Effectiveness of motor control exercises versus other musculoskeletal therapies in patients with pelvic girdle pain of sacroiliac joint origin: A systematic review with meta-analysis of randomized controlled trials
Abstract
BACKGROUND:
Pelvic girdle pain represents a group of musculoskeletal pain disorders associated with the sacroiliac joint and/or the surrounding musculoskeletal and ligamentous structures. Its physical management is still a serious challenge as it has been considered the primary cause of low back pain.
OBJECTIVE:
This review sought to determine the effectiveness of motor control exercises for two clinically relevant measures; i.e., pain and disability, on patients with pelvic girdle pain of sacroiliac joint origin.
METHODS:
This review covered only randomized controlled studies. Online databases, such as PubMed, Embase, Scopus, and Cochrane Library, were searched from January 1, 1990, to December 31, 2019. PEDro scale was used to assess the methodological quality of included studies, while Review Manager was employed to synthesize data in view of meta-analysis. The PRISMA guidelines were applied for this review.
RESULTS:
Twelve randomized controlled trials of moderate-to-high quality were included in this review. The studies involved 1407 patients with a mean age ranging from 25.5 to 42.1 years as well as intervention and follow-up durations from 1 week to 2 years. Motor control exercises alone for pelvic girdle pain of sacroiliac joint origin were not effective in terms of pain reduction (SMD
CONCLUSION:
Motor control exercises alone were not found to be effective in reducing pain at short-term. However, their combination with other musculoskeletal therapies revealed a significant and clinically-relevant decrease in pain and disability at short-term, especially in peripartum period.
1.Introduction
Pelvic girdle pain (PGP) represents a small but significant group of musculoskeletal pain disorders associated with the sacroiliac joint (SIJ) and/or the surrounding musculoskeletal and ligamentous structures [1]. Specific inflammatory pain disorders of the SIJs, such as sacroiliitis, are the most readily identified PGP disorders [2]. However, PGP more commonly presents as ‘non-specific’, often arising during or shortly after pregnancy [3, 4, 5] or following traumatic injury to the pelvis (pelvic bone fractures, ligamentous injuries) [6, 7].
SIJ pain has been acknowledged to be localized or pseudoradicular [8]. In 1905, it was for the first time reported to a potential source of low back pain (LBP) [9], whereas later, it was considered its primary cause in 15 to 72% of cases [10, 11], its prevalence ranging from 10 to 75% [12, 13]. The SIJ pain can cause groin, buttock, and thigh pain; via this mechanism it is likely to affect pelvic girdle biomechanical efficiency, daily life activities and functional movements [10].
Some risk factors such as abnormal gait pattern, leg length discrepancy, scoliosis, direct trauma, natural lumbar fusion with the sacrum, post-surgery, idiopathic onset, and pregnancy state have been reported to date [14, 15, 16]. In pregnant women, the increased laxity of soft-tissues surrounding the SIJ and greater synovial fluid volume can lead to increased SIJ motion, which diminishes the efficiency of load transmission and increases the sheer forces across the joint [17]. SIJ assessment is specific and is based on combining several pain provocation tests [18], whereas LBP assessment is based on a problematic and specific movement direction in addition to contributing factors [19]. However, PGP probably stems from multifactorial sources as does non-specific LBP within the biopsychosocial model [20]. Therefore, this review focused on PGP of SIJ origin.
Table 1
Search terms used for database searches
| 1 | (“sacroiliac joint/pathology”[MeSH]) OR sacroiliac joint pain*[Title/Abstract] OR sacroiliac joint dysfunction*[Title/Abstract] OR sacroiliac joint syndrom*[Title/Abstract] OR “pelvic girdle pain”[Mesh] OR lumbopelvic pain*[Title/Abstract] OR lumbopelvic disorder*[Title/Abstract] OR “pelvic pain”[Mesh] OR lumbopelvic dysfunction*[Title/Abstract] OR sacroiliac joint disorder*[Title/Abstract] OR pelvic disorder*[Title/Abstract] OR pelvic dysfunction*[Title/Abstract] OR sacroiliac joint instability[Title/Abstract] OR posterior pelvic pain[Title/Abstract]) |
|---|---|
| AND | |
| 2 | (motor control exercis*[Title/Abstract] OR stabiliz* exercis*[Title/Abstract] OR isometric exercis*[Title/Abstract] OR stability exercis*[Title/Abstract] OR physical therapy modalities [MeSH Terms] OR physical therapy exercis*[Title/Abstract] OR physiotherapy exercis*[Title/Abstract] OR physical therap*[Title/Abstract] OR physiotherap*[Title/Abstract] OR physical activit*[Title/Abstract] OR “physical training” [Title/Abstract] OR “exercise therapy”[MeSH]))]) Filters: Clinical Trial, Humans, from 1990/1/1 – 2019/12/31 |
Standard physical therapies are being used to cure the underlying pathology, in addition to reducing or alleviating the SIJ symptoms. Such interventions include manual joint mobilization and manipulation, sacroiliac belts, massage, patient education, aerobic conditioning, electrotherapy, and repetitive exercises, including motor control exercises (MCE) [21, 22].
Concerning physical therapy, there is an urgent need for an effective intervention strategy for managing PGP of SIJ origin. Such a treatment strategy has already been reported in the literature. However, no systematic review with meta-analysis, which aimed to investigate the effectiveness of MCE alone or MCE combined with other musculoskeletal therapies (MSKTS), has been conducted while being focused on PGP of SIJ [10, 23]. Nevertheless, definite conclusions concerning the use of MCE in patients with PGP of SIJ are still pending. Therefore, this research primarily sought to determine the effectiveness of MCE, as the standard exercise, on two clinically relevant parameters, i.e. pain and disability on patients with PGP of SIJ origin.
2.Methods
The review protocol was registered into PROSPERO under registration number CRD42020193186. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were employed for conducting this review [24].
2.1Search strategy
The PubMed, Embase, Scopus and Cochrane Library databases were searched for relevant clinical trials. The following criteria were definied to guide our search strategy:
Participants/population: Patients (men and women) suffering from PGP of SIJ origin.
Interventions: These were MCE, such as pelvic girdle muscle strengthening exercises, pelvic-tilt exercises with pelvic floor muscle (PFM) voluntary contraction, as well as exercises involving hip extension, abduction, and abdominal crunches.
Comparators: These were other MSKTs that were used as controls, such as physical therapy modalities (massage, relaxation, joint mobilization, electrotherapy, hot packs, mobilizing and strengthening exercises, manipulation), pelvic realignmet device, as well as no rigid lumbopelvic belt.
