The effect of muscles energy technique in the management of chronic mechanical low back pain: A scoping review
Abstract
BACKGROUND:
The Muscle Energy Technique (MET) is one of the treatments of choice for the management of chronic mechanical low back pain (MLBP); however, there is a paucity of evidence to justify its effectiveness.
OBJECTIVES:
The objectives of this review are to explore, analyze and summarize the available evidence related to the effectiveness of MET in the management of chronic MLBP.
METHOD:
The scoping review methodology was adopted based on a recommendation from the work of Arksey and O’Malley, to systematically appraise literature and map the existing evidence on the effectiveness of MET in the management of chronic MLBP. A systematic search was performed comprising of an electronic search of online databases using key search terms and subsided by a hand search to identify the existing literature on the topic which was summarized and discussed.
RESULT:
Initially 25,195 hits were identified which were screened to examine their eligibility based on predetermined inclusion criteria after removing duplicate articles. Eleven articles met the inclusion criteria and were discussed.
CONCLUSIONS:
Generally there exists a scarcity of published articles on the effect of MET in chronic MLBP. However, the analysis of the retrieved articles showed that the MET procedure is a favourable intervention that is safe (i.e. no adverse effects) and can be effective as a standalone treatment or in combination with other treatment strategies for patients with chronic MLBP with the potential to provide numerous physical and psychosocial benefits.
1.Introduction
Low back pain (LBP) is arguably the most prevalent musculoskeletal condition found among both developed and developing nations [1, 2, 3]. It is the leading cause of activity limitations and loss of productivity resulting in high annual medical expenditure [3, 4]. According to the 2019 Global Burden of Disease (GBD) study, LBP is currently the sixth highest burden on a list of 291 conditions and is the cause of more years lived with disability globally than any other disease [4, 5]. The prevalence of LBP worldwide is estimated to be between 30 and 80% among the general population and has been found to increase with age [6]. Also, a higher prevalence of LBP has been associated with lower socioeconomic status and lower education levels [6, 7]. Because of the link between LBP prevalence and socioeconomic and educational background, it has been postulated that the burden of LBP is greater in lower and middle-income countries [8, 9]. Indeed in the past few decades, there has been an increase in disability rates caused by LBP across such countries located in Asia, the Middle East and Africa [14, 15], which has been attributed to poorly equipped health and social systems.
The prognosis after an acute episode of LBP is less favourable than once thought, as 60–80% of the patients will experience recurrence or persistence of this disabling condition [12]. Despite the high worldwide incidence and prevalence of LBP, little is known about the precise causes. As a clear patho-anatomic diagnosis cannot be identified in 85% of the patients [13], LBP in these patients is labelled as mechanical low back pain (MLBP). Despite extensive research, the issue of spinal pain management still constitutes a challenge for physicians, physiotherapists, and researchers [14]. Many therapies (education and self-care, cognitive behavioural therapy, superficial heat applications, exercise therapy, spinal manipulation, massage, acupuncture, yoga and pharmacological therapies) claim to be useful for the treatment of MLBP, but most of these treatments have not been well investigated or have been found to have modest effects in terms of pain relief and improving disability and chronicity [14, 15]. Conservative treatment remains the best choice, especially in case of chronic MLBP, and usually involves physiotherapy [14, 16]. The current practice guidelines for the treatment of MLBP encourage active treatments that address psychosocial factors and focus on improvement in function (which include graded exercises programs, spinal manipulation and mobilization, cognitive behavioral therapy and stress management) and focus less on pharmacological and surgical treatments (until non-pharmacological care has not worked) [14, 17, 18, 19]. However, these guidelines have been developed by, and for use in, high-income countries, and recommendations might be less feasible to apply in middle and low-income countries. For instance, factors such as cultural acceptability of treatments, patient attitudes towards and adherence to treatment, and treatment providers’ knowledge and adherence to the practice guidelines could vary systematically between countries and influence treatment outcomes [10, 20]. Furthermore, in some countries access to some treatments endorsed in practice guidelines is poor or non-existent [10] due to lack of expert care givers coupled with non-availability of equipment, also in some cases even patients education on pain physiology and self-care could be challenging in regions where many different dialects are used or where patients have no basic education. In general, the poor medical and rehabilitation infrastructures hamper the implementation of such clinical practice guidelines in these regions, and these countries need specifically adapted guidelines which are feasible to implement [15, 20]. Furthermore, studies examining the feasibility and effects of treatment strategies to manage MLBP associated with disability in low-income and middle-income countries are scarce [15].
