Medial femoral plate with cannulated screw for Pauwels type III femoral neck fracture: A meta-analysis
Abstract
BACKGROUND:
Femoral neck fractures often occur in the elderly, which usually results in hip pain.
OBJECTIVE:
The purpose of this study was to evaluate the difference in the treatment of Pauwels type III femoral neck fractures with medial femoral support plate combined with cannulated screws and cannulated screws alone.
METHODS:
PubMed, ScienceDirect, China Academic Journals Full-text Database (CNKI), Wanfang Database, Chinese Biomedical Literature Database (CBM), Embase and Cochrane Library were used to collect clinical controlled trials of the medial femoral support plate combined with hollow screw internal fixation and simple hollow screw internal fixation for Pauwels type III femoral neck fracture.
RESULTS:
Seven articles (
CONCLUSION:
Medial femoral plate combined with cannulated screw for Pauwels type III femoral neck fracture can shorten healing time, reduce postoperative complications, and improve the postoperative Harris score.
1.Introduction
Femoral neck fractures often occur in the elderly, which usually results in hip pain [1, 2, 3]. In recent years, with the intensification of the population aging process, its incidence rate has been increasing year by year, accounting for about 3.58% of systemic fractures and 54% of hip fractures [4, 5]. Good reduction and fixation is an important principle for the treatment of femoral neck fractures, and also a basic guarantee to promote patient rehabilitation and joint function recovery [6]. To improve the effect of internal fixation of femoral neck fracture cannulated nails, Filipov reported an F-shaped spatial layout method for internal fixation of femoral neck fracture cannulated nails [7]. In this method, three hollow nails are distributed in an F shape on the femoral neck and the coronal plane of the proximal femur.
The focus of the Pauwels classification of femoral neck fractures is on mechanical angles [8, 9]. When the cutting fracture line is 50
Some studies suggest that this type of fracture is treated by using a nail plate system. Hollow nails and medial support plates are an emerging treatment method that can be used to treat Pauwels type III femoral neck fractures [13, 14, 15]. At present, a medial femoral neck support plate combined with hollow screw internal fixation is an emerging treatment of Pauwels type III femoral neck fracture in clinical practice [16, 17]. However, whether it can accelerate fracture healing and reduce femoral head necrosis is still controversial. Therefore, relevant clinical trials were retrieved for meta-analysis to provide a scientific basis for Pauwels type III femoral neck fractures.
2.Materials and methods
2.1Search strategy
The following keywords were used for the search: “Pauwels III femoral neck fractures”, “Inner support plate”, “Medial support plate”, “Buttress plate”, and “Cannulated compression screws”. PubMed, ScienceDirect, China Academic Journals Full-text Database (CNKI), Wanfang Database, Chinese Biomedical Literature Database (CBM), Embase and Cochrane Library were used to collect clinical controlled trials of medial femoral support plates combined with hollow screw internal fixation and simple hollow screw internal fixation for Pauwels type III femoral neck fracture. The study was conducted in January 2020 and included literature up to December 2019. There was no limit on the language of document retrieval. In addition, the references of related articles were also searched, and supplemented by a manual search and download of related documents.
2.2Inclusion and exclusion criteria
2.2.1Inclusion criteria
Pauwels type III femoral neck fracture. The experimental group used a medial femoral neck support plate combined with hollow screw internal fixation, and the control group used simple hollow screw internal fixation for clinical trials. Outcome indicators included a Harris score of at least one, operation time, intraoperative blood loss, postoperative complications, fracture reduction quality, and hip joint function excellent rate. All patients were followed up.
2.2.2Exclusion criteria
Non-Pauwels type III femoral neck fractures, animal experiments, missing data, and repeated literature.
2.3Literature screening and quality evaluation
Two researchers independently used the established inclusion and exclusion criteria to conduct a literature search and screening. After the screening was completed, the results were compared and analyzed. If there were any objections, they were discussed with senior authors. Finally, the literature was incorporated and data was extracted. Two reviewers independently evaluated the included literature, and if there were disagreements, they discussed them with the senior authors to re-evaluate the quality of the literature. The randomized controlled trials were strictly carried out in terms of risk assessment of bias according to the Cochrane Bias Risk Assessment Manual. The improved Jadad scale was used to evaluate the quality of the literature. The full score was 7 points, of which 1–3 were low-quality literature and 4–7 were high-quality literature. The retrospective cohort study used the risk of bias in non-randomized studies of interventions (ROBINS-I) to evaluate the quality of the literature. The final result was scored according to the correlation with the overall risk bias (low, moderate, severe, extremely severe, and no information).