Outcome measures: Pain [Visual Analogue Scale (VAS)] and disability [Pelvic Girdle Questionnaire (PGQ), Disability Rating Index (DRI), and Oswestry Disability Index (ODI)] were the main outcomes.
Selection criteria: (1) Randomized controlled trials (RCTs); (2) concerning patients with PGP of SIJ, diagnosed by means of SIJ tests or SIJ intra-articular steroid injections; (3) using specific MCE or exercises aimed at activating, training, or restoring PFM’s stabilization function; (4) reported lower back, lumbopelvic, or PGP referred from SIJ; (5) reports published between January 1,1990, and December 31, 2019; (6) papers written in English or French. The exclusion criteria for studies were as follows: (1) score
2.2Methodological assessment of RCTs
The PEDro scale, which is deemed a valid and reliable tool for assessing RCTs [25, 26], was used for sample assessment. RCTs’ quality was blindly judged by two different reviewers (MJ and NG) in order to minimize potential bias [27]. Accordingly, RCTs were divided into three categories, as follows: low quality (0–3/10), moderate quality (4–6/10), and high quality (7–10/10). An overall assessment of the studies included was additionally performed based on whether each individual criterion was fulfilled.
2.3Quality of evidence assessment
The reviewers (MJ and NG) employed the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework to assess the evidence level for each study included in the meta-analysis [28]. Evidence from RCTs considered of ‘high’ quality was graded down in the presence of concerns with risk of bias, indirectness, inconsistency, imprecision, or publication bias [29, 30, 31, 32, 33]. The risk of bias among the studies was considered ‘serious’ when the studies that contributed the most to the pooled result exhibited a ‘high’ risk of bias. For qualitative analysis, strength of evidence was determined by grouping similar Patients Interventions Comparisons Outcomes Study design (PICOs) to provide an overall level of evidence [34, 35].
2.4Study selection and data extraction
The studies, along with their titles, abstracts and data were identified and screened by two independent reviewers (MJ and NG). Only eligible full text studies were retrieved and then screened again by the same reviewers. In addition, the reference lists of the identified studies were manually checked for further inclusions. The same reviewers collected the included studies, classified them and displayed their main characteristics (Table 1).
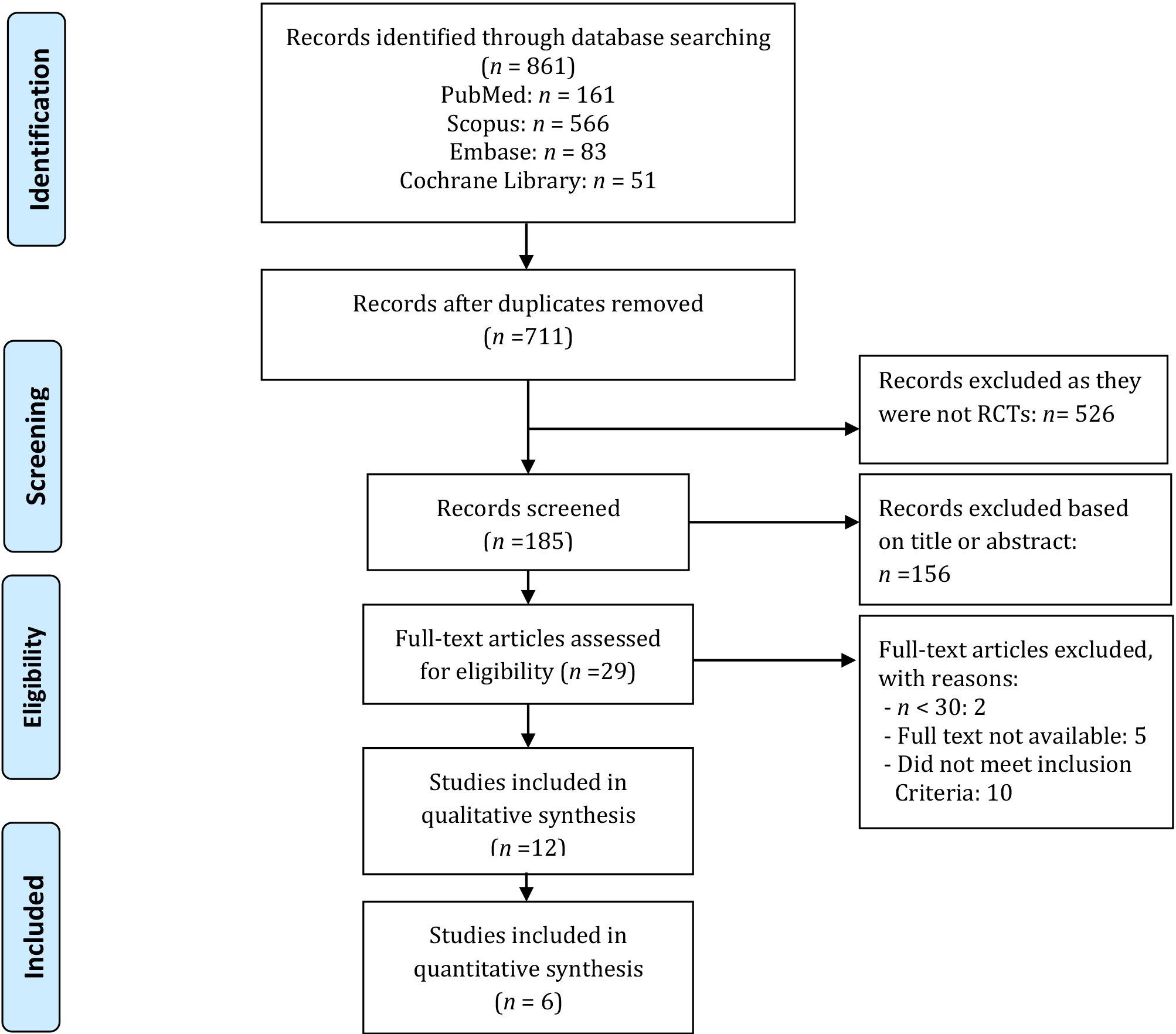
Figure 1.
Flowchart of the study design.
2.5Data synthesis
Results from studies exhibiting similar PICOs were considered for being pooled into separate meta-analyses. Pooled standard mean differences (SMDs) were calculated using Review Manager (RevMan V.5.3). Pooled estimates were calculated with their 95% confidence intervals (CIs) and an alpha level set at 0.05 [36]. Analyses were performed with random effects. The forest plots visual inspection was performed. The effect sizes (ES) calculated with SMD were interpreted using Cohen’s method; the effect was defined as small (0–0.20), medium (0.20–0.50), or large (0.50–0.80) [37].
