Identifying prognostic factors to determine the level of recovery in servicemembers with chronic low back pain: A prospective cohort study
Abstract
OBJECTIVE:
The main objective of this study was to identify general and military-related factors that are associated with the level of recovery in Dutch service members with chronic low back pain (CLBP) who followed a rehabilitation program.
MATERIAL AND METHOD:
One hundred five consecutive service members with CLBP were included in this study. The level of disability, was used to distinguish a recovered and non-recovered group. Level of pain and self-perceived recovery were used as secondary outcome measurements. Differences were evaluated within and between the groups using the Student’s
RESULTS:
After following the rehabilitation program, 64.8% of the service members recovered from CLBP. The recovered group, demonstrated significant effect sizes in disability and in pain The non-recovered group showed on disability a non-significant effect and in pain a significant effect. The self-perceived recovery in the recovered group was “much improved” and the non-recovered group “slightly improved”. The results of the bivariate regression analyses showed no significant independent prognostic factors related to recovery.
CONCLUSIONS:
In this study, no significant independent prognostic factors could be identified that were associated to the various outcomes of recovery in service members with CLBP who followed a rehabilitation program.
1.Introduction
In the Dutch Armed Forces (DAF), low back pain is the third most reported musculoskeletal disorder following knee and lower extremity injuries [1]. Among active military members of the US Army between 2011 and 2014, over 6 million medical encounters with the diagnosis of low back pain and two-thirds of the outpatient visits were labelled chronic low back pain (CLBP) [2]. CLBP causes high medical costs as well as a socio-economic burden due to high absence from work. In the US Army, low back pain has been demonstrated to be the highest cumulative risk of disability discharge and is a common reason for causing medical evacuation [3, 4]. For the DAF these figures are not available however, it is reasonable to believe that they are comparable with the situation in the US.
On that account, more and more research is being performed about the prognosis of CLBP to improve prevention as well as achieving to find more matching effective treatments. However, a recent systematic review shows that only limited evidence is available with regard to the prognosis for recovery and that the overall quality of the studies is low [5]. Also, a broad variety of prognostic variables have been found due to the high degree of heterogeneity in the CLBP population [6]. Thus, it is important to distinguish different subgroups within the CLBP population by identifying the associated prognostic factors for recovery which may improve intervention effectiveness [7].
At present, limited research is available on the prognostic factors specific to service members with CLBP [8]. It is not clear which prognostic factors affect recovery from CLBP in service members following a multidisciplinary therapy program and whether this program frames matching treatment for this subgroup. It is plausible that more knowledge on matching treatment in the military rehabilitation setting might improve the effectiveness. This also might result in a higher level of recovery meeting military occupations that demands heavy physical tasks. The contribution of this study to the body of knowledge will be the military setting.
The objective of this study is to identify general and militaryrelated factors that might be associated with the level of recovery in DAF service members with CLBP who followed a rehabilitation program, as well as to evaluate whether military-related factors add to the general prognostic factors. Our hypothesis is that military related factors might be an addition to the general prognostic factors for predicting the recovery of CLBP in service members.
2.Material and method
2.1Subjects and setting
This prospective cohort study included consecutive servicemembers with CLBP who followed a multidisciplinary program at the Military Rehabilitation Centre (MRC) Doorn, the Netherlands, from September 2016 and November 2018. The servicemembers were referred by either a general practitioner of the military health centre at their unit or a medical specialist of the Central Military Hospital in Utrecht.
A participant was included in the study if the low back pain (with or without leg pain) was non-specific fora duration of more than 3 months and the individual was in active duty with the DAF. Before the start of treatment, CLBP was diagnosed in a triage setting at the MRC by a rehabilitation physician, manual therapist and a psychologist. Patients were excluded from this study in cases of manifestation of neurological or rheumatological problems, stenosis complaints, multiple diseases pregnancy, psychiatric or primary psychological problems, as stated in DSM V and drugs and/or alcohol abuse.
