The effects of proprioceptive neuromuscular facilitation in treating chronic low back pain: A systematic review and meta-analysis
Abstract
BACKGROUND:
Proprioceptive neuromuscular facilitation (PNF) has been widely used in the clinical treatment of chronic low back pain (LBP) in recent years. However, its role remains controversial and it is unclear whether PNF offers more advantages for patients with chronic LBP.
OBJECTIVE:
The purpose of this systematic review is to evaluate the evidence on the effect of PNF on pain, waist function, pulmonary function and dynamic balance in patients with chronic LBP.
METHODS:
Seven English and Chinese electronic databases were searched to identify articles published from 1970 to February 2020. Relevant randomized controlled trials (RCTs) were selected by two independent reviewers to investigate PNF in treatment of chronic LBP. Data extraction was performed by the same reviewers.
RESULTS:
Twelve eligible trials involving 410 participants were included in this meta-analysis. Compared with the control group, the aggregated results suggested that PNF showed beneficial effects in relieving pain (SMD
CONCLUSIONS:
PNF showed more beneficial effects in pain relief and waist function improvement in patients with chronic LBP in the short term (4 to 8 weeks of intervention) or at 12-week follow-up and also played a positive role in pulmonary function. However, no significant effect of PNF on dynamic balance was found compared with the control group. However, these results have certain limitations, and these conclusions were supported by low-quality data. Therefore, articles that are methodologically reasonable and more authoritative are required to verify the effects. In addition, articles with long-term follow-up and other outcomes are needed to confirm additional findings.
1.Introduction
Low back pain (LBP) is the most common musculoskeletal condition and constitutes a global public health problem. It is also one of the diseases that causes the most individual disability worldwide [1, 2, 3]. The painful areas of LBP are usually distributed below the costal margin and above the inferior gluteal folds and are often accompanied by clinical symptoms such as muscle tension, stiffness and even sciatica [4]. Back pain lasting longer than 12 weeks is defined as chronic LBP, which seriously affects people’s work and life activities and reduces quality of life [5, 6]. Recent research shows that the number of people with disabilities caused by chronic LBP has increased by 54% in the last 30 years [7, 8]. Thus, LBP poses substantial challenges for the medical system, creates socioeconomic issues for working-age adults, and levies a severe medical burden on individuals and society [3, 7, 8]. According to statistics, the total cost of treatment for chronic LBP in the United States is estimated to exceed US $100 billion per year [11, 12].
Numerous factors have been proven as underlying causes of persistent LBP, including trunk proprioception dysfunction, back muscle weakness or delayed activation, lumbar joint imbalance and important defects in the neural control unit of spinal stabilization system [13, 14, 15, 16, 17, 18]. Therefore, improving trunk proprioception function and back muscle strength were the focus of treatment [19]. In most clinical practice guidelines, physical therapy is a common treatment method for chronic LBP, including trunk muscle training, proprioceptive neuromuscular facilitation (PNF) and electromagnetic stimulation.
PNF is a multifaceted exercise therapy method based on the theory of human development and neurophysiology, and it has important physiological and health benefits in improving trunk proprioception, muscle strength, exercise control, balance and endurance [20, 21, 22, 23]. Recently, PNF training has been widely used by physical therapists to treat patients with chronic LBP, and the mechanism elicits a neuromuscular response by stimulating proprioceptors to relieve the symptoms of low back pain [24, 25, 26, 27, 30, 31, 32, 33, 34, 35]. Moreover, the proprioceptors of the joints and muscles in the lumbar region of patients with chronic LBP were stimulated by PNF training to improve sensorimotor regulation and balance performance [27]. PNF technology has multiple movement patterns. Studies have shown that PNF training promotes muscle performance of chronic LBP mainly through its movement patterns because its movement patterns are basically consistent with topographic arrangement of muscles used in activities and sports [26, 28]. Additionally, PNF training adopts diagonal and spiral directions, which are more effective than conventional single-direction exercise training in enhancing human performance and relieving clinical symptoms of chronic LBP [28].
Currently, no systematic review of PNF training for chronic LBP exists, although certain published articles have reported the positive effects of physical therapists using PNF training in chronic LBP. Therefore, it is highly meaningful to confirm whether PNF training produces more beneficial effects than general exercise or conventional therapy in chronic LBP according to evidence-based medical studies, which can offer reference suggestions for clinical treatment of chronic LBP. The purpose of this systematic review is to evaluate the effect of PNF on pain, waist function, pulmonary function and dynamic balance in patients with chronic LBP.
2.Methods
2.1Search strategy
Randomized controlled trials (RCTs) were identified by electronically searching the following online databases up to February 2020: PubMed, Embase, Cochrane Library, Web of Science, EBSCO, China National Knowledge Infrastructure and WanFang Data.