MCE efficacy was judged based on the SMD interpretation [38]. Thus a SMD of zero means that the treatment in the intervention group (IG) and that in the control group (CG) display equivalent effects. If the improvement is associated with higher scores on the outcome measure, SMDs greater than zero indicate the degree to which the IG treatment is more effective than that administered to the CG, while SMDs less than zero indicate the opposite. If the improvement is associated with lower scores on the outcome measure, SMDs less than zero indicate the degree to which the IG treatment is more effective than that administered to the CG, while SMDs greater than zero indicate the opposite. In this review, considering the outcome measures (VAS and ODI), when SMD is less than zero the improvement is in favor of the IG, while SMD greater than zero indicates the opposite.
A quantitative analysis was performed for meta-analysis. I
• 0% to 40%: not relevant;
• 30% to 60%: may represent moderate heterogeneity;
• 50% to 90%: may represent substantial heterogeneity;
• 75% to 100%: considerable heterogeneity.
If a quantitative pooling was not performed, results were then qualitatively synthesized.
3.Results
3.1Study selection
We identified 861 potentially relevant studies, and after removing duplicates, 711 remained. Following title and abstract screening, we assessed 29 fulltext studies. Of these, 17 studies were excluded for different reasons after fulltext evaluation (Fig. 1). This systematic review took into account the remaining 12 RCTs, six of which were suitable for meta-analysis.
Table 2
Characteristics of studies included in the review
| Study | PEDro score | Purpose | Participants | Interventions | Number of participants | Duration and FU period | Outcome measure | Main results |
|---|---|---|---|---|---|---|---|---|
| Elden et al. [43] | 8/10 | To compare the efficacy of standard treatment, standard treatment plus acupuncture, and standard treatment plus stabilizing exercises for PGP during pregnancy | G | 1 week | VAS | Betweengroup comparison [Median difference (95% CI)] at 1 week after treatment: G | ||
| Saleh et al. [45] | 7/10 | To investigate the effect of core stability exercises on postpartum LPP | G | 6 weeks | VAS ODI | Pre/posttreatment (Mean | ||
| EIDeeb et al. [46] | 7/10 | To investigate the effect of stabilizing exercises with or without PFM training on pain functional disability, trunk ROM and PFM strength in PGP women | G | 12 weeks | VAS ODI | Pre/posttreatment (Mean | ||
| Stuge et al. [22] | 7/10 | To evaluate a treatment programme focusing on whether specific SE for patients with PGP after pregnancy reduce pain, and improve functional status and QOL | G | 20 weeks, 1 year | VAS ODI | Group difference in median values for evening pain after treatment was 30 mm on VAS. |
Abbreviations: LPP
|
Table 2, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | PEDro score | Purpose | Participants | Interventions | Number of participants | Duration and FU period | Outcome measure | Main results |
| Teymuri et al. [47] | 6/10 | To investigate the effect of stabilization exercises on pain, disability; and PFM function in postpartum LPP | G | 6 weeks | VAS ODI | Pre/posttreatment (Mean | ||
| Nilsson-Wikmar et al. [44] | 6/10 | To compare three different physical therapy treatments in PGP women during pregnancy and at 3,6- and 12-month post-partum | G | 3 weeks during pregnancy and 3, 6, 12 months PP | VAS DRI | Change score [median (range)] at inclusion-gestation Week 38/Gestation week 38-12 months PP G | ||
| Kamali et al. [23] | 5/10 | To compare the effects of manipulation and stabilization exercises in SIJD patients | G | 2 to 4 weeks | VAS ODI | Pre/posttreatment (Mean | ||
Abbreviations: PFM
|
Table 2, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | PEDro score | Purpose | Participants | Interventions | Number of participants | Duration and FU period | Outcome measure | Main results |
| Sakamoto et al. [40] | 5/10 | To determine the effects of a pelvic realignment device-aided exercise programme after childbirth | G | 4–9 weeks | VAS PGQ | Changes [mean (95% CI)] at baseline/4 | ||
| Kordi et al [39] | 5/10 | To compare the effect of lumbopelvic belt plus information, home based pelvic girdle SE plus information and information alone on pain, functional status and QOL of pregnant PGP women | G | 3, 6 weeks | VAS ODI | Between groups comparison [Mean difference (95% CI)] at 3 | ||
| Elden et al. [42] | 5/10 | To describe the regression of pelvic girdle pain after delivery in PGP women | G | 1–12 weeks | VAS | Changes score [median (25–75 | ||
Abbreviations: QOL
|
Table 2, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | PEDro score | Purpose | Participants | Interventions | Number of participants | Duration and FU period | Outcome measure | Main results |
| Stuge et al. [41] | 5/10 | To examine the effect of a treatment programme focusing on specific stabilizing exercises after a 2-year FU period | G | 20 weeks, 2 years | VAS ODI | Minimal evening pain was reported by 68% of the G | ||
| Nejati et al. [10] | 4/10 | To compare exercises therapy, manipulation, and a combination of the two in terms of their effectiveness in treating SIJD | G | 6, 12, 24 weeks | VAS ODI | Time effect of treatments at baseline/6 | ||
Abbreviations: FU
Table 3
PEDro scores
| Studies | A | B | C | D | E | F | G | H | I | J | Total score | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Elden et al. [43] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 | High |
| Saleh et al. [45] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 | High |
| ElDeeb et al. [46] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 | High |
| Stuge et al. [22] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 | High |
| Teymuri et al. [47] | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 6/10 | Moderate |
| Nilsson-Wikmar et al. [44] | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6/10 | Moderate | ||
| Kamali et al. [23] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5/10 | Moderate |
| Sakamoto et al. [40] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5/10 | Moderate |
| Kordi et al. [39] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 | Moderate |
| Elden et al. [42] | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5/10 | Moderate |
| Stuge et al. [41] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5/10 | Moderate |
| Nejati et al. [10] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 4/10 | Moderate |
A
3.2Participant characteristics of the selected studies
The twelve RCTs included 1407 participants with a mean age ranging from 25.5 to 42.1 years. Ten RCTs involved only women in peripartum period. Only one paper included both genders, while the remaining other did not report the participant characteristics. For more details, see Table 2.