The multidisciplinary rehabilitation program consisted of a 12 weeks treatment period, 3 days per week and included the following elements: physical therapy (2 times 30 minutes per week), occupational therapy (1 time 30 minutes per week), sports therapy (3 times 60 minutes per week), social work (1 time 30 minutes per 2 weeks), psychology (1 time 60 minutes per 2 weeks) and vocational therapy (2 times 30 minutes per week). All therapists used a biopsychosocial treatment approach, in which a time-focused, gradual increase of activity was the main focus/option. Whereas, physical therapy and sports trainers focused on gradual increasing physical activity in the domain of daily activities, sports and military skills. The content of occupational and vocational therapy was aimed on posture and/or movement advice and also how to handle physical boundaries in daily life and work situations. The psychosocial factors that influenced the CLBP, such as anxiety, work problems or somatization, were handled by the social worker and psychologist. At the end of the rehabilitation program, further build-up of physical capacity for duty was advised, either independent at their unit or under supervision of coaches at the MRC. All participants provided written informed consent. The Central Commission Medical Research (CCMO) confirmed that this study did not require ethical approval because the protocol was ‘Care As Usual’ (CAU). The Dutch Defence Health Organization also approved this study (DGO170616006).
2.2Prognostic variables
As stated in other literature, the prognostic factors for this study related to biopsychosocial factors that are associated with CLBP and are distinguished in general and military-related factors (Table 1) [9].
Table 1
Prognostic variables
| General factors | Measurement properties |
|---|---|
| Self-efficacy | Pain Self Efficacy Questionnaire (PSEQ) shows the confidence in the ability to perform tasks despite the pain. Scores range from 0 to 60, whereas higher scores reflect stronger self-efficacy beliefs [11]. |
Psychological distress
| Symptom CheckList-90-R (SCL-90-R). A 90-item self-report symptom inventory that measures psychological symptoms and psychological distress, the SCL-90-R has nine symptom dimensions: anxiety, agoraphobia, depression, somatization, insufficiency, sensitivity, hostility and insomnia. Each of the 90 items is rated on a five-point Likert scale, ranging from ‘not at all’ to ‘extremely’ [12]. |
| Level of disability | Roland Morris Disability Questionnaire (RMDQ) consists of 24 items representing physical activities that are likely to be affected by low back pain. Range of score is 0 to 24, where a higher score means more disability [13]. |
| Level of pain | Numeric Pain Rating Scale (NPRS). An 11-point scale that measures pain intensity, where ‘0’ |
| Military-related factors | |
| Basic military physical test | The basic military physical test (DCP) consists of three elements: a 12-minute run, push-ups and sit-ups. The ability to complete the test was measured dichotomously (positive/negative). |
| Cluster level | Reflects the physical requirements of military functions, ranging from cluster 1 ‘administrative work’ to cluster 6 ‘high physical work’. Measured dichotomously (‘cluster 1–3’ and ‘cluster 4–6’). |
| Duration of military service | Measures how long the participant has worked in the DAF and is measured dichotomously (‘0–10 years’ and ‘10 |
The general factors were derived from recent studies that showed a prognostic value on recovery from CLBP [10]. The military-related factors were based on our clinical experience and relevant for the military population. These military factors represent particularly physical elements of military duty. The factors qualify the level of the basic physical condition of a service member, the level of physical requirements of the military function and the duration of military service which reflects the heavy workload capacity in years of the service member.
At the MRC, the general factors were extracted from validated and reliable questionnaires before the start of treatment and in addition, the military-related factors have been measured by a questionnaire at baseline.