A non-invasive, safe and inexpensive treatment technique used by physiotherapists, osteopaths, chiropractors and manual therapists in the treatment of MLBP is Muscle Energy Technique (MET) [21]. The technique can aid self-management of MLBP and thus prevent long-term disability, improves functions, activity limitations and participation restrictions [22]. The MET is a manual therapy procedure that involves alternating periods of resisted muscle contractions and assisted stretching [22, 23]. Although it has been suggested that MET can be used to lengthen a shortened muscle, reducing muscular tension, mobilize an articulation with restricted mobility, strengthen a physiologically weakened muscle, relaxing and stretching contracted musculature and reduce localized oedema and passive congestion [22, 24, 25], but the physiological mechanisms underlying the therapeutic effects of MET are currently unclear [22, 24]. Mechanisms of altered proprioception, motor programming and control have been proposed, but research is required to confirm these hypotheses [26].
While MET is often used for the treatment of MLBP, a 2016 Cochrane review concluded that there is a lack of strong evidence on its effectiveness in the management of chronic MLBP [22]. More specifically, this review concluded that it is unclear whether MET is effective in reducing pain and improving function in people with chronic MLBP. However, the authors remarked that although MET alone or in combination with other therapies has shown favourable effects, the quality of the evidence is low implying that further research is warranted, which is likely to have an important impact on the confidence of the estimate and thus might change the estimate and the drawn conclusions.
More recently there has been an increase in the number of studies on the effectiveness of MET in the management of MLBP with encouraging results. Therefore, the current paper aims to summarize all available literature on the effect of MET as a standalone or combine treatment intervention in the management of chronic MLBP. Besides, this review will not only consider randomized control trials (RCTs) but all type of study designs which is in line with the concept of performing a scoping review of the literature. This type of review is believed to help map out all the available evidence across different studies that meet this study inclusion criterion and present a broader spectrum of information on the topic. The current scoping review will focus mainly on the mode of application, evaluation and outcome of the MET intervention, as well as on study location, setting, participants’ characteristics, and study design. By taking into account and discussing the later characteristics, this review will help identify the available studies on the effect of MET in the management of chronic MLBP.
2.Methods
2.1Study design
The concept of this scoping review is based on the recommendation from the work of Arksey and O’Malley [27], which was further developed by Levac and co-workers [28]. The methodological framework of Arksey and O’Malley [27] proposes five stages that include: identifying the research question, identifying relevant studies, study selection, charting the data and collating, and summarizing and reporting the result of the study.
The first stage is to identify gaps in the empirical evidence on the effectiveness of MET in the management of chronic MLBP and the final stage is to conclude from the existing literature with regard to the overall state of studies on MET. The scoping review methodology will capture a range of studies on the topic with the purpose of summarizing (knowledge syntheses) the existing literature for the benefit of researchers and clinicians. This type of review does not focus on assessing the quality of the studies, rather the aim is to capture a broader range of literature, including all types of study designs [27].
2.2Research question
To ensure that a broad range of relevant literature is identified, the following research question was set: “What are the treatment effects of MET on pain, bodily structures and functions, quality of life, and activities of daily living in the management of chronic MLBP?” In determining the question, we acknowledge the recommendation to maintain a wide approach in defining the parameters at this stage of the study to generate a wide breadth of coverage [27, 29].
2.3Search strategy
The electronic databases Cochrane Library, PubMed, Europe PMC, PEDro, Google Scholar, ScienceDirect, WorldCat, Osteopathic Medicine Digital Repository (OSTMED-DR), EBSCOhost, Osteopathic Research Web and ClinicalTrials.gov were screened to retrieve the available evidence regarding this topic from 2003 to 2019. To identify relevant studies an electronic search was performed in these databases using the combination of the following keywords and/or their synonyms: (“muscle energy technique” OR “MET” OR “manual therapy”) AND (“mechanical low back pain” OR “non-specific low back pain”) AND (“management” OR “treatment of low back pain”). Eligibility assessment of the retrieved articles was performed by screening them against the predefined inclusion and exclusion criteria as outlined in Table 1. In short, all English full-text reports of original studies examining the intervention effects of MET (as a standalone or combined treatment) delivered by a physiotherapist, osteopathic physician or chiropractor for the management of chronic MLBP in an adult patient population were eligible for study inclusion. To search as complete as possible, a hand search was performed entailing that reference lists and citations of the included studies retrieved from the electronic search were screened to identify additional relevant studies. In case such studies were retrieved they were screened for the fulfilment of the inclusion criteria.
