular signals. In humans, responses to visual egomotion-compatible optic flow stimuli have been demonstrated for multiple cortical areas in the parieto-temporal, cingulate, insular and occipital cortex. Of these regions, areas MST, CSv and VIP have been shown to respond to vestibular stimulation. The egomotion network structure in a comprehensive whole-brain approach however has not been systematically investigated to date.
We applied visual self-motion and galvanic vestibular stimulation using high resolution multi-band neuroimaging to characterize the entire cortical and subcortical egomotion network in humans in a large cohort (n=131). Responses during egomotion perception suggest a network including cortical areas CSv, PcM, human VPS, the cerebellar uvula and an area in the supramarginal gyrus. With respect to its delineated cortical connections and anatomical localization, we propose that this area represents the human homologue of macaque area 7a. The whole-brain functional connectivity analysis point at a central role of the connections between area CSv and the uvula of the cerebellum, possibly representing feedback loops involved in updating visuo-spatial and vestibular information during egomotion. All egomotion hubs showed varying functional connections with visual, vestibular, somatosensory and higher order motor areas, underlining their common function in sensorimotor integration essential for the guidance of locomotion.
Target audience: Clinicians and researchers interested in understanding the structural correlates of the human egomotion system and its functional connections.
3.- FP1044Accelerated Cognitive Decline due to Hearing Loss and Bilateral Vestibulopathy: Insights from a Cognitive Evaluation in DFNA9-patients: a Cross-Sectional Study using the Repeatable Battery for the Assessment of Neuropsychological Status adjusted for the Hearing Impaired in the DFNA9 Population
Hanne Gommeren1,2; Joyce Bosmans1; Julie Moyaert2; Griet Mertens1,2; Patrick Cras1,3; Sebastiaan Engelborghs4,5; Angelique Van Ombergen1; Annick Gilles1, 2, 6; Erik Fransen7,8; Raymond van de Berg2,9; Sebastien P.F. JanssensdeVarebeke1,10; Vincent Van Rompaey1,2
1Department of Translational Neurosciences, Faculty of Medicine and Health Science, University of Antwerp, Antwerp, Belgium; 2University Department of Otorhinolaryngology-Head and Neck Surgery, Antwerp University Hospital, Edegem, Belgium; 3Department of Neurology, Antwerp University Hospital and Institute Born-Bunge, University of Antwerp, Antwerp, Belgium; 4Department of Neurology, University Hospital Brussel and Center for Neurosciences (C4N), VrijeUniversiteit Brussel (VUB), Brussels, Belgium; 5Department of Biomedical Sciences and Institute Born-Bunge, University of Antwerp, Antwerp, Belgium; 6Department of Education, Health & Social Work, University College Ghent, Ghent, Belgium; 7Center of Medical Genetics, University of Antwerp, Antwerp, Belgium; 8StatUa, University of Antwerp, Antwerp, Belgium; 9Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Maastricht, The Netherlands; 10Department of Otorhinolaryngology—Head & Neck Surgery, Jessa Hospital, Hasselt, Belgium;
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract
Background: Deafness autosomal dominant 9 (DFNA9) is hereditary disorder known to affect both hearing and vestibular function in its carriers. Its phenotype is characterized by a progressive sensorineural hearing loss (SNHL) and vestibular dysfunction evolving towards bilateral vestibulopathy (BV) by the 3rd to 5th life decade. Recent studies have identified the impact of hearing loss and vestibular dysfunction on cognitive function.
Objective: The main objective of this study is to investigate how cognitive functioning of carriers of the p.Pro51Ser variant in the COCH gene is affected by the disease and compare these results with a healthy matched control group.
Materials and Methods: Forty-seven carriers of the pathogenic p.Pro51Ser variant in the COCH gene were included in this study, of which 38 met the Bárány Society criteria and were thus diagnosed with BV. Each control was individually matched based on age, gender and education level. A cognitive, vestibular and hearing assessment was performed in all subjects. All participants completed the Repeatable Battery for the Assessment of Neuropsychological Status, adjusted for the Hearing Impaired (RBANS-H), a cognitive screening test which includes subtests probing Immediate and Delayed Memory, Visuospatial Capabilities, Language and Attention. Hearing assessment consisted of a liminal audiometry and speech-in-noise testing (SPIN) using the Leuven Intelligibility Sentence Test (LIST). This was followed by a vestibular assessment, including video Head Impulse Test (vHIT) and electronystagmography (ENG). Mean RBANS-H scores of DFNA9 patients and controls were compared using the non-parametric Wilcoxon rank-sum test.
Results: DFNA9 patients demonstrated significantly lower scores on all subscales (except the Language subscale) and total percentile score compared with their healthy matched controls. The total sample was divided into two groups: age < 55 years old and age = 55 years old Cognition of DFNA9 patients aged < 55 years old did no longer differed significantly from their matched controls, except for the Immediate Memory subscale.
Conclusion: DFNA9 patients’ cognition scored significantly worse when compared with their healthy matched controls, suggesting an impact of their SNHL and vestibular loss on their cognitive performances. This significant effect was not observed in the age group younger than 55 years old. Further research is needed on the individual trajectory of SNHL, vestibular function and how hearing rehabilitation affects cognitive functioning.
4.- FP1182The Human Vestibular Cortex: Functional Anatomy, Connectivity and the Effect of Peripheral Vestibular Disease
Richard Ibitoye1,2, Emma-Jane Mallas1,3, Niall J. Bourke1, Diego Kaski4, Adolfo M. Bronstein2, David J. Sharp1,3,5
1Computational, Cognitive and Clinical Neuroimaging Laboratory, Department of Brain Sciences, Imperial College London, London, UK. 2Neuro-otology Unit, Department of Brain Sciences, Imperial College London, London, UK. 3UK Dementia Research Institute, Care Research & Technology Centre, Imperial College London, London, UK. 4Department of Clinical and Motor Neurosciences, Centre for Vestibular and Behavioural Neurosciences, University College London, London, UK. 5Centre for Injury Studies, Imperial College London, London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and Aims: Area OP2 in the posterior peri-sylvian cortex has been proposed to be the core human vestibular cortex. The organisation of visual and vestibular processing in OP2 and immediately adjacent areas (OP2+) remains unclear. We investigated the functional anatomy and connectivity of OP2+.
Methods: We defined the functional anatomy of OP2+ using spatially constrained independent component analysis of functional MRI data from the Human Connectome Project. OP2+ responses to caloric irrigation and visual motion were then investigated in seventeen controls and seventeen age-matched chronic right vestibular neuritis patients.
Results: Ten subregions were identified by independent component analysis, and most had significant connectivity to known vestibular areas. In controls, a posterior part of right OP2+ showed: direction-selective responses to visual motion; and activation during caloric stimulation that correlated positively with perceived self-motion, and negatively with visual dependence and peak nystagmus slow phase velocity. Patients showed abnormal OP2+ activity, with an absence of visual or caloric activation of the healthy ear and no correlations with dizziness or visual dependence – despite normal brainstem responses to caloric stimulation (slow-phase nystagmus velocity). A lateral part of right OP2+ showed activity that correlated with chronic dizziness (situational vertigo) in patients.
Conclusion: A posterior subregion of right OP2+ shows strong functional connectivity to other vestibular regions and a profile of caloric and visual responses suggesting a central role for vestibular function in health and disease.
5.- FP1230Subjective Cognitive Dysfunction in Neuro-Otology Patients is a Function of Psychological Distress
Jack Tame1, Danica Xie2, Haydan Bonnacorsi2, Rengen Parlane2, Miriam S. Welgampola2,3, Sally M. Rosengren2,4
1Audiology Department, Macquarie University, Sydney Australia; 2Central Clinical School, University of Sydney, Sydney, Australia; 3Institute of Clinical Neurosciences, Royal Prince Alfred Hospital, Camperdown, Australia; 4Neurology Department, Royal Prince Alfred Hospital, Camperdown, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Patients with vestibular disorders sometimes complain of ‘brain fog’. We recently reported higher levels of subjective cognitive dysfunction in patients attending a neuro-otology outpatient clinic compared to controls, which persisted after accounting for demographic variables and measures of psychological distress. We now report the results of a larger group of patients, who also underwent vestibular function testing.
Methods: We asked 287 neuro-otology clinic outpatients whether they experienced difficulties with thinking, memory or concentration as a result of dizziness/vertigo. All patients and 115 control subjects) completed two questionnaires: the neuropsychological vertigo inventory (NVI) and depression, anxiety and stress scales (DASS). A subset of patients also completed the Wayfinding Questionnaire (WQ; N = 148) and the Metacognition Index of the Behaviour Rating Inventory of Executive Functioning - Adult Version (BRIEF-A; N = 146). Patient and control scores were compared using age, gender and DASS score as covariates. For this purpose, four DASS categories were formed using z scores: <0, 0 to 0.99, 1-1.99, and ≥2. Video head impulse and cervical and ocular vestibular evoked myogenic potential test results were available for 275 patients.
Results: Many patients (62%) reported having cognitive difficulties as a result of their dizziness. Although patients reported more dysfunction than controls on all questionnaires except the WQ and BRIEF-A Task Monitoring and Organisation of Materials subscales, DASS scores were also significantly greater in the patients (mean DASS score difference = 16.83, p<0.001). Comparison of patient and control scores, adjusted for DASS scores, showed no significant differences between groups. Sixty-three patients had at least one vestibular test abnormality, however when this group was compared to controls there were no significant differences on any questionnaire after accounting for DASS scores.
Conclusions: Patients with dizziness and vertigo reported higher levels of subjective cognitive dysfunction than controls, but these differences disappeared when psychological distress was taken into account. Using a larger sample size and more DASS categories to define depression, anxiety and stress than our previous study, we have shown that subjective cognitive dysfunction in patients with dizziness and vertigo is due to concomitant high levels of emotional distress. This study highlights the critical importance of measuring psychological variables when measuring subjective cognitive dysfunction, which is not a routine feature of similar papers in the neuro-otology literature.
6.- FP1223EEG Markers of Asymmetric Vestibular Stimulation: Role of α-band in Vestibular Adaptation
Josephine I. Cooke1, Onur Guven1, Patricia Castro Abarca1,2, Richard Ibitoye1, Vito E. Petorossi3, Adolfo M. Bronstein1
1Neuro-otology Unit, Department of Brain Sciences, Imperial College London, Charing Cross Hospital, London, UK; 2Escuela de Fonoaudiología, Facultad de Medicina, Clínica Alemana Universidad del Desarrollo, Santiago, Chile; 3Department of Medicina Interna, Sezione di Fisiologia Umana, Università di Perugia, Perugia, Italy
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and Aims: Asymmetric whole-body rotations have been shown to result in rapid adaptation of vestibular perception (Pettorossi et al. 2013, J Physiol). When given a series of sinusoidal oscillations in which the two hemicycles have equal amplitude but asymmetric velocity, healthy subjects begin “neglecting” (= not feeling) the slower hemicycle (SHC), reporting a drift in perceived heading orientation towards the faster hemicycle (FHC). This perceptual adaption is not reflected in the vestibular-ocular reflex or in perceptual thresholds, suggesting it is facilitated by higher-order mechanisms. The current study aimed to quantify electroencephalographic (EEG) markers of this adaptive response, with the hypothesis that it would be mediated in the alpha frequency band (8-14 Hz), given its previously reported role in vestibular processing.
Methods: Twenty-five healthy young subjects (mean age: 28.46±6.35 years) were given a set of symmetric or asymmetric whole-body oscillations in the dark (FHC: 1s (1 Hz), SHC: 4s (.25 Hz), symmetric consisted of two SHC). Subjects verbally reported their perceived final position after each trial using landmarks in the testing room; this was converted into total position error (TPE). Thirty-two channel EEG was recorded pre, during, and post-adaptation for each condition. EEG recordings were filtered, cleaned, then epoched to correspond to each oscillation. Average alpha power was calculated for each epoch and a logistic regression curve was fit over the first six epochs for each subject. The beta-coefficients for these regression curves were analysed with linear mixed models were used to determine a region-by-condition effect of the adaptation.
Results: TPE was significantly higher in the asymmetric condition and was always in the direction of the FHC (p < 0.001). In both conditions, alpha power was initially suppressed in response to the vestibular stimulation, but then recovered back toward pre-adaptation values in both the frontal and parietal regions, although power was consistently more suppressed in the symmetric condition. However, this pattern diverged in the prefrontal and occipital regions during the asymmetric condition only (p = .04); alpha recovered rapidly in the prefrontal region but was stagnant in the occipital region.
Conclusions: These findings suggest that the perceptual “neglect” induced by asymmetric stimulation is partially mediated by the alpha frequency band. The finding further supports the role played by alpha rhythm in vestibular perception and adaptation.
10:00:00 AM EPIDEMIOLOGY
1.- FP1004Assessment of vertigo in the emergency department: three tools to double diagnosis rate
Nham B1,2, Reid N1, Bein K2,3, Bradshaw AP1,2, McGarvie LA1, Argaet EC2, Young AS2, Watson SR4, Halmagyi GM1,2, Black DA5, Welgampola MS 1,2
1Institute of Clinical Neurosciences, Royal Prince Alfred Hospital, Sydney, NSW, Australia; 2Central Clinical School, University of Sydney, Sydney, NSW, Australia; 3Department of Emergency Medicine, Royal Prince Alfred Hospital, Sydney, NSW, Australia; 4Prince of Wales Clinical School, University of New South Wales, Sydney, NSW, Australia; 5Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Aims: Many patients presenting to the emergency-department (ED) with vertigo, leave without a diagnosis. We assessed whether three tools could improve ED diagnosis of vertigo.
Methods: A prospective observational study was undertaken on 539 patients presenting to ED with vertigo. We used three tools in an intervention-group: a structured history and examination, nystagmus video-oculography (VOG) in all patients and additional video head-impulse testing (vHIT) for acute-vestibular-syndrome (AVS). The diagnosis rate in this intervention group was compared to a control ‘management-as-usual’ ED group.
Results: In the intervention-group (n=424), case-history classified AVS in 34.9%, episodic spontaneous-vertigo (ESV, 32.1%), and episodic positional-vertigo (EPV, 22.6%). In AVS, we employed “Quantitative-HINTS plus” (Head-Impulse, Nystagmus and Test-of-Skew quantified by vHIT and VOG, audiometry) to identify vestibular-neuritis (41.2% of AVS) and stroke (31.1% of AVS). vHIT gain =0.72, catch-up saccade amplitude >1.4, saccade-frequency >154%, and unidirectional horizontal-nystagmus, separated stroke from vestibular neuritis with 93.1% sensitivity and 88.5% specificity. In ESV, 66.2% and 14% were diagnosed with vestibular migraine and Meniere’s Disease respectively by using history and audiometry. Horizontal-nystagmus slow phase velocity was lower in migraine 0.4±1.6/s than Meniere’s 5.7±5.5/s (p<0.01). In EPV, benign positional vertigo (BPV) was identified in 82.3% using VOG. Paroxysmal positional nystagmus lasting <60s separated BPV from non-BPV with 90% sensitivity and 100% specificity. In the control group of ED patients undergoing management-as-usual (n=115), diagnoses included BPV (38.3%) and non-specific vertigo (41.7%).
Unblinded assessors reached a final diagnosis in 90.6% and 30.4% of the intervention and control groups. Blinded assessors provided with the data gathered from each group reached a diagnosis in 86.3% and 41.1%.
Conclusion: The use of three tools: a structured clinical assessment, vHIT and VOG doubled the rate of diagnosis in the ED.
2.- FP1017Balance and Dizziness Problems in Children: The 2016 National Health Interview Survey of 9,247 Children in the United States
Howard J. Hoffman1, Chuan-Ming Li1, Katalin G. Losonczy1, Christa L. Themann2, Devin McCaslin3, Rose Marie Rine4,5, Keiko Hirose6, Anne E. Hogan7, Helen S. Cohen8, Charles C. Della Santina9
1Division of Scientific Programs, National Institute on Deafness and Other Communication Disorders (NIDCD), National Institutes of Health (NIH), Bethesda, Maryland, USA; 2Division of Field Studies and Engineering, National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC), Cincinnati, Ohio, USA; 3Otorhinolaryngology, Mayo Clinic, Rochester, Minnesota, USA; 4Specialty Therapy Source, LLC, Jacksonville, Florida, USA; 5School of Physical Therapy, Marshall University, Huntington, West Virginia, USA; 6Washington University School of Medicine, St. Louis, Missouri, USA; 7School of Audiology, Pacific University, Hillsboro, Oregon, USA; 8Department of Otolaryngology–Head and Neck Surgery, Baylor College of Medicine, Houston, Texas, USA; 9Departments of Otolaryngology–Head and Neck Surgery and Biomedical Engineering, Johns Hopkins School of Medicine, Baltimore, Maryland, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Dizziness and balance problems comprise many symptoms, e.g., a motion or spinning sensation (vertigo), light-headedness, disequilibrium or unsteadiness. In 2012, the United States National Health Interview Survey (NHIS) found a prevalence of balance and dizziness problems (BDP) of 5.3% in children. In 2016, the NHIS BDP child survey was repeated with refined BDP descriptions and additional risk factors. Purpose: Describe prevalence and characteristics of BDP in children and identify risk factors. Methods: A multistage, nationally representative sample of children (n=9,247; aged 3-17 years) was selected for the 2016 NHIS. Parents reported if their child had BDP (i.e., vertigo/motion sensation, poor balance when standing-up or walking, clumsiness/poor coordination, frequent unexpected falls, light-headedness/fainting, blurred vision, or other BDP) last 12 months, association with headache/migraine and history of significant head injury or concussion. Logistic regression adjusting for socio-demographic factors was used to assess BDP risk factors. Results: BDP prevalence was 5.6% (3.5 million US children); 5.8% of females, 5.5% of males. Prevalence increased with age from 3.5% (3-5 years) to 9.1% (15-17 years), p<0.001. Prevalence of head injury was 7.0% (4.3 million); 5.8% females, 8.1% males, p<0.001. Among children with BDP, 38.8% had one, 28.9% had two, 13.7% had three, 10.2% had four, and 8.4% had five+ symptoms reported. For those with BDP, 62.1% of “episodes” lasted <2 minutes, 17.1% lasted 2-20 minutes, 13.0% lasted 20 minutes to 8 hours, and 7.9% lasted >8 hours. Multivariable logistic models for BDP indicated: (a) diagnosis of early developmental delay increased risk 5-fold, (b) significant head injury increased risk 2.6-fold, and (c) high birthweight (4000+ g) increased risk 1.6-fold, all p<0.001. Among those with a diagnosis from a health professional (43.6%), common diagnoses were (a) neurological, e.g., cerebral palsy, seizures (11.5%), (b) anxiety including panic syndrome (10.2%), (c) depression (7.2%), (d) medication side effects (6.6%), (e) developmental motor coordination disorder, e.g., “clumsy” child, (5.1%), and (f) head injury (4.7%). Parents reported severity of their child’s BDP as “none” (41.0%), “small” (42.2%), “moderate” (13.8%), or “big/very big” (3.0%). The percentage of children with BDP seen by healthcare professionals was 37.8% overall but increased to 93.7% for children with big/very big problems. Conclusions: US children have a high prevalence of BDP. About 1 in 20 children aged 3-17 years has a BDP, and about 1 in 600 has a BDP reported by parents as a “big” or “very big” problem.
3.- FP1146Predicting the Occurrence and Functional Impact of Early Vestibular Loss in Congenital Cytomegalovirus Infection
Cleo Dhondt1, Sarie Martens2, Marieke Sucaet2, Saartje Vanaudenaerde3, Lotte Rombaut3, Els De Leenheer1,3, Helen Van Hoecke1,3, Leen Maes2,3, Ingeborg Dhooge1,3
1Department of Head and Skin, Ghent University, Ghent, Belgium; 2Department of Rehabilitation Sciences, Ghent University, Ghent, Belgium; 3Department of Otorhinolaryngology, Ghent University Hospital, Ghent, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Research background: Congenital cytomegalovirus (cCMV) infection is the most common non-genetic cause of childhood sensorineural hearing loss and an important cause of pediatric vestibular loss. The aim of this study was to depict the occurrence, predictors and functional impact of vestibular loss occurring in a child’s early development (< 18 months).
Methods: In our center, all children diagnosed with cCMV are enrolled in a 4-year longitudinal audiovestibular and motor follow-up. In this analysis, data of the most reliable assessment before the age of 18 months (mean age 8.9, SD 3.2 mo) was included, comprising results of the video Head Impulse Test for lateral canals, the cervical Vestibular Evoked Myogenic Potential test and the Alberta Infant Motor Scale (AIMS) of 169 patients. Simple logistic and linear regression analyses were used to identify predictive factors for vestibular and motor function and Mann Whitney U Tests were used for group comparisons of motor performance.
Results: At birth, 55% of all children were asymptomatic and 45% symptomatic. Fourteen percent had hearing loss at the moment of vestibular testing (8% unilateral, 6% bilateral) and 3% had a cochlear implant. Vestibular dysfunction before the age of 18 months occurred in 12% of all patients (8% unilateral, 4% bilateral). Overall, the odds for a vestibular dysfunction were 17 times higher (p < 0.001, 95% CI = [3.74 – 81.36]) for patients with bilateral refer on the neonatal hearing screening compared to those with normal hearing at birth. Within the latter group, the risk for a vestibular dysfunction was significantly higher for patients with periventricular cysts on magnetic resonance imaging (p < 0.005, OR = 13.65, 95% CI = [2.16 – 86.16]) and patients that had developed hearing loss after the neonatal hearing screening (p < 0.003, OR = 21.75, 95% CI = [2.85 – 165.83]). Analyses of the motor function results showed that a vestibular dysfunction was a significant predictor for the AIMS z-score (p < 0.001, ß=-1.814, 95% CI = [-2.62 – -1.01]). Moreover, motor performance was significantly weaker when the vestibular deficit had been present from the first assessment onwards (p = 0.030).
Conclusions: Abnormalities on neonatal brain imaging and hearing status have great predictive value for early vestibular dysfunction in children with cCMV. Early diagnosis of vestibular dysfunction, especially when congenital, is essential as it has an important impact on a child’s early motor development.
4.- FP1170Vertigo and dizziness in children and adolescents.
Philippe Perrin1,2,3, Gilles Bosser1,4, Anne Borsa-Dorion5, Irene Stella1,6, Olivier Klein1,6, François Feillet7, Laurent Coffinet1,2
1DevAH - Development, Adaptation and Handicap, University of Lorraine, Faculty of Medicine, France; 2Department of Pediatric Oto-Rhino-Laryngology, University Hospital of Nancy, Vandoeuvre-lès-Nancy, France; 3Laboratory for the Analysis of Posture, Equilibrium and Motor Function (LAPEM), University Hospital of Nancy, Vandoeuvre-lès-Nancy, France; 4Cardiopediatric Department, Children Hospital, University Hospital of Nancy, France; 5Pediatric Emergency Department, Children Hospital, University Hospital of Nancy, France; 6Pediatric Neurosurgery Department, University Hospital of Nancy, France; 7University Hospital of Nancy, Reference Centre for Inborn Errors of Metabolism, Children Hospital, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objectives – At the University Hospital of Nancy, France, a young patient who experiences vertigo or dizziness is often referred to the pediatric otolaryngology department by the pediatric emergency department and the care is made, according to the diagnostic orientation, mainly with the pediatricians, in particular pediatric neurologists and children’s oncologists, pediatric neurosurgeon, the physiotherapists, the cardio-pediatricians and the child psychiatrists. The aim of this study was to evaluate the diagnostic features of vertigo or dizziness at the pediatric otolaryngology department.
Methods – The diagnosis of the conditions associated with these symptoms were retrospectively reviewed.
Results – The study group concerned 400 patients (2-16 years old). Brief duration, isolated, recurrent vertigo often corresponds to benign paroxysmal vertigo (BPV) (25) (2-5 years) or to a migraine associated vertigo (MAV) (98) (older child, convergence insufficiency), more rarely to an epilepsy (9). Recurrent vertigo or dizziness associated to hearing signs can arise within the framework of otitis media (24). The long-lasting vertiginous crisis is close from the point of view of the etiologies of those of the adult, i.e. vestibular neuronitis or labyrinthitis (24). Chronic instability was noted in ataxia (medulloblastoma (6), chickenpox (4), intoxications (4), familial paroxystic ataxia (3), opsoclonus myoclonus syndrome (2)), bilateral vestibular deficit (13), multiple sclerosis (1), “cervical vertigo” (post-trauma (12), Chiari malformation (6)). Genetic etiologies are suspected during a gait acquisition disorder or in the presence of a syndromic disorder (6). Vertigo can also be related to autoimmune diseases (4). Orthostatic hypotension arises in phase of fast growth (30). Another cardiovascular cause is the vasovagal syncope (17). Somatoform dizziness arises in particular during the adolescence (family difficulties, bullying at school or in social networks) (60) or may be related to an organic disease. 16% of the study group had vertigo of multiple causes while 13% had vertigo of unknown origin.
Conclusion – One of the main objectives is to recognize the most serious conditions (posterior fossa tumor) and the most frequent (BPV, MAV). The diagnostic uncertainty is more frequent in children than in adults. Collecting reliable information from a child can be challenging due to a lack of compliance, which can make it more difficult to tailor the assessment. In the case of recurrent vertigo, the family will be asked to keep a diary of the vertiginous episodes and of any triggering factors. Collaboration with other medical disciplines is often required to reach the correct diagnosis and treatment while avoiding unnecessary examinations.
5.- FP1186Prospective study to establish the relationship between episodes of vertigo and the development of cerebrovascular accidents
Emilio Domínguez-Durán, Irene Mármol-Szombathy, Serafín Sánchez-Gómez
Hospital Universitario Virgen Macarena
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: patients who underwent any type of vertigo have an increased risk of suffering a cerebrovascular accident (CVA). It is unclear if the increased risk is due to a greater number of cardiovascular risk factors (CVFR) in these patients, or it is due to the vertigo itself.
Objective: to determine if balance disorders are independent CVRF for the development of CVA.
Material and methods: Prospective cohort study. The population studied was obtained through non-probabilistic sampling by selecting all patients from the quotas of five volunteer doctors specializing in Family and Community Medicine in our hospital area. First, the following data were obtained from all the patients in our population: sex, age, smoking habit, high blood pressure, diabetes, dyslipidemia, atrial fibrillation, peripheral arterial disease, ischemic heart disease and treatment with antiplatelet or anticoagulants. Next, all patients who were diagnosed of any kind of vertigo or dizziness were studied and a specific diagnosis was made. Later, all patients who developed a CVA up to six months after the development of vertigo or dizziness were considered as cases. Finally, six logistic regression models (LRM) were built using a stepwise forward selection of variables, in which the well-known CVRF were included as well as the antecedent of vertigo or dizziness, taking into account the diagnosis behind these symptoms.
Results: Depending on the definition of vertigo or dizziness, six different LRM were built. In all of them, the variable related with vertigo or dizziness was selected; however, well-known CVRF could not be included in the model, such as atrial fibrillation and diabetes mellitus. The odds ratio of the variable related with vertigo or dizziness were significant in all models.
Conclusion: we cannot consider balance disorders as an independent risk factor for the development of CVA. However, balance disordes are still useful red flags to identify those patients with increased risk of ACV.
6.- FP1198Paraneoplastic Cochleovestibulopathy: Clinical, Oncological, and Serological Features of a Large Case Series
Scott D.Z. Eggers1; M. Bakri Hammami2,3; Ajay Madhavan1; Mayra J. Montalvo1; Sean J. Pittock1,2; Divyanshu Dubey1,2
1Department of Neurology, Mayo Clinic, Rochester, Minnesota, USA; 2Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota, USA; 3Department of Medicine, Jacobi Medical Center-Albert Einstein College of Medicine, Bronx, New York, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Paraneoplastic cochleovestibulopathy is a distinct but heterogeneous clinical syndrome of sudden or rapid hearing loss and vestibular dysfunction with a detectable malignancy and/or known high-risk paraneoplastic antibody. Patients may present to otologists or neurologists with limited features before the full clinical picture emerges. In this study, we evaluate the clinical presentation, tumor types, serological associations, and outcomes of paraneoplastic cochleovestibulopathy.
Methods: Retrospective chart review of patients with hearing loss and/or vestibulopathy who underwent serological evaluations for paraneoplastic antibodies between 2007 and 2021 was performed.
Results: Twenty-six patients were identified (23 men, median age 45, range 28-70). Laboratory biomarkers included: KLHL11-IgG (n=20, 77% (coexisting LUZP4-IgG, n=8)), ANNA1-IgG (n=3, 12%), amphiphysin-IgG (n=2, 8%) and LUZP4-IgG alone (n=1, 4%). Active tumor was found in 18 patients (69%), most commonly testicular or extra-testicular seminoma (n=13). Six others (23%) had a regressed germ cell tumor. Detecting KLHL11-IgG or LUZP4-IgG predicted one of those tumor types in 90%. Other oncological associations were non-small cell lung cancer (n=3) and breast adenocarcinoma (n=2). Symptoms preceded tumor discovery in 96% by a median of 8 months. Fifteen patients (58%) had cochleovestibulopathy as their initial presentation before CNS manifestations. Four of those (27%) had hearing loss alone, 8 (53%) had acute vertigo alone, and 3 (20%) had combined hearing loss and vertigo before rhombencephalitis/encephalomyelitis manifestations developed, on average 5.5 months later. Nystagmus in 15/26 (58%) was spontaneous (vertical n=6, horizontal n=3) or gaze-evoked (n=6). Other ocular motor findings included gaze palsy (n=11), slow or dysmetric saccades (n=9), impaired pursuit (n=15), and misalignment (n=9, as skew, exotropia or esotropia). Hearing loss was bilateral in 16/20 undergoing audiometry. Thirteen had severe-profound hearing loss affecting one (4/13) or both (9/13) ears. Sixteen (62%) developed vertigo during their illness (constant n=12, positional n=4). Of 14 patients undergoing vestibular evaluation, 9 (64%) had pure central vestibulopathy, 4 (29%) combined central and peripheral vestibulopathy, and 1 (7%) had isolated bilateral peripheral vestibulopathy. Central signs localized to the cerebellum (5/13), brainstem (3/13), or both (5/13). Most patients had a refractory course despite immunotherapy and/or cancer treatment.
Conclusions: Paraneoplastic cochleovestibulopathy commonly presents with rapidly progressive bilateral hearing loss and/or acute vertigo often months before brainstem or cerebellar manifestations develop. KLHL11-IgG and seminoma are the most common serological and cancer associations, respectively, typically affecting young or middle-aged men. Recognizing features of this phenotype may aid in earlier diagnosis and treatment of paraneoplastic autoimmunity and associated cancer.
SY0027SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Giacinto Asprella Libonati |
| TOPIC DESCRIPTIVE TITLE: | Apogeotropic variant of PSC BPPV: differential diagnosis from ASC BPPV |
| ACADEMIC / HOSPITAL AFFILIATION: | U.O.S.D. Vestibologia e Otorinolaringoiatria Ospedale Giovanni Paolo II, Policoro, Italy |
- SPEAKER 2
| NAME AND SURNAME: | Leonardo Manzari |
| TOPIC DESCRIPTIVE TITLE: | Cupulopathy: a pathophysiological model of semicircular canal dysfunction |
| ACADEMIC / HOSPITAL AFFILIATION: | MSA ENT Academy Center, Cassino (FR) - Italy |
- SPEAKER 3
| NAME AND SURNAME: | Andrea Castellucci |
| TOPIC DESCRIPTIVE TITLE: | Canalith jam, clinical features and role of vHIT in diagnosing |
| ACADEMIC / HOSPITAL AFFILIATION: | ENT Unit, Department of Surgery, Arcispedale Santa Maria Nuova, AUSL - IRCCS, Reggio Emilia, Italy |
- SPEAKER 4
| NAME AND SURNAME: | Salvatore Martellucci |
| TOPIC DESCRIPTIVE TITLE: | BPPV upright nystagmus features: any news in minimum stymulus strategy |
| ACADEMIC / HOSPITAL AFFILIATION: | ENT Unit, Ospedale Santa Maria Goretti, Latina - Italy |
Positional vertigo is still a topic of great interest and in constant evolution: alongside the typical BPPV of the posterior and lateral semicircular canals, other variants, recently described, can frequently occur. The approach to these variants of positional vertigo may be controversial due to the lack of diagnostic criteria and shared therapeutic strategies. This symposium will be focused on some hot topics: the apogeotropic variant of PSC BPPV and the differential diagnosis from ASC BPPV, the pathophysiology of light and heavy cupola and the canalith jam, highlighting the diagnostic role of vHIT. The Speakers will deal with the pathophysiology and clinical features of each variant of peripheral positional vertigo, presenting the differential diagnosis with the central forms. Furthermore, some clinical cases resulting from the Authors’ experience will be shown. The last presentation will address the nystagmus features in upright position, presenting a new diagnostic algorithm addressed to diagnose in BPPV both: the affected ear and the involved semicircular canal, keeping the patient in the sitting position and, in so doing, causing him as little discomfort as possible.
The knowledge of the positional vertigo clinical variants of peripheral origin will allow the attendees to recognize even the rarest forms and to perform a clinical bedside examination according to the strategy of the minimum stimulus, also making them experts in the choice and interpretation of any instrumental examinations if advisable.
ABSTRACT 1
Sometimes debris could be located inside posterior canal close to the common crus, thus configuring the apogeotropic variant of posterior canal-paroxysmal positional vertigo (aPC-PPV), characterized by torsional down beating nystagmus in Dix-Hallpike position.
Two tecniques have been proposed to distinguish apogeotropic posterior canal variant from anterior canal-paroxysmal positional vertigo, both characterized by the same nystagmus direction: a liberatory manoeuvre (Demi Semont) and a forced prolonged position (FPP). Both these tecniques need to observe the torsional component in Dix Hallpike in order to diagnose the affected side.
A new technique is proposed for patients in whom the torsional component of the nystagmus is not visible in Dix Hallpike, which is achieved by bringing the patient from side to side with the head rotated in the plane of the posterior canal. It allows to transform the aPC-PPV into a typical PSC BPPV, which can be subsequently treated by the Semont meneuver.
ABSTRACT 2
The most common type of positional vertigo is Benign Paroxysmal Positional Vertigo (BPPV). Cupulopathy can be considered as an emerging clinical entity in the vestibular field.
Cupulolithiasis-type of BPPV involving the lateral semicircular canal (LSCC) shows a characteristic direction-changing positional nystagmus (DCPN) which beats away the lower ear (apogeotropic) on turning the head to either side in a supine position while canalolithiasis-type of BPPV shows a characteristic direction-changing positional nystagmus (DCPN) which beats towards the lower ear (geotropic).
Anyway direction-changing positional nystagmus (DCPN) has also been observed as persistent horizontal apogeotropic and is considered as “cupulopathy - heavy cupula”.
More recently, persistent horizontal geotropic direction-changing positional nystagmus (DCPN) has also been described and is considered as “cupulopathy - light cupula”.
However, the light cupula is not systematically described and for this reason the identification and diagnosis of “light cupula” should be improved.
ABSTRACT 3
A canalith jam (CJ) can occur when an otolith clot occludes a narrow portion of a membranous duct. It results in an endolymphatic flows blockage and a persistent deflection of cupula generating a nystagmus aligning with the plane of the plugged canal, regardless of head position. It may occur either spontaneously or following repositioning procedures for BPPV. CJ diagnosis is challenging, as resulting spontaneous nystagmus could be mainly horizontal or downbeat/upbeat depending on the involved canal. Clinical features of cases presenting with CJ will be presented, pertinent literature will be reviewed and the pivotal role of video-head impulse test (vHIT) in diagnosing, in particular in differentiating CJ from an acute vestibular loss or central disorders, will be discussed. It will be also discussed the role of vHIT in differentiating positional nystagmus due to apogeotropic posterior canal-BPPV from anterior canal-BPPV, where an incomplete CJ behaving as a “low-pass filter” is hypothesized.
ABSTRACT 4
To diagnose which is the affected side, which semicircular canal is involved and geotropic from apogeotropic variant can be challenging in BPPV patients with recent onset of vertigo and intense autonomic symptoms. The Minimum Stimulus Strategy (MSS) is a nystagmus-based algorithm which aims to diagnose any variant of BPPV by causing as little discomfort as possible to the patient. The first MSS step involves the observation of the nystagmus features keeping the patient in upright position and looking for any pseudo-spontaneous nystagmus and direction-changing nystagmus evoked by the head pitch test (HPT). If the posterior semicircular canal is involved, the evaluation of oculomotor responses to the HPT can suggest both: the affected side and the BPPV variant. Horizontal direction-changing nystagmus evoked by HPT indicates the involvement of the lateral semicircular canal, and the upright Head Roll Test (uHRT) can allow the diagnosis of the involved ear and the BPPV variant.
CP0005CONTROVERSY PANEL FORM
SPEAKERS PER CONTROVERSY PANEL:
SPEAKER 1
| NAME AND SURNAME: | Todt Ingo |
| TOPIC DESCRIPTIVE TITLE: | CTP evaluation in cases of sudden hearing loss and RW/OW revision |
| ACADEMIC / HOSPITAL AFFILIATION: | Bielefeld University, Germany |
SPEAKER 2
| NAME AND SURNAME: | Eduardo Martin-Sanz |
| TOPIC DESCRIPTIVE TITLE: | Changes in auditory and vestibular function after PLF management |
| ACADEMIC / HOSPITAL AFFILIATION: | European University. University Hospital of Getafe |
THEME: we discuss the resemblances and differences of otic capsule dehiscence syndrome (OCDs) and perilymphatic fistula with perilymph leakage (PLF w/leakage), clinical characteristics of PLF w/leakage and treatment strategies. Target audience: Neuro-otologists, Ear surgeons.
PLF is defined as an abnormal communication between the perilymph-filled space and the middle ear, or cranial spaces. By this definition, OCDs and PLF w/leakage both belong to the same clinical entity “PLF”. The diagnosis has been established in OCDs, which has typical symptoms and CT findings. On the other hand, the clinical entity of PLF w/leakage has remained a topic of controversy for more than 50 years due to the lack of an appropriate biomarker to detect perilymph leakage.
We have reported a clinical test for the diagnosis of PLF by detecting a perilymph specific protein, CTP (Cochlin-tomoprotein), as a diagnostic marker using ELISA. The ROC curve in differentiating the perilymph leakage condition from the normal middle ear was significant (P < 0.001) with an area under the curve (AUC) of 0.918 (95% CI 0.824-0.100). Diagnostic criteria using CTP has been established, and the test is available nationwide in Japan.
The manifestations of PLF w/leakage include a broad spectrum of neuro-otological symptoms such as hearing loss, vertigo/dizziness, disequilibrium, aural fullness, tinnitus, and cognitive dysfunction. This makes the diagnosis difficult. Typical symptoms and signs among CTP positive cases will be discussed.
It is noteworthy that, unlike other causes of sensorineural hearing loss and dizziness, PLF w/leakage is surgically correctable by sealing the fistula. By sealing the fistula, PLF is a surgically correctable disease. Also, appropriate recognition and treatment of PLF can improve a patient’s condition and hence, the quality of life.
ABSTRACT 1
Introduction: Sudden sensorineural hearing loss (SSNHL) is assumed to be multicausal and has often been associated with PLF. Although RW/OW closure is regularly performed in the treatment pathway of SSNHL in many departments in Germany, so far no evidence was given of the existence of a PLF. The aim of the present study was to evaluate SSNHL cases for CTP.
Material and Methods: We evaluated 21 cases of SSNHL for CTP after performing an unsuccessful steroid treatment. During a RW and OW closure, middle ear fluid was taken for CTP evaluation. Additionally, controls were taken from inner ear, middle ear and mastoid cavity (N=10).
Results: We observed a rate of 28,5 % (6 out of 21) positive CTP cases. In 9 cases the results was intermediate. In the group of CTP positive cases, the occurrence of vertigo was more frequent, and the probability of an increase of the PTA after the RW closure higher. All controls were in line with the clinical expectation.
Conclusion: CTP is a promising tool for the objective evaluation of PLF
ABSTRACT 2
The typical PLF present with a sudden onset of hearing loss, vertigo or disequilibrium. Associated trauma includes surgery, head blows or barotrauma. Some patients are idiopathic. A classification based on the preceding events is utilized in our clinic. There is a similarity in symptoms with Meniere’s disease, superior canal dehiscence syndrome.
Currently, studies employ clinical symptoms / histories as the tool to suspect PLF. We have recently included typical symptoms such as popping sound on the onset, stream water-like tinnitus in patient interview. Four PLF associated with stapedotomies, 4 cholesteatoma, 2 due to internal barotraumatic events and 2 idiopathic cases were analyzed. Auditory and vestibular test were performed, with a significant improvement of both vestibular and auditory function after its surgical or clinical management. We found above mentioned typical symptoms were crucial for suspecting / diagnosing PLF.
OC03Free Papers Form
1.- FP0958Chair versus manoeuvre canalith repositioning for benign paroxysmal positional vertigo: a randomised, multicentre, controlled clinical trial
Shujian Huang, Qingxiu Yao, Hui Wang, Yanmei Feng, Dongzhen Yu, Haibo Shi, Shankai Yin
Shanghai Jiao Tong University Affiliated Sixth People’s Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: To evaluate the efficacy and safety of the chair canalith repositioning (Chair-CRM group) compared with the manoeuvre canalith repositioning (canalith repositioning manoeuvre, Bedside-CRM) in patients with benign paroxysmal positional vertigo (BPPV) involving the posterior (pc-BPPV) or horizontal semi-circular canal (hc-BPPV).
Methods: We conducted a prospective, multicenter, open-label, parallel group, superiority trial in three tertiary hospitals in Shanghai, China between September 2017 and February 2019. Randomization sequence was created by an investigator with no clinical involvement and was competitively recruited for each centre with a 1:1 allocation. All participants were assessed immediately and 1,2,3, and 4 weeks after enrollment. The primary outcome was the efficacy rate at the 1-week follow-up. The evaluation of treatment was classified into cured, effective, ineffective according to Chinese guideline of BPPV revised in 2017. When both vertigo and nystagmus were absent, the patients were considered cured. When vertigo reported by patients and nystagmus evaluated by nystagmus lasting time and max slow phase velocity were relieved but not disappeared during the Dix-Hallpike and roll tests, the treatment was considered effective. When both vertigo and nystagmus were aggravated or not changed, or even the involved canal was changed into another one, the treatment was considered ineffective. The efficacy rates were defined as the ratio of patients with effective and cured patients to all patients and the curative rates were defined as the ratio of patients with cured patients to all patients respectively in each group at each follow-up. Safety was assessed based on reports of adverse events (AEs), as well as laboratory parameters.
Results: In the primary analysis, the efficacy rate of the Chair-CRM group was significantly higher than that of the Bedside-CRM group (98.52% vs. 86.23%) at 1 week. Upon secondary analysis, the efficacy rate was maintained at a significantly higher rate in the Chair-CRM group at 2-week (100% vs. 92.91%), and 3-week follow-up (100% vs. 95.97%). Curative rates at the first treatment (61.38% vs. 47.92%) and 3-week follow-up (93.13% vs. 84.68%) were significantly higher in the Chair-CRM group, as was the cumulative efficacy rate and repeated measures. The efficacy and curative rates did not differ between the two groups at other follow-up points. Safety analysis revealed no statistically significant differences in AEs between the two groups, or in laboratory parameters before and after treatment.
Conclusions: Chair canalith repositioning is a little more effective than manoeuvre canalith repositioning and is safe in treating pc-BPPV and hc-BPPV.
2.- FP0982Objiective findings in patients with multi-canal benign paroxysmal positional vertigo
Liying Chang, Yanhan Zhu, Wenjing Qin, Zheng Liu
Department of Neurology, Xiangyang Central Hospital, Affiliated Hospital Of Hubei University of Arts and Science. Xiangyang Hubei province,441021, P.R. China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: The study aimed to investigate the clinical characteristics of patients with multi-canal benign paroxysmal positional vertigo (MC-BPPV).
Methods: We performed a retrospective analysis of 927 patients with BPPV who were admitted to our hospital between January 1, 2016 and December 31, 2019. The clinical data of all patients were collected. The Dix-Hallpike, straight head hanging and supine Roll tests were performed in all patients. The nystagmus was recorded using videonystagmography. The clinical characteristics of patients with MC-BPPV and single canal BPPV (SC-BPPV) was analyzed and compared.
Results: Among 927 patients included in the study, 49 (5.29%) patients had MC-BPPV, 878 (94.71%) patients had SC-BPPV. There were significant differences in the male to female ratio (1:3.90 vs 1:1.81, P<0.05), mean age (62.47±12.51 vs 59.04±13.72,P<0.05), as well as the ratio of cupulolithiasis to canalithiasis (1:1.45 vs 1:4.78, P<0.01) between patients with MC-BPPV and SC-BPPV. The frequency of involvement of PC, HC, and AC were involved for 66 (67.35%), 23 (23.47%) and 9 (9.18%) times, respectively, in patients with MC-BPPV, which were involved in 581 (66.17%), 281 (32.0%) and 16 (1.82%) patients, respectively, in patients with SC-BPPV. No significant difference was found in the frequency of involvement of PC and HC between patients with MC-BPPV and SC-BPPV, while there was significant difference in the frequency of AC involvement between two groups (P<0.01). Ipsilateral PC-HC-BPPV (n=18) and bilateral PC-BPPV (n=19) were the most common among patients with MC-BPPV. 26 (53.06%) patients had ipsilateral MC-BPPV, 23 (46.94%) had bilateral MC-BPPV. Of the 26 patients with ipsilateral MC-BPPV, 7 patients combined with unilateral peripheral vestibular disorder.
Conclusion: Patients with MC-BPPV had a significantly older mean age at disease onset and a higher proportion of females compared with patients with SC-BPPV. Cupulolithiasis was more common in MC-BPPV. AC involvement was also much more common in MC-BPPV than in SC-BPPV.
Keywords: multiple semicircular canals; benign paroxysmal positional vertigo; clinical characteristics
3.- FP0918Recurrence of benign paroxysmal positional vertigo: experience in 3042 patients
Roberto Teggi1, Riccardo Guidetti2, Iacopo Cangiano1, Marco Familiari1, Giorgio Guidetti2
1San Raffaele Scientific Institute, Milano - Italy; 2Vertigo Centre, Poliambulatorio Chirurgico Modenese, Modena - Italy
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Benign paroxysmal positional vertigo (BPPV) represents nowadays the most frequent cause of peripheral vertigo, characterized by a tendency to recurrence of episodes. The main etiology remains idiopathic but several factors have been proposed as favoring the frequent detachment of otoconia and the recurrence of episodes. The purpose of our work was to retrospectively analyze the clinical data of 3042 patients treated for BPPV without other lifetime vertigo of any kind, focusing on the prevalence of the following factors as possible causes of relapses: vascular disorders of the central nervous system, heart disorders, migraine, recent head trauma, presence of anti-thyroid autoantibodies. In our sample the mean age of the first BPPV was 52.8 ± 14.5 years; there were 2339 females (76.9%). Recurrences were 2048 and a strong correlation was found with age (r = -0.14, 95% CI -0.17-0.10, p < 0.0001). In order of frequency, thyroid autoantibodies were demonstrated in 801 subjects (26.3%), vascular disorders of the central nervous system in 382 subjects (12.5%), 324 were migraineurs (10.6%), heart disorders were present in 269 subjects (8.8%) and a recent head trauma was reported by 212 subjects (6.9%). Moreover, we studied the frequency of migraine, thyroid antibodies positivity, heart disorders, CNS vascular disorders and head trauma separately in the subgroups of patients with onset of the first BPPV below 40, between 40 and 60 and over 60 years. Recent head trauma was the main causal factor for recurrence, while positivity for thyroid autoantibodies was correlated with relapsing episodes only in the subgroup of subjects aged between 40 and 60 years.
Our data are consistent with the hypothesis that previous factors are associated with recurrences, in particular anti-thyroid autoantibodies may play a role in recurrences in subjects with initial manifestations between 40 and 60 years.
4.- FP1127Benign Paroxysmal Positional Vertigo: Comparision of the “SémontPLUS Maneuver” with the Epley Maneuver – an Interim Analysis after 142 Patients of a Prospective Multinational Randomized Trial
Michael Strupp1, Anne-Sophie Vinck2, Otmar Bayer1, Nicolina Goldschagg1, Vergil Mavrodiev1, Marco Mandala4
1University of Munich, Dept. of Neurology, 2ENT, AZ Sint-Jan Brugge, 3University of Siena, Dept. of ENT
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To compare the efficacy of the new SémontPLUS maneuver (SM+) with the Epley maneuver in a prospective multinational randomized single-blinded trial in patients with posterior canal benign paroxysmal positional vertigo (pc-BPPV canalithiasis).
Background: In a previous study we demonstrated that the SM+ is superior to the regular SM. Since other studies showed that the regular SM and the Epley maneuver are equally effective, we hypothezised that the SM+ is more effective than the Epley maneuver for the treatment of the posterior canal BPPV canalithiasis.
Design/Methods: In a prospective multinational (Germany, Italy, Belgium) randomized treatment trial, patients with proven posterior canal BPPV canalithiasis – according to the diagnostic criteria of the International Classification of Vestibular Disorders – were randomly assigned (1:1) to “SM+” or Epley treatment. The SM+ is characterized by an overextension of the head/body by at least 60° below earth horizontal line during step 2 of the maneuver. The first three maneuvers were performed by the physician. The patients were then instructed on how to do the self-maneuvers which they perform three times in the morning, three times at noon and three times at night. Each morning after the first maneuver of each day the patient documented in a standardized evaluation sheet whether vertigo occurred. The primary endpoint was: “How long (in days) does it take until no attacks can be induced “in the morning” by the maneuvers?”
Results: In the 142 patients so far analysed (interim analysis), it took a mean of 3.55 days (range 1-20 days) and a median 1 day for the Epley maneuver; for the SM+ it took a mean 2.06 days (range 1-8 days) and a median 1 day for recovery. Statistical analysis with the two-sided Mann-Whitney-u-test revealed a P value of 0.06.
Conclusions: This interim analysis of this prospective tri-national randomized trial suggests that the SémontPLUS maneuver is evidently superior to the Epley maneuver in terms of the time it takes until recovery. Final statistical inference will be drawn, once the planned number of patients are recruited and analysed.
5.- FP0979Simulations of BPPV Maneuvers: Three Dimensional Visualization to Understand and Improve Management
Anita Bhandari1,Rajneesh Bhandari1, Herman Kingma2, Michael Strupp3
Background and Objectives: BPPV is a mechanical disorder of the inner ear. This study aims to show how 3D dynamic simulation models of BPPV can help to visualize the movement of the debris within the canals during head movement. Simulations can be used for a better understanding of the theoretical efficacy of maneuvers and help in development of new maneuvers to treat different BPPV variants.
Methods: Based on reconstructed MRI images and fluid dynamics, a 3D dynamic simulation model (as a function of time) was developed and applied. Maneuvers used to treat canalithiasis affecting the posterior, horizontal and anterior canals were studied.
Results: 3D visualization of the canals linked to head movement displays the importance of each step of various maneuvers to bring the affected canal at an angle at which gravity can act best. The simulations have shown how the Semont Plus maneuver and Modified Yacovino maneuver improve the efficacy of previously described maneuvers.The modified 3600 roll and Zuma maneuver were seen to be effective for all hc-BPPV variants, while some maneuvers, like the Gufoni maneuver for apogeotropic ampullary arm horizontal canal BPPV, have been theoretically shown to be less effective in particle repositioning.
Conclusions: The 3D simulations for movement of the otoconia debris can be used to test the mechanism of action and the theoretical efficacy of existing maneuvers for the diagnosis and the treatment of different BPPV variants. It can also provide a visual explanation for the need of specific maneuvers for each type of BPPV. The simulator software can help in optimizing maneuvers along with eliminating incorrect and unnecessary steps and are also useful for teaching of doctors and physiotherapists.
6.- FP0987How efficient is the Rotundum Rotational Chair in the treatment of Posterior Benign Paroxysmal Positional Vertigo?
Dan D. Hougaard1,2
1Department of Otolaryngology, Head & Neck Surgery and Audiology, Aalborg University Hospital, Aalborg, Denmark; 2Department of Clinical Medicine, Aalborg University, Aalborg, Denmark.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Benign Paroxysmal Positional Vertigo (BPPV) is the most common inner ear disease and is usually successfully treated by means of traditional repositional maneuvers on an examination bed. The Epley maneuver is by far the most commonly used method for this type of repositioning. Despite successful results by means of these manual maneuvers, there has been a growing demand for additional treatment modalities to the more retractable cases of BPPV. Therefore, several different mechanical rotational chairs have been developed. These chairs are able to position the patients in all desired positions because these chairs are able to turn the patients 360 degrees in both the horizontal and vertical planes. Because this repositional chair is fairly new, no studies have been completed on the efficacy rate of BPPV treatment with this chair yet.
Method: Randomized prospective clinical trial. Approximately 100 subjects diagnosed with posterior canalolithiasis Benign Paroxysmal Positional Vertigo (BPPV) will undergo treatment with the Rotundum Rotational Chair. Both diagnostics and treatments will take place in the Rotundum Chair. If diagnosed with posterior canalolithiasis type BPPV, patients will undergo block randomization to one of three separate treatment options with this chair: 1) Epley Maneuver, 2) Semont Maneuver or 3) 360-degree vertical rotation maneuver. For diagnostics, patients will wear a VNG google with vision denied.
Results: In average, 1.4 treatments were required for successful treatment with all three treatment options. Following one treatment with requirements of both subjective and objective improvement, successful treatment rate was 65.6% with the Epley maneuver, 51.4% with the Semont maneuver, and 32.3% with the 360-degree maneuver. Following a maximum of four treatments, the total number of successful treatments were 75%, 62.9%, and 54.8% respectively. In average, all three treatments offered equally good subjective relief (94.9% of cases).
Conclusion: The Rotundum Rotational Chair is efficient in the treatment of non-retractable BPPV. The Epley maneuver seems to provide the fastest concomitant relief of both subjective symptoms and objective findings. The three separate treatments offered with this chair were equally good in providing subjective relief.
1.- FP1067The Neural Basis of Skull Vibration Induced Nystagmus (SVIN)
Ian Curthoys
University of Sydney, NSW, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Low frequency (100Hz) bone conducted vibration stimulation of either mastoid in patients with total unilateral vestibular loss (TUVL) causes a low velocity, mainly horizontal skull vibration induced nystagmus (SVIN) with quick phases beating away from the affected ear (Dumas et al 2017). This nystagmus is maintained at about the same velocity for the duration of the stimulation and its abrupt onset and abrupt offset correspond to stimulus onset and offset. 100Hz vibration activates semicircular canal neurons as well as otolith neurons, whereas 500Hz vibration selectively activates otolithic neurons.
Methods: Extracellular single neuron recordings from primary semicircular canal or otolithic afferents with irregular resting discharge in anaesthetized guinea pigs, show that semicircular canal neurons are activated and phase lock to low vibration frequencies (less than 300Hz). Canal neurons are rarely activated by 500Hz vibration. Otolithic neurons are activated by both 100Hz and 500Hz vibration.
Conclusion: Healthy subjects do not show vibration induced nystagmus to 100Hz probably because canal neurons from both labyrinths will be simultaneously activated and so cancel at the level of the vestibular nuclei. In patients with total unilateral vestibular loss the irregular horizontal canal neurons on the remaining healthy side will be activated by vibration of either mastoid, and that activation will not be cancelled and so will result in a predominantly horizontal nystagmus with quick phases beating away from the lesioned ear, irrespective of which mastoid is stimulated. The nystagmus is not due to cupula deflection but to phase locked neural activation which starts at stimulus onset and terminates at stimulus offset resulting in the abrupt onset and offset of SVIN in TUVL patients. The clinical value is that SVIN shows the symmetry of semicircular canal function in the two labyrinths.
Curthoys IS, The neural basis of skull vibration induced nystagmus (SVIN). Audiology Research 2021, 11: 557-566.
Dlugaiczyk J et al. Otology and Neurotology 2020, 41: e961-e970.
2.- FP1426Diagnostic Impact of a Device-Enabled Remote “Tele-Dizzy” Consultation Service in the Emergency Department
Daniel Gold, Susan Peterson, Justin Bosley, Shervin Badihian, Barbara Maliszewski, Mehdi Fanai, Jorge Otero-Millan, Ayodele McClenney, David Newman-Toker
The Johns Hopkins University School of Medicine
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Target audience: any clinician who sees acute vertigo in their clinics or in the emergency department.
Theme: see abstract below
Background: Missed stroke in the emergency department (ED) is a leading cause of misdiagnosis-related harms. The symptom most tightly linked to missed stroke is dizziness/vertigo, because these strokes mimic inner ear vestibular disorders closely. Diagnostic errors in acute dizziness/vertigo are frequent for both vestibular disorders (~80% misdiagnosed) and stroke (~35% missed).
Design/Methods: This is a case study of a hospital-level quality improvement intervention. We deployed a remote, video-oculography-enabled Tele-Dizzy (TD) consultation service to improve diagnosis of dizziness and vertigo in the ED. We compared the diagnostic yield and neuro-imaging utilization rates between Tele-Dizzy patients and a concurrent control group of 374 ED patients with presenting symptom of dizziness (seen outside of Tele-Dizzy consultation hours) who had mention of “nystagmus” in notes and were comparable on the variables age, sex, and ED triage acuity. In addition, the baseline 30-day stroke hospitalization rate was calculated for all non-Tele-Dizzy ED patients (unmatched baseline) with a presenting symptom of dizziness.
Results: Between July 2017 and September 2021, we offered a Tele-Dizzy consultation service during business hours. We performed 287 consults at Johns Hopkins Hospital (JHH) and saw substantial improvements in diagnostic yield, as well as reductions in unnecessary test utilization, and potentially a reduction in follow-on stroke hospitalizations.
Diagnostic Yield: There were 2.8-fold more specific vestibular diagnoses (e.g., benign positional vertigo, vestibular neuritis) in the TD group (57% vs. 21%, p<0.001), 26-fold more cerebrovascular diagnoses (7.0% vs. 0.3%, p<0.001), and half as many non-diagnoses (30% vs. 63%, p<0.001)
Utilization: In the TD group, there were 54% fewer patients recommended for any imaging, including 96% fewer recommended for CT or CT/CTA studies. There were 46% more MRIs recommended in the TD group, but the rate of stroke detection was correspondingly increased, such that there was no statistically significant difference among patients ultimately diagnosed with something other than stroke (16.9% vs. 15.5%, p=0.658).
Outcomes: So far with TD (n=287) there have been zero delayed stroke admissions, as compared to the baseline rate of 0.1%. These presumably reflect diagnostic adverse events (initially missed minor stroke or transient ischemic attack events with follow-on strokes). In this small sample, however, this difference is not statistically signficant.
| Category | Parameter | Control/Baseline | Tele-Dizzy | P-value |
| Diagnostic yield | Specific vestibular diagnosis | 77 (20.6%) | 163 (56.8%) | <0.001 |
| Cerebrovascular | 1 (0.3%) | 20 (7.0%) | <0.001 | |
| Non-diagnosis | 235 (62.8%) | 86 (30.0%) | <0.001 | |
| Imaging | Any neuroimaging | 198 (52.9%) | 70 (24.4%) | <0.001 |
| CT or CTA | 184 (49.2%) | 5 (1.7%) | <0.001 | |
| MRI (all) | 58 (15.5%) | 65 (22.6%) | <0.019 | |
| MRI (final diagnosis not stroke) | 58 (15.5%) | 45 (16.9%) | 0.658 | |
| Outcomes | 30-day stroke admission | 0.1% | 0% | N/A |
Conclusions: Our Tele-Dizzy service provides substantially greater diagnostic yield combined with greater efficiency. Next steps include expansion of this novel service to other hospitals, which will include training ED personnel to perform VOG testing. Larger studies are needed to measure the impact on diagnostic adverse events.
3.- FP0887Role of the vestibular System in Sleep Regulation
Stephane Besnard1, Charles Maquet1, Martin Hitier1, Paul Smith2
1Université de Caen Normandy, Caen, France, 2Dept Pharmacology, Otago University, NZ
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
In the scope of the role of the vestibular system in chronobiology i.e synchronizer of the circadiens rythms at the hypothalamic level, we have questionned about the role of the reciprocal neuroanatomical route between the vestibular nuclei and the orexinergic neurons. Indeed, sleep deprivation and sleep apnea syndrome alter vestibular-related oculo-motor and postural control, and that, in turn, vestibular pathologies induce sleep disturbances. Moreover, sleep-related neuroplasticity might serve the adaptation and compensation processes following vestibular lesions in patients. While orexinergic modulation of the vestibular nuclei related to postural control has been suggested, we postulate that vestibular inputs might in turn influence the sleep-wake state switch, informing the brain about the daily quantity of motion. Here, we propose an overview of the sleep and vestibular system interaction from rodents to patients and to present new findings of sleep disturbances following vestibular lesion in a rodent model as well as to highlight the effects of gravitationnal level on sleep changes.
Audience: otolaryngologist, neurologist, practionners, scientists.
4.- FP0952Acoustically Enhanced Video Head Impulse Test for Near-blind and Blind Individuals
Maja Striteska1,2, Lukas Skoloudik1, Martin Valis3, Ondrej Hrbacek4, Viktor Chrobok1, Jan Kremlacek6
1Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 2Department of Otorhinolaryngology, Charles University in Prague, 3rd Faculty of Medicine, University Hospital Kralovske Vinohrady, Czech Republic; 3Department of Neurology, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 4Department of Ophthalmology, Hospital Litomysl, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 5Department of Auditory Neuroscience, Institute of Experimental Medicine of the Czech Academy of Sciences, Prague, Czech Republic; 6Biophysics and Department of Pathological Physiology, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: (1) To evaluate the possibility of testing visually impaired subjects by a VHIT procedure. (2) To test the necessity of a fixation target during a VHIT procedure. (3) To introduce and test the utility of a novel acoustically enhanced vHIT paradigm, in which acoustic stimulus represents the fixation target.
Methods: In a prospective experimental study, we compared vHIT gains recorded under three conditions: visual fixation target, acoustic fixation, and without any fixation target. We enrolled 20 subjects to a visual deficit group, 17 emmetropic subjects with a unilateral peripheral vestibular deficit, and 17 healthy emmetropic controls.
Results: There was no difference between visual and acoustic condition in the controls (p > 0.155) and in the vestibular deficit group on the unaffected side (p = 0.297). In the visual deficit group, the acoustic vHIT gains were significantly higher compared to no fixation vHIT in near-blind patients (p = 0.015), but there was no difference in completely blind (p = 0.622). Higher acoustic VHIT gains significantly correlated with better visual acuity (rho > 0.80, p < 0.001) and shorter blindness duration (rho < -0.85, p < 0.001).
Conclusion: Our results comparing visual, acoustic and no fixation vHIT showed: (1) the vHIT reliability in near-blind subjects with at least light perception preserved, (2) the advantage of the fixation target during the vHIT procedure, although the vestibular deficit was well detectable in all conditions, even without any fixation target, (3) the benefit of a novel acoustically enhanced vHIT paradigm in near-blind subjects. Contrary, the vHIT was found to be not as such a reliable tool to evaluate vestibular function in patients with total blindness accompanied with roving eye movements.
5.- FP1402Subjective visual vertical and postural control in patients following cochlear implantation
Ondrej Cakrt1, Kryštof Slabý1, Klára Kucerová1, Jaroslav Jerábek2 and Jan Boucek3
1Department of Rehabilitation and Sports Medicine; 2nd Faculty of Medicine, Charles University and Motol University Hospital, Prague, Czech Republic; 2Department of Neurology, 2nd Faculty of Medicine, Charles University and Motol University Hospital, Prague, Czech Republic; 3Department of Otorhinolaryngology and Head and Neck Surgery, 1st Faculty of Medicine, Charles University and University Hospital Motol, Postgraduate Medical School, Czech Republic
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
BACKGROUND: Cochlear implantation (CI) is associated with changes in the histopathology of the inner ear and impairment of vestibular function. OBJECTIVE: Aims of our study were to assess patients for clinical manifestations of vestibular and balance changes before surgery, compare them with asymptomatic subjects (controls) and report changes in posturography and in static and dynamic subjective visual vertical (SVV) during the acute post-surgery period in patients. METHODS: Examination was performed using posturography and the SVV measurement. We examined 20 control subjects and 20 CI patients pre-surgery (Pre). Patients were examined 2nd day (D2) and then 14th day (D14) after surgery. RESULTS: Baseline SVV was not different between patients and control group. There was a statistically significant difference (p<0.001) in dynamic SVV between subgroups of right- and left-implanted CI at D2 (-3.92 ± 4.25° and 2.38 ± 2.53°, right and left side implanted respectively) but not Pre (-0.48 ± 1.80° and -1.00 ± 0.79°) or D14 (-1.81 ± 3.31° and -0.10 ± 1.56°). Baseline posturography parameters between patients and control group were statistically significantly different (p<0.01). There was no statistically significant difference in posturography among Pre, D2 and D14. CONCLUSIONS: CI candidates have impaired postural control before surgery. CI surgery influences perception of subjective visual vertical in acute post-surgery period with dynamic SVV deviation contralateral to side of cochlear implantation, but not after two weeks.
6.- FP1410Vestibular Assessment in Children with Sensorineural Hearing Loss
Tamara Hundscheid1, Catherine Jorissen2, Stefanie Vanhecke2, An Boudewyns2, Vincent van Rompaey2, Denise van Barneveld3, Raymond van de Berg1, Josine Widdershoven1,2
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center+, Maastricht, The Netherlands; 2Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Antwerp, Belgium; 3Department of Audiology, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center+, Maastricht, The Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Vestibular hypofunction (VH) is found in 30-70% of children with sensorineural hearing loss (SNHL) due to the proximity of the cochlea and vestibular system. Vestibular assessment in children with SNHL is not standard yet, but critical to locate the optimal cochlear implantation side and start rehabilitation therapy to promote motor development.
Objectives: Evaluate diagnostic accuracy of vestibular tests and provide clinical recommendations for diagnosis.
Methods: The retrospective double-center study included 86 children with SNHL aged 08-18 years. At least two of the following tests were applied per patient: video head impulse test (vHIT, canal test), cervical evoked myogenic potentials (cVEMP, otolith test), rotary chair test (canal test) and caloric test (canal test). VH was diagnosed based on the vestibular test results and clinical presentation.
Results: In the cohort prevalence was 37% (24 patients bilateral and 14 unilateral VH). Diagnostic accuracy was 92% for caloric test, 91% for vHIT, 75% for cVEMp and 77% for rotary chair. Optimal diagnostic accuracy was achieved with the combination of cVEMP and caloric test (92%), or vHIT and cVEMP (90%).
Conclusion: As caloric testing is invasive and differences are small, the clinical recommendation based on this study is to implement vHIT and cVEMP as a first assessment in children with SNHL. These tests assess vestibular function of the canals and otoliths respectively. The need for accurate testing will increase as therapeutic options (e.g. vestibular implant) are under development.
7.- FP1418Skull Vibration Induced Nystagmus Test (SVINT) in Menière’s disease and Vestibular Neuritis
Georges Dumas1,2; Christol Fabre1; Haoyue Tan3; Philippe Perrin2; Sébastien Schmerber1,4
1Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Grenoble Alpes, France; 2EA 3450 DevAH, Development, Adaptation and Handicap, Faculty of Medicine, University of Lorraine, Vandoeuvre-lès-Nancy, France; 3Department of Otolaryngology H&N surgery. Shanghai Ninth people’s Hospital. Shanghai Jiaotong University School of Medicine, Shanghai 200011, China; 4INSERM S 1039 Bioclinic Radiopharmaceutics Laboratory, University Grenoble Alpes, France
OC04
Abstract
Background/objectives: Skull Vibration Induced Nystagmus Test (SVINT) uses Bone conducted Vibrations applied to the cranium to reveal a vibration induced Nystagmus (VIN) related to a vestibular asymmetry in unilateral vestibular lesions (UVL). VIN is relevant from a global canal (predominant) and otolith structures contribution. The aim of this work was to find out in Meniere’s disease (MD) SVIN possible characteristics when compared to those in other acute vestibular disorder [Vestibular neuritis (VN)] and describe its interest among other common vestibular explorations.
Methods: in this retrospective cohort study 32 MD (60 ±18 yo) and 47 VN (59±13yo) were included. Each mastoid was stimulated at 100Hz during 10 seconds. The SVIN slow phase velocity (SPV) was measured in °/s and recorded with a VNG 2D and 3 D.
All the VN had within 1 month and all MD patients had on the same day an audiogram, SVIN, HST, caloric test (CaT), VHIT; some patients had a SVV and VEMPs.
Results: SVIN (corresponding to strict criteria defined) was positive in 21/32 MD (66%) and 42/47 VN (89%), usually beating away from the lesion side. A VIN beating toward the lesion was observed in 3/21 (14%) MD and 1/42 (3%) VN. In VN, SVINT Sensitivity (Se) was equivalent to CaT (Se 86%) and VHIT (Se= 90%) and in MD it was not different from CaT (Se =76%) but different from VHIT (Se=7%)(p< 0.01). SVIN-SPV was significantly higher in VN (7.3±4.9°/s) than in MD (3.89 ± 3.9°/s) (p= 0.001). SVIN direction showed discrepancies with CaT, VHIT, HSN results in 30% of MD.
SVIN-SVP horizontal component was correlated with results of the tests exploring the horizontal canal (Caloric-hypofunction and L-VHIT % asymmetry) in VN and only CaT in MD.
Conclusion: SVINT is a sensitive first line examination test to reveal a vestibular asymmetry in peripheral vertiginous patients during the acute, subacute or chronic period. It has a higher SVIN-SPV in VN than in MD. SVIN is usually beating toward the intact side but is more often beating toward the lesion in MD than in VN. CaT, VHIT, HST, SVIN results are well correlated in VN but often discordant in MD. SVINT Se is equivalent to CaT to reveal MD or VN but SVINT is more sensitive than VHIT in MD. In acute cases of vestibular syndromes its positivity associated with a negative HIT or VHIT suggests usually strongly a MD when performed at the initial consultation.
1.- FP1108Selective Asymmetry of Ocular Vestibular-Evoked Myogenic Potential in Patients with Acute Utricular Macula Loss
Leonardo Manzari1, Marco Tramontano2
1MSA ENT ACADEMY CENTER , Cassino (FR), Italy; 2Fondazione Santa Lucia IRCCS, Rome, Italy
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: An acute vertigo is a challenge for clinicians, who must differentiate a central from different peripheral problems in the acute clinical setting. These conditions cause vertigo and nystagmus, but the assessment, treatment, therapeutic progression, and prognosis could be very different. The bedside oculomotor exam (Head-impulse—nystagmus—test-of-skew (H.I.N.T.S.)) could help in differentiating peripheral from central causes of acute vestibular syndrome (AVS) in the emergency department; however, to establish the damage of vestibular organs and to determine their possible functional recovery, more exams are required
Several studies reported single cases of selective utricular loss in an acute patient diagnosed with ocular vestibular-evoked myogenic potential (oVEMPs) or with subjective visual vertical (SVV), while the remaining sense organs showed normal function on specific tests. In these clinical cases, the authors reported patients with an AVS
Objectives: We retrospectively evaluated a chart review of 3,525 patients evaluated for any acute disturbance. A total of 1,504 patients with acute AVS received an instrumental vestibular assessment within 72 h from the onset of the symptoms evaluated using simultaneously a combination of oVEMPs, cervical vestibular-evoked myogenic potential (cVEMPs), video head-impulse test (vHIT), and SVV were included in this study.
Methods: A total of 41 patients with AVS that showed a normal horizontal canal function tested with vHIT, a normal cVEMP function, unilaterally reduced or absent oVEMP n10, and an altered SVV were enrolled.
Results: We found that although these patients referred acute vertigo and presented spontaneous nystagmus, they showed physiological values of vHIT and a normal saccular function, as shown by symmetrical cVEMPs.
Conclusion: Our findings support the hypothesis that a percentage of patients evaluated during an AVS using an instrumental vestibular assessment could present selective utricular macula dysfunction.
2.- FP1060Side dependent hemispheric influences upon motion detection in acute vestibular neuritis
Qadeer Arshad1 and Adolfo Bronstein
Neuro-Otology Unit, Imperial College London
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Considerable evidence supports the notion that vestibulo-cortical areas are predominantly represented in the non-dominant hemisphere. In healthy individuals, the degree of vestibulo-cortical dominance impacts upon body sway and motion perception. However, the functional relevance of cortical lateralisation in patients with peripheral vestibular loss remains unknown. To investigate this, we performed a retrospective analysis on 34 right-handed patients with acute vestibular neuritis (VN) (21 right-sided VN; 13 left-sided VN; mean age 53) and assessed the interrelationship between a novel surrogate marker of hemispheric vestibulo-cortical dominance and motion detection. To assess motion detection, patients were seated on a motorized chair and rotated from rest with an initial acceleration of 0.3°/s2, increasing by 0.3°/s2 every 3 s until a consistent oculomotor response was observed. In patients with right VN, we observed a positive correlation (R2 0.497) between hemispheric dominance and oculomotor thresholds, whereas, in left VN patients we observed a negative correlation (R2 0.459). Our findings, (i) illustrate the importance of interhemispheric competition on gating subconscious brainstem functions regarding physical motion onset and, (ii) provide a behavioral demonstration of lateralised asymmetries in vestibulo-cortical processing influencing vestibular-behaviour following acute side-specific peripheral vestibular loss.
3.- FP0894Ocular Laterodeviation With Brief Removal of Visual Fixation Differentiates Central form Peripheral Vestibular Syndrome
Sherwin Badihian, John H Pula, Alexander Tarnutzer, David Newman-Toker, David S Zee
University of illiniois College of Medicne. Peoria
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Kattah JC, Badihian S, Pula JH, Tarnutzer AA, Newman-Toker DE, Zee DS.
Objective: Ocular laterodeviation (OLD) is a conjugate, ipsilesional, horizontal ocular deviation with brief (3-5 s) closing of the eyes, commonly linked with the lateral medullary syndrome (LMS). There is limited information regarding OLD in patients with the acute vestibular syndrome (AVS). In one case series 40 years ago, OLD was a central sign. Recently, horizontal ocular deviation on imaging (Rad-OLD) was frequently associated with anterior circulation stroke, e.g., LMS and cerebellar stroke, but without clinical correlation with OLD.
Methods: This is a prospective, cross-sectional diagnostic study of 151 acute AVS patients. All had spontaneous nystagmus. Horizontal gaze palsy was an exclusion criterion. We noted the effect of brief (3-5 s) eyelid closure on eye position and then used the HINTS algorithm (The head impulse test, nystagmus characteristics and skew deviation) and Rad-OLD to establish a correlation between clinical and radiologic findings.
Results: Of the 151 patients, 100 had a central and 51 had a peripheral lesion; 29 of the central lesions were LMS and 11 had OLD. Additionally, one lateral pontine syndrome had OLD. On opening their eyes 11 patients with OLD and LMS made multiple, hypometric corrective saccades to bring gaze back to straight ahead. 10/11 patients with LMS showed Rad-OLD.
Conclusion: OLD with multiple hypometric corrective saccades on opening the eys was an infrequent but highly localizing and lateralizing. We emphasize how simple it is to test OLD, with the caveat that to be specific, it must be present after just brief (3-5 s) eyelid closure
4.- FP1022Short-Latency Covert Saccades - The Explanation for Good Dynamic Visual Performance After Unilateral Vestibular Loss?
Julia Sjögren1, Mikael Karlberg1, Craig Hickson2, Måns Magnusson1, Per-Anders Fransson1, Fredrik Tjernström1
1Department of Clinical Sciences, Otorhinolaryngology Head and Neck Surgery, Skåne University Hospital, Lund University, Lund, Sweden; 2Department of Otorhinolaryngology Head and Neck Surgery, William Harvey Hospital, East Kent Hospitals University Foundation Trust, Ashford, United Kingdom.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Functional head impulse test (fHIT) tests the ability of the vestibulo-ocular reflex (VOR) to allow visual perception during head movements. Our previous study showed that active head movements to the side with a vestibular lesion generated a dynamic visual performance that were as good as during movements to the intact side.
Objective: To examine the differences in eye position during the head impulse test when performed with active and passive head movements, in order to better understand the role of the different saccade properties in improving visual performance.
Method: We recruited 8 subjects with complete unilateral vestibular loss (4 men and 4 women, mean age 47 years) and tested them with video Head Impulse Test (vHIT) and Functional Head Impulse Test (fHIT) during passive and active movements while looking at a target. We assessed the mean absolute position error of the eye during different time frames of the head movement, the peak latency and the peak velocity of the first saccade, as well as the visual performance during the head movement.
Results: Active head impulses to the lesioned side generated dynamic visual performances that were as good as when testing the intact side. Active head impulses resulted in smaller position errors during the visual perception task (p = 0.006) compared to passive head-impulses and the position error during the visual perception time frame correlated with shorter latencies of the first saccade (p < 0.001).
Conclusion: Actively generated head impulses toward the side with a complete vestibular loss resulted in a position error within or close to the margin necessary to obtain visual perception for a brief period of time in patients with chronic unilateral vestibular loss. This seems to be attributed to the appearance of short-latency covert saccades, which position the eyes in a more favorable position during head movements.
5.- FP1081Postural and Head Responses to Sensory Perturbations in People with Unilateral Hearing or Vestibular Loss vs. Healthy Controls: A Pilot Study
Anat V. Lubetzky1, Jennifer L. Kelly2,3, Daphna Harel4, Bryan D. Hujsak2,3, Maura Cosetti3
1Department of Physical Therapy, Steinhardt School of Culture Education and Human Development, New York University, New York, NY, USA; 2Vestibular Rehabilitation, New York Eye and Ear Infirmary of Mount Sinai, New York, NY, USA; 3Department of Otolaryngology-Head and Neck Surgery, New York Eye and Ear Infirmary of Mount Sinai, New York, NY, USA; 4New York University, Department of Applied Statistics, Social Science and Humanities, Steinhardt School of Culture Education and Human Development
Background: The mechanism underlying the relationship between hearing loss and balance dysfunction is still debatable and is and possibly relates to concurrent subclinical vestibular impairment. In addition, the specific implications of Unilateral Sensorineural Hearing Loss (USNHL) to balance are not well understood. This pilot study aimed to identify postural strategies in response to sensory perturbations (visual, auditory, somatosensory) in adults with and without sensory loss.
Methods: We tested people with unilateral peripheral vestibular hypofunction (N=12, mean age 62, range 23-78), or with USNHL (N=9, 48, 22-82), or healthy controls (N=21, 52, 28-80). Postural sway and head kinematics parameters (Directional Path in the anterior-posterior and medio-lateral directions (sway & head); pitch, yaw and roll (head) were analyzed in response to 2 levels of auditory (none, rhythmic sounds via headphones), visual (static stars, the stars walls oscillated in the anterior-posterior direction at 0.2 Hz, 32 mm amplitude) and somatosensory cues (floor, foam) within a simulated, virtual 3-wall display of stars projected from the HTC Vive Pro Eye.
Results: No differences were observed when auditory cues were added for any of the outcome measures. The two levels of sounds were then combined for further analysis. The effect of surface was magnified in the vestibular group compared with controls for anterior-posterior and medio-lateral postural sway, and all head direction except for medio-lateral. The USNHL group did not increase their medio-lateral sway with the foam as much as controls did. Unlike the control and vestibular groups, the USNHL group did not increase their anterior-posterior and medio-lateral sway and head movement with the increased visual load, particularly when standing on foam. The vestibular group had significantly larger anterior-posterior and medio-lateral postural sway and head movement on the static scene compared with controls. Differences in pitch, yaw and roll emerged between vestibular and controls only with sensory perturbations.
Conclusion: Patients with vestibular hypofunction were destabilized by the sensory perturbations more than healthy controls in all directions. Postural patterns of participants with USNHL did not resemble any of the other groups and demonstrated minimal sway changes with perturbations. It is possible that individuals with USNHL employ a compensatory strategy of conscious control of balance unlike people with vestibular hypofunction who demonstrated difficulty in sensory weighting and reweighting. Head movement was similar between USNHL and controls and notably larger in the vestibular group, adding to prior data suggesting a specific pattern of head kinematics unique to vestibular dysfunction.
6.- FP1102Yaw, Pitch and Roll Plane Instability: Axis differences following acute Unilateral Vestibular Loss.
John H.J. Allum, Claudia Candreia and Flurin Honegger.
Departments of ORL, University of Basel Hospital, Basel and Cantonal Hospital, Luzern, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
BACKGROUND: For a number of reasons, clinical dynamic posturography concentrates on pitch and roll and not yaw plane measures. This emphasis may not represent axis instability observed in clinical stance and gait tasks for heathy control (HC) subjects and patients with balance deficits, as well as group differences. To examine this question, we measured trunk sway in all 3 directions (pitch, roll and yaw) during stance and gait tasks for healthy controls (HC) and patients with acute unilateral vestibular neuritis (aUVN).
METHODS: Results of 12 patients (mean age 61 years) recorded within 6 days of aUVN onset were compared within those of 8 age-matched healthy controls (HCs). All subjects performed a 2-legged stance task, standing eyes closed on foam (S2ecf), a semi-gait task - walking 8 tandem steps (tan8), and 4 gait tasks – walking 3m with head rotating laterally, pitching, or eyes closed (w3hr, w3hp, w3ec), and walking over 4 barriers 24 cm high, spaced 1 m apart (barr). Task peak-to-peak yaw, pitch and roll angles and angular velocities were measured with a gyroscope-system (SwayStarTM) mounted at L1-3 and combined into 3, axis specific, balance control indexes (BCI) using angles (a) for tandem gait and barriers task and angular velocities (v) for all other tasks:
((2*s2ecf) + 1.5*(w3hr+w3hp+w3ec))v + (tan8+12*barr)a
RESULTS: Yaw and pitch BCIs were significantly (p=0.004) greater (88 and 30%, respectively) than roll BCIs for aUVN patients. For HCs only yaw but not pitch BCIs were greater (p=0.002) than those of roll (72%). The order of BCI aUVL vs. HC differences was pitch, yaw, and roll: 55, 44 and 31%, respectively (p=0.002).
CONCLUSIONS: These results indicate greater yaw than pitch and roll trunk motion during clinical balance tasks is common for aUVN patients and HCs. However, aUVN leads to a larger increase in pitch than yaw plane instability and a smaller increase in roll plane instability This difference with respect to roll corresponds to the known greater yaw plane than roll plane asymmetry (40 vs 22%) following aUVN observed in vestibular ocular reflex (VOR) responses. However the lower pitch plane asymmetry (3.5%) in VOR responses does not correspond with the greater pitch plane instability observed in balance control. Whether the directional specific recovery processes for balance control and VOR responses are similar remains to be investigated. The current results provide a strong rationale for clinical testing of directional specific balance responses, concentrated on pitch and yaw.
7.- FP1262Longitudinal whole-brain metabolic network changes following peripheral acute unilateral vestibulopathy
Andreas Zwergal, Maximilian Grosch, Hans-Georg Buchholz, Sibylle Ziegler, Thomas Brandt, Marianne Dieterich, Sandra Becker-Bense
German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Symptoms of acute unilateral vestibulopathy (AUV) partially recover due to adaptive brain plasticity. In this study, we analysed whole-brain metabolic connectivity changes after peripheral AUV by longitudinal [18]F-FDG-PET imaging.
Methods: 22 patients with AUV underwent resting state [18]F-FDG-PET scans in the acute stage (mean: 6 d) and after partial behavioural compensation in the chronic stage (mean: 6 m). PET data were compared to 22 matched controls. Images were flipped, reconstructed, registered, filtered, normalized, and segmented (AAL2/3 atlas). Pearson’s correlations between all segmented brain regions were performed (|r| > 0.5, p < 0.001 or p < 0.05 for subgroup analysis). Functional metabolic connections between and within hemispheres, and in vestibular/multisensory/motor/cognitive networks were calculated.
Results: Patients had severe vestibular asymmetry in the acute stage (mean horizontal slow-phase velocity (SPV): 9.9 °/sec, tilt of subjective visual vertical (SVV): 7.6 °), which recovered until 6 m after AUV (SPV: 0.7 °/sec, SVV: 1.7 °). As compared to controls, whole-brain metabolic network analysis indicated a significant drop in the total number of connections (by 52%), and specifically in interhemispheric projections between homotopic regions (by 61%) in the acute stage. In the chronic stage, the asymmetry in interhemispheric connections of homotopic regions persisted. Multisensory network connectivity relatively increased in the ipsilesional hemisphere compared to the early stage as a sign of sensory substitution. Patients with a persistent caloric vestibular deficit had a higher asymmetry index compared to those with reconstituted peripheral function (32.4% vs 52.1% homotopic regions).
Conclusion: AUV disrupts the symmetry of multisensory metabolic networks between hemispheres persistently and especially in patients with a chronic peripheral vestibular deficit. These data are important for the understanding of higher sensory network dysfunction and may explain a conversion risk to functional dizziness after AUV.
Authors:
Eugen Ionescu
Ashley Wackym
Gerard Gianoli
Abstract: While superior semicircular canal dehiscence is relatively well-known in the medical community, there are many other sites of dehiscence creating a third mobile window resulting in Third Window Syndrome. Over the past quarter century, there has been tremendous expansion of the depth of our knowledge and understanding of third window syndrome; however, the identification of lesser-known sites of dehiscence remains an important diagnostic and therapeutic challenge. This is more so as in our experience third window syndrome, including superior semicircular canal dehiscence, remains under-diagnosed. Therefore, the development of a unitary anatomical-clinical and radiological classification would be an important step for a better understanding of these pathologies by neurotologists, otologists, neurologists, auditory-vestibular specialists, otolaryngologists and neuroradiologists. Thus, the probability of being left without an etiological diagnosis in the case of pseudo conductive hearing loss with or without obvious associated vestibular phenomena should become lower.
Materials and methods: Imaging records of 259 patients who underwent, over the last six years, a high-resolution computed tomography (HRCT) of the petrosal bone for conductive hearing loss were analyzed retrospectively. Patients with degenerative, traumatic or chronic infectious petrosal bone pathology were excluded. As cases with a clinical presentation similar to those of a third window syndrome have recently been described in the literature but without these being confirmed radiologically, we thought it necessary to be integrated in a separated branch of this classification as “CT - TMWA”. The same goes for certain intralabyrinthine pathologies also recently reported in the literature, which mimic to some extent the symptoms of a third window pathology. Therefore, we suggest calling them intralabyrinthine TW- like abnormalities.
Results: Temporal bone HRCT and, in some cases, 3T MRI of 97 patients presenting symptomatic or pauci-symptomatic, single or multiple, unilateral or bilateral OCD were used to develop this classification. According to the topography and anatomical structures involved at the site of the interface of the third window, a third-type classification of OCD is proposed.
Conclusion: A classification reuniting all types of TWMA as the one proposed in this paper would allow for a better systematization and understanding of this complex pathology and possibly pave the way for innovative therapeutic approaches. To encompass all clinical and radiological variants of TMWA reported in the literature so far, TWMAs have been conventionally divided into two major subgroups: Extralabyrinthine (or “true” OCD with three subtypes) and Intralabyrinthine (in which an additional mobile window-like mechanism is highly suspected) or TMWA-like subtype. Along these subgroups, clinical forms of OCD with multiple localization (Multiple OCD) and those that, even though they have obvious characteristics of OCD have a negative CT scan (or CT – TMWA), were also included.
9.- FP1424Otolith-ocular Function and Compensatory Effect of Neck Following Vestibular Loss
Yuchen Yang1, Jing Tian1, Jorge Otero-Millan2, Michael C Schubert3,4, Amir Kheradmand1,3
1 Department of Neurology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA; 2Herbert Wertheim School of Optometry & Vision Science, The University of California, Berkeley, CA, USA; 3Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD, USA; 4Department of Physical Medicine and Rehabilitation, The Johns Hopkins University School of Medicine, Baltimore, MD, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ✓ No
Vestibular inputs converge with visual and proprioceptive information to serve sensorimotor functions that control posture and gaze. In this multimodal process, neck proprioception contributes to gaze control through the cervico-ocular reflex in conjunction with vestibular inputs. Such contribution has been mainly studied with respect to the semicircular canals and not much is known about interactions between the neck proprioception and otolith inputs. Here we studied the contribution of neck inputs to otolith-ocular function at different stages of recovery from vestibular loss. We used video-oculography (VOG)-based measurement of static ocular counter-roll (vOCR) determined 30 seconds after the dynamic tilt to assess otolith function. To elucidate a compensatory effect of neck proprioception, vOCR was measured with 30° static whole-body tilt (WBT) and head-on-body tilt (HBT). The vOCR with WBT is primarily driven by the otolith inputs, whereas with HBT there is also a neck contribution. Fifty-six subjects were recruited including patients with acute (9 days [mean]), subacute (61 days), and chronic (985 days) unilateral loss of vestibular function, as well as a group healthy controls. The vOCR on the lesion side was lower with WBT than with HBT in the acute and subacute groups but not in the chronic group or controls (HBT: acute 3.45±0.44°, subacute 4.27±0.33°, chronic 3.82±0.47°, control 4.79±0.32°/ WBT: acute 2.19±0.50°, subacute 3.37±0.39°, chronic 4.00±0.49°, control 5.40±0.35°). The vOCR on the non-lesion side with WBT was not different than with HBT in all patient groups or controls (HBT: acute 4.38±0.44°, subacute 4.13±0.27°, chronic 3.75±0.48°, control 4.79±0.32°/ WBT: acute 3.80±0.54°, subacute 3.92±0.37°, chronic 4.00±0.42°, control 5.40±0.35°). The vOCR with WBT, as opposed to HBT, could distinguish among the patient groups at various stages of vestibular loss. These findings show a compensatory effect of neck proprioception that can enhance otolith-ocular function following vestibular loss.
SY0036SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Dr. Aasef G. Shaikh |
| TOPIC DESCRIPTIVE TITLE: | Big Data Analytics to dissect waveform patterns in cerebellar and brainstem disorders of gaze holding. |
| ACADEMIC / HOSPITAL AFFILIATION: | Neurology, Case Western Reserve University, Cleveland, OH, USA |
- SPEAKER 2
| NAME AND SURNAME: | Dr. Andreas Zwergal |
| TOPIC DESCRIPTIVE TITLE: | The role of machine learning in identifying central vestibular syndromes |
| ACADEMIC / HOSPITAL AFFILIATION: | Neurology, University Hospital of Munich, LMU Munich, Munich, Germany |
- SPEAKER 3
| NAME AND SURNAME: | Dr. Alexander Tarnutzer |
| TOPIC DESCRIPTIVE TITLE: | Pattern recognition in peripheral-vestibular disorders - impact of machine learning |
| ACADEMIC / HOSPITAL AFFILIATION: | Neurology, Cantonal Hospital of Baden, Switzerland |
- SPEAKER 4
| NAME AND SURNAME: | Click here to write |
| TOPIC DESCRIPTIVE TITLE: | Click here to write |
| ACADEMIC / HOSPITAL AFFILIATION: | Click here to write |
Pattern recognition is an important approach in neuroscience to classify observations and to establish links between reported symptoms, observed findings, and specific disorders. Disorders with distinct underlying pathophysiology can cause subjectively similar vestibular deficits and ocular motor syndromes. This is true both in the setting of acute (either new-onset or episodic) vertigo or longstanding ocular motor deficits presenting with chronic gaze instability, oscillopsia, and balance impairment. In this context, making the correct diagnosis is often challenging, delaying appropriate treatment and thus significantly affecting the patient’s quality of life. Machine learning algorithms and Big Data Analytics techniques were recently proposed and have advanced our ability to accurately recognize abnormal vestibular and ocular motor patterns. This approach has significantly impacted diagnostic accuracy. This symposium will address the impact of machine learning algorithms and Big Data Analytics on neuro-otology, highlightening advances made and limitations faced when implementing this technique. The symposium has three lectures featuring different diagnostic scenarios focusing on acute, episodic or chronic vertigo/dizziness and ocular motor deficits. Dr. Aasef Shaikh will summarize the role of Big Data Analytics in signal processing and pattern recognition of heteroneous nystagmus waveforms of immune and degenerative disorders. Shaikh will demonstrate how these techniques facilitate knowledge of mechanistic underpinning and measures therapeutic response. Dr. Andreas Zwergal will address the impact of machine-learning algorithms in identifying potentially life-threatening conditions in the context of acute vestibular syndromes. Dr. Alexander Tarnutzer will discuss the value of machine-learning-based pattern recognition in peripheral-vestibular disorders. All three speakers will emphasize the future applications of machine learning and Big Data Analytics in neuro-otology, its current limitations, and strategies for overcoming such limitations.
ABSTRACT 1
Gaze-holding disorders suggest abnormal brainstem and cerebellar physiology. Dissecting the waveform patterns is fundamental to understanding the disease, knowing its impact on the quality of life, and assessing the treatment efficacy. The waveform heterogeneity poses a significant challenge for such a task. We will discuss how Big Data Analytics and machine learning dissect the heterogeneous waveform shapes and how signal entropy measures the waveform complexity. We will demonstrate Big Data Analytics facilitated classification of the gaze-holding deficits in the syndrome of anti-GAD antibodies. We will discuss how this approach has provided insight into the pathophysiological framework of this autoimmune disease. We will highlight Big Data Analytics technique revealing distinct patterns of the oscillatory waveform in the syndrome of ocular palatal tremor. Waveform pattern analysis has revealed the physiological foundation for suboptimal symptom resolution. Finally, we will discuss how this approach can be powerful in a much broader scheme.
ABSTRACT 2
Multivariable analyses (MVA) and machine learning (ML) applied on large datasets may have the potential to support clinical decisions in neuro-otology. The speaker will illustrate the application of novel MVA/ML methods in different clinical scenarios. Firstly, the classification accuarcy of MVA/ML techniques for peripheral vs. central etiologies of acute vestibular disorders will be discussed against standard approaches (e.g., HINTS). If based on a multimodal dataset (including VOG-data) ML-approaches can increase the sensitivity and selectivity of correct diagnosis and learn to put weights on clinically plausible features (e.g., HIT). Secondly, the potential of MVA/ML techniques for the classification of episodic and chronic vestibular disorders will be described for typical clinical scenarios. In this context, the speaker will report on a systematic evaluation of different classification methods implemented in a new open-source tool. Finally, the current challenges and limitations of MVA/ML and future perspectives for a more appropriate use will be discussed.
ABSTRACT 3
This talk will focus on how to implement machine-learning algorithms to advance our understanding of unilateral and bilateral peripheral-vestibular disorders. The speaker will summarize progress recently made in pattern recognition of quantitative vestibular testing results (including the semicircular canals and the otolith organs). It will compare patterns identified in various vestibular disorders including acute peripheral vestibulopathy, Menière’s disease and aminoglycoside-related vestibulopathy and illustrate the impact of machine-learning algorithms in these disorders. The speaker will demonstrate how the hierarchical clustering analysis significantly facilitated pattern recognition in peripheral-vestibular disorders, but also address limitations faced in this field. This includes the difficulty of selecting the most appropriate clustering algorithm, parameter validation and arbitrary choices that have to be made in the process of setting up machine-learning algorithms. Furthermore, emerging future applications of machine-learning algorithms in peripheral-vestibular disorders will be discussed and expected challenges considered.
ABSTRACT 4
Click here to write.
OC05 1.- FP0921Development of a Combined Audio-Motion System to Drive Cochleo-Vestibular Implants
David Lanthaler1, Patrick P. Hübner2, Matthew D. Parker2, Angélica Pérez Fornos3, Viktor Steixner1, Andreas Griessner1, Clemens M. Zierhofer1
1University of Innsbruck – Department of Mechatronics, 2MEDEL – Innsbruck, 3Geneva University Hospitals and University of Geneva – Cochlear Implant Center
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
We present a wearable audio-motion system, which has been developed to drive the cochleo-vestibular implants that have been implanted at the Geneva University Hospitals and at the Maastricht University Medical Centre. These implants are used daily by people with both severe hearing loss and bilateral vestibular loss but only for hearing restoration. Electrodes placed in the semicircular canals allow laboratory-controlled investigations into electrical stimulation of the labyrinth. The presented system therefore provides a new research platform for combined stimulation in subjects with hearing and vestibular loss. It consists of an off-the-shelf audio processor, a novel motion processor, and a transmitting coil. As in a standard cochlear implant system, sound from the environment is recorded with microphones and processed by the audio processor. In addition, the motion of the head is recorded with a 6-axis inertial measurement unit, and transformed into stimulation commands in the motion processor. Both the audio and motion command signals are then merged within the motion processor and transmitted via an inductive link to a cochleo-vestibular implant, which stimulates the semicircular canals of the vestibular organ and the cochlea accordingly through a custom electrode array.
The presented work gives insights into the system architecture of the device for combined stimulation and shows first results. The presentation is intended for audiences who are interested in combined vestibular and cochlear implant technologies, and may additionally be interesting for clinicians.
2.- FP0973Ionic Direct Current Vestibular Prosthesis Initiative at Johns Hopkins University
Gene Fridman
Johns Hopkins University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Vestibular prostheses designed to replace semicircular canal function in patients with bilateral vestibular disorders use biphasic charge-balanced stimuli to excite neural activity. Because biphasic pulses cannot inhibit activity, to generate bidirectional encoding of motion, implants must artificially elevate the verstibular afferents’ spontaneous rate and then modulate around this increased baseline. The VOR responses to this stimulation modality are severely attenuated in both directions of motion (toward and away from the implanted side). The elevated baseline of activity delivered by pulsatile stimuli was shown to lead to synchronous unnatural activation of the vestibular afferents that then cause attenuation of the PVP neural responses in the vestibular nucleus that receive their inputs.
In our laboratory, we are developing a novel vestibular implant that is capable of delivering ionic direct current (iDC) instead of biphasic pulses to modulate vestibular nerve activity. This has not been possible before because direct current delivered to metal electrodes causes electrochemical reactions. Our implant, called Freeform Stimulator (FS) uses a microfluidic circuit to convert biphasic pulses delivered to electrodes positioned inside the device to direct ionic current delivered to the neural targets.
Over the past five years we, along with multiple other invstigators at Johns Hopkins University made considerable strides toward technology development, toward our understanding of how iDC can be delivered to the vestibular labyrinth, and toward how it can be used to deliver the sensation of head velocity independently about the three spatial axes of head motion. Our initial experiments were conducted in gentamicin-treated chinchillas to ablate normal vestibular sensation and implanted with intra-labyrinthine microcatheter tubes that deliver iDC. These experiments show that the range of encoding of head motion toward the implanted side using cathodic stimulation is approximately 2-3x that of pulsatile modulation. The range of head velocities in the direction away from the stimulated canal using anodic current to inhibit firing rate is approximately 2x that of pulsatile modulation. These results are especially exciting because the responses are achieved with reduced error in alignment of VOR eye response to desired angle of motion compared to pulsatile stimulation, including when the stimulation is delivered via multiple canals simultaneously to span the range of possible angles in 3D space. In follow-up in-vitro experiments, we characterized the afferent responses to iDC stimulation and identified that these responses are remarkably similar to the normal responses to mechanical stimuli.
3.- FP1221First-in-Human Trial of the Labyrinth Devices Multichannel Vestibular Implant – Interim Results After 1-5 Years of Continuous Daily Use
Charles C Della Santina1,2,3, Margaret R Chow2,3, Andrianna I Ayiotis2, Desi P Schoo1, Peter J Boutros2, Mehdi Rahman1,2,3, Nicolas S Valentin1,2,3,4, Stephen Bowditch1, Celia Fernandez Brillet2, Brian Morris2, Kelly Lane1, Yoav Gimmon1, John P Carey1, Bryan K Ward1, and the Labyrinth Devices LLC3 and MED-EL GmbH4 Vestibular Implant Research and Development Teams
1Johns Hopkins School of Medicine Department of Otolaryngology – Head & Neck Surgery; 2Johns Hopkins University Department of Biomedical Engineering; 3Labyrinth Devices, LLC; 4MED-EL GmbH
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Bilateral loss of vestibular sensation is disabling. Affected individuals suffer chronic disequilibrium, increased fall risk and inability to maintain stable vision during head movement. To determine whether prosthetic electrical stimulation via intra-ampullary electrodes targeting semicircular branches of the implanted ear’s vestibular nerve is feasible, safe and effective, we initiated a first-in-human clinical trial of continuous motion-modulated prosthetic stimulation using the MVI™ Multichannel Vestibular Implant System developed by Labyrinth Devices LLC and MED-EL GmbH.
Methods: Ten subjects (5 male, 5 female, age 52-66 years at implantation) with bilateral vestibular hypofunction proven by caloric nystagmography, video head impulse testing, rotary chair testing, history and examination underwent unilateral implantation from August 2016 to July 2021. Seven had ototoxic loss due to intravenous or intratympanic injection; three had idiopathic loss. Duration since onset of symptoms ranged from 2-24 years. We assessed pre-op and post-activation performance using binocular 3-dimensional vestibulo-ocular reflex (3D VOR) responses to head rotation (yaw, LARP and RALP head-on-body impulses delivered by a Labyrinth Devices aHIT motorized system; 0.1-2 Hz whole-body yaw rotation via rotary chair), pure tone and speech audiometry, dynamic visual acuity, clinical tests of posture and gait, and validated patient-reported outcome instruments for disability (Dizziness Handicap Inventory, Vestibular Activities of Daily Living) and health-related quality of life (SF36 and Health Utilities Index [HUI3]).
Results: Every subject has worn the system’s external component daily since device activation. Six wear it 24 hr/day; 4 take it off while in bed. All subjects have electrically-evoked VOR responses (typically ranging from ~5-100°/s and aligned approximately with the stimulated canal) for at least one electrode for each of the three implanted canals. VOR responses are significantly greater with motion-modulated stimulation than without. Motion perception thresholds are below VOR thresholds. Hearing sufficient for unaided telephone use has been preserved in 6 of 10 implanted ears. Posture, gait metrics, dizziness handicap, vestibular disability and health-related quality of life (quantified by SF36-derived SF6D utility) improved significantly compared to preop for the group. HUI3, which more heavily weights hearing, did not significantly change.
Conclusions: The Labyrinth Devices MVI™ vestibular implant system can be implanted in an outpatient surgery, generates motion percepts and 3DVOR responses consistent with semi-selective stimulation of each of the three implanted canals, can be implanted with a preservation of useful hearing, and yields significant improvement in postural stability, gait, patient-reported disability and quality of life.
Support: NIH R01DC13536, U01DC0019364; Labyrinth Devices LLC; MED-EL GmbH
4.- FP1288Clinical results of otolith electrical stimulation using a vestibular implant in patients with bilateral vestibular loss
Speaker: Angel Ramos Macias1
Co-Authors: Andrzej2, Manuel Manrique3, Maurizio Barbara4, Carl van Himbeeck5 , Angel Ramos de Miguel1
Type: ORAL PRESENTATION
1. Las Palmas de Gran Canaria University (SIANI), Las Palmas,Spain. Department of Otolaryngology, Head and Neck Surgery, Complejo Hospitalario Universitario Insular Materno Infantil de Gran Canaria, Las Palmas, Spain.
2. Otolaryngology Dept . University Hospital , Antwerp. Belgium
3. Otolaryngology Dept . Navarra University . Spain
4. Otolaryngology Dept . Sapienza University . Rome . Italy
5. Cochlear AG . Switzerland.
Objective: The objective of this study is to analyze the clinical outcomes in patients with Otolith chronic electric stimulation by using a cochlea/vestibular implant .
Material and Methods: 11 patients with bilateral vestibular loss (BVL) were recruited for unilateral cochleo/vestibular research implant (CVI) for Otolith chronic electric stimulation .We use a two electrode array stimulation ( Cochlear and Otolith) were three Full-band electrode array were implanted close to the to the saccular area, and 19 were located intracochlear in a second independent array. The objective was to analyse the effect of chronic electrical stimulation and the adaptation to electrical stimulation of the vestibular system in humans when the otolith organ is stimulated with a constant pulse train to mitigate imbalance due to bilateral vestibular dysfunction.
In this research we will present the postoperstive results with a minimum follow up of 6 months up to 1 year. Dynamic Visual Acuity testing (DVA), subjective visual horizontal and vertical tests, Dizziness Handicap Index (DHI), Timed Up and Go Test (TUG) and Dynamic Gait Index (DGI) were used.
Results: The analysis revealed a statistically significant benefit when the vestibular implant system is in “switch on” test condition , compared with the “switch off” situation, in all tests.
Preliminary Conclusions: These results demonstrate that gaze stabilization abilities can be restored by using a chronic electrical otolith stimulation delivered by a vestibular research implant. The otolith implant shows considerable promise of being an effective therapeutic alternative for patients with a BVL.
5.- FP1291Electrical stimulation of the human semicircular canals and possible other solutions for bilateral vestibulopathy
Raymond van de Berg1, Sharon Cushing2
1The Hospital for Sick Children, University of Toronto (Canada)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
The Geneva-Maastricht team currently investigates the Vestibular Implant (VI). This is a modified cochlear implant that restores hearing as well as vestibular function. It comprises a cochlear array that is inserted into the cochlea, and 3 vestibular arrays that are inserted into the semicircular canals or directly onto the nerves. Thirteen patients have been implanted. The main results are: 1) electric vestibular stimulation is feasible and safe in humans; 2) an electrically evoked vestibulo-ocular reflex can be elicited in all frequency domains; 3) perceptual symptoms can be elicited by VI-stimulation; 4) canal stimulation also stimulates the otolith organs: electrically evoked VEMPs and postural responses have been obtained; 5) the dynamic visual acuity can be improved. Although many biomechanical issues still need to be addressed before it can be clinically applied, these results show that the VI is feasible as a therapeutic device in the near future.
6.- FP1343Vestibulo-cochlear implants in humans: rehabilitation of the inner ear
Nils Guinand1, Raymond van de Berg2,3, Maurizio Ranieri1, Samuel Cavuscens1, Anissa Boutabla1, Julie Corrre1, Herman Kingma2,3, and Angélica Pérez Fornos1
1Division of Otorhinolaryngology Head and Neck Surgery, Geneva University Hospitals and University of Geneva, Geneva, Switzerland; 2Division of Balance Disorders, Department of ENT, Maastricht University Medical Centre, Maastricht, The Netherlands; 3Faculty of Physics, Tomsk State Research University, Tomsk, Russia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Bilateral vestibulopathy is a heterogeneous disorder resulting in many disabling symptoms, including imbalance, oscillopsia, reduced mobility, and increased risk of falling. It has even been associated with cognitive impairments. Unfortunately, the prognosis is poor and currently available treatment options have very low efficacy.
Vestibular implants are medical devices that aim to restore vestibular function in patients with severe bilateral vestibulopathy using motion modulated electrical stimualtion. Our group, the Geneva-Maastricht team, developed an original concept based on a modified cochlear implant. This Vestibulo-Cochlear implant, developed in close collaboration with MED-EL (Innsbruck, Austria), provides 1 to 3 extra-cochlear electrodes which are implanted in the vicinity of vestibular afferents in addition to the “standard” cochlear implant array. Since 2007, 17 deaf ears in 17 patients with severe bilateral vestibulopathy have been implanted without surgical or medical complications.
Humans have demonstrated surprising adaptation capabilities to the artificial vestibular electrical stimulation. Successful restoration of the vestibulo-ocular reflex in the mid- to high- frequency range has been demonstrated using standard clinical tests (rotatory chair and video-head impulse test). We also showed that it is possible to activate the vestibulo-collic reflex using measures of cervical myogenic vestibular evoked potentials. Controlled postural responses could also be obtained with our prototype vestibular implant device. Finally, visual abilities in dynamic settings were restored with the vestibular implant. The latter is a major step forward, providing the first ever demonstration of useful rehabilitation of this patient population.
Recent refinement of the electrodes design and the use of peroperative monitoring of the electrode insertion has allowed otpimization of the surgical procedure. Thanks to the new wearable “Auditory-Motion-Processor”, implanted patients are currently beeing tested in close to real life conditions. Hearing performance and potential interference with the vestibular stimulation are also being assessed.
Results obtained so far in humans are very encouraging. We hope that the increasing interest in this field and the substantial research efforts allocated lead to a clinical application in the near future. It should also be mentioned that the vestibular implant opens new possibilities for exploring several fundamental issues: balance function, the adaptive capacities of the brain, the processes of temporal integration of sensory information necessary for equilibrium, and probably for better understanding vestibular physiology and vestibular disorders. Therefore, the vestibular implant opens new perspectives, not only as an effective therapeutic tool, but also pushes us to go beyond current knowledge and well established clinical concepts.
SY0029SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Pieter Medendorp |
| TOPIC DESCRIPTIVE TITLE: | Multisensory processing and sensory reweighting in bilateral vestibulopathy |
| ACADEMIC / HOSPITAL AFFILIATION: | Radbound University/ Donders Institute for Brain, Cognition and Behaviour |
- SPEAKER 2
| NAME AND SURNAME: | Marianne Dieterich |
| TOPIC DESCRIPTIVE TITLE: | Neuroimging insights into the cerebral cortical involvement in functional dizziness |
| ACADEMIC / HOSPITAL AFFILIATION: | Ludwig-Maximilian-University/ German Center for Vertigo and Balance Disorders |
- SPEAKER 3
| NAME AND SURNAME: | Jeffrey P. Staab |
| TOPIC DESCRIPTIVE TITLE: | Pathological shifts in spatial perception – PPPD and vestibular migraine |
| ACADEMIC / HOSPITAL AFFILIATION: | Mayo clinic/ Mayo clinic |
- SPEAKER 4
| NAME AND SURNAME: | Qadeer Arshad/Amir Kheradmand |
| TOPIC DESCRIPTIVE TITLE: | Multisensory mechanisms of dizziness in vestibular migraine/ Synopsis and Further Directions |
| ACADEMIC / HOSPITAL AFFILIATION: | University of Licester/ Johns Hopkins |
Clinical research into the vestibular system has mainly focused on the low-level, brainstem or cerebellar mediated vestibulo-ocular functions in recent decades. Relatively little attention has been paid to the perceptual functions of the vestibular system including its role in spatial orientation, which is directly linked with the disabling symptoms of diseases affecting the vestibular system. In recent years, however, with the progress in the clinical classifications of the vestibular disorders, and the formal recognition of conditions such as vestibular migraine and persistent postural-perceptual dizziness (PPPD), the gaps in understanding higher-level vestibular functions and their link to the clinical symptoms are now more evident than ever.
In this symposium our goal is to present recent findings focused on the pathophysiology of vestibular perception and advances made in their clinical applications. Given the translational nature of this topic, both clinicians and scientists with interest in the vestibular disorders and sensory physiology will be the proper target audience for these presentations. In the first talk, Pieter Medendorp will start with the effect of peripheral vestibular loss on perception of spatial orientation, and how the findings can be applied clinically for diagnosis and development of targeted treatments. The second talk by Marianne Dieterich will discuss the neuroimaging evidence for involvement of specific brain regions in perceptual symptoms of PPPD. In the third talk, Jeffrey Staab will review the emerging concepts related to the pathophysiology of vestibular perception based on the common features in PPPD and vestibular migraine. Finally, the last talk by Qadeer Arshad will provide updates on vestibular migraine with a review of recent findings related to the pathophysiology of spatial disorientation and motion perception in these patients. At the end, Amir Kheradmand will provide a summary of scientific findings from other talks and their clinical relevance to highlight some of the key findings and ‘take-home’ messages.
ABSTRACT 1
Perception of spatial orientation involves a weighted fusion of visual, vestibular, proprioceptive and somatosensory signals, as well as internal beliefs. When one of these signals breaks down, such as the vestibular signal in bilateral vestibulopathy, patients can compensate by relying more on the remaining cues. How the remaining signals are reweighted in this integration process has remained difficult to quantify since the quality of these signals can typically not be measured in isolation. I will present our recent work combining experimental psychophysics with a reverse engineering approach based on Bayesian inference principles to characterize sensory reweighting in individual bilateral vestibular patients. This personalized quantification approach could aid in the diagnostics and prognostics of multisensory integration deficits in vestibular disorders, and contribute to the evaluation of the effect of rehabilitation therapies, including balance training exercises.
ABSTRACT 2
Functional dizziness is among the most common diagnoses in patients with vestibular symptoms with largely unknown pathophysiology. In this presentation I will review the recent neuroimaging studies in patients with persistent postural perceptual dizziness (PPPD), which found structural changes in the prefrontal cortex and the associated thalamic projection zones. With respect to the visual functions, the patients showed increased visual motion-induced activity and aftereffect in the anterior cingulum compared to healthy controls. The results agree with the features of dizziness in PPPD, including excessive self-awareness, anxious appraisal, and obsessive controlling of posture. These findings indicate that the symptoms are caused not only by aberrant processing in the cortical visual or vestibular regions, but they also involve the networks that contribute to mood regulation, fear generalization, and interoception as part of the pathophysiology.
ABSTRACT 3
Persistent postural-perceptual dizziness (PPPD) and vestibular migraine (VM) are two of the most common diagnoses in tertiary neurotology. Both are associated with increased sensitivity to space-motion stimuli. In physiological studies, patients with PPPD and VM showed increased sensitivity to complex or moving visual stimuli compared to healthy controls. Patients with VM also showed increased sensitivity to head tilt. In resting state and task-driven functional MRI studies, patients with PPPD compared to healthy controls had reduced activity and connectivity in vestibular cortex and hippocampus, but increased activity and connectivity in frontal and occipital regions. In a PET study, two patients with VM had increased activity in the vestibular cortex and decreased activity in visual areas during attacks. Thus, patients with PPPD and VM both demonstrate alterations in perception of space-motion information, though underlying brain mechanisms may involve differential hypersensitivity to visual and vestibular stimuli.
ABSTRACT 4
Patients with vestibular migraine typically have a normal vestibulo-ocular examination with no sign of peripheral vestibular dysfunction. Further, objective laboratory testing of peripheral vestibular function is unremarkable, implying that dizziness in these patients is mediated by higher-level central mechanisms. Accordingly, elucidating the neural correlates of spatial disorientation in vestibular migraine and the link with dizziness in these patients is a research priority, as it can open the window to novel therapeutic strategies. This presentation will focus on recent findings in vestibular migraine related to multisensory mechanisms that contribute to spatial disorientation and altered weighting of visual and vestibular signals that contribute to motion misperception in these patients. We will also address the clinical gap related to lack of objective measures of dizziness in vestibular migraine and how the approaches outlined here can be applied to develop biomarkers for diagnosis, track recovery, or evaluate the effects of treatments in these patients.
OC06 1.- FP1300Concurrent Brain Structural and Functional Alterations in Patients with Chronic Unilateral Vestibulopathy
Lihong Si, Xiang Li, Zheyuan Li, Bo Shen, Kangzhi Li, Xia Ling, Xu Yang
Department of Neurology, Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine, Beijing 100049, People’s Republic of China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract
Background: Chronic unilateral vestibulopathy (CUVP) is often accompanied by dizziness and / or postural instability, resulting in the limitation of daily activities.. Recent studies have shown that the lack of central compensation strategy rather than the impairment of peripheral vestibular function is the main cause of chronic clinical symptoms and incomplete recovery.
Methods: This study recruited 18 patients with right CUVP and 18 age-, sex-, and education level-matched healthy controls (HCs). Vestibular evaluations such as videonystagmography (VNG), caloric test were performed. Dizziness Handicap Inventory (DHI) score for all patients were determined. All subjects underwent multimodal magnetic resonance imaging (MRI) of brain, including functional magnetic resonance imaging (fMRI) and three-dimensional T1-weighted MRI. We analyzed the amplitude of low frequency fluctuations (ALFF), regional homogeneity (ReHo), seed based functional connectivity (sFC) and voxel-based morphometry (VBM).
Results: Compared with HCs, patients with CUVP showed significantly increased ALFF values in the right supplementary motor area, significantly decreased ALFF values in the right middle occipital gyrus, significantly decreased ReHo values in the bilateral superior parietal lobule, as well as significantly enhanced ReHo values in the bilateral cerebellar hemisphere. Compared with HCs, patients with CUVP showed increased gray matter volumes in the left medial superior frontal gyrus and left middle cingulate gyrus. Compared with HCs, the FC were enhanced between left medial superior frontal gyrus and left orbital inferior frontal gyrus, left angular gyrus , and were significantly decreased between left medial superior frontal gyrus and right dorsolateral superior frontal gyrus in patients with CUVP. Pearson correlation analysis showed that there was a positive correlation between DHI score and VBM value of left medial superior frontal gyrus in patients with CUVP.
Conclusion: There are abnormalities of neuronal activity intensity and overall activity synchronization in multiple brain regions in patients with CUVP, suggesting that patients with CUVP have extensive brain functional abnormalities, which in turn affects spatial perception and motor perception. The increased gray matter volume and FC of the default mode network may be utilized as potential imaging biomarkers of chronic symptoms in patients with CUVP.
Figure 1
ALFF values in the right middle occipital gyrus was signifi cantly lower in patients with CUVP than in HCs.
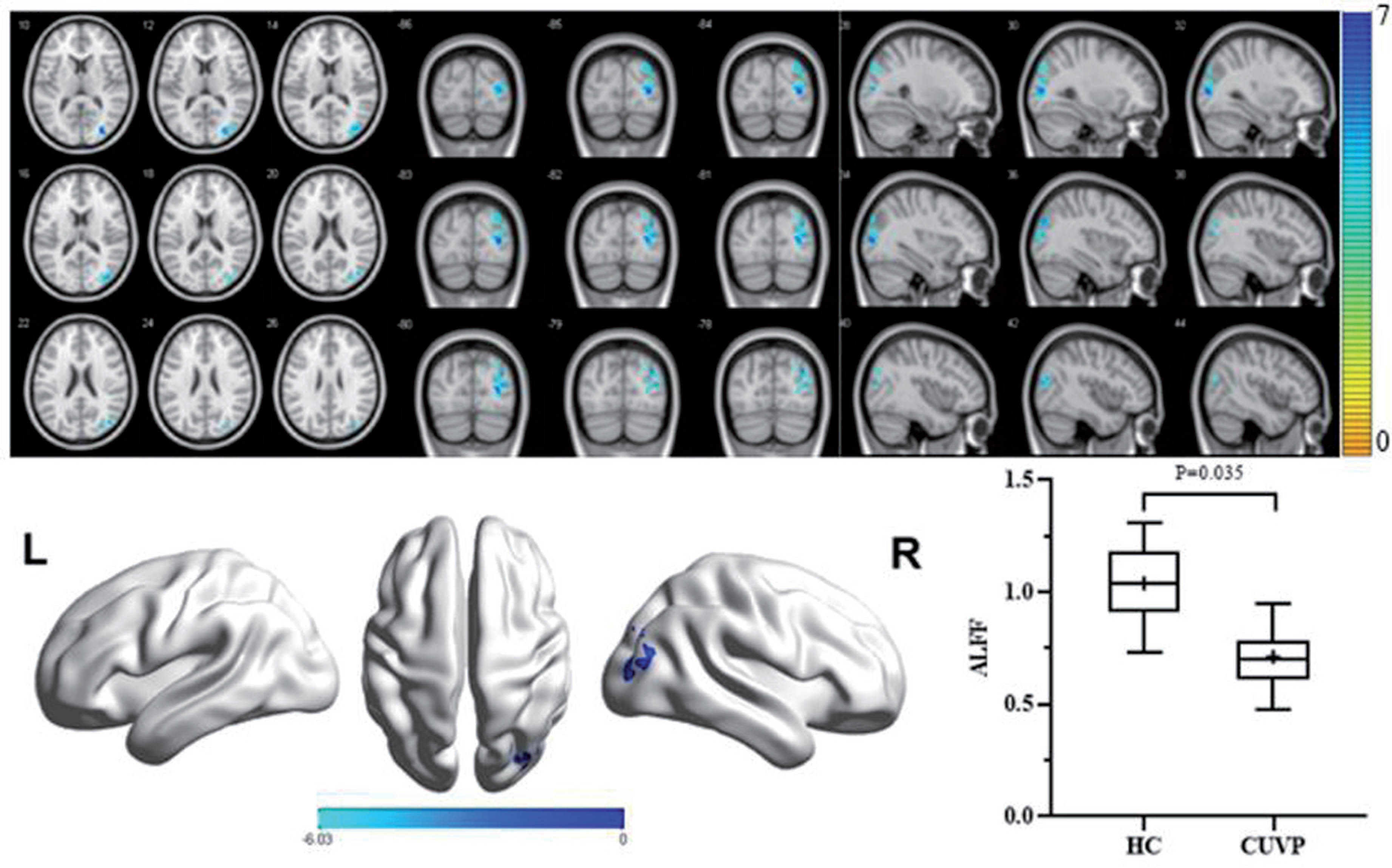
Figure 2
ALFF values in the right supplementary motor area was signifi cantly higher in patients with CUVP than in HCs.
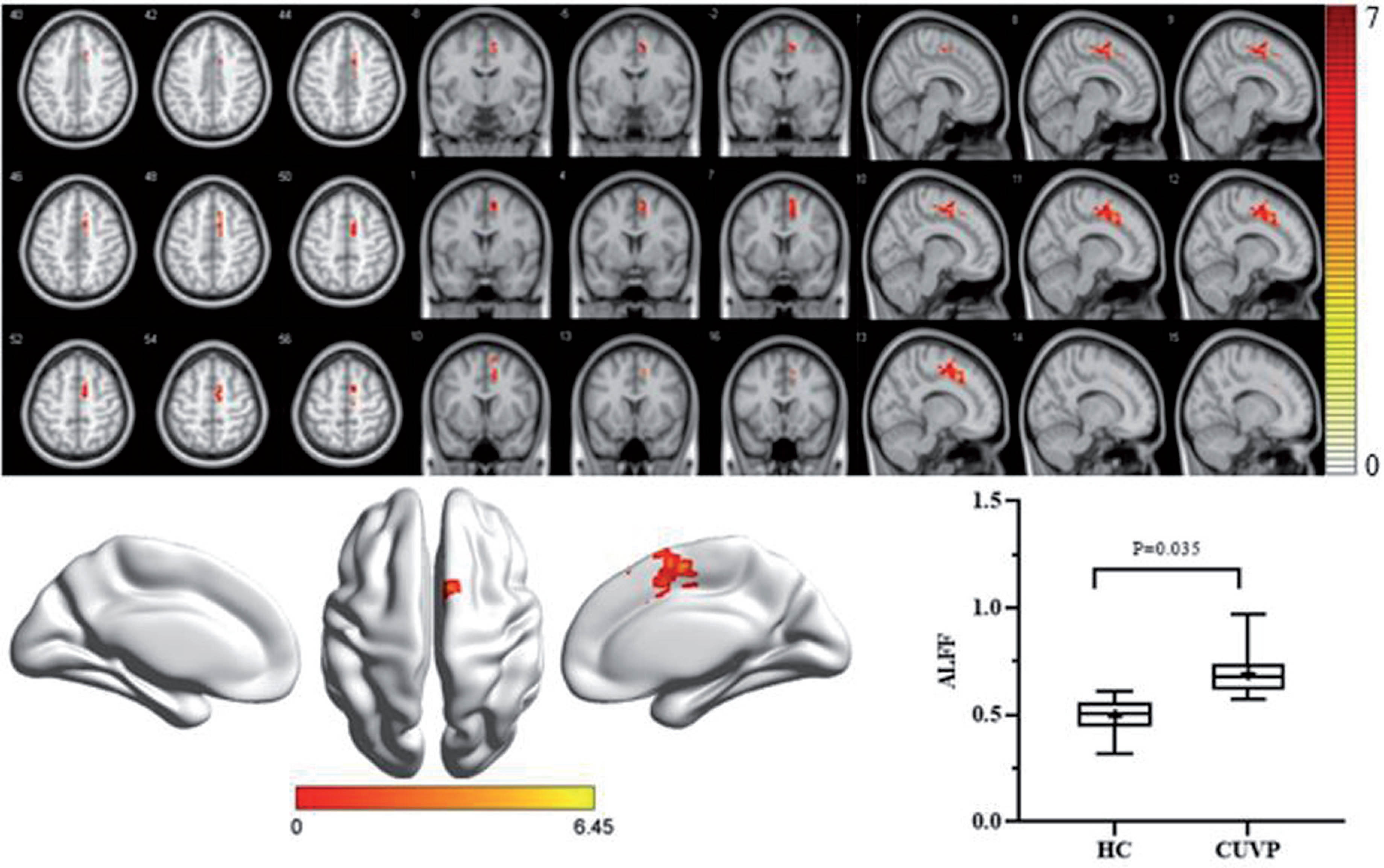
Figure 3
The ReHo values in the left superior parietal lobule and right superior parietal lobule were significantly lower in patients with CUVP than in HCs.
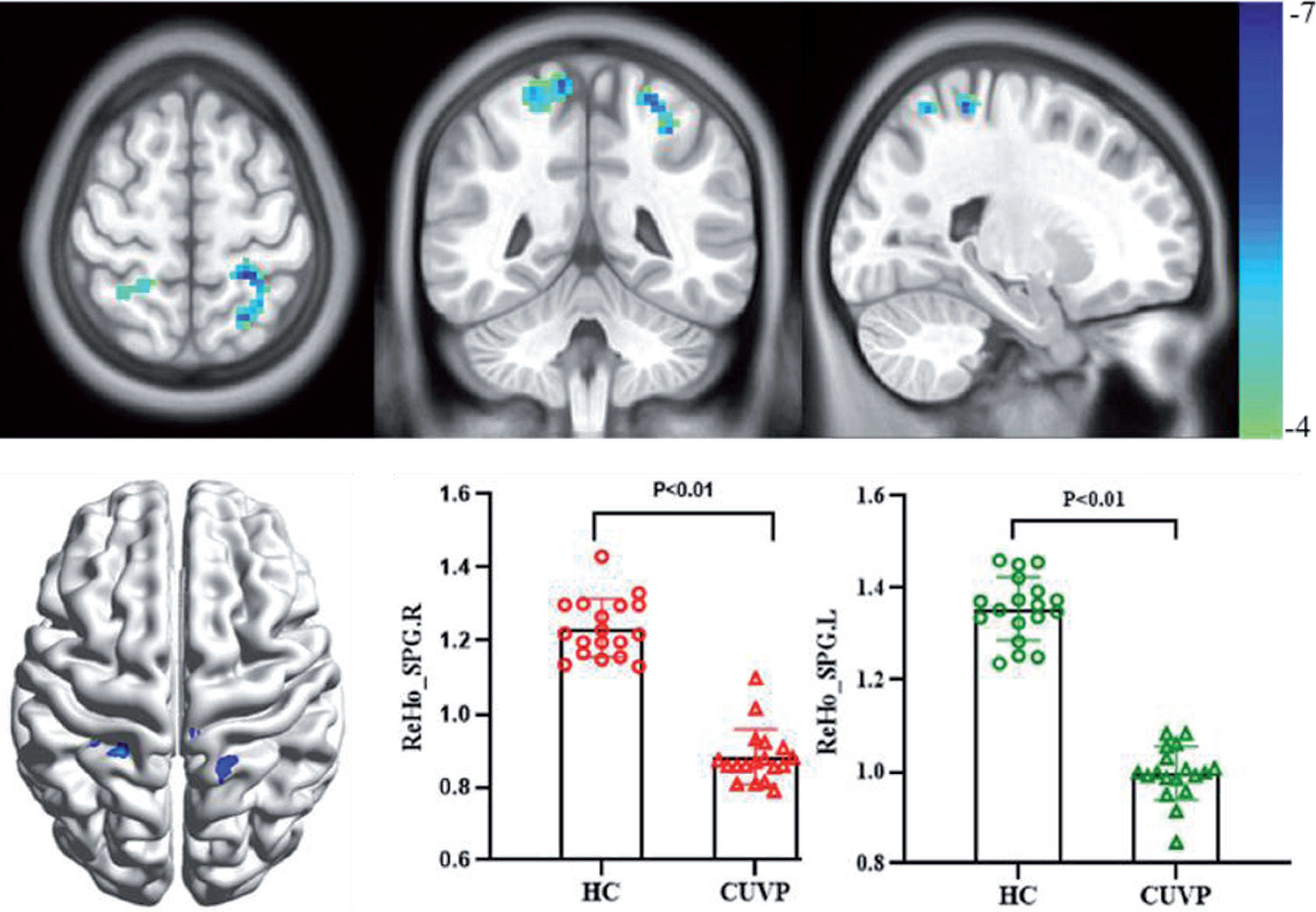
Figure 4
The ReHo values in the lower part of the left cerebellar hemisphere and the lower part of the right cerebellar hemisphere were signifi cantly higher in patients with CUVP than in HCs.
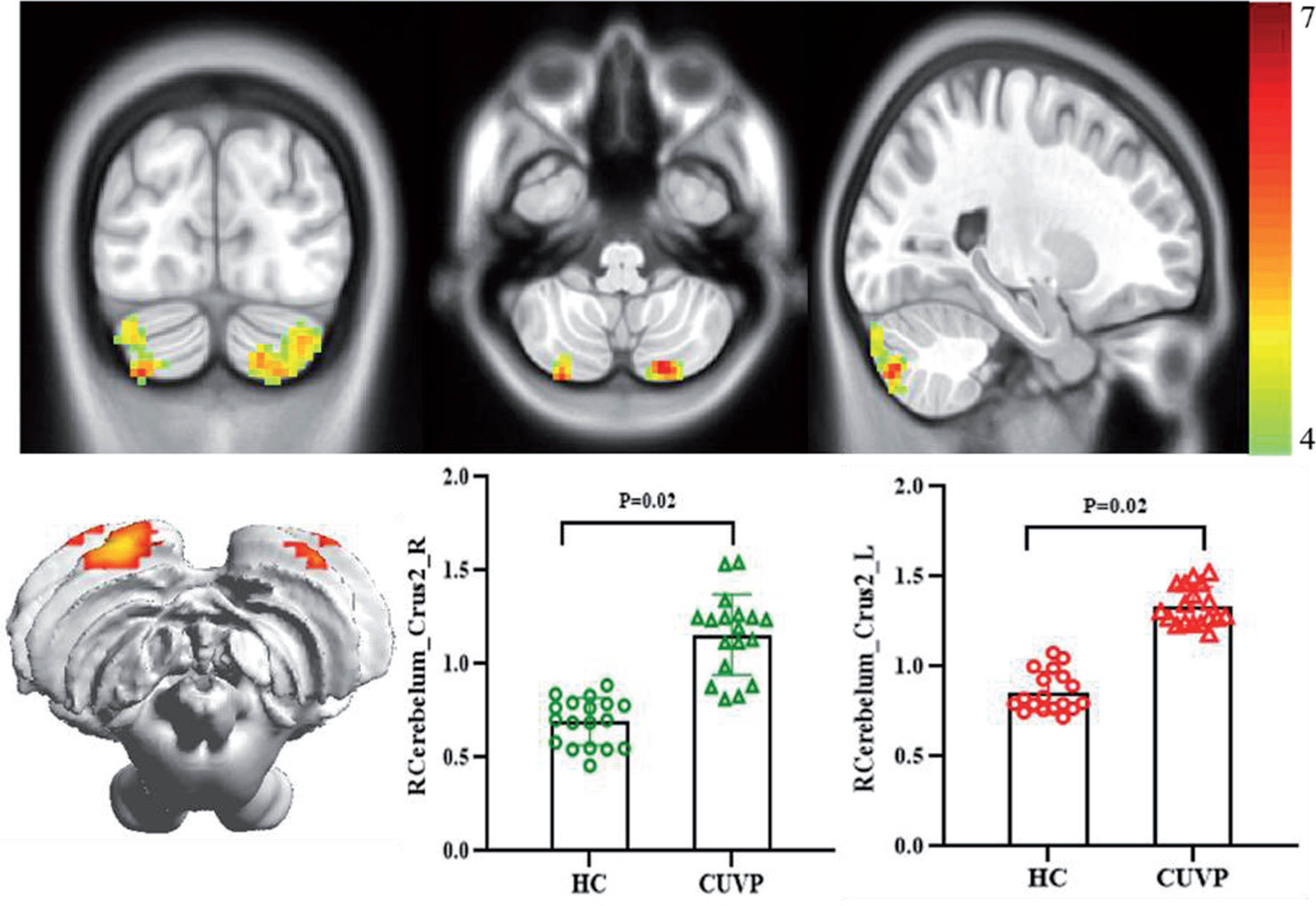
Figure 5
The gray matter volume in the left medial superior frontal gyrus and left middle cingulate gyrus was signifi cantly higher in patients with CUVP thant in HCs.