Table 1
General characteristics of the included studies
| Study | Year of publication | Study type | Follow-up time (months) | Jadad score | Experimental group | Control group | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | Age, years (mean | Male ( | Sample size | Age, years (mean | Male ( | |||||
| Ding WX, 2018 [21] | 2018 | Randomized controlled study | 12 | 2 | 12 | NA | 8 | 14 | NA | 8 |
| Li P, 2018 [22] | 2018 | Randomized controlled study | 3 | 4 | 31 | 45.56 | 16 | 31 | 43.32 | 19 |
| Li RH, 2018 [20] | 2018 | Retrospective cohort study | 12–15 | 2 | 20 | NA | NA | 30 | NA | NA |
| Qin YP, 2018 [19] | 2018 | Randomized controlled study | 12–18 | 4 | 30 | NA | NA | 30 | NA | NA |
| Shen DH, 2019 [23] | 2019 | Randomized controlled study | 6 | 2 | 35 | 38.82 | 19 | 35 | 38.86 | 21 |
| Xu YK, 2018 [18] | 2018 | Randomized controlled study | 12 | 2 | 25 | 50.4 | 19 | 20 | 49.9 | 15 |
| Yang B, 2019 [16] | 2019 | Randomized controlled study | 12 | 2 | 49 | 37.86 | 35 | 47 | 38.05 | 32 |
2.4Statistical analysis
RevMan 5.3 software was used to perform the meta-analysis on the collected relevant data. Binary variables used were odd ratio (OR) and 95% confidential interval (CI) for data analysis, and continuous variables used were mean difference (MD) and 95% CI for data analysis. When performing the heterogeneity analysis, when I
3.Results
3.1Literature search results and basic features
Among the 473 retrieved documents, 458 irrelevant or duplicate documents were excluded. Finally, seven articles were evaluated for quality and included in the meta-analysis [16, 18, 19, 20, 21, 22, 23], including six randomized controlled trials and one retrospective cohort study. The flow diagram of the included studies is shown in Fig. 1. A total of 409 patients with Pauwels type III femoral neck fractures were included. The Jadad scores included in the literature were all two or above. The follow-up time of the participants was 3–18 months. The basic characteristics of the included studies are shown in Table 1.
Figure 1.
Flow diagram of the included studies.
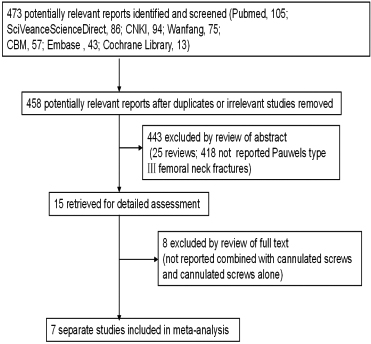
Figure 2.
Forest plot of the operation time.
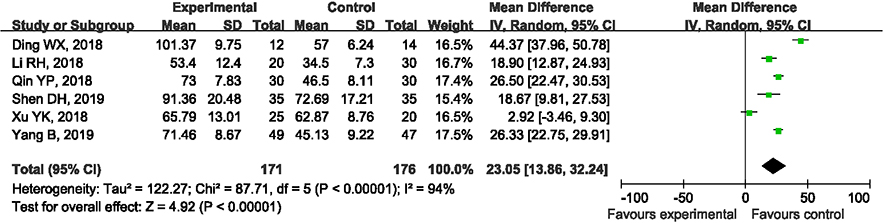
Figure 3.
Forest plot of the bleeding volume.