Table 2
Demographic characteristics and prognostic variables at baseline between recovered and non-recovered group prognostic variables at baseline between recovered and non-recovered group
| Characteristics | Recovered group | Non-recovered group | |||
|---|---|---|---|---|---|
| Age (years, | 35.26 | (10.49) | 35.59 | (11.01) | 0.880 # |
| Male ( | 65 | (95.60) | 32 | (86.49) | 0.126 $ |
| Residency ( | |||||
| Clinical | 26 | (38.24) | 19 | (51.35) | |
| Outpatient | 42 | (61.76) | 18 | (48.65) | 0.22 $ |
| Period treatment (weeks, | 10.38 | (2.59) | 9.97 | (1.76) | 0.392 # |
| Body weight (kg, | 90.60 | (13.44) | 85.36 | (13.30) | 0.062 # |
| Smoking (yes, | 26 | (38,24) | 10 | (27,03) | 0.287 $ |
| Partner (yes, | 57 | (83,82) | 30 | (81,08) | 0.789 $ |
| Sport ( | |||||
| Military sport | 6 | (8.82) | 7 | (18.92) | 0.186 * |
| Fitness | 22 | (32.35) | 14 | (37.84) | |
| Ball sport | 4 | (5.88) | 1 | (2.70) | |
| Biking | 11 | (16.18) | 1 | (2.70) | |
| Running | 11 | (16.18) | 4 | (10.81) | |
| Other | 8 | (11.77) | 8 | (21,62) | |
| No sports | 6 | (8.82) | 2 | (5.41) | |
| Military service ( | |||||
| Army | 35 | (51.47) | 21 | (56.76) | 0.420 * |
| Air force | 13 | (19.12) | 7 | (18.92) | |
| Navy | 12 | (17.65) | 2 | (5.40) | |
| Military police | 8 | (11.76) | 7 | (18.92) | |
| Other complaints (yes, | 24 | (35.29) | 18 | (48.65) | 0.214 $ |
| Work reduction (yes, | 16 | (23.53) | 11 | (29.73) | 0.642 $ |
| Previous treatment (yes, | 43 | (63.24) | 28 | (75.68) | 0.275 $ |
| Prognostic variables | |||||
| Specific military-related factors | |||||
| Ability to execute DCP (yes, | 31 | (45.59) | 18 | (48.65) | |
| Cluster level ( | |||||
| 1–3: mild physical work | 44 | (64.71) | 25 | (67.57) | |
| 4–6: intensive physical work | 20 | (29.41) | 9 | (24.32) | |
| Duration of military service ( | |||||
| | 24 | (35.29) | 16 | (43.24) | |
| | 44 | (64.71) | 21 | (56.76) | |
| General factors | |||||
| Self-efficacy (PSEQ, | 43.30 | (10.41) | 39.63 | (12.19) | |
| Psychological distress (SCL-90-R, m range) | |||||
| Total score | 117 | (94–256) | 119 | (89-220) | |
| Anxiety symptoms | 12 | (9–25) | 12 | (10–26) | |
| Depression symptoms | 19 | (16–50) | 19.5 | (15–49) | |
| Somatisation symptoms | 20 | (14–41) | 20.5 | (12–36) | |
| Level of disability (RMDQ, m range) | 9 | (1–19) | 9 | (2–20) | |
| Level of pain (NPRS, m range) | 7 | (0–10) | 7 | (3-9) | |
DCP, Defence Condition Proof; m, median; n, sample size; NPRS, Numeric Pain Rating Score; PSEQ, Pain Self Efficacy Questionnaire; RMDQ, Roland Morris Disability Questionnaire; SCL-90, Symptom Check List; *, chi-square test;