Table 1
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Original peer-reviewed articles of experimental studies | Non-peer-reviewed articles (e.g. books, seminar/workshop materials, position statements, etc.) of non-experimental studies (e.g. literature reviews, commentaries, etc.) |
| Full-text reports | Abstracts, congress proceedings, research protocols, posters, etc. |
| Articles must be written in English | Articles not written in English |
| Chronic MLBP population | Healthy, or other patient populations than chronic MLBP |
| Adults ( | Adolescents or children ( |
| Examining the intervention effects of MET (as a standalone or as combination treatment) | Not examining interventions effects or not using MET intervention |
| MET delivered by a physiotherapist, osteopathic physician or chiropractor | MET delivered by other occupations than physiotherapist, osteopathic physician or chiropractor |
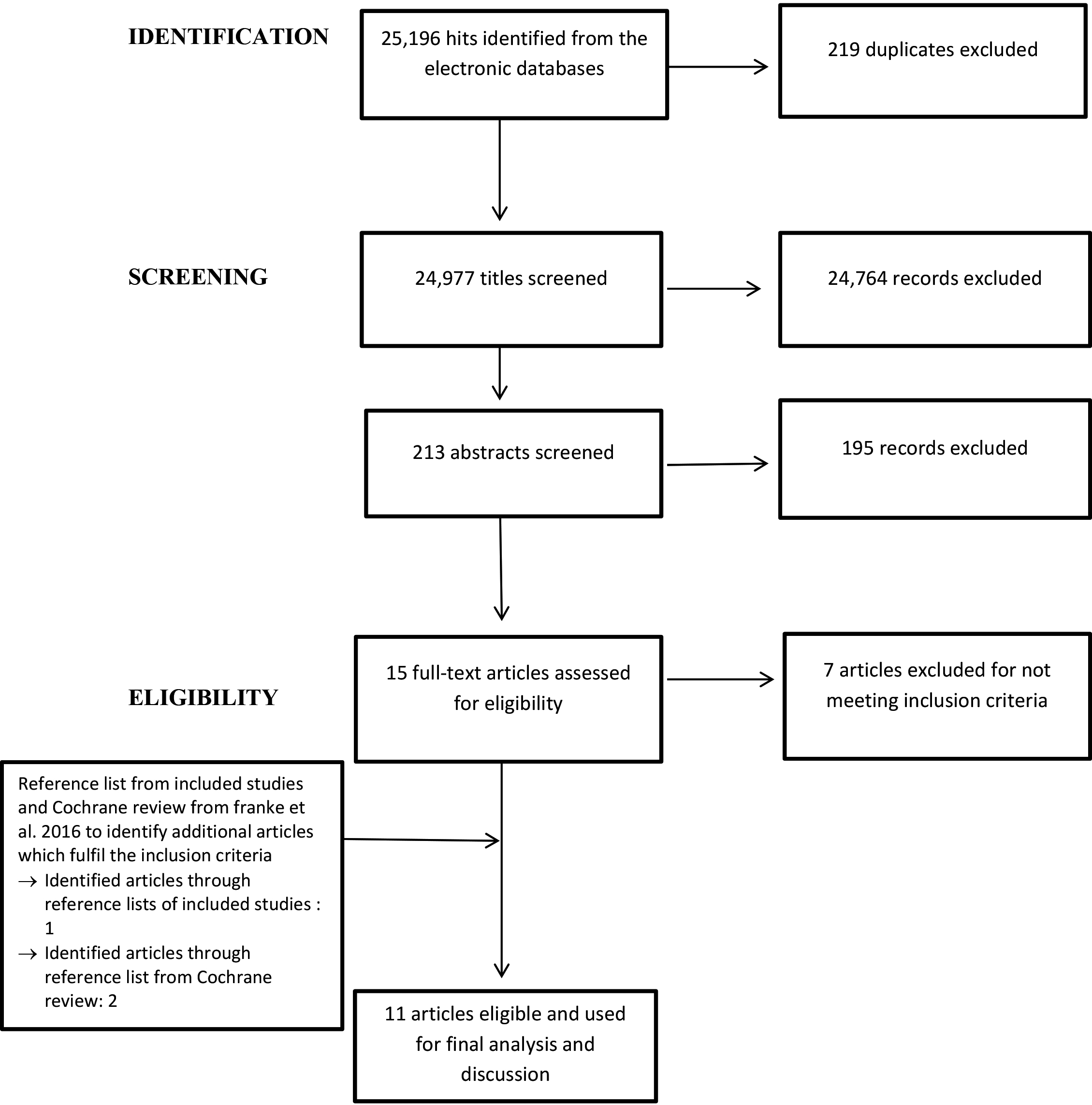
Figure 1.
