The impact of disease duration in persistent postural-perceptual dizziness (PPPD) on the quality of life, dizziness handicap and mental health
Abstract
BACKGROUND:
Persistent Postural-Perceptual Dizziness (PPPD) is a chronic functional disorder which interferes with the way individuals experience their personal, social and work life.
OBJECTIVE:
To study the impact of disease duration in PPPD on the quality of life (QOL), dizziness handicap and mental health on the patients.
METHODS:
A prospective study comparing the EQ-5D for QOL, Dizziness Handicap Inventory (DHI) and DASS-21 between 27 patients with PPPD and 27 of those who have recovered from an acute vestibular event. Similar parameters between PPPD patients with symptoms less than one year and more than a year were compared.
RESULTS:
The PPPD patients were predominantly females and middle-aged with significantly higher DHI scores (mean 48.3 + 25.7, p = 0.00002), higher total mean scores in the DASS-21 (mean 21.6 + 13.7, p = 0.009) and poorer QOL with mean EQ-5D VAS of 67.9 + 17.3 (p < 0.00001). PPPD patients with symptoms for more than a year had significant increase in physical handicap (p = 0.041) as well as anxiety levels (p = 0.008).
CONCLUSIONS:
PPPD is predominantly seen in females and middle-aged which significantly reduces the QOL, increases dizziness handicap and increases depression, anxiety and stress levels. The increase in duration of illness further increases the anxiety levels and physical handicap.
1Introduction
In 2017, the Barany’s Society Classification Committee amalgamated the main elements of postural phobic vertigo, space motion discomfort, visual vertigo and chronic subjective dizziness to form persistent postural-perceptual dizziness (PPPD) [21]. It is essentially a chronic functional disorder plaguing the sufferers with persistent dizziness or unsteadiness for at least 3 months which is exacerbated by upright position, being in motion and or exposure to busy visual stimuli [21]. While the disorder is largely precipitated by an acute vestibular event such as BPPV, there has since been reports of primary PPPD where no acute event is reported [9].
As physical examination, clinical laboratory testing and vestibular evaluation may be normal in PPPD [21, 22], advances in neuroimaging have provided new insights in patients with PPPD illustrating the delicate changes in functional activity and inter-network connectivity involving the vestibular, visual and emotion processing centers [10, 12, 13, 24, 26]. However, the functional MRI is not easily available and diagnosis relies heavily on clinical history [21].
Studies have since shown that PPPD is more often seen in females and middle aged [1, 4, 26, 27], interferes with the way individuals experience their personal, social and work life [20] and treatment is patient centric that begins with communication and education regarding the disorder [16]. However, there has not been studies that investigated the impact of disease duration in an already chronic ailment. Hence, the aim of this study is to understand the impact of disease duration in PPPD on the quality of life, dizziness handicap and mental health on the patients.
2Methodology
This was a prospective observational study registered with the National Medical Research Ethics Committee (NMRR-19-35-45775). Consenting patients diagnosed with PPPD aged 18 and above, attending the Otorhinolaryngology (ORL) Clinic between 2019 and 2021 were recruited. Demographic data such as age, gender, co-morbidity illnesses were documented. Patients were examined and had hearing and vestibular assessment performed including pure-tone audiometry, tympanometry, video nystagmography, video head impulse test, rotatory chair and VEMP to confirm the diagnosis of PPPD. The PPPD patients were treated based on their complaints with vestibular rehabilitation therapy (VRT) with or without cognitive behavioral therapy (CBT) and medications such as Selective Serotonin Reuptake Inhibitor (SSRI) under the counsel of a psychiatrist. The control arm consisted of age and gender-matched patients attending the ORL Clinic who had dizziness but resolved within three months and was not on any psychotropic or vestibular drugs. Sample size was calculated with a significance level (α) of 5%, power (1-β) of 80% and using continuous means of DHI as an endpoint from the study conducted by Ertugrul 2019 [7] with mean of 51.81 and standard deviation of outcome of 17.04 (control mean 38), total sample size required was 48 (24 in each group).
2.1Questionnaires
Recruited patients (PPPD and controls) were required to answer three validated questionnaires. EuroQol-5D (EQ-5D) [2] which was designed to measure and value health status was used to evaluate the generic quality of life (QOL) by measuring one question for each of the five dimensions which include mobility, self-care, usual activities, pain/discomfort and anxiety/depression. If the patient had no problems carrying out a task, they scored 1 and if they had some problems, they scored 2 and if they were unable or has severe pain, they scored 3. The lower the score, the better the QOL. It also included a Visual Analogue Scale (EQ-5D VAS) where respondents could gauge their perceived health status from 0 (worst health state) to 100 (best health state).
