Comparison of attitudes and beliefs of physical therapists and primary care physicians regarding low back pain management: A cross-sectional study
Abstract
BACKGROUND:
The first-line contact for patients seeking care for low back pain (LBP) can potentially change the disease course. The beliefs and attitudes of healthcare providers (HCPs) can influence LBP management. Although referring patients with LBP to physical therapy is common, the first-line contact for patients with LBP in Saudi Arabia is the primary care physician (PCP). Physical therapy will soon be integrated into primary care; therefore, it is rational to compare physical therapists’ (PTs) beliefs and attitudes regarding LBP with those of PCPs.
OBJECTIVE:
We compared PCPs’ and PTs’ attitudes and beliefs regarding LBP management.
METHODS:
We employed a cross-sectional, voluntary response sample research design using the Pain Attitudes and Beliefs Scale (PABS). Participants were PTs and PCPs practicing in Saudi Arabia.
RESULTS:
In total, 153 participants completed the PABS (111 PTs and 52 PCPs). PCPs demonstrated significantly higher PABS biomedical subscale scores than did the PTs.
CONCLUSIONS:
HCPs in Saudi Arabia should receive additional training to adopt a biopsychosocial approach to managing LBP. In this study, the HCPs’ treatment recommendations may not correspond with contemporary clinical guidelines. Research to facilitate the implementation of optimal professional education and training to adopt a biopsychosocial approach is an urgent priority.
1.Introduction
Low back pain (LBP) is considered a major musculoskeletal health issue [1] and is one of the most common causes of disability, causing substantial socioeconomic burden worldwide [2]. In Saudi Arabia, LBP is the most commonly reported type of pain, with an overall lifetime prevalence between 63.8% and 89% [3]. Chronic LBP, defined as persistent pain in the lower back for more than three months, was the second most common site of pain after lower extremities in patients with chronic pain (
Although multiple factors can influence the chronicity of LBP, the psychosocial profile of the patient has been reported to be a critical prognostic factor for pain persistence, response to treatment and rehabilitation, and the likelihood of developing disability [5]. Several studies have focused on analyzing the potential link between psychosocial factors, such as catastrophizing, fear avoidance, and the treatment response in patients with chronic LBP, and this topic has been a popular area of research over the past few years [5, 6].
The beliefs and attitudes of healthcare providers (HCPs) can significantly influence their clinical deci-sion-making and the psychosocial status of their patients [7, 8, 9, 10]. All clinical guidelines on LBP are in agreement that HCPs should have a broad psychosocial perspective; however, studies show that the actual beliefs and attitudes of HCPs vary between biomedical or biopsychosocial frameworks [7, 10, 11, 12, 13].
Attitudes and beliefs can influence the extent to which HCPs adhere to the clinical guidelines for managing LBP. For instance, those who focus on biomedical management and have fear-avoidance beliefs themselves have been shown to display suboptimal adherence to LBP guidelines [12]. Further reasons for lack of guideline adherence include a lack of biopsychosocial knowledge, the belief that they are not sufficiently qualified to adapt their practice to a biopsychosocial approach, and patient demands to define pain biomedically; for instance, by imaging [11, 13]. Several measures can be used to assess the attitudes and beliefs of HCPs concerning LBP. Bishop et al. [8] highlighted the Pain Attitudes and Beliefs Scale (PABS) as a reliable and feasible measure to evaluate the attitudes and beliefs of HCPs regarding LBP management.
There is ample evidence supporting the early management of LBP in primary care practice and the use of nonpharmacologic treatments while discouraging medication and imaging for LBP [14, 15, 16, 17]. In Saudi Arabia, physical therapy services are not available in primary care centers yet and are offered only at secondary level centers based on specialist referrals [18].
However, there is an agreement among patients and stakeholders that physical therapy services are best suited to the primary care setting [19, 20] and physical therapy will soon be integrated into the primary care setting. Moreover, various studies from different countries have demonstrated successful implementation of physical therapy at the first point of contact for patients with musculoskeletal conditions [21, 22, 23]. The biopsychosocial and biomedical orientations toward LBP appeared to be low among physiotherapists according to a recent study [24]. A stronger orientation toward biopsychosocial beliefs and attitudes regarding LBP management was associated with a better selection of guideline-based physiotherapy interventions [24]. Multiple publications have indicated a profound biomedical orientation and low adherence to LBP guidelines among PCPs internationally [12, 25, 26]. However, there are no studies exploring the beliefs and attitudes of PCPs regarding LBP in Saudi Arabia.
