Danish short form Örebro Musculoskeletal Pain Screening Questionnaire: Translation, cross-cultural adaptation, and evaluation of measurement properties
Abstract
BACKGROUND:
Low back pain (LBP) is the leading cause of disability and an increasing sick leave in Denmark. Psychosocial risk factors have been linked to the development of LBP-related disability and work-absenteeism. The short form Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ-sf) was developed to screen for psychosocial risk factors and assess the risk of long-term disability and work-absenteeism.
OBJECTIVE:
To translate and cross-culturally adapt ÖMPSQ-sf into Danish and evaluate test-retest reliability with relative and absolute reliability and internal consistency in LBP-patients in a secondary setting.
METHODS:
A six-step translation and cross-culturally adaptation process was used. Forty-four patients with subacute and chronic LBP were recruited at an outpatient clinic.
RESULTS:
Test-retest reliability (
CONCLUSION:
The Danish ÖMPSQ-sf showed acceptable measurements properties in subacute and chronic LBP-patients. Further research is needed to assess other measurement properties of the ÖMPSQ-sf, in relation to validity, responsiveness, and the predictive ability before application in research or clinical practice.
1.Introduction
Low back pain (LBP) is globally the leading cause of disability and work absenteeism and it is considered a significant public health problem [1]. There is an increasing recognition of the multi-dimensional nature of LBP including genetic, biophysical, psychological, and social factors along with comorbidities [2, 3, 4].
The psychosocial factors also known as “yellow flags”, include a range of constructs such as psychological distress, painrelated fear, pain cognitions, and coping strategies and have been linked to the risk of and the development of persistent pain, disability and work absenteeism, although their individual importance and role is still unclear [5, 6].
As LBP most often is a self-limiting condition that passes within weeks with little or no intervention, identifying patients at risk of developing long term pain and disability is important, thus allowing health care professionals (HCPs) to allocate more comprehensive treatment and scarce resources to those who would benefit the most [3].
Assessment of psychosocial risk factors has become widely included in clinical guidelines on the management of LBP [7]. Studies suggest, however, that HCPs are not always able to accurately identify these risk factors by themselves [8], but that this can be improved by the use of patient reported screening tools [9, 10].
Several patient-reported measurements exist to evaluate psychosocial factors, e.g. the FearAvoidance Beliefs Questionnaire [11], the Start Back Tool [12], and the Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ-21) [13]. The ÖMPSQ-21 is a patient-reported psychosocial screening tool that has shown promising measurement properties [14]. It consists of 21 items that covers six factors: Function, pain, distress, fear-avoidance, return-to-work expectancy, and coping [5]. The ÖMPSQ-21 was designed to identify patients at risk of long-term work absenteeism and physical disability in relation to musculoskeletal pain [15, 16].
A shorter 10-item form of the Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ-sf) was developed from the original ÖMPSQ-21 in a Swedish and an English version to make the questionnaire easier to administer and thus enhancing its clinical utility [17]. The ÖMPSQ-sf was composed by selecting two items from five of the six factors identified in the original ÖMPSQ-21 as having the highest predictive ability. Thus, the questionnaire covers the factors: Pain, function, distress, return to work expectancy and fear-avoidance. The first item concerning pain duration is rated by selecting the appropriate time interval and scored from 1–10 points. The remaining nine items are rated on a 0–10 scale with 0 representing one extreme and 10 the opposite extreme leading to scores ranging from 1–100 [17]. Subsequently, other short versions of the ÖMPSQ have been proposed including a 10 and a 12-item version differing from the original ÖMPSQ-sf with regards to the items included [18, 19].
The ÖMPSQ-sf has shown acceptable measurement properties in both the original and translated versions including moderate predictive ability for long term sick leave in both an occupational population and a backpain population with an area under the curve (AUC) of 0.70 and 0.71, respectively [17, 20]. Two studies that used translated versions of the ÖMPSQ-sf have shown adequate to substantial relative and absolute reliability in different samples of patients diagnosed with backpain and that the short form performs comparable to the original ÖMPSQ-21 [20, 21]. The ÖMPSQ-sf has been found suitable to detect individuals with risk factors for prolonged disability from LBP in a working-age population with LBP [22].
The aim of the study was to translate and cross-culturally adapt the original short form Örebro Musculoskeletal Pain Screening Questionnaire [17] into Danish and subsequently to evaluate the test-retest reliability, internal consistency, measurement error, and smallest detectable change in a population of patients diagnosed with LBP recruited in a secondary setting.