To assess the dizziness handicap, the English and Malay version of Dizziness Handicap Inventory (DHI/MYDHI) [28, 29] was used. It consisted of 25 questions, seven to assess physical aspects; nine to assess emotional aspects and nine to assess functional aspects. Patients answered no (score 0), sometimes (score 2) or always (score 4). The maximum score indicating highest handicap is 100 points.
The Depression Anxiety and Stress Scales or DASS-21 [14] was used to assess the psychometric characteristics with 21 items. Patients answered either no (score 0), sometimes (score 1), good part of (score 2) or most of the time (score 3). At the end of scoring, level of depression, anxiety and stress was scored separately as well as the total was tabulated (maximum score 63 indicating poorest mental health). The English and validated Malay version was used in this study was based on patient preference.
2.2Statistical analysis
To compare continuous variables including the changes over time for the DHI, DASS-21 and EQ-5D between the two groups, the student’s t test was used. The chi-squared and Fischer’s exact test methods were used for comparison of categorical variables between the 2 groups. Linear regression modeling was used to study the relationship between EQ-5D VAS, DHI and DASS-21. The level of significance was set at 5% (p = 0.05).
3Results
3.1Quality of life, Dizziness Handicap and Mental Health in PPPD
There were 27 patients with PPPD with mean age 45.2±10.9 who participated in this study with 18 (66.7%) females. 4 (14.8%) of the PPPD patients did not have any obvious precipitating triggers, 8 (29.6%) patients were triggered by BPPV, 5 (18.5%) vestibular neuritis, 4 (14.8%) stroke, 3 (11.1%) labyrinthitis, 2 (7.4%) panic attacks and 1 (3.7%) post concussion. The 27 age and gender-matched controls had a mean age of 45.8±13.2 (difference between mean age p value = 0.434). Results of the questionnaires are presented in Table 1. QOL was significantly affected as more patients with PPPD reported having problems with mobility (p = 0.004), usual activities (p = 0.0004), pain or discomfort (p = 0.003) and anxiety or depression (p = 0.029). Only the aspect of self-care was unaffected. PPPD patients also perceived their overall health status (EQ-5D VAS) significantly lower with a mean score of 67.9±17.3 as compared to 88.3±12 in the control group (p < 0.00001). In terms of the DHI, when compared to controls, PPPD patients had significant handicap in the individual elements in the form of physical (mean = 13.4±7.9, p = 0.0006), functional (mean = 19.7±10, p = 0.00001) and emotional (mean = 15.3±10, p = 0.00005) aspects as well overall scores (mean 48.3±25.7, p = 0.00002). PPPD patients also score higher in their DASS-21 with means scores for depression of 6±4.7, anxiety of 8±5.1, stress of 7.5±4.8 and overall mean scores of 21.6±17.3) (p < 0.05).
Table 1
Comparison between subjects with PPPD and those who have recovered from the acute vestibular symptoms (control group)
| PPPD | Controls | p value | |
| Age (years) | 45.2 | 45.8 | 0.434 |
| Gender (number of subjects) | |||
| Male | 9 | 9 | 1 |
| Female | 18 | 18 | |
| EQ5D (number of subjects) | |||
| Mobility | |||
| No problems | 13 | 23 | 0.004* |
| Has problems | 14 | 4 | |
| Self-Care | |||
| No problems | 24 | 26 | 0.299 |
| Has problems | 3 | 1 | |
| Usual Activities | |||
| No problems | 8 | 21 | 0.0004* |
| Has problems | 19 | 6 | |
| Pain/ Discomfort | |||
| None | 9 | 20 | 0.003* |
| Moderate to extreme | 18 | 7 | |
| Anxiety/Depression | |||
| None | 9 | 17 | 0.029* |
| Moderate to extreme | 18 | 10 | |
| EQ5D VAS (score) | 67.9 | 88.3 | < 0.00001* |
| DHI (score) | |||
| Physical | 13.4 | 6.4 | 0.0006* |
| Functional | 19.7 | 7.6 | 0.00001* |
| Emotional | 15.3 | 5.1 | 0.00005* |
| Total | 48.3 | 19.1 | 0.00002* |
| DASS-21 (score) | |||
| Depression | 6 | 3.3 | 0.015* |
| Anxiety | 8 | 4.1 | 0.002* |
| Stress | 7.5 | 5.2 | 0.048* |
| Total | 21.6 | 12.6 | 0.009* |
*p value < 0.05.