We hypothesized that PCPs in Saudi Arabia might demonstrate a higher biomedical orientation than PTs; however, both may demonstrate low biopsychosocial orientation. Similarly, we hypothesized that a negative association may be found between the two orientations – biomedical and biopsychosocial – in general, regardless of the study sample. Hence, we aimed to compare the beliefs and attitudes of PCPs and PTs in Saudi Arabia regarding LBP management.
2.Methods
We used a cross-sectional, voluntary response sample design to examine the attitudes and beliefs of PCPs and PTs regarding LBP management in Saudi Arabia. This study was approved by the Institutional Review Board of the Ministry of Health (IRB# 2019-0060 E). Each participant provided a signed informed consent form prior to participation. We targeted PCPs and PTs in Saudi Arabia whose clinical practice frequently involved treating patients with LBP, and this was an introductory question in the invitation that was sent to them.
2.1Primary care physician sampling
An invitation for PCPs to participate in the study was sent via email to all 400 primary care centers in the Riyadh region, in which, there are 288 currently practicing PCPs. Notably, rural primary care centers service patients two to three days a week.
Riyadh region’s primary care centers account for 20% of all primary centers in Saudi Arabia [27]. Additionally, the capital city of Riyadh encompasses more than 22% of the country’s medical facilities that include more than five tertiary care centers in which patients seek care from around the country [27].
2.2Physiotherapist sampling
As physiotherapy services are not available in primary care centers, PTs were recruited via a web-based survey that was distributed through various social media channels and email.
2.3Self-administered survey
Once the respondents agreed to participate, they were able to access an online survey using a link provided in the email. This survey comprised two sections: the first section collected demographic data, including age (categorical variable), sex, and years of experience, and the second section used the PABS to assess the respondents’ treatment orientation (biomedical or biopsychosocial) toward LBP. The PABS is a 19-item self-administered questionnaire that examines the strength of the two treatment orientations toward LBP: biomedical (10 items) and behavioral (9 items) [8]. Each item is rated on a 6-point Likert scale (“totally disagree”
The test re-test reliability of the PABS was good, with intraclass correlation coefficients for the biomedical scale ranging from 0.73 to 0.81, and 0.65 to 0.82 for the biopsychosocial scale [28]. Additionally. construct validity was confirmed to a two-factor structure using exploratory factor analysis [28, 29]
2.4Data analysis
The analyses were performed using the Statistical Package for the Social Sciences (SPSS, Version 25). The level of significance was set at
3.Results
The invitation link was visited by 72 PCPs, suggesting a response rate of 58%. Nonetheless, because we used multiple recruitments platforms to invite PTs, the response rate might be difficult to estimate. In total, 153 participants (111 PTs and 42 PCPs) completed the survey. The demographic data of the PTs and PCPs are shown in Table 1. The PT sample was similar to the PCP sample with respect to sex. However, the PCP group was older in age and had more clinical experience than the PT group [
Table 1
Personal and professional characteristics of physical therapists and primary care physicians
| PCP | PT | |||
|---|---|---|---|---|
|
| % |
| % | |
| Sex | ||||
| Male | 24 | 60 | 65 | 58.6 |
| Female | 16 | 40 | 46 | 41.4 |
| Age (in years) | ||||
| 20–30 | 6 | 15 | 51 | 45.9 |
| 31–35 | 12 | 30 | 25 | 22.5 |
| 36–40 | 7 | 17.5 | 23 | 20.7 |
| 41–45 | 5 | 12.5 | 4 | 3.6 |
| 46–50 | 2 | 5 | 7 | 6.3 |
| | 8 | 20 | 1 | 0.9 |
| Level of education | ||||
| Bachelor of science | 57 | 51.4 | ||
| Master of science | 34 | 30.6 | ||
| Doctoral degree holder | 16 | 14.4 | ||
| Doctor of physical therapy | 4 | 3.6 | ||
| Current qualification | ||||
| General practitioner | 27 | 67.5 | ||
| Family medicine physician | 10 | 25 | ||
| Other | 3 | 7.5 | ||
| Years of experience | ||||
| | 6 | 15 | 27 | 24.3 |
| 2–5 | 13 | 32.5 | 28 | 25.2 |
| 6–10 | 8 | 20 | 18 | 16.2 |
| 11–15 | 1 | 2.5 | 26 | 23.4 |
| 16–20 | 4 | 10 | 4 | 3.6 |
| | 8 | 20 | 8 | 7.2 |
| Province or region of practice | ||||
| Central region (Riyadh) | 37 | 92.5 | 57 | 51.4 |
| Central region (out of Riyadh) | 3 | 7.5 | 11 | 9.9 |
| Northern region | 3 | 2.7 | ||
| Western region | 19 | 17.1 | ||
| Eastern region | 10 | 9.0 | ||
| Southern region | 11 | 9.9 | ||
| Nationality | ||||
| Saudi | 17 | 42.5 | 104 | 93.7 |
| Non-Saudi | 23 | 57.5 | 7 | 6.3 |
PCP: primary care physician, PT: physical therapist.