Appendix 1 presents a detailed description of the complete electronic search strategy for PubMed. Generally, the medical subject headings (MeSH) were composed of the following: low back pain, proprioceptive neuromuscular facilitation and back pain. The keywords were randomized controlled trials (RCTs), single-blind method, double-blind method, random allocation, low back pain, back pain, low back ache, proprioceptive neuromuscular facilitation, PNF, and PNF stretching. Duplicate articles were removed if found in multiple database searches.
2.2Inclusion criteria
1. Types of studies. Only RCT experiments were selected to examine the effects of PNF in treating chronic LBP. There were no language or publication date restrictions for this study.
2. Types of participants. The subjects in our selected article included participants (over 18 years old) who suffered from chronic LBP for longer than
Table 1
Characteristics of included studies
| Author, year | Sample size Participant characteristic duration of complaint | Intervention | Exercise frequency and study duration | Outcomes | Follow-up (time) |
|---|---|---|---|---|---|
| Areeudomwong 2019 (English) | 44 subjects, mean age G1 | G1: PNF training G2: General trunk exercise | Three times per week for 4 weeks | NRS; RMDQ; CoP velocity; ellipse sway area | No |
| Kumar 2011 (English) | 30 subjects, mean age G1 | G1: PNF training G2: Conventional treatment | Five times per week for 4 weeks | VAS; ODI; ROM Curl-up test; Sorenson test | No |
| Lee 2014 (English) | 40 subjects, mean age G1 | G1: PNF training G2: Ball exercise | Four times per week for 6 weeks | VAS; EMG | No |
| Areeudomwong 2017 (English) | 42 subjects, mean age G1 | G1: PNF training G2: LBP booklet | Five times per week for 4 weeks | NRS, RMDQ, HRQOL LES muscle activity Patient satisfaction | Yes, twelve weeks |
| Kim 2017 (English) | 30 subjects, mean age G1 | G1: PNF-AMST program G2: Traditional physical therapy | Five times per week for 6 weeks | FEV | No |
| Areeudomwong 2019 (English) | 45 subjects, mean age G1 | G1: Therapeutic | Four weeks of intervention | VAS; RMDQ, SEMG, Patient satisfaction | Yes, twelve weeks |
| Kofotolis 2006 (English) | 86 subjects, mean age G1 | G1: PNF-RST program G2: PNF-COI program G3: No intervention | Eight weeks of intervention | Borg Back Pain Intensity, ODI, ROM | No |
| Young 2015 (English) | 48 subjects, mean age (unclear) LBP duration for six month or longer | G1: PNF (PIP pattern) training G2: Swiss ball training | Three times per week for 6 weeks | Mean velocity in the X and Y directions FRT, TUG, VAS | No |
| Bong 2014 (Korean) | 14 subjects, mean age G1 | G1: PNF abdominal training G2: Abdominal muscle exercise | Five times per week for 6 weeks | VAS; FEV | No |
|
Table 1, continued | |||||
|---|---|---|---|---|---|
| Author, year | Sample size Participant characteristic duration of complaint | Intervention | Exercise frequency and study duration | Outcomes | Follow-up (time) |
| Jeon 2017 (Korean) | 20 subjects, mean age G1 | G1: PNF | Three times a week for 6 weeks | VAS; ODI | No |
| Kim 2017 (Korean) | 30 subjects, mean age G1 | G1: PNF abdominal training G2: Abdominal strengthening training G3: Conventional physiotherapy | Three times per week for 6 weeks | VAS; BBS | No |
| Jeon 2013 (Korean) | 34 subjects, mean age G1 | G1: Integrated PNF on sprinter and skater patterns exercise G2: Swiss ball exercise | Three times per week for 6 weeks | X and Y speed, FRT, TUG | No |
Abbreviations: LBP, low back pain; ODI, Oswestry Disability Index; MRDQ, Roland Morris Disability Questionnaire; VAS, Visual Analog Scale; NRS, Numerical Rating Scale; Borg, Borg Back Pain Intensity; BBS, Berg Balance Scale; FEV
12 weeks. The articles on chronic LBP caused by pathology or organic causes were excluded.
3. Types of interventions. Trials were divided into a PNF group and a control group. The control group only received one of the treatment methods of “general exercise, conventional physical therapy, electromagnetic therapy, electrotherapy, low back pain education” and the experimental group, received PNF training or treatment.
4. Types of outcome measures. The primary outcomes included pain intensity scores (VAS/Borg Back Pain Intensity Scale/NRS) and waist functional status (Oswestry Disability Index, ODI; Roland Morris Disability Questionnaire (RMDQ). Secondary outcomes included other indices of forced expiratory volume at one second (FEV
2.3Selection of studies
The relevant titles, abstracts and full reviews were screened by two reviewers (PG and FT) according to the included criteria. An article was deleted if it did not fulfill the inclusion criteria. If disagreement occurred between reviewers in reaching the final selection decisions, then it was necessary to consult the third reviewer (WL).