3.2Relationship between EQ5D, DHI and DASS-21
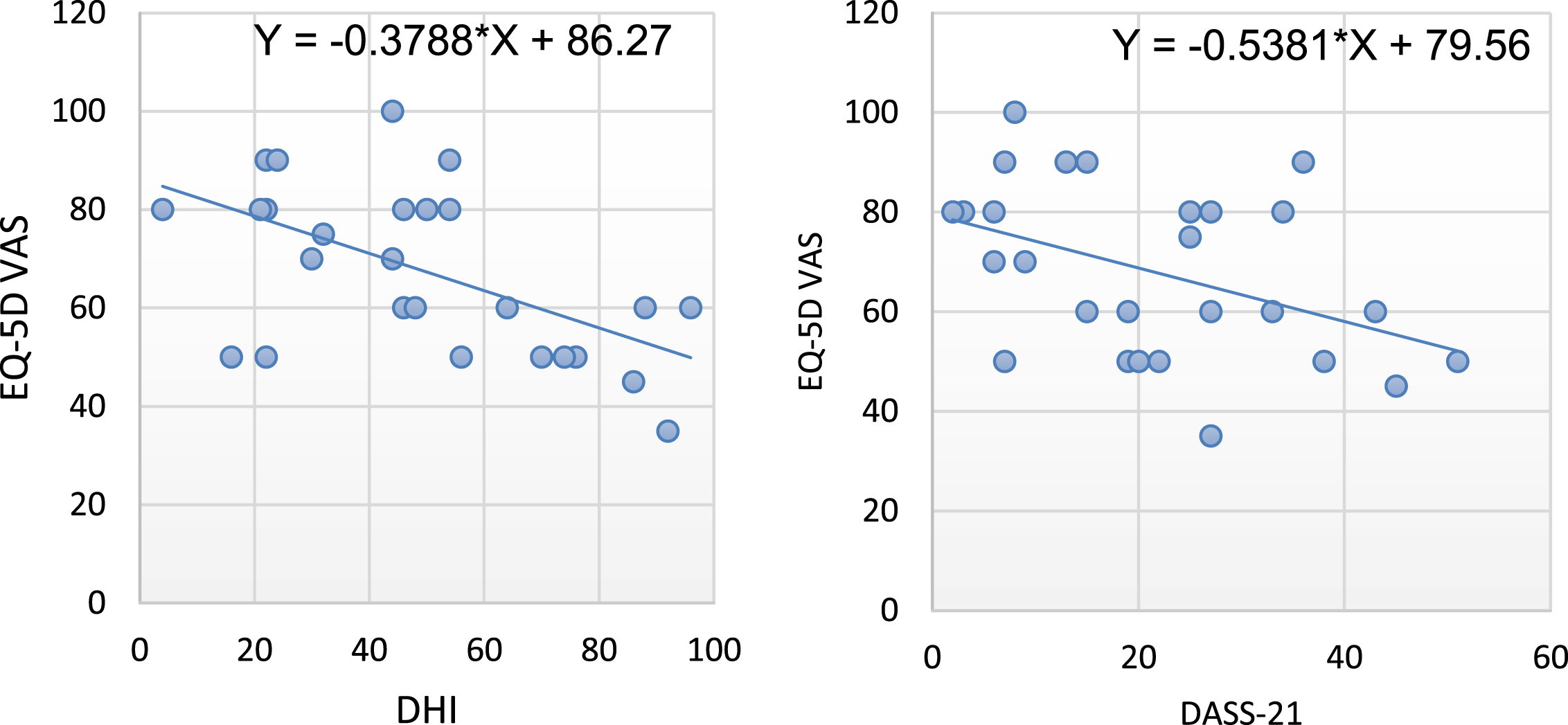
There was a significant negative linear relationship between the QOL using the EQ-5D VAS and the degree of dizziness handicap (DHI) (R2 = 0.3163, p = 0.0023) and total scores for DASS-21 (R2 = 0.183, p = 0.026) indicating reduction in QOL with worsening of dizziness handicap and mental well-being (Fig. 1).
Fig. 1
A significant negative linear relationship between the severity of Dizziness Handicap Index (DHI) and the health-related quality of life measured by EQ-5D VAS indicating poorer perception of health with increased dizziness handicap (R2 = 0.3163, p = 0.0023). There is also a significant negative linear relationship between DASS-21 and the health-related quality of life measured by EQ-5D VAS indicating poorer perception of health with worsening mental health (R2 = 0.183, p = 0.026).
