Translating the new International IFOMPT Cervical Framework into a framework flowchart for clinical practice and education
Abstract
BACKGROUND:
In 2020, a revised version of the International IFOMPT Cervical Framework was published. This framework provides both physical therapists and educators the necessary information to guide the assessment of the cervical spine region for potential vascular pathologies of the neck in advance of planned Orthopaedic Manual Therapy (OMT) interventions.
OBJECTIVE:
The objective was to develop a framework flowchart which is useful in clinical practice and education to assist physical therapists to improve the safety of OMT, and apply this in a case report.
METHODS:
The framework was developed in co-creation with manual therapy experts, researchers, educators in manual therapy, patients, medical specialists and the Manual Therapy Association in The Netherlands and Belgium. Manual therapists and patients tested the framework for intelligibility and usefulness.
RESULTS:
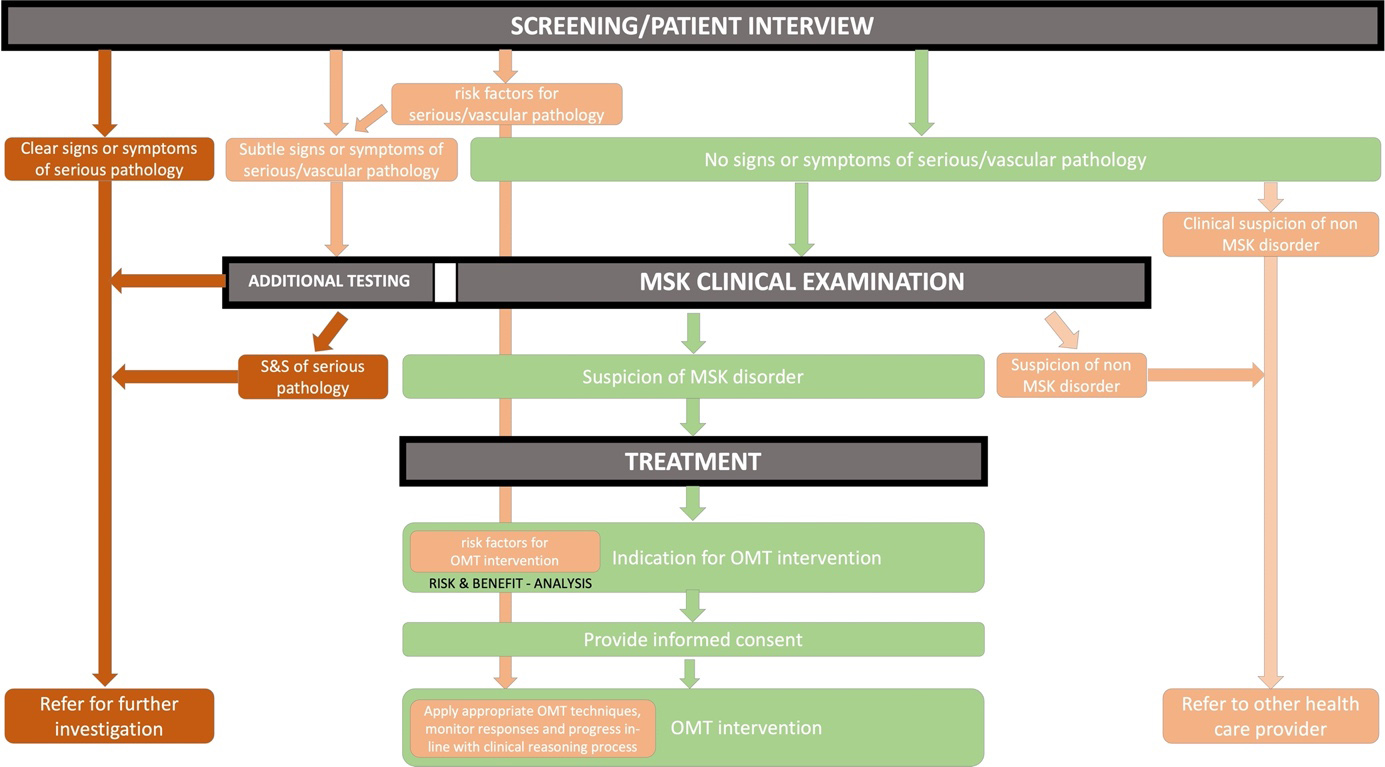
A framework flowchart is developed and presented, that is easy to use in both clinical practice and education. It is a visual representation of the sequence of steps and decisions needed during the process. A case description of a patient with neck pain and headache is added to illustrate the clinical usefulness of the framework flowchart.