2.4Data extraction
The relevant data from the eligible articles were extracted, such as author and year of publication, sample size, participant characteristics, duration of complaint, description of interventions between the experimental and control groups, outcomes, and follow-up status (Table 1).
2.5Assessing the risk of bias
The risk of bias in all articles was evaluated using the Cochrane Collaboration recommendations [29]. The following information was assessed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, incomplete outcome data, selective reporting and other bias. The methodological quality of all articles was independently assessed by two reviewers (PG and YM). Any disagreements in the risk bias assessment were settled by consulting a third reviewer (WL).
2.6Statistical analysis
Data analysis was conducted using Manager Software (RevMan5.3). The I
3.Results
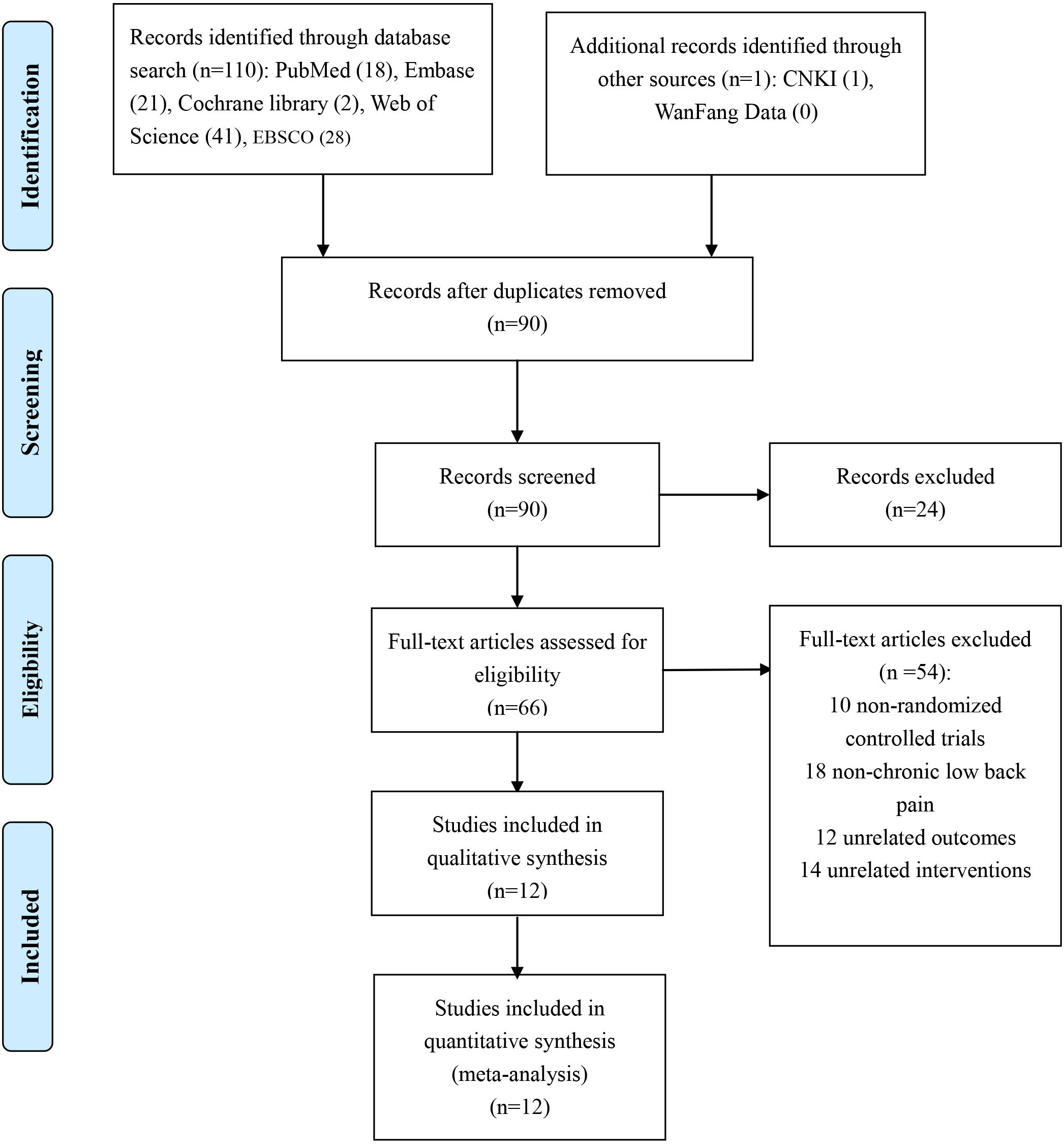
3.1Search results
A total of 111 records were initially identified from PubMed, Embase, Cochrane Library, Web of Science, EBSCO, and China National Knowledge Infrastructure and WanFang Data (Fig. 1). A total of 21 duplicate articles identified in multiple database searches were removed, and 66 articles were retained according to their title and abstract. Furthermore, only 12 articles [25, 26, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39] fulfilled the inclusion criteria after these 54 potential articles were assessed in full texts. Table 1 shows the characteristics of each included study.