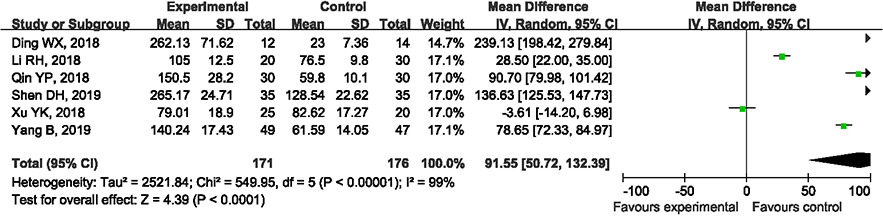
Figure 4.
Forest plot of the healing time.
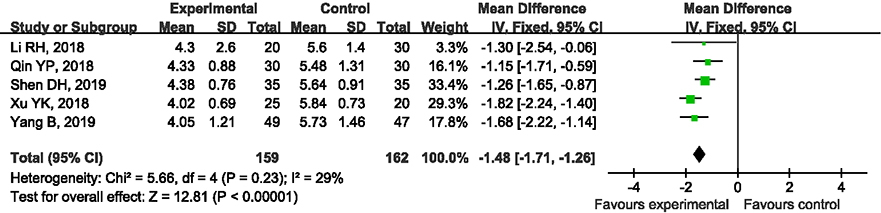
Figure 5.
Forest plot of the complication.
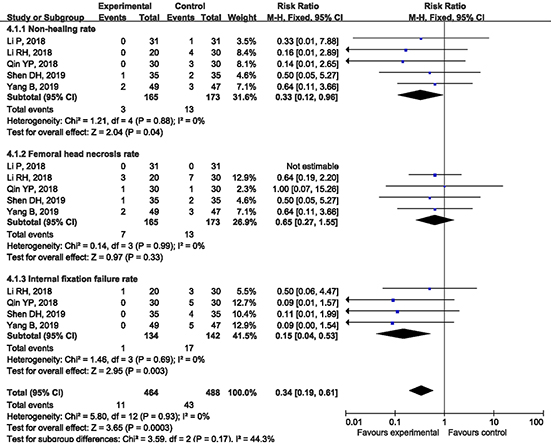
Figure 6.
Forest plot of the xcellent rate.
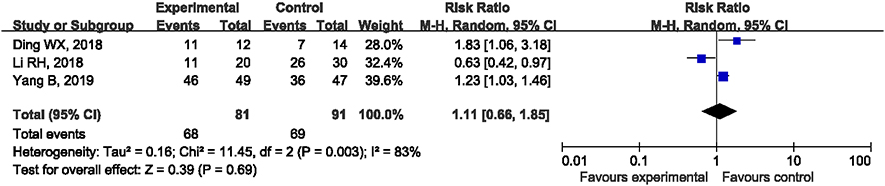
Figure 7.
Forest plot of the VAS score.
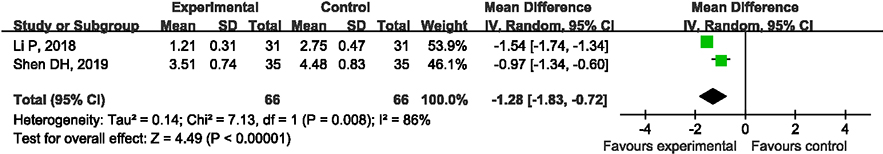
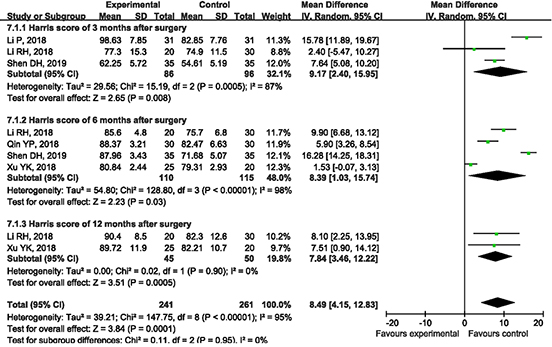
Figure 8.
Forest plot of the Harris score.