CONCLUSION:
The framework flowchart helps physical therapists in their clinical reasoning to provide safe OMT interventions.
1.Introduction
In 2013, the Dutch Health and Youth Care Inspectorate identified an increased number of complications following upper cervical spine manipulations and asked the Dutch Association for Manual Therapy to provide a professional standard. This standard should lead to (further) improved safety of manual therapy in the upper cervical spine and was published in 2014 [1]. A safety committee was launched by the Dutch Association for Manual Therapy which needed to monitor and update this professional standard based on new available research, information from clinical practice and reported complications.
In 2020, a revised version of the International IFOMPT Cervical Framework was published to guide the assessment of the cervical spine region for potential vascular pathologies of the neck in advance of planned Orthopaedic Manual Therapy (OMT) interventions as used by OMT certified physical therapists [2]. The aim of the framework is to provide both physical therapists and educators the necessary information to teach and practice the examination of the cervical spine. In combination with sound clinical reasoning, clinicians may avoid the risk of misdiagnosis of an existing vascular pathology and diminish the risk of serious adverse events following OMT. This framework consists of the best evidence derived from systematic reviews, clinical guidelines, and expert opinion.
Although it is important that this framework is carefully read by every clinician who treats patients with neck complaints, translation of this framework into an easy applicable flowchart and adapted to the Dutch Standard is recommended. Therefore, a framework flowchart was developed, based on the IFOMPT framework, and adapted to the Dutch and Flemish context.
2.Development process
To translate, promote and support implementation of the IFOMPT framework, the framework flowchart was developed in a subgroup committee (
3.The framework flowchart
The framework flowchart is intended to be simple and flexible and is based on a thorough patient interview, focused clinical examination, and appropriate treatment/referral with sound clinical reasoning. It is a visual representation of the sequence of steps and decisions needed during the process (Fig. 1). The colors (red, orange, green) refer to the safety of the pathways to OMT intervention. The red color is used to signify the ‘danger’ of a vascular hypothesis that needs (urgent) referral to further investigation; The orange color is used to show that precaution is needed during the clinical examination and treatment; the green color indicates a safe pathway to OMT intervention.
Figure 1.
IFOMPT framework flowchart.
3.1Patient interview
As with any patient’s health problem, a good interview is essential to assess the nature and severity of the presenting symptoms, and to determine whether the problem has the potential to respond to OMT or needs further referral. The physical therapist’s aim is to use the patient interview to make the best judgment on the probability of either the presence of serious pathology or contraindications to treatment, and to generate hypotheses.
Signs and symptoms of serious pathology (i.e., vascular pathology) should be recognized in the patient interview. During clinical reasoning, this can be ‘divided’ into (1) clear, (2) subtle or (3) no signs and symptoms of the suspected pathologies.
• Identification of clear signs and symptoms warrants a medical referral for further investigation. It is recommended that physical therapists refer for immediate medical investigation when their clinical suspicion is supported by the structured patient interview.
• Subtle signs and symptoms may require additional testing to support or refute the vascular hypothesis. Existing data support the use of conventional vascular examination [3] whereby the following tests are recommended [2]: blood pressure, cranial nerve examination and gait pattern. Having a high index of suspicion of vascular pathology may justify referral for further investigation. However, if a vasculogenic contribution is highly unexpected, the physical therapist may continue assessment and treatment according to the green pathway.
• In case of no relevant signs or symptoms of serious/vascular pathology, other information from the patient interview and the clinical examination, should confirm or reject the clinical suspicion of a musculoskeletal (MSK) disorder. If a non-MSK disorder is suspected, referral to other healthcare providers is warranted. For example, lightheadedness as one of the symptoms of hyperventilation, is not considered a red flag for physical therapy intervention but cannot be labelled as an MSK disorder. Therefore, referral to health care providers that are trained to treat this condition is indicated.
In addition, it is important to identify risk factorsindicating the potential for serious/vascular pathology. These risk factors should be ‘taken into account’ throughout the whole clinical reasoning process. This is indicated in the framework flowchart by the orange arrow starting from the patient interview to OMT intervention. Identification of risk factors may lead to additional testing or referral for further investigation. However, in case of a clear suspicion of a MSK disorder with no clear suspicion of a vascular hypothesis, these risk factors should be included in the risk & benefit analysis and used to determine the most suitable and safe OMT technique(s).