Figure 1.
Flowchart of the study selection procedure.
3.2Risk of bias of included studies
According to the Cochrane Collaboration recommendations, eight studies described the process of random sequence generation [25, 26, 30, 31, 33, 34, 35, 38], and the remaining trials only mentioned randomization without describing a specific method of random sequence generation [32, 36, 37, 39]. Three articles described the allocation concealment method, but the allocation concealment of the other nine studies was not determined [25, 26, 30, 31, 32, 36, 37, 38, 39]. Seven articles were deemed at a high risk of bias in blinding of participants and personnel [26, 30, 35, 36, 37, 38, 39], and this issue was unclear in two articles [31, 32]. Nine articles displayed a high risk of bias in blinding of outcome assessments [25, 26, 30, 31, 32, 36, 37, 38, 39]. Incomplete outcome data and selective reporting were at a low risk of bias in all articles. However, the possibility of other bias in each article was unclear [25, 26, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39]. Therefore, the evidence of this systematic review has a certain high risk of overall bias. The risk of bias assessment of all included studies is described in Figs 2 and 3.
Figure 2.
Risk of bias summary: Review authors’ judgments of bias items for each included study.
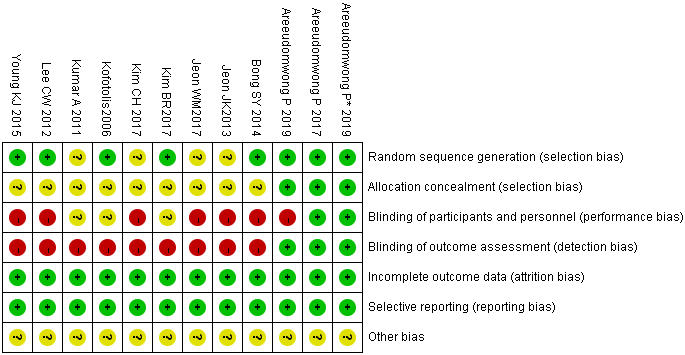
Figure 3.
Risk of bias graph: Reviewers’ judgments of each bias item, presented as percentages.
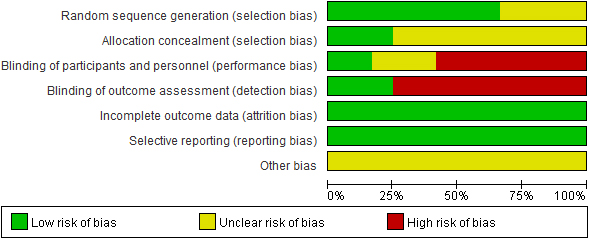
Figure 4.
Meta-analyses of the effect of PNF on pain intensity compared with the control group as conducted in different intervention duration and follow-up periods.
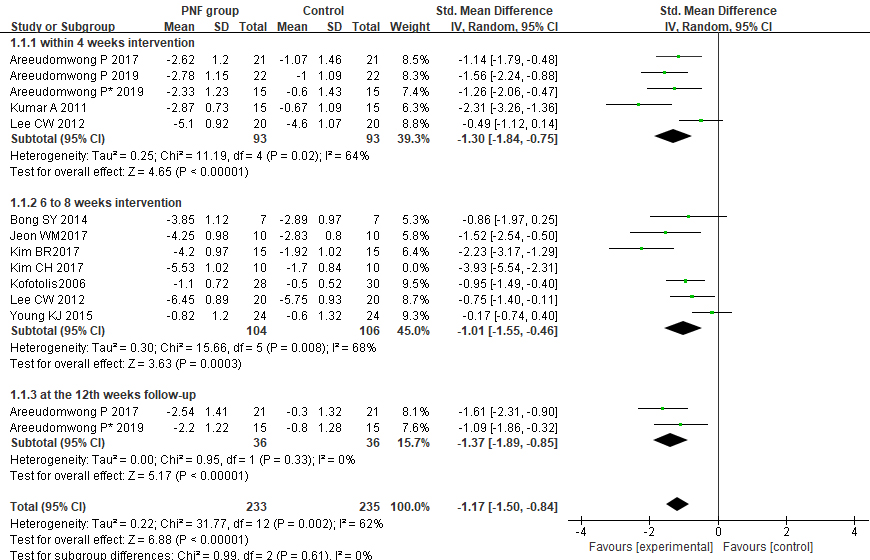
Figure 5.
Meta-analyses of the effect of PNF on functional disability compared with the control group as conducted in different intervention duration and follow-up periods.