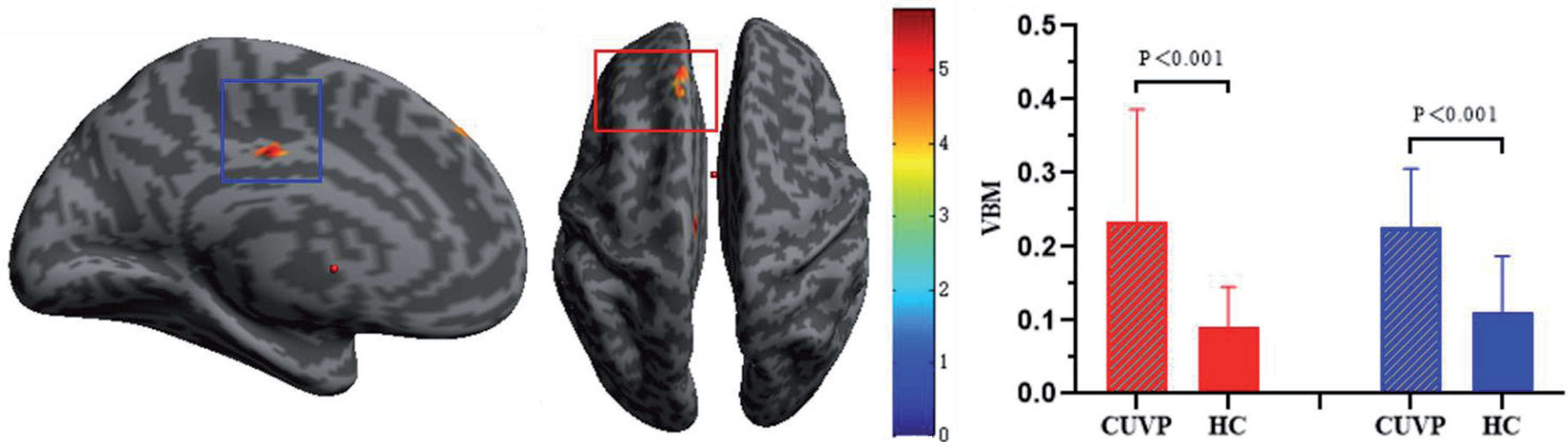
Figure 6
Patients with CUVP demonstrated enhanced FC between the left middle frontal gyrus and left orbital inferior frontal gyrus and left angular gyrus, weakened FC between the right dorsolateral superior frontal gyrus. Compared with healthy controls, the FC between left cingulate gyrus and the left cingulate gyrus was enhanced in patients with CUVP, which overlaps with the gray matter volume enhancement area.
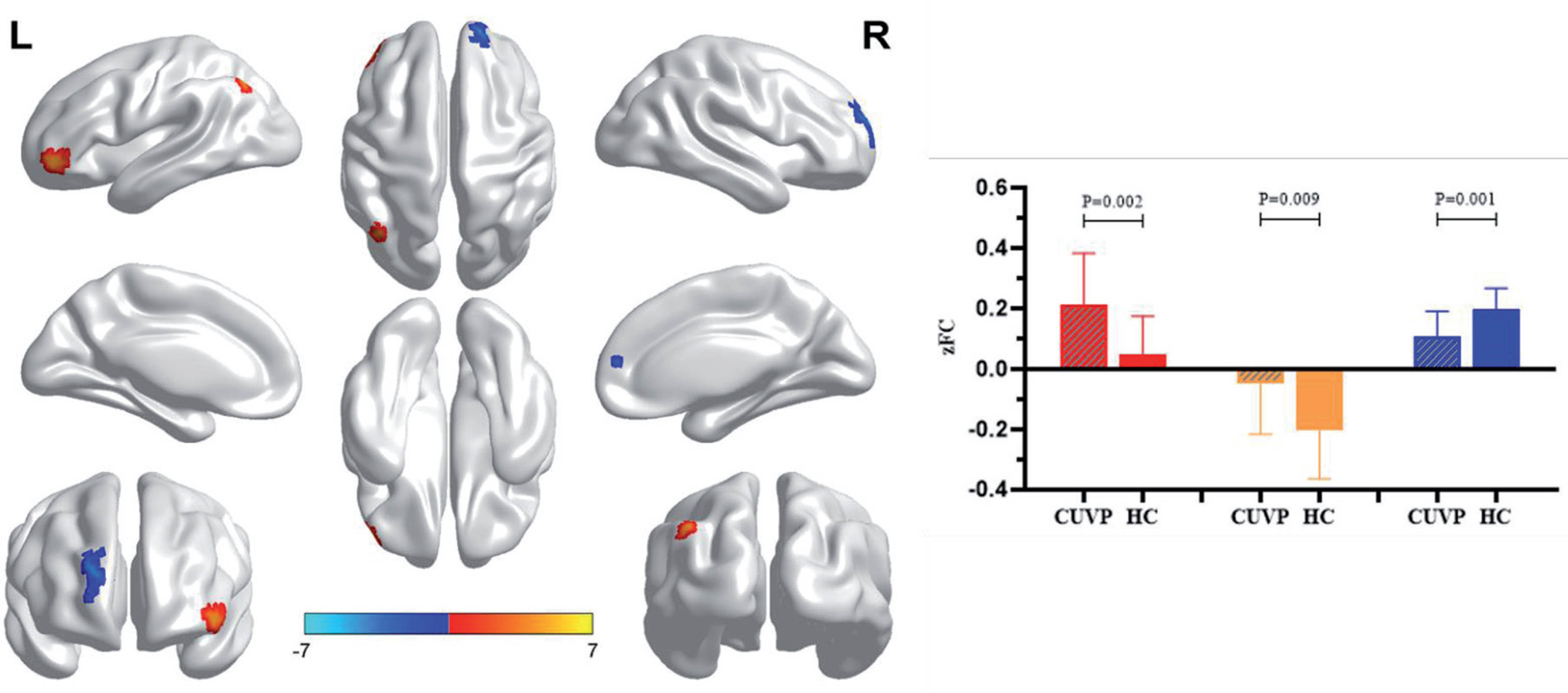
2.- FP1361Research on Application Value of Post-contrast 3D-FLAIR in Unilateral Peripheral Vestibular Dysfunction
Menglu Zhang, Xu Yang
Department of Neurology, Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine, Beijing 100049, People’s Republic of China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract
Background:It is difficult to clarify the lesion site and mechanism of unilateral peripheral vestibular dysfunction (UPVD). But with the development of three-dimensional fluid attenuation inversion recovery magnetic resonance imaging(3D-FLAIR MRI), it is possible to speculate the location and mechanism of UPVD patients.
Objective: To explore the relationship between the classification of post-contrast 3D-FLAIR and the cochleovestibular function tests in UPVD patients and its possible pathogenesis.
Methods: Forty patients (age=52.70±14.30) with UPVD underwent post-contrast 3D-FLAIR ,detailed history collection, pure tone audiometry(PTA), caloric test, and video head impulse test(vHIT).Patients with vestibular endolymphatic hydrops (EH), cochlear EH and perilymph enhancement(PE)were referred to MRI+ group(n=18,45.0%),other patients were divided into MRI- group(n=22,55.0%). The degree of vestibular EH, and cochlear EH was evaluated according to the Bernairt’s modified classification and Barráth’s classification.
Results: (1)22.5%(9/40)patients with vestibular EH,25.0%(10/40)with cochlear EH and 15.0%(6/40)with PE. PTA of MRI+ group was higher than MRI- group(64.36 ±25.75dB vs 23.45 ±16.29dB, p<0.001) .The PTA of patients with PE was higher than vestibular EH and cochlear EH(89.75±7.18dB vs. 57.00±22.78dB vs.56.5 ±21.05dB, p=0.027); In vestibular EH, the PTA of grade 2 was higher than grade 0 and grade 1.(66.20±8.79 dB vs. 23.45±16.29dB vs. 45.50±31.03dB, p<0.001). In cochlear EH, the PTA of grade 2 was higher than grade 0(68.50±13.40dB vs. 28.23±24.13dB, p=0.003), and there was a positive correlation between the degree of vestibular EH(r=0.66 p<0.001), cochlear EH (r=0.535 p=0.002) and hearing loss. (2) In MRI+ group, the vHIT gain of PE was lower than vestibular EH and cochlear EH(0.57±0.27 vs. 1.06±0.18 vs.1.10 ±0.24, p=0.001). (3)ROC curve analysis: In MRI +group, PTA and vHIT gain had higher diagnostic efficiencies for predicating whether there is PE or not (PTA:AUC=0.983, p=0.002, cut off=73.0;vHIT gain:AUC=0.992 p=0.002 cut off=0.64); (4) Possible pathogenesis: (a)Vascular risk factors: 32.5% (13/40) of MRI+ group and 20.0% (8/40) of MRI- group (20.0%).15.0% (6/40) of PE,15.0% (6/40) of vestibular EH and 20% (8/40) of cochlear EH. (b)Immune injury:0 (0/40) of PE,15.0% (6/40) of vestibular EH (p=0.014) and 15%(6/40) of cochlear EH(p=0.014).
Conclusion: PE is associated with hearing and vestibular function impairment. It’s more likely to occur when the PTA is greater than 73.0dB and vHIT gain is less than 0.64; There was a positive correlation between the EH and cochleovestibular function impairment, and EH may be related to autoimmune diseases.
Key words: unilateral peripheral vestibular dysfunction, endolymphatic hydrops, perilymphatic enhancement.
3.- FP1049Role Of MRI Visualizing Endolymphatic Space in Diagnosing Meniere’s Disease
Seung Cheol Han1, Young Seok Kim2, Yehree Kim1, Sang-Yeon Lee2, Jae-Jin Song1, Byung Yoon Choi1, Ji Soo Kim3, Yun Jung Bae4, Ja-Won Koo1
1Department Of Otorhinolaryngology-Head And Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea; 2Department Of Otorhinolaryngology-Head And Neck Surgery, Seoul National University Hospital, Seoul, Korea; 3Department Of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea; 4Department Of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Diagnosis of Meniere’s disease (MD) has been made based on the clinical history and audiometry. According to 1995 American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) guideline, for diagnosis of certain MD, histopathologic confirmation of endolymphatic hydrops (EH) is necessary. Symptoms such as dizziness and earfullness are important for diagnosis of MD, but these are nonspecific and frequently accompanied in many other otologic disorders. Therefore, recently developed magnetic resonance image (MRI) protocol documenting EH can be useful tool to understand the status of inner ear in MD patients. We took MRI using HYDROPS (HYbriD of Reversed image Of Positive endolymph signal and native image of positive perilymph Signal) protocol in MD patients and analyzed the role of MRI in visualizing the endolymphatic space for the diagnosis of MD.
Total 123 MD patients were recruited for study. Patients were categorized in 80 definite MD, 11 probable MD, and 32 possible MD patients based on 1995 AAO-HNS guideline. The grade of EH on HYDROPS MRI (hydrops grade) was independently measured by two otologists and confirmed by radiology department. Hydrops grade was correlated with several clinical parameters including diagnostic classification of MD (1995 AAO-HNS guideline), mean pure tone audiometry threshold, low frequency threshold, caloric test result, and duration of disease.
MD classification was significantly different both in cochlear and vestibular hydrops grade. In MD patients, mean pure tone audiometry threshold significantly increased by cochlear hydrops grade and was significantly different by whether hydrops exist or not in vestibule from HYDROPS MRI. Also, mean low frequency threshold was significantly different by whether hydrops exist or not, both in cochlea and vestibule from HYRDOPS MRI in MD patients. Canal paresis value was significantly different by whether hydrops exist or not in cochlea, and vestibular hydrops grade 2 was significantly different from others in MD patients. Disease duration and hydrops grade were not related.
Severity of EH described by hydrops grade from HYDROPS MRI showed significant correlation with MD classification, mean pure tone audiometry threshold, mean low frequency threshold, and canal paresis value, but not with disease duration. Radiological evaluation of MD using HYDROPS protocol seems to be a valuable tool to evaluate the extent and severity of EH in diagnosing the MD based on its pathophysiologic mechanism.
4.- FP0907Comparison between high-resolution 3D-IR with REAL Reconstruction and 3D-FLAIR sequences in the assessment of Endolymphatic Hydrops in 3 Tesla
Víctor Manuel Suárez-Vega, Pablo Domínguez, Meylin Caballeros-Lam, José Ignacio Leal, Nicolas Perez-Fernandez
Clínica Universidad de Navarra
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Research background: The purpose of this study is to describe the two main sequences used in the assessment of endolymphatic hydrops (EH) -the 3D-IR with real reconstruction and the 3D-FLAIR-, and to compare both sequences in terms of EH detection and grading.
Methods: 42 consecutive patients diagnosed with Probable or Definite MD were referred from the ENT Department for a 3 Tesla MR examination. Sequences acquired were a heavily T2 weighed axial 3D SPACE, axial 3D-FLAIR and axial 3D-IR 4 hours after a single dose of intravenous Gadolinium.
Vestibular and cochlear EH in both 3D-IR and 3D-FLAIR sequences were read by two independent head and neck radiologists, unaware of the patient’s clinical status.
The primary study endpoint was the concordance in the hydrops detection and severity with both imaging sequences. This was assed using the Cohen’s kappa K statistic for disease grading and Pearson X2 test to test the difference in detection rates of hydrops. Statistical significance was defined as two-sided P<0.05.
Results: We obtained an excellent overall concordance within both techniques, with a kappa of 0.821, (p<0.001) when comparing hydrops detection.
The degree of concordance is higher in vestibular hydrops than in cochlear hydrops, irrespective of affected side.
Regarding overall cochlear hydrops detection, the 3D-IR detected more hydrops than the 3D FLAIR, (62% vs 39.5%, p<0.03).
Conclusions: The 3D-IR sequence seems to be superior to the 3D-FLAIR for the assessment of EH and should be taken into account as a standalone parameter for a shorter and optimized EH MRI protocol.
Target audience Othologists with interest in Meniere’s disease and Head and Neck Radiologists
Moderate EH, c and d. Mild dilatation of the cochlear duct (arrows), with a scala vestibuli still patent. Vestibular EH grade II is depicted when the surface of the saccule, utricle or both is >50% of the bony vestibule /arrowheads). Some perilymphatic enhancing space can still be visible.
Severe EH, e and f. The cochlear duct is greatly dilated and pushes away completely scala vestibuli (arrows). Vestibular EH grade III is shown with the surface of the saccule and utricle completely occupying the vestibule and no high signal perilymphatic space can be seen (arrowheads).
Fig. 1:
a,c,e, 3D-IR sequences. b,d,f, 3D-FLAIR sequences. No EH in a and b. The saccule and the utricle are depicted separately in the vestibule (arrowheads) and no signifi cative engorgement of the cochlear duct is detected.
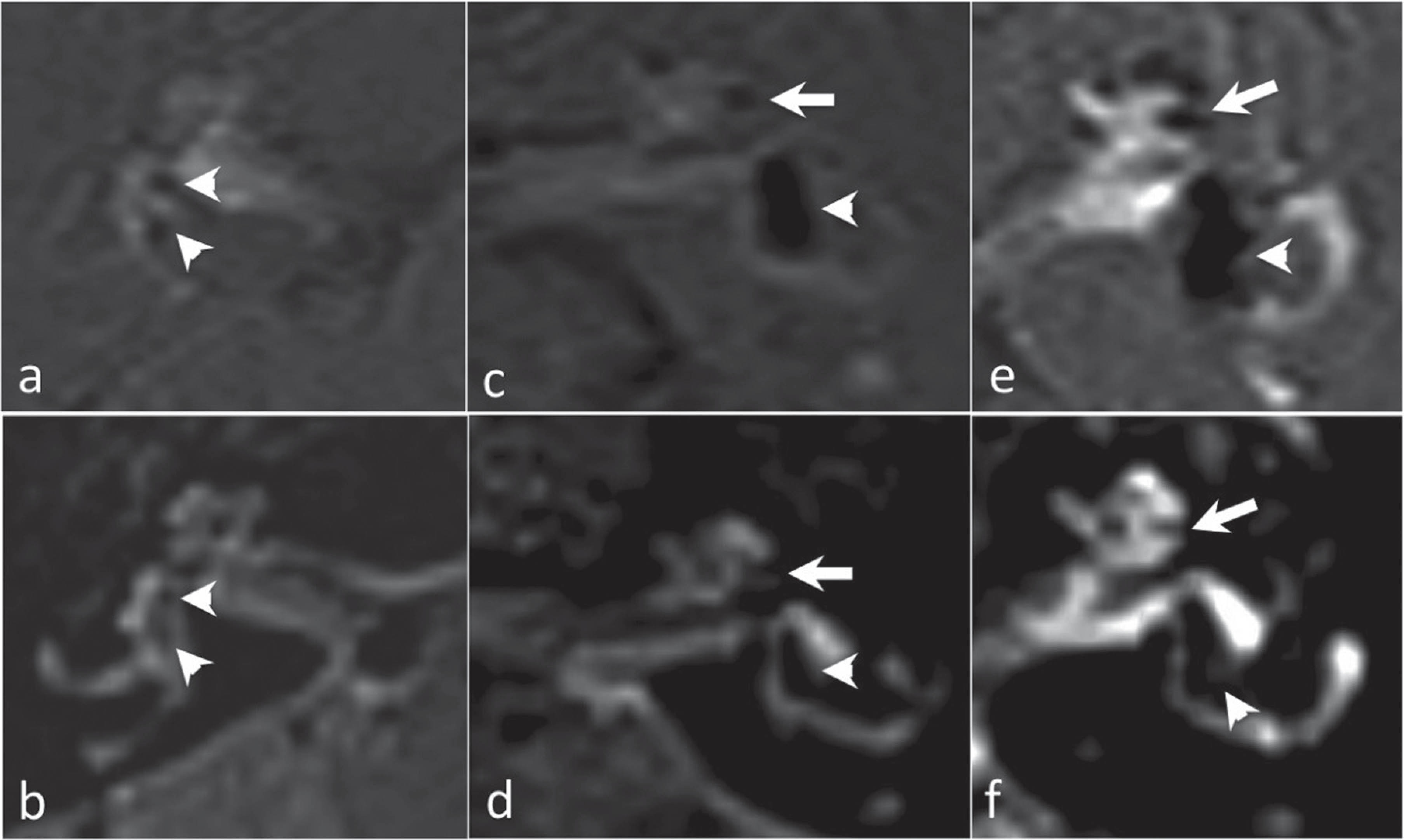
Fig. 2:
3D-IR sequence (a) and 3D-FALIR (b). Mild cochlear EH is clearly depicted on the 3D-IR (arrowhead) in a, as a dark smooth line corresponding to the mildly dilated cochlear duct. The contrast between the perilymph (high signal) and the surrounding bone (grey, intermediate signal) makes this diagnosis possible. On the contrary, when we analyze the 3D-FLAIR image in b, the surrounding bone -which is also low signal-, makes it almost impossible to distinguish the mild cochlear EH.
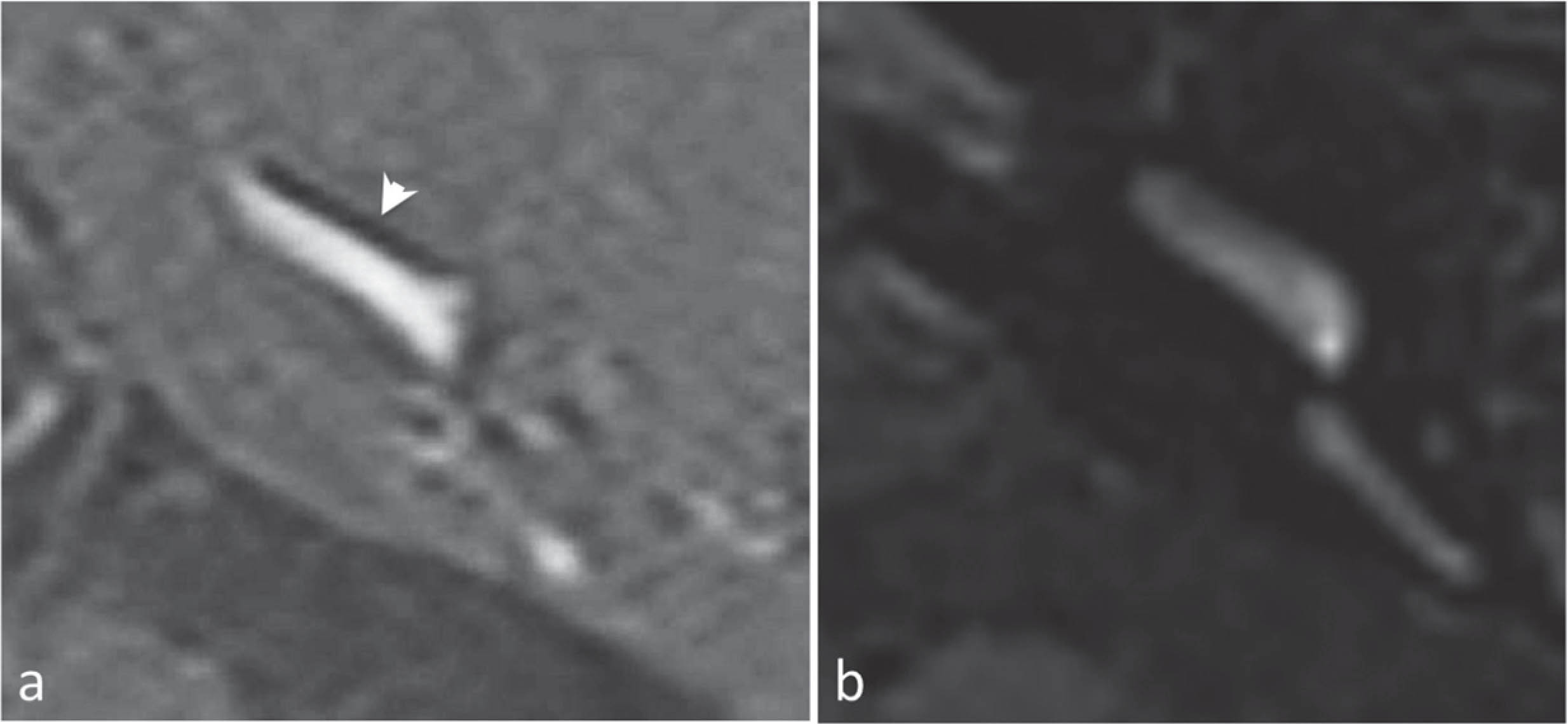
Fig. 3:
3D-IR sequence (a) and 3D-FLAIR sequence (b). Note severe cochlear (arrow) and vestibular (arrowhead) EH that is clearly visible on 3D-IR. In the 3D-FLAIR sequence, a severe vestibular EH can be assessed. However, for the cochlear EH there is a signifi cant discrepancy in the grading, with a very diffi cult to asses low signal dilated cochlear duct.
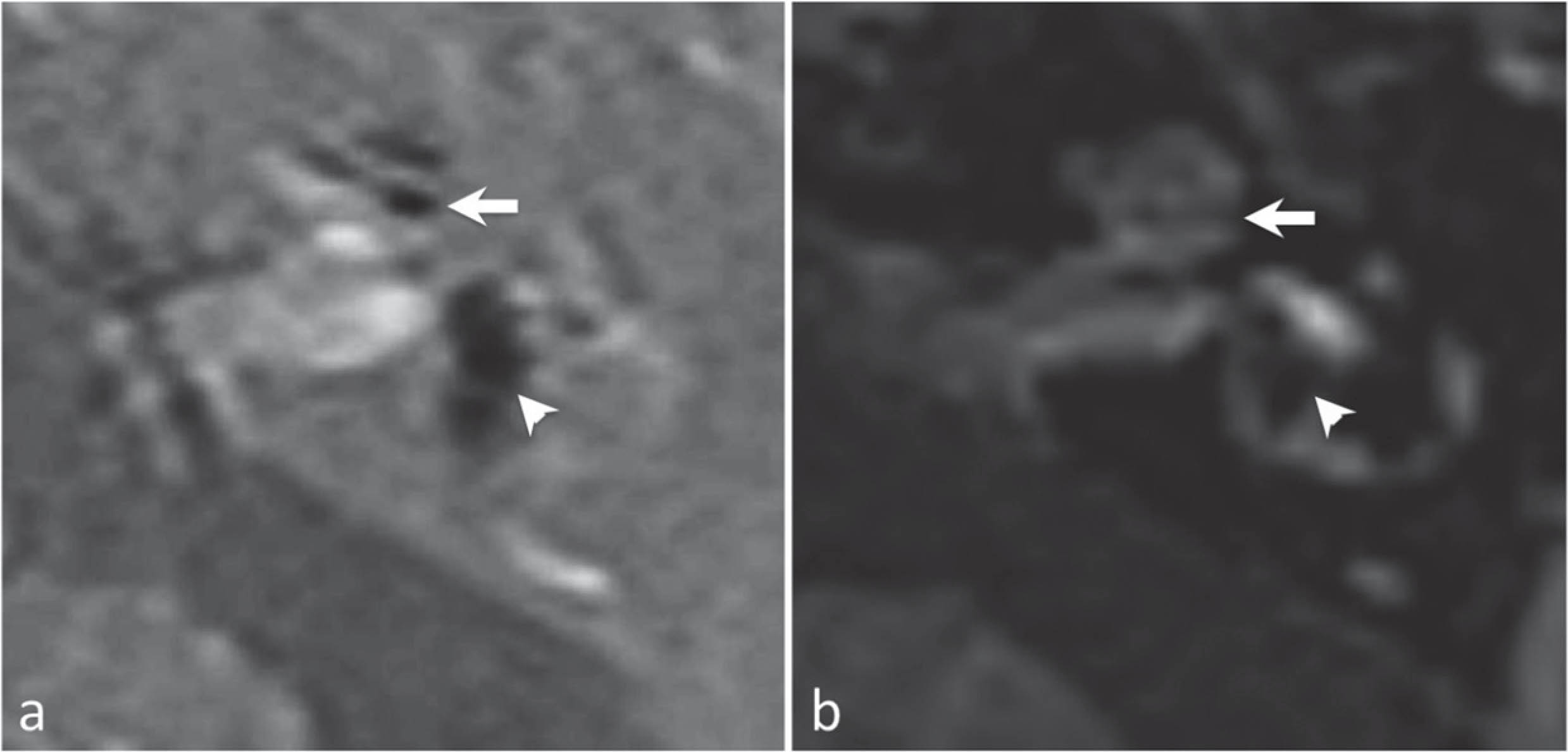
5.- FP1119Meniere’s disease: different mechanisms for hydrops and implication of treatments – an update.
Måns Magnusson1, Anki Pålbrink2, René in t’Zandt3, Mikael Karlberg1, Fredrik Tjernström1 Eva Degerman2
1Dept of clinical Sience, Section of Otorhinolaryngology; 2Dept of Experimental Medical Science; 3Lund University Biomedical Imaging Center. Lund University, Skane University Hospital, Lund, Sweden.
The course and symptoms in Meniere’s disease is highly variable. While some patients have a high frequency of attacks and continuous symptoms, other have sporadic attacks and others again go into remissions that last for years. The responses to different treatments are similar. While one patient may respond to a certain treatment, this may not help another. This holds true for most non-destructive approaches. Actually, the literature report most treatments seems to have a success rate of about 2/3rd. which, resembles the number going into spontaneous remission when observed for several months. We can thus suggest the “two-third problem” in Meniere’s disease. The heterogenicity of treatment responses, the number of different treatments suggested and the variety in the spontaneous course and in symptoms, may lead to a suspicion that there is either more than one etiology causing similar symptoms and/or that this is actually more than one disorder.
Meniere’s disease is suggested to be related to endolymphatic hydrops, and it is now possible to visualize the endolymphatic compartment with MRI after either an i.v. or intratympanical administration of gadolinium.
As we have encountered, developing an experimental model creating a hydrops in mice, visualizing it with a 9,4T animal MRI system with specially developed sequences, there seem to be different mechanisms to develop hydrops. Even on a cellular level. This has implication on the treatment regime.
Here, we will present an overview on treatments relative etiology of Meniere’s disease or hydropic inner ear disease, as based on present knowledge and experience. We will suggest that the new data seems ro suggests an open minded approach to the patients and and a multii modal therapeutic approach.
We have developed an experimental model for creating a hydrops in mice, visualizing it with a 9,4T animal MRI system with specially developed sequences. The endolymphatic hydrops is induced by either administration of vasopressin over 3 weeks, or by different phosphodiesteras inhibitors (PDE3 PDE4, PDE5). The Vasopressin and PDE4 inhibitors affects intracellular cAMP while PDE3 also effects cGMP and PDE5 only affects PDE5. In a series of experiments we could demonstrate that we could block the development of hydrops with spironlactone if hydrops was induced by vasopressin or PDE4 inhibitors, but not if hydrops was induced by PDE3 inhibitors. Thus, if hydrops is induced by one pathway it may be open to treatments, but not if it is induced by another mechanism. This falls well in line with the observation of different responses to similar treatment in different patients and, may be seen as a first evidence that Meniere’s disease or at least endolymphatic hydrops may have multiple etiologies. This suggest that we will have to continue work to separate these different entities, maybe by genetic testing as has been suggested, but also that we still have to work with personalized treatment regimes and try different treatments to find out what works for a certain patient. The findings also points out the great difficulties in doing randomized trials when the included patients might have different etiologies and mechanisms for their disease.
6.- FP1305Cortical representation of acute dizziness in strokes is not limited to a specific area.
Oi Yean Wong1, Yuk Man Chan1, Noorulain Khalid2, Stephen Wastling1, Indran Davagnanam1, Diego Kaski1
1University College London, Queen Square, Institute of Neurology, London WC1N 3BG, UK; 2Department of Life Sciences, Queen Mary University of London, Mile End Rd, London E1 4NS
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The anatomy of the vestibular system involving the inner ear and labyrinth, and centrally, the involvement of the vestibular nuclei in the brainstem and cerebellum, have been consistently described and demonstrated in the literature. The cortical areas that make up the ‘vestibular cortex’ are however less clearly defined. A number of cortical areas subserving vestibular functions have been described, including the precuneus, intraparietal sulcus, orbitofrontal cortex, cingulate gyrus, insula, retroinsular cortex, superior temporal gyrus, hippocampus, and parietal operculum. Here we sought to assess the cortical areas involved in patients presenting with acute dizziness and diagnosed with strokes on MRI, to determine whether there is a correlation between vestibular symptoms and lesion site.
We collected symptom-questionnaires from patients presenting with hyperacute strokes at the Univesity College Hospital. A total of 71 patients with confirmed strokes on MRI and acute dizziness have been identified. The acute stroke lesions are defined as hyperintense areas on the b1000 sequence, these are correlated to the ADC sequence by a senior radiologist. The regions of infarcts on the b1000 are segmented using ITK-Snap, followed by coregistration of the segmented regions to MNI space using FMRIB’s Linear Image Registration Tool. The cortical areas are recorded using Talairach coordinates (Brodmann areas) and Harvard-Oxford Cortical Structural Atlas (gyri).
23 patients were excluded due to unsatisfactory coregistration with the MNI atlas. A total of 28 Brodmann areas have been identified in the 48 patints analysed, with the largest number seen in Brodmann area 19, 40, 6, 4, 3. We did not observe a statistically significance between cortical areas affected in patients with vestibular symptoms compared to the rest of the areas identified. Using the Harvard-Oxford Atlas, a total of 32 cortical regions were involved, with the precentral and postcentral gyri being most common, but without statistical significance.
From our preliminary findings, we report that there is no correlation between acute dizziness symptoms in acute stroke and lesion location. This is an important finding as it shows that the cortical network in the generation of vestibular symptoms is most likely complex and widespread. The anatomical sites of acute cortical infarcts are not reliable markers to indicate the presence of vestibular symptoms, and vice versa. Our data also provides insight into functional vestibular anatomy which may have implication for surgery and rehabilitation.
SATELLITE - 10-TUESDAY
8:30:00 AM Bárány Award Ceremony
SY0031SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Jose Antonio Lopez-Escamez |
| TOPIC DESCRIPTIVE TITLE: | A multiallelic model of inheritance for Meniere disease |
| ACADEMIC / HOSPITAL AFFILIATION: | Instituto de Investigación Biosanitaria de Granada, Spain |
- SPEAKER 2
| NAME AND SURNAME: | Andreas H. Eckhard |
| TOPIC DESCRIPTIVE TITLE: | Emerging endotype-phenotype patterns based on inner ear pathologies in Meniere’s Disease |
| ACADEMIC / HOSPITAL AFFILIATION: | University Hospital Zurich, Switzerland |
- SPEAKER 3
| NAME AND SURNAME: | Anna Lysakowski |
| TOPIC DESCRIPTIVE TITLE: | Mouse models of familial Meniere’s Disease |
| ACADEMIC / HOSPITAL AFFILIATION: | University of Illinois at Chicago, USA |
- SPEAKER 4
| NAME AND SURNAME: | Maria Teresa Requena Navarro |
| TOPIC DESCRIPTIVE TITLE: | Drosophila and zebrafish models for understanding the basis of Meniere’s Disease |
| ACADEMIC / HOSPITAL AFFILIATION: | University of Edinburgh, UK |
Meniere’s Disease (MD) has a long and prominent history in the world of neuroscience as a loss of balance and hearing. An interesting challenge for MD research today is a lack of knowledge of the mechanisms involved, especially genetic backgrounds, the inner ear cells that are affected, and the molecular pathways involved.
MD can be characterized as follows: recurrent episodes of vertigo, fluctuating and progressive sensorineural hearing loss (SNHL) and tinnitus. MD is a heterogeneous clinical syndrome. The prevalence of MD is about 0.5-1/1000. The usual age of onset ranges from 30-50 years. Both ears are affected, leading to severe hearing impairment and chronic imbalance, resulting in a huge burden for patients and a significant impact on health-related quality of life. Because of a lack of knowledge of the molecular mechanisms involved, it is difficult to generate treatments for these patients. We are interested in developing new approaches to understand how the inner ear cells might be degraded to generate the disease phenotype at a relatively young age in these adult patients.
To be effective, we propose research that integrates four different approaches: 1) genetic studies in familial Meniere’s patients; 2) neuroimaging and histopathology of the human temporal bone focusing on the endolymphatic sac; 3) mice as an animal model to understand the molecular basis behind the human disease; and 4) the use of flies and fish as animal models to filter potential candidate genes.
The purpose of this symposium is to explore a variety of cutting-edge approaches. We suggest that the target audience could be the leading researchers and clinicians who have worked with different paradigms (emphasizing approaches from the clinic to basic science) to explore a synergy that will exploit the best of each.
ABSTRACT 1
The genetic underpinnings of Meniere’s disease (MD) include some rare monogenic forms in isolated families and a polygenic contribution in most familial and sporadic cases. So, familial MD has been reported in 6-8% of sporadic cases and several genes have been described in single Familial MD including FAM136A, DTNA, PRKCB, SEMA3D and DPT, suggesting genetic heterogeneity. Multiplex rare missense variants in OTOG gene have been reported in 33% of familial MD, supporting a multiallelic inheritance. Moreover, the genetic landscape of sporadic MD is more complex and it involves multiplex rare variants in several SNHL genes such as GJB2, USH1G, SLC26A4, ESRRB, and CLDN14 and axonal-guidance signalling genes such as NTN4 and NOX3. Here, we proposed a multiallelic model to explain the hearing loss phenotype in MD. The interaction of common cis-regulatory variants located in non-coding regions and rare variants in coding regions in one or more target genes will determine the variation on the phenotype in MD, explaining the incomplete phenotype and variable expressivity in the condition.
ABSTRACT 2
Meniere’s disease (MD) is commonly associated with a pathological accumulation of endolymphatic fluid, termed “idiopathic” endolymphatic hydrops (iEH). Although numerous precipitating/exacerbating factors have been proposed for MD, its etiology remains elusive. Here, using immunohistochemistry and in situ protein–protein interaction assays, we demonstrate regulated sodium and calcium transport mechanisms in the epithelium of the extraosseous portion of the endolymphatic sac (eES) in murine and human inner ears. Histological analysis in an extensive series of human temporal bones consistently revealed pathological changes in the eES in cases with iEH and a clinical history of MD, but no such changes were found in cases with “secondary” EH, due to other otological diseases, or in healthy controls. Notably, two etiologically different pathologies—degeneration and developmental hypoplasia—that selectively affect the eES in MD were distinguished. Clinical records from MD cases with degenerative and hypoplastic eES pathology revealed distinct intergroup differences in clinical disease presentation. Overall, we have identified two inner ear pathologies consistently present in MD that are directly linked to EH pathogenesis and which potentially affect the phenotypical presentation of MD.
ABSTRACT 3
We have been working with one mouse model, Fam136a knockout (KO), using biochemical, immunohistochemical and behavioural approaches, to understand how its inner ear might be degraded to generate the disease phenotype. Fam136a is a protein localized in mitochondria that is highly conserved across species (from plants to humans), and it is coded for by a gene on Chromosome 2. We have reported its presence in the rodent inner ear (Requena et al. 2014). Through whole exome sequencing, this gene was found in multiple generations of a human family with familial MD (fMD). In wild type (WT) and KO mice, we have found significantly reduced differences in both Rotarod performance over time and mitochondrial function, supporting the hypothesis of its role in the dysfunction occurring in fMD. A second mouse model, a DTNA KO (coding for the cytoskeletal protein alpha-dystrobrevin, also found in inner ear), is also being tested and analyzed.
ABSTRACT 4
Multiple genes and variants are arising as candidate targets for Meniere’s disease (MD). These genes must be screened using functional animal models able to reproduce both the hearing and vestibular phenotypes. Zebrafish inner ears contain the semicircular canals and utricular maculae, concerned with balance, acceleration and gravity-sensing, whereas saccular and lagenar maculae manage the hearing function. The fly’s ‘inner ear’, the Johnston’s organ, is a chordotonal organ localized in the 2nd-antennal segment, which mediates the sensations of hearing, gravity and wind. In both organisms, MD candidate gene orthologues are predicted to be found in cells of the auditory/proprioceptive chordotonal sensory organs. Given the large number of candidate genes, a mammal model can be expensive, experimentally laborious and time consuming. In contrast, development of a zebrafish or drosophila model to investigate the role of MD candidate genes in hearing and balance would significantly reduce both costs and time for preliminary screening.
OC07 1.- FP0872FREE PAPER FORM
Laboratory characterization of VestAid: a tablet-based technology for objective exercise monitoring in vestibular rehabilitation
Shamus Roeder 1, Pedram Hovaresht1, Lisa Holt1, Pan Gao1, Lemin Xiao1, Devendra Tolani1, Chad Zalkin1, Yonatan Vaknin1, Jody Underwood1, Carlos Esquivel2, Yadira Del Toro2, Susan Whitney3
Intelligent Automation, Inc.1, AFMO SGAR Hearing Center for Excellence, San Antonio, TX, USA,2 University of Pittsburgh, PA, USA3
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
We developed and characterized VestAid, an innovative, low-cost home-exercise system that helps patients follow therapists’ instructions and uses the tablet camera to automatically assess compliance in the performance of vestibulo-ocular reflex (VORx1) exercises. The system provides the physical therapist with near real-time objective (head speed, gaze compliance) and subjective (pre- and post- exercise symptoms, perceived difficulty) metrics of compliance through a web-based provider portal.
The system is implemented as a tablet-based app for the patient and a web-based portal for the physical therapist. The physical therapist inputs the parameters of the exercises (suggested dosage, direction and speed of head movement, optotype shape and type, contrast with background). Video instructions on the tablet help patients recall how to perform the VOR exercises and a metronome guides head speed during the exercises. The system collects symptom data before and after each exercise which is then combined with objective performance data to provide feedback to both the patient and the physical therapist.
Using the video stream of head movement, we developed fast and accurate face and facial landmark detection algorithm to compute the head pitch, roll, and yaw angles. A peak detection algorithm is used to determine head speed compliance to VOR x1 set parameters. A Convolutional Neural Network was trained for eye-gaze classification and compliance determination.
We characterized the accuracy of the head angle estimation by comparing its performance on a subset of the BIWI public dataset with Hopenet, a state of art deep-learning method that cannot be implemented on the tablet due to high computational load. Comparable performance to Hopenet was observed with less than10 degrees average geodesic error and less than6 degrees average absolute degrees in yaw plane. We characterized the accuracy of VestAid’s head-turn frequency measurements by performing the head turn exercise with the VestAid system with an Inertial Measurement Unit (IMU) affixed to the back of a head worn helmet. Data from 15 instances of 20 second head-yaw movements with frequencies 80, 120, and 160 bpm yielded a median of average head angle error less than 10 degrees. Publicly available data from 10 persons was utilized to train and evaluate the eye-gaze model, which yielded above 90% accuracy, precision, and recall.
Initial results suggest that the VestAid system can determine the head frequency and eye gaze classification within the required accuracy. Systematic data collection and human studies to further validate the technology are under way.
This work is supported by the US Army Medical Research and Materiel Command under Contract Number listed on W81XWH-18-C-0030. The views, opinions and/or findings contained in this report are those of the author(s) and should not be construed as an official Department of the Army position, policy or decision unless so designated by other documentation.
2.- FP0879Vestibular Rehabilitation with Mobile Posturography as a “Low-Cost” Alternative to Vestibular Rehabilitation with Computerized Dynamic Posturography, in Elderly People with Instability
Andrés Soto-Varela1,2, Marcos Rossi-Izquierdo3, María del-Río-Valeiras4, Ana Faraldo-García4, Isabel Vaamonde-Sánchez-Andrade4, Antonio Lirola-Delgado4 and Sofía Santos-Pérez1,2
1Division of Neurotology, Department of Otorhinolaryngology, Complexo Hospitalario Universitario, Santiago de Compostela, Spain; 2Department of Surgery and Medical-Surgical Specialities, University of Santiago de Compostela, Spain; 3Department of Otorhinolaryngology, University Hospital Lucus Augusti, Lugo, Spain. 4Department of Otorhinolaryngology, Complexo Hospitalario Universitario, Santiago de Compostela, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background. Accidental falls, especially for the elderly, are a major health issue. Balance disorders are one of their main causes. Vestibular rehabilitation (VR) has proven to be useful in improving the balance of elderly patients with instability. Specifically, VR with dynamic computerized posturography (CDP) has proven to be especially useful for elderly patients, because it not only improves the stabilisation of the centre of gravity (where sensorial stimuli are absent or altered), but also improves the limits of stability levels of the patient (and thus reduces the risk of falling). Its major handicap is probably its cost, which has hindered its generalisation. One possible solution to reduce this cost is performing VR with mobile posturography systems, which allows assessment of balance at center of body mass in daily-life conditions, where falls among elderly patients commonly occur. Also, rehabilitation with vibrotactile neurofeedback training could be used in dynamic tasks.
Methods. A clinical trial comparing VR with CDP exercises and VR with mobile posturography (Vertiguard) exercises, was designed. The participants were people over 65 years, with instability. The percentage of average balance in the sensory organization test (SOT) of the CDP (main outcome mesure), other CDP scores, time and steps in the “timed up and go” test, scores of Dizziness Handicap Inventory DHI), short Falls Efficacy Scale-International (short FES-I), and Vertiguard, were compared before and three weeks after VR, and between both intervention groups.
Results. 40 patients were included in the study (19 in the CDP-VR group and 21 in the Vertiguard-VR group). Both groups were comparable regarding age, sex, and balance pre-VR. Average balance was significantly improved in both intervention groups (51 pre-VR vs 60 post-VR, p=0.002, CDP-VR group; 49 pre-VR vs 57 post-VR, p=0.008, Vertiguard-VR group); no significative differences in this improvement were found comparing both groups (p=0.580). Condition 4, condition 5, and vestibular input scores improved in both groups too, without differences between them. Only the directional control, in limits of stability, showed significative differences (improvement in CDP-VR group and no improvement in Vertiguard-VR group, p=0.010). No substantial improvement was detected regarding timed up and go (time and steps), DHI, and short FES-I scores.
Conclusions. VR using mobile posturography is useful to improve balance in elderly people with instability, showing similar improvement rates to those of VR using computerized dynamic posturography. This would reduce the costs of posturographic vestibular rehabilitation and facilitate its dissemination around the world.
3.- FP1131Diagnosis and Rehabilitation of Vergence Eye Movement Abnormalities in Vertigo patients
Zoï Kapoula1, Aakash Ganesan1, Alain Bauwens2
1IRIS Laboratory, CNRSUAR 2022, University of Paris, France; 2Unity of Functional Rehabilitation of vertigo, Hospital Saint Therese, Bastogne & CHU UCL site de Dinant, Belgique
The vestibular function is in synergism with the oculomotor vergence. Vertigo may be related to vergence disorders and conversely, vestibular pathologies may affect vergence. To consolidate this hypothesis, we conducted a clinical study at the vestibular orthoptic clinic of the Bastogne Hospital.
Fourteen patients with vertigo, aged 30 to 62 years were studied; the origin of vertigo varied (Meniere’s disease, organic pathology, sensitivity to visual movement). An assessment with objective measurement of vergence was done with the REMOBI & AIDEAL (patent REMOBI WO2011073288, AIDEAL analysis software PCT/EP2021/06222), coupled with an eyetracker (pupil core). Then, four vergence neuro-rehabilitation sessions were performed using the double-step in depth paradigm also at the REMOBI device; within each session vergence blocs of rehabilitation was done alternating sitting and standing positions to involve the body. To evaluate the effects of rehabilitation, an assessment of vergence was done 1 to 2 months after the end of the four sessions. The initial assessment also included a posture test in quiet stance while fixating at near (40 cm), at far (150 cn) or while making active vergence movements between a far near; body sway was measured with the dynaport minimod Mc robedrts device.
The results showed smaller acceleration of Medio lateral body sway when the patients were making vergence eye movements than when fixating, particularly in patients with vertigo in the absence of organic deficit. This confirms the stabilizing effect of vergence eye movements on posture that is known in healthy also exists in patients with vertigo.
Assessment of eye movements revealed problems of magnitude and/or speed or increased variability of vergence for 11 of the patients. After the 4 sessions of neuro-rehabilitation, an improvement in one or more parameters was observed in 8 of the patients. At the group level, the latency of divergence decreased significantly, and its amplitude increased particularly for patients with functional vertigo and hyper sensibility to visual motion. Significant changes occurred mainly when testing vergence in the standing position. At the subjective level, patients reported increased confidence on their space perception and ambulation in their every day life.
The results confirm the hypothesis of a symbiosis between vergence posture and vestibular function. Clinically, diagnosis and rehabilitation of the vergence disorder, could be a means to improve space perception, space attention, and general motor control in vertigo patients. Further results from various clinics using the method will be reported.
4.- FP1174The INVEST Trial: A feasibility randomised controlled trial of integrated cognitive-behavioural therapy and vestibular rehabilitation for people with persistent dizziness
David Herdman1,2, Sam Norton2, Kate Frost2, Louisa Murdin3, Marousa Pavlou 1, Rona Moss-Morris1
1King’s College London, London, UK; 2St George’s University Hospitals NHS Foundation Trust, London, UK; 3Guy’s & St Thomas’ NHS Foundation Trust, London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Purpose: This study assessed the feasibility, acceptability, and potential benefits of integrating vestibular rehabilitation (VR) and cognitive behavioural therapy designed specifically for persistent dizziness (INVEST intervention).
Methods: This was a feasibility randomised controlled trial of the INVEST intervention vs a time matched physiotherapy control. Participants were recruited from a tertiary vestibular clinic in London, UK. Measures of feasibility and clinical outcome were collected and assessed at 4 months.
Results: Forty patients (80% female, mean age 44.5 years ± 17, range 19-79) with PPPD (persistent postural perceptual dizziness) were recruited and individually randomised, using a minimisation procedure, to six sessions of INVEST (n=20) or physiotherapy control (n=20). 59% of patients screened met the inclusion criteria, of which 80% enrolled. Acceptability of the intervention was high across all the Theoretical Framework of Acceptability (TFA) constructs and 85% adhered to all 6 sessions. There were small to moderate treatment effects between the groups in favour of INVEST across all outcomes and process variables, including dizziness handicap (standardised mean difference [SMD]g = 0.45). No intervention-related serious adverse events occurred.
Conclusions: This feasibility study demonstrated high rates of recruitment, retention, and acceptability in both arms. There was promising evidence in support of the need and benefits of integrated cognitive behavioural therapy-based vestibular rehabilitation compared to current best practice VR. The study fulfilled all the a priori criteria to advance to a full-scale efficacy trial.
Target Audience: This study would be of interest to anyone involved in vestibular rehabilitation and treatment for PPPD
5.- FP1386Vestibular Rehabilitation in Europe: A Survey of Clinical and Research Practice.
Dara Meldrum1, Lisa Burrows2, Ondrej Cakrt3, Hassen Kerkeni4, Christophe Lopez5, Frederik Tjernstrom6, Luc Vereeck7, Oz Zur8, Klaus Jahn9
1Academic Unit of Neurology, School of Medicine, Trinity College Dublin, Ireland; 2Community Rehabilitation Team, Southport, UK; 3Department of Rehabilitation and Sports Medicine, Second Faculty of Medicine, Charles University and Motol University Hospital, Czech Republic; 4Department of Neurology, University Hospital of Bern, University of Bern, Switzerland; 5Laboratoire de Neurosciences Sensorielles et Cognitives, Marseille University, France; 6Department of Otorhinolaryngology, Head and Neck Surgery, Lund University, Sweden; 7Faculty of Medicine, University of Antwerp, Belgium; 8Ben-Gurion University of the Negev, Beersheba, Israel; 9Department of Neurology Schoen Clinic Bad Aibling andGerman Center for Vertigo and Balance Disorders University of Munich, Germany.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Vestibular rehabilitation (VR) is practiced across Europe but little in this area has been quantified. The aim of this study was to investigate current VR assessment, treatment, educational and research practices.
This was an online, cross-sectional survey with 39 VR specific questions and 4 sections: demographics, current practice, education and research. The survey was disseminated through the DIZZYNET network to individual therapists, and through country-specific VR special interest groups. Results were analysed descriptively, and a thematic approach was taken to analyse open questions.
A total of 476 individuals (mean age 41±10yrs, 74.5% women), predominately physiotherapists (88.5%) from 20 European countries responded to the survey. They had worked for a median of 4 years (range 0-35) in VR. The majority (58.7%) worked in hospital settings and 22.4% in dedicated VR services. Most respondents specialized in neurology, care of the elderly and ENT. VR was reported as hard/very hard to access by 48%, with the main barriers to access identified as lack of knowledge of HCPs, particularly GPs, lack of trained therapists and lack of local services.
The commonest conditions treated were BPPV (87.5%), vestibular neuritis (66.2%), other unilateral vestibular hypofunction (75.6%) and cervicogenic dizziness (63%). The use of vestibular assessment equipment varied widely; over 70% used high density foam and objective gait speed testing and over 50% used DVA equipment. Infrared systems, Frenzel lenses and Dynamic Posturography/Stabilometry were not commonly employed (<20%). The most frequently used physical outcome measures were the mCTSIB, Functional Gait assessment/Dynamic Gait index and Romberg/Tandem Romberg. The DHI, visual analogue scale, Falls Efficacy Scale and the Vertigo Symptom Scale were the most commonly used patient outcome measures. Adaptation, balance and habituation exercises were most frequently used (>80%), with virtual reality used by 15.6%. Over 70% reported knowledge/use of Semont, Epley and BBQ Roll manoeuvres.
Most education regarding VR was obtained at post-registration level (89.5%) with only 19% reporting pre-registration education. There was strong (78%) agreement that therapists should have professionally accredited postgraduate certification in VR, with blended learning the most popular mode. Three major research questions were identified for priority: management of specific conditions, effectiveness of VR, and mechanisms/factors influencing vestibular compensation and VR.
The survey quantified current clinical practice in VR across Europe. Knowledge and treatment of common vestibular diseases was high, but use of published subjective and objective outcome measures varied widely, and use of vestibular assessment technology equipment such as infrared goggles/forceplates was low.
Target Audience-Health care professionals practising or referring to vestibular rehabilitaiton
6.- FP1440The Role of Vestibular Cues in Postural Sway
Faisal Karmalia, Adam D. Goodworthb, Yulia Valkoa,c, Robert J. Peterkad, Daniel M. Merfelda,e
aHarvard Medical School / Massachusetts Eye and Ear, Boston, USA; bWestmont College, Santa Barbara, CA, USA; cUniversity Hospital Zurich, University of Zurich, Switzerland; dVA Portland Health Care System, Portland, OR, USA; eOhio State University, Columbus, OH, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and aim. Sensory feedback plays a considerable role in posture sway and the detection of body motion and orientation. The vestibular organs are unique amongst the sensory systems as they provide cues related to head orientation and motion relative to gravity. Little is known about the role of tilt vs. translational vs. rotational vestibular cues; indeed, the role of otolith organ and semicircular canal cues has been debated. In this study, we examined if inter-subject differences in postural control are correlated with inter-subject differences in vestibular function.
Methods. To assess vestibular function, we used an established protocol to quantify vestibular direction-recognition perceptual thresholds, which assay the smallest motion a subject can reliably perceive. Seated subjects were passively moved in the dark via a motorized platform. Directions included lateral translation, vertical translation, yaw rotation, and head-centered roll tilts. Postural sway was also quantified via center of pressure root-mean-square measures in both sagittal and frontal planes during the Sensory Organization Tests (SOT). Healthy adult subjects were tested.
Results. We had three main results. First, the variability across subjects was high in both threshold measures and posture sway. Coefficient of variation was about 50-60% for posture sway (highest in sagittal plane for SOT tests requiring high reliance on vestibular cues) and between 33-68% for vestibular threshold testing. Second, we found a strong positive relationship between lateral translation thresholds and postural sway but not between other thresholds. Generally, since thresholds assay sensory noise in the vestibular system, these results support the hypothesis that sensory noise contributes to postural sway. More specifically, higher precision of vestibular cues in the lateral direction is related to one’s ability to limit postural sway in the frontal plane. Third, we found that lateral thresholds had the highest correlation with postural sway in SOT conditions that cause elevated reliance on vestibular cues. This result is consistent with postural sway being more influenced by vestibular noise when vestibular contributions to balance are higher.
Conclusions. Elucidating a previously undescribed role for translational motion cues in postural control, lateral translation vestibular thresholds were correlated with posture sway amongst the healthy adults investigated. This correlation was strongest in SOT conditions requiring the highest vestibular reliance. Our results generally show that precision of vestibular cues contributes to sway variability in healthy subjects.
Acknowledgements: Funded by NIH/NIDCD R03-DC013635, R01-DC04158, and R01-DC014924.
OC08 1.- FP1398Enrichment of Rare Missense Variants in Patients with Meniere Disease with Severe Tinnitus.
Alberto M. Parra-Pérez1,2,3, Alvaro Gallego-Martinez1,2,3, Jose Antonio Lopez-Escamez1,2,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain; 2Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en Enfermedades Raras, CIBERER, 28029 Madrid, Spain; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.GRANADA, Hospital Universitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4 Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
• Yes
Background: Tinnitus is the perception of noise in the absence of an external acoustic stimulation. Hearing loss is the main risk factor to develop tinnitus, however it is also associated with other conditions such as hyperacusis, anxiety, depression, hypertension, insomnia or migraine. Meniere Disease (MD) is an inner ear disorder that is characterised by episodic vertigo and associated with sensorineural hearing loss (SNHL), tinnitus and/or aural fullness. Although vertigo attacks are considered as the main symptom in the first years of the disease, persistent tinnitus is described as the most troublesome symptom by many MD patients.
Methods: Patients with MD were ranked according to the Tinnitus Handicap Inventory (THI) score. Whole Exome Sequencing (WES) was performed on 164 individuals: 78 patients with MD and high THI score (THI>66, 4th quartile of total distribution) considered as case group with severe tinnitus, and 86 MD patients with low THI (THI≤24, 1st quartile) used as internal control (no or mild tinnitus). A gene burden analysis was done filtering missense variants by a Minor Allele Frequency < 0.05 and using gnomAD (non-Finish European - NFE - and global) and CSVS (Spanish) databases as reference populations. Genes expressed in the mammalian inner ear were retrieved for further analyses.
Results: An significant enrichment of rare missense variants was found in 77 genes. (FDR<0.05) when comparing with NFE, global and Spanish population; this burden of missense variants was not found in patients with low THI score. Two of these genes have been previously associated with SNHL: PDZD7 (OR=10.29[4.21-25.17], FDR=3.23E-3) and MYH9 (OR=75.74[26.02-220.44], FDR=2.03E-15). PDZD7 is expressed in the ankle-links of the stereocilia of cochlear hair cells in mice and in several areas of the brain in humans. PDZD7 is related to deafness and Usher Syndrome. MYH9 is expressed in both hair and non-sensory cells in cochlea and vestibule and it is related with deafness autosomal dominant 17.
Conclusions: A burden of rare missense variants in PDZD7 and MYH9 is related with severe tinnitus in MD patients. Rare variation on coding regions in PDZD7 and MYH9 genes may show pleiotropic effects on the development of SNHL and tinnitus. Further studies including segregation analysis are needed to confirm the role of these variants in tinnitus.
Funding: European Union’s Horizon 2020 Research and Innovation Programme, Grant Agreement Number 848261.
2.- FP1407Rare missense variants and frameshift deletions in TECTA gene in familial Meniere disease
Alberto M. Parra-Perez* 1,2,3, Pablo Román-Naranjo* 1,2,3,4, Alba Escalera1,2,3, Paula Robles-Bolivar1,2,3, Lidia Frejo1,2,3, José A. Lopez-Escamez1,2,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre forGenomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government,PTS, 18016 Granada, Spain; 2Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en EnfermedadesRaras, CIBERER, 28029 Madrid, Spain; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, HospitalUniversitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain. * Shared first authorship
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Meniere disease (MD) is a rare inner ear disease defined by episodes of vertigo associated with SNHL initially affecting low- to medium frequencies, tinnitus, and aural fullness. Although most of MD patients are diagnosed as sporadic patients, familial aggregation is reported in 9-10% of these patients showing, mostly, an autosomal dominant inheritance pattern with incomplete penetrance. Nevertheless, recessive and digenic inheritance patterns have been recently proposed involving rare variants in OTOG and MYO7A genes.
The tectorial membrane (TM) is an extracellular matrix localized over the Organ of Corti. This membrane, composed of a mixture of collagenous and noncollagenous proteins, plays a critical role in the process of hearing mediating the mechanical stimulation of cochlear hair cells. Thus, variants in these noncollagenous proteins of the TM, namely otogelin (OTOG), otogelin-like (OTOGL), α-tectorin (TECTA), β-tectorin (TECTB) and the carcinoembryonic antigen cell adhesion molecule 16 (CEACAM16), may result in different types of autosomal dominant or autosomal recessive hearing loss in humans. In this study we identified 5 rare variants and deletions in the TECTA gene in 4 multicase Meniere disease families and 2 families with Meniere disease and partial syndromes by exome sequencing.
We performed bioinformatic analyses in 99 individuals (from 77 families with MD) where TECTA gene was highlighted as candidate for 4 multicase MD families carrying rare missense heterozygous variants (F1 – F3) and a short deletion (F4) in this gene (Table 1). Variants in this gene were also found in two additional families with one MD patient and relatives with partial syndromes carrying a missense heterozygous variant (F5) and a short deletion (F6). The three variants in the 4 multicase MD families were found clustered in the zonadhesin-like region. On the other hand, the two variants observed in the two families with partial syndromes were found close to the zona pellucida (Figure 1). We suggest that these deletions and missense variants in the TECTA gene could alter the TM mechanics involved in the sound-evoked motion of stereocilia in familial MD.
Funding: This project was partially funded by H2020-SC1-2019-848261 (UNITI) and CECEU PY20-00303 (EPIMEN)
Table 1:
Candidate variants in TECTA gene in 4 multicase MD families and 2 additional families with one MD patient and partial syndromes
| Location | Protein change | Info | MD family | MAF NFE | ACMG |
| 11:121158016T>C | p.Val1494Ala | Missense | F1 & F2 | 8.8x10-5 | LP |
| 11:121152980G>C | p.Cys1402Ser | Missense | F3 | 1.5x10-5 | VUS |
| 11:121157956AC>A | p.Asn1474LysfsTer91 | Deletion | F4 | Novel | LP |
| 11:121165368C>T | p.Pro1790Ser | Missense | F5 | Novel | VUS |
| 11:121189864GC>C | p.Gly2118ProfsTer22 | Deletion | F6 | Novel | LP |
MAF: Minor Allele Frequency; NFE: Non-Finish European population. LP: Likely Pathogenic; VUS: Variant of Unknown Significance.
Figure 1:
Variants distribution across the TECTA gene sequence in the studied FMD cohort.
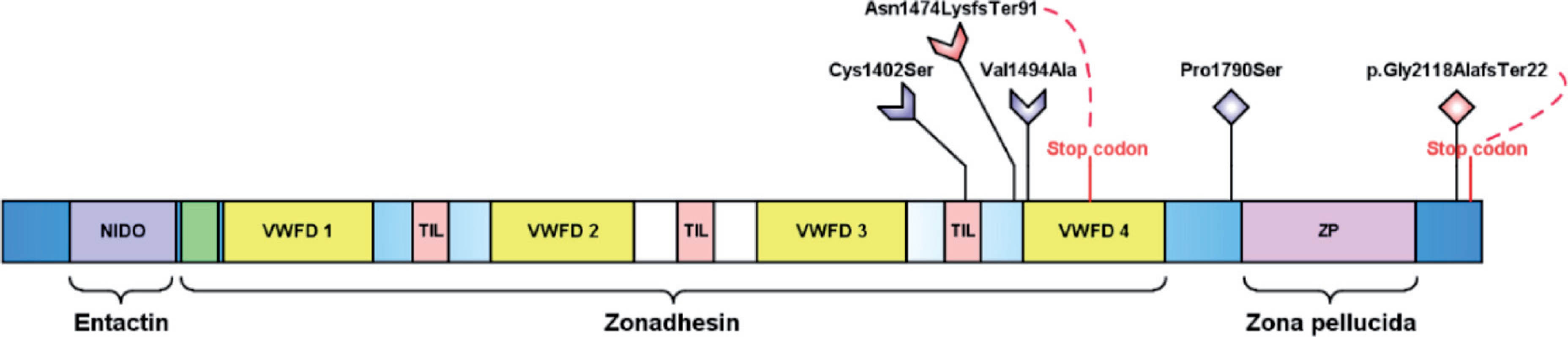
3.- FP1025KCNQ4 plays an essential role in protecting vestibular function against excessive rotational and gravity stimulation
Hansol Hong1, Eun Ji Koo2, Yesai Park3, Gabae Song1, Sun Young Joo4, Jung Ah Kim4, Heon Yung Gee4, Jinsei Jung1, Gyu Cheol Han2, Jae Young Choi1, Sung Huhn Kim1
1Department of Otorhinolaryngology, Yonsei University College of Medicine; Seoul, Republic of Korea; 2Department of Otorhinolaryngology, Gachon University College of Medicine; Incheon, Republic of Korea; 3Department of Otorhinolaryngology, Incheon St. Mary’s Hospital, Catholic University College of Medicine; Incheon, Republic of Korea4Department of Pharmacology, Graduate School of Medical Science, Brain Korea 21 Project, Yonsei University College of Medicine, Seoul, Republic of Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
KCNQ4 is a voltage-gated K+ channel distributed over the synaptic calyx and heminode of the vestibular nerve of type 1 vestibular hair cells of the inner ear. However, little is known about the vestibular phenotypes of KCNQ4 dysfunction or the definite role of KCNQ4 in vestibular organs. This study was conducted to identify the role of KCNQ4 in the vestibule by investigating the vestibular function and histological and molecular changes in vestibular sensory epithelium in p.W276S/p.W276S Kcnq4 transgenic mice after the application of 6G hypergravity stimulation for 24 hours, which represents excessive mechanical stimulation of the sensory epithelium. We also investigated the vestibular phenotype of human KCNQ4 mutations. Baseline vestibular function measured by the vestibulo-ocular reflex in Kcnq4+/+, Kcnq4+/p.W276S and Kcnq4p.W276S/p.W276S mice was normal. It was significantly decreased after hypergravity stimulation. In particular, the vestibular function decrease was more severe in the Kcnq4p.W276S/p.W276S mice than in the Kcnq4+/+ and Kcnq4+/p.W276S mice. Hair cell loss in the sensory epithelium was more significant in the Kcnq4p.W276S/p.W276S mice than in the Kcnq4+/+ and Kcnq4+/p.W276S mice. Hair cells in the sensory epithelium of the Kcnq4p.W276S/p.W276S mice showed a significantly increased depolarization duration compared with those in the mice with other genotypes. Retigabine, a KCNQ activator, prevented hypergravity-induced vestibular dysfunction and hair cell loss. Most patients (72.7%) with KCNQ4 mutations showed abnormal findings in clinical vestibular function tests. These findings suggest that KCNQ4 plays an essential role in protecting vestibular hair cells against excessive mechanical stimulation by contributing to the regulation of hair cell repolarization.
4.- FP0896What induces endolymph formation in the developing inner ear: RNAseq-based functional study
Sang Hyun Kwak1, Seong Hoon Bae2, Jinwoong Bok3*, Sung Huhn Kim2*
1Dep. of Otorhinolaryngology, St. Vincent’s Hospital, The Catholic University of Korea; 2Dep. of Otorhinolaryngology, Dep.Of Anatomy, 3Yonsei Univ. College of Medicine,
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Purpose: Endolymph is formed from E14.5 of developing murine inner ear. Although it was suggested that osmotic gradient created by changes of ionic composition plays a role in the endolymph formation, nothing has been known about the molecular mechanism of endolymph formation. We tried to investigate the mechanism of endolymph formation in the developing inner ear.
Methods: We collected extra-sensory epithelium of vestibule at the age of E16.5, E18.5, and P4, and divided it according to the presence of dark cells as follows: utricular roof epithelium and common crus which contained dark cells and semicircular canals which did not contain dark cells. RNAseq was performed with those samples to analyze the changes of ion channels according to the development. After selecting candidate genes for endolymph formation, we measured endolymphatic volume changes using confocal 3D live imaging with the application of candidate ion channel inhibitors for functional study. The localization of the candidate ion channels was examined by immunohistochemistry.
Results: A total of 48440 known genes were identified by RNAseq analysis. The genes in each sample formed close clusters according to the cell types and development period. The majority of genes are related to ion activities such as ion transport, membrane transport. Four major ions thought to be involved in the endolymph formation with high probability were sodium, chloride, calcium, and potassium ions. A functional study using 3D volume change with the application of chloride-free solution at E16.5 showed blockage of endolymphatic fluid secretion. Intracellular calcium activity is also important by means of endolymph formation. The functional study showed decreased endolymph secretion later stage. Potassium ions only worked at P5, which was confirmed with XE991(KCNQ inhibitor)
Conclusion: During inner ear development, sodium and chloride ion is strongly likely to be associated with endolymphatic fluid secretion, not the potassium ion. This finding may contribute to elucidating the mechanism of inner ear formation and possible mechanism for congenital hearing loss and vestibular disorders.
5.- FP0878Cross-sectional correlation study of vestibular decline in 111 p.Pro51Ser carriers causing DFNA9: new insights
Sebastien Janssens de Varebele, MD, PhD1; Katrien Devroye1; Julie Moyaert2; Erik Fransen, MSc, PhD3; Ronald Pennings, MD, PhD4; Raymond Van de Berg, MD, PhD5; Guy Van Camp, MSc, PhD3; Vincent Van Rompaey, MD, PhD2
1Department of ENT, Jessa Hospital, Hasseltn Belgium; 2Department of ENT, University Hospital Antwerp, Antwerp, Belgium; 3Center of Medical Genetics, University of Antwerp, Antwerp, Belgium; 4Radboud University Hospital, Nijmegen, The Netherlands; 5Maastricht University Medical Centers, Maastricht, The Netherlands
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
This presentation provides an overview of the new insights regarding the progressive decline of a wide coverage of vestibular sensors in the largest series until present of p.Pro51Ser (P51S) -carriers in the COCH gene causing DFNA9. In total 111 confirmed P51S carriers were enrolled in this study and were administered caloric tests, vHIT (video Head Impulse tes) tests and Vestibular Evoked Myogenic Potentials (VEMPs). The study population was aged between 18 to 80 years. Not only was the hearing function already showing signs of deviation from age-referenced limits in the youngest age-group (18-25 years) (estimated start of decline: 27 years), it even started prior to the vestibular function for the highest frequencies (6 and 8 kHz). The first vestibular sensor to show signs of decline was the saccular function (31 years), followed by the caloric function (35 years) and vHIT vestibulo-ocular reflex (VOR)-gains (44 years at the posterior semicircular canal (SCC); 45 years at the horizontal SCC and 49 years at the superior SCC). It is striking that the VOR-gains obtained with vHIT tests were relatively stable compared to the hearing function regardless of any frequency and compared to all other vestibular sensors, as these were the very last to start the decline. Like the hearing decline, the vestibular deterioration occurred with a high degree of asymmetry in the majority of the subjects. The status of bilateral vestibulopathy was achieved in all carriers aged older than 65 years, depending of the vestibular sensor: < 6th decade for the caloric function and VEMPs, 6th decade for PSCC and 7th decade for HSCC and SSCC. These findings suggest that the vestibular function starts to deteriorate simultaneously with the hearing function, while it was previously estimated to start 9 years prior to the latter. Even though the phenotypic expression of the p51S COCH variant is the same for all carriers, it seems that there is a wide variety according to the beginning of the decline for each individual, regardless of any hearing and vestibular sensor, witness the broad interquartile range observed in the plots depicting the progressive decline of both hearing and vestibular sensors.
6.- FP1253Quantitative proteomics analysis to identify biomarkers of refractory benign paroxysmal positional vertigo
Yanmei Feng, Guang Yang, Zhong Zheng, Dongzhen Yu, Hui Wang, Zhengong Chen, Haibo Shi, Shankai Yin
Shanghai Jiaotong University Affiliated Sixth People’s hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Benign paroxysmal positional vertigo (BPPV) is transient vertigo and paroxysmal nystagmus induced by changes in head position. This study was conducted to investigate the differential expression of serum proteins in patients with refractory BPPV and to screen for prognostic biomarkers. Serum samples were collected from patients with BPPV; tandem mass tag-based quantitative proteomics technology was used to detect and quantify the serum proteins of 30 individuals with refractory BPPV and 30 control volunteers. Bioinformatics analysis of differentially expressed proteins was performed using hierarchical clustering, gene ontology annotation, Kyoto Encyclopedia of Genes and Genomes analysis, and protein–protein interaction network analysis. A total of 769 proteins were identified, and 57 differentially expressed proteins were screened between the two groups; 15 genes were upregulated, whereas 42 were downregulated. The results revealed cholesterol metabolism, platelet activation, PPAR signaling pathway, and p53 signaling pathway were involved in refractory BPPV. Five differentially expressed proteins were chosen for parallel reaction monitoring analysis to confirm the results. Apolipoprotein A-I, apolipoprotein A-II, apolipoprotein C-III, fibrinogen gamma chain, and fructose-bisphosphate aldolase B were the five potential candidate biomarker proteins. This is the first quantitative proteomic study to reveal prognostic factors in patients with BPPV using tandem mass tag labeling technology. The identified differential proteins may improve the understanding of the pathogenesis and molecular mechanism of BPPV.
SY0035SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Lees Maes |
| TOPIC DESCRIPTIVE TITLE: | Vestibular infant screening |
| ACADEMIC / HOSPITAL AFFILIATION: | Ghent University Hospital, Belgium |
- SPEAKER 2
| NAME AND SURNAME: | Sharon Cushing |
| TOPIC DESCRIPTIVE TITLE: | Vestibular disorders in children with sensorineural hearing loss |
| ACADEMIC / HOSPITAL AFFILIATION: | Hospital for Sick Children, Toronto, Canada |
- SPEAKER 3
| NAME AND SURNAME: | Josine Widdershoven |
| TOPIC DESCRIPTIVE TITLE: | Classification of vestibular disorders in children |
| ACADEMIC / HOSPITAL AFFILIATION: | Maastricht University Medical Center, the Netherlands |
- SPEAKER 4
| NAME AND SURNAME: | Sylvette Wiener Vacher |
| TOPIC DESCRIPTIVE TITLE: | Incidence of vestibular disorders in children |
| ACADEMIC / HOSPITAL AFFILIATION: | University Hospital Robert Debré, Paris, France |
This symposium will focus on vestibulas assessment in children. It is an area that is getting increased attention in vestibular research. On the one hand this is due to increased awareness of the existence of vestibular pathologies in children, as a number of dedicated pediatric vestibular centers have come up in the past few years worldwide, both from otolaryngologic and neurologic experts. On the other hand, awareness has increased as a result of the advancement of cochlear implantation surgery, which likely has both positive and negative effects on vestibular function.
The recent development of the diagnostic criteria consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society and the International Headachge Society entitled “Vestibular Migraine of Childhood and Recurrent Vertigo of Childhood” illustrates the increased demand for knowledge in this area.
The target audience comprises of both neurologists and otorhinolaryngologists, especially those involved in the care of children. In addition, general practitioners, pediatricians, physiotherapists, audiologists and other professionals occupied in the care of children with vestibular pathologies will benefit from the lectures.
ABSTRACT 1
Hearing-impaired children are at risk for a vestibular impairment, as auditory and vestibular end-organs are closely related. Pediatric vestibular assessment is challenging and often not routinely performed in this population. Consequently, vestibular deficits often go unnoticed, giving rise to associated disorders such as a delayed motor development.
In Flanders (Belgium) a vestibular screening programme has been implemented since June 2018, giving each congenitally hearing-impaired child access to a basic vestibular screening. This screening should increase awareness and lead to early identification of vestibular deficits and referral for motor assessment and rehabilitation, in order to limit the impact on a child’s development and improve their quality of life.
In this presentation, the results of 4 years of screening will be presented, along with some tips on how to maximize the feasibility of pediatric vestibular assessment.
ABSTRACT 2
Concurrent and severe vestibular deficits occur in 30-40% of children with sensorineural hearing loss, with many of these children having bilateral vestibular loss. The prevalence of vestibular dysfunction varies by etiology of deafness with cochleovestibular anomalies, meningitis, congenital cytomegalovirus and recessive genetic causes such as Usher Type 1, being amongst the most likely etiologies. The impact of these primarily congenital, sensory deficits is widespread, as they influence not only balance and motor function but also spatial navigation, memory and learning. Vestibular impairment likely also explains some of the variability in outcomes in children with hearing loss who receive interventions such as amplification or cochlear implants. It is therefore important that vestibular function be assessed in the child presenting with hearing loss. Doing so will allow them to access appropriate rehabilitative strategies that consider the nature and extent of their sensory impairments with the view of optimizing development and outcome.
ABSTRACT 3
Vestibular disorders in children are more common that previously expected. Children often do not report typical vestibular symptoms and cannot describe their complaints very well. Nonetheless, it is estimated that vestibular loss in children is as common as sensorineural hearing loss. This validates the need for screening children with sensorineural hearing loss for vestibular loss. What’s more, known vestibular pathologies, such as Meniere’s disease, BPPV, and vestibular migraine do occur in children and should be looked out for in the pediatric population. In this presentation we would like to discuss the presence of vestibular pathologies in children and practical advice on how to carry out a vestibular assessment in children. The recent development of the diagnostic criteria consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society and the International Headache Society entitled “Vestibular Migraine of Childhood and Recurrent Vertigo of Childhood” will be discussed.
ABSTRACT 4
To report on vestibular impairment (VI) in children with balance disorders (BD) or hearing loss (H). VI was shown in 51.5% of children. For BD (e.g., vertigo, instability, delay in posturomotor development), VI was found in 36.5%. Causes of BD with VI included inner ear malformation, trauma, vestibular neuritis, meningitis, Meniere, and BPPV. After exclusion of vestibular origin to BD, other diagnoses were found: migraine, ophthalmological disorders, neurological disorders or somatoform dizziness. Of children referred for hearing loss, 68.5% were tested without cochlear implantation (CI). Of these, 54.5% presented with VI. This was mostly found in cytomegalovirus infection, inner ear malformation, and genetic syndromes. CI candidates had complete bilateral vestibular loss in 20% and 80% had partial or normal vestibular function. Vestibular testing permits ruling out VI and hence seeking other causes for BDs such as migraine and helps lower the risk of inducing bilateral vestibular loss in CI protocols.
CP0004CONTROVERSY PANEL FORM
2 SPEAKERS PER CONTROVERSY PANEL:
- SPEAKER 1
| NAME AND SURNAME: | Michael Strupp, MD. FRCP, FAAN |
| TOPIC DESCRIPTIVE TITLE: | Conservative treatment of Menière’s disease: past, present and future |
| ACADEMIC / HOSPITAL AFFILIATION: | Dept. of Neurology and German Center for Vertigo and Balance, Ludwig Maximilians University, Munich, Germany |
- SPEAKER 2
| NAME AND SURNAME: | Issam Saliba, MD, FRCSC |
| TOPIC DESCRIPTIVE TITLE: | Endolymphatic duct blocage: a novel treatment for refractory Ménière’s disease |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Otolaryngology, Head & Neck Surgery - Otology & Neurotology. Univesrity of Montreal, Montreal - Quebec, Canada |
In this controversery panel the current status of treatment options for preventive treatment of Menière’s disesase will be discussed, in particular the efficacy of non-invasive versus semi-invasive and invasive measures and the controversy between these these approaches.
Since Menière’s disease is often a chronic remitting disease, a preventive treatment is highly needed in most patients. However, although various therapeutic approaches have been proposed, there is so far insufficient evidence of the effectiveness of the following measures: low-salt, -caffeine, -alcohol diet (Cochrane review (CR)), diuretics (CR), pulsed low-pressure delivery (RCT), endolymphatic sac surgery (CR), and betahistine in dosages of 48 mg/d and 144 mg/d (RCT). There is also far no really convincing evidence for the efficacy of intratympanic steroids. Intratympanic gentamycine is effective but impairs vestibular function and may impair hearing. One option for preventive treatment are high dosages of betahistine or the combination of betahistine with Selegiline which leads to 100fold! higher serumr concentrations (phase I trial in healty volunteers, unpublished).
On the other hand labyrinthectomy/neurectomy are invasive and cause vestibular loss. It is important to note that the latter three procedures should particularly not be applied in bilateral MD, which affects up to 45% of all patients in the long-term. In this Controversy Panel alternative invasive treatment option will be presented.
At the end methodological aspects for the design of future RCTs which all have to be placebo-controlled! because of a placebo-effect of up to 70% in Meniere’s disease will be presented.
ABSTRACT 1
Endolymphatic sac surgery has been a favorable option for patients as it is a hearing preservation surgery and has a low surgical morbidity. Its effectiveness has been debated and published results are highly variable. We have, over the past few years, established a novel surgical technique for the treatment of Meniere’s disease: The Endolymphatic Duct Blockage(EDB); by comparing EDB to Endolymphatic Sac Decompression(ESD), 96.5% of the EDB group had achieved : a complete control of vertigo spells against 37.5% of the ESD group(p=0.00; a better control of tinnitus and aural fullness with EDB(p=0.021 and p=0.014 respectively). There was no statistically significant difference in hearing level preoperatively(p= 0.976) and 24 months postoperatively(p=0.287) between the two groups. Hearing level was preserved in each group.
Today, out of 300 cases operated through the last 10 years, we have at least more than 5 years follow-up for more than 150 patients. Results still stable.
ABSTRACT 2
Since Menière’s disease is often a relapsing disease, a preventive treatment is highly needed in most patients. However, although various therapeutic approaches have been proposed (with 4550 papers in PubMed with the search terms “Menière therapy”), there is so far insufficient evidence of the effectiveness of the following measures: low-salt, -caffeine, -alcohol diet (Cochrane review (CR) (1)), diuretics (CR(2)(2), pulsed low-pressure delivery (RCT(3)), endolymphatic sac surgery (CR (4)), and betahistine in dosages of 48 mg/d and 144 mg/d (RCT(5) and reviews (6, 7)). The latter RCT also showed a strong placebo-effect of 70%. One new option is the combination of betahsitine with selegiline which leads to 100fold! Higher betahistine serum concentrations as a monotherapy as we just showed in a phase I trial in 15 healthy adults (Strupp et al, unpublished).
There is so far no really convincing evidence for the efficacy of intratympanic steroids (state-of-the-art placebo-controlled RCT, press-release). Intratympanic gentamicine is evidently effective but impairs vestibular function and may impair hearing.
Methodologically it is not sufficient to compare various treatments with each other (like intrarympantic steroids with gentamicine) as long as we do not have a gold-standard for treatment. We need placebo-controlled RCTs with clinically meaningful endpoints, like “days with vertigo”.
Reference List
(1) Hussain K, Murdin L, Schilder AG. Restriction of salt, caffeine and alcohol intake for the treatment of Meniere’s disease or syndrome. Cochrane Database Syst Rev 2018 Dec 31;12:CD012173.
(2) Thirlwall AS, Kundu S. Diuretics for Meniere’s disease or syndrome. Cochrane Database Syst Rev 2006;3:CD003599.
(3) Russo FY, Nguyen Y, De SD, et al. Meniett device in meniere disease: Randomized, double-blind, placebo-controlled multicenter trial. Laryngoscope 2017 Feb;127:470-475.
(4) Pullens B, Verschuur HP, van Benthem PP. Surgery for Meniere‘s disease. Cochrane Database Syst Rev 2013;2:CD005395.
(5) Adrion C, Fischer CS, Wagner J, Gurkov R, Mansmann U, Strupp M. Efficacy and safety of betahistine treatment in patients with Meniere‘s disease: primary results of a long term, multicentre, double blind, randomised, placebo controlled, dose defining trial (BEMED trial). BMJ 2016;352:h6816.
(6) Holmes S, Lalwani AK, Mankekar G. Is Betahistine Effective in the Treatment of Meniere‘s Disease? Laryngoscope 2021 Dec;131:2639-2640.
(7) Van EB, Zaag-Loonen H, Bruintjes T, van Benthem PP. Betahistine in Meniere‘s Disease or Syndrome: A Systematic Review. Audiol Neurootol 2021 Jul 7;1-33.
OC09 1.- FP1120FREE PAPER FORM
Effects of interval time of the Epley Maneuver on immediate reduction of positional nystagmus: A randomized, controlled, non-blinded clinical trial
Takao Imai1, Tomoko Okumura1, Takashi Sato1, Yumi Ohta1, Takefumi Kamakura1, Hidenori Inohara1
Department of Otorhinolaryngology - Head and Neck Surgery, Osaka University Graduate School of Medicine, Osaka, Japan
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: The Epley maneuver (EM) has an immediate effect: rapid reduction of positional nystagmus. Benign paroxysmal positional vertigo (BPPV) causes BPPV fatigue, which constitutes fatigability of positional nystagmus and vertigo with repeated performance of the Dix-Hallpike test; notably, BPPV fatigability becomes ineffective over time. We hypothesized that the immediate effect of the EM is caused by BPPV fatigue. Therefore, we suspected that performance of the EM with intervals between head positions would worsen the immediate reduction of positional nystagmus in patients with BPPV, because BPPV fatigability would become ineffective during performance of this therapy. Methods: Forty patients with newly diagnosed BPPV were randomly assigned to the following two groups; one group performed the EM without intervals between positions (group A), and the other group performed the EM with 3 min intervals between positions (group B). The primary outcome measure was the ratio of maximum slow-phase eye velocity (MSPEV) of positional nystagmus soon after the EM, compared with that measured before the EM. Secondary outcome included whether a 30 min interval after the EM enabled recovery of MSPEV of positional nystagmus to the original value. This study followed the CONSORT 2010 reporting standards. Results: In both groups A and B, the immediate effect of the EM could be observed, because MSPEV during the second Dix-Hallpike test was significantly smaller than MSPEV during the first Dix-Hallpike test (p < 0.0001 in group A, p < 0.0001 in group B). The primary outcome measure was larger in group B than in group A (p = 0.0029). The immediate effect faded 30 min later (secondary outcome). Conclusions: This study showed that the EM had an immediate effect both with and without interval time in each head position of the EM. Because setting interval time in each head position of the EM reduced the immediate effect of the EM, interval time during the EM adds less benefit. This finding can reduce the effort exerted by doctors, as well as the discomfort experienced by patients with pc-BPPV, during EM. However, this immediate effect may be caused by BPPV fatigue, and may fade rapidly. Classification of Evidence: 1b.
2.- FP1250FREE PAPER FORM
Geriatric Benign Paroxysmal Positional Vertigo: A Single-center Study
Ning Song, Yuexia Wu, Li Xiang, Ling Xia, Xu Yang
Department of Neurology, Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine, Beijing 100049, People’s Republic of China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract
Background: Dizziness and imbalance are among the most common problems in the elderly. Benign paroxysmal positional vertigo (BPPV) is the most common cause of these problems.
Objective: To comparatively analyze the clinical features and canalith repositioning maneuver (CRM) treatment efficacy in geriatric and non-geriatric BPPV patients based on the Bárány Society's BPPV diagnostic criteria.
Methods: 575 patients diagnosed with BPPV were enrolled. All patients were diagnosed based on the presence of nystagmus during the Dix-Hallpike, supine Roll tests. CRM were performed according to the involvement of canals. The subjects were divided into two groups by age (geriatric group =60 years and non-geriatric group 13-59 years), and the gender, subtype distribution and CRM treatment efficacy were analyzed.
Results: (1) Age ranged from 60 to 88 years in geriatric group (70.16±7.384 years, n=270) and from 13 to 59 years in non-geriatric group (44.57±10.174 years, n=305).The geriatric group included 178 women and 92 men(1.9:1), the non-geriatric group included 237 women and 68 men(3.5:1)(p=0.002).The gender ratio changed with age.(2)Subtype distribution: (a)posterior canal BPPV(PC-BPPV):in geriatric group, 156(57.7%) were diagnosed with PC-BPPV, among which 117(43.3%) had canalolithiasis (PC-BPPV-ca),39(14.4%) had cupulolithiasis (PC-BPPV-cu). In non-geriatric group, 199(65.2%) were diagnosed with PC-BPPV, among which 141(46.2%) had PC-BPPV-ca, 58(19.0%) had PC-BPPV-cu. (b)horizontal canal BPPV(HC-BPPV): 82(30.4%) in geriatric group and 69(22.6%) in non-geriatric group were diagnosed with HC-BPPV(p=0.035). In geriatric group,40(14.4%) had HC-BPPV-ca, 42(15.6%) had HC-BPPV-cu. In non-geriatric group,44(14.4%) had HC-BPPV-ca, 25(8.2%) had HC-BPPV-cu(p=0.006). (c) anterior canal (AC-BPPV): 14(5.2%) in geriatric group and 32(10.5%) in non-geriatric group were diagnosed with AC-BPPV (p=0.019). (d) multi-canal BPPV (MC-BPPV):18(6.7%) in geriatric group and 5(1.6%) in non-geriatric group were diagnosed with AC-BPPV(p=0.002). (3) CRM treatment efficacy: treatment outcome was compared among two groups. The treatment efficacy by one session CRM was 58.1% (111/191) in geriatric group and 73.8% (163/221) in non-geriatric group (p=0.001), which had a tendency to decrease with age.
Conclusion: BPPV is more common among women, and our study showed for geriatric men, there was a tendency to increase with age. The proportion of HC-BPPV-cu and MC-BPPV was higher in geriatric BPPV, while AC-BPPV was less than younger BPPV. Treatment efficacy by CRM may decrease with age.
Keywords: Benign paroxysmal positional vertigo, Geriatric, Cupulolithiasis, Canalith repositioning maneuver
Fig.1
BPPV gender ratio (n=575)
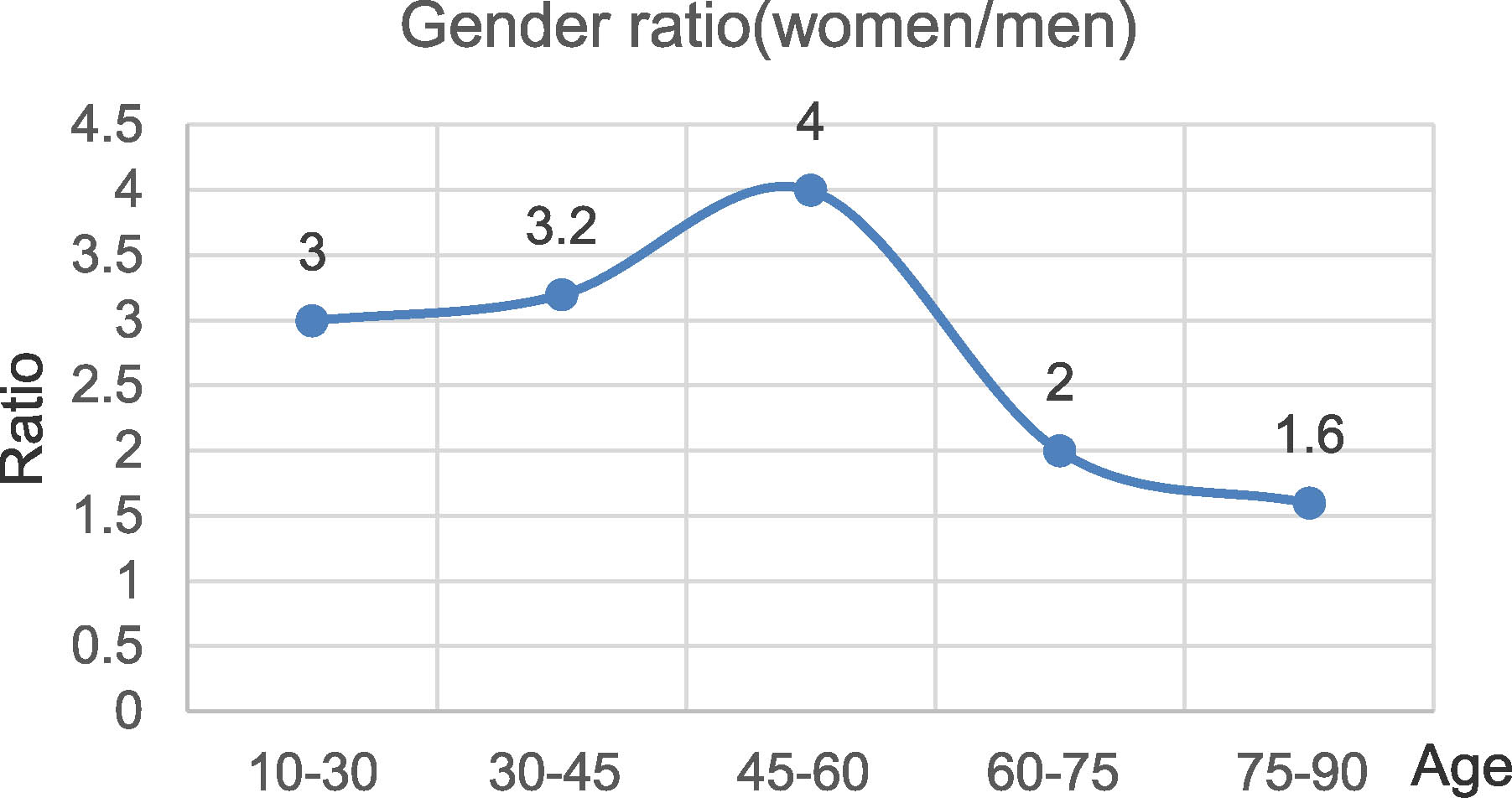
Fig.2
CRM treatment efficacy (n=412)
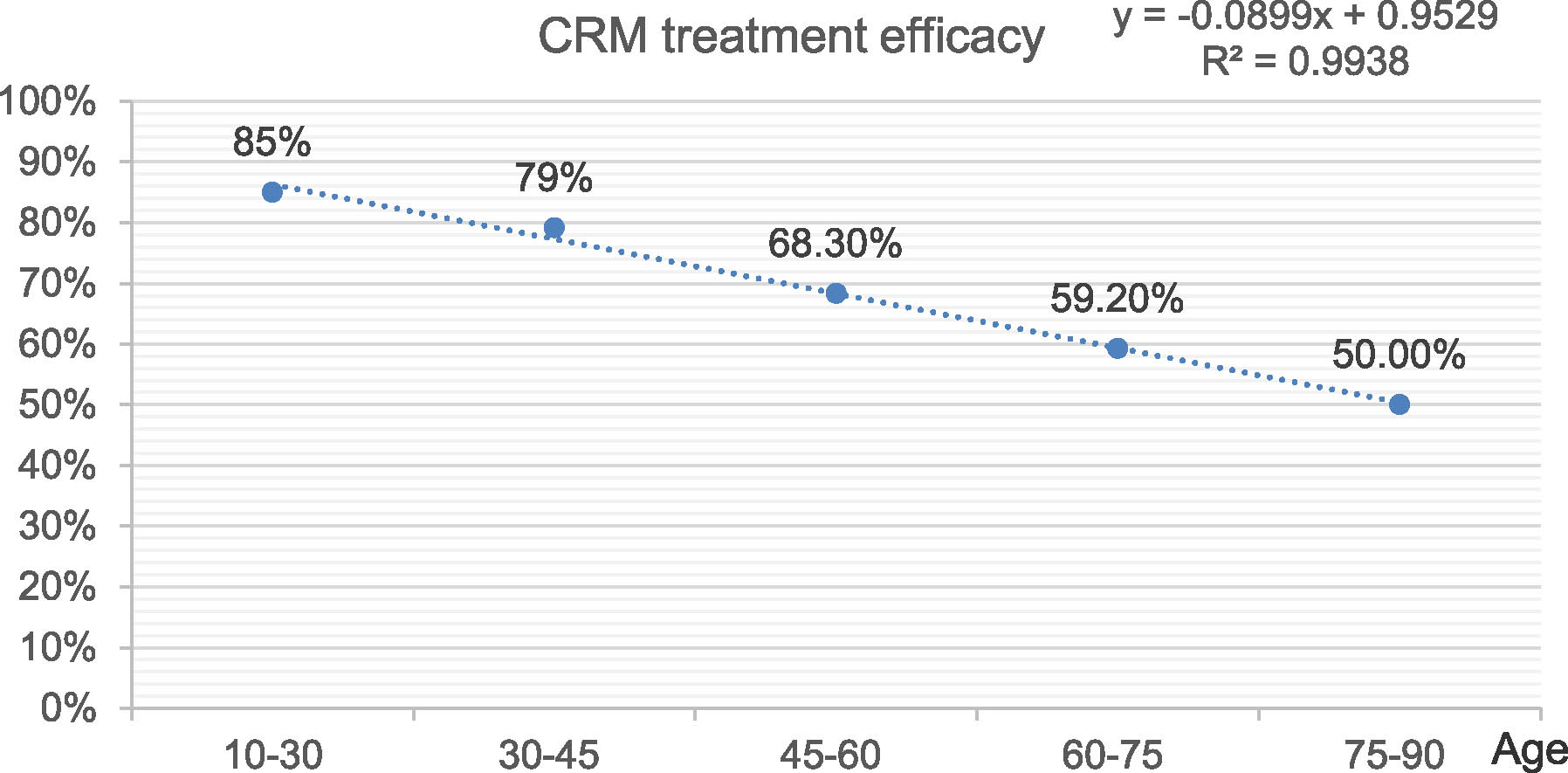
Table1.
BPPV subtype distribution(n=575); CRM, canalith repositioning maneuver
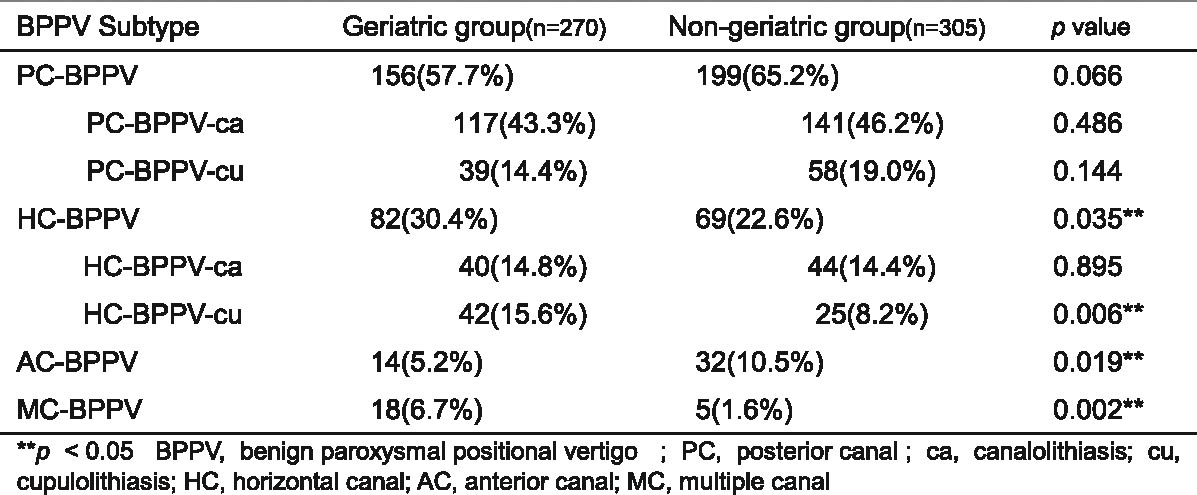 |
3.- FP1365Clinical Characteristics and Associated Factors of Canal Switch in Benign Paroxysmal Positional Vertigo
Yuexia Wu, Xu Yang
Department of Neurology, Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine, Beijing 100049, People’s Republic of China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract
Background: Canal switch benign paroxysmal positional vertigo (CS-BPPV) is a transition of BPPV involving one canal to another canal on the same side during or after canalith repositioning procedures (CRP).
Objective: To investigate the clinical characteristics of CS-BPPV and its associated factors.
Methods: 1,031 patients with BPPV were retrospectively analyzed. The percentage of CS-BPPV among three canals was analyzed and the baseline characteristics, intensity of nystagmus and the percentage of direction-reversing nystagmus were compared between patients with and without CS-BPPV.
Results: (1) baseline characteristics A total of 1031 patients (including 46 patients with multi-canal BPPV) with BPPV were retrospectively analyzed, including 51 patients had CS-BPPV (51/1031, 4.9%) and 980 patients had non-CS BPPV(980/1031, 95.1%). There was no statistical significance between the two groups regarding age, sex, side of affected semicircular canal (p=0.159, 0.465, and 0.341, respectively).
(2) CS-BPPV rate: Of 1031 BPPV, (a) there were 601 (58.3%) patients with posterior canal BPPV (PC-BPPV), among which 25 (4.2%) PC-BPPV exhibited canal switch phenomenon, including 11 (1.8%) conversion to horizontal canal BPPV (HC-BPPV) and 14 (2.3%) conversion to anterior canal BPPV(AC-BPPV); (b) There were 289 (28.0%) HC-BPPV, 17 (5.9%) exhibited canal switch, including 14 (4.8%) conversion to PC and 3 (1.0%) conversion to AC; (c) there were 95 (9.2%) AC-BPPV, including 9 (9.5%) exhibited canal switch phenomenon, including 8 (8.4%) conversion to PC and 1 (1.1%) conversion to AC.
(3) Direction-reversing nystagmus and maximum slow phase velocity (mSPV) of nystagmus: Direction-reversing nystagmus occurred in 11 patients (21.6%) of the CS-BPPV group and 45 patients (4.6%) of the non-CS-BPPV group (p < 0.001). The mSPV of nystagmus in patients with CS-BPPV was significantly higher when compared with patients with non-CS-BPPV (p < 0.001).
Conclusion: The canal switch phenomenon occurs in BPPV patients. AC-BPPV has a higher canal switch incidence, followed by HC-BPPV and PC-BPPV. For patients with different types of BPPV, CS-BPPV has a higher SPV value and is prone to show reverse nystagmus.
Keywords: benign paroxysmal positional vertigo canal conversion, canal switch, direction-reversing nystagmus
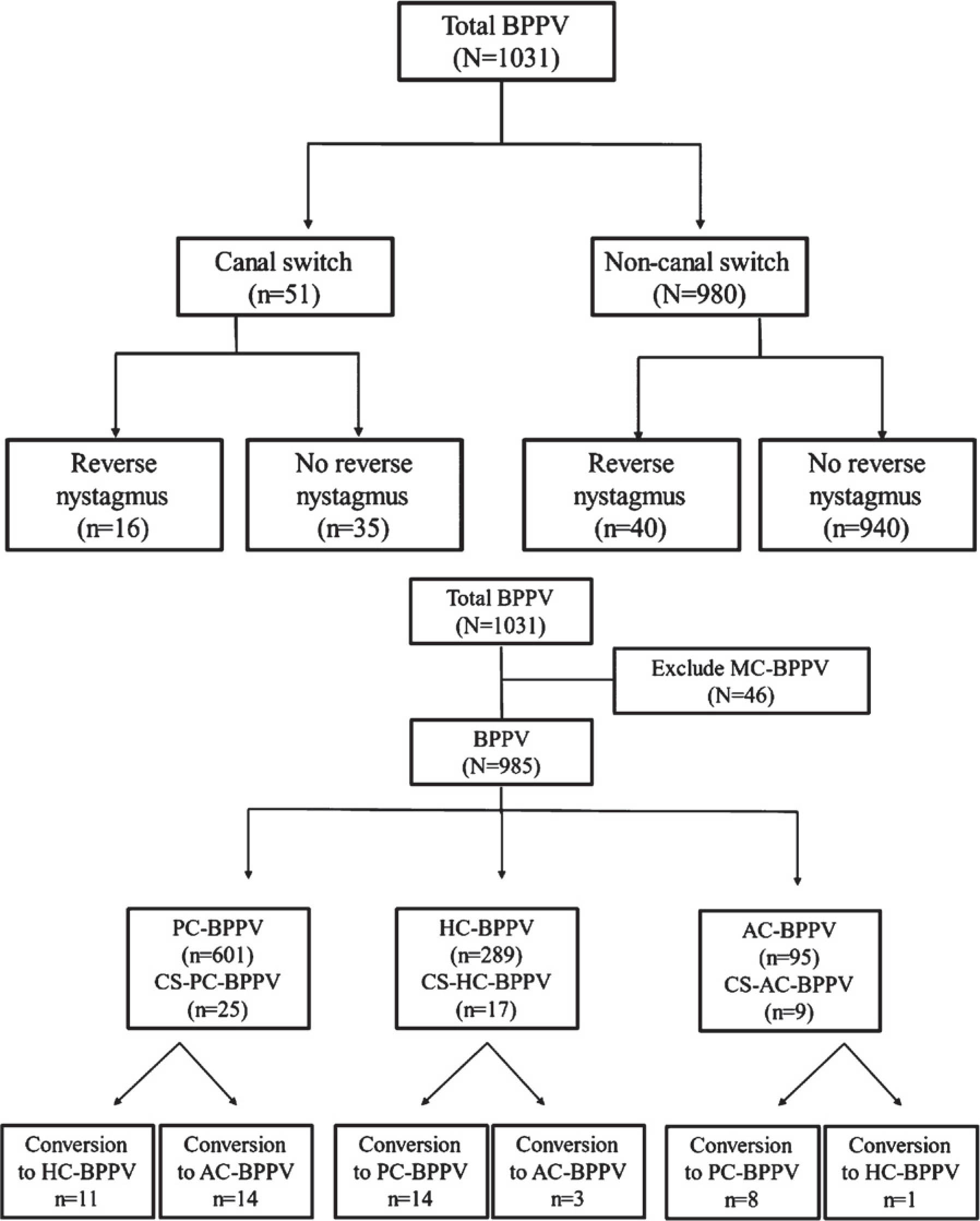
4.- FP0956Upright BPPV Protocol: sensitivity of a new protocol for the diagnosis of Benign Paroxysmal Positional Vertigo
Salvatore Martellucci2, Andrea Castellucci3, Giacinto Asprella Libonati4
1ENT Unit, Department of Surgery, Santa Maria Goretti Hospital, AUSL Latina, Italy; 2Audiology & Vestibology Service, Centromedico, Bellinzona, Switzerland; 3ENT Unit, Arcispedale Santa Maria Nuova, AUSL - IRCCS, Reggio Emilia, Italy; 4Vestibology and ENT Unit, Giovanni Paolo II Hospital, Policoro, Matera, Italy.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
The diagnosis of benign paroxysmal positional vertigo (BPPV) traditionally relies on well-known positioning tests. Patients are brought to the supine position and the head is quickly turned towards the side to be tested. Nevertheless, standard positionings can be poorly tolerated in patients with intense autonomic symptoms and anxiety-related issues, especially in the acute stage. Furthermore, the diagnosis of the affected side in horizontal semicircular canal (HSC)-BPPV may require some test repetitions. We gathered under the so-called “Upright BPPV Protocol” (UBP) those diagnostic tests performed with patient in the sitting position by moving the head along the spatial axes and observing nystagmus features. This protocol includes the evaluation of spontaneous nystagmus in the primary gaze position, the Head Pitch Test (HPT), head movements along RALP and LARP axes (URALP/ULARP test) and the Upright Head Roll Test (UHRT). Firstly, we retrospectively analyzed 134 patients with HSC-BPPV. They received both UBP and a complete diagnostic protocol (CDP), including UBP, seated-supine positioning test and standard supine roll test. A correct diagnosis for HSC-BPPV was achieved in 95.5% of cases using the UBP exclusively, with a highly significant concordance with the CDP (p<0.000, Cohen’s kappa=0.94), regardless of the time elapsed from symptoms onset to the diagnosis. The concordance between CDP and UBP was not impaired even if the latter protocol only provided incomplete results (p<0.000). A correct diagnosis using the sole standard supine roll test was achieved in 85.1% of cases, with a weaker strength of relationship (Cohen’s kappa=0.80). In a second prospective study, 109 patients diagnosed with posterior semicircular canal (PSC)-BPPV were enrolled. HPT was carried out first. In case it was useless for the diagnosis, it was sensitized by flexing the patient’s head backward and forward along the RALP and LARP planes (URALP/ULARP test). The diagnosis was then confirmed by bilateral Dix-Hallpike test. A correct diagnosis of PSC-BPPV was achieved in 75.2% with the sole HPT, whereas in 87.2% of cases with the URALP/ULARP test. The sensitivity of the Upright Protocol was related to the diagnostic delay, as the correct diagnosis was achieved in 100% of patients with recent onset of symptoms (<7 days), while reducing to 68.9% in subjects with longer-lasting vertigo (p<0.001).In conclusion, the proposed UBP allows a correct diagnosis from the sitting position in most patients presenting with the most common BPPV-forms, especially in the acute stage, sparing the patient traditional positioning tests and related symptoms.
5.- FP1080The impact of Benign Paroxysmal Positional Vertigo (BPPV) on gait and falls: a systematic review and meta-analysis.
Sara Pauwels1, Laura Casters1, Nele Lemkens2, Sus Indesteege2, Kenneth Meijer3, Pieter Meyns1, Raymond van de Berg4, Joke Spildooren1
1REVAL - Rehabilitation Research Center, Faculty of Rehabilitation Sciences, Hasselt University, Diepenbeek, Belgium; 2Hospital Oost-Limburg, Genk, Belgium; 3Maastricht University, Maastricht, The Netherlands; 4Maastricht University Medical Centre, Maastricht, The Netherlands.
The goal of this systematic review and meta-analysis is to give insight in the influence of Benign Paroxysmal Positional Vertigo (BPPV) on gait, falls and fear of falling. As such, this is an important topic for otolaryngologists and physical therapists. Preliminary results show the following:
Background: Benign Paroxysmal Positional Vertigo (BPPV), characterized by vertigo after head rotations is the most common cause of balance disorders and dizziness among older adults. The influence on gait and falls is unclear. BPPV is well treatable with a Particle Repositioning Maneuver (PRM).
Methods: Pubmed, Web of Science and Scopus were systematically searched for articles comparing gait and/or falling between 1) people with BPPV (pwBPPV) and controls and 2) pre- and post-treatment. When possible, standardized mean differences (SMD) or Odds-ratio (OR) were calculated.
Results: 14 from the 18 included studies were useful for a meta-analysis. Gait velocity was 0.072m/s lower in pwBPPV in comparison to controls (SMD -0.73; p<0.001). Differences in gait velocity were even more present during head rotations, as PwBPPV walked 0.11m/s slower during that condition in comparison to controls (p<0.001). After PRM gait velocity significantly increased during normal walking (SMD -0.51; p<0.001) and walking with head rotation (p<0.01). Further, gait became safer according to the Dynamic Gait Index and Functional Gait Assessment (SMD -0.81; p<0.001).
The amount of fallers was not significantly different between pwBPPV and controls (OR 2.0; p=0.11). However, after treatment the reported number of falls, the amount of pwBPPV that fell and fear of falling reduced significantly.
Discussion: The difference in gait velocity between pwBPPV and controls on one hand and post-treatment on the other hand is clinically meaningful. The fall related difference between pwBPPV and controls might be underestimated, as only 46 pwBPPV were included for this outcome. Studies including more older adults with BPPV are necessary to evaluate the influence of BPPV on fall incidence.
Conclusion: even though fall incidence in pwBPPV is not significantly higher in comparison to controls, treatment with a PRM has a tremendous influence on gait and fall outcomes post-treatment. Gait velocity (with and without head rotations), DGI, FGI, fear of falling and fall incidence improved after treatment in pwBPPV. As such, a good diagnosis and treatment of BPPV is of utmost importance.
6.- FP1156Personalized Medicine for Optimal Stimulation of the Semicircular Canals
Andrés Soto Varela2, Vicente Pérez Muñuzur1, Ismael Arán González3, Alberto Pérez Muñuzuri1
1Group of Non-Linear Physics of the University of Santiago de Compostela, 2Spain Otoneurology Unit of the Complexo Hospitalario Universitario de Santiago de Compostela, Spain, 3Otoneurology Unit of the Complexo Hospitalario Universitario de Pontevedra, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
BACKGROUND. The rotational tests are always performed following a specific procedure independently on the angular arrangement of the semicircular canals for a given patient. This might result in an impairing diagnostic ability. Considering the personalized medicine in the development of rotational tests, there are certain optimized angular directions that maximize stimulation in a certain canal, almost completely inhibiting the other two. It is expected that this plane of rotation, known as prime direction, can provide a better response on clinical test.
METHODS. Based on mathematical models of the membranous labyrinth and their simulation by means of Computational Fluid Dynamics techniques, we evaluate how different planes of rotation affect the vestibular diagnosis.
RESULTS. Both ideal and real models predict similar behavior in terms of pressure distribution, velocities and vorticity (Figure 1 and Figure 2). Evaluating the transcupular pressure, the degree of optimization varies depending on the selected plane of rotation (Table 1 and Table 2). The prime directions show an optimization of the rotational testing when the angular relationship between semicircular canals is lower than 90°, increasing as they move away from the ideal orthogonality.
Figure 1.
The total pressure obtained under Htest angular direction for rotating reference frame, with amplifi ed vision of cupula walls, where horizontal ones show the biggest pressure differences. The data was obtained at the end of stimulation when the head returns to the initial position (clockwise rotation). A) Pressure distribution for the real model. B) Pressure distribution for the orthogonal model.
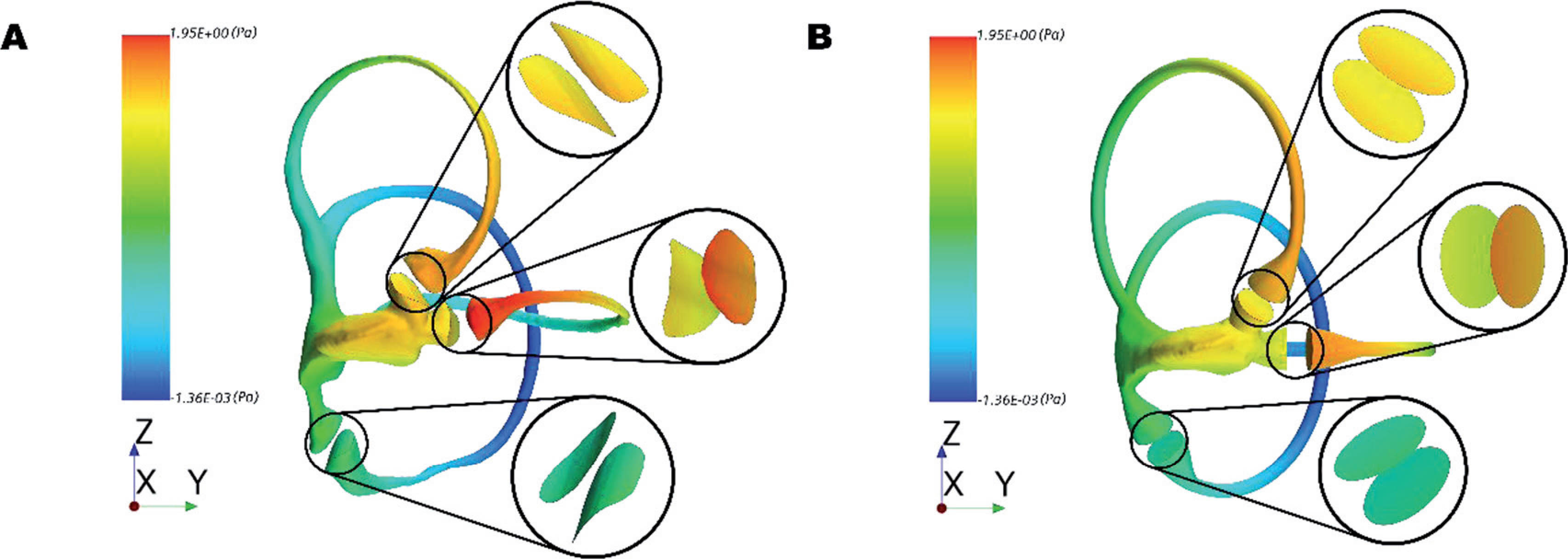
Figure 2.
The velocity and vorticity in rotating reference frame, obtained under Htest angular direction for the orthogonal model. Slides were made considering the centerline of each idealized semicircular canal. A) Vortices in the frontside and backside of the utricle. Vortices in B) the horizontal ampullae C) the superior ampullae D) the posterior ampullae.
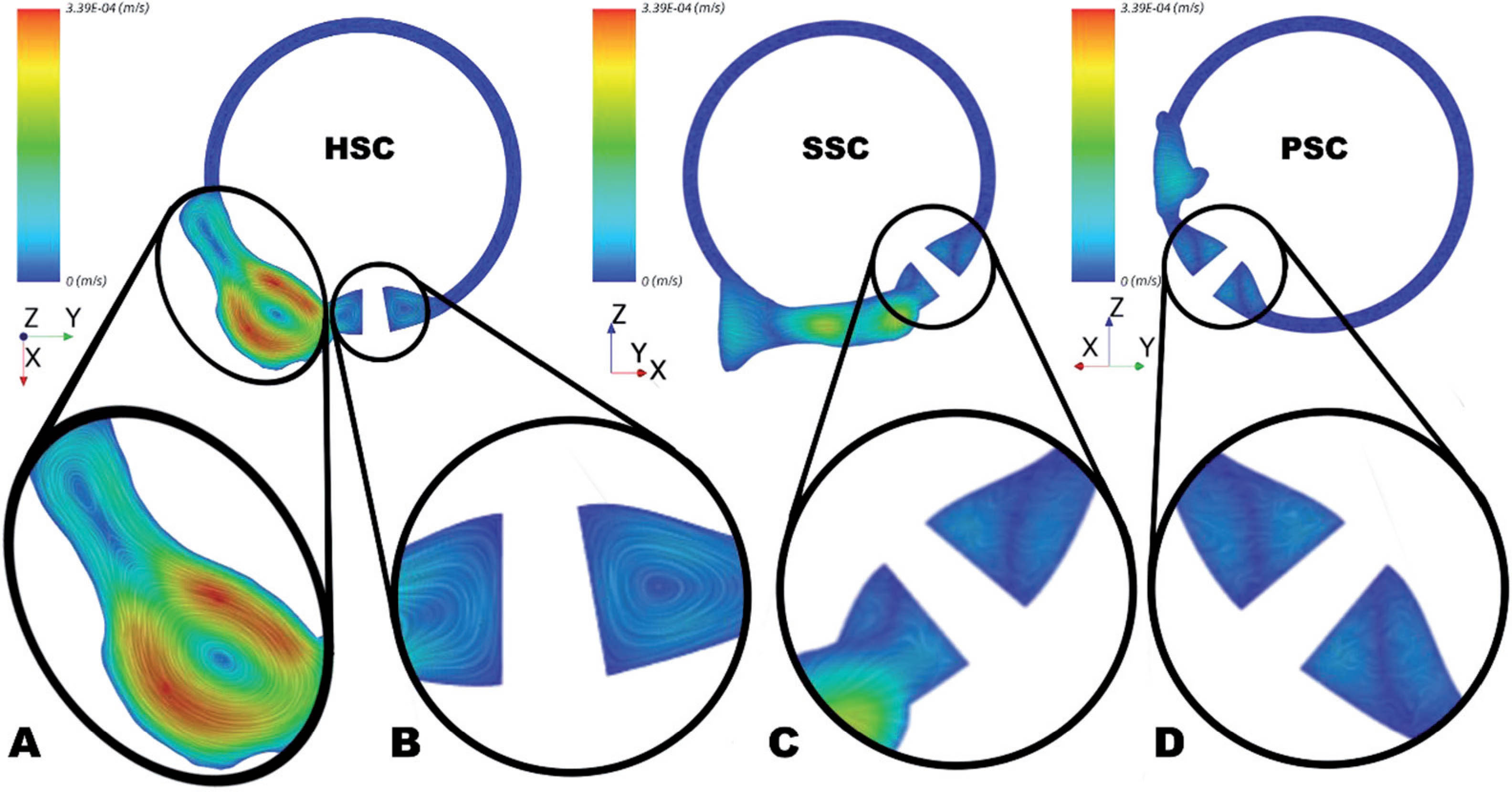
Table 1.
Degree of optimization for prime directions compared with test and max directions for the real model. Where the positive percentages indicate optimization and negative lack of effectivity.
| Rotational direction | Canal excited | Optimization respect to test | Optimization respect to max |
| Hprime | Horizontal | 9.19% | 18.01% |
| Sprime | Superior | -4.09% | -4.98% |
| Pprime | Posterior | 12.68% | 11.65% |
Table 2.
Grade of optimization for prime directions compared with test and max directions for the idealized models. Where the positive percentage indicates an optimization and negative a lack of effectivity.
| Model | Name | Rotational direction | Canal excited | Optimization respect to test | Optimization respect to max |
 | HS75 | Hprime | Horizontal | 22.17% | 22.17% |
| HS75 | Sprime | Superior | 0% | 11.80% | |
| HS75 | Pprime | Posterior | 0% | 0% | |
 | HS105 | Hprime | Horizontal | -4.45% | -4.45% |
| HS105 | Sprime | Superior | 0% | 21.08% | |
| HS105 | Pprime | Posterior | 0% | 0% | |
 | HP75 | Hprime | Horizontal | 32.26% | 32.26% |
| HP75 | Sprime | Superior | 0% | 0% | |
| HP75 | Pprime | Posterior | 0% | 7.4% | |
 | HP105 | Hprime | Horizontal | -1.90% | -1.90% |
| HP105 | Sprime | Superior | 0% | 0% | |
| HP105 | Pprime | Posterior | 0% | 12.02% |
CONCLUSION. We demonstrate that a different plane of rotation, selected following the angular relationships between the planes of the semicircular canals, helps to distinguish each cupular stimulus contribution on the nystagmus, resulting in an optimization of the rotational testing of the vestibular function. To study the individualities of the membranous labyrinths through numerical simulations can serve as a tool to increase the vestibular diagnosis success.
TARGET AUDIENCE. Physicists, mathematicians and otolaryngologists specialized in otoneurology.
ST02 1.- FP0953The effect of size and location of superior canal dehiscence on audiometric measurements, vestibular-evoked myogenic potentials and video-head impulse testing
Andrea Castellucci1,2, Cristina Brandolini2, Valeria Del Vecchio2,3, Gianluca Piras2,4, Salvatore Martellucci5, Pasquale Malara6, Angelo Ghidini1
1ENT Unit, Arcispedale Santa Maria Nuova, AUSL - IRCCS, Reggio Emilia, Italy; 2ENT and Audiology Unit, S.Orsola-Malpighi University Hospital, Bologna, Italy; 3UOC Audiology and Vestibology, University Hospital Federico II, Naples, Italy; 4Department of Otology and Skull Base Surgery, Gruppo Otologico, Piacenza-Rome, Italy; 5ENT Unit, Santa Maria Goretti Hospital, AUSL Latina, Italy; 6Audiology & Vestibology Service, Centromedico, Bellinzona, Switzerland.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Even though superior canal dehiscence (SCD) syndrome has already been widely studied from a clinical, etiopathogenetic and therapeutic point of view, some diagnostic aspects have yet to be clarified. Although it is well known how this condition can lead to unusual clinical pictures presenting with different instrumental patterns, no univocal explanation to the wide variability of SCD symptoms and signs has been offered yet. In order to further elucidate the underlying pathophysiology, several studies have examined the relationship between morphology and location of dehiscence and clinical variables. Studies seem to agree that SCD size is directly correlated with air-bone gap (ABG) and both cervical/ocular-VEMPs amplitudes, whereas it shows an inverse correlation with VEMPs thresholds. Moreover, wide dehiscencee are believed to result in impaired vestibulo-ocular reflex (VOR) for the superior canal (SC). Lack of univocal results among different investigations probably reflects the small samples analysed and the differences in selection criteria. The aim of this paper is to provide further evidences for these assumptions, correlating objective measures of audio-vestibular function with SCD size and location in ears with SCD and compare results with literature. We retrospectively evaluated 242 patients exhibiting SCD and/or extremely thinned bone overlying superior canals (SC) on CT scans and selected 73 SCD patients (95 ears with SCD). Data concerning audiometry, impedance audiometry, video-head impulse test (vHIT), cervical vestibular-evoked myogenic potentials (cVEMPs) and ocular VEMPs (oVEMPs) to air- (AC) and bone-conducted (BC) stimuli were collected for each pathologic ear and correlated with dehiscence size and location. AC pure-tone average (PTA) (p=0.013), low-frequency ABG (p<0.001), AC-cVEMPs amplitude (p=0.002), BC-cVEMPs amplitude (p<0.001) and both AC and BC-oVEMPs amplitude (p<0.001) positively correlated with increasing SCD size. An inverse relationship between dehiscence length and both AC-cVEMPs and oVEMPs thresholds (p<0.001) and SC VOR-gain (p<0.001) was observed. Dehiscences at the arcuate eminence (AE) exhibited lower SC VOR-gain compared to SCD along the ampullary arm (p=0.008) and less impaired BC-thresholds than dehiscences at the superior petrosal sinus (p = 0.04). We confirmed that SCD size affects AC-PTA, ABG and both amplitudes and thresholds of cVEMPs and oVEMPs. We also described a tendency for SC function to impair with increasing SCD size and when dehiscence is located at the AE. The latter data may be explained either by a spontaneous canal plugging exerted by middle fossa dura or by a dissipation through the dehiscence of mechanical energy conveyed to the endolymph during high-frequency impulses.
2.- FP1048What could tell us posturography about balance in essential tremor?
Marcos Rossi-Izquierdo1, Virginia Franco-Gutierrez1, Elena San-Román-Rodríguez1, Berta Patiño-Castiñeira1, Miguel Alberte-Woodward2, Mónica Guijarro-Del Amo3, Sofía Santos-Perez4,5, Isabel Vaamonde-Sanchez-Andrade4, Andrés Soto-Varela4,5
1Department of Otolaryngology, University Hospital Lucus Augusti, Lugo, Spain; 2Department of Neurology, Complexo Hospitalario Universitario de Santiago de Compostela, Spain; 3Department of Neurology, University Hospital Lucus Augusti, Lugo, Spain; 4Department of Otolaryngology, Complexo Hospitalario Universitario de Santiago de Compostela, Spain; 5Department of Surgery and Medical-Surgical Specialities, Universidade de Santiago de Compostela, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: Essential tremor (ET) is a neurological disorder characterized primarily by action tremor. Balance impairments in ET patients were considered to be uncommon and simply age related. However quantitative assessment with posturography has revealed impairments in both static and dynamic balance control.
The aim of the present study is to assess postural stability with different posturographic techniques in ET patients.
Study Design: Prospective study
Setting: University Hospitals, ambulatory care (outpatient clinic)
Patients: Eleven patients diagnosed with essential tremor and Twelve healthy controls were included.
Intervention: Balance assessment
Main Outcome Measures: Sensory organization test (SOT) and Limits of stability (LOS) of the computer dynamic posturography (CDP), results of free-field body sway analysis with mobile posturography (Vertiguard), modified timed up and go test (TUG), Dizziness handicap inventory (DHI) and activities-specific balance confidence scale (ABC).
Results: Patients with ET showed poorer scores in the SOT than controls for composite balance and somatosensory input. They also performed worse in LOS tests and Vertiguard device indicated a higher risk of falling. There were no differences in the modified TUG. The mean score of DHI was 15.64 and 85.16 for ABC.
Conclusion: Posturography assessment (CDP and Vertiguard) is more accurate in showing balance impairment in ET patients than clinical evaluation (modified TUG). Balance impairment involves deteriorated processing of somatosensory input which could be explained by cerebellar dysfunction. Balance deficits could be included in future diagnostic criteria.
Keywords: Mobile posturography – sensory organization test – limits of stability – timed up and go test – Essential tremor – ABC – DHI – computer dynamic posturography - Vertiguard
3.- FP1088Diagnostic agreement between video oculography and MRI for diagnosing internuclear ophthalmoplegia in multiple sclerosis
Rawan Omary1, Christopher J. Bockisch1,2,3, Shila Pazahr4, Anthony J. De Vere-Tyndall4, Krisztina Baráth5, Konrad P. Weber1,2
1Departments of Ophthalmology; 2Neurology; 3ENT; 4Neuroradiology, University Hospital Zurich, University of Zurich, Switzerland; 5Radiologie und Neuroradiologie am Glattzentrum, Switzerland.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ No
Internuclear ophthalmoplegia (INO) occurs in 20-30% of patients with multiple sclerosis (MS). Magnetic resonance imaging (MRI) is a widely used ancillary examination to detect lesions in the medial longitudinal fasciculus (MLF). Early detection of INO is important for disease subtyping, treatment, and prognosis of MS. In this study, we compared the diagnostic accuracy of video oculography (VOG) compared to MRI for the diagnosis of INO. We prospectively compared 3T MRI and VOG of 66 MS patients and VOG of 28 healthy volunteers to compare their diagnostic agreement. The saccadic versional disconjugacy index (VDI, peak velocity ratio of the abducting to the adducting eye) was calculated for each patient and a cutoff (upper 95th percentile of healthy volunteers) was defined for the diagnosis of INO. For each patient a concurrent MRI was reviewed by three experienced neuroradiologists independently for findings suggestive of INO. The consensus MRI score and inter-rater agreement were calculated. The consensus MRI score for INO was compared to the VDI of each patient. Of the 66 patients, INO could be detected neither on MRI nor VOG in 35 patients. In fourteen patients, INO was found with both tests. 17 cases showed conflicting test results: 11 patients were INO-positive on VOG and INO-negative on MRI, and 6 patients were INO-positive on MRI and INO-negative on VOG. Compared with VOG, MRI had a positive percent agreement (PPA) of 56% and a negative percent agreement (NPA) of 85%. Conversely, compared with MRI, VOG had a PPA of 70% and an NPA of 76%. Hence VOG was more sensitive for detecting INO than MRI. Therefore, a normal VOG is helpful to rule out INO. Contrary, a positive MRI is specific to rule in INO. In conclusion, VOG is a simple, rapid, and noninvasive test that aids in the diagnosis of INO in MS patients.
4.- FP1094Three Years of Vestibular Infant Screening - Flanders: Results, Sensitivity and Refinement of the Vestibular Screening Protocol in Infants with Sensorineural Hearing Loss
Sarie Martens1, Ingeborg Dhooge2,3, Cleo Dhondt3, Marieke Sucaet1, Saartje Vanaudenaerde2, Lotte Rombaut2, Leen Maes1,2
1Faculty of Medicine and Health Sciences, Department of Rehabilitation Sciences, Ghent University, Ghent, Belgium; 2Department of Oto-rhino-laryngology, Ghent University Hospital, Ghent, Belgium; 3Faculty of Medicine and Health Sciences, Department of Head and Skin, Ghent University, Ghent, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Hearing-impaired children have an increased risk for vestibular deficits, which can affect the development of children on many levels. As pediatric vestibular assessment has not yet been routinely integrated in clinical practice, the Vestibular Infant Screening (VIS)-Flanders project has implemented a standard vestibular screening for each six-month-old hearing-impaired child in Flanders (Belgium) since June 2018. This study aimed (1) to report the vestibular screening results after three years, and (2) to map the sensitivity of the vestibular screening protocol based on the results of an extensive vestibular follow-up protocol at the Ghent University Hospital in order to refine the vestibular screening.
Methods: (1) Cervical Vestibular Evoked Myogenic Potentials (cVEMP) with bone-conduction were used as vestibular screening tool in all 25 reference centres responsible for the neonatal hearing screening in Flanders. From June 2018 until June 2021, 254 children (mean age: 7.4 months) with sensorineural hearing loss were screened. (2) Between November 2017 and September 2021, 71 children with sensorineural hearing loss were referred to the Ghent University Hospital. An extensive vestibular assessment was performed at the age of six months, one year, two years, and three years old. Children below the age of three years were examined with the video Head Impulse Test (vHIT) of the horizontal semicircular canals (SCC), the cVEMP, and the rotatory test at 0.16, 0.04 and 0.01 Hz. At the age of three years old, the vHIT of the vertical SCC and ocular Vestibular Evoked Myogenic Potentials (oVEMP) were added.