3.2Clinical examination
Careful planning of the clinical examination is required to refine, re-rank or reject the hypotheses generated from the patient interview and to facilitate optimal clinical reasoning in OMT [4]. Clinical examination may consist of additional questions, or MSK examination and any additional testing to support or reject the vascular hypothesis. The physical therapist should define the type and order of testing with consideration of any risks and precautions associated with performing the tests.
3.3Treatment
The decision to refer for further vascular diagnostic evaluation or proceed with physical therapy management needs to be made following the evaluation of the patient interview and clinical examination. If OMT intervention is indicated, and suspicion of underlying vascular pathology is refuted, the physical therapist weighs the anticipated risks all treatment modalities within the OMT intervention. This will be based on the clinical characteristics of the patient to the expected beneficial effects (risk and benefit analysis) to minimize the risk of complications. If the benefits outweigh the risks, appropriate OMT techniques should be applied.
Before proceeding to OMT intervention, individual practitioners will need to deliberate the treatment plan, adopt an approach to consent which includes sharing (verbal and written) information to the patient, explaining the expected treatment benefits, arguing alternative treatments and considering inherent risks associated with the patient’s presentation and the interventions that the practitioner is advocating. Additionally, the patient has to provide (verbal or written) informed consent. All this information needs to be reported in the (electronic) patient record. The therapist monitors response to treatment and any harmful incidents throughout treatment and progress in line with the clinical reasoning process.
4.A case study
To illustrate the clinical usefulness of the framework flowchart, a case study is presented.
4.1Description of the case
4.1.1History of presenting complaint (HPC)
A 64 years-old woman working as a nurse-practitioner at a local hospital, visited a physical therapist for her neck pain and headache after an abrupt left rotation of her neck during a visit to the cinema two weeks ago. Immediately following this movement, she felt a sharp and high intensity pain at the left side of her neck, radiating to the left occipital, parietal, and frontal sites of the head. At that moment, she could barely move her neck. In addition, she experienced an unremitting headache, nausea and lightheadedness during the first two days after the onset of the pain. Pain killers (paracetamol) did not relieve these symptoms.
At her first visit to the manual therapist, the following signs and symptoms were noted.
• The neck pain was located at both sides, predominantly at the left side, with an average pain intensity of 7 out of 10 (0–10 scale, numeric pain rating scale (NPRS))
• The headache was constantly present as a dull pain (NPRS 0–10: 4) at the left side of her head. Rotation to both sides and extension of the cervical spine increased the headache.
• No signs of neurological deficit; no nausea or dizziness.
For two weeks, she experienced a major loss of activities such as biking and driving her car because of the restricted cervical range of motion. Lying down and sitting on a chair, not moving her neck, reduced the neck pain and headache.
4.1.2General health
She is used to perform exercises (yoga) and hiking regularly to keep her physically fit. She used to smoke for 35 years, but stopped 6 months ago, and is in good physical and mental health.
4.1.3Past Medical history
Hypertension (ranges at 140/85) and diabetes type 2.
4.1.4Medication
Metoprolol and metformin.
4.1.5Attitudes/expectations
Her coping behaviour appears to be adequate.
4.2Clinical reasoning
The first step is to recognize signs and symptoms of severe (vascular) pathology during the patient interview. In this case description, the sudden onset, high initial pain intensity (headache and neck pain), the restricted cervical rotation movement, nausea, ipsilateral headache, smoking history, hypertension, comorbid diabetes mellitus are signs and symptoms of the patient’s history that can be linked to potential vascular pathologies of the neck [2, 5].
However, at her first visit to the therapist who assessed the patient according to the IFOMPT Framework, no clear signs or symptoms of serious vascular pathology appeared to be present that needed referral to further investigation.
The next step is to assess the patient for both other subtle signs and symptoms, and risk factors for vascular pathology. As the patient complained of neck pain, ipsilateral headache, nausea, and lightheadedness, additional tests (neurological examination, coordination and gait, and blood pressure and auscultation) were indicated. Moreover, the patient interview highlighted the presence of hypertension, which is recognized as a risk factor for dissecting and non-dissecting stroke [2].
The additional testing as mentioned above did not reveal any abnormal findings, but the presence of subtle signs and symptoms and hypertension indicated that precaution is needed during the clinical examination, especially in older people [6, 7].
The next step is to define whether the signs and symptoms are related to a musculoskeletal disorder. If a non-MSK disorder is considered, the patient must be referred to other health care providers and should be excluded for further examination. If an MSK-disorder is suspected, a clinical diagnosis/hypothesis must be constructed based on the information from the interview.