2.3Outcome measures
The primary outcome measure was the level of functional disability measured by the RMDQ. A decrease of
The secondary outcome measurements were level of pain and self-perceived recovery, respectively measured with the Verbal Rating Score (VRS) and the Global Perceived Effect Questionnaire (GPE) [16, 17]. At baseline and follow-up, the VRS was recorded after a 1 km run at a comfortable speed. Two sports trainers with a mean experience of 12 years executed this test and obtained beforehand consensus about the performance of the test. The VRS is the verbal equivalent of the NPRS [17]. The classification of recovery after the MRC rehabilitation program was set at a decrease of
2.4Statistical analysis
The sample size choice was based on the COSMIN guidelines box F “hypothesis testing” arguing that a sample size of
All outcome measurements, at baseline and follow-up were used to calculate the number and percentages of recovered and non-recovered participants in the two groups. Also, the group means including the standard deviation were evaluated with corresponding effect sizes and p-values within the group and between the recovered and non-recovered group based on the primary outcome measurement using the Student’s t-test or Mann-Whitney U test. To evaluate the magnitude of prognostic factors, bivariate logistic regression analyses were performed on the primary and secondary outcome variables from which odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. All analyses were performed using R software version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
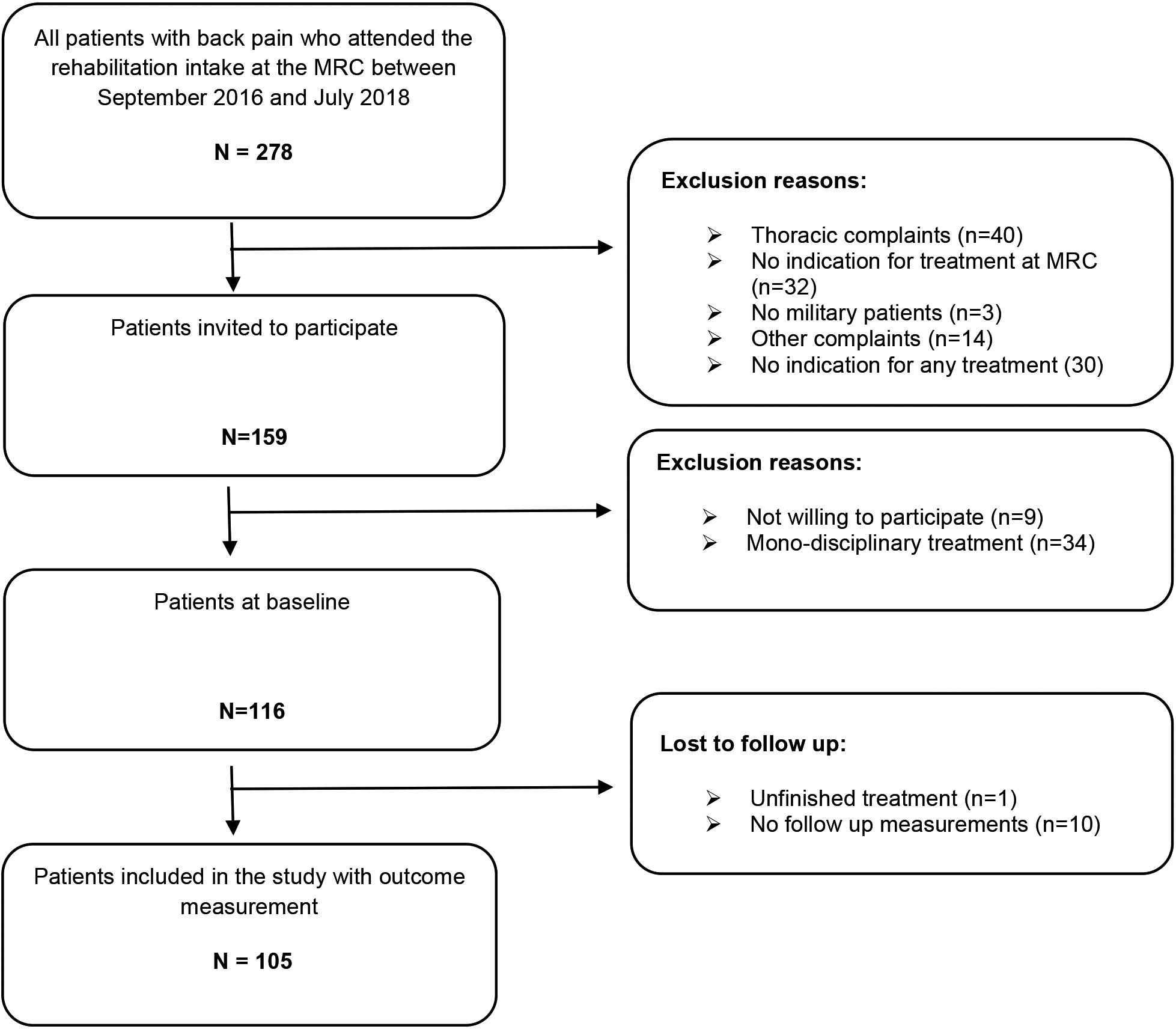
Figure 1.
Flowchart of study population.
3.Results
Between September 2016 and November 2018, a total of 278 patients were screened in the triage setting at the rehabilitation intake (Fig. 1). Of the 116 included patients with CLBP, 105 participants completed the multidisciplinary program and their data were used for the analysis. The descriptive statistics and baseline measurement of prognostic factors are presented in Table 2. No significant differences between the two groups on patient characteristics were obtained. For efficiency and reliability of estimates, multiple imputations chained equations (MICE) was performed for missing data (4,1%). The outcome variables level of pain and self-perceived recovery have the highest percentage of missing data, however they are missing completely at random (MCAR) or missing at random (MAR).