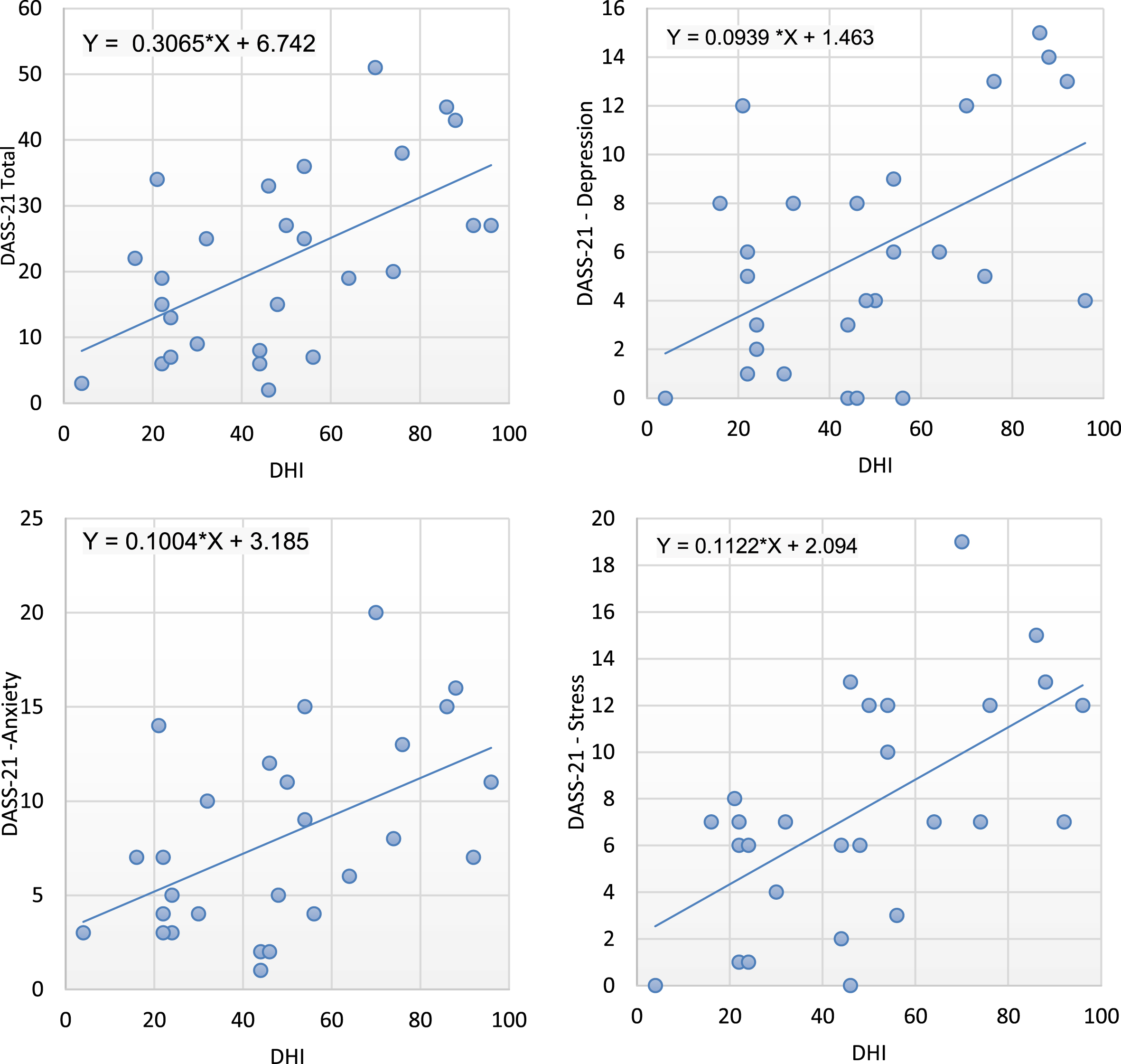
There was also significant positive linear relationship between the degree of dizziness handicap (DHI) and the level of depression (R2 = 0.2608, p = 0.0065), level of anxiety (R2 = 0.2555, p = 0.0072), level of stress (R2 = 0.3552, p = 0.001) and overall DASS-21 scores (R2 = 0.3277, p 0.0018). (Fig. 2)
Fig. 2
A positive linear relationship is seen between the DHI and overall mental health (R2 = 0.3277, p = 0.0018)as well as independently on depression (R2 = 0.2608, p = 0.0065)), anxiety (R2 = 0.2555, p = 0.0072)and stress levels (R2 = 0.3552, p = 0.001).