2.Materials and methods
2.1Design
Translation and cross-cultural adaptation was conducted methodologically based on the model described by Beaton et al. [23] and subsequently the testing of measurement properties was conducted.
2.2Study sample
2.2.1Eligibility criteria
Patients between 18–60 years diagnosed with nonspecific LBP, disc herniation, spondylosis, spondylolisthesis, and central or lateral spinal stenosis referred to treatment at the outpatient back pain clinic at Bispebjerg and Frederiksberg Hospital in the Capital Region of Copenhagen, Denmark were consecutively screened for eligibility from June through August 2017. Patients were excluded if they had serious pathology (e.g., malignancy, spinal fractures, cauda equina syndrome), were receiving early retirement or disability pension, had serious cognitive impairments or if they were not able to read Danish, and hence, could not independently fulfill the outcome measurement.
2.2.2Recruitment
Patients were recruited by a physiotherapist in the outpatient clinic at their 2nd or 3rd visit to the clinic for both the translation and cultural adaptation process and for the evaluation of measurement properties. Eligible patients received verbal and written information about the study and signed informed consent before enrollment in the study.
2.3Translation process
Other translations of the ÖMPSQ-sf have been done through translating the original 21-item version and subsequently extracting the 10 short form items [20, 21]. The authors decided to translate the ÖMPSQ-sf directly from English to Danish, because the ÖMPSQ-sf performs comparable the original ÖMPSQ-21 [17].
The translation of the ÖMPSQ-sf was performed in accordance to the six-step guideline presented by Beaton et al. in 2000 [23]. This involves forward translation by two independent translators with the target language as their first language and synthesis of the forward translation. Then the synthesis was translated back to English by two independent native English-speaking persons with the aim of evaluating if the translation process changed the construct under investigation.
The pre-final version of the questionnaire was pretested through cognitive interviewing among the target population. The interviews explored the respondent’s comprehension of the individual questionnaire items, their process of choosing and reporting responses, and was done until data saturation. Data saturation was considered to be reached when three consecutive interviews identified no new problems and when the informants responded to all items as intended. Patients for the pretest interviews were recruited with as large heterogeneity as possible regarding age sex and educational level.
An expert panel consisting of health professionals with specialist knowledge within the field of LBP with relevant language skills and knowledge of translation of measurement tools produced the final version of the Danish ÖMPSQ-sf.
2.4Testing of measurement properties
The evaluation of measurement properties of the final Danish version of the ÖMPSQ-sf was based on and reported in relation to the COSMIN framework and taxonomy [24].
Patients were recruited consecutively and answered the questionnaire electronically on a tablet in a quiet environment at the inclusion site. Four days later an auto-generated email with a link for the second assessment were sent to the participants. If the respondents did not complete the questionnaire at the second assessment the system autogenerated a remainder email after 24 hours.
The four days interval were chosen as the participants were not considered to have neither progression nor regression in relation to the construct being assessed, and that an interval of four days between assessments days were considered sufficient to minimize the risk of recall bias [24, 25].
All surveys were distributed from the online survey distribution tool (SurveyXact®, Ramboell Management Consulting, Aarhus, Denmark).
2.5Statistical analysis
All analysis was conducted with SPSS version 22.0 (IBM Corp. Armonk, NY, USA). Internal consistency reliability was evaluated using Cronbach’s alpha. Cronbach’s alpha coefficients between 0.70 and 0.95 were considered to be adequate [26].
Test–retest reliability was evaluated using data from both assessments and a two-way random effects model, absolute agreement, single measurement model (ICC model 2,1), and ICC were interpreted as
Absolute reliability was evaluated using Standard Error of measurement (SEM), the 95% Limits of Agreement (LOA) and the Smallest Detectable Change (SDC).
The calculation of the SEM was based on the standard deviation of the measurements and the ICC2.1 from the test-retest reliability analysis [28], using the following formula:
Table 1
Characteristics of included participants
| Variable | |
|---|---|
| Participants included | 44 |
| Sex Female, | 26 (59) |
| Age, mean (SD) Pain within the last week Duration of pain 0–5 weeks, | 41.86 (11.33) 4.95 (2.20) 0 (0) 1 (2.3) 1 (2.3) 9 (20.5) 8 (18.2) 7 (15.9) 18 (40.9) 13.61 (2.97) 7.14 (4.69) 8.55 (4.16) 9.52 (4.69) 11.11 (4.51) 49.93 (14.03) 7.88 |
The 95% LOA was calculated to investigate the reproducibility and illustrated using a Bland Altman plot. The LOA is expressed in the same unit as the scale. SDC was calculated based on the formula:
Paired
Floor or ceiling effects was considered to be present if more than 15 % reached either the highest or the lowest score possible [29].