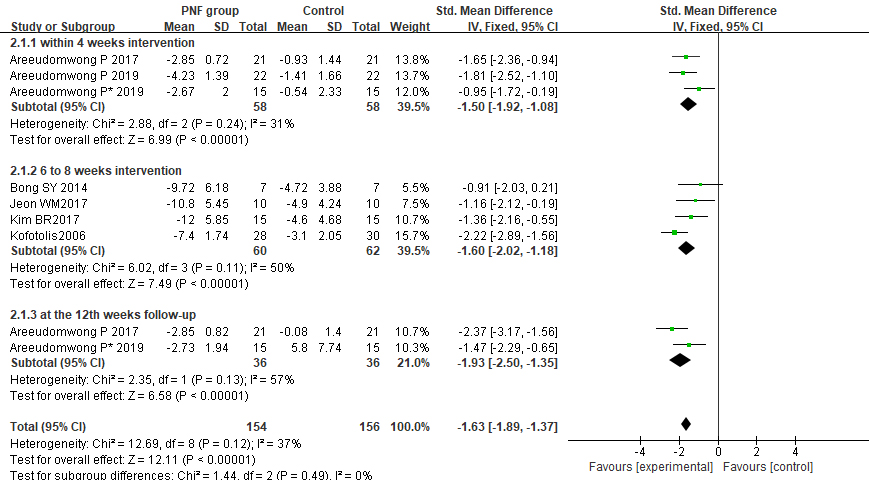
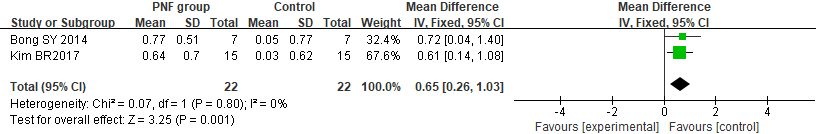
Figure 6.
Meta-analyses of the effect of PNF on pulmonary function.
3.3Effects of PNF on primary outcomes
The primary outcomes included pain intensity and waist functional status. First, a total of 11 articles used pain intensity as a low back pain evaluation index, including 8 articles using the visual analog scale (VAS), 2 articles using the numerical rating scale (NRS) and 1 article using the Borg Back Pain Intensity Scale. Overall, the results showed that compared with the control group, PNF significantly relieved pain (SMD
3.4Effects of PNF on secondary outcomes
Two articles used pulmonary function and dynamic balance indicators. As displayed in Fig. 6, PNF was shown to have a significant effect on pulmonary function (MD
Figure 7.
Meta-analyses of the effect of PNF on dynamic balance. FRT (functional reach test); TUG: (timed up and go test).
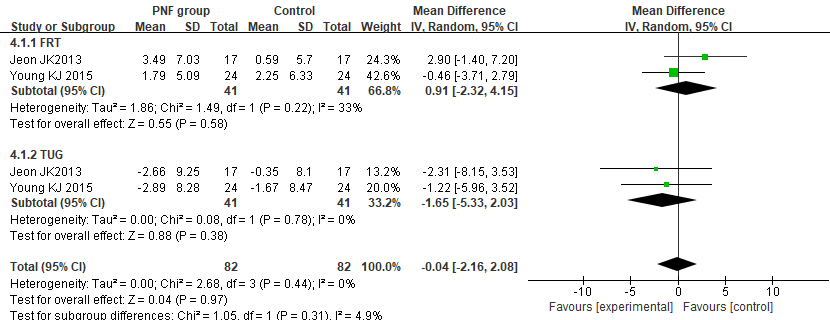
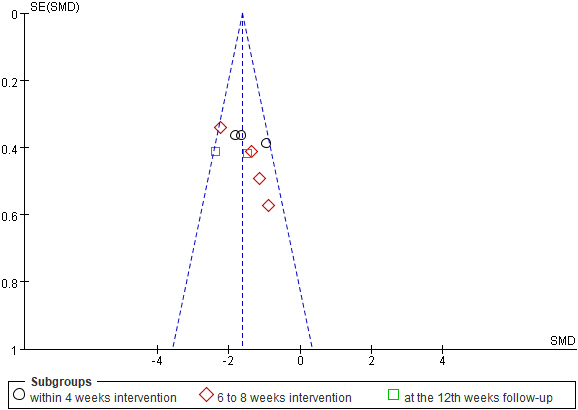
Figure 8.
Funnel plot for evaluating the publication bias of function disability.
3.5Sensitivity analyses
High heterogeneity was found in the pain intensity index of 6 to 8 weeks intervention in forest plot (Fig. 4), and after sensitivity analysis, we found that the statistical heterogeneity of pain intensity was mainly caused by the trials of Kim [31], Kim [36], and Young [30], and we should thus pay additional attention to them in the analysis of the results.