3.1Primary and secondary outcomes
The mean of the primary outcome measure at baseline is lower in the non-recovered group and the degree of pain is higher compared with the recovered group; however the differences are not significant (Table 3). The effect size within the recovered group on the level of disability is
Table 3
Outcome measurements recovered and non-recovered patients
| Recovered group ( | Non-recovered group ( | Missing data ( | |
| Level of disability (RMDQ) | 68 (64.77) | 37 (35.24) | 0 (0) |
| Level of pain (NPRS) | 54 (51.43) | 30 (28.57) | 21 (20) |
| Perceived recovery (GPE) | 48 (45.71) | 31 (29.52) | 26 (24.76) |
| Baseline and follow-up outcome measurements in recovered and non-recovered group | |||
| Baseline | 9–12 weeks follow-up | |||
|---|---|---|---|---|
| Recovered group | Non-recovered group | Recovered group | Non-recovered group | |
| Level of disability (RMDQ) | 9.84 (4.31) | 9.32 (5.13) | 3.12 (2.58) | 8.84 (4.15) |
| Level of pain (NPRS) | 4.28 (2.36) | 4.86 (2.76) | 1.84 (2.08) | 3.97 (2.65) |
| Perceived recovery (GPE) | 2.21 (0.50) | 2.96 (0.74) | ||
GPE, Global Perceived Effect;
3.2Prognostic factors
The results of the bivariate logistic regression analysis performed on the primary outcome shows that in servicemembers with CLBP no independent prognostic factors on recovery in functional disability can be identified (Table 4). An identical finding is derived from the bivariate logistic regression on the classification of recovery in pain and in self-perceived recovery in back complaints (Table 4). The OR’s of almost all prognostic variables are not consistent
Table 4
Bivariate logistic regression analyses
| OR (95% CI) | ||
| Bivariate logistic regression analysis on primary outcome measurement (RMDQ) | ||
| Ability to execute DCP | 1.13 (0.50–2.55) | 0.765 |
| Cluster level | 0.72 (0.31–1.64) | 0.425 |
| Duration of military service | 0.79 (0.31–2.03) | 0.623 |
| Self-efficacy (PSEQ) | 1.03 (0.99–1.07) | 0.134 |
| Psychological distress (SCL-90-R) | ||
| Total score | 0.997 (0.98–1.01) | 0.705 |
| Anxiety symptoms | 0.96 (0.87–1.07) | 0.506 |
| Depression symptoms | 1.00 (0.95–1.06) | 0.967 |
| Somatisation symptoms | 0.98 (0.91–1.06) | 0.597 |
| Level of disability (RMDQ) | 1.02 (0.93–1.11) | 0.689 |
| Level of pain (NPRS) | 0.94 (0.76–1.17) | 0.608 |
| Bivariate logistic regression analysis on secondary outcome measurement (NRS) | ||
| Ability to execute DCP | 0.67 (0.27–1.67) | 0.382 |
| Cluster level | 0.77 (0.31–1.94) | 0.573 |
| Duration of military service | 0.61 (0.21–1.74) | 0.352 |
| Self-efficacy (PSEQ) | 0.99 (0.95–1.04) | 0.648 |
| Psychological distress (SCL-90-R) | ||
| Total score | 1.01 (0.99–1.03) | 0.199 |
| Anxiety symptoms | 1.10 (0.95–1.26) | 0.186 |
| Depression symptoms | 1.04 (0.97–1.13) | 0.239 |
| Somatisation symptoms | 1.02 (0.93–1.12) | 0.643 |
| Level of disability (RMDQ) | 1.01 90.92–1.12) | 0.820 |
| Level of pain (NPRS) | 0.93 (0.70–1.24) | 0.637 |
| Bivariate logistic regression analysis on secondary outcome measurement (GPE) | ||
| Ability to execute DCP | 0.94 (0.37–2.35) | 0.889 |
| Cluster level | 1.15 (0.43–3.05) | 0.773 |
| Duration of military service | 1.05 (0.36–3.04) | 0.931 |
| Self-efficacy (PSEQ) | 1.02 (0.98–1.07) | 0.321 |
| Psychological distress (SCL-90-R): | ||
| Total score | 0.99 (0.98–1.01) | 0.936 |
| Anxiety symptoms | 1.04 (0.92–1.18) | 0.512 |
| Depression symptoms | 1.00 (0.94–1.08) | 0.894 |
| Somatisation symptoms | 0.97 (0.87–1.07) | 0.501 |
| Level of disability (RMDQ) | 0.98 (0.89–1.08) | 0.761 |
| Level of pain (NPRS) | 0.87 (0.68–1.11) | 0.257 |
CI, confidence interval; DCP, Defence Condition Proof; GPE, Global Perceived Effect; m, median; n, sample size; NPRS, Numeric Pain Rating Score; OR, Odds Ratio; PSEQ, Pain Self Efficacy Questionnaire; RMDQ, Roland Morris Disability Questionnaire; SCL-90, Symptom Check List.