3.2Comparison of operation time between the groups
Six articles compared the operation time between the two treatment methods. After analysis, there was a large heterogeneity between the research results (I
3.3Comparison of intraoperative blood loss between the groups
Six articles compared intraoperative blood loss between the two treatment methods. After analyzing the heterogeneity in the results of various studies (I
3.4Comparison of fracture healing time between the groups
Five articles compared the fracture healing time between the two treatment methods. The heterogeneity between the results of the various studies was small (I
3.5Subgroup analysis of complication rate
Five articles compared the incidence of complications between the two treatments. Postoperative complications include fracture nonunion rate, femoral head necrosis rate, and internal fixation failure rate. A subgroup analysis was performed on each group of data to determine the incidence of complications. After analysis, the heterogeneity between the results of the various studies was small (I
3.6Comparison of excellent rate of hip joint function between the two groups of patients
The three included articles compared the excellent rate of hip joint function with two treatment methods. After analyzing the heterogeneity in the results of various studies (I
3.7Comparison of VAS scores between the two groups of patients
The two included articles compared the VAS scores of the two groups of patients after treatment. After analyzing the heterogeneity in the results of various studies (I
3.8Subgroup analysis of the Harris score
The five included articles carried out the Harris scoring of the hips at different times for the two treatment methods, so a subgroup analysis was used to conduct a comprehensive analysis of the Harris scoring. After the analysis, the heterogeneity between the results of the various studies was relatively large (I
4.Discussion
Pauwels type III fracture is a vertical fracture of the femoral neck, which occurs after high-energy trauma, especially in the middle-aged population [15, 24, 25, 26, 27]. This type of fracture is dominated by shear force, which causes the proximal femur to shift and collapse during varus and is prone to internal fixation failure and other complications [28]. In recent years, the use of medial femoral neck support plate combined with cannulated screw internal fixation has been proposed for the treatment of Pauwels type III femoral neck fracture [16, 29, 30], which can reduce the incidence of complications, such as nonunion of femoral neck fracture and femoral head necrosis.
Femoral neck fractures are common and serious types of fractures in the clinic, which yields extremely high disability and mortality rates [31, 32]. Femoral neck fractures should be treated in a timely manner after proper evaluation of the condition. If it can be effectively reset, internal fixation is the first choice. Pauwels type III femoral neck fracture is a clinically refractory fracture type because of its vertical fracture line and the need to withstand huge shear stress, which can cause high-risk complications, such as broken nails and retracted nails after clinical treatment of hollow nails [23, 33]. Nevertheless, from the perspective of biomechanics, its inverted triangular structure can withstand the tensile stress of the fracture and effectively resist the torsional force. It can also produce a compression effect on the fracture site, so it has a certain therapeutic effect. The hollow nail plus the inner support steel plate is a combination of three hollow nails and the steel plate to form an integral fixture. It is not easy to withdraw the nail and is fixed firmly, and will achieve good therapeutic effects. The steel plate combined with the hollow screw is fixed on the basis of the conventional hollow screw and the support plate is placed on the inner side of the femoral neck. It not only retains the good anti-rotation ability of the internal fixation of the hollow screw, but also directly resists the shear force generated by the fracture end.
The results of this study show that, in terms of fracture healing and the incidence of complications, the medial support plate can resist the shear force of the fracture and increase the stability of the internal fixation nail, which can reduce postoperative complications and promote fracture healing. For the postoperative complications of patients, some studies indicate that the surgical method supported by the medial plate not only increases the amount of intraoperative bleeding, but may also damage the blood supply of the femoral neck and femoral head, increasing the risk of postoperative fracture necrosis. The blood supply of the femoral head and neck is mainly provided by the medial femoral artery, which is distributed on the posterior side of the femoral neck. The upper support belt artery of the terminal branch of the internal circumflex femoral artery is divided into the upper lateral and the lower support belt artery is divided into the lower medial. Both through the support belt and reach the head and neck of the femur. In addition, the lateral femoral artery provides blood supply of 20–30% of the femoral head and neck, mainly reaching the femoral neck from the anterior side of the femoral neck. Therefore, placing a support plate on the anterior medial side of the femoral neck during surgery will not damage the main blood supply source of the medial femoral artery. Clinical studies have reported that the blood circulation of the femoral neck will not increase the damage due to the medial support plate, and will not increase the incidence of fracture nonunion, internal fixation failure and ischemic necrosis [34, 35, 36].