4.Discussion
This study is conduct a systematic review and meta-analysis of the pooled effects of PNF on chronic LBP. In this meta-analysis, we identified 12 RCTs involving 410 patients who explore the effects of PNF on chronic low back pain. The Cochrane Collaboration recommendations were used to evaluate the risk bias of each article. However, it is difficult to determine the other risks of bias in each article. No serious adverse events were found during PNF treatment in the eligible studies. In addition, we could not determine the safety of PNF training because the number of patients was too small.
Our research found that PNF is an effective therapy, and the results of this meta-analysis indicate that PNF intervention is superior to the control group for relieving pain and improving functional disability in short-term intervention within 4 weeks or 6 to 8 weeks, and similar results were found at the 12-week follow-up. The results of this study are consistent with those of Paolucci et al. [40], suggesting that PNF is a beneficial nonpharmacological treatment for chronic LBP and has a unique effect on the treatment of pain and waist function in chronic LBP. In addition, the results of this meta-analysis showed that PNF can improve the pulmonary function of chronic LBP, but no significant effect of PNF on dynamic balance were observed in the results of the meta-analysis. PNF could improve waist function of chronic LBP patients mainly because it can improve the trunk muscle strength and coordination ability, so as to enhance the stability of the trunk. In the practice process, PNF not only improves the waist muscle strength, but also enhances the power of the abdominal muscle group at the same time, including the abdominis rectus and internal and external oblique muscle. Thus, PNF training indirectly improves lung function because the ability of abdominal breathing increased. Kim et al. [41] conducted PNF-AMST exercises on the waist and abdomen for 5 days in patients’ caregivers with chronic LBP. They found that it significantly reduced VAS and improved FEV
It is worth noting that the eligible articles in this review only consider patients with chronic LBP (duration of pain
Previous studies have found that the activation and coordination of trunk muscles is impaired in patients with chronic LBP, which can further lead to excessive movement and lumbar spine instability, resulting in greater pain and dysfunction [43, 44, 45]. PNF emphasizes the overall movement of multiple joint proprioceptors and multiple trunk muscle groups rather than the movement of a single muscle, and thus PNF played a positive role in pain relief and waist functional improvement in chronic low back pain.
4.1Limitations
This meta-analysis is not without limitations. First, the findings from the systematic reviews were based on relatively low-quality data, which have a potential high risk of bias, and the number of methodologically rigorous articles is still insufficient. Second, the sample size of the participants in this meta-analysis was too small to determine the effectiveness of PNF training for chronic LBP. The third limitation was the possibility of publishing bias, and we attempted to reduce this bias via a large number of database searches. However, we did not search for unpublished articles. Finally, this meta-analysis contains too few qualified articles for a secondary outcome index, and thus the secondary results of this meta-analysis require further demonstration.
4.2Implications for practice
Previous research shows that the main roles of PNF technology include reducing pain and fatigue, enhancing muscle strength, increasing flexibility, improving coordination and control, improving stability and balance, and enhancing endurance in patients with chronic LBP [46, 47, 48]. Judging from the results of this systematic review, PNF could indeed improve the pain and functional status of patients with chronic LBP, and thus it can be used in clinical treatment of chronic LBP. We determined that the dose of 4 to 8 weeks intervention of PNF training had a positive therapeutic effect. It still maintains a certain effect at the 12th week of follow-up after the treatment is over. However, the results of this systematic review show that the effects of PNF on dynamic balance were not ideal, and we lack sufficient eligible RCT trails to demonstrate the secondary outcome.
5.Conclusions
Compared with the control group, PNF showed more beneficial effects in relieving pain and improving the functional status of patients with chronic LBP in the short term of 4- to 8-week intervention and it remained a positive role at 12th-week follow-up. However, no significant effect of PNF on dynamic balance was found compared with the control group. However, these results have certain limitations. These conclusions were supported by low-quality data, and there was a certain publication bias, and thus articles that are methodologically rigorous and more authoritative are required to confirm the effects. In addition, articles with long-term follow-up and other outcomes are required to confirm more findings.
Author contributions
The study was conceived by PG and FT. YM and PG primarily contributed to the collection of study information and data extraction. WG assisted in the search process for studies. All authors participated in drafting the manuscript, read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Funding
This research was supported by the National Natural Science Foundation of China (Grant no. BLA150064), the Educational Research Project of Hunan Province (Grant no. 19C1330), and the Higher Education Teaching Reform Project of Hunan Province (Grant no. 2019-1165).
Systematic review registration
This study was registered at https://www.crd.york.ac. uk/prospero/PROSPERO under registration number CRD42020163955.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-200306.
Acknowledgments
The authors would like to thank American Journal Experts for English language editing (AJE verification code 9983-02D7-A903-D56C-E8EC).
Conflict of interest
None of the authors have any competing interests to report.