4.Discussion
The objective of this study was to identify general and military-related factors associated with the level of recovery in service members with CLBP who have followed a rehabilitation program, as well as to investigate whether military-related factors add to the general prognostic factors.
The result of this study shows no significant independent prognostic factors that determine the level of recovery from CLBP despite the more homogeneous population of service members. The explanation could be that the degree of homogeneity within the military group with CLBP is still too low, which prevents identification of a subgroup with equal prognosis. Also, in the general CLBP population, it is challenging to find strong independent prognostic factors due to a high degree of heterogeneity, as well as various outcomes and interventions and use of low methodological quality studies [5, 20].
In this study, level of disability is used as a prognostic factor and primary outcome measurement, both measured with the RMDQ. Due to the use of a relative score as criterion for recovery, it is common that an association occurs with the baseline score as prognostic factor. This is because participants with a high baseline score have to decrease a larger number of points to recover compared to participants with a low baseline score. This association is also seen in a study by Verkerk [9]., where a higher disability at baseline is a significant prognostic factor for
An association between psychosocial factors and level of recovery is not detected by this study, however, reported in a systematic review, reasonable evidence indicates symptoms of distress, depression and somatization as prognostic factors [21]. Regrettably, there is still a lack of knowledge about the mechanism that influences the relationship between symptoms of depression and CLBP. It is unclear which of the problems causes the other, but if both exist, there is an impact on the prognosis [22]. Therefore, addressing symptoms of depression in the treatment might have a positive effect on the level of recovery from CLBP. Other studies show that a lower self-efficacy at baseline increases the risk of non-recovery from CLBP [23, 24, 25, 26]. This can result in modifying the content of the rehabilitation program which could put more emphasis on increasing self-efficacy for the purpose of reducing disability. However, as is mentioned in a systematic review by Tseli et al, treatment should not only target negative psychological factors, but also increase focus on positive protective factors which are associated with a better prognosis [27].
By lack of identifying significant prognostic factors in this study, a multivariate analysis for building a prediction model was not conducted. The sample size of this study is probably too small to detect significance. For further research, the study results can be used for a power analysis to calculate an appropriate sample size. A larger sample might provide further evidence for identifying prognostic factors associated with the level of recovery of CLBP in service members and the ability to perform a multivariate analysis.
Furthermore, the results show that the military-related factors have no significant contribution to predict the level of recovery from CLBP in addition to the general factors, which may be caused by using non-validated questionnaires or improperly used cut-off points. To our knowledge, there is limited literature about specific military-related factors predicting the recovery or course of CLBP. Most research within the army is focused on risk factors of low back pain [28]. Therefore, more research is needed about military-related factors that may affect the course of CLBP in the military population.
In this study, almost 65% of the service members recovered from CLBP after a rehabilitation program. In two systematic reviews, it also shows that multidisciplinary treatment of CLBP has a moderate effect in short term recovery in disability [29, 30]. However, this is in contrast with the study of Ravenek who concluded in his systematic review that there is no effect on the level of disability [31]. This conflicting evidence could be attributed to difference in content of treatment, difference in outcome classification, or heterogeneity of the CLBP population. This study sample differs from the general CLBP population, since there is a notable difference in gender, age and work reduction [31]. This difference may be the result of the military setting, in which there are a higher number of males and adolescents. Moreover, in this study a relative score of greater than 30% on the RMDQ has been used for the classification of recovery, which varies from other literature using absolute differences or using the Oswestry Disability Index (ODI) [15, 30]. This difference could also affect the proportion of recovery.
This research presented several limitations that may affect the results. First, only short-term measurements are used for the classification of recovery. The lack of long-term follow-up means that we cannot be certain whether the results apply to long-term recovery of CLBP as well. However, it has been noted that after 12 weeks and 1 year follow up, improvement in recovery is slower than in the first 6 weeks [32]. Moreover, the choice for disability as primary outcome measurement does not mean that recovered service members are also able to return to work, because a military job often requires a higher physical load capacity. Second, although the treatment was offered as stated in protocol, a minority of the participants received less mental coaching due to magnitude of psychosocial problems. This difference could lead to bias (i.e., the level of recovery) however, two randomized controlled trials showed that there is no extensive difference in effect due to different intensity of treatment [33, 34]. Finally, the findings of this study are restricted to the military population with CLBP and cannot be taken as evidence for the entire population of patients with CLBP.