In terms of the operation time and the amount of bleeding, the internal support steel plate needs to be cut for treatment [37]. The internal fixation of hollow nails is generally closed reduction and internal fixation, so simple hollow nails have advantages in operation time and bleeding volume [38, 39]. Therefore, older patients who cannot tolerate long-term surgery and large bleeding should consider internal fixation with hollow nails. In terms of the Harris score, the score of the test group was higher than that of the control group at three, six, and 12 months after surgery. For the recovery of long-term hip function, the included literature did not follow up for a long time, so more clinical long-term follow-up trials are needed to compare the differences in long-term efficacy of the two groups.
The results of this study suggest that there is no statistical difference between the two groups in terms of the excellent rate of hip function. Due to the difference in the evaluation methods used for the excellent rate of hip joint function between the two groups, there is a large heterogeneity between the two groups and there is no statistically significant difference between the groups. However, because of the different surgical methods used in the two groups, the medial support uses open reduction internal fixation, and the hollow screw internal fixation mostly uses closed reduction internal fixation [40].
4.1Limitations
There are some limitations in this study. First, seven clinical trials were included, with a total of 409 patients. The small number of clinically relevant studies led to limitations in clinical promotion. Second, the evaluation indicators included in the literature are heterogeneous and have a certain influence on the analysis results. They may be derived from the length of time from injury to operation in different literature, the choice of internal fixation plate, and the method of the surgical approach and reduction of different physicians have an impact on the test results.
5.Conclusion
In conclusion, the medial femoral neck support plate combined with cannulated screw internal fixation for Pauwels type III femoral neck fracture has a low complication rate and better recovery of hip function, but it will increase operation time and intraoperative bleeding. In the treatment of Pauwels type III femoral neck fractures, hollow nails combined with medial support plates have advantages over pure hollow nails in terms of healing time, postoperative complications, postoperative VAS score and Harris score, and have a good clinical application prospect. However, more high-quality and multi-center experiments are needed for in-depth research.
Conflict of interest
None to report.
References
[1] | Koldaas MIB, Pedersen JN, Hojsager FD, Palm H, Viberg B. Implant positioning (IMPO) in undisplaced femoral neck fractures: association to reoperation and development of an IMPO scoring system. Injury (2020) ; 51: (2): 372-379. |
[2] | Slobogean GP, Sprague S, Bzovsky S, Heels-Ansdell D, Thabane L, Scott T, et al. Fixation using alternative implants for the treatment of hip fractures (FAITH-2): design and rationale for a pilot multi-centre 2 × 2 factorial randomized controlled trial in young femoral neck fracture patients. Pilot and Feasibility Stud (2019) ; 5: : 70. |
[3] | Higashikawa T, Shigemoto K, Goshima K, Usuda D, Okuro M, Moriyama M, et al. Urinary retention as a postoperative complication associated with functional decline in elderly female patients with femoral neck and trochanteric fractures: a retrospective study of a patient cohort. Medicine (2019) ; 98: (24): e16023. |
[4] | Rashidifard CH, Romeo NM, Muccino P, Richardson M, DiPasquale TG. Palliative management of nonoperative femoral neck fractures with continuous peripheral pain catheters: 20 patient case series. Geriatr Orthop Surg Rehabil (2017) ; 8: (1): 34-38. |