References
[1] | Rubin DI. Epidemiology and risk factors for spine pain. Neurologic Clinics. (2007) ; 25: (2): 353-371. |
[2] | Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. (2012) ; 64: (6): 2028-37. |
[3] | Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D, et al. Asystematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord. (2014) ; 15: : 50. |
[4] | Koes BW, Van T, Thomas S. Diagnosis and treatment of low back pain. J Orthop. Trauma. (2006) ; 332: : 1430-1434. |
[5] | Crow WT, Willis DR. Estimating cost of care for patients with acute low back pain: A retrospective review of patient records. J Am Osteopath Assoc. (2009) ; 109: : 229-33. |
[6] | França FR, Burke TN, Hanada ES, et al. Segmental stabilization and muscular strengthening in chronic low back pain. Clinics. (2010) ; 65: : 1013-1017. |
[7] | Croft P, Ferreira M, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. (2018) ; 392: : 2356-2367. |
[8] | Morris LD, Daniels KJ, Ganguli B, et al. An update on the prevalence of low back pain in Africa: A systematic review and meta-analyses. BMC Musculoskeletal Disorders. (2018) ; 19: : 196. |
[9] | Beith ID, Kemp A, Kenyon J, Prout M, Chestnut TJ. Identifying neuropathic back and leg pain: A cross-sectional study. Pain. (2011) ; 152: : 1511-6. |
[10] | Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. (2010) ; 24: (6): 769-81. |
[11] | Woolf AD, Erwin J, March L. The need to address the burden of musculoskeletal conditions. Best Pract Res Clin Rheumatol. (2012) ; 26: (2): 183-224. |
[12] | Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am. (1991) ; 22: : 263-71. |
[13] | Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: What works? Pain. (2004) ; 107: (1-2): 176-90. |
[14] | Lee JH, Hoshino Y, Nakamura K, Kariya Y, Saita K, Ito K. Trunk muscle weakness as a risk factor for low back pain: A 5-year prospective study. Spine. (1999) ; 24: (1): 54-57. |
[15] | Cho KH, Beom JW, Lee TS, Lim JH, Lee TH, Yuk JH. Trunk muscles strength as a risk factor for nonspecific low back pain: A pilot study. Ann Rehabil Med. (2014) ; 38: (2): 234-240. |
[16] | Tong MH, Mousavi SJ, Kiers H, Ferreira P, Refshauge K, van Dieën J. Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Arch Phys Med Rehab. (2017) ; 98: (1): 120-136. |
[17] | da Silva RA, Vieira ER, Fernandes KB, et al. People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil. (2017) ; 27: : 1-7. |
[18] | Tsigkanos C, Gaskell L, Smirniotou A, Tsigkanos G. Static and dynamic balance deficiencies in chronic low back pain. J Back Musculoskelet Rehabil. (2016) ; 29: (4): 887-893. |
[19] | Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians Noninvasive Treatments for acute, subacute, and chronic low back pain. Annals Intern Med. (2017) ; 166: (7): 514-530. |
[20] | Sharman MJ, Cresswell AG, Riek S. Proprioceptive neuromuscular facilitation stretching: mechanisms and clinical implications. Sports Med. (2006) ; 36: (11): 929-939. doi: 10.2165/00007256-200636110-00002. |
[21] | Hindle K, Whitcomb T, Briggs W, et al. Proprioceptive neuromuscular facilitation (PNF): Its mechanisms and effects on range of motion and muscular function. Journal of Human Kinetics. (2012) ; 31: (-1). |
[22] | Cayco CS, Gorgon EJR, Lazaro RT. Effects of proprioceptive neuromuscular facilitation on balance, strength, and mobility of an older adult with chronic stroke: A case report. J Bodyw Mov Ther. (2017) ; 21: (4): 767-774. doi: 10.1016/j.jbmt.2016.10.008. |
[23] | Szafraniec R, Chromik K, Poborska A, et al. Acute effects of contract-relax proprioceptive neuromuscular facilitation stretching of hip abductors and adductors on dynamic balance. Peer J. (2018) ; 13; 6: e6108. |
[24] | George AJ, Kumar D, Nikhil NP. Effectiveness of trunk proprioceptive neuromuscular facilitation training in mechanical low back pain. International Journal of Current Research. (2013) ; 5: (7): 1965-1968. |
[25] | Kofotolis N, Kellis E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility and functional performance in women with chronic low back pain. Physical Therapy. (2006) ; 86: (7): 1001-1012. |
[26] | Lee CW, Hwangbo K, Lee IS. The effects of combination patterns of proprioceptive neuromuscular facilitation and ball exercise on pain and muscle activity of chronic low back pain patients. Journal of Physical Therapy Science. (2014) ; 26: (1): 93-96. |
[27] | Adler SS, Beckers D, Buck M. PNF in Practice (4thedn). Berlin: Springer-Medizin. (2014) . |
[28] | Westwater-Wood S, Adams N, Kerry R. The use of proprioceptive neuromuscular facilitation in physiotherapy practice. Physical Therapy Reviews. (2010) ; 15: (1): 23-28. |