5.Conclusion
In this study, no significant independent prognostic factors could be identified to determine the level of disability, level of pain or self-perceived recovery in service members with CLBP who have followed a rehabilitation program. Also, the military-related factors have no additional contribution to predict the level of recovery. A larger sample might provide further evidence for identifying general and military-related factors For future research, we also suggest to use long-term outcomes, as well as involving “return to work” and possibly considering other military-related factors.
Acknowledgments
The authors express their gratitude to the staff of the physiotherapy, psychology and sport department from the Military Rehabilitation Centre, Doorn, the Netherlands.
Conflict of interest
None to report.
References
[1] | Helmhout PH, Harts CC, Staal JB, de Bie RA. Rationale and design of a multicenter randomized controlled trial on a ’minimal intervention’ in Dutch army personnel with nonspecific low back pain [ISRCTN19334317]. BMC Musculoskelet Disord. (2004) ; 5: (1): 40. doi: 10.1186/1471-2474-5-40. |
[2] | Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. (2008) ; 8: (1): 8-20. doi: 10.1016/j.spinee.2007.10.005. |
[3] | Cohen SP, Brown C, Kurihara C, Plunkett A, Nguyen C, Strassels SA. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: A prospective cohort study. Lancet. (2010) ; 375: (9711): 301-9. doi: 10.1016/S0140-6736(09)61797-9. |
[4] | Lincoln AE, Smith GS, Amoroso PJ, Bell NS. The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work. (2002) ; 18: (2): 99-113. PMCID: PMC2151132 |
[5] | Verkerk K, Luijsterburg PA, Miedema HS, Pool-Goudzwaard A, Koes BW. Prognostic factors for recovery in chronic nonspecific low back pain: a systematic review. Phys Ther. (2012) ; 92: (9): 1093-108. doi: 10.2522/ptj.20110388. |
[6] | Kent PM, Keating JL. Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review. Man Ther. (2008) ; 13: (1): 12-28. doi: 10.1016/j.math.2007.05.009. |
[7] | Patel S, Friede T, Froud R, Evans DW, Underwood M. Systematic review of randomized controlled trials of clinical prediction rules for physical therapy in low back pain. Spine (Phyla Pa 1976); (2013) ; 38: (9): 762-9. doi: 10.1097/BRS.0b013e31827b158f. |
[8] | Helmhout PH, Staal JB, Heymans MW, Harts CC, Hendriks EJ, de Bie RA. Prognostic factors for perceived recovery or functional improvement in non-specific low back pain: secondary analyses of three randomized clinical trials. Eur Spine J. (2010) ; 19: (4): 650-9. doi: 10.1007/s00586-009-1254-8. |
[9] | Verkerk K, Luijsterburg PA, Heymans MW, Ronchetti I, Pool-Goudzwaard AL, Miedema HS, et al. Prognosis and course of pain in patients with chronic non-specific low back pain: A 1-year follow-up cohort study. Eur J Pain. (2015) ; 19: (8): 1101-10. doi: 10.1002/ejp.633. |
[10] | Verkerk K, Luijsterburg PA, Heymans MW, Ronchetti I, Pool-Goudzwaard AL, Miedema HS, et al. Prognosis and course of disability in patients with chronic nonspecific low back pain: a 5- and 12-month follow-up cohort study. Phys Ther. (2013) ; 93: (12): 1603-14. doi: 10.2522/ptj.20130076. |
[11] | Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. Eur J Pain. (2007) ; 11: (2): 153-63. doi: 10.1016/j.ejpain.2005.12.008. |
[12] | Derogatis LR. SCL-90-R: Administration, Scoring & Procedures Manual-II, for the R (Revised) Version and Other Instruments of the Psychopathology Rating Scale Series. 2nd Edition ed. Towson: Clinical Psychometric Research, Inc, (1992) . |
[13] | Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phyla Pa 1976). (1983) ; 8: (2): 141-4. doi: 10.1097/00007632-198303000-00004. |
[14] | Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) (2011) ; 63: (Suppl 11): S240-52. doi: 10.1002/acr.20543. |
[15] | Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phyla Pa 1976). (2008) ; 33: (1): 90-4. doi: 10.1097/BRS.0b013e31815e3a10. |