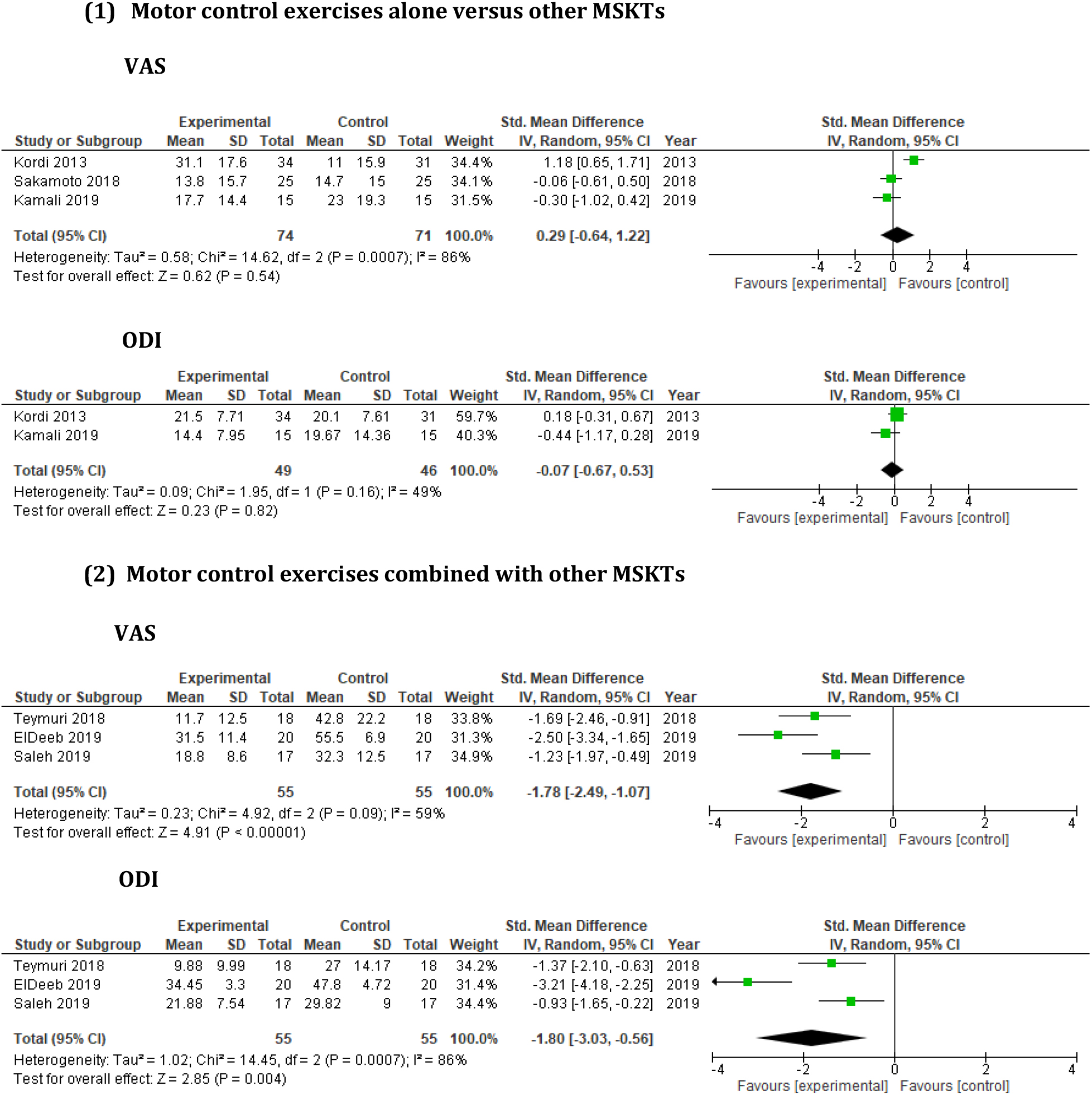
Figure 2.
Short-term effect of MCE versus other MSKTs on pain and disability.
3.3Methodological assessment
The PEDro score of the included studies ranged from 4 to 8/10. Four RCTs were considered as being of high quality (PEDro score: 7–8/10), with the remaining ones being of moderate quality (PEDro score: 4–6/10) (Table 3).
3.4Interventions and comparators
Four RCTs compared MCE alone to other MSKTs [23, 39, 40, 41], while eight RCTs compared MCE (as detailed above) in combination with other MSKTs (as detailed above) to these MSKTs [10, 22, 42, 43, 44, 45, 46, 47].
3.5Outcome measures
For pain assessment, the Visual Analogue Scale was used in all RCTs, but the assessment method was not further described in any study (Table 2). For self-reported function, Sakamoto et al. [40] and Nilsson-Wikmar et al. [44] used the Pelvic Girdle Questionnaire (PGQ) and Disability Rating Index (DRI) in their studies, respectively; the remaining studies used the Oswestry Disability Index (ODI) instead (Table 2).
3.6Subgroup analysis
3.6.1Short-term (⩽
Short-term effect of MCE alone on pain and disability
Three RCTs [23, 39, 40] involving 145 participants were considered in order to evaluate the short-term effect of MCE alone on pain and disability, and were suitable for meta-analysis (Fig. 2).
Kordi et al. [39] compared the effects of lumbopelvic belt plus information about anatomy, body posture, and ergonomic advice, home based pelvic girdle MCE (pelvic girdle muscle strengthening such as aerobic, stretching and strengthening exercises) plus information and these information alone on pregnant women with PGP. Lumbopelvic belt was removed only during the sleeping time. MCE were performed 2–3 times per week for 6 weeks. The pain intensity in the belt group, in comparison to other groups, significantly decreased at both 3-week and 6-week follow-ups. The mean ODI score was also significantly more improved in the belt group compared to the MCE and information alone groups.
Sakamoto et al. [40] compared the effect of MCE (isolated voluntary contraction of the PFMs, pelvic-tilt exercises with voluntary contraction PFM contraction, exercises involving hip extension, abduction, and abdominal crunches) to exercises (stepping, pelvis shifting, pelvis rotation with knee extension, pelvis rotation with knee flexion, and trunk flexion and extension) with pelvic realignment device and to no therapy on LBP and PGP after childbirth. MCE and other exercises were repeated 10 and 10–20 times per session, respectively, and twice a day for four weeks post-delivery. The immediate and short-term exercise effects with a pelvic realignment device resulted in greater improvements in pain and disability compared to pelvic MCE alone.