3.1Pain attitudes and beliefs scale
The means and SDs of the PABS for PTs and PCPs are presented in Table 2. PCPs had significantly higher PABS biomedical subscale scores (Mdn
Table 2
Pain Attitudes and Beliefs Scale descriptive statistics
| PCP | PT | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| PABS | ||||
| Biomedical subscale | 36.5 | 7.8 | 32.7 | 9.1 |
| Behavioral subscale | 31.5 | 7.2 | 32.3 | 7.8 |
PCP: primary care physician, PT: physical therapist, SD: standard deviation, PABS: pain Attitudes and Beliefs Scale.
Figure 1.
The relationship between the two Pain Attitudes and Beliefs subscale scores in the physical therapy sample.
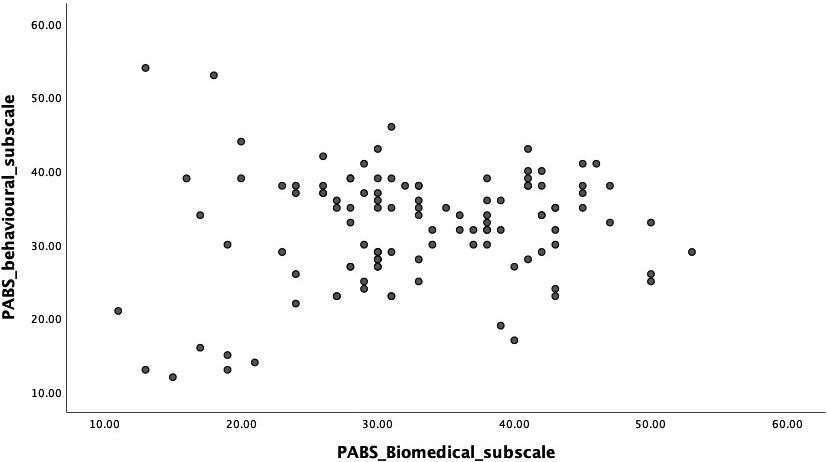
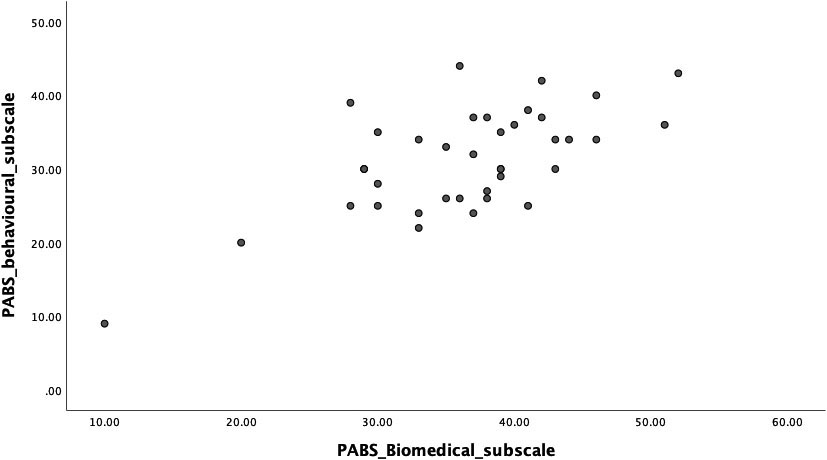
The correlation between the two PABS subscale scores was not significant (
A comparison between the two samples for each of the 19 PABS items is shown in Supplementary Figures S1 to S19.
Figure 2.
The relationship between the two Pain Attitudes and Beliefs subscale scores in the primary care physician sample.