Results: (1) In total, abnormal vestibular screening results were found in 14% (35/254) of the children, in which most had unilateral or bilateral severe to profound sensorineural hearing loss with various etiologies (e.g. syndromes, congenital cytomegalovirus (cCMV), meningitis and cochleovestibular anomalies). (2) The results of the extensive vestibular assessment showed that the cVEMP is an appropriate screening tool to detect vestibular deficits since a high feasibility (90%), sensitivity (75%), and specificity (98%) could be demonstrated. However, isolated SCC deficits were found in some children with cCMV and cochleovestibular anomalies.
Conclusions: Vestibular deficits were mainly found in children with unilateral or bilateral severe to profound hearing loss, in which the majority could be detected by means of the cVEMP screening. Since vestibular deficits in a few children with specific etiologies of hearing loss would remain unnoticed by only using the cVEMP, clinical guidelines were set to refine the vestibular screening.
5.- FP1114The Human Vestibulo-Ocular Reflex and Saccades in Peripheral Neuropathies
Stojan Peric, Milorad Vujnic, Ivo Bozovic, Bogdan Bjelica, Ivana Basta, Vidosava Rakocevic-Stojanovic, Miriam Welgampola
1Department of Neurophysiology, Liverpool Hospital, 2170, Australia; 2South Western Sydney Clinical School, University of New South Wales, Sydney, 2170, Australia; 3Ingham Institute for Applied Medical Research, Liverpool, 2170, Australia; 4Neurology Clinic, Clinical Centre of Serbia, Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 5Institute of Clinical Neurosciences, Royal Prince Alfred Hospital, Camperdown, 2006, Australia; 6Central Clinical School, Sydney Medical School, University of Sydney, Camperdown, 2006, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Aim: This study analyses the vestibulo-ocular reflex (VOR) as measured by the video-head impulse test (v-HIT) and refixation saccade characteristics in patients with genetically confirmed Charcot-Marie-Tooth disease 1A (CMT1A) and chronic inflammatory demyelinating polyneuropathy (CIDP).
Method: 22 patients (age 51.9±13.8 years, 17F/5M) with CMT1A with a mean disease duration of 25.2±17.5 years, mean MRC Sum Score of 47.4±6.8, mean Charcot-Marie-Tooth Examination Score (CMTES) score of 12.4±6.2 and 10 patients with CIDP (age 54.7±21.8 years, 5F/5M) mean disease duration of 4.2 years, mean MRC Sum Score of 51.9±5.5 were prospectively recruited from an Outpatient Neuromuscular Clinic, Clinical Centre of Serbia, Belgrade. Three-dimensional v-HIT was performed. VOR-gain, refixation saccade prevalence and first saccade amplitude, onset latency, peak velocity and duration were examined and compared against age-matched normal controls (NC).
Results: In CMT1A group, 18 (82%) patients reported severe imbalance resulting in recurrent falls in 14 (64%) patients, 6 (27.3%) patients reported history of vertigo/dizziness. VOR-gain was reduced (mean-2SD) in 10 (45%) patients, and was associated with longer disease duration and higher CMTES score. Refixation saccade prevalence for horizontal, anterior and posterior canal (HC, AC, PC) were 52%, 22%, 46% in CMT1A and 59%, 11% and 53% in NC. First saccade onset latency was longer in all three canals in CMT1A compared to NC (p<0.05). In the HC plane first saccade amplitude, peak velocity and duration were significantly different from NC (p<0.05).
In CIDP group, 6 (60%) patients reported severe imbalance resulting in recurrent falls in four patients, one patient reported past history of vertigo/dizziness. VOR-gain was reduced in five (50%) patients and was associated with history of recurrent falls (p<0.05). Refixation saccade prevalence for HC, AC, PC were 52%, 23%, 59% in CIDP and 60%, 24% and 54% in NC. First saccade onset latency was longer in the HC and PC plane (p<0.05).
Conclusion: Gait imbalance resulting in recurrent falls and reduction in the VOR-gain are common in patients with CMT1A and CIDP. Our findings indicate that gait imbalance in these conditions may be also linked to vestibular impairment. Prolonged onset latency of refixation saccades in both conditions suggest underlying demyelinating process of the vestibular nerve. Complementary otolith function testing is necessary to better characterise pattern of vestibular impairment and its correlation with v-HIT findings.
6.- FP1152Wireless magnetic scleral coil.
Lorenzo Bellizzi, Giuseppe Bevilacqua, Valerio Biancalana, Mario Carucci, Roberto Cecchi, Piero Chessa, Aniello Donniacuo, Marco Mandalà, Leonardo Stiaccini
University of Siena
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
We present the results obtained with an innovative eye-tracker based on magnetic dipole localization by means of an array of magnetoresistive sensors. The system tracks both head and eye movements with a high rate (100-200 Hz but can reach 1000 Hz) and in real time. The system consists of a head mounted googles where is mounted an array of magnetoresistive detectors and a a small size magnet (2 mm diameter, 0.5 mm width) inserted in a scleral contact lens. The present device has several advantages in respect to the available eye movements recording systems. The gold standard for high resolution eye tracking is the magnetic tracking with scleral search coils, based on Faraday s induction law but it is neither comfortable to wear for the patient nor portable. Furthermore, the device is very expensive. Our device overcomes all these limitations of currently available magnetic search coil. The described system can record torsional eye movements, a peculiarity shared with some implementations of the magnetic search coil technique and barely achievable with video-oculography. Apart from the need of using a contact lens, the proposed technique is neither invasive nor intrusive, and enables the construction of wearable devices more precise and cost-effective than other low-invasivity competing technologies (high-speed infrared cameras). In addition, the system enables simultaneous determination of environmental field and position-orientation of the dipolar source. Preliminary results obtained with the first prototype used in humans showed an error in localizing the magnetic field of the magnet inside the contact lens better than 0.1 degree precision, and a typical accuracy of 2 degrees, depending on the homogeneity of the environmental field. In conclusion, this newly developed wireless magnetic scleral coil seems to have all the advantages of traditional magnetic scleral coil devices associated with a non-invasive and all-day wearable device.
7.- FP1341Development of an Automated Triage Algorithm for Patients with Dizziness
Devin McCaslin1, Jeffrey Staab2, Scott Eggers4, Neil Shepard3, Santiago Romero-Brufau3, Kalyan Pasupathy5, James McPherson3, and Colin Driscoll3
1Department of Otolaryngology, University of Michigan, Ann Arbor, Michigan, USA; 2Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN USA; 3Department of Otorhinolaryngology – Head and Neck Surgery, Mayo Clinic, Rochester, MN USA; 4Department of Neurology, Mayo Clinic, Rochester, MN USA; 5Deparment of Biomedical and Health Information Sciences in the UIC College of Aplied Health Sciences, Chicago, IL
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Failures of care coordination and ineffective treatments waste more than US$175 billion in the USA alone. One of the most challenging problems is matching the right clinician to the right patient at the right time. Dizziness and vertigo exemplify this problem. Symptoms may be caused by illnesses that cross multiple medical specialties, requiring evaluations by well-coordinated teams of experts to achieve the best clinical outcomes. This study reviewed the first steps of a large project to automate and optimize scheduling of multi-disciplinary consultations for patients with dizziness at our center. Published efforts by other research groups to automate assessments of patients with vestibular symptoms focused on developing diagnostic aids. The goal of this project was different. Our purpose was to improve the care delivery process.
Methods: We developed a pre-visit self-report questionnaire to query patients about their vestibular complaints and associated medical and psychiatric symptoms. Experienced clinicians reviewed completed questionnaires and available medical records to establish itineraries for patients’ consultations with experts in otology, neurology, and psychiatry and audiometric and vestibular testing at our center. A panel of expert clinicians subsequently reviewed those evaluations and diagnostic outcomes for 98 patients to retrospectively create ideal appointment combinations that would best meet each patient’s needs, comparing them to actual schedules. We applied machine learning to these results to develop an automated triage process in which data from the pre-visit questionnaire were obtained directly from patients via a secure online platform and fed into an artificial intelligence algorithm to create itineraries. Our expert panel reviewed diagnostic outcomes of 73 subsequent patients who underwent multidisciplinary evaluations following schedules created by automated triage and compared them to ideal itineraries.
Results: Visits scheduled by our triage clinicians and ideal itineraries determined retrospectively by our expert panel showed fair to moderate agreement regarding the need for consultations in otology (concordance rate 68.9%, k=0.38), neurology (66.0%, k=0.34), and psychiatry (76.7%, k=0.49). Comparable results were obtained by our automated triage algorithm compared to ideal itineraries for consultations in otology (concordance rate 74.0%, k=0.44), neurology (61.6%, k=0.23), and psychiatry (72.6%, k=0.45).
Conclusions: Manual triage by clinicians was a time-consuming and costly process. Our first-generation automated triage algorithm achieved similar results using data obtained directly from the online pre-visit questionnaire. Thus, we achieved considerable efficiency in scheduling patients. Future advances in the triage algorithm will improve concordance with ideal itineraries and offer an opportunity to provide more cost-effective patient care.
8.- FP1394What is the Relevance of OVEMP Morphology?
Arthur Mallinson, Neil S. Longridge, Shannon Roseborough
Faculty of Medicine; University of British Columbia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Caloric testing measures only one parameter of vestibular function (difference in semicircular canal response). The utricular analogy to this is measurement of OVEMP amplitudes. The OVEMP stimulus (usually with a latency of about 7 microvolts) is a fragile response which is sometimes variable. Amplitude measurement prevents the detection of bilateral OVEMP pathology. Measurement of latencies increases the sensitivity of OVEMP assessment. Bilaterally absent OVEMPs in our lab are extremely rare.
Some OVEMPS are morphologically straightforward and are easily measured, even to the minimally trained diagnostician. But what If the OVEMP recording is a little more challenging to interpret? Our clinical concern is that many centres have given up relying on OVEMP assessment because the morphology of the averaged wave is poor, or because of a potential disagreement between two assessors. When collecting our normative data, (39 ears), 8 ears showed reasonable responses with respect to amplitude and latency measurements but were of poor morphology.
Our OVEMPs are carried out in a seated position with the head essentially fixed. The patient’s chin is placed on a sphygmomanometer cuff on a tray table while they elevate gaze 30 degrees, with the assessor preventing any neck extension by placing a hand at the back of the head.
As the OVEMP is a crucial aspect of diagnosis of the vestibular patient, we wished to investigate the clinical significance, if any, of a “poor morphology” OVEMP response.
Methods: We analyzed the OVEMP recordings of 60 patients sequentially referred to our tertiary care unit. Recordings were assessed by a single assessor and judged blindly (i.e. with no knowledge of the patient history, etc.) with respect to their morphological appearance, regardless of any amplitude or latency abnormality. Assessments were grouped as:
1. “easy to identify” (i.e. obvious to even a minimally trained assessor)
2. “difficult to identify” (i.e. latency landmarks not immediately obvious, and “needing a second look” from a second set of eyes).
The two groups were compared with respect to
a) Latency abnormality
b) Age
c) Sex
d) presence of trauma
e) Other diagnostic test abnormalities
We will be reporting on the results and discussing the clinical conclusions we have arrived at. We feel that this discussion is of extreme importance in order to further our understanding of what OVEMPs tell us in the patient with obvious otolith complaints.
9.- FP1270Novel diagnostic index test CATCH2 improves detection of acute vestibular stroke (EMVERT study)
Andreas Zwergal, Ken Möhwald, Hristo Hadzhikolev, Patricia Jaufenthaler, Eva Grill, Marianne Dieterich, Klaus Jahn
German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University, Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Patients with acute vertigo and dizziness account for about 4% of all visits in the emergency department (ED). Stroke is the underlying cause in 4-15% of these patients. About 10% of all vestibular strokes are missed at first contact. Therefore, improvement of the diagnostic algorithms is urgently needed.
Methods: 410 consecutive patients with acute vertigo, dizziness or imbalance were included in the prospective EMVERT (EMergency VERTigo) study in the ED of a tertiary referral center (University Hospital Munich). All patients underwent a structured history taking, clinical neurological exam and neurophysiological assessment (including videooculography, mobile posturography) in the ED. A cranial MRI was performed within 7 days to detect stroke. Post-hoc analysis identified factors, which had the highest accuracy to indicate vestibular stroke in the acute setting.
Results: A novel diagnostic index test – called CATCH2 – was composed, which included the following features: C – central clinical signs and symptoms (e.g. dysarthria, hemiataxia), A – age > 60 years, T –triggers absent, C – cover test with skew deviation, H – head impulse test normal, H – history of vertigo or dizziness absent. Each feature was weighted with 1 point, if present. For sum values of = 4 of 6 points, the AUC to detect vestibular stroke was 0.90, the sensitivity 91% and specificity 87%. CATCH2 thereby outperformed ABCD2 (sensitivity: 64%; specificity: 53%) and HINTS (sensitivity: 86%, specificity: 36%).
Conclusion: CATCH2 is a reliable and clinically feasible diagnostic index test to detect acute vestibular stroke in patients with different presentations of vertigo and dizziness (including those without spontaneous nystagmus).
OC10 1.- FP1312Evaluating Efficacy and Safety of Chronic Daily Stimulation with a Multichannel Cochleo-Vestibular Implant Prototype: The VertiGO! Trial
Bernd Vermorken1, Benjamin Volpe1, Stan van Boxel1, Elke Loos1,2, Nils Guinand3, Angélica Pérez Fornos3, Elke Devocht1, Raymond van de Berg1,4
1Department of Otorhinolaryngology and Head and Neck Surgery, Division of Balance Disorders, School for Mental Health and Neuroscience (MHENS), Maastricht University Medical Center, P. Debyelaan 25, 6229 HX Maastricht, The Netherlands; 2KU leuven, University of Leuven, Department of Neurosciences, Research Group ExpORL, Leuven, Belgium; & University of Hospitals Leuven, Department of Otorhinolaryngology-Head and Neck Surgery; 3Service of Otorhinolaryngology Head and Neck Surgery,Department of Clinical Neurosciences, Geneva UniversityHospitals, Geneva, Switzerland; 4Faculty of Physics, Tomsk State Research University, Tomsk, Russia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Bilateral vestibular function loss is an as-of-yet untreatable disorder causing severe impairment and discomfort. Since 2012 a combined multichannel vestibular implant (VI) and cochlear implant (CI) device, also known as the cochleovestibular implant (CVI), is clinically investigated by the Geneva-Maastricht group. This CVI aims to restore vestibular function in patients suffering from bilateral vestibulopathy (BV). Although recent studies showed that CVI stimulation enables compensatory eye, body and neck movements, the results so far were limited to stimulation in laboratory settings in case-by-base study designs. To create more general statements of responses in the BV population, the VertiGO! Trial presents an alternative clinical trial to investigate safety and efficacy of chronic daily stimulation of a multichannel CVI in a more rigorous trial setting.
Methods/ design: A randomized single-center single-blind cross-over controlled clinical trial is implemented, focusing on prolonged daily VI stimulation, including the efficacy of three different stimulation types (i.e. angular modulation vs. linear modulation vs. unmodulated baseline stimulation), the interaction between the CI and VI while simultaneously stimulated, and the general CVI device safety. Furthermore, this trial will serve as a proof-of-concept for a VI rehabilitation program. A total of eight participants suffering from BV and severe sensorineural hearing loss at the side of implantation will be included. After completion of the CI rehabilitation, the VI is fitted. One day of baseline testing is planned before three periods of four days of prolonged VI stimulation are scheduled. The efficacy of VI stimulation will be evaluated by collecting both fundamental (i.e. vestibulo-ocular/collar reflexes and perception) and functional (i.e. image stabilization and balance) outcome measures. Subjective outcome measures are included in the form of questionnaires and semi-structured interviews, to further build on the fundamental knowledge of vestibular organ stimulation while also taking into account the patient perspective. A five-year follow-up period will order to evaluate long-term CVI performance.
Results: From July 2021, participants are included in the VertiGO! Trial. From October 2021, CVI implantation surgeries are performed. Per- and postoperative implant telemetry and vestibulo-oculography images, showing well aligned electrically evoked eye movements, are collected. Together with a more detailed overview of the VertiGO! Trial protocol, these preliminary results will be presented.
Conclusion: The feasibility and safety of restoring vestibular function by making use of prolonged VI stimulation by a multichannel CVI prototype will be assessed by a new rigorous randomized cross-over controlled clinical trial: The VertiGO! Trial.
2.- FP0902Radiography-Guided Electrode Insertion During Vestibular Implantation
Joost J.A. Stultiens1, Alida A. Postma2, Nils Guinand3, Angélica Pérez Fornos3, Hermanus Kingma1, Raymond van de Berg1
1Department of Otorhinolaryngology & Head and Neck Surgery, School for Mental Health and Neuroscience, Faculty of Health Medicine and Life Sciences, Maastricht University Medical Center, Maastricht, The Netherlands; 2Department of Radiology and Nuclear Medicine, School for Mental Health and Neuroscience, Faculty of Health Medicine and Life Sciences, Maastricht University Medical Center, Maastricht, The Netherlands; 3Division of Otorhinolaryngology and Head-and-Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The vestibular implant aims to restore vestibular information in patients with bilateral vestibulopathy. Multiple studies have investigated the feasibility of a clinical device in the near future and results are promising. However, correct electrode placement remains a challenge. In the intralabyrinthine insertion technique, an electrode lead is inserted in each semicircular canal with the intent of placing the electrodes in the close vicinity of the ampullary nerve fibers to optimize stimulation. Fluoroscopy uses x-rays to provide moving images in real-time. Electromagnetic neuronavigation can be used to compare the live surgical situation with a preoperative CT-scan to identify anatomical structures. The aim of this study is to investigate these supportive imaging techniques to improve electrode placement.
Methods: For investigation of fluoroscopic-guidance, six ears of three human heads were sequentially implanted with electrodes in all three semicircular canals while visualizing insertion in real-time. A CT scan was performed immediately after each labyrinth’s implantation. Neuronavigation was utilized to implant additional cadaveric human heads. A fixed distance from fenestration to the center of the ampulla was used and the neuronavigation was used to guide the surgeon to the correct location for semicircular canal fenestration. For both techniques, on the unimplanted CT scan the center of the ampulla was determined, while the post-implantation CT scan was utilized to determine the tip of the electrodes. After fusing of CT images, distances from the electrode tips to the corresponding ampullae were calculated. A distance <1.5mm was deemed correct electrode placement. Differences with previous data from “blind” insertion (n=12 electrodes) were calculated.
Results: Fluoroscopy was able to identify the semicircular canal ampullae. Median distances to the target were 0.60mm, 0.85mm and 0.65mm for the superior, lateral and posterior semicircular canal, respectively. Overall, 17 of the 18 electrodes (94%) were implanted correctly. The mean distance was significantly lower compared to “blind” insertion (p=0.01). Neuronavigation was able to determine the location of fenestration to obtain correct electrode placement in 2/2 semicircular canals. Further results are still pending.
Conclusions: Fluoroscopy can provide live visual-feedback during electrode insertion and can consequently improve electrode placement. Neuronavigation might also be able to improve electrode insertion by determining the ideal location of semicircular canal fenestration in combination with a fixed electrode insertion depth.
3.- FP1185Fluoroscopy-guided Vestibular Implantation
Elke Loos1,2, Joost Sultiens2, Benjamin Volpe2, Bernd Vermorken2, Elke Devocht2, Christian Desloovere1, Nicolas Verhaert1, Raymond Van de Berg2
1KU Leuven, University of Leuven, Department of Neurosciences, Research Group ExpORL, Leuven, Belgium; & University Hospitals Leuven, Department of Otolaryngology, Head and Neck Surgery, Leuven, Belgium; 2Department of ENT/Audiology, School for Mental Health and Neuroscience (MHENS), Maastricht University Medical Center, Maastricht, The Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Research background: During the last decades, much research has been performed to develop an implantable vestibular prosthesis to artificially restore vestibular function. The first results of vestibular implantation in humans were very promising, but current surgical approaches still entail the challenge of correct electrode positioning. In the labyrinthine technique, it is preferred to only make a small fenestration in the semicircular canals because opening up the canals might induce hearing loss and loss of residual vestibular function. Therefore, this technique implies an almost blindly insertion of the electrodes, which led to suboptimal electrode positioning in the past. Fluoroscopy-guided electrode insertion could help surgeons to overcome this problem. Fluoroscopy is an imaging technique that captures moving images in real-time using x-rays. It has already been useful in cochlear implantation in cases of difficult cochlear anatomy and showed some promising results in vestibular implantation of cadaveric human heads, but up until now, it has never been used in vivo.
The aim of this study was to investigate a new operative technique for vestibular implantation using fluoroscopy-guided electrode insertion.
Methods: We performed vestibular implantation (cochleovestibular implant of the Geneva-Maastricht group, MED-EL Innsbruck, Austria) using fluoroscopy-guided electrode insertion in 2 patients. In each patient, at first the electrodes were blindly inserted to minimize radiation exposure. Afterwards, fluoroscopy was used to visualize and optimize electrode positioning aiming to reach the center of the ampulla. After electrode positioning, electrically evoked eye movements were recorded and a perioperative CT scan was performed. The results were analyzed using 3D slicer software, measuring the distance between the electrodes and the center of the ampullas. Additionally, these obtained distances were compared with previously reported mean distances from our formerly blindly inserted electrodes.
Results and Conclusion: Our preliminary results of this new technique for vestibular implant insertion will be presented. Next steps include more implanted subjects and a thorough comparison between electrode position and the functional outcome. We believe that fluoroscopy-guided vestibular implantation can overcome the lack of visibility during vestibular implant insertion, which could lead to better functional results.
4.- FP1215Effects of Vestibular Implant Stimulation on Gait during Cognitive Distraction and in Dim Lighting
Margaret R. Chow1, Celia Fernandez Brillet1, Kelly E. Lane2, Brian J. Morris1, Desi P. Schoo2, Yoav Gimmon2, Andrianna I. Ayiotis1, Carolina Treviño Guajardo2, Michael C. Schubert2, John P. Carey2, Charles C. Della Santina1,2
1Department of Biomedical Engineering; and 2Department of Otolaryngology–Head and Neck Surgery – both part of Johns Hopkins School of Medicine, Baltimore, Maryland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Individuals with bilateral vestibular hypofunction (BVH) experience visual instability and postural imbalance while walking and driving. Previously, Vestibular implants improved performance on posture and gait tests in a small cohort of individuals with vestibular hypofunction. However, standardized clinical tests of posture and gait function do not always capture all environmental factors relevant to real-world activities, such as walking in dimly lit conditions or while focused on a conversation. We examined effects of dim lighting and cognitive distraction on gait in adults with BVH before and after vestibular implantation.
Methods: Ten participants in the Multichannel Vestibular Implant Early Feasibility Study (NCT02725463) performed two clinical gait tests: walking 4m at their preferred pace and Timed Up and Go (TUG). Performance, measured as gait velocity or time to complete the task, respectively, was recorded 3-4 times in each condition. A GaitRite™ system measured gait patterns. For the 4m walk, participants were tested in three conditions: bright light without distraction, dim light without distraction, and dim light During Serial 7’s downward counting. TUG was completed in bright light and then repeated during Serial 7’s downward counting. The 4m walk and TUG assessment in bright light without distraction was done pre-operatively and repeated at participants’ most recent visits (2-55 months after implantation) with their vestibular implant providing electrical stimulation to the vestibular nerve in treatment mode (modulated by head motion) and placebo mode (constant pulse rate and amplitude). Within-participant change in performance across repeated trials from before implantation was compared for bright and dim lighting, distraction and no distraction, and between each vestibular implant stimulation mode. Cognitive costs were computed and compared across stimulation modes and distraction conditions.
Results: Relative to testing in bright light without distraction, dim lighting alone did not change gait performance. However, performance worsened during cognitive distraction. Vestibular implant stimulation in treatment mode improved performance in every test condition compared to placebo mode stimulation. Velocity, test completion time, stride time, swing time, and cognitive cost all indicated performance differences between treatment modes and between distraction conditions.
Conclusions: In individuals with bilateral vestibular hypofunction, motion-modulated artificial stimulation improves posture and gait performance during cognitive distraction compared to performance during non-modulated placebo stimulation. Testing gait performance with Serial 7’s distraction improves ability to detect effects of cognitive load on walking and effects of vestibular implant stimulation on ability to walk without focusing cognitive effort on avoiding a fall.
Support: NIH R01DC0013536, U01DC0019364
5.- FP1251Characterization of Intraoperative Electrically Evoked Compound Action Potentials of the Vestibular Nerve
Anissa Boutabla1, Joost Stultiens2, Samuel Cavuscens1, Maurizio Ranieri1, Herman Kingma2, Raymond van de Berg2, Nils Guinand1, and Angélica Pérez Fornos1
1Division of Otorhinolaryngology Head and Neck Surgery, Geneva University Hospitals and University of Geneva, Geneva, Switzerland; 2Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Maastricht, the Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Intraoperative protocols have to be further developed to optimize electrode positioning and monitoring electrically evoked vestibular responses during vestibular implantation surgery. Electrically evoked compound action potentials of the vestibular nerve (vECAPs) provide an objective electrophysiological measurement of the nerve response to electrical stimulation. The goal of this study was to demonstrate the feasibility of recording vECAPs in intralabyrinthine (stimulating and recording electrode in the same semicircular canal) and traslabyrinthine (stimulation electrode and recording electrode in different semicircular canals) configurations, to describe their morphology, and to compare their main characteristics.
Ten adult patients undergoing destructive labyrinthine surgery due to vestibular schwannoma participated in this approved study (ABR NL 54761.068.15; https://www.trialregister.nl/trial/6839) for which they gave written informed consent. The vestibular intraoperative prototype used in this experimental protocol was provided by MED-EL (Innsbruck, Austria). It is composed of 4 separate branches. The two outer branches comprise 3 independent active contacts. We compared the vECAPs measured in a classical intralabyrinthine configuration (stimulating and recording electrodes in the same semicircular canal ampulla) to vECAPs measured in a translabyrinthine configuration (stimulating electrode in one ampulla and stimulating electrode in another ampulla) and described their main characteristics (latencies, amplitude growth function). Due to the tight time and safety constraints during clinical surgery, Maestro software (v6, MED-EL, Innsbruck, Austria) was used for vECAPs recordings.
We were succesful in recording vECAP responses using both translabyrinthine and intra-labyrinthine configurations in 5 out of the 10 enrolled patients. A total of 180 vECAPs were initially identified, but only 26 valid vECAP were selected for further analysis after visual inspection. Within the selected vECAPs, 4 were recorded in intralabyrinthine configuration and 22 in translabyrinthine configuration. The amplitude of vECAPs responses increased monotonically with increasing current amplitudes, even though notable differences are observed across stimulation-recording pairs, both within and between semicircular canals. Finally, mean latencies for the first negative peak of both configurations showed comparable results to cochlear ECAPs recorded in humans (360-366 µs).
In conclusion, we demonstrated that vECAPs could be succesfully recorded in both tested configurations, but transabyrinthine configurations seemed more robust. vECAPs could potentially be a useful tool to optimize electrode positioning during vestibular implant surgery and could be integrated in the post-operative battery to monitor device function and improve fitting procedures. Their relevance in respect to clinical outcomes should still be determined.
6.- FP1289Chronic electrical stimulation of the otolith organ. Preliminary results in humans with bilateral vestibulopathy and sensorineural hearing loss.
Angel Ramos Macías1, Sharon Cushing2
1University of Las Palmas (Spain), 2The Hospital for Sick Children, University of Toronto (Canada)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Bilateral vestibulopathy is an important cause of imbalance that is misdiagnosed. The clinical management of patients with bilateral vestibular loss remains difficult as there is no clear evidence for an effective treatment. In this paper we try to analyze the effect of chronic electrical stimulation and adaptation to electrical stimulation of the vestibular system in humans when stimulating the otolith organ with a constant pulse train to mitigate imbalance due to bilateral vestibular dysfunction,
We have included 3 patients in our study with bilateral vestibular dysfunction according to Criteria Consensus of the Classification Committee of the Bárány Society. All cases were implanted by using a full-band straight electrode to stimulate the otoliths organs and simultaneously for the cochlear stimulation we use a perimodiolar electrode , with a follow up from 12 to 24 months.
In all cases Vestibular and clinical test (Video Head Impulse Test, Videonistagmography Vestibular Evoked Myogenic Potentials, cVEMP and oVEMP), Subjective vertical visual test, Computerized Dynamic Posturography, Dynamic Gait Index, Time UP and Go test and Dizziness Handicap Index) were performed. Posture and gait metrics reveal important improvement if compare with preoperartive situation. Oscillopsia, unsteadiness, independance and quality of life improved to almost normal situation.
7.- FP1338Modulating Vestibular Implant Stimulation Using Angular Head Velocity and Acceleration
Andrianna I. Ayiotis1, Margaret R. Chow1,2, Celia Fernandez Brillet1, Kelly E. Lane3, Desi P. Schoo3, John P. Carey3, Charles C. Della Santina1,2,3
1Johns Hopkins University Department of Biomedical Engineering; 2Labyrinth Devices; 3Johns Hopkins Department of Otolaryngology--Head and Neck Surgery
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The Multichannel Vestibular Implant Early Feasibility Study (NCT02725463) is a non-randomized, controlled clinical trial active since 2016 that is investigating vestibular implants as an intervention for people with bilateral vestibular hypofunction (BVH) who remain disabled despite standard-of-care vestibular rehabilitation. The implant delivers electrical pulses to branches of the vestibular nerve that innervate the semicircular canals, modulating stimulation using 3-dimensional head angular velocity measurements from a motion sensor magnetically coupled to the scalp over an implanted stimulator. Ten participants with severe, adult-onset BVH for >1 year, who had undergone >6 months of vestibular rehabilitation therapy, and had an intact vestibular nerve underwent unilateral implantation of the device and received motion-modulated vestibular stimulation 24hrs/day or during all waking hours since initial device activation, for durations ranging from 0.5-5 years.
Until recently, the system assigned stimulus pulse rate and pulse amplitude as functions of instantaneous angular velocity. This study investigated whether adding an angular acceleration term to the stimulation modulation paradigm of a vestibular implant, which effectively adds high-pass frequency dynamics to the stimulus encoding scheme, can improve video head impulse test (vHIT) responses and dynamic visual acuity (DVA). Head impulse testing of the implanted canals was used to measure vestibulo-ocular reflex (VOR) gain and latency relative to head motion. DVA was measured while subjects walked at 0.5-3 miles per hour (mph) on a treadmill. Eight subjects were assessed during three implant stimulation conditions: constant-rate/constant-amplitude stimulation (a placebo control), velocity modulation, and acceleration modulation. Averaged over all 24 implanted canals, vHIT gain was significantly greater during acceleration modulation compared to velocity modulation (mean±SD: 0.38±0.18, 0.24±0.17, p<0.001) and significantly greater compared to constant stimulation (0.38±0.18, 0.11±0.10, p<0.001). Average vHIT VOR latency was significantly better using acceleration modulation compared to velocity modulation (35±16, 55±25, p<0.001) and compared to constant stimulation (35±16, 67±30, p<0.001). Parametrized by slope of the decrement in visual acuity with increasing treadmill speed, DVA was significantly better during acceleration modulation (-0.09±0.04 logMAR/mph) compared to velocity modulation (-0.14±0.07, p=0.042) and compared to constant stimulation (-0.19±0.13, p=0.033).
Adding an angular head acceleration term (i.e., high-pass dynamics) to the modulation paradigm of a vestibular implant increased vHIT gain, decreased vHIT latency and increased visual acuity during treadmill walking.
Support: NIH R01DC013536, U01DC0019364; Labyrinth Devices LLC; MED-EL GmbH
8.- FP1346Optimization of Stimulating Electrode Array Design for a Vestibular Implant in Rhesus Macaque
Brian J. Morris1, Margaret R. Chow1, Abderrahmane Hedjoudje2, Dale Roberts2, Kathleen E. Cullen1,2,3, Roland Hessler4, Charles C. Della Santina1 2
1Biomedical Engineering; 2Otolaryngology – Head & Neck Surgery; 3Neuroscience, Johns Hopkins School of Medicine, Baltimore, MD, USA and 4Med-El GmbH, Innsbruck, Austria
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Prosthetic electrical stimulation targeting ampullary (semicircular canal) branches of the vestibular nerve can partially restore the 3-dimensional vestibulo-ocular reflex (3DVOR). However, current spread can limit activation of a targeted branch while instead exciting other branches, resulting in misaligned VOR responses. Computational modeling and archival animal data suggest (1) stimulating electrodes closer to the bone septum between the anterior and horizontal canal ampulla should more optimally couple stimulus currents to the ampullary nerves of those canals, and (2) deeper intra-ampullary electrode insertion (to near the crista) should yield better prosthetic responses, despite greater trauma to the membranous labyrinth.
To test these hypotheses, we quantified 3D VOR responses as functions of stimulating electrode position in two unilaterally-implanted rhesus monkeys (RhN and RhG). We implanted horizontal, anterior, and posterior ampullae with linear arrays of three stimulating electrodes (deep, outer-middle and shallow, 0.5 mm center-to-center). RhN also had inner-middle electrodes on the horizontal and anterior canal arrays. Return electrodes were in common crus (CC) or beneath temporalis muscle (distant). Stimuli were 200 pulse/s trains of 0-250µA cathodic-first, symmetric biphasic current pulses delivered with each animal head-fixed and alert in darkness. We recorded electrically-evoked 3DVOR responses using scleral coil oculography.
We calculated the ratio of VOR responses elicited by the outer-middle versus the inner-middle electrode for 50/75/100/125/150µA stimulus currents delivered using each of four return electrodes (one distant and 3 CC). Mean±SD outer-middle/inner-middle electrode 3DVOR magnitude and misalignment ratio across all current and return electrodes for the horizontal canal was 0.52±0.09 and 1.19±0.20, and 0.90±0.11 and 1.03±0.21 respectively for the anterior canal. For 5 of 6 implanted canals (all except RhG’s anterior), the deep stimulating electrode outperformed all other stimulating electrodes, maximizing VOR while minimizing misalignment. The distance from deepest to middle electrode was sufficient to significantly change performance.
Relative to the outer-middle electrode, a twofold improvement in VOR magnitude was achieved by the inner-middle electrode for the horizontal canal, while marginal benefit was seen with the anterior canal. However, the deepest electrode usually achieved the best performance. Therefore, if a vestibular/cochlear implant were constrained to only have one stimulating electrode per canal, that electrode should be at the tip of each shank to provide the best chance of achieving good performance. Multi-electrode ampullary arrays offer more chances to get at least one electrode in the optimal position. Enlarging single electrodes might also achieve that goal.
Support: NIH R01DC13536, R01DC009255, R01DC2390, F31DC019861; MED-EL GmbH
SY0041SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Michael Schubert PT, PhD, FAPTA |
| TOPIC DESCRIPTIVE TITLE: | Incremental VOR Adaptation; Clinical Trial Data |
| ACADEMIC / HOSPITAL AFFILIATION: | Professor, The Johns Hopkins University, Laboratory of Vestibular NeuroAdaptation, Department of Otolaryngology Head and Neck Surgery |
- SPEAKER 2
| NAME AND SURNAME: | Susan L Whitney DPT, PhD, NCS, ATC, FAPTA |
| TOPIC DESCRIPTIVE TITLE: | The use of gaming and eye and gaze feedback in vestibular rehabilitation |
| ACADEMIC / HOSPITAL AFFILIATION: | Professor, Department of Physical Therapy, University of Pittsburgh School of Health and Rehabilitation Science |
- SPEAKER 3
| NAME AND SURNAME: | Tzu-Pu Chang MD |
| TOPIC DESCRIPTIVE TITLE: | Vergence-mediated VOR Enhancement and Its Potential Application in Gaze Stabilization Exercise |
| ACADEMIC / HOSPITAL AFFILIATION: | Assistant Professor, Department of Neurology/Neuro-Medical Scientific CenterTaichung Tzu Chi Hospital, Tzu Chi University |
- SPEAKER 4
| NAME AND SURNAME: | Laurie King PhD PT, MCR |
| TOPIC DESCRIPTIVE TITLE: | Update on novel assessment and treatment for balance and gait deficits after mild traumatic brain injury |
| ACADEMIC / HOSPITAL AFFILIATION: | Professor of Neurology, Oregon Health & Sciences UniversityPortland OR |
The theme of this symposia is to review novel rehabiliation therapies for patients suffering symptoms of imbalance and dizziness due to vestibular hypofunction or traumatic brain injury. Expert clinician and seasoned researchers from the United States of America and Taiwan will discuss novel topics relating to rehabilitation methods for increasing gain of the vestibulo-ocular reflex (VOR), assessing and treating balance and gait deficits, and the increased use of gaming applications and virtual platforms. The target audience is for clinicians and researchers interested to learn cutting edge clinical and research applications designed to improve the rehabilitative care for those patients suffering symptoms related to vestibular pathology.
ABSTRACT 1
Incremental VOR adaptation (IVA) training is a technique that can increase the VOR gain to one or both sides via controlling visual target motion with respect to the head, so that the gain demand required to stabilize the target (and minimize the retinal image error) increases in small increments, thereby demanding a gradual increase in the subject’s actual VOR gain (eye/head velocity). The IVA technique in humans demonstrates significant increases of VOR gain with just 15 minutes of training. Clinical trial evidence of IVA training will be discussed as related to improved subjective and objective performance in patient with vestibular hypofunction.
ABSTRACT 2
The use of eye and gaze accuracy in the performance of vestibular eye exercises captured via a tablet will be discussed and demonstrated. Patient performance data of persons with vestibular disorders and a demonstration of virtual reality games developed for vestibular rehabilaiton will be provided. Physiotherapists were shown data from persons with vestibular disorders using the tablet device and asked to adjust the persons exercise program. Data from the physiotherapist decisions about exercise progression will be summarized.
ABSTRACT 3
When the eyes converge to view a near target, the vestibulo-ocular reflex (VOR) is enhanced reflexively in order to maintain gaze stability. This physiological phenomenon is called vergence-mediated VOR enhancement, and is supposed to derive from cerebellum which integrates the head velocity signals from irregular afferents and eye position signals. We are interested to know if this phenomenon is preserved in patients. We studied 22 patients with unilateral vestibular hypofunction during near- and far-viewing video head impulse testing. We found the vergence-mediated VOR enhancement is preserved during contralesional but impaired during ipsilesional head rotation, which results in greater retinal slip during head motion viewing near targets. Since retinal slip creates the error driving vestibular adaptation, a novel “convergence” gaze stabilization exercise may potentially enhance vestibular compensation, mediated by either physiologic vergence-mediated enhancement or greater erroneous signal (i.e. retinal slip). The related study of convergence gaze stabilization exercise is ongoing.
ABSTRACT 4
Little is known on the peripheral and central sensory contributions to persistent dizziness and imbalance following mild traumatic brain injury (mTBI). This talk will discuss our results that ongoing balance complaints in people with chronic mTBI are explained more by central sensory integration dysfunction rather than peripheral vestibular or oculomotor dysfunction.
OC11 1.- FP0897Internet-based vestibular rehabilitation with and without physiotherapeutic support for adults aged 50 years and older with a chronic vestibular syndrome in general practice: a three-armed randomised controlled trial
Vincent A. van Vugt1; Johannes C. van der Wouden1; Rosie Essery2; Lucy Yardley2; Jos W. R. Twisk3; Henriëtte E. van der Horst1; Otto R. Maarsingh1
1Department of general practice, Amsterdam UMC, Amsterdam Public Health, The Netherlands; 2Department of psychology, University of Southampton, Southampton, UK; 3Department of epidemiology and biostatistics, Amsterdam UMC, Amsterdam Public Health, The Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: To investigate the clinical effectiveness and safety of stand-alone and blended internet-based vestibular rehabilitation in the management of chronic vestibular syndromes in general practice.
Design Pragmatic, three-armed, parallel group, individually randomised controlled trial.
Setting: 59 general practices in The Netherlands.
Participants: 322 adults, aged 50 years and older, with a chronic vestibular syndrome.
Interventions: Stand-alone vestibular rehabilitation consisted of a six-week, internet-based intervention with weekly online sessions and daily exercises (10-20 minutes per day). In the blended vestibular rehabilitation group, the same internet-based intervention was supplemented by face-to-face physiotherapeutic support (home visits in week one and three). Participants in the usual care group received usual GP care without any restrictions.
Main outcome measures: The primary outcome was vestibular symptoms after six months as measured by the Vertigo Symptom Scale - Short Form (VSS-SF; range 0-60; clinically relevant difference =3 points). Secondary outcomes were impairment due to dizziness, anxiety, depressive symptoms, subjective improvement of vestibular symptoms after three and six months and adverse events.
Results: In the intention-to-treat analysis, stand-alone and blended vestibular rehabilitation participants had lower VSS-SF scores at six months than usual care participants (adjusted mean difference -4.1 points; 95% confidence interval -5.8 to -2.5; and -3.5 points; 95%-CI -5.1 to -1.9), respectively. Similar differences in VSS-SF scores were seen at three months follow-up. Participants in the stand-alone and blended vestibular rehabilitation groups also experienced less dizziness-related impairment, less anxiety, and more subjective improvement of vestibular symptoms at three and six months. No serious adverse events related to online vestibular rehabilitation occurred during the trial.
Conclusion: Stand-alone and blended internet-based vestibular rehabilitation are clinically effective and safe interventions to treat patients aged 50 years and older with a chronic vestibular syndrome. Online vestibular rehabilitation is an easily accessible form of treatment with the potential to improve care for an undertreated group of patients in general practice.
Trial registration: Netherlands Trial Register NTR5712
2.- FP1126100-fold increase of BETAHISTINE bioavailabality by the monoamine oxidase-B inhibitor SELEGILINE in humans – a phase I trial in 15 healthy volunteers
Michael Strupp1, Grant Churchill2, Ivonne Naumann1, Ulrich Mannsmann3, Amani Altawil3, Anastasia Golentsova1, Nicolina Goldschagg1
1Ludwig Maximilians University (LMU), Munich, Germany Dept. of Neurology and German Center for Vertigo and Balance Disorders; 2University of Oxford, UK, Dept of Pharmacology; 3LMU, Dept. of Medical Information Sciences, Biometry and Epidemiology
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To evaluate the effect of the monoamine oxidase B (MAO-B) inhibitor selegiline on betahistine serum concentration in humans.
Background: Betahistine was already registered in Europe in the 1970s, was approved in 80+ countries and there it is the first-line treatment for Menière’s disease. It has been administered to more than 150 million patients so far. According to Cochrane systematic reviews of betahistine and recent metaanalyses, there is, however, insufficient evidence to say whether betahistine has any effect in the currently approved dosages of up to 48 mg/d. Higher dosages and the combination with the MAO-B inhibitor selegiline are evidently effective.
Design/Methods: In a phase I trial, 15 healthy volunteers received three single dosages of betahistine (24, 48, and 96 mg in this sequence with at least 2 days washout period (> 10 half-life times of betahistine)) without and with Selegiline (5 mg per day with a loading period of 7 days). Betahistine serum concentrations were measured over a period of 240 min at 8 time points, including its measurement immediately before each dosage.
Results: In all three single betahistine dosages, selegiline increased the betahistine bioavailability about 100-fold (Figure). For instance the mean (+/-SD) of the area under curve for betahistine 48 mg alone was 0.64 (+/-0.47) h*ng/mL and for betahistine plus selegine 53.28 (+/-37.49) h*ng/mL. The half-life time of around 30 min was largely unaffected.
Figure.
Selegiline increases the oral bioavailability of betahistine in humans as demonstrated by plots of serum concentrations of betahistine over time. Betahistine was orally dosed at 24, 48 and 96 mg/person (labelled on graph as B24, B48 and B96) alone or in combination with 5 mg selegiline (labelled on graph as mean +/-SD). The total number of participants was 15 and each received all treatments.
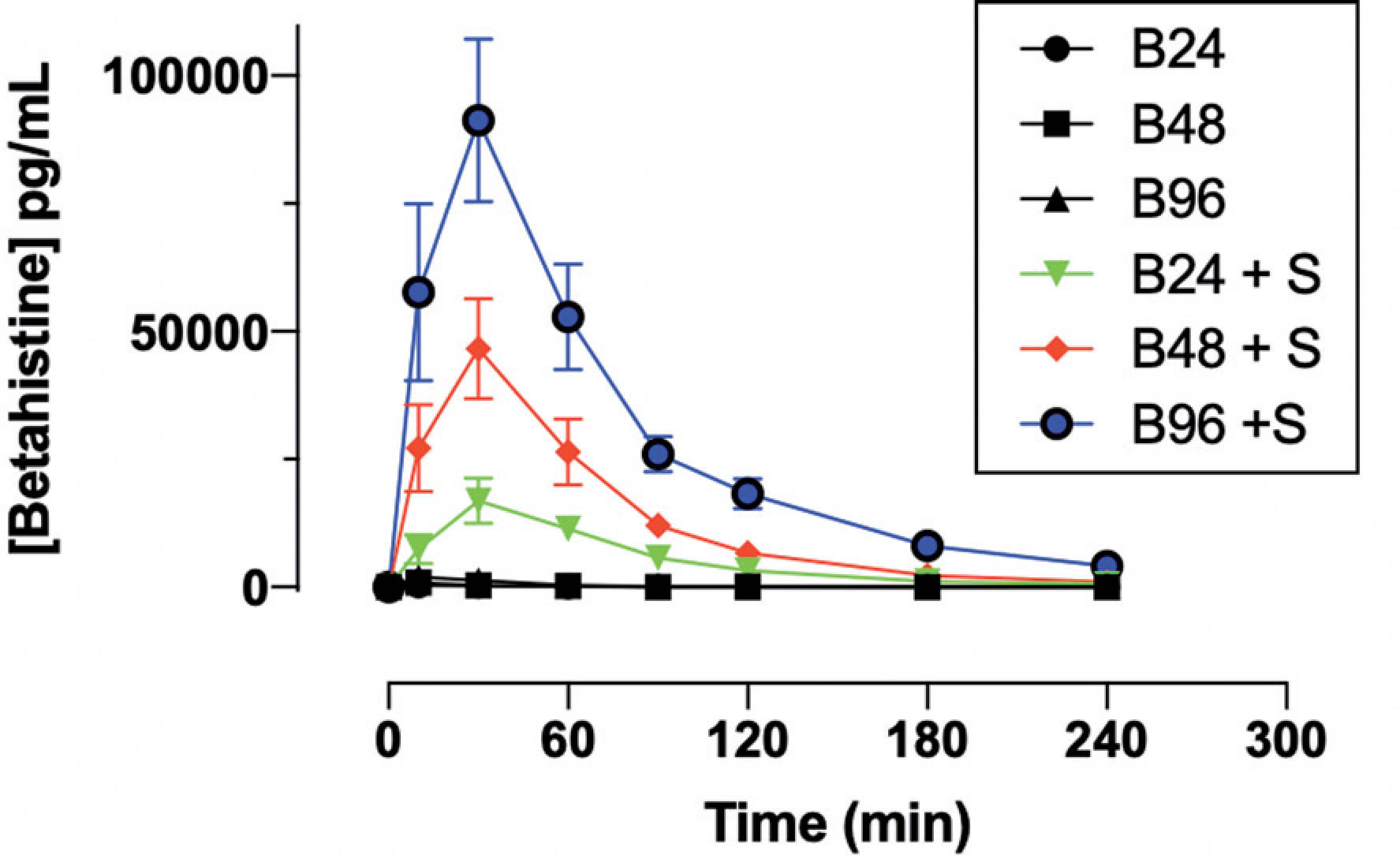
Conclusions: This phase I pharmacokinetic study in 15 healthy volunteers showed that the MAO-B inhibitor selegiline increases betahstine bioavailability by a factor of about 100. Based on these findings placebo-controlled trials with a combination therapy in, for instance, Menière’s disease, acute vestibular syndrome and post-repostioning otolith dizziness in BPPV are justified.
3.- FP1376BEtahistine for central VESTibular compensation in acute unilateral vestibulopathy/vestibular neuritis - The BETAVEST randomised placebo-controlled clinical trial
Michael Strupp1, Otmar Bayer1, Ulrich Mansmann2, Christine Adrion2
1Ludwig Maximilians University (LMU), Munich, Dept. of Neurology and German Center for Vertigo and Balance Disorders; 2LMU, Dept. of Medical Information Sciences, Biometry and Epidemiology (IBE)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
OBJECTIVE: To evaluate whether a 28-day symptomatic treatment with betahistine-dihydrochloride (144 mg/day) is superior to placebo in acute unilateral vestibulopathy (AUVP)/vestibular neuritis.
BACKGROUND: Betahistine-dihydrochloride registered in Europe in the 1970s is the first-line treatment for Menière’s disease with a currently approved dosage of up to 48 mg/day. To date, there is no randomised-controlled solid evidence to support the use of betahistine in the symptomatic treatment of patients with AUVP.
DESIGN/METHODS: This investigator-initiated, multicentre, double-blind, randomised, placebo-controlled, 2-arm, parallel-group, phase II/III superiority trial over two months (maximum of 28 day treatment period plus a subsequent 1-month follow-up) was designed to be conducted at tertiary neurology or ENT referral centres of six German university hospitals. The planned sample size was a total of 210 patients to be allocated. Adults =18 years with a history of acute/sub-acute onset of severe prolonged spining vertigo, nausea, postural imbalance, and a clinically confirmed diagnosis of AUPV were randomly assigned 1:1 to treatment with betahistine-dihydrochloride (BE), 3×48 mg per day, or a matched placebo. The two pre-specified primary efficacy outcomes were the total sway path (TSP), in length per time [m/min], on a compliant foam-padded posturography platform for postural control with test condition ‘eyes closed’, and peak slow phase velocity (PSPV) [°/second] of the spontaneous nystagmus (SPN). In each case, assessments at day 10 (medium-term) and day 3 (short-term efficacy) after randomisation resulted in two 2-dimensional primary efficacy endpoints. Secondary outcomes included time to self-reported recovery from acute symptoms due to AUPV, the Dizziness Handicap Inventory (DHI) patient questionnaire and clinical assessments. Adverse events were reported throughout the whole 8-week observation period.
RESULTS: After randomising 144 patients (BE: 68 patients; placebo: 73 patients) between 12/2010 and 04/2016, BETAVEST was terminated because of slower-than-expected recruitment and funding discontinuation. On a 2.5% significance level, no significant treatment differences were found at day 10 and at day 3 concerning mean TSP and PSPV values of the SPN. Regarding TSP, no difference for postural instability was found on BE compared to placebo treatment (day 10: risk for instability reduced by 1.50% on BE vs. on placebo (p=0.53); day 3: reduced by 9.00%, p=0.06). Besides, there was no treatment benefit with respect to the patient-oriented endpoint “time to subjective recovery” (hazard ratio 0.95 (95% CI 0.64 to 1.42; p=0.80) on BE vs on placebo.
CONCLUSIONS: Use of oral betahistine in a dosage of 3x48 mg per day did not prove to be more effective than placebo for the acute treatment of AUVP. Investigational and placebo treatment were approximately equally safe and well tolerated with no unexpected safety findings.
4.- FP1279Comparison of Incremental Vestibulo-ocular Reflex Adaptation Training Versus x1 Training in Patients With Chronic Peripheral Vestibular Hypofunction: A Two-Year Randomized Controlled Trial
Carlo N Rinaudo1,2, Michael C Schubert3,4, William V C Figtree1,2, Chris J Todd1,2, Phillip D Cremer1,5, Americo A Migliaccio1,2,5,6,7
1Balance and Vision Laboratory, Neuroscience Research Australia, Cnr Barker Street & Easy Street, Randwick, NSW, 2031, Australia; 2University of New South Wales, Sydney, NSW, 2033, Australia; 3Laboratory of Vestibular NeuroAdaptation, Department of Otolaryngology - Head and Neck Surgery, Johns Hopkins University, Baltimore, MD, 21205, USA; 4Department of Physical Medicine and Rehabilitation, Johns Hopkins University, Baltimore, MD, 21205, USA; 5Royal North Shore Hospital, Sydney, Australia; 6Department of Otolaryngology - Head and Neck Surgery, Johns Hopkins University, Baltimore, MD, 21205, USA. ; 7School of Biomedical Sciences and Pharmacy, University of Newcastle, Newcastle, Australia. .
• ELIGIBLE FOR THE WON-SANG LEE AWARD?
No
Target audience is vestibular rehabilitation practitioners
Background and purpose: A crossover, double-blinded randomized controlled trial to investigate once-daily incremental vestibulo-ocular reflex (VOR) adaptation (IVA) training over 2 years in people with stable and chronic peripheral vestibular hypofunction.
Methods: Twenty-one patients with peripheral vestibular hypofunction were randomly assigned to intervention-then-control (n = 12) or control-then-intervention (n = 9) groups. The task consisted of either x1 (control) or IVA training, once daily every day for 15 minutes over 6-months, followed by a 6-month washout, then repeated for arm 2 of the crossover. Primary outcome: vestibulo-ocular reflex gain. Secondary outcomes: compensatory saccades, dynamic visual acuity, static balance, gait, and subjective symptoms. Multiple imputation was used for missing data. Between-group differences were analyzed using a linear mixed model with repeated measures.
Results: On average patients trained once daily 4 days per week. IVA training resulted in significantly larger VOR gain increase (active: 20.6% ± 12.08%, P = 0.006; passive: 30.6% ± 25.45%, P = 0.016) compared with x1 training (active: -2.4% ± 12.88%, P = 0.99; passive: -0.6% ± 15.31%, P = 0.68) (P < 0.001). The increased IVA gain did not significantly reduce with approximately 27% persisting over the washout period. x1 training resulted in greater reduction of compensatory saccade latency (P = 0.04) and increase in amplitude (P = 0.02) compared with IVA training. There was no difference between groups in gait and balance measures; however, only the IVA group had improved total Dizziness Handicap Inventory (P = 0.006).
Discussion and conclusions: Our results suggest IVA improves VOR gain and reduces perception of disability more than conventional x1 training. We suggest at least 4 weeks of once-daily 4 days-per-week IVA training should be part of a comprehensive vestibular rehabilitation program
5.- FP1303A Randomized Controlled Trial of Rizatriptan versus Placebo for Treating Vestibular Symptoms, Headache, and Associated Symptoms during Attacks of Vestibular Migraine
Jeffrey P. Staab1,2, Scott D. Z. Eggers3, Joanna Jen4, Allison M. LeMahieu5, Jennifer R. Geske5, Honghu Liu6, Deanna R. Hofschulte1, G. Roxana Gonzalez7, Brian A. Neff2, Neil T. Shepard2, Devin L. McCaslin8, Robert W. Baloh7
1Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN USA; 2Department of Otorhinolaryngology – Head and Neck Surgery, Mayo Clinic, Rochester, MN USA; 3Department of Neurology, Mayo Clinic, Rochester, MN USA; 4Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY USA; 5Department of Quantitative Health Sciences, Mayo Clinic, Rochester, MN USA; 6Section of Public Health and Community Dentistry, School of Dentistry, University of California, Los Angeles, CA USA; 7Department of Neurology, University of California, Los Angeles, CA USA; 8Department of Otolaryngology – Head and Neck Surgery, University of Michigan, Ann Arbor, MI USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Vestibular migraine produces attacks of vestibular and headache symptoms. This double-blind, placebo-controlled, randomized trial tested the efficacy of rizatriptan for aborting vestibular symptoms, headache, and associated symptoms of vestibular migraine attacks.
Methods: 1364 adults aged 18-65 years with vestibular symptoms and headache were screened for possible entry into this trial between August 2014 and January 2020; 842 were ineligible, mostly due to diagnoses other than vestibular migraine; 300 declined to enroll. Two hundred twenty-two patients (71.2% women, 71.1% Caucasian white) who met International Classification of Vestibular Disorders criteria for vestibular migraine provided informed consent to participate. They were observed prospectively to verify the diagnosis and ensure adequate illness activity; 134 had 2+ verified vestibular migraine attacks within 12 months of enrollment. They were randomized 2:1 to treat up to three subsequent attacks with rizatriptan 10 mg or placebo orally. Primary outcomes were proportions of attacks with vertigo or unsteadiness/dizziness reduced from moderate/severe to absent/mild one hour after participants took study drug. Secondary outcomes were resolution of vestibular symptoms at one hour; need for additional medication after one hour; absent/mild vestibular symptoms, headache, photophobia/phonophobia, nausea/vomiting, and motion sensitivity at 24 hours; treatment satisfaction and well-being at 48 hours; and rates of serious adverse effects.
Results: Participants treated 307 attacks. Primary outcomes were evaluated in 240 attacks with moderate/severe pre-treatment vestibular symptoms. Rizatriptan did not differ from placebo in reducing vertigo [73/151 (48.3%) vs. 50/88 (56.8%) attacks, p=0.331] or unsteadiness/dizziness [29/151 (19.2%) vs. 11/89 (12.4%) attacks, p=0.184] at one hour. Rizatriptan was superior to placebo for unsteadiness/dizziness [90/109 (82.6%) vs. 41/62 (66.1%) attacks, p=0.041] and motion sensitivity [95/109 (87.2%) vs. 42/62 (67.7%) attacks, p=0.006] at 24 hours and treatment satisfaction [regression estimate 10.44, 95% CI (0.65, 20.23), p=0.035] and physical well-being [regression estimate 4.65, 95% CI (1.16, 8.13), p=0.009] at 48 hours. Rates of supplemental medication use (26.4%) were the same in both groups. No participants experienced serious adverse effects.
Post-hoc analyses examined the incongruity between negative primary outcomes and positive treatment satisfaction. These analyses of all treated attacks included ‘real world’ situations of drug administration errors (N=7), treatment of attacks with mild symptoms (N=60) and use of supplemental medications (N=80) that had been excluded from a priori analyses. They found rizatriptan efficacious for unsteadiness/dizziness, headache, photophobia/phonophobia, and motion sensitivity at 24 hours.
Conclusions: Rizatriptan did not reduce vertigo but improved other symptoms of vestibular migraine attacks 24 hours after treatment.
6.- FP1447Expert Diagnosis by Video-oculography is More Accurate than In-Person ED Diagnosis in Acute Dizziness—Preliminary Results of the AVERT Trial
Shervin Badihian1,2, David S. Zee1, Adriana Batazzi2, Ari M. Blitz, John P. Carey4, Tracey Economas2, Jonathan A. Edlow5, Joshua N. Goldstein6, Joshua Gruber2, Meghan Hildreth2, Michael Iacobelli2, Joanna C. Jen7, Jorge C. Kattah8, Kevin A. Kerber9, Doris D. M. Lin10, Nichol McBee2, William J. Meurer11; Rodney Omron12, Noeleen Ostapkovich2, Karen Lane2, Susan M. Peterson12, Richard E. Rothman12, Ali S. Saber Tehrani1, Ying Wang2, Zheyu Wang13, Daniel F. Hanley2, David E. Newman-Toker1,2
1Department of Neurology; Johns Hopkins University School of Medicine; 2Department of Neurology, Divison of Brain Injury Outcomes, Johns Hopkins University School of Medicine; 3Department of Radiology, Case Western Reserve University School of Medicine; 4Department of Otolaryngology–Head and Neck Surgery, Johns Hopkins University School of Medicine; 5Beth Israel Deaconess Medical Center, Harvard Medical School; 6Department of Emergency Medicine, Massachusetts General Hospital; 7Departments of Neurology, Otolaryngology, NeurosurgeryIcahn School of Medicine at Mount Sinai; 8University of Illinois College of Medicine at Peoria, Illinois Neurological Institute; 9Department of Neurology, University of Michigan Medical School; 10Department of Radiology, Johns Hopkins University School of Medicine; 11Departments of Emergency Medicine and Neurology - University of Michigan; 12Department of Emergency Medicine, Johns Hopkins University School of Medicine; 13Departments of Biostatistics, The Johns Hopkins Bloomberg School of Public Health
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Introduction: Diagnosis of dizziness/vertigo is challenging for many emergency department (ED) clinicians. Video-oculography (VOG) is routinely used in specialty clinics but not in EDs. In the context of a multicenter diagnostic strategy trial, we compared the diagnostic accuracy of ED clinician to expert diagnosis using VOG and a clinical summary in dizziness/vertigo visits.
Methods: From 2/6/2018 to 3/9/2020, The AVERT trial (NCT02483429) was performed at six tertiary-care EDs and designed to compare VOG-enhanced diagnostic decision support with standard care. We recruited adult patients with dizziness. Potentially-eligible patients completed a survey about the history of present illness (HPI), past medical history (PMH), and underwent structured tests including VOG (ICS Impulse, Schaumberg, IL, USA) and standardized neurologic exam scales administered by a trained research coordinator or vestibular nurse. VOG-testing included tests for spontaneous/gaze/positional nystagmus, horizontal head-impulse vestibulo-ocular-reflex, and skew deviation.
Gold standard diagnoses were made by a multi-disciplinary panel using ED charts plus a 1-week oto-neurologist evaluation, repeat VOG and MRI, and one-month follow-up. Diagnoses were grouped according to prespecified schemas of varying granularity. The ED provider diagnosis was the primary listed diagnosis in the treating provider’s final clinical note. Expert ED index diagnoses were selected from a 12-category scheme by a single oto-neurologist (who subsequently participated in the gold standard panel classification) after reviewing only the ED visit VOG and a summary of the HPI/PMH .
Results: we enrolled 130 patients (52.3% female; 76.9% white, non-Hispanic) with a mean age of 59.2±15 years. Diagnostic accuracy for the oto-neurologist using VOG alone was higher than the ED primary diagnosis with greater differences noted for more granular diagnoses (12-category schema: 50.9% vs 21.8%,p<0.001), Table). In the subset of patients with a gold standard diagnosis of benign-paroxysmal-positional-vertigo (BPPV) or vestibular neuritis (VN), the difference in diagnostic accuracy were as follows: BPPV, (70.5% vs. 13.6%, (p<0.001); VN (79.2% vs. 37.5%,p=0.021). Difference in stroke diagnosis was 21.4% vs 50%% (p=0.219).
Table:
ED index visit diagnostic accuracy for ED clinical team vs. vestibular specialist using only VOG
| Final Diagnosis after Follow-up, Adjudicated by Multidisciplinary Panel | ED Clinical, % (95% CI) | Oto-neurologist Using VOG-only, % (95% CI) | Relative Change in Diagnostic Accuracy | p-value (McNemar’s test) |
| All Causes (n=110*) | ||||
| 3-Category† Schema (n=110) | 35.5% (26.6-45.1) | 69.1% (59.6-77.6) | ↑ 95% | <0.001 |
| 6-Category‡ Schema (n=110) | 24.5% (16.8-33.7) | 52.7% (43.0-62.3) | ↑ 115% | <0.001 |
| 12-Category£ Schema (n=110) | 21.8% (14.5-30.7) | 50.9% (41.2-60.6) | ↑ 133% | <0.001 |
| Subset with Most Common Inner Ear Diseases (n=68) | ||||
| BPPV (n=44) | 13.6% (5.2-27.4) | 70.5% (54.8-83.2) | ↑ 418% | <0.001 |
| Vestibular neuritis (n=24) | 37.5% (18.8-59.4) | 79.2% (57.8-92.2) | ↑ 111% | 0.021 |
| Cerebrovascular (n=14) | 50.0% (23.0-77.0) | 21.4% (4.7-50.8) | ↓ 57% | 0.219 |
* Randomized cases with an unknown final diagnosis despite follow-up (n=20) are excluded from this analysis.
† 3-Category Schema: central, peripheral, or other/unknown.
‡ 6-Category Schema: posterior canal BPPV, vestibular neuritis, central, non-neurovestibular, or unknown.
£ 12-Category Schema: posterior canal BPPV, vestibular neuritis, horizontal canal BPPV, other BPPV, Meniere’s disease, vestibular migraine, peripheral other, thiamine deficiency, cerebrovascular, central other, non-neuovestibular, or unknown.
Conclusion: Our findings show that a remote VOG evaluation from oto-neurologists in ED dizziness/vertigo presentations could substantially improve diagnostic accuracy, particularly for BPPV and VN. These results suggest that two common causes of dizziness/vertigo can be almost correctly diagnosed with VOG technology without need for further testing. The study was not able to determine if ED provider diagnosis would improve if they selected diagnoses using the 12-category diagnosis scheme. The design was limited by the single oto-neurologist scoring the VOG-based diagnosis and contributing to the gold standard determination.
SY0028SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Dr. Bryan K. Ward |
| TOPIC DESCRIPTIVE TITLE: | Magnetic vestibular stimulation (MVS) - physiology and mechanistic underpinning |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Otorhinolaryngology, Johns Hopkins School of Medicine, Baltimore, MD, USA |
- SPEAKER 2
| NAME AND SURNAME: | Dr. Aasef G. Shaikh |
| TOPIC DESCRIPTIVE TITLE: | Deep brain stimulation (DBS) of the central vestibular system |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Neurology, Case Western Reserve University, Cleveland, OH, USA |
- SPEAKER 3
| NAME AND SURNAME: | Dr. Alexander Andrea Tarnutzer |
| TOPIC DESCRIPTIVE TITLE: | MVS and DBS in clinical neurotology - are we there yet? |
| ACADEMIC / HOSPITAL AFFILIATION: | Neurology, Cantonal Hospital of Baden, Baden, Switzerland |
- SPEAKER 4
| NAME AND SURNAME: | Click here to write |
| TOPIC DESCRIPTIVE TITLE: | Click here to write |
| ACADEMIC / HOSPITAL AFFILIATION: | Click here to write |
Advances in neurotechnologies has offered a new dynamic picture of the brain revolutionizing our understanding of complex neural circuits and has enabled us to seek for new ways to treat disorders of human brain. In vestibular system the artificial stimulation of inner ear endorgans, the vestibular prosthesis, and magnetic or electrical non-invasive modulation of the cerebellum or cortex (i.e., transcranial magnetic and direct current stimulation) had provided evidence to experimentally and clinically change the way our brain manages the sensation of self-motion. Recently two serendipitous observations informed us that it is possible to modulate peripheral and central vestibular system in a completely different way. One is called magnetic vestibular stimulation (MVS), while the other is deep brain stimulation (DBS). Proof of principle underlying MVS comes from the fact that individuals working next to strong static magnetic fields occasionally feel disoriented. Theoretically, magnetic field interacts with naturally occurring ionic current flowing through the inner ear resulting in the Lorentz force displacing the endolymph generating sensation of constant acceleration rotation. Dr.Ward will discuss physiology and physics underlying MVS. We learnt that Parkinson patients undergoing DBS for surgical treatment of their motor symptoms often feel electric stimulation dependent vertigo. This serendipitous finding led to novel discovery that DBS in the dorsal aspect of subthalamus modulates central vestibular pathways that carry motion perception information via influencing the cerebellar outflow, indirectly via subthalamo-cerebellar projections and directly via modulating cerebello-thalamic fibers (that are in proximity to the subthalamus). Dr.Shaikh will discuss physiology, psychophysics, neuroimaging, and computational modeling data explaining the mechanistic underpinning of DBS influencing the central vestibular system. The application of MVS and DBS in treatment of vertigo and dizziness is still far from clinical practice. Dr.Tarnutzer will provide clinician’s perspective on application these novel modality in dizzy patients.
ABSTRACT 1
Mammals experience vertigo and nystagmus in strong MRI machines. The effect is believed to be the result of a Lorentz force generated by interactions of the normal vestibular ion currents and the strong magnetic field of the MRI machine, and pressing on the semicircular canal cupulae. This magnetic vestibular stimulation (MVS) constantly displaces the semicircular canal cupulae, delivering a force similar to constant acceleration, while a human lies comfortably in an MRI machine. The nystagmus partially adapts in the MRI, and upon exiting the MRI, an after effect emerges in which the nystagmus reverses direction. By measuring how the nystagmus adapts during MVS, we can learn how the brain adapts to a new set-point. Dr. Bryan Ward will discuss the mechanism of MVS, what we have learned about vestibular set-point adaptation, and the advantages and disadvantages of using MVS as a tool for studying the vestibular system.
ABSTRACT 2
Deep brain stimulation (DBS) is a state-of-art treatment of debilitating movement disorders such as Parkinson’s disease. While optimizing subthalamic nucleus DBS for the treatment of Parkinson we observed that subject experienced stimulation dependent vertigo. This findings resulted in multi-displinary research examining the effects of subthalamic deep brain stimulation on human motion perception on variety of subtypes of Parkinson patients who already had DBS implant. Over last five years, in experiments using pure vestibular heading perception, pure visual heading perception, and visual scanning behavior combined with patient-specific DBS volume of tissue activation models, we discovered a fundamental role of specific subthalamic nucleus region and cerebellar-thalamic projection when the subthaalmic DBS modulates motion perception. This novel results are not only critical to better treat disroders of balance and falls in Parkionson’s disease, but also provide important insights for future treatments of mysterious central vestibular disroders presenting with intractable perception of vertigo.
ABSTRACT 3
Neuromodulation offers unique adjustable way to control signal transduction through the nervous system. While standard-of-care for some neurological indications, neuromodulation strategy is in infancy for clinical application or confined to research laboratories. Vestibular system is one of such examples. In last one decade a novel way to modulate the vestibular labyrinth, magnetic vestibular system, was identified. Several years later it was discovered that deep brain stimulation can also modulate vestibular perception. While these novel interventions are already tested in humans, their stand-alone application for the treatment of perceptual balance dysfunction needs more evidence before used for primary application in clinical neurotology. We will discuss which human disorders could be ideal responders for the magnetic vestibular stimulation and which ones would respond better to the deep brain stimulation. We will discuss various (speculated) pathways to reach the ultimate goal of its application for the treatment of disorders affecting the vestibular system.
ABSTRACT 4
Click here to write.
OC12 1.- FP0931Horizontal Vestibulo–Ocular Reflex deficit as a biomarker for disease onset, severity, and progression of Spinocerebellar Ataxia type 3
Carlos R. Gordon1,2,3, Dario Geisinger2, Zohar Elyoseph4, Roy Zaltzman1,2 and Matti Mintz3,4,5
1Department of Neurology, Meir Medical Center; 2Sackler Faculty of Medicine, 3Sagol School of Neuroscience, 4School of Psychological Sciences, Tel Aviv University, Tel Aviv; 5Academic College Ashkelon; Israel
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Spinocerebellar Ataxia type 3 (SCA3), also known as Machado-Joseph Disease, is an autosomal dominant neurodegenerative disease caused by the expansion of CAG trinucleotide repeats in the ATXN3 gene. The search for a biomarker that would identify the disease presence and progression is crucial for designing clinical trials in SCA3. In previous studies we have demonstrated that the horizontal Vestibulo-Ocular Reflex (VOR) deficit is part of the SCA3 phenotype. Nowadays, the VOR gain (eye velocity/head velocity) can be easily and accurately quantified using the video Head Impulse Test (vHIT), in which fast camera records eye movement responses to abrupt head rotations.
Objective: To evaluate the VOR gain as a neurophysiological biomarker of SCA3.
Methods: Participants were 35 SCA3 patients, 11 pre-symptomatic (PS) SCA3 subjects (genetically confirmed but without symptoms or signs) and 20 healthy controls (HC). Following a detailed neurological examination, ataxia severity was assessed by the Scale for the Assessment and Rating of Ataxia (SARA) and vestibular function was evaluated using the vHIT measuring the horizontal and vertical VOR gain. Twenty of the SCA3 patients were re-tested after a period of 1-3 years.
Results: The horizontal VOR gain was significantly lower among SCA3 as compared to PS and HC ]0.53, 0.86 and 0.94 respectively]. Six out of the 11 PS subjects demonstrated mild abnormal horizontal VOR gain (>0.8). SCA3 patients showed a significant negative correlation between the horizontal VOR gain and the SARA score in the two tests separated by an interval of 1-3 years. Multiple regression analysis found that horizontal VOR gain, and disease duration are significant independent predictors of SARA score. The negative correlation between the percentage of change in horizontal VOR gain and the percentage of change in SARA score across the two tests indicates that the VOR gain could be used as a biomarker for disease progression.
Conclusions: The present findings confirm that horizontal VOR gain impairment may serve as a neurophysiological biomarker for detecting the onset, severity, and progression of SCA3.
Target Audience: Vestibular researchers, Ataxia researchers, Neurologists
2.- FP1018Assessment of vestibulo-ocular reflex in spinocerebellar ataxia with video head impulse test
Jae-Myung Kim, Shina Kim, Hyeon-Joong Park, You-Ri Kang, Kyung Wook Kang, Tai-Seung Nam, Seong-Min Choi, Seung-Han Lee
Department of Neurology, Chonnam National University Hospital and Chonnam National University Medical School
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Spinocerebellar ataxia (SCA) is a heterogenous, inherited ataxia characterized by progressive ataxia associated with degeneration of cerebellum and their connections. Since SCA is a genetically confirmed disorder and share the clinical manifestations considerably among subtypes, discriminating subtype in SCA could be challenging. There have been several studies regarding vestibuo-ocular reflex (VOR) impairments in SCA but, scant data concerning analysis of VOR function using video head impulse test (vHIT) according to the SCA subtypes. We aimed to evaluate VOR in SCA patients with vHIT device and to determine whether the pattern of VOR impairments can be a differentiating factor of SCA subtypes.
Methods: A total of 30 genetically confirmed SCA patients (SCA2=7, SCA3=4, SCA6=10, SCA7=9) were enrolled. Clinical characteristics, neurological and neuro-otological evaluations were performed. To investigate VOR, the vHIT (ICS Impulse; Otometrics, Taastrup, Denmark) was checked in all patients. Normative data obtained from 40 age-matched healthy control were compared to those from each SCA subgroups.
Results: In all 30 SCA patients, men were 16, and mean age was 42.3 (range: 17-67). Spontaneous nystagmus was documented in only SCA6 (80%) and gaze-evoked nystagmus was showed in SCA3 (75%) and SCA 6 (90%). On the other hands, saccadic slowing was documented in majority of SCA2 (71.4%) and SCA7 (66.7%) but absent in SCA6. Smooth pursuit abnormalities were documented in most of the patients regardless of subtypes. Compared to normal control, the VOR gains were spared in SCA2, but globally decreased in SCA3 (HCs, median=0.58, IQR=0.49-0.69 vs. median=1.04, IQR=0.93-1.11, p<0.001; ACs, median=0.56, IQR=0.47-0.70 vs. median=0.95, IQR=0.87-1.01, p<0.001; PCs, median=0.57, IQR=0.52-0.60 vs. median=0.905, IQR=0.83-0.96, p<0.001). SCA6 showed posterior canal-dominant gain impairments (median=0.68, IQR=0.51-0.83 vs. median=0.91, IQR=0.83-0.96, p<0.001), but SCA7 exhibited impaired gains in both anterior and posterior canals with anterior canal predominancy (ACs, median=0.54, IQR=0.44-0.73 vs. median=0.95, IQR=0.87-1.01, p<0.001; PCs, median=0.78, IQR=0.59-0.88 vs. median=0.905, IQR=0.83-0.96, p<0.001). The gains for the horizontal canals in SCA6 and the vertical canals in SCA7 were negatively correlated with disease severity.
Conclusions: VOR impairments are common in SCA, but their patterns were various according to the subtypes. Distinctive VOR performance for each subtype using video HITs may aid the differential diagnosis of the SCA genotypes and may lead to a better understanding of the neuropathology of SCA.
3.- FP1166Oscillopsia in patients with Cerebellar Ataxia and its relation with Dynamic Visual Acuity
Michaela Dankova1, Jaroslav Jerabek1, Dylan J. Jester2, Martin Vyhnalek1
1Department of Neurology, Centre of Hereditary Ataxias, 2nd Faculty of Medicine, Charles University and Motol University Hospital, Prague, Czech Republic, 2School of Aging Studies, University of South Florida, Tampa, FL, United States of America
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Oscillopsia due to the DVA impairment has been demonstrated as major factor affecting the quality of life in patients with compensated vestibular lesion. Recently, high prevalence of dynamic visual acuity impairment has been described in patients with cerebellar ataxia (CA) – both with and without vestibulopathy (CA-V and CA-NV), where objective DVA impairment in CA patients was related to the vestibular function measured by video head impulse test (VOR gain). Our aim was to assess subjective severity of oscillopsia in CA and to evaluate its relation to the alterations of DVA and vestibular function.
32 patients with CA and 3 control groups: 13 patients with unilateral and 13 with bilateral vestibulopathy and 21 age matched healthy volunteers were examined by clinical DVA test, VOR was assessed by video Head Impulse Test and caloric irrigation. Subjective oscillopsia was assessed by our newly prepared and administered Oscillopsia severity scale. Relationship between Oscillopsia severity scale and DVA impairment in CA patients was examined by Pearson’s product-moment correlations.
The presence of oscillopsia was reported by both subgroups of patients with CA (56,2% of CA: 58,3% of CA-V and 55% of CA-NV patients reported the presence of oscillopsia compared to 53,8% UV, 76,9% BV and 0% HC). The oscillopsia severity score assessed by our questionnaire correlated significantly with DVA impairment during clinical DVA test at 1 and 2 Hz (r= 0,44 [0,23 - 0,61] and 0,56 [0,37 - 0,70] respectively in the full sample, and 0,57 [0,26 - 0,77] and 0,45 [0,11 - 0,70] respectively in ataxia group). CA-V patients reported similar severity of oscillopsia as patients with compensated bilateral vestibular lesion.
We have demonstrated high prevalence oscillopsia in CA patients, where more than a half of CA patients reported signs of oscillopsia. Severity of oscillopsia expressed as Oscillopsia severity score was related to the objective DVA impairment according to the clinical DVA test in CA patients. We believe that analogously to the patients with BV, oscillopsia could be an important cause of disability in CA patients and we suggest that DVA and oscillopsia evaluation should be a standard part of clinical evaluation in CA patients as this information can help to target vestibular and oculomotor rehabilitation.
4.- FP1195Standardizing a Protocol for the Performance of Anti-Saccades captured by Video-Oculography
Michelle Petrak, Glen Zielinski, Shelley Massingale, Amy Alexander, Richard Gerkan, Liz Fuemmeler
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Our objective was to collect performance data from healthy volunteers in each decade of life for anti-saccade directional error rates and latencies in a standardized protocol.
The pro-saccade test (random or overlapped), although clinically valuable, often isn’t sensitive enough to flag dysfunction. The anti-saccade test is promising as more complex tasks can in many cases be a more sensitive indicator of potential pathology. In the anti-saccade test a subject is asked to ignore a stimulus and voluntarily move their eyes in the opposite direction. It is differentiated from a pro-saccade by nature of cognitive complexity, response inhibition and dual-tasking. The underlying neural networks of a pro-saccade also subserve the anti-saccade, with the addition of increased demand on inter-cortical frontal and parietal eye fields. Timing and strength of the inhibitory signal between frontal eye fields seems to be a major factor in correctly completing an anti-saccade. These areas of the brain underlie much of executive function and mental set. Oculomotor function has been well studied for decades and more recently anti-saccade research has been an area of focus. Several studies have looked at mixed pro-saccade/anti-saccade test (interweaved or blocked). This study measured an isolated anti-saccade block trial, sacrificing some of the potential neurological cost of switching tasks but more closely mimics a bedside clinical exam gaining familiarity and feasibility of time.
Anti-saccade performance data for different age groups are collected here. We add to the growing literature of anti-saccades and adding for the first time performance data for directional error rates and latencies. Our intention is to aid future studies distinguishing normal from abnormal, the progression there-of and underlying pathological dysfunction involved. Anti-saccade testing is valuable and should be included in oculomotor or psychomotor test batteries as a screening tool in addition to pro-saccades.
5.- FP1308Saccadic bradykinesia in Parkinson’s disease: Preliminary Observations
Nehzat Koohi1,2,3, Matthew J. Bancroft2, Jay Patel3, Patricia Castro2,3, Harry Akram3, Warner TT4,5, Diego Kaski2,3
1The Ear Institute, University College London, London, UK; 2Centre for Vestibular and Behavioural Neuroscience, Department of Clinical and Movement Neurosciences, Institute of Neurology, University College London, London, UK; 3Department of Neuro-otology, Royal National ENT and Eastman Dental HospitalsUCLH, London, UK; 4Reta Lila Weston Institute, Department of Clinical and Movement Neurosciences, UCL Queen Square Institute of Neurology, London, UK; 5Queen Square Brain Bank for Neurological Disorders, UCL Queen Square Institute of Neurology, London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Bradykinesia (low velocity) and hypokinesia (reduced amplitude) of limb movements are features of Parkinson’s Disease (PD), exacerbated when patients perform self-guided, repetitive limb movements, such as finger tapping – the so-called ‘sequence effect’. In the oculomotor system, both hypometria and slowing of voluntary saccades have been described in PD (1) but never as a change over time, which is the defining feature of this phenomenon.
Methods: We examined six mildly- or moderately-impaired PD patients (Unified Parkinson’s Disease Rating Scale: UPDRS motor part, 11±2.8 points; duration of illness, 2.2±0.4 years) aged 69±5 yrs (one female) and seven age-matched healthy control individuals (five female, 56±7 years). Voluntary and reflexive horizontal saccadic eye movements were recorded with infrared binocular videonystagmography (VNG) (Micromedical Visual Eyes 525 system™) sampled at 250Hz.
Results: Voluntary horizontal saccadic eye movements without visual targets led to a progressive decrease in PD saccadic amplitude over time (hypometria). In addition, PD saccadic velocity progressively reduced over time, even when accounting for smaller saccadic amplitudes (c.f. main sequence effect. Group (PD vs. Controls) and time (first six vs. final six saccades) interacted for both amplitude and velocity (F(1,11)>6.1; p<0.0031), with a decrease over time in PD (p=0.001) but not controls (p>0.110). PD saccadic velocity in the final six saccades was lower than normative amplitude-matched velocities (p=0.039) whereas no difference was present in the first six saccades (p=0.547).
Conclusions: Our data suggest that saccadic bradykinesia can be elicited at the bedside and was apparent in all consecutive patients, but absent in age-matched controls. “Saccadic bradykinesia” may be a useful and early clinical sign of PD but future studies should confirm these findings and assess its specificity as a clinical biomarker of disease progression.
6.- FP1436Towards robust saccade parameters for longitudinal video-based eye movement recordings
Martin Gorges, Erich Schneider
Institute of Medical Technology, Brandenburg University of Technology Cottbus - Senftenberg, Cottbus, Germany.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Neurodegenerative diseases negatively impact the brain and ubiquitously result in characteristically impaired eye movement control. Video-based eye tracking devices have become increasingly popular to gain insights into (dys)functions of the brain and the vestibular system. Eye tracker recordings during the application of visual and mechanical stimuli including smooth pursuit, visually guided reactive saccades, attempted steady fixation, anti-saccades, and head impulses allow for the quantification of eye movement parameters. Saccadic eye movements play a key role and provide essential parameters including saccade amplitude, duration, and peak eye velocity. Specific parameter constellations demonstrated diagnostic value such as differentiating within neurodegenerative parkinsonian syndromes. For instance, reduced peak eye velocity is a hallmark for patients with progressive supranuclear palsy. Longitudinal analyses of eye movement measures in patients are rare due to the lack of precise and robust repeated measures. High-quality recording of eye movements in patients with advanced movement disorders is limited and these recordings are usually corruptd by head motion-corrupted and other pronounced artefacts. This raises the question of whether the large variety of different algorithms for saccade classification can be considerably improved for precise and robust parameter quantification. We adapted and merged existing saccade classification algorithms and developed a new processing cascade including data cleaning, adaptive filtering, adaptive calibration, saccade classification, and computation of saccade parameters. Applying our new approach, we were able to compute a highly robust ‘main sequence’ (Figure) from poor-quality data that allows for robust and reproducible longitudinal analyses. Our approach is of particular interest for eye movement event classification in healthy participants and also in severely impaired patients (e.g. advanced parkinsonian syndromes) aiming at providing robust eye movement parameters that allow for detecting longitudinal differences at the individual level. In summary, the improved data analyses pipeline form the groundwork for specific and highly robust ‘dry’ biomarkers that are mandatory for future clinical trials and diagnosis.
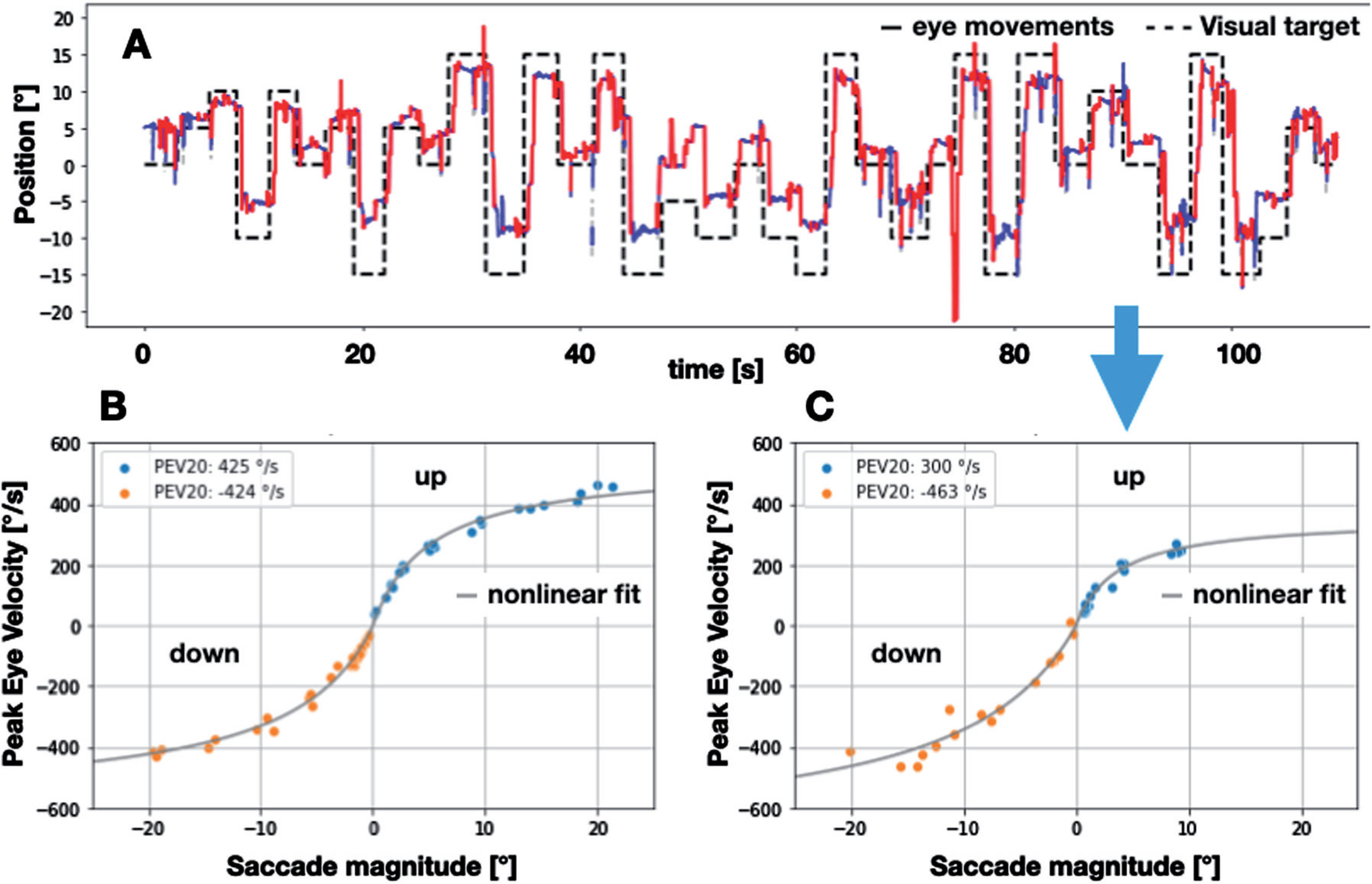
SATELLITE - 11-WEDNESDAY
8:30
SY0037SYMPOSIUM FORM
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Prof Peter ZU EULENBURG |
| TOPIC DESCRIPTIVE TITLE: | Bottom-up mapping of the human vestibular system |
| ACADEMIC / HOSPITAL AFFILIATION: | German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University Munich, Munich, Germany |
- SPEAKER 2
| NAME AND SURNAME: | Dr Elisa Raffaella FERRE |
| TOPIC DESCRIPTIVE TITLE: | Vestibular system: from sensory encoding to perception |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Psychological Sciences, Birkbeck University of London, London, United Kingdom |
- SPEAKER 3
| NAME AND SURNAME: | Prof Fred W. MAST |
| TOPIC DESCRIPTIVE TITLE: | Mental simulation and the brain’s vestibular network |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Psychology, University of Bern, Switzerland |
- SPEAKER 4
| NAME AND SURNAME: | Dr Christophe LOPEZ |
| TOPIC DESCRIPTIVE TITLE: | Distorted own-body and self representations in patients with dizziness |
| ACADEMIC / HOSPITAL AFFILIATION: | CNRS and Aix Marseille University, Marseille, France |
This symposium aims at providing an update on the vestibular cortical network and links these anatomical findings to high-level cognitive functions. The different contributions present results from recent research in neuroimaging, otoneurology, cognitive psychology and cognitive neuroscience. The range of contributions includes the largest neuroimaging study of the human vestibular cortex to date, which identified ten cortical homologues to known vestibular representations in non-human primates (P. zu Eulenburg). Moreover, we will present data about sensory integration for self-motion perception in the multisensory cortical vestibular network (E. Ferrè). The vestibular system is ideal to study how the brain makes sensory inference, and we will combine computational approaches with cognitive studies (F. Mast). The symposium will close with studies showing that sensory conflicts in the multisensory vestibular system can lead to perceptual incoherence and deteriorates own-body and self representations, adding to the complex symptomatology of patients with dizziness (C. Lopez). This symposium provides a multidisciplinary approach of high-order vestibular functions, their neural underpinnings and their clinical implications. The talks will cover topics that are relevant to clinicians, physiotherapists and basic scientists alike, and it serves as a platform for those interested in understanding the cognitive and perceptual aspects of the vestibular system.
ABSTRACT 1
The majority of human cerebral regions receiving vestibular information originating from our so-called sixth sense have evaded a definitive localization for more than two decades. Neuron recordings and tracer studies in several primate species had previously established a cortical vestibular network of at least seven regions per hemisphere. Multiple unaddressed confounders have impeded the delineation of a human vestibular cortex. These included underpowered group studies, somatosensory side effects, unaccounted head motion artifacts, unnaturalistic vestibular percepts and spatio-temporal signal limitations in neuroimaging. We have overcome these obstacles and delineated and replicated the entire human vestibular cortex and its nodes in a large-scale study (discovery sample n=75, replication sample n=150). We were able to identify ten cortical homologues to known vestibular representations in non-human primates. The talk will summarize these findings and will suggest a potential role for each delineated cortical vestibular region with respect to vestibular cognition.
ABSTRACT 2
Moving through the environment elicits a constant stream of sensory signals about self motion. Head rotation is coded through information from the three semicircular canals, while head translation is detected by the otoliths. Although rotation and translation can provide an accurate percept of self-motion, where these cues are represented in the human brain and how they interact with other sensory inputs is not yet clear. We have combined innovative methods for eliciting virtual rotation and translation sensations with fMRI to identify brain areas representing vestibular self-motion signals. We have identified a bilateral inferior parietal, ventral premotor/anterior insula and prefrontal network and confirmed that these areas reliably possess information about the perceived rotation and translation. We have also investigated how vestibular signals are integrated with other sensory cues to generate a self-motion percept. Our results demonstrate that vestibular-multisensory interaction within the cortical vestibular network in the human brain.
ABSTRACT 3
The brain makes use of prior knowledge in order to extract information provided by the vestibular senses. Bayesian filtering requires a dynamic generative model, which describes both the dynamics of head movements and how vestibular sensory data are generated as a function thereof. We implement the distinction between active and passive movements. Interestingly, knowledge of cognitive origin can inform sensory inference, and the same probabilistic model used for active self-motion (e.g., efference copy) can also be applied when self-motion is passive but predictable. Offline usage, such as running a simulation or planning a head movement correspond to sampling from the prior and performing inference conditioned on certain target states, respectively. We simulate motion when we imagine actions, take the spatial perspective of someone else or when we travel in time. Higher cognitive operations rely on mechanisms that are an integral part of sensory inference in the vestibular domain.
ABSTRACT 4
Vestibular disorders evoke complaints reaching far beyond imbalance and oscillopsia. Yet, how they affect own-body representations has been overlooked. In a first study in 60 patients with dizziness, we found that 12% of the patients have experienced distorted own-body representations (their hands or feet felt larger or smaller), 37% reported abnormal sense of agency and 35% reported disownership for the body. These proportions were larger in patients than in healthy controls. A second study aimed at testing whether caloric vestibular stimulation (CVS) produced comparable distortions in healthy volunteers. In a proprioceptive pointing task, the perceived length of the dorsum of both hands increased during Left-warm/Right-cold CVS. A third, prospective study in 420 participants showed a higher occurrence of out-of-body experiences in patients with dizziness (14%) than in healthy participants (5%). Altogether, our studies show a vestibular contribution to own-body representations and help understand the complex symptomatology of patients with dizziness.
OC13 1.- FP0895FREE PAPER FORM
Prognostic factors that modify outcomes of vestibular rehabilitation in elderly patients with falls
Marcos Rossi-Izquierdo1, Pilar Gayoso-Diz2, Sofía Santos-Perez3,4, María Del-Rio-Valeiras3,4, Ana Faraldo-Garcia3, Isabel Vaamonde-Sanchez-Andrade3, Antonio Lirola-Delgado3,4, Andrés Soto-Varela3,4
1Department of Otolaryngology, University Hospital Lucus Augusti, Lugo, Spain; 2Institute of Health Carlos III, Madrid, Spain; 3Department of Otolaryngology, Complexo Hospitalario Universitario de Santiago de Compostela, Spain; 4Department of Surgery and Medical-Surgical Specialities, Universidade de Santiago de Compostela, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Our previous study has shown that vestibular rehabilitation (VR) is an effective technique to reduce falls in elderly patients. It would be interesting to establish patients’ clinical characteristics in which vestibular rehabilitation is expected to be more effective.
Aims: Evaluate factors that could modify rehabilitation outcomes in elderly patients with previous falls.
Methods: Fifty-seven patients randomized to one of the intervention group (computerized dynamic posturography—CDP—training, optokinetic stimulus or exercise at home) and with previous falls were analyzed. Patients were assessed with objective outcome measures (sensorial organization test and limits of stability—LOS—of CDP, modified timed up and go test—TUG—and number of falls) and with subjective outcome measures (dizziness handicap inventory and Short falls efficacy scale-international—Short FES-I) during a 12-month follow-up period.
Results: In the logistic regression model, a worse score in the maximum excursion (MXM), and a shorter time in the TUG significantly associated with a reduction > 50% of falls. Also, association with a higher score in the Short FES-I was close to a statistical significance. There was no statistical significance association with other covariables.
Discussion: In patients with reduced limits of stability, VR seems to be more effective and they should be encouraged to perform it. But on the other hand, patients with longer time in the TUG show worse outcomes and may benefit more with gait training.
Conclusions: VR in elderly people with previous falls is effective regardless of their age and gender.
Keywords: Vestibular rehabilitation · Outcomes · Prognostic factor · Falls · Elderly
2.- FP0980Subconscious haptic feedback used to improve mobility, balance and quality of life in patients with imbalance due to severe bilateral vestibular loss: a prospective longitudinal study
Herman Kingma1 and Raymond van de Berg2
1Maastricht University Hospital, The Netherlands and 2Aalborg University Hospital, Denmark
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Aim of the study: evaluation of the impact of ambulant haptic feedback (complex vibration pattern around the waist depending on trunk tilt angle and movement) upon balance, mobility and quality of life in patients with severe bilateral vestibular loss.
Type of study: prospective longitudinal.
Inclusion criteria: 47 patients with severe bilateral vestibular loss according to the criteria of the Bárány Society Classification Commitee suffering from severe imbalance that did not improve anymore on sustained vestibular rehab. Exclusion criteria: neurological, orthopedic or otherwise mobility disorders.
Method: after inclusion, patients rated their mobility and balance score (MBS) between 0-10, where 0 ment maximum and severe impairment and 10 ment normal mobility and balance as was experienced by each individual patient before they had noted any reduced balance in the past. After a technical explanation of the usage of the belt, patients were instructed NOT to pay attention to the haptic feedback in daily life and to try to regain balance and mobility in daily life as much as possible without additional training or support. By that, the patients avoided to use the belt as an additional cognitive load (double tasking), while the belt provided subsconscious information about the spatial orientation of the upper trunk, comparable to the subconsious vestibular perception of verticality. The MBS was rated before the use of the belt, after two weeks, 2 months, 6 months and 1 year.
Results: 16 patients did not notice any or substantial improvement within two months and decided to stop using the belt. 31 patients reported substantial benefit which was objectivied by an increase of the individual MBS scores by 3 to 5 points. The improvement was stabilised within 2 months and stable during the maximum observation period of 1 year. Patients reported that they experienced a wide range of positive effects of the belt upon their quality of life and self-readiness. By interviews, further analysis was made of the impact of the belt in these patients. Specially DFNA9 patients reported an impressive impact on their quality of life and mobility, whereas patients with an inclusion value of the MBS of 6 or more, generally did not experience substantial benefit.
3.- FP1008Changes in Measures of Vestibular Function and Hippocampal Volume in Patients with Alzheimer’s Disease and Mild Cognitive Decline
Helen S Cohen1, Christie M Lincoln2, Valory N Pavlik3, Haleh Sangi-Hahgpeykar4, Nathan Silver1
1Baylor College of Medicine, Houston, TX, USA; 2Departments of Otolaryngology; Radiology; 3Neurology; 4Obstetrics and Gynecology
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Some evidence indicates anatomical projections of the vestibular system to the hippocampus. Other evidence indicates that patients with Alzheimer’s disease have abnormal results on cervical vestibular evoked myogenic potentials cVEMP). The goals of this study were to determine if patients with Alzheimer’s disease (AD) and mild cognitive impairment (MCI) have any other vestibular impairments and to determine if vestibular disorders are related to decreased hippocampal volume in these patients.
Methods: Patients with AD and MCI due to AD were recruited from an academic Alzheimer’s disease center after having been diagnosed by a neurologist based on clinical exam, neuropsychological testing and clinical MRI. They were tested on the objective battery of objective vestibular tests (VNG), including low frequency sinusoidal tests of the vestibulo-ocular reflex in darkness, bi-thermal caloric tests, cVEMP, and Dix-Hallpike and other positional tests.
Results: Alzheimer’s and MCI patients did not differ significantly. Compared to historical healthy controls from this lab the group, as a whole, had increased frequency of impaired responses on cVEMP and also increased frequency of abnormal Dix-Hallpike responses. MRI data from a subset of the sample were available for analysis. From that subsample, subjects with abnormal VNG results had decreased hippocampal volume compared to normals.
Conclusion: These data suggest that vestibular impairment is more common in this population than in the age-matched healthy population. These data also suggest that these changes may be related to decreased hippocampal volume found in these patients.
Supported by NIH grant 2R01-DC009031-10S1.
4.- FP1180Frontal White Matter Integrity and Idiopathic Dizziness in Cerebral Small Vessel Disease
Richard Ibitoye1,2, Patricia Castro1, Josie Cooke1, John Allum3, Louisa Murdin4, Joanna Wardlaw5, Diego Kaski2,6, David J. Sharp2, Adolfo M. Bronstein1
1Neuro-otology Unit, Imperial College London, London, UK; 2The Computational, Cognitive and Clinical Neuroimaging Laboratory (C3NL), Imperial College London, London, UK; 3Department of Otorhinolaryngology (ORL), University Hospital Basel, Basel, Switzerland; 4Guy’s and St Thomas’ NHS Foundation Trust, London, UK; 5Centre for Clinical Brain Sciences, The University of Edinburgh, UK; 6Department of Clinical and Movement Neurosciences, University College London, London, UK.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and Aims: Three in ten older people (>60 years) complain of persistent dizziness which often remains unexplained despite specialist assessment and vestibular tests. The pathophysiology of such idiopathic dizziness in older people has remained unclear. We investigated if idiopathic dizziness was associated with vascular injury to white matter tracts relevant to balance or vestibular self-motion perception in sporadic small vessel disease.
Methods: We prospectively recruited 38 vestibular clinic patients with idiopathic dizziness (median 77 years) and 36 asymptomatic controls (median 76 years) who underwent clinical, cognitive, balance, gait and vestibular assessments, and structural and diffusion brain MRI.
Results: Patients had more vascular risk factors, poorer balance and worse executive cognitive function in association with greater white matter hyperintensity in frontal deep white matter, and lower fractional anisotropy in the genu of the corpus callosum and the right inferior longitudinal fasciculus. Tracts with lower fractional anisotropy in idiopathic dizziness overlapped with those in which lower fractional anisotropy correlated with worse balance across participants. More vestibular symptoms correlated with worse balance in patients. Vestibulo-ocular reflex and perceptual vestibular function was similar in patients and controls, though a white matter network involved in vestibular perception had lower connectivity in patients.
Conclusion: Our results show a relationship between lower microstructural integrity in frontal balance-relevant white matter tracts in cerebral small vessel disease, poorer balance and idiopathic dizziness. This suggests cerebral small vessel disease may be involved in the pathogenesis of dizziness in some older people.
5.- FP1183Vestibular Loss Disrupts Visual Reactivity in the Alpha Rhythm
Patricia Castro1, Richard Ibitoye1, Toby Ellmers1, Diego Kaski2, Adolfo Bronstein1
1Neuro-otology Unit, Department of Brain Sciences, Imperial College London, London, UK; 2Department of Clinical and Movement Neurosciences, University College London, UK. **P. Castro and R. Ibitoye are joint first authors in this work**
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and Aims: Stimulus-induced change in cortical activity is a key neural mechanism underpinning multisensory information and is important for cognitive function. Multisensory integration is frequently studied using known interactions of vestibular and visual systems. Visual motion stimuli deactivate vestibular networks and vice versa. Relatedly, vestibular loss leads to increased visual dependence - a bias in multisensory perceptual judgements towards vision (e.g. ‘which way is up?’). These findings imply normal vestibular function is essential for the tuning of visual cortical activity. This predicts usual deactivation of the visual cortex on eye closure is impaired following vestibular loss, in association with greater visual dependence. We test this hypothesis using alpha EEG power as a corollary of visual cortical activity in patients with bilateral vestibulopathy and controls.
Methods: Fifteen bilateral vestibulopathy patients (mean age 62 +/- 18 years [standard deviation] years), and fifteen age-matched controls (62 +/- 20 years) had 32-channel EEG recordings in seated and standing postures, as well as measures of the subjective visual vertical, and visual dependence by a computerised rod and disc task. Alpha band (8-14Hz) EEG power was calculated at each channel. Statistical tests were undertaken by linear regression, adjusted for multiple comparisons across channels by threshold-free cluster enhancement.
Results: With the eyes open, average alpha EEG power was similar in patients with bilateral vestibulopathy and controls, in both seated and standing postures. Alpha EEG power enhanced on eye closure in both patients and controls (p<.05) such that alpha enhancement on eye closure was significantly less in patients. Group (patients/controls) influenced the effect of eye closure on alpha EEG power (p<.05); posture (seated/standing) did not moderate this effect (p>.05). Group influenced the relationship between visual dependence and alpha enhancement (p<.05). In patients, visual dependence correlated with less frontal alpha enhancement (p<.05), whereas no significant correlation was present in controls. More visually dependent patients thus had less alpha enhancement on eye closure.
Conclusions: Our results show vestibular loss disrupts usual increases in alpha EEG oscillations on eye closure. Correlation in patients between more visual dependence and less alpha enhancement suggests vestibular loss and central visuo-vestibular integration drive the reduction in alpha reactivity. Given the reactivity of alpha oscillations to vision has been shown to be important in normal cognitive function, our finding of a relationship between the alpha rhythm and vestibular functioning finding may have broader implications for cognitive functioning following vestibular loss.
6.- FP1348Vestibular Thresholds Explain Nearly Half of Age-related Balance Declines and Correlate with Sway
Andrew R. Wagner1,2 , Megan J. Kobel1,3 , Daniel M. Merfeld1,2,3,4
1Otolaryngology — Head & Neck Surgery, Ohio State University Wexner Medical Center, Columbus, OH, USA; 2Health and Rehabilitation Sciences, Ohio State University, Columbus, OH, USA; 3Speech and Hearing Science, Ohio State University, Columbus, OH, USA; 4Biomedical Engineering, Ohio State University, Columbus, OH, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Objectives: Falls are a major public health burden. A body of literature supports that imbalance contributes to falls and vestibular dysfunction has long been known to contribute to imbalance. This study was designed to quantify links between vestibular function and subclinical balance dysfunction in healthy asymptomatic individuals.
Design: Over a series of studies, we assessed vestibular function using self-motion perceptual thresholds. In one study, our population included 105 asymptomatic humans aged 18 to 80. 99 of these 105 individuals also participated in a modified Romberg balance test. Failing the 4th condition (eyes closed, on foam) of this exact test had previously been shown to correlate with more than a six times higher chance of reporting a difficulty with falls in the past year. In a second study, our population included 33 asymptomatic humans (20-32 years old) who, in addition to threshold testing, participated in a modified Romberg balance test performed on a force plate.
Results: We found a substantive and significant correlation between increasing age and increasing vestibular thresholds. We also found significant correlations between: (a) increasing age and imbalance, (b) increasing vestibular thresholds and imbalance, as well as (c) the combined effect of increasing vestibular thresholds and age on imbalance. We also performed mediation analyses to quantify whether vestibular function might be a causative mediator of imbalance in normal asymptomatic humans and found that 46% of the decline in balance with age in adults above the age of 40 was mediated by vestibular function. Finally, we found that vestibular tilt thresholds positively correlated with sway - even in a young healthy adult population.
Conclusions: Vestibular function seems to explain a large fraction of age-related balance declines as assayed via a Romberg balance test. This is surprising, since balance declines are known to be multi-factorial and aging results in declines in nearly all physiologic contributors to balance (e.g., kinesthesia, vision, motor control, strength, vestibular function, etc.). Identifying vestibular function as a pre-dominant physiologic cause of suboptimal balance is important as it provides a target for interventions tailored specifically to reduce falls in older adults.
OC14
1.- FP1167Bayesian computations and age-related changes in the percept of vertical
W. Pieter Medendorp
Radboud University, Donders Institute for Brain, Cognition and Behaviour, Nijmegen, The Netherlands
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
This is 1 of 4 linked talks concerning “HIGHER ORDER VESTIBULAR PROCESSING, SPATIAL ORIENTATION AND POSTURAL CONTROL” (Barry Seemungal, Kathy Cullen, Stefan Glasauser, Pieter Medendorp)
While it has been well established that optostatic and optokinetic cues contribute to the perception of vertical, it is unclear how the brain processes their combined presence with the nonvisual vestibular cues. I will present a series of psychophysical experiments in humans that measure their percept of vertical under different manipulations of a static visual frame, an optokinetic roll-stimulus, or under galvanic vestibular stimulation. Within a Bayesian modeling perspective, I will show that the dynamic effects of roll optokinetic stimuli and galvanic vestibular stimulation have different time constants but combine linearly into a single, vestibular-optokinetic estimate, which is integrated with an optostatically-derived estimate of vertical. I will also show that, with age, the vestibular information contribution to spatial orientation is down-weighted whereas the visual weight is increased, primarily due to an age-related increase of the noise of vestibular signals.
2.- FP1203Modelling Vestibular-Guided Spatial Orientation
Stefan Glasauer
Brandenburg University of Technology Cottbus-Senftenberg, and Faculty of Healthy Sciences Brandenburg, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
This is 1 of 4 linked talks concerning “HIGHER ORDER VESTIBULAR PROCESSING, SPATIAL ORIENTATION AND POSTURAL CONTROL”.
Spatial orientation depends to a large extent on vestibular inputs, which provide sensory information about movement with respect to an inertial frame of reference. We investigated vestibular-guided spatial orientation during active and passive whole-body motion, focussing on the ability to estimate magnitudes such as distances and angles in simple navigation tasks. In one experiment participants sitting on a rotating chair had to replicate the previously experienced rotation angle by rotating the chair the same amount using a joystick. In another experiment, blindfolded participants, after being guided along two legs of a triangular path, had to return to the point of origin by active walking. In both experiments, vestibular self-motion cues play a dominant role. To explain the results of these and several previous experiments, we propose computational models of vestibular processing for orienting and navigation, which are based on the concept of probabilistic Bayesian estimation. This framework provides methods for optimally integrating uncertain information from various sources, such as sensory input and prior knowledge. We show that Bayesian models of processing sensory information can explain various aspects of vestibular processing for spatial orientation and navigation. However, in most cases the estimation models that best explain the experimental results are clearly sub-optimal for the experimental task to be solved, but may be appropriate in more naturalistic situations.
3.- FP1209The Neural Basis for Vestibular Perception during Unexpected versus Actively Generated Self-motion
Kathleen E. Cullen1, Alexis Dale2, Jerome Carriot2, Maurice Chacron2
1The Johns Hopkins University; 2McGill University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
This is 1 of 4 linked talks concerning “HIGHER ORDER VESTIBULAR PROCESSING, SPATIAL ORIENTATION AND POSTURAL CONTROL”.
I will present an overview of my group’s recent work establishing a neural basis for self-motion perception during unexpected versus actively generated self-motion. I will first discuss the results establishing the neural basis – at the level of vestibular thalamocortical neurons - for the violations of Weber’s law observed in the perception of applied vestibular stimulation. I will then discuss our findings that these same neurons selectively encode unexpected applied versus actively generated motion, thereby providing a neural correlate for ensuring perceptual stability. These results provide new insights into how the thalamus in general relays sensory information to cortex during our everyday activities.
Target audience - both Basic and Clincal Scientists
4.- FP1287Vestibular Agnosia: Link to Abnormal Structural and Functional Brain Circuits & Clinical Impact
Barry M. Seemungal
Neuro-Otology Unit, Department of Brain Sciences, Imperial College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
This is 1 of 4 linked talks concerning “HIGHER ORDER VESTIBULAR PROCESSING, SPATIAL ORIENTATION AND POSTURAL CONTROL”. I will present an overview of my group’s recent work characterising a syndrome called vestibular agnosia seen in brain disease patients with network dysfunction (e.g. traumatic brain injury and neurodegeneration) in which patients’ perception of vertigo is impaired or even absent. I will discuss the overlap between vestibular agnosia and postural imbalance and I will link behavioural abnormalities with structural and functional brain imaging. I will also discuss the everyday clinical consequences of vestibular agnosia for the diagnosis, treatment (and nomenclature) of common inner ear disorders in brain disease patients.
5.- FP1329Perceiving Illusory Self-Motion without Motion
Anna J. C. Reuten1,2, Jeroen B. J. Smeets1, Marieke H. Martens3,4, Jelte E. Bos2,1
1Department of Human Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands; 2Human Performance, The Netherlands Organization for Applied Scientific Research (TNO), Soesterberg, The Netherlands; 3Traffic and Transport, The Netherlands Organization for Applied Scientific Research (TNO), The Hague, The Netherlands; 4Department of Industrial Design, Eindhoven University of Technology, Eindhoven, The Netherlands
Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
Yes
Previous studies demonstrated a role for cognition on self-motion perception. However, those studies all concerned perceptual modulations of a physical motion stimulus. We here investigated whether cognitive cues can elicit a percept of self-motion in the absence of any actual motion. As the perception of illusory self-motion without sensory stimulation would result in a neural mismatch between actual and estimated sensory signals, we were also interested whether participants reported motion sickness. We accordingly seated blindfolded participants on a swing that remained motionless during two experimental sessions, apart from a deliberate transient perturbation at the start of a session. The two sessions only differed regarding instructions and a secondary task, suggesting either a quick halt (Distraction from motion) or continuous oscillations of the swing (Suggestion of motion). Participants reported that the swing oscillated with larger displacements and for a longer period of time in the Suggestion compared to Distraction session. This increase in perceived motion did however not influence the motion sickness scores. As the perceived motion was rather limited (displacement of about 30 cm), the lack of an effect on motion sickness can be explained by assuming a subthreshold neural conflict. Our results speak in favor of the existence of internal models that provide estimations on self-motion and sensory signals, which estimations we here successfully modulated via cognitive cues. This supports the success of cognitive (behavioral) therapies in alleviating medical disorders with distorted sensory processing like tinnitus and potentially mal de débarquement syndrome. We conclude that studies on self-motion perception do require the recognition of cognitive cues.
6.- FP1372Influence of Magnetic Vestibular Stimulation on Self-motion Perception
Gerda Wyssen1, Miranda Morrison2, Athanasia Korda2, David Zee3, Georgios Mantokoudis2, Fred W. Mast1
1Department of Psychology, University of Bern, Bern, Switzerland; 2Department of Otolaryngology, Head and Neck Surgery, Inselpital, University Hospital Bern and University of Bern, Bern, Switzerland; 3Department of Neurology, Johns Hopkins Unversity School of Medicine, Baltimore MD, USA
Ultrahigh magnetic fields (UHF) induce dizziness, vertigo and nystagmus due to Lorentz forces acting on the cupula in the semi-circular canals, an effect called magnetic vestibular stimulation (MVS) (Roberts et al., 2011; Ward et al., 2015). As the effect of the magnetic field on the cupula remains constant throughout the exposure, MVS is specifically suitable for studying cognitive performance under vestibular stimulation. The effect of MVS can be set near to zero by tilting the head 30° forward towards the body, allowing to compare different strengths of MVS within subjects (Mian et al., 2016). Furthermore, MVS serves as a suitable non-invasive model for unilateral failure of the vestibular system, which enables studying compensatory processes (Ertl and Boegle, 2019). We conducted our study in a Siemens Terra 7 Tesla Scanner and tested 8 young, healthy participants and plan to include 30 more.
The study had two main goals. First, to investigate the process of perception-reflex uncoupling, as under MVS self-motion perception differs from measured nystagmus in direction as well as time course. While horizontal nystagmus was predominant, most participants report a percept of roll rotation, and less frequent a percept of yaw rotation or a mixture of both when moving in to and out of the magnetic field. This matches previous studies (Mian et al., 2013). Reported percepts did not correspond fully to measured reflexive eye-movements. Overall, stronger nystagmus indicated stronger percepts. Roll percepts make sense because the brain integrates the prior knowledge and sensory evidence. In supine position, yaw but not roll rotation would also elicit change in direction of gravity. Second, to quantify influence of continuous vestibular stimulation on cognitive functions with spatial components. Behavioral and neuroimaging studies have shown repeatedly that caloric, galvanic and motion platform-induced vestibular stimulation can affect performance in spatial tasks, such as mental rotation (Klaus et al., 2019; Falconer & Mast, 2012). The influence of MVS on spatial cognition is relevant for fMRI studies as MVS can be a confounder, especially in studies using UHFs. In our study, we did not find a meaningful effect of MVS on mental body rotation performance, neither in allocentric nor in egocentric strategy.
In the future, we aim to compare healthy participants and patients with vestibular disorders to investigate adaption and habituation mechanisms.
Target audience: Interest in research bridging reflexes, perception and cognition in the vestibular domain
SP10
SY0034SYMPOSIUM FORM
| •ORGANIZER’S NAME and SURNAME: | Georges DUMAS, Sébastien SChmerber |
| •ORGANIZER’S E-MAIL: | |
| •ACADEMIC/HOSPITAL AFFILIATION: | CHU Grenoble Alpes |
| •SESSION TITLE: | Skull vibration induced nystagmus |
3 or 4 SPEAKERS PER SYMPOSIUM:
- SPEAKER 1
| NAME AND SURNAME: | Georges DUMAS |
| TOPIC DESCRIPTIVE TITLE: | The Skull Vibration-Induced Nystagmus Test (SVINT): Charateristics. |
| ACADEMIC / HOSPITAL AFFILIATION: | Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University Hospital, Grenoble, France EA 3450 DevAH, Development, Adaptation and Disadvantage, Faculty of Medicine and UFR STAPS, University of Lorraine, Villers-lès-Nancy, France |
- SPEAKER 2
| NAME AND SURNAME: | Roberto Teggi |
| TOPIC DESCRIPTIVE TITLE: | The skull vibration induced nystagmus test in Menière’s disease, Benign recurrent vertigo and vestibular migraine. |
| ACADEMIC / HOSPITAL AFFILIATION: | ENT Division, San Raffaele Scientific Institute, Milano, Italy; [email protected], Milano, Italy I |
- SPEAKER 3
| NAME AND SURNAME: | Solara SINNO |
| TOPIC DESCRIPTIVE TITLE: | The skull vibration induced nystagmus test in children. |
| ACADEMIC / HOSPITAL AFFILIATION: | EA 3450 DevAH, Development, Adaptation and Disadvantage, Faculty of Medicine and UFR STAPS, University of Lorraine, Villers-lès-Nancy, France Laboratory for the Analysis of Posture, Equilibrium and Motor Function (LAPEM), University Hospital of Nancy, F-54500 Vandoeuvre-lès-Nancy, France |
- SPEAKER 4
| NAME AND SURNAME: | Angel Batuecas-Caletrío |
| TOPIC DESCRIPTIVE TITLE: | Skull vibration Induced Nystagmus as predictor of vertigo attacks after intratympanic gentamicin. |
| ACADEMIC / HOSPITAL AFFILIATION: | Otoneurology Unit, Department of Otorhinolaryngology, University Hospital of Salamanca, IBSAL, UNiversity of Salamanca. Salamanca, Spain; |
A 100-Hz bone-conducted vibration applied to either mastoid induces instantaneously a predominantly horizontal nystagmus, with quick phases beating away from the affected side in patients with a unilateral vestibular loss (UVL). The same stimulus in healthy asymptomatic subjects has little or no effect. The skull vibration-induced nystagmus (SVIN) is a useful, simple, non-invasive, robust indicator of asymmetry of vestibular function and the side of the vestibular loss. The nystagmus is precisely stimulus-locked: it starts with stimulation onset and stops at stimulation offset, with no after nystagmus. It is sustained during long stimulus durations; it is reproducible; it beats in the same direction irrespective of which mastoid is stimulated; it shows little or no habituation; and it is permanent—even well-compensated UVL patients show SVIN.The SVIN -SPV must be > 2.5°/s. Stimulus frequency, location, and intensity modify the results. We describe the optimum method of stimulation. Recent neural evidence clarifies which vestibular receptors are stimulated, how they cause the nystagmus. This presentation focuses not only on the optimal parameters of the stimulus and response of UVL and SCD patients but also on the criteria of positivity of SVIN. We conclude that the presence of SVIN is a useful indicator of the asymmetry of vestibular function.
ABSTRACT 1
Skull-Vibration-Induced-Nystagmus Test (SVINT), a non-invasive first line examination test, stimulates both otolith and canal structures and shows instantaneously a vestibular asymmetry. The purpose of this study was to establish normative data for SVINT that can be used clinically in the assessment of vestibular disorder in children. Hence a total of hundred twenty healthy children were recruited and equally distributed according to age and gender to each of the following age groups: 5-8, 9-11, 12-14, and 15-17 years old. Participants had a comprehensive otological and neurological assessment prior to inclusion in the study. All participants were able to perform SVINT , and the majority of healthy children tolerated it well (n=89, 74%), the others found it mildly disturbing. In normal children, clinically significant nystagmus was recorded in only 2.50 % of the cases (N=3), a negative SVINT result was observed in the rest (97.50 %) in accordance with the criteria defined. The SVINT results are conformed in both adults and children.
ABSTRACT 2
Vestibular Migraine (VM) and Menière’s Disease (MD) are the most frequent long-lasting episodic vertigo. Diagnoses, above all in early stages is troublesome. We compared positivity for this test in two samples, the first composed by 605 MD and the second by 200 VM subjects. We found that 59.2% MD subjects presented a positive SVINT while only 6% VM. Since SVINT is positive above all in a peripheral vestibular deficits, we think that our data support the hypothesis that, in the pathophysiology of VM attacks central vestibular pathways are mainly involved.
Moreover, we studied 28 migraneurs subjects presenting episodic vertigo without cochlear symptoms during the first attacks; in the follow-up they presented cochlear symptoms addressing toward the diagnosis of MD. Results of SVINT was compared with a group of 48 definite VM. Ten patients with MD (35.7%) and seven with VM (14.6%) had a positive SVINT during the first consultation.
ABSTRACT 3
Skull-Vibration-Induced-Nystagmus Test (SVINT), a non-invasive first line examination test, stimulates both otolith and canal structures and shows instantaneously a vestibular asymmetry. The purpose of this study was to establish normative data for SVINT that can be used clinically in the assessment of vestibular disorder in children. Hence a total of hundred twenty healthy children were recruited and equally distributed according to age and gender to each of the following age groups: 5-8, 9-11, 12-14, and 15-17 years old. Participants had a comprehensive otological and neurological assessment prior to inclusion in the study. All participants were able to perform SVINT, and the majority of healthy children tolerated it well (n=89, 74%), the others found it mildly disturbing. In normal children, clinically significant nystagmus was recorded in only 2.50 % of the cases (N=3), a negative SVINT result was observed in the rest (97.50 %) in accordance with the criteria defined. The SVINT results are conformed in both adults and children.
ABSTRACT 4
The usefulness of Skull-Vibration-Induced-Nystagmus Test (SVINT) in detecting vestibular asymmetry is well known. Previous studies determine that there is a good correlation between the presence of the Skull- Vibration-Induced-Nystagmus (SVIN) and the vestibular function measured through the caloric test or the vHIT. Furthermore, the Slow Phase Velocity (SPV) of the SVIN is related to the severity of unilateral vestibular deficit. We studied a group of 88 patients with definitive Meneire’s disease who had been instilled with intratympanic gentamicin to control their vertigo attacks. We started the follow-up of these patients after six months without suffering vertigo attacks after intratympanic gentamicin. We studied the patients using vHIT and SVIN and separated them into two groups based on whether or not they had suffered from vertigo attacks again during their follow-up. 70/88 patients (79.5%) did not have vertigo attacks again and both the vHIT and the SPV of the SVIN did not change. 18/88 patients (20.5%)suffered from vertigo attacks again in the follow up. These generally appeared in the first year of follow-up and 15/18 patients showed a recovery of gain in the vHIT. 18/18 patients showed a decrease in SPV of the SVIN when vertigo attacks reappeared, with a mean reduction of the SPV of 40% over the SPV at the beginning of the follow-up. The SPV of the SVIN could be a good follow-up parameter for patients treated with intratympanic gentamicin in order to determine the recovery of vestibular function and the possibility of vertigo attacks relapsing.
ST03
1.- FP0966FREE PAPER FORM
A Tinnitus Suite for two ears and one brain in patients with Meniere’s Disease
Patricia Perez-Carpena1,2, Marta Martinez-Martinez2,3; Ramón Antonio Martínez Carranza4, Angel Batuecas Caletrio4, Jose A. Lopez-Escamez 1,2,5
1Department of Otolaryngology, Hospital Universitario Virgen de las Nieves, ibs.Granada, Granada, Spain; 2Otology & Neurotology Group CTS495, GENYO - Centre for Genomics and Oncological Research, Granada; 3Department of Otolaryngology, Hospital Universitario San Cecilio, ibs.Granada, Granada, Spain; 4Department of Otolaryngology, Hospital Universitario de Salamanca, IBSAL Salamanca Spain; 5Department of Surgery, Division of Otolaryngology, Universidad de Granada, Granada, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Meniere’s disease (MD) is a chronic disorder of the inner ear characterized by vertigo attacks with aural fullness, tinnitus and sensorineural hearing loss. Tinnitus is considered the most annoying symptom, but it is seldom investigated. Although there is no evidence that tinnitus is induced by anxiety, some studies suggest a possible association between these symptoms. Our objective is to perform a psychoacoustic characterization of tinnitus in MD, and to determine if the tinnitus perception is related to anxiety or to the cochlear damage itself, to define an extreme phenotype for tinnitus.
Methods: A cross-sectional multi-center study was designed, including 100 patients diagnosed with defined MD who reported tinnitus, from hospital from Granada and Salamanca. A detailed anamnesis was carried out, including clinical variables (age, gender, age of onset, duration of the disease, uni or bilateral involvement, hearing thresholds, fluctuation and location of the tinnitus) and psychoacoustic variables (type of sound, tinnitus loudness matching, minimum masking level, and residual inhibition). Perceived disability was assessed by a visual analogue scale (VAS) and the Tinnitus Handicap Inventory (THI). Anxiety and depression symptoms were evaluated with the Hospital-Anxiety Depression Scale (HADS).
Results: Tinnitus was permanent in 79 patients. Most of these patients described a tonal tinnitus (n =44), followed by the subgroup of patients describing a noise-like tinnitus (n =35). Meniere’s disease patients with tonal tinnitus presented higher scores in THI compared with the patients with noise-like tinnitus. We found a statistically significant correlation between the scores obtained in VAS and THI (r =0.67; p = 0.001). Both scales showed a moderate correlation with the total HADS score (VAS-HADS, r =0.32, p =0.004; THI-HADS, r =0.56, p =0.001). No statistically significant association was found between these scores and the intensity of tinnitus, the age of patients or the duration of the disease.
Conclusions: Tinnitus is a heterogeneous symptom in patients with MD, which includes tonal and noise like tinnitus. This heterogeneity could be related to the clinical differences described in MD tinnitus. Most patients with MD develop a persistent, constant tinnitus, but few of them report an annoying tinnitus with a significant impact on their quality of life, to be considered a tinnitus extreme phenotype. The type of tinnitus and the hearing involvement in MD have shown a correlation with the disability perceived by patients estimated by the THI.
2.- FP1019Neuroinflamation and Venous Lesion of the Neck Veins in Patients with Meniere’ Disease. Reuslts of a Multicentric Study
A. Bruno md1, G. Attanasio md2, L. Califano md3, A. Casani md4, PP.Cavazzuti md5, G. Neri md6
1Vasc. Dep. Gepos Clinic, Telese T. (BN) Italy; 2G. Attanasio Dep. Head and Neck Sapienza University Rome; 3L- Califano Dep. Audiology and Vestibology Rummo Hospital Benevento; 4ENT Dep. Pisa University Italy; 5DEP ENT Maggiore Hospital Bologna Italy; 6ENT Dep. Chieti University Italy
Key Words: CCSVI – chronic cerebrospinal venous insufficiency; PTA – percutaneous transluminal angioplasty; IJV – internal jugular vein.
ABSTRACT
Purpose: To evaluate the relationship between Meniere’s disease (MD) and chronic cerebrospinal venous insufficiency (CCSVI) and the effectiveness of angioplasty for reducing the symptoms of MD using ultrasonography, magnetic resonance imaging, and venography.
Materials and Methods: A total of 590 patients diagnosed with definite MD who had not experienced improvement with medical and surgical therapy underwent duplex ultrasonography and MRI to diagnose the presence of venous stenosis of the neck.
Results: A total of 472 (80%) MD patients were diagnosed with venous lesion of the neck. In the healthy population, was evident in only 12% of patients. Venography was performed in 165 patients to confirm the diagnosis of CCSVI. In 80% of these patients, PTA of the IJVs and/or azygos veins was effective for treating the signs and symptoms of CCSVI and MD.
Conclusions: Venous lesion of the neck was prevalent in patients with MD. Most patients responded favorably to PTA. Our results suggest a possible etiological relationship between venous stenoses and MD that warrants further investigation.
Bibliography:
1) Chronic cerebro-spinal venous insufficiency in Meniere’s Disease. F. Di Bernardino, D,C. Alpini, P. Bavera. Phlebology 2015, vol.30 (4) 274-279
2) Truncular Venous Malformation in Meniere’s Disease Patient: the Key for new treatment perspective? D. Piraino, G. Andolina, A. Messina. J.V.I.R. 2016
3) The Prevalence of Chronic Cerebro-Spinal Venous Insufficiency in Meniere’s Disease: 24 Months Follow-up after Angioplasty. A. Bruno, M.S. Napolitano, L. Califano: J.Vasc. Int. Rad. 2017, 28:388-391
4) Chronic Cerebrospinal Venous Insufficiency and Menière’s Disease: Interventional Versus Medical Therapy. G. Attanasio, L. Califano, A. Bruno ed al.: Laryngoscope nov. 2019
3.- FP1073Computing Endolymph Hydrodynamics During Head Impulse Test on Normal and Hydropic Vestibular Labyrinth Models
Jorge Rey-Martinez1, Xabier Altuna1, Kai Cheng2, Ann M. Burgess2, Ian S. Curthoys2
1Neurotology unit. ENT. Hospital Universitatio Donostia. San Sebastian. Spain; 2Vestibular Research Laboratory. School of Pshychology. University of Sidney. Australia
Hypothesis: Build a biologic geometry based computational model to test the hypothesis that, in some circumstances, endolymphatic hydrops can mechanically cause enhanced eye velocity responses during clinical conditions of the head impulse test.
Background: Some recent clinical and experimental findings had suggested that enhanced eye velocity responses measured with the video head impulse test could not only be caused by recording artifacts or central disfunction but also could be directly caused by the mechanical effect of endolymphatic hydrops on horizontal semicircular canal receptor.
Methods: Eighteen head impulses were computed in three biologic-based geometry models governed by Navier-Stokes equations; six head impulses of incrementally increasing peak head velocity were computed in each one of the three different geometric models, depending on absence, canal or utricular hydrops.
Results: For all computed head impulses an increased endolymphatic pressure was measured at the ampullar region of the horizontal semicircular canal on conservative canal and utricular hydrops models. The mean of aVOR gain was 1.00 ± 0 for the no-hydrops model, 1.128 ± 0.009 for the canal hydrops model was, and 1.104 ± 0.005for the utricular hydrops model. All measured differences were statistically significant (p < 0.001).
Conclusion: The results of the physical computation models support-the hypothesis that in endolymphatic hydrops conditions, which are affecting horizontal semicircular canal and utricular region on moderate dilatations, the eye velocity responses output-by the aVOR will be enhanced by a 1.12 factor and aVOR gain values will be enhanced by over 1.1 for impulses to the right side.
4.- FP1143The Relationship between Cochleovestibular Function Tests and Endolymphatic Hydrops grading on MRI in patients with Menière’s Disease.
Morgana Sluydts1, Anja Bernaerts2, Jan Casselman2, Bert De Foer2, Cathérine Blaivie1, Andrzej Zarowski1, Joost van Dinther1, Erwin Offeciers1, Floris L Wuyts3, Robby Vanspauwen1
1European Institute for ORL-HNS, NKO Dienst Sint-Augustinus Hospital GZA, Wilrijk, Belgium; 2Department of Radiology, GZA Hospitals Antwerp, Wilrijk, Belgium; 3Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Research background: The clinical profiles of patients with Menière’s disease (MD) are variable, leading to complicated differential diagnostics with other vestibular disorders. In order to improve the diagnostic accuracy, imaging-based classification systems have been developed for identifying endolymphatic hydrops (EH). However, the question is raised to which extent the EH is associated with the (residual) peripheral function of the auditory and vestibular system. In the past, the relationship between several imaging-based grading systems and the results of cochleovestibular function tests has been investigated with variable results. Recently, Bernaerts et al. (2019) proposed a modified classification system for endolymphatic hydrops and perilymphatic enhancement on MRI after a 4 h delayed gadolinium administration. The current study was designed to define to which extent this classification system is related to cochlear or vestibular dysfunctions, measured through standard auditory and vestibular tests.