Kamali et al. [23] compared the effect of manipulation and MCE (voluntary contraction of the local stabilizers of the lumbopelvic region to ensure segmental control in different positions such as supine, crook-lying, side-lying, prone, four-point kneeling, sitting, and standing) in patients with subacute or chronic SIJD. Patients pertaining to the manipulation group were treated individually three times a week for two weeks. In the MCE group, exercises in each position were performed using 10 repetitions for 20 min three times a week, for 4 weeks. Both groups demonstrated significant improvements in pain and disability, and there was no significant between-group difference in the treatment effects. This result suggests that neither manual therapy nor MCE therapy proves to be superior for treating PGP of SIJ.
Concerning the meta-analysis of the three above studies, in terms of pain and disability, the overall analysis demonstrated non-significant effect and moderate heterogeneity (Fig. 2). For pain and disability, SMDs were small and respectively greater and less than zero. These results showed that MCE alone for PGP were not effective in terms of pain reduction compared to other MSKTs, such as manipulation, pelvic realignment device, or no rigid lumbopelvic belt; however, MCE alone for PGP were slightly effective in terms of disability reduction at short-term follow-up (FU).
Short-term effect of MCE combined with other MSKTs on pain and disability
Seven RCTs involving 1051 participants were considered in order to evaluate the short-term effect of MCE combined with other MSKTs on pain and disability [42, 43, 44, 45, 46, 47]. Nevertheless, only three RCTs [45, 46, 47] were suitable for meta-analysis (Fig. 2).
Elden et al. [43] compared the efficacy of standard treatment (patient education about the condition, and back and pelvis anatomy, pelvic belt, home exercise programme designed to increase abdominal and gluteal muscle strength), standard treatment plus MCE (activation and control of local deep lumbopelvic muscles; training of more superficial muscles in dynamic exercises to improve mobility, strength, and endurance capacity) for PGP, and standard treatment plus acupuncture during pregnancy. Treatment was given twice a week over six weeks. After treatment, the MCE group experienced less pain in both the morning and evening than the standard group. The acupuncture group, in turn, had less pain in the evening than the MCE group. Moreover, the acupuncture group had less pain in both the morning and evening than the standard treatment group. These results indicate that both MCE and acupuncture constitute efficient complements to standard treatment for managing PGP with acupuncture being somewhat superior to MCE. In 2008, the same authors [42] described the post-delivery regression of PGP observed in these women using similar interventions over six weeks. Three-quarters of the women were pain-free three weeks after delivery, and there were no differences in recovery between the three treatment groups. PGP had resolved in 99% of the women twelve weeks after delivery.
Nilsson-Wikmar et al. [44] compared the efficacy of non-elastic sacroiliac belt plus oral or written information (about anatomy, body posture and ergonomic device), non-elastic sacroiliac belt plus oral or written information about PGP plus training programme (strengthening and MCE; lateral pulls, standing, leg press, sit-down rowing, and curl-ups), and non-elastic sacroiliac belt plus oral or written information plus home exercises in order to stabilize PFMs (exercises performed with a ball between knees in sitting, standing, and in four-point kneeling position with arm or leg movements, stretching of hamstrings, hip flexors and calf muscles at the end of exercise programme) in pregnant women with PGP. The treatments were performed twice a week from inclusion to gestation week 38; FUs were carried out at 3, 6, and 12 months after delivery. There was no significant difference in terms of pain and activity noticed among the three groups during pregnancy or at FUs.
Nejati et al. [10] compared the effectiveness of exercise therapy (self-mobilization, SIJ stretches, and spinal MCE), manipulation therapy, and the combination of the two on patients with SIJD. All groups demonstrated significant improvement in pain and disability compared to baseline. At 6 weeks, manipulation therapy showed notable results, while exercise therapy was associated with remarkable effects at 12 weeks.
Teymuri et al. [47] investigated the effects of MCE, such as local segmental control exercises (isometric contraction of PFMs and transverse abdominis co-contraction), open chain segmental control exercises (adding limbs’ movements during PFMs contraction), and closed chain segmental control exercises combined with electrotherapy in comparison to electrotherapy alone, in postpartum patients with lumbopelvic pain. Both groups were treated for 6 weeks, three times per week. After treatment, there was a significant decrease in pain and disability observed in both groups. However, MCE group showed a significant decrease in pain and disability, as compared to the electrotherapy group.
Saleh et al. [45] investigated the effect of core MCE (abdominal hollowing, bilateral knee raise, supine extension bridge, straight leg rise from prone, alternate arm and leg raise from quadruped position, and prone abdominal body bridge) in addition to infrared radiation and continuous ultrasound in comparison to infrared radiation and continuous ultrasound alone on lumbosacral region in patients with postpartum lumbopelvic pain. Both groups performed three sessions per week for 6 weeks. Both groups reported a significant improvement in VAS and ODI post-treatment. In MCE group, the improvements in VAS and ODI were more significant compared to traditional treatment group.
ElDeeb et al. [46] investigated the effect of PFM training, such as rhythmic, and sustained contractions combined with MCE (lumbar multifidus activation exercise and transverse abdominis drawing-in maneuver) versus these MCE alone on postpartum women with PGP. Both groups carried out the exercises three times a week for 3 months. In both groups, there was a significant decrease in pain and disability following the intervention. However, the PFM group exhibited a significant decrease in pain and disability, along with a significant increase in PFM strength, compared to the MCE group.
Concerning the meta-analysis of the three studies [45, 46, 47], the overall analysis demonstrated a significant effect with moderate and substantial heterogeneity for pain and disability, respectively, with large SMDs less than zero (Fig. 2). This analysis revealed that MCE when combined with other MSKTs prove to be more effective in terms of pain and disability reduction than control interventions alone in post-delivery patients at short-term FU.
3.6.2Long-term (>
Long-term effect of MCE alone on pain and disability
One RCT involving 81 participants was considered to evaluate the long-term effect of MCE alone on pain and disability [41]. The authors compared the efficacy of specific MCE (deep local muscle training: transverse abdominal wall muscles with coactivation of the lumbar multifidus in the lumbosacral region; superficial global muscles training: gluteus maximus, latissimus dorsi, oblique abdominal, erector spinae, quadratus lumborum, as well as hip adductors and abductors) to physical therapies on post-pregnancy patients with PGP. Treatment was performed over 20 weeks with a 2-year FU. Significant between-group differences were observed in functional status, pain, and physical health in favor of MCE group, which were maintained at 2-year FU.
Long-term effect of MCE combined with other MSKTs on pain and disability
Three RCTs involving 250 participants were considered in order to evaluate the long-term effect of MCE combined with other MSKTs on pain and disability [10, 22, 44].