3.3Effect of duration of PPPD
In terms of duration of illness, 6 PPPD patients had the symptoms for less than 6 months, 5 had between 6 months and a year, 10 had between a year and 5 years and 6 had more than 5 years of symptoms. All of the patients did not receive a diagnosis for their condition until the day of the consultation in the ORL clinic. PPPD patients with symptoms for more than a year had significant increase in physical handicap (p = 0.041) as well as anxiety levels (p = 0.008). (Table 2)
Table 2
Effects of disease duration on PPPD patients
| Duration of PPPD | |||
| < 1 year | > 1 year | p value | |
| Age (years) | 48.1 | 43.3 | 0.133 |
| Gender (number of subjects) | |||
| Male | 3 | 6 | 0.58 |
| Female | 8 | 10 | |
| EQ5D (number of subjects) | |||
| Mobility | |||
| No problems | 7 | 6 | 0.182 |
| Has problems | 4 | 10 | |
| Self-Care | |||
| No problems | 9 | 15 | 0.332 |
| Has problems | 2 | 1 | |
| Usual Activities | |||
| No problems | 4 | 4 | 0.525 |
| Has problems | 7 | 12 | |
| Pain/ Discomfort | |||
| None | 6 | 3 | 0.053 |
| Moderate to extreme | 5 | 13 | |
| Anxiety/Depression | |||
| None | 5 | 4 | 0.268 |
| Moderate to extreme | 6 | 12 | |
| EQ5D VAS (score) | 73.2 | 64.4 | 0.099 |
| DHI (score) | |||
| Physical | 10.2 | 15.6 | 0.041* |
| Functional | 17.6 | 21.1 | 0.191 |
| Emotional | 14.2 | 16 | 0.322 |
| Total | 42 | 52.7 | 0.148 |
| DASS-21 (score) | |||
| Depression | 5 | 6.7 | 0.186 |
| Anxiety | 5.3 | 9.9 | 0.008* |
| Stress | 5.8 | 8.7 | 0.066 |
| Total | 16.1 | 25.3 | 0.043 |
*p value < 0.05.
4Discussion
This study recruited consecutive PPPD patients who visited the ORL Clinics and all consented to the study as they were keen to learn more about this condition. Our local PPPD patients were no different from the published demographic data of being predominantly females (66.7%) and middle aged [1, 4, 7, 27]. The DHI in PPPD had a mean of 48.3±25.7. This fell within the documented range of 44.5±18.9 to 59.8±19.3 in the recent literature [4, 9]. The DHI was significantly higher (p = 0.00002) than in the controls which had a mean of 19.1±22.2 and this further supports the findings of those in literature [7, 9, 25].
The raised dizziness handicap was accompanied with a reduction in QOL in PPPD patients by 20 points where PPPD patients scored the EQ-5D VAS at 67.9±17.3 as compared to 88.3±12 in those who recovered from the vestibular event (p = 0.00001). Habs et al also found a 20 point drop in the EQ-5D VAS scores from 78 points which was the country-related population norm to 58±20 reported by their PPPD patients [9]. It was interesting to note that while most of the dimensions in the QOL in our PPPD patients was affected, self-care was spared. However, when looking back on data studying non-specific dizziness and its impact on QOL, it has been established that dizziness leads to poorer QOL especially in physical and social functioning [8]. Cheng et al had found that more severe dizziness tended to have poorer quality of health which was not seen in mild and moderate dizziness handicap levels. Bodily pain, general health, role limitation due to emotional problems and mental health were the main domains affecting the QOL [5] which were similar to the domains our population had problems with such as mobility, performing usual activities, pain and mental health.
We also noted a linear positive relationship where higher levels of DHI also had higher overall DASS-21 scores (p = 0.0018) as well as individual aspects such as depression (p = 0.0065), anxiety (p = 0.0072) and stress (p = 0.001). Correlation between mood disorders and dizziness has been established and impairment is increased with comorbid anxiety [5]. Dizzy patients with anxiety and depressive moods also had greater emotional distress and handicaps [6]. Thus it is not surprising that PPPD is predisposed in subjects with anxiety or depression [7, 18, 25] and this was seen in our study population with significantly higher scores in depression (p = 0.015), anxiety (p = 0.002) and stress (p = 0.009) when compared to the control group. The mean value for depression was 6 which placed it as mild, anxiety was 8 (moderate) at and stress at 7.5 (mild). These values do not characterise them as having depression or an anxiety disorder as the values are borderline. However, they certainly demonstrate traits of anxiety and with greater tendencies for depressed mood. The anxiety trait affects the assessment of postural challenges resulting hypervigilance and adopting the high-risk control strategies during movement [4]. The functional MRI (fMRI) studies have shown significant functional alterations in the amygdala, insula, anterior cingulate, prefrontal cortex, superior frontal gyrus, para-cingulate and inferior frontal gyrus which are responsible for emotion processing and anxiety but also have connections to the central vestibular system [11, 12, 17, 24, 26]. Other fMRI studies also demonstrated the increase in activity and connectivity to the visual centres which explains the visual dependence in PPPD and this was particularly increased in neuroticism [15, 19, 24, 26].