Cervicogenic headache appears to be the most plausible hypothesis based on the symptoms experienced by the subject, i.e., neck pain, one-sided headache and restricted movement of the neck after a sudden onset (rotation of the neck) [8, 9]. As cervicogenic headache is defined as referred pain from the cervical spine to the head, the nociceptive drivers (articular joints, myofascial structures) of the pain should be identified during the MSK clinical examination [10, 11].
Table 1
Findings of the clinical examination
| Clinical examination | Findings |
|---|---|
| Inspection | Forward head position |
| Movement examination |
|
| Articular examination |
|
| Myofascial examination |
|
| Motor control examination |
|
The clinical examination included inspection, movement examination, and articular and myofascial examination (including provocation and function tests) [12]. Motor control examination, including neuromuscular control (e.g. craniocervical flexion test [13], and evaluation of endurance/force (e.g. [14]) was not relevant at this time point due to the irritability of the current headache and neck pain. The order of testing was chosen carefully, the examination was carried out safely, and the therapist monitored the patient’s signs and symptoms during the examination. The clinical examination findings are shown in Table 1.
The results of the clinical examination guided further clinical reasoning and seemed to confirm the hypothesis of cervicogenic headache with an underlying cervical articular joint dysfunction and myofascial involvement. The signs and symptoms revealed during the patient interview (headache started after neck distorsion, a one sided and side-locked headache), the major loss of movement in rotation and extension, together with the painful C1-2 and C2-3 articular joints that provoked the familiar headache, the headache was finally classified as a cervicogenic headache.
As cervicogenic headache with an underlying articular joint dysfunction is considered as an indication for OMT intervention, the therapist must then weigh all included factors within a risk- benefit analysis and propose the most adequate and suitable treatment for this patient. In this scenario, the initial proposed treatment was education regarding pain and posture combined with passive high and low-velocity mobilizations of the cervical and thoracic spine, home-exercises and myofascial release techniques [15, 16, 17, 18]. According to the shared decision-making process, the therapist explained and discussed the indication, expected benefits, treatment options and potential risks with the patient. By giving the informed consent, the patient agreed to a multimodal treatment that included education, cervical and cervical-thoracic spine mobilization, and myofascial release techniques to reduce pain. Active midrange mobilization techniques were taught as home exercises.
5.Conclusion
In this case description, the framework flowchart was applied to guide clinical reasoning in a patient with neck pain and headache. Although the patient’s history appeared to be suspicious for serious vascular pathology, continuing of the patient interview and testing did not reveal additional relevant signs/symptoms, risk factors for vascular pathology, or positive additional tests. When outweighing the risks to the benefits, an appropriate OMT treatment was applied. The framework flowchart intends to guide and help physical therapists in their clinical reasoning to provide safe OMT interventions.
Ethical approval
Not applicable.
Funding
The authors report no funding.
Informed consent
Informed consent was obtained.
Author contributions
Conceptualization and design: B.C., R.C., G.G.M.S.; Data collection: R.C.; Interpretation: B.C., R.C., G.G.M.S.; Writing – original draft: B.C., R.C., G.G.M.S.; All authors read and approved the final manuscript.
Acknowledgments
The authors would like to thank the safety committee of the Dutch Association for Manual Therapy (Nederlandse Vereniging voor Manuele Therapie, NVMT), the NVMT, the Manual Therapy Association Belgium (MATHERA), all patients, manual therapists, medical specialists and the educators of the Gent University and SOMT University of Physiotherapy, Amersfoort who participated in the development of this framework flowchart.
Conflict of interest
The authors declare that they have no conflict of interest.