Stuge et al. [22] investigated the efficacy of physical therapy (massage, joint mobilization, relaxation, and stretching) combined with specific MCE and physical therapy alone on post-pregnancy patients with PGP. Treatment was performed three times a week for 18 to 20 weeks with a 1-year FU. After intervention and at 1-year FU, the MCE group exhibited significant lower pain intensity and disability compared to the control group.
In addition to the above short-term results, Nilsson-Wikmar et al. [44] also reported that pain and disability decreased in all groups between gestation week 38 and 12 months postpartum. Indeed, neither home nor clinic exercises had any additional value as compared to providing a nonelastic sacroiliac belt and information.
In addition to the detailed short-term results, Nejati et al. [10] found no significant difference among the study groups at week 24. Based on the study results, exercises and manipulation therapy appeared to be effective in reducing pain and disability; their combination, however, did not bring about significantly better therapeutic results than either approach implemented separately in SIJD-affected patients.
4.Discussion
This review sought to investigate the effectiveness of MCE of two clinical measures; i.e., pain and disability on patients with PGP of SIJ origin. Initially, the research concerned patients with PGP of SIJ in general, but applying the selection criteria led us to retrieve a majority of studies involving women in their peripartum period. This review identified twelve studies evaluating MCE either administered alone or combined with other MSKTs, as an intervention to manage PGP of SIJ. Nevertheless, only six studies were suitable for the meta-analysis.
With a high quality of evidence (Table 4), the overall findings revealed that MCE alone proved to be uneffective for PGP in terms of pain reduction compared to MSKTs; yet, these MCE were demonstrated to be slightly effective in terms of disability reduction at short-term. These results are similar to those from recent studies which did not conclude on the effectiveness of MCE on PGP, whereas they were effective on LBP [51, 52]. However, the combination of MCE with other MSKTs was found to be more effective than the MSKTs alone in reducing pain and disability at short-term with a strong evidence.
For qualitative analysis, three studies [10, 41, 44] evaluating the effectiveness of MCE combined with other MSKTs at long-term exhibited a PEDro score ranging from 4 to 6/10. Consequently, evidence level in favour of intervention group was considered to be only moderate. Nevertheless, evidence at short-term was revealed to be conflicting [10, 42, 43, 44].
Regarding methodological consideration, the majority of studies were shown to be of moderate quality, as based on their PEDro score, with most of them failing to blind the participants, therapists, and assessors. This, however, is very difficult to avoid in physical therapy unless participants and therapists are both naive to the treatment [10, 23, 39, 40, 41, 42, 45].
Table 4
Evidence quality of the meta-analysis
| (1) Motor control exercises alone compared to other MSKTs for sacroiliac joint pelvic girdle pain. References: Kamali et al. [23], Kordi et al. [39], and Sakamoto et al. [40] | ||||||||||||||
| Certainty assessment | Summary of findings | |||||||||||||
| Study event rates (%) | Anticipated absolute effects | |||||||||||||
|
| Risk of bias | Inconsi- stency | Indire- ctness | Impre- cision | Publication bias | Overall certainty of evidence | With other MSKTs | With Motor control exercises alone | Relative effect (95% CI) | Risk with other MSKTs | Risk difference with Motor control exercises alone | |||
| Pain (follow-up: from 2 to 9 weeks; assessed using VAS) | ||||||||||||||
|
| Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected strong association | 74/82 (90.2%) | 71/81 (87.7%) | RR 0.76 (0.28 to 2.10) | 902 per 1 000 | 217 fewer per 1 000 (from 650 fewer to 993 more) | ||||
| Disability (follow-up: from 2 to 4 weeks; assessed using ODI) | ||||||||||||||
| 110 (2 RCTs) | Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected strong association | 46/55 (83.6%) | 49/55 (89.1%) | RR 0.61 (0.19 to 1.92) | 836 per 1 000 | 326 fewer per 1 000 (from 677 fewer to 769 more) | ||||
| (2) Motor control exercises combined with other MSKTs compared to MSKTs for sacroiliac joint pelvic girdle pain. References: Teymuri et al. [47], Saleh et al. [45], and ElDeeb et al. [46] | ||||||||||||||
| Pain (follow up: range 6 weeks to 12 weeks; assessed with: VAS) | ||||||||||||||
| 121 (3 RCTs) | Not serious | Serious | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effect | 55/61 (90.2%) | 55/60 (91.7%) | RR 1.20 (0.31 to 4.65) | 902 per 1 000 | 180 more per 1 000 (from 622 fewer to 1 000 more) | ||||
| Disability (follow up: from 6 to 12 weeks; assessed using ODI) | ||||||||||||||
| 121 (3 RCTs) | Not serious | Serious | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effect | 55/61 (90.2%) | 55/60 (91.7%) | RR 1.20 (0.31 to 4.65) | 902 per 1 000 | 180 more per 1 000 (from 622 fewer to 1 000 more) | ||||
CI: confidence interval; RR: risk ratio; a: I
For included study characteristics, MCE slightly differed in their design. Thus, MCE included PFM training, local stabilization exercises (SE), specific SE, pelvic SE, and specific pelvic SE. All these interventions were targeted at recruiting pelvic girdle muscles for different durations which varied considerably, ranging from 1 to 20 weeks. This heterogeneity in intervention duration may have impacted the results. It must also be noted that the study heterogeneity in terms of sample size, FU, duration, and blinding, could have affected the results of this review. This highlights the need for further research.
Considering MCE effectiveness, four outcome measures (VAS and ODI, PGQ or DRI) were employed to assess the MCE effectiveness in terms of pain and disability. MCE were beneficial in reducing disability in PGP of SIJ patients. Although MCE were effective, they proved to be more effective when combined with other MSKTs [45, 46, 47]. Nevertheless, this statement must be taken with caution. While dealing with quantitative analysis, the studies that applied MCE alone involved patients with different characteristics in terms of pregnancy period, postpartum period, and gender, particularly in the studies conducted by Kordi et al. [39], Sakamoto et al. [40], and Kamali et al. [23]. In contrast the studies where MCE were combined with other MSKTs considered only patients being in their postpartum period. This setting could have brought about the superior effectiveness when combining the two intervention options. Based on this review, it can be confirmed that SIJ PGP is mainly a problem of women being in their peripartum period. Among all included studies, one study included nine men [23], whereas another [10] did not report the patients’ characteristics. The remaining studies were only conducted on women in their peripartum period. This context can be explained by pregnancy-related physiological and biomechanical changes, resulting in imbalance in PFMs and between the two iliac joints, thereby causing SIJ pain and stress.