Addressing the matter of chronicity, Best et al showed that there was no correlation between acute or chronic vestibular dysfunction on psychometric testing. Instead, a more important factor is how one reacts to the dysfunction [3]. Co-morbid psychiatric disorders are known to emerge in a vestibular event leading to psychological reactions such as anxiety, phobias, avoidance and depressive symptoms and this relationship is bidirectional as the anticipatory anxiety about future spells can sustain both physical and functional impairments [3, 23]. Our study went one step ahead to look at the effects of disease duration in a chronic condition in a population who already have anticipatory anxiety. We found a further increase in anxiety levels among those who had PPPD for more than a year (p = 0.008). This was accompanied by significant increase in physical handicap (p = 0.041). While it is now established that anxiety mood is not a core PPPD symptom but predisposes one to it [21], our findings support the notion that chronicity of PPPD symptoms worsens the mental health especially anxiety. This may lock the PPPD patient in a vicious never-ending cycle where being anxious predisposes one to PPPD and PPPD worsens the anxiety. Interestingly, the PPPD patients did not note any significant drop in overall health quality nor overall DHI scores with increased disease duration. There was also no significant effect on the depression or stress levels.
Grimby et al found that QOL decrease was most pronounced in those having experienced dizziness for less than 6 months and speculates that after 6 months, coping process begins and that reduces the negative effects of dizziness. However, they too found that physical mobility scores continued to worsen with the duration of dizziness as was seen in our study population [8]. Another aspect should be highlighted is the possible reason for the chronicity is the delay of diagnosis. Sezier et al reported their PPPD patients had lost confidence or trust in their health professionals with some being aloof or unable to provide them with answers or cure. While the patients did not necessarily expect the health care professionals to have all the answers, they wanted validation for an invisible and unidentifiable condition. This is where it is important for health care providers to build and sustain a stable therapeutic relationship tailored to the individual PPPD patient while providing validation to prevent self-stigmatisation [20]. Of the 27 PPPD patients in the study, 25 underwent vestibular rehabilitation, 4 were started on SSRI with CBT and 2 defaulted follow-up. After 3 months of treatment, 4(16%) patients reported complete resolution of symptoms of which 1 had less than a year of symptoms and 3 had more than a year of symptoms. 20 (80%) reported improvement of symptoms with 1 reporting no change in symptoms. More details on PPPD treatment outcome in this study group is being prepared for publication (CS Teh et al).
4.1Limitations
There is selection bias in this study as the patients were recruited from an ORL Clinic in a tertiary centre in a full COVID-19 hospital. While outpatient services are ongoing, the fear of the hospital’s reputation have reduced the number of potential PPPD patients walking in, especially those with milder symptoms. This has also resulted in the small sample size in the analysis of the effects of disease duration.
5Conclusion
Persistent postural-perceptual dizziness is a chronic functional disorder predominantly seen in females and middle-aged which significantly reduces the quality of life, increases dizziness handicap and increases depression, anxiety and stress levels. The increase in duration of illness further increases the anxiety levels and physical handicap. As anxiety predisposes and likely to perpetuate PPPD, the increased anxiety levels in an untreated patient may worsen the PPPD patient’s symptoms and quality of life. Hence, it is important to diagnose and begin therapy early to break the cycle.
Acknowledgements
We would like to thank Professor Dr Tan Seng Beng for his consultation on the matters of data analysis which has helped in making this study statistically meaningful.
Ethical approval
This study is registered National Medical Research Register and approved by the Medical Research and Ethics Committee (MREC) with the registration number NMRR-19-35-45775.
Conflict of interest and source of funding
This study was self-funded. There are no conflicts of interest, financial or otherwise.
Author contribution statements
All authors contributed equally to this work. CS Teh and N Prepageran were involved in the conception and design of the study. CS Teh was involved in the data acquisition, analysis and interpretation of data. CS Teh wrote the main paper. All authors discussed the results and implications and commented on the manuscript at all stages.