4.Discussion
In this study, the PABS was used to compare the attitudes and beliefs of PTs and PCPs in Saudi Arabia regarding LBP management. We found that the total scores on the biomedical and behavioral subscales among the PTs were remarkably close (32.7
Additionally, the results showed that the biomedical score was significantly higher among PCPs than PTs. PTs appear to hold a stronger opinion than PCPs regarding the point that patients with severe back pain would benefit from physical exercise. This is comparable to the findings of a previous study involving Dutch PTs [30]. In contrast, PCPs appear to hold the opinion that patients with back pain should preferably practice only pain-free movements. This corresponds to previous studies, which state that a stronger biomedical orientation among HCPs is associated with higher overall disagreement with the reported recommendations to return to usual activity or work [7, 28, 32]. These reported beliefs among PCPs might reflect fear and are contradictory to the recent recommendations for LBP management that encourage providing clear information on continuation of activities, even if there is some pain [33, 34].
Evidence has shown that HCPs who embrace more biomedical than behavioral beliefs regarding the underlying cause and mechanism of LBP may perceive daily activities as more harmful [7, 10]. Consequently, they are more likely to recommend that their patients limit their daily activity levels and avoid returning to work [9, 10]. This may lead to the patient developing unhelpful beliefs, avoiding activities perceived to be damaging, restricting social participation, and contributing to greater levels of disability [12, 24, 25, 26, 35]. Our results are consistent with the findings of a study in the United Kingdom, which reported that 28% of HCPs would recommend patients with LBP to remain off work, and this advice was significantly related to a higher biomedical score in the PABS [36]. However, further research is required to examine the association between advice based on such beliefs and development of subsequent beliefs and behaviors in Saudi individuals with LBP.
4.1Clinical implications
Overall, the findings of this study suggest that more training should be given to HCPs in Saudi Arabia to adopt a biopsychosocial approach to manage LBP. This is important because LBP is a multifactorial health condition that can be influenced by various biological and psychosocial risk factors [5, 37, 31, 38]. Similarly, disability related to LBP is known to be influenced by factors from different domains, including individual (e.g., age) and psychological (e.g., psychological distress and pain-related fear) factors, in the Saudi population [33, 34]. In addition, there is robust evidence suggesting that the attitudes and beliefs of patients regarding LBP are influenced by the attitudes and beliefs of HCPs [7, 8, 9, 10] as well as other factors, including painful past experiences [39, 40].
4.2Limitations
The study results should be considered within some limitations. First, we sought to reach a representative sample of both PCPs and PTs; however, the number of samples collected in this study may limit the generalizability of the findings. Therefore, further research may be needed. Second, the beliefs and attitudes of HCPs in this study were measured using a self-reported survey, which raises the possibility that the results may reflect an individual propensity to select the behavioral approach. Third, selection bias might have occurred because the study included a higher number of PTs than PCPs, limiting the ability to explore differences between the two research groups. Moreover, all the PCPs and most PTs were from Riyadh which also might have introduced selection bias. Nonetheless, Riyadh is the capital city of Saudi Arabia and is composed of diverse HCPs coming from different regions and backgrounds. Finally, the study was conducted as a convenience sample, which may need further evaluation with a probability population to generalize outcomes to a broader population.
5.Conclusions
Our results showed ambiguous orientation among PTs, and stronger biomedical orientation among PCPs than PTs. Beliefs regarding treatment recommendations among the participants did not correspond to the clinical guidelines for LBP management. This may negatively influence the attitudes and beliefs of patients and might contribute to unfavorable outcomes in individuals with LBP. This uncertainty and stronger biomedical orientation among participants may have a negative influence on patients’ attitudes and beliefs, thus contributing to the burden related to LBP.
Acknowledgments
This project was supported by the Deanship of Scientific Research at Prince Sattam Bin Abdulaziz University under the research project No: 2019/01/13195. The authors are immensely grateful to the participants of this study.
Conflict of interest
None to report.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-200295.