Although the mechanisms through which exercise may reduce pain severity remain unclear, it is suggested that being physically active lessens the degree of biomechanical change, thereby decreasing the load on the spine, increasing joint stabilization, and contributing to both better spinal alignment and segmental motion [53]. From a more general standpoint, exercise may help reverse trunk muscle imbalance [54] or initiate a pain desensitization process, resulting in an increased pain detection threshold [55].
Previous systematic reviews conducted on similar topics have led to unreliable conclusions concerning the effectiveness of MCE, owing to conflicting evidence levels [56, 57, 58]. In contrast, Al-subahi et al. [21] concluded that MCE is a most effective physical therapy modality for SIJD. A recent systematic review and meta-analysis conducted on exercise for preventing and treating LBP, PGP, and lumbopelvic pain during pregnancy found that prenatal exercise decreased pain severity during and following pregnancy; however, prenatal exercise did not decrease the odds of any of these conditions at any time point [53].
Finally, the heterogeneity ranging from moderate to substantial detected in the analyses that examined MCE’s impact when administered either alone or in combination with other MSKTs on the odds of pain (I
5.Study limitations
This study displays several limitations that must be mentioned. Indeed, our review only considered studies that were published between 1990 and 2019, as well as only studies published written in either English or French. This means that there may have been relevant articles written in another language or published before 1990 which were not included in our analysis. PGP of SIJ is a multifactorial condition that may concern both women and men. Therefore, our main goal was to investigate the effectiveness of MCE versus other MSKTs on both PGP of SIJ genders. However, our study selection process mainly identified studies involving patients in their peripartum period, which amounted to about 83% of studies. With one study that did not report patient characteristics, the percentages of men and women in the remaining studies were 0.64%, and 96.0% respectively, of all cases. Thus, whilst the population was mixte, it was mainly composed of women. This has certainly impacted the possibility of generalizing our results and extrapolating them to both genders.
Finally, the included studies failed to report on exercise adherence, whereas some of them involved home exercises [23, 39, 40]. Evidence clearly suggests that the effectiveness of patients’ exercises depends on their exercise adherence; moreover, about 70% of patients with chronic musculoskeletal pathologies do not regularly engage in prescribed exercise programs [59].
6.Conclusion
Despite the limited studies of high quality for MCE in management of PGP of SIJ origin, this review revealed that MCE alone, especially concerning PFMs and other local stabilizing muscle training, are apparently not more effective in terms of pain reduction than MSKTs (i.e.; passive and active physical therapy interventions); however, a slight clinical effect in terms of disability reduction at short-term was found. The most effective approach was combining MCE with other MSKTs. These results should be taken with caution as the majority of studies included patients in their peripartum period. Therefore, they cannot be applied to all patients with PGP of SIJ origin. Further research projects are warranted, with exercise adherence assessment included.
There is insufficient evidence to conclude on the effectiveness of MCE alone, therefore clinicians should not focus only on MCE in their daily practice but they should combine MCE with other MSKTs in managing PGP of SIJ origin.
Conflict of interest
None to report.
Author contributions
Concept development (provided idea for the research): JM and GN; Design (planned the methods to generate the results): JM and GN; Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): BH and PM; Data collection/processing (responsible for experiments, patient management, organization, or reporting data): JM and GN; Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): JM and GN; Literature search (performed the literature search): JM and GN; Writing (responsible for writing a substantive part of the manuscript): JM and GN; Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): BH and PM.
References
[1] | O’Sullivan PB, Beales DJJMT. Changes in pelvic floor and diaphragm kinematics and respiratory patterns in subjects with sacroiliac joint pain following a motor learning intervention: A case series. (2007) ; 12: (3): 209-218. |
[2] | Maksymowych WP, et al., Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. (2005) ; 53: (5): 703-709. |
[3] | Berg G, et al., Low back pain during pregnancy. (1988) ; 71: (1): 71-75. |
[4] | Bastiaanssen JM, et al., A historical perspective on pregnancy-related low back and/or pelvic girdle pain. (2005) ; 120: (1): 3-14. |
[5] | Ostgaard H, Andersson G, Karlsson KJS. Prevalence of back pain in pregnancy. (1991) ; 16: (5): 549-552. |
[6] | Chou LH, et al., Inciting events initiating injection-proven sacroiliac joint syndrome. (2004) ; 5: (1): 26-32. |
[7] | O’Sullivan PB, et al., Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. (2002) ; 27: (1): E1-E8. |
[8] | DonTigny RLJPT. Anterior dysfunction of the sacroiliac joint as a major factor in the etiology of idiopathic low back pain syndrome. (1990) ; 70: (4): 250-262. |
[9] | Goldthwait JE, Osgood RBJTBM, Journal S. A consideration of the pelvic articulations from an anatomical, pathological and clinical standpoint. (1905) ; 152: (21): 593-601. |
[10] | Nejati P, Safarcherati A, Karimi FJPP. Effectiveness of exercise therapy and manipulation on sacroiliac joint dysfunction: a randomized controlled trial. (2019) ; 22: (1): 53-61. |
[11] | Slipman CW, et al., Sacroiliac joint pain referral zones. (2000) ; 81: (3): 334-338. |
[12] | Hamidi-Ravari B, et al., Diagnosis and current treatments for sacroiliac joint dysfunction: a review. (2014) ; 2: (1): 48-54. |
[13] | Simopoulos TT, et al., A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician. (2012) ; 15: (3): E305-44. |
[14] | Cohen SPJA, Analgesia, Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. (2005) ; 101: (5): 1440-1453. |
[15] | Schuit D, McPoil T, Mulesa PJJOTAPMA. Incidence of sacroiliac joint malalignment in leg length discrepancies. (1989) ; 79: (8): 380-383. |
[16] | Zelle BA, et al., Sacroiliac joint dysfunction: evaluation and management. (2005) ; 21: (5): 446-455. |
[17] | Vermani E, Mittal R, Weeks AJPP. Pelvic girdle pain and low back pain in pregnancy: a review. (2010) ; 10: (1): 60-71. |