2.5.1Power calculation
A power calculation to establish a relevant sample size for the test-retest reliability analysis was calculated to
3.Results
3.1Translation process
The two forward translations were synthetized, and the two backward translations revealed no significant discrepancies. Thus, the synthesis was carried forward to the pretest. The pretest interviewing process reached data saturation after interviews with 15 participants. The translation process resulted in the inclusion of “normal daily activities” to items 8 and 10 to cover the concept of “unpaid work” such as home making or studying and shortening of the instructions for items 9 and 10 as they were found to be overly long and confusing. Changes were accepted by the expert panel, and subsequently approved by the first author of the original questionnaire. The final version of the Danish ÖMPSQ-sf is listed in the Appendix.
3.2Measurement properties
Forty-four participants, not including the pretest participants, were included and provided data for the first assessment. However, seven participants failed to complete the second assessment resulting in a response rate of 86% and a sample of 37 who provided data on both assessments. Most patients included in the study had a chronic pain problem as 95% of participants reported to have had their pain for more than 3 months. Characteristics of included participants are presented in Table 1.
3.2.1Internal consistency
The internal consistency (
3.2.2Test-retest reliability
Table 2
Test scores from test-retest analysis of the ÖMPSQ-sf, (
| Variable | Mean | SD |
|---|---|---|
| Total ÖMPSQ-sf score at first assessment* | 50.78 | 14.45 |
| Total ÖMPSQ-sf score at second assessment* | 50.86 | 15.25 |
ÖMPSQ-sf Örebro Musculoskeletal Pain Screening Questionnaire short form, SD standard deviation, *No significant difference between men and women.
Figure 1.
Bland and Altman plot – 95% limits of agreement. X-axis: The mean of test 1 and 2. Y-axis: The difference between test 1 and 2. The central horizontal line shows the mean difference between test 1 and 2 (
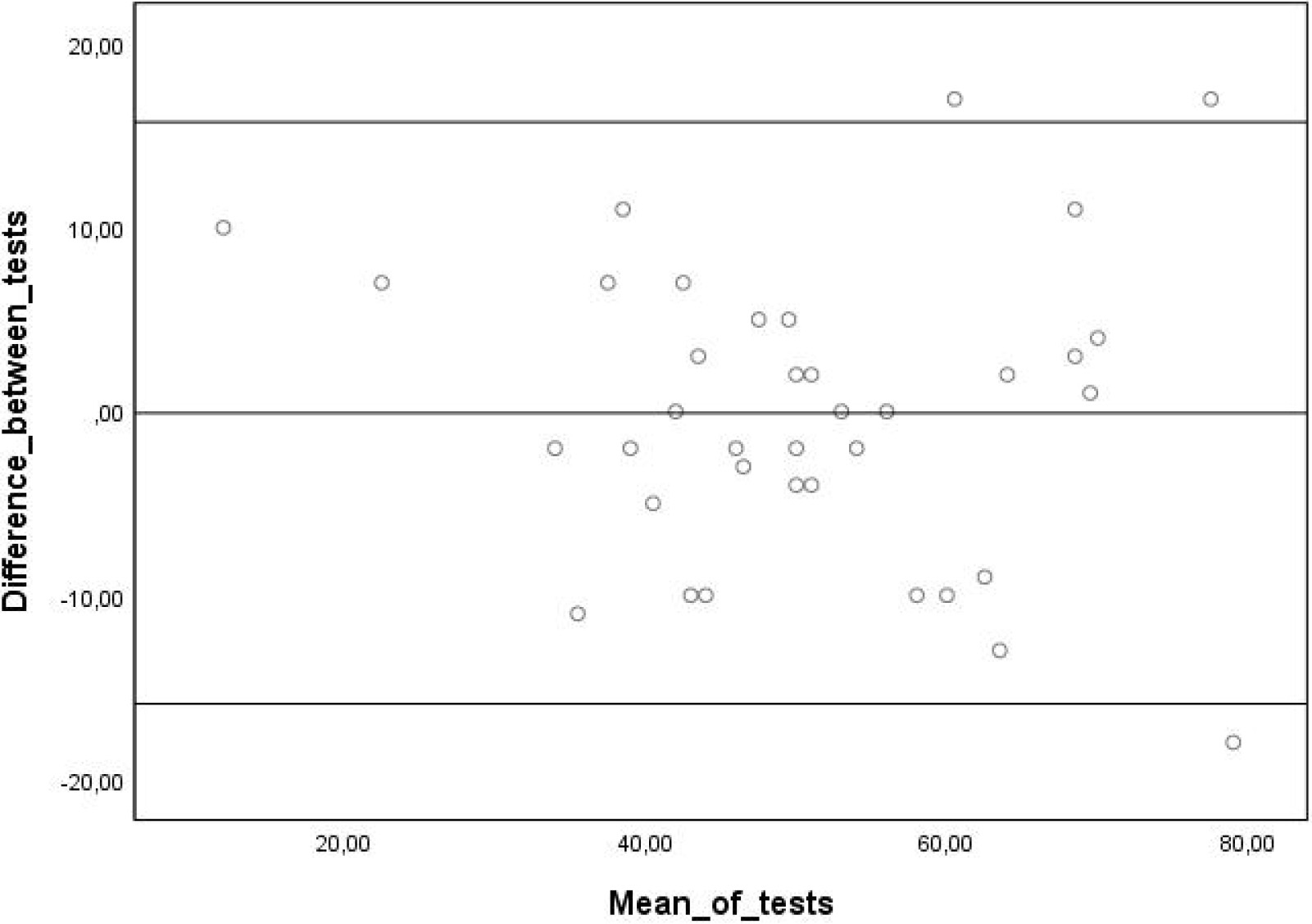
Thirty-Seven participants completed the two assessments with a mean of 4.89 days (1.08 SD) in between. Test scores from the test-retest analysis are shown in Table 2. The test-retest reliability (ICC2.1) for the total ÖMPSQ-sf score was found to be excellent,