Methods: Seventy-eight patients underwent radiological and cochleovestibular work-up. Pure Tone Audiometry with averages of 500, 1000, and 4000 Hz (i.e. PTA), and 125, 250, and 500 Hz (PTA Low), caloric irrigation, cervical vestibular evoked myogenic potentials, and video head impulse test were retrospectively compared between the grades of endolymphatic hydrops (EH) and perilymphatic enhancement (PE) on MRI.
Results: Significant differences were only found for low frequency PTA between cochlear EH grades I and II (p = 0,036; Grade I: mean (Standard Deviation, SD) = 51 decibel Hearing Level (dB HL) (18 dB HL); Grade II: mean (SD) = 60 dB HL (16 dB HL)), and vestibular EH grades 0 and III (p = 0,018; Grade 0: mean (SD) = 43 dB HL (21 dB HL); Grade III: mean = 60 dB HL (10 dB HL)). The ipsilateral caloric sum of ears with vestibular EH grade I was increased with regards to vestibular EH grades 0 (p = 0,001), II (p < 0,001), and III (p < 0,001) (n = 6; Grade 0: mean (SD) = 24°/s (15°/s); Grade I: mean (SD) = 47°/s (11); Grade II: mean (SD) = 21°/s (13°/s); Grade III: mean (SD) = 16°/s (8°/s)).
Conclusions: According to these results we can conclude that 1) only the highest grades of cochlear and vestibular EH seem to be associated with decreased cochleovestibular functioning; and 2) vestibular test parameters might not be suitable for diagnosing MD.
5.- FP1196Comparison between 3D SPACE FLAIR and 3D TSE FLAIR in Menière’s Disease
Floris Wuyts2,3, Anja Bernaerts1, Nick Janssen1, Cathérine Blaivie3, Robby Vanspauwen3, Joost van Dinther3, Andrzej Zarowski3, Erwin Offeciers3, Filip Deckers1, Jan W. Casselman1,4, Bert De Foer1
1Department of Radiology, GZA Hospitals Antwerp, Oosterveldlaan 24, 2610 Wilrijk, Belgium; 2Lab for Equilibrium Investigations and Aerospace, Universiteitsplein 1, 2610 Wilrijk, Belgium; 3European institute for ORL-HNS, GZA Hospitals Antwerp, Oosterveldlaan 24, 2610 Wilrijk, Belgium; 4Department of Radiology, AZ Sint-Jan Hospital, Ruddershove 10, 8000 Bruges, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Purpose: Meniere’s disease has become more and more identifyable over the past years by means of the so called MRI Hydrops scans which are based on delayed Gadolinium contrast scans. Heavily T2-weighted 3D FLAIR sequence with constant flip angle (CFA) has been reported as being more sensitive to low concentrations of Gd enabling endolymphatic hydrops visualization (EH). The purpose of this study was to compare contrast-to-noise ratio, detection rate of EH and degree of perilymphatic enhancement (PE) as well as diagnostic accuracy in detecting definite MD, using 3D-SPACE FLAIR versus conventional 3D-TSE FLAIR.
Methods: This retrospective study included 29 definite MD patients who underwent a 4-h delayed IV Gd-enhanced 3D-TSE FLAIR and 3D-SPACE FLAIR MRI between February 2019 and February 2020. MR images were qualitatively and quantitively analyzed twice by 2 experienced head and neck radiologists. Qualitative assessment included evaluation of cochlear and vestibular EH and visual comparison of PE. Quantitative assessment of PE was performed by placing a region of interest (ROI) and ratio calculation in the basal turn of the cochlea and the brainstem.
Results: The intra- and inter-reader reliability for grading of EH and PE was excellent (0.7<kappa<0.9) for 3D-SPACE FLAIR and exceeded the values for 3D-TSE FLAIR (0.5<kappa<0.9) The combination of endolymphatic hydrops and visual PE has the highest diagnostic accuracy for detection of definite MD on 3D-SPACE FLAIR with a sensitivity of 0.91 and a specificity of 0.98 with a raise in sensitivity of 6% compared to 3D-TSE FLAIR.
Conclusion: 4-h delayed IV Gd enhanced 3D-SPACE FLAIR sequence has a higher sensitivity and reproducibility than 3D-TSE FLAIR for the visualization of EH and increased PE in definite MD patients.
6.- FP1197Interobserver agreement and clinical correlation of different visual grading scales in the MRI evaluation of endolymphatic hydrops and vestibular hydrops herniation towards the horizontal semicircular canal
Pablo Dominguez1, Ana Ezponda1, Patricia Malmierca1, Marta Calvo1, Alba Igual1, Victor Suarez2, R. Garcia de Eulate1, Raquel Manrique1, Nicolas Perez2
1Clinica Universidad de Navarra Sede de Pamplona; 2Sede de Madrid
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Purpose
- To analyze the degree of inter-observer agreement on the detection and grading of endolymphatic hydrops (EH) with different visual scales.
- To correlate MRI findings with pure tone audiometry (PTA) and caloric test.
- To evaluate if vestibular EH herniation towards the non-ampullary end of the horizontal semicircular canal (HSC) correlates with canal paresis in the ipsilateral HSC and/or with dissociation between the caloric test (abnormal result) and vHIT (normal result).
Methods and Materials: 75 patients, diagnosed of unilateral definite Meniere’s disease, undergoing 3T-MRI of the inner ear were retrospectively recruited after Ethics Committee approval. Cisternography, T2-FLAIR and REAL-IR imaging were performed 4 hours after intravenous contrast administration. Two independent radiologists blinded to clinical data analyzed images. Vestibular EH was evaluated using 4-stage (none/mild/moderate/severe), 3-stage (none/moderate/severe) and 2-stage (none/present) visual scales. Three-point (none/present/severe) and two-point (none/present) scales were employed for cochlear EH assessment. Discrepancies were solved by consensus. Inter-observer agreement was evaluated with weighted-kappa (w-K) statistics. The association of PTA and caloric test with MR findings of EH with the different visual scales was analyzed with one-way ANOVA (p<0.05).
One radiologist evaluated herniation of the vestibular EH towards the non-ampullary end of the HSC of the clinically affected side, blinded to other data. Association between herniation (present or absent) and percentage of canal paresis was analyzed with a Student’s t-test, and versus caloric-vHIT dissociated response with Chi-square test (p<0.05).
Results: Out of 75 patients, we identified EH in 90.6% of the clinically affected ear and in 17.3% on the silent side. Substantial or excellent inter-observer agreement was found in all cases (mean w-K=0.83; range 0.7-0.91). Agreement was almost perfect with the 4-point vestibular EH scale (0.91±0.1). For cochlear EH, the highest consistency was obtained with the 2-point-scale (0.76±0.1). A statistically significant association was found between PTA and vestibular and cochlear EH, with all the scales. The strongest association was observed with the 2-stage cochlear (49.5±22vs25.4±21.5, F=45.1, p<0.001) and vestibular EH (54.8±20.1vs27.1±21.2, F=64.9, p<0.001) grading systems. Caloric test was also associated with 2-stage and 4-stage vestibular EH scales (F=4.5, p=0.034 and F=2.9, p=0.035, respectively). Significant association was found between vestibular HE herniation and HSC caloric paresis (p<0.001) and caloric-vHIT dissociation (p<0.001).
Conclusion: 4-stage vestibular EH grading system gave the best inter-observer consistency. Vestibular and cochlear EH detected by MRI were associated with PTA and caloric test, especially with the 2-scale grading system. Vestibular EH herniation was strongly associated with HSC paresis and caloric-vHIT dissociation.
OC15
1.- FP0903“Comparison of the Effects of Galvanic and Pulsatile Stimulation on Vestibular Afferents in-silico”
Current vestibular prostheses use pulsatile electrical stimulation to elicit neural activity in vestibular afferents. Pulse rate modulation results in limited evoked vestibulo-ocular reflex eye responses in patients suffering from vestibular disorders. We developed a detailed computational model of vestibular afferent extracellular electrical stimulation. The results predict complex interation between pulse-evoked responses and spontaneous activity. We observed in-silico that pulses can facilitate new action potentials, interfere with spontaneous action potentials, and facilitate and block themselves from producing additional action potentials. We characterized these interactions and found that there is a non-linear but predictable relationship between pulse parameters and induced firing rate. We described the predicted firing rate mathematically as a function of pulse amplitude, pulse rate, and the spontaneous firing rate of the vestibular afferent being stimulated. These results agree with previously published rhesus macaque experimental data and are predictive of the reduced vestibulo-ocular reflex observed in the clinic. Using the non-linear equations, pulse parameters can be chosen to create the optimal pattern for producing a firing rate modulation in an afferent. However, because afferents vary in their spontaneous activity, the findings suggest that individual vestibular afferents will be affected differently by the train of pulsatile stimulation.
Using the same biophysical model, we studied the effects of galvanic vestibular stimulation (GVS) on individual vestibular afferents. Experiments show that the amplitude of GVS has a nearly linear relationship to the firing rate produced in a targeted vestibular afferent and can modulate vestibular afferent firing up or down within the full natural range. The biophysical modeling suggests the difference in effects is due to a fundamental difference in how GVS interacts with afferents and hair cells. Our simulations suggest that GVS modulates the sensitivity of the afferent to incoming EPSCs, which allows for smooth nearly-linear modulation of firing rate with current amplitude. Additionally, we found a transient change in firing rate to steps of GVS. This could be modeled accurately at various current levels by assuming changes in vesicle release rate from the hair cell proportional to GVS amplitude. This result suggests that GVS could be affecting the hair cell in concert with the afferent membrane potential. The model predicts that if GVS works in this way it should affect afferent firing rate across vestibular populations in the same way. Together, these findings provide an explanation for differences in the vestibulo-ocular reflex produced by each form of stimulation in experimental data.
2.- FP0939MRI Spectroscopy Analysis of GABA and Glutamate Levels in Bilateral Auditory Cortex: A Case-Control Study in Tinnitus
Tobias Kleinjung1,2, Benjamin Isler1,2, Niklaus Zölch3, Philipp Stämpfli4, Martin Meyer5, Patrick Neff6,7,8
1Department of Otorhinolaryngology, Head & Neck Surgery, University Hospital Zurich, Switzerland; 2University of Zurich, Switzerland; 3Institute of Forensic Medicine, University of Zurich, Switzerland; 4MR-Center of the Department of Psychiatry, Psychotherapy and Psychosomatics and the Department of Child and Adolescent Psychiatry and Psychotherapy, Psychiatric Hospital, University of Zurich, Switzerland; 5 Neuropsychology Division, Department of Psychology, Zurich, Switzerland; 6Department of Psychiatry and Psychotherapy, University of Regensburg, Germany; 7Center for Cognitive Neuroscience (CCNS), University of Salzburg, Austria; 8University Research Priority Program “Dynamics of Healthy Aging”, University of Zurich, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and Aim: MRI Spectroscopy allows for quantification of neurotransmitter concentration levels in predefined brain regions. The method therefore qualifies to better understand neurochemical and neuroplastic changes related to tinnitus as well as to identify possible targets for pharmacological interventions. Previous studies have demonstrated lowered GABA levels in tinnitus patients vs. healthy controls using a MEGA-PRESS sequence and a reduction of glutamate (Glu) levels after transcranial magnetic stimulation (TMS) using a STEAM sequence. The aim of our study was to extend, complement and replicate former findings, mainly with respect to GABA and Glu by applying a JPRESS sequence.
Methods: 20 right-handed tinnitus patients with no hearing impairment and 20 case-matched controls were recruited from the University Hospital of Zurich (5 females per group).
A comprehensive set of variables comprising audiometry as well as tinnitus-related, hyperacusis, health, quality of life, and stress questionnaires was assessed. Metabolite concentration levels were measured in bilateral target voxels covering the primary auditory cortex in a 3-T MRI scanner. Spectroscopy data was analyzed using a modified version of the ProFit toolbox in Matlab. Statistics on extracted metabolite concentration levels relative to creatine were calculated in R.
Results: There were no significant differences between the groups with regards to matching variables, namely age, sex, hearing loss, hyperacusis, health, stress and quality of life (p > 0.1). MRI spectroscopy results indicated a lower Glu concentration in right auditory cortex of the tinnitus group and a trend of reduced GABA concentration in the left auditory cortex.
Conclusion: These results are novel given that it was the first study to quantify cortical Glu concentrations in humans. Within the tinnitus group, Glu levels positively correlated with tinnitus loudness measures whereas no meaningful correlations were found for tinnitus duration or GABA. While the GABA finding is in line with former findings and theories about a dysfunctional auditory inhibition system in tinnitus, the reduced Glu levels came as a surprise and is discussed under a putative framework of inhibitory mechanisms related to Glu throughout the auditory pathway. Our results help to differentiate and extend former findings in MRI spectroscopy of tinnitus with a well-matched case-control design.
3.- FP1014Mapping the vestibular cortex using intracerebral stimulation in patients with epilepsy
Christophe Lopez1, Zoé Dary1, Samuel Medina2, Stanislas Largarde2, Fabrice Bartolomei2
1Laboratoire de Neurosciences Cognitives, CNRS and Aix-Marseille University, Marseille, France; 2Aix Marseille University, APHM, INSERM, INS, Inst Neurosci Syst, Timone Hospital, Epileptology Department, Marseille, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The present study provides a functional mapping of vestibular responses in the human cerebral cortex. We retrospectively analyzed all clinical manifestations induced by direct electrical stimulation of the cerebral cortex and subcortical structures in patients with epilepsy. A cohort of 329 pharmaco-resistant patients with epilepsy underwent stereo-encephalography (SEEG) for presurgical evaluation of epilepsy between August 2000 and September 2020. 254 left hemispheres and 260 right hemispheres were implanted. A total of 10,106 high frequency electrical stimulations (50 Hz) have been applied in these patients, evoking 2,320 clinical responses (e.g. somatosensory or visual illusions, motor or autonomic responses). Vestibular responses represented 5% of the evoked responses and were found in 46 patients. The most common vestibular sensations were sensations of dizziness and vertigo, followed by sensations of swaying, sensations of floating/rising in the air, sensations of rotations and of falling. Vestibular sensations were mostly obtained after electrical stimulation of the inferior parietal cortex, posterior insula, cingulate cortex and superior temporal neocortex. Vestibular responses were most often evoked by stimulation of the right cerebral hemisphere. The present results add to the understanding of the multisensory vestibular cortical network with another functional mapping technique than fMRI.
4.- FP1244The effect of previous spaceflight on otolith-mediated ocular counter-roll in cosmonauts after long duration spaceflight
Catho Schoenmaekers1, Ludmila Kornilova2, Dmitrii Glukhikh2, Gilles Clément3, Hamish MacDougall4, Ivan Naumov2, Chloë De Laet1, Leander Wille1, Steven Jillings1, Floris Wuyts1
1Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Belgium; 2Institute of Biomedical Problems, Moscow, Russia; 3Lyon Neuroscience Research Center, University of Lyon, Lyon, France; and 4University of Sydney School of Psychology, Sydney, New South Wales, Australia.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
INTRODUCTION The ototlith system plays an essential role in the estimation of verticality, where an otolith driven eye movement, the ocular counter-roll (OCR), is important to ensure gaze stabilization, as the eyes tilt in the opposite direction to the direction of the head tilt. Long duration spaceflight exposure to microgravity, as experienced aboard the International Space Station (ISS), will cause a deconditioning of the otolith system. As a result, cosmonauts will experience balance disorders and problems with gaze stabilization after returning in Earth. The aim of this study is to measure the effect of long-term spaceflight on the otolith-mediated OCR, in cosmonauts, with focus on the difference between first time flyers versus frequent flyers.
MATERIAL AND METHODS 44 cosmonaut experiments were performed, first time flyers (1F, N=13) and frequent flyers (FF, N=31), were exposed to off-axis centrifugation before and after their 6-month space mission to the ISS. The OCR induced by the Visual and Vestibular Investigation System (VVIS) mini centrifuge was assessed and recorded for 20 seconds at a maximal velocity of 254°/s, out of a total duration of 5 minutes centrifugation. The OCR measurements were further statistically analyzed in SPSS, with p<0,05 as significance threshold.
RESULTS We found a significant decrease in OCR early postflight (R+1/4, one to four days after return) for both the 1F group and the FF group. The post-flight OCR decrease in the 1F group was significantly different from the FF group with a greater reduction in the 1F group. A full recovery was seen nine to twelve days after their return (R+9/12) (Figure 1).
Figure 1
Visual representation of BDC1, BDC2, R3/5 and R9/11 for the CCW centrifugation. On the x-axis, BDC1 and BDC2 indicates preflight measurements, R3/5 indicates measurement timepoint three to five days after landing and R9/11 nine to eleven days after landing. The y-axis represents the average OCR for these measurement time points. 1F, first-time flyers and FF, frequent flyers.
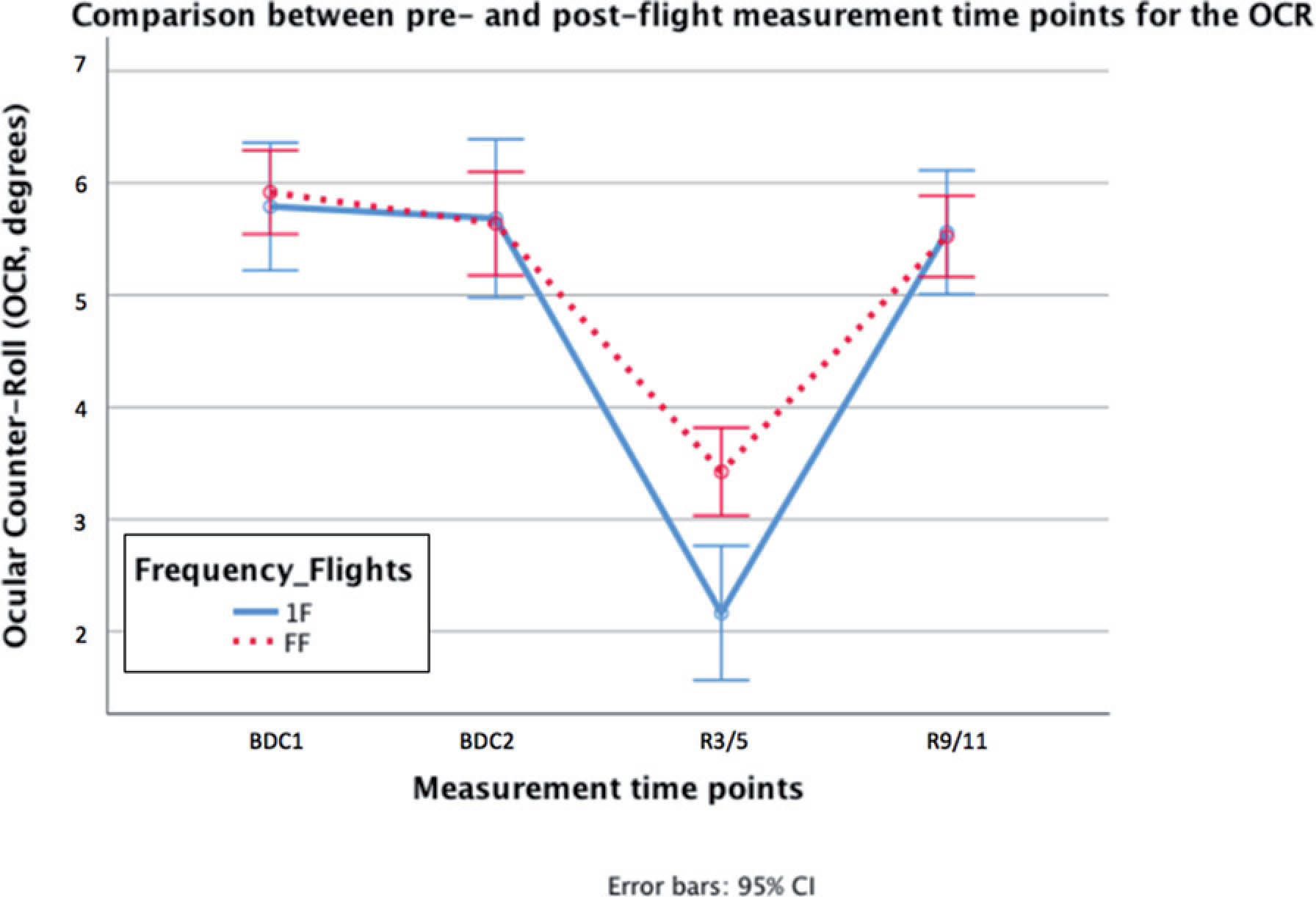
CONCLUSION The FF group suffered less from a deconditioning of the otoliths, because they may have acquired a central adaptation from previous space missions. The results argue for that for important missions, e.g. to the Moon and Mars, it is more advisable to send experienced cosmonauts or astronauts because they are noticeably less affected by microgravity regarding the vestibular system.
5.- FP1245The impact of long-duration spaceflight on the horizontal Vestibulo-Ocular Reflex (hVOR)
Chloë De Laet1, Ludmila Kornilova2, Dmitrii Glukhikh2, Catho Schoenmaekers1, Hamish MacDougall3, Steven T. Moore4, Ivan Naumov2, Leander Wille1, Steven Jillings1, Floris Wuyts1
1Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Belgium; 2Institute of Biomedical Problems, Moscow, Russia; 3Lyon Neuroscience Research Center, University of Lyon, Lyon, France; 4University of Sydney School of Psychology, Sydney, New South Wales, Australia.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
INTRODUCTION The Semi-Circular Canals (SCCs) and the Otoliths are the two main organs of the vestibular system responsible for balance and gaze-stabilization. Weightlessness impacts the otolith organs, the main gravity detectors, which is evident from the decreased otolith-mediated ocular counter roll reflex observed after spaceflight. However, as the SCCs are not gravity-dependent, it is expected that a prolonged stay in microgravity would not affect the vestibulo-ocular reflex (VOR) generated by the SCCs. But little is known about the intricate interplay between the otoliths and the canals. Despite the number of studies that have tried to reveal the effect of microgravity on the SCCs through VOR measurements in the past decades, most of those studies were strongly limited by a restricted sample size and short-duration missions. This study aims to characterize the hVOR changes before and after a long duration spaceflight (>6 months) in an unprecedently large cohort of 44 pre- and post-flight vestibular measurements in cosmonauts.
MATERIAL AND METHODS 44 pre- and post-flight measurements were performed, of which 13 were from first time flyers (1F group) and 31 were from frequent flyers (FF, N=31), by exposing cosmonauts to off-axis centrifugation before and after their 6-month space mission to the ISS. This study was conducted between ISS expedition 16 (2007) and ISS expedition 61 (2020). The hVOR induced by the Visual and Vestibular Investigation System (VVIS) mini centrifuge was assessed and recorded with infrared googles during a 30-second acceleration phase until the maximum velocity of 254°/s was reached. Extraction of nystagmi and associated computations of Slow-Phase Velocity (SPV) and Time Constant (Tc) were made using a custom MatLab routine (Fig.1). The Time Constant of hVOR was then further statistically analyzed in SPSS (V.27), using a linear mixed-model with p<0.05 as significance threshold.
Figure 1
Processing of the horizontal position of the eye. Horizontal position of the eye in degrees in the first row, slow phase of the nystagmus in blue and fast phase in green, Angular speed of the VVIS (w) (°/s2) in the second row, Slow Phase Velocity (SPV) of the eye (°/s) in the third row and the Log transform of the SPV in the last row.
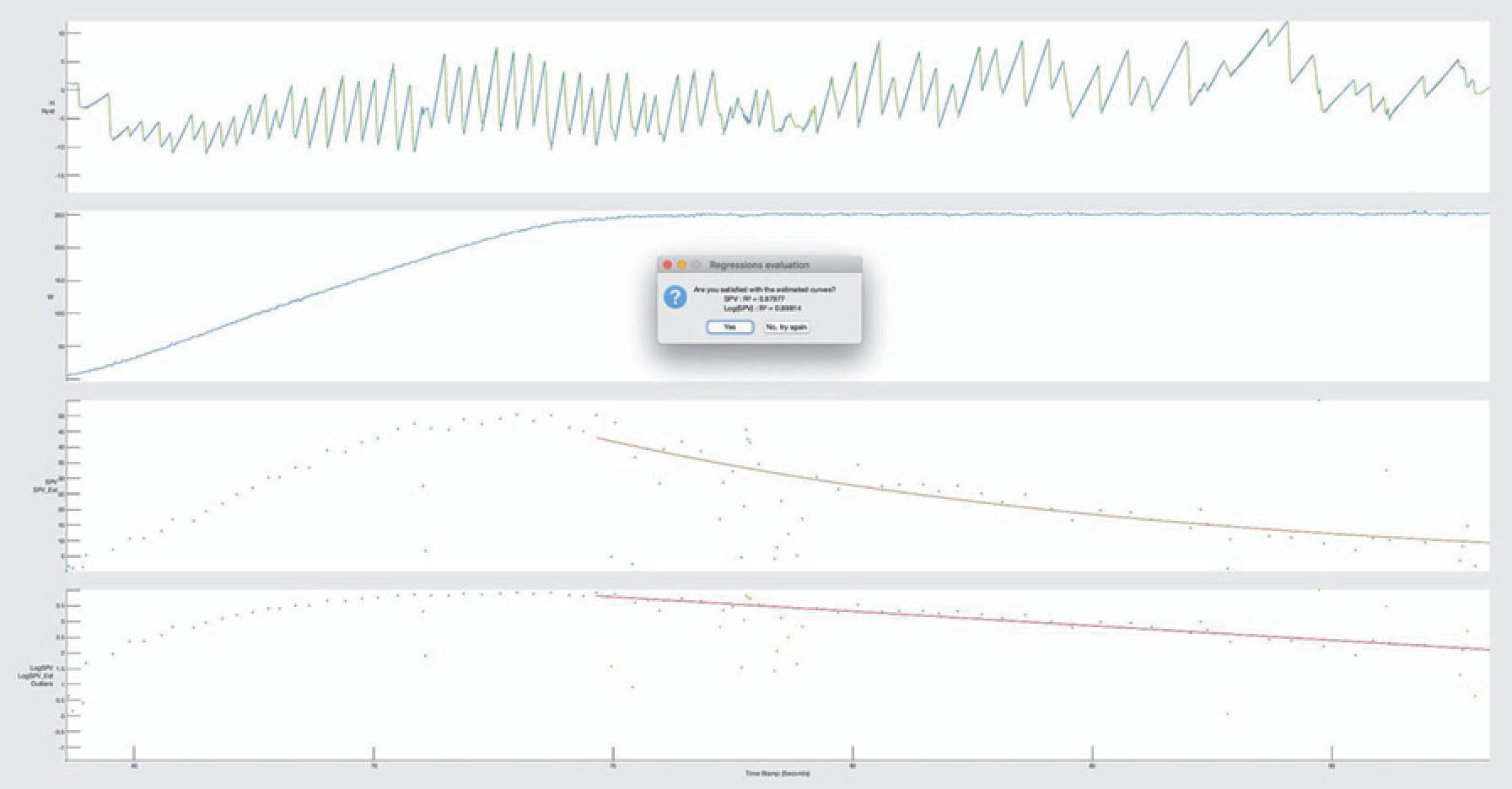
RESULTS We found a significant decrease in hVOR time constant Early postflight (R+3) and Late postflight (R+9) compared to preflight (p<0.001). A partial but incomplete recovery was seen nine days after the return of the cosmonauts (Late postflight R+9) (Fig. 2).
Figure 2
Comparison of the Time Constant values for hVOR preflight and respectively early and late postflight during CCW centrifugation acceleration. Preflight are measurements acquired before launching, Early postflight and Late postflight measurements are respectively acquired 3 and 9 days after landing. The y-axis depicts the average hVOR Time Constant for these timepoints. Preflight vs Early postflight and Preflight vs Late postflight comparison were significantly different (p<0.001).
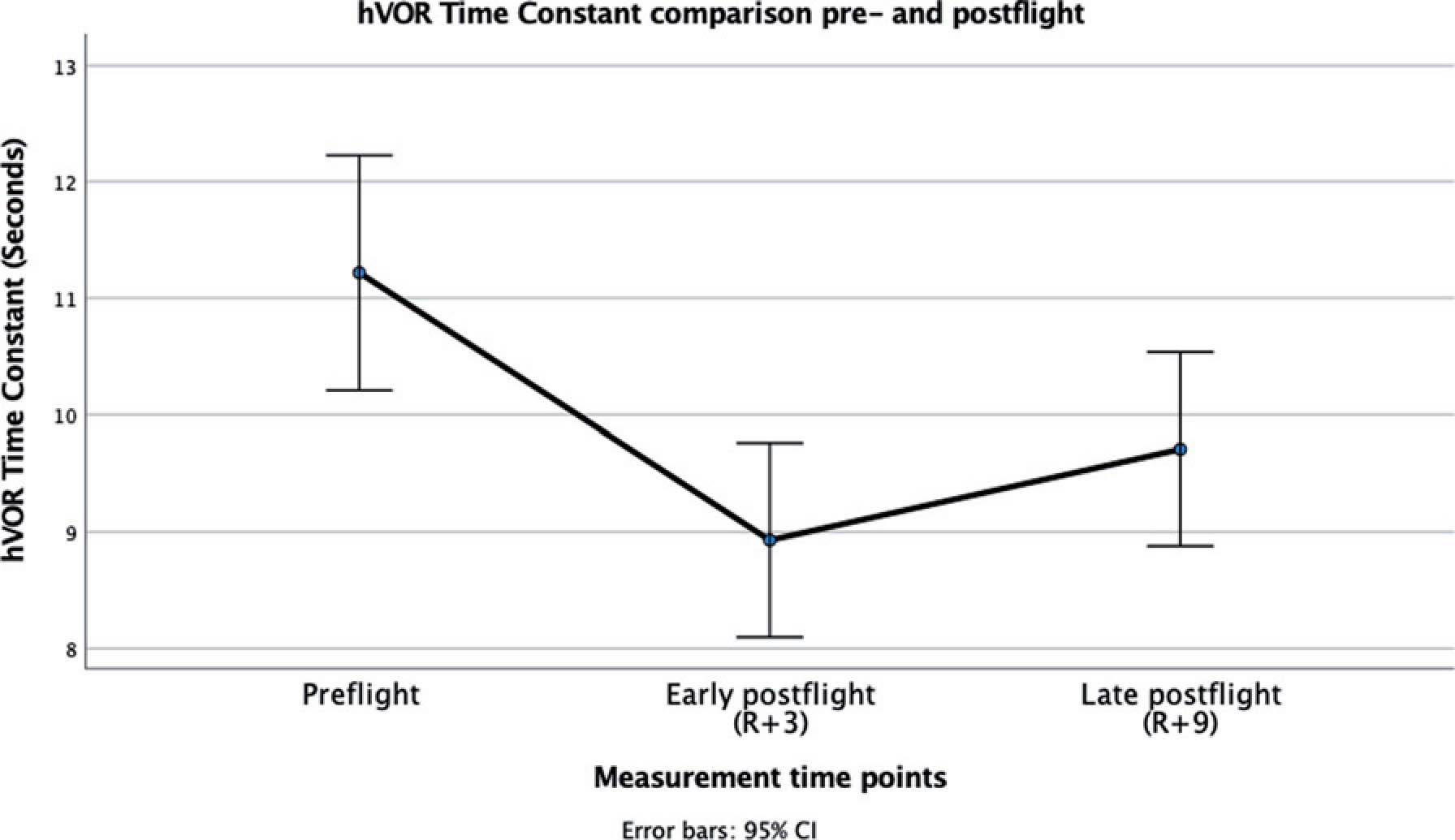
CONCLUSION For the first time, our large sample size allowed us to reveal a significant effect of spaceflight on the hVOR. The time constant values measured in cosmonauts are in the physiological range. These findings show an interaction between the otoliths and the canals. Our hypothesis is that the effect shown after spaceflight on both the otolith and the canals are centrally mediated rather than peripheral.
6.- FP1375Functional Connectivity Characteristics of Vestibular, Visual and Multisensory Cortex in Fighter Pilots Exposed to Gravity Level Alterations
Wilhelmina E. Radstake1, Steven Jillings2, Angelique Van Ombergen3, Floris Wuyts2
1Environment, Health and Safety, Radiobiology Unit, Belgian Nuclear Research Center SCK CEN, Mol, Belgium; 2Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Antwerp, Belgium; 3Department of Translational Neurosciences - ENT, University of Antwerp, Antwerp, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Vestibular signaling is dependent on the presence of a gravity force, serving as a vertical reference frame to detect head and whole-body tilts. How the brain processes vestibular signals with gravity alterations remains poorly understood. This study investigated the effects of frequent g-level transitions and high g-levels on neuroplasticity by comparing fighter jet pilots to matched controls.
We acquired resting-state functional magnetic resonance imaging data to assess differences in brain functional connectivity (FC) between fighter pilots and controls. Both hypthesis-free whole-brain and hypthesis-driven region-of-interest (ROI) analyses were performed. The first ROI was defined in the right parietal operculum 2 (OP2), which is a main cortical hub for processing vestibular information. The second ROI was defined in a specific region of the right angular gyrus (AG), which was previously shown to have suppressed global functional connectivity after gravity alterations induced by parabolic flight.
Our results reveal decreased whole-brain connectivity of the left inferior frontal gyrus (IFG) in fighter pilots compared to controls. The left IFG showed decreased FC with the medial superior frontal gyrus. Connectivity increased between the right OP2 and the left visual cortex, and between the right AG and the left AG in pilots compared to controls.
These findings suggest that visual and vestibular information is differentially processed in the brains of fighter pilots compared to non-pilot controls. We suggest that these results reflect neuroplasticity as an adaptive response to increased exposure to sensory conflicts during flight. Stronger interhemispheric angular gyrus connectivity may reflect multisensory integration changes. Altered connectivity in frontal areas may rather be associated with cognitive strategies that are specific to the challenging tasks that are presented to pilots during flight. Altogether, we provide novel insights into neuroplastic mechanisms of spatial sensory information processing induced by g-level transitions. Such findings may have downsteam applications to studying (adaptation to) vestibular disorders and to investigating the vestibular adaptations of space travelers to microgravity.
OC-16 1.- FP0868Research to Practice: Treatment of Mal de Debarquement Syndrome in a Computerized Assisted Rehabilitation Environment
Carrie W. Hoppes1, Michael Vernon2, Rebecca L. Morrell3, Susan L. Whitney4
1Army-Baylor University Doctoral Program in Physical Therapy, Fort Sam Houston, Texas, USA; 2Center for the Intrepid, Department of Rehabilitation Medicine, Brooke Army Medical Center, Fort Sam Houston, Texas, USA; 3Physical Therapy Services, Brooke Army Medical Center, Fort Sam Houston, Texas, USA; 4 Department of Physical Therapy, University of Pittsburgh, Pittsburgh, Pennsylvania, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and Purpose: Individuals with Mal de Debarquement Syndrome (MdDS) describe symptoms of swaying, rocking, and/or bobbing after sea or air travel. Other symptoms can include disorientation, impaired cognition, ataxia, fatigue, insomnia, headache, anxiety, and depression. These symptoms may be the result of maladaptation of the vestibulo-ocular reflex (VOR) to roll of the head during rotation. Dai and colleagues developed a treatment paradigm that involves passive roll of the patient’s head while watching optokinetic stripes in yaw, resulting in adaption of the VOR and improvement of MdDS. The purpose of this case study is to describe replication of this treatment paradigm in a virtual reality environment with successful resolution of symptoms in two visits.
Case Study: A 39-year-old female reported swaying and rocking after returning from a seven-day cruise. Bedside assessment of the vestibular system was normal. Her Hospital Anxiety and Depression Scale score was 13 for anxiety and 4 for depression, and her Dizziness Handicap Inventory score was 30. Her pre-treatment severity of MdDS was rated as 1 (0 asymptomatic to 10 most severe). The patient was treated with two sessions in the Computerized Assisted Rehabilitation Environment (CAREN) (Motek Medical, Amsterdam, Netherlands). Her head was passively rolled at 50 bpm (first visit) or 60 bpm (second visit) while watching optokinetic stripes in yaw moving from right to left for 5 minutes (Figure 1). She then walked on the right-hand sidewalk of a virtual reality city scene at 0.85 m/s for 10 minutes, with head turns to identify objects in the scene (Figure 2). During the second visit, medial-lateral perturbations of the visual surround were introduced during this walking task.
Figure 1.
Optokinetic stripes in a Computerized Assisted Rehabilitation Environment for use during treatment of Mal de Debarquement Syndrome. The patient is seated in the chair during treatment.
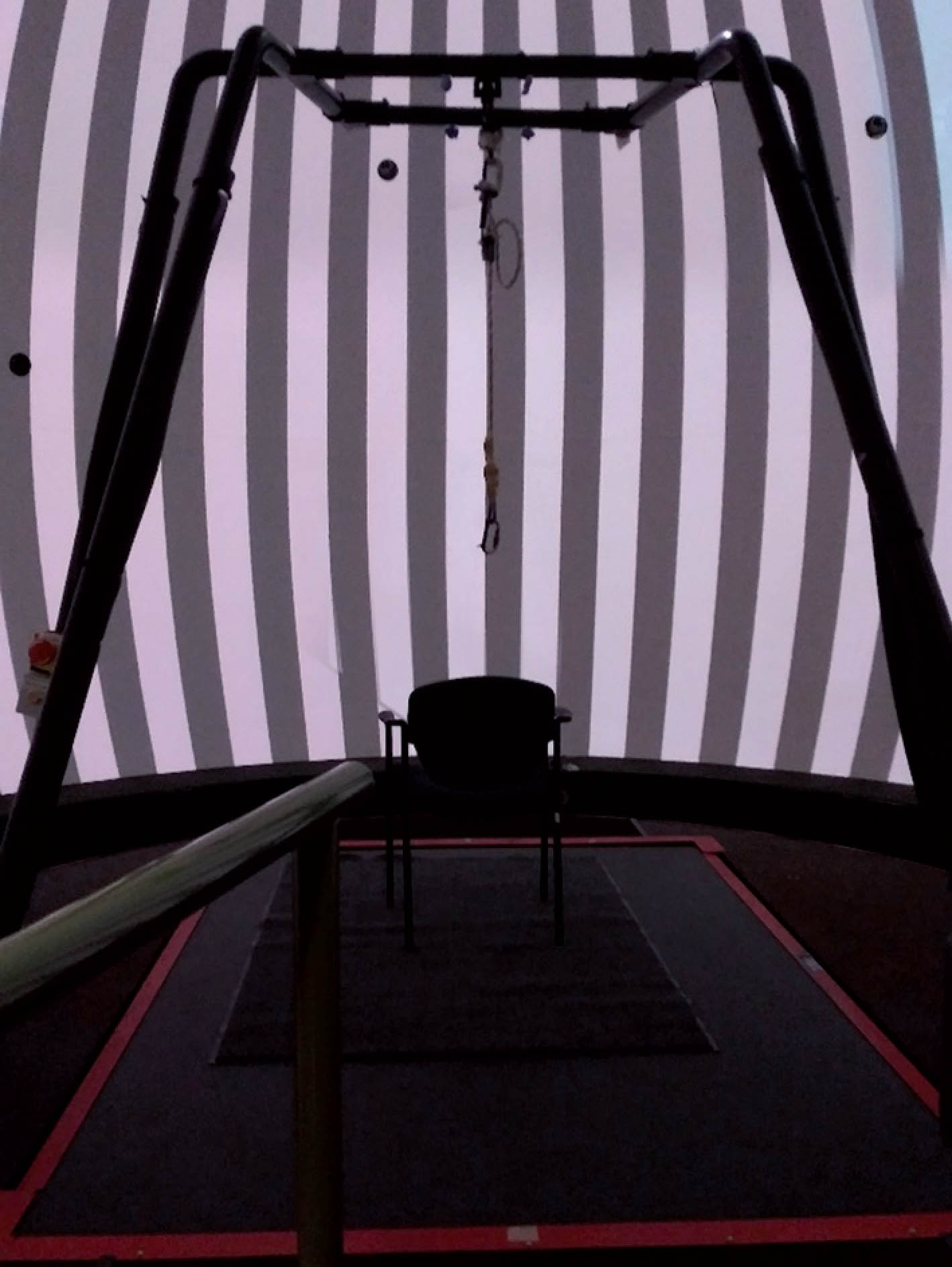
Figure 2.
Virtual reality city scene in a Computerized Assisted Rehabilitation Environment for use during treatment of Mal de Debarquement Syndrome.

Results: Her post-treatment severity of MdDS was rated as 2 (immediately after first visit) and 1 (immediately after second visit). The patient elected to cancel her third visit due to complete resolution of her symptoms (36 days after returning from the cruise). Her Global Rating of Change was +7 (on a 15-point scale of -7 to +7), her severity of MdDS was rated as 0, and her Dizziness Handicap Inventory score was 0. She had returned to all of her previous activity and participation.
Conclusions: This case report is the first to describe use of the CAREN for effective treatment of MdDS by replicating the treatment paradigm developed by Dai and colleagues. Two sessions were effective in resolving symptoms and improving quality of life.
Keywords: Mal de Debarquement Syndrome, Optokinetic, Computerized Assisted Rehabilitation Environment, Virtual Reality
2.- FP1001The vestibular time constant and anti-motion sickness drugs’ efficacy
Daniel Lagami1,2,3, Avi Shupak2,4, Dror Tal1
1Israel Naval Medical Institute, 2Faculy of Social Welfare and Health Sciences, 3Department of Brain Sciences, Weizmann Institute of Science, Rehovot, Israel, 4Unit of Otoneurology, Lin Medical Center, Haifa, Israel
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: Motion sickness is a major constraint for travellers, depending on the means of transport and the ambient conditions. Seasickness is one of the prevalent forms of motion sickness. The efficacy of seasickness drugs is usually tested during exposure to sea conditions in a “trial and error” design. Receptors of the medications scopolamine and meclizine often prescribed for the treatment of motion sickness were identified in the vestibular nuclei, which also determine the time constants (Tc) of the vestibulo-ocular reflex (VOR) nystagmic response. The purpose of the study was to find whether drug-induced changes in the angular VOR (aVOR) Tc might be employed as a bioequivalent for anti-motion sickness drug efficacy.
Subjects and Methods: Subjects were 36 crewmembers suffering from the highest grade of seasickness, who were found to be responsive or non-responsive to scopolamine and meclizine. Seasickness severity was determined using the Wiker seasickness questionnaire. Subjects whose seasickness severity score failed to improve after drug treatment were defined as non-responsive. To be classified as responsive, subjects had to demonstrate a reduction in seasickness severity score by at least three of the seven grades on the Wiker scale. Scopolamine, meclizine or placebo were administered to each subject in a crossover, double-blind design. The aVOR Tc was determined by the rotatory chair Velocity Step test before, one and two hours after drug or placebo administration.
Results: The aVOR Tc was significantly shortened in the scopolamine responsive group two hours post-administration (16.01±3.43 vs. 12.55±2.40 sec, p<0.001), whereas in the non-responsive group there was no significant difference post-treatment (15.45±3.34 vs. 13.84±3.61 sec). No differences were found for the meclizine groups, although a trend towards shortening of aVOR Tc was observed in the responsive group. Placebo had no effect on the aVOR Tc in any of the scopolamine and meclizine groups.
Conclusions: The aVOR Tc constant may be employed as a bioequivalent for scopolamine efficacy, enabling the administration of appropriate treatment without the need for prior exposure to sea conditions. The same study paradigm may be used for the evaluation of anti-vertigo medications, paving the way for personalized treatment.
3.- FP1058Acquired sex-related hormonal differences in motion sickness susceptibility
Yougan Saman1, Angela Bonsu1, Abigail Lee1, Mishaal Sharif1, Peter Rea1, Qadeer Arshad1
1inAmind Laboratory, Department of Neuroscience, Psychology and Behaviour, University of Leicester, Leicester, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Previous research has illustrated strong hormonal related influences upon the evolution of dizziness and nausea in patients with vestibular migraine and during exposure to motion in healthy individuals respectively. Specifically, that is in females there is a close relationship between the menstrual cycle and episodic attacks of vestibular migraine as well as an enhancement in motion sickness susceptibly a few days preceding the mensuration period. However, whether acquired hormonal dysregulation can differentially modulate (males vs. females) motion sickness susceptibility remains unknown. To address this, we recruited 42 males and 42 females with adrenal insufficiency: matched for age, pre-morbid motion sickness susceptibility, aetiology, duration of disease, medication (steroid dosage) and co-morbidities (i.e. diabetes, thyroid disease) and assessed changes in motion sickness pre/post adrenal insufficiency utilising validated questionnaire measures. We observed that in females motion sickness susceptibility significantly increased (almost doubling) following the development of adrenal insufficiency, whereas in males it remained unchanged. Our findings demonstrate that in individuals with acquired adrenal insufficiency, the dysregulation of sex hormones plays a pivotal role in governing susceptibility to motion sickness.
4.- FP1160Evaluation of the effects of optokinetic and rotational stimulus with functional head impulse test (fHIT) in individuals with motion sickness
Ercan Karababa1 Bülent Satar2
1University of Health Sciences, Gulhane Faculty of Health Sciences Department of Audiology; 2Health Sciences University Gulhane Medical Faculty ENT Department
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Motion sickness is a complex syndrome that affects almost everyone at some point in their life, especially with symptoms such as nausea and vomiting. Diagnostic criteria have recently been published by the Bárány Society. However, there is no objective test that reliably determines motion sickness. To evaluate effects of optokinetic stimulus and rotational stimulus in individuals with and without motion sickness with functional head impulse test.
Methods: A total of 70 individuals between the ages of 18-40 were included in the study. 35 individuals diagnosed with motion sickness were assigned to experimental group, and 35 individuals without any vertigo were included in the control group. Functional Head Impulse Test (fHIT) and Motion Sickness Susceptibility Questionnaire (MSSQ) were applied to all individuals in the experimental and control groups. The percentage of correct answer (%CA) with and without optokinetic stimulus (o-fHIT) in the frontal plane with the functional head impulse test was compared in both groups. In addition, experimental and control subjects were seated on an ordinary rotating office chair. %CA was compared in both groups by applying the rotational fHIT (r-fHIT) test after all individuals of the experimental and control subjects were rotated randomly to the right and left. In addition, the Graybiel scale was used to subjectively determine the discomfort experienced by the individuals in the experimental and control groups after rotational stimulus.
Results: There was no significant difference in the percentage of correct answer in fHIT o-fHIT and r-fHIT tests applied in the control group. CA percentages in the fHIT, o-fHIT, and r-fHIT tests applied to the individuals in the patient and control groups were found to be significant in all SCCs except for the right lateral semicircular canal (SCC) and left posterior SCC. A statistically significant difference was found between the experimental and control groups in Graybiel scores (p<0.05). The mean total score of the individuals in the experimental group on the motion sickness susceptibility questionnaire was 28.48 ± 7.62, and the mean total score of the individuals in the control group was 5.26 ± 4.99.
Conclusion: Since individuals with motion sickness are affected by visual and rotational stimuli, the fHIT test performed after these stimuli can be used as a confirming objective test in diagnosing motion sickness.
5.- FP1240Vestibular Migraine in Children
Sudhira Ratnayake1, Rosa Crunkhorn2, John Wong2, Soumit Dasgupta1
1Department of Audiovestibular Medicine and Audiology, Alder Hey Children’s Hospital, Liverpool, UK AND University of Liverpool, UK; 2Department of Audiovestibular Medicine and Audiology, Alder Hey Children’s Hospital, Liverpool, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Vestibular Migraine (VM) and the migraine variants are the commonest causes of episodic vertigo in children. VM is a clinical diagnosis with no specific vestibular diagnostic features or other biomarkers. Whilst there are numerous studies on VM in adult patients, there is a paucity of evidence in paediatric patients, particularly on clinical characterisation. Currently diagnosis and management strategies are largely based on evidence from adult populations. This study aims to describe a large cohort of patients diagnosed with VM at a tertiary Audiovestibular Medicine (Medical Neurotology) Department, describing clinical presentation, examination, diagnosis, and management.
Methods: This is a retrospective electronic case note review of all patients presenting to Audiovestibular Medicine clinics in a tertiary unit between January and December 2018. The diagnostic criteria of VM or its variants was based on the Joint Bárány Society and International Headache Society criteria (2012). All patients, new or follow-up, with a diagnosis of VM or migraine variants during this time were included. Data on the following were analysed: presenting symptoms (including headache and vertigo, other symptoms, medical comorbidities and impact of symptoms); clinical examination findings; diagnostic test findings (including vestibular diagnostics, blood tests and neuroimaging); treatment and overall outcome.
Results: 81 children (Male: Female = 38:43 and age range = 2-17 years) were identified. 30 (37%) had normal examination and diagnostic findings. 20 (25%) had one abnormal finding whilst 31 children (38%) had =2 clinical and/or diagnostic abnormalities. No headache was reported in 29 children, however photophobia and phonophobia were common (68 and 54 children respectively). Abnormal central oculomotor signs were detected in 20 (25%). Neurovestibular signs to assess vestibular angular and gravitational motion sensor function were abnormal in 37 children (45%). In the whole cohort, 21 (26%) had significant semicircular canal abnormalities (low vestibular-ocular reflex (VOR) gain, high VOR gain or saccades in the video head impulse test). Vertical semi-circular canal VOR gains (anterior and posterior) were higher in the migraine group than our hospital norms (p=0.0001). Up to 90% of children who were followed up responded to migraine prophylaxis and about a third showed changes in their neurovestibular tests that were heterogeneous.
Conclusions: There is a high-yield of central and neuro-vestibular features in paediatric VM. The high VOR gain observed in the series appears to be a promising possible biomarker for VM. These findings are useful for clinical correlation at initial and follow-up assessments.
6.- FP1383Endolymphatic hydrops of the inner ear: A common finding in vestibular migraine
Valerie Kirsch1-3, Rainer Bögle1-3, Johannes Gerb1-2, Emilie Kierig1-2, Birgit Ertl-Wagner4-5, Sandra Becker-Bense1-2, Marianne Dieterich1-3,6
1Department of Neurology; 2German Center for Vertigo and Balance Disorders (DSGZ), 3Graduate School of Systemic Neuroscience (GSN), 4 Department of Radiology, Ludwig-Maximilians-University, Munich, Germany; 5Department of Radiology, The Hospital for Sick Children, University of Toronto, Toronto, Canada; 6Munich Cluster for Systems Neurology (SyNergy), Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The clinical differentiation between Vestibular Migraine (VM) and Menière’s Disease (MD) can be complex [1]. This is mainly due to our diagnostic processes’ lack of selectivity [2]. A possible remedy is thought to be the inclusion of intravenous contrast agent enhanced magnet resonance imaging of the inner ear (iMRI), which can permit the in-vivo non-invasive verification of an endolymphatic hydrops (ELH). However, so far, published studies are inconclusive and sparse.
Methods: This more extensive clinical study examined 190 participants, 150 patients with definitive and probable VM (n=75) or MD (n=75) in comparison to 40 healthy controls (HC; patients with no inner ear or neurological symptoms that had to undergo MRI with contrast agent). A multimodal approach included iMRI findings with typical clinical symptoms, behavioral and electrophysiological data. Diagnostic workup included neurologic and neuro-orthoptic assessment, VOG during caloric stimulation, and head-impulse test [vHIT], as well as audiometry. ELH was characterized according to prior published criteria [3]. Volumetric assessment of endolymphatic space (ELS) used a pipeline with deep learning-based segmentation [4] and 3D local thresholding algorithms [5].
Results: The mere verification of the ELH did not prove to be the clear-cut discriminatory diagnostic criterion between VM and MD. However, the pattern of ELH in VM patients differed significantly (p<0.05) when compared to MD patients concerning the extent of degree, volume and uni-/bilateral appearance of both ears. Other highly discriminative characteristics were the occurrence of headache, sensitivity to light and/or noise in VM patients on the one hand, and MD-typical ear symptoms, audiometric deficits and vestibular deficits in caloric or vHIT testing in MD patients on the other.
Conclusion: iMRI helps to discriminate between VM and MD by the ELH pattern, especially in non-clear-cut cases of patients’ history or diagnostic neurophysiological results. In turn, ELH should rather be regarded as a common pathophysiological endpoint of different etiologies than as a discriminatory or pathognomonical mechanism, at least when dealing with VM and MD patients [1,2].
References
[1] Brandt et al. (2022) 3rd ed. Springer-Verlag, London
[2] Oh & Dieterich et al. (2021) Front. Neurol. 12: 594481.
[3] Boegle et al. (2021) Front. Neurol. 12: 647296.
[4] Ahmadi et al. (2022) Front. Neurol. under review
[5] Gerb et al (2020) J Neurol, 267(Suppl 1): 185–196.
Acknowledgments: This work was partially funded by Deutsche Stiftung Neurologie (DSN).
ST04
1.- FP0912Novel Mediation Analysis of the Impact of Vestibular Disruption on Cognition
Jeremy Corcoran1,2, John Golding1, Anthony Towell1, Mark Gardner1
1Department of Psychology, University of Westminster, 115 New Cavendish Street, London W1W 6UW; 2Multidisciplinary Balance Clinic, Guy’s Hospital, Great Maze Pond, London SE1 9RT
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
ABSTRACT:
BACKGROUND: Prevailing theory implies that disruption of cognition is an indirect, mediated consequence of aberrant vestibular information. The objective was to determine if such misinformation can also affect cognition directly.
METHODS: Seventy-eight healthy participants undertook either the ‘Single Avatar Stimulus Set’ (SASS) task, invoking mental self-translocation, or one of two spatial control tasks. All tasks were administered six times, in one-minute trial blocks, after one minute of constant angular velocity (90°/s). Halfway through alternate trial blocks, chair velocity reduced abruptly from 90 to 0°/s, giving rise to aberrant vestibular information. A measure of anxiety, the low frequency-high frequency ratio, was calculated from pulse recordings acquired during all trial blocks. A novel mediation model was applied to test for a direct effect of the aberrant vestibular information on task performance.
RESULTS: Following abrupt deceleration, responses on the SASS task were less cautious as denoted by a significant decrease in boundary separation, a latent performance variable (simple effect: p = .014). The disruption of performance was selective to the SASS task (interaction effect: p = .025), and not secondary to an increase in anxiety according to mediation analyses (direct effect: p = .009).
CONCLUSION: The selective disruption of an aspect of SASS task performance by abrupt deceleration, in the absence of a concurrent disturbance of the physiological state of the participants in the SASS task group, suggests that aberrant vestibular information can affect cognition directly. The mediation model applied in this study could help to stratify domains of cognition in terms of their vulnerability to vestibular disruption.
THEME
The prevailing mechanistic theories imply that vestibular disruption, due to pathology or incongruous environmental conditions, impairs cognition via an indirect mechanism whereby a change in physiological or emotional state outcompetes cognition for limited processing resources. For example, the ‘posture-first principle’ (Gresty and Golding 2009) implies that vestibular disruption disturbs postural stability which leads to a diversion of attention towards postural control processes to the detriment of other cognitive processes. This and other similar principles are analogous to the indirect pathway of a mediator model. Two reviews of note (Smith et al. 2005, Smith and Zheng 2013) try to make a case for a direct, unmediated effect of vestibular disruption on cognition. However, no research to date has employed the appropriate design or analyses to show whether cognitive disturbance can occur even when there are adequate cognitive processing resources. Regression-based path analysis is an accepted means of assessing the indirect, direct and total effects implied by mediator models (Hayes 2013).
This research represents a novel approach to developing our knowledge of the interplay between vestibular and cognitive integrity. The mediation model applied in this study could help to stratify domains of cognition in terms of their vulnerability to vestibular disruption. In turn, we might better appreciate the cognitive domains to focus on during the assessment and rehabilitation of patients with vestibular disorders.
The lead author, Jeremy Corcoran, developed the research theme, inclusive of the mediation model, as part of his PhD studies. The theme stemmed from his 10 years of experience as a vestibular physiotherapist in London, UK. Jeremy successfully defended his PhD thesis during examination by Dr Barry Seemungal (Imperial College London) in May 2019. Jeremy is in the process of writing-up his PhD research for publication. He has presented some of his other findings at the Meeting of the British Society of Neuro-Otology and at the Cognitive Psychology Section Annual Conference of the British Psychological Society.
TARGET AUDIENCE: This presentation should appeal to those academics and clinicians with an interest in vestibular cognition. More specifically, this presentation is targeted at scientists who focus on the higher processing of vestibular information, beyond the main reflexes associated with the peripheral vestibular system.
References
Gresty, M.A. and Golding, J.F. (2009) ‘Impact of Vertigo and Spatial Disorientation on Concurrent Cognitive Tasks’. Annals of the New York Academy of Sciences 1164, 263–267
Hayes, A.F. (2013) Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: The Guilford Press
Smith, P.F. and Zheng, Y. (2013) ‘From Ear to Uncertainty: Vestibular Contributions to Cognitive Function.’ Frontiers in Integrative Neuroscience 7 (November), 1–13
Smith, P.F., Zheng, Y., Horii, A., and Darlington, C.L. (2005) ‘Does Vestibular Damage Cause Cognitive Dysfunction in Humans?’ Journal of Vestibular Research : Equilibrium & Orientation 15 (1), 1–9
2.- FP1010Ocular Vestibular Evoked Myogenic Potentials to high frequencies show semicircular canal dehiscence (SSCD), the effect of rise time
Leonardo Manzari1, Ann M. Burgess2, Ian S. Curthoys2
1MSA ENT ACADEMY CENTER, Cassino(FR), Italy; 2Vestibular research Laboratory, School of Psychology, the University of Sydney, NSW, Australia.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
In 15 patients with CT-verified SSCD, to investigate the effect of frequency on the n10 component of the ocular vestibular-evoked myogenic potential (oVEMP n10) evoked by air conducted sound (ACS) and bone conducted vibration (BCV) at the midline forehead at the hairline (Fz).
Methods: A hand-held Bruel & Kjaer 4810 minishaker provided BCV stimulation, using surface EMG electrodes beneath both eyes, to record oVEMP n10. The stimulus ACS or BCV at either Fz or at the vertex of the skull (Cz) were very short tone bursts ranging from 500 Hz to 8000Hz. 60 healthy subjects were tested in the same paradigm. All the stimuli used in the experiments consisted of a sine wave of 2 ms duration, with a trapezoidal envelope with rise time equal to fall time 0 (zero) ms duration or 2ms rise time.
Results: In response to ACS and Fz BCV from 500 Hz up to 8000 Hz in SSCD patients the oVEMP n10 amplitude beneath the contraSSCD eye was substantially and significantly larger than the oVEMP n10 beneath the ipsiSSCD eye. In normals ACS oVEMPs n10 is present and reproducible up to 1000 Hz while in SSCD ACS oVEMPs n10 is present up to far higher frequencies (8000 Hz).
To Fz BCV oVEMPs n10 is present up to 4000 Hz but only to 1000 Hz in normals. Increasing the rise time reduced or abolished the n10 response at high frequencies.
Conclusion: Testing OVEMP responses to very high frequency with ACS and BCV allows very simple, very fast identification of a probable unilateral SSCD in a manner which is very easy even for junior and senior patients. Particular emphasis should be given to the effect of rise time In summary, our results suggest that the optimum oVEMPs stimulus is a tone burst with a zero rise time.
Reference
1 Burgess AM, Mezey LE , Manzari L., MacDougall HG, McGarvie LA , Curthoys IS Effect of Stimulus Rise-Time on the Ocular Vestibular-Evoked Myogenic Potential to Bone-Conducted Vibration. Ear Hear, 34 (6), 799-805 Nov-Dec 2013
3.- FP1124A clinical test for enhanced auditory sensitivity for body vibrations in superior semicircular canal dehiscence syndrome
Luca Verrecchia1,2, Magnus Vestin1, Aleksandr Velikoselskii1, Karl-Johan Fredén Jansson3, Sabine Reinfeldt3, Bo Håkansson3
1Department of Ear Nose and Throat, Audiology and Neurotology, Karolinska University Hospital, Stockholm Sweden; 2Ear Nose and Throat Unit, CLINTEC Department, Karolinska Institutet, Stockholm, Sweden; 3Biomedical signals and systems research group, Chalmers University of Technology, Gothenburg, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Patients affected by superior canal dehiscence syndrome (SCDS) complain about a specific hypersensitivity for internal body sounds (bone conducted hyperacusis - BCH). They refer to an excessive hearing of cardiac pulse, own voice, breathing, joint movements, borborygmi or sometimes eye movements. BCH may be enhanced to a level compromising sleeping, hearing, social communication and often disturbing the cognitive work. BCH can be treated by surgical resurfacing of canal bone dehiscence. Today BCH is evaluated by questionnaires and a fork test at malleolus - with uncertain diagnostic precision-. BCH is a major complaint in SCDS and may be corrected by surgery, thus an objective CBH measure is worth consideration and clinically requested.
Here we present a new clinical test, developed to obtain a measure of the CBH. It is a psychoacoustic audiometry test in which stimulation is provided by bone vibration at a distant point from the ear, specifically at the malleolus. This method was experimentally proven by our research group (Brantberg K et al, 2016. PMID:28081534), however hard to translate into a clinical environment due to technical shortcomings, mainly using an experimental bone vibrator (Minishaker B&K 4810). In this study we have replicated the results obtained by the previous study, but using the new B250 bone transducer, developed at Chalmers University of Technology (Gothenburg, Sweden) in collaboration with Ortofon A/S (Denmark) and designed for a clinical use (Fredén Jansson KJ et al, 2021. PMID:34267559).
We compared the psychoacoustic hearing thresholds given by a group of 20 SCDS patients with the thresholds of a group of 20 age matched healthy subjects. The subjects were stimulated by the B250 at malleolus with a bone conduction vibration consisting of a pure tone at frequencies 125, 250, 500 and 750 Hz and with intensity 85-135 dB RMS FL. Results showed that SCDS patients heard the bone vibrations at malleolus at a significantly lower intensities than the control group. In particular, the 250 Hz frequency had the best diagnostic accuracy for SCDS according to a receiver operating characteristic analysis. Translating these results in clinical terms, using a B250 stimulation at ankle with a 250 Hz tone delivered at 120 dB RMS FL, it is possible to screen patients who are suffering of SCDS with a sensitivity of 90% and specificity of 80%. And more important, the method is easily scalable at non-experimental audiological facilities, configuring an accessible clinical screening test for SCDS.
4.- FP1213Vestibular Stimulation Targeting the Utricle and Saccule Partially Restores Otolith-Ocular Reflex in Chinchillas after Intratympanic Gentamicin Injection
Celia Fernandez Brillet1, Margaret R Chow1, Kristin N Hageman1, Andrianna I Ayiotis1, Dale C Roberts2, Charles C Della Santina1 3
1Department of Biomedical Engineering; 2Department of Neurology; and 3Department of Otolaryngology–Head and Neck Surgery – all part of Johns Hopkins School of Medicine, Baltimore, Maryland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Driving reflexes such as the otolith-ocular reflex (OOR) to stabilize the eyes during translational motion (e.g., moving forward without rotating) or head tilt with respect to gravity, the otolith end-organs inform the brain about gravitational and linear accelerations. We previously characterized the OOR in normal chinchillas and responses to prosthetic electrical stimulation targeting the utricle and saccule in implanted but otherwise-normal ears. Here we extend that work to examine prosthetically-driven OOR responses in animals with unilateral or bilateral vestibular hypofunction after unilateral ototoxic injury followed by contralateral surgical disruption of the labyrinth.
Methods: Five chinchillas were unilaterally injected with gentamicin in the right ear and developed a head tilt consistent with onset of unilateral vestibular hypofunction. Subsequently, a contralateral lesion was induced in three animals by implanting the intact left labyrinth with electrodes targeting the semicircular canals, utricle, and saccule. OOR responses were recorded using scleral coils in response to static reorientations and linear translations after unilateral gentamicin injection and again after electrode implantation surgery. Responses were compared for mechanical stimulation alone, prosthetic electrical stimulation alone (using stimuli intended to emulate motion stimuli), and combinations of mechanical and electrical stimuli.
Results: Unilateral ototoxic injury decreased OOR response eye movement magnitude by half and increased response latency while maintaining similar response direction and symmetry. Implantation of electrodes in the contralateral ear’s semicircular canals and vestibule further decreased OOR magnitude and increased latencies. During unilateral prosthetic stimulation of stationary animals with a unilateral gentamicin lesion on the right and electrode implantation on the left, eye movements driven by the OOR had magnitudes and latencies closer to normal responses than during mechanical stimulation alone. Combining mechanical and electrical stimuli in phase with each other increased OOR magnitude relative to responses during mechanical motion or electrical stimulation alone. Variability observed in electrically-evoked OOR across chinchillas was corroborated by post-mortem CT images showing variation in electrode position.
Conclusions: Vestibular implants may partially restore the OOR after inner ear injury caused by gentamicin or surgical destructive procedures like those used to treat Meniere’s disease. Despite its potential, this approach heavily depends on surgical precision and accuracy during placement of the electrode arrays near the maculae. Priorities for future studies include reducing variability in surgical technique (to maximize efficacy while minimizing current spread to nontarget neurons) and examining OOR responses of animals after adaptation to long-term motion-modulated electrical stimulation.
Support: NIH R01DC009255, ADC15001001; MED-EL GmbH
5.- FP1247Postural Sway as a Predictor of Volumetric Growth in Untreated Vestibular Schwannoma.
Kathrin Skorpa Nilsen2,3,4, Dhanushan Dhayalan1,4, Morten Lund-Johansen1,4, Stein Helge Glad Nordahl2,3,4; Frederik Kragerud Goplen2,3,4
1Department of Neurosurgery, Haukeland University Hospital, Bergen, Norway; 2Department of Head and Neck Surgery, Haukeland University Hospital, Bergen, Norway; 3Norwegian National Advisory Unit on Vestibular Disorders, Haukeland University Hospital, Bergen, Norway; 4Department of Clinical Medicine, University of Bergen, Norway.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Target audience for this abstract is otoneurologists and otosurgeons interested in postural balance, dizziness and management of small to medium-sized vestibular schwannoma.
Background: Small and medium-sized vestibular schwannomas are often observed with serial imaging and treated only if evidence of growth. Approximately one in three tumors will grow within three years after diagnosis, but no reliably baseline parameter has been found to predict tumor growth.
Methods: Patients with untreated vestibular schwannoma selected to a wait-and-scan protocol were included. Baseline data contained measurement of postural sway on a force platform (steady/unsteady), history of unsteadiness, tinnitus or dizziness (yes/no), audiometry (pure tone average on tumor side) and bithermal caloric test (canal paresis yes/no). Relative tumor growth (%) and volume-doubling time were quantified based on tumor volume at the diagnostic MRI and a control scan within the following three years.
Results: Out of 204 patients initially managed with a wait-and-scan policy, 104 of them had a significant tumor growth (relative growth >20%) within the period of observation. Mean follow-up time was 2.3 years (range 0.5 – 3.7). Median tumor volume was 0.32 cm3 (range 0.02-4.79). Unsteadiness on posturography were found in 53 (26%) of the patients. Significant tumor growth was found in 77 % of unsteady patients and 42 % of steady patients. Using multivariate regression analysis, unsteady patients had an odds ratio of 5.6 (95% CI 2.6-11.8) for significant tumor growth within three years. The analysis was adjusted for age, sex, symptoms, clinical and radiological parameters at baseline.
Conclusions: This study is the first to find an objective predictor of future vestibular schwannoma growth. Our results might be useful for clinicians to recognize patients with higher odds for tumor growth and thereby improve timing of treatment and monitoring of the individual patient.
6.- FP1266Structural and functional neuroplasticity following bilateral vestibular loss: a longitudinal [18F]-UCB-H/ [18F]-FDG dual tracer rat study
Melissa Antons, Magdalena Lindner, Maximilian Grosch, Sibylle Ziegler, Marianne Dieterich, Andreas Zwergal
German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Lesion-induced adaptive neuroplasticity is a general principle across mammalian species, which supports functional recovery and is an attractive target for therapy. Several mechanisms from single neuron to network level are involved, which develop at different speeds. Rapid-onset functional plasticity consists of altered neuronal excitability, while structural plasticity, e.g., by synaptic reorganization, may arise with a longer time constant.
Methods: The current study applied a methodological approach based on serial [18F]-UCB-H and [18F]-FDG measurements before and 1, 3, 5, 7, 9 weeks after bilateral labyrinthectomy in two groups of rats (with and without locomotor training). The general purpose was to depict both the spatial distribution and temporal scale of functional plasticity, estimated by regional glucose metabolism (rCGM), and structural plasticity, quantified by synaptic density, across all rats. The secondary aim was to investigate the effect of locomotor training on the structure-function relationship after bilateral labyrinthectomy. Dynamic changes of global mean normalized activity values in brain regions segmented by Schiffer’s atlas were analyzed based on longitudinal [18F]-UCB-H and [18F]-FDG data. In addition, voxel-wise comparisons between time points and subgroups were performed. All rats were tested serially in the open field to document changes in locomotor and spatial exploration behaviour following bilateral labyrinthectomy.
Results: Comparison of rCGM and [18F]-UCB-H binding revealed complex structure-function changes after bilateral labyrinthectomy: in brainstem-cerebellar circuits (vestibular nuclei, vestibular cerebellum, colliculus inferior) early-onset rCGM decrease was followed by reduced synaptic density from 3 weeks post lesion. In the thalamus, increased [18F]-UCB-H binding preceded a higher rCGM uptake. In frontal-basal ganglia loops, an increase in synaptic density was paralleled by a decrease in rCGM. In the group with locomotor training, thalamic rCGM increased 1-3 weeks and thalamic [18F]-UCB-H binding 1 week post lesion compared to the no training group. Rats with training had relatively fewer body rotations at 1-3 weeks after bilateral labyrinthectomy, while locomotor velocity and spatial exploration increased in both groups post lesion.
Conclusions: Combined [18F]-UCB-H/ [18F]-FDG dual tracer imaging is a promising approach to depict lesion-induced functional and structural neuroplasticity. Here we show that adaptive plasticity after bilateral vestibular loss is not a uniform process but is composed of complex spatial and temporal patterns of structure-function coupling in networks for vestibular, multisensory, and motor control, which can be modulated by early physical training.
ST0065Posters Satellite list
SATELLITE FREE PAPERS FORM
Visual-inertial heading perception: Effect of heading direction, offset, and visual field size on multisensory integration and perception of common causation
Benjamin T. Crane1,2,3, Raul Rodriguez3
University of Rochester Departments of Otolaryngology1, Neuroscience2, and Bioengineering3
Visual and inertial cues are the sensory modalities for heading determination. The visual cue is ambiguous as it can represent either self-motion through a fixed environment or environmental motion. When there are offsets between visual and inertial headings, it is only appropriate to integrate them when they are both due to motion through a fixed environment, a situation known as common causation. Difference in heading direction is one factor that makes common causation less likely to be perceived, although surprisingly large differences can be perceived as common causation. We looked at the effects of visual field size, heading offset and direction on common causation and integration. Experiments were done using 102° of the horizontal visual field and 70° of the vertical visual field and these were compared with a visual field of 38° in both directions (11% size). Both inertial and visual stimuli consisted of 2s of synchronized motion. The visual stimulus consisted of a 70% coherence star field. Trial blocks included 12 possible visual and inertial headings which covered the full 360° range in the horizontal plane in 30° increments. Every heading combination was presented in random order with 144 stimuli per block. A dial was used to report the perceived direction of the visual or inertial heading and buttons were pressed to report if the headings were the same or different. Six trial blocks were performed per subject, in 3 blocks inertial heading was reported and in 3 visual heading was reported. In all 6 blocks subjects reported if headings were the same or different. Greatly diminishing the visual field size and removing peripheral vision had a surprisingly small effect on visual direction determination or common causation perception. The lateral component of non-cardinal visual headings (e.g. 30°, 60°) was over-estimated by about 20°. Perception of common causation was also very similar to a full field with common causation which was highest when stimuli were aligned in cardinal directions and very low when stimuli were separated by 90° or more. When offset, visual headings continued to have a large influence on inertial heading perception – 10° with a 30° offset, 8° with 60-90° offsets, and 3° with a 120-150° offset. These were smaller than the offsets seen with the full visual field (13° with a 30° offset, and 13-19° with 60-120° offsets. The inertial stimulus influence on the visual stimulus was minimal (<2°) in both conditions.
ST0066Diagnosis of inner ear disorders using MRI -from animal study to clinical application
Maoli Duan1, Jun Yang2
1Department of Otolaryngology Head and Neck Surgery & Audiology and Neurotology and Department of Clinical Science, Intervention and Technology, Karolinska Institute, Stockholm, Sweden; 2Department of Otolarynggology Head and Neck Surgery, Shanghai Xinhua Hospital, Shanghai Jiaotong University, China
We have performed MRI scanning from in vitro to in vivo animal study and found that the method is useful mean to diagnose inner ear disorders using 4.7 Tesla MRI. The important findings are that Gd cannot enter endolymph but perilymph. We further expanded the findings to patient study using 3.0 Tesla MRI and found that Gd cannot enter endolymph but enter easily in perilymph. Thus, the findings provide critical means to diagnose inner ear diseases.
ST0068Allelic variants in KCNQ2 and KCNQ3 genes in Spanish patients with sporadic Meniere Disease.
Patricia Perez-Carpena1,2, Alvaro Gallego-Martinez2, Sana Amanat2; Pablo Román-Naranjo2; Jose A. Lopez-Escamez2,3,4
1Department of Otolaryngology, Hospital Universitario Clínico San Cecilio. ibs.Granada, Granada, Spain; 2Otology & Neurotology Group CTS495, GENYO - Centro de Genómica e Investigación Oncológica, Granada; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria Ibs.GRANADA, Hospital Universitario Virgen de las Nieves, Granada; 4Department of Surgery, Division of Otolaryngology, Universidad de Granada, Granada, Spain
Introduction: Meniere’s disease (MD) is a chronic disorder characterized by sensorineural hearing loss, tinnitus, aural fullness and episodic vertigo. The genetic hypothesis of MD relies on the different prevalence observed according to the ethnic background, familial aggregation studies, and the identification of some genes in familial cases. The voltage-dependent potassium channel K7.2/3 has been involved in the dorsal cochlear nucleus in a tinnitus noise-induced mouse model. Our objective is to investigate the role of rare allelic variants in KCNQ2 and KCNQ3 genes in Spanish patients with MD by target exome sequencing.
Methods: DNA samples were obtained from peripheral blood of patients with MD using the DNA Isolation Kit QIAamp DNA Blood Kit (QIAGEN). A target-sequencing panel including coding regions of genes KCNQ2 and KCNQ3 genes was designed and used to sequence 860 patients with MD. After quality filtering, we annotated vcf files using ANNOVAR, adding information for minor allele frequencies (MAF) from several reference population databases and pathogenic prediction tools. Statistical analyses were done with SPSS, Excel and R packages. Gene burden analysis was addressed using 2x2 contingency tables comparing the allelic frequencies with the three reference databases (CSVS from Spain, Non-Finnish European (NFE) from ExAC and gnomAD). Odds ratios with 95% confidence intervals were calculated using Fisher’s exact test, obtaining corrected p-values by Bonferroni’s method.
Results: A total 175 different allelic variants were found in KCNQ2 and KCNQ3 genes. Multiallelic variants and variants with a MAF >0.10 were excluded, obtaining a final set of 71 SNV (11 for KCNQ2 and 60 for KCNQ3). Most of our single variant analyses showed that allelic frequencies were not different when they we compared to reference databases (CSVS, NFE from both ExAC and gnomAD). However, one of the variant observed in KCNQ3 (8:133141822 G>T) showed significant differences when compared to NFE from ExAC and gnomAD, although we could not confirm this difference with Spanish controls. Although gene burden analysis of KCNQ2 and KCNQ3 showed differences for missense variants in KCNQ3 when compared to NFE controls from ExAC and gnomAD, these results were not replicated after comparison with Spanish controls.
Conclusions: Although we observe some promising results in the variant 8:133141822 G>T from KCNQ3, we could not find a burden of missense variants of KCNQ2 and KCNQ3 gene in patients with MD.
Funding. This project was partially funded by the H2020-MSC-ITN-722046 Grant, an European School for Interdisciplinary Tinnitus Research (ESIT).
ST0075The human egomotion network
Ria Maxine Rühl1,2, Leoni Ophey2,Theresa Raiser, Katharina Seiderer, Virginia Flangin, Matthias Ertl2,3, Julian Conrad1,2 and Peter zu Eulenburg2,4
Department of Neurology1 and German Center for Vertigo and Balance Disorders2 IFB-LMU, Ludwig-Maximilians-University, Munich, Institute of Psychology and Inselspital3, University of Bern, Institute for Neuroradiology4, Ludwig-Maximilians-University Munich, Munich, Germany4
Theme: Volitional movement in a three-dimensional environment requires multisensory integration, in particular of visual and vestibular signals. In humans, responses to visual egomotion-compatible optic flow stimuli have been demonstrated for multiple cortical areas in the parieto-temporal, cingulate, insular and occipital cortex. Of these regions, areas MST, CSv and VIP have been shown to respond to vestibular stimulation. The egomotion network structure in a comprehensive whole-brain approach however has not been systematically investigated to date.
We applied visual self-motion and galvanic vestibular stimulation using high resolution multi-band neuroimaging to characterize the entire cortical and subcortical egomotion network in humans in a large cohort (n=131). Responses during egomotion perception suggest a network including cortical areas CSv, PcM, human VPS, the cerebellar uvula and an area in the supramarginal gyrus. With respect to its delineated cortical connections and anatomical localization, we propose that this area represents the human homologue of macaque area 7a. The whole-brain functional connectivity analysis point at a central role of the connections between area CSv and the uvula of the cerebellum, possibly representing feedback loops involved in updating visuo-spatial and vestibular information during egomotion. All egomotion hubs showed varying functional connections with visual, vestibular, somatosensory and higher order motor areas, underlining their common function in sensorimotor integration essential for the guidance of locomotion.
Target audience: Clinicians and researchers interested in understanding the structural correlates of the human egomotion system and its functional connections.
ST0076Functional Head Impulse Testing Might Be Useful for Assessing Vestibular Compensation After Unilateral Vestibular Loss
Julia Sjögren, Per-Anders Fransson, Mikael Karlberg, Måns Magnusson, Fredrik Tjernström
Department of Clinical Sciences, Otorhinolaryngology Head and Neck Surgery, Skåne University Hospital, Lund University, Lund, Sweden
Background: Loss of the vestibulo-ocular reflex (VOR) affects visual acuity during head movements. Previous studies have shown that compensatory eye-saccades improve visual acuity and that the timing of the saccade is important. Most of the tests involved in testing VOR are made with passive head movement, that do not necessarily reflect the activities of daily living and thus not being proportionate to symptoms and distresses of the patients.
Objective: To examine differences between active (self-generated) or passive (imposed by the examiner) head rotations while trying to maintain visual focus on a target.
Method: Nine subjects with unilateral total vestibular loss were recruited (4 men and 5 women, mean age 47) and tested with video Head Impulse Test (vHIT) and Head Impulse Testing Device-Functional Test (HITD-FT) during passive and active movements while looking at a target. VOR gain, latencies of covert saccades, frequency of covert saccades and visual acuity were measured and analyzed.
Results: Active head-impulses toward the lesioned side resulted in better visual acuity (p = 0.002) compared to conventional passive head-impulses and generated eye-saccades with significantly shorter latencies (p = 0.004). Active movements to the lesioned side generated dynamic visual acuities that were as good as when testing the intact side.
Conclusion: Actively generated head impulses resulted in normal dynamic visual acuity, even when performed toward the side of total vestibular loss. This might be attributed to the appearance of short-latency covert saccades. The results show a strong relationship between self-generated movements, latencies of covert saccades and outcome in HITD-FT, i.e., a better dynamic visual function with less retinal slip which is the main function of the VOR. The method of active HITD-FT might be valuable in assessing vestibular compensation and monitoring ongoing vestibular rehabilitation.
ST0078Importance of Establishing Protocols in the Sequence of Diagnostic Positional Tests for Posterior and Horizontal Canal BPPV
Anita Bhandari1, Rajneesh Bhandari2, Herman Kingma3, Michael Strupp4
(ENT) Vertigo and Ear Clinic, IndiaRajneesh BhandariNeuroEquilibrium Diagnostics, Jaipur, India; 2Department of Ear Nose Throat, Maastricht University, Maastricht, Netherlands; 3Faculty of Physics, Tomsk State National Research University, Tomsk, Russia; 4Department of Ear Nose Throat, Aalborg University, Aalborg, Denmark; Professor of Neurology, Department of Neurology and German Center for Vertigo and Balance Disorders, Hospital of the Ludwig Maximilians University Munich, Germany
Introduction: The diagnosis of BPPV is established by the type of nystagmus induced during the different positional tests. The Dix-Hallpike and the diagnostic Sémont manoeuvre are used for the diagnosis of posterior canal BPPV and the Supine Roll test for horizontal canal BPPV. Simulations of the diagnostic tests show how the otolith debris in the canals can be displaced during these manoeuvres, which may have an impact on the test results. In this study, we examined the effect of the sequence of positional tests on diagnosis of canalithiasis affecting posterior and horizontal canals.
Methods: A 3D simulation model was developed based on reconstructed MRI images. Movement of the otolith debris within the canals was tracked with applied fluid dynamic principles (as a function of time). Each canal was linked with the associated extraocular muscles to visualize nystagmus generated by debris movement within the affected canal. Canalithiasis affecting the ampullary and non-ampullary arms of the horizontal canals and posterior canal long arm was studied. Simulations were used to study the movement of the debris during the diagnostic Dix-Hallpike test and Supine Roll test performed from right and left sides.
Results: The simulations show that the Dix-Hallpike and Supine Roll tests could displace the debris within the horizontal canal from its initial position. In contrast, these positional tests did not change the position of the debris in the posterior canal. By changing the sequence of these three tests, different kinds of horizontal nystagmus patterns, such as bilateral direction-changing, bilateral direction-fixed and unilateral nystagmus, were found. We also observed that the Supine roll and Dix-Hallpike diagnostic tests themselves can also result in repositioning of the debris back to the utricle. The simulations show that the diagnostic tests (including the Dix-Hallpike) may already result in repositioning of debris in the horizontal canals back to the utricle. This could explain why it is possible that sometimes no nystagmus is detected during the repositioning manoeuvre in the case of canalithiasis of the horizontal canal after performing the Dix-Hallpike; in contrast, we observed that the Supine Roll test did not affect the position of the debris in the posterior canals.
Conclusions: Depending on the sequence of diagnostic manoeuvres, the change of debris position can result in various nystagmus patterns. Based on the simulations, it is recommended that the Supine Roll test is performed before the Dix-Hallpike test to avoid shifting of the debris in the horizontal canal when testing for posterior canal BPPV.
ST0090Enrichment of Missense Variants in Axonal Guidance Signalling-related genes in Sporadic Meniere’s Disease cases
Alvaro Gallego-Martinez1, Teresa Requena1, Pablo Roman-Naranjo1, Patrick May2, Jose A. Lopez-Escamez1,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain; 2Bioinformatics core, Luxembourg Centre for Systems Biomedicine, University of Luxembourg, Esch-Sur-Alzette, Luxembourg; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, Hospital Universitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain
Introduction: Meniere’s disease (MD) is a rare inner ear disorder defined by episodic vertigo, sensorineural hearing loss and tinnitus. MD is suspected to have an important genetic background. Although it has been mostly described in sporadic cases, around 10% of the observed individuals reports familial cases. It is associated with an accumulation of endolymph in the inner ear and the formation of endolymphatic hydrops, but the molecular mechanisms remain still unknown. However, it is suspected that supporting cells of the inner ear may be an important biological target for the disease. Previous studies detected that the main molecular pathways showing higher differentially expressed genes in the supporting cells are related to cochlea-vestibular neuronal innervation, cell-cell adhesion and leucocyte extravasation. In this study, our objective is to analyse a possible burden of rare variants in genes that interact with the main signalling pathways in supporting cells of the inner ear in patients with sporadic MD.
Methods: We designed a targeted-sequencing panel including genes related with the main molecular pathways in supporting cells and sequenced 860 Spanish patients with sporadic MD. We selected variants with minor allele frequencies <0.1 in the gene panel and were compared with three independent population reference datasets (CSVS for spanish population, GnomAD NFE for non-finnish european population and GnomAD ALL for global population). Variants were classified as loss of function, missense and synonymous. Missense variants with a combined annotation dependent depletion score (CADD) of >20 were classified as damaging missense variants. We calculated odds ratio for each gene in the panel for every group of variants in every population frequency dataset. Genes significantly enriched in our cohort for the different comparisons were ranked, pointing to which pathway was more represented by missense variant-enriched genes.
Results: We have observed a significant burden of damaging missense variants in few key genes, including the NTN4 and NOX3 genes, associated with axon guidance signalling pathways in patients with sporadic MD. We have also identified active subnetworks having an enrichment of rare variants in sporadic MD.
Conclusion: The enrichment of missense variants genes such as NTN4 and NOX3 suggests that axonal guidance signalling gene network could be a novel pathway involved in sporadic MD.
Acknowledgments: This study was funded by the Luxembourg National Research Fund Inter/Mobility/17/11772209 grant and EF-0247-2017 from Andalusian Health Government.
ST0091Prevalence and impact of dizziness, unsteadiness and falls in adults positive for COVID-19. An online anonymous survey
Viktoria Azoidou1, Louisa Murdin2, Doris-Eva Bamiou3, Marousa Pavlou1
1Centre for Human and Applied Physiological Sciences, King’s College London, London, United Kingdom, ; 2Audiovestibular Medicine Department, Guy’s Hospital, Guy’s and St Thomas NHS Foundation Trust, London, United Kingdom, ; 3Neuto-otology Department, National Hospital for Neurology and Neurosurgery, and Ear Institute, University College London, London, United Kingdom, ; 1Centre for Human and Applied Physiological Sciences, King’s College London, London, United Kingdom, .
Background: Dizziness and unsteadiness are common clinical manifestations of coronavirus-disease-2019 (COVID-19). Falls were observed in older adults positive for COVID-19. Some COVID-19 survivors, do not fully recover, and experience lingering symptoms for longer than six months. It is not clear how many adults positive for COVID-19 have been affected by dizziness, unsteadiness and/or falls and the impact these symptoms have on their lives.
Methods: A 37-item-close-ended-online-anonymous-survey delivered via Jisc-platform between April-August 2021 aimed to investigate the prevalence and impact of dizziness, unsteadiness and/or falls in adults aged 18-95 years’ old positive for COVID-19 with (Group P) and without (Group N) previous diagnosis of a pathology which provoked these symptoms. Recruitment was via social media, community, and patient organisations representing people with COVID-19 or the investigating symptoms.
Results: In both Group P (n=481, females=390, mean age ±SD= 30.34±13.23 years) and Group N (n=513, females=416, mean age ±SD= 30.99±12.88), dizziness was the most prevalent symptom followed by unsteadiness and falls (Group P: 74.2%, 60.5%, 20.8%; Group N: 74.7%, 61.6%, 18.5%, respectively). The majority of responders experienced these symptoms for >six months (Group P: 60.5%; Group N: 65.7%). Responders experienced dizziness and unsteadiness on a daily basis (Group P: 29.9%, 28.3%; Group N: 22%, 21.1%, respectively), or 1-2 times per week (Group P: 23.3%, 21%; Group N: 28.1%, 25%, respectively) with each episode lasting for a few seconds up to 2 minutes (Group P: 37.2%, 36.2%; Group N: 46.2%, 46%, respectively). Falls were reported by younger adults in both Group P and N (mean age ±SD =33.24 ±13.04 and =35.35±12.17 years, respectively). The most common symptoms triggers were different body movements (Group P: 50.3%; Group N: 46.6%) and moving from a lying down or sitting position to standing up (Group P: 44.1%; Group N: 43.1%). Between- groups there was a statistically higher prevalence in Group P for persons who reported to be severely impacted by dizziness and unsteadiness (37% versus 23%; and 32% versus 18%, respectively) in daily activities. All severely impacted persons in Group P had a previous diagnosis of a pathology causing dizziness and/or unsteadiness with most prevalent peripheral vestibular disorder (88/481), vestibular migraine (43/481), anxiety/stress (41/481), and low blood pressure (41/481).
Conclusions: Persons affected by COVID-19 may experience new onset or exacerbation of previous symptoms of dizziness and unsteadiness and increased incidence of falls for >six months post-COVID with a significant impact on their ability to perform daily activities.
ST0103Sensitivity and Stimulation Characteristics of the Mammalian Vestibular short-latency Evoked Potential
Christopher J. Pastras1, Ian S. Curthoys2, Daniel J. Brown3
1School of Medical Sciences. The University of Sydney; 2Vestibular Research Laboratory, The University of Sydney; 3School of Pharmacy and Biomedical Science, Curtin University.
The Vestibular short-latency Evoked Potential (VsEP) has been used as an objective measure of vestibular nerve function and represents the synchronous firing of vestibular primary afferents to the onset of motion. It was first termed the short latency vestibular evoked potential by Elidan et al. in 1982 due to its similarity to the auditory brainstem evoked potential. Since then, the VsEP has been measured in various vertebrate models and preparations; the most common being a non-invasive, scalp recording to linear-jerk pulses. This approach is attractive for several reasons, such as the ability to measure vestibular nerve function in chronic recovery animal models without disturbance of the labyrinth. However, with the cochlea intact, this approach is prone to auditory contamination, making interpretation difficult. Given the increased popularity of the VsEP in recent years, it’s important to validate key features of the response for future interpretation and use. This work aimed to characterise the near-field VsEP recorded close to the vestibular afferents from facial nerve canal in anaesthetized guinea pigs. Linear-jerk pulses of varying widths (~0.1-3ms) were used to evoke the VsEP and were compared to responses with the cochlea intact, before and after controlled experimental manipulations, such as acoustic-masking, changes in stimulation rate, and cochlear ablation. Responses from the facial nerve canal were also compared to the vertex. Responses evoked by a 2ms jerk pulse were not suppressed by acoustic forward-masking but were significantly masked using continuous broadband noise. Changing the stimulation rate was used to characterise differences in cochlear and vestibular neuronal forward masking. With the cochlea intact, 50% of the response was forward-masked with a stimulation rate of 60Hz, whereas the response after cochlear ablation did not forward-mask. Overall, surgical ablation of the cochlea revealed significant cochlear contribution of the response across all linear-jerk pulse widths. An iso-acceleration, iso-jerk, and iso-VsEP paradigm was used to probe the kinematic vector sensitivity of the VsEP. Surprisingly, results indicate that the VsEP scales with linear acceleration of the earbar, rather than kinematic jerk. Interestingly, responses with the cochlea intact from both the facial nerve canal and vertex, scaled with kinematic jerk, rather than acceleration. This work reveals new findings that call into question the original interpretation of the sensitivity and stimulation characteristics of the mammalian VsEP.
The target audience is basic vestibular researchers; however, we believe this work will be of interest to a wide readership such as clinicians.
ST0104Similarities and Differences between Vestibular and Cochlear Systems – In Vivo Evoked Potentials.
Christopher J. Pastras1, Daniel Brown2, Ian Curthoys3
1School of Medical Sciences. The University of Sydney; 2School of Pharmacy and Biomedical Science, Curtin University; 3Vestibular Research Laboratory, The University of Sydney
Auditory evoked potentials have been critical to our understanding of mammalian cochlear function and hearing loss. These measures have allowed a differential assessment of auditory hair cell and neural dysfunction in experimental animal models of disease, such as endolymphatic hydrops and ototoxicity. However, their vestibular counterparts have been more challenging to record due to difficulties in stimulating (and recording) from the labyrinth in isolation of the cochlea. Recently, however, gross utricular nerve and hair cell responses have been recorded from the facial nerve canal and utricular macula of anaesthetized guinea pigs, following cochlear ablation. Vestibular nerve measurements include the Vestibular short-latency Evoked Potential (VsEP) and the Vestibular Nerve Neurophonic, while vestibular hair cell responses include the Utricular Microphonic and utricular Summating Potential. These vestibular responses are analogous to the widely recorded cochlear evoked responses; the Compound Action Potential, Auditory Nerve Neurophonic, Cochlear Microphonic, and Summating Potential. The ability to record similar response measures across inner ear sensory systems highlights commonalities in hair cell and afferent receptor mechanisms and sensory coding. However, clear and important differences exist, such as distinctions in response threshold, sensitivity, dynamic range, frequency selectivity, and characteristics of peripheral response generators, such as, stereocilia polarisation, etc. Comparisons of these response measures can enhance our basic understanding of inner ear physiology, as well as provide a more holistic understanding of cochleovestibular disorders and related therapies.
The target audience is primarily basic inner ear researchers and physiologists; however, we believe this work will be of interest to a wide readership, such as clinicians.
ST0108Galvanic Vestibular Stimulation Improves Spatial Cognition After Unilateral Labyrinthectomy in Mice
Thanh Tin Nguyen1,2,3†, Gi-Sung Nam2,4†, Jin-Ju Kang2,5, Gyu Cheol Han6*, Ji-Soo Kim7, Marianne Dieterich8,9,10 and Sun-Young Oh1,2,5*
1Jeonbuk National University College of Medicine, Jeonju, South Korea; 2Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea; 3Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 4Department of Otorhinolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Kwangju, South Korea; 5Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, South Korea; 6Department of Otolaryngology-Head and Neck Surgery, Graduate School of Medicine, Gachon University of Medicine and Science, Incheon, South Korea; 7Department of Neurology, Seoul National University Hospital & School of Medicine, Seoul, South Korea; 8Department of Neurology, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany. 9-German Center for Vertigo and Balance Disorders-IFB, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany. 10-Munich Cluster for Systems Neurology (SyNergy), Munich, Germany.
Objectives: To investigate the deficits of spatial memory and navigation from unilateral vestibular deafferentation (UVD) and to determine the efficacy of galvanic vestibular stimulation (GVS) for recovery from these deficits using a mouse model of unilateral labyrinthectomy (UL).
Methods: Thirty-six male C57BL/6 mice were allocated into three groups that comprise a control group and two experimental groups, UVD with (GVS group) and without GVS intervention (non-GVS group). In the experimental groups, we assessed the locomotor and cognitive behavioral function before (baseline) and 3, 7, and 14 days after surgical UL, using the open field (OF), Y maze, and Morris water maze (MWM) tests. In the GVS group, the stimulations were applied for 30 min daily from postoperative day (POD) 0–4 via the electrodes inserted subcutaneously close to both bony labyrinths.
Results: Locomotion and spatial cognition were significantly impaired in the mice with UVD non-GVS group compared to the control group. GVS significantly accelerated recovery of locomotion compared to the control and non-GVS groups on PODs 3 (p < 0.001) and 7 (p < 0.05, Kruskal–Wallis and Mann–Whitney U tests) in the OF and Y maze tests. The mice in the GVS group were better in spatial working memory assessed with spontaneous alternation performance and spatial reference memory assessed with place recognition during the Y maze test than those in the non-GVS group on POD 3 (p < 0.001). In addition, the recovery of long-term spatial navigation deficits during the MWM, as indicated by the escape latency and the probe trial, was significantly better in the GVS group than in the non-GVS group 2 weeks after UVD (p < 0.01).
Conclusions: UVD impairs spatial memory, navigation, and motor coordination. GVS accelerated recoveries in short- and long-term spatial memory and navigation, as well as locomotor function in mice with UVD, and may be applied to the patients with acute unilateral vestibular failure.
ST0109Effects of Galvanic Vestibular Stimulation on Vestibular Compensation in Unilaterally Labyrinthectomized Mice
Gi-Sung Nam1,2†, Thanh Tin Nguyen1,3,4†, Jin-Ju Kang1,3,5, Gyu Cheol Han6* and Sun-Young Oh1,3,5*
1Jeonbuk National University College of Medicine, Jeonju, South Korea; 2Department of Otorhinolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Gwangju, South Korea; 3Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea; 4Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 5Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, South Korea; 6Department of Otolaryngology-Head and Neck Surgery, Graduate School of Medicine, Gachon University of Medicine and Science, Incheon, South Korea.
Objectives: To investigate the ameliorating effects of sinusoidal galvanic vestibular stimulation (GVS) on vestibular compensation from unilateral vestibular deafferentation (UVD) using a mouse model of unilateral labyrinthectomy (UL).
Methods: Sixteen male C57BL/6 mice were allocated into two groups that comprise UL groups with GVS (GVS group, n = 9) and without GVS intervention (non-GVS group, n = 7). In the experimental groups, we assessed vestibulo-ocular reflex (VOR) recovery before (baseline) and at 3, 7, and 14 days after surgical unilateral labyrinthectomy. In the GVS group, stimulation was applied for 30 min daily from postoperative days (PODs) 0–4 via electrodes inserted subcutaneously next to both bony labyrinths.
Results: Locomotion and VOR were significantly impaired in the non-GVS group compared to baseline. The mean VOR gain of the non-GVS group was attenuated to 0.23 at POD 3 and recovered continuously to the value of 0.54 at POD 14, but did not reach the baseline values at any frequency. GVS intervention significantly accelerated recovery of locomotion, as assessed by the amount of circling and total path length in the open field tasks compared to the non-GVS groups on PODs 3 (p < 0.001 in both amount of circling and total path length) and 7 (p < 0.01 in amount of circling and p < 0.001 in total path length, Mann–Whitney U-test). GVS also significantly improved VOR gain compared to the non-GVS groups at PODs 3 (p < 0.001), 7 (p < 0.001), and 14 (p < 0.001, independent t-tests) during sinusoidal rotations. In addition, the recovery of the phase responses and asymmetry of the VOR was significantly better in the GVS group than in the non-GVS group until 2 weeks after UVD (phase, p = 0.001; symmetry, p < 0.001 at POD 14).
Conclusion: Recoveries for UVD-induced locomotion and VOR deficits were accelerated by an early intervention with GVS, which implies that GVS has the potential to improve vestibular compensation in patients with acute unilateral vestibular failure.
ST0110Vibration-Induced Downbeat Nystagmus: A New Cerebellar Sign Observed in Paraneoplastic Cerebellar Degeneration Associated with Anti-Ri Antibody
Jong-Hee Lee1, Hyo-Jung Kim2, Ji-Soo Kim1,3
1Dizziness Center, Seoul National University Bundang Hospital, Seongnam, Korea; 2Research Administration Team, Seoul National University Bundang Hospital, Seongnam, Korea; 3Department of Neurology, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Vibratory stimuli on the sternocleidomastoid muscle or skull may enhance the vestibular asymmetry and evoke nystagmus. This vibration-induced nystagmus (VIN) mostly beat toward the healthy or less affected ear in unilateral or asymmetric peripheral vestibulopathy. We report downbeat VIN, a hitherto undescribed sign, in a patient with paraneoplastic cerebellar degeneration (PCD) due to cervix cancer with a peritoneal metastasis and anti-Ri antibody. This 47 year-old women had suffered from dizziness and imbalance for several months after the diagnosis, and examination showed spontaneous upbeat nystagmus with and without visual fixation that decreased during the lateral gazes and changed into downbeat nystagmus during convergence. The spontaneous upbeat nystagmus also changed into downbeat after horizontal head-shaking for about 15 seconds and during vibratory stimuli on either mastoid and the forehead. Additional findings included positional downbeat nystagmus, impaired smooth pursuit, hypermetric horizontal saccades, and truncal ataxia. The dizziness and ataxia did not respond to steroid pulse and intravenous IgG therapy. Along with head-shaking nystagmus, the downbeat VIN observed in our patient indicates a cross coupled responses of the vestibular system during or after stimulation of the semicircular canals or otolithic organs due to cerebellar dysfunction. Vibration-induced downbeat nystagmus should be added to the list of central vestibular signs, probably due to cerebellar dysfunction.
ST0111The Differential Effects of Acute Right- vs. Left-Sided Vestibular Deafferentation on Spatial Cognition in Unilateral Labyrinthectomized Mice
Thanh Tin Nguyen1,2, Gi-Sung Nam3,4, Jin-Ju Kang1,4, Gyu Cheol Han5, Ji-Soo Kim6, Marianne Dieterich7,8,9 and Sun-Young Oh1,4*
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea; 2Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 3Department of Otorhinolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Gwangju, South Korea; 4Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, South Korea; 5Department of Otolaryngology-Head and Neck Surgery, Gachon University of Medicine and Science, Graduate School of Medicine, Incheon, South Korea; 6Department of Neurology, Seoul National University Bundang Hospital & School of Medicine, Seoul, South Korea; 7Department of Neurology, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 8German Center for Vertigo and Balance Disorders-IFB, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 9Munich Cluster for Systems Neurology (SyNergy), Munich, Germany.
Objectives: This study aimed to investigate the disparity in locomotor and spatial memory deficits caused by left- or right-sided unilateral vestibular deafferentation (UVD) using a mouse model of unilateral labyrinthectomy (UL) and to examine the effects of galvanic vestibular stimulation (GVS) on the deficits over 14 days.
Methods: Five experimental groups were established: the left-sided and right-sided UL (Lt.-UL and Rt.-UL) groups, left-sided and right-sided UL with bipolar GVS with the cathode on the lesion side (Lt.-GVS and Rt.-GVS) groups, and a control group with sham surgery. We assessed the locomotor and cognitive-behavioral functions using the open field (OF), Y maze, and Morris water maze (MWM) tests before (baseline) and 3, 7, and 14 days after surgical UL in each group.
Results: On postoperative day (POD) 3, locomotion and spatial working memory were more impaired in the Lt.-UL group compared with the Rt.-UL group (p < 0.01, Tamhane test). On POD 7, there was a substantial difference between the groups; the locomotion and spatial navigation of the Lt.-UL group recovered significantly more slowly compared with those of the Rt.-UL group. Although the differences in the short-term spatial cognition and motor coordination were resolved by POD 14, the long-term spatial navigation deficits assessed by the MWM were significantly worse in the Lt.-UL group compared with the Rt.-UL group. GVS intervention accelerated the vestibular compensation in both the Lt.-GVS and Rt.-GVS groups in terms of improvement of locomotion and spatial cognition.
Conclusion: The current data imply that right- and left-sided UVD impair spatial cognition and locomotion differently and result in different compensatory patterns. Sequential bipolar GVS when the cathode (stimulating) was assigned to the lesion side accelerated recovery for UVD-induced spatial cognition, which may have implications for managing the patients with spatial cognitive impairment, especially that induced by unilateral peripheral vestibular damage on the dominant side.
ST0113Selectively Targeting Efferent Synaptic Mechanisms in the Mouse Inner Ear
Choongheon Lee1, Anjali Sinha2, Kenneth Henry1,2, Anqi W. Walbaum3, Peter A. Crooks3, Joseph C. Holt1,2,4
1Department of Otolaryngology, University of Rochester, Rochester, NY, United States; 2Department of Neuroscience,University of Rochester, Rochester, NY, United States; 3Department of Pharmaceutical Sciences, College of Pharmacy,University of Arkansas for Medical Sciences, Little Rock, AR, United States; 4Department of Pharmacology & Physiology,University of Rochester, Rochester, NY, United States
Electrical stimulation of inner ear efferents gives rise to a number of diverse effects on vestibular and auditory physiology. The bulk of these effects are the product of acetylcholine (ACh), the predominant efferent neurotransmitter, and subsequent activation of several ACh receptors (AChRs) and downstream modulation of potassium channels on afferents and hair cells in the cochlea and vestibular endorgans. On the vestibular side, pharmacological evidence has suggested that efferent-mediated fast of vestibular afferents is mediated by α4β2*-containing nicotinic AChRs (nAChRs) while efferent-mediated slow excitation of vestibular afferents is mediated by the activation of muscarinic AChRs (mAChRs) and subsequent closure of KCNQ potassium channels. In contrast, activation of α9α10-nAChRs and SK2 potassium channels in type II hair cells gives rise to efferent-mediated inhibition of vestibular afferents. On the auditory side, efferent-mediated suppression of the compund action potential and distortion product otoacoustic emissions (DPOAEs) is also mediated by α9α10nAChRs and SK2 channels in outer hair cells. Previous pharmacological characterization of the above synaptic mechanisms have primarily relied on the use of systemically-administered cholinergic drugs that, in addition to entering the inner ear, also readily access the CNS and other peripheral tissues where they could interact with similar synaptic mechanisms. Some of these off-target effects could potentially complicate interpretation of our pharmacological observations and certainly may limit the use of these drugs in behavioral paradigms designed to probe efferent mechanisms in the inner ear. To avoid or minimize these off-target effects, we thought that the use of peripherally-acting cholinergic drugs in combination with different administration strategies might be of some utility. However, details about whether such drugs can enter the ear were lacking. Using a variety of administration routes, we performed both vestibular afferent and DPOAE recordings during efferent stimulation in mice to characterize whether charged mAChR or α9α10nAChR antagonists, that exhibit little CNS entry, still retain their ability to target these synaptic mechanisms in the inner ear. We can report that systemic, middle ear, or direct perilymphatic administration of the charged mAChR antagonists glycopyrrolate and methscopolamine will block efferent-mediated slow excitation of mouse vestibular afferents. Furthermore, the same data also reveal these mAChR antagonists can move from one ear to the other. The charged α9nAChR antagonists, however, were ineffective when administered systemically and only blocked efferent-mediated suppression of DPOAEs upon direct perilymphatic application. These data reveal additional details about the rules of drug entry into the inner ear.
ST0114Using Mouse Behavioral Models for Assaying Vestibular Efferent Function
Anjali Sinha1,2, Natalie B. Dang1, Choongheon Lee1, Joseph C. Holt1,2,3
1Department of Otolaryngology, University of Rochester, Rochester, NY, United States; 2Department of Neuroscience,University of Rochester, Rochester, NY, United States; 3Department of Pharmacology & Physiology,University of Rochester, Rochester, NY, United States
The efferent vestibular system (EVS) in mammals starts as a small number of bilateral, multipolar neurons in the dorsal brainstem. Axons of contralateral and ipsilateral vestibular efferent neurons (VENs) travel to multiple vestibular end organs on each side and extensively branch to give rise to an abundance of synaptic varicosities on hair cells and afferent terminals. While electrical stimulation of mammalian VENs in the laboratory setting profoundly modulates both the resting discharge and sensitivity of vestibular afferents, the functional framework, for how and when the mammalian EVS is employed under normal physiological conditions, is poorly understood. Pharmacological data regarding EVS actions in mice from our lab have characterized a number of cholinergic synaptic mechanisms that underlie the responses of vestibular afferents to efferent stimulation, including multiple muscarinic and nicotinic acetylcholine receptors. Some of our interest in performing vestibular studies in mice was having access to transgenic animals where these specific EVS synaptic mechanisms, implicated by our pharmacological data, have been disrupted. These mice are likely to present with distinct vestibular phenotypes that can be characterized in both electrophysiological and behavioral assays.
The utility of such an approach is highlighted by a number of recent observations made in mice where the alpha9 nicotinic acetylcholine receptor subunit (α9nAChR-KO) has been altered. Loss of functional α9nAChRs in α9nAChR-KO animals is associated with modifications in the response properties of vestibular afferents that likely give rise to changes in the vestibulo-ocular reflex (VOR), vestibular sensory evoked potential (VsEP), and vestibulo-autonomic pathways. For further insight into EVS function, we have recently employed a suite of behavioral assays that might reveal vestibular deficits in transgenic mice missing critical EVS signaling components. As our first test, we probed if α9nAChR-KO animals, relative to their controls (α9nAChR-WT), behave differently before and/or after being subjected to a provocative vestibular stimulus. Postural sway and center of pressure (COP) measurements were made on a miniature force plate from α9nAChR-WT and α9nAChR-KO mice before and after a 5-min rotation at 125 RPMs on an orbital shaker. Before stimulation, both groups of mice readily explored the confines of the force plate and exhibited comparable COP metrics. In the poststimulus period, however, α9AChR-KO mice displayed a striking reduction in their movement on the force plate which was often associated with a significant compression of postural sway space, bouts of immobilization along the corners and walls of the plate enclosure, and reduced point-to-point movements. Interestingly, older α9nAChR-KO, but not WT, animals exhibited similiar mobility phenotypes during the prestimulus period which may point to interactions among aging, stress, and vestibular function.
ST0115Thresholds for vestibular and cutaneous perception, and oculomotor response induced by galvanic vestibular stimulation
Thanh Tin Nguyen1,2,4,*, Jin-Ju Kang2,3,*, Sun-Young Oh1,2,3
1Jeonbuk National University College of Medicine, Jeonju, South Korea; 2Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, South Korea; 3Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, South Korea; 4Department of Pharmacology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam
Objectives: The aim of this study was to detect the specific threshold intensities and response characteristics of galvanic vestibular stimulation (GVS) on vestibular (conscious) and cutaneous (detrimental) perception, as well as on oculomotor nystagmus (reflex).
Methods: These thresholds were determined concurrently, but separately, in 15 right-handed healthy subjects (aged 32.8 ± 6.76 years; 66.7% female) seated upright and wearing a Frenzel goggle while applying a direct current (DC) GVS with a cathode right and anode left paradigm using a two-step approach (gradual increasing followed by decreasing intensities).
Results: The mean vestibular threshold was 0.83 ± 0.45 mA and above the currents, dizziness of whirling sensation or falling tendency, which was more frequently directed to the clock-wise (33.3%) than the counter-clockwise (66.7%) rotation were induced. The mean cutaneous threshold was 0.88 ± 0.4 mA and the currents above which triggered mild tingling sensation on the cathode (66.7%), which was more frequent than on the anode (13.3%) (p=0.039, one-sample binomial test) or both sides (20%). The mean oculomotor threshold was 1.27 ± 0.53 mA and above the currents, right-beating horizontal (cathode) or clock-wise torsional nystagmus (77.3%), which was more frequent than the left-beat (anode) or counter clock-wise torsional nystagmus (26.7%) (p=0.035, one-sample binomial test) were induced. The oculomotor threshold was significantly lower than the vestibular threshold (p=0.023) and oculomotor threshold (p=0.036) (Mann-Whitney U test). Vestibular threshold was significantly higher in the male participants than the female (1.3 ± 0.45 mA vs. 0.6 ± 0.21 mA, p=0.022, independent t-test).
Conclusion: Our findings showed that the vestibular perception threshold was the highest sensitivity with the lowest level of current intensity compared to the oculomotor threshold. It implies that a strategy of lowering GVS current intensity, at the level of vestibular perception threshold, may prioritize eliciting beneficial vestibular stimulating effects while avoiding simultaneously detrimental effects such as oculomotor consequences.
ST0118How peripheral vestibular damage affects velocity storage
Amsal Madhani1, Richard F. Lewis1,2,3, Faisal Karmali1,3
1Jenks Vestibular Physiology Laboratory, Massachusetts Eye and Ear Infirmary, Boston, MA; 2Department of Neurology, Harvard Medical School, Boston, MA; 3Department of Otolaryngology, Harvard Medical School, Boston, MA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Velocity storage is a centrally-mediated mechanism that processes peripheral vestibular inputs. One prominent aspect of velocity storage is its effect on dynamic responses to yaw rotation. Specifically, when normal human subjects are accelerated to constant angular yaw velocity, horizontal eye movements and perceived angular velocity decay exponentially with a time constant circa 15-30 s, even though the input from the vestibular periphery decays much faster (~ 6 s). Peripheral vestibular damage causes a time constant reduction, which is useful for clinical diagnoses, but a mechanistic explanation for the relationship between vestibular damage and changes in these behavioral dynamics is lacking. It has been hypothesized that Bayesian optimization determines ideal velocity storage dynamics based on statistics of vestibular noise and experienced motion. Specifically, while a longer time constant would make the central estimate of angular head velocity closer to actual head motion, it may also result in the accumulation of neural noise which simultaneously degrades precision. Thus, the brain may balance these two effects by determining the time constant that optimizes behavior. We applied a Bayesian optimal Kalman filter to determine the ideal velocity storage time constant for unilateral damage. Predicted time constants were substantially lower than normal, similar to patients, and modeled interactions between age-related hair cell loss and peripheral damage. These results provide a mechanistic explanation for changes in velocity storage after peripheral damage. Results also suggested that even after peripheral damage, ipsilateral noise originating in the periphery or early central processing remains relevant in neurocomputations. Overall, our findings support the hypothesis that the brain optimizes velocity storage based on the vestibular signal-to-noise ratio.
ST0119Proposed Diagnostic Criteria for Definite Isolated Otolith Dysfunction
Myung-Whan Suh 1, Toshihisa Murofushi2
1Department of Otolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea; 2Department of Otolaryngology, Teikyo University School of Medicine Mizonokuchi Hospital, Kawasaki, Japan
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and objectives: Dizzy patients with abnormal otolith function tests, despite a normal caloric response, are defined as having specific (isolated) otolith organ dysfunction. This study was performed to compare the differences in clinical presentation between isolated otolith dysfunction (iOD) patients with lab- and Sx-based iOD group and lab-based iOD symptoms.
Subject and methods: The medical records of 23 iOD patients with normal caloric response but abnormal cervical vestibular evoked myogenic potential (VEMP), ocular VEMP, or subjective visual vertical were reviewed. Non-spinning vertigo was considered as otolith-related symptoms. The patients’ age, onset of dizziness, Numeric Rating Scale on the severity of dizziness, and concomitant vestibular disorders were analyzed.
Results: Patients in the lab-based iOD group were significantly older than those in the lab- and Sx-based iOD group. Known vestibular disorders were significantly more common in the lab-based iOD group (83.3%) compared to the lab- and Sx-based iOD group (18.2%). Despite the normal caloric response, catch-up saccade was found in the video head impulse test in more than half (54.5%) of the lab-based iOD group patients. There was no catch-up saccade in the lab- and Sx-based iOD group. There were no significant differences in gender ratio, frequency of dizziness attacks, and duration of illness.
Conclusions: We propose new definitions of definite iOD (lab- and Sx-based iOD) and probable iOD (lab- or Sx-based iOD). These new definitions may help researchers to identify patients who are more likely to have true iOD, and facilitate comparisons of results between different studies.
ST0124Stop-Gain Variant in the CENPP gene affecting Kinetochore assembly and Mitotic Progression segregates low frequency Sensorineural Hearing Loss
Paula Robles-Bolivar1,2,3, Alberto Parra-Perez1,2,3, Alba Escalera-Balsera1,2,3, Alvaro Gallego-Martinez1,2,3, Pablo Roman-Naranjo1,2,3, Jose A. Lopez-Escamez1,2,3,4
1Otology & Neurotology Group CTS495, Department of Genomic Medicine, GENYO, Centre for Genomics and Oncological Research, Pfizer University of Granada Andalusian Regional Government, PTS, 18016 Granada, Spain; (P.R.-B.); (A.P.-P.); (A.E.-B.); (A.G.-M.); (P.R.-N.); (JA.L.-E.); 2Sensorineural Pathology Programme, Centro de Investigación Biomédica en Red en Enfermedades Raras, CIBERER, 28029 Madrid, Spain; 3Department of Otolaryngology, Instituto de Investigación Biosanitaria ibs.Granada, Hospital Universitario Virgen de las Nieves, Universidad de Granada, 18014 Granada, Spain; 4Division of Otolaryngology, Department of Surgery, University of Granada, 18011 Granada, Spain
Background: Low-frequency sensorineural hearing loss (SNHL) is a rare condition with a prevalence of 18 per 100.000 population. It is characterized by losses at tones under 1000Hz, accompanied by ear fullness and tinnitus, but without vertigo. When it overlaps with vestibular symptoms is considered an initial stage for Meniere disease (MD). To date, there is a total of 130 described genes underlying non-syndromic NSHL, but only five have been associated with low-tones phenotype, such as DIAPH1, WSF1, TNT, SLC26A4 or CCDC50, appearing with an autosomal dominant inheritance pattern. The purpose of this study is to determine the genetic cause of low frequency hearing loss diagnosed in four women from a Swiss family over three generations.
Methods: Four cases and one control were submitted to otological-audiometric examinations and exome sequencing from saliva samples. Bioinformatic data processing and subsequent candidate prioritization included variants with minor allele frequency (MAF)<0.001 in non-Finnish European population, pathogenic CADD score>20 and segregation in all affected members but absent in control. The coding genes from variants should also be expressed in inner ear.
Results: Audiological profile described an up-slopping configuration, with mild-moderate losses below 500Hz and progression to high frequencies over time, without tinnitus or vestibular symptoms. After prioritization process, the exome analysis pointed a novel non-sense variant in the Centromeric Protein P (CENP-P) gene, segregating in heterozygosis in cases. CENP-P is a subunit of CENPA-CAD (nucleosome distal complex), involved in assembly of kinetochore proteins, mitotic progression and chromosome segregation. RNA-seq studies revealed CENP-P expression in mouse inner ear in embryonic and postnatal stages, more in supporting than hair cells in both, the cochlea and the vestibular epithelia. The candidate variant (CENP-P,C283*) is classified as “Likely pathogenic” by ACMG guidelines, turning to “Pathogenic” when PP1 parameter (meaning co-segregation of these variant with phenotype in multiple family members) is manually activated. Variant generates a five amino truncation at the end of the protein, which it suggested to produce loss of electrostatic interactions by in sillico modelling, that could slightly alter the stability. Conservational analysis indicated limited conservation of altered residue between the top 50 sequences with higher identity with human CENP-P.
Conclusions: In conclusion, we present the gene coding for centromeric protein P (CENP-P) as a possible responsible for hearing loss at low frequencies. Consecutive advances in genetic defining this condition will enable us to improve its diagnosis, prognosis and treatment.
This project was partially funded by H2020-SC1-2019-848261 and the Swiss Schmieder-Bohrisch Foundation
ST0127Vestibular Adaptation Mitigates Unwanted Effects of Magnetic Vestibular Stimulation with Slow Bore Entry Velocity
Jacob M. Pogson1,3, Dale C. Roberts1, Jorge Otero-Milan1,2, Ari Shemesh4,5, David S. Zee1, Bryan K. Ward1
1The Johns Hopkins University, Baltimore, United States; 2University of California Berkeley, United States; 3Royal Prince Alfred Hospital, Camperdown, Australia; 4Technion Israel Institute of Technology, Haifa, Israel; 5Hadassah Medical Center, Jerusalem, Israel
Magnetic Resonance Imaging (MRI) requires a powerful static electromagnetic field. Exposure of the inner ear to this magnetic field generates a magnetohydrodynamic Lorentz force in the endolymph, which pushes the cupulae of the lateral and superior semicircular canals, causing subjective vertigo and objective nystagmus. This force is proportional to magnetic field strength, so increases as subjects enter the MRI bore, remains constant within the bore, and then decreases on exit. However, for a typical 20 second entry duration, the nystagmus response usually increases to a peak over tens of seconds after entering the bore, and then exponentially reduces over seconds, minutes, and hours. The response is presumably mediated by a combination of central vestibular velocity storage and adaptation mechanisms. Here, we investigated if better matching the magnetic field entry time to the vestibular adaptation time-constants could mitigate the subjective and objective vestibular effects.
First, with Matlab SimuLink we built a three-axis mathematical model of the vestibular system which incorporates gravity, velocity storage (Tc=16sec), rotational feedback, and vestibular adaptation (Tc=100sec, Tc=1000sec). These parameters were set as determined by previous studies. We simulated nystagmus responses in the supine position with movement durations of 20, 120, and 300 seconds; the longer the entry and exit durations the lower the per and post peak slow-phase velocities (SPV).
Second, we collected data from 4 control subjects using a 7 Tesla MRI; 2 were naive to the stimulus. Binocular eye movements were recorded at 100 Hz, along with head orientation in the gravity and magnetic fields. Subjects were manually moved on the MRI bed to linearly increase or decrease the magnetic field over durations of 20, 120, and 300 seconds. As in our model simulations, longer entry and exit durations reduced the nystagmus peak SPV. All subjects reported that the 20 sec duration generated the most intense vertigo, all subjects reported some mild vestibular symptoms e.g., tilting without vertigo, for the 120s condition, whereas no subject reported any vestibular symptoms during the 300s condition.
In summary, the model successfully predicted that longer entry durations (120 and 300 secs) lower the peak SPV. Together, the model and data demonstrate a new method to mitigate the objective and subjective effects of MVS by taking advantage of vestibular adaptation. About 120s MRI entry and exit duration may be an ideal tradeoff between practical implementation and reduction of discomforting vestibular symptoms.
ST0129A Case of Virtual Reality In Visual Vertigo
Lennox, Amy; Morrow, Stacy
Vestibular rehabilitation (VRT) is used to manage the symptomatic manifestations of vestibular conditions. However often the outcomes of vestibular rehabilitation are limited by patient compliance and time constraints. The introduction of virtual reality technology can provide interesting interactions for patients thus encourage patients to actively participate in various repetitive rehabilitation exercises and overcoming the aforementioned barriers. Despite this, the efficacy of virtual reality for vestibular rehabilitation remains unclear. Preliminary evidence suggest the benefit of virtual- reality. Here, we present one case which will seek to address the utility of virtual reality.
The case demonstrates outcome measures pre and post vestibular rehabilitation utilising virtual reality technology in a patient who describes visual vertigo. The patient is a 29 year old male, referred to the service post head injury. The diagnosis was concluded as unilateral deficit as defined by video head impulse testing (vHIT) and Supression Head Impulse Paradigm test (SHIMP) results. The patient was initially seen 2 years post accident and sponteneous compensation/recovery had not occured. Subjective measures to monitor outcomes for rehabilitation included the Dizziness Handicap Inventory (DHI) and Visual Vertigo Analogue Scale (VVAS). The patient was asked to spend 5-10 minutes completing the tasks within virtual reality environment. The visually stimuating environment would increase to 20minutes after a period of desensitisation. After 9 months (time span due to travel restrictions and COVID19) the patients subjective scores and self reporting of visual vertigo increased significantly alongside the objective measurements. In vHIT Vestibulo-ocular reflex morphology was non-pathologocal with increased gains (increases of Lateral, 0.1, Posterior, 0.3 and Anterior, 0.2 in gain) and reduced asymmetry (Lateral, 9%, LARP, 35%, RALP, 26%). The Saccades of overt nature, become covert and gathered. Similarly with SHIMP the VOR morphology improved to mimic a non-pathological presentation, asymmetry significantly decreased and corrective saccades became gathered denoting a significantly reduced PR score (Left improvement, 14%, Right Improvement, 34%).
This case, albeit interesting, has limitations, predominantly due to the N number. However expansion of the study is in progress, inlusion criteria will be introducted, testing procedures randomly assigned and a statistically significant population will be recruited. The question of interest is whether virtual reality-based balance exercises performed during vestibular rehabilitation are superior to conventional balance exercises during vestibular rehabilitation in unilateral peripheral vestibular loss.
ST0130Apo-geotrophic nystagmus in a patient with cerebellar bleed
Hanaan Ashraf1,Vishal Pawar2
1Aster Al Rafa Polyclinic, International city Br. Dubai,U.A.E.; 2Aster Gardens Specialty clinic, Dubai, UAE
Target audience- Neurologists, Neurotologists, Otologists, Audio-vestibular physician
Theme
Introduction: Apogeotropic positional nystagmus is commonly seen with horizontal canal cupulolithiasis. However, it can be seen in some central lesions. The central causes include Vestibular migraine and tumours, stroke, demyelination, degenerative disorders involving the brainstem and cerebellum. It is imperative to differentiate it from benign paroxysmal positional vertigo (BPPV) involving the horizontal semicircular canal. We are presenting a case of apogeotrophic nystagmus seen in a patient with cerebellar nodular bleed.
Materials and Methods: The study was conducted at the outpatient dizziness unit, Aster Speciality Clinic, Dubai, UAE. All patients with positional vertigo underwent the Dix-Hallpike test (DHT), Head Roll test (HRT), Supine straight head extension (SSHE). We are presenting a case of cerebellar nodular haemorrhage manifesting positional vertigo and apo-geographic horizontal nystagmus.
Results: A 71 years gentleman, known diabetic and hypertensive, presented with positional vertigo for one month, each episode lasting 2-5 minutes. The patient was hospitalised with severe vertigo, imbalance, vomiting and headache one month ago in another facility and was diagnosed to have Intracerebellar bleed (Fig-1).
Fig-1)
CT brain showing left cerebellar hemorrhage involving the nodulus.

Cerebral angiography showed arteriovenous malformation. After discharge, he continued to have positional vertigo and nausea. Video-oculography (VOG) showed hypometric saccades, impaired smooth pursuit in horizontal and vertical planes. He had down-beating nystagmus in the dark suppressed on fixation. There were square wave jerks in central and horizontal gazes. HRT on the left showed right beating (apogeotrophic) nystagmus (Fig-2).
Fig-2)
Head roll test on left side showed right beating (apo-geotrophic) nystagmus
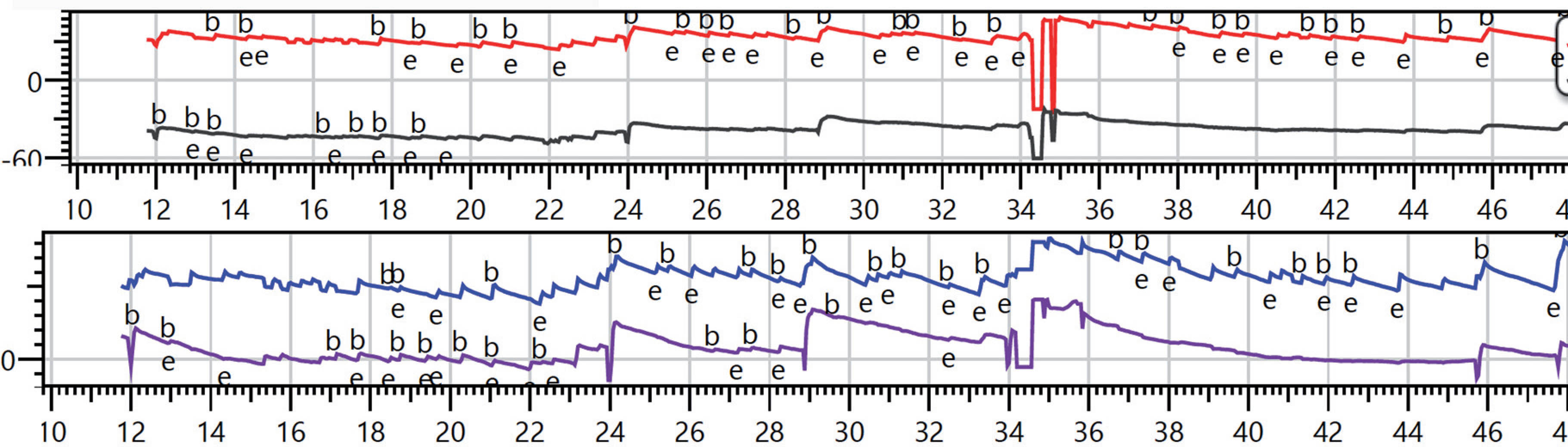
Discussion: The pathophysiological basis of the findings in our case is as follows.1) Positional nausea: It could be explained by the irritation of area postrema secondary to intraventricular haemorrhage or due to intracranial pressure changes. 2) Positional vertigo and nystagmus: Cerebellar nodulus is sensitive to gravity, and nodular lesions can cause positional vertigo and nystagmus, which explains the apogeotrophic nystagmus seen during the supine head roll test on the right in our patient. 3) Downbeating nystagmus suppressed by fixation: Nystagmus suppressed by fixation is usually seen in peripheral vestibular lesions. However, if flocculus or its connections are intact (as in our patient), the central nystagmus can get suppressed by fixation and mimic like peripheral. Hence, nystagmus seen without fixation does not exclude central aetiology.
Conclusion: Central pathologies should be considered in patients with apogeotrophic positional nystagmus. The pointers towards the central localisation include other central signs like saccadic abnormalities, impaired smooth pursuit, square wave jerks, down beating nystagmus. Hence thorough ocular motor testing is of paramount importance in the localisation of patients presenting with positional vertigo.
ST0131An explanation for individual variations in three-dimensional vestibular behavior
Chengqi Wang1, Amsal Madhani1, Faisal Karmali1
1Harvard Medical School / Massachusetts Eye and Ear, Boston, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Many vestibular patients complain of inappropriate perceptions of three-dimensional motion, and subjectively there are differences even amongst vestibular-normal individuals. In this study, we used computational models to begin to develop hypotheses for the physiologic reasons for these variations. It is well accepted that the vestibular organs are imperfect, yet the brain is able to synthesizes a robust estimate of three-dimensional motion and orientation in most individuals. Computational models accurately describe these central processes. A growing body of computational and experimental evidence suggests that these central processes are adaptatively adjusted to minimize error – i.e., optimize in a Bayesian sense - based on the statistics of vestibular neural noise (i.e., variability) and experienced motion. For example, we have previously used this approach to study changes with aging and peripheral damage that occur in the yaw angular velocity. In this case, while a longer time constant would be advantageous because this would make the VOR accurate over a longer period of time, it has been argued that this would result in the accumulation of noise by the velocity storage mechanism, which would result in drift and make the VOR less precise. In this study, we extended these results to three-dimensional processing. The first behavior we studied was post-rotatory tilts - 45 deg tilts of the body following the cessation of constant-velocity upright yaw rotation. As in previous studies, we used perceptual thresholds and signal detection theory to estimate vestibular noise. We predicted responses that cover the normal range of human vestibular noise by using published data on the range of human thresholds. These predictions showed that changing only SCC noise resulted in substantial variations in estimates of angular velocity, linear acceleration and the direction of gravity. These inappropriate estimates of motion persisted for many seconds. The second behavior we studied was off-vertical axis rotation – constant-velocity rotation about an axis tilted relative to the vertical. These predictions showed that changing only SCC noise resulted in notable variations in estimates of angular velocity, minor variations in estimates of linear acceleration, and no variations in the estimates of gravity. These results provide a first step in explaining interindividual variations in three-dimensional vestibular responses and could lead to a better understanding of dizziness and vertigo.
Acknowledgements: Funded by NIH/NIDCD R01-DC018287.
Posters Main Meeting
FP0865Effect of Gentamicin Induced Vestibular Ablation on Quality of Life and Visual Sensitivity in Patients after the Vestibular Schwannoma Surgery
Zuzana Balatkova1, Zdenek Cada1, Silvie Hruba1, Vladimir Koucky1, Veronika Bandurova1 Martin Komarc2, Rudolf Cerny3, Jan Plzak1
1Department of Otorhinolaryngology and Head and Neck Surgery, 1st Faculty of Medicine Charles University in Prague and Motol University Hospital, Postgraduate Medical School; 2Department of Anthropomotorics and Methodology, Faculty of Physical Education and Sport, Charles University in Prague; 3Department of Neurology, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: Improvement of quality of life and minimizing of vestibular disorders postoperatively is one of the current goals in treatment of patients with vestibular schwannoma. Postoperative dizziness and postural instability are not the only problems, increased sensitivity to complex visual stimuli may persist in a long term and thus deteriorates the quality of life. Preoperative chemical vestibular ablation can reduce vestibular symptoms in patients after vestibular schwannoma resection. Our aim was to evaluate the effect of preoperative application of gentamicin on postoperative quality of life and visual sensitivity.