References
[1] | Professional standard of the Dutch Association for Manual therapy. Available from: https://nvmt.kngf.nl/article/richtlijnen-en-factsheets/richtlijnen/beroepsnorm-hoog cervicale-man-ipulaties. |
[2] | Rushton A, Carlesso L, Flynn T, Wing W, Kerry R, Rubinstein S, Vogel S. International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical Framework, IFOMPT October (2020) . |
[3] | Elder A, Japp A, Verghese A. How valuable is physical examination of the cardiovascular system? British Medical Journal. (2016) ; 354: : i3309. doi: 10.1136/bmj.i3309. |
[4] | Jones MA, Rivett DA. Introduction to clinical reasoning. In: M.A. Jones and D.A. Rivett, eds. Clinical Reasoning for Manual Therapists. Butterworth-Heinemann: Edinburgh; (2004) . pp. 3-24. |
[5] | Debette S. Pathophysiology and risk factors of cervical artery dissection: What have we learnt from large hospital-based cohorts? Curr Opin Neurol. (2014) ; 27: (1): 20-8. |
[6] | Taylor A, Kerry R. Vascular profiling: Should manual therapists take blood pressure? Manual Therapy. (2013) ; 18: (4): 351-3. |
[7] | Hutting N, Wilbrink W, Taylor A, Kerry R. Identifying vascular pathologies or flow limitations: Important aspects in the clinical reasoning process. Musculoskelet Sci Pract. (2021) ; 53: : 102343. |
[8] | Antonaci F, Ghirmai S, Bono G, Sandrini G, Nappi G. Cervicogenic headache: Evaluation of the original diagnostic criteria. Cephalalgia. (2001) ; 21: (5): 573-583. |
[9] | Antonaci F, Sjaastad O. Cervicogenic headache: A real 291 headache. Current Neurology and Neuroscience Reports. (2011) ; 11: (2): 149-155. |
[10] | Bogduk N, Govind J. Cervicogenic headache: An assessment of the evidence on clinical diagnosis, invasive tests, and treatment. The Lancet Neurology. (2009) ; 8: (10): 959-968. |
[11] | Hall T, Briffa K, Hopper D, Robinson K. Reliability of manual examination and frequency of symptomatic cervical motion segment dysfunction in cervicogenic headache. Manual Therapy. (2010) ; 15: (6): 542-546. |
[12] | Luedtke K, Boissonnault W, Caspersen N, Castien R, Chaibi A, Falla D, Fernández-de-Las-Peñas C, Hall T, Hirsvang JR, Horre T, Hurley D, Jull G, Krøll LS, Madsen BK, Mallwitz J, Miller C, Schäfer B, Schöttker-Königer T, Starke W, von Piekartz H, Watson D, Westerhuis P, May A. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: A Delphi study. Man Ther. (2016) ; 23: : 17-24. doi: 10.1016/j.math.2016.02.010. |
[13] | Hall TM, Briffa K, Hopper D, Robinson K. Comparative analysis and diagnostic accuracy of the cervical flexion-rotation test. Journal of Headache and Pain. (2010) ; 11: (5): 391-397. |
[14] | Harris KD, Heer DM, Roy TC, Santos DM, Whitman JM, Wainner RS. Reliability of a measurement of neck flexor muscle endurance. Phys Ther. (2005) ; 85: (12): 1349-55. |
[15] | Côté P, Yu H, Shearer HM, Randhawa K, Wong JJ, Mior S, Ameis A, Carroll LJ, Nordin M, Varatharajan S, Sutton D, Southerst D, Jacobs C, Stupar M, Taylor-Vaisey A, Gross DP, Brison RJ, Paulden M, Ammendolia C, Cassidy JD, Loisel P, Marshall S, Bohay RN, Stapleton J, Lacerte M. Non-pharmacological management of persistent headaches associated with neck pain: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. Eur 314 J Pain. (2019) ; 23: (6): 1051-1070. doi: 10.1002/ejp.1374. |
[16] | De Pauw R, Dewitte V, de Hertogh W, Cnockaert E, Chys M, Cagnie B. Consensus among musculoskeletal experts for the management of patients with headache by physiotherapists? A delphi study. Musculoskelet Sci Pract. (2021) ; 52: : 102325. doi: 10.1016/j.msksp.2021.102325. |
[17] | Dunning JR, Butts R, Mourad F, Young I, Fernandez-de-Las Peñas C, Hagins M, Stanislawski T, Donley J, Buck D, Hooks TR, Cleland JA. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: A multi-center randomized clinical trial. BMC Musculoskelet Disord. (2016) ; 6: (17): 64. doi: 10.1186/s12891-016-0912-3. |
[18] | Varatharajan S, Ferguson B, Chrobak K, Shergill Y, Côté P, Wong JJ, Yu H, Shearer HM, Southerst D, Sutton D, Randhawa K, Jacobs C, Abdulla S, Woitzik E, Marchand AA, van der Velde G, Carroll LJ, Nordin M, Ammendolia C, Mior S, Ameis A, Stupar M, Taylor-Vaisey A. Are non-invasive interventions effective for the management of headaches associated with neck pain? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J. (2016) ; 25: (7): 1971-99. doi: 10.1007/s00586-016-4376-9. |