[18] | Cook CE, Hegedus E. Orthopedic physical examination tests: an evidence-based approach. (2012) ; Pearson Higher Ed. |
[19] | Hides JA, et al., Convergence and divergence of exercise-based approaches that incorporate motor control for the management of low back pain. (2019) ; 49: (6): 437-452. |
[20] | Casagrande D, et al., Low back pain and pelvic girdle pain in pregnancy. (2015) ; 23: (9): 539-549. |
[21] | Al-Subahi M, et al., The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. (2017) ; 29: (9): 1689-1694. |
[22] | Stuge B, et al., The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. (2004) ; 29: (4): 351-359. |
[23] | Kamali F, et al., Comparison of manipulation and stabilization exercises in patients with sacroiliac joint dysfunction patients: A randomized clinical trial. (2019) ; 23: (1): 177-182. |
[24] | Moher D, et al., Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) ; 6: (7): e1000097. |
[25] | de Morton NAJAJOP. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. (2009) ; 55: (2): 129-133. |
[26] | Maher CG, et al., Reliability of the PEDro scale for rating quality of randomized controlled trials. (2003) ; 83: (8): 713-721. |
[27] | Moseley AM, et al., Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: A meta-epidemiological study of randomized controlled trials of physical therapy interventions. (2019) ; 14: (9): e0222770. |
[28] | Higgins J, Altman D, Sterne JJAFWCHO. Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, (2011) , 2011. |
[29] | Guyatt GH, et al., GRADE guidelines 6. Rating the quality of evidence – imprecision. (2011) ; 64: (12): 1283-1293. |
[30] | Guyatt GH, et al., GRADE guidelines: 8. Rating the quality of evidence – indirectness. (2011) ; 64: (12): 1303-1310. |
[31] | Guyatt GH, et al., GRADE guidelines: 7. Rating the quality of evidence – inconsistency. (2011) ; 64: (12): 1294-1302. |
[32] | Guyatt GH, et al., GRADE guidelines: 5. Rating the quality of evidence – publication bias. (2011) ; 64: (12): 1277-1282. |
[33] | Guyatt GH, et al., GRADE guidelines: 4. Rating the quality of evidence – study limitations (risk of bias). (2011) ; 64: (4): 407-415. |
[34] | Furlan AD, et al., 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. (2009) ; 34: (18): 1929-1941. |
[35] | Van Tulder M, et al., Updated method guidelines for systematic reviews in the cochrane collaboration back review group. (2003) ; 28: (12): 1290-1299. |
[36] | Deeks JJ, et al., Analysing data and undertaking meta-analyses. (2019) ; 241-284. |
[37] | Cohen JJH, New Jersey, Statistical Power Analysis for the Behavioral Sciences – Second Edition. 12 Lawrence Erlbaum Associates Inc. (1988) , 13. |
[38] | Faraone SVJP, Therapeutics, Interpreting estimates of treatment effects: implications for managed care. (2008) ; 33: (12): 700. |
[39] | Kordi R, et al., Comparison between the effect of lumbopelvic belt and home based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. (2013) ; 26: (2): 133-139. |
[40] | Sakamoto A, et al., Effect of exercise with a pelvic realignment device on low-back and pelvic girdle pain after childbirth: A randomized control study. (2018) ; 50: (10): 914-919. |
[41] | Stuge B, et al., The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. (2004) ; 29: (10): E197-E203. |
[42] | Elden H, et al., Regression of pelvic girdle pain after delivery: follow-up of a randomised single blind controlled trial with different treatment modalities. (2008) ; 87: (2): 201-208. |
[43] | Elden H, et al., Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. (2005) ; 330: (7494): 761. |
[44] | Nilsson-Wikmar L, et al., Effect of three different physical therapy treatments on pain and activity in pregnant women with pelvic girdle pain: a randomized clinical trial with 3, 6, and 12 months follow-up postpartum. (2005) ; 30: (8): 850-856. |
[45] | Saleh MSM, et al., Effect of core stability exercises on postpartum lumbopelvic pain: A randomized controlled trial. (2019) ; 32: (2): 205-213. |
[46] | ElDeeb AM, et al., Effect of segmental stabilizing exercises augmented by pelvic floor muscles training on women with postpartum pelvic girdle pain: A randomized controlled trial. (2019) ; 32: (5): 693-700. |
[47] | Teymuri Z, et al., The effect of stabilization exercises on pain, disability, and pelvic floor muscle function in postpartum lumbopelvic pain: A randomized controlled trial. (2018) ; 97: (12): 885-891. |
[48] | Cho J, Lee E, Lee S. Upper thoracic spine mobilization and mobility exercise versus upper cervical spine mobilization and stabilization exercise in individuals with forward head posture: a randomized clinical trial. BMC Musculoskelet Disord. (2017) ; 18: (1): 525. |
[49] | Hidalgo B, et al., Short-term effects of Mulligan mobilization with movement on pain, disability, and kinematic spinal movements in patients with nonspecific low back pain: a randomized placebo-controlled trial. J Manipulative Physiol Ther. (2015) ; 38: (6): pp. 365-74. |
[50] | Ziaeifar M, et al., Dry needling versus trigger point compression of the upper trapezius: a randomized clinical trial with two-week and three-month follow-up. J Man Manip Ther. (2019) ; 27: (3): 152-161. |
[51] | O’Keeffe M, et al., Are group-based and individual physiotherapy exercise programmes equally effective for musculoskeletal conditions? A systematic review and meta-analysis. Br J Sports Med. (2017) ; 51: (2): 126-132. |
[52] | Shiri R, Coggon D, Falah-Hassani K. Exercise for the prevention of low back and pelvic girdle pain in pregnancy: A meta-analysis of randomized controlled trials. Eur J Pain. (2018) ; 22: (1): 19-27. |
[53] | Davenport MH, et al., Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: a systematic review and meta-analysis. (2019) ; 53: (2): 90-98. |
[54] | Gutke A, Östgaard HC, Öberg BJJORM. Association between muscle function and low back pain in relation to pregnancy. (2008) ; 40: (4): 304-311. |
[55] | Rainville J, et al., Exercise as a treatment for chronic low back pain. (2004) ; 4: (1): 106-115. |
[56] | Almousa S, Lamprianidou E, Kitsoulis GJPRI. The effectiveness of stabilising exercises in pelvic girdle pain during pregnancy and after delivery: a systematic review. (2018) ; 23: (1): e1699. |
[57] | Ferreira CWS, Alburquerque-Sendın F. Effectiveness of physical therapy for pregnancy-related low back and/or pelvic pain after delivery: a systematic review. (2013) ; 29: (6): 419-431. |
[58] | Tseng P-C, et al., A systematic review of randomised controlled trials on the effectiveness of exercise programs on Lumbo Pelvic Pain among postnatal women. (2015) ; 15: (1): 316. |
[59] | Beinart NA, et al., Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: A systematic review. (2013) ; 13: (12): 1940-1950. |