3.2.3Absolute reliability
For the total score of the ÖMPSQ-sf the SEM was calculated to 3.97 points and the SDC to 10.87 points.
The LOA found in this study is (
4.Discussion
This study aimed to translate and culturally adapt the ÖMPSQ-sf to Danish conditions and subsequently test measurement properties. The questionnaire was successfully translated with minor changes implemented in the Danish version. An excellent ICC2.1 for test-retest reliability of the ÖMPSQ-sf was found in the present sample. Three studies have formerly investigated the test-retest reliability in patients diagnosed with non-specific LBP. Contrary to our findings, Fagundes et al. [21] reported the ICC for the Brazilian-Portuguese ÖMPSQ-sf to
In the evaluation of reliability of both the Brazilian Portuguese and the Hong Kong Chinese ÖMPSQ-sf the data for analysis was extracted from the original ÖMPSQ-21 [20, 21].
As in the present study, Beales et al. [9] tested the test-retest reliability ÖMPSQ-sf and found a comparable ICC of 0.90. The study, however, included participants with musculoskeletal pain that was recruited from a primary care setting with a rather short test interval time (a mean of 1.7 days). Apart from the shorter time-interval between assessments the findings are in line with those reported in the present study.
The absolute reliability in terms of SEM (3.97 points) and SDC (10.87 points) found in the present study were smaller than those found by both Fagundes et al. and Tsang et al. [20, 21], respectively SEM (6.67 and 5.9 points) and SDC (15.51 and 16.50 points). Also, for the 95% LOA the interval was narrower in the present study LOA (
There are no established guidelines on the appropriate time interval between the two assessments for evaluating test-retest reliability, as it depends on the stability of the property measured and in the case of patient-reported outcome measures, the number, and the complexity of the questions. Fewer items are easier to remember than many, and needs more time between measurements to minimize the recall bias [26]. The present study had a mean time between completion of the two assessments of 4.89 days, and similar to the time interval applied in other translation studies [20, 21]. A longer interval could possibly increase the likelihood of patients receiving treatment in between the two assessments thus compromising the stability of the construct.