Methods: 0.5-1.0 mL of 40 mg/mL nonbuffered gentamicin in at least three intratympanic instillations in 11 patients was administered two months prior to the surgery. Head impulse and caloric tests confirmed reduction of vestibular function in all patients. The control group consisted of 21 patients. Quality of life in both groups was evaluated by the Glasgow Benefit Inventory (GBI), the Glasgow Health Status Inventory (GHSI) and the Dizziness Handicap Inventory questionnaires. The psychological profile was evaluated using GAD-7, Generalised Anxiety Disorder Assessment and Zung Self-Rating Depression Scale questionnaires. Visual symptoms and optokinetic sensation were evaluated by specific questionnaire developed by our team and by measuring preoperative and postoperative gains of optokinetic nystagmus with routine electronystagmography in both groups.
Results: There were no statistically significant differences between both groups with regards to the results of questionnaires. Patients who received preoperative gentamicin were less sensitive to visual stimulation (p <0.10). Many of them had significantly higher gain in the optokinetic nystagmus than the control group. Significant difference of psychological profile survey was observed between the groups.
Conclusions: Preoperative gentamicin induced vestibular ablation helps to lower the level of anxiety in patients and improves their general postoperative status. Pre-treatment also helps to decrease the sensitivity to complex visual stimulation and combined sensory perception.
Study registration number is NCT03638310.
FP0866Does the pre-treament by chemical vestibular ablation decrease patients’sensitivity to optokinetic and optic flow stimulation after vestibular schwannoma retrosigmoid suboccipital resection?
Zdenek Cada1, Zuzana Balatková1, Rudolf Cerný2, Ondrej Cakrt3, Jan Plzák1
1Department of Otorhinolaryngology and Head and Neck Surgery, 1st Faculty of Medicine Charles University in Prague and Motol University Hospital, Postgraduate Medical School; 2Department of Neurology, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital; 3Department of Rehabilitation and Sports Medicine, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: Surgical removal of vestibular schwannoma causes acute vestibular symptoms, including postoperative vertigo, oscillopsia. Some patients are also more sensitive to optokinetic stimulation (optic flow). Preoperative chemical vestibular ablation can reduce vestibular symptoms postoperatively.The goal of two presented studies was to determine whether chemical vestibular prehabituation influences the patients’sensitivity to optokinetic stimulation.
Methods: In both studies 0.5-1.0 mL of 40 mg/mL nonbuffered gentamicin was injected preoperatively transtympanically in 21 patients (study group). Head impulse and caloric tests confirmed reduction of vestibular function in all patients. The control group consisted of 31 patients. Visual symptoms and optokinetic sensation were evaluated using a specific questionnaire developed by our team and by measuring optokinetic gain preoperatively and postoperatively in both groups. The psychological profile was evaluated in both groups by using the validated questionnaires for depression and anxiety.
Results: Gentamicin group was less sensitive to visual stimulation in both studies (p <0.05, p <0.10). Already preoperatively had the majority in the study group a significantly higher gain in the optokinetic nystagmus measurement than the control group.
Conclusion: Patients who received preoperative gentamicin were more resilient to optokinetic and optic flow stimulation.
This trial is registered with clinical study registration number NCT02963896.
FP0870Safe Stability! The importance of multisensory input for balance control in people with intellectual disabilities: a pilot study.
Laura Leyssens1, Ruth Van Hecke1, Karlien Moons1, Sofie Luypaert1, Melina Willems2,3, Maya Danneels1, Sarie Martens1, Cleo Dhondt4, Leen Maes1,5
1Department of Rehabilitation Sciences, University of Ghent, Belgium; 2Artevelde University of Applied Sciences, Ghent, Belgium; 3Special Olympics International; 4Department of Head and Skin, University of Ghent, Belgium; 5Department of Ear, Nose and Throat, University Hospital of Ghent, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background. Substantial evidence indicates that persons with intellectual disabilities (ID) are more susceptible for sensory impairments (e.g. hearing loss) and often experience motor problems (e.g. postural instability, frequent falling). Despite the anatomical and physiological proximity between the hearing and vestibular organ, and the well-established role of the vestibular system in several gross motor skills, data on the (peripheral) vestibular function is scarce in this population. This urged us to estimate the occurrence and characteristics of vestibular dysfunctions in the ID population, by applying a vestibular screening in a heterogeneous group of adult persons with ID and an age- and gender-weighted control group. Additionally, in a subgroup of the participants with ID, the auditory, visual, and postural balance function was evaluated in addition to the vestibular function, to explore the impact of (multi)sensory dysfunctions on the postural balance performance.
Methods. 45 adults with ID (18-61 years) participated to a vestibular screening protocol (cVEMP & vHIT) at the National Games of Special Olympics Belgium, of which 30 athletes (18-61 years) also completed an auditory (sequential protocol consisting of DPOAEs, tympanometry, and audiometry), visual (SVA), and postural balance evaluation (RS and SLS on a force platform, mFRT, and TUGT). Additionally, an age- and gender-weighted control group of 42 adults without ID (19-58 years) was subjected to the same vestibular screening protocol, of which 25 subjects (19-59 years) also underwent the postural balance evaluation.
Results. Compared to the control group, the occurrence of abnormal cVEMP and vHIT responses was significantly higher in the ID group, and the ID subjects performed significantly worse and/or showed more body sway for all balance tasks except the TUGT. Within the ID group, a significant positive correlation was observed between the number of failed sensory screening items and the number of failed balance tasks.
Conclusion. This study suggests an increased prevalence of peripheral vestibular deficits and postural balance problems in people with ID relative to the general population, and significant involvement of peripheral sensorial deficits in these postural balance dysfunctions.
Abbreviations.
ID=intellectual disabilities
cVEMP = cervical vestibular evoked myogenic potentials
vHIT = video head impulse test
DPOAEs = distortion product otoacoustic emissions
SVA = static visual acuity
RS = Romberg stance
SLS = single leg stance
mFRT = modified functional reach test
TUGT = timed-up-and-go test
FP0873A New Spin on Sensory Organization Testing
Colin R. Grove1, G. Mark Pyle2, Bryan C. Heiderscheit3, Kristin E. Caldera3, Scott J. Hetzel4, Susan L. Whitney5
Johns Hopkins University1; University of Wisconsin-Madison: Departments of Surgery2; Orthopedics and Rehabilitation3; and Biostatistics4; University of Pittsburgh: Department of Physical Therapy5
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: The Sensory Organization Test (SOT) is a test of balance in vestibular-impaired persons. Historically, despite excellent sensitivity, its diagnostic value has been diminished by poor specificity. Further, there is lingering uncertainty regarding what this test measures since performance on the SOT has not been strongly correlated with vestibular function tests, patient-reported outcomes, functional balance tests, or gait. Despite its shortcomings, the SOT is frequently used as an outcome in vestibular rehabilitation. Recently, the Bertec Balance Advantage (BBA) computerized dynamic posturography device was developed which includes a new version of the SOT (BBA-SOT). The protocol for the BBA-SOT is similar to the SOT; however, the new test is implemented using high-precision force plates and a virtual reality projection system. Given these enhancements, the psychometric properties of the BBA-SOT must be explored. The aims of this study were to examine the criterion and convergent validity of the BBA-SOT.
Methods: A total of 34 adults, 17 vestibular-impaired (9 women, age 61.1; sd 10.2) and 17 healthy (13 women, age 39.3; sd 11.2) participated in this study. Criterion validity was evaluated by calculating the area under the curve (AUC) using receiver operator characteristic analysis. We assessed convergent validity by calculating Spearman’s correlation coefficient between overall performance on the BBA-SOT and the Activities-specific Balance Confidence (ABC) scale, Dizziness Handicap Inventory (DHI), non-instrumented Dynamic Visual Acuity Test (NI-DVAT), Five-times Sit to Stand Test (FTSTST), Functional Gait Assessment (FGA), and an instrumented 2-minute walk test (i2MWT).
Results: The AUC (95% CI) for the BBA-SOT composite score was 0.95 (0.88,1). The correlations (95% CI) between the BBA-SOT composite score and other specific outcomes of interest were: 0.71 (0.49, 0.85) (ABC average score), -0.8 (-0.9, -0.64) (DHI total score), -0.69 (-0.83, -0.46) (degradation in visual acuity, horizontal NI-DVAT), -0.69 (-0.83, -0.45) (degradation in visual acuity, vertical NI-DVAT), -0.59 (-0.77, -0.31) (FTSTST time), 0.73 (0.52, 0.86) (FGA total score), as well as 0.51 (0.18, 0.74) (gait speed), -0.61 (-0.8, -0.32) (terminal double support, left), -0.44 (-0.69, -0.1) (terminal double support, right), 0.63 (0.36, 0.81) (turn velocity), and -0.61 (-0.8, -0.32) (turn duration) from the i2MWT.
Conclusions: The BBA-SOT composite score has excellent ability to discriminate between healthy and vestibular-impaired adults. Overall performance on the BBA-SOT is moderately to strongly correlated with measures of balance-related confidence, dizziness-related perceived handicap, dynamic visual acuity, balance, and gait. These findings support the use of the BBA-SOT as a valid balance test.
FP0877A Link Between Posturography and Vestibulo-Ocular Reflex
Manuel Oliva-Domínguez1; María Dolores Aguilar-Conde2; Juan Bartual-Magro3; Juan Bartual-Pastor4
1Hospital Costa del Sol (Marbella, Spain); 2Hospital Virgen de la Victoria (Málaga, Spain); 3Hospital Virgen de la Cocha (Zamora, Spain); 4Chairman of Otolaryngology, retired (Cádiz, Spain)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Our study wil connect the vestíbulo-ocular reflex gain to the performance in posturographic tests.
Material and Methods: all patients included in this study underwent a vHIT in the horizontal plane, recording the instantaneous gain at 60 msec. To get a result regardless of the affected side, we added the results to the right and left manoeuvres in the same patient.
Posturographics tests were recorded by means of a triaxial accelerometer device attached to the patient’s head. This device records the acceleration exerted in every spatial plane. Through trigonometry, we can calculate the angle made up in every plane. Eventually, 90% of the amplitude of the angle change was calculated. To get a single representative value, the equation 2*Pitch + Roll + Yaw was applied.
All patients underwent the mCTSIB protocol plus Unterberger-Fukuda test, recording 20 secs for every test.
Next, we applied a linear regression fit model, pairing the oscillation amplitudes in posturography with the vestíbulo-ocular reflex gain, working out the regression coefficient and statistic significance by means of p value. Significance was set up to 0.05
In the end, we also checked out the relationship between vHIT and oscillations in every spatial plane, if a significant p value is found in a test
RESULTS: our series includes 165 patients, mean age 56.85 years, 40% men and 60% women. Results in mCTSIB are, regression coefficient and p value, -0.02 and 0.56 (s2eo), -0.03 and 0.54 (s2ec), -0.04 and 0.43 (s2eof), -0.08 and 0.31 (s2ecf). Unterberger-Fukuda test, however yielded a coefficient of -0.28 and p value 0.000043.
Next, linear fit model was applied, as detailed before, for Unterberger-Fukuda test in every spatial plane. Results were, coefficient and p value: -0.05 and 1.27e-06 (Roll), -0.03 and 0.001 (Pitch), -0.16 and 0.005 (Yaw)
CONCLUSIONS: Unterberger-Fukuda test is the only posturographic test were significant statistical results were found, showing that head oscillations increase as vestíbulo-ocular reflex gain decreases. This link is more pronounced in the yaw plane, which meets the plane where the vHIT was performed
FP0882Including an Otoneurologist in the infectious endocarditis protocol
Angel Batuecas Caletrío, Sofía Ferreira Cendón, Maria José Fernandez Nava, María Gil Melcón, Hortensia Sánchez Gómez
Otoneurology unit. ENT Department. IBSAL. University Hospital of Salamanca. Salamanca. Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
POSTER: Infectious endocarditis is a serious infection in the heart cavities. Systemic gentamicin is the first choice treatment in most protocols. The vestibulotoxic effect of gentamicin is well demonstrated. We studied the importance of including the vestibular tests in the assistance protocol of patients treated of infective endocarditis with systemic gentamicin.
Methods: We studied two groups of patients treated for their infectious endocarditis with systemic gentamicin. The first group before including an otoneurologist in the assitance protocol and the second group after including it.
We analyze the time from the beginning of the treatment until the onset of symptoms, the time to be assessed by an otoneurologist, the vestibular damage produced, the presence or not of oscillopsia and the recovery of the damage.
Results: 29 patients were included in the study. 13 in group 1 and 16 in group 2. The paceintes of group 1 took 65 days to be assessed by an otoneurologist and those of group 2 only 2. The average VOR gain measured through vHIT was 0.39 and 0.44 in patients in group 1 and 0.64 and 0.71 in group 2. 5/13 patients in group 1 suffered from oscillopsia while in group 2 only 3/16.
Conclusions: Since the effect of systemic Gentamicin in the vestibule is known and that this mediation is of first choice in the treatment of infective endocarditis, an otoneurological assessment should be included in these patients to prevent severe damage to vestibular function.
FP0883Skull VIbration induced nystagmus: optimizing tests
Angel Batuecas Caletrío1, Sofía Ferreira Cendón1, Maria José Fernandez Nava1, Juan Carlos del Pozo de Dios1, Hortensia Sánchez Gómez1, Vanessa Pérez Guillén2
1Otoneurology unit. ENT Department. IBSAL. University Hospital of Salamanca. Salamanca. Spain; 2Otoneurology unit. ENT Department. Hospital universitario La Fe. Valencia. Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
POSTER: Skull vibration induced nystagmus (SVIN) is a useful and easy resource that provides great information about vestibular function.
The relationship of the findings in the SVIN with other vestibular tests has already been studied. But the relationship between the SVIN findings and the findings in the Video Head impulse test is unknown.
Methods: We analyze and compare the findings in 63 patients with vestibular neuritis in both SVIN and vHIT. Patients were studied at least six months after suffering vestibular neuritis.
Results: 38 men and 25 women were included in the study. 33 right and 30 left. In all cases the nystagmus was directed towards the healthy side.
The stimulation frequency that achieved a higher percentage of SVIN appearance was 100Hz. A moderate correlation was obtained between the appearance of SVIN and the gain asymmetry measured through vHIT. The SVIN appeared in all cases in which there was a difference between the gains of the healthy side and the affected side above 0.31
Conclusions: In cases of vestibular neuritis, the presence of a positive SVIN correlates with a large asymmetry in the vestibuloocular reflex gains. The SVIN is a useful test for the location of the diseased side in cases of vestibular neuritis.
FP0884Advantages of VHIT in the evaluation of recently postoperated patients
Zenaida Piñeiro-Aguín1, Albert Pujol-Olmo2, Olga Ferrer-Andino3
1Parc de Salut Mar – Hospital del Mar. Barcelona; 2Hospital de la Santa Creu i Sant Pau. Barcelona; 3Pars Sanitari Sant Joan de Deu. Sant Boi de Llobregat
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Advantages of VHIT in the evaluation of recently postoperated patients
Introduction: After middle ear surgery, especially Stapedectomy, acute episodes of vertigo and vestibular syndromes may occur. From the introduction of VHIT, these patients can be evaluated 24 hours after the intervention or even immediately if the patient has symptoms. The precision in the involvement of the VOR gives us a topographic diagnostic.
Material and methods: Over a period of three years (2016 - 2019), 16 patients with postoperative vestibular symptoms were reviewed. Mainly stapedectomy (9 cases) and myringoplasty (7 cases) performing VHIT initially, at 3 months and one year after the intervention, if the initial VHIT was pathological. In 5 patients, vestibular pathology with alteration of the VOR was found and in two cases the examination was normalized. In two of the cases the affectation was due to the inferior vestibular nerve only, ipsilateral to the surgery.
Results and Discussion: In the 5 pathological cases, an improvement of the dispersion in the PR index was observed, well correlated with the patient’s clinic that improves the symptomatology as the saccades are grouped. In accordance with the literature, VHIT is a good predictor of clinical improvement in postoperative patients. With this method, the function of the vestibule can be evaluated even with the healing eardrum and without applying water or air to the surgical bed.
Conclusions: VHIT is an effective and safe method for the evaluation of patients after middle ear surgery. The speed and simplicity of the method gives us security and precision in the diagnosis of possible postoperative hipofunctions of the vestibule. In future work, the vestibular function must be evaluated before and after surgery, mainly in Otosclerosis.
FP0885Value of targeted bedside neuro-otological examination in the acutely dizzy patient
Alexander A. Tarnutzer1,2, Daniel Gold3, Zheyu Wang4,5, Karen A. Robinson6, Jonathan A. Edlow7,8, Terry D. Fife9,10, Jorge C. Kattah11, Kevin A. Kerber12, Georgios Mantokoudis13, Elizabeth Marsh3, Ali S. Saber Tehrani3, David S. Zee3, David E. Newman-Toker3
1Cantonal Hospital of Baden, Baden, Switzerland; 2Faculty of Medicine, University of Zurich, Zurich, Switzerland; 3Johns Hopkins University School of Medicine, Department of Neurology, Baltimore, MD; 4Division of Biostatistics and Bioinformatics, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University School of Medicine; 5Johns Hopkins Bloomberg School of Public Health, Department of Biostatistics, Baltimore, MD; 6Johns Hopkins University School of Medicine, Department of Medicine, Baltimore, MD; 7Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, MA; 8Harvard Medical School, Boston, MA; 9Department of Neurology, Barrow Neurological Institute, Phoenix, AZ; 10Department of Neurology, University of Arizona College of Medicine, Phoenix, AZ; 11University of Illinois College of Medicine. Peoria, IL; 12Department of Neurology, Health Services Research Program, University of Michigan, Ann Arbor, MI; 13Department of Otorhinolaryngology, Head and Neck Surgery, lnselspital, Bern University Hospital, University of Bern, Bern, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Acute dizziness/vertigo is usually due to benign inner ear causes but occasionally due to dangerous neurologic causes, particularly stroke. Because symptoms and signs are superficially similar, misdiagnosis is a serious concern and overuse of diagnostic tests is common. Here we assessed the accuracy of symptoms and physical examination findings in acutely dizzy adults to identify those with central neurologic causes, particularly stroke. We performed a systematic search of MEDLINE and Embase (1980-2016) to identify studies reporting on the diagnostic accuracy of bedside vestibular tests in acutely dizzy patients. Studies were included that measured the performance of bedside findings for identifying peripheral versus central causes using a reference standard of neuroimaging (magnetic resonance imaging with diffusion weighted images [MRI-DWI]). Studies reporting on either episodic, positionally-triggered vertigo or acute, prolonged vertigo were screened. 3722 unique articles were identified, of which 18 met inclusion criteria. Two authors independently performed critical appraisal and data extraction. Sensitivity, specificity and likelihood ratios were calculated for individual physical examination findings for acute vertigo. Six studies reported preliminary data. No high-quality studies differentiating benign paroxysmal positional vertigo from central positional vertigo in patients with positionally-triggered episodes were identified. For the acute vestibular syndrome (AVS), 12 studies (prospective=6; retrospective=6) with a total of 607 patients were included with a range of 8 to 191 patients per study. 415 patients had central causes (with 373 ischemic strokes). Eye movement abnormalities and truncal instability/gait disturbance were the clinical signs with the highest diagnostic value to distinguish peripheral and central causes of AVS. A three-step bedside testing battery “H.I.N.T.S.” (Head Impulse, Nystagmus, Test of Skew) had excellent diagnostic properties when performed by specialists (sensitivity 0.97 [0.94-0.99, 95%CI]; specificity 0.91 [0.87-0.95]). Severe (grade 3) truncal/gait ataxia had high specificity (0.96 [0.93-0.99]) but low sensitivity (0.45 [0.37-0.52]). Early MRI-DWI (i.e., within the first 24-48 hours) was able to be assessed in 124 patients and was falsely negative in one of five stroke patients (sensitivity 0.79 [0.72-0.86]). In AVS, eye movement examination by specialists can differentiate peripheral from central causes and appears to have higher diagnostic accuracy for stroke than even MRI-DWI in the first 48 hours after onset of symptoms. Future studies should design and evaluate methods to disseminate and implement these techniques to frontline clinical practice.
FP0889The Dizziness Handicap Inventory as a predictor of sick leave
Mari Kalland Knapstad1,2, Frederik Kragerud Goplen1,3, Stein Helge Glad Nordahl1,3, Jan Erik Berge1,3
1Norwegian National Advisory Unit on Vestibular Disorders, Department of Otorhinolaryngology & Head and Neck Surgery, Haukeland University Hospital, Bergen, Norway; 2Department of Health and Functioning, Western Norway University of Applied Sciences, Bergen, Norway; 3University of Bergen, Department of Clinical Medicine, University of Bergen, Bergen, Norway
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Dizziness is a common complaint in the adult population and is associated with reduced quality of life, psychological comorbidity and financial burden for both patients and health care systems. The Dizziness handicap inventory (DHI) is a commonly used questionnaire for assessing the self-perceived handicap in dizzy patients. The aim of this study was to examine the association between the DHI and sick leave.
Methods: This was a cross-sectional study conducted at an otolaryngology clinic. We included a total of 238 patients between 18 – 67 years old, referred for either balance or dizziness symptoms during a 1-year period. Sick leave the last 30 days was categorized as no sick leave, <50% sick leave, >50% sick leave or 100% sick leave. The association between sick leave over the last 30 days and DHI was examined with binary and ordinal logistic regression analysis. The hospital anxiety and depression scale (HADS), Health-related quality of life (RAND-12), diagnosis, duration of dizziness, age and gender were used as covariates.
Results: A total of 63 males (mean age 46.4 (SD 10.8)) and 175 females (45.4 (SD 12.6)) were included, with 46% diagnosed with a peripheral vestibular disorder. Adjusting for covariates, the logistic regression analysis showed that a 10-point increase on DHI (range: 0 – 100) was associated with being on sick leave (yes/no) the last 30 days (OR: 1.50, 95% CI: 1.25 – 1.90, p <0.001). Categorizing sick leave status, using no absence as base outcome, a 10-point increase in DHI-score was associated with a higher degree of sickness absence in the adjusted analysis (OR: 1.50, 95% CI: 1.25 – 1.80, p < 0.001).
Conclusion: In this study, we found that a higher score on DHI is associated with the degree of sick leave the last 30 days, even after adjusting for health-related quality of life, anxiety and depression symptoms. These results indicate the clinical usefulness of the DHI as a possible predictor of sick leave in patients with dizziness.
FP0891Development of an Application for Vestibular Rehabilitation for Older Adults Informed by Clinical Care
Linda D’Silva2, Karen Skop3, Michael Rossi1, Jeremy Martin1, Katherine Marschner1, Nathan T. Pickle1, Timothy Zehnbauer1, Paulien E. Roos1
1CFD Research Corporation, Huntsville AL, USA; 2University of Kansas Medical Center, Kansas City, KA; 3: Jame Haley VA Hospital, Tampa, FL
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Almost half of people over the age of 60 experience dizziness. Vestibular rehabilitation has been proven effective in reducing dizziness and falls. However, adherence to exercise programs remains a major problem and can be below 50%. Clinicians typically rely on patient self-reporting to assess adherence and are often unsure if exercises were performed correctly at-home. Therefore, this research aimed to develop an app with gaming elements and remote monitoring to improve adherence of older adults to gaze stabilization and balance exercises.
Methods: Games for VORx1, two target, and two different balance exercises (weight shift and single leg) were developed and incorporated in an app. The app allows exercise prescription and remote monitoring through a web portal. A clinician informed design was used when five physical therapists were asked identical questions about the exercises they would like to see represented in the app, the duration, and frequency of exercises. The app provides exercises in the form of games that are controlled by an Inertial Measurement Unit (IMU) sensor placed on the head or sacrum. The app was tested on ten healthy females aged 60-74 years (69.1± 5.1 years). Participants completed gaze stabilization and balance exercises using the app and provided feedback on use intention, ease of use, usefulness and enjoyment using questionnaires and open-ended questions.
Results: for 2 out of 4 games, 9 out of 10 subjects showed high enjoyment. All 10 subjects responded they would find the app easy to use, found it useful to do exercises, would use it again if they had dizziness issues, and felt motivated when playing the games. 3 out of 10 subjects felt frustrated and/or worried while using the app. The open-ended questions showed this was due to confusion on game instructions. Subjects liked the colors and graphics in the games for the different exercise levels.
Conclusions: This study demonstrated that an app for vestibular rehabilitation with gaming elements was found enjoyable and useful by older adults and was easy to use. It highlighted areas that may cause frustration and need improvement. On the longer term the app may increase adherence of older adults to vestibular rehabilitation exercises due to the game design, remote monitoring, and feedback.
This research was supported by the NIDCD of the NIH (Award R44DC017408). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
FP0892Influence of Testing and Measurement Variables on High Frequency Visuo-Vestibular Interaction and VOR Suppression Quantified Clinical Tests.
Maria Montserrat Soriano-Reixach, Elisabeth Ninchritz-Becerra, Izaskun Thomas-Arrizabalaga, Ariadna Valldeperes-Vilanova, Jorge Rey-Martinez, Xabier Altuna.
Neurotology Unit. ENT Department. Hospital Universitario Donostia. San Sebastián - Donostia. Spain.
Quantified VVOR and VORS tests has been recently added to available clinical vestibular tests. But despite clinical validity of these quantified tests that appear to have an increasing clinical interest, the influence of most of clinical testing method and mathematical analysis variables are not well defined for clinical testing purposes. The objective of this study is to investigate the main influence of some testing and analysis variables on clinical quantified VVOR and VORS results. For that, a prospective observational clinical study on 19 heathy patients has been realized. Every participant was examined with quantified visually enhanced vestibular-ocular reflex test and vestibulo-ocular reflex suppression test. The results of the study are the follow ones: a significant statistical difference between the three VVOR, VORS with no reinforce paradigm and VORS reinforce paradigm tests was found for a mean gain values of 0.91 ± 0.09 and 0.6 ± 0.15 and 0.57 ± 0.16 respectively (p < 0.001). Optimized linear model showed a significant influence of frequency on gain values for reinforced VORS and non-reinforced VORS test (p = 0.01 and p = 0.004, respectively). Attending to gain analysis method, statistical significant differences were found depending on the short time sample location of the records for initial location of VVOR test (p < 0.006) and final location of VORS with reinforced paradigm test (p < 0.023). In conclusion, there are significant differences for gain values according to VVOR and VORS testing as effect of VOR suppression. Head movement frequency is a significant factor that affect to the gain values especially for VORS testing. Also, for VORS testing there is a significant effect of participant concentration on testing task for suppression gain values. When a short time window sample is considered for VVOR and VORS testing, middle located time samples appears to be most adequate for both tests.
FP0898Psychometric properties of the abbreviated Dizziness Handicap Inventory (DHI-S) in general practice
Vincent A. van Vugt1, Henrica C.W. de Vet 2, Johannes C. van der Wouden1, Henk C. P. M. van Weert1, Henriëtte E. van der Horst1, Otto R. Maarsingh1
1Department of general practice, Amsterdam UMC, Amsterdam Public Health, The Netherlands; 2Department of epidemiology and biostatistics, Amsterdam UMC, Amsterdam Public Health, The Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The 25-item Dizziness Handicap Inventory (DHI) is worldwide the most used questionnaire to assess impairment due to vestibular symptoms and measure treatment success. However, the DHI’s length limits applicability in daily clinical practice. The abbreviated 10-item DHI-S is a promising alternative. The aim of this study was to assess the validity, reliability, responsiveness, optimal cut-off point for substantial impairment and the minimally important change of the DHI-S in general practice.
Methods: We performed a psychometric evaluation of the DHI-S questionnaire in general practice. In a prospective cohort study 415 adults with vestibular symptoms (aged = 65 years) were diagnosed with regard to subtype(s) and underlying cause(s) after a full diagnostic workup. Participants filled out the 25-item DHI at baseline, and one week, six months and ten years follow-up. The DHI answers were used to calculate DHI-S scores. Validity was assessed by criterion validity (Pearson’s r) at each measurement. Longitudinal measurements were used for test-retest reliability (intraclass correlation coefficient) and responsiveness (Pearson’s r). We used ROC curve analyses to determine optimal DHI-S cut-off points for substantial impairment (=30 DHI) and minimally important change (>11 DHI).
Results: The DHI-S demonstrated excellent criterion validity (r = 0.93-0.96), test-retest reliability (ICC =0.86) and responsiveness (r = 0.89). The DHI-S reliably distinguished substantial impairment and identified minimally important change, with optimal DHI-S cut-off scores of =12 points and >5 points, respectively.
Conclusion: The DHI-S is a valid, reliable, and responsive questionnaire that can replace the DHI in general practice. The DHI-S could potentially become a valuable tool in the management of patients with vestibular symptoms.
FP0901The Resilience of the Inner Ear - Vestibular and Audiometric Results after Transmastoidal Plugging of a Semicircular Canal
Joost J. A. Stultiens1, Nils Guinand2, Vincent van Rompaey3, Angélica Pérez Fornos2, Henricus P.M. Kunst1, Hermanus Kingma1, Raymond van de Berg1
1Department of Otorhinolaryngology & Head and Neck Surgery, School for Mental Health and Neuroscience, Faculty of Health Medicine and Life Sciences, Maastricht University Medical Center, Maastricht, The Netherlands; 2Division of Otorhinolaryngology and Head-and-Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 3Department of Otorhinolaryngology and Head & Neck Surgery, Faculty of Medicine and Health Sciences, Antwerp University Hospital, Antwerp, Belgium.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Currently, only few indications exist for surgical intervention in peripheral vestibular disorders. However, some patients are not sufficiently treated by conservative care and the pathophysiology provides options for surgical therapy. Certain patients with intractable benign paroxysmal positional vertigo or superior canal dehiscence syndrome may opt for plugging of the affected semicircular canal to relieve them from disabling symptoms. However, structured data of the impact of this procedure on vestibular function and hearing is lacking. The aim of the current study is to assess evolution of vestibular and audiometric function after transmastoidal plugging of a semicircular canal.
Methods: Patients undergoing transmastoidal plugging of a semicircular canal for superior semicircular canal dehiscence syndrome or for benign paroxysmal positional vertigo were selected and underwent pre- and postoperative assessment of vestibular and audiometric function. This assessment consisted of bithermal caloric irrigation test, video Head Impulse Testing, cervical and ocular vestibular evoked myogenic potentials, and pure tone audiometry. Patients were tested postoperatively at one week, two months and six months follow up. A CT scan was performed six months postoperatively.
Results: Low-frequency vestibulo-ocular reflex (VOR) response declined initially in 6/6 patients and high-frequency VOR gain declined in 4/6 patients. Postoperative VOR response recovered to >60% in 4/6 patients and high-frequency VOR gain was restored to =86% of the preoperative value in 5/6 patients for both ipsilateral non-plugged semicircular canals. Four patients preserved cervical and ocular VEMP responses. Bone conduction hearing deteriorated in 3/6 patients, but recovered within six months postoperatively, although one patient had a persistent loss of 15 dB at the 8 kHz threshold.
Conclusion: Impact of semicircular canal plugging varies widely between patients. It seems that ipsilateral vestibular function decreases postoperatively in all patients and auditory function decreases in some patients. However, several patients show almost full restoration of the function of the two non-plugged semicircular canals and auditory function within six months postoperatively. Therefore timing of the postoperative assessment is essential for outcome assessment. These results are important for counseling of patients undergoing plugging of a semicircular canal and for the development and implementation of other procedures involving surgery of the semicircular canal, such as vestibular implantation.
FP0905SHIMP versus HIMP in diagnosing patients with Bilateral Vestibulopathy
T.S. van Dooren1,4, B. Dobbels8*, F.M.P. Lucieer1*, D. Starkov1,2, A.M.L. Janssen4,5, N. Guinand1,6, A. Pérez Fornos6, V. Van Rompaey7,8, H. Kingma1,2, R. van de Berg1,2* both authors share equal contribution
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Centre, Maastricht, Netherlands; 2Faculty of Physics, Tomsk State Research University, Tomsk, Russia; 3Faculty of Health, Medicine and Life Sciences, University of Maastricht, Maastricht, Netherlands; 4Department of ENT/Audiology, School for Mental Health and Neuroscience (MHENS), Maastricht University Medical Centre, Maastricht, The Netherlands; 5Department of Methodology and Statistics, Care and Public Health Research Institute (CAPHRI), Maastricht University, Maastricht, The Netherlands; 6Service of Otorhinolaryngology Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 7Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; 8Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Edegem, Belgium.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Introduction. A horizontal vestibulo-ocular reflex gain (VOR gain) of < 0.6, measured by the video head impulse test (VHIT or HIMP), is one of the diagnostic criteria for bilateral vestibulopathy (BV) according to the Báràny Society. However, VOR gain calculations can be influenced by compensatory saccades during the head impulse (i.e. covert saccades). To overcome this issue, eye movements are desaccaded by the HIMP paradigm. An alternative is the Suppression Head Impulse test (SHIMP), since it reduces covert saccades in BV patients which make VOR gain calculations probably more reliable. The goal of this study was to determine the clinical consequences of using SHIMP instead of HIMP when diagnosing BV.
Methods. This study comprised 98 BV patients (diagnosed according to the Báràny criteria in Antwerp University Hospital and Maastricht University Medical Centre). They were sequentially tested with HIMP and SHIMP paradigm (Otometrics). Artefacts were removed from all impulses. A custom-made algorithm was used for saccade detection. VOR gain (area under the curve) was calculated on the artefact free impulses. Both VOR gain and the frequency of covert saccades were compared between the two tests. Lastly, the agreement on BV diagnosis (VOR gain < 0.6 or not) between the two paradigms (HIMP and SHIMP) was assessed.
Preliminary results. BV patients in this study showed significantly fewer covert saccades during SHIMP, compared to HIMP (p=0.001 and p=0.006 for rightwards and leftwards head impulses respectively). VOR gain differed statistically significant between SHIMP and HIMP for both rightwards and leftwards head impulses (p < 0.000), where mean VOR gain during SHIMP was lower (0.35 in HIMP for both sides, 0.32 in SHIMP rightwards, and 0.33 in SHIMP leftwards). In 90% of the patients there was agreement between SHIMP and HIMP on the diagnoses of BV (VOR gain <0.6 or not).
Conclusion. To our knowledge, this is the largest study population on SHIMP testing in BV patients. Covert saccades and VOR gains were significantly reduced during SHIMP, compared to HIMP. However, the clinical relevance of these statistically significant differences is small. Based on this large study population, current HIMP and SHIMP paradigm are both able to diagnose BV. To conclude, the current HIMP paradigm seems to be sufficient to identify BV, despite of the interference of covert saccades.
FP09083 Tesla MRI of Vestibular Endolymphatic Space in patients with isolated Cystic Lateral Semicircular Canal Malformation
Víctor Manuel Suárez-Vega, Pablo Domínguez, Nicolás Perez-Fernandez
Clínica Universidad de Navarra
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Research background: Congenital malformations of the inner ear are characterized by small structural changes and variations in the anatomical development. Among them, one of the most frequent malformation of the bony labyrinth is the one affecting the lateral semicircular canal (LSCC). Isolated LSCC dysplasia (LSCCD) shows no cochlear associated abnormalities and no dilated vestibular aqueduct. The aim of this study is to depict morphology and size of the endolymphatic space in the vestibules of patients with isolated LSCCD using a dedicated 3D high resolution MR sequence called 3D inversion recovery with REAL reconstruction (3D-REAL-IR).
Methods: From January 2018 to February 2020, we reviewed 281 CT and 241 MR temporal bone studies as well as 103 MR studies performed for the evaluation of endolymphatic hydrops (EH). Five patients with LSCCD were found, one of them with bilateral malformation. Three patients (4 affected ears) underwent specific MR examination for the evaluation of EH, consisting on a heavily T2-weighed cysternography sequence (T2 SPACE) and a 3D inversion-recovery with REAL reconstruction. The endolymphatic volumetric ratio (ELR) was calculated as the total endolymphatic volume divided by the total perilymph volume multiplied by 100. Manually delineation of structures by an experienced radiologist and semi-automated generated volumes by the software were obtained.
Results: Hydrops MR imaging was available in 4 of the affected ears. According to the endolymphatic ratio, the most severe ear had a clinical diagnosis of Meniere’s disease and the endolymphatic space encompassed the 81% of the total vestibular lymphatic space, whereas the contralateral “asymptomatic” ear showed a physiological ER of 16%. A patient affected with hearing loss had an ER of 33% and the last affected ear was found incidentally in a patient who was scanned for migraine, with a surprising ER of 42%.
Conclusions: Endolymphatic hydrops imaging is feasible and can be performed on patients with inner ear malformations like the LSCCD. The endolymphatic volumetric ratio could be a useful and easily applicable tool in daily clinical practice. The Target audience Othologist with special interest in vestibular pathologies and Meniere’s disease, as well as Head and Neck Radiologists.
FP0913Bilateral Vestibulopathy Patients’ Perspectives on Vestibular Implant Treatment: A Qualitative Study
Lisa van Stiphout1, Florence Lucieer1, Nils Guinand2, Angélica Perez Fornos2, Maurice van de Berg1, Vincent van Rompaey3, Josine Widdershoven1,3, Herman Kingma1,4, Manuela Joore5,6, Raymond van de Berg1,4
1Department of Otorhinolaryngology and Head and Neck Surgery, Division of Balance Disorders, Maastricht University Medical Center, School for Mental Health and Neuroscience, Maastricht, Netherlands; 2Service of Otorhinolaryngology Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 3Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; 4Faculty of Physics, Tomsk State Research University, Tomsk, Russian Federation; 5Department of Clinical Epidemiology and Medical Technology Assessment (KEMTA), Maastricht University Medical; 6Care and Public Health Research Institute (CAPHRI), Maastricht University, Maastricht, The Netherlands
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: The aim of this study was to explore expectations of patients with bilateral vestibulopathy regarding vestibular implant treatment. This could advance the definition of recommendations for future core outcome sets of vestibular implantation and help to determine on which characteristics of bilateral vestibulopathy future vestibular implant research should focus.
Methods: Semi-structured interviews were conducted with 50 patients diagnosed with bilateral vestibulopathy at Maastricht UMC+. Interviews followed a semi-structured interview guide and were recorded and transcribed. Transcripts were analysed thematically by two independent researchers. A consensus meeting took place to produce a joint interpretation for greater dimensionality and to confirm key themes.
Results: Overall, patient expectations centralized around three key themes: (physical) symptom reduction, functions and activities, and quality of life. These themes appeared to be interrelated. Patient expectations focused on the activity walking (in a straight line), reducing the symptom oscillopsia and being able to live the life they had before bilateral vestibulopathy developed. In general, patients indicated to be satisfied with small improvements.
Conclusion: This study demonstrated that patient expectations regarding a vestibular implant focus on three key themes: symptom reduction, functions and activities, and quality of life. These themes closely match the functional improvements shown in recent vestibular implantation research. The results of this study provide a clear guideline from the patient perspective on which characteristics of bilateral vestibulopathy, future vestibular implant research should focus.
FP0914Development and content validity of the Bilateral Vestibulopathy Questionnaire
Lisa van Stiphout1, Israt Hossein1, Merel Kimman2, Susan Withney3, Andrianna Ayiotis4, Michael Strupp5, Nils Guinand6, Angélica Pérez Fornos6, Angel Ramos7, Vincent Van Rompaey8, Raymond van de Berg1
1Department of Otorhinolaryngology and Head and Neck Surgery, Division of Balance Disorders, Maastricht University Medical Center, School for Mental Health and Neuroscience, Maastricht, Netherlands; 2Department of Clinical Epidemiology and Medical Technology Assessment (KEMTA), Maastricht University Medical center, Maastricht, Netherlands; 3Department of Physical Therapy, School of Health and Rehabilitation Sciences, Duquesne University, Pittsburgh, Pennsylvania, U.S.A; 4The Departments of Otolaryngology–Head and Neck Surgery and Biomedical Engineering, Johns Hopkins University School of Medicine, Baltimore, U.S.A.; 5The Department of Neurology, University of Munich, Munich, Germany; 6Service of Otorhinolaryngology Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 7Department of Otolaryngology, Head and Neck Surgery, Complejo Hospitalario Universitario Insular Materno Infantil de Gran Canaria, Las Palmas, Spain; 8Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: To date, the burden and severity of the full spectrum of bilateral vestibulopathy (BV) symptoms is not measured in a standardized manner. Since therapeutic interventions focusing on improving BV symptoms are emerging (e.g. the vestibular implant, balance belt and noisy galvanic stimulation), the need for a new standardized assessment tool that embraces all aspects of BV arises. Therefore, the aim of this study was to develop a multi-item Patient Reported Outcome Measure, that captures all clinically important symptoms of BV and assesses its impact on daily life.
Methods: The development of the Bilateral Vestibulopathy Questionnaire (BVQ) consisted of two phases: (I) initial item generation and (II) face and content validity testing using cognitive interviews to gain insight in patients’ perspectives and an international expert meeting to obtain input from BV experts. Items were derived from a previous literature review and individual semi-structured interviews focusing on the full spectrum of reported BV symptoms (I). Subsequently (IIa), individual patient interviews were conducted using thinking aloud and concurrent verbal probing techniques to assess the comprehensibility of the instructions, questions and response options, and the relevance, missing domains or missing items. Finally, international experts with extensive experience in the field of the physical, emotional and cognitive symptoms of BV were invited to participate in an online focus group to assess the relevance and comprehensiveness of the BVQ (IIb).
Results: The BVQ that was developed consisted of two sections. The first section included seven constructs with a total of 50 items scored on a six-point Likert scale: three constructs regarding physical symptoms (imbalance, oscillopsia and other physical symptoms), one construct encompassing cognitive symptoms, one construct encompassing emotional symptoms, one construct comprising limitations and behavioral changes and one construct regarding social life. The second part consisted of four items, each scored on a visual analog scale from zero to 100, to inquire about limitations in daily life, perceived health and expectations regarding future recovery. Interviews with BV patients (n=8, 50% female, mean age 56 years (range 24-88 years)) and the expert meeting confirmed face and content validity of the developed BVQ.
Conclusion: The BVQ, which was developed to assess the full spectrum of BV symptoms and its impact on daily life, proved to have good face and content validity. It can be used to characterize the current self-reported symptoms and disability and to depict symptom burden before and after therapeutic interventions such as vestibular implant therapy.
FP0916Case report: Paroxysmal positional vertigo - not always benign
Maritta Spiegelberg, Alexander Tarnutzer
Neurology Department, Cantonal Hospital Baden, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: BPPV is the most common cause of positional vertigo. However, in a small fraction of cases, central and potentially life-threatening underlying diseases may mimic the clinical presentation of BPPV. Thus persistent paroxysmal positional nystagmus not responding to repositioning maneuvers for BPPV should result in a careful search for additional neurological symptoms and investigations.
Objective: The case report presented here should promote awareness that persistent positional vertigo and nystagmus not responding to repositioning maneuvers and / or with associated neurological symptoms require further diagnostic testing including neuro-imaging in every doubtful case to rule out intracranial pathologies.
Case report: A 45-year old man complained about a sudden onset of episodic positional spinning vertigo with nausea / vomiting when lying down on the left and right side since two weeks and a gait disorder. Right supine roll 90° maneuver revealed a discreet horizontal apogeotropic persistent nystagmus and vertigo, left supine roll maneuver provoked a moderate horizontal apogeotropic nystagmus and severe vertigo. After otokonia mobilisation by vibration, a 360°-barbecue repositioning maneuver was performed leading to an improvement of symptoms. A diagnosis of cupulolithiasis of the right horizontal semicircular canal was made. During the control the next day, however, the patient again presented with a horizontal apogeotropic persistent nystagmus and vertigo. Hence a brain-MRI scan was scheduled due to newly arising complaints of pharmacoresistent nausea and vomiting and worsening gait disorder. The brain MRI scan revealed multiple intracranial, mainly cystic lesions with compression of the fourth ventricle, the brainstem and the left cerebellar hemisphere. Neurosurgical resection of the cerebellar mass revealed a diagnosis of cerebral metastases of an until then undiagnosed adenocarcinoma of the lung.
Conclusion: Central causes must be suspected when progressive, therapy-resistant paroxysmal positional nystagmus and vertigo in combination with other neurological deficits occur or if nystagmus pattern are atypical during provocation maneuvers. In 12 – 20 % of cases an underlying central pathology is identified, including cerebellar tumors, internal auditory canal masses, cerebello-pontine angle tumors, obstructive hydrocephalus, lipoma, glioma and meningioma. Furthermore BPPV and additional intracranial tumors may coexist.
FP0917Functional head impulse test in PPPD subjects without and with Optokinetic Stimulation
Cangiano Jacopo, Gatti Omar, Bussi Mario
San Raffaele Scientific Institute
Persistent Postural Perceptual Dizziness (PPPD) is a functional chronic clinical condition characterized by unsteadiness present on most days for a period of at least 3 months. Either a vestibular disorder or a psychological distress may lead to the disorder. Visual stimuli are commonly reported among exacerbating conditions. In our cross sectional prospective study we studied vestibular function in 25 PPPD subjects through a video-HIT, a bedside examination (including skull vibration test, head shaking and positional tests) and a functional-HIT. The latter is based on having the patient identify an optotype displayed on a computer screen for a short time during passive head rotations; results are expressed in percentage of recognized optotypes. The test was repeated while an optokinetic stimulation (OKS) was given on the screen. Results of the functional-HIT without and with OKS have been compared with those of 25 healthy subjects. Moreover, patients were asked to perform a STAI questionnaire and anxiety levels before and after OKS test were assessed with a VAS scale. Video-HIT and f-HIT without OKS showed normal values in all subjects. F-HIT with OKS provoked more reading errors in patients than in controls. The interaction of group per time detected a different trend of decrease between the two groups (p=0.0002). Patients presented increased anxiety levels before testing, which was reduced after the exam. Among PPPD subjects nine fulfilled criteria for definite vestibular migraine and 8 of them presented nystagmus in at least one of the tests during bedside examination. Only anxiety before OKS test was predictive of worsening of f-HIT results (p=0.0007). Different possibilities have been considered to explain results. Increased anxiety levels may play a role in visuo-vestibular interactions; moreover our data are not inconsistent with the possibility that these subjects present a “hypersensitive” visual alarm system, and OKS might provoke a “threatening effect”, leading to a gaze bias during examination
FP0919Primary Large B-cell Lymphoma of the Central Nervous System presenting as a Vestibular Syndrome
Pedro Valente, Cristina Aguiar, Eugénia Castro, Artur Condé, João Larangeiro
Otolaryngology Department of Centro Hospitalar de Vila Nova de Gaia/Espinho
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Dizziness and vertigo are frequent complaints in patients seeking care in emergency departments. Although they are typically considered to have a peripheral cause, the underlying pathology can be serious, and misdiagnosis may have a significant impact on treatment, quality of life and patient outcome. The authors present a case of a patient diagnosed with Primary Diffuse Large B-Cell Lymphoma (DLBCL) of the Central Nervous System (CNS) and review the literature regarding the presentation, diagnosis, treatment and prognosis of this entity.
Case Presentation: A 74-year-old woman presented to the ENT emergency department due to dizziness complaints during the previous two months, associated with intense nausea/vomiting. She described frequent episodes of instability, with non-spinning quality, triggered by head movements, which worsened progressively, leading to significant weight loss and generalized asthenia. The patient denied focal neurologic deficit or other cochleovestibular complaints, fever, chills, or night sweats.
On admission, vital signs were stable. The otoneurological examination showed direction-changing, bilateral horizontal gaze-evoked nystagmus, with an upbeat vertical component during upward-gaze, negative head impulse test and absence of skew deviation. Non-contrast head computed tomography (CT) demonstrated no visible masses or hemorrhage. Brain magnetic resonance imaging (MRI) revealed a homogeneous T2 hyperintense, gadolinium-enhancing lesion involving the fourth ventricle, brainstem, cerebellar peduncles and hemispheres (Figure 1). Cerebrospinal fluid analysis was normal and flow cytometry was negative for malignancy. The patient underwent a posterior fossa craniotomy with stereotactic biopsy of the lesion. Histopathological analysis showed large neoplastic lymphoid cells and immunohistochemical staining was consistent with the diagnosis of DLBCL.
Figure 1:
CNS Primary DLBCL on MRI.
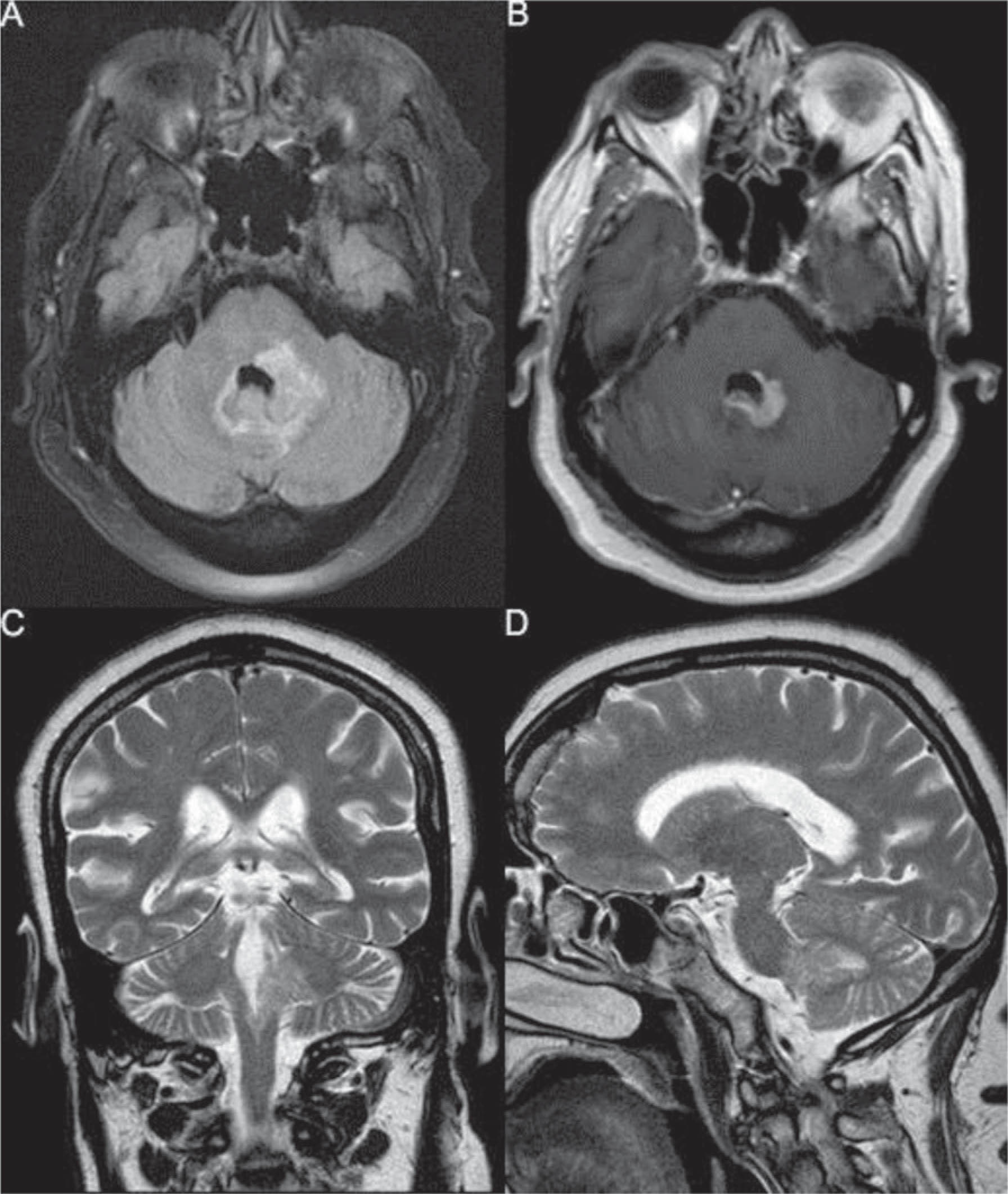
The patient was considered unfit for systemic intensive chemotherapy and started on palliative treatment with dexamethasone and procarbazine. She deceased due to a respiratory infection two months later.
Discussion and Conclusion: Primary DLBCL of the CNS is a rare, malignant non-Hodgkin lymphoma (NHL), estimated to account for less than 1% of all NHLs. Although typically associated with immunocompromised patients; its incidence among the immunocompetent elderly population is increasing.
Tumor location determines the clinical presentation, most frequently with non-specific focal neurological or neuropsychiatric symptoms. Isolated vestibular complaints have been seldomly reported as the initial manifestation. The histopathological examination with adequate immunohistochemistry testing is the diagnostic gold standard. Primary DLBCL of the CNS is an aggressive tumor with high rates of recurrence after treatment. The combination of chemotherapy and radiotherapy is the standard treatment and have consistently improved survival, despite the overall poor prognosis.
FP0920Clinically Isolated Syndrome presenting with Vertigo, Hearing Loss and normal HINTS examination
Pedro Valente, Isabel Pinto, Eugénia Castro, Artur Condé, João Larangeiro
Otolaryngology Department of Centro Hospitalar de Vila Nova de Gaia/Espinho
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Acute vestibular syndrome (AVS) presents as a spontaneous episode of severe vertigo, with sudden onset and prolonged duration. Causes of AVS most often include vestibular neuritis and stroke, although demyelinating diseases may also mimic vestibular neuritis and are estimated to account for 4% of all AVS episodes.
Case Presentation: A 17-year-old female teenager presented to the ENT emergency department due to complaints of spontaneous, persistent vertigo and right-sided hearing loss in the previous seven days, associated with nausea and vomiting. The otoneurological examination showed unidirectional left-beating horizontal-torsional nystagmus, grade 3 (all gaze positions), pathological head impulse test to the right side and absence of skew deviation. Pure-tone audiometry confirmed a right-sided moderate high-frequency sensorineural hearing loss (Figure 1A) and a video head impulse test (vHIT) revealed a slightly reduced vestibulo-ocular reflex (VOR) gain (0.77) in the right horizontal canal (Figure 2A). The patient was admitted due to a presumed acute labyrinthitis and started treatment with corticosteroids and anti-emetic medication. Improvement on dizziness and hearing impairment was remarkable with complete recovery of normal hearing levels within just four days of treatment (Figure 1B) and normalized horizontal canal VOR gain (Figure 2B). A brain magnetic resonance imaging (MRI) was performed, revealing multiple lesions including in the right middle cerebellar peduncle and cerebellar hemisphere white matter, suggestive a demyelinating etiology (Figure 3). The patient was discharged and completed adequate study, which confirmed the diagnosis of Multiple Sclerosis.
Figure 1:
Right-ear pure tone audiograms. A – Initial audiogram; B – Post-treatment audiogram showing complete recovery of normal hearing levels.
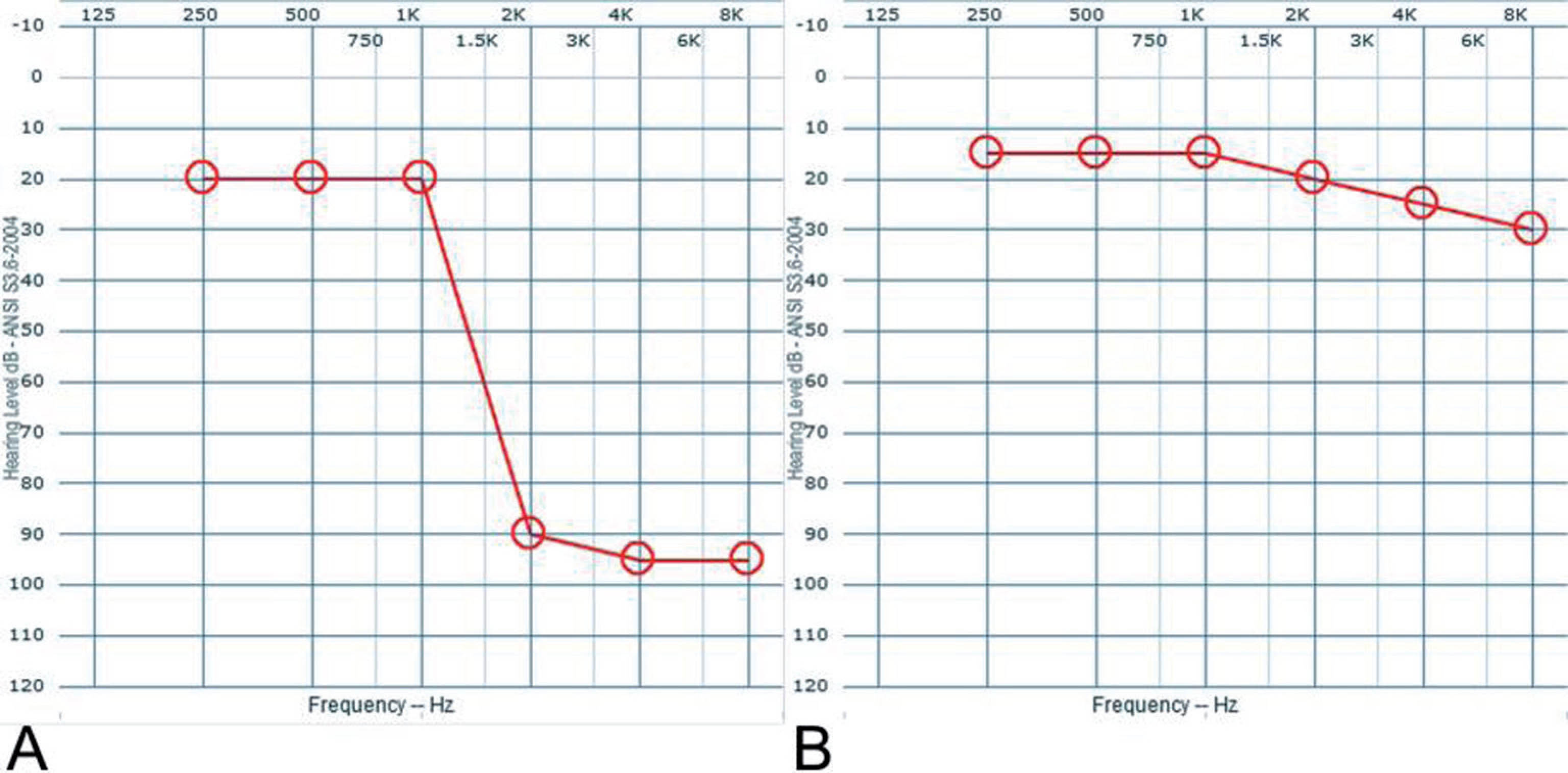
Figure 2:
Lateral canal (LC) video head impulse test (vHIT) in both ears at the time of diagnosis. Blue and orange waves represent head velocity, green waves represent inverted eye velocity, and red waves represent saccades. A – Initial vHIT with reduced VOR gain (0.77) in the right LC. B – Follow-up vHIT assessment with normal VOR gain (1.07) in the right LC.
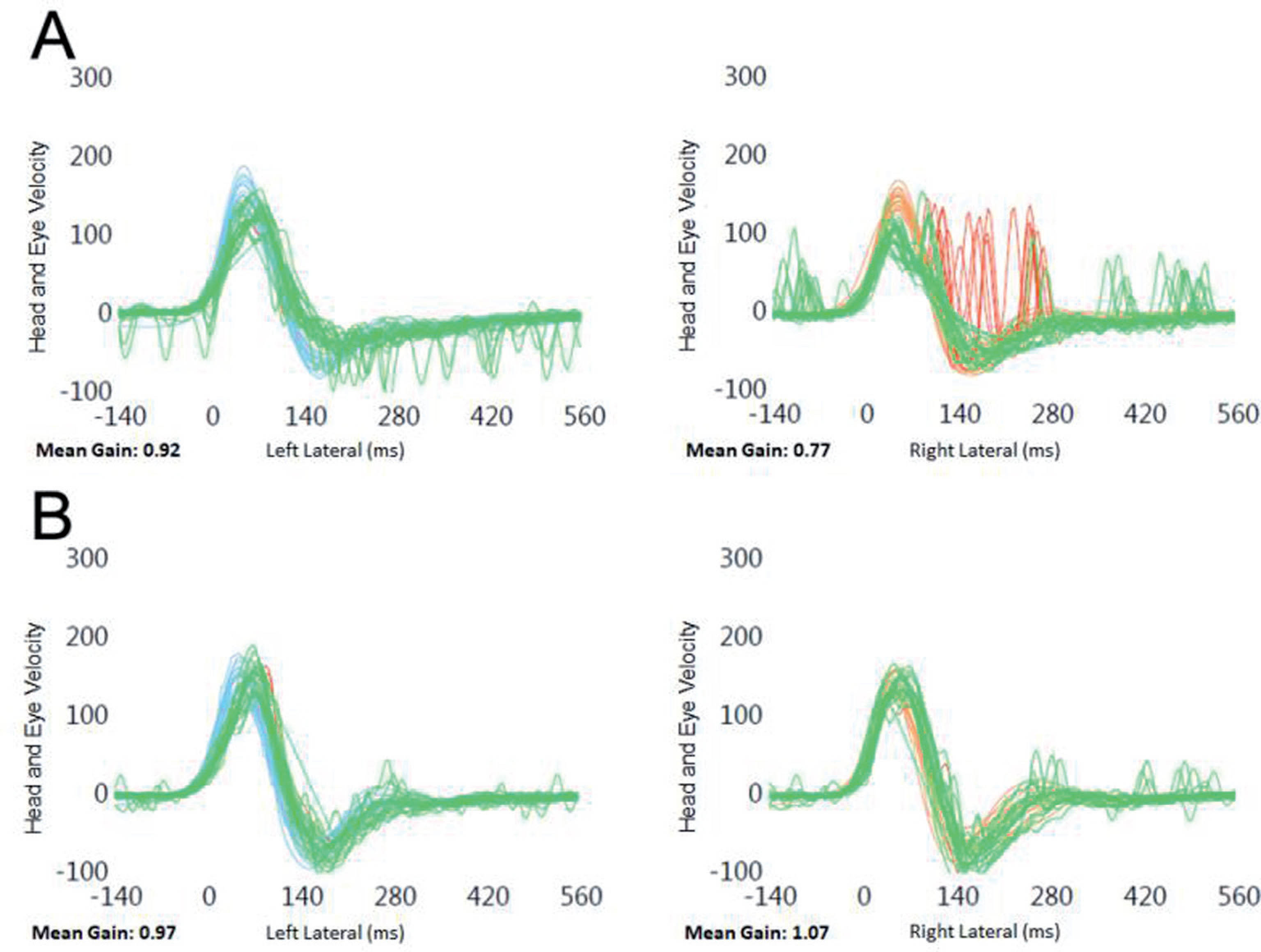
Figure 3:
Brain MRI revealed multiple high-intensity lesions in a typical demyelinating disease topography including the right middle cerebellar peduncle (A) and the cerebellar hemisphere white matter (B).
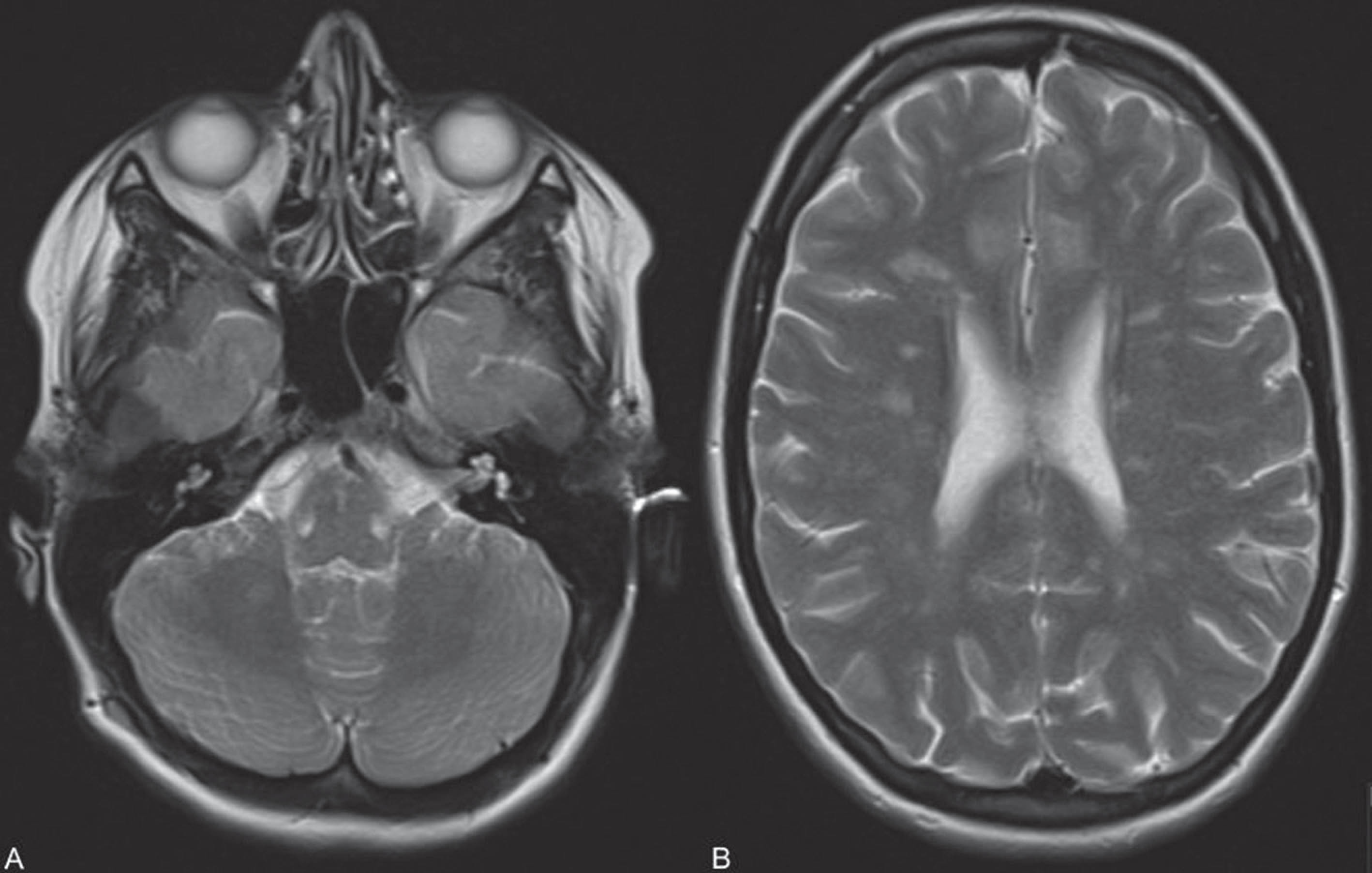
Discussion and Conclusion: Multiple sclerosis is the most common chronic inflammatory disease of the central nervous system (CNS) and, despite the continuous evolution in our understanding of this pathology, its underlying cause remains elusive and it is currently incurable. Patients with MS commonly report dizziness and vertigo either as an initial manifestation or during the course the disease. On the other hand, hearing impairment, specifically sudden sensorineural hearing loss (SSNHL), is rarely found in an initial presentation of MS. In the reported case, the initial bedside testing was suggestive of a peripheral vestibular cause, according to the HINTS paradigm and vHIT testing. The presence of SSNHL raised the suspicion of CNS disease and prompted imaging evaluation, which allowed the final diagnosis of MS. This case highlights the importance of an accurate diagnosis in patients presenting with an acute vestibular syndrome, keeping in mind the uncommon central causes, namely multiple sclerosis, where the timely initiation of appropriate disease-modifying therapies has been shown to be clinically effective.
FP0923Analysis of heel stepping motion using nine-axis motion sensor.
Toru Miwa
Department of Otolaryngology-Head and Neck Surgery, Graduate School of Medicine, Kyoto University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
A motion sensor is an electronic device that is designed to detect and measure movement. Motion sensors are used primarily in home and business security systems, but they can also be found in phones, paper towel dispensers, game consoles, and virtual reality systems. This technology will be utilized to improve the body balance in the future. We collected heel step test data on the force plate (Foulage test) for 6 healthy adults (all men aged 27.32±5.89) using an accelerometric device, nine-axis motion sensor. The subjects were demonstrated Foulage test with nine-axis motion sensor in their lumbar spine, and data were analyzed and examined correlations. Root mean square (RMS), auto-correlation coefficient (AC) and Euler horn were calculated from nine-axis motion sensor. Moving distance (FT value) and rotation angle (θ value) were calculated from Foulage test. There were significant correlations between AC x-axis of linear/ angular acceleration and FT value. There were also significant correlations between Euler horn y-axis and θ value. Our results suggested x-axis of lumbar spine affected Foulage stepping. This accelerometric device is easy to use and requires no specialized equipment and could be used to analyze Foulage test in clinical practice. We will show the results of relationship between Foulage test and motion sensor of head and neck spine during the conference.
FP0927Does the tuning property shift in cVEMP reflect endolymphatic hydrops revealed by MRI study?
Toshihisa Murofushi, Masahito Tsubota, Koji Nishimura
Teikyo University School of Medicine Mizonokuchi Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Meniere’s disease (MD) is one of the representative peripheral vestibular diseases, characterized by episodic vertigo attacks accompanied by fluctuated auditory symptoms/signs. As endolymphatic hydrops (EH) is one of the histopathological features of MD, detection of EH using clinical neurophyiological tests such as cervical vestibular evoked myogenic potential (cVEMP), electrocochleography (ECoG) and so on have been performed. Nowadays MRI has been applied for detection of EH. However, correspondence of neurophysiological test results to MRI findings is not fully investigated.
Objective: In this study we tried to examine correspondence of cVEMP tuning property test results to MRI findings.
Subjects and Methods: Patients diagnosed with having MD or MD related vestibular diseases were enrolled. These patients underwent cVEMP tuning property test and MRI for assessment of EH. For cVEMP tuning property test, cVEMPs were measured using 500Hz and 1000Hz short tone bursts (STB)(air-conducted, 125dBSPL). As an index of EH, 500-1000 Hz cVEMP slope (=SLOPE) was calculated. Here, SLOPE = 100x(A500-A1000)/(A500+A1000). A500: normalized amplitude of p13-n23 to 500Hz STB, A1000: normalized amplitude of p13-n23 to 1000Hz STB. According to the previous studies, SLOPE< -19.9 was regarded as EH positive. Inner ear scans using 3T-MRI was taken 4 hours after gadolinium intravenous injection. For assessment of EH in MRI, we used grading by Nakashima T et al. (Acta Otolaryngol 2009;129:5-8) and regarded “Significant” in this grading as EH positive.
Results: Statistically significant association was shown between cVEMP slope findings and MRI findings (chi-square test, p<0.01).
Conclusion: EH positive and EH negative in cVEMP tuning property test correspond to MRI findings of EH.
FP0928PPPD patients show lack of habituation to repetitive stimuli? Study in auditory middle latency response (AMLR)
Toshihisa Murofushi, Fumiyuki Goto
Teikyo University School of Medicine Mizonokuchi Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: We have reported that vestibular miraine (VM) patients show lack of habituation to repetitive stimuli in auditory middle latency responses (AMLR). This phenomenon is considered to be caused by sensory processing disorders in the central nervous system. Habituation diorders in other chronic vestibular disease remain unclear.
Objective: To clarify whether PPPD (persistent perceptual postural dizziness) patients show lack of habituation to repetitives stimuli using auditory middle latency response (AMLR).
Subjects and Methods: Patients diagnosed with having PPPD were enrolled. Also, patients with vestibular migraine (VM), Meniere’s disease (MD) and healthy subjects (HC) were enrolled for comparison. These subjects underwent AMLR tests. The electrodes were placed on the vertex and the spinal process of the fifth cervical vertebra. Binaural click stimulation (0.1 msec, 70dBnHL) was presented. Totally 800 responses were averaged. Averaged responses were divided into 4 sets (S1 to S4) according to the temporal order. No, Po, Na, and Pa were identified, and amplitudes and latencies were measured. Because Na-Pa amplitudes showed significant difference amogb VM, MD, and HC in the previous study (Murofushi T et al. 2020), we mainly studied Na-Pa amplitude.
Results: While relative amplitude of Na-Pa in S4 to S1 showed decreasing in MD patients and HC (habituation), VM patients and PPPD patients showed lack of habituation. Although difference between VM patients and PPPD patients was not significant, VM patients showed tendency of clearer potentiaton than PPPD patients.
Conclusion: Habituation disorders to repetitive sensory stimuli might be a part of sensory processing disorders in PPPD patients, leading to prolongation of their symptoms.
FP0929Acute Unilateral Vestibular Hypofunction, Is It Vestibular Neuronitis... Or not?
R Andrés Navarro-Mediano, Estefanía Hernández-García, Mar Martínez and Guillermo Plaza
Hospital Universitario de Fuenlabrada
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Vertigo in an emergency room context is challenging and may involve different pathologies which converge in the same symptoms. This poster shows the case of a 58 years old woman who came to our hospital referring 1 week of continuous vertigo, inestability and nausea. She had no other symptoms. She presented a grade 1 left nystagmus and the v-HIT showed unilateral right hypofunction and overt and covert saccades. She was diagnosed of right vestibular neuronitis and started ambulatory treatment. She returned after 10 days with the same symptoms and underwent a CT brain scan that was informed as not presenting relevant findings. Three weeks later she returned with persistent vertigo and inestability and right facial palsy with peripheral characteristics. She underwent another CT scan which then showed right temporal subcortical hypodensity, and a MRI thereafter revealed multiple bilateral T2-hyperintense periventricular and deep supratentorial lesions at the union between the medium right cerebellar peduncule and the posterior bulbopontine region suggesting demyelinating disease or subacute encefalitis. She was treated with antivirals, ampicillin and steroids, and the serologies and the cerebrospinal fluid findings were negative which left the diagnose to demyelinating disease. After a month she was revaluated and she had no longer vertigo or facial palsy but she kept complaining of instability. Then, v-HIT improved showing bilateral normofunction with no saccades. She is still being studied by neurology up to date with no definite diagnose. This clinical case shows that acute vestibular syndromes, even when having compatible exploration and v-HIT can surprise us and we must stay alert of other possibilities.
FP0935Vestibular compensation and perceived disability in a population of vestibular neuritis
Jonathan Esteban-Sanchez1, Almudena Rueda-Marcos2, Eduardo Martin-Sanz1
1Otoneurology Unit. University Hospital of Getafe; 2Neurology Unit. University Hospital of Getafe
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Vestibular neuritis (VN) is the most common cause of acute spontaneous vertigo.
An individual’s progress or lack of progress in vestibular restoration is usually measured by observing changes in vhit gain values, some patterns of saccades, motion intolerance, balance, functional abilities and more recently, health-related quality of life
Objetives: In this study we used CDP, SF36, AVS, DHI to evaluate the unsteadiness and quality of life status in patients with VN. To evaluate vestibular impairment and recovery/compensation mechanisms.
Material and Methods: A prospective, longitudinal study was conduced in the ENT Department between January 2018 and December 2019. There was 38 consecutive patients diagnosed with vestibular neuritis. All patients were monitored for 12 months
All patients underwent a complete physical examination and currently available conventional diagnostic test (bed-side vestibular examination, videonystagmography, VHIT, caloric test, cervical and ocular VEMP and computerized dynamic posturography (CDP).
All patients were submitted to customize a SF36 health survey questionnaire, an AVS and the DHI for assessing the disability.
Results: Demographic and clinical data were comparable between men and women.
Successive vHIT results showed a significantly vestibulo-ocular reflex gain recovery in vestibular neuritis patients. There is a reduction in percentaje of saccades with decrease in the latency, velocity, and organization of the compensatory saccades was observed.
This study shows statistically significant association between the VHIT test and SOT and limits of stability results of CDP.
There was a statistical significant difference for each parameter of DHI score (the emotional, functional and physical) between all visits. There is also statistical significant difference for almost all dimensions evaluated by SF-36 test between all visits. AVS showed similar results with great correlation with gain values of vHIT.
Conclusions: Vestibular neuritis is caused by an unilateral vestibular function, which is restored over time.
In addition to the recovery of the vestibulo-ocular reflex, the reduction of latency, velocity and the organization of compensatory saccades play a role in vestibular compensation.
Questionnaires such as DHI, SF-36 or AVS are useful tools to quantify the disability perceived by the patients. These questionnaires improve their values with great correlation with vHIT and CDP.
FP0938Postural instability in Parkinson disease and the association with the vestibulospinal tracts involvement
Luciana Cristina Matos Cunha, Sarah Teixeira Camargos, Anna Paula Batista de Ávila Pires, Denise Utsch Gonçalves
Universidade Federal de Minas Gerais
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: postural instability in Parkinson’s disease (PD) is common, has an unknown pathophysiology and has been associated to cognitive impairment. Galvanic vestibular stimulation (GVS) applied to the mastoid bone triggers a motor response in the posture-controlling muscles. The consequent electromyographic response, which is the vestibular-evoked myogenic potential (VEMP), provides information about the central pathways of the vestibular system, including brainstem, reticulospinal tract and vestibulospinal tracts extending from the cervical to the lumbar spine. Objective: To evaluate the vestibulospinal reflex in PD and to correlate it with cognitive impairment. Methodology: In a transversal design, 60 individuals with PD, of whom 30 presented postural instability (mean age 63 + 54-70 years, 11 women) and 30 did not (56 + 50-63 years, 15 women) as well as 32 healthy controls (58 + 51-68 years, 21 women) were submitted to galvanic stimulation to evoke VEMP and the response was recorded from the soleus muscle (sVEMP). The GVS was characterized as a direct, monophasic, and rectangular current with an intensity of 2 mA and a duration of 400 ms applied as a transmastoid binaural stimulation. The postural instability was defined by a score equal to or greater than 1 in the pull test at the Unified Parkinson Disease Rating Scale (UPDRS) and the Berg Balance Scale (BBS). The cognitive evaluation consisted of a mini examination of the mental state, a clock drawing test, a figures memory test and verbal fluency. Cognitive variables were reduced by means of factorial analysis to only one component called global cognition. The sVEMP variables were the latency and the morphology of the waves. They were correlated with the global cognition, BBS, UPDRS II (functional evaluation) and UPDRS III (motor evaluation). Results: PD with postural instability presented the worst results in UPDRS III (p<0.001), BBS (p<0.001) and global cognition (p=0.005), as expected. The sVEMP variables were not different in the groups with and without instability (p>0.005), but these groups presented worse sVEMP latencies comparing to the controls. Global cognition was not correlated with alteration in sVEMP. Conclusion: The vestibulospinal reflex was found to be altered in the early stages of PD, which supports the theory that the vestibular system plays a role in, but not truly explain, the postural instability in PD. The association of bad cognition and postural instability seems to be multifactorial, since an alteration in the vestibulospinal reflex was found before any clinical symptom of cognitive alteration.
FP0940Vibration-Induced-Nystagmus Contribution to the Unilateral Superior Semicircular Canal Dehiscence Syndrome vs Otosclerosis Diagnosis
Armin De Luca; Vanesa Pérez Guillén; Lidia Torres García; Ana Belén Castilla Jiménez; Herminio Pérez Garrigues
Hospital Universitari y Politècnic La Fe
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: The Superior Semicircular Canal Dehiscence Syndrome (SSCDS) is an infrequent entity that can present itself with vestibular symptoms associated with loud noises or increases in the intracranial pressure, as well as, conductive hearing loss, aural fullness and tinnitus. It’s not uncommon for this syndrome to present itself only with audiological symptoms mimicking Otosclerosis (OS).
Even though the definitive diagnosis for both entities relies strongly on temporal bone computerized tomography (CT), the vibration-induced-nystagmus (VIN) test may be a useful initial in-office evaluation to discriminate SSCDS from OS.
Methods and Material:
Studied population:
- 6 patients with confirmed SSCDS using temporal bone CT in whom tonal audiometry, tympanometry, stapedial reflex, video head impulse test (vHIT) and VIN test were performed.
- 11 patients with confirmed OS using temporal bone CT in whom the same complementary tests as in the SSCDS group were performed.
The VIN test was performed by using a 100Hz stimulus on both mastoids and the ophryon (anterior central cranial point) using a Sinapsis VVIV stimulator.
Results: Four of the patients with SSCDS presented a unilateral low frequency conductive hearing loss and all of them had a normal tympanometry and stapedial reflex. The vHIT was also normal in the six patients. The temporal CT showed a SSCD in every patient (2 of them bilateral). Every patient that had a unilateral finding (radiologic and audiometric) had a positive VIN test while stimulating with 100HZ (x=9.76 DS 3,24 °/second) at the ophryon. The direction of the fast phase of said nystagmus, while stimulating a central cranial point, beat to the same side of the dehiscence. Patients with bilateral findings had a negative VIN test. Each one of the patients with OS had a conductive hearing loss associated with a negative stapedial reflex and radiologic findings suggestive of otospongiosis. The VIN test was also negative in the 11 patients.
Conclusion: The VIN test is an un-expensive, simple and well-tolerated tool that may be useful as a guide in those patients in which the clinical presentation is unspecific and suggestive of either SSCDS or OS. Nevertheless, a negative finding in a patient with bilateral SSCDS compels to continue to perform other complementary tests to better discriminate the diagnosis.
FP0942Parameters of Off-Vertical Axis Rotation in Unilateral andBilateral Vestibulopathy and Their Correlation with VestibularEvoked Myogenic Potentials
Goun Choe1, Shin Hye Kim2, Sang-Yeon Lee3, Ji-Soo Kim4 and Ja-Won Koo1
1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam 13620, Korea; 2Uijeongbu Eulji Medical Center, Department of Otorhinolaryngology-Head and Neck Surgery, Eulji University College of Medicine, Uijeongbu 11759, Korea; 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea; 4 Department of Neurology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam 13620, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Off-vertical axis rotation (OVAR) is a laboratory test to assess the otolith function. This study aimed to analyze the parameters of OVAR in patients with unilateral vestibular hypofunction (UVH) and bilateral vestibulopathy (BVP), and to correlate the parameters of OVAR with those of VEMPs. Ten healthy volunteers, 41 UVH, and 13 BVP patients performed OVAR. Bias component (BIC) and modulation component (MOC) of UVH and BVP patients were compared with those of healthy controls. BIC and MOC were correlated with amplitude and interaural difference (IAD) of cervical VEMP (cVEMP) and ocular VEMP (oVEMP). In UVH patients, the direction of BICs to affected side rotation were reversed and the absolute value of BICs were decreased when they were compared to healthy controls. In BVP patients, BICs were markedly attenuated. MOCs were not changed in UVH and BVP patients. There was no statistically significant correlation between VEMPs and OVAR.
FP0944VEMPlitude: Is It Worth It?
Harry Akram, Laura Freeman
University College London Hospitals
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
I describe and discuss results of a study on Ocular VEMP amplitudes, comparing conventional montage to a variation of the “Belly-Tendon” montage (as described by Sandhu, 2013 and Colebatch, 2013) showing, on average, amplitudes are twice as large with the “BT” method and at worst, exactly the same. Previous studies describe the risk of ocular mygonenic interference from non-test sites but we demonstrate that it is a very low risk. We discuss the advantages and disadvantages and also my motivations for exploring this in relation to public health and vestibular assessments. This will be of interest to diagnosticians, particularly Audiologists, Audiological Scientists and anyone conducting oVEMP on their clinic. Finally, I propose that my new montage is named after popular Rythm and Blues vocalist Missy Elliot.
FP0949Effect of Electric Vestibular Stimulation on Oculomotor Control During Head Movements in Healthy and Vestibular Lesions
Maja Striteska1,2, Jan Kremlacek3
1Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 2Department of Otorhinolaryngology, Charles University in Prague, 3rd Faculty of Medicine, University Hospital Kralovske Vinohrady, Czech Republic; 3Department of Medical Biophysics and Department of Pathological Physiology, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Study preliminary data:
Introduction: Transcranial electric vestibular stimulation (tEVS) plays an essential role in the quest to understand sensory signal processing in the vestibular (balance) system and in investigating future treatment options for patients with different vestibular lesions. The study arises from a need to understand the tEVS interaction with a concurrent vestibular signal from an intact side during natural head movements.
Methods: Different tEVS attributes such as the type of current modulation (waveform, pulses, etc.), timing of pulses, signal intensity (0.3 to 0.5 mA), etc., were explored during motionless condition and during active or passive head movements (rotations), using the current and shame signals in healthy volunteers first. The head movements were explored in the frequency range from 1 Hz (VOG) to approximately 5 Hz (VHIT). During the second phase patients with different one sided peripheral vestibular lesions will be enrolled and divided in subgroups according to their diagnosis. The same protocol from the first phase will be used. Statistical data will be evaluated.
Preliminary data: The VOG traces showed well detectable vestibular responses to tDCS. Opposite, the VHIT gains were not affected neither from any stimulation in healthy. We hypothesize, the current provides such a small vestibular excitation (in spontaneous nystagmus only 1-2 aSPV response, emphasized by a head shake to 3-4 aSPV), that this small change in a function is well-tolerated or hidden as a small error during such a strong vestibular impulse, as high head acceleration during a head impulse test. This could affect some other hypotheses. Especially, why in some vestibular disorders like vestibular schwannoma or Meniere’s disease, low frequencies (of head movement) of tested vestibuloocular reflex (as spontaneous nystagmus and head shake are), are affected first, while high frequencies are affected later. Maybe due to a tolerance of a signal error. Next hypothesis could be based on a different vestibular hair cells type I and II sensitivity to electrical stimulation, while type I hair cells are associated with large vestibular afferents with an irregular neural firing pattern, while type II are associated with small vestibular afferents that display a regular neural firing pattern (Baloh a Honrubia 2001), dimorphic units could be either regular or irregular units. Irregular nerve fibres are larger and have higher conduction velocities (Goldberg, Fernandez, 1977[1]), are more efficient at transmitting excitatory information and are more sensitive to transient motion (Fernandéz, Goldberg, 1976, Goldberg 2000 [2, 3]).
FP0950Head-shaking Test discriminates Growth and Stable Vestibular Schwannoma
Maja Striteska1,2, Martin Valis3, Martin Chovanec2, Oliver Profant2,4, Jan Kremlacek5
1Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 2Department of Otorhinolaryngology, Charles University in Prague, 3rd Faculty of Medicine, University Hospital Kralovske Vinohrady, Czech Republic; 3Department of Neurology, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 4Department of Auditory Neuroscience, Institute of Experimental Medicine of the Czech Academy of Sciences, Prague, Czech Republic; 5Biophysics and Department of Pathological Physiology, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Abstract
Objective: To assess the potential of the head-shaking test to discriminate between the stable and growing vestibular schwannoma.
Study Design: Prospective study, schwannoma patients and healthy controls were enrolled.
Setting: Outpatients of a tertiary referral center.
Methods: One-hundred twenty-eight subjects were enrolled in a study from September 2016 to August 2021. Two vestibular schwannoma groups (stable and growing group) and one control group of healthy volunteers were examined with a Videooculography test battery and Video Head Impulse Test.
Results: We analysed the potential of each test to discriminate between growing and stable vestibular schwannomas. The ROC analysis of spontaneous nystagmus showed 48% specificity and 96% sensitivity for the average slow phase velocity cut-off (aSPV) 0.5 o/s. The caloric test cut-off 41% unilateral weakness had 59% specificity and 100% sensitivity, video head impulse test gain cut-off 0.8 had 56% specificity and 96% sensitivity, head-shaking induced nystagmus cut-off 0. 5 o/s aSPV showed 96% specificity and 89% sensitivity.
Conclusions: Our study showed the potential of the head-shaking test to identify a growth activity of vestibular schwannoma.
FP0951Estimated Vestibulogram (EVEST) for Effective Vestibular Assessment
Maja Striteska1,2, Lukas Skoloudik1, Martin Valis3, Jan Mejzlik1, Katerina Trnkova2, Martin Chovanec2, Oliver Profant2,4, Viktor Chrobok1, Jan Kremlacek5
1Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 2Department of Otorhinolaryngology, Charles University in Prague, 3rd Faculty of Medicine, University Hospital Kralovske Vinohrady, Czech Republic; 3Department of Neurology, University Hospital Hradec Kralove, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic; 4Department of Auditory Neuroscience, Institute of Experimental Medicine of the Czech Academy of Sciences, Prague, Czech Republic; 5Department of Biophysics and Department of Pathological Physiology, Charles University, Faculty of Medicine in Hradec Kralove, Czech Republic
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Abstract
Background. The availability and development of methods testing the vestibuloocular reflex (VOR) brought a broader view into the lateral semicircular canal (L-SCC) function. However, the higher number of evaluated parameters makes more difficult the specialist’s diagnose-making process. Purpose. To provide medical specialists, a new diagnostic-graphic tool, Estimated Vestibulogram- EVEST, enabling a quick and easy-to-read visualization and comparison of the VOR test results within the L-SCC. Methods. The development of EVEST involved 148 participants, including 49 healthy volunteers (28 female and 21 male) and 99 (58 female and 41 male) patients affected by different degrees of peripheral vestibular deficit. The corresponding L-SCC VOR test results, from patients meeting the diagnostic criteria, were used to create the EVEST. Results. Based on the test results, we depicted and calculated the EVEST vestibular function asymmetry (VFA) in all the groups. To assess a feasibility of EVEST to describe a vestibular function deficit, we calculated sensitivity and specificity of VFA using a receiver operating characteristic curve (ROC) and compared it to single tests. In all the tests, we determined the cutoff value as the point with the highest sensitivity and specificity. For discrimination of any vestibular deficit, the VFA with cutoff 6.5% was more sensitive (91%) and specific (98%) than single tests. Results showed that EVEST is a beneficial graphic tool for quick multifrequency comparison and diagnosis of different types of the peripheral vestibular loss. Conclusions. EVEST can help to easily evaluate various types of peripheral vestibular lesion.
FP0954Impairment of the high-frequency vestibulo-ocular reflex for dehiscent semicircular canals: incomplete natural plugging or mechanical energy dissipation?
Andrea Castellucci1,2, Enrico Armato3, Cristina Brandolini2, Pasquale Malara4, Salvatore Martellucci5, Valeria Del Vecchio2,6, Angelo Ghidini1
1ENT Unit, Arcispedale Santa Maria Nuova, AUSL - IRCCS, Reggio Emilia, Italy; 2ENT and Audiology Unit, S.Orsola-Malpighi University Hospital, Bologna, Italy; 3ENT Unit, SS Giovanni e Paolo Hospital, ULSS Serenissima, Venice, Italy; 4Audiology & Vestibology Service, Centromedico, Bellinzona, Switzerland; 5ENT Unit, Santa Maria Goretti Hospital, AUSL Latina, Italy; 6UOC Audiology & Vestibology Unit, University Hospital Federico II, Naples, Italy.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
It is well known how superior canal dehiscence (SCD) results in audio-vestibular symptoms with low-frequency air-bone gap (ABG) and reduced thresholds for cervical- and ocular-VEMPs for air-conducted (AC) stimuli. Authors have demonstrated on animal models and humans how these data derive from the so-called “third-window effect”, where reduced impedance in the vestibular compartment results in dissipation of acoustic energy and enhanced otolith response to sounds. According to correlation studies, these phenomena seem to occur the wider is the dehiscence. Similarly, most subjects with wide-sized SCD present with impaired vestibulo-ocular reflex (VOR) on video-HIT for the affected superior canal (SC). It has been assumed that this finding might be due to a natural auto-plugging process exerted by middle fossa dura prolapsing through the dehiscence, as it overlaps postoperative VOR-gain measurements in surgically plugged patients who benefit from surgery. Accordingly, patients with wide-sized SCD presenting with SC-VOR hypofunction would be therefore expected to develop poor symptoms. Nevertheless, it is true only for few of them, whereas most patients continue to be symptomatic despite functional SC impairment. We hypothesize that, whereas wide-sized SCD may allow an incomplete canal plugging in some conditions, in most patients membranous SC continues to be patent allowing a dissipation of mechanical energy through the dehiscence. The aim of this paper is to provide further evidences for these assumptions. We compared instrumental data of 36 ears of 35 patients (17 males, 18 females, mean age 56.1 ± 13.6 years old) with SCD presenting with SC VOR-gain impairment (< 0.7) with post-operative data of 10 ears of 10 patients (mean age 51.4 ± 15.7 years old) with SCD who developed SC VOR-gain deficit after surgical canal plugging. All patients underwent audiometry, cervical- and ocular-VEMPs for AC/BC stimuli and video-HIT. Whereas no significant difference was found between the two groups in terms of mean VOR-gain for the affected SC (p > 0.05), mean ABG was significantly smaller (p < 0.01), both cervical- and ocular-VEMPs thresholds for AC stimuli were significantly higher and amplitudes significantly smaller (p < 0.01) in post-operative ears compared with non-surgical patients. In our opinion, these data suggest that the affected canal is patent in the majority of SCD-patients presenting with impaired SC VOR-gain and dissipation of mechanical energy through the dehiscence is more likely to occur than a spontaneous auto-plugging process, where ABG closure and VEMPs data normalization would be rather expected.
FP0955Feasibility of using Video Head Impulse Test to detect the involved canal in Benign Paroxysmal Positional Vertigo presenting with Positional Downbeat Nystagmus
Andrea Castellucci1, Pasquale Malara2, Salvatore Martellucci3, Enrico Armato4, Giacinto Asprella Libonati5
1ENT Unit, Arcispedale Santa Maria Nuova, AUSL - IRCCS, Reggio Emilia, Italy; 2Audiology & Vestibology Service, Centromedico, Bellinzona, Switzerland; 3ENT Unit, Santa Maria Goretti Hospital, AUSL Latina, Italy; 4ENT Unit, SS Giovanni e Paolo Hospital, ULSS Serenissima, Venice, Italy; 5Vestibology and ENT Unit, Giovanni Paolo II Hospital, Policoro, Matera, Italy.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Positional-downbeat nystagmus (pDBN) represents a relatively frequent finding in clinical practice. Though classically considered a sign of central disorders, thanks to recent advances in vestibular diagnostics and imaging, its primarily peripheral origin could have been ascertained. Nevertheless, distinguishing features of peripheral positional nystagmus, including latency, paroxysm and torsional components, may be missing, resulting in challenging differential diagnosis with central pDBN. Moreover, in case of benign paroxysmal positional vertigo (BPPV), detecting the affected canal may be challenging as the involvement of the non-ampullary arm of posterior canal (PC) results in the same oculomotor responses generated by contralateral anterior canal (AC)-canalolithiasis. Recent acquisitions suggest that patients with persistent pDBN due to vertical canal-BPPV may exhibit impaired vestibulo-ocular reflex (VOR) for the involved canal on video-head impulse test (vHIT). Since canal hypofunction normalizes following proper canalith repositioning procedures (CRP), an incomplete (or transient/positional) canalith jam acting as a “low-pass filter” for the affected ampullary receptor has been hypothesized. This study aims to determine the sensitivity of vHIT in detecting canal involvement in patients presenting with pDBN due to vertical canal-BPPV. We retrospectively reviewed the clinical records of 59 consecutive subjects presenting with peripheral pDBN. All patients were tested with video-Frenzel examination and vHIT at presentation and after resolution of symptoms or transformation in typical BPPV-variant. BPPV involving the non-ampullary tract of PC was diagnosed in 78%, AC-BPPV in 11.9% whereas in 6 cases the involved canal remained unidentified. Presenting VOR-gain values for the affected canal were greatly impaired in cases with persistent pDBN compared to subjects with paroxysmal/transitory nystagmus (p<0.001). VOR-gain values for the affected canal were even more impaired in patients (n.6) presenting with spontaneous DBN (p=0.002), consitent with a complete canalith jam within the PC. Each patient received CRP for BPPV involving the hypoactive canal or, in case of normal VOR-gain, the assumed affected canal. Each subject exhibiting VOR-gain reduction for the involved canal developed normalization of vHIT data after proper repositioning (p<0.001), proving a close relationship with otoliths altering high-frequency cupular responses. According to our results, overall vHIT sensitivity in detecting the affected SC was 72.9%, increasing up to 88.6% when considering only cases with persistent pDBN where an incomplete canal plug is more likely to occur. vHIT should be routinely used in patients with pDBN as it may enable to localize otoconia within the labyrinth, providing further insights to the pathophysiology of peripheral pDBN.
FP0957Overlapping Ménière’s Disease and Vestibular Migraine : Our Experience in Tertiary Referral Institution
Victoria Rivero de Jesús1, Laura Ruiz Sevilla1, Francesc Larrosa Diaz1, Rosana Rodriguez Villalba2, Manuel Bernal S1, Isabel Vilaseca1
1Hospital Clínic - Barcelona, Spain; 2Althaia Xarxa Universitaria de Manresa, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Ménière’s Disease (MD) and Vestibular Migraine (VM) are two clinical entities with overlapping signs and symptoms. The differential diagnosis is sometimes hard to perform when MD and VM are simultaneous, the diagnostic is really challenging.
Material and Methods: We analyze a series of 76 patients complying with Bárány’s Society diagnostic criteria for definite MD and/or Definite VM; 10 patients were excluded; we consider 66 patients (24 males, 52 females; age between 31 and 76) attended between 2018 and 2020. We divided them into 3 groups: definite MD group (uni and bilateral), definite VM group and MD + VM group. All patients were submitted to an accurate clinical history, physical examination, tonal audiometry, computerized vestibular testing and the Dizziness Handicap Inventory (DHI).
Results: According to Bárány’s Society diagnostic criteria, we find that 52 patients were definite MD, 11 were definite VM and 13 were overlapping VM / MD. Four patients of the simultaneous VM / MD group presented a positive familiar history for vertigo and/or migraine, 3 suffered a bilateral MD and 10 a unilateral MD .
Conclusion: In our experience, overlapping MD/ VM group is affected by more frequent crisis than definite MD group. DHI demonstrated a worse quality of life in MD + VM group. Females are more represented than males in all 3 groups; 4 patients of the MD/VM group had a positive family history for migraine or definite MD.
In our experience it is difficult to make a diagnostic of overlapping VM/MD. An accurate medical history can lead us to a better diagnostic and treatment.
FP0963Vestibular syncope : Recurrent syncope during the attacks of Meniere’s disease
Eunjin Kwon1, Ju-Young Lee2 Hyo-Jung Kim3, Jeong-Yoon Choi4, and Ji-Soo Kim4
1Deparment of Neurology, Chungnam National University Hospital, Daejeon, Korea; 2Department of Neurology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea; 3Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea; 4Research Administration Team; Seoul National University Bundang Hospital, Seongnam, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background & Significance : Vestibulosympathetic reflex is referred to as the relation between the sympathetic nervous system and the vestibular system. We herein the case, who had recurrent syncope that associated with vestibular stimulation. Case : A 79-year-old woman with Meniere’s disease was referred to the clinic to evaluate for recurrent syncope for 12 years. She felt vertigo with tinnitus and hearing difficulty in the left ear. As her symptom got progressed, she had diagnosed with Meniere’s disease 5 years ago. The patient got syncope attack when she felt vertigo, had a loss of consciousness about 2 hours. As she fell, she got a traumatic temporal bone fracture and a small amount of subarachnoid hemorrhage in the bilateral temporal lobes. After the event, she had experienced similar events 4 times within 2 weeks after the discharge. Cardiologic and neurologic syncope evaluation was done and all excluded. In her interictal stage, vestibular function tests were done. As she was diagnosed with Meniere’s disease, the syncope associated with Meniere’s attack was suspected. Thiazide and betahistine for the prevention of syncope were applied and she has gotten free from syncope for 2-year-follow-up. Conclusions : Tumarkin’s otolithic crisis or drop vestibular attack is the main sign of Meniere’s disease, which is syncope with vestibular symptoms. However, the mechanism of the syncope and vestibular dysfunction is not clear yet. There were some studies about sympathetic and cardiovascular activity along with vestibular activity variation both in human and animal. We suggest the mechanism of drop attack as a vestibulosympathetic reflex failure with vestibular pathway impairment.
FP0968The Proteome of the Human Endolymphatic Sac Endolymph
Christine Ölander1, Jesper Edvardsson Rasmussen1, Per Olof Eriksson1, Göran Laurell1, Helge Rask-Andersen1, Jonas Bergquist2
1Department of Surgical Sciences, Otorhinolaryngology and Head and Neck Surgery, Uppsala University, Uppsala, Sweden; 2Department of Chemistry – BMC, Analytical Chemistry, Uppsala University, Uppsala, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Advancements in mass spectrometry for the analysis of proteins have greatly improved protein identification. Sampling of endolymph from the endolymphatic sac is difficult because of its small volume and anatomical location, with a high risk of contamination with surrounding tissue fluids and blood. For successful sampling refined techniques are required.
With a tailored solid phase micro-extraction probe we were able to collect five endolymphatic sac endolymph samples and six endolymphatic sac tissue biopsies in patients undergoing trans-labyrinthine surgery for sporadic vestibular schwannoma. After preparation, the samples were analysed with nano-liquid chromatography - tandem mass spectrometry (nLC-MS/MS). The data were analysed with MaxQuant software to identify the total number of proteins. Pathway identification regarding molecular function and protein class was analysed using PANTHER classification system.
In total, 1656 proteins were found. 1211 different proteins were found in the endolymphatic sac endolymph samples and 1546 in the endolymphatic sac tissue biopsies. 1101 of the proteins overlapped, thus the proteins were found in both the endolymph samples and the sac biopsies. 110 of the proteins were unique for the endolymphatic sac endolymph samples as compared to 445 proteins unique for the endolymphatic sac biopsies.
To our knowledge, this mapping of the proteome of the human endolymphatic sac is unique and may form a platform for further investigations to better understand the function of this intriguing tissue in the human inner ear.
FP0970The Suitability of the CAVA Device as an Ambulatory Monitor for Detecting Dizziness
John Phillips1, Jacob Newman2, Stephen Cox2
1Ear, Nose and Throat Dept., Norfolk and Norwich University Hospital, Norwich, UK; 2School of Computing Sciences, University of East Anglia, Norwich, UK.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Diagnosis of the dizzy patient is challenging due to its episodic nature, its many possible causes and ambiguity in patient reporting of symptoms. To overcome these limitations, we have developed the CAVA system. The system comprises a medical device that is worn on the face and which continuously records eye and head movement data, and associated computer software for analysing the data collected. The device is intended to be worn by patients in the community for up to thirty days, is designed to be easy to use by non-experts, to be comfortable and unobtrusive to wear, and to require minimal user and expert intervention. In 2018, we undertook a clinical investigation to evaluate the suitability of the CAVA system in these areas. Seventeen healthy participants wore the device for up to thirty days. Six withdrew prematurely because of a minor skin issue related to the specific electrode pad used with the device, which has since been rectified. Ten participants completed the full trial and answered a questionnaire designed to evaluate their experiences. Their answers revealed that all participants found the device easy to apply and remove by themselves, and found it comfortable and unobtrusive to normal daily activities. A majority found it easy to sleep while wearing the device, and adapted to the presence of the device on their face. Furthermore, the CAVA system was shown to be capable of identifying short periods of induced nystagmus with a high degree of accuracy. In conclusion, the CAVA device functioned well as an ambulatory monitor, with a high level of participant compliance resulting from a number of intentional design features of the device. This work will be of general interest due to the novelty of the device we have developed, but it will also be of specific interest to those interested in balance, dizziness and eye movements.
FP0971Using the CAVA Device to Assess Patients with Meniere’s Disease
John Phillips1, Jacob Newman2, Stephen Cox2
1Ear, Nose and Throat Dept., Norfolk and Norwich University Hospital, Norwich, UK; 2School of Computing Sciences, University of East Anglia, Norwich, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Until recently, it was impossible to objectively assess a patient’s reports of dizziness without physically observing them during an attack. The CAVA system has made it possible to record the physiological parameters necessary to retrospectively assess patients that report dizziness. This is achieved by way of a medical device worn on the face that simultaneously records head and eye movements. The data captured provides a novel and interesting insight into the disparities between the symptoms reported by patients and the objective signs recorded by the device. During an ongoing clinical investigation of the CAVA system involving patients suffering from dizziness, we recruited three patients who had previously been diagnosed with unilateral Meniere’s disease. All three patients reported rotatory vertigo lasting for hours at a time, severe nausea and plugging in the affected ear. Each patient wore the CAVA device for twenty-three hours a day, for thirty days, and all three reported at least one episode of vertigo during their trial period. Data captured by the CAVA device revealed that only one of the patients had experienced a typical, acute Meniere’s attack, easily identifiable in the data as episodic nystagmus, changing direction over the course of three-hours. One patient experienced short bursts of nystagmus which appeared to be motion-provoked, and the data from the final patient did not reveal any evidence of nystagmus. These results show that the objective signs observed from dizzy patients can be vastly different, despite similar reports of symptoms, and despite similar histories and diagnoses. These findings suggest that an objective measure of a patient’s signs, such as that offered by CAVA, is necessary to correctly assess patients with Meniere’s disease and could significantly change the way in which such patients are managed. For example, it could identify potentially incorrect diagnoses, suggest an alternative diagnosis, or guide the most appropriate treatment options for the patient. These findings will be of interest to those interested in balance, dizziness and eye movements, and specifically to those interested in Meniere’s disease.
FP0975Identification of Stroke and TIA in Patients with Acute Dizziness, Vertigo or Imbalance in Emergency Departments of Primary Care Hospitals: Early Experiences with a Network-based Telemedical Approach
Peter Müller-Barna1, Christina Leinweber1, Julia Pfaffenrath1, Nina Schütt-Becker1, Rascha von Martial1, Susanne Greck1, Nikolai Hubert1, Holger Rambold2,3,4, Roman Haberl1, Gordian Hubert1
1TEMPiS telestroke center, Department of Neurology, München Klinik, Academic Teaching hospital of the Ludwig-Maximilians-University, Munich, Germany; 2InnKlinikum Altötting, Department of Neurology, Altötting, Germany; 3Department of Neurology, University of Regensburg, Regensburg, Germany; 4MVZ Kliniken Mühldorf, Mühldorf am Inn, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Acute dizziness, vertigo and imbalance are frequent and difficult to interpret symptoms in the emergency department (ED). Primary care hospitals often lack the expertise to identify stroke or TIA as underlying causes. A telemedical approach based on telestroke networks may offer adequate diagnostics and treatment.
Aim: Aim of this study is to evaluate the accuracy of a novel ED algorithm in differentiating between peripheral and central vestibular causes.
Methods: Within the Telemedical Project for Integrative Stroke Care (TEMPiS) a telemedical application including a videooculography (VOG) system was introduced in 2018 in 19 primary care spoke hospitals. An ED triage algorithm was established for all patients with acute dizziness, vertigo or imbalance of unknown cause (ADVIUC) as a leading complaint. In three predefined months all ADVIUC cases were prospectively registered and discharge letters analyzed. Accuracy of the ED triage algorithm in differentiation between central and peripheral vestibular cases was analyzed by comparison of ED diagnoses to final discharge diagnoses. The rate of missed strokes was calculated in relation to all cases with a suitable brain imaging. Acceptance of teleconsultants and physicians in spoke hospitals was assessed by surveys.
Results: A total number of 388 ADVIUC cases were collected, with a median of 12 cases per months and hospital (IQR 8-14,5). The most frequent hospital discharge diagnoses are vestibular neuritis (22%), stroke/TIA (18%), benign paroxysmal positioning vertigo (18%) and dizziness due to internal medicine causes (15%). Detection of a central vestibular cause by the ED triage algorithm has a high sensitivity (98.6%), albeit poor specificity (45.9%). One stroke out of 32 verified by brain scan was missed (3.1%). User satisfaction, helpfulness of the project, improvement of care, personal competence and satisfaction about handling of the VOG systems were rated consistently positive.
Discussion: The concept shows good acceptance for a telemedical and network-based approach to manage ADVIUC cases in the ED of primary care hospitals. Identification of stroke cases is accurate, while specificity needs further improvement. The concept could be a major step toward a broadly available state of the art diagnostics and therapy for patients with ADVIUC in primary care hospitals.
FP0976The Use of a Gaze Stability Test with Exertion to measure physiological recovery of the vestibular-ocular reflex: a case series
Amy Alexander1, Shelly Massingale1, Nicholas Hattrup2, Jamie Pardini1
1Banner Sports Medicine and Concussion Specialty Clinic; 2Boston University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Following concussion, a graded exercise test can be utilized to measure the autonomic recovery of patients through heart rate, blood pressure, and self-perceived fatigue levels. The gaze stability test (GST) has been observed to decline in individuals following concussion. In addition, the GST acts as a measure of the vestibular-ocular reflex during faster movements, like those occurring during sport activities, and the vestibular-ocular reflex (VOR) has been shown to be unaffected by aerobic activity. With prior studies demonstrating that higher GST values are observed in an athlete population, observing the effect of aerobic activity on GST may reveal subtle lingering deficits during concussion recovery. Therefore, the use of GST with an aerobic exertion protocol may help determine physiological recovery of the VOR. This case series examined the utility of this protocol in a group of athletes recovering from concussion.
Case Description: 16 athletes (7 female) with dizziness and balance symptoms following sport-related concussion (SRC) underwent vestibular physical therapy. Individuals were injured while participating in combat, contact and non-contact sports, with seven patients having no prior history of concussion.
The average time from injury to start of care was 24.5 days (range = 8 - 221) with initial average yaw GST values of 164.81 deg/s in leftward direction movements and 165.0 deg/s in rightward direction movements. Over the course of treatment, athletes completed active rehabilitation consisting of vestibular exercises and aerobic sport specific activity, in clinic and at home. Once athletes achieved higher levels of GST on a subsequent assessment day (average 221.56 deg/s leftward and 223.68 deg/s rightward), they underwent a sport specific aerobic exertion protocol to understand if the VOR declined with aerobic activity. Following the initial exertion protocol, 8 individuals demonstrated a negative decline, ranging from -2.0% to -15.0%, and were not released to return to play. This group continued with vestibular therapy and at the end of treatment, the GST values, on average, were 244.37 deg/s in leftward and 239.66 deg/s in the rightward direction for the entire group of athletes.
Discussion: Assessing GST with exertion may provide a way to evaluate higher-level vestibular dysfunction in athletes following SRC. Having athletes exercise at an intensity that approximates their sport during the SRC recovery process may reveal a functional deficit that does not otherwise appear in traditional assessments. Ultimately, the optimal management of SRC is intended to contribute to safer return to play.
FP0977Gaze Stability in Young Athletes: performance and gender differences
Amy Alexander1, Shelly Massingale1, Nicholas Hattrup2, Jamie Pardini1
1Banner Sports Medicine and Concussion Specialty Clinic; 2Boston University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Understanding how healthy athletes perform is important to optimally manage recovery from injury, especially in sport related concussion (SRC). Premature return to competition has been associated with an increased risk of orthopedic injury. The gaze stability test (GST) is a functional assessment of the vestibular ocular reflex (VOR), which assesses the maximum velocity a person’s head can move and maintain acuity. This ability relates to better athletic performance for many precision tasks as well as potential avoidance of injury. Studies have established norms in the athlete population, but none have included female athletes, and none have focused on youth athletes.
Methods: 101 (25 female) club sport athletes aged 7 to 17 years (mean age = 13.74 ±2.0) presented to an urban concussion specialty clinic for a multi modal preseason baseline test battery, of which the GST was one element. The clinic protocol used consisted of three tests using Bertec® Vision Advantage: static visual acuity (SVA)-calibrated for 5 ft from laptop screen, visual perception time test (VPT), and yaw GST in the high-performance range (GST-HP) starting at 140 deg/s-as detected by an accelerometer secured to the athlete’s head, with a maximum 400 deg/s. The optotype is 0.2 logMAR larger than SVA, flashed on the screen when the athlete was within an acceptable range of that trial’s intended velocity for 3 turns in a row. GST-HP results are determined by the program’s algorithm.
Results: Average leftward direction head movement for the athletes was 183.55 deg/s (± 41.83) with range = 120-330 deg/s and 191.24 deg/s (± 42.09) with range = 120-280 deg/s in the rightward direction. Consistency indexes within the program indicated that all trials were valid. Analyses using a 2-tailed independent sample t-test determined no significant difference between males and females for either left or right GST (leftward male
Conclusions: Each of the Concussion in Sport Group consensus statements underscores the importance of a multidisciplinary approach to managing recovery in the injured athlete. This study adds to the scientific literature by providing objective information on normal GST performance in youth athletes, which should in turn assist clinicians in understanding when an injured athlete has returned to expected levels of function and can safely return to play.
FP0983A Quantitative Analysis of Sway Patterns in Vestibular Assessment using an Open Source Sensor System.
David Ávila-Quezada1, Haydee Barrientos-Ojeda2, Enrique Gallo-Barraza3, Elvis Mancilla-Goldschmidt4, Julio Soto-González5, Jorge Mardones-Meléndez6, María Latorre-González7, Ignacia Inarejo-Inarejo8
Universidad Austral de Chile
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
For the assessment of sway, clinic has a wide range of tests, such as Romberg’s, Fukuda’s stepping, or dynamic gait. However, these are, mostly, subjective and qualitative in character. At present, technological advances have allowed the development of new assessment instruments, such as inertial measurement devices (IMU), which aim to complement the results, from an objective and quantitative point of view. The inertial sensors used to measure acceleration and axial turn in three dimensions, which are then transformed into digital information.
The objective of this investigation, has been to create and test a platform for measuring the body sway and gait disturbance, for its use in vestibular evaluation and/or rehabilitation. The platform used was designed as open source; a model that allows open collaboration, creation of decentralized knowledge, always being in continuous evolution.
Methods: To achieve this objective, a protocol with different tests that contemplated measurements was designed, including: Romberg’s Test, Timed up and go, and walk test. All tests with and without sensor system. 86 subjects were examined, ranging from ages between 19-32 (71 cases), and older than 65 years (15 cases). The selected subjects were individuals without vestibular alterations.
For the evaluation, the equipment was set in the back, between L4-L5.
Results Romberg’s Test: The obtained results were the antero-posterior and lateral oscillations. The obtained values through the sample were 1.1 Hz (sd +-0.7), being within the observed ranges for the oscillations of human movements.
TUG: The results analyzed with the traditional measurement, compared to the IMU evaluation, showed a strong positive correlation (p.96), showing that the equipment measurements can replace the chronometer measurements. Also, a graph that allows for posterior analysis and extraction of more data was obtained (see fig. 1).
Figure 1:
TUG results.
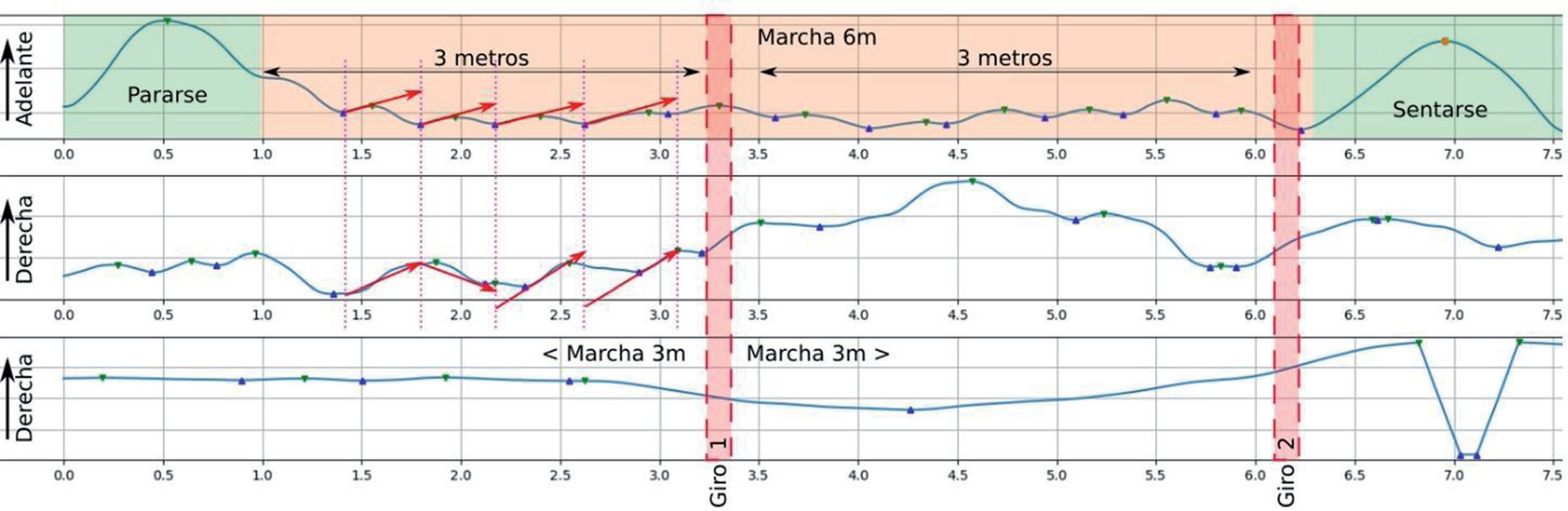
Walk test: The results obtained in this test showed a strong correlation (p .9), between the analogue observation and the IMU evaluation. Nonetheless, the most important result was the characterization of the march oscillations (see fig. 2).
Figure 2:
Cyclical pattern of march phases.
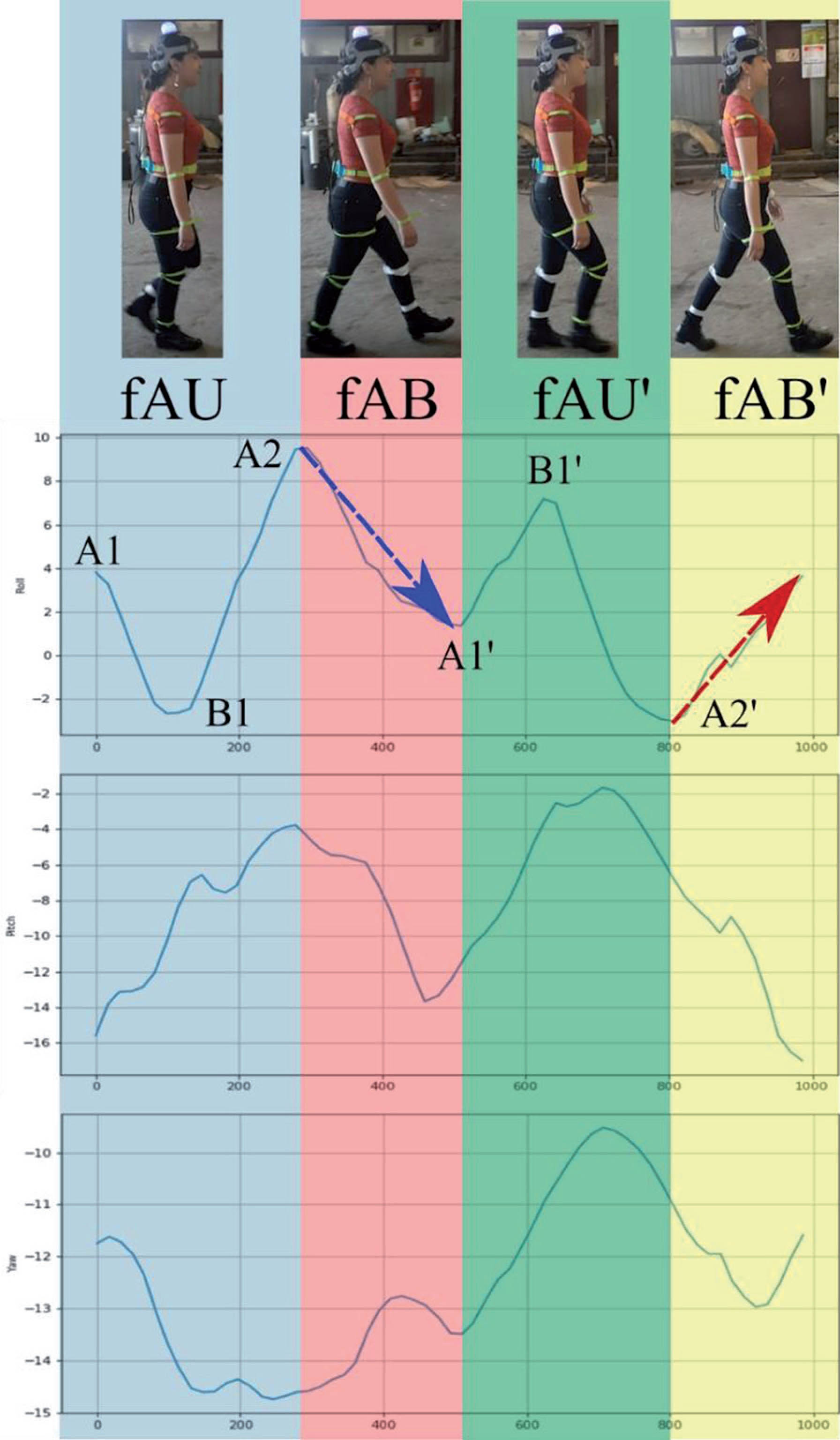
Conclusions: The obtained results allowed us to describe patterns of the different tests used in Vestibular Assement with IMU. At present, we are increasing the studied population; also, regression formulas are being worked on, to determine possible alterations in patterns.
For more information and download or sponsor this project, please visit https://github.com/Debaq/Fullaxis
FP0988Are gain values significantly altered by manual data selection when performing the video Head Impulse Test on all six semicircular canals with two different v-HIT systems?
Abrahamsen1,2, Regitze Skals3, Dan D. Hougaard1,2
1Department of Otolaryngology, Head & Neck Surgery and Audiology, Aalborg University Hospital, Aalborg, Denmark; 2Department of Clinical Medicine, Aalborg University, Aalborg, Denmark; 3Unit of Clinical Biostatistics and Bioinformatics, Aalborg University Hospital, Aalborg
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: It has not yet been tested whether mean gain values and the presence of pathological saccades are significantly altered by manual data selection or if data selection done by the incorporated software detection algorithms alone provides a reliable data set following video head impulse testing (v-HIT).
Methods: 120 subjects with neither vestibular nor neurological disorders underwent four separate tests of all six SCCs with either EyeSeeCam® (Interacoustics©, Middelfart, Denmark) or ICS Impulse® (Otometrics©, Taastrup, Denmark). All v-HIT test reports underwent manual data selection by an experienced ENT Specialist with deletion of any noise and/or artifacts. A paired T-test comparing mean gain values based upon unsorted data gain values and sorted data gain values was performed.
Results: EyeSeeCam®: Horizontal semicircular canals (SCCs): The estimate and the p-value for respectively the right lateral SCC and the left lateral SCC were 0.00088 (0.69) and 0.00004 (0.95). Vertical SCCs: The estimate varied from -0.00858 to 0.00637 with p-values ranging from 0.27 to 0.79. ICS Impulse®: Horizontal SCCs: The estimate and the p-value for respectively the right lateral SCC and the left lateral SCC were 0.00071 (0.26) and 0.00159 (0.06). Vertical SCCs: The estimate varied from 0.00217 to 0.01357 with p-values ranging from 0.00 to 0.05. Based upon the mean gain value from the individual SCC being tested, 148 tests before and 127 after manual data selection were considered pathological.
Conclusion: None of the two v-HIT systems revealed any clinically important effects of manual cleaning. However, 21 fewer tests were considered pathological following manual data selection.
FP0992V-HIT in darkness
Paz Pérez-Vázquez1, Virginia Franco-Gutiérrez2
1Hospital Universitario de Cabueñes, Gijón, Spain; 2Hospital Universitario Lucus Augusti, Lugo, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: The earliest components of the Head Impulse Test (HIT) (within 70-80 ms of the onset of head rotation) are controlled by the vestibulo-ocular reflex (VOR), complemented by the optokinetic and pursuit systems, with a relatively long delay (70-80 ms).
The purpose of this study was to evaluate the possibility of individualizing the VOR contribution to the V-HIT.
Methods: Thirty-six healthy individuals (19 males, 17 females; age 21-64 years, mean 39 years) underwent horizontal video HIT (vHIT). This was first conducted in darkness (covering the eyes with an adapted opaque cap) without visual target and then visually tracked.
An EyeSeeCam device (software version 1.3.0.008, Interacoustics, Denmark) was employed for both paradigms.
Results: After rejecting artifacts, 691 (342 right, 349 left) impulses in darkness and 886 (434 right, 452 left) impulses visually guided were analyzed. Seventy per cent of the impulses performed in darkness delivered ocular responses opposite to the head direction, matching its velocity to a point where a quick anti-compensatory eye movement (SQEM) stopped the response; of these, 75% recaptured the head velocity after culmination. Thirty per cent of the responses completed a bell-shaped curve. SQEM mean latency was 58.21 ms (interquartile range 60-67 ms)
Men and women showed different behavior: Females completed more bell-shaped curves than males (42 vs 15%, respectively; p=0.01). SQEM latency was longer (62.81 vs 55,71 ms; p<0.01) and time to recapture the bell-shaped curve was shorter (77.51 vs 92.52 ms; p<0.01) in females than in males.
When comparing vHIT responses in darkness and in the visually guided test, the completed bell-shaped curve gains and instantaneous gains (at 40, 60 and 80 ms) before SQEM were equivalent for both paradigms, as well as regression gains. Men and women showed comparable gains in both paradigms.
Conclusions: Lateral canals VOR effect can be localized in the first 70 ms of the responses. HIT paradigm responses seem to be not only influenced by vision and other influences, pre-programing the response, might be contemplated. Since gender quantitative differences related to functional test have not been stated, the qualitative differences founded in this study led to consider the significant relationship between vestibular function, particularly horizontal canal function, and topographical memory that has been previously demonstrated. Interestingly, topographical memory tests have shown large differences between males and females.
FP0995Aetiology, diagnosis and management of vestibular disorders in children
Sudhira Ratnayake
Alder Hey Children’s NHS Foundation Trust/University of Liverpool, Liverpool, United Kingdon
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Vestibular disorders in children are significant causes for childhood morbidity with various manifestations that are often unrecognised or undiagnosed. Dizziness/vestibular symptoms are usually managed by paediatricians and paediatric neurologists or neurotologists and surgeons who primarily deal with adults. Dedicated paediatric neurotologists require training in all aspects of paediatric diseases for a holistic approach for management that is crucial for best outcomes.
The aetiological profile for peripheral and central disorders is markedly different from that in adults. For example, vestibular migraine is the commonest paediatric vestibular affliction; third window disorders in children may follow a different course than adults; idiopathic Meniere’s disease and benign positional paroxysmal vertigo are very rare and a third of sencorineural hearing losses due to any cause is also accompanied with a vestibular deficit. The diagnostic algorithm with latest technology is also different as children are far more difficult to obtain anamnesis from and to test as compared to adults. Examining a child is really an art that can come from years of experience and the knowledge about the paediatric vestibular system and its development. Following diagnosis, treatment might follow a different trajectory than adults and it is important to acknowledge this. It is also important to recognise the close overlap with paediatric neurology and indeed, a robust knowledge in neurology is essential to practice paediatric neurotology.
This presentation includes a brief overview of no more than 8 minutes of the developing paediatric vestibular system in children, aetiology of paediatric vestibular disorders, the diagnostic process with evidence based latest methods and their management. The differences in paediatric vestibular diagnosis and disease profiles as compared to adults are also highlighted from the authors’ personal series. The target audience is neurotologists who practice vestibular medicine, audiologists and audiological scientists, physiotherapists and neurologists.
FP0996Development of a diagnostic framework for vestibular causes of dizziness and unsteadiness in patients with mitochondrial disease – A Delphi consensus
Amanda Male1,2; Sarah Holmes3; Ros Quinlivan3; Michael Hanna3; Robert D.S. Pitceathly3; Gita Ramdharry3; Diego Kaski2
1Therapy Services, The National Hospital for Neurology and Neurosurgery, Queen Square, London, WC1N 3BG, United Kingdom; 2Department of Clinical and Movement Neurosciences, University College London, Queen Square, London, WC1N 3BG, United Kingdom; 3MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology and National Hospital of Neurology and Neurosurgery, Queen Square London, WC1N 3BG, United Kingdom
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
PURPOSE: Mitochondrial diseases are a diverse group of genetic conditions for which limited treatment options exist. Adult mitochondrial disease (MD) is among the commonest adult form of inherited neurological disorders. Unsteadiness is a commonly reported problem for adults with MD, and is frequently attributed to ataxia and/or peripheral neuropathy.
Holmes et al 2018, identified benign paroxysmal positional vertigo (BPPV), peripheral vestibulopathy and vestibular migraine as frequent causes of unsteadiness and dizziness in adults with MD. Each of these diagnoses require specific diagnostic tests and management, including vestibular rehabilitation.
Vestibular diagnoses are commonly missed so we aimed to develop a diagnostic framework to enable earlier diagnosis. We used consensus methods to guide the diagnostic questions included in the framework.
METHODS: A modified electronic Delphi approach was used comprising three rounds. Round one developed the statements from research evidence-based literature, for BPPV, peripheral vestibulopathy and vestibular migraine. The statements were emailed by the secretary to members of the European Academy of Neurology (EAN), specialist panel of neuro-otologists. Two emails were sent each round.
Specialists were asked to rate how much they agreed or disagreed with the statements being included in the framework using a six-point scale (0=strongly agree, 5=strongly disagree). Respondents could also suggest any rewording to be considered for the next round if consensus was not met.
Consensus per statement was defined when >75% of the responses were in the lower or higher tertile (Boulkedid et al., 2011). Only the statements that did not reach consensus were recirculated in round three.
RESULTS: Twenty nine percent of EAN members replied to round two (n=12) and 24% for round three (n=10). Twelve statements were emailed in round two, with five reaching consensus. Four were removed for round three due to the comments from specialists that they were not sensitive enough to discriminate multiple causes of dizziness. Three statements were reworded for round three, with only one reaching consensus. A total of six statements were included in the diagnostic framework.
CONCLUSION: A modified Delphi study has identified key questions to ask patients with mitochondrial disease reporting dizziness and unsteadiness, in order to identify vestibular causes. These questions have been included in a diagnostic framework that will be validated in an observational cohort study design.
FP1002The Interplay between Bone Mineral Density and Meniere’s Disease
Avi Shupak1,2, Nabil Faranesh1
1Unit of Otoneurology, Lin and Carmel Medical Centers; 2Faculty of Social Welfare and Health Sciences, The University of Haifa
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Previous studies have reported an association between reduced bone mineral density and the occurrence of benign paroxysmal positional vertigo, balance impairment, and saccular dysfunction. Also, the results of recent animal studies have raised the possibility that vestibular dysfunction could affect bone remodeling and bone mass. The goal of the study was to compare bone mineral density of patients suffering from definite Meniere’s disease to that of a matched control group.
Subjects and Methods: The study group included 23 patients suffering from definite Meniere’s disease and the control group 23 patients matched in their race, gender and age parameters in whom no vestibular pathology could be found. Dual energy x-ray absorptiometry of the femoral head was used for the assessment of bone mineral density.