[5] | Park BJ, Cho HM, Min WB. Surgical treatment of undisplaced femur neck fractures in dementia patients using proximal femoral nail antirotation. Hip pelvis (2015) ; 27: (3): 164-172. |
[6] | Siddiqi A, Forte S, Collier AJ, McPhilemy JJ. Bilateral femoral neck fractures in a middle-aged female after a low-energy fall. Surg Technol Int (2019) ; 34: : 421-424. |
[7] | Filipov O. Biplane double-supported screw fixation (F-technique): a method of screw fixation at osteoporotic fractures of the femoral neck. Eur J Orthop Surg Traumatol (2011) ; 21: (7): 539-543. |
[8] | Nayak C, Acharyya B, Jain M, Kamboj K. Valgus osteotomy in delayed presentation of femoral neck fractures using fixed angle simple dynamic hip screw and plate. Chin J Traumatol (2019) ; 22: (1): 29-33. |
[9] | Levack AE, Gausden EB, Dvorzhinskiy A, Lorich DG, Helfet DL. Novel treatment options for the surgical management of young femoral neck fractures. J Orthop Trauma (2019) ; 33: (Suppl 1): S33-S37. |
[10] | Knobe M, Bettag S, Kammerlander C, Altgassen S, Maier KJ, Nebelung S, et al. Is bone-cement augmentation of screw-anchor fixation systems superior in unstable femoral neck fractures? A biomechanical cadaveric study. Injury (2019) ; 50: (2): 292-300. |
[11] | Yamamoto T, Kobayashi Y, Nonomiya H. Undisplaced femoral neck fractures need a closed reduction before internal fixation. Eur J Orthop Surg Traumatol (2019) ; 29: (1): 73-78. |
[12] | Slobogean GP, Stockton DJ, Zeng B, Wang D, Ma BT, Pollak AN. Femoral neck fractures in adults treated with internal fixation: a prospective multicenter chinese cohort. J Am Acad Orthop Surg (2017) ; 25: (4): 297-303. |
[13] | Johnson J, Deren M, Chambers A, Cassidy D, Koruprolu S, Born C. Biomechanical analysis of fixation devices for basicervical femoral neck fractures. J Am Acad Orthop Surg (2019) ; 27: (1): e41-e48. |
[14] | Bigoni M, Turati M, Leone G, Caminita AD, D’Angelo F, Munegato D, et al. Internal fixation of intracapsular femoral neck fractures in elderly patients: mortality and reoperation rate. Aging Clin Exp Res (2020) ; 32: (6): 1173-1178. |
[15] | Ozkul E, Serdar Necmioglu N, Onur Ziyadanogullari M, Alemdar C, Arslan H, Uzel K. An evaluation of treating non-union of femoral neck fractures with valgus angulation osteotomy using sliding hip screws. Acta Orthop Belg (2019) ; 85: (2): 210-217. |
[16] | Yang B, Yang J, Li L, Lan JP, Ran MB. A clinical comparative study of hollow nail plus medial support plate and hollow nail internal fixation for Pauwels type III femoral neck fracture. Journal of Traumatic Surgery (2019) ; 21: (11): 821-825. |
[17] | Cha YH, Yoo JI, Hwang SY, Kim KJ, Kim HY, Choy WS, et al. Biomechanical evaluation of internal fixation of Pauwels type iii femoral neck fractures: a systematic review of various fixation methods. Clin Orthop Surg (2019) ; 11: (1): 1-14. |
[18] | Xu YK, Wei YZ. Clinical effect of hollow nail combined with supporting plate on Pauwels III femoral neck fracture. Chinese and Foreign Medical Research (2018) ; 16: (26): 37-39. |
[19] | Qin YP, Song Y, Hou HT, Li PF, Sun Z, Zhang HL, et al. Comparison of two methods in the treatment of Pauwels type III femoral neck fractures. Journal of Practical Orthopedics (2018) ; 24: (10): 890-893. |
[20] | Li RH, Wang SL, Wang SQ, Xu HH, Bi RX. Observation on the therapeutic effect of hollow nail combined with medial support plate on Pauwels III femoral neck fracture. World Latest Medical Information Digest (2018) ; 18: (A5): 32-34. |
[21] | Ding WX, Wei P, Jiang K. Comparison of the short-term effects of two surgical methods on Pauwels type III femoral neck fractures. Sichuan Medical Journal (2018) ; 39: (5): 64-68. |
[22] | Li P, Luo JP, Peng XZ. Observation on the effect of medial femoral steel plate combined with hollow nail internal fixation in the treatment of unstable femoral neck fractures in young and middle-aged. Modern Diagnosis and Treatment (2018) ; 29: (24): 3943-3945. |