References
[1] | Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. (2014) ; 73: (6): 968-74. doi: 10.1136/annrheumdis-2013-204428. |
[2] | Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. (2008) ; 8: (1): 8-20. doi: 10.1016/j.spinee.2007.10.005. |
[3] | Aldera MA, Alexander CM, McGregor AH. Prevalence and incidence of low back pain in the Kingdom of Saudi Arabia: A systematic review. J Epidemiol Glob Health. (2020) ; 10: (4): 269-75. doi: 10.2991/jegh.k.200417.001. |
[4] | Almalki MT, BinBaz SS, Alamri SS, Alghamdi HH, EL-Kabbani AO, Al Mulhem AA, et al. Prevalence of chronic pain and high-impact chronic pain in Saudi Arabia. Saudi Med J. (2019) ; 40: (12): 1256-66. doi: 10.15537/smj.2019.12.24690. |
[5] | Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). (2002) ; 27: (5): E109-20. doi: 10.1097/00007632-200203010-00017. |
[6] | Gheldof EL, Crombez G, Van Den Bussche E, Vinck J, Van Nieuwenhuyse A, Moens G, et al. Pain-related fear predicts disability, but not pain severity: A path analytic approach of the fear-avoidance model. Eur J Pain. (2010) ; 14: (8): 870.e1-9. doi: 10.1016/j.ejpain.2010.01.003. |
[7] | Houben RM, Ostelo RW, Vlaeyen JW, Wolters PM, Peters M, Stomp-van den Berg SG. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. (2005) ; 9: (2): 173-83. doi: 10.1016/j.ejpain.2004.05.002. |
[8] | Bishop A, Thomas E, Foster NE. Health care practitioners’ attitudes and beliefs about low back pain: A systematic search and critical review of available measurement tools. Pain. (2007) ; 132: (1-2): 91-101. doi: 10.1016/j.pain.2007.01.028. |
[9] | Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: A systematic review. Eur J Pain. (2012) ; 16: (1): 3-17. doi: 10.1016/j.ejpain.2011.06.006. |
[10] | Gardner T, Refshauge K, Smith L, McAuley J, Hübscher M, Goodall S. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: A systematic review of quantitative and qualitative studies. J Physiother. (2017) ; 63: (3): 132-43. doi: 10.1016/j.jphys.2017.05.017. |
[11] | Schers H, Wensing M, Huijsmans Z, van Tulder M, Grol R. Implementation barriers for general practice guidelines on low back pain: A qualitative study. Spine (Phila Pa 1976). (2001) ; 26: (15): E348-53. doi: 10.1097/00007632-200108010-00013. |
[12] | Corbett M, Foster N, Ong BN. GP attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract. (2009) ; 26: (5): 359-64. doi: 10.1093/fampra/cmp042. |
[13] | Sanders T, Ong NB, Sowden G, Foster N. Implementing change in physiotherapy: Professions, contexts and interventions. J Health Org Manag. (2014) ; 28: (1): 96-114. doi: 10.1108/JHOM-10-2011-0102. |
[14] | Fritz JM, Brennan GP, Hunter SJ, Magel JS. Initial management decisions after a new consultation for low back pain: Implications of the usage of physical therapy for subsequent health care costs and utilization. Arch Phys Med Rehabil. (2013) ; 94: (5): 808-16. doi: 10.1016/j.apmr.2013.01.008. |
[15] | Frogner BK, Harwood K, Andrilla CH, Schwartz M, Pines JM. Physical therapy as the first point of care to treat low back pain: An instrumental variables approach to estimate impact on opioid prescription, health care utilization, and costs. Health Serv Res. (2018) ; 53: (6): 4629-46. doi: 10.1111/1475-6773.12984. |
[16] | Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al.. What low back pain is and why we need to pay attention. Lancet. (2018) ; 391: (10137): 2356-67. doi: 10.1016/S0140-6736(18)30480-X. |
[17] | Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. (2018) ; 27: (1): 60-75. doi: 10.1007/s00586-017-5099-2. |
[18] | Al-Ahmadi H, Roland M. Quality of primary health care in Saudi Arabia: A comprehensive review. Int J Qual Health Care. (2005) ; 17: (4): 331-46. doi: 10.1093/intqhc/mzi046. |
[19] | Al-Abbad HM, Al-Haidary HM. The perception of physical therapy leaders in Saudi Arabia regarding physical therapy scope of practice in primary health care. J Phys Ther Sci. (2016) ; 28: (1): 112-7. doi: 10.1589/jpts.28.112. |
[20] | Al-Abbad HM, Madi S. Perception of tertiary care clients toward the availability of physical therapy service at primary health care centers in Saudi Arabia: A cross-sectional survey. J Phys Ther Sci. (2020) ; 32: (5): 323-31. doi: 10.1589/jpts.32.323. |