Results: The average T scores were -1.53±1.08 in the study and -0.39±0.72 (P=0.016) in the control group and the Z scores -0.4±0.63 and 0.33±0.31 (P=0.018) respectively. 17 patients (74%) of the study group and 9 (39%) of the control had T scores less than -1.0 indicating osteopenia/osteoporosis (P=0.036).
Conclusions: The results show significant association between Meniere’s disease and reduced bone mineral density of the femoral head. Bone mineral density studies of the weight bearing bones are warranted in Meniere’s disease for the early diagnosis and treatment of osteopenia/osteoporosis on one hand and possible benefit of this treatment on Meniere’s diseases evolution on the other hand.
FP1007Screening Measures and Prediction of Vestibular Diagnostic Test Results
Helen S Cohen1, Haleh Sangi-Hahgpeykar2, Megan Watts1, Alex D Sweeney1, Angela S Peng1, Nathan Silver1
1Departments of Otolaryngology - Head and Neck Surgery, Baylor College of Medicine, Houston, TX, USA; 2Department of Obstetrics and Gynecology, Baylor College of Medicine, Houston, TX, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Many patients come for care of “dizziness” with vague complaints, not all of which are true vertigo or oscillopsia. Many patients, especially seniors, have multiple health problems. Some of those problems cause symptoms that patients may associate with vestibular disorders, even though they may not be related. Because some patients may not understand the questions they may give misleading answers to questions that clinicians ask patients during the initial visit.
Objective: The goal of this study was to determine if some screening measures are useful for predicting the presence of vestibular impairments as indicated by results of objective diagnostic tests of the vestibular system.
Methodology: This retrospective study examined electronic medical records of 150 adult patients who had visited a neurotologist and were then referred for the complete objective vestibular test battery (VNG). We noted blood pressure and pulse as measured by the clinic nurse, responses to screening questions asked by the neurotologist, and outcome of the VNG.
Results: Blood pressure in the range of Stage 2 hypertension and responses to the question about vertigo predicted abnormal VNG responses. Pulse, blood pressure in the range of Stage 1 hypertension, and responses to questions about balance, lightheadedness and oscillopsia did not predict VNG outcome. Subjects with blood pressure in the range of Stage 2 hypertension had high rates of diabetes and diagnosed hypertension diagnosed by primary care physician or cardiology.
Conclusions: Clinicians can use these two responses, very high blood pressure as measured in the clinic by a nurse and responses to questions about vertigo, to help decide whether or not a VNG is indicated. Other screening measures may not be so useful.
Supported by NIH grant 2R01-DC009031
FP1011Otoneurological manifestations and VHIT findings in CANVAS
Emilio Ruiz Fernandez2, Laura Rebolledo Bernad1, Ernesto Sanchez Llanos1, Diego Casas Sanz1, Jose Gazulla Abio2, Jesus J. Fraile Rodrigo1
1Otorhinolaryngology Department, Miguel Servet University Hospital, Zaragoza, Spain; 2Neurology Department, Miguel Servet University Hospital, Zaragoza, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS) is a neurodegenerative disease that causes progressive imbalance. The sensory deficits found in this syndrome have been attributed to a neuronopathy, that would affect the Scarpa’s ganglion, leaving the spiral ganglion unaffected. We present a prospective study describing the characteristics and otoneurological manifestations of four patients meeting CANVAS criteria, two women and two men. Age ranged from 60 to 83 years. All patients underwent neurological and otoneurological examination using videonystagmography and vHIT. Two of them had been previously identified as carriers of a biallelic expansion of an intronic repeat in the RFC1 gene. All four patients showed progressive cerebellar ataxia, lower limb proprioceptive sensory loss, dysarthria and unsteady gait. Two patients had spasmodic cough at the symptom debut. The otoneurological examination found a bilateral vestibulopathy in all of them, as well as downbeating nystagmus and gaze nystagmus. Audiometry test showed moderated mixed hearing loss in all four patients, with symmetrical sensorineural hearing loss related to old age. There was no relationship between the progression of the disease and the hearing impairment. Our findings confirm the association of bilateral vestibulopathy and preserved hearing in CANVAS patients, although further research is needed to fully describe the phenotype of the disease. In our opinion, vHIT is a useful test to identify the global and bilateral vestibulopathy in a systematic and objective way.
FP1012Change of VOR gain after surgical plugging in superior canal dehiscence syndrome
Ja-Won Koo1, Jaehong Park2, Sang-Yeon Lee1
1Department of Otorhinolaryngology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea; 2Wirye Hana Otorhinolaryngology Clinic, Seongnam, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Superior semicircular canal dehiscence (SCD), which is characterized by a “third mobile window” in the inner ear, causes various vestibular and auditory symptoms and signs. Surgical plugging of the superior canal (SC) can eliminate the symptoms associated with increased perilymph mobility due to the presence of the third window. However, the natural course of vestibular function after surgical plugging remains unknown. In this study, we explored longitudinal vestibular function after plugging surgery in subjects with SCD.
Materials and Methods: A total of 11 patients, who underwent SCD repair via middle fossa approach were included in this study. Changes in vestibulo-ocular reflex (VOR) gain in all planes were measured over 1 year with the video head impulse test. We also evaluated surgical outcomes, including changes in symptoms, audiometric results, and electrophysiological tests, to assess whether plugging eliminated third mobile window effects.
Results: The mean VOR gain for the plugged SC decreased from 0.81 ± 0.05 before surgery to 0.65 ± 0.08 on examinations performed within 1 week after surgery but normalized thereafter. Four of seven subjects who were able to perform both VOR tests before surgery and immediately after surgery had pathologic values (SC VOR gain < 0.70). Conversely, the mean VOR gain in the other canals remained unchanged over 1 year. The majority of symptoms and signs were absent or markedly decreased at the last follow-up evaluation, and no complications associated with the surgery were reported. Surgical plugging significantly attenuated the air-bone gap, in particular at low frequencies, because of increased bone conduction thresholds and deceased air conduction thresholds. Moreover, surgical plugging significantly increased vestibular-evoked myogenic potential thresholds and decreased the ratio of summating potential to action potential in plugged ears. Postoperative heavily T2-weighted images were available for two subjects and showed complete obliteration of the T2-bright signal intensity in the patent SC lumen in preoperative imaging based on filling defect at the site of plugging.
Conclusion: Our results suggest that successful plugging of dehiscent SCs is closely associated with a transient, rather than persistent, disturbance of labyrinthine activity exclusively involved in plugged SCs.
FP1013Quantitative three-dimensional image analysis of the superior canal after surgical plugging of superior semicircular canal dehiscence
Ja-Won Koo1, Sang-Yeon Lee2, Won-Ki Jeong3
1Department of Otorhinolaryngology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam; 2Department of Otorhinolaryngology, Seoul National University Hospital, Seoul, 3Department of Computer Science and Engineering, Korea University, Seoul, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Surgical plugging to treat superior semicircular canal dehiscence (SCD) has been proven to impede the effect of the third mobile window, abating cochleovestibular symptoms. Knowledge of superior semicircular canal (SC)-plugging status has been proposed to serve as a guide for adjuvant treatment. Here, we investigated disturbances in the inner ear fluid space following SC plugging using a novel three-dimensional (3D) reconstruction-based method.
Methods: The study was conducted in 7 subjects who had undergone surgical plugging of SC via MFA. MRI examination were performed around 1 year after surgery using a 3 T MR scanner. 3D images were reconstructed by combining manual segmentation of the labyrinth and an automatic thresholding algorithm to visualize the surgical plugging status of a dehiscent SC. In this process, assessment of the 3D volume of the SC plugging and its application to interpret the clinical results are indispensable. This approach used a semi-automatic segmentation algorithm and a direct volume rendering method derived from conventional magnetic resonance images. The variable extents of filling defects at the sites of SC plugging and the positional relation of the defect to the ampulla and common crus were identified.
Results: The success group exhibited markedly reduced volumes following surgery, whereas one subject who could not achieve surgical resolution displayed no changes in volume. These results indicate that the success or failure of SC plugging was related to 3D volume changes in the labyrinth fluid signal. Sparing ampulla in success group seems to be related to restored VOR gain after surgery.
Conclusion: This study presents individualized SC-plugging statuses using a novel 3D reconstruction-based method and it facilitates future work regarding easy-to-measure 3D volume changes. This current technology also aids in the exploration of pathologic changes in various targets of interest.
FP1015Abnormal sense of self in a cohort of patients with otoneurological disorders: clinical features and precipitating factors
Maya Elzière1,2, Marco Bressan3, Christophe Lopez1
1Laboratoire de Neurosciences Cognitives, CNRS and Aix-Marseille University, Marseille, France; 2Centre des Vertiges, Hôpital Européen de Marseille, Marseille, France; 3 Laboratoire de Psychologie Cognitive, CNRS and Aix-Marseille University, Marseille
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
An increasing number of reports indicates that vestibular disorders evoke deficits reaching far beyond postural and oculomotor reflexes, including deficits in cognition and affective control, resulting in severe everyday life limitations. Pioneering work in otoneurology and epileptology have associated vestibular disorders with disturbances in the sense of self and own-body representations. Among the most consistently reported symptoms are sensations resembling depersonalization-derealization (DD) – indicating a sense of unreality and estrangement of the self ; out-of-body experiences or Alice in Wonderland syndrome. However, research into these phenomena was mostly based on case reports or small patients groups lacking proper otoneurological examination. Research has poorly described the relation between different etiologies of dizziness and vertigo, comorbidities such as migraine, anxiety and depression, with the sense of self.
The aims of this prospective, observational study was to compare DD symptoms in 390 patients with dizziness/vertigo with 390 age- and sex-matched participants with no history of dizziness/vertigo. The DD was evaluated using the Cambridge Depersonalization Scale from Sierra and Berrios (2000). We analyzed precipitating factors of DD such as sociodemographic data, history of the disease, frequency of vertigo/dizziness, clinical parameters from otoneurological examination, anxiety and depression.
The total DD score was significantly higher in patients than in controls. Symptoms of DD in patients were reported as significantly more frequent and to last significantly longer than in controls. 12% of patients with dizziness had scores above the cut-off point for DD, whereas only 2% of controls had scores above the cut-off point, in line with DD prevalence in the general population. Among patients, DD intensity increased significantly with the frequency of vertigo/dizziness, but DD intensity did not differ significantly between etiologies of vertigo/dizziness.
The structure of DD symptoms was analyzed using an exploratory factor analysis, which revealed 4 components (distorted body and self experience, distorted subjective recall, numbing, perceptual alterations). A mediation analysis indicated that between 39% (distorted body and self experience) and 100% (distorted subjective recall) of the observed differences in DD components scores between the two groups are explained by the mediation effect of anxiety and depression.
In conclusion, DD is not a rare phenomenom in otoneurological populations. Anxiety and depression mediate most of the differences between DD intensity in patients and controls, probably in line with the frequency of the perceptual incoherence created by multisensory misintegration in the brain during vertigo/dizziness.
FP1020Functional Head Impulse Testing Might Be Useful for Assessing Vestibular Compensation After Unilateral Vestibular Loss
Julia Sjögren, Per-Anders Fransson, Mikael Karlberg, Måns Magnusson, Fredrik Tjernström
Department of Clinical Sciences, Otorhinolaryngology Head and Neck Surgery, Skåne University Hospital, Lund University, Lund, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Loss of the vestibulo-ocular reflex (VOR) affects visual acuity during head movements. Previous studies have shown that compensatory eye-saccades improve visual acuity and that the timing of the saccade is important. Most of the tests involved in testing VOR are made with passive head movement, that do not necessarily reflect the activities of daily living and thus not being proportionate to symptoms and distresses of the patients.
Objective: To examine differences between active (self-generated) or passive (imposed by the examiner) head rotations while trying to maintain visual focus on a target.
Method: Nine subjects with unilateral total vestibular loss were recruited (4 men and 5 women, mean age 47) and tested with video Head Impulse Test (vHIT) and Head Impulse Testing Device-Functional Test (HITD-FT) during passive and active movements while looking at a target. VOR gain, latencies of covert saccades, frequency of covert saccades and visual acuity were measured and analyzed.
Results: Active head-impulses toward the lesioned side resulted in better visual acuity (p = 0.002) compared to conventional passive head-impulses and generated eye-saccades with significantly shorter latencies (p = 0.004). Active movements to the lesioned side generated dynamic visual acuities that were as good as when testing the intact side.
Conclusion: Actively generated head impulses resulted in normal dynamic visual acuity, even when performed toward the side of total vestibular loss. This might be attributed to the appearance of short-latency covert saccades. The results show a strong relationship between self-generated movements, latencies of covert saccades and outcome in HITD-FT, i.e., a better dynamic visual function with less retinal slip which is the main function of the VOR. The method of active HITD-FT might be valuable in assessing vestibular compensation and monitoring ongoing vestibular rehabilitation.
FP1023AQEM: a Marker of Peripheral Involvement in the Acute Vestibular Diseases
Enrico Armato, Marta Mion, Andrea Castellucci
San Giovanni e Paolo Hospital, Venice; Santa Maria della Misericordia, Rovigo; Arcispedale Santa Maria Nuova, Reggio Emilia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: with the term AQEM (Anticompensatory Quick Eye Movements) we define some anticompensatory saccades detected during video Head Impulse Test (vHIT) examination on the healthy side in patients with an acute peripheral vestibular disease (APVD). AQEM can be considered a sign of peripheral involvement in cases of spontaneous nystagmus and can be found in many vHIT tracks, though usually neglected by examiners.
Methods: we retrospectively analyzed 60 vHIT tracks of patients presenting to our attention with acute vertigo.
Results: AQEM occurred in 30 patients (50%). Mean latency was 338.33 ± 24.76 msec. 55% of cases had a history consistent with recent acute rotatory vertigo. 75% of patients presented with horizontal spontaneous nystagmus in hibited by visual fixation and 90% of vHIT documented a specific and isolated impairment of the vestibulo-ocular re flex (VOR) for horizontal canals. AQEM on one side were associated with lower VOR-gain on the contralateral ear (p < 0.0001). 24 patients among 30 cases exhibiting AQEM underwent neuroimaging and none of them showed central nervous system (CNS) pathologies.
Conclusions: standard profile of AQEM can be summarized as follows. VOR-gain is close to zero for horizontal canal contralateral to the affected side. Typically, there is a spontaneous nystagmus inhibited by visual fixation. Patients mostly present a history of recent acute rotatory vertigo. Mainly horizontal canals are involved. AQEM seem to represent a transient finding. In contrast to few works dealing with this subject, we found very broader and heterogeneous categories of patients, though most of them did not show CNS involvement. AQEM could represent an interesting marker of APVD.
FP1024Etiologic Distribution of Dizziness and Vertigo
Hyo-Jung Kim, PhD1, Ja-Ok Lee, MSc2, Jeong-Yoon Choi, MD, PhD2,3, Ji-Soo Kim, MD, PhD2,3
1Research Administration Team, Seoul National University Bundang Hospital, Seongnam, Korea; 2Dizziness Center, Seoul National University Bundang Hospital, Seongnam, Korea; 3Department of Neurology, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: This study aimed to determine the etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea.
Methods: We analyzed the diagnoses of 21,166 consecutive dizzy patients (12,691 women, mean age = 57.9±15.7) seen from 2003 to 2019 using a registry and medical records. Overall, dizziness and vertigo were more common in women (60.0%, CI=0.59~0.61) than in men without a difference in age (57.7±15.5 vs. 58.1±16.1, p=0.094).
Results: Benign paroxysmal positional vertigo (BPPV, 24.1%) was the most common cause of dizziness/vertigo, followed by psychiatric or persistent postural perceptual dizziness (20.8%), vascular disorders (12.9%), vestibular migraine (10.2%), Meniere’s disease (7.2%), vestibular neuritis (5.4%). These six disorders comprised more than 80% of all disorders. The etiology could not be determined in 5.0%, and more than one etiology were found in 14.1%. Vestibular migraine was the most common disorder in children and adolescents (<19 years), psychiatric or persistent postural perceptual dizziness (26.3%) in the adults (19-64 years), and BPPV (28.2%) in the elderly (= 65 years). We estimated the number of hospital visits due to dizziness/vertigo in South Korea in 2050 using the data from the KOSIS and the Healthcare Bigdata Hub (health insurance review & assessment service in South Korea). 3,974 visits per 100,000 of general population in 2019 and 6,057 in 2050, an increase of 52% over the years.
Conclusion: This etiologic distribution is similar to that reported in another country, and indicates no significant differences in the proportion of diseases causing dizziness and vertigo across different ethnic groups. This study provides valuable information to establish healthcare policy for dizziness and vertigo.
FP1029The use of smartphones in the treatment of MdDS and other vestibular disorders
Michiel Carpentier, Jan Van Riel
MdDS Reset
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
MdDS Reset was founded by Jan Van Riel and Michiel Carpentier.
Jan Van Riel is a software engineer and a serial entrepreneur. He holds over 30 software patents and has co-founded five startups, several of which had very successful exits. He co-founded startup Twintag, where he is also still active as both as Chairman of the Board and software engineer.
After disembarking from a long flight, somewhere in 2018, Jan kept feeling swaying emotions when sitting still, as if he would still be on the plane. This condition now seemed permanent, sometimes somewhat better and then a few days later again worse. This was the third incident in a decade. Not a single doctor could tell him what was wrong. He was tested extensively yet nothing could be found.
Finally he was diagnosed with MdDS by Prof. Floris Wuyts of the University of Antwerp, a Bárány Society member. Prof. Wuyts also proposed optokinetic treatment in an optokinetic (OKN) booth. While receiving treatment in October 2019, Jan realised that there should be an easier way to deliver such optokinetic stimuli, using a simple smartphone mounted inside VR glasses.
After some discussions with Michiel Carpentier, a longtime colleague and associate of Jan, they decided to found a company in March 2020 to develop such a treatment. Towards the end of 2021 the product was ready for release, and a prototype of the software was tested by Floris Wuyts and Catho Schoenmaekers, who is doing an elaborate clinical trial of the mask, comparing it with the OKN booth (see separate free paper form submitted by Catho).
During the development many different improvements were discovered, as well as other possibilities of smartphone technology as a medical device, like e.g. using a smartphone’s sensors to objectively measure a Romberg balance test, or creating a treatment for Visually Induced Dizziness (VID).
Next to the treatment, all data gathered by the smartphone sensors is being stored in a big data platform (while respecting patient’s privacy) and can be made available for further research.
The submitter would like to present our first findings of actual patients using the device, as well as gather feedback from the audience.
FP1030Implementation of a vestibular test within a hearing screening program.
Background: Postural control depends on the integration of visual, vestibular and proprioceptive information. Balance and vestibular disorders in adults are well studied, but we know less about them in children. Although motor and balance function in children is still under development throughout childhood, the vestibular function is present at birth and becomes fully integrated in puberty. A vestibular assessment in infants and children is increasingly required in clinical practice especially in those undergoing cochlear implantation and children with delayed motor skills.
Methods: We propose a child-friendly method to screen the vestibular function along with the hearing screening program based on an application of cervical Vestibular Evoked Myogenic Potentials (cVEMP), induced by a vibratory stimulus and a stimulus delivery protocol regulated by the activity level of cervical muscles.
According to our feasibility study it is possible to test the vestibular function on a large scale in newborns and infants with cVEMP. cVEMP was used alongside the Stockholm Newborn Hearing Screening Programme in newborns that did not pass the hearing screening. cVEMP were obtained by mastoid stimulation with bone conducted tone burst at safe intensity levels and with a stimulus delivery regulated by the electromyographical (EMG) levels at the site of recording. Fifty infants were tested. cVEMP was defined as a short latency positive-negative electromyographic (EMG deflection), with a 12–17 ms positive peak (p1) and 20–25 ms the negative peak (n1) after stimulus. cVEMP could be completed in the majority of the children (86% and 97% in optimized test conditions) and a response identified in 73% of the tested ears (91% in optimized test conditions). The control of muscle activity under recording was the most critical factor to obtain responses with readable results. We also propose a technique to optimise the neck muscle activity under recording
Conclusions: Our results support the use of cVEMP as a vestibular screening tool in infants along with hearing screening programs.
FP1031The Relation Between Migraine and BPPV Characteristics
Pinar Yalinay-Dikmen1, Ozlem Gedik-Soyuyuce2, Alper Ozdilek3, Nazim Korkut4
1Acibadem Mehmet Ali Aydinlar University Neurology Department; 2Acibadem Maslak Hospital Audiology Department; 3Acibadem Mehmet Ali Aydinlar University ENT Department; 4Acibadem Maslak Hospital ENT Department
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
No
Objectives: Benign paroxysmal positional vertigo (BPPV) is the most common type of vertigo and the patients with migraine tend to experience various subtypes of BPPV. This study was designed to describe the relation between Migraine and BPPV characteristics in 2610 patients diagnosed with BPPV in our vertigo center in three years.
Materials and Methods: We retrospectively analyzed the records of 2610 patients (1705 female, 905 male; age range: 2-95 years, mean age 47.71±16.57) diagnosed with BPPV in the vertigo center of a tertiary hospital. BPPV diagnosis of all patients was made by using videonystagmography (VNG). BPPV was characterized by the presence of short-lasting positional vertigo with and/or without visual fixation induced by diagnostic tests specific for each semicircular canal. The migraine evaluation in all BPPV patients was done by a neurologist. None of the patients included in the study had central nervous system pathology.
Results: Migraine was diagnosed in 20.22% of all patients. Coexisting motion sickness was present in 94% of the migraine patients and was present in 40.8% of all patients. A recent history of trauma was present in 0.88%. Coexisting vestibular neuritis (VN) was present in 7.20%, coexisting Meniere’s Disease (MD) was present in 1.72% and coexisting labyrinthitis was present in 0.26% of all BPPV patients. The most common semicircular canal involvement in BPPV was the posterior with 60.45%. The other canal involvements were 30.61% lateral, 8.46% multiple and 0.45% anterior respectively. The right ear was affected in 32.83%, the left ar was affected in 30.80% and both ears were affected in 36.36%. Spontaneous nystagmus was observed in 11.57% of all patients and in 7.76% of the migraine patients; pseudo-spontaneous nystagmus was observed in 2.75% of all patients and in 1.89% of the migraine patients. All patients were successfully treated by canal-specific repositioning maneuvers. An average of 1.82±1.40 maneuvers were necessary for the complete abolition of positional nystagmus without visual fixation. The recurrence rate of BPPV was 34.71%. Our study demonstrated a positive correlation between migraine and the recurrence rate (p=0.000), a positive correlation between migraine and spontaneous nystagmus (p=0.001), but no correlation between migraine and the number of maneuvers necessary for complete recovery (p=287).
Conclusions: The clinicians should be aware of the coexistance of both migraine and BPPV in the same patient to enhance the diagnosis and management of recurrent spontaneous vertigo.
The target audience would be all vestibular specialists.
FP1032Analysis of the effectiveness of the prophylaxis of vestibular migraine depending on the diagnostic category and the prescribed drug
Emilio Domínguez-Durán1, María Alharilla Montilla-Ibáñez2, María Guadalupe Álvarez-Morujo de Sande3, Esther Domènech-Vadillo4, Carmen Bécares-Martínez5, Rocío González-Aguado6, Gloria Guerra-Jiménez7
1Hospital QuironSalud Infanta Luisa, Sevilla, Spain; 2Complejo Hospitalario de Jae’n, Jae’n, Spain; 3Hospital Universitario Puerta del Mar, Ca’diz, Spain; 4Hospital Universitari Joan XXIII, Tarragona, Spain; 5Hospital Universitario de Torrevieja, Torrevieja, Spain; 6Hospital Universitario Marque’s de Valdecilla, Santander, Spain; 7Complejo Hospitalario Universitario Insular Materno-Infantil, Las Palmas de Gran Canaria, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Vestibular migraine (VM) consists of recurrent episodes of vestibular symptoms that are accompanied by migraine in at least 50% of the episodes. The criteria of the Ba’ra’ny Society include two diagnostic categories: “actual” vestibular migraine and probable vestibular migraine. There is a wide range of drugs that can be prescribed for the prophylactic treatment of VM, but recommendations for the selection of the most appropriate drug are currently lacking. Objective: To measure the extent to which the prophylactic treatment of VM reduces vestibular symptoms, headache and the number of crises depending on the diagnostic category of the Ba’ra’ny Society and the drug used for prophylaxis.
Material and methods: This is a multicenter prospective study. Patients with VM who presented to any of the participating centers and who subsequently met the VM criteria were prescribed one of the following types of prophylaxis: acetazolamide, amitriptyline, flunarizine, propranolol or topiramate. Patients were called back for a follow-up visit 5 weeks later. This allowed the intensity of vestibular symptoms, headache and the number of crises before and during treatment to be compared.
Results: 31 Patients met the inclusion criteria. During the treatment, all the measured variables decreased significantly. In a visual analogue scale, the intensity of vestibular symptoms decreased by 45.8 points, the intensity of headache decreased by 47.8 points and patients suffered from 15.6 less monthly crises compared to the period before the treatment. No significant between-group differences were found when patients were divided based on their diagnostic category or the choice of prophylaxis prescribed to them.
Conclusion: Five weeks after the prescription of the treatment of VM, a reduction of their symptoms and crises was observed with no significant differences based on patients’ diagnostic categories or the choice of prophylaxis prescribed to them.
FP1033Exploring the frontiers of vestibular migraine: A case series
Emilio Domínguez-Durán1, Esther Domènech-Vadillo2, Carmen Bécares-Martínez3, María Alharilla Montilla-Ibáñez4, María Guadalupe Álvarez-Morujo de Sande5, Rocío González-Aguado6, Gloria Guerra-Jiménez7
1Hospital QuironSalud Infanta Luisa, Sevilla, Spain; 2Hospital Universitari Joan XXIII, Tarragona, Spain; 3Hospital Universitario de Torrevieja, Torrevieja, Spain; 4Complejo Hospitalario de Jae’n, Jae’n, Spain; 5Hospital Universitario Puerta del Mar, Ca’diz, Spain; 6Hospital Universitario Marque’s de Valdecilla, Santander, Spain; 7Complejo Hospitalario Universitario Insular Materno-Infantil, Las Palmas de Gran Canaria, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Patients with episodic vestibular syndrome (EVS) whose symptoms resemble those of vestibular migraine (VM) but who do not meet the criteria for it are common. Objective: To describe those patients suffering from EVS in whom defined etiologies have been ruled out in order to determine if their symptoms can be linked to VM.
Material and methods: Prospective multicenter study. The medical records of patients with VM and patients with EVS suggestive of VM but not meeting the criteria for it were examined. The characteristics of headache, the number and the length of attacks, the association of vestibular symptoms and headache, the intensity of symptoms and the response to treatment were recorded.
Results: 58 patients met the criteria for VM or probable VM; 30 did not. All of the symptoms improved significantly in the treated patients with VM or probable VM; in the rest of the treated patients, only the vestibular symptoms improved.
Conclusion: A subgroup of patients that cannot be attributed to any known vestibulopathy according to present day VM criteria profited from migraine treatment, suggesting that their vestibular symptoms belong to the migraine.
FP1034Persistent Postural-Perceptual Dizziness (PPPD) and Quality of Life: A Cross-Sectional Study on 212 Patients
Malin Herwander Steensnæs1, Mari Kalland Knapstad2,3, Frederik Kragerud Goplen1,2, Jan Erik Berge1,2
1University of Bergen, Norway; 2Department of Otorhinolaryngology, Haukeland University Hospital, Norway; 3Department of Health and Functioning, Western Norway University of Applied Sciences
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Target audience: Clinicians working with patients with chronic dizziness and researchers in the field.
Objective: To investigate whether Persistent Postural-Perceptual Dizziness (PPPD) was associated with increased burden of dizziness and reduced quality of life, and if so, to determine if this association could be explained by differences in anxiety and/or depression between patients with PPPD and dizzy patients without PPPD.
Study design: Cross-sectional study.
Setting: Outpatient otolaryngology clinic at a tertiary referral center.
Patients: 212 patients aged 18-67 years referred for dizziness were included. 155 (73%) were women. 39 (18,4%) were diagnosed with PPPD.
Main outcome measures: Patients underwent clinical examination and completed the following questionnaires: Dizziness Handicap Inventory (DHI), RAND-12 Health Status Inventory and Hospital Anxiety and Depression Scale (HADS). Scores in DHI and RAND-12 were compared between patients diagnosed with PPPD and patients without PPPD. Associations were tested by linear regression and adjusted for age, gender and HADS.
Results: Patients in the PPPD group had increased burden of dizziness and reduced quality of life (QoL) as shown by a higher DHI score (48.25 vs. 31.38, p<0.001) and reduced RAND-12 physical score (39.5 vs. 44.6, p=0.006). After adjusting for age, gender and HADS, PPPD was associated with a 14.3 (p<0.001) points increase in DHI, and a 3.74 (p=0.022) points reduction in RAND-12 physical score.
Conclusion: Patients with PPPD have a higher burden of dizziness and a lower physical health-related quality of life (HRQoL) compared to other dizzy patients. The difference was evident also after adjusting for anxiety and depression, illustrating how PPPD is a different entity than these common psychiatric conditions
FP1035A Retrospective Analysis of Patients with Vestibular Disorders
Ozlem Gedik Soyuyuce1, Zeynep Gence Gumus1, Alper Ozdilek2, Nazim Korkut3
1Acibadem Maslak Hospital Audiology Department; 2Acibadem Mehmet Ali Aydinlar University ENT Department; 3Acibadem Maslak Hospital ENT Department
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
No
Objectives: This study was designed to describe the epidemiological clinical profile of the most common vestibular disorders in adult patients.
Materials and Methods: Data from 1252 (798 women, 454 men) adults with a mean age of 44,52±15,37 (range, 19-92) years were collected from patients who underwent vestibular assessment at a vertigo center in a tertiary hospital over a 1-year period.
Results: Benign paroxysmal positional vertigo (BPPV) was the most common diagnosis in our group of patients (70.04%; n=877), which involved both primary BPPV (n=671), and secondary BPPV that was associated with vestibular migraine (VM; n=128), vestibular neuritis (VN; n=44), Meniere’s Disease (MD; n=30), and labyrinthitis (n=4). In patients with BPPV, the posterior (73.54%; n=645), lateral (19.15%; n=168), anterior (0.68%, n=6), and multiple (6.61%; n=58) semicircular canals were affected. BPPV was unilateral in 72.17% (n=633) and bilateral in 27.82% (n=244). BPPV recurrence over a 1-year period was 6.49% (n=57). VM was the second most common diagnosis (16.77%; n=210) followed by VN (7.66%, n=96), MD (4.39%, n=55), and persistent postural-perceptual dizziness (PPPD; 3.83%, n=48). Our study showed that central vertigo (0.87%, n=11), and labyrinthitis (0.47%, n=6) were less commonly diagnosed. Vestibular paroxysmia was diagnosed in only one patient.
Conclusions: BPPV and VM were the most common vestibular disorders in our study. Clinicians should be aware of the prevalence of the most common vestibular disorders to improve treatment outcomes and differential vestibular function testing is valuable in increasing diagnostic accuracy.
FP1038Benign paroxysmal positional vertigo and vestibular impairment among older adults with dizziness
Ellen Lindell1,5*, Therese Karlsson1,2, Lena Kollén3, Mia Johansson4,6, Caterina Finizia1,2
1Department of Otorhinolaryngology, Head and Neck Surgery, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 2Region Västra Götaland, Sahlgrenska University Hospital, Department of Otorhinolaryngology, Head and Neck Surgery, Gothenburg, Sweden; 3Department of Occupational Therapy and Physiotherapy, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 4Region Västra Götaland, Sahlgrenska University Hospital/Sahlgrenska, Department of Oncology, Gothenburg, Sweden; 5Region Västra Götaland, Södra Älvsborg Hospital, Department of Otorhinolaryngology, Boras, Sweden; 6Department of Oncology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Theme: BPPV among older adults reporting dizziness but not seeking medical care for their symptoms.
Target audience: ENT doctors, geriatrics, physiotherapists
Objective: This study aimed to investigate older adults visiting a geriatric institution for a bone density measurement who reported dizziness on a daily or weekly basis (but who are not seeking care for dizziness), according to BPPV, vestibular function, walking abilities and frequency of falls.
Methods: Patients coming for a bone density measurement answered questions regarding occurrence of dizziness. Patients having dizziness on a daily or weekly basis were considered eligible for the study and invited for investigation at the Ear, Nose and Throat clinic at Södra Älvsborg Hospital, Sweden. The patients answered questions about history of dizziness, medications, and comorbidities. They were also investigated for BPPV, vestibular deficits using the video head impulse test, walking speed, Timed Up and Go test (TUG) and for perception of verticality and horizontality and Romberg test.
Results: A total of 55 patients with dizziness were included. Fifteen (27%) were diagnosed with BPPV. Forty (73%) patients reported falling during the previous year, including 11 with BPPV. Dizziness when turning in bed was more common among patients with BPPV and increased the risk of BPPV eight-fold.
Conclusion: BPPV is common among older adults with dizziness, including among those not seeking medical care. It is important to identify older adults with BPPV and treat the condition since BPPV may contribute to falls. Asking about dizziness when turning in bed can help to distinguish patients with increased risk for BPPV and older adults with dizziness should be investigated for BPPV even when typical history is lacking.
FP1039The Concussion Balance Test (COBALT): Not Just for Youth Athletes Anymore. Norms for Ages up to 90
Shelly Massingale, Amy Alexander, Jamie Pardini
Banner University Sports Medicine and Concussion Specialists
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Purpose: The concussion Balance Test (COBALT) is an eight-condition postural control measure that assesses high-level balance skills initially designed for youth athletes (ages 10-18) participating in contact sports. Conditions 7 (C7) and 8 (C8) are the most challenging, requiring headshake eyes closed (C7) and a visual motion sensitivity (C8), both performed on foam. The purpose of this study was to explore the potential utility of these higher-demand tasks in an active older adult population. A sample of younger to middle-aged adults was used for comparison.
Methods: Subjects (ages 25-90; 49% female) were 85 active and healthy adults. All athletes ages 60+ were participating in the Huntsman Senior World Games (HSWG) athletic events, and athletes in the younger adult sample ranged from triathletes to average active adults exercising 3-4 times per week. COBALT was administered to all athletes, and sway scores and error rates were coded for all athletes able to complete each condition. For purposes of this study, only completion rates by age were examined.
Results: Initial completion rate for athletes ages 25-59 (22 subjects) was 100%; ages 60-69 (33 subjects) was 79%; ages 70-79 (27 subjects) was 63% and 80-89 (4 subjects) was 33%. The primary reason for not being able to complete these conditions was inability to keep up with the pace of the metronome or limited range of cervical spine motion required to move the head the required distance.
Conclusion: Active healthy adults through age 59 appear to be able to complete COBALT conditions C7 and C8, like younger athletes. However, as age increases past 60 years, the ability to complete these challenging conditions decreases. Thus, it will be useful to develop normative data for older age ranges, not only for sway and error rates, but also for completion rate. Clinically, it will be important to understand the impact that non-vestibular factors may have when assessing balance function of older athletes. In addition, study results demonstrate the usefulness of having individual baselines for athletes at all levels against which to compare in the event of an injury.
FP1041Video-oculography ‘HINTS’ in acute vestibular syndrome: a prospective study
Korda Athanasia1, Michailidou Efterpi1, Zamaro Ewa1, Wagner Franca2, Caversaccio Marco D.1, Mantokoudis Georgios1
1Department of Otorhinolaryngology, Head and Neck Surgery, Inselspital, University Hospital Bern and University of Bern, Bern, Switzerland; 2University Institute of Diagnostic and Interventional Neuroradiology, Inselspital, University Hospital Bern and University of Bern, Bern, Switzerland.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: The bedside three steps test known, as ‘HINTS’ (Head Impulse-Nystagmus-Test of Skew), is nowadays a well-established way to discern between peripheral and central causes in patients with acute vestibular syndrome (AVS). Currently, the use of videooculography gives the physicians the possibility to quantify all these eye movements. However, the accuracy of video-oculography (VOG) ‘vHINTS’ is still unknown.
Methods: We performed a prospective study from February 2015 until September 2020 on all patients presenting at the emergency department (ED) with signs of an AVS. All patients underwent a bedside expert ‘bHINTS’ examination and VOG ‘vHINTS’ followed by a delayed MRI, which served as a gold standard for stroke confirmation.
Results: We assessed 46 AVS patients 35 acute unilateral vestibulopathy patients (AUVP) and 11 stroke patients. The overall accuracy of ‘vHINTS’ to detect a stroke was 94% with 100% sensitivity and 88.9% specificity. On the other side, expert ‘bHINTS’ showed a lower accuracy of 88% with 90.9% sensitivity and 85.7% specificity. The agreement between bedside evaluation and videooculography for the head impulse test was good, for the nystagmus test was fair, whereas for the test of skew was almost perfect.
Conclusions: Bedsite ‘HINTS’ performed by experts was accurate for detecting strokes in AVS patients. Video-oculography ‘HINTS’ increased the accuracy of this test with an improvement of its sensitivity and specificity. The quantification of eye movements proves to be a valuable tool for a standardized assement of ‘HINTS’, which heps us to minimize the diagnostic erros.
FP1042Effect of Visual Target Ambiguity on the Semicircular Ocular Reflex
Yumiko O. Kato1, Fumihiro Mochizuki1, Koshi Mikami1, Shuichi Sakamoto2, Izumi Koizuka1
1Department of Otolaryngology, St. Marianna University School of Medicine; 2Tohoku University Research Institute of Electrical Communication
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
To estimate the effect of multi-modal vestibular rehabilitation, we are attempting to find the common scale for accuracy of location perception among modalities. We evaluated the effect on Semicircular Ocular Reflex (ScOR) gain by the visual stimuli with various ambiguity.
14 healthy adults participated in the present study. Horizontal eye movements were recorded by video-oculography under three conditions. In the earth fixed (EF) condition, the absolute position of the visual target was fixed. In the head fixed (HF) condition, the visual target was rotated in same direction to head rotation. In the pursuit (P) condition, the visual target was rotated sinusoidally without head rotation. We used six-patterns visual targets in three levels of blurriness and two levels of brightness. As the blurriness level, we set the circle with clear edge at one-degree diameter, the blur circle about 20 degrees diameter, and about 40 degrees diameter. The blurriness was made with Gaussian filter. The visual stimuli were projected on cylindrical screen (OKN screen) around the subjects. The chair the subjects were sitting on was rotated sinusoidally in the yaw-axis at 0.32Hz at an amplitude of 20 degrees. For the control, we observed the ScOR in complete darkness at the same frequency and amplitude. The Visual ScOR (VScOR) gain under the EF and HF conditions and the pursuit gain under the P condition were analyzed by the Steel-Dwass test, in which the significant level was 0.05.
Under the EF condition, visual stimuli enhanced ScOR gain. The gain enhancement was significantly different among both brightness levels and blurriness levels. Brighter and clearer stimulus tended to cause larger effect on ScOR. Under P condition, also the pursuit gain was significantly different among both brightness levels and blurriness levels. Under the HF condition, visual stimuli suppressed ScOR gain. The VScOR gain with brighter stimulus tended to be smaller. No significant difference in VScOR gain among blurriness levels, was indicating that even ambiguous position information could suppress eye movement. Under all conditions, with brighter target, there was no difference among blurriness levels, but with dark target, blurriness levels could affect the eye movement. These suggested that the effect on ScOR may be possible to estimate the amount of information in location perception throughout plural modalities. Ambiguous stimuli caused less effect on ScOR. This suggested that the effect on ScOR may indicate accuracy of perceived position.
This work is supported by JSPS KAKENHI Grant Number JP19K12088.
FP1043Feasibility of VestAid: A Tablet-based Technology for Objective Exercise Monitoring in Vestibular Rehabilitation
Brooke N. Klatt1, Pedram Hovareshti2, Lisa S. Holt2, Pamela M. Dunlap1, C Zalkin2, D Tolani2, Susan L. Whitney1,3
1Department of Physical Therapy, School of Health and Rehabilitation Sciences, University of Pittsburgh, Pittsburgh, PA, USA; 2Intelligent Automation, A BlueHalo Company., Rockville, MD, USA; 3Department of Otolaryngology, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
A low-cost home-exercise system called VestAid has been developed to assist participants in the performance of vestibulo-ocular reflex (VOR x1) gaze stabilization exercises outside of clinic visits. VestAid includes a tablet-based app for the participant and a web-based portal for the physical therapist that provides exercise accuracy and performance data. VestAid utilizes a computer tablet camera to assess gaze stabilization accuracy and head motion performance, records participant-imputed symptom data before and after each exercise, and provides clinicians with near real-time objective (head speed compliance, gaze stabilization accuracy) and subjective (symptoms and perceived difficulty) metrics of exercise performance.
The feasibility and acceptability of VestAid was assessed in a study of ten participants (mean age = 45, SD = 19, 6 females) with various vestibular diagnoses. All participants completed twelve 30-second horizontal VOR x1 exercises in a seated position. The exercises differed by variations in the background color, pattern, and movement. One of the exercises was repeated to assess the test-retest reliability of gaze stability accuracy and head motion compliance during the exercise. After completing an exercise, each participant rated the perceived difficulty of the exercise using a 0 to 10 scale (0 = extremely easy and 10 = extremely difficult). Participants were asked about their experience and completed usability surveys using eight qualitative open-ended questions and ten statements to which they indicated their agreement (strongly disagree, disagree, neutral, agree, or strongly agree).
Participants with vestibular disorders were able to complete the trials without adverse events. The responses from the usability survey demonstrate acceptability of the VestAid device evident by the favorable feedback provided. Nine out of ten participants agreed or strongly agreed that it was easy to rate the difficulty of exercises. The study team categorized the twelve VOR x1 exercises as either “easy” or “difficult” (six of each). The mean rating of the “easy” exercises across participants was 2.7/10, SD = 1.9. The mean rating for the “difficult” exercises across participants was 4.8/10, SD = 2.1. The consistency of the mean ratings of the participants with the exercise classifications (“easy” and “difficult”) by physical therapists suggests that the VestAid device has clinical utility. Gaze stabilization accuracy output had excellent reliability (r=0.98) and head motion compliance output had good reliability (r=0.82).
VestAid provides an objective way to monitor gaze stabilization exercise performance outside of the clinic and has the potential to motivate participants to complete their home exercise program.
FP1045Analysis of 25-OH Vitamin D in Persistent Benign Paroxysmal Positional Vertigo, an observational study
Alberto Codina-Aroca1, Darío Agudelo2, Santiago Díez2, Núria Mir2
1Hospital Clinic de Barcelona (Barcelona, Spain); 2Fundació Hospital de l’Esperit Sant (Santa Coloma de Gramenet, Spain)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Benign Paroxysmal Positional Vertigo (BPPV) is the most frequent type of vertigo and of special interest are those which don’t improve after several consecutive repositioning maneuvers. We included patients diagnosed with Benign Paroxysmal Positional Vertigo (BPPV) who didn’t improve after three canalith repositioning maneuvers (CRM) and performed blood tests which included 25-OH Vitamin D, Calcium, and Parathyrin (PTH). We found that all the patients that require a Canalith repositioning maneuver (CRM) in three consecutive weeks have low levels of vitamin D. We also started treatment to these patients with an improvement after the correction. Vitamin D deficit could cause a hyperlability state in otoconiae that could be responsible for a persistent BPPV that doesn’t improve with repositioning maneuvers.
FP1046Frequencies of Vestibular Syndromes, diagnosis and change of diagnosis rates in patients with Dizziness presenting to a tertiary Emergency Department
Georgios Mantokoudis1, Athanasia Korda1, Lukas Comolli1, Ewa Zamaro1, Franca Wagner2, Thomas Sauter3, Marco D. Caversaccio1
1Department of Otorhinolaryngology, Head and Neck Surgery, Inselspital, University Hospital Bern and University of Bern, Bern, Switzerland; 2Department of Diagnostic and Interventional Neuroradiology, Inselspital, University Hospital Bern and University of Bern, Bern, Switzerland; 3Department of Emergency Medicine, Inselspital, University Hospital Bern and University of Bern, Bern, Switzerland.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Our aim was to determine the frequency of vestibular syndromes, frequencies of diagnoses, diagnosis change rates, and resources used in patients with dizziness in a tertiary emergency department (ED) as well as in the follow-up examination.
Methods: In this retrospective longitudinal study, we included all adult patients presenting with dizziness in the ED from 07/2015 until 08/2020. Based on medical history we determined the type of vestibular syndrome. We collected data about baseline demographics, medical history, clinical findings, resources used, and diagnosis from the initial ED report and from the follow-up report if available.
Results: Overall, we included 1535 patients with dizziness. 429 of these 1535 patients (27,9%) had an acute vestibular syndrome (AVS), 35,0% an episodic vestibular syndrome (EVS), 4,8% a chronic vestibular syndrome (CVS), and 23,2% no vestibular syndrome. The three most frequent diagnosis were Stroke / minor Stroke (10.1%), BPPV (benign paroxysmal positional vertigo) (9,7%) and vestibular neuritis (9,6%). In patients with an AVS (30,3%) had a stroke. In 45% the cause of the dizziness remained unknown und 31.4% received a false diagnosis. In cases with a follow-up available, 58.2% of the initially unknown diagnoses received a diagnosis in the follow-up. In 29 cases (4,4%) a dangerous diagnose was missed at the ED. Overall, 69.9% of all 1535 dizzy patients received neuroimaging (MRI 58,2%, CT 11,6%) at the ED visit.
Conclusions: One third of dizzy patients in the ED present with AVS with a high prevelance of vestibular strokes. Episodic vertigo (EVS) was equally frequent, however, the rate of undiagnosed patients was high due to a symptom free interval at the time of ED presentation. The proportion of patients receiving neuroimanging was very high, however, almost half of them still remained without diagnosis and among those diagnosed were often misclassified. Many unclear cases of vertigo could be diagnostically clarified after a follow-up visit.
FP1052Clinical Characteristics in Unilateral Vestibular Atelectasis
Morgane Marc, Charlotte Hautefort, Jean Pierre Guichard, Philippe Herman, Emmanuel Houdart, Michel Toupet, Michael Eliezer
APHP, Université de Paris
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Unilateral vestibular atelectasis (UVA), an entity first described by Merchant and Schuknecht in 1988, has rarely been reported in vivo as of yet. We specify here the clinical characteristics of 22 patients diagnosed with UVA.
Materials and methods: Patients with a radiological diagnosis of UVA who underwent delayed inner ear MRI were included between April 2017 and January 2020. Full clinical testing including ocular infrared video-oculography, oVEMPs, cVEMPs, vHIT, bithermal caloric testing and auditory testing was performed.
Results: There were 13 men and 9 women, of mean age 58.6 ± 13.7 years. Onset was more frequently sudden (73%) than insidious (27%) though both clinical presentations were reported, and positional vertigo was described in 41% of cases. There were only two (9%) patients reporting Tullio’s phenomenon. Vestibular testing showed that in 90% of cases, there was utricular dysfunction on oVEMP, while in 77% of cases, saccular function was preserved on cVEMP. vHIT showed high-velocity canal function impairment in all 22 patients: 8 patients (36%) had one impaired canal, 5 (23%) had two and 9 (41%) had all three canals affected. Caloric tests found complete unilateral areflexia, in 65% of tested cases, and partial deficiency in 35% of cases. Nine patients (40%) displayed asymmetrical hearing.
Conclusion: We described in this study the various clinical presentations of a disease rarely reported in vivo, UVA. Initial clinical presentation can appear similar to an acute vestibular deficit, a recurrent positional vertigo, or fluctuating dizziness.
FP1053Electrophysiological and Inner Ear MRI findings in Patients with Bilateral Vestibulopathy
Michael Eliezer1, Charlotte Hautefort2, Christian Van Nechel3, Ulla Duquesne3, Jean Pierre Guichard1, Philippe Herman2, Romain Kania2, Emmanuel Houdart1, Arnaud Attyé4, Michel Toupet5
1Department of Neuroradiology and MR Unit, Lariboisière, Université de Paris. 2Department of Head and Neck Surgery, Lariboisière, Université de Paris. 3Clinique Des Vertiges, Brussel, Belgique. 4Department of Neuroradiology and MRI, SFR RMN Neurosciences, Grenoble Alpes University Hospital, Grenoble, France. 5Centre d’Explorations Fonctionnelles Otoneurologiques, Paris, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Purpose: Bilateral vestibulopathy (BV) is an uncommon disorder and the etiology remained idiopathic in most cases. Delayed 3D-FLAIR sequences have provided new insights into various inner ear diseases, allowing the evaluation of the endolymphatic space and the permeability of the blood-labyrinthine barrier (BLB). The aim of this study was to assess both the morphology of the endolymphatic space and the permeability of the BLB in patients with BV as evaluated by delayed 3D-FLAIR sequences.
Methods: In this retrospective study, we performed 3D-FLAIR sequences 4 h after administering contrast media to 42 patients with BV. Two radiologists independently evaluated the morphology of the endolymphatic space (either vestibular atelectasis or endolymphatic hydrops) and the permeability of the BLB.
Results: Morphologic anomalies of the endolymphatic space and vestibular blood-labyrinthine barrier impairment were observed in 59.6% of patients with BV. Bilateral vestibular atelectasis (VA) was found in 21 patients (50%), involving only the utricle and all three ampullas while the saccule was always observed with no sign of collapse: idiopathic BV (n = 19), aminoglycoside administration (n = 1) and few days following abdominal surgery (n = 1). One patient had bilateral vestibular malformation. BLB impairment was observed in five patients (11.9%): paraneoplastic (n = 1), lymphoma (n = 1), autoimmune (n = 1), and vestibular “neuritis” (n = 2). Seventeen patients (40.4%) had normal MRI with no endolymphatic space anomaly or BLB impairment.
Conclusion: Patients with BV presented with morphologic anomalies of the endolymphatic space or BLB impairment in 59.6% of patients.
FP1055Delayed onset of vertigo/dizziness in patients with posttraumatic perilymph fistula
Kazuhiko Kubo, Yuki Naritomi
Department of Otorhinolaryngology & Head and Neck Surgery, Chidoribashi General Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Perilymph fistula is a rupture of two windows of inner ear and is characterized by Meniere’s disease-like symptoms including vertigo/dizziness, hearing loss, tinnitus and ear fullness. Although it is well known that traffic accidents induce perilymph fistula, the onset of vertigo/dizziness is not necessarily the same as the day of traffic injury and then this mismatch often gets into trouble between those patients and insurance providers. Since there are posttraumatic patients with delayed onset of vertigo/dizziness in actuality, it is important to reveal characteristics of patients with delayed onset of vertigo/dizziness after traffic accident and to discuss the mechanism of this mismatch.
Methods: Retrospective electric records-based study was designed. The posttraumatic subjects with delayed onset of vertigo/dizziness were recruited from the lists of patients who underwent the surgical closure of perilymph fistula at the department of otorhinolaryngology & Head and Neck Surgery of Kyushu University Hospital from 2007 to 2018. We collected age, gender, symptoms, the day of onset of vertigo/dizziness, vestibular examination, audiogram, site of fistula, outcome etc. for descriptive statistics. This study was approved by our institutional ethics committee.
Results: Twelve patients were recruited and a half of patients complained vertigo/dizziness later. There were no association between the persistent vertigo/dizziness and many parameters including age, gender, symptoms, nystagmus, fistula phenomenon, hearing level and caloric response. The patients with persistent vertigo/dizziness tended to have abnormal vestibular evoked myogenic potential.
Conclusions: The onset of vertigo/dizziness after traffic accident was not related to medical parameters. We should know that posttraumatic onset of vertigo/dizziness delays not infrequently.
FP1056Characteristics of patients with vertigo/dizziness in emergency facility having an MRI device
Yuki Naritomi, Kazuhiko Kubo
1Department of Otorhinolaryngology & Head and Neck Surgery, Chidoribashi General Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Vertigo/dizziness are one of most common causes for calling the emergency services. The patients with emergent vertigo/dizziness are usually referred to emergency hospital. Up to now, many reports demonstrated the characteristics of emergent care of patients with vertigo/dizziness in emergent hospital. However, those have diversity among reports because there are many differences in the level of medical services and insurances among countries. The specificity of emergent care for patients with vertigo/dizziness is easy to take MRI imaging in most Japanese emergent hospitals. The diffusion-weighted MRI images have an ability of early detection of acute brain infarction. The aim of this study is to reveal characteristics of patients with vertigo/dizziness in in emergency facility having an MRI device.
Methods: Retrospective electric records-based study was designed. The subjects with vertigo/dizziness were recruited from the lists of patients whom an ambulance car took to the emergency unit at Chidoribashi General Hospital in the second half of 2019. We collected age, gender, diagnosis, MRI images, admission, duration of admission, outcome etc. for descriptive statistics. This study was approved by our institutional ethics committee.
Results: Many patients with acute vestibular syndrome were referred to our hospital using an ambulance car. Many of them underwent MRI scan to exclude acute brain infarction just after vital check, an examination of blood and electrocardiogram. As a result, many patients were diagnosed as peripheral vertigo and selected whether to be admitted to hospital.
Conclusions: Several methods for assessment of cerebral infarction without MRI, such as HINTS and ABCD2 score, were developed to evaluate whether the patients with vertigo/dizziness have an infarction in the brain or not. Early MRI imaging may bring a secure feeling to the patients with vertigo/dizziness and facilitate the following process of treatment.
FP1063The Impact of Muscle Mass in the Body Balance of Morbidly Obese
Camila Brock, João Grossi, Bruno Hochhegger Camila Martins Brock1, João Vicente Machado Grossi2, Bruno Hochhegger3
Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, Rio Grande do Sul, Brazil
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Abstract:
Background: The decrease of muscle mass in obesity is linked to body instability. However, the pathway of this correlation is not fully understood.
Objective: To study the relationship between body balance and muscle mass in morbidly obese patients.
Methods: 40 subjects, 6 men, (average age 38,03 ± 10,63) enrolled the study. 20 obese with body mass index 3 35 kg/m2 and 20 non morbidly obese were submitted to body balance assessment with portable posturography equipment (BAP - Balance Angular Posturography). The stability limits were measured and the Sway per minute (Sway/m) obtained in the X and Y axis under 4 different conditions, combining opened eyes, closed eyes, firm platform and unstable platform. Data were related to the measurement of cervical, waist and hip circumference in centimeters (cm) and to the percentage of fat and muscle mass of the lower limbs and trunk by bioimpedanciometry (Beurer).
Results: The data were analysed by SPSS using the t-test. The Sway/m on the X axis in the condition opened eyes and firm platform was higher in the morbidly obese group (p = 0,006). In the condition closed eyes and unstable platform, the value of Sway/m on the X axis (p = 0,006) and on the Y axis (p = 0,014) was also higher in the obese group. There was significant difference in cervical circumference (p = 0,007), waist (p = 0,001), hip (p < 0,001), percentage of muscle mass per lower limb (left leg and right leg p < 0,001) and trunk (p = < 0,001). The oscillatory area of the stability limits did not show statistical result (p = 0,483).
Conclusion: Body balance initially prioritizes muscle activation around the ankle joint. When challenged by the lack of visual fixation and/or the proprioception, the perception of the proximal body is recruited to contain the tendency to increase instability. The decrease in the percentage of muscle mass in morbidly obese individuals alters the body balance, reducing the capacity for postural control.
FP1064The DizzyQuest: an app-based diary for vestibular disorders
E.C. Martin1, C. Leue2, P. Delespaul2, F. Peeters3, A. Erdkamp4, S.C.F. van de Weijer4, L. de Joode1, D. Sitters1, R. Verkaik1, H. Blom5, T. Bruintjes6, A. Zwergal7, E. Grill8, N. Guinand9, M.R. van de Berg1, J.J.A. Stultiens1, H. Kingma1,10, R. van de Berg1,10
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Maastricht, The Netherlands; 2Department of Psychiatry and Neuropsychology, School for Mental Health and Neuroscience, Maastricht University Medical Center, Maastricht, The Netherlands; 3Department of Clinical Psychological Science, Faculty of Psychology and Neuroscience, Maastricht University, Maastricht, The Netherlands; 4Department of Psychiatry and Psychology, Maastricht University Medical Center, Maastricht, The Netherlands; 5Department of Otolaryngology - Head and Neck Surgery, HagaZiekenhuis, the Hague, The Netherlands; 6Apeldoorns duizeligheidscentrum, Gelre ziekenhuizen, Apeldoorn, The Netherlands; 7Department of Neurology, Ludwig-Maximilians-University of Munich, Munich, Germany; 8Department of Medical Informatics, Ludwig-Maximilians-University of Munich, Munich, Germany; 9Service of Otorhinolaryngology - Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 10Faculty of Physics, Tomsk State Research University, Tomsk, Russia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Currently used questionnaires for vestibular disorders are mainly retrospective, inducing recall bias and decreasing ecological validity. To overcome these problems, the DIZZYNET network recently introduced an app-based diary for vestibular disorders: The DizzyQuest. It investigates vestibular symptoms in their psychosocial context within the same person, using multiple daily questionnaires. Hereby, fluctuating symptoms (like in Meniere’s disease) can be captured more reliably. Study objectives were to investigate: 1) response rates; 2) convergent validity; 3) the agreement between reported vertigo attacks in the evening- and attack-questionnaire; and 4) the relation between self-reported hearing symptoms and objective hearing thresholds.
Methods: Seventy-nine patients were included to use the DizzyQuest for one month. For each research question, a different subset of this eighty patients was used for analysis, based on the inclusion criteria. In the first week, the questionnaires were administered at different frequencies: morning- (1x), day- (10x), evening- (1x), attack-questionnaire (to be filled in directly after a vertigo attack). In week two to four, the evening- and attack-questionnaire remained to be filled in at the same frequency. Response rates were measured by dividing the amount of completed questionnaires by the amount of administered questionnaires. Convergent validity was investigated by comparing twelve questions of the DizzyQuest with ten corresponding questions from the Dizziness Handicap Inventory, Hospital Anxiety and Depression Scale and EuroQol-5D-5L. Vertigo attack symptoms of the evening-questionnaire were compared to the symptoms that were reported in the attack-questionnaire. Self-reported hearing symptoms were compared to hearing thresholds obtained with an iPad-based hearing test, that was directly administered after completing the DizzyQuest evening-questionnaire.
Preliminary results: Average response rates varied from around 70% (day-questionnaire) to >90% (evening-questionnaire). Regarding convergent validity, significant correlations (4 strong, 4 moderate, 1 weak) were found in 9 out of 10 investigated combinations of questions. A discrepancy was found between reported symptoms in the evening-questionnaire versus the attack-questionnaire regarding nature and frequency (749 versus 199 reported vertigo attacks respectively) of vertigo attacks. Self-reported hearing symptoms significantly correlated with hearing thresholds on an intrapersonal level, but not on an interpersonal level.
Conclusion: The DizzyQuest seems a promising tool for investigating vestibular symptoms and their psychosocial context, with low recall bias and high ecological validity. It shows desired response rates, an acceptable convergent validity and self-reported hearing symptoms correlate well on an individual level with objective measures. To investigate vertigo-attacks, the combination of an evening-questionnaire and attack-questionnaire seems complementary to capture vertigo attacks reliably, but needs further investigation.
FP1066Preliminary Study on the Effectiveness of the Geneva Balance Test (GBT) on Children with Bilateral Vestibulopathy
Emile G. Monin, Céline Bahim, Maurizio Ranieri, Jean-François Cugnot, Nils Guinand, Angélica Pérez Fornos, & Hélène Cao Van
Hôpitaux Universitaires de Genève
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Vestibular deficits are considered to be rare in children, but the lack of systematic screening leads to underdiagnosis. The few studies made on this topic have demonstrated that chronic vestibular dysfunction impacts psychomotor development of children. Early screening of these children is needed to allow optimal follow-up, ensuring better global development. To this purpose, we have developed a screening test to quantify the balance capacity of children over a broad age range, the Geneva Balance Test (GBT).
Methods: The aim of the study was to determine the possibility of quantifying balance deficits in children with bilateral vestibulopathy (BV) using the GBT. We conducted an observational prospective study in a population of 11 children with BV. Two age-matched control groups were included in the study, composed of (1) 15 healthy children without vestibular nor auditory disorder (HS) and (2) 11 pediatric cochlear implant recipients (CI) without vestibular disorders (since sensorineural deafness is frequent in children with BV). Results of the three populations have been compared in 3 age groups (3-5 years, 6-9 years, =10 years), and with results of the Bruininks-Oseretsky Test of Motor Proficiency Ed. 2 (BOT-2).
Results: Statistical analyses demonstrated significant differences in the GBT scores between 3-5 and =10 years children with BV and both control populations. A similar tendency was observed in the 6-9 years group, but results did not reach significance for this smaller group. Children in the 3-5 years CI group showed intermediate balance capacities (worse than HS but better than BV), that normalize in the 6-9 years group. All the results of the GBT were significantly correlated with BOT-2 results, but the GBT was better tolerated in all populations.
Conclusions: In this small study, the GBT allowed to quantify balance deficits in children with BV. These results were comparable with the results of the BOT-2, which has been validated by multiple studies. However, the BOT-2 test is not validated for children <4,5 years, and results quickly saturate reaching maximal values already at 6-9 years. The GBT showed potential to be a useful tool to monitor the development of balance capacities with age and as such could be used in the follow-up of children with BV. Interestingly, we observed a significant difference in balance capacities in very young CI children which normalized by 6-9 years, potentially due to hearing rehabilitation with CI. A study with a larger population is necessary to confirm these results.
FP1068Altered hippocampal functional connectivity in persistentpostural perceptual dizziness
He Zhao1, Xiaozhen Li2, Zheng-guang Chen2, Li-qun Zhong1
1Department of Neurology, Dongzhimen Hospital, Beijing University of Chinese Medicine,5 Hai Yun Cang Hutong, Beijing, 100700, PR China; 2Department of Radiology, Dongzhimen Hospital, Beijing University of Chinese Medicine, 5 Hai Yun Cang Hutong, Beijing, 100700, PR China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Persistent postural perceptual dizziness (PPPD) is a vestibular disorder of persistent dizziness and unsteadiness. Many studies demonstrate the importance of vestibular–hippocampal interactions for hippocampal function and indicated the hippocampus might be important for compensation of vestibular function. Resting-state functional magnetic resonance imaging (rs-fMRI) has been widely used in brain function studies. However, hippocampal functional connectivity using rs-fMRI in patients with PPPD has not been reported.
Methods: A total of 30 subjects, including 14 patients with PPPD and 16 healthy controls underwent rs-fMRI on a 3T MR scanner. After the imaging preprocessing, seed-based functional connectivity analysis was performed on the bilateral hippocampus using AFNI software. The independent sample t test was used to compare the differences between two groups of hippocampal functional connectivity with age and sex as covariates.
Results: PPPD showed significantly increased hippocampal functional connectivity in the right lingual gyrus, left cuneus, right precuneus and right cerebellum adjusted for age and sex. We also found decreased connectivity in the left inferior parietal lobule, left medial frontal gyrus, left putamen and left precentral gyrus.
Conclusion: The hippocampal functional activities in PPPD patients were altered, potentially leading to abnormal integration of visual and vestibular information. Patients with PPPD showed the regions with increased connectivity linking visual spatial processing, while reduced connectivity among the areas involved in multisensory vestibular processing and body movement. Hippocampal functional connectivity patterns may become an imaging biomarker of PPPD and helpful for early diagnosis.
Keywords: Persistent postural-perceptual dizziness (PPPD); Resting state functional magnetic resonance imaging (rs-fMRI); Functional connectivity; Hippocampus
Key points: *The hippocampus may be important for compensation of vestibular function in patients with PPPD.
*This study investigated the hippocampal functional connectivity changes using rs-fMRI in PPPD.
*Hippocampal functional connectivity patterns may become an imaging biomarker of PPPD and helpful for early diagnosis.
Target Audience: Neurologist and others
FP1069Discrepancy between the video head impulse and bithermal caloric tests; prevalence, etiology and localization in dizzy patients
Ju-Young Lee, MD1, Eunjin Kwon, MD2, Hyo-Jung Kim, PhD3, Jeong-Yoon Choi, MD, PhD4, Hui Jong Oh, MD, PhD5, Ja-Won Koo, MD, PhD6, Ji-Soo Kim, MD, PhD4
1Department of Neurology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Republic of Korea; 2Department of Neurology, Chungnam National University Hospital, Daejeon, South Korea; 3Research Administration Team, Seoul National University Bundang Hospital, Seongnam, South Korea; 4Dizziness center, Clinical Neuroscience Center, and Departmemt of Neurology, Seoul National University Bundang Hospital, Seongnam, South Korea; 5The MTV (Migraine, Tinnitus, and Vertigo) Clinic, Oh Neurology Center, Daegu, South Korea; 6Dizziness center, Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, South Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: This study investigated the prevalence, pattern, lesion location, and etiology of discrepancy in the results of caloric test and video head impulse test (vHIT) in patients with vestibular symptoms from diverse etiologies and disease duration.
Methods: We reviewed the results of vHIT and caloric test in 893 consecutive patients who had taken both tests within 10 days from March 2016 to May 2018.
Results: The discrepancy between the tests was found in 162 (18.1%) patients. Among them, 123 (75.9%) revealed abnormal caloric tests with normal vHIT (abnormal caloric test group). In this group, most patients (118/123) had unilateral canal paresis and 5 had bilateral canal paresis. Regarding lesion location, 105 (85.4%) patients had etiologies belonged to the peripheral pathology, such as Meniere’s disease (62/105, 59%) and vestibular neuritis/labyrinthitis (29/105, 27.6%). 18 (14.6%) showed central pathology in diverse etiologies. Meanwhile, abnormal vHIT and normal caloric response (abnormal vHIT group) was observed in 39 (24.1%), in which patients with bilaterally positive vHIT was observed in 18, unilaterally positive in 19, and hyperactive in 2. These patients showed a similar distribution of the central (n=19) and peripheral (n=20) lesions. Vestibular neuritis/labyrinthitis (7/20, 35%) and Meniere’s disease (7/20, 35%) were evenly included in the peripheral lesions, while the etiology of the central lesions varied.
Conclusion: The discrepancy between vHIT and bithermal caloric tests is not uncommon. The abnormal caloric test groups mostly had peripheral disease while the abnormal vHIT group had a substantial chance for central lesions.
FP1070Therapeutic Efficacy of Botulinum Toxin Type A in Patients with Vestibular Migraine: Changes in Resting-State Functional Connectivity in a Longitudinal fMRI Study
Sun-Young Oh, MD, PhD1,2, Jin-Ju Kang, MD1,2, Sohui Kim3, Jong-Min Lee, PhD4, Ji Soo Kim, MD, PhD5,6; Marianne Dieterich, MD, PhD7-9
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, Korea; 2Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, Korea; 3Department of Electronic Engineering, Hanyang University, Seoul, Korea; 4Department of Biomedical Engineering, Hanyang University, Seoul, Korea; 5Department of Neurology, Seoul National University College of Medicine, Seoul, Korea; 6Department of Neurology, Dizziness Center, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea; 7Department of Neurology, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 8German Center for Vertigo and Balance Disorders, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 9Munich Cluster for Systems Neurology (SyNergy), Munich, Germany a: These three authors contributed equally to this work as first authors. b: These two authors contributed equally to this work as corresponding authors
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Vestibular migraine (VM) has been recognized as a distinct clinical entity with recently published diagnostic criteria. Although migraine prophylactic medications can improve headache profiles and dizziness symptoms, treatment trials that focus on VM are scarce. Botulinum toxin type A (BTX-A) has been approved for prophylactic treatment of chronic and episodic migraine; however, its efficacy for migraine-related dizziness or VM has not been validated. The purpose of this study was to investigate the efficacy of BTX-A in prophylactic treatment of VM and to determine whether this treatment modulates intrinsic functional brain network connectivity.
Methods: Twenty patients (mean age 45.4 years, range 20–69 years) who satisfied the Bárány Society and International Headache Society diagnostic criteria for VM and who were refractory to conventional prophylactic therapies for more than five months had BTX-A injection and resting-state fMRI (rs-fMRI) before and 2 months after the injection. We measured the changes in the frequency of vertigo and migraine attacks, symptomatic functional disability scores, and neuropsychiatric inventories before and after the treatments.
Results: After BTX-A injection, the mean monthly frequencies of migraine and vertigo episodes decreased significantly compared to baseline (p<0.01, Wilcoxon signed rank test). The headache impact, as measured by the Headache Impact Test-6 score and the Migraine Disability Assessment, was improved (p<0.001). The vertigo parameters, measured by the Dizziness Handicap Inventory and the Vertigo Symptom Scale, showed an improvement (p<0.001), as did the anxiety and depression scores (p<0.001) 2 months after BTX-A treatment. The low-frequency fluctuation analysis of the rs-fMRI data found significant changes in functional connectivity of the right superior temporal gyrus (STG). Adoption of the right STG cluster as the seed region, increased functional connectivity with the left post-central gyrus, right supramarginal gyrus, and right middle temporal gyrus was seen after BTX-A treatment.
Conclusion: This prospective study shows that BTX-A treatment is effective at ameliorating migraine headache and vertigo symptoms in VM patients who were refractory to conventional medical therapies. Along with symptomatic improvements, changes in the functional connectivity within the multisensory vestibular and pain networks in the right temporal regions suggest that abnormal brain activity leads to dysmodulation of multimodal sensory integration and abnormal cortical processing of the vestibular and pain signals in VM patients.
FP1071Fatigability Presenting with Video-oculographic findings in Myasthenia gravis
Jin-Ju Kang, MD1, Eunsu Lee, MD1, Sun-Young Oh, MD, PhD1,2
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, Korea; 2Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Myasthenia gravis (MG) is an autoimmune disease caused by abnormal transmission of neuromuscular junction, and it is characterized by diplopia, ptosis, ophthalmoplegia and muscle weakness. And it features fatigability that means fluctuating symptoms and worsen due to muscle movement. In the early stage, the patients complain of eye symptoms, 46% of patients are not adequately diagnosed during the first year of illness. Ancillary test such as antibody assays, edrophonium test, and electrophysiologic test including repetitive nerve stimulation test, and single fiber EMG. However, gold standard of diagnosis is not defined until now. We therefore analyzed eye movement findings in myasthenia gravis using video-oculography.
Methods: We performed a total of 46 MG patients and 24 controls. All MG patients complained of ocular symptoms such as ptosis and diplopia. Patients who were positive for one or more of the repetitive stimulation test, edrophonium test, and acetylcholine receptor antibody test were selected. Video-oculography was performed the range of 20 degree was measured for 6 minutes to measure rapid eye movement, and 20 degree range for 6 minutes to measure slow eye movement.
Results: 50 repetitive saccades and smooth pursuit movements of both eyes (more and less affected eye) tested in both vertical and horizontal planes allowed for effective differentiation between MG patients and healthy subjects. Repetitive vertical saccadic eye movements yielded the best differentiation between patients with MG and controls with a sensitivity of 73% and a specificity of 92% when using a gain decrement of 9.3% as cutoff.
Conclusions: Eye movements are caused by using different rates of twitch fiber and tonic fiber. If tonic fibers are mainly involved in myasthenia gravis, smooth pursuit movement can be impaired. Therefore, quantitative analysis of the slow eye movement as well as rapid eye movement in patient with MG who is showed fatigability, can be helpful in early diagnosis and understanding pathology of MG.
FP1077The Factors of the Compliance to the Customized Vestibular Exercise
Eun-Ju Jeon, Hyun Jin Lee
The Catholic University of Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Vestibular rehabilitation is one of the essential parts in the treatment of dizziness. Customized vestibular exercise is considered superior to generic exercise. However, it is hard to approach since it varies on the individual patient’s functional status and therapist’s knowledge and experience.
Since the customized vestibular exercise (CVE) was initiated in this clinic in April, 2017, 89 patients were undergone the customized exercise treatment for control of dizziness and unsteadiness. The formal CVE schedule was consisted of 4 sessions of 30 minute of supervised exercise at weekly base. After supervised exercise for 30 minutes in the clinic, home exercise 3 times/day was prescribed. If multiple session treatments were not possible due to personal circumstances, such as a remote location, work-related reasons, or cost burden, single session treatment was performed.
The prediction of non-adherence to a CVE treatment, prior to initiation of the treatment, would allow optimization of health resources. We tried to find what factors determine the compliance to the CVE.
62 patients agreed to proceed with formal 4 sessions of CVE. Vestibular neuritis was the most common etiology. Unilateral vestibular hypofunction, acoustic neuroma, BPPV, Meniere’s disease, etc. followed as common etiology for CVE treatment. Three patients abandoned the treatment at the beginning. One patient discontinued the treatment after one session. 32 patients (51.6%) completed the 4 sessions of CVE. In terms of disease category, VM and labyrinthits showed 100% of adherence.
The patients were divided into 2 groups: Adherence group (group A) was defined as who completed 3 to 4 sessions. Non-adherence group (group NA) was who performed 0~2 sessions of CVE. Group A showed less fall number (2.4±2.8) at sensory organization test (SOT) than group NA (4.5±4.1), and it was statistically significant (P=0.026). Age, sex, dizziness related questionnaire score, VFT parameters except for fall number at SOT were not significantly different between the two groups. The patients most likely to abandon a CVE program are who showed multiple falls (>4.5) at SOT. It seems that the subjective perception of instability limitations does not affect motivation for vestibular rehabilitation. It is necessary to pay special attention to the patients with multiple falls, and have regular follow-up appointments to encourage adherence.
FP1078Variability and efficacy of prophylactic treatment in patients with Probable and Definite Menière’s Disease
Iveta Csekesova1, Lukas Varga2, Agnesa Nagy Potasch2
1Center for Vestibular Disorders, Komarno Agel Hospital, Komarno, Slovakia; 2Department of Otorhinolaryngology – Head and Neck Surgery, Faculty of Medicine and University Hospital, Comenius University, Bratislava, Slovakia; 3Center for Vestibular Disorders, Komarno Agel Hospital, Komarno, Slovakia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Menière’s Disease is a chronic inner ear disorder, common cause of hearing and balance impairment, which may have long-term negative impact on patient’s quality of life. At the present time, there is no causal cure, but there are always ways to manage the condition and help control the symptoms. The aim of our study was to investigate and define effective prophylactic treatment in patients with Probable or Definite Menière’s Disease, particularly focused on vertigo and achieving at least 6 months of attack-free interval or only sporadic seizures.
Methods: Single-center retrospective study on 237 patients with Probable or Definite Menière’s Disease who were diagnosed and treated from 2019 to 2020. Prophylactic treatment usually started with single administered drug containing Betahistine. Hydrochlorothiazide was used as an option in case of reported allergy or intolerance. Sufficiency of disease control was assessed on the regular visits after the 1st, 3rd, 6th and 12th months of treatment. It was based on patient’s self-reported data with no or only sporadic /1-2/ episodes of vertigo during the previous 6 months. According to variable response, other drugs (Hydrochlorothiazide, Cinnarizine, Prednisolone or Carbamazepine) were also included. The treatment was considered insufficient if there was no improvement after 1 month, or less than 50% reduction of vertigo seizures after 3 months. In case of pharmacoresistance lasting for 6 months, intratympanic Gentamicin was administered to the affected ear. All patients were advised to keep specific dietary restrictions. Dizzines Handicap Inventory was used to evaluate subjective efficiency of the treatment.
Results & Conclusions: In our study group 64,13% of patients met the ICVD criteria for Probable and 35,86% for Definite Menière’s Disease. We found that 30,8% achieved satisfactory reduction of vertigo attacks by treatment with single administered drug, 52,32% on combination of 2 and 12,23% on 3 prescribed drugs, whereas 4,64% were considered as pharmacoresistant. We observed variable response to the administered drugs, which cannot be exactly predicted on first examination. This can be explained by various factors such as heterogenity of the study group, variable activity of the disease, predominant symptoms, vestibular or other comorbidity, or other medication. Different lifestyle and daily stress level is also assumed to affect the clinical picture, but according to DHI all of the patients reported improvement.
In conclusion we suggest that by thorough investigation, regular follow-ups and adjusting the therapeutic strategy a satisfactory disease control may be achieved within a year in the vast majority of the cases.
FP1083Endoscopic Transcanal Labyrinthectomy for Intractable Meniere’s Disease: An Alternative to Transmastoid Labyrinthectomy?
Se A Lee, Jong Dae Lee
Department of Otorhinolaryngology/Soonchunhyang University Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: To describe a novel approach for intractable Meniere’s disease exclusively through a transcanal endoscopic ear surgery (TEES) approach.
Patient: A 56-year-old male with intractable Meniere’s disease despite conservative treatment and chemical labyrinthectomy.
Interventions: Transcanal endoscopic labyrinthectomy.
Main Outcome Measure: Subjective vertigo control, surgical morbidity.
Results: The TEES approach provided a wide exposure of the oval window. This facilitated removal of stapes crura and footplate. After widening of the oval window, the perilymph was suctioned, and gentamicin was injected through the oval window. The oval window was obliterated using the perichondrium of the tragal cartilage and fibrin glue. After 2 years of follow-up, there was no recurrence of vertigo.
Conclusions: As a compelling alternative to the transmastoid approach, we propose endoscopic labyrinthectomy as an option for patients with intractable MD without functional hearing who have failed chemical labyrinthectomy.
FP1084Differential Involvement of Lateral Semicircular Canal and Otolith Organs in Common Vestibular Disorders
Yehree Kim1, Byung Chul Kang2, Myung Hoon Yoo3 and Hong Ju Park1
1Department of Otorhinolaryngology-Head and Neck Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea;2Department of Otorhinolaryngology-Head and Neck Surgery, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, South Korea; 3Department of Otorhinolaryngology-Head and Neck Surgery, School of Medicine, Kyungpook National University, Daegu, South Korea
Abstract
Semicircular canal and otolith functions came to be evaluated recently, but comprehensive and comparative analysis of canal and otolith dysfunction in common vestibular disorders is lacking. We aimed to analyze the abnormal rates of canal and otolith function in common vestibular disorders. We enrolled 302 patients who were managed for 2 months in a dizziness clinic. Results of caloric, video head impulse test (vHIT), and cervical and ocular vestibular evoked myogenic potential (cVEMP and oVEMP) tests were analyzed and compared among various diagnoses. Vestibular disorders diagnosed included recurrent vestibulopathy (RV, 27%), vestibular migraine (VM, 21%), benign paroxysmal positional vertigo (BPPV, 17%), Meniere’s disease (MD, 11%), vestibular neuritis (VN, 10%), orthostatic dizziness (7%), and central lesions (3%). Lateral canal dysfunction was found most in VN (100%) and less commonly in definite MD (75%), RV (46%) and definite VM (29%). Abnormal caloric results were more common than abnormal vHIT in all disorders. Otolith dysfunction was found more frequently than lateral canal dysfunction in most vestibular disorders except VN. An abnormal cVEMP was more frequent in definite MD than the other disorders. Isolated otolith dysfunction without lateral canal dysfunction was the most found in BPPV, followed by definite VM, RV, and definite MD in decreasing order. Various patterns of involvement in canal and otoliths were revealed in vestibular disorders, suggesting different pathogenesis.
FP1085Vascular Episodic Dizziness or Vertigo: clinical, diagnostic and therapeutic considerations
Arlindo C. Lima Neto, Roseli S. M. Bittar
Department of Neurotology, Hospital das Clínicas FMUSP, São Paulo, BR.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Dizziness or vertigo can be the only symptom of posterior circulation (PC) ischemia. In July/2021 the Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack - AHA/ASA shed light on the treatment of these ischemic conditions. The current study aims to describe symptoms, diagnosis, MRI results and PC blood flow tests (PCBFT) findings (magnetic resonance angiography, computed tomographic angiography and/or transcranial Doppler ultrasound). Dizziness remission and association with test results were evaluated.
Methods: A longitudinal case series of the outpatient Neurotology HC-FMUSP, Brazil was treated from July to October/2021. Subjects with episodic dizziness or vertigo associated to visual darkening, syncope, paresthesia, balance-related fall and/or dysphagia were selected. Patients with non-vascular etiology were excluded. Participants were submitted to anamnesis, bedside tests (including HINTS), MRI, PCBFT. The impact of 3-week-antithrombotic therapy on dizziness was assessed using a visual analogue scale (VAS).
Results: Eight patients (3 males and 5 females), 70,25 +/- 9,27 years old were included. The most frequently observed symptoms were syncope (4/50%) and visual darkening (3/37%). Two subjects (25%) had ischemic signs on MRI and 4 patients (50%) had obstructive findings on PCBFT. Final diagnosis: cerebellar stroke (1/12%), cardioembolic stroke (1/12%), isolated labyrinthine ischemia (1/12%) and TIA (5-62%, one of them due to vertebral artery dissection). After treatment, 6 patients (75%) reported dizziness improvement above 70%, while 2 (25%) reported improvement of 30-50%. No correlation was detected between intensity of symptoms, diagnosis of stroke, PCBFT results or VAS response.
Conclusion: Syncope and visual darkening have been the most frequently symptoms associated with vascular dizziness or vertigo. The most common diagnosis was TIA, but stroke and isolated labyrinthine ischemia were also identified. Half of participants presented PC flow obstruction. Most of them had significant improvement in dizziness or vertigo with antithrombotic therapy. No correlation was detected between intensity of symptoms, diagnosis of stroke, PCBFT results nor treatment response. In the absence of contraindications, early antithrombotic therapy should be considered in patients with vascular dizziness or vertigo.
FP1086Head and Postural Sway Dynamics during a Virtual Reality Dual-Task Standing Paradigm in People with Persistent postural-perceptual dizziness vs. Healthy Controls
Anat V. Lubetzky1, Moshe M.H. Aharoni2, Liraz Arie1, Tal Krasovsky2,3
1Department of Physical Therapy, Steinhardt School of Culture Education and Human Development, New York University, New York, NY, USA; 2Department of Physical Therapy, University of Haifa, Haifa, Israel; 3Pediatric Rehabilitation Department, Sheba Medical Center, Ramat Gan, Israel
Background: Persistent postural-perceptual dizziness (PPPD) is characterized by chronic dizziness and imbalance exacerbated by visual load with normal laboratory testing. Identifying mechanisms of instability in PPPD could drive development of clinical balance assessments and effective rehabilitation programs. This study aimed to evaluate movement strategies in patients with PPPD in complex visual environments under challenging balance and cognitive conditions as compared with healthy adults.
Methods: We tested 22 patients with PPPD diagnosed according to the ICD-11/Bárány Society diagnostic criteria (mean age 32 [21,66], 10 women) and 20 controls (mean age 39, [21,66], 12 women). Participants stood in tandem position (heel-to-toes), wearing the HTC Vive and observing a 3-wall display of stars. The display was either static or moving in the anterior-posterior direction at 0.2 Hz and 5mm amplitude (AP5) or at 0.2 Hz and 32 mm amplitude (AP32). All scenes repeated 4 times in a randomized order: twice with a secondary cognitive task (serial subtraction by 3) and twice without. Anterior-posterior (AP) and medio-lateral (ML) postural sway (center-of-pressure, COP) and head kinematics (from the headset) were recorded. A repeated measures Analysis of Variance assessed main effect of visual (Static, AP5, AP32), task (single, dual) and group (PPPD, control) on directional path and acceleration.
Results: Controls significantly increased all COP and head parameters with the cognitive task whereas PPPD increased only COP ML path and acceleration. Only controls significantly increased head anterior-posterior & medio-lateral acceleration with moving visual load. Cognitive task performance was similar between groups. Between-group comparison showed that the groups were different on the least complex scenes only: the PPPD group was significantly higher (P<0.05) on all head outcome measures for the static single-task scene, and on all outcome measures but ML head acceleration on the AP5 single-task scene.
Conclusion: Balance responses to cognitive and visual load varied between people with PPPD and controls such that controls demonstrated increased movement with increased task difficulty and the PPPD group did not. These altered postural strategies were particularly observed around the head segment. Head-mounted displays thus appear to provide adequate input and output to study postural responses in people with PPPD. Future studies should examine the mechanism underlying altered movement strategies in response to cognitive and visual load in individuals with PPPD and whether reduced head degrees of freedom is adopted to avoid symptom exacerbation.
FP1087Vibration-Induced nystagmus evaluation in a population wtih long-term vestibular neuritis
Marta Chaure-Cordero, Eduardo Martín-Sanz, Jonathan Esteban-Sánchez
Hospital Universitario de Getafe
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Vestibular neuritis (VN) is a clinical entity characterized by acute, prolonged vertigo, constituting one of the most frequent peripheral acute vestibular disorders. The restoration of vestibular function is key on patients suffering this entity and depends on vestibular compensation: restoration, adaptation, and habituation. Skull vibration-induced nystagmus (SVIN) is an easy and replicable tool used to detect minimal vestibular asymmetries. Stimulus at 100Hz activates the vestibular receptors and produces a nystagmus, lacking adaptation. Once the stimulation is over, the nystagmus disappears.
The aim of this project is to study the ocular response after vibration stimulation, its influence, and the mechanisms of vestibular compensation in a population with VN.
Methods: We present a longitudinal cross-sectional study of 40 patients affected with VN of more than 6 month-course diagnosed between January-2017 and July-2019. The population was diagnosed with VN after a congruent clinical history and caloric tests, v-HIT and VEMPs performed. Every patient was put through a new v-HIT of every semicircular canal and a videonystagmography while applying a vibration stimulus at 30, 60 and 100Hz between December-2020 and February-2021. Patients were categorized in three groups depending on restoration of the gain of the vestibulo-ocular reflex, comparing results of v-HIT at diagnosis and time after the beginning of the symptoms.
Results: The group’s median age was 54.63 years, and 60% had their right ear affected . Median time of follow-up was 1,558 days. The median gain on the affected ear after the acute phase of the VN was 0.82 on the horizontal semicircular canal (HSC), 0.84 on the posterior semicircular canal and 0.85 on the SSC. 50% of our patients presented SVIN at 100Hz on the mastoid of the affected ear with a median slow-phase eye velocity of nystagmus of 7.3°/s. In addition, 57.5% presented VIN on the contralateral mastoid at 7.04°/s when stimulating at 100Hz. Patients without restoration showed a more intense VIN than the ones that restored (p<0.05). Besides, significant correlation was shown between the function of the HSC and the nystagmus’ speed. Frequency of VIN was significantly higher in patients in which, despite the long-evolution of VN, still showed overt saccades with an odds ratio of 8.
Conclussion: VIN is an adequate tool to analyze vestibular asymmetries. Its presence seems independent of the mechanisms of vestibular compensation if restoration is not achieved.
FP1095Vestibular functions of adolescents with idiopathic scoliosis: A comprehensive assessment and comparative study
Klára Kucerová1, Zuzana Balatková2, Kryštof Slabý1, Ondrej Cakrt1
1Department of Rehabilitation and Sports Medicine, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital; 2Department of Otorhinolaryngology and Head and Neck Surgery, 1st Faculty of Medicine, Charles University in Prague and Motol University Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: Idiopathic scoliosis (IS) is characterized by a three-dimensional deformity of the spine with unknown etiopathogenesis. There is evidence that IS may be associated with abnormalities of the vestibular system. Therefore, the purpose of this study was to evaluate vestibular function in adolescents with IS.
Methods: We examined 20 patients with IS and 20 healthy controls. The examination involved assessment of the perception of subjective visual vertical (SVV) in static and dynamic conditions, posturography (six conditions: eyes open/closed, firm/foam surface, tandem stand), and vestibular evoked myogenic potential (VEMP) testing. Results of the tests were compared between the groups.
Results: In SVV, there was no significant difference in static conditions. However, in dynamic conditions, the deviation was significantly greater in patients than in controls (p < 0.05). Posturography parameters of patients were significantly greater (p < 0.05) when standing on a foam surface with eyes open. In this condition, patients had greater center of foot pressure sway area and sway velocity. The patients and controls also differed in terms of sway path, sway velocity, and maximal amplitude in the medial-lateral direction. In VEMP testing, 38% of patients with IS had an abnormal response.
Conclusions: This study provides a comprehensive assessment of vestibular abnormalities in patients with IS. We found greater variations in dynamic SVV, greater values of posturography parameters, and some abnormal VEMP responses in patients with IS. Further studies are needed to find out if vestibular rehabilitation can improve these abnormal functions.
FP1097Evaluation of a New Web-based, Mobile Intervention for Improving Balance Disorders Among Elderly in Residential Home Care: A Prospective Study
Oz Zur1,2, Hadas Ben-Rubi Shimron1, Lisa Deutsch3, Eli Carmeli4
1The Israeli Center for Dizziness and Balance Disorders, Raanana, Israel; 2Department of Physical Therapy, Ben Gurion University of the Negev, Beer Sheva, Israel; 3BioStats Statistical Consulting, Ltd., Maccabim, Israel; 4Department of Physical Therapy, University of Haifa, Haifa, Israel
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Falls are common among the elderly and sensory integration training can decrease that risk. As people become homebound for many reasons, Tele-medicine and Tele-training have become essential alternatives. This study evaluated the efficacy of the Bbalance application (app), a new web-based, mobile balance rehabilitation program, in improving balance scores, increasing self-confidence and decreasing anxiety. Methods: Forty-one residents of an assisted-living facility, ages 71-94 years, participated and were divided into intervention (n=28) and control groups (n=13). All participants underwent clinical tests for balance (ZBS) and completed self-confidence (ABC) and general anxiety (SAST) questionnaires. The intervention group practiced twice daily using the BBalance app, for one month. Tests were conducted four months before the intervention (T1), at the beginning of intervention (baseline, T2) and at its end (T3).
Results: During T1–T2, ZBS scores between groups were similar (P=0.503). Between T2 and T3, ZBS scores in the intervention group improved significantly compared to controls (P<0.0001). Self-confidence and anxiety showed a trend toward improvement. After using the BBalance app, twice daily for one month, balance scores improved. Anxiety and self-confidence demonstrated a trend toward improvement.
Conclusion: The BBalance app can be a useful tool for balance rehabilitation when Tele-health is required.
FP1100Prebycusis and Presbyvestibulopathy: balance improvement after hearing loss restoration.
Giacinto Asprella Libonati1, Pasqualina Maria Picciotti2, Tiziana Di Cesare2, Fernanda Asprella Libonati2, Guido Conti2
1U.O.S.D. Vestibologia e Otorinolaringoiatria Ospedale Giovanni Paolo II, Policoro, Italy; 2Otolaryngology Department, Fondazione Policlinico Universitario “A. Gemelli” – IRCCS, Rome, Italy
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
In last decades, life expectancy increased and the general aging of the world’s population has increased at the same time the interest in aging-related diseases. Presbycusis is the most common hearing disorder and a major cause of chronic disability in older age. Hearing loss affects approximately one-third of adults aged between 61 and 70 years and more than 80% of those older than 85 years. It is considered a multifactorial complex pathology caused by the age-related degeneration of the hearing system and by environmental and genetic factors. Age-related hearing loss can cause difficulty in speech comprehension compromising communication. Hearing impairment can have psychological, physical, and social consequences.
Presbyvestibulopathy (PVP) is a chronic vestibular syndrome characterized by unsteadiness, gait disturbance, and/or recurrent falls in the presence of mild bilateral vestibular deficits. The diagnosis of PVP is based on the patient history, bedside examination and laboratory evaluation, requiring bilaterally reduced function of the vestibulo-ocular reflex (VOR). The Classification Committee of the Bárány Society has described diagnostic criteria for PVP.
Different papers investigated the correlation, prevalence, and time patterns of prebycusis and presbyvestibulopathy development. However, few papers studied the impact of diagnosed and treated hearing loss on presbyvestibolopathy. The aim of the present study was to investigate patients affected by presbycusis in order to define if hearing aid can improve vestibular function reducing risk-to fall.
We enrolled 20 patients (mean age 75 years). At the first observation, auditory threshold was performed through pure-tone and speech audiometry and MMSE was used for cognitive function screening. Before and after hearing aid fitting we evaluated “Conley scale” (for the fall risk assessment), “Corsi Blocks Task Test” (assessing visuo-spatial working memory) and Dizziness Handicap Inventory (DHI) (quantifying dizziness-related physical and emotional symptoms and restrictions in daily activities).
After hearing aid fitting, we observed a good proethesic gain with subjective benefit from the patients. We also found an improvement of DHI, Conley Scale and Corsi Test. Treatment of hearing loss is useful not only for reducing the fall risk but also for improving the spatial orientation and the quality of life.
Further studies are needed to confirm our data, which support the hypothesis that early hearing restoration could improve vestibular function and balance.
FP1101The Zur Balance Scale: Reliability, validity and characteristics of norms
Oz Zur1,2, Hadas Ben-Rubi Shimron1, Lisa Deutsch3, Eli Carmeli4
1The Israeli Center for Dizziness and Balance Disorders, Raanana, Israel; 2Department of Physical Therapy, Ben Gurion University of the Negev, Beer Sheva, Israel; 3BioStats Statistical Consulting, Ltd., Maccabim, Israel; 4Department of Physical Therapy, University of Haifa, Haifa, Israel
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: The first step of any fall prevention program is balance and postural control assessment. Most clinical balance tests primarily challenge the visual and proprioceptive systems. The few that provide information about the dynamic function of the vestibular system have a ceiling effect. The objectives of this study were to determine the reliability, inter- and intra-class correlation coefficients, and normative scores of the Zur Balance Scale (ZBS)—a clinical sensory integration test.
Methods: Two-hundred-fifty-one healthy participants, ages 29-70 years were recruited and tested for inter-tester (n=65), intra-tester kinetic measurements on a force plate and validity, compared to the modified clinical test of sensory interaction and balance (mCTSIB) (n=44), and normative values (n=251). Results: Inter- and intra-tester reliability of the ZBS was high, with no ceiling effect. ZBS was valid and reliable compared to the mCTSIB, and as good as the mCTSIB for evaluating postural sway among healthy adults. Normative ZBS values decreased with age, especially after age 60.
Conclusions: The ZBS can be used to assess sensory integration for balance at young adults to the elderly, with no ceiling effect. By including head rotations, the ZBS might be better for differentiating vestibular or mild balance impairments.
FP1103Alterations in Trunk Yaw Rotations during Object Circumvention following acute Unilateral Vestibular Neuritis. Data indicating a direct role of Vestibular Signals during circumvention
John H.J. Allum, Heiko M. Rust, and Flurin Honegger
Department of ORL, University of Basel Hospital, Basel, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Walking among crowds avoiding colliding with people is described by vestibular deficit patients as vertigo-inducing. Accurate body motion whilst circumventing an impeding person in the gait pathway is dependent on integration of multimodal sensory cues. However, the impact of acute vestibular loss on human balance control in the context of obstacle circumvention and its effect on spatial perception of distance and orientation to the impeding person has not been investigated to date.
Methods: We examined lower-trunk yaw motion during circumvention in 4 patients 2-5 days after onset of acute unilateral vestibular loss (aUVL) due to vestibular neuritis, and compared their results with age-matched healthy controls (HCs). Subjects performed 5 gait tasks with eyes open twice: walk 6m in total, but after 3m, circumvent to the left or right as closely as possible a cylindrical obstacle representing a person, then veer back to the original path; walk 6m but after left and right circumvention at 3m veer, respectively, to the right, and left 45 deg; and walk 6m without circumvention. Trunk yaw angular velocities (TYAV) were measured with a gyroscope-system.
RESULTS: YAV peak amplitudes approaching to and departing from the circumvented object were always greater for aUVLs compared to HCs, when passing to the aUVLs’ deficit or normal side. The departing peak TYAV was always greater, ca. 52 and 87%, than the approaching TYAV for HCs when going straight or veering 45 deg (p=0.0006), respectively. For aUVLs departing velocities were marginally greater (12%) than approaching YAVs when going straight (p<0.05) and were 40% greater when veering 45 deg (p=0.05). The differences in departing TYAV resulted in significantly lower trajectory-end yaw-angles for veering trials to the deficit side in aUVLs (34 vs 43 degs in HCs).
Conclusions: These results demonstrate, for the first time, the effects of acute vestibular loss on trunk yaw velocity control during the 3 phases of circumvention. Firstly, on approaching an obstacle, greater TYAV is programmed by aUVLs than for HCs. Secondly, the departing TYAV is programmed to be proportionally less, with respect to the approaching velocity than for HCs, resulting in larger deficit side passing yaw angles. Thirdly, aUVLs have yaw errors returning to the desired trajectory. These results could provide a basis for further studies on understanding the role of the peripheral vestbular system in spatial orientation during circumvention and also for rehabilitation protocols helping patients to avoid collisions while walking in crowded spaces.
FP1106Injuries to the inferior vestibular nerve are overrepresented in post-concussive vestibular dysfunction
Anna Gard1, Ali Al-Husseini1, Evgenios N Kornaropoulos3, Alessandro de Maio3,5, Yelverton Tegner6, Isabella M. Björkman-Burtscher6,7, Karin Markenroth Bloch4, Markus Nilsson3, Måns Magnusson2, Niklas Marklund1
1Department of Clinical Sciences Lund, Neurosurgery; and 2Otolaryngology; 3 Diagnostic Radiology, Lund University, Skåne University Hospital, Lund, Swede and Lund University; 4Lund University Bioimaging Center, Lund, Sweden; 5Department of Health Sciences, Luleå University of Technology, Luleå, Sweden; 6 Department of Radiology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 7Department of Radiology, Sahlgrenska University Hospital, Region Västra Götaland, Gothenburg, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Dizziness and vertigo are common following sports related concussions (SRC). Vestibular dysfunction following SRC, can be due to an impairment of the peripheral or central neural parts of the vestibular system, or both in concert. We investigated 21 atheletes with previous SRC and with postconcussive symptoms with a duration of more than 6 months and compared those with with 21 healthy, atheletic, age and gender-matched controls that were not involved in sports with increased risk of SRC or had history of head trauma. Subjects were tested with vHit of all canals; with subjective horizont and vertical, with cVEMP and with recording of calorics, gaze stabilization, voluntary pursuit and saccades. Subjects were also assessed with cerebellar volumetrics and diffusion tensor imaging (DTI) of cerebellar white matter tracts using 7T magnetic resonance imaging (MRI), Vestibular dysfunction was observed in 13 SRC athletes and 3 controls (p=0.001). Athletes differed from controls in pathological video head impulse test results, escpecially for the posterior canal (vHIT; p<0.001) and cervical vestibular evoked myogenic potentials (cVEMP; p=0.002. thus, suggesting a peripheral vestibular dysfunction and specifically indicating injury to the inferior vestibular nerve. Although the cause of this sqewed deviation has to be specuated upon, the anatomy of the inferior compared to the superior vestibular nerve, might suggest that the inderior nerve may be less protected.
FP1107The Predictive Validity of the 9-Item Vestibular Activities Avoidance Instrument
Pamela M. Dunlap1, Claudia M. Costa2, Fai Alradady1, Patrick J. Sparto1, Joseph M. Furman3, Gregory F. Marchetti4, Jeffrey P. Staab5, Anthony Delitto1, Susan L. Whitney1
1University of Pittsburgh, Department of Physical Therapy, Pittsburgh, PA, USA; 2Faculty of Medicine, Unversity of Lisbon, Lisbon, Portugal; 3University of Pittsburgh, Department of Otolaryngology, Pittsburgh, PA, USA; 4Duquesne University Department of Physical Therapy, Pittsburgh, PA, USA; 5Mayo Clinic, Departments of Psychiatry and Psychology and Otolaryngology Head and Neck Surgery, Rochester, MN, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background/Objective: The 9-Item Vestibular Activities Avoidance Instrument (VAAI-9) is a reliable and valid tool developed to identify fear avoidance beliefs among persons with vestibular disorders. The purpose of this study was to determine the association between fear avoidance beliefs at baseline and disability measures at three-month follow-up in persons with vestibular disorders and to identify potential cut-off scores for the VAAI-9 that may indicate poorer outcomes.
Methods: This prospective cohort study included participants =18 years of age recruited from a tertiary care balance disorders clinic and an outpatient vestibular physical therapy clinic who reported dizziness. All participants completed the VAAI-9 at baseline and the following measures at three-month follow-up: Patient Acceptable Symptom State (PASS), Vestibular Activities and Participation measure (VAP), Dizziness Handicap Inventory (DHI), and Activities-Specific Balance Confidence Scale (ABC), and the Global Rating of Change (GROC). Predictive validity was determined by assessing the relationships between the baseline VAAI-9 scores (range: 0-54) and follow-up outcome measures using Spearman’s correlation coefficient rho. Baseline cut-off scores for the VAAI-9 were determined by receiver operating characteristic (ROC) curve to identify those who reported that their symptoms were not acceptable at follow-up according to the PASS.
Results: Participants (n=100) (mean age 49±16 years; 73% female) completed the baseline assessment and 53% (n=53) have completed the three-month assessment (follow-up data collection is ongoing; estimated response rate=70-80%). The mean VAAI-9 score was 25.4 (SD=13.3) at baseline and was significantly associated with VAP (rho=0.61), DHI (rho=0.64), ABC scores (rho=-0.58), and the GROC at follow-up (rho=-0.3), (p<0.05). The mean VAAI-9 score for those who were not satisfied with their current state at follow-up (n=23) was 32.1 (SD=11.1) and was 18.2 (SD=13) among those who were satisfied with their current state at follow-up (n=30) according to the PASS (p<0.001). The results from the ROC curve indicate that a baseline VAAI-9 score of 24.5 was able to identify those who were not satisfied with their symptoms at 3 months with 73.3% sensitivity and 78.3% specificity (AUC=0.8, p<.001).
Conclusions: The results provide evidence for the predictive validity of the VAAI-9 and confirm that fear avoidance beliefs are associated with outcomes at three-month follow-up. A score of 24.5 or greater on the VAAI-9 may indicate poorer prognosis among persons with vestibular disorders, suggesting that an assessment of fear avoidance beliefs could be valuable for clinicians to identify individuals at greater risk of poor outcomes after a vestibular disorder.
FP1113A Sensitive Clinical Test to identify Central Vestibular Disorder: the Suppression rate of Caloric Nystagmus during Eye Tracking
Hiroaki Fushiki1, Mayumi Endo1, Reiko Tsunoda1, Tatsuaki Kuroda2, Yukio Watanabe3
1Department of Otolaryngology, Mejiro University Ear Institute Clinic, Japan; 2Kuroda ear, nose and throat Clinic, Japan; 3Osawano Long-Term Care Health Facility, Kagayaki, Japan
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Backgrounds: We have demonstrated a sensitive test that combines a visual stimulus with caloric nystagmus (CN) as a diagnostic method that detects central vestibular disorder. Unlike healthy subjects, eye-tracking during CN was not smoothly maintained in most patients with central vestibular disorder, including patients who showed normal visual-fixation. This test required a special visual stimulator; therefore, we developed the test so that visual stimulation can be performed using a mobile application in clinical practice.
Methods: For the induction of CN, the subject’s ear was stimulated with cold air for 60 s. After CN was established, the subject was instructed to fixate on a small target and then follow a target oscillating with 30° amplitude at a frequency of 0.3 Hz. A series of these visual stimuli procedures were built into our iPhone app. A total of 15 waveforms during 3 eye-tracking periods were quantitatively examined using spectral analysis with discrete Fourier transformation. Data were compared with our previous data using a special visual stimulator.
Results: In healthy subjects, the eye-tracking during CN appearance was smooth and the suppression rate of CN was excellent. The suppression rates were 69.0% ± 16.6% when eye-tracking was directed to the slow phase of CN and 52.9% ± 26.6% when eye-tracking was directed to the fast phase, respectively. These rates were equivalent to those in healthy subjects with a special visual stimulator and significantly higher than those in patients with central vestibular disorders.
Conclusion: We examined an interaction between visual-vestibular in the central vestibular system and detected central vestibular disorders in clinical practice.
FP1115Validation of inner ear MRI in patients with Ménière’s disease by comparing endolymphatic hydrops from histopathologic specimens
Sung Min Koh1, Young Sang Cho1, Yi-Kyung Kim2, Hyung-Jin Kim2, & Won-Ho Chung1
1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: Intravenous gadolinium-enhanced inner-ear magnetic resonance imaging (IV-Gd inner-ear MRI) has been used to visualize endolymphatic hydrops (EH) in clinical diagnosis of Ménière’s disease (MD). However, lack of histological validation has led to several concerns regarding how best to interpret the resulting images. Here, we compared hydropic changes in temporal bone specimens with the results of IV-Gd inner-ear MRI in patients with MD.
Material and methods: Histopathologic images of temporal bones from 37 patients with MD and 10 healthy controls were collected from the National Temporal Bone Bank of the Massachusetts Eye and Ear Infirmary in the United States. The EH ratios in the vestibule and cochlea were calculated from temporal bones using the methods used for IV-Gd inner-ear MRI, and the degree to which the saccular and utricular hydrops contributed to vestibular hydrops was measured. The presence of hydropic change in each semicircular canal was assessed using temporal bone images and compared with IV-Gd inner-ear MRI scans of 74 patients with MD.
Results: Based on human temporal bone imagery, the EH ratios in the cochlea and the vestibule on the affected side were 0.314 and 0.757, respectively. In the healthy control group, the ratio was 0.064 for the cochlea and 0.289 for the vestibule; these values were significantly different from those for the affected side of MD patients. The values for the affected ear were similar to the ratios from the IV-Gd inner-ear MRI scans in MD patients. In the vestibule, saccular hydrops was more common than utricular hydrops. The average EH ratios in the saccule and utricle were 0.513 and 0.242, respectively. No significant hydropic change from each of three semicircular canals was evident in temporal bone histopathology. However, herniation of otolithic organs (saccule or utricle) into the lateral semicircular canal was found in 44.4% of the patients, with saccular herniation (24.8%) more common than utricular herniation (16.7%).
Conclusion: As a result of this study, it was confirmed that the study of EH through MRI were similar to the actual histopathological findings.
FP1116Discordant Horizontal-Torsional Nystagmus: Underlying Disorders and Mechanisms
Sun-Uk Lee, MD1,2, Hyo-Jung Kim, PhD 3, Jeong-Yoon Choi, MD, PhD2,4, Byung-Jo Kim, MD, PhD1,5, Ji-Soo Kim, MD, PhD2,4
1Department of Neurology, Korea University Medical Center, Seoul, South Korea; 2Department of Neurology, Seoul National University College of Medicine, Seoul, South Korea; 3Research Administration Team, Seoul National University Bundang Hospital, Seongnam, South Korea; 4Dizziness Center, Seoul National University Bundang Hospital, Seongnam, South Korea; 5Department of Neurology, Korea University College of Medicine, Seoul, South Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Objectives: In central as well as peripheral vestibular lesions, right-beating horizontal nystagmus is almost always associated with clockwise (upper poles of the eyes beating to the right ear) torsional nystagmus when observed and vice versa (concordant nystagmus). This study aimed to determine the etiologies and mechanisms of horizontal and torsional nystagmus beating in the opposite directions (discordant nystagmus).
Methods: We reviewed the medical records of 16 consecutive patients with discordant horizontal-torsional nystagmus who had been evaluated at the dizziness clinics of Seoul National University Bundang Hospital (n=11, March 2003 to March 2021) and Korea University Medical Center (n=5, March 2019 to March 2021).
Results: The underlying etiologies included inferior vestibular neuritis (n=7), Meniere’s disease (n=4), internuclear ophthalmoplegia (n=3), medullary hemorrhage (n=1), and normal pressure hydrocephalus (n=1). The torsional nystagmus decreased during the gaze in the same direction (for instance, during rightward gaze in clockwise nystagmus) and increased during the gaze in the opposite direction. Head-impulse tests (HITs) were positive for the ipsilesional posterior canal (PC) in all 11 patients with unilateral peripheral vestibulopathy and in two of the three patients with unilateral central vestibulopathy.
Conclusion: Discordant horizontal-torsional nystagmus may be observed in peripheral as well as central lesions. Given the findings of HITs and modulation of spontaneous nystagmus during lateral gazes, discordant horizontal-torsional nystagmus may be ascribed to selective damage of the excitatory or inhibitory pathway from the PC that innervates the ipsilateral superior oblique and contralateral inferior rectus muscles.
FP1118Dizziness, physical function, and health-related aspects among 70-year-olds in an urban population
Ellen Lindell1, 2, 3, Caterina Finizia1,4, Kerstin Frändin6, Hanna Falk Erhag6, Therese Rydberg Sterner6, Ingmar Skoog6,7, Lena Kollén4,5
1Department of Otorhinolaryngology, Head and Neck Surgery, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 2Region Västra Götaland, Södra Älvsborg Hospital, Department of Otorhinolaryngology, Borås, Sweden; 3Region Västra Götaland, Södra Älvsborg Hospital, Department of Research, Education and Innovation, Borås, Sweden; 4Region Västra Götaland, Sahlgrenska University Hospital, Department of Otorhinolaryngology, Gothenburg, Sweden; 5Department of Occupational Therapy and Physiotherapy, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Sweden; 6Neuropsychiatric Epidemiology Unit, Institute of Neuroscience and Physiology, Sahlgrenska Academy, Centre for Ageing and Health (AgeCap) at the University of Gothenburg, Gothenburg, Sweden; 7Region Västra Götaland, Sahlgrenska University Hospital, Psychiatry, Cognition and Old Age Psychiatry Clinic, Gothenburg, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Abstract: Dizziness is a common complaint among older adults and one of the most important risks for falls. We believe that dizziness already at the age of 70 negatively affects health and should be taken seriously and assessed for finding treatable causes, like BPPV, or rehabilitation to avoid fall accidents and reduce fear of falling. 70-year-olds were examined for dizziness, balance, and physical function to increase knowledge about dizziness on a population-based level.
Aims: This study aimed to report falls, physical fitness, and self-rated health in men and women with and without dizziness in a population-based sample of 70-year-olds, and to investigate which factors that are associated with falls and dizziness.
Methods: A cross-sectional population-based sample from 1203 70-year-olds (644 women, 559 men, response rate 72%) was surveyed regarding dizziness, falls, physical fitness, medications, and self-rated health. Fitness level was assessed using the six-minute walk test, chair stand test, and tandem standing test with eyes opened and closed.
Results: Dizziness was more commonly reported among women than among men (p<0.0001) and associated with decreased self-rated health and fitness levels among both men and women. Dizzy women tended to fall more often, performed worse in fitness measurements (chair stand, tandem standing), exercised less frequently, and went for walks less often than non-dizzy women. The number of medications and dizziness were identified to have significant associations with falls.
Conclusions: The study shows that the experience of dizziness already at 70 affects the person’s health and fitness levels in both men and women, and dizzy women tended to fall more often than non-dizzy women. We suggest that dizziness among older adults should be carefully evaluated regarding medications, physical function and treatable causes and when needed initiate postural training, vestibular rehabilitation to avoid future falls and improve quality of life.
Keywords: Dizziness, fitness level, falls, self-rated health, walking
FP1121Vestibular Evoked Myogenic Potentials using the B250 transducer
Karl-Johan Fredén Jansson1, Bo Håkansson1, Sabine Reinfeldt1, Ann-Charlotte Persson2, Måns Eeg-Olofsson3
1Department of Electrical Engineering, Chalmers University of Technology, Gothenburg, Sweden; 2Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden; 3Department of Otolaryngology, Head and Neck Surgery, Sahlgrenska Academy, Gothenburg, Sweden.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: A new bone conduction (BC) transducer, called B250, has been developed to improve investigations of vestibular evoked myogenic potentials (VEMPs). The aim of this study is to evaluate B250 on a population of healthy subjects in comparison with the widely used Minishaker B&K4810 (Brüel & Kjaer A/S, Denmark) and conventional air conduction (AC) earphones. It is hypothesized that B250 can simplify clinical VEMP and the risks related to high sound levels using AC stimulation can be avoided. The B250 can be attached on the mastoid using a P3333 (Brüel & Kjaer) steel-spring head band, while the Minishaker B&K4810, which is about 30 times larger, must be hand-held on the forehead.
Methods: BC and AC stimulated oVEMP (ocular) and cVEMP (cervical) were measured in 30 healthy subjects between 18 and 40 years old (15f, 15m). Four different stimulation alternatives were tested: AC with insert earphones, B250 on the mastoid and both B250 and Minishaker B&K4810 on the forehead. The stimulation signals were 4 ms long tone-bursts at 500 Hz for AC and 250 Hz for BC, respectively. The Eclipse EP25 platform (Interacoustics A/S, Denmark) was used for signal generation and VEMP recordings.
Results: At an average level, oVEMP and cVEMP with BC stimulation could be performed at 40.7 ± 8.6 dB and 35.4 ± 9.6 dB lower hearing level than AC stimulation, respectively, see the figures below. No statistically significant difference was found between the waveforms generated by the different BC stimulation alternatives.
Conclusions: The results show that mastoid stimulation with B250 can improve and simplify VEMP for clinical settings as compared to both AC stimulation with insert phones and BC stimulation with the Minishaker B&K4810. In summary, B250 requires 35 to 41 dB lower sound exposure than AC stimulation and the VEMP parameters obtained with B250 are very similar to those obtained with the Minishaker.
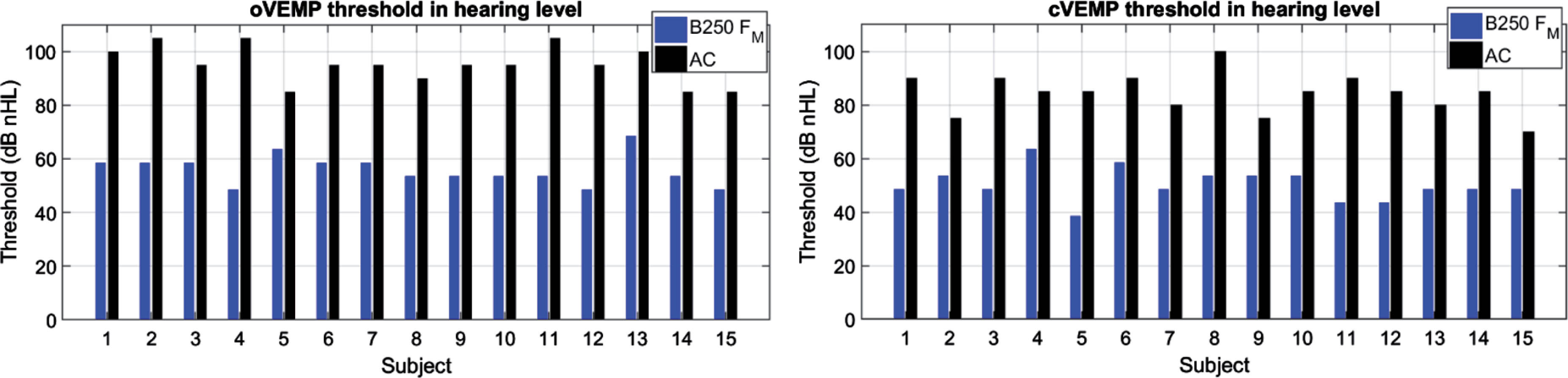
FP11222BALANCE: Cognitive-Motor Dual-Tasking in Individuals with Vestibular Dysfunction
Maya Danneels1, Ruth Van Hecke1, Laura Leyssens1, Dirk Cambier1, Raymond van de Berg2,3, Vincent Van Rompaey4,5, and Leen Maes1,6
1Ghent University, Department of Rehabilitation Sciences, Ghent, Belgium; 2Maastricht University Medical Center, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht, Netherlands; 3Faculty of Physics, Tomsk State Research University, Tomsk, Russia; 4Department of Otorhinolaryngology and Head & Neck Surgery, Antwerp University Hospital, Edegem, Belgium; 5Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; 6Ghent University Hospital, Department of Otorhinolaryngology, Ghent, Belgium.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background. Patients with bilateral vestibulopathy often suffer from cognitive impairment. On the one hand, this can be attributed to extensive vestibular projections throughout the cerebral cortex and subcortex. On the other hand, increased cognitive-motor interference (CMI) might occur. CMI can be assessed by performing dual-tasks, consisting of the simultaneous performance of a cognitive and a motor task. However, standardized and validated dual-task protocols were lacking in the vestibular population. Therefore, the 2BALANCE protocol was developed, based on a systematic review on psychometric properties of dual-tasks in a variety of populations such as Parkinson’s Disease, multiple sclerosis, dementia, and elderly (Danneels et al. 2019). The test-retest reliability was first verified in a group of healthy and young adults. The current presentation focuses on presenting the 2BALANCE protocol and the dual-task performance in a group of persons with bilateral vestibulopathy compared to a healthy cohort.
Methods and Design. The 2BALANCE protocol consists of seven different cognitive tasks, comprising all cognitive domains which are suspected to be impaired in persons with vestibular disorders. These tasks are combined with a static motor task on the one hand (balancing on a force platform with foam pad) and a dynamic motor task on the other hand (walking at a self selected speed on a pressure sensitive walkway). Both the cognitive and motor tasks are additionally performed in single task condition to enable calculating dual-task cost. A group of persons with bilateral vestibulopathy and normal hearing (n=20) was compared to a healthy age, gender, and educational level matched control group (n=20). Cognitive and motor dual-task cost was calculated as the difference in performance on the single compared to dual-task conditions.
Results. Data collection was delayed because of COVID-19 measures. Therefore, data anlysis is still ongoing, but will be presented.
Discussion. The 2BALANCE protocol will give a more accurate and daily life representation of cognitive and motor deficiencies and their interaction in persons with bilateral vestibulopathy. This might enable objectifying subtle cognitive and motor complaints, for which single tasks might not be sufficiently sensitive. Additionally, the current study will also highlight task prioritization in the healthy, compared to the vestibular-impaired population.
FP1128Bitter Vertigo: A case report
Nicolina Goldschagg1, Christian Brem2, Michael Strupp1
1Ludwig Maximilians University (LMU), Munich, Dept. of Neurology and German Center for Vertigo and Balance Disorders; 2LMU, Institute of Neuroradiology
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Case Report. A 71-year-old patient presented with a two-year history of recurrent short attacks of vertigo. Each of these attacks started with an altered feeling on the left side of the face, followed by a bitter taste on the left half of the tongue and subsequently vertigo lasting for up to 12 seconds. He had a high frequency of attacks: up to 80 times per day.
Neurological examination revealed a horizontal head-shaking nystagmus. There were neither signs of sensory or motor deficits nor of taste deficit between the attacks. Video head impulse test showed a decreased gain of the vestibulo-ocular reflex and caloric testing a reduced amplitude on the left side. Ocular vestibular evoked myogenic potentials as well as cervical vestibular evoked myogenic potentials showed reduced amplitudes on the left side; acoustic evoked potentials were normal. There was no macroangiopathy or stenosis of the neck vessels detectable, measured with ultrasound.
MRI of the brain showed an elongated basilar artery leading to an indentation of the facial and vestibulocochlear nerve on the left side. The trigeminal and glossopharyngeal nerve were not affected. Treatment with lacosamide 50mg in the evening and later 100mg per day p.o. led to a significant reduction of the attack frequency and intensity.
Conclusions. Paroxysmal dysgeusia, with bitter taste in this case, is rarely described. We propose ephatic discharges leading to pathological ephatic transmission between neighbouring axon in the proximal part of the facial nerve due to pulsatile compression of the nerve by the elongated basilar artery. In this case, this starts with the particular viszeral efferent fibres of the facial nerve leading to an altered feeling of the face muscles following the special visceral afferent fibres of the facial nerve from the ipsilateral nucleus solitarius. This fibres travel with the chorda tympani and the lingual nerve to the anterior two-thirds of the tongue, which leads to an altered and in this case bitter taste: “bitter vertigo”.
FP1129Examination of vestibular function to differentiate between vestibular migraine, Menière’s disease, and other vestibular disorders: a study in 2101 patients
V. Mavrodiev1, R. van de Berg2, A.S. Vinck3 and M. Strupp1
1Department of Neurology and German Center for Balance and Vertigo Disorders, LMU Hospital Munich, Germany; 2ENT Department University of Maastricht, NL; 3ENT Department, AZ Sint-Jan Brugge, Brugge, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Vestibular migraine (VM) and Menière’s disease (MD) are characterized by vertigo attacks of similar duration. Differentiation between the two diseases is not always possible based only on the patient history and a physical examination. In addition to audiological testing, the quantification of the vestibular function can also be helpful, since, among patients with MD, there is often a dissociation between a (pseudo?) normal video head impulse test (vHIT) and reduced caloric excitation. The goal of the study was to determine the sensitivity, specificity, positive and negative predictive values (PPV and NPV) of this dissociation for the purpose of differentiating between MD and VM and also between MD and other vestibular diseases.
Methods: We performed a retrospective multicentric analysis of 2101 patients. The examination group consisted of 1100 patients – 57% with MD and 43% with a vestibular migraine. The comparison group consisted of 1001 patients with other peripheral, central or functional vertigo disorders.
Results: We calculated the diagnostic strength of this dissociation as follows: MD vs VM: specificity 83.6%, sensitivity 58.9%, PPV 82.6%, NPV 60.5%. MD vs all observed vestibular disorders (including VM): specificity 83.5%, sensitivity 58.9%, PPV 60.3%, NPV 82.7%.
Conclusion: We confirm that the dissociation between a normal vHIT and a reduced caloric stimulation response has a high specificity and PPV for differentiation between MD and VM. The new aspect of this large study is that if there is NO dissociation the diagnosis of MD in comparison to all other vestibular disorders included is unlikely.
FP1130Etiology of bilateral vestibulopathy: a retrospective analysis in 394 patients
Vergil Mavrodiev and Michael Strupp
Department of Neurology and German Center for Balance and Vertigo Disorders, LMU University Hospital Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Bilateral vestibulopathy (BV) is a chronic vestibular disorder. It is the most common known cause of postural instability in the elderly. Symptoms typically worsen in darkness or on an uneven surface. Studies show that BV remains idiopathic in 60-75% of cases despite extensive diagnostics.
Methods: We performed a retrospective analysis with data from 394 patients with BVP and probable BVP according to the current diagnostic criteria of the Bárány society. We focused on pre-existing medical conditions, medication use, as well as known and possible causes and diseases which can lead to BVP. We also estimated the certainty of the causality of the etiology.
Results: Statistical analysis revealed the following results on the etiology of causes of BVP: 49% idiopathic; 12% antibiotics, 11% of which were gentamicin; 11% degenerative disorders with CANVAS as the most common disorder; 9% bilateral Menière’s disease (MD); 6% autoimmune; 6% postinfectious, including meningitis; 2% chemo- or radiotherapy; 5% other causes. Of the 51% patients with a known BV etiology, the causality was clinically certain in 65.5% of the cases and probable in 34.5%. Additional sensory polyneuropathy was diagnosed in 29% of patients.
Conclusion: In half of the cases, the underlying etiology of BVP remains so far unclear. The most frequent cause is ototoxic antibiotics. Bilateral MD seems to be underestimated as a cause in part due to possible difficulties differentiating MD from other vestibular syndromes. Additional sensory polyneuropathy was found frequently, which worsens the symptoms and increases the risk of falls. In future research the focus should be on possible underlying causes of what is currently classified as “idiopathic BVP”.
FP1134Menieres disease at prespective and retrospective studies
Maoli Duan, Jun Yan
Department of Otolaryngology Head and Neck Surgery & Audiology and Neurotology, Department of Clinical Science, Intervention and Technology, Karolinska University Hospital, Karolinska Institute; Xinhua Hospital, Shanghai Jiaotong University, China
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
In retrospective study, we performed three-dimensional fluid-attenuated inversion recovery (3D-FLAIR) MRI scanning and visuliazed endolymphatic-hydrops clearly in menieres disease (MD) patients but not control ones. Further, we analysed correlation hydrops with electrocochleography and vestibular functional test and found that there is clear significant correlation in MD patients. In addition, in our prospective study, we used intratympanic gadolinium-based contrast media (GBCM) administration in MD patients, we found that the diagnostic sensitivity and specificity of MRI were 79% and 81% respectively. Thus, our findings may play role in MD diagnosis in the future.
FP1136Aplication of Bárány Criteria for Vestibular Migraine and Recurrent Vertigo in childhood
Patricia Sommerfleck1, Romina Weisnchelbaum2, Grinstein Gabriela2, MS Cardozo1, CSPastore1, Sergio Carmona2
1Hospital de Pediatria “Prof. Dr. Juan P. Garrahan” Buenos Aires; 2Instituto de Neurociencias de Buenos Aires INEBA. Argentina
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
We discuss the application of the ICVD for Vestibular Migraine (VM) and Recurrent Vertigo in the Childhood to a population of 561 patients between 1-18 y.o. 286 girls (50,98%) and 275 (49%), the median age was 9 y.o. In the group from 1-5 y.o. only 2 patients fulfilled the criteria for VM and 63 were BPVC, only 1 has criteria con Recurrent Vertigo. 6-11 y.o. 38 had primary headaches, 32 VM, 10 Recurrent Vertigo and 6 BPVC 12-18 y.o. 25 had primary headaches, 19 VM and 5 Recurrent Vertigo. The criteria are not easily applied in the pediatric population. Under 5 y.o. the previous criteria are more specific. The follow up is mandatory to define how to classify the patients under 18 y.o.
FP1138International Survey on current practices on Vestibular assessment and management
Alfarghal Mohamad, Sujeet Kumar Sinha, Raymond van de Berg
Abstract
Introduction: The prevalence of vestibular disorders has been estimated in several population-based studies, and the prevalence of vestibular disorders varies across the population. There is a dearth of information on current practices of vestibular assessment and management across the globe. Much of the research that explores the current methods of vestibular assessment and management in adults have been conducted in developed countries.
Objective: The objective of the present study was to find out the current practices in evaluating and managing various vestibular disorders across the globe by various professionals.
Method: An e-survey was performed. Total thirty questions were prepared for the survey, and it was circulated to four hundred and eighteen participants who were working in the area of vestibular assessment and management. All four hundred and eighteen participants responded to the survey.
Results: Out of 418 participants, 135 participants were Audiologists, ninety-six participants were practising in audiovestibular medicine, 128 participants were general ENT, 15 participants were neurootologists, thirty were physiotherapists, 5 were neurologists, and others were nine. Out of 418 respondents, 240 were from Asia, 81 from Africa, 56 from Europe, 20 from Latin America, 14 from North America and seven respondents were from Australia. Most of the professionals were doing repositioning manuever for benign paroxysmal positioning vertigo(BPPV) followed by vestibular rehabilitation therapy. Also, when it comes to gentamycin therapy for Meniere’s disease, 108 participants responded that it was not applicable to them, 107 participants responded that they were not providing intratympanic gentamycin to individuals with Meniere’s disease. Only 25 participants provided gentamycin to individuals with Meniere’s disease regularly. Most of the participants who did not provide gentamycin or were not applicable to their profession were either Audiologists or Physiotherapists, or other professionals. Professionals also did not prefer to do surgical intervention of BPPV, Meniere’s disease and third window syndrome. Only eleven professionals performed surgery for third window syndromes, and only 6 participants performed surgery for Meniere’s disease on a routine basis. Most of the participants who were not performing surgery were either Audiologists or Physiotherapists, or other allied health professionals. Also, most professionals reported that awareness about the vestibular assessment among the patients was significantly less. Most of the respondents were dependent upon a Frenzel glass only for the vestibular evaluation. The majority of the people did not have high-end equipment to do the vestibular assessment.
Conclusions: There is a lot of variability in assessment and management procedures among the professionals. There is a need to make uniform protocol across the country, and also, the vestibular assessment and management should be included as a separate course in their curriculum.
FP1144Radiologic Features of Temporal Bones in Meniere’s Patients with Different Endolymphatic Sac Pathologies
David Bächinger1,2, Noemi Filidoro2, Marc Naville2, Norman Juchler3,4, Bernhard Schuknecht5, Joseph B. Nadol, Jr.6,7, Andreas Eckhard1,2
1Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital Zurich, Zurich, Switzerland; 2University of Zurich, Zurich, Switzerland; 3Institute of Applied Simulation, ZHAW University of Applied Sciences, Wädenswil, Switzerland; 4The Interface Group, Institute of Physiology, University of Zurich, Switzerland; 5Medical Radiological Institute MRI, Zurich, Switzerland; 6Otopathology Laboratory, Department of Otolaryngology, Massachusetts Eye and Ear Infirmary, Boston, MA, USA; 7Department of Otolaryngology, Harvard Medical School, Boston, MA, USA.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Patients with Meniere’s disease (MD) exhibit either of two pathologies (i.e., endotypes) of the endolymphatic sac (ES): progressive ES degeneration (MD-dg group) or developmental ES hypoplasia (MD-hp group), which correspond to two clinically meaningful groups with differing clinical presentations, comorbidities and prognosis. Here, we investigated further radiological features of the temporal bone (TB) associated with the two ES pathologies.
Material and methods: In patients with definite MD, endotyping was performed based on gadolinium-enhanced MRI (Gd-MRI) of the vestibular aqueduct, according to previously established methods. We assessed two-dimensional TB dimensions, the width of the sigmoid sinus and the signal intensity of the ES. Further, we performed volumetric quantification of TB pneumatization as well as a two-dimensional shape analysis of the posterior surface of the TB.
Results: Amongst others, in the MD-dg group (n = 55), a relative T2 signal loss in the ES region upon Gd-MRI correlated with the clinically affected side (median signal intensity affected to unaffected side 0.59 [IQR 0.31 – 0.89])). Further, the sigmoid sinus width was significantly smaller on the affected side compared to the contralateral side in MD-dg (6.5 ± 1.7 mm vs. 7.6 ± 2.1 mm, p = 0.04). In the MD-hp group (n = 16), several morphometric parameters indicated a significant thinning and flattening of the retrolabyrinthine area of the TB compared to the MD-dg group, such as e.g. the posterior bone cover of the posterior semicircular canal (1.04 ± 0.69 mm vs. 3.1 ± 1.9 mm vs., p < 0.001) or the tortuosity of the posterior border of the TB (mean arch to chord ratio 1.02 ± 0.01 vs. 1.10 ± 0.04, p < 0.001).
Conclusion: Several radiological features were identified that hint towards underlying etiologies and pathophysiology of MD-dg and MD-hp patient groups. The signal loss in MD-dg patients may indeed indicate the loss of the ES. In MD-hp patients, thinning and flattening of the retrolabyrinthine area of the TB may indicate that hypoplasia of the ES is associated with additional presumably developmental anomalies of the TB.
FP1145Validation of a Low-Cost Cephalic Impulse Test Device for the Detection of Corrective Overt Saccades
Karina Aracena1,2, Macarena Gallardo2, Javier Oyarzun1, Salomé Alfaro1, Sofia Waissbluth1, Phoebe Ramos1
1Department of Otorhinolaryngology, Pontificia Universidad Católica, Santiago Chile; 2Department of Health and Sciences, Pontificia Universidad Católica, Santiago Chile
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Overview: When patients present to the emergency department with symptoms of acute vertigo or dizziness, the H.I.N.T.S protocol is performed, which includes a horizontal head impulse test (HIT). If a benign etiology is present, a compensatory eye saccade, an overt saccade, is observed on the HIT. The video head impulse test (V-HIT) can detect and quantify these saccades, but has the disadvantage of a high cost, and is usually not available in emergency departments. For this reason, a low-cost HIT device was developed. The purpose of this study is to validate a low-cost HIT device by comparing saccade detection with the V-HIT.