References
[1] | Adamec I. , Juren S. , Meaški M. , Krbot Skorić K. , Jažić L. , Crnošija I. , Milivojević and Habek M. , Persistent postural-perceptual dizziness: Clinical and neurophysiological study, J Clin Neurosci 72: ((2020) ), 26–30. https://doi.org/10.1016/j.jocn.2020.01.043 |
[2] | Balestroni G. and Bertolotti G. , EuroQol-5D (EQ-5D): An instrument for measuring quality of life, Monaldi Arch Chest Dis 78: (3) (2015) . https://doi.org/10.4081/monaldi.2012.121 |
[3] | Best C. , Interaction of somatoform and vestibular disorders, J Neuro, Neurosurg & Psy 77: (5) ((2006) ), 658–664. https://doi.org/10.1136/jnnp.2005.072934 |
[4] | Bittar R.S.M. and von Söhsten Lins E.M.D. , Clinical characteristics of patients with persistent postural-perceptual dizziness, Brazilian J Otorhinolaryngology 81: (3) ((2015) ), 276–282. https://doi.org/10.1016/j.bjorl.2014.08.012 |
[5] | Cheng Y.-Y. , Kuo C.-H. , Hsieh W.-L. , Lee S.-D. , Lee W.-J. , Chen L.-K. and Kao C.-L. , Anxiety, depression and quality of life (QoL) in patients with chronic dizziness, Arch Gerontology and Geriatrics 54: (1) ((2012) ), 131–135. https://doi.org/10.1016/j.archger.2011.04.007 |
[6] | Eckhardt-Henn A. , Breuer P. , Thomalske C. , Hoffmann S.O. and Hopf H.C. , Anxiety disorders and other psychiatric subgroups in patients complaining of dizziness, J Anxiety Dis 17: (4) ((2003) ), 369–388. https://doi.org/10.1016/S0887-6185(02)00226-8 |
[7] | Ertugrul S. , Söylemez E. and Soylemez T. , Determination of Predictors for Persistent Postural-Perceptual Dizziness, KBB-Forum 18: (3), ((2019) ) 249–256. |
[8] | Grimby A. and Rosenhall U. , Health-Related Quality of Life and Dizziness in Old Age, Gerontology 41: ((1995) ), 286–298. |
[9] | Habs M. , Strobl R. , Grill E. , Dieterich M. and Becker-Bense S. , Primary or secondary chronic functional dizziness: Does it make a difference? A DizzyReg study in 356 patients, J Neurology 267: (S1) ((2020) ), 212–222. https://doi.org/10.1007/s00415-020-10150-9 |
[10] | Huber J. , Flanagin V.L. , Popp P. , Eulenburg P. and Dieterich M. , Network changes in patients with phobic postural vertigo, Brain and Behavior 10: (6) (2020) . https://doi.org/10.1002/brb3.1622 |
[11] | Indovina I. , Riccelli R. , Chiarella G. , Petrolo C. , Augimeri A. , Giofrè L. , Lacquaniti F. , Staab J.P. and Passamonti L. , Role of the Insula and Vestibular System in Patients with Chronic Subjective Dizziness: An fMRI Study Using Sound-Evoked Vestibular Stimulation, Frontiers in Behavioral Neuroscience 9: (2015) . https://doi.org/10.3389/fnbeh.2015.00334 |
[12] | Lee J.-O. , Lee E.-S. , Kim J.-S. , Lee Y.-B. , Jeong Y. , Choi B.S. , Kim J.-H. and Staab J.P. , Altered brain function in persistent postural perceptual dizziness: A study on resting state functional connectivity, Human Brain Mapping 39: (8) ((2018) ), 3340–3353. https://doi.org/10.1002/hbm.24080 |
[13] | Li K. , Si L. , Cui B. , Ling X. , Shen B. and Yang X. , Altered intra- and inter-network functional connectivity in patients with persistent postural-perceptual dizziness, NeuroImage: Clinical 26: ((2020) ), 102216. https://doi.org/10.1016/j.nicl.2020.102216 |
[14] | Norton P.J. , Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups, Anxiety, Stress & Coping 20: (3) ((2007) ), 253–265. https://doi.org/10.1080/10615800701309279 |
[15] | Passamonti L. , Riccelli R. , Lacquaniti F. , Staab J.P. and Indovina I. , Brain responses to virtual reality visual motion stimulation are affected by neurotic personality traits in patients with persistent postural-perceptual dizziness, J Vest Res 28: (5–6) ((2019) ), 369–378. https://doi.org/10.3233/VES-190653 |