In correspondence with the results found in the present study both Fagundes et al. and Tsang et al. reports an adequate internal consistency for the ÖMPSQ-sf (
As one of the key assumptions for the calculation of coefficient alpha is that the scale is unidimensional [30, 31], it can be discussed whether Cronbach’s
4.1Strengths and limitations
A strength of the present study was the online service for data collection that allowed for an accurate measure of time between completion of assessments and the possibility of sending automated follow up mails to non-responders. The small number of respondents in the testing of measurement properties is a limitation, as the recommended sample size is
The direct translation and subsequent testing of measurement properties of the ÖMPSQ-sf as its own entity, instead of translating the original questionnaire and constructing the short form and calculating measurement properties from the relevant items, is regarded as a strength of this study. It has increased user-friendliness through the removal of redundant meta text in the questionnaire. Furthermore, it may have increased the validity of the results as items may perform differently when answered as part of either the original 21-item questionnaire compared to answering the short form of the questionnaire alone. The authors of the present study decided to translate from English to Danish to ensure uniformity as most translations are likely to be based on the English version, and due to availability of health professionals with the required language skills. To further ensure the retention of the meaning the first author of the original ÖMPSQ-sf was included in the translation process. The items in the ÖMPSQ-sf were considered not to represent any significant differences between an Anglo-Saxon and the Scandinavian culture. The Danish translation and cross-cultural adaptation was a direct translation and adaptation of the English version of ÖMPSQ-sf compared with the Brazilian-Portuguese and Hong Kong Chinese versions where the items of the short form were extracted from the translation of the ÖMPSQ-21 [20, 21]. This might explain the need to shorten some of the additional text instructions between the items of the ÖMPSQ-sf in the present study.
4.2Implications
The Danish ÖMPSQ-sf will add a short and easy to use tool to the body of assessment tools available to Danish health care professionals working and doing research within the field of subacute and chronic LBP in a hospital setting. In a clinical setting the ÖMPSQ-sf can assist the clinician in the psychosocial domains of a comprehensive bio-psycho-social patient evaluation. Nonetheless, further research is needed to investigate validity and responsiveness as well as the predictive ability for both work absenteeism and disability and the clinical utility for this patient population. Furthermore, the psychometric properties of the Danish ÖMPSQ-sf need to be established for acute and subacute LBP to determine the appropriateness for these populations.
5.Conclusion
In conclusion, the cross-cultural adaptation of a Danish version of the ÖMPSQ-sf showed acceptable test-retest reliability and absolute reliability in subacute and chronic LBP patients in a Danish hospital outpatient setting. This constitutes a promising first step towards its potential application in research and clinical practice.
Funding
The authors report no funding.
Author contributions
All authors have accepted responsibility for the entire content of this manuscript and approved the final version for publication.
Informed consent
Informed consent has been obtained from all individuals included in this study.
Ethical approval
According to the Danish National Committee on Health Research Ethics’ Guidelines about Notification etc. of a Biomedical Research Project to the Committee System on Biomedical Research Ethics, No. 9154, 5 May 2011, chapter 2.8, notification is not warranted for projects on health surveys or interviews.
Permission for data collection, handling, storage, and analysis was granted by the local regional data security council (BFH-2017-038).
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-230363.
Acknowledgments
We wish to thank the participants who contributed to the study. Furthermore, we also wish to thank the physiotherapists at the outpatient Back Pain Clinic at Bispebjerg and Frederiksberg Hospitals for including patients for the study.
Conflict of interest
The authors declare that they have no conflict of interest. Upon publication the Danish ÖMPSQ-sf is free to use.