[21] | François D, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advanced practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskelet Disord. (2012) ; 13: : 107. doi: 10.1186/1471-2474-13-107. |
[22] | Bornhöft L, Larsson ME, Thorn J. Physiotherapy in primary care triage-the effects on utilization of medical services at primary health care clinics by patients and sub-groups of patients with musculoskeletal disorders: A case-control study. Physiother Theory Pract. (2015) ; 31: (1): 45-52. doi: 10.3109/09593985.2014.932035. |
[23] | Downie F, McRitchie C, Monteith W, Turner H. Physiotherapist as an alternative to a GP for musculoskeletal conditions: A 2-year service evaluation of UK primary care data. Br J Gen Pract. (2019) ; 69: (682): e314-20. doi: 10.3399/bjgp19X702245. |
[24] | Alshehri MA, Alzahrani H, Alotaibi M, Alhowimel A, Khoja O. Physiotherapists’ pain attitudes and beliefs towards chronic low back pain and their association with treatment selection: A cross-sectional study. BMJ Open. (2020) ; 10: (6): e037159. doi: 10.1136/bmjopen-2020-037159. |
[25] | Fullen BM, Baxter GD, Doody C, Daly LE, Hurley DA. General practitioners’ attitudes and beliefs regarding the management of chronic low back pain in Ireland: A cross-sectional national survey. Clin J Pain. (2011) ; 27: (6): 542-9. doi: 10.1097/AJP.0b013e31821771e2. |
[26] | Epstein-Sher S, Jaffe DH, Lahad A. Are they complying? Physicians’ knowledge, attitudes, and readiness to change regarding low back pain treatment guideline adherence. Spine. (2017) ; 42: (4): 247-52. doi: 10.1097/BRS.0000000000001714. |
[27] | Hospitals Hospital Beds. [Internet] Saudi Arabia: 2021. [cited 11 February 2021]. Available from: https//www.moh.gov.sa/en/Ministry/Statistics/book/Documents/1433.pdf. |
[28] | Eland ND, Kvåle A, Ostelo RWJG, Strand LI. The Pain Attitudes and Beliefs Scale for physiotherapists: Dimensionality and internal consistency of the Norwegian version. Physiother Res Int. (2017) ; 22: (4). doi: 10.1002/pri.1670. |
[29] | Mutsaers JH, Peters R, Pool-Goudzwaard AL, Koes BW, Verhagen AP. Psychometric properties of the Pain Attitudes and Beliefs Scale for Physiotherapists: a systematic review. Man Ther. (2012) ; 17: (3): 213-8. doi: 10.1016/j.math.2011.12.010. |
[30] | Bunzli S, Smith A, Schütze R, O’Sullivan P. Beliefs underlying pain-related fear and how they evolve: A qualitative investigation in people with chronic back pain and high pain-related fear. BMJ Open. (2015) ; 5: (10): e008847. doi: 10.1136/bmjopen-2015-008847. |
[31] | Jensen MP, Romano JM, Turner JA, Good AB, Wald LH. Patient beliefs predict patient functioning: Further support for a cognitive-behavioural model of chronic pain. Pain. (1999) ; 81: (1-2): 95-104. doi: 10.1016/s0304-3959(99)00005-6. |
[32] | Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: Are we fear-avoidant? J Occup Rehabil. (2002) ; 12: (4): 223-32. doi: 10.1023/a1020218422974. |
[33] | Alamam D, Moloney N, Leaver A, Alsobayel HI, Mackey MG. Pain intensity and fear avoidance explain disability related to chronic low back pain in a Saudi Arabian population. Spine J. (2019) ; 44: (15): E889-98. doi: 10.1097/BRS.0000000000003002. |
[34] | Alamam DM, Moloney N, Leaver A, Alsobayel HI, Mackey MG. Multidimensional prognostic factors for chronic low back pain-related disability: A longitudinal study in a Saudi population. Spine J. (2019) ; 19: (9): 1548-58. doi: 10.1016/j.spinee.2019.05.010. |
[35] | Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. (1993) ; 52: (2): 157-68. doi: 10.1016/0304-3959(93)90127-b. |
[36] | Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain. (1999) ; 80: (1): 329-39. doi: 10.1016/s0304-3959(98)00229-2. |
[37] | Bishop A, Foster NE, Thomas E, Hay ME. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. (2008) ; 135: (1-2): 187-95. doi: 10.1016/j.pain.2007.11.010. |
[38] | Vlaeyen JW, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. (2016) ; 157: (8): 1588-9. doi: 10.1097/j.pain.0000000000000574. |
[39] | Alshami A. Physical and psychological aspects of low back pain among Saudi patients: A case-control study. Saudi J Med Sci. (2014) ; 2: (1): 24-9. doi: 10.4103/1658-631X.128407. |
[40] | Buragadda S, Aleisa ES, Melam GR. Fear avoidance beliefs and disability among women with low back pain. Neuropsychiatry (London). (2018) ; 8: (1): 73-9. doi: 10.4172/Neuropsychiatry.1000326. |