[29] | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) ; 343: : 889-93. doi: 10.1136/bmj.d5928. |
[30] | Young KJ, Je CW, Hwa ST. Effect of proprioceptive neuromuscular facilitation integration pattern and Swiss ball training on pain and balance in elderly patients with chronic back pain. J Phys Ther Sci. (2015) ; 27: (10): 3237-3240. |
[31] | Kim BR, Lee HJ. Effects of proprioceptive neuromuscular facilitation-based abdominal muscle strengthening training on pulmonary function, pain, and functional disability index in chronic low back pain patients. Journal of Exercise Rehabilitation. (2017) ; 13: (4): 486-490. |
[32] | Kumar A, Zutshi K, Narang N. Efficacy of trunk proprioceptive neuromuscular facilitation training on chronic low back pain. International Journal of Sports Science and Engineering. (2011) ; 5: (3): 174-180. |
[33] | Areeudomwong P, Witchayut Wongrat, Nertnapa Neammesri & Thanaporn Thongsakul. A randomized controlled trial on the long-term effects of proprioceptive neuromuscular facilitation training, on pain-related outcomes and back muscle activity, in patients with chronic low back pain. Musculoskeletal Care. (2017) ; 15: (3): 218-229. |
[34] | Areeudomwong P*, Buttagat V. Comparison of core stabilisation exercise and proprioceptive neuromuscular facilitation training on pain-related and neuromuscular response outcomes for chronic low back pain: a randomised controlled trial. Malays J Med Sci. (2019) ; 26: (6): 77-89. |
[35] | Areeudomwong P, Vitsarut Buttagat. Proprioceptive neuromuscular facilitation training improves pain-related and balance outcomes in working-age patients with chronic low back pain: A randomized controlled trial. Brazilian Journal of Physical Therapy. (2019) ; 23: (5): 428-436. |
[36] | Kim CH, Kim BR. The effects of abdominal strength training using proprioceptive neuromuscular facilitation on the balance ability and pain of patients with chronic lower back pain. PNF and Movement. (2017) ; 15: (2): 141-148. |
[37] | Jeon HJ, Lee MH. The effects of PNF technique versus trunk exercise program on the pain, disability, and balance in chronic LBP patients. The Korea Contents Association. (2009) ; 9: (12): 665-673. |
[38] | Bong SY, Kim YJ, Kang MG, et al. Effects of proprioceptive neuromuscular facilitation exercise on forced expiratory volume at one second, pain, and functional disability index of chronic low back pain patients. PNF and Movement. (2016) ; 14: (3): 185-193. |
[39] | Jae-Keun Jeon. The effects of combination patterns exercise of proprioceptive neuromuscular facilitation on balance in chronic low back pain elderly patients. Journal of Digital Convergence. (2013) ; 11: (4): 361-368. |
[40] | Paolucci T, Attanasi C, Cecchini W, Marazzi A, Capobianco SV, Santilli V. Chronic low back pain and postural rehabilitation exercise: A literature review. J Pain Res. (2018) ; 12: : 95-107. Published 2018 Dec 20. doi: 10.2147/JPR.S171729. |
[41] | Kim KS, Kwon OY, Yi CH. Effect of abdominal drawing-in maneuver on peak expiratory flow, forced expiratory volume in 1 second and pain during forced expiratory pulmonary function test in patients with chronic low back pain. J Korean Acad Univ Trained Phys Ther. (2009) ; 16: : 10-17. |
[42] | Lee BK. The effect of the forced pulmonary function of young female, by changes in lung function related to postures and by transverse abdominis activation in standing position. J Korean Soc Phys Med. (2012) ; 7: : 267-274. |
[43] | Ringheim I, Austein H, Indahl A, Roeleveld K. Postural strategy and trunk muscle activation during prolonged standing in chronic low back pain patients. Gait Posture. (2015) ; 42: (4): 584-589. |
[44] | Tsao H, Druitt TR, Schollum TM, Hodges PW. Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. J Pain. (2010) ; 11: (11): 1120-1128. |
[45] | Borghuis J, Hof LA, Lemmink KA. The importance of sensory-motor control in providing core stability. Sports Med. (2008) ; 38: (11): 893-916. |
[46] | Yuktasir B, Kaya F. Investigation into the long-term effects of static and PNF stretching exercises on range of motion and jump performance. Journal of Bodywork & Movement Therapies. (2009) ; 13: (1): 0-21. |
[47] | Osternig LR, Robertson RN, Troxel RK, et al. Differential responses to proprioceptive neuromuscular facilitation (PNF) stretch techniques. Medicine & Science in Sports & Exercise. (1990) ; 22: (1): 106-111. |
[48] | Hindle K, Whitcomb T, Briggs W, et al. Proprioceptive neuromuscular facilitation (PNF): Its mechanisms and effects on range of motion and muscular function. Journal of Human Kinetics. (2012) ; 31: (-1). |