References
[1] | Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine. (2020) ; 8: (6): 299. |
[2] | Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) ; 391: (10137): 2356-67. |
[3] | Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. (2018) ; 391: (10137): 2368-83. |
[4] | Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. European Spine Journal. (2018) ; 27: (1): 60-75. |
[5] | Westman A, Linton SJ, Ohrvik J, Wahlen P, Leppert J. Do psychosocial factors predict disability and health at a 3-year follow-up for patients with non-acute musculoskeletal pain? A validation of the Orebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain. (2008) ; 12: (5): 641-9. |
[6] | Alhowimel A, AlOtaibi M, Radford K, Coulson N. Psychosocial factors associated with change in pain and disability outcomes in chronic low back pain patients treated by physiotherapist: A systematic review. SAGE Open Medicine. (2018) ; 6: : 2050312118757387. |
[7] | Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CWC, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. European Spine Journal. (2018) ; 27: (11): 2791-803. |
[8] | Brunner E, Dankaerts W, Meichtry A, O’Sullivan K, Probst M. Physical therapists’ ability to identify psychological factors and their self-reported competence to manage chronic low back pain. Physical Therapy. (2018) ; 98: (6): 471-9. |
[9] | Beales D, Kendell M, Chang RP, Hamso M, Gregory L, Richardson K, et al. Association between the 10 item Orebro Musculoskeletal Pain Screening Questionnaire and physiotherapists’ perception of the contribution of biopsychosocial factors in patients with musculoskeletal pain. Man Ther. (2016) ; 23: : 48-55. |
[10] | Patel MS, Lee KC, Dhake RP, Longworth S, Sell P. Ability of spine specialists to identify psychosocial risk factors as obstacles to recovery in patients with low back pain-related disorders. Asian Spine Journal. (2021) ; 15: (2): 224-33. |
[11] | Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. (1993) ; 52: (2): 157-68. |
[12] | Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, et al. A primary care back pain screening tool: Identifying patient subgroups for initial treatment. Arthritis and Rheumatism. (2008) ; 59: (5): 632-41. |
[13] | Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Orebro Musculoskeletal Pain Questionnaire. Clin J Pain. (2003) ; 19: (2): 80-6. |
[14] | Hockings RL, McAuley JH, Maher CG. A systematic review of the predictive ability of the Orebro Musculoskeletal Pain Questionnaire. Spine (Phila Pa 1976). (2008) ; 33: (15): E494-500. |
[15] | Linton SJ, Hallden K, editors. Risk Factors and the Natural Course of Acute and Recirrent Musculoskeletal Pain: Developing a Screening Instrument. Proceedings of the 8th World Congress on Pain, Progressin Pain Research and Mannagement; 1997; Vancouver, B. C.: IASP Press; (1997) . |
[16] | Linton SJ, Hallden K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain. (1998) ; 14: (3): 209-15. |
[17] | Linton SJ, Nicholas M, MacDonald S. Development of a short form of the Orebro Musculoskeletal Pain Screening Questionnaire. Spine (Phila Pa 1976). (2011) ; 36: (22): 1891-5. |
[18] | Gabel CP, Burkett B, Melloh M. The shortened Orebro Musculoskeletal Screening Questionnaire: evaluation in a work-injured population. Man Ther. (2013) ; 18: (5): 378-85. |
[19] | Schmidt CO, Kohlmann T, Pfingsten M, Lindena G, Marnitz U, Pfeifer K, et al. Construct and predictive validity of the German Orebro questionnaire short form for psychosocial risk factor screening of patients with low back pain. Eur Spine J. (2016) ; 25: (1): 325-32. |
[20] | Tsang RCC, Lee EWC, Lau JSY, Kwong SSF, So EML, Wong TFY, et al. Development of a short form of the Hong Kong Chinese orebro musculoskeletal pain screening questionnaire. Hong Kong Physiother J. (2019) ; 39: (1): 57-66. |
[21] | Fagundes FR, Costa LO, Fuhro FF, Manzoni AC, de Oliveira NT, Cabral CM. Orebro Questionnaire: short and long forms of the Brazilian-Portuguese version. Qual Life Res. (2015) ; 24: (11): 2777-88. |
[22] | Simula AS, Ruokolainen O, Oura P, Lausmaa M, Holopainen R, Paukkunen M, et al. Association of STarT Back Tool and the short form of the Örebro Musculoskeletal Pain Screening Questionnaire with multidimensional risk factors. Scientific Reports. (2020) ; 10: (1): 290. |
[23] | Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). (2000) ; 25: (24): 3186-91. |
[24] | Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. (2010) ; 19: (4): 539-49. |
[25] | Furr RM, Bacharach VR. Psychometrics: An introduction. London: SAGE Publications; (2008) . |
[26] | Vet HCWd. Measurement in medicine: A practical guide. Cambridge; New York: Cambridge University Press; (2011) ; x, 338 s. p. |
[27] | Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. (2016) ; 15: (2): 155-63. |
[28] | Carter R, Lubinsky J, Domholdt E. Rehabilitation research: principles and applications. 4. ed. Philadelphia, Pa.; London: Saunders; (2011) . vii, 503 s. p. |
[29] | Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. (2006) ; 60: (1): 34-42. |
[30] | Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. (2014) ; 105: (3): 399-412. |
[31] | Tavakol M, Dennick R. Making sense of Cronbach’s alpha. International Journal of Medical Education. (2011) ; 2: : 53-5. |
[32] | Mokkink LB, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, de Vet HCW, et al. COSMIN Study Design checklist for Patient-reported outcome measurement instruments 2019. [Available from: https://wwwcosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf]. |