[23] | Shen DH, Zhou GS, Zha XS, Huang K, Huang C. Observation of the short-term effect of hollow screw combined with medial support plate in the treatment of Pauwels type 3 femoral neck fracture. Journal of Chinese Physician (2019) ; 21: (5): 776-779. |
[24] | Johnson JP, Borenstein TR, Waryasz GR, Klinge SA, McClure PK, Chambers AB, et al. Vertically oriented femoral neck fractures: a biomechanical comparison of 3 fixation constructs. J Orthop Trauma (2017) ; 31: (7): 363-368. |
[25] | Sancar Serbest, Uur Tiftikçi, Hacı Bayram Tosun, Üçler Kısa. The irisin hormone profile and expression in human bone tissue in the bone healing process in patients. Med Sci Monit (2017) ; 23: : 4278-4283. |
[26] | Sancar Serbest, Ugur Tiftikci, Haci Bayram Tosun, Seyit Ali Gumustas, Abuzer Uludag. Is there a relationship between fracture healing and mean platelet volume? Ther Clin Risk Manag (2016) ; 12: : 1095-1099. |
[27] | Seyitali Gumustas, Haci Bayram Tosun, Mehmet Isyar, Sancar Serbest, Kadir Oznam, Güven Bulut. Femur neck fracture in young adults, is it really an urgent surgery indication: retrospective clinical study. (2018) ; 30: : 112. |
[28] | Chiang MH, Wang CL, Fu SH, Hung CC, Yang RS. Does fully-threaded headless compression screw provide a length-stable fixation in undisplaced femoral neck fractures? Asian J Surg (2019) ; 42: (1): 320-325. |
[29] | Knobe M, Altgassen S, Maier KJ, Gradl-Dietsch G, Kaczmarek C, Nebelung S, et al. Screw-blade fixation systems in Pauwels three femoral neck fractures: a biomechanical evaluation. Int Orthop (2018) ; 42: (2): 409-418. |
[30] | Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma (2017) ; 31: (3): 131-137. |
[31] | Flury A, Finsterwald M, Dimitriou D, Hasler J, Antoniadis A, Helmy N. Could a simple screening procedure identify patients with early cognitive impairment? Implications for the treatment of geriatric femoral neck fractures. J Arthroplasty (2020) ; 35: (4): 1023-1028. |
[32] | Unnanuntana A, Saiyudthong N. Outcomes of cerclage wiring to manage intra-operative femoral fracture occurring during cementless hemiarthroplasty in older patients with femoral neck fractures. Int Orthop (2019) ; 43: (11): 2637-2647. |
[33] | Kuan FC, Hsu KL, Lin CL, Hong CK, Yeh ML, Su WR. Biomechanical properties of off-axis screw in Pauwels III femoral neck fracture fixation: bicortical screw construct is superior to unicortical screw construct. Injury (2019) ; 50: (11): 1889-1894. |
[34] | Schmaranzer F, Arendt L, Lerch TD, Steppacher SD, Nuss K, Wolfer N, et al. Femoral osteochondroplasty can be performed effectively without the risk of avascular necrosis or femoral neck fractures in an experimental ovine FAI model. Osteoarthritis Cartilage (2018) ; 26: (1): 128-137. |
[35] | He M, Han W, Zhao CP, Su YG, Zhou L, Wu XB, et al. Evaluation of a bi-planar robot navigation system for insertion of cannulated screws in femoral neck fractures. Orthop Surg (2019) ; 11: (3): 373-379. |
[36] | Elgeidi A, El-Negery A. Fibular strut graft for nonunited femoral neck fractures in children. J Child Orthop (2017) ; 11: (1): 28-35. |
[37] | Zajonz D, Behrens J, Brand AG, Hoch A, Fakler JKM, Roth A, et al. Femoral neck fractures in old age treated with hemiarthroplasty: effects of preoperative waiting time and timing of surgery on the risk of periprosthetic infections. Orthopade (2019) ; 48: (3): 224-231. |
[38] | Jianbo J, Ying J, Xinxin L, Lianghao W, Baoqing Y, Rongguang A. Hip hemiarthroplasty for senile femoral neck fractures: minimally invasive SuperPath approach versus traditional posterior approach. Injury (2019) ; 50: (8): 1452-1459. |
[39] | Leer-Salvesen S, Dybvik E, Dahl OE, Gjertsen JE, EngesaeTer LB. Postoperative start compared to preoperative start of low-molecular-weight heparin increases mortality in patients with femoral neck fractures. Acta Orthop (2017) ; 88: (1): 48-54. |
[40] | Temmesfeld MJ, Dolatowski FC, Borthne A, Utvag SE, Hoelsbrekken SE. Cross-table lateral radiographs accurately predict displacement in valgus-impacted femoral neck fractures. JB JS Open Access (2019) ; 4: (1): e0037. |