Methods: Patients referred for vestibular evaluation with V-HIT at the otolaryngology department were recruited. The first examiner performed the V-HIT in the horizontal plane, and the second examiner performed the evaluation with the low-cost device, both were blinded evaluators. The latter reported the presence or absence of overt corrective saccades. The low-cost HIT has an accelerometer calibrated between 150 and 200 degrees/sec in a horizontal cephalic plane, where a green light is illuminated when the impulse is properly executed, and simultaneous red light when the impulse is improperly executed.
Results: We have currently recruited 15 patients, ten women and five men, average age 58,5 ± 17,7 yrs. Twelve patients presented overt saccades on V-HIT testing, of which five were bilateral. Saccades were seen in ten patients with the low-cost HIT device; hence two cases were discordant. For now, we have observed an almost perfect agreement between both tests ( = 0.83).
Conclusion: These preliminary results allow us to conclude that there appears to be an adequate correlation between the low-cost HIT device and the V-HIT. We hope to include this low-cost device in the H.I.N.T.S protocol locally in order to improve interpretation, evaluator’s technique, and finally, the diagnosis in patients with acute vertigo. The implementation of low-cost diagnostic tool allows for a greater access to accurate diagnosis.
FP1147An Examination of The Potential for Autonomic Nervous System Responses and Postural Sway to Serve as Indicators of Visual-Vestibular Mismatch
Emily Keshner1, Carole Tucker2, Donna Coffman1, Mariam ALShammari3
1Temple University, Philadelphia, USA, 2The University of Texas Medical Branch, Galveston, USA.3 Hafr Albatin Central Hospital, Hafr Albatin, KSA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD? Yes
Background. Although treatments for dizziness as a result of visual-vestibular mismatch (VVM) exist, the lack of prognostic information about this population affects the quality of their rehabilitation care. Despite numerous studies showing that individuals presenting with non-specific dizziness are likely to have VVM, and despite VVM being recognized by to the international classification of vestibular disorders by the Bárány Society, it remains unknown how prevalent this condition is. The VVM diagnostic questionnaire has not yet been generally accepted as a useful tool for diagnosis. In this study the use of measures of electrodermal activity (EDA) of the autonomic nervous system (ANS) and postural acceleration during vestibulo-visual challenges are explored in individuals with vestibular migraine (VM) both with and without VVM.
Purpose. The aims of this study were to examine, in adults with VM: 1) the presence of VVM and visual dependency in individuals presenting with complaints of dizziness using the VVM questionnaire and the Rod and Frame protocol, respectively; 2) the potential of EDA activity and postural responses to differentiate between VM and healthy individuals when accommodating for postural instability and visual-vestibular conflict; and 3) the effect of exposure to different visual contexts of VR) environments on EDA phasic and tonic responses and postural responses in identified adults with VM with VVM.
Method. the VVM questionnaire and the Rod and Frame protocol were used to test the presence of VVM and visual dependency, respectively. A Shimmer 3 IMU sensor accelerometer was used to assess trunk acceleration in the anterior-posterior, medial-lateral, and vertical directions with different VR environments (STREET and SPACE). EDA measurements were assessed with a wireless wearable Shimmer 3 GSR+. Clinical measures of dizziness and mobility were concurrently tested. A linear mixed model was used to examine the effect of VM with and without VVM on standing balance and EDA activity.
Results. The presence of VVM, headache, and visual dependency demonstrated a strong association. EDA activity and postural acceleration significantly differed between VM and healthy individuals. Specific self-confidence and dizziness severity subjective reporting tools were reliable for distinguishing between VM and healthy individuals. Lastly, VM individuals with VVM exhibited significantly greater normalized path length (NPL) of trunk accelerations in the vertical plane than VM individuals without VVM with the STREET environment compared to the SPACE environment.
Target Audience. Our findings have important implications for otolaryngologists and physical therapists in future assessment and intervention.
FP1148Use of Electrocochleography in patients with Meniere’s Disease who present Discordant Caloric and Video Head Impulse Test
Phoebe Ramos2, Jai-sen Leung2, Sofia Waissbluth2, Javier Oyarzun2, Macarena Gallardo1, Salomé Alfaro2, Nicolás Perez-Fernandez3, Karina Aracena1,2
1Department of Health Sciences, Pontificia Universidad Católica Santiago, Chile; 2Department of Otorhinolaryngology, Pontificia Unviersidad Católica Santiago, Chile; 3Department of Otorhinolaryngology, Complejo Hospitalario de Navarra, España
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Overview: The results of the caloric test (CAL) and video head impulse test (V-HIT) in Ménière’s disease (MD) are sometimes concordant or discordant, evidence suggests that this is due to the different hydropic stages of the disease. A complementary study such as electrocochleography (ECochG) allows to identify the presence and / or absence of cochlear endolymphatic hydrops (EH) in these patients.
The purpose of this study is to show the presence of EH through extratympanic ECochG in patients with definitive unilateral MD who present with discordant CAL and V-HIT.
Methods: Analytic cross-sectional study. Patients diagnosed with definitive unilateral MD, over 18 years, without MD surgical management, without intratympanic treatment for MD. Patients were evaluated by an otolaryngologist, and every test was performed the same day (audiometry, impendaciometry, balance tests, oculomotor tests, ECochG, CAL and V-HIT).
Preliminary results: For the moment only fourteen patients have been evaluated, 9 women and 5 men, average age of 47,27 ± 18,28. Allowing to obtain two subgroups: (A) nine patients with discordant CAL and V-HIT result, 77,78% presented altered ECochG and audiometry; (B) two patients with altered CAL and V-HIT result, 100% presented altered ECochG and audiometry. Due to low sample size, there is limited variability between studied variables (p value > 0,05). The three remaining patients presented with unexpected results, (1) altered audiometry, altered bilateral V-HIT, normal CAL with altered ECochG, (2) normal audiometry, V-HIT and CAL with normal ECochG, (3) altered audiometry, normal CAL and VHIT with normal ECochG.
Conclusion: Despite no statistically significant results, more than 50% of patients with discordant CAL and V-HIT result presented with an altered ECochG. We believe that with a larger sample size we will obtain a higher number of patients with this result. All patients in group B presented an altered ECochG, an expected result considering that these patients EH should be more intense and/or present with increased vestibular compromise. Preliminary data in this study, suggest that ECochG is a complementary exam that could potentially predict EH localization in the inner ear. This study also allows to illustrate the diverse results that can be obtained between patients with MD when these exams are taken simultaneously on the same day.
FP1149Vestibular Costimulation with a commercially available Cochlear Implant in adults
Morgana Sluydts1, Marc Leblans1, Robby Vanspauwen1, Floris L Wuyts1,2, Andrzej Zarowski1
1European Institute for ORL-HNS, NKO Dienst Sint-Augustinus Hospital GZA, Wilrijk, Belgium; 2Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Research background: The hypothesis that cochlear implantation typically leads to vestibular loss has been partially refuted. The natural evolution of cochleovestibular disorders can result in decreased vestibular functioning after implantation. Moreover, analyses of individual cases have provided evidence for stable or even improved postoperative vestibular performance. In addition to these observations, it has been proven that cochlear implant (CI) activation during postoperative vestibular assessments can improve the outcome as the currents from the cochlear implant may spread towards surrounding structures, like the vestibular system. This phenomenon is called vestibular costimulation. The goal of this study was to evaluate whether it is feasible to functionally modify such current spread.
Methods: Four adult patients (2 males, 2 females) who received a commercially available CI were enrolled in this study at least six months after activation of the CI. All the participants had a working vestibular system. Counterbalanced biphasic pulses were presented as single pulses, as bursts, or as an amplitude modulated biphasic pulse train (modulation frequencies of 1, 2, 5, 10, 20, 50, 100, 200, 300, 400, and 500 Hz). Before the stimuli were presented for 60 seconds, an upper comfortable level was defined for each stimulus. In order to evaluate a possible effect on the vestibulo-ocular reflex, the eye movements were captured with video goggles (with both eyes covered to prevent fixation suppression). The participants were instructed repeatedly to report every sensation that they experienced (vestibular or not).
Results: All four participants described auditory sensations and one of them also reported vibrations. The same participant described some sensation of a fading cyclic head tilt in response to a biphasic pulse train that was amplitude modulated with a modulation frequency of 2 Hz. A similar sensation could be evoked with a 400 Hz modulation frequency. Six months later, this participant was invited for an additional study visit but none of the vestibular sensations could be replicated. Furthermore, the eye movement recordings did not show any sign of electrically mediated vestibulo-ocular reflexes or ocular counter-rolling in any of the participants.
Conclusions: Subjective vestibular sensations or vestibular-mediated eye movements could not be electrically evoked with a commercially available cochlear implant in four adult patients with almost normal vestibular function.
FP1150Worldwide survey on the treatment of peripheral vestibular disorders
Michael Strupp1, Nils Lucca Kern1, Göran Laurell2, Eva Grill3, Ralf Strobl3
1Ludwig Maximilians University (LMU), Munich, Germany, Dept. of Neurology and German Center for Vertigo and Balance Disorders (DSGZ); 2Uppsala University, Sweden, Department of Surgical Sciences; 3LMU, Insitute for Medical Information Processing, Biometrics and Epidemiology and DSGZ
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To evaluate the currently used treatment options of the six most frequent peripheral vestibular disorders: Menière’s disease, acute unilateral vestibulopathy (AUVP)/vestibular neuritis, benign paroxysmal positional vertigo (BPPV), bilateral vestibulopathy (BVP), vestibular paroxysmia and superior canal deshiscence syndrome (SCDS).
Background: For the therapy of vestibular disorders, there are basically four treatment options: physiotherapy (liberatory maneuvers or balance training), pharmacotherapy, surgery and psychotherapy. Since there are very few state-of-the-art placebo-controlled trials, the treatment of patients with vestibular disorders is so far not standardized and various methods and modalities and their combinations are applied with heterogeneous efficacy.
Design/Methods: A web-based standardized survey questionnaire on the treatment of the six most frequent peripheral vestibular disorders was used to collect data. 234 replies from five continents, 47 countries, 162 cities and 188 centers were received.
Results: (% from all 234 replies; multiple answers possible): Menière’s disease: 85% pharmacotherapy, namely 65% betahistine, 21% diuretics, 20% steroids, 16% antiemetics, 14% gentamicin; 37% surgery. AUVP: 79% pharmacotherapy, namely 47% glucocorticoids, 39% antiemetics, and 24% betahistine; 67% physiotherapy. Vestibular paroxysmia: 65% pharmacotherapy, namely 57% anticonvulsants; 7% surgery. SCDS: 50% Surgery, namely 19% canal plugging, 12% capping, and 8% resurfacing. BVP: 77% physiotherapy. BPPV: posterior canal: 71% Epley, 40% Sémont, and 12% others. Horizontal canal BPPV canalithiasis: 58%% roll-maneuver, 33% Gufoni, 7% prolonged rest, and 9% others. Horizontal canal cupulolithiasis: 35% Gufoni, 27% roll maneuver, 9% Zuma, and 7% head shaking; anterior canal: 36% Yacovino maneuver, and 14% modified Epley maneuver.
Conclusions: In this world wide survey with 234 replies from 188 centers widely heterogeneous applied treatment options were reported for the six most frequent peripheral vestibular disorders. For example, medication use is often not supported by evidence. Namely in Menière’s disease, AUVP and vestibular paroxysmia well designed controlled trials are needed with clinically meaningfull endpoints are needed.
FP1151Controversies in Lateral Canal BPPV physiopathology
Daniele Nuti, Marco Mandalà
University of Siena
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Benign paroxysmal positional vertigo (BPPV) of the lateral (horizontal) canal physiopathology, despite an agreement regarding the association of geotropic positional nystagmus and canalolithiasis as well as apogeotropic positional nystagmus and cupulolithiasis, remain controversial.
Positional nystagmus features (intensity, duration and latency), characteristics of the otoconia clusters, anatomical variations of the bony and membranous labyrinth will be discussed with practical examples and mathematical models to underline light and shadows in the understanding of lateral canal BPPV physiopathology both for the geotropic and apogeotropic variants.
The light cupula hypothesis will be critically described in the geotropic variant of lateral canal BPPV. Furthermore, the null point phenomenon in the apogeotropic lateral canal BPPV variant will be discussed according to possible cupula orientations in space. Most of the described physiopathological characteristics are in favour of the canalolithiasis theory both for the geotropic and apogeotropic variant of lateral canal BPPV.
FP1154Towards a bedside pointing test for spatial orientation: egocentric retinotopic vs. allocentric world-based strategies
Gerb J1,3 , Brandt T2-4, Dieterich M1-3, 5
1Department of Neurology, Ludwig-Maximilians University, Munich, Germany; 2Graduate School of Systemic Neuroscience, Ludwig-Maximilians University, Munich, Germany; 3German Center for Vertigo and Balance Disorders, Ludwig-Maximilians University, Munich, Germany; 4Hertie Senior Professor for Clinical Neuroscience, Ludwig-Maximilians University, Munich, Germany; 5Munich Cluster for Systems Neurology (SyNergy), Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: To examine systematic differences between possible solution strategies (egocentric/retinotopic vs. allocentric/world-based) in a pointing task, using a smartphone-based pointing device.
Background: Deficits in spatial memory, orientation, and navigation can occur in degenerative and vestibular neurological disorders [1]. Pointing at targets in the 3D environment can be solved using both an egocentric approach (aligning one’s fingertip with the retinotopic representation of the target) or an allocentric world-based solution (where the pointing vector reaches the target by aligning one’s index finger as extension of the stretched arm with the visual line of sight) which requires more complex integration of different sensory systems [2]. Given the anatomical offset between both reference frames, the resulting pointing vector might differ.
Design/Methods: We used a smart phone-based pointing device [3] attached to the subject’s forearm harnessing the built-in inertial sensors [4] for analysis of pointing performance in azimuth and polar spatial coordinates. Fifty subjects (mean age 56 yrs, 18 female) were positioned in an upright, sitting position facing a wall with nine targets in a 3x3 square matrix. The subjects were then asked to point to the targets in random order with their eyes open. We examined two paradigms: first, the pointing device had a laser pointer attached to it, acting as a directional extension of the pointing vector. This visualization of the world-based vector allowed the subjects to use an allocentric pointing strategy with direct feedback by moving the laser point on the wall. Second, the laser was switched off and the subjects were asked to place their fingertip on the retinotopic representation of the targets (retinotopic approach).
Results: Mean absolute deviation between the two paradigms was 5.7° in azimuth and 4.6° in polar direction; minimum mean azimuth deviation was 1.5° (polar: 1.1°), maximum mean azimuth deviation 24.8° (polar: 14.2°).
Conclusion: Subjects can apply different strategies when performing a pointing task. Objective performance measurement showed a non-negligible difference between retinotopic and world-based pointing [5]. These differences vary individually. When assessing orientational deficits in peripheral disorders (unilateral/bilateral vestibulopathy) or central diseases (hippocampal or cortical), these different available pointing strategies should be accounted for.
[1] Brandt et al (2017) Curr Opin Neurol
[2] Keefe & Watt (2017) Exp Brain Res
[3] Flanagin et al (2019) J Neurol
[4] Kok M et al (2017) Trends Signal Process
[5] Gerb J et al (2022) J Neurol (in press)
Acknowledgments: Partially funded by the Deutsche Stiftung Neurologie (DSN)
FP1157Reported Thresholds of Self-Motion Perception are Influenced by Testing Paradigm
M. Pleshkov1,2, N. Rondas3, F. Lucieer1, L. van Stiphout1, M. Janssen1,4, N. Guinand5, A. Perez-Fornos5, V. Demkin2, V. van Rompaey6, H. Kingma1,2, R. van de Berg1,2
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, School for Mental Health and Neuroscience, Maastricht, Netherlands; 2Faculty of Physics, Tomsk State Research University, Tomsk, Russia; 3Faculty of Health, Medicine and Life Sciences, Maastricht University, Netherlands; 4School for Public Health and Primary Care (CAPHRI), Department of Methodology and Statistics, Maastricht University, Maastricht, The Netherlands; 5Service of Otorhinolaryngology Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland6Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background/Objective: Different testing paradigms have been proposed to investigate reported thresholds of self-motion perception. They can differ regarding the amount of possible motions that patients have to choose from. Objective of this study was to compare the two-option paradigm and twelve-option paradigm, in order to investigate whether reducing the choice options significantly influences the reported thresholds of self-motion perception of healthy subjects.
Methods: Thirty-three volunteers with no prior vestibular complaints were included and sequentially tested with both paradigms at a random sequence. Vestibular perceptual thresholds were measured using a hydraulic motion platform in the absence of external visual and auditory cues. The platform delivered twelve different movements: six translations and six rotations. The subject had to report the correct type and direction of movements. Thresholds were determined by a double confirmation of the lowest threshold, in combination with a double rejection of the one-step lower stimulus. Vestibular perceptual thresholds of both paradigms were compared using the mixed model analysis.
Results: The twelve-option paradigm showed significantly higher vestibular perceptual thresholds for yaw rotations and translations left, right and down (p < 0.001), compared to the two-option paradigm. No statistical difference was found for rolls and translations up. No significant gender effect, learning effect and carry-over effect were present in any of the applied motion directions.
Conclusion: Reported thresholds of self-motion perception of healthy subjects are influenced by the testing paradigm. The twelve-option paradigm showed significantly higher thresholds than the two-option paradigm measured by the double confirmation of upper stimulus with the double rejection of lower one, and these thresholds seem to better reflect the true vestibular perceptual thresholds.
FP1158Bilateral Vestibulopathy and Age Increase Drop-out Rate when Testing Dynamic Visual Acuity During Walking
Dmitrii Starkov1,2, Marlou Snelders1, Floor Lucieer1, Miranda Janssen1,3, Maksim Pleshkov1,2, Herman Kingma1,2, Vincent van Rompaey4,5, Nolan Herssens6,7, Ann Hallemans6,7,8, Luc Vereeck6,7, Nils Guinand1,9, Angelica Perez-Fornos8, Raymond van de Berg1,2
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Centre, Maastricht, Netherlands; 2Faculty of Physics, Tomsk State Research University, Tomsk, Russia; 3 Department of Methodology and Statistics, Care and Public Health Research Institute (CAPHRI), Maastricht University, Maastricht, Netherlands; 4 Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; 5Department of Otorhinolaryngology and Head and Neck Surgery, Antwerp University Hospital, Edegem, Belgium; 6Department of Rehabilitation Sciences and Physiotherapy, Faculty of Medicine and Health Science, University of Antwerp, Antwerp, Belgium; 7 Multidisciplinary Motor Centre Antwerp (M2OCEAN), University of Antwerp, Belgium; 8The research group MOVANT (MOVement ANTwerp), University of Antwerp, Belgium; 9Service of Otorhinolaryngology Head and Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: The vestibular implant can become a therapeutic option for patients with bilateral vestibulopathy (BV) soon. The impact of the vestibular implant can be assessed in many ways, one of which is the test on the dynamic visual acuity (DVA) measured with a treadmill. The test outcome measure, Dynamic Visual Acuity Loss (DVAL), can be used to quantify oscillopsia due to BV. DVAL is usually calculated as the difference between visual acuity in static and dynamic conditions. Evidence of the influence of age on DVA in literature is scarce. In addition, it is known that walking abilities can be impaired by aging. Therefore, the objective of the present study was to investigate whether DVA tested while walking, and the drop-out rate (inability to accomplish the test) are significantly influenced by age in BV-patients and healthy subjects. Methods: Forty-four BV- patients (20 male, mean age 59 years, standard deviation 11 years) and 63 healthy subjects (27 male, mean age 46 years, standard deviation 20 years) performed the DVA test on a treadmill at 0, 2, 4, 6 km/h. A Sloan optotype chart was used to test visual acuity in both static and dynamic conditions. The drop-out rate and DVAL were defined for all walking speeds. The dependency of the drop-out rate and DVAL on BV and age was investigated at all walking speeds, as well as the dependency of DVAL on speed. Results: Age and BV significantly increased the drop-out rate (p=0.038). A significantly lower DVAL value was found at all speeds in BV- patients compared to healthy subjects (p<0.001). Age showed no effect on DVAL in both groups. In BV-patients increasing walking speeds resulted in a decrease of DVAL (p=0.036). Conclusion: Bilateral vestibulopathy and age significantly increase the drop-out rate when DVA is tested while walking. It would therefore be recommended to use age-matched controls at all walking speeds while testing DVA. However, given the high drop-out rate and the higher age of most bilateral vestibulopathy patients, testing DVA on a treadmill might not be the preferable for vestibular implantation in the setting of a clinical trial.
FP1161Does the Anna Karenina principle apply to vestibular migraine and Meniere’s disease?
Emilie Kierig1,2, Sandra Becker-Bense1,2, Marianne Dieterich1,2,5,6, Valerie Kirsch1,2,5
1Department of Neurology, University Hospital, Ludwig-Maximilians-Universität (Munich, Germany); 2German Center for Vertigo and Balance Disorders-IFB, University Hospital, Ludwig-Maximilians-Universität; 3Department of Radiology, The Hospital for Sick Children, University of Toronto (Toronto, Canada); 4Department of Radiology, University Hospital, Ludwig-Maximilians-Universität; 5Graduate School of Systemic Neuroscience (GSN), Ludwig-Maximilians-Universität (Munich, Germany); 6Munich Cluster for Systems Neurology (SyNergy) (Munich, Germany)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
Introduction: To date it is unclear how Meniere’s disease (MD) and vestibular migraine (VM), which often appear in clinically similar attacks, differ from healthy controls (HC) in functional brain connectivity (measured by fcMRI), especially during the interictal phase. The central functional connectivity feature of VM and MD might be “disorganization” relative to HC, due to unpredictable attacks that cannot be compensated for. This “Anna Karenina principle” states that all HCs are very alike while all patients are very dissimilar from each other and the HCs. Here we examined the distribution parameters of functional connectivity between HC, VM and MD to elucidate the state of disorganization in the interictal phase.
Methods: 93 patients (42 VM, 51 MD) and 50 HCs underwent fMRI while resting in a 3T MRI (Siemens). Resting-state fMRI connectivity measures were extracted via dual regression and normalized in mean and standard deviation relative to HCs. Robust distribution parameters for all voxels in the grey matter were compared between groups.
Results: Distribution parameters were compact for HCs, while those of VM and MD patient groups were significantly more dispersed, i.e., disorganized (Abb 1). In figure 1 the bulk of values for the HCs were marked by black outline and superimposed onto the values for the MD and VM groups.
Distribution parameters per voxel relative to healthy control (HC) group. Values for healthy controls (HC) were marked with a black line and superimposed on Meniere disease (MD) and vestibular migraine (VM) group data. Color of dots indicates the median relative to the HC group (blue to yellow). The data of the healthy controls was normalized to mean of 0 and standard deviation 1, and these parameters were used to normalize the MD and VM patients, i.e., everything is presented in the scale of the HC group such that parameters can be compared visually.
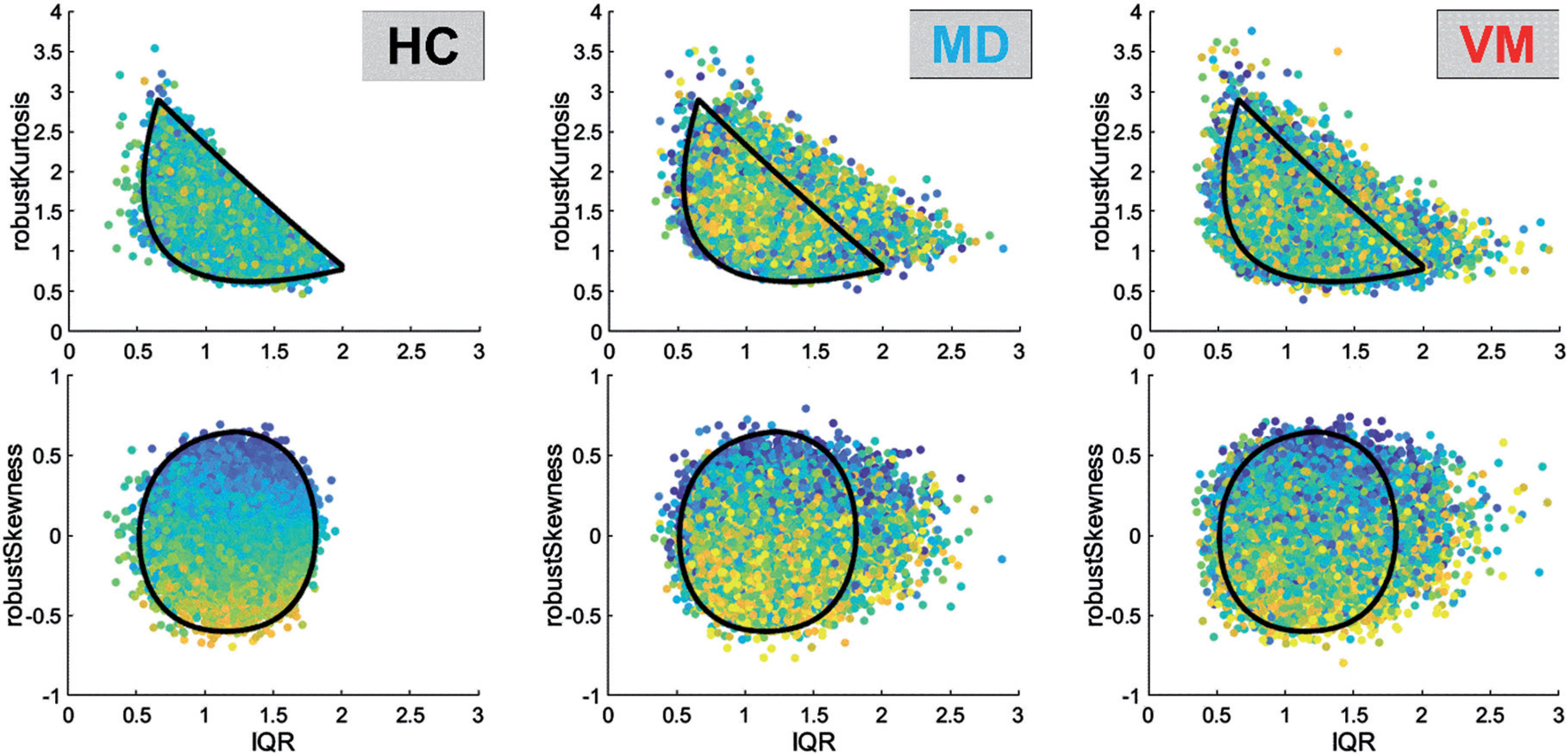
Conclusion: Resting-state functional connectivity measures imply disorganized interactions between patients relative to HCs, even in the interictal phase. VM and MD patients are very different in functional connectivity, suggesting that the Anna Karenina principle might apply to these patients.
References:
1) Dieterich et.al. J Neurol (2016); 2) Liu & Xu, Behav Neurol (2016); 3) Tabet & Saliba, J Clin Med Res (2017)
FP1162The Bárány-Cajal Letters: the Correspondence between Robert Bárány and Santiago Ramón y Cajal.
Juan M. Espinosa-Sanchez1, Ángel Batuecas-Caletrío2, Tatjana von Stackelberg3, Fernando de Castro4
1Otology & Neurotology Group CTS 495, Department of Genomic Medicine, GENYO. Centre for Genomics and Oncological Research: Pfizer / University of Granada / Andalusian Regional Government, Granada, Spain; Division of Otoneurology, Department of Otolaryngology, Instituto de Investigación Biosanitaria Ibs.GRANADA, Hospital Universitario Virgen de las Nieves, Universidad de Granada, Granada, Spain; 2Otoneurology Unit, ENT Department, University Hospital of Salamanca, IBSAL, University of Salamanca, Salamanca, Spain; 3Privatpraxis für Hals-Nasen-Ohrenheilkunde, Meerbusch, Germany; 4Grupo de Neurobiología del Desarrollo-GNDe, Instituto Cajal (CSIC), Madrid, Spain.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The Bárány-Cajal correspondence comprises a series of letters exchanged between Robert Bárány (1876-1936) and Santiago Ramón y Cajal (1852-1934). Cajal received the Nobel Prize in 1906 in recognition of his work on the structure of the nervous system, whereas Bárány was awarded the Nobel Prize in 1914 for his work on the physiology and pathology of the vestibular apparatus. Up to now the single known correspondence were that included in the Cajal’s collected letters filed in the Biblioteca Nacional de España. These were four letters from Bárány to Cajal dated between 1924-1928, along with the response from Cajal to the last Bárány’s letter. Most of these letters are about administrative issues related to Rafael Lorente de Nó’s fellowship in Upsala. Now, we have localized an initial letter from Bárány to Cajal dated in 1913, guarded in the Fernando de Castro Archive, which is included in the UNESCO Memory of the World Register as part of the Archives of Santiago Ramón y Cajal and the Spanish Neurohistological School. We have also found two more letters in the Lorente de Nó case file preserved in the Archivo de la Residencia de Estudiantes (Madrid). The aim of this communication is to present and comment these unpublished letters.
FP1163Cajal’s contributions to Vestibular Research
Juan M. Espinosa-Sanchez1, Angel Batuecas Caletrio2, Tatjana von Stackelberg3, Nicolas Perez-Fernandez4
1Otology & Neurotology Group CTS 495, Department of Genomic Medicine, GENYO. Centre for Genomics and Oncological Research: Pfizer / University of Granada / Andalusian Regional Government, Granada, Spain; Department of Otolaryngology, Instituto de Investigación Biosanitaria Ibs.GRANADA, Hospital Universitario Virgen de las Nieves, Universidad de Granada, Granada, Spain; 2ENT Department, University Hospital of Salamanca, IBSAL, University of Salamanca, Salamanca, Spain; 3Privatpraxis für Hals-Nasen-Ohrenheilkunde, Meerbusch, Germany; 4Department of Otorhinolaryngology, Clínica Universidad de Navarra, Madrid, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Santiago Ramón y Cajal (1852-1934) was awarded the Nobel Prize in Physiology or Medicine in 1906 in recognition of his work on the structure of the nervous system. Nowadays, Cajal is widely recognized as the father of neurosciences, as he established the central principles of modern neurobiology: 1) the neurone doctrine, which identifies the neuron as the basic anatomical and functional unit of the nervous system, in such a way that each nerve cell is an independent entity, and nerve synapses transfer nerve impulses from one cell to another by contact and not by contiguity, and 2) the law of dynamic polarization, which stated that nerve impulses are transmitted from the dendrites to the cell body and from there to the axon, to later reach the dendrites of the neighboring neurons. Furthermore, he discovered the dendritic spines and described the growth cone. Equally, his researches on the degeneration and regeneration of the nervous system are essential.
Cajal modified the staining method of the Italian Camilo Golgi by applying a double impregnation technique. This technique, together with other staining procedures, such as the reduced silver technique, developed by Cajal and his disciples allowed the members of Spanish Neurological School to deepen into the histology of the nervous system.
Many of these findings were collected in Cajal’s magnum opus “Textura del Sistema Nervioso del Hombre y de los Vertebrados”, published in three volumes in 1897, 1898 and 1904 respectively. The French translation of the original Spanish version contained additional information and was available in 1911 with the title “Histologie du système nerveux de l’homme et des vertébrés”.
Cajal described the microscopic anatomy of the cerebellum, retina and hippocampus in minute detail but his contributions to the knowledge of the vestibular system were also of great significance. He studied the innervation of the posterior labyrinth, including the endings of the vestibular afferents in the cristae of the semicircular canals of the birds, the paths of the vestibular nerve fibers, the vestibular nuclei describing the interstitial nucleus of Cajal in the midbrain reticular formation, which serves as the neural integrator for vertical and torsional eye movements. He detailed also the lateral vestibulospinal tract and the vestibulo-cerebellar connections.
The aim of this communication is to present the contributions of Cajal to the knowledge of the vestibular system from the original sources and drawings.
FP1164Looking for the Truth: The first description of Meniere’s Disease
Juan M. Espinosa-Sanchez1, Maria Martinez-Martinez1, Angel Batuecas Caletrio2
1Otology & Neurotology Group CTS 495, Department of Genomic Medicine, GENYO. Centre for Genomics and Oncological Research: Pfizer / University of Granada / Andalusian Regional Government, Granada, Spain; Department of Otolaryngology, Instituto de Investigación Biosanitaria Ibs.GRANADA, Hospital Universitario Virgen de las Nieves, Universidad de Granada, Granada, Spain; 2ENT Department, University Hospital of Salamanca, IBSAL, University of Salamanca, Salamanca, Spain
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Prosper Menière (1799 – 1862) was the physician at the Imperial Institute for the Deaf and Mute in Paris. Habitually, it is considered that the description of the disease that bears his name was done in a series of four papers published by Menière along 1861. In particular, the last paper, appeared in the Gazette Médicale de Paris on September 21, corresponds to his presentation read before the Imperial Academy of Medicine in Paris at the meeting on January 8, 1861. In this lecture, entitled “Mémoire sur des Lésions de L’oreille interne donnant lieu a des symptômes Congestion Cérébrale Apoplectiforme“ (A Report on Lesions of the Inner Ear giving rise to Symptoms of Cerebral Congestion of Apoplectic Type), Menière described the findings of the autopsy of a young girl dead after presenting a complete sudden deafness accompanied by vertigo and vomiting. He found “the presence of a reddish, plastic lymph, replacing the liquid of Cotugno”, that is, the endolymph, and filling the semicircular canals but not the cochlea. Based on the previous experiments of the anatomist and physiologist Marie Jean Pierre Flourens (1794 – 1867) with pigeons, Menière then concluded that when vertigo nausea and vomiting “are accompanied by a buzzing in the ears, by continuous and variable head noises, and above all when there arises rapidly a notable diminution of hearing, then the trouble has its seat in the labyrinth and more particularly in the semicircular canals”. This way, Menière was the first author that related vertigo episodes with a labyrinth impairment rather than a primary brain problem.
Strikingly, when Meniére described the findings of his famous autopsy he referred that had spoken elsewhere, a long time ago, of this precise anatomo-clinical case. This previous reference was found by Dan M’Kenzie in 1924 in the commentaries added by Menière to a textbook of Otology published in 1836 by the German otologist Wilhelm Kramer (1801 – 1876). The book entitled “Die Erkenntniss und Heilung der Ohrenkrankheiten” was translated into French by Meniére as “Traité des maladies de l’oreille” in 1848.
Here we present Menière’s original case as published in 1848 and discuss the differences with the 1861 description.
FP1165Vestibulospinal signs in Acute Vestibular Syndrome
Carlos Martínez1, Guillermo Zalazar1, Joao Lemos2, Angel Batuecas3, Carlos Gordon4 Guillermo Zalazar1, Sergio Carmona1
1Fundacion San Lucas, Rosario, Argentina; 2Coimbra University Hospital Centre, Portugal; 3Hospital Universitario de Salamanca, España; 4Tel Aviv University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
We studied 52 patients with isolated AVS or central vascular cause (AICA 15%and PICA 33% infarcts) and vestibular neuritis (52%). When evaluating grade 2 ataxia in its ability to differentiate patients with stroke from vestibular neuritis, we found a sensitivity of 34% (95% CI 13-56%), specificity 70% (95% CI 51-89%), with an LR + 1.1 and LR-1, 1. Regarding grade 3 ataxia, to differentiate stroke from vestibular neuritis we found a sensitivity of 65% (95% CI 43-86%), specificity 100% (95% CI 98-8%), with an LR + 23 and LR-1, 73. The combination of grade 2-3 ataxia to differentiate stroke from vestibular neuritis obtained a sensitivity of 92% (95% CI 79-100%), specificity 70% (95% CI 51-89%), with an LR + 3 and LR- 8.79. Patients with grade 2 ataxia were able to remain seated but with the presence of an impulse, which varied according to the site of the injury. All the lesions in the AICA territory had grade 3 ataxia and were unable to remain seated, it is a possible substitute for grade 3 ataxia
FP1168Ménière’s Disease and Endolymphatic Hydrops in Children: Report of two cases.
Rosana Rodriguez-Villalba1, Victoria Rivero De Jesús2, Jorge Salmerón Pintos3
1Department of Otolaryngology, Althaia Xarxa Assistencial Universitària de Manresa; 2Department of Otolaryngology, Hospital Clínic de Barcelona; 3Department of Radiology, Institut Guirado
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Ménière’s disease (MD) is a disorder involving the inner ear that rarely affects children (less than 3% of cases occur in children under 18 years of age) and can be difficult to diagnose. The patients we describe fulfill diagnostic criteria for Ménière’s disease according to the Classification Committee of the Bárány Society.
Endolymphatic hydrops (ELH) is found in all patients with MD, but not all patients with ELH have concurrent MD. ELH may be necessary but not enough for MD development. Recent advances in Magnetic Resonance Imaging (MRI) have helped in cases of difficult diagnosis of MD. ELH can be recognized using three-dimensional Fluid-Attenuated Inversion-Recovery sequences (3D-FLAIR) four hours after intravenous injection of 0,2 ml/kg body weight of Gadolinium.
We present two cases of unilateral MD in children: Patient 1 (fifteen year-old boy, complaining of symptoms of MD since he was ten years of age), and Patient 2 (fifteen year-old girl, who has complained of symptoms of MD for one year). The two patients presented with tinnitus, aural fullness and low to midfrequency, sensorineural hearing loss in the left ear. None of the chidren had a family background of MD.The two patients underwent MRI showing endolymphatic hydrops.
In patient 1, the left ear had a grade I hydrops in the cochlea and a grade I hydrops in the vestibul according to Nakashima’s classification
Patient 2 had a grade II hydrops in the cochlea and a grade I hydrops in the vestibul.
Conclusion: MD in children is rare and diagnosis can be difficult. The visualization of ELH through 3T MRI can be useful in these cases.
FP1169Performance in Anti-Saccades Among Healthy Young to Middle Aged Adults
Liz Fuemmeler, Au.D., Amy Alexander, PT, Shelly Massingale, PT, MsPT, Michele Petrak, PhD, CCC-A
1Hearing and Balance Specialists of Kansas City; 2Banner Sports Medicine and Concussion Specialists; 3Banner Orthopedic and Sports Medicine 4Interacoustics®
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
The random saccade test has been utilized for many years in the videonystagmography (VNG) evaluation to provide insight on possible central origin. However, saccadometry may be more sensitive to identifying dysfunction due to its test complexity, particularly in the post-head injury population. Saccadometry includes pro-saccade and anti-saccade testing, the latter which has been shown to present with a higher cognitive load. In anti-saccade testing, a subject is asked to ignore a stimulus and voluntarily move their eyes in the equal distance away from midline. This involves response inhibition and dual-tasking. A small pilot study examined differences between concussed and uninjured subjects in random saccades, pro-saccades, and anti-saccades, with anti-saccade error rates and latencies being the only significant differences between the two groups. The purpose of this study is to examine differences in error rates, latency, and velocity in both pro and anti-saccades between a pilot study control sample (N=15) and a larger normative data sampling (N=192). Data for each group was collected at different time points, a single clinic for the pilot study and 4 clinics for the larger group. Some similarities were noted, longer latencies, increased error rates, and slower velocities for anti-saccades compared to prosaccades. There were two noticeable differences between the groups, the velocities in the pro saccade test were slower for the pilot study group and latencies were longer. This was an observational study without statistical analysis. It does highlight the need to expand the normative study with narrower age ranges by decade to determine if age is a factor in the differences. Insight in to how the anti-saccade test changes with age may also be of use in medical management after injury. Future studies will help distinguish normal from abnormal, as well as origin of dysfunction.
FP1173The ‘Placebo Problem’ in Meniere’s Disease: A systematic review and meta-analysis of placebo and sham controlled Randomised Controlled Trials.
David Herdman1,2, Kostas Tsioulos1, Rebecca Webster3, Louisa Murdin4
1St George’s University Hospitals NHS Foundation Trust, UK; 2King’s College London, UK; 3University of Sheffield, UK; 4Guy’s & St Thomas’ NHS Foundation Trust, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The placebo response is conventionally asserted to be high in Meniere’s Disease (MD), which poses a challenge when it comes to studying the effects of treatments in clinical trials. We therefore conducted a systematic review to evaluate the magnitude of the placebo response on vertigo outcomes in placebo or sham controlled trials of any treatment in people with Meniere’s disease.
Methods: PubMed, Embase, and Web of Science databases, and the reference lists of the identified articles were searched, and experts were contacted for any unpublished studies. Randomized and placebo-controlled clinical trials of people with MD were included if relevant quantitative data were extractable in the placebo arm. Placebo response was defined as the within-group change from baseline, using any patient-reported scale measuring dizziness/vertigo related outcome. Articles were screened and data were extracted by two reviewers independently. Random effects meta-analysis was used to pool the percentage of placebo responders. Quality assessment was measured using the TIDier-Placebo checklist for reporting placebo and sham controls. The PROSPERO registration number is CRD42020210697.
Results: Fifteen papers could be included in the meta-analysis (377 participants). The included studies used placebo medication (n=7), intratympanic injection (n=3), sham cereal (n=3), surgery (n=1) and a pressure device (n=1). The pooled percentage of placebo responders was 42.69% (95% CI = 28.50% to 57.53%). The differences between trials were very large (88% inconsistency). Insufficient data were available to study some of the placebo determinants. The TIDier-Placebo checklist revealed the need to improve the description of placebo components alongside those of the active comparator.
Conclusion: The placebo response in Meniere’s disease is highly variable, supporting the continued use of placebo groups and suggesting the need for more research into the placebo effect in people with MD. Clinicians and researchers should be careful about how they present the treatments they are administering or prescribing. We intend to make several key recommendations to inform the design and interpretation of future clinical trials.
Target Audience: Clinicians and researchers treating patients with Meniere’s Disease, and those with an interest in placebo effects.
FP1175Audiovestibular changes in chronic HIV infection undergoing antiretroviral therapy
Annel Gomez-Coello2, Arianne Idaly Ramos Galvan1, Kathia Elizabeth Tapia Diaz1, Nallely Bueno Hernandez3, Gustavo Reyes Terán4
1Infectious Diseases Research Department, Instituto Nacional de Enfermedades Respiratorias. Mexico City, Mexico; 2Audiology subdivision, Instituto Nacional de Rehabilitacion. Mexico City, Mexico; 3Research division, Hospital General de México; 4Comisión Coordinadora de Institutos Nacionales de Salud y Hospitales de Alta Especialidad
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Abstract
The main objective of this paper was to assess changes in audiovestibular function following antiretroviral therapy. Since HIV can affect this function, we recruited both patients with HIV+ tests and patients at risk of contracting HIV undergoing preexposure profilaxis. We performed a Quasiexperimental prospective study comparing audiovestibular function measured with vHIT, tonal audiometry, and otoacoustic emissions before antiretrovirals were given. Follow up studies were performed. The main outcome variable was VOR gain on the vHIT. Statistical analysis was performed No difference was found between HIV and no HIV patients, nor before and after antiretroviral therapy. We found no evidence of audiovestibular disturbances caused by HIV; antiretroviral therapy appears to be safe since no ototoxicity could be determined.
Our results should encourage team work between infectious diseases physicians and audiovestibular experts to emphasize long term care for vulnerable populations. Further research from vestibular physiology experts in this diseases is needed.
***I cant check the box for applying to the WON-SANG LEE AWARD but I would like to be considered***
FP1178In Search for a Vestibular Pattern: Exploring Head Stability in Virtual Environments
Anat V. Lubetzky1, Maura Cosetti2,3, Brittani Morris1, Andrew Medlin1, Sarah Mischianti1; Katherine Scigliano2, Jennifer L. Kelly2,3
1Department of Physical Therapy, Steinhardt School of Culture Education and Human Development, New York University, New York, NY, USA; 2Ear Institute, New York Eye and Ear Infirmary of Mount Sinai, New York, NY, USA; 3Department of Otolaryngology-Head and Neck Surgery, Ichan School of Medicine at Mount Sinai, New York, NY, USA
Background: Individuals with vestibular disorders vary in clinical presentation and differential diagnosis can be challenging. In our previous work, we showed that head kinematics were sensitive to unilateral peripheral vestibular hypofunction (VH) as compared to controls. The purpose of this pilot study was to investigate whether an in-clinic assessment of head kinematics can differentiate vestibular disorders from controls.
Methods: Sample: 20 controls (mean age 35.3 [minimum 23, maximum 60]), 22 VH (44.9 [21, 73]), and 11 Meniere’s disease (MD) (59 [30, 81]). Self-reported outcomes included the Dizziness Handicap Inventory (DHI) and the Activities-Specific Balance Confidence Scale (ABC). Participants performed the Time-up-and-go test (TUG) and Four-square Step Test (FSST). Root Mean Square Velocity of their head was calculated in the medio-lateral and anterior-posterior directions in response to static or dynamic display of stars projected from the HTC Vive Pro Eye. All outcomes were compared between groups during the static and dynamic scene separately. If the Kruskal-Wallis Test showed a main effect of group, Mann-Whitney comparisons were made. We also ran correlations analysis per group.
Results: MD and VH showed significant, clinically important differences from controls on the TUG and FSST with moderate correlations between performance and age across groups. MD and VH had similar ABC (VH: mean 73.06 [24.38, 100], MD: mean 74.95 [20, 99.38]) and both were significantly lower than controls (98.87 [96.25, 100]). DHI was significantly higher in VH vs MD (P=0.005, VH: mean 54.36 [24, 100], MD: 22 [0,82] with a mean of 0.27 [0, 4] for controls. Main effect of group was observed for velocity under all conditions. VH was significantly higher than controls on medio-lateral static (P=0.017) and dynamic (P=0.003) and anterior-posterior static (P=0.013) but not dynamic (P=0.06). MD was significantly higher than controls on anterior-posterior static (P=0.007) and dynamic (P=0.03) but not on medio-lateral static (P=0.053) or dynamic (P=0.08). Velocity was not correlated with age but showed moderate to strong negative correlations to ABC among the MD group: Dynamic: medio-lateral: R=-0.69; anterior-posterior: R=-0.44; Static: medio-lateral: R=-0.84, anterior-posterior: R=-0.87.
Conclusions: These results suggest a distinct head pattern among vestibular disorders, even on a static scene. These differences appear to be independent of age. We will continue to study the clinical importance of the slightly different responses and varying correlations between VH and MD. Head kinematics are sensitive to vestibular dysfunction. This line of research will help determine whether it can differentiate between sub-groups of vestibular conditions.
FP1187A New Technology Used in Vestibular Rehabilitation: The Pilot Study
Gonul Ertunc Gulcelik1, Devrim Tarakci2, Ozlem Gedik Soyuyuce3, Zeynep Gence Gumus4, Nazim Korkut5, Zeliha Candan Algun6
1Asst. Prof. Istanbul Gedik University, Faculty of Health Sciences, Physiotherapy And Rehabilitation Department, Istanbul, Turkey; 2Assoc. Prof. Istanbul Medipol University, Faculty of Health Sciences, Physiotherapy And Rehabilitation Department, Istanbul, Turkey; 3AuD. Acibadem Maslak Hospital, Department Of Audiology, Istanbul, Turkey; 4AuD. Acibadem Maslak Hospital, Department Of Audiology, Istanbul, Turkey; 5Prof. Dr. Acibadem Maslak Hospital, Department Of Ear Nose And Throat, Istanbul, Turkey; 6Prof. Dr. Istanbul Medipol University, Faculty of Health Sciences, Physiotherapy And Rehabilitation Department, Istanbul, Turkey.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and purpose: The variety and use of technologies used in vestibular rehabilitation is very limited. Simulation of Vestibulo-ocular Exercises (SVORE) is a vestibular system that supports vestibulo-ocular reflex with the oculomotor and optokinetic stimulus. The aim of our study is to investigate the effectiveness of this new system on vestibular rehabilitation.
Matherials and Methods: 10 volunteer patients with vestibular disorders aged 18-70 years, with unilateral vestibular hypofunction, no visual impairment, no neurological disease, no communication problems were included in the rehabilitation programme. In the 8-week treatment protocol; a vestibular rehabilitation program was applied to the study group received treatment with the web-based system supporting the vestibulo-ocular reflex with oculomotor and optokinetic stimulus (SVORE). Pre- and post-treatment vestibular and balance tests, oculomotor function level determination, Dizziness Handicap Inventory were applied to evaluate the treatment’s effectiveness. Statistical analyzes were performed in intra-group results.
Results: In the study group, intra-group analysis showed significant improvement in vestibular symptoms and findings, balance tests, oculomotor functions, Dizziness Handicap Inventory compared to pretreatment values (p<0.05).
Conclusion: It has been observed that the web-based system with oculomotor and optokinetic stimuli is an effective means in vestibular rehabilitation.
FP1188Fear of falling: real fear of a perceived abyss
Patricia Castro1,2,3, Shree Vadera1, Matthew Bancroft1, Joseph Butell4, Diego Kaski1
1Centre for Vestibular and Behavioural Neurosciences, Department of Clinical and Movement Neurosciences, University College London, 33 Queen Square, London WC1N 3BG; 2Department of Neuro-otology, Division of Brain Sciences, Imperial College London, Charing Cross Hospital, London W6 8RF; 3Universidad del Desarrollo, Escuela de Fonoaudiología, Facultad de Medicina Clínica Alemana. Santiago, Chile; 4Regional Neurological Rehabilitation Unit, Homerton University Hospital Foundation NHS Trust. Homerton Row, London E9 6SR
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Fear of falling (FoF) is prevalent in older adults, especially those with previous falls, and typically starts insidiously. We present a 78-year-old woman with an abrupt onset FoF and no history of falls, balance problems, vertigo, oscillopsia, psychiatric or psychological issues to account for this. These cognitive changes led to a behavioural alteration of her gait that became slow and wide-based, with her gaze fixed on the floor. She began a tailored program of “Cognitive Physical Therapy (CPT)” combining cognitive behavioural therapy (CBT) and physical rehabilitation. One month later her 6m walk time and steps were reduced by a 25% and 35%, respectively and the stride length increased by 34%, with further improvement 2 months later. We postulate that the abrupt onset of symptoms triggered a central shift towards postural hypervigilance and anxiety, suppression of anticipatory (feed forward) postural adjustments (APA) leading to FoF. CPT improved objective gait parameters related to FoF and reduced postural anxiety suggesting that early diagnosis and prompt treatment may avoid chronic symptoms and social isolation.
FP1189Vestibular Rehabilitation In A Patient With Vestibular Neuritis With A Stroke History: A Case Report
Gonul Ertunc Gulcelik1, Tugba Arda Sinmaz2, Mete Iseri3
1Asst. Prof. Istanbul Gedik University, Faculty of Health Sciences, Physiotherapy And Rehabilitation Department, Istanbul, Turkey; 2Audiometrician ENT Academy Group Clinic, Kocaeli, Turkey; 3Prof. Dr. ENT Academy Group Clinic, Kocaeli, Turkey
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background and purpose: Vestibular Rehabilitation is an exercise-based approach group initiated to maximize central nervous system compensation for vestibular pathology. In peripheral vestibular diseases, vestibuloocular reflex adaptation, vestibular symptoms, balance and daily life activities how a linear improvement with rehabilitation. However, this process slows down in patients with central components.
Matherials and Methods: A 67-year-old patient with a history of stroke and right hemiparesis and right facial paralysis was diagnosed with right vestibular neuritis, and a 12-week structured vestibular rehabilitation program based on Cawthorne Cooksey exercises was applied. In evaluation, before and after treatment; VNG, balance tests (open and closed romberg, semitandem and tandem positions) and Dizziness Handicap Inventory (DHI) were used.
Results: Before rehabilitation; there was a horizontal nystagmus (4 degrees / sec) beating the left in the head shake test, in the lateral head impulse test; the right gaze gain was 0.38 ± 0.08, the left gaze gain was 0.88 ± 0.07; In the caloric test, the right hypofunction (~ 51%) was observed.In the balance tests, romberg position was measured 14 sec, semitandem position was measured 3 sec, tandem position was measured 0 sec with eyes open; while the romberg position was measured as 2 seconds with eyes closed, it was unsuccessful in semitandem and tandem positions. The initial DHI score was 74. After rehabilitation; head shake test was normal, in the lateral head impulse test, the right gaze gain was 0.26 ± 0.05, the left gaze gain was 0.93 ± 0.09; In the caloric test, right hypofunction (~ 20%) was observed. In balance tests, romberg position was measured 26 sec, semitandem position was measured 14 sec, tandem position was measured 11 sec with eyes open; with eyes closed, romberg position was measured 18 sec, semitandem position was measured 9 sec, tandem position was measured 5 sec. The end DHI score was 6.
Conclusion: Vestibular rehabilitation is also effective in vestibular diseases with a neurological component, only the process is slower.
FP1190Priming overconfidence in belief systems reveals negative return on postural control mechanisms
Patricia Castro1,2, Efstratia Papoutselou1, Sami Mahmoud3, Shahvaiz Hussain1, Constanza Fuentealba-Bassaletti1, Diego Kaski1,4, Adolfo Bronstein1, Qadeer Arshad1,5
1Neuro-otology Unit, Division of Brain Sciences, Imperial College London, London, UK; 2Universidad del Desarrollo, Escuela de Fonoaudiologia, Facultad de Medicina Clinica Alemana. Santiago, Chile; 3Fakultät für Medizin, Technische Universität München, München, Germany; 4Department of Clinical and Motor Neurosciences, Centre for Vestibular and Behavioural Neurosciences, University College London, London, UK; 5inAmind Laboratory, Department of Neuroscience, Psychology and Behaviour, University of Leicester, Leicester, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Modulation of postural control strategies and heightened perceptual ratings of instability when exposed to postural threats, illustrates the association between anxiety and postural control.
Research Question: Here we test whether modulating prior expectations can engender postural-related anxiety which, in turn, may impair postural control and dissociate the well-established relationship between sway and subjective instability.
Methods: We modulated expectations of the difficulty posed by an upcoming postural task via priming. In the visual priming condition, participants watched a video of an actor performing the task with either a stable or unstable performance, before themselves proceeding with the postural task. In the verbal priming paradigm, participants were given erroneous verbal information regarding the amplitude of the forthcoming platform movement, or no prior information.
Results: Following the visual priming, the normal relationship between trunk sway and subjective instability was preserved only in those individuals that viewed the stable but not the unstable actor. In the verbal priming experiment we observed an increase in subjective instability and anxiety during task performance in individuals who were erroneously primed that sled amplitude would increase, when in fact it did not.
Significance: Our findings show that people’s subjective experiences of instability and anxiety during a balancing task are powerfully modulated by priming. The contextual provision of erroneous cognitive priors dissociates the normally ‘hard wired’ relationship between objective measures and subjective ratings of sway. Our findings have potential clinical significance for the development of enhanced cognitive retraining in patients with balance disorders, e.g. via modifying expectations.
FP1191Development of an online vestibular diagnostic tool
Vestibular disorders can pose diagnostic challenges given non-specific symptoms and overlapping clinical features. As such, efficient clinical management of patients with vestibular symptoms can be challenging, with patients frequently seeing multiple providers prior to obtaining a definitive diagnosis. To improve the efficiency of diagnosis and treatment of patients with vestibular symptoms, we developed an online diagnostic tool that queries patients about specific symptoms, specifically the nature of their dizziness symptom (room-spinning, provoked by lying down); associated change in hearing or tinnitus; history of migraine, light/sound sensitivity, motion sensitivity; and duration of dizziness symptoms. The tool then assigns a probability of 3 specific diagnoses – Meniere’s disease, vestibular migraine, and benign paroxysmal positional vertigo (BPPV) – based on validated algorithms previously published by Friedland et al 2016. The online tool is being integrated into our patient access decision trees, to direct patients to the best initial specialist, specifically Otolaryngology if highest probability of Meniere’s disease, Neurology if highest probability of vestibular migraine, and physical therapy if highest probability of BPPV. Data regarding time to diagnosis, number of referrals, and ancillary testing ordered before and after deployment of the online calculator will be presented.
FP1193Implementing natural strategies of neural encoding optimizes vestibular prosthesis performance
Kantapon Pum Wiboonsaksakul1, Dale C Roberts2, Charles C Della Santina2, Kathleen E Cullen1
1Department of Biomedical Engineering, Johns Hopkins University; 2Department of Otolaryngology-Head and Neck Surgery, Johns Hopkins University School of Medicine
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Even the simplest sensorimotor transformations require precise neural dynamics to produce accurate and well-timed behavior. Accordingly, recent developments of sensory prostheses have focused on mimicking the response dynamics of peripheral sensors/afferent systems. The vestibular system is particularly well suited for such biomimetic prosthesis development because of the well-characterized sensor and afferent response dynamics, as well as the peripheral anatomy that allows for specific stimulation. Here, we tested the performance of a biomimetic vestibular prosthesis that implemented afferent response dynamics in the mapping between virtual head motion and pulse rate. We measured the eye movements produced by the vestibulo-ocular reflex (VOR), which plays an essential role in maintaining visual stability, and found that such biomimetic mappings produced more temporally accurate VOR eye movements. Further exploration of the parameter space revealed that incorporating even more extreme tunings than those naturally displayed by vestibular afferents provided unnatural phase advances, as well as undesirable nonlinear gain saturation. Using computational methods, we then demonstrate that the same model can account for the eye movements evoked by sinusoidal and transient stimulation and that the stimulation efficacy between the prosthesis and afferent firing is substantially less than 1:1 as is commonly assumed. Thus, taken together our results establish that vestibular prosthesis mappings that incorporate naturalistic afferent dynamics and account for activation efficacy are well suited for restoration of gaze stability. More generally, these results also emphasize the benefits of leveraging the brain’s endogenous coding strategies to ensure vestibular sensorimotor accuracy, which could directly translate to better functional outcomes in patients.
FP1194Emotional Impact of Dizziness: Comparison between Two Self-report Questionnaires in patients with Vestibular Disorders
Maria Luiza di Carlo Riato1, Vanessa Brito Campoy Rocha2, Raquel Mezzalira2, Guita Stoler2, Maria Isabel Ramos do Amaral1
1Department of Human Development and Rehabilitation - DDHR/(University of Campinas - UNICAMP), Brazil; 2Department of Otorrinolaringology, Head and Neck - UNICAMP, Brazil
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Research Background: Vertigo and dizziness can affect patients’ quality of life in their daily lives. There is solid evidence regarding the association between limbic and vestibular systems showing that vestibular symptoms might lead to a higher incidence of psychological and psychiatric diseases. Therefore, recent research investigates the relation of the cause and consequence of vestibular symptoms and psychological disorders. Self-questionnaires are considered a way to identify subjective symptoms since they consider the subject’s perspective. A complete evaluation results in an assertive diagnosis and improves prognoses. Objective: To analyze the emotional impact caused by vertigo and dizziness in patients with vestibular disorders treated at Ambulatory of Otoneurology from a University Hospital through the application and comparison of two protocols aiming to evaluate the impact of dizziness, validated to the Portuguese language: Dizziness Handicap Inventory (DHI) and Questionário de Impacto Emocional da Vertigem (CIEV).
Methods: Quantitative, descriptive, and cross-sectional research, approved by the Ethics Research Committee of Faculty of Medical Sciences (n°2.344.836). 42 male and female individuals, aged between 23,4 and 85,2 (average 58,5 +15,94). complaints related to dizziness/vertigo and, eventually, episodes of instability or falls. Both protocols, (DHI) and (CIEV), were applied. The obtained scores were calculated and statistically analyzed with a confidence interval of 95%. A descriptive analysis of the performance of the protocols was carried out, and then, both questionnaires were correlated.
Results: 28 (66,67%) participants were females. There was a statistical prevalence of women in the sample (p<0,001). The participants described more than one type of dizziness: 24 (19%) referred to vertigo, and 17 (35%) postural symptoms. The most frequent diagnostic hypotheses obtained from the patient’s medical record were classified as mixed (23/54,76%). Scores from DHI varied from 14 to 88 points (48,27 +22,08), demonstrating worse handicap in physical scale (16,97 +7,14). 27 (72,9%) participants were classified as moderate/severe handicap. Scores in CIEV protocol varied from 2 to 35 points (18,65 +8,22). Among 31(73,8%) at-risk participants in CIEV, 25(80,6%) had a moderate or severe handicap in DHI.
Conclusion: Both questionnaires (DHI and CIEV) are statistically correlated. From these results, it is possible to conclude that these questionnaires are potential tools to identify and monitor psychological components involved in the evaluation and rehabilitation of dizziness among patients with vestibular disorders.
FP1195Standardizing a Protocol for the Performance of Anti-Saccades captured by Video-Oculography
Michelle Petrak, Glen Zielinski, Shelley Massingale, Amy Alexander, Richard Gerkan, Liz Fuemmeler
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Our objective was to collect performance data from healthy volunteers in each decade of life for anti-saccade directional error rates and latencies in a standardized protocol.
The pro-saccade test (random or overlapped), although clinically valuable, often isn’t sensitive enough to flag dysfunction. The anti-saccade test is promising as more complex tasks can in many cases be a more sensitive indicator of potential pathology. In the anti-saccade test a subject is asked to ignore a stimulus and voluntarily move their eyes in the opposite direction. It is differentiated from a pro-saccade by nature of cognitive complexity, response inhibition and dual-tasking. The underlying neural networks of a pro-saccade also subserve the anti-saccade, with the addition of increased demand on inter-cortical frontal and parietal eye fields. Timing and strength of the inhibitory signal between frontal eye fields seems to be a major factor in correctly completing an anti-saccade. These areas of the brain underlie much of executive function and mental set. Oculomotor function has been well studied for decades and more recently anti-saccade research has been an area of focus. Several studies have looked at mixed pro-saccade/anti-saccade test (interweaved or blocked). This study measured an isolated anti-saccade block trial, sacrificing some of the potential neurological cost of switching tasks but more closely mimics a bedside clinical exam gaining familiarity and feasibility of time.
Anti-saccade performance data for different age groups are collected here. We add to the growing literature of anti-saccades and adding for the first time performance data for directional error rates and latencies. Our intention is to aid future studies distinguishing normal from abnormal, the progression there-of and underlying pathological dysfunction involved. Anti-saccade testing is valuable and should be included in oculomotor or psychomotor test batteries as a screening tool in addition to pro-saccades.
FP1199Therapeutic Efficacy of Botulinum Toxin Type A in Patients with Vestibular Migraine: Changes in Resting-State Functional Connectivity in a Longitudinal fMRI Study
Sun-Young Oh, MD, PhD1,2,a,b, Jin-Ju Kang, MD1,2,a, Sohui Kim3,a, Jong-Min Lee, PhD4,b, Ji Soo Kim, MD, PhD5,6 Marianne Dieterich, MD, PhD7-9
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, Korea 2Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, Korea; 3Department of Electronic Engineering, Hanyang University, Seoul, Korea; 4Department of Biomedical Engineering, Hanyang University, Seoul, Korea; 5Department of Neurology, Seoul National University College of Medicine, Seoul, Korea; 6Department of Neurology, Dizziness Center, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea; 7Department of Neurology, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 8German Center for Vertigo and Balance Disorders, University Hospital, Ludwig-Maximilians-Universität, Munich, Germany; 9Munich Cluster for Systems Neurology (SyNergy), Munich, Germany a: These three authors contributed equally to this work as first authors.b: These two authors contributed equally to this work as corresponding authors.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Vestibular migraine (VM) has been recognized as a distinct clinical entity with recently published diagnostic criteria. Although migraine prophylactic medications can improve headache profiles and dizziness symptoms, treatment trials that focus on VM are scarce. Botulinum toxin type A (BTX-A) has been approved for prophylactic treatment of chronic and episodic migraine; however, its efficacy for migraine-related dizziness or VM has not been validated. The purpose of this study was to investigate the efficacy of BTX-A in prophylactic treatment of VM and to determine whether this treatment modulates intrinsic functional brain network connectivity.
Methods: Twenty patients (mean age 45.4 years, range 20–69 years) who satisfied the Bárány Society and International Headache Society diagnostic criteria for VM and who were refractory to conventional prophylactic therapies for more than five months had BTX-A injection and resting-state fMRI (rs-fMRI) before and 2 months after the injection. We measured the changes in the frequency of vertigo and migraine attacks, symptomatic functional disability scores, and neuropsychiatric inventories before and after the treatments.
Results: After BTX-A injection, the mean monthly frequencies of migraine and vertigo episodes decreased significantly compared to baseline (p<0.01, Wilcoxon signed rank test). The headache impact, as measured by the Headache Impact Test-6 score and the Migraine Disability Assessment, was improved (p<0.001). The vertigo parameters, measured by the Dizziness Handicap Inventory and the Vertigo Symptom Scale, showed an improvement (p<0.001), as did the anxiety and depression scores (p<0.001) 2 months after BTX-A treatment. The low-frequency fluctuation analysis of the rs-fMRI data found significant changes in functional connectivity of the right superior temporal gyrus (STG). Adoption of the right STG cluster as the seed region, increased functional connectivity with the left post-central gyrus, right supramarginal gyrus, and right middle temporal gyrus was seen after BTX-A treatment.
Conclusion: This prospective study shows that BTX-A treatment is effective at ameliorating migraine headache and vertigo symptoms in VM patients who were refractory to conventional medical therapies. Along with symptomatic improvements, changes in the functional connectivity within the multisensory vestibular and pain networks in the right temporal regions suggest that abnormal brain activity leads to dysmodulation of multimodal sensory integration and abnormal cortical processing of the vestibular and pain signals in VM patients.
FP1200Fatigability Presenting with Video-oculographic findings in Myasthenia gravis
Jin-Ju Kang, MD1, Eunsu Lee, MD1, Sun-Young Oh, MD, PhD1,2
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, Korea; 2Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Myasthenia gravis (MG) is an autoimmune disease caused by abnormal transmission of neuromuscular junction, and it is characterized by diplopia, ptosis, ophthalmoplegia and muscle weakness. And it features fatigability that means fluctuating symptoms and worsen due to muscle movement. In the early stage, the patients complain of eye symptoms, 46% of patients are not adequately diagnosed during the first year of illness. Ancillary test such as antibody assays, edrophonium test, and electrophysiologic test including repetitive nerve stimulation test, and single fiber EMG. However, gold standard of diagnosis is not defined until now. We therefore analyzed eye movement findings in myasthenia gravis using video-oculography.
Methods: We performed a total of 46 MG patients and 24 controls. All MG patients complained of ocular symptoms such as ptosis and diplopia. Patients who were positive for one or more of the repetitive stimulation test, edrophonium test, and acetylcholine receptor antibody test were selected. Video-oculography was performed the range of 20 degree was measured for 6 minutes to measure rapid eye movement, and 20 degree range for 6 minutes to measure slow eye movement.
Results: 50 repetitive saccades and smooth pursuit movements of both eyes (more and less affected eye) tested in both vertical and horizontal planes allowed for effective differentiation between MG patients and healthy subjects. Repetitive vertical saccadic eye movements yielded the best differentiation between patients with MG and controls with a sensitivity of 73% and a specificity of 92% when using a gain decrement of 9.3% as cutoff.
Conclusions Eye movements are caused by using different rates of twitch fiber and tonic fiber. If tonic fibers are mainly involved in myasthenia gravis, smooth pursuit movement can be impaired. Therefore, quantitative analysis of the slow eye movement as well as rapid eye movement in patient with MG who is showed fatigability, can be helpful in early diagnosis and understanding pathology of MG.
FP1201The Epidemiology and Clinical characteristics of Presbyvestibulopathy : A Single-Center analysis
Jin-Ju Kang, MD1,2, Sun-Young Oh, MD, PhD1,2
1Department of Neurology, Jeonbuk National University Hospital & School of Medicine, Jeonju, Korea; 2Research Institute of Clinical Medicine of Jeonbuk National University-Jeonbuk National University Hospital, Jeonju, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: The Aging of the population is a global phenomenon of the 21st century that has changed the demographic profile of many countries, experiencing the major shifts, especially in public health impacts. There is growing awareness of the impact of aging on the human sensory systems, and many studies also reported that aging has a substantial effect on the vestibular sensory system. Accordingly, in 2019, the diagnostic criteria for a new disease entity called presbyvestibulopathy (PVP) which is intended to encompass mild vestibular hypofunction attributable to the normative aging process has been proposed by the Bárány Society.
Objective: To determine the epidemiology of PVP defined recently by the Bárány Society and to reveal their clinical characteristics and laboratory findings.
Methods: Data from 1774 adult patients aged 20 years or older who visited the department of neurology at Jeonbuk National University Hospital with symptom of dizziness from January 1, 2018 to December 31, 2018 were retrospectively analyzed.
Results: Thirty-seven patients (2.1%) who met the diagnostic criteria for PVP with mild bilateral peripheral vestibulopathy documented in one or more vestibular tests, complaining of two or more symptoms lasting more than 3 months, were identified. Benign paroxysmal positional vertigo, the most important differential diagnosis, was 157 (9.0%), persistent unilateral vestibulopathy was 14 (0.8%), bilateral vestibulopathy was 5 (0.3%), functional dizziness like persistent postural-perceptual dizziness was 23 (1.3%), and orthostatic hypotension was 178 (10.2%). All patients with PVP (mean age, 73.57±9.62 years; 21 women, 56.5%) had chronic dizziness, 28 (75.7%) reported postural imbalance or unsteadiness, 16 (43.2%) experienced gait disturbance, and 10 (27.0%) presented recurrent fall. Bilaterally decreased angular vesibulo-ocular reflex gain (between 0.6 and 0.8) to video head impulse test were reported in 9 of the 24 patients evaluated. Bilateral hyporesponsiveness (sum of peak slow phase velocity on each side between 6 and 25 °/sec) was presented during bithermal caloric tests in 25 of the 32 patients who underwent testing. 14 patients had diminished angular vestibulo-ocular responses (between 0.1 and 0.3 upon sinusoidal stimulation) during rotatory chair test.
Conclusions: The emergence of new diagnostic criteria for PVP made it possible to accurately diagnose and induce effective recovery through vestibular rehabilitation by recognizing patients who had previously been considered mild bilateral peripheral vestibulopathy as a single disease entity. However, an objective definition is still required for a clear diagnosis, and consideration for the establishment of additional laboratory findings is needed.
FP1202New Norms Across the Lifespan for the modified Clinical Test of Sensory Integration and Balance (Romberg on Foam) and Tandem Walking
Phyllis Friello1, Nathan Silber2, Haleh Sangi-Haghpeykar2, Helen S Cohen
1Space Center Houston, Houston, TX, USA; 2Baylor College of Medicine, Houston, TX, USA2
Background: Although norms for adults have been published based on a small sample size no norms have been collected for children. Therefore, no data have been available on changes across the lifespan. Similarly, no data have been available for children on tandem walking with eyes closed.
Methods: Subjects aged 4 to 90 years old were recruited from among visitors to Space Center Houston. They were all participants in educational programs there and were tested by education staff. They were tested on 10 steps tandem walking with eyes closed and on three conditions of CTSIB on compliant foam with eyes closed: head still, head nodding in pitch at 0.3 Hz, and head shaking in yaw at 0.3 Hz.
Results: Preliminary resuls show classic bell curves for all tests. Norms are slightly different than those with a smaller sample under more controlled laboratory conditions.
Conclusions: These easily administered tests may be useful for screening children and adults in the community by trained staff, either in a clinical office or in other siutations where testing of vestibularly-mediated balance skill would be useful.
Supported by NIH grant 2R01-DC009031.
FP1205Differences in the clinical characteristics of idiopathic benign paroxysmal positional vertigo according to serum vitamin D status
Jae-Myung Kim, Jae-Hwan Im, Shina Kim, Hyeon-Joong Park, You-Ri Kang, Kyung Wook Kang, Tai-Seung Nam, Seong-Min Choi, Seung-Han Lee
Department of Neurology, Chonnam National University Hospital and Chonnam National University Medical School
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Benign paroxysmal positional vertigo (BPPV) is the most common peripheral vestibular disorder caused by dislodged otoconia. Vitamin D is known to be associated with homeostasis in calcium metabolism of the otolith organ. Several studies have reported that vitamin D deficiency is a risk factor for idiopathic BPPV and may influence the recurrence rate of BPPV. However, to our knowledge, no study to date has compared treatment responses and characteristics of positional nystagmus in idiopathic BPPV according to serum vitamin D levels. This study aimed to evaluate whether serum vitamin D levels lead to clinical differences in idiopathic BPPV.
Methods: A total of 217 consecutive BPPV patients were enrolled between March 2017 and February 2020. The diagnosis of BPPV was based on the diagnostic criteria of BPPV suggested by the Bárány Society. Patients with a history of inner ear diseases, head trauma, or other vestibular disorders (e.g., vestibular neuritis) were excluded. Based on serum vitamin D levels, we divided the study population into two subgroups: a ‘normal group (= 20 ng/ml)’ and a ‘decreased group (< 20 ng/ml)’. Demographics, clinical characteristics, and treatment outcomes were compared between the two groups.
Results: Vitamin D deficiency was found in 133 patients (61.3%). The mean age, sex, and subtype of BPPV (e.g., posterior canal-BPPV, horizontal canal-BPPV), and success rates of the canalith repositioning maneuver (CRM) were not different between the two groups. However, in terms of seasonal distribution, BPPV was more prevalent during autumn (27.3%) and winter (28.4%). The median serum vitamin D levels in the winter subgroup were lower than they were in the other seasonal subgroups (p<0.05). BPPV patients with vitamin D deficiency required more CRMs for successful treatment (normal group=2.01±0.89, decreased group=2.38±1.04, p=0.02). In addition, both the onset latencies (p=0.028) and the onset-to-peak latencies (p<0.001) of the nystagmus elicited by provocative positioning maneuvers in horizontal canal-BPPV were longer the group with decreased serum vitamin D levels.
Conclusions: In this study, overall demographics, vascular risk factors and subtypes of BPPV in the patients did not differ according to their serum vitamin D status. However, there was a seasonal variation in the prevalence of BPPV, and it may be related to serum vitamin D levels. Longer latencies of positional nystagmus and more CRMs were required for treatment of the vitamin D deficient group, suggesting that vitamin D deficiency may affect the character of dislodged otoconia.
FP1206Development of an artificial intelligence method for automatic measurement of hydrops ratio on inner ear MR images for Meniere’s disease
Young Sang Cho1, Chae Jung Park2, Yi-Kyung Kim4, Hyung-Jin Kim4, Baek Hwan Cho2,3, and Won-Ho Chung1
1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 2Smart Healthcare & Device Research Center, Samsung Medical Center, Seoul, Korea; 3Department of Medical Device Management and Research, SAIHST, Sungkyunkwan University, Seoul, Korea; 4Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Ménière’s Disease (MD) is difficult to diagnose and evaluate objectively over the course of treatment. Recently, several studies have reported MD diagnoses by MRI-based endolymphatic hydrops (EH) analysis. However, this method is time-consuming and complicated. Therefore, a fast, objective, and accurate evaluation tool is necessary. The purpose of this study was to develop an algorithm that can accurately analyze EH on intravenous (IV) gadolinium (Gd)-enhanced inner-ear MRI using artificial intelligence (AI) with deep learning. In this study, we developed a convolutional neural network (CNN)-based deep-learning model. The developed networks were trained for inner ear segmentation using MR images of 124 subjects and were embedded in a new automated EH analysis system, INner ear Hydrops Estimation via ARtificial InTelligence (INHEARIT). After 5-fold cross validation, an additional test was performed using 60 new unseen MR images to evaluate the performance of our system. Compared with the ratio measured by experienced physicians, the average interclass correlation coefficient (ICC) for all cases was 0.953; the average ICC of the vestibules was 0.968, and that of cochleae was 0.914. The time required for the fully automated system to accurately analyze the EH ratio in one patient’s MR stack was approximately 3.5 seconds. In this study, a fully automated full-stack MR analysis system of the EH ratio was developed, named INHEARIT, which showed high agreement with experts in an additional test. This new model can help clinicians by providing an objective analysis result and reduce their workload in reading MRIs.
FP1210Vestibular Loss Impairs Postural Corrections for Support Surface Tilts in Nonhuman Primates
Olivia M. E. Leavitt, Kathleen E. Cullen
Biomedical Engineering, Johns Hopkins University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Vestibular prostheses are an innovative and emerging technology for improving outcomes in patients with peripheral vestibular loss. The rhesus macaque is a particularly promising preclinical model for optimizing the effectiveness of vestibular prostheses, as well as providing a method for applying direct perturbations to the vestibular periphery to understand the role of the vestibular system in natural behaviors. Accordingly, here we aim to establish baselines of normal and vestibular-deficient postural responses in the awake behaving rhesus macaque. Three animals, two normal and one with BVL, assumed a natural upright posture in a behavioral chamber mounted on a six-degree-of-freedom motion platform. Three classes of perturbations were applied to the support surface on the roll axis: (i) sinusoidal stimuli comprising 6 frequencies (0.25, 0.5, 1, 2, 5, 10 Hz) with a constant peak velocity of 5 deg/s, (ii) a multisine pseudorandom stimulus containing 5 frequencies (0.25, 0.5, 1, 3, 5 Hz), and (iii) transient ramp-and-hold stimuli for which we independently varied peak velocity and peak acceleration. In response to each class of perturbation, we measured the ground reaction force on each limb with a force plate under the animal; the 6-dimensional motion of the head via a head-mounted IMU; and joint positions using video-based markerless pose estimation (DeepLabCut). In response to sinusoidal stimuli, we found that the head motion of normal animals matched that of the support surface at lower frequencies (<1Hz) but was stabilized relative to space at higher frequencies. While the BVL animal’s response was similar to that of normal animals at low frequencies, its head motion instead continued to match support surface at higher frequencies. We obtained similar results based on our analysis of the multisine stimuli, where notably the abnormal matching of head motion to support surface motion at high frequencies persisted in the BVL animal. Finally, during transient ramp-and-hold stimuli, the head motion responses of normal animals both increased in magnitude and decreased in latency with increasing peak acceleration. In contrast, during transient perturbations with increasing peak velocity, normal animals exhibited increasing magnitude head responses, but their latencies were unchanged. The dynamics of the BVL animal’s head motion also varied with support surface acceleration but strikingly the direction of response was opposite to that of normal animals. Taken together, these results suggest that BVL animals exhibit postural responses that differ measurably from normal, underscoring the role of vestibular signals in directing and modulating postural responses to perturbations.
FP1212Vestibulocollic Reflexes in Response to Natural Passive Motion and Perturbations During Voluntary Head Movements in Non-human Primates
Robyn Mildren, Omid Zobeiri, Kathleen Cullen
Department of Biomedical Engineering, Johns Hopkins University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The theme is vestibular contributions to postural stability through examining vestibular reflexes (vestibulocollic reflex in neck muscles). The target audience is clinical and basic science researchers.The vestibulocollic reflex (VCR) is thought to play an essential role in stabilizing the head in space. However, to date, the VCR has not been examined across a bandwidth of motion naturally experienced during everyday activities. Instead, the efficacy of the VCR has been inferred from head kinematics and only at low frequencies (below 4 Hz) [1]. In addition, most testing to date has been done in response to passive stimulation. Yet, in our daily lives most head motion is generated by active voluntary movement, where reflexes could be counterproductive to the intended movement goal. Thus, we predicted that the VCR would be suppressed during voluntary movement and only ungated in the face of unexpected passive perturbations.
Thus, here we first established the efficacy of the VCR by directly recording neck muscle activity during naturalistic passive whole-body motion in the yaw plane in alert rhesus monkeys (N = 2 healthy and 1 bilateral vestibular loss). We applied sinewaves, broadband white noise, and naturalistic stimuli from 0–20 Hz. Responses were recorded with indwelling EMG in the splenius capitis and sternocleidomastoid muscles. Analysis of rectified EMG and single motor unit activity revealed that VCR gain increased with frequency until ~15 Hz in splenius capitis. Further, as expected, the VCR was not observed in the vestibular loss monkey.
Next, we established the efficacy of the VCR as monkeys performed active head movements. We applied four levels of unexpected velocity-dependent perturbations to either assist or resist the intended movement. In contrast to comparable passive motion, active head movements generated minimal activity in the antagonist neck muscles. However, when perturbations influenced the intended movement velocity we observed EMG responses (increased gain) in the antagonist neck muscles that scaled with the perturbation amplitude. These compensatory responses were absent in the vestibular loss monkey, despite intact neck proprioceptive feedback.
Taken together our findings demonstrate that the VCR contributes to stabilizing the head across the bandwidth of natural motion experienced during everyday activities. Furthermore, during voluntary movement, perturbations cause an ungating of the VCR to stabilize the head in space. These reflex stabilizing mechanisms are absent following vestibular loss. Thus, these findings provide insight into the function of the VCR in stabilizing the head during activities where both passive and active self-motion are experienced by the vestibular system.
[1] Keshner FA, Peterson BW. 1995 J Neurophysiol. 73(6), 2293-301
FP1216The Three-Dimensional Angular Vestibulo-Ocular Reflex in Chinchillas Depends on Head Orientation Relative to Gravity
Margaret R. Chow1, Kristin N. Hageman1, Celia Fernandez Brillet1, Dale C. Roberts2, Americo A. Migliaccio1,3, Charles C. Della Santina1,3
1Department of Biomedical Engineering; 2Department of Neurology; and 3Department of Otolaryngology–Head and Neck Surgery – both part of Johns Hopkins School of Medicine, Baltimore, Maryland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The vestibulo-ocular reflex (VOR) maintains stable gaze during head movement. Ideally, eye movements perfectly compensate for head movement, but it is not always a one-to-one response. In a prior study, we found differences in angular VOR performance between forward-eyed squirrel monkeys and lateral-eyed chinchillas, with the former having anisotropic gain (different magnitude for different axes of rotation) and the latter, nearly isotropic. Both species had conjugate VOR responses (left and right eye move in the same direction and magnitude). That study used an Earth-vertical axis rotator with animals realigned to position each semicircular canal axis with the motor’s rotation axis. Here we examined whether chinchilla VOR responses measured using that arrangement differ from responses measured with the animal in its usual resting head/body orientation.
Methods: We measured three-dimensional VOR of twelve chinchillas during rotations starting from a natural resting position using binocular, three-dimensional scleral coil ocular recording. We rotated animals sinusoidally at 0.5, 1, and 2Hz about three cardinal axes (naso-occipital, interaural, and superior-inferior) and two axes aligned with the vertical canals (LARP: left anterior/right posterior, and RALP: right anterior/left posterior). We compared results with previously published VOR data from nine chinchillas reoriented so that each axis of interest was aligned with an Earth-vertical axis.
Results: Compared to the prior study of responses to rotations about an Earth-vertical axis, there were significant differences in responses, with anisotropic gains and disconjugacy between the left and right eye when animals started in a natural, prone position. For LARP head rotations about an Earth-horizontal LARP axis, the right eye rotates (mainly torsion) significantly less than the left (mainly pitch in eye coordinates). For RALP, the converse is true. The eyes rotate conjugately about the three cardinal axes. In an eye-fixed coordinate frame, this anisotropy follows trends of forward-eyed animals, explaining disconjugacy during certain rotations. Responses at different frequencies were similar throughout the limited range of frequencies tested.
Conclusions: Head orientation influences chinchilla VOR response. From a natural resting position, their VOR shows anisotropic characteristics, akin to forward-eyed animals, once eye responses are referenced to an eye-fixed frame rather than a head-fixed coordinate frame. Otolith-ocular-mediated tilt reflexes augment canal-ocular responses for animals rotated about an Earth-horizontal axis. That contribution is not seen during Earth-vertical-axis rotation of animals reoriented to align the LARP or RALP canals with Earth vertical (an orientation rarely encountered in an animal’s typical experience).
Support: NIH R01DC009255; MED-EL GmbH
FP1219Coexistence of Canalolithiasis and Cupulolithiasis in Lateral Semicircular Canal. Review and a case report
Diego Olmedo Gallo1, Paula Altamirano Carreño2.
1Department of Otorhinolaryngology, Hospital Clínico de la Universidad de Chile; 2Department of Otorhinolaryngologic, Clínica INDISA.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
Yes
OVERVIEW:
Benign paroxysmal positional vertigo (BPPV) is an episodic vestibular syndrome (EVS), and it is characterized by short acute vertigo crises that are related to changes in the head position relative to gravity. It can affect the posterior, horizontal and/or anterior semicircular canals (SCC). The pathophysiology of BPPV can be described by several theories, but the two classical ones are: canalolithiasis and cupulolithiasis. Specifically for the horizontal SCC (HSCC), the coexistence of the two classical variants of BPPV are not exclusive and can coexist simultaneously in the same SCC, however, this combination has only been demonstrated by experimental models; and to the date, has not been document with VNG recordings.
A brief overview and one VNG case showing a probable coexistence between canalolithiasis and cupulolithiasis of the HSCC are presented.
METHODS: One subject was registered in September 2018, who had consulted for typical symptoms of EVS in the otolaryngology service at Hospital Clínico de la Universidad de Chile.
The patient was evaluated and recorded according to the following protocol:
I. Dix-Hallpike.
II. Supine head roll test (SHRT).
III. Bow and lean test (BLT).
After the evaluation, the subject was treated with the particle repositioning maneuvers for the affected SCC.
RESULTS: The results of the case are summarized in the Table n°1.
I. Dix-Hallpike: Negative positional nystagmus.
II. SHRT:
› Left: A geotropic horizontal nystagmus (Ny) starts, it stops and then an apogeotropic Ny starts.
› Right: When turning the head, a few seconds of inertia are observed, followed by a geotropic Ny, it stops and an apogeotropic Ny starts.
III. BLT:
› Bowing: A right Ny is observed, it is reversed, and it beats with higher intensity. It stops again, and a left Ny starts.
› Leaning: It starts with a right Ny, it stops, and then a left Ny starts with lower intensity.
The presumptive diagnosis corresponds to a BPPV with a probable coexistence of canalolithiasis and cupulolithiasis in the left HSCC.
The patient was treated with the Appiani maneuver followed by the Casani maneuver (both also named Gufoni maneuver) to the left canal. After one session of each maneuver, the positional nystagmus and vertigo disappeared.
Conclussion: Due to observed parameters (nystagmus direction, duration, and latency), it is possible to determine the coexistence between a canalolithiasis and cupulolithiasis on the left HSCC, whose analysis was made based on the mathematical model’s literature pertaining to the classic variants of BPPV.
ANNEXES:
I. Table n°1:
| DIRECTION | DURATION | |
| SHRTL | → | 17″ |
| ← | >45″ | |
| SHRTR | ← | 15″ |
| → | >60″ | |
| BLT: BOWING | ← | 10″ |
| → | 30″ | |
| ← | >10″ | |
| BLT: LEANING | ← | 18″ |
| → | >20″ | |
| DIX-HALLPIKE | Negative positional nystagmus. | |
| The presumptive diagnosis corresponds to a BPPV with a probable coexistence of canalolithiasis and cupulolithiasis in the left HSCC. | ||
←: Horizontal nystagmus, beating to right.
→: Horizontal nystagmus, beating to left.
“: seconds.
II. Link to the videos (VNG):
https://drive.google.com/drive/folders/1O90RRlbPyPRnYudECufbd6cnEZGpgqty?usp=sharing
FP1234Higher risk of falls in adults with Central Auditory Processing Disorders
Yolanda R. Peñaloza-López2, Gabriel Valadez-R2, Daniel Ramos-Maldonado1, Annel Gómez-Coello3
1Otoneurology Department, Instituto Nacional de Rehabilitación, Luis Guillermo Ibarra Ibarra, México; 2Investigation Unit, Instituto Nacional de Rehabilitación, Luis Guillermo Ibarra Ibarra, México; 3Head of Phoniatrics, Instituto Nacional de Rehabilitación, Luis Guillermo Ibarra Ibarra, México.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Patients with vestibular dysfunction have attention, memory, and learning difficulties. These crucial skills are the fundamental substrate of central auditory processing. The central auditory processing disorders (CAPD) have been considered comorbidity of several pathologies; however, studies are scarce regarding the presence of these disorders in patients with vestibular dysfunction.
Objective: Evaluate the central auditory processing in patients with vestibular dysfunction and the risk of falling.
Methods: We performed a comparative cross-sectional study in subjects between 18 and 59 years of age from the National Institute of Rehabilitation LGII in Mexico City, with a diagnosis of vestibular dysfunction. The patients were divided into two groups (with and without falling risk) using the Dynamic Gait Index. The Walking While Talking test was performed with a selection of psychoacoustic tests to diagnose CAPD.
Results: We included 86 subjects; the most frequent diagnosis was vestibular dysfunction (86%), followed by benign paroxysmal positional vertigo (19%). We divided the sample into two groups through the Dynamic Gait Index, 42 with risk of falling and 44 without risk. No correlations were found between the etiology of the vestibular disorder with the risk of falling. In contrast, subjects with a risk of falling are 2.7 times more likely to have central auditory processing disorders than subjects without a risk of falling.
Discussion: In the present work, we explore central auditory processing disorder in patients with vestibular dysfunction. We demonstrated that patients with more significant vestibular dysfunction, evidenced by the risk of falls, present CAPD. The application of the Walking While Talking Test has shown that when two tasks require attention, patients with vestibular disorders fail by not having attentional skills. According to the psychoacoustic tests used, it was found that patients with vestibular disorders at risk of falling have CAPD in a higher proportion than patients without risk of falling. The conjunction of these results suggests that the auditory and vestibular pathways at central levels share anatomical-physiological areas, which are made evident by dysfunctional conditions, making deep structural anatomical investigation necessary and allowing us to expand the diagnostic tools and therapeutic tools techniques used in vestibular patients.
Conclusions: Our results open the possibility of expanding the evaluation of patients with vestibular dysfunction, as well as the possibility of studying the effects of an integral rehabilitation that includes central auditory processing and vestibular therapy.
FP1236Postoperative vestibular symptoms after stapes surgery
Takaaki Kobayashi,Yasuhiro Osaki, Katsumi Doi.
Department of Otolaryngology, Kindai University Faculty of Medicine
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Otosclerosis is an abnomal bone growth in the otic capsule that can result in hearing loss. In this study, we compared postoperative vestibular symptoms with stapes surgery.
Methods: The medical charts of 120 ears treated with stapes surgery were retrospectively reviewed.
Results: A stapedotomy, partial stapedectomy, or total stapedectomy was conducted in 45, 54, and 21 ears, respectively.
Postoperative vestibular symptoms vertigo were observed in 27.5% of subjects. Compared with cases with or without symptom of vertigo, there were no significant differences in sex, age, the way of anesthesia, affected side, flow of perilymph leakage. There were statistically higher rate of vertigo in cases with total stapedectomy than in cases of stapedotomy (p<0.01).
Conclusions: The way of fenestration of the oval footplate was suggested to be one of the risk factor of postoperative vertigo.
FP1242High Frequency Vestibular Function in Paediatric Enlarged Vestibular Aqueducts
Sudhira Ratnayake1, Soumit Dasgupta1
1Department of Audiovestibular Medicine and Audiology, Alder Hey Children’s Hospital, Liverpool, UK AND University of Liverpool, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Enlarged vestibular aqueduct (EVA) is known to cause hearing and vestibular deficits. The low-frequency vestibular function in children with EVA is published but there is paucity in high-frequency vestibular data. Our aim was to review the high-frequency vestibular function in children with EVA.
Methods: This is a retrospective case series of children with radiologically confirmed EVA (Valvassori criterion) in a tertiary paediatric centre. Those with additional labyrinthine radiological anomalies were excluded. Vestibular quantification was undertaken from 2014 to 2018.
The following details were analysed: hearing and balance complaints, dysmorphology, neuro-otological examination, audiometry (average of 500, 1000, 2000 and 4000 Hz for both Air Conduction and Bone Conduction thresholds), radiology, genetics and high-frequency vestibular quantification by video head impulse test (VHIT).
Results: During the study period, 14 children with EVA underwent VHIT, ranging from 8 to 17 years (mean age 12.1 years). Eleven (78%) were females. EVA was bilateral in 8 (57%) and unilateral in 6 (3 in each side). They presented with a range of hearing and balance features.
Audiometry showed bilateral normal hearing (<20dBHL) in 1, unilateral deafness in 5 and bilateral deafness in 8. There was 5 with sensorineural hearing loss (SNHL), 6 with mixed deafness and 2 with conductive deafness.
Pendred syndrome was confirmed in in 4. Pendrin mutation was negative in 2. One had genetically confirmed Branchio-Oto-Renal syndrome. Genetic analysis was pending in 7.
The lateral semi-circular canal (SCC) was measured by VHIT in all children. On the right lateral SCC, all had Vestibular-Ocular-Reflex (VOR) gains of >0.8 but 2 had covert saccades. On the left lateral SCC, 12 children had reduced VOR gains and 2 of these had pathological saccades. Of the 2 with normal left lateral SCC VOR gain, one had covert & overt saccades.
The vertical SCC VHIT was completed in all except one child. In the other 13 children, the left superior SCC and left posterior SCC VHIT gave a higher yield of saccadic intrusions, with and without VOR gain anomalies.
Conclusions: The VHIT assesses the high-frequency function of all six SCC. Our cases demonstrate that, especially in bilateral EVA, there could be high-frequency vestibular deficits, including saccadic intrusions, with and without VOR gain anomalies. The entire case series is undergoing Vestibular Evoked Myogenic Potential (VEMP) tests.
FP1252Stimulation Paradigms for Vestibular Implants: Stimulus Profile and Multimodal Activation
Angélica Pérez Fornos1, Anissa Boutabla1, Samuel Cavuscens1, Maurizio Ranieri1, Céline Crétallaz1, Herman Kingma2, Raymond van de Berg2, and Nils Guinand1
1Division of Otorhinolaryngology Head and Neck Surgery, Geneva University Hospitals and University of Geneva, Geneva, Switzerland; 2Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Maastricht, the Netherlands.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
The basic parameters of the electrical stimulus profile used in vestibular implant devices (phase duration, rate, etc.) have to be carefully chosen in order to optimize the efficacy of stimulation. We present data on how the electrical profile influences the dynamic range available for stimulation and the extent to which the different vestibular pathways are activated. Four patients with bilateral vestibulopathy who received a prototype implant with 1-3 vestibular electrodes (MED-EL, Innsbruck, Austria) participated in this study. First, activation thresholds and amplitude growth functions of electrically evoked vestibulo-ocular reflexes (eVOR), cervical myogenic potentials (ecVEMPs) and vestibular percepts (vestibulo-thalamo-cortical, VTC) were recorded upon stimulation with single, biphasic current pulses delivered through five different vestibular electrodes. Latencies of eVOR and ecVEMPs were also characterized. We also investigated how the velocity of the eVOR, the amplitude of the ecVEMPs, and the perceived intensity of electrically evoked percepts are affected by variations of the electrical stimulation profile (phase duration, pulse rate, baseline level, modulation depth).
The median latencies of the eVOR and ecVEMPs were 8 ms (8–9 ms) and 10.2 ms (9.6–11.8 ms), respectively. While the amplitude of eVOR and ecVEMP responses increased with increasing stimulation current, the VTC pathway showed a different, step-like behavior. Shorter phase durations and, to a lesser extent, slower pulse rates maximized the electrical dynamic range available to elicit a wider range of percept intensities. Larger dynamic ranges did not result in higher velocities of the eVOR, while current modulation depth was the main parameter affecting the velocity of eVOR responses. Simultaneous recording of these three vestibular pathways showed that the amplitude of the vestibular reflexes (eVOR and ecVEMPs) did not seem to be as sensitive to electrical stimulation as the VTC pathway responsible for conscious vestibular percepts.
This study is a first attempt to evaluate the simultaneous activation of different vestibular pathways. While shorter phase durations and slower pulse rates maximized the dynamic range available for stimulation, current modulation depth appeared as the main factor to maximize response amplitude. Our present results highlight the necessity of dedicating to this issue further and more detailed investigation to determine the actual possibility of selective stimulation of a given pathway, as well as the functional impact of the contribution of each pathway to the overall rehabilitation process. The actual possibility of selective stimulation of each vestibular pathway deserves further investigation.
FP1255Does a Mechanical Rotational Chair provide Gold Standard Diagnostics of Benign Paroxysmal Positional Vertigo?
Mathias Winther Bech1, Alexander Torp Staffe1, Dan Dupont Hougaard1,2
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: To investigate the agreement between BPPV diagnostics performed with a mechanical rotation chair and traditional diagnostics on an examination bed. Secondary objectives of this study were to 1) examine if the two test modalities differ in diagnostic properties when diagnosing uncomplicated BPPV compared to intractable BPPV and 2) examine whether impaired participant cooperation during manual diagnostics alters agreement, sensitivity and specificity.
Method: Prospective randomized clinical study in which patients with suspected BPPV were recruited from referrals by general practitioners, otorhinolaryngologists and other hospital departments in the Northern Region of Denmark. Participants underwent diagnostic testing twice: once by traditional diagnostics on an examination bed and once with a mechanical rotation chair (TRV chair®, Interacoustics©, Middelfart, Denmark. The most sensitive test modality was considered “gold standard,” to allow for calculations of sensitivity, specificity, negative predictive value, and positive predictive value. All tests were performed by the same two separate examiners. Initial examiner and order of test modality were randomized. Examiners were blinded to each other’s diagnostic test results.
Results: Agreement between the two test modalities, when testing the ability to diagnose BPPV, was 0.83: Cohen’s kappa 0.66. Sensitivity of 71 %, specificity of 98 %. Negative predictive values of 73 %, and positive predictive values of 97 % were determined for manual diagnostics when compared to diagnostics with the mechanical rotation chair. Agreement of BPPV subtype classification was found to be 0.71, and Cohen’s kappa 0.58. Agreement when isolating the diagnosis to posterior canalolithiasis (p-CAN) was 0.89, Cohen’s kappa 0.78.
Conclusions: Diagnostics aided by a mechanical rotation chair are more sensitive (and thereby accurate) than manual BPPV diagnostics. The overall agreement level between test modalities was found to be weak to moderate. When isolating diagnostics to p-CAN, the level of agreement increased from moderate to strong. Results also showed higher agreement between test modalities and a significantly higher negative predictive for manual diagnostics when examining uncomplicated BPPV. The diagnostic properties of manual diagnostics improved in cases where the examiner noted “adequate participant cooperation,” compared to cases with impaired, but acceptable participant cooperation.
FP1263Self motion perception induced by galvanic vestibular stimulation according to gravity: a fNIRS study.
Eléonore Vayssade2, Mariane Fasan2 Miora Pujol Ravalomanda1, Marc Rajoelinantenaina 1, Julie Vidal1, Maxime Rosito1, Radouane El Yagoubi2, Alexandra SEVERAC CAUQUIL1
1CerCo UMR 5549 CNRS Université Toulouse 3 Paul Sabatier, France; 2CLLE UMR 5263 CNRS Université Toulouse 2 Jean-Jaurès, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Self-motion perception relies on a central multi-sensory integration of somesthesic, visual and vestibular afferents. Galvanic stimulation (GVS) is an efficient way to artificially activate the vestibular system. Widely used in posture and balance research for decades, it is been more recently included in neuroimagery studies. Our team used it to show that anteroposterior and lateral GVS activates distinct cortical networks (Aedo-Jury et al., 2020). Nevertheless, the conscious percept induced by GVS has barely been described, neither its sensitivity to head position according to gravity. Indeed, the vestibular system is affected by the suppression of gravity: one of its two subparts, the otolithic apparatus, is still coding translation of the head, but not head tilt any more. Also, supine position of the body in the MRI scanner raises the question of sensitivity to the head orientation with respect to gravity in the cerebral construction of the self-motion percept. The present study attempts to describe the percept induced by anteroposterior and lateral GVS in both upright and lying down position, and its cortical correlates using functional Near Infrared Spectroscopy (fNIRS). We used similar anteroposterior and lateral GVS protocol and analysis as in our former fMRI study in order to 1/ validate fNIRS as a valuable tool for investigating cortical networks activated by GVS and 2/assess the effect of head position according to gravity on both the induced percept and cortical activations.The studies are carried out on 15 healthy subjects between 18 and 40 years of age, without vestibular pathology, with eyes closed and restrained to prevent any postural reaction.We hypothesize that a decreased perception of illusory movements and an increase in latency in the perception of forward self-motion could be observed in lying-down subjects. The present work will allow to establish how gravity affects self-motion perception, that could have a valuable impact on further vestibular neuroimagery studies.Aedo-Jury
F, Cottereau BR, Celebrini S and Séverac Cauquil A (2020) Antero-Posterior vs. Lateral Vestibular Input Processing in Human Visual Cortex. Front. Integr. Neurosci. 14:43. doi: 10.3389/fnint.2020.00043
FP1267Vestibular impairment is associated with specific visuospatial deficits in older adults – results from the LIFE-Adult survey
Eva Grill, Steffi Riedel-Heller, Joseph Claßen, Andreas Zwergal
German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University, Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Impairment of the vestibular system can have widespread consequences for various higher brain functions, including spatial cognition, visuospatial function, memory, attention, emotion or the regulation of sleep. While vestibular function commonly decreases with age, the implications for cognitive function and decline in older adults are still incompletely understood. Objective of the study was to examine the association of vestibular impairment with performance in cognitive subdomains in older adults.
Methods: We used cross-sectional data from the baseline survey of the population-based prospective “Leipzig Research Center for Civilization Diseases”(LIFE-Adult) cohort in Leipzig, Germany. Participants underwent structured neurophysiological and neuropsychological testing, as well as medical examinations. Vestibular function was operationalised by measuring postural control (sway path, sway area, sway velocity) by posturography with eyes open and closed and calculating Romberg’s ratios, and by testing the subjective visual vertical (SVV). To assess executive, memory and processing speed functions, participants completed the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) battery. The short form of the Judgement of Line Orientation Test (JLO) was used to quantify visuospatial function. To examine the association between vestibular function and neuropsychological test results, three Romberg’s ratios for postural performance (sway path, sway area and sway velocity) were tested in generalized linear regression models with the summary scores of executive function, memory, processing speed and visuospatial function as dependent variables. Variables with theoretical relevance for cognitive status, namely sex, age, ApoE status, socioeconomic status, mild cognitive impairment and previous history of stroke were included as covariates. As diabetes may impair postural stability by concomitant polyneuropathy we also adjusted for known diabetes in multivariable models.
Results: A total of 461 participants were analysed (mean age 68.6 years, range 56 to 80, 47.5% female). A higher Romberg’s ratio for sway area was a significant indicator for impaired visuospatial function as measured by the JLO (Odds Ratio = 1.42, 95% CI 1.07; 1.88). Romberg’s ratios were associated neither with executive or memory functions, nor with procedural speed. JLO results also showed a relevant and significant correlation with the SVV.
Conclusions: This study confirmed a cross-sectional association of vestibular and visuospatial impairment in older adults. The cognitive effects of vestibular loss might be of particular relevance in old age and a potential precondition for cognitive decline. Longitudinal studies are needed to establish causality.
FP1272Mal de Debarquement Syndrome (MdDS) a poorly understood disorder of the vestibular system
Catho Schoenmaekers1, Jan Van Riel2, Michiel Carpentier2, Tyche Perkisas4, Morgana Sluydts3, Andrzej Zarowski3, Joost van Dinther3, Dylen Philips3, Jolien Daniels1, Jitse Verstraeten1, Chloë De Laet1, Steven Jillings1, Floris Wuyts1
1Lab for Equilibrium Investigations and Aerospace, University of Antwerp, Belgium; 2 MdDS Reset, Belgium; 3European Institute for ORL-HNS, GZA Sint-Augustinus hospital, Belgium; 4electron microscopy for materials science, University of Antwerp, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Mal de Debarquement Syndrome (MdDS) is a disorder where a patient experiences a continuous perception of self-motion, like for example being on a boat, while not moving at all. A theory regarding MdDS pathophysiology is based on the Vestibulo Ocular Reflex (VOR) and velocity storage maladaptation. As soon as the patient moves passively, like for example during a car ride, the perception of self-motion disappears. Only in December 2020, the first consensus paper regarding the diagnosis and classification of MdDS by the International Bárány Society was published. This inevitably yields that many healthcare professionals are not aware of MdDS. Consequently, treatment options and symptom management strategies are poor and inadequate. Therefore, a treatment option capable of diminishing MdDS symptoms is needed.
Material and Methods: 56 MdDS patients have been treated with optokinetic stimulation combined with the roll movement of the head at a frequency of 0.167 Hz, at the European Institute for ORL-HNS in the Antwerp St Augustinus Hospital. From these 56 patients, 32 were treated with the OKN booth, 20 with the MdDS Reset virtual reality application and 4 with a combination of both. Before and after the treatment they gave a score on a VAS scale. The VAS indicates how the patient subjectively experiences the perception of self-motion, with 0 = no conplaints and 10 = maximum perception of self-motion. Also, we are currently running a clinical trial where we compare the OKN booth with a smart phone based application (MdDS Reset) and perform pre- and post-treatment MRI scans to unravel the underlying mechanism of this debilitating syndrome. Up to date, 5 patients have been enrolled in the study. We have identified 2 distinct groups based on Motion Triggered MdDS and Non-Motion Triggered MdDS.
RESULTS The difference between the pre- and post-treatment VAS score is significant (p-value < 0.001), with on average a difference of 2.81 towards a lower and thus better rating (pre 5.75 and post-treatment VAS-score 2.95). While 79% of the cohort are women, gender (Sex, p-value = 0.326), type of onset (MT MdDS or Non-MT MdDS, p-value = 0.734), and type of device (Booth0VR1 = 0.302) have no significant effect on the VAS improvement. Regarding success rate, our results show that 70% is significantly better post-treatment, 27% is status quo (no effect), and 3% is worse after the OKN treatment, whereas the worse cases were only in the non-MT MdDS group.
CONCLUSION Our results show that the given OKN treatment is successful in 70% of all patients regardless of gender, type of onset, and type of device. Additionally, the MdDS application could be a ground-braking and crucial step in the development of a portable device that can be used to alleviate MdDS symptoms, worldwide.
Figure 1
A) OKN booth and B) MdDS Reset virtual reality application, used for the OKN treatment in MdDS patients
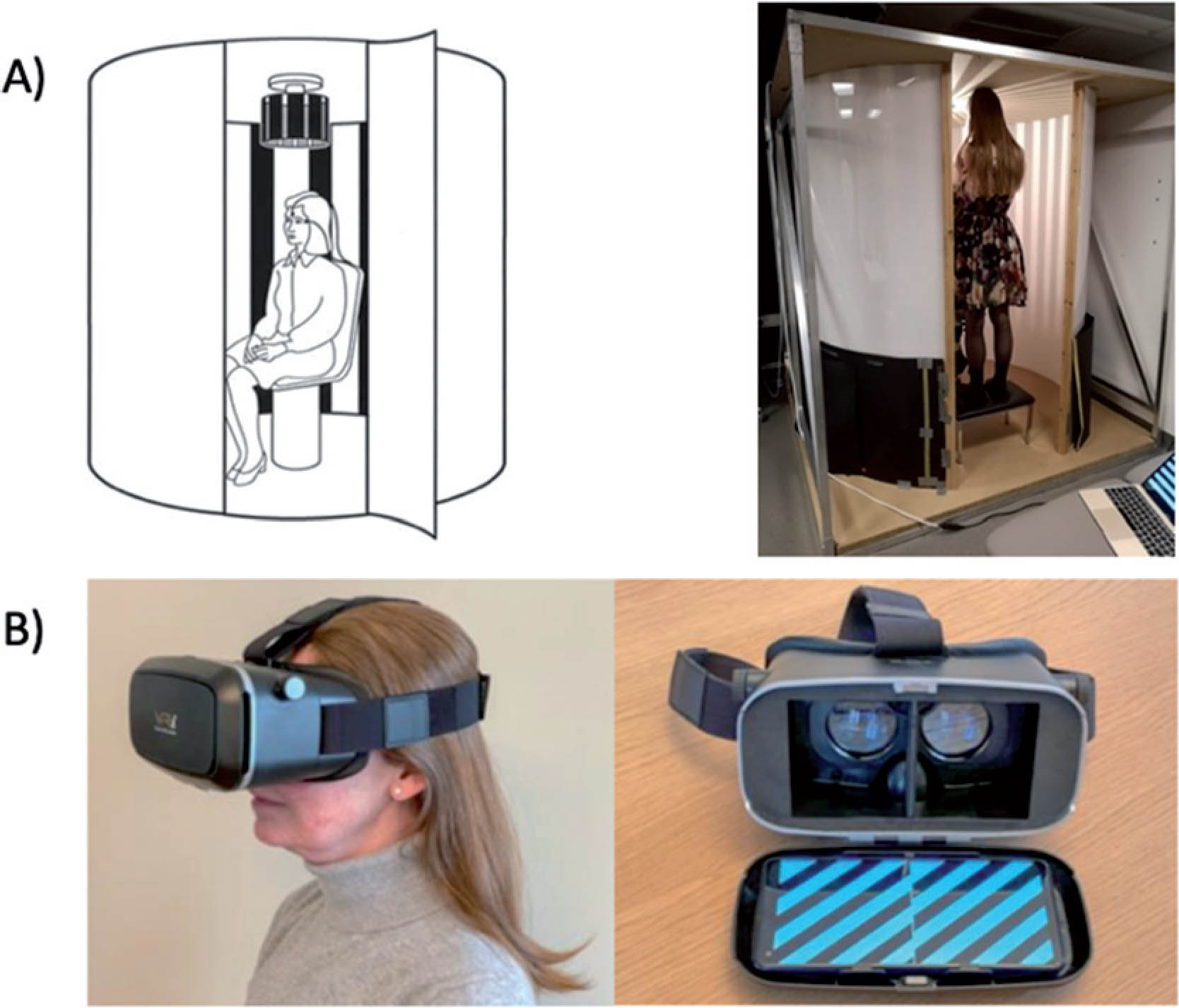
Figure 2
Success rate of the given OKN treatment in MdDS patients
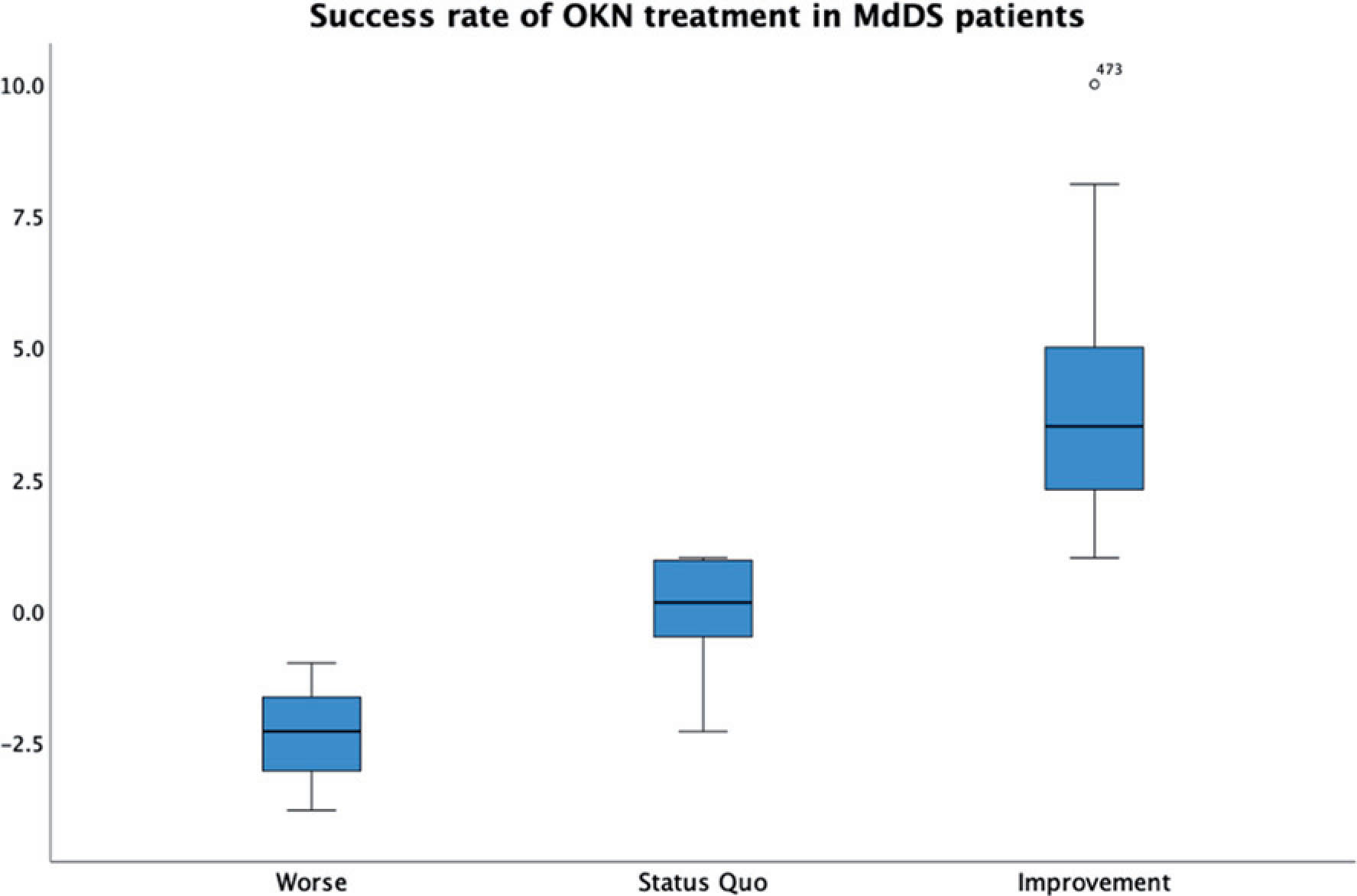
FP1273CANVAS: a case series
Pedro Marques1,2, Luis Braz3,4, Andre Fernandes3,4, Pedro Alexandre1,2 , Carla P Moura1,5,6
1Department of Otorhinolaryngology, S. João University Hospital, Porto, Portugal; 2Department of Surgery and Physiology/Otorhinolaryngology, Faculty of Medicine, University of Porto, Porto, Portugal; 3Department of Neurology, S. João University Hospital, Porto, Portugal; 4Department of Clinical Neurosciences and Mental Health, Faculty of Medicine, University of Porto, Porto, Portugal; 5Department of Genetics, Faculty of Medicine, University of Porto, Porto, Portugal; 6I3S, Institute of Research and Innovation in Health, University of Porto, Porto, Portugal
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Cerebellar ataxia with neuropathy and vestibular areflexia syndrome (CANVAS) is a recently described genetic degenerative disease affecting the vestibular and proprioceptive afferents and their cerebellar modulation. It presents itself with a significant impact in the patients’ quality of life, as this grouping can originate key disturbances on the balance system. After the discovery of the underlying genetic defect, the disease has received an increased attention.
Material and Methods: Retrospective case review of patients followed in the Otorhinolaryngology and Neurology clinics with suspected diagnosis of CANVAS, based on clinical signs of dysfunction in any the three systems affected by CANVAS (vestibular, cerebellar and proprioceptive) without other identifiable cause. These patients were submitted to an exhaustive neurological and neurotological clinical evaluation, brain MRI, video head impulse test, caloric test, dynamic posturography, electromyography/nerve conduction studies, and genetic testing for RFC1 gene pathologic expansion.
Results: Twenty patients were selected and thoroughly evaluated. Every patient characteristically reported progressive unsteadiness starting after the 5th decade. Sensory symptoms, gait ataxia and imbalance were reported by all patients and oscillopsia, dysarthria, cough and dysautonomia were variably associated. A positive familiy history was recalled by 9 patients. Most (90%) presented bilateral vestibular deficits in both video head impulse and caloric tests. The average balance score was diminished with different patterns of sensory analysis.
Conclusions: A broad and comprehensive neurologic and vestibular analysis of a large series of CANVAS patients is presented with focus on the vestibular function, increasing the understanding of this multi-system disorder, thus clarifying the picture of this (probably not so) rare disease.
FP1274The Relationship between Physical Activity and Chronic Symptoms after an Acute Unilateral Vestibular Deafferentiation: a Narrative Review
Lien Van Laer1,2, Nolan Herssens3; Ann Hallemans1,2, Vincent Van Rompaey4, Mustafa Karabulut5, Raymond van de Berg5 and Luc Vereeck1,2
1Department of Rehabilitation Sciences and Physiotherapy / Movant, Faculty of Medicine and Health Science, University of Antwerp, Belgium; 2Multidisciplinary Motor Centre Antwerp M2OCEAN, University of Antwerp, Belgium; 3Space Medicine Team HRE-OM, European Astronaut Centre, European Space Agency, Cologne, Germany; 4Department of Otorhinolaryngology and Head & Neck Surgery, Faculty University Hospital of Antwerp of Medicine and Health Sciences, University of Antwerp, Edegem, Belgium; 5Department of Otorhinolaryngology and Head and Neck Surgery, Faculty of Health Medicine and Life Sciences, Maastricht University Medical Centre, Maastricht, Netherlands
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To investigate the level of physical activity (PA) and its relation with chronic symptoms after an acute unilateral vestibular deafferentiation (UVD)
Importance: After an acute UVD, most symptoms are expected to resolve spontaneously due to central vestibular compensation. Literature revealed however, that 29 to 66% of UVD-patients develop chronic symptoms. After a UVD, PA is often advised to enhance the process of central vestibular compensation. However, (head)movements provoke symptoms, which possibly leads to avoidance behavior and consequently a lower level of PA. Hence, the level of PA, or the lack thereof, could be an influencing factor for developing chronic symptoms.
Observations: Three databases were searched for studies investigating the relation between PA and chronic symptoms in UVD-patients, which led to 1196 unique citations. After screening, eight studies were included Three cross-sectional studies objectified the level of PA (with a questionnaire, tri-axial accelerometer and wrist-worn device) and compared it between chronic UVD-patients and healthy controls, revealing a lower level of PA in UVD-patients (Figure 1). Also, significant negative correlations were found between the level of PA and dizziness, vertigo, balance performance or vestibular function in UVD-patients (Figure 2). Five interventional studies investigated the effect of a PA intervention on dizziness and balance performance, and were divided into two categories: movement sessions (Tai Chi, Lian Gong and Aquatic Physiotherapy) and technology assisted PA using a balance platform. Although all interventions led to significant improvements, only two out of five interventions showed significant effect sizes as well. When comparing the effect of a PA intervention to vestibular rehabilitation, little or no significant differences were found.
Conclusions and relevance: The evidence gathered in this review seems to confirm (1) the hypothesis that UVD-patients have a reduced PA level despite, and in contrast to, the advice to remain physically active, (2) a relationship exists between PA and chronic symptoms and (3) a structured PA intervention results in similar improvements compared to vestibular rehabilitation. This might imply that measuring PA is necessary to determine patient compliance concerning PA prescriptions, and thus enabling a timely intervention and guidance when needed.
FP1275Long-term effect of dizziness on quality of life of patients with unilateral vestibular schwannoma.
Constanza Fuentealba Bassaletti, Olaf M. Neve, Erik F. Hensen, Babette F. van Esch, Peter P.G. van Benthem
Leiden University Medical Center / LUMC
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objectives: To analyze the long-term effect of dizziness-related symptoms on the quality of life (QoL) of patients with unilateral vestibular schwannoma
Materials and Methods: This cross-sectional study was performed in a University Hospital in the Netherlands. Patients diagnosed with unilateral vestibular schwannoma between 2004-2013 were asked to participate. The study population contained patients undergoing different treatment strategies (active surveillance, surgery, or radiotherapy). Participants completed a disease specific quality of life questionnaire (Penn Acoustic Neuroma Quality of Life [PANQOL]), the Dizziness Handicap Index (DHI), and demographic questions (sex, age and level of education). Linear regression was performed to assess the effect of DHI scores on QoL. Potential confounders such as age, sex, tumor size at baseline, treatment modality were included in the model. An additional regression was performed to assess the effect of the DHI domains (functional, emotional, physical) on QoL.
Results: In total 304 participants completed both the DHI and the PANQOL. After correction for confounders such as age, sex and educational level, the DHI total score was significantly associated with PANQOL total score (-0.65 CI95% -0.72;-0.59), indicating that for each point of the DHI there is a reduction of 0.65 points in QoL on the PANQOL. The DHI emotional domain was the most prominent determinant for poorer QoL. Each point on the emotional subscale was associated with a -1.4 (CI 95% -1.8;-1.1) PANQOL score. An emotional domain score =9 will result in a PANQOL deterioration that exceeds the minimal clinical important difference of 12.5.
Conclusions: Dizziness has a significant and clinically relevant effect on the reported QoL of patients with unilateral vestibular schwannoma. Specifically, the emotional subscale of the DHI is the larger determinant of deterioration in QoL. These findings indicate that patients could benefit from receiving counselling by addressing their emotional burden, next to existing modalities of treatment.
FP1277Determinants of health-related quality of life and functioning after vestibular stroke - results from the EMVERT cohort study
Andreas Zwergal, Franziska Schuhbeck, Julian Conrad, Ralf Strobl, Ken Möhwald, Klaus Jahn, Marianne Dieterich, Eva Grill
German Center for Vertigo and Balance Disorders, Ludwig-Maximilians-University, Munich, Germany
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Stroke accounts for 5-10% of all acute vestibular presentations. However, long-term functional outcomes of vestibular stroke have not been assessed systematically. The objective of the current study was to examine the determinants and trajectories of health-related quality of life and functioning after vestibular stroke.
Methods: Patients with MRI-proven vestibular stroke (presenting with isolated vertigo, dizziness, or postural instability) were followed prospectively in the context of the EMVERT (Emergency VERTigo) cohort study at the Ludwig-Maximilians-University Munich, Germany. Health-related quality of life (HRQoL) with utility score (UT) and visual analogue scale (VAS) of the European Quality of Life scale-five dimensions-five levels (EQ5D) and vertigo-specific functioning with the Dizziness Handicap Inventory (DHI) were assessed in the acute stage and during follow-up. Anxiety state and trait were evaluated by STAI-S/STAI-T, depression by Patient Health Questionnaire-Depression (PHQ-D) questionnaires. Lesion volume and localization were analysed by voxel-based lesion mapping in normalized MRIs. Trajectories of outcomes were analysed using mixed linear regression models.
Results: A total of 36 participants were included of whom 33 were followed-up at least once for a median of 30 months (minimum one month, maximum 52 months, mean age at stroke 65.5 years, range 41 to 90, 39% female). Mean HRQoL (UT/VAS) changed not significantly from 0.691/59.2 at baseline to 0.810/65.3 at last follow-up. Mean symptom scores in DHI improved significantly from 43.6 at baseline to 17.5 at last follow-up. Higher scores of STAI-T and PHQ-D were significantly associated with worse symptom intensity at follow-up. Lesions involving the medial PICA territory overlapping the dentate nucleus regions had the worst functional outcome.
Conclusions: The average functional outcome of isolated vestibular stroke is favourable. The most relevant predictors for individual outcomes are the personal anxiety and depression traits and the lesion localization in the medial PICA territory. These factors should also be considered for therapeutic decisions in the acute stage of vestibular stroke.
FP1281Self motion perception induced by galvanic vestibular stimulation according to gravity: a fNIRS study.
Sarah Marchand1, Marine Balcou1, Philippine Picher1, Maxime Rosito1, Damien Mateo1, Nathalie Vayssiere1, Alexandra Severac-Cauquil1
1CerCo UMR 5549 CNRS Université Toulouse 3 Paul Sabatier, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
The integration of visual and vestibular information, providing information on the position and movement of the head in space, is crucial for spatial perception in humans. The combination of information from these two sensory systems takes place at several levels in the central nervous system, notably in the brainstem and cortex. A simple and effective way to selectively activate the vestibule is galvanic vestibular stimulation (GVS). This non-invasive method of stimulation consists in sending a small electric current via electrodes, affecting the vestibulocochlear nerve VIII afferents (Kwan et al., 2019), which induces oculomotor, postural responses, as well as an illusion of movement. Although this method is mostly used to induce a lateral input, there is a monopolar binaural (GVSbm) configuration of the electrodes that allows responses to be redirected in the anteroposterior plane. At the cortical level, we recently showed that visual areas V6 and VIP respond to vestibular information associated with anteroposterior movement but not to vestibular information of lateral movement (Aedo-Jury et al., 2020). The main objective of the present project is to describe the GVSbm activation combined with optical flow visual stimulation, either congruent or incongruent. 15 healthy subjects underwent 2 MRI sessions: the first aimed to localize the brain areas of interest and during the second, the subjects received visual and vestibular stimuli. The stimuli were grouped in 6 conditions: visual only forward (expanding dots), visual only backward (contracting dots), front visual and congruent GVS, rear visual and congruent GVS, front visual and incongruent GVS (mimicking a backward movement), and finally backward visual and incongruent GVS. A first-level analysis did not reveal the activation of the areas of interest. Nevertheless, the visual + GVS versus visual contrast shows a good level of activation, with symmetrical clusters in both hemispheres, corresponding to areas known to be activated by the GVS, and thus process specifically vestibular information. The congruent versus incongruent, and incongruent versus congruent contrasts show no, or very few, clusters of activation. The forward versus backward contrast shows an unexpected lateralized cluster in the right hemisphere only, while the back versus front contrast shows no lateralization. We hypothesize that ROI analysis would allow us to consider V6 as a cornerstone of sensory integration between the visual and vestibular systems, stating that this region is more activated when signals from these two modalities are congruent. Aedo-Jury F, Cottereau BR, Celebrini S and Séverac Cauquil A (2020) Antero-Posterior vs. Lateral Vestibular Input Processing in Human Visual Cortex. Front. Integr. Neurosci. 14:43. doi: 10.3389/fnint.2020.00043 Kwan A, Forbes PA, Mitchell DE, Blouin J-S, Cullen, KE (2019) Neural substrates, dynamics and thresholds of galvanic vestibular stimulation in the behaving primate. Nature Communications 10, Article number: 1904
FP1284Concepts and physiological acpects of stimulating the vestibular system
Ian Curthoys1, Sharon Cushing2
1Vestibular Research Laboratory, School of Psychology, University of Sydney, Sydney, NSW (Australia); 2The Hospital for Sick Children, University of Toronto (Canada)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Issues to be discussed: 1) Convergence of otolith and canal afferents implies that canal electrical stimulation generates otolith-related neural signals. 2) Each otolithic macula contains receptors with opposite preferred directions of stimulation, unlike the uniform polarization of receptors in each canal crista so in response to the one linear acceleration in the one macula, some otolithic afferents have an increased activation whereas others have decreased activation. Uchino has shown that at the vestibular nucleus this opposite receptor polarization generates an enhanced response to the one linear acceleration, via a “push-pull” neural mechanism between contralateral otolithic maculae in a manner analogous to the enhancement of semicircular canal responses to angular acceleration via commissural inhibition. 3) Afferents in the sustained and transient otolithic neural systems have different responses to stimulus onset vs maintained stimulation, different thresholds for activation by electrical stimulation and different adaptation rates to maintained stimulation.
FP1286Unravelling Risk Factors for Developing Chronic Dizziness after an Acute Unilateral Vestibular Deafferentiation: Preliminary Data
Lien Van Laer1,2, Ann Hallemans1,2, Vincent Van Rompaey3 and Luc Vereeck1,2
1Department of Rehabilitation Sciences and Physiotherapy / Movant, Faculty of Medicine and Health Science, University of Antwerp, Belgium; 2Multidisciplinary Motor Centre Antwerp (M2OCEAN), University of Antwerp, Belgium; 3Department of Otorhinolaryngology and Head & Neck Surgery, Faculty University Hospital of Antwerp of Medicine and Health Sciences, University of Antwerp, Edegem, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To identify predictors of chronic dizziness after an acute unilateral vestibular deafferentiation (UVD)
Introduction: After an acute UVD, symptoms are expected to resolve spontaneously because of central vestibular compensation. However, 29-66 % of the UVD-patients develop disabling chronic dizziness lasting > 1 year after the acute event. Identifying patients at risk of chronic dizziness would allow targetted therapy to improve the patients’ quality of life and reduce healthcare costs.
Methods: Between May 2021 and April 2023, a prospective cohort study will be performed in 200 patients that experienced an acute UVD due to vestibular neuritis, labyrinthitis or after a vestibular neurectomy, labyrinthectomy, vestibular neurectomy or gentamicin injection. During the acute phase and at 4, 10, 26 and 52 weeks after the acute event the following risk factors will be assessed: (1) the level of physical activity by using MOX1-activity loggers (Maastricht Instrument, the Netherlands), (2) avoidance behavior by the Vestibular-Activities-Avoidance-Instrument (= VAAI), (3) the influence of visual stimuli on the perception of verticality, balance and the level of dizziness by the Rod&Disc test, visually induced postural sway and the Visual Vertigo Analogue Scale (VVAS) respectively and (4) the level of central vestibular compensation by the video Head Impulse Test including the Perez&Rey-score (PR-score). The score on the Dizziness Handicap Inventory (DHI) at six months will be used to divide the patients into two groups: (1) chronic dizziness patients with a score > 30 and (2) non-chronic dizziness patients with a score ≤ 30. The risk factors will be used as independent variables in a logistic regression model, that predicts whether a patient will have a DHI-score above or below 30.
Results and discussion: From the beginning of May until the 15th of December 2021, nineteen patients were included of which two were assessed up to six months. A male, 80 years old, was diagnosed with a left vestibular neuritis and a female, 46 years old, with a right labyrinthitis. Neither developed chronic dizziness, although the younger female did report a higher perceived handicap due to dizziness at six months (score 18/100 on DHI). She already showed higher levels of avoidance behavior (VAAI) and visually-induced dizziness (VVAS) during the subacute phases. The level of physical activity and central compensation (PR-score) was similar in both patients (Figure 1). Although preliminary, these data already confirm variation in the process following a UVD. First publications are expected, starting from November 2023.