[16] | Chiarotto A, Boers M, Deyo RA, Buchbinder R, Corbin TP, Costa LOP, et al. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. (2018) ; 159: (3): 481-95. doi: 10.1097/j.pain.0000000000001117. |
[17] | Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symp Manage. (2011) ; 41: (6): 1073-93. doi: 10.1016/j.jpainsymman.2010.08.016. |
[18] | Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine (Phyla Pa 1976). (2000) ; 25: (24): 3167-77. doi: 10.1097/00007632-200012150-00012. |
[19] | Terwee CB, Mokkink LB, Knol DL, Ostelo RW, Bouter LM, de Vet HC. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res. (2012) ; 12: (4): 651-7. doi: 10.1007/s11136-011-9960-1. |
[20] | Hayden JA, Chou R, Hogg-Johnson S, Bombardier C. Systematic reviews of low back pain prognosis had variable methods and results: guidance for future prognosis reviews. J Clin Epidemiol. (2009) ; 62: (8): 781-96.e1. doi: 10.1016/j.jclinepi.2008.09.004. |
[21] | Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phyla Pa 1976). (2002) ; 27: (5): E109-20. doi: 10.1097/00007632-200203010-00017. |
[22] | Linton SJ, Bergbom S. Understanding the link between depression and pain. Scand J Pain. (2011) ; 2: (2): 47-54. doi: 10.1016/j.sjpain.2011.01.005. |
[23] | Ahmed SA, Shantharam G, Eltorai AEM, Hartnett DA, Goodman A, Daniels AH. The effect of psychosocial measures of resilience and self-efficacy in patients with neck and lower back pain. Spine J. (2019) ; 19: (2): 232-7. doi: 10.1016/j.spinee.2018.06.007. |
[24] | Duray M, Yagci N, Ok N. Determination of physical parameters associated with self-efficacy in patients with chronic mechanic low back pain. J Back Musculoskel Rehabil. (2018) ; 31: (4): 743-8. doi: 10.3233/BMR-170993. |
[25] | Jackson T, Wang Y, Wang Y, Fan H. Self-efficacy and chronic pain outcomes: a meta-analytic review. J Pain. (2014) ; 15: (8): 800-14. doi: 10.1016/j.jpain.2014.01.499. |
[26] | Karasawa Y, Yamada K, Iseki M, Yamaguchi M, Murakami Y, Tamagawa T, et al. Association between change in self-efficacy and reduction in disability among patients with chronic pain. PloS One. (2019) ; 14: (4): e0215404. doi: 10.1371/journal.pone.0215404. |
[27] | Tseli E, Boersma K, Stalnacke BM, Enthoven P, Gerdle B, Ang BO, et al. Prognostic Factors for Physical Functioning After Multidisciplinary Rehabilitation in Patients With Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Clin J Pain. (2019) ; 35: (2): 148-73. doi: 10.1097/AJP.0000000000000669. |
[28] | Moshe S, Zack O, Finestone AS, Mishal M, Segal N, Slodownik D, et al. The incidence and worsening of newly diagnosed low back pain in a population of young male military recruits. BMC Musculoskel Disord. (2016) ; 17: : 279. doi: 10.1186/s12891-016-1136-2. |
[29] | Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. The Cochrane Database of Systematic Reviews. (2002) (1): Cd000963. |
[30] | Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. The Cochrane Database of Systematic Reviews. (2014) (9): Cd000963. |
[31] | Ravenek MJ, Hughes ID, Ivanovich N, Tyrer K, Desrochers C, Klinger L, et al. A systematic review of multidisciplinary outcomes in the management of chronic low back pain. Work. (2010) ; 35: (3): 349-67. doi: 10.3233/WOR-2010-0995. |
[32] | Waterschoot FP, Dijkstra PU, Hollak N, de Vries HJ, Geertzen JH, Reneman MF. Dose or content? Effectiveness of pain rehabilitation programs for patients with chronic low back pain: a systematic review. Pain. (2014) ; 155: (1): 179-89. doi: 10.1016/j.pain.2013.10.006. |
[33] | Rose MJ, Reilly JP, Pennie B, Bowen-Jones K, Stanley IM, Slade PD. Chronic low back pain rehabilitation programs: a study of the optimum duration of treatment and a comparison of group and individual therapy. Spine (Phyla Pa 1976). (1997) ; 22: (19): 2246-51; discussion 52-3. doi: 10.1097/00007632-199710010-00009. |
[34] | Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine (Phyla Pa 1976). (2002) ; 27: (9): 901-9; discussion 9-10. doi: 10.1097/00007632-200205010-00002. |