[16] | Popkirov S. , Staab J.P. and Stone J. , Persistent postural perceptual dizziness (PPPD): A common, characteristic and treatable cause of chronic dizziness, Practical Neurology 18: (1) ((2108) ), 5–13. https://doi.org/10.1136/practneurol-2017-001809 |
[17] | Popp P. , zu Eulenburg P. , Stephan T. , Bögle R. , Habs M. , Henningsen P. , Feuerecker R. and Dieterich M. , Cortical alterations in phobic postural vertigo—A multimodal imaging approach, Annals of Clinical and Translational Neurology 5: (6) ((2018) ), 717–729. https://doi.org/10.1002/acn3.570 |
[18] | Powell G. , Derry-Sumner H. , Rajenderkumar D. , Rushton S.K. and Sumner P. , Persistent postural perceptual dizziness is on a spectrum in the general population, Neurology 94: (18) ((2020) ), e1929–e1938. https://doi.org/10.1212/WNL.0000000000009373 |
[19] | Riccelli R. , Passamonti L. , Toschi N. , Nigro S. , Chiarella G. , Petrolo C. , Lacquaniti F. , Staab J.P. and Indovina I. , Altered Insular and Occipital Responses to Simulated Vertical Self-Motion in Patients with Persistent Postural Perceptual Dizziness, Frontiers in Neurology 8: ((2017) ), 529. https://doi.org/10.3389/fneur.2017.00529 |
[20] | Sezier A.E.I. , Saywell N. , Terry G. , Taylor D. and Kayes N. , Working-age adults’ perspectives on living with persistent postural-perceptual dizziness:Aqualitative exploratory study, BMJ Open 9: (4) ((2019) ), e024326. https://doi.org/10.1136/bmjopen-2018-024326 |
[21] | Staab J.P. , Eckhardt-Henn A. , Horii A. , Jacob R. , Strupp M. , Brandt T. and Bronstein A. , Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Bárány Society, J Vest Res 27: (4) ((2017) ), 191–208. https://doi.org/10.3233/VES-170622 |
[22] | Staab J.P. , Ruckenstein M. , Expanding the differential diagnosis of dizziness, Arch Otolaryngol Head Neck Surg 133: ((2007) ), 170–176. |
[23] | Staab J.P. and Ruckenstein M.J. , Which comes first? Psychogenic dizziness versus otogenic anxiety, The Laryngoscope 113: (10) ((2010) ), 1714–1718. https://doi.org/10.1097/00005537-200310000-00010 |
[24] | Teh C.S. , Mah M.C. , Rahmat K. and Prepageran N. , Neuroimaging Systematic Review in Persistent Postural Perceptual Dizziness: The Elaborate Alterations in the Delicate Network to Remain Balanced, Otol & Neurotol 2021; doi: 10.1097/MAO.0000000000003389 |
[25] | Trinidade A. , Harman P. , Stone J. , Staab J.P. and Goebel J.A. , Assessment of Potential Risk Factors for the Development of Persistent Postural-Perceptual Dizziness:A Case-Control Pilot Study. Frontiers in Neurology 11: ((2021) ), 601883. https://doi.org/10.3389/fneur.2020.601883 |
[26] | von Söhsten Lins E.M.D. , Bittar R.S.M. , Bazán P.R. , Amaro Júnior E. and Staab J.P. , Cerebral Responses to Stationary Emotional Stimuli Measured by fMRI in Women with Persistent Postural-Perceptual Dizziness, International Archives of Otorhinolaryngology (2020), s-0040-1716572. https://doi.org/10.1055/s-0040-1716572 |
[27] | Yan Z. , Cui L. , Yu T. , Liang H. , Wang Y. and Chen C. , Analysis of the characteristics of persistent postural perceptual dizziness: A clinical-based study in China, International JAudiology 56: (1) ((2017) ), 33–37. https://doi.org/10.1080/14992027.2016.1211763 |
[28] | Yorke A. , Ward I. , Vora S. , Combs S. and Keller-Johnson T. , Measurement Characteristics and Clinical Utility of the Dizziness Handicap Inventory Among Individuals With Vestibular Disorders, Arch Physical Medicine and Rehab 94: (11) ((2013) ), 2313–2314. https://doi.org/10.1016/j.apmr.2013.07.007 |
[29] | Zainun Z. , Na A. and Saat Ga M. , Translation and validation study of Malay version of dizziness handicap inventory (MYDHI), Medeniyet Med J 2017; https://doi.org/10.5222/MMJ.2017.170 |