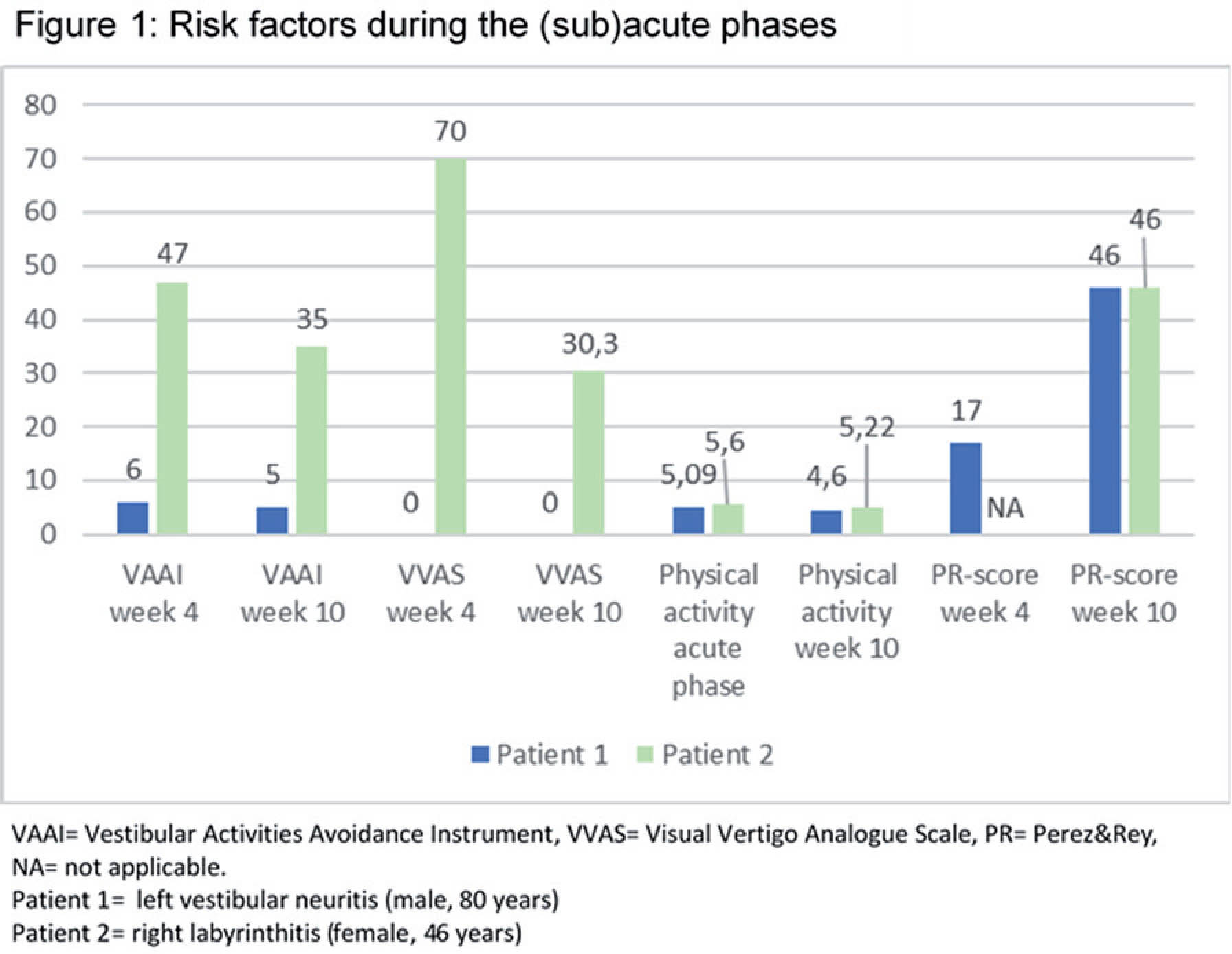
FP1290Electrical stimulation of the vestibular system: solutions in a pediatric population
Sharon Cushing
The Hospital for Sick Children, University of Toronto (Canada)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Children with profound sensorineural hearing loss have a high risk of concurrent vestibular dysfunction, with severe areflexia occurring in 30-40%. These peripheral deficits translate into balance dysfunction which impairs functional outcomes, increases risk of injury and reduces quality of life. Given that cochlear implants are housed within the same fluid filled space as the vestibular end-organs, electrical current from these arrays has the capacity to flow toward and activate the vestibular periphery. Otolithic stimulation as measured by vestibular evoked myogenic potentials can be elicited by current from the intracochlear array. Likewise, cochlear implant stimulation can improve the perception of the visual vertical. Ongoing work is investigating the benefit of coupling head position with electrical stimulation from the cochlear implant. The aim is to provide these children with some of the head referenced information that they do not receive from their dysfunctional vestibular system with the goal of optimizing their balance.
FP1293Prepulse Inhibition As A Tool For Assessing Pedunculopontine Nucleus Function In Postural Control
Matteo Ciocca, Zaeem Hadi, Mohammad Mahmud, Abed Saad, Yen Tai, Barry Seemungal
Department of Brain Sciences, Imperial College London, Charing Cross Campus, Margravine Rd, London W6 8RP, United Kingdom
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Prepulse inhibition (PPI) is a paired-pulse neurophysiological paradigm in which any subthreshold stimulus induces significant changes in the response to a subsequent suprathreshold stimulus. Measuring changes in the R2 area of the blink reflex is a reliable method to quantify PPI. More inhibition is observed when PPI is tested while standing, suggesting that PPI may be modulated in different postural conditions. Here we describe how somatosensory PPI (sPPI) from the leg is modulated in four different balance conditions. We also correlate it with sway measured on a balance platform.
We divided the experiment in four parts. In the first experiment, we record an input-output curve testing 11 interstimulus intervals (ISI) in 20 healthy subjects. In the second experiment, we investigate the effect of two different intensities of the subthreshold stimulus. In the third experiment, we tested sPPI in four different conditions (lying down, standing on hard surface, standing on soft surface, and standing on hard surface during tandem stance). In the fourth part, we collected data on sway on a force platform. For experiments 1 to 3, intensity for evoking a blink reflex was set at 3 times the motor threshold for R2, while the peripheral stimulus was delivered over the lateral aspect of the right ankle.
No significance differences between each ISI were noted. ISI 110 showed a consistent inhibition across all subjects, and it was chosen for experiment 2 and 3. An intensity of twice the sensory threshold was chosen for experiment 3. In standing on hard surface and, to less extent, on soft surface, R2 area was more reduced than in supine condition. Inhibition in tandem gait do not differ significantly from the supine condition. A correlation between sway in the antero-posterior plane and PPI was noted.
PPI is differently modulated according to the posture. A possible mechanism may lie in the different integration of tactile, vestibular, and proprioceptive inputs that contribute to posture and balance control while standing on different surface and under different circumstances. As PPI is thought to be a measure of peduncolopontine nucleus (PPN) activity, the PPN may be differently modulated by specific postural tasks. In this hypothesis, PPI may be considered a marker of PPN activity, and it can be investigated in neurological diseases with postural disorders.
FP1294A Single Centre Prospective Study on Acute Dizziness Care by Non-specialists at a Tertiary Vestibular Centre
Mohammad Mahmud1, Abdel Rahman Saad1, Mabel Prendergast2, Jordan Elliot3, Viva Levee3, Matteo Ciocca3, Barry Seemungal
Imperial College London
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Acute vertigo is a common emergency presentation amounting to 2-5% of emergency department visits with 4% of cases with balance complaints having had a stroke. Stroke doctors find vestibular presentations challenging. We assessed our stroke unit’s ability to diagnose patients presenting with an acute vestibular syndrome. We screened acute patients referred to the stroke team over a three month period (August-November 2021). We selected patients identified via key words dizziness, vertigo or imbalance, or any combination of these symptoms. We phenotyped these patients by review of case records and subsequent follow-up assessment, identifying the final diagnosis and recording any recurrence of their symptoms post-discharge and new diagnoses including recurrent or new strokes. Of the 20,310 patients who presented to ED between August and November 2021, 332 were referred to the stroke team for a suspected stroke. Of 240 cases analysed (i.e. 92 cases remain to be analysed) 36 cases presented with symptoms suggestive of a posterior circulation stroke. 19/36 (52 %) of those were diagnosed as stroke, of which 7 were transient ischaemic attacks (TIA). 5/36(13%) were discharged without a definitive diagnosis. The HINTS examination was not clearly documented or performed in 18/36 (50%). 23/36 had an in-patient MRI, 10/23 (43%)were positive for stroke. Of 36 cases assessed so far, 4 patients had a review by a vestibular specialist with the final diagnosis changing in 4/4 cases. We have followed up 16/36 patients so far. 2/16 patients had further stroke and 9/16 had no further vestibular episodes. Our provisional analysis shows that clinicians without vestibular expertise have difficulty in accurately diagnosing acute vestibular syndrome presentations.
FP1298Postoperative dizziness or vertigo after stapes surgery
Takaaki Kobayashi,Yasuhiro Osaki,Katsumi Doi.
Department of Otolaryngology, Kindai University Faculty of Medicine
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Background: Otosclerosis is an abnomal bone growth in the otic capsule that can result in hearing loss. In this study, we compared postoperative vestibular symptoms with stapes surgery.
Methods: The medical charts of 120 ears treated with stapes surgery were retrospectively reviewed.
Results: A stapedotomy, partial stapedectomy, or total stapedectomy was conducted in 45, 54, and 21 ears, respectively.
Postoperative dizziness or vertigo were observed in 27.5% of subjects. Compared with cases with or without symptom of dizziness or vertigo, there were no significant differences in sex, age, the way of anesthesia, affected side, flow of perilymph leakage. There were statistically higher rate of dizziness or vertigo in cases with total stapedectomy than in cases of stapedotomy (p<0.01).
Conclusions: The way of fenestration of the oval footplate was suggested to be one of the risk factor of postoperative dizziness or vertigo.
FP1304Acute vertigo in the emergency department: use of bedside oculomotor examination
Clovis Rau1, Lovisa Terling2, Samer Elkhodair1, Diego Kaski3
1Department of Emergency Medicine, University College London Hospitals, London, UK; 2Department of Neurology, Lund University, Sweden; 3Department of Clinical and Motor Neurosciences, 33 Queen Square, London WC1N 3BG;
Vertigo is a common symptom reportedly experienced by nearly 1 in 4 adults in the United Kingdom (UK) as well as being one of the top reasons for patients to present to the Emergency Department (ED). Differentiating between peripheral (usually benign) and central (possibly sinister) causes of vertigo ranks among the highest challenges in Emergency Medicine, and the ability to do so relies upon experience in performing a focussed oculomotor examination. The HINTS examination (an acronym of Head Impulse, direction-changing Nystagmus, and a Test of Skew) can be used to help identify posterior circulation strokes in patients with acute vertigo and one or more risk factors for stroke, but its use has not been validated in an ED setting, where it appears to be under-utilised. Here, we retrospectively evaluated current ED practice in the assessment, diagnosis, and management of 100 patients presenting with acute vertigo to a large University Hospital in the UK. Our primary aim was to establish the percentage of patients undergoing the Dix-Hallpike manoeuvre and HINTS examination in an ED setting. Of the 100 patients included in the study, 43 were male and 57 were female (male:female ratio 1:1.33). The mean age at presentation was 49.8 years. The HINTS examination was performed on 18 patients. The Dix-Hallpike manoeuvre was performed on 13 patients, and an Epley manoeuvre performed on 7 patients. Only 5 patients underwent both a HINTS examination and Dix-Hallpike manoeuvre, and no patients had a bedside test of hearing documented. The most common final diagnosis, as determined by the discharging team, was BPPV (43%), followed by acute vestibular neuritis (26%), migraine (6%), postural/orthostatic hypotension (4%), ear infections (3%), Ménière’s disease (2%) and stroke (2%). Of 41 that were given a diagnosis of BPPV by the ED team, only 10 (24%) had undergone a Dix-Hallpike manoeuvre to elicit the diagnosis. Although there is no evidence base for medication in the management of BPPV, 21 of these 41 patients were discharged with a course of prochlorperazine, rather than correcting the underlying pathology with a repositioning manoeuvre. In the 26 patients where specialty teams were involved with the patient’s care as either an inpatient or outpatient, the initial ED diagnosis was revised in 12 cases (46%), suggesting that acute ED diagnosis of dizziness and vertigo is inaccurate. Our study suggests that UK ED clinicians are not confident in using clinical examination tools such as the HINTS examination and the Dix-Hallpike manoeuvre to distinguish between peripheral and central causes of vertigo. There is a need for educational programmes to enhance the use of bedside examination in the assessment of the acutely dizzy patient, and prospective studies with formal neurootological follow-up to elicit the true incidence of conditions presenting with acute vertigo to UK EDs.
FP1306Assessment of vestibular function before and after cochlear implantation with round window approach.
Katsumi Doi, Ko Shiraishi, Takaaki Kobayashi, Syusuke Iwamoto
Department of Otolaryngology & HNS, Kindai University Faculty of Medicine
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Nowadays, the preservation of cochlear function can be highly predicted after cochlear implantation (CI) by using round window approach (RWA) with a combination of systemic and local applications of steroid during the surgery. The preservation of vestibular function might also be possible and highly expected after CI surgery with RWA.
The assessment of vestibular function before and after CI surgery (n=35) with RWA was completed by using Caloric test, vHIT (video head impulse test), cVEMP (cervical vestibular evoked myogenic potential), and oVEMP (ocular vestibular evoked myogenic potential). All the surgeries were done by a senior surgeon (KD). Dizziness immediately after the surgery was found in 17% (6/35 case), while no dizziness in 83%. As for Caloric test, CP% before and after the the CI surgery was 27.4% and 28.3%, respectively. There was no statistical difference between them (P=0.43). As for vHIT, VOR (vestibul0-ocular reflex) gain for horizontal SCC (semicircular canal) before and after the surgery was 0.94 and 0.89, respectively. There was no statistical difference between them (P=0.22). VOR gain for anterior SCC (semicircular canal) before and after the surgery was 1.16 and 1.14, respectively. There was no statistical difference between them (P=0.38). VOR gain for posterior SCC (semicircular canal) before and after the surgery was 0.98 and 1.00, respectively. There was no statistical difference between them (P=0.41). As for cVEMP, AR (asymmetry ratio of r-and l-potentials) before and after the surgery was 26.6% and 32.0%, respectively. There was no statistical difference between them (P=0.22). As for oVEMP, AR (asymmetry ratio of r-and l-potentials) before and after the surgery was 21.7% and 20.7%, respectively. There was no statistical difference between them (P=0.44).
These results suggest that the preservation of vestibular functions after our CI surgery with RWA should be excellent. Systemic and local applications of steroid during the surgery would be strongly recommended to reinforce it.
FP1307A ‘shoulder tap’ test for functional gait disorders: a sign of abnormal anticipatory behaviour
Coebergh J1,2, Zimianiti I3, Kaski D4
1Ashford St Peter’s NHS Foundation Trust, London UK; 2St George’s NHS Foundation Trust, London, UK; 3Imperial College London, School of Medicine, London, UK; 4Centre for Vestibular and Behavioural Neurosciences, Institute of Neurology, University College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Objective: To describe the range of postural responses to the pull test in patients with functional gait disorders (FGDs) and explore the utility of the ‘shoulder tap test’ in these patients.
Methods: Patients with a diagnosis of FGD were identified from movement disorders clinics at Ashford St Peter’s and St George’s University Hospitals NHS trusts. Reactions to being ‘tapped’ at the shoulders or pulled were retrospectively analysed using clinical records. For the shoulder tap test, patients were instructed that “on the count of three please try to keep upright if you are moved backwards” and that they were allowed to take as many steps as needed to avoid falling.
Results: Thirty-one patients with FGDs in whom responses were documented to either shoulder tap, pull test, or both were included in the analysis (mean age: 59.65 ± 15.27 years). All patients in whom a shoulder tap was performed (n=25) had an abnormal response, including taking multiple steps (n=9), significant body sway or a startle response (n=4), falling into the examiner’s arms (n=7), or anticipatory body movement before being tapped (n=4). Abnormal responses to pull were documented in 14/17 patients (82.35%).
Conclusions: The ‘shoulder tap test’ was abnormal in all patients with FGD, even in those with a normal pull test, and may reflect postural hypervigilance and abnormal expectation in these individuals.
FP1309Bone Conduction Transmission in VEMP Testing
Bo Håkansson1, Karl-Johan Freden Jansson1, Måns Eeg-Olofsson2, Luca Veerecchia3,4, Sabine Reinfeldt1
1Department of Electrical Engineering, Chalmers University of Technology, Gothenburg, Sweden; 2Department of Otolaryngology, Head and Neck Surgery, Sahlgrenska Academy, Gothenburg, Sweden; 3Department of Ear Nose and Throat, Audiology and Neurotology, Karolinska University Hospital, Stockholm Sweden; 4Ear Nose and Throat Unit, CLINTEC Department, Karolinska Institutet, Stockholm, Sweden.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Using air conduction (AC) stimuli for evoking vestibular evoked myogenic potentials (VEMP) require relatively high sound levels and the use is limited to patients without conductive hearing loss. By using BC stimuli a conduction loss can be by-passed and it has recently been shown that the hearing levels can be reduced by 35-41 dB with a 250 Hz burst stimuli*. In these tests a new BC transducer (B250) specifically intended for BC-VEMP investigations at 250 Hz, was used. Questions have been raised on how vibration from BC stimulation reach the vestibular organ at both sides. In this study different stimulation positions and BC transmission to the vestibular organ are investigated.
Methods: First, the mechanical impedance of the human head from previous studies were analyzed to determine the skull movements using BC stimuli over the skin. Secondly, a single sine 250 Hz (4 ms) BC stimuli was applied using a B250 and a Minishaker at the mastoid, forehead and vertex. The resulting velocity at the skin level over both mastoids behind the ear was recorded using a laser Doppler vibrometer (LDV). The LDV response was analyzed to determine delay time, amplitude and phase dependence in relation to the mechanical stimuli. Electro-mechanical simulations were also performed to verify the experimental results.
Results and discussion: From the impedance measurements it was concluded that the skull moves like rigid body at 250 Hz except for a local compliance around the attachment point. Both vestibular organs are thus assumed to move essentially in phase when stimulated at the mastoid. This finding was also indicated by the preliminary LDV measurements and in electro-mechanical simulations. This means that when stimulating at the forehead or the vertex, an inward force results in an outward velocity at the mastoid skin surface on both sides. This may be explained by that the cranial vault flexes inwards and thus the skull sides flexes outwards.
Conclusions: Preliminary results suggest that a mastoid BC vibration creates an in phase motion of the vestibular apparatus when the stimuli is applied at the mastoid and essentially an out of phase motion when applied at the vertex or the forehead.
Footnote *: Håkansson et al., VEMP using a new low frequency bone conduction transducer, Medical Devices: Evidence and Research 2018:11, 301–312.
Fredén Jansson et al., Bone Conduction Stimulated VEMP Using the B250 Transducer, Medical Devices: Evidence and Research 2021:14 225–237.
FP1311How unsteady do you feel you are? Instability perception in unexplained dizziness
Patricia Castro1,2, Richard Ibitoye1, Diego Kaski3, Toby Ellmers1, Adolfo Bronstein1
1Department of Brain Sciences, Neuro-otology, Imperial College London, London, UK; 2Universidad del Desarrollo, Escuela de Fonoaudiología, Facultad de Medicina Clínica Alemana, Santiago, Chile; 3Department of Clinical and Motor Neurosciences, Centre for Vestibular and Behavioural Neurosciences, University College London, London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Introduction: Body sway and perceived instability are tightly correlated in healthy subjects. However, a substantial proportion of older adults describe themselves as almost constantly dizzy or unstable without an identifiable cause, hence evidencing a de-coupling between objective and subjective stability. Here, we investigate the relationship between objective and subjective instability in patients with unexplained dizziness and in patients with no vestibular function to understand the role of the peripheral input in this relationship.
Methods: Thirty patients with unexplained dizziness in the elderly (UDE) and 13 patients with bilateral vestibular hypofunction (BVH) with their corresponding age matched controls experienced external perturbations to their balance. We measured objective (upper trunk sway, steps taken) and subjective (self-reported) instability, and anxiety.
Results: Body sway and subjective instability were significantly related in both patients’ groups, following a logarithmic function. However, UDE patients reported more instability for the same amount of body sway when compared to controls. Sway path was not different between UDE and controls, but was larger in BVH than controls. Preliminary analysis revealed that patients with UDE present a lower “step-generation threshold”, whereby they generate a step or foot lift with a smaller stimulus than controls. This was not observed in the BVH group.
Conclusions: Our data confirms the strong relationship between objective and subjective instability in two patient groups. Interestingly, patients perceive higher instability when facing a similar amount of body sway, suggesting a distorted sense of instability. As expected, BVH patients sway significantly more than controls hence their perception of instability follows objective instability, unlike UDE patients. Nonetheless, step generation was earlier for UDE patients, suggesting a balance difficulty which could account for some of their increased subjective instability. As cerebral small vessel disease (SVD) likely contributes to the UDE syndrome, SVD may also interfere with internal estimates of self-stability.
FP1314Clinician’s perspectives of Head Impulse-Nystagmus-Test of Skew for Acute Vestibular Syndrome.
Charlotte L. Barrett1, Lisa Bunn2, Nehzat Koohi3, Gunnar Schmidtmann2, Jenny Freeman2, Diego Kaski3
1North Bristol NHS Trust, University of Plymouth; 2Faculty of Health, School of Health Professions, University of Plymouth; 3Institute of Neurology, University College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Acute vestibular syndrome (AVS) features continuous dizziness and may result from a benign inner ear disorder or potentially life-threatening stroke. Misdiagnosis is common and can lead to poor long-term outcome. An oculomotor bedside assessment, the Head Impulse-Nystagmus-Test of Skew (HINTS) is more sensitive than brain Magnetic Resonance Imaging in identifying stroke as the cause of AVS within the first 48 hours, when applied by specialist clinicians. Clinicians’ perspectives of the test in secondary care remains unknown. Here, we explore frontline clinicians’ perspectives of use of the HINTS
Methodology: Clinicians from two large UK hospitals who assess AVS completed a short online survey, newly designed with closed and open questions.
Results: Almost half of 73 total responders reported limited, or no experience (n=19), reflected in low rates of use (n=31) of HINTS. Whilst the potential utility of HINTS was recognised, many reported concerns about subjectivity, need for specialist skills and poor patient compliance. No clinicians reported high levels of confidence in performing HINTS, with 98% identifying training needs. A lack of formalised training was associated with onward specialist referrals and neuroimaging (p=.044).
Conclusions: We identified barriers to the application of the HINTS and training needs to improve rapid, cost effective and accurate clinical diagnosis of stroke presenting with vertigo.
FP1316Predicting Factors for Prolonged Vestibular Rehabilitation Therapy in patients with Unilateral Vestibular Hypofunction and Bilateral Vestibulopathy
Phoebe Ramos1,2, Dinko Vuskovic3, Magdalena Eyzaguirre2, Hayo Breinbauer2,3,4
1Department of Otolaryngology, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile; 2Department of Otolaryngology, Facultad de Medicina Clinica Alemana, Universidad del Desarrollo, Santiago, Chile; 3Department of Otolaryngology, Facultad de Medicina, Universidad de Chile, Santiago, Chile; 4Department of Neurocience, Facultad de Medicina, Universidad de Chile, Santiago, Chile.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Overview: Vestibular rehabilitation (VR) is one of the main treatments for vestibular disorders. Most patients with peripheral vestibular disorders experience significant improvement following VR, as well as patients with bilateral vestibulopathy and central etiologies. VR must be individualized and focused on patient’s symptoms and specific vestibular deficiency, identifying factors that may influence the patient’s rehabilitation progress. To our knowledge there is scarce literature describing predicting factors that may influence and anticipate total time needed for these patients to complete VR. The purpose of this study is to describe our institution’s VR program and predicting factors associated with prolonged therapy.
Methods: A prospective study was conducted of all patients treated with our institution’s VR program at Clinica Alemana Santiago, Chile between the years 2019 and 2020 with the diagnosis of unilateral vestibular hypofunction or bilateral vestibulopathy. All evaluated variables were submitted to a database and analyzed through multivariate regression.
Results: Our vestibular rehabilitation program relies on an “on-demand” paradigm, where patients are seen once per week for 60 minutes (90 minutes on their first session), until symptoms are solved. During this process, several assessments are conducted, including the Dynamic Gait Index, Time Up and Go Test, walking speed, and the Dizziness Handicap Index (DHI) among others. We completed 227 therapeutic processes where these variables were reliably obtained. 12 % of patients abandoned therapy without a satisfactory outcome in terms of symptoms. From the remaining 88%, 82% of patients with positive outcome, solved their symptoms with 3 sessions or less (two weeks from beginning to end). 8% of patients required more than 8 sessions (more than 2 months) of therapy. A multivariate regression analysis was conducted to identify predictors of the amount of therapy needed before reaching success. From this analysis the main predictor for a prolonged therapy was a poor Dynamic Gait Index outcome (b=0.52), while other aspects such as age, DHI value, gain at vHIT recordings or abnormalities in VEMP testing had little impact on recovery speed (b<0.12 in all cases).
Conclusion: Recognition of predicting factors that may influence patients VR amount of therapy needed is key to evaluate patients’ recovery and final outcomes. In this study age, DHI value, gain at vHIT or VEMP abnormalities had little impact on speed recovery. Whilst low Dynamic Gait Index value was the main predictor for a prolonged VR therapy. Although there is strong evidence that backs up the benefits of VR, there are still important questions whether which patients would be more benefited by this type of therapy. Predicting factors may help identify treatment frequency and total duration, identifying patients that may need more intense therapy than others to set realistic expectations.
FP1318Innovative Dynamic Posturography Tasks to Complement Vestibular Disorders Diagnosis
Phoebe Ramos1,2, Hayo Breinbauer2,3,4
1Department of Otolaryngology, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile; 2Department of Otolaryngology, Facultad de Medicina Clinica Alemana, Universidad del Desarrollo, Santiago, Chile; 3Department of Otolaryngology, Facultad de Medicina, Universidad de Chile, Santiago, Chile; 4Department of Neurocience, Facultad de Medicina, Universidad de Chile, Santiago, Chile
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Overview: Posturography evaluates the interaction and contribution of vestibular function with other functions such as proprioception, visual component, and their central integration in balance performance to be able to maintain correct stability during expected and unexpected altercations. All this done through an integrated dynamic system with virtual reality that measures postural oscillation when exposed to different stimuli. Sensory Organization Test (SOT) are the most frequent tasks used to evaluate balance components. Different research protocols beyond SOT have been described trying to correlate and to add diagnostic value to other vestibular disorders, proving that posturography is a very versatile tool. Posturography at our institution evaluates additional parameters to complement diagnosis of other balance disorders such as persistent postural perceptual dizziness (PPPD) and vestibular migraine (VM), among other.
Methods: To describe the different tasks added to our institution’s Dynamic Posturography and how analyzing these tasks may allow to complement vestibular disorders diagnosis such as PPPD and VM, among other.
Results: Cognitive tasks such as math additions and substructions, naming fruits and vegetables that start with specific letters while performing SOT 5 (cognitive task) and SOT 6 (cognitive and visual simultaneous tasks) help with diagnosis of PPPD. Balance performance metrics improve in these patients while being concentrated in cognitive tasks. Simple optokinetic stimuli while performing SOT 4 (optokinetic stimuli), as well as applying tunnel optokinetic stimuli while performing SOT 4 (complex visual stimuli) help complement diagnosis of VM. Balance performance metrics drop while being exposed to visual stimuli specially with complex visual stimuli, characteristics that can also be seen in patients with PPPD. Adding head turns to SOT 6 (vestibular stimuli) and, adding head turns to tunnel optokinetic stimuli while standing on a foam platform (vestibular visual stimuli) help decompose balance components, specifically isolating the vestibular component. Considering a total of 109 posturography tests, we have found a strong correlation of cognitive demanding subtasks (including the addition of cognitive challenges during classical SOT settings) with PPPD (r=0.78) and subtasks including visually complex stimuli (optokinetic tunnel) during classical SOT settings with VM (r=0.72).
Conclusion: Adding cognitive and visual tasks, as well as head movements to already known and internationally used SOT in dynamic posturography improves and complements vestibular disorders diagnosis. And may as well, be useful for a more targeted and personalized vestibular rehabilitation in these patients.
FP1319Validation of an Automated Head Impulse System
Desi Schoo1, Andrianna Ayiotis2, Celia Fernández Brillet2, Margaret Chow2, Grace Tan1, Matthew Ehrenberg1, John P Carey1, Charles C Della Santina1,2
1Johns Hopkins School of Medicine, Department of Otolaryngology-Head and Neck Surgery; 2Johns Hopkins University, Department of Biomedical Engineering
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The video head impulse test (vHIT) enables canal-specific assessment of semicircular canal function. Automating delivery of head impulses with a motorized unit may decrease the test’s operator dependence while increasing consistency and reliability of stimuli and responses. Past work studying subjects without known vestibular dysfunction demonstrated that an automated head impulse test (aHIT) system can deliver head impulses in each of the six semicircular canal planes with motion profiles that are similar to manually-delivered impulses but less variable. In the present study, we sought to characterize performance of the aHIT system when used to assess patients with vestibular dysfunction.
Methods: Nine patients under clinical evaluation for symptoms consistent with bilateral vestibular hypofunction were enrolled in the study. Each participant underwent concurrent 6-canal vHIT testing with head impulses delivered manually and via the aHIT. The GN Otometrics ICS Impulse system was used for data collection. Eye and head movement data were analyzed with a custom MATLAB program, which allowed analysis of every head impulse, rather than only those accepted for analysis by the system’s turn-key software. We compared peak head velocity and acceleration, width of the head motion waveform, vestibulo-ocular reflex (VOR) gain, and VOR latency for manually and motorized impulses.
Results: Data from a total of 52 canals were assessed with both manual and automated testing. There was no statistically significant difference in the VOR gain measurements between head impulses applied manually as opposed to automatically; however, there were statistically significant (p<0.05) decreases in the variances of peak head velocity and acceleration, head impulse width, VOR gain, and VOR latency.
Conclusions: These findings support the use of the aHIT system in conjunction with a commercially available vHIT system to evaluate patients with vestibular dysfunction. The aHIT delivered more consistent and reliable head impulses compared to a clinician tester, resulting in decreased inter-impulse variability of head motion profile and VOR gain.
Support: NIH R01DC1356, U01DC0019364, T32000027; Equipment provided by Labyrinth Devices LLC
FP1320The Effects of vibro-tactile Biofeedback Training on Balance Control and Dizziness in patients with Persistent Postural Perceptual Dizziness (PPPD)
Heiko Rust, Flurin Honegger, Claudia Candreia and John Allum.
Departments of ORL, University of Basel Hospital, Basel, and Cantonal Hospital, Luzern Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Patients with PPPD frequently report on being “off-balance”. Systems providing sensory substitution of natural sensory signals are known to improve balance control. The question arises whether such artificial systems improve dizziness and balance control in patients with PPPD. Therefore, we assessed the effects of vibro-tactile feedback training (VT-fb) of trunk sway on balance control during stance and gait tests and on perceived dizziness in patients with PPPD of primary (no organic) and secondary (with organic) origin.
Methods: Balance control during stance and gait tests was assessed in 11 patients with PPPD using a SwayStar SystemTM. The Dizziness Handicap Inventory (DHI) was used to assess dizziness. Patients with central vestibular lesions were excluded. Subjects first underwent a standard balance assessment from which vibration thresholds in 8 directions were calculated for each assessment test based on 70% of the maximum trunk sway in the pitch and roll directions for the test. A head mounted vibrotactile-feedback system (VT-fb), connected to the SwayStarTM system was active in 1 of the 8 directions when the threshold for that direction was exceeded. Subjects trained with the feedback system twice per week for a total of 3 consecutive weeks. Balance in the form of a combined test index (BCI) and DHI were reassessed each week and the thresholds reset.
Results: The 9 patients with secondary PPPD showed improved balance control after 3 weeks VT-fb training. Six of these subjects also had lower DHI values after the training. The 2 patients with primary PPPD had worse balance control with only one subject reporting a subjective benefit.
Conclusions: These initial results show that in a majority of secondary PPPD subjects an improvement of balance control and DHI assessed dizziness was evident after VT-fb training. For primary PPPD patients no balance improvement was present. Thus selection criteria need to be established indicating which PPPD patients could benefit subjectively from sensory substitution procedures during balance control. Because no improvement in balance control was registered with primary PPPD patients and no subjective improvement in dizziness for some of the secondary PPPD patients, our results point to the expected dissociation between balance control and preceived symptoms of dizziness in those with PPPD.
FP1322Changes in postural stability in patients with symptoms of dizziness or vertigo with overweight or obese
Background: The National Health and Nutrition Survey in Mexico reports that in adults aged 20 years and over, the combined prevalence of overweight and obesity is 72.5%. These are related to cochleovestibular and neurological damage, like disability and deterioration of quality of life.
Objective: Determine and compare the characteristics of vestibular function and postural stability in symptomatic patients with normal weight, overweight, and obesity.
Methodology: Observational, analytical cross-sectional study. We included patients of both genders, aged 18 to 59 years, with vestibular symptoms, dizziness, and postural instability. We perform a descriptive analysis and Cramer’s V for all the variables.
Results: The predominant symptom was dizziness (69%), followed by vertigo and instability (54% each), mainly in overweight and obese patients. In the sensory organization test (SOT) in the posturography (Equitest Neurocom, Natus, Denmark) was observed that the performance was decreasing with the progress of the conditions evaluated (regardless of the nutritional status), and those with overweight present a lower performance than the group with normal weight (especially in conditions 4, 5 and 6; where they have in common a mobile platform with a more significant challenge to the vestibular system). In the V-HIT, we obtain a significant gain on the left side, but there is no diminished global gains. In the Cramer’s V, we observed a moderate effect of the weight with instability, with no impact on vertigo, dizziness, or falling risk.
Conclusion: Our study observed that overweight and obese subjects present an ocular vestibule function (studied with VHIT) within normal parameters. In contrast, the postural control given by the integration of the spinal vestibule reflex is deficient when performing a greater range of movement. Gravitational orientation depends on complex posturographic conditions; associated with alterations in somatosensory perceptions integrated into the balance system. More studies are required to achieve specific targets of therapies for these conditions.
FP1323Balanced Growth project: a Single-center Observational Study on the Involvement of the Vestibular System in a Child’s Motor and Cognitive Development
Ruth Van Hecke1, Frederik J.A. Deconinck2, Jan R. Wiersema3, Chloe Clauws1, Maya Danneels1, Ingeborg Dhooge4,5, Laura Leyssens1, Hilde Van Waelvelde1, Leen Maes1,5
1Ghent University, Department of Rehabilitation Sciences, Ghent, Belgium; 2Ghent University, Department of Movement and Sports Sciences, Ghent, Belgium; 3Ghent University, Department of Experimental-Clinical and Health Psychology, Ghent, Belgium; 4Ghent University, Department of Head and Skin, Ghent, Belgium; 5Ghent University Hospital, Department of Otorhinolaryngology, Ghent, Belgium;
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Introduction: The involvement of the vestibular system in the motor and higher (cognitive) performances of typically developing or vestibular-impaired children is currently unknown or has only scarcely been explored. Interestingly, arguments for an interaction between vestibular, motor and cognitive functions in children can also be supported by research on children known for their difficulties in motor and/or cognitive processing (eg, children with neurodevelopmental disorders (NDD)), as they often present with vestibular-like characteristics. Therefore, in order to elucidate this interaction, and to increase the understanding of the pathophysiology and symptomatology of vestibular disorders and NDD in children, the Balanced Growth project was developed. It includes the following objectives: (1) to understand the association between motor skills, cognitive performances and the vestibular function in typically developing school-aged children, with special focus on the added value of the vestibular system in higher cognitive skills and motor competence; (2) to investigate whether a vestibular dysfunction (with/ without an additional auditory disease) has an impact on motor skills, cognitive performances and motor–cognitive interactions in children and (3) to assess if an underlying vestibular dysfunction can be identified in school-aged children with NDD, with documentation of the occurrence and characteristics of vestibular dysfunctions in this group of children using an extensive vestibular test battery.
Methods and analysis: In order to achieve the objectives of the observational cross-sectional Balanced Growth study, a single-task and dual-task test protocol was created, which will be performed in three groups of school-aged children (6–12 years old): (1) a typically developing group (n=140), (2) (audio) vestibular-impaired children (n=30) and (3) children with an NDD diagnosis (n=55) (ie, autism spectrum disorder, attention deficit/ hyperactivity disorder and/or developmental coordination disorder). The test protocol consists of several custom made tests and already existing validated test batteries and includes a vestibular assessment, an extensive motor assessment, eight neurocognitive tests, a cognitive–motor interaction assessment and includes also additional screenings to control for potential confounding factors (e.g., hearing status, intelligence, physical activity, etc.).
Ethics and dissemination: The current study was approved by the ethics committee of Ghent University Hospital on 4 June 2019 with registration number B670201940165 and is registered at Clinical Trials (clinicaltrials.gov) with identifier NCT04685746. All research findings will be disseminated in peer-reviewed journals and presented at vestibular as well as multidisciplinary international conferences and meetings.
FP1324Serum Albumin Levels as a Potential Marker for the Predictive and Prognostic Factor in Sudden Sensorineural Hearing Loss: A Prospective Cohort Study
Zhong Zheng1, Chengqi Liu1, Ying Shen1, Liang Xia1, Hui Wang1, Zhengnong Chen1, Yaqin Wu1, Haibo Shi1, Yanmei Feng1, Shankai Yin1
Shanghai Jiao Tong University Affiliated Sixth People’s Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objectives: As a common otology emergency, sudden sensorineural hearing loss (SSNHL) has a great impact on quality of life. The diagnosis and treatment of SSNHL remain challenging. This study aims to identify and investigate the association of liver functions with SSNHL. Methods: A total of 135 SSNHL patients and 135 sex- and age-matched controls were prospectively enrolled. The baseline and clinical characteristics, along with liver function levels of participators, were collected. Linear correlation, logistic regression, and receiving operator characteristic curve analysis tests were applied to examine the association between liver function levels and SSNHL. Results: There were no differences in baseline characteristics between SSNHL and control groups. The albumin (ALB) level of the SSNHL group was significantly lower than that in the control group (p < 0.001). The logistic regression showed that the low ALB level may be a predictive factor of SSNHL with an adjusted OR of 0.809 (95% CI, 0.742–0.882, p < 0.001). By comparing the indicators of different prognosis groups, we found that the effective group had a significantly lower hearing impair onset and higher ALB (p = 0.001) and AGR (p = 0.003) levels than the ineffective group. Logistic regression revealed that the hearing level onset (OR, 0.976; 95% CI, 0.956–0.997; p = 0.026) and ALB level (OR, 1.181; 95% CI, 1.071–1.301; p = 0.001) showed strong associations with treatment outcome.
Conclusions: Lower ALB levels, within the normal ranges, were associated with the occurrence and unfavorable outcome of SSNHL. However, further research on the underlying mechanisms needs to be conducted.
FP1325Thyroid-Related Hormone Levels in Clinical Patients With Moderately Severe-to-Profound Sudden Sensorineural Hearing Loss: A Prospective Study
Zhong Zheng1, Ying Shen1, Liang Xia1, Hui Wang1, Zhengnong Chen1, Yaqin Wu1, Haibo Shi1, Yanmei Feng1, Shankai Yin1
Shanghai Jiao Tong University Affiliated Sixth People’s Hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objectives: Sudden sensorineural hearing loss (SSNHL) is a common otological emergency, causing a measure of hearing loss and affecting the quality of life. This study aims to investigate the association of thyroid-related hormone levels with moderately severe-to-profound SSNHL. Methods: The study included 70 patients with moderately severe-to-profound SSNHL and 100 age- and sex-matched healthy controls. Peripheral venous blood samples were taken from the participants, and their thyroid-related hormone levels were measured at admission and 1 week after treatment. Results: In moderately severe-to-profound SSNaHL patients, the concentrations of total triiodothyronine (TT3), total thyroxine (TT4), free triiodothyronine (FT3), and thyroid-stimulating hormone (TSH) (all P < 0.05) were significantly lower than in the control group. The TT3, TT4, FT3, and TSH levels were significantly higher in the effective group than in the ineffective group (all P < 0.05). Linear correlation analysis revealed that TSH level (R = 0.707, P < 0.05) elevation after treatment successfully predicted a favorable outcome of hearing recovery. Logistic regression analyses suggested low FT3 and TSH levels to be independent occurrence predictors, while the increase of TSH level may be an independent favorable outcome predictor.
Conclusions: The results suggest that low FT3 and TSH levels are risk factors for moderately severe-to-profound SSNHL. By discovering the positive association between TSH elevation and hearing recovery, along with the potential novel predictors of FT3 and TSH, our study may contribute valuable insights to the research and treatment of moderately severe-to-profound SSNHL.
FP1326Vestibular Function in Children with Neurodevelopmental Disorders: A Systematic Review.
Ruth Van Hecke1, Maya Danneels1, Ingeborg Dhooge2,3, Hilde Van Waelvelde1, Jan R. Wiersema4, Frederik J.A. Deconinck5, Leen Maes1,2
1Ghent University, Department of Rehabilitation Sciences, Ghent, Belgium; 2Ghent University Hospital, Department of Otorhinolaryngology, Ghent, Belgium; 3 Ghent University, Department of Head and Skin, Ghent, Belgium; 4Ghent University, Department of Experimental-Clinical and Health Psychology, Ghent, Belgium; 5Ghent University, Department of Movement and Sports Sciences, Ghent, Belgium.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Emerging evidence suggests that a vestibular dysfunction may considerably influence children’s development and may result in motor, cognitive, educational and/or psychosocial symptoms which tend to overlap with symptoms found in children with neurodevelopmental disorders (NDDs). Furthermore, several children with NDDs are known to have postural and/or motor disturbances. Evidence whether these balance problems are accompanied with a vestibular dysfunction is limited. Therefore, to investigate the characteristics of vestibular function in this population, a systematic review was performed.
Methods: MEDLINE, EMBASE, Cochrane Register of Controlled Trials and reference lists of all included studies were screened by two independent researchers. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines were followed. Risk of bias was verified using the Newcastle-Ottawa Scale and interrater reliability was established using Cohen’s Kappa.
Results: Twenty studies, discussing vestibular function in children with NDDs were retained for synthesis. Several authors suggested a possible vestibular involvement in patients with NDDs since in a subset of these patients central and/or peripheral vestibular aberrations were found. These alterations may result in symptoms of distorted motor coordination or postural instability, respectively, and might explain the balance problems observed in some of these children. However, current findings are ambiguous and mainly based on evaluation of the horizontal semicircular canals alone.
Conclusions: High-quality studies with an extensive vestibular test battery are required to further characterize the vestibular function in children with NDDs. Importantly, since comparable symptoms may occur in both groups, clinicians should be aware of these similarities when establishing the diagnosis in these patients.
FP1327Vestibular information is insufficient for reliably encoding head positions
Gerda Wyssen, Fred W. Mast, Matthias Ertl
Department of Psychology, University Bern, Switzerland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
Spatial memory refers to stored information regarding the location of objects or the self in the three dimensional space and is most frequently studied in the visual domain. To study the role of vestibular input in spatial memory, we designed a novel, kinesthetic spatial memory task where a target position is encoded and retrieved via active, passive, and imagined head rotations. The passive rotations were performed by a motion platform where participants perceived vestibular input, which enabled them to encode the target position. In the imagination condition the participants were asked to imagine a head rotation onto the target as vividly as possible without executing any head or eye movements. The visual target points were presented using a virtual reality headset. Targets were presented in 14 different positions (3°, 6°, 9°, 12°, 15°, 18°, 21°) left and right of the center. In total 55 participants were tested in this experiment.
We found, that the accuracy (absolute errors) during retrieval was smaller for the active (median error: 1.83°), than for the passive (median error: 2.34°) rotation condition. Surprisingly, the performance in the imagination condition was comparable to active head rotations (median error: 1.87°). A more detailed analysis of the data with respect to the target angles showed that in the active condition all target angles were overestimated. Such an overshoot is in line with reports on the kinematics found in cervical joint positioning tasks (Revel et al., 1991). For the passive and imagination condition a more complex relationship between target angle and errors was found. In both conditions, smaller target angles (< 6°) were overestimated, but the large target angles (>= 15°) were underestimated. Interestingly, for the 12° target angle the errors in the passive and imagination condition were smaller than in the active condition.
Our findings suggest, that the availability of only vestibular input is insufficient to reliably encode a head position in 3D space, and that for an optimal encoding vestibular, proprioceptive, and the motor information as available in the active condition are required. The comparable performance in the imagination condition supports the emulation theory of representation, which predicts that motor imagery can produce corollary discharges similar to motor commands while also emulating the sensory consequences of an action (Grush 2004). In future studies we plan to investigate whether motor imagery allows to promote spatial memory in patients with vestibular failure.
FP1331Remote assessment of Acute Stroke with Vertigo - The ReActiVe study
Abdel Rahman Saad1, Mohammad Mahmud2, Zaeem Hadi2, Matteo Ciocca3, Barry M Seemungal
Imperial College London
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Vertigo one of the commonest symptom due to brainstem stroke. Early treatment of stroke with vertigo improves outcome. The diagnosis of stroke with vertigo is usually delayed because non-expert clinicians find vertigo difficult to diagnose. Clinicians tend to over-investigate (e.g. brain MRI) acute vertigo patients. Prospective studies show that expert clinical assessment outperforms brain MRI in the first 24hrs in diagnosing stroke. No studies were designed to compare the efficacy of remote assessment done by a vestibular expert compared to direct clinical assessment and investigations of a panel of specialists.
The main objective of this feasibility study is to compare the sensitivity and specificity of experts’ remote assessment via high resolution video technology of acute vertigo patients on the stroke ward with the gold standard (direct clinical assessment plus additional investigations). The final agreed diagnosis will be confirmed by regular, joint case conference reviews between vestibular, stroke, and neuroimaging specialists.
We aim to recruit patients who were admitted at Hyper Acute Stroke Unit at our tertiary center with suspected posterior circulation stroke. These subjects will then be assessed remotely, by a blinded vestibular expert, using high resolution and high-frame-rate video-streaming mobile video technology that is HIPAA/BAA compliant, and has an end-to-end encryption option. The diagnosis of the remote assessor will then be weighed against the final diagnosis following the joint case conference review and sensitivity/specificity calculated. A successful remote technology will be defined with a sensitivity >95% and a specificity of 75%. We will recruit circa 70-80 patients, we expect to recruit around 4 patient volunteers a week.
The short term outcomes of this study is to demonstrate the effectiveness of remote expert clinical assessment in healthcare delivery for acute vertigo patients in a service that covers around 650 thousand people. Implementing a successful remote assessment service will likely reduce inequalities in healthcare, costs of over-investigating and enhance safety by ensuring prompt diagnosis and correct treatment for both benign conditions and stroke with vertigo. A promising result will allow us to apply for funding for a larger multi-center study.
FP1332Percentillary values of Latency and Amplitude of the cervical vestibular evocated myogenic potential (CVEMP) in the population aged 18 To 50
Pérez Chirino Emma Genesis, Ramos Maldonado Daniel, Calderón Leyva Ivonne, Gomez Coello Annel
Introduction: The vestibular evoked myogenic potential analysis is performed based on parameters such as: amplitude, latency, threshold, among others; cVEMP is a fundamental tool for the diagnosis of the vestibular system. An alteration in the latency and amplitude values indicates the presence or absence of some pathology of the inner ear.
Objective: To establish the percentile values of latency and amplitude of the cervical vestibular evoked myogenic potential in the population between 18 and 50 years of age without documented audiovestibular pathology.
Materials and Methods: Descriptive, analytical and cross-sectional study. 158 ears without vestibular pathology were evaluated, in people aged 18-50 years (Eclipse, Interacoustics, Denmark) with a tone of 500 and 1000 Hz or clicks of 0.1 ms, with a stimulus rate of 5.1 ms in rarefaction polarity at the intensity of 110 dB nHL. Measures of central tendency, frequencies and percentage were carried out for all variables. For the values derived from cVEMP (N1, P1, N1-P1, amplitude) ANOVA was performed for independent samples; plus percentiles.
Results: Percentiles were obtained obtaining for latency of the P1 wave (p50 = 14.67), N1 (p50 = 24.5), N1-P1 (p50 9.33) and amplitude of the N1-P1 complex (p50 = 110.5) at 500 Hz and P1 ( p50 = 13.67), N1 (p50 = 22.0), N1-P1 (p50 8.33) and amplitude of the N1-P1 complex (p50 = 127.65) at 1000 Hz.
Conclusions: there is no difference in the latency values N1, P1 and amplitude of the complex N1-P1, neither between the right and left ear between the ranges of 18-50 years the analysis in percentiles of the values of latency, interlatency interval and amplitude it is a watershed for the classification of the alterations in the VEMPs so it is important that each laboratory obtain data of normality.
FP1333Quantitative assessment of self-treated canalith repositioning procedures using inertial measurement unit sensors
Chiheon Kwon1, Yunseo Ku2, Shinhye Seo2, Eunsook Jang3, Hyoun-Joong Kong4,5, Myung-Whan Suh3, Hee Chan Kim1,4,6
1Interdisciplinary Program in Bioengineering, Graduate School, Seoul National University, Seoul, Korea; 2Department of Biomedical Engineering, College of Medicine, Chungnam National University, Daejeon, Korea; 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea; 4Institute of Medical & Biological Engineering, Medical Research Center, Seoul National University, Seoul, Korea; 5Transdisciplinary Department of Medicine & Advanced Technology (TDMAT), Seoul National University Hospital, Seoul, Korea.6Department of Biomedical Engineering, College of Medicine, Seoul National University, Seoul, Korea.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Background: Low success and high recurrence of benign paroxysmal positional vertigo (BPPV) after home-based self-treated Epley and Barbeque (BBQ) roll maneuvers is an important issue.
Objective: To quantify the cause of low success rate of self-treated Epley and BBQ roll maneuvers and provide a clinically acceptable criterion to guide self-treatment head rotations.
Methods: Twenty-five participants without active BPPV wore a custom head-mount rotation monitoring device for objective measurements. Self-treatment and specialist-assisted maneuvers were compared for head rotation accuracy. Absolute differences between the head rotation evaluation criteria (American Academy of Otolaryngology guidelines) and measured rotation angles were considered as errors. Self-treatment and specialist-treated errors in maneuvers were compared. Between-trial variations and age effects were evaluated.
Results: A significantly large error and between-trial variation occurred in step 4 of the self-treated Epley maneuver, with a considerable error in the second trial. The cumulative error of all steps of self-treated BBQ roll maneuver was significantly large. Age effect occurred only in the self-treated BBQ roll maneuver. Errors in specialist-treated maneuvers ranged from 10 to 20 degrees.
Conclusions: Real-time feedback of head movements during simultaneous head-body rotations could increase success rates of self-treatments. Specialist-treated maneuvers can be used as permissible rotation margin criteria.
FP1335Patient Reported Outcomes and Quality of Life in Individuals with a Vestibular Implant
Andrianna I. Ayiotis1, Desi P. Schoo2, Celia Fernandez Brillet1, Kelly E. Lane2, John P. Carey2, Charles C. Della Santina1,2,3
1Johns Hopkins University Department of Biomedical Engineering; 2Johns Hopkins Department of Otolaryngology--Head and Neck Surgery; 3Labyrinth Devices
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Vestibular implants are a promising intervention for people with bilateral vestibular hypofunction (BVH) who remain disabled despite standard-of-care vestibular rehabilitation therapy. The Labyrinth Devices Multichannel Vestibular Implant (MVI) System delivers electrical pulses to branches of the vestibular nerve innervating the semicircular canals to provide artificial sensation of head rotation. It modulates stimulation using head motion measurements from a sensor magnetically coupled to the scalp. The MVI Early Feasibility Study (MVI EFS, NCT02725463) is a non-randomized, controlled clinical trial active from 2016-present. We investigated patient-reported outcomes (PRO) for MVI EFS applicants (who have not yet undergone MVI implantation) and implanted participants with BVH, quantifying changes in self-reported dizziness handicap, disability and health-related quality of life changed over a 6-month interval for each group.
We examined PRO data for ten participants with severe adult-onset BVH for >1 year who had undergone >6 months of vestibular rehabilitation therapy and underwent unilateral implantation of an MVI stimulator, which continuously delivers motion-modulated electrical stimulation 24hr/day or during all waking hours. We also examined data for 53 trial applicants with self-reported BVH who have not yet undergone implantation. Questionnaires assayed self-reported health-related quality of life (utilities derived from the Health Utilities Index Mark 3 [HUI3] and Short Form-36 [SF-36U]) dizziness handicap (Dizziness Handicap Index, DHI) and disability (Vestibular Disorders Activities of Daily Living, VADL). Of the 53 candidates, 20 submitted follow-up questionnaires 6 months later. The minimum detectable Cohen effect size for a paired t-test with alpha=0.05, power=0.8 and N=20 was 0.7. Nine of the candidates who submitted follow-up questionnaires were age-matched with the implanted participants. The minimum detectable Cohen effect size for this comparison was 1.4.
For the 20 candidates who completed questionnaires after six months without undergoing implantation, within-participant changes in DHI (-4[15], p=0.47), VADL (0[2], p=1.00), SF-36U (0.00[0.06], p=0.78) and HUI3 (0.06[0.16], p=0.09) did not differ significantly from zero. Comparison of within-participant changes over six months for implant recipients and age-matched BVH candidates who have not yet undergone implantation revealed significant improvements for implanted participants relative to the non-implanted group for DHI (-40[44], p=0.0044), VADL (-1[2], p=0.003) and SF-36U (0.10[0.05], p=0.01) but not for HUI3 (0.05[0.39], p=0.53).
Unilateral implantation and long-term continuous use of a vestibular implant improved patient-reported dizziness, vestibular disability and health-related quality of life compared to age-matched controls with BVH who have not yet undergone implantation.
Support: NIH R01DC13536, U01DC0019364; Labyrinth Devices LLC; MED-EL GmbH
Andrianna I. Ayiotis1, Margaret R. Chow1,2, Celia Fernandez Brillet1, Kelly E. Lane3, John P. Carey3, Charles C. Della Santina1,2,3
1Johns Hopkins University Department of Biomedical Engineering; 2Labyrinth Devices; 3Johns Hopkins Department of Otolaryngology--Head and Neck Surgery
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
The Multichannel Vestibular Implant (MVI) Early Feasibility Study (NCT02725463) is an active clinical trial investigating vestibular implants as an intervention for people with bilateral vestibular hypofunction (BVH) who remain disabled despite standard-of-care vestibular rehabilitation. The implant system senses 3-dimensional head angular velocity and electrically stimulates branches of the vestibular nerve that innervate the semicircular canals. Ten participants with severe, adult-onset BVH for >1 year, who had undergone >6 months of vestibular rehabilitation therapy underwent unilateral implantation of the device and received motion-modulated vestibular stimulation 24hr/day or during all waking hours since initial device activation, for durations ranging from 0.5-5 years. Individuals with BVH experience diminished vestibular-ocular reflexes, which lead to blurry vision during head movement. This can be quantified by measuring dynamic visual acuity (DVA) while walking.
For this study, DVA was measured by having subjects read letters from a standard ETDRS eye chart with Sloan optotypes while they walked at 0.5-3 miles per hour (mph) on a treadmill. The change in DVA from static (head not moving) visual acuity was linearly fit to derive the slope of the decrement in visual acuity with increasing treadmill speed. We quantified changes in DVA slope relative to pre-operative baseline for six subjects tested >2 months after unilateral MVI implantation. For ten implanted subjects, we compared DVA slope during motion-modulated stimulation using the standard operating parameters of the device, during tonic stimulation (a placebo control), at the subjects’ most recent measurement on or before December 2021. For false discovery rate=0.05, power=0.8 and N=10, the minimum detectable Cohen effect size is 1.
Preoperative DVA slope was -0.13±0.07 (mean±SD) logMAR/mph. For the postoperative measurement taken before device activation, DVA slope was -0.14±0.07, suggesting that DVA was neither affected by implantation alone nor significantly confounded by a learning effect. DVA slope during tonic/placebo MVI stimulation (-0.19±0.16) was lower than the postoperative/no-stimulation value, and DVA slope during motion-modulated stimulation (-0.08±0.03) exceeded that for all other conditions. For all ten subjects, the DVA slope during motion modulated prosthetic stimulation was significantly better than during tonic stimulation (-0.09±0.04 to –0.19±0.12, p=0.02).
Motion-modulated stimulation delivered by a unilateral vestibular implant improved dynamic visual acuity relative to preoperative baseline and relative to a tonic stimulation placebo control.
Support: NIH R01DC13536, U01DC0019364; Labyrinth Devices LLC; MED-EL GmbH
FP1337Video Head Impulse Testing in Individuals with a Unilateral Vestibular Implant
Andrianna I. Ayiotis1, Desi P. Schoo2, Margaret R. Chow1,3, Celia Fernandez Brillet1, Kelly E. Lane2, John P. Carey2, Charles C. Della Santina1,2,3
1Johns Hopkins University Department of Biomedical Engineering; 2Johns Hopkins Department of Otolaryngology--Head and Neck Surgery; 3Labyrinth Devices
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Individuals with bilateral vestibular hypofunction (BVH) who remain disabled despite standard-of-care vestibular rehabilitation therapy have no adequate treatment options. Vestibular implants provide artificial sensation of balance by delivering electrical pulses to branches of the vestibular nerve that innervate the semicircular canals. The Labyrinth Devices Multichannel Vestibular Implant (MVI) System modulates stimulation using head motion measurements from a sensor magnetically coupled to the scalp. The MVI Early Feasibility Study (MVI EFS, NCT02725463) is a non-randomized, controlled clinical trial active from 2016-present.
Ten participants with severe adult-onset BVH for >1 year who had undergone >6 months of vestibular rehabilitation therapy, underwent unilateral implantation of an MVI stimulator, which continuously delivers motion-modulated electrical stimulation 24hr/day or during all waking hours. Head impulse testing of the implanted canals was used to measure vestibulo-ocular reflex (VOR) gain and latency relative to head motion, two measures of device efficacy. Across six subjects, the VOR gain and latency for 18 implanted canals was tested during a pre-operative baseline and >2 months after unilateral MVI implantation at the subjects’ most recent measurements on or before December 2021. VOR gain and latency were measured in two implant stimulation conditions: motion-modulated stimulation using the system’s dynamic velocity-to-pulse-rate-and-amplitude mappings (with signals in phase with angular acceleration) and operating parameters and during tonic stimulation (a placebo control). For false discovery rate=0.05, power=0.8 and N=18, the minimum detectable Cohen effect size would be 0.7.
Averaged over all 18 implanted canals, pre-operative baseline vHIT gain was (0.32±0.17, mean±SD). During motion-modulated input, it was 0.43±0.16 (p=0.06). That gain during motion-modulated input was significantly greater than gain during tonic/placebo stimulation (0.11±0.09, p<0.001). Average vHIT VOR latency was significantly better using motion modulation (30±8 ms) compared to pre-operative baseline (41±21 ms, p=0.04) and compared to tonic stimulation (75±29 ms, p<0.001).
Motion-modulated stimulation delivered by a unilateral vestibular implant using dynamic-velocity maps significantly improved VOR latency relative to preoperative baseline and significantly improved VOR gain and latency compared to a tonic stimulation placebo control.
Support: NIH R01DC013536, U01DC0019364; Labyrinth Devices LLC; MED-EL GmbH
FP1342Contemplating V6 as the cortical cornerstone for the perception of forward self-motion: an fMRI study
Sarah Marchand1, Marine Balcou1, Philippine Picher1, Maxime Rosito1, Damien Mateo1, Nathalie Vayssiere1, Alexandra Severac-Cauquil1
1CerCo UMR 5549 CNRS Université Toulouse; 3Paul Sabatier, France
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
The integration of visual and vestibular information, providing information on the position and movement of the head in space, is crucial for spatial perception in humans. The combination of information from these two sensory systems takes place at several levels in the central nervous system, notably in the brainstem and cortex. A simple and effective way to selectively activate the vestibule is galvanic vestibular stimulation (GVS). This non-invasive method of stimulation consists in sending a small electric current via electrodes, affecting the vestibulocochlear nerve VIII afferents (Kwan et al., 2019), which induces oculomotor, postural responses, as well as an illusion of movement. Although this method is mostly used to induce a lateral input, there is a monopolar binaural (GVSbm) configuration of the electrodes that allows responses to be redirected in the anteroposterior plane. At the cortical level, we recently showed that visual areas V6 and VIP respond to vestibular information associated with anteroposterior movement but not to vestibular information of lateral movement (Aedo-Jury et al., 2020). The main objective of the present project is to describe the GVSbm activation combined with optical flow visual stimulation, either congruent or incongruent. 15 healthy subjects underwent 2 MRI sessions: the first aimed to localize the brain areas of interest and during the second, the subjects received visual and vestibular stimuli. The stimuli were grouped in 6 conditions: visual only forward (expanding dots), visual only backward (contracting dots), front visual and congruent GVS, rear visual and congruent GVS, front visual and incongruent GVS (mimicking a backward movement), and finally backward visual and incongruent GVS. A first-level analysis did not reveal the activation of the areas of interest. Nevertheless, the visual + GVS versus visual contrast shows a good level of activation, with symmetrical clusters in both hemispheres, corresponding to areas known to be activated by the GVS, thus processing specifically vestibular input. The congruent versus incongruent, and incongruent versus congruent contrasts show no, or very few, clusters of activation. The forward versus backward contrast shows an unexpected lateralized cluster in the right hemisphere only, while the back versus front contrast shows no lateralization. We hypothesize that ROI analysis would allow us to consider V6 as a cornerstone of sensory integration between the visual and vestibular systems, stating that this region is more activated when signals from these two modalities are congruent.
References: Aedo-Jury F, Cottereau BR, Celebrini S and Séverac Cauquil A (2020) Antero-Posterior vs. Lateral Vestibular Input Processing in Human Visual Cortex. Front. Integr. Neurosci. 14:43. doi: 10.3389/fnint.2020.00043
Kwan A, Forbes PA, Mitchell DE, Blouin J-S, Cullen, KE (2019) Neural substrates, dynamics and thresholds of galvanic vestibular stimulation in the behaving primate. Nature Communications 10, Article number: 1904
FP1347The Effect of Vestibular Implant Stimulation on Utricular Primary Afferents in Rhesus Macaque
Brian J. Morris1, Margaret R. Chow1, Abderrahmane Hedjoudje2, Dale Roberts2, Chenkai Dai2, Kathleen E. Cullen1,2,3, Roland Hessler4, Charles C. Della Santina1,2
1Biomedical Engineering, 2Otolaryngology – Head & Neck Surgery, 3Neuroscience, Johns Hopkins School of Medicine, Baltimore, MD, USA, and 4Med-El GmbH, Innsbruck, Austria
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
During vestibular implant programming, 3-dimensional vestibulo-ocular reflex (3DVOR) axis and speed are taken as indicators of activity in the three ampullary (semicircular canal) nerve branches. This approximation ignores utricle and saccule activity for the practical reason that relationships between that activity and 3DVOR responses remain poorly defined. Finite element modeling predicts that prosthetic current targeting semicircular canals inadvertently activates utricular and/or saccular neurons. To test this hypothesis, we measured single-unit utricular afferent neuron activity and 3DVOR of a rhesus monkey implanted unilaterally with electrodes in each ampulla.
We delivered cathodic-first, charge-balanced, symmetric biphasic, 100µS/phase, 20-200µA current pulse trains at 200pulses/s to a head-fixed, alert rhesus monkey in darkness using intra-ampullary stimulating electrodes and a return electrode beneath the temporalis muscle. We recorded single-unit electrophysiologic activity of vestibular primary afferents and scleral coil 3DVOR oculography during electrical and mechanical stimulation. Mechanical stimuli (whole body rotation and translation) were delivered using a hexapod motion platform.
Eight vestibular afferents, confirmed to be utricular by responses to mechanical stimuli, were isolated and responded to electrical stimulation. Analyzable data for both mechanical and electrical stimuli were obtained for two single units. Most increased in spike probability at ~50µA and reached saturation by 150µA for most horizontal and anterior canal stimulating electrodes. The deepest electrodes in the horizontal, anterior and posterior canals elicited utricular neuron spike probabilities up to 80%, 77%, and 58%, respectively, at 100µA, and also elicited the largest VOR magnitude for each current amplitude, reaching maxima of 192 deg/s, 126 deg/s and 93 deg/s, respectively, at 200µA. VOR magnitude at 100µA for the horizontal and anterior canals and 125µA for the posterior canal, the current step below the facial nerve stimulation threshold, was 108 deg/s, 28 deg/s, and 31 deg/s respectively. VOR responses aligned to within 8.5, 14, and 12 deg, respectively, of the targeted canal axis.
Vestibular implant stimulus currents intended for canal neurons also activated utricular neurons at currents close to the threshold for eliciting canal-driven 3DVOR responses. Anterior and horizontal canal electrodes activated utricular units at lower stimulus currents than did posterior canal electrodes. Given similarity of labyrinth anatomy and physiology across primate species, these data suggest that patients who rely on vestibular implant stimulation to elicit motion-modulated ampullary nerve activity should experience prosthetically-driven utricular nerve activity. Whether that spurious activity is necessarily detrimental or potentially useful merits further investigation.
Support: NIH R01DC13536, R01DC009255, R01DC2390, F31DC019861; MED-EL GmbH
FP1349Acute Vestibulopathy after COVID-19 Vaccination: Possible Pathophysiology and Prognosis
Junsic Yoon1, Min Young Lee2, and Myung-Whan Suh1
1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul; 2Department of Otorhinolaryngology-Head & Neck Surgery, Dankook University Hospital, Cheonan, Korea
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Many patients complain of dizziness after COVID-19 vaccination. But the symptom, vestibular function test (VFT) results, mechanism, and prognosis of these patients have not been elucidated.
Patients and Methods: The VFTs and audiometry of nine patients complaining of dizziness after COVID-19 vaccination were evaluated. The symptoms were considered to be related with the vaccination when they occurred within 48 hours.
Results: Patients were 61.4±12.9 years old and 4 were female. Spinning vertigo was the chief complaint in 30% of the patients. Others complained of non-whirling dizziness. Onset of symptom was 14.9±15.1 hours after the vaccination (5 Pfizer and 4 AstraZeneca). The dizziness symptoms were paroxysmal vertigo attacks with symptom free intervals or decompensation of past vestibulopahty. The symptoms were most severe after 3.0±3.8 days and resoled after 47.7±51.1 days. Thromocytopoenia or thrombosis was not found in any of the patients. Unilateral or bilateral vestibulopathy was documented in all the patients. VFT findings were not consistent with peripheral disorders. Atypical findings were found, such as 1) periodic nystagmus with symptom/sign free intervals, 2) abnormal high VOR gain, 3) reduced saccade velocity, and 4) phase lag in slow harmonic acceleration test. Two subjects were also diagnosed of Immune related encephalopathy. The symptoms resolved with no sequelae in all cases after vestibular rehabilitation +/- intravenous immunoglobulin therapy.
Conclusion: Coexisting peripheral and central vestibulopathy may be the cause of dizziness after COVID-19 vaccination. VFT patterns and symptoms were not typical to peripheral vestibulopathy in 56%. 1) Cross immune reaction that misidentify inner ear antigens as the virus or 2) overzealous production of proinflammatory cytokines can be proposed mechanism of the acute onset dizziness. All patient fully recovered with 47.7±51.1 days with the help of vestibular rehabilitation.
FP1350A Randomised Double Blinded Controlled Trial of Galvanic Vestibular Stimulation and Posturography in Healthy Controls
Mohammad Mahmud, Elisa Bernado, Zaeem Hadi, Mabel Predergast, Matteo Ciocca, Abdel Saad, Barry M Seemungal
Neuro-otology Unit, Department of Brain Sciences, Imperial College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Sub-threshold galvanic vestibular stimulation (GVS) is thought to enhance the sensitivity of the peripheral vestibular system to head inertial stimuli and hence may modulate vestibular sensorimotor function.
Objective: To examine the effects of GVS upon postural control performance in healthy subjects standing on a soft surface with eyes closed.
Methods: We administered bipolar noisy GVS (frequency 0-30Hz) with the anode and cathode placed on the mastoids of healthy controls. Subjects stood on a soft-foam surface, placed upon a force platform for 120 seconds, with eyes closed. Either anodal or sham stimulation was applied for the first and last 30 seconds of the balance task, in randomised order. Results in 50 subjects with a primary outcome of sway comparing anodal stimulation to sham will be presented. Conclusions will assess whether subperceptual GVS modulates balance performance and hence provide evidence to use GVS to enhance postural control in patient populations.
FP1352The Role of Interhemispheric Coherence in Postural Control in Healthy Subjects
Mohammad Mahmud, Elisa Bernado, Zaeem Hadi, Matteo Ciocca, Abdel Saad, Barry M. Seemungal
Neuro-otology Unit, Department of Brain Sciences, Imperial College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Human balance control requires sensori-motor integration that engages widespread brain regions. Based upon previous imaging and neurophysiological work, including that linking alpha EEG rhythms to postural control, we hypothesised that postural control is critically reliant upon interhemispheric processing which predicts that markers of interhemispheric communication, e.g. interhemispheric EEG coherence, may be linked to postural control. Methods: Force platform recordings of sway during steady standing in 35 healthy controls was obtained in four conditions: hard vs. soft standing surface x eyes open vs. eyes closed. Each condition lasted 60 seconds and repeated 3 times so the total time per condition with EEG recording was 180seconds. Current analyses (via MATLAB) involve assessing interhemispheric coherence across different EEG frequency bands with a specific focus on the alpha rhythm.
FP1353Physical Activity Level: a Prognostic Factor for developing Chronic Dizziness after Vestibular Schwannoma Resection?
Lien Van Laer1,2; Vincent Van Rompaey3; Ann Hallemans1,2, and Luc Vereeck1,2
1Department of Rehabilitation Sciences and Physiotherapy / Movant, Faculty of Medicine and Health Science, University of Antwerp, Belgium; 2Multidisciplinary Motor Centre Antwerp (M2OCEAN), University of Antwerp, Belgium; 3Department of Otorhinolaryngology and Head & Neck Surgery, Faculty University Hospital of Antwerp of Medicine and Health Sciences, University of Antwerp, Edegem, Belgium
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Objective: To explore the relation between chronic dizziness after vestibular schwannoma (VS) resection and the subacute self-reported level of physical activity ( PA)
Introduction: A VS resection causes an acute unilateral vestibular deafferentiation resulting in postoperative symptoms such as acute dizziness, unsteadiness and nausea which may occur to a greater or lesser extent. Despite the expected resolution of most of the symptoms due to the process of central vestibular compensation, more than one out of four patients develop persistent vertigo (28%). Several predictive factors for developing chronic dizziness, such as age, tumor size and preoperative vestibular function, have been suggested. Despite its potential effect on the process of central vestibular compensation, PA was not yet considered. Therefore, the relation between PA during the subacute phase and chronic dizziness will be investigated.
Methods: This retrospective cohort study included seventy-four patients that underwent retrosigmoid VS resection between November 2001 and February 2005. Patients were assessed prior to surgery and at nine and twenty-six weeks postoperatively. At nine weeks patients were asked to report their level of PA during the past week by using a visual analogue scale (0 = zero PA, 100 = vigorous PA) and their static balance performance was assessed by calculating the summed score of four standing balance test conditions with eyes closed (maximum score of 120 seconds). However, not all patients were able to attend each session, leading to inclusion of fourty-five patients with a mean age of 42.1 years (standard deviation 9.5) in the statistical analysis. Following prognostic factors were used in a linear regression model that predicts the DHI-score at six months: age, static balance performance and PA level. To identify the main predictive variables for this model, a univariable regression was performed beforehand (see examples in Figures 1-3).
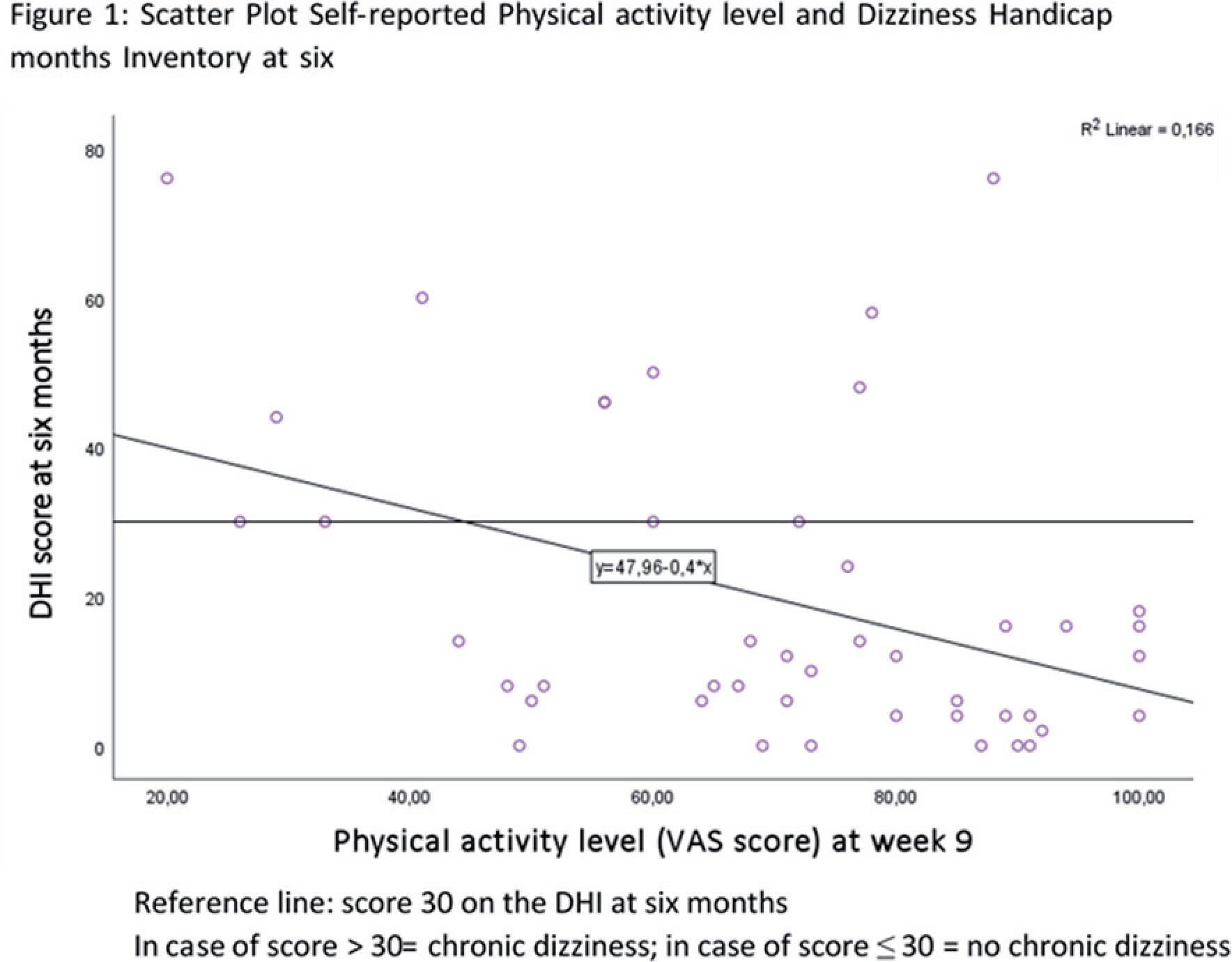
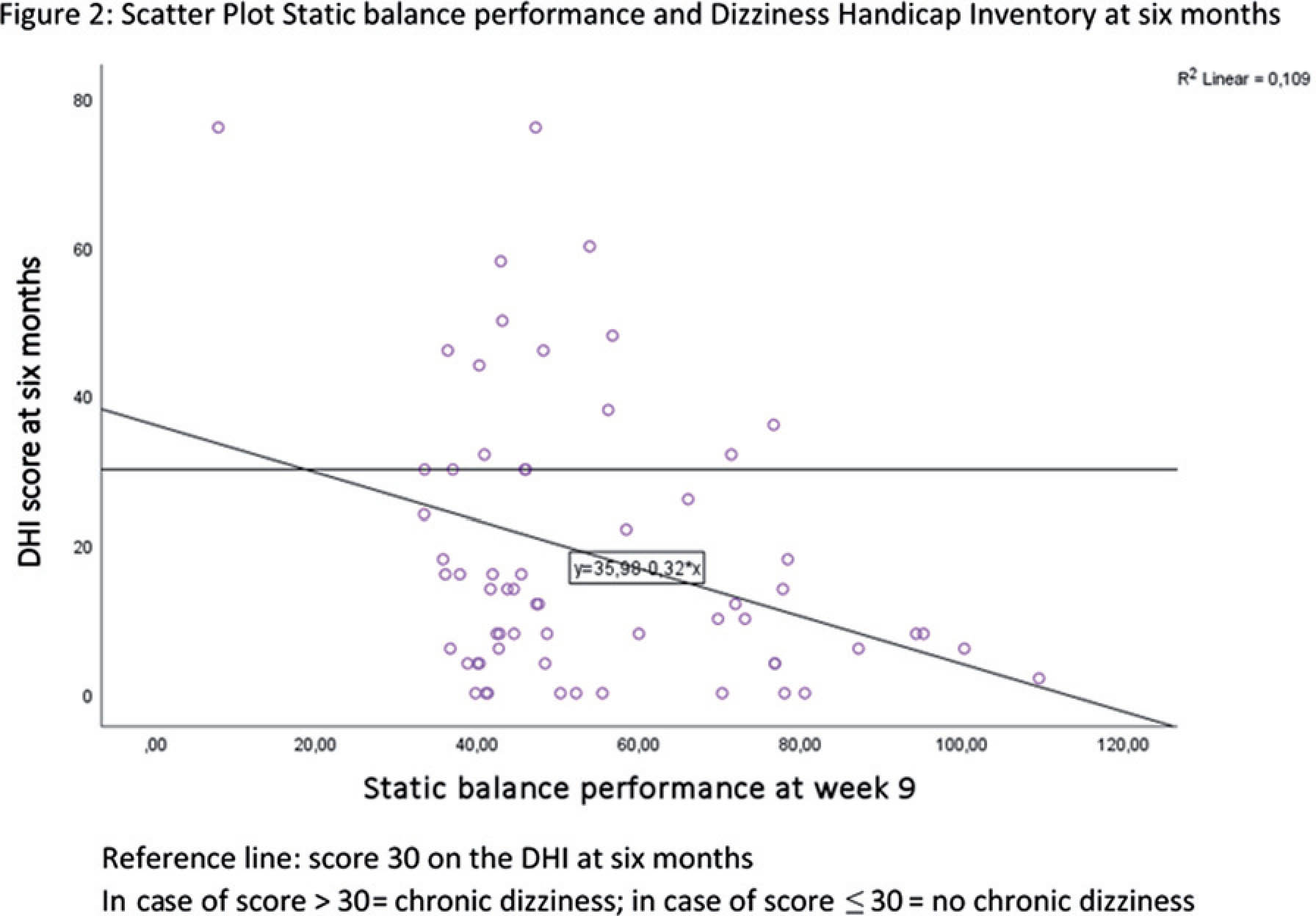
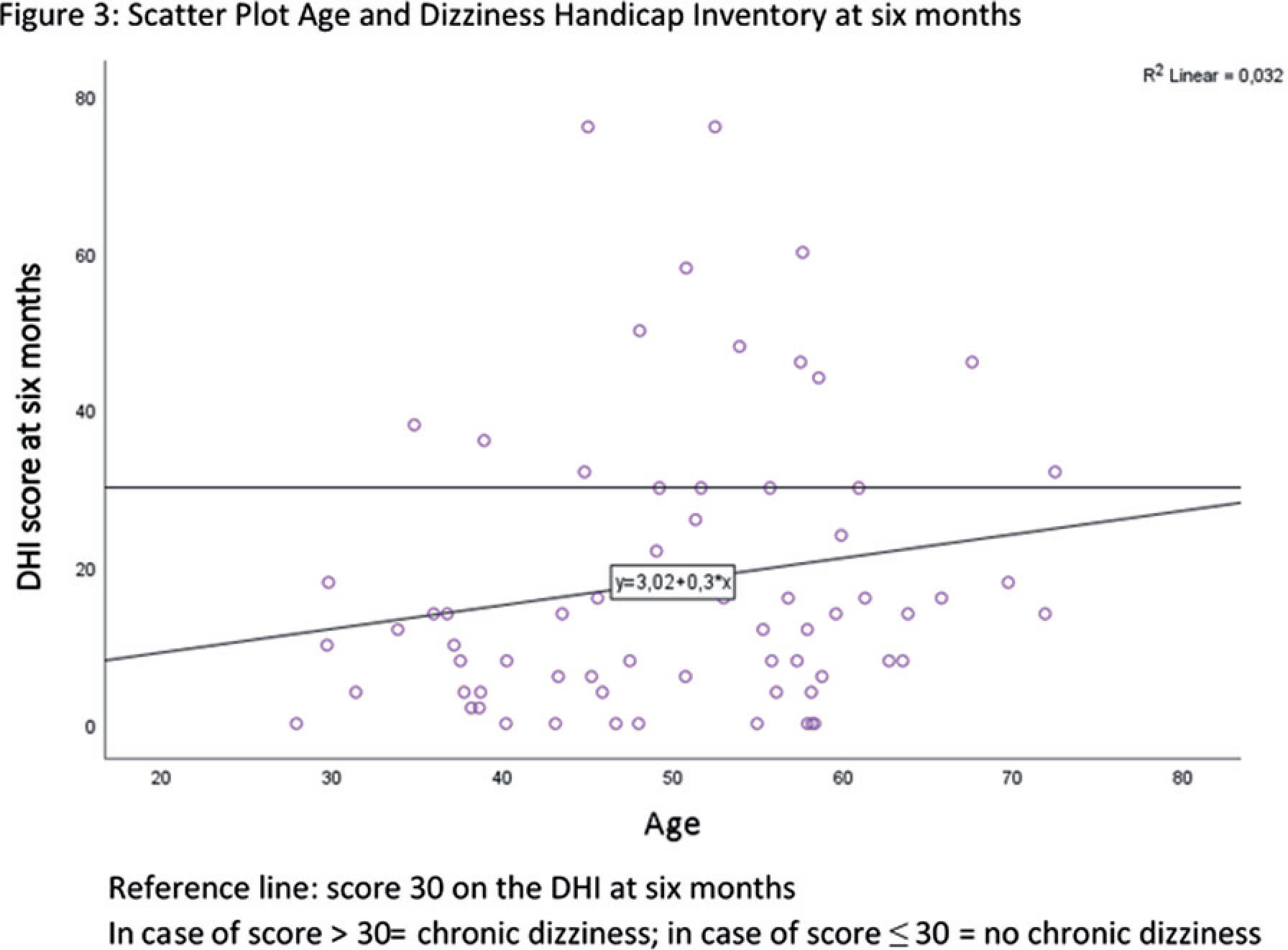
Results: After elimination, two variables (PA level and static balance performance) remained in the model which significantly predicted the DHI-score (F2,42= 6,198; R2= 0,228; p= 0,004). The level of PA itself proved to be a significant predictor (β= -0.318, p= 0.033) whereas static balance performance (β= -0.264, p= 0,074) and age (β= 0,010, p= 0.949) did not.
Discussion/conclusion: These results reveal the importance of monitoring PA after a VS resection. Additional assessment of the level of PA during the subacute phase could increase awareness and lead to appropriate interventions if necessary.
FP1356Longitudinal Resting State fMRI Changes Predicting Vestibular Agnosia in Traumatic Brain Injury
Zaeem Hadi1, Yuscah Pondeca1, Elena Calzolari1, Mariya Chepisheva1, Rebecca M Smith1, Mohammad Mahmud1, Heiko Rust1, David J Sharp2, Barry M Seemungal1
1Department of Brain Sciences, Neuro-otology unit, Imperial College London, UK; 2Computational, Cognitive and Clinical Neuroimaging Laboratory (C3NL), Department of Brain Sciences, Imperial College London, UK.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Peripheral vestibular activation elicits a simultaneous reflex vestibular nystagmus and perception of self-motion. In a recently characterized condition called “Vestibular Agnosia”, the link between vestibular nystagmus and perception is decoupled resulting in loss of self-motion perception. Vestibular agnosia is mostly present in conditions with damage to brain networks (e.g. Traumatic Brain Injury (TBI), and neurodegenerative diseases). We recently identified brain regions predicting vestibular agnosia in acute TBI, however, it remains unknown whether longitudinal changes predict recovery from vestibular agnosia.
Methods: The data was collected as part of an MRC-funded prospective study (Calzolari et al., 2021). Resting state fMRI was acquired from 39 acute TBI patients (and 37 matched controls) with preserved peripheral and reflex vestibular function, along with self-motion perceptual thresholds during passive yaw rotations in the dark, and posturography. Using left frontal and right parietal resting-state networks as regions of interests (ROIs), based on previously identified regions that are associated with vestibular agnosia.
Results: Since vestibular agnosia was predicted by increased connectivity within ROIs (left frontal networks, and right parietal networks) at acute stage. A decrease of functional connectivity in ROIs at 6 months compared to acute stage would likely predict recovery from vestibular agnosia.
FP1357Effect of Clinician Experience on Video Head Impulse Testing
Desi Schoo1, Andrianna Ayiotis2, Celia Fernandez Brillet2, Matthew Ehrenberg1, Margaret Chow2, Grace Tan1, John P Carey1, Charles C Della Santina1,2
1Johns Hopkins School of Medicine, Department of Otolaryngology-Head and Neck Surgery; 2Johns Hopkins University, Department of Biomedical Engineering
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: The video head impulse test (vHIT) is a common clinical assessment of semicircular canal function. Current commercially available testing systems rely on clinicians to deliver head impulses. The effect of clinician experience on vHIT testing and results has not been fully characterized.
Methods: We recruited thirteen clinicians with various levels of experience to perform a standard 6-canal vHIT exam on the same normal subject using the GN Otometrics ICS Impulse system. Participants were attendees of a 3-day advanced vHIT course that included hands-on instruction. During data collection, a complete test of each canal was defined as twenty head impulses accepted for analysis by the OTOsuite Vestibular software (GN Otometrics, version 4.00). Individual test results were compared. To ensure that every head impulse motion was capture and none were excluded from analysis, a custom MATLAB program was used to analyze the head motion profiles.
Results: All participants were able to complete vHIT testing of the horizontal canals. Complete six-canal vHIT assessments were completed by 5/5 experts, 3/5 clinicians with an Intermediate level of experience, and 3/3 novices. Each of the two clinicians who failed to complete the testing session reported difficulty with obtaining data accepted by the OTOsuite software for the LARP plane. VOR gains consistent with normal semicircular canal function in every canal as reported by the OTOsuite software were achieved by 3 testers (1 tester at each experience level). Normal VOR gains were reported for the horizontal canals for all testers. Abnormal VOR gains (<0.8) were most often reported for the LARP canals across all experince levels. No trend was observed related to the inter-impulse variance of peak head velocity or width of the head motion waveform when the head motion profile data were analyzed in MATLAB.
Conclusions: With appropriate instruction, clinicians with limited experience performing vHIT testing can perform assessment of the horizontal semicircular canals using a commercially available vHIT system. Additional experience may be required to perform vertical canal assessments.
Support: T32000027
FP1360Resting State fMRI Correlates of Postural Control Deficit in Traumatic Brain Injury
Zaeem Hadi1, Yuscah Pondeca1, Elena Calzolari1, Mariya Chepisheva1, Rebecca M. Smith1, Mohammad Mahmud1, Heiko Rust1, David J. Sharp2, Barry M. Seemungal1
1Department of Brain Sciences, Neuro-otology unit, Imperial College London, UK; 2Computational, Cognitive and Clinical Neuroimaging Laboratory (C3NL), Department of Brain Sciences, Imperial College London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Introduction: Traumatic Brain Injury (TBI) is one of the commonest cause of the disability in young adults. About 50% of TBI patients suffer from imbalance at acute stage and many of those patients underreport symptoms. Thus, imbalance and the lack of perception of imbalance also contributes to falls in TBI and thus disability. We recently localised correlates of imbalance and vestibular perception, in right inferior longitudinal fasciculus using structural imaging. Here, we identify functional brain networks associated with imbalance using resting state functional brain networks.
Methods: The data was collected as part of an MRC-funded prospective study (Calzolari et al., 2021). Resting state fMRI was acquired from 39 acute TBI patients (and 37 matched controls) with preserved peripheral and reflex vestibular function, along with self-motion perceptual thresholds during passive yaw rotations in the dark, and posturography. Posturography was performed in four conditions: (i) Hard surface and Eyes Open; (ii) Hard surface and Eyes Closed; (iii) Soft surface and Eyes Open; (iv) Soft surface and Eyes Closed. We found that Soft surface and Eyes Closed (SC) condition was the best predictor of patients’ imbalance compared to controls and thus used SC condition as a predictor of imbalance in resting state fMRI analysis.
Results: We expect increased functional connectivity in right mid-temporal regions in grey matter, and in right superior longitudinal fasciculus and right inferior longitudinal fasciculus in white-matter at acute stage. Moreover, a decrease in functional connectivity from acute to 6 months would predict the recovery of imbalance in TBI.
FP1367An N-of-1 trial of a vibrotactile feedback ‘balance belt’ in someone with bilateral peripheral vestibulopathy
David Herdman, Tom Jenkins, Sally Durham, Sarah Taylor
St George’s University Hospitals NHS Foundation Trust, London, UK
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Purpose: A ‘balance belt’ (Elitac BalanceBelt), providing haptic vibrotactile feedback, has recently come on the market which claims to improve balance and mobility in people with bilateral vestibular hypofunction (BVH). The N-of-1 has emerged as an important methodological tool for testing these new technologies, enabling researchers to compare the effectiveness of health interventions and medical devices at the level of a single individual. Here we present such a study to test the balance belt on someone with BVH using objective gait laboratory measures.
Methods: We conducted an exploratory independent evaluation of the balance belt in our gait laboratory using N-of-1 methodology, with an ABA design. The patient was a 45-year-old male, with bilateral vestibular hypofunction confirmed on rotational chair. He described oscillopsia and disequilibrium following aminoglycoside treatment during a prolonged intensive care admission due to pneumonia in 2018. He had a normal MRI and did not carry the m.1555A>G genetic mutation. He also had chronic back pain. The protocol was practical in terms of time, costs and the demands on the patient’s time and mobility. Three conditions were chosen, with four trials per condition: (1) steady state walking, (2) walking with head turns in yaw, and (3) cognitive dual task walking. Markers were placed on the torso and lower limbs to assess kinematic outcomes including postural sway, joint kinematics, and temporal-spatial parameters. The patient was also asked to complete a perceived disequilibrium visual analogue scale following each trial.
Results: The vibrotactile belt demonstrated positive changes in kinematic data and subjective disequilibrium in favour of the balance belt for all conditions.
Conclusion: The vibrotactile belt was shown to improve dynamic gait stability. This study shows the feasibility of n-of-1 trials to measure the response of medical devices that purport to improve balance for people with BVH. The protocol can be adapted and replicated in other patients to explore clinical phenotyping on the characteristics of patients found to respond and other trends in the data about the merits of the balance belt.
Target audience: This study would be of interest to anyone involved in therapy for people with BVH, rehabilitation technologies, and novel research designs including single case experimental designs.
FP1371The Association of Visual Vertigo with Function, Quality of Life and Perceived Change in Health
Cláudia M. Costa1,2; Pamela M. Dunlap2; Carrie W. Hoppes3; Brooke N. Klatt2; Patrick J. Sparto2,4; Joseph M. Furman2,4; Susan L. Whitney2,4
1Faculty of Medicine, Lisbon University, Lisbon, Portugal; 2Department of Physical Therapy, University of Pittsburgh, Pittsburgh, PA, USA; 3Army-Baylor University DPT Program, San Antonio, Texas, USA; 4Department of Otolaryngology, University of Pittsburgh, Pittsburgh, PA, USA
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and Purpose: Visual vertigo (VV) is a common complaint among persons with dizziness. As VV is often related to the development of Persistent Postural-Perceptual Dizziness (PPPD), it is important to understand how these symptoms can affect function, quality of life and perceived change in health. This study aims to determine the relationship between visual vertigo baseline ratings, quality of life, self-reported function and perceived change in health condition at three months.
Methodology: A convenience sample of 232 subjects from 18 to 88 years of age (54 ± 17 y, 155 females) with vestibular disorders were recruited from a tertiary care balance center and outpatient physical therapy clinics. Subjects were asked to complete the Visual Vertigo Analogue Scale (VVAS) at baseline, the Patient Perception of Function (PPF) and the 12 item Short Form Survey-12 (SF-12) at baseline and at three months, plus the Global Rating of Change Scale (GROC) at three months. Pearson correlation coefficients were used to determine the associations among the measures.
Results: There was a significant moderate negative relationship between the baseline VVAS and the PPF at baseline (r = -0.45, p < 0.001) and at 3 months (r = -0.34, p < 0.001). The baseline VVAS demonstrated a moderate negative correlation with the SF-12 mental component summary score at baseline (r = -0.32, p < 0.001) and at 3 months (r = -0.31, p < 0.001); and with the physical component summary score at baseline (r = -0.47, p < 0.001) and at 3 months (r = -0.34, p < 0.001). There was a significant weak negative correlation between the VVAS and the GROC (r = - 0.13, p = 0.041).
Discussion and Conclusions: Higher levels of visual vertigo at baseline were associated with lower ratings of mental and physical health-related quality of life, a lower perception of function, and less perceived improvement in health at three months.
Clinical Implications: Quality of life and perception of function is related to VV complaints in persons with vestibular disorders. Future work should address the impact of these associations on the person’s recovery and, consequently, explore the best therapeutic strategies for individuals with VV.
Keywords: Visual Vertigo; Perceived Change in Health Condition; Patient’s Perception of Function; Quality of Life
FP1374Scaling mis-match in persistent postural-perceptual dizziness: an objective measure of subjective sway mis-perception
Eduardo San Pedro1, Matthew Bancroft1, Nehzat Koohi1, Patricia Castro1,2,3, Diego Kaski1
1Centre for Vestibular and Behavioural Neurosciences, Department of Clinical and Movement Neurosciences, University College London, 33 Queen Square, London WC1N 3BG; 2Department of Neuro-otology, Division of Brain Sciences, Imperial College London, Charing Cross Hospital, London W6 8RF; 3Universidad del Desarrollo, Escuela de Fonoaudiología, Facultad de Medicina Clínica Alemana. Santiago, Chile
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background: Persistent Postural Perceptual Dizziness (PPPD) is a functional neurological disorder (FND) consisting of a persistent sensation of dizziness and/or unsteadiness (but not vertigo) aggravated by upright posture.
Aim: The aim of this study was to compare the relationship between objective and subjective instability between PPPD and a disease control group with bilateral peripheral vestibulopathy. We expected PPPD patients’ subjective instability to be disproportionately worse than their objective instability, in relation to patients with bilateral peripheral vestibulopapthy.
Methods: 14 patients with PPPD, and 9 controls with bilateral peripheral vestibulopathy were recruited. First, subjects stood upright on firm ground with their eyes closed for three 20-second trials to evaluate objective instability. All subjects were then asked to rate their subjective instability experienced during the objective instability test using a 0–10 ranked scale, where 0 corresponds to being “completely steady” and 10 “so unsteady that I would fall”). Next, subjects were asked to objectivise the subjective sensation of instability by replicating the perceived degree of sway they experienced during the objective instability test for three 20-second trials (objectivised-subjective instability). Instability was measured as the horizontal plane deviation of the centre of pressure over each 20-second trial, where a greater value represents greater instability and sway. The relationship between objective, subjective and objectivised-subjective instability was compared between groups. Subjects also completed two self-administered questionnaires: the State-Trait Anxiety Inventory, form Y, State scale (STAI-S), and the Dizziness Handicap Inventory (DHI).
Results: Bilateral peripheral vestibulopathy patients tended to sway more than PPPD (objective instability: p=0.05). Despite this, PPPD patients perceived greater instability than bilateral peripheral vestibulopathy (subjective instability: p=0.006). Generally, bilateral peripheral vestibulopathy patients were able to replicate their perceived instability accurately and their objective instability correlated with objectivised-subjective instability at close to parity (slope=0.94; intercept=4.8; R2=0.64; p=0.006). However, the relationship between objective and objectivised-subjective instability was disordered in PPPD patients (p=0.68). When expressed as a gain function (objectivised-subjective instability/objective instability), PPPD patients swayed over three times more in the objectivised-subjective than objective instability trials and this tended to be greater than bilateral peripheral vestibulopathy patients (p=0.07).
Discussion: The results suggest that PPPD patients’ mis-perceive and upscale their degree of sway and instability when stood in an upright posture. PPPD patients’ subjective instability is disproportionately worse than their objective instability when compared to a cohort with objective instability (bilateral peripheral vestibulopapthy).
FP1377Comparison of Clinical Characteristics between Patients with Chronic Dizziness of Cervicogenic and Non-Cervicogenic Origin
Charlotte De Vestel1,2, Luc Vereeck1,2, Vincent Van Rompaey3, Susan A. Reid4, Willem De Hertogh1,2
1Department of Rehabilitation Sciences and Physiotherapy/Movant, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Wilrijk, Belgium; 2Multidisciplinary Motor Centre Antwerp (M2OCEAN), University of Antwerp, Antwerp, Wilrijk, Belgium; 3Department of Otorhinolaryngology and Head & Neck surgery, Antwerp University Hospital, Wilrijk, Belgium; Department of Translational Neurosciences, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Wilrijk, Belgium; 4Department of Physiotherapy, Faculty of Health Sciences, School of Allied Health, Australian Catholic University, North Sydney, NSW, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Background and objectives: Cervicogenic dizziness (CGD), due to disturbed proprioceptive afferents, can cause chronic dizziness. However, it is difficult to detect CGD in patients with chronic dizziness since bedside/laboratory/imaging tests often correlate weakly with the symptoms present. Objective: to investigate how patients with CGD differ clinically from patients with other forms of chronic dizziness. Methods: A cross-sectional study was conducted in the Antwerp University Hospital assessing 60 consecutive patients with chronic dizziness. Of those patients, 18 received the diagnosis of CGD. The diagnosis of CGD was made on the basis of the following criteria: (1) dizziness provoked by head positions, (2) temporal relationship between intensity of dizziness and neck pain, and (3) the absence of any other disorder which explains the dizziness (Knapstad et al. 2019, and Reiley et al. 2017 [1, 2]). Clinical assessment included neck (i.e. mobility, proprioception, muscle function and disability) and balance tests (i.e. static and dynamic balance). Patients with and without CGD were compared using independent samples t-tests. Results: Regarding the neck tests, patients with CGD had significantly higher scores on the NBQ (p=0.011) and head repositioning accuracy (HRA) test towards extension (p=0.039) compared to patients without CGD. There were no significant differences between both groups in scores for cervical range of motion (flexion (p=0.885); extension (p=0.756); rotation left (p=0.910); and rotation right (p=0.593)), HRA test (towards flexion (p=0. 166); extension (p=0.0); rotation left (p=); and rotation right (p=)), deep neck flexors test (p=0.540); myofascial TRPs (amount (p=197), pain intensity (p=0.969) and dizziness intensity (p=0.156)). Regarding the balance tests, patients with CGD had a significantly better score on the Tandem Gait (p=0.039) than patients without CGD. For static balance (p=0.542), Timed-up and Go test (p=455), Functional Gait Assessment (p=752) there were no significant differences between both groups.
Conclusion: Patients with CGD have higher scores on NBQ, HRA towards extension and Tandem Gait compared to patients without CGD. There were no differences in scores between patients with and without CGD on the other neck and balance tests. Further research into the diagnostic value of the NBQ, HRA extension and tandem gait tests is needed.
References
1. Knapstad, M.K., Clinical characteristics in patients with cervicogenic dizziness: A systematic review. Health science reports, 2019.
2. Reiley, A.S., et al., How to diagnose cervicogenic dizziness. Arch Physiother, 2017. 7: p. 12.
Evaluation of the effect of dynamic visual acuity exercises in covert and overt saccades in unilateral vestibular loss. The vestibular ocular reflex (VOR) ensures gaze stability during head rotation by generating eye movements that are equal and opposite to head rotation. When vestibular loss is pre-
sent, an individual is unable to maintain gaze on a target during ipsilesional head rotation. Instead, the eyes move with the head(due to the reduction in VOR gain), which causes visual blurring for the patient with uncompensated vestibular loss. The purpose of the present study was to examine the efffect of dynamic visual acuity in the latency of the corrective (covert and overt) saccades.
A total of seven patients diagnosed with unilateral vestibular hypofunction were examined with vídeo head impulse test before and after vestibular rehabilitation. The gain of vestibular ocular reflexe (VOR) and the latency of the covert and overt saccades were measured. The vestibular rehabilitation were six sessions of exercices of dymamic visual acuity (Framiral ©)with passive head movements, in three weeks, twenty minutes per session.
All of patients had improved the score in Dizziness Handicap Invetory and reported less symptomatic to return to their typical activities of daily living.
The study of the correcitve saccades showed that the latency of covert saccades were reduced after rehabilitation, while the latency of the overt saccades were increased.
Even though this is a small study and the results are initials, we believe that exercices of dynamic visual acuity can be effective in patients with unilateral vestibular loss.
And our findings suggest that corrective saccade latency can be related to measures of physical function.The extent to which saccade latency has the potential to be a useful target for vestibular rehabilitation is still to be determined and may be promising target to improve functional outcomes.
FP1380A case of juvenile cerebellar tumor ending in death
Akiyuki Yamato1,Takao Imai2
1Suita municipal hospital; 2Osaka university hospital
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
A 23-year-old man presented with a history of dizziness and headache for two months. He could not work because of the dizziness. He showed leftward horizontal nystagmus and mild bilateral low-tone sensorineural hearing loss. We suspected he had Meniere disease and prescribed him isosorbide. One week later, he showed wide step walking as cerebellar symptom. And he showed spontaneous upbeat nystagmus at sitting position, downbeat nystagmus in bowing and apogeotropic positional nystagmus in supine. MRI findings revealed a cerebellar cystic mass as an angioblastoma. He was planned to have a surgery at department of neurosurgery in our hospital. Next day, when he was in our hospital to check the examination for surgery, sudden-onset consciousness disturbance was occurred and was performed emergency decompressive craniectomy. But the surgery did not improve cerebral edema, and he died two weeks later.
Cerebellar infarction which is presented as acute vertigo can be diagnosed early. But on the other hand, cerebellar tumor is delayed in recognition because the cerebellar symptom progress gradually. When the recognition is delayed, like this case, brainstem compression is occurred suddenly. When we see patients complaining of dizziness with headache and vertical spontaneous nystagmus, we should consider the possibility of the brain tumor and perform MRI examination.
FP1382How peripheral vestibular damage affects velocity storage
Amsal Madhani1, Richard F. Lewis1,2,3, Faisal Karmali1,3
1Jenks Vestibular Physiology Laboratory, Massachusetts Eye and Ear Infirmary, Boston, MA; 2Department of Neurology, Harvard Medical School, Boston, MA; 3Department of Otolaryngology, Harvard Medical School, Boston, MA.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Velocity storage is a centrally-mediated mechanism that processes peripheral vestibular inputs. One prominent aspect of velocity storage is its effect on dynamic responses to yaw rotation. Specifically, when normal human subjects are accelerated to constant angular yaw velocity, horizontal eye movements and perceived angular velocity decay exponentially with a time constant circa 15-30 s, even though the input from the vestibular periphery decays much faster (~ 6 s). Peripheral vestibular damage causes a time constant reduction, which is useful for clinical diagnoses, but a mechanistic explanation for the relationship between vestibular damage and changes in these behavioral dynamics is lacking. It has been hypothesized that Bayesian optimization determines ideal velocity storage dynamics based on statistics of vestibular noise and experienced motion. Specifically, while a longer time constant would make the central estimate of angular head velocity closer to actual head motion, it may also result in the accumulation of neural noise which simultaneously degrades precision. Thus, the brain may balance these two effects by determining the time constant that optimizes behavior. We applied a Bayesian optimal Kalman filter to determine the ideal velocity storage time constant for unilateral damage. Predicted time constants were substantially lower than normal, similar to patients, and modeled interactions between age-related hair cell loss and peripheral damage. These results provide a mechanistic explanation for changes in velocity storage after peripheral damage. Results also suggested that even after peripheral damage, ipsilateral noise originating in the periphery or early central processing remains relevant in neurocomputations. Overall, our findings support the hypothesis that the brain optimizes velocity storage based on the vestibular signal-to-noise ratio.
FP1387Towards a digital health intervention for vestibular rehabilitation- usability, and outcomes of a novel platform
Dara Meldrum1, Deirdre Murray1,2, Roisin Vance2, Sarah Coleman2, Sonya McConnell2, OrlaHardiman1,3, Rory McConn Walsh14
1 Academic Unit of Neurology, School of Medicine, Trinity College Dublin Ireland. 2 Rehabilitation Department, Beaumont Hospital, Dublin, Ireland. 3Department of Neurology, Beaumont Hospital, Dublin, Ireland. 4 Department of Otorhinolaryngology, Beaumont Hospital, Dublin, Ireland
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Digital technologies are increasingly available and are reducing in cost. There is an opportunity to move to a digital health approach in vestibular rehabilitation but there is a paucity of suitable systems available and consequent lack of evidence to support their use. This study aimed to investigate a novel digital platform developed specifically for vestibular rehabilitation (comprising clinician software, a wearable sensor, and a patient facing app). Ethical approval was obtained from the local medical research ethics committee. Consenting participants (n=14; 9F:5M mean age 54) with a confirmed unilateral peripheral vestibular hypofunction used the app for treatment, and therapists (n=4) used the platform to deliver vestibular rehabilitation over a mean of 17.4±8.8 weeks. The design of the system enabled individualisation of all exercise parameters (frequency, intensity, type and time). In addition, and specifically for gaze stabilisation exercises, the target frequency (in beats per minute) at which the head was to move during exercise could be prescribed and adjusted by the clinician. During exercise, the metronome was audible to the patient at the prescribed frequency. Outcomes included the System Usability Scale (SUS), the Patient Enablement Instrument (PEI), change in subjective symptoms (numerical rating scales), percentage adherence to prescribed exercise and a semi structured interview on utility.
A significant reduction was found in symptoms of vertigo/dizziness (p<0.004), imbalance (p<.002), oscillopsia (p<0.04), and anxiety (p<0.02) after use. System Usability Scores were high for both clinicians (mean 85/100) and participants (mean 83.3/100) and high enablement was reported (mean PEI 7/12). No adverse events were recorded. Overall percentage adherence to the exercise prescription when measured digitally was highly variable and ranged from (4%-77%). At semi structured interviews, participants reported a high level of acceptance and satisfaction with digital delivery and no adverse events were recorded. Further work is required to investigate efficacy and how the wearable sensor impacts delivery of care. In conclusion, this usability study provided support for the digital delivery of vestibular rehabilitation.
Target Audience- Health care professionals referring to, or practicing in the area of vestibular rehabilitation.
FP1390Identification of early-stage Meniere’s disease as a cause of unilateral tinnitus
Haider Alsarhan
College of medicine / Mustansiriyah University
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD? No
Introduction: Meniere’s disease (MD) is characterized by episodic symptoms, including vertigo, hearing loss, and tinnitus.
Objectives: in this study, cases of unilateral tinnitus were investigated for MD.
Method: Twenty-two patients who presented with chronic unilateral tinnitus on puretone audiograms showing an average threshold better than 25 dB HL and thresholds in the lower frequencies worse than those in the higher frequencies by more than 10 dB were suspected to have early-stage MD and underwent electrocochleography (ECochG). Patients showing ECochG findings conclusive for MD were compared to a control group of patients presenting with chronic unilateral tinnitus on pure-tone audiograms showing an average threshold better than 25 dB and thresholds in the higher frequencies worse than those in the lower frequencies by more than 10 dB.
Results: Eighteen of the 22 patients included in this study showed elevated summating potential amplitude to action potential amplitude ratios in ECochG (suggestive of endolymphatic hydrops due to MD) and were followed up for 2 months; 14 of them experienced at least two attacks of vertigo or unsteadiness. In contrast, only one patient in the control group reported two or more attacks of vertigo or unsteadiness in the 2 month observation period. The incidence of this finding in the two groups was significantly different.
Conclusion: Patients with early-stage MD can present with only unilateral tinnitus. Thus, the addition of “pure-tone audiograms showing lower-frequency thresholds worse than higher-frequency thresholds” to the probable MD category in the globally agreed diagnostic criteria for MD, may be useful
FP1401Combined Furosemide and Methylpredisnolone Dehydration test for Ménière disease, A Case Series
Rosario La Gumina, Alfarghal Mohamad, Giulio Dehesh
Sciacca Hospital, ENT Department, Sciacca (Ag)
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
Purpose: In this case series , we explore the efficacy of combined Furosemide and Methylpredinsolone dehydration test on recovery of vertigo and hearing loss in patients with Meniere’s disaese with findings suggestive of Endolymphatic Hydrops
Materials and Methods: Non-invasive Electrocochleography was recorded using TM-Wick tympanic electrodes, the test was conducted for 30 patients (20 Females, 10 Males; Age range between 25-75 years)
At the early stage of Meniere’s disease with initial presentaion of symptoms, when the diagnosis is uncertain, the ECochG test could show a typical pattern suggestive of endolymphatic hydrops (levine 1992, aso 1991), thus it could be useful in differential diagnosis . ECochG tests were conducted on patients during the initial activity of the disease, with vertigo, fluctuating SNHL, ear fullness and tinnitus, or in absence of vertigo (cochlear hydrops ) . Non-invasive Electrococleography was performed before adminstration of the dehydartion combination, then at 30 minutes, 45 minutes and 60 minutes after administration of a diuretic and Steroid, using 40 mg Frusemide and 40 mg Methylpredinsolone intramuscular injection
The ECochG test results were analyzed and interpreted according to the follwoing parameters :
• SP / AP amplitude ratio greater than 0.4 indicative of Endolymphatic Hydrops
• SP / AP area ratio > 194 is a discriminative indicator of the presence of hydrops (Al- Momani et.al, 2009)
Conclusions: The Frusemide -Methyl-predinsolne dehydration test has shown to have significant effect on all the patients included in the series and it can be important for several reasons:
First. It can drastically reduce endolymphatic hydrops with immediate sense of well-being of the patient and immediate improvment of hearing
Second: It can guide the choice of the therapeutic regimen to be used as maintinance oral therapy
Third, in cases where there is no improvment of hearing or reduction of SP/AP ratio with this combination of drugs, then it is necessary to shift to other therapeutic strategies as intra-tympanic injections or hearing aid fitting
A progressive reduction of the SP/AP & SP/AP area ratio from pathological to physiological values was found to be correlated to a partial recovery of patient’s hearing loss, this was clear from ECochG tests performed at 30, 45, and 60 minutes after adminstartion of Frusemide and Methylpredinsolone in patients with Meniere’s disease
FP1422Investigation of Chronic Symptoms in Patients with Unilateral Vestibular Hypofunction: A Systematic Review
Karabulut M1, Laer van L2,3, Rompaey van V4, Hallemans A2,3, Vereeck L2,3, Guinand N5, Perez Fornos A5, Berg van de R1,6
1Division of Balance Disorders, Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Centre+, Maastricht, The Netherlands; 2Department of Rehabilitation Sciences and Physiotherapy / Movant, Faculty of Medicine and Health Science, University of Antwerp, Belgium; 3Multidisciplinary Motor Centre Antwerp (M2OCEAN), University of Antwerp, Belgium; 4Department of Otorhinolaryngology and Head & Neck Surgery, University of Antwerp, Edegem, Belgium; 5Division of Otorhinolaryngology and Head-and-Neck Surgery, Department of Clinical Neurosciences, Geneva University Hospitals, Geneva, Switzerland; 6Faculty of Physics, Tomsk State University, Tomsk, Russia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Aim: To systematically review the full spectrum of chronic symptoms in patients with unilateral vestibular hypofunction (UVH).
Method: An extensive search was performed in Pubmed, Web of Science, Embase, and Scopus to investigate self-reported symptoms and questionnaire-based symptoms in patients with UVH. All original studies ranging from full-text clinical trials to case reports, written in English, German, and French, were included. Manuscripts in which the methodology was insufficiently reported, were excluded. Conference abstracts/-reports, letters, abstract only, animal studies, editorials, (systematic) reviews, and meta-analysis were also excluded.
Results: A total of 1608 studies were retrieved in four different databases. Forty-six studies were included after title-abstract selection and full-text selection by two independent reviewers. The frequency of self-reported symptoms of UVH patients included: chronic dizziness (89.62%), imbalance (81.06%), oscillopsia (22.36%), and recurrent vertigo (71.03%). UVH could be accompanied by hearing loss (82.43%) and tinnitus (80.45%). Four clinical studies reported additional symptoms beyond vestibular and hearing deficits such as headaches, autonomic symptoms, limited social activities, depression, concentration difficulties, memory impairment, and reduced quality of life. Regarding questionnaire-based symptoms, mean total scores of DHI and VAS scores were reported. Mean total DHI scores (20 studies) were 47.85±13.68 (pre-intervention, e.g. before vestibular rehabilitation) and 25.64±10.90 (post-intervention). In five studies, mean total VAS scores were 6.55±1.26 (pre-intervention) and 3.30±1.38 (post-intervention).
Conclusions: This systematic review demonstrates that a spectrum of symptoms is associated with UVH, of which chronic dizziness and imbalance are most reported. These symptoms can significantly influence quality of life. However, none of the reviewed studies in this systematic review provided a comprehensive overview of all chronic symptoms in UVH. Therefore, qualitative studies such as semi-structured interviews should be performed to investigate the full spectrum of chronic symptoms in UVH.
Keywords: unilateral vestibular hypofunction, chronic symptoms, dizziness, imbalance, vertigo
FP1429Vestibular Precision: Impacts on Perception, Eye Movements, Posture, and Neurons
Faisal Karmali1, Ana Diaz-Artiles2
1Harvard Medical School / Massachusetts Eye and Ear, Boston, USA; 2Texas A&M University, College Station, USA.
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ⊙ No
Two fundamental properties of any system are accuracy and precision. This includes the nervous system and the vestibular system in particular. While inaccuracy is a measure of mean error from an ideal response, imprecision assesses variability in the response. One cause for this imprecision (i.e., reduced precision) is thought to be neural noise in sensory, motor, and perceptual processing. In this presentation, we will review the literature on this topic. Our first goal is to demonstrate the benefits of examining vestibular precision, and that fundamental characteristics of vestibular function may be missed if accuracy alone is studied. Our second goal is to bring together findings about the role of vestibular precision in the vestibulo-ocular reflex, perception, posture and neurons. Studying interrelationships between these behaviors is possible because most methods used to study vestibular precision relate responses to the underlying neural noise, described by the standard deviation of a Gaussian function. A number of factors that influence vestibular precision have been studied. For example, variations in vestibular precision have been found with age, pathology, medication, body orientation, stimulus amplitude, stimulus frequency, motion direction, and electrical/mechanical vestibular stimulation. No evidence has been found for sex differences. Precision is optimized by the CNS during fusion of multisensory cues, including vestibular cues. Vestibular precision is correlated between perception and the vestibulo-ocular reflex, and perception and posture, suggesting that these measures reflect a common, sensory source of noise. These results underscore the significance of incorporating both vestibular precision and accuracy measures into studies. (This presentation will review material that was also reviewed in a peer-review article: Diaz-Artiles A, Karmali F. Vestibular precision at the level of perception, eye movements, posture, and neurons. Neuroscience. 2021 Jun 2.)
Supported by NIH/NIDCD R03-DC013635 and R01-DC018287 and NASA 80NSSC20K1499.
FP1433Catch-up saccades in unilateral vestibulopathy: the role of prediction
Hassen Kerkeni1, Athanasia Korda2, Miranda Morisson2, Georgios Mantokoudis2, David Samuel Zee3, Stefano Ramat4
1Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 2Department of Otorhinolaryngology, Head and Neck Surgery, Bern University Hospital, University of Bern, Bern, Switzerland; 3Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA; 4Laboratory of Bioengineering, Department of Electrical, Computer and Biomedical Engineering, University of Pavia, Pavia, Italy
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
⊙ Yes ○ No
When the demands for visual stabilization during head rotations overwhelm the ability of the VOR to produce compensatory eye movements, our brain produces corrective saccades that bring gaze towards the intended target. This behavior is seen during head impulse testing in unilateral loss vestibular patients with rotations toward the affected side. These catch-up saccades help improve visual stabilization by increasing the time during which gaze is on target. Saccadic corrections triggered, even while the head is still rotating, improve dynamic visual acuity. We investigated the role of prediction in producing such corrective movements in 14 subjects during passive, automated head impulses while viewing a stationary target with both unpredictable (speed and direction) and predictable stimuli. On the affected side with unpredictable head impulses, gaze error at the end of the head movement, and saccade latency were significantly (p<<0.001) greater, and VOR gain was significantly (p<<0.001) less. With predictable head impulses, analyzing trials with saccades beginning before the end of the head movement (covert saccades), gaze error at the end of the saccade was significantly less than with unpredictable ones (4.2±2.8 and 5.6 ±3.2 degrees, p<<0.001). No significant differences in saccade latency, gaze error at the end of the head movement or at the end of the corrective saccade, or in VOR gain, were found during head impulses to the healthy side.
Using a LATER (Linear Approach to Threshold with Ergodic Rate) analysis of saccade latency distributions on the affected side we developed a hypothesis for the mechanism triggering compensatory saccades in the time window before new visual error information might be used; during or in the immediate post head movement period. We propose two rise-to-threshold decision mechanisms for triggering saccades in this time frame. One mechanism is responsible for most corrective saccades, the other triggers saccades earlier (< 100 ms after the onset of head movement). The larger number of early corrections during predictable head impulses suggests that the threshold for the early mechanism is reduced, indicating a higher level of confidence in the mechanism that decides to trigger the earliest corrections.
FP1434Biphasic nystgamus in supine straight head extension: Consider Bilateral Benign paroxysmal positional vertigo
Hanaan Ashraf1, Vishal Pawar2
1Aster Al Rafa Polyclinic, International city Br. Dubai,U.A.E.; 2Aster Gardens Specialty clinic, Dubai, UAE
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Target audience- Neurologists, Neurotologists, Otologists, Audio-vestibular physician
Purpose: Bilateral benign paroxysmal positioning vertigo (bBPPV) is rare, accounting for up to <10 % cases in the reported series. As per the literature, patients with bBPPV can show pure up-beating nystagmus in supine straight head extension due to the cancellation of the torsional components. Here we present an interesting case of bBPPV with biphasic nystagmus without cancellation of the torsional components.
Materials and Methods: The study was conducted at the outpatient dizziness unit, Aster Speciality Clinic, Dubai, UAE, from Jan 2019-Dec 2020. Detailed history taking and neurotological examination were performed in every patient. All patients with positional vertigo underwent positional testing with Dix-Hallpike testing (DHT), Head Roll test, Supine straight head extension (SSHE). 177 patients were diagnosed to have BPPV. We are presenting a case of bBPPV who satisfied the diagnostic criteria of both right and left posterior canal involvement as per the consensus documents of the committee for the Classification of Vestibular Disorders of the Bárány Society.
Results: 45 years gentleman presented with positional vertigo lasting for less than a minute on turning to either side in the supine position. He had a history of head injury 7 days ago. DHT on the right showed up-beating torsional (Dextro-cyclo-rotatory) nystagmus (Fig-1). DHT on the left showed up-beating torsional (Levo-cyclo-rotatory) nystagmus. SSHE showed up-beating torsional (Dextro-cyclo-rotatory) nystagmus followed by a pause and then up-beating torsional (Levo-cyclo-rotatory) nystagmus.
Fig-1)
Findings during the positional testing.
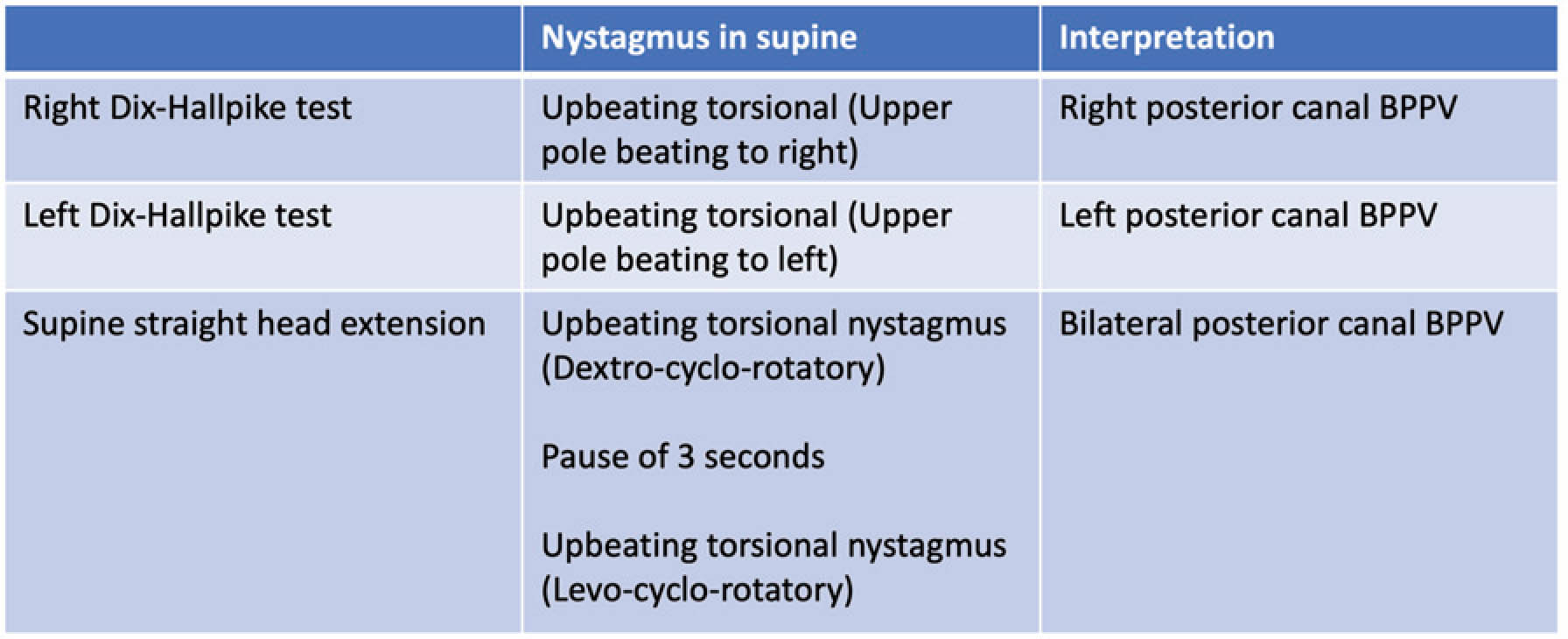
The patient was treated with Epley’s manoeuvre for either side, one after the other. The patient showed complete recovery after a one-week follow-up.
Fig-2)
Effect of the therapeutic manoeuvres.
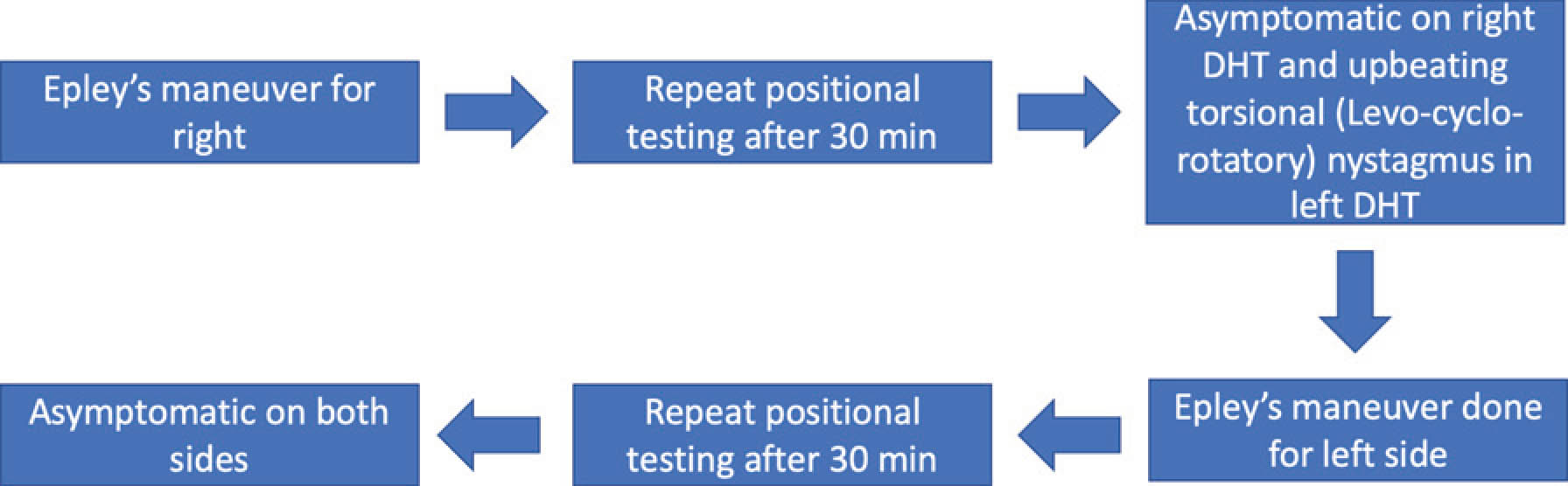
The points in favour of bBPPV over bilateral symptomatising unilateral BPPV were
1) Opposite sense nystagmus in the right and left DHT
2) Unilateral resolution of symptoms with Epley’s manoeuvre on either side
3) Biphasic nystagmus during SSHE
Conclusion: Bilateral BPPV is rare, and diagnosis can be challenging. Torsional components beating in opposite senses suggests a diagnosis of bBPPV over bilaterally symptomatic unilateral BPPV. SSHE can test all four canals in one go. This test can differentiate bilateral BPPV from bilateral symptomatising unilateral BPPV. Bilateral BPPV can present with biphasic nystagmus without cancellation of the torsional components during SSHE. We propose SSHE as a complementary test in cases of bilateral positive DHT.
FP1435The Magnetic Vestibular Response is Not Reduced in Meniere’s Disease
Jacob M Pogson1,3, Dale C Roberts1, Jorge Otero-Milan1,2, David S Zee1, Bryan K Ward1
1The Johns Hopkins University, Baltimore, United States; 2University of California, Berkeley, United States; 3Royal Prince Alfred Hospital, Camperdown, Australia
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes
Many studies have found that ears with Meniere’s Disease (MD) show a reduced caloric response and a normal head impulse test (HIT) response. One hypothesis suggests a deficit in low-frequency sensitivity with intact high-frequency sensitivity, while another attributes abnormal thermal endolymph hydrodynamics. Like the caloric test, magnetic vestibular stimulation (MVS) provides a relatively sustained (low-frequency) deflection of the cupula but probably involves more localized endolymph hydrodynamics—between the utricula macula and lateral and anterior cupolae. An important caveat is that MVS stimulates the lateral and anterior canals in both ears, with a specific horizontal-torsional pattern, different from unilateral caloric stimulation. We hypothesized that the MVS response would be reduced like the caloric response.
We examined the horizontal VOR response in 7 subjects (8 ears) with definite MD using the bi-thermal air caloric test for 60 seconds; the rotatory chair at a 60 °/s constant velocity, calculating using the slow-phase velocity (SPV) gain and Tc; the 3D video HIT gain; the MVS peak and final SPV to 5-minute exposures of 7 Tesla. We inferred utricular macula function measuring the amplitude of bone-conduced (BC) vestibular-evoked myogenic potentials (VEMPs). Ten control subjects (20 ears) were tested with the same battery. Comparisons were made using linear mixed models (LMM).
In MD ears the mean caloric peak SPV was significantly reduced (-4.6 °/s, p = 0.0005) compared to normal ears, but there were no significant differences in vHIT gain, rotatory chair gain or Tc (p > 0.85), MVS peak or final (p > 0.80) SPV, or BC VEMP amplitude (p = 0.53). In conclusion, the MVS and caloric response are dissociated. The reduction of the caloric but not MVS response in MD ears suggests stimulus frequency alone does not account for the dissociation between caloric and VHIT responses in MD. MVS provides a complementary test of horizontal canal function in MD ears.
FP1441Report of a pilot study of intratympanic corticosteroids in Ménière’s disease: Vertigo control
Gabriella Josefsson1, Dr Andra Lazar1, Mircea Romanitan MdPhD2 Tatjana Tomanovic, MdPhD1,2;
1-Hearing and Balance Department Karolinska University Hospital Stockholm, Sweden, Introduction; 2CLINTEC, ENT, Karolinska Institute, Stockholm, Sweden
The main objective with this study was to assess the efficacy of intratympanic dexamethasone injection in controlling vertigo in a group of patients with unilateral Ménière›s disease refractory to medical treatment. Randomized studies of intratympanic corticosteroids treatment (ITS) in patients with Ménière’s disease (MD) have shown significant improvement in vertigo control but also in retaining vestibular function.
Materials and Methods: Adults with definite Ménière’s disease at the Department of Hearing and Balance at Karolinska University Hospital, who were refractory to regular medical treatment were offered to enroll in the study. A total of 4 injections of Dexamethasone 4 mgs/ml, over a 10 days period was given to the 28 participants. They fill out forms for vertigo before the treatment, 1 month respectively 4 months after the last intratympanic injection. The questionnaires used were FLS (Functional level scale), DHI (Dizziness Handicap Inventory), visual analogue scale of overall dizziness and quantity of vertigo attacks longer/shorter than 20 minutes.
Results: Twenty-eight patients, aged M ≈ 55 (27-78) affected by definite unilateral MD enrolled in a study. DHI shows a significant improvement one month and 4 months after treatment (p< 0,005), without any significant difference between follow up time points. FLS after 4 months shows mean reduction for 1 point. Four months after overall dizziness decreases for two points. Effective vertigo control for attacks shorter and longer than 20 min was achieved in >65% after one and 4 months of the treatment, evaluated according to AAO-HNS 1995.
Conclusion: Out of the 27 patients enrolled in this study 4 were consequently treated with gentamicin. One patient reported worsening of vertigo was found to have BPPV and was successfully treated with repositioning maneuver. The goal of ITS treatment is to avoid destructive treatments with gentamicin. In this study ITS showed a stable 4-month effect in vertigo control, which could be used as a precursor to destructive treatments.
FP1442Combo manoeuvre for unresolved Benign Positional Paroxysmal Vertigo
Tatjana Tomanovic
1Department of Hearing and Balance Disorders, Karolinska Hospital, Solna; 2Department of Clinical Science, Intervention and Technology, Karolinska Institute, Stockholm, Sweden
• Are you eligible and do you want to apply for the WON-SANG LEE AWARD?
○ Yes ○ No
Introduction: Since 1952 when Dix-Hallpike (DH) established positional testing is possible to recognize benign paroxysmal positional vertigo (BPPV). DH test is aimed specifically to reveal free-floating otoliths in posterior semicircular canal and provoke an objective nystagmus and subjective vertigo, simultaneously. Therefore the clinician can diagnose the vertical semicircular canal lithiasis if the typical nystagmus pattern is presented (combined vertical and rotatory nystagmus).
Material and Method: At our tertiary neurotology referral center comprised a group of 12 patients with typical up /down beating rotational nystagmus in DH position with typical duration, latency but without fatigability and resolution on repeated Yacovino, Semont and Epley manoeuvre applied at least two times with a month apart. Finally, all patients were obtained with “combo manoeuvre” (CM) with direct resolution.
Results: In our interventional clinical study 6 /12 patients (M age=67) were treated with CM after two to three months of the BPPV onset. Remaining five patients were effectively threated with TTCM at first consultation with immediate symptom resolution. Adverse event in form of lateral canal BPPV was obtained in one of the patients, afterwards successively threated with Barbeque manoeuvre.
Conclusion: Patients with history of long-lasting symptoms of positional vertigo with unresolved BPPV on repeated repositioning manoeuvres were studied. Patients displayed every time the typical up beating nystagmus in DH indicating that otoliths are not living the vertical canals. The pathophysiology behind it can be the anatomy variation in form of flattened superior part of the semicircular canal. Combined treatment (Epley + Barbeque) named “combo manoeuvre” showed effectiveness in symptom and nystagmus release in this group of patients. Effective treatment of patients with persistent BPPV requires a different treatment algorithm and CM can be one of them.