Article selection process.
2.4Study selection
The process of article selection includes four steps: identification of relevant literature, screening of the title and abstract against inclusion and exclusion criteria (Table 1), assessing eligibility based on full-text screening to the in/exclusion criteria, and final inclusion of the article for the review [27, 28]. The number of records retrieved and included in each of these steps is depicted in Fig. 1. The electronic search was performed by the first author UAA. UAA and SSM screened the retrieved articles against the inclusion and exclusion criteria, first based on title and abstract, second based on the full text. The hand search existing of reference list screening was performed by UAA, and the screening of the resulting articles for study eligibility by title and abstract and subsequently full text was performed by UAA and SSM. Two experts in manual therapy and musculoskeletal research provided their expert opinion on the recommendations for appropriate electronic databases and relevance of any article that the reviewers disputed on with regards to the inclusion.
2.5Charting the data
A data charting form was developed as recommended by the work of Arksey and O’Malley [27] and used to extract and summarize the data from individual articles included in this scoping review. The data extracted includes general information about the article (title, author(s), journal and year of publication), and information on the study design, study setting, participants characteristics and methodology. Also, a summary of the main results, limitations and recommendations are presented in the data charting form.
2.6Summarizing and reporting findings
Arksey and O’Malley [27] describe the final stage of scoping reviews to provide an overview of the results of the reviewed articles, in this case, the reportage focuses on the results of the studies in regards to the effectiveness of MET in the management of chronic MLBP.
3.Results
3.1Population
The systematic search strategy as demonstrated in Fig. 1 yielded eleven articles which were considered eligible for this review [30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40]. Table 2 illustrates the details of the eleven articles used for the final analysis and discussion. All the studies were carried out in an urban setting, although in three studies the authors did not specify the location of the study [30, 31, 32]. Among the selected studies two studies were carried out in North Africa [30, 31], three were conducted in India [33, 34, 35], two in North America [36, 37], one in South America [38], and two in Europe [39, 40]. The study by Lamberth et al. [32] did not disclose in which geographic region the study was carried out, however, all authors are from Denmark and therefore we presume the study was conducted in Europe. Ten of the eleven studies performed a randomized controlled trial (RCT), while only one study used a case design [32]. Both male and female adult participants with chronic MLBP were recruited for all the studies and with age ranges of 20–60 years.
3.2Interventions
In all the selected studies, the effectiveness of MET was tested as outlined in Tables 2 and 3. However, in two of the studies [36, 37], the name MET was not used, rather the terms used were ‘manual therapy’ and ‘regional manual therapy’ respectively. In ten out of the eleven studies the interventions were administered by a physical therapist, and in one study [32] by a medical doctor with a diploma in musculoskeletal medicine. In four studies [35, 36, 37, 39] the interventions were exclusively conducted by physical therapists specialized in musculoskeletal therapy and many years of experience in the practice. Additionally, seven of the nine studies were conducted in hospital located in urban settings where patients were also recruited for study participation (Table 2). The study by Geisser and et al. [36] was carried out in a university spine laboratory on chronic MLBP patients. The studies by Ellythy [30, 31] and Rana et al. [35], did not specify the type of location (i.e. whether urban or rural) of the studies settings. The participants received multiple sessions of interventions ranging from 5 to 24 sessions, conducted within a span of 1 to 8 weeks. All studies aimed to determine the effectiveness of MET or its combination with other therapeutic interventions in the management of chronic MLBP. The other interventions MET was combined with included McKenzie method therapy, specific motor control exercises, conventional therapy, and G.D. Maitland’s concept of mobilization, myofascial release and segmental stabilization.
In the study by Szulc et al. [40] McKenzie techniques that involve hyperextension techniques, hyperextension with self-pressure or pressure applied by the therapist and hyper-extensive mobilization were used. The sagittal plane was used to apply the techniques following the rule of force progression. This procedure was applied isolated in one group and in-combination with MET in another group. The MET is a technique of post-isomeric relaxation at the end of each McKenzie session and involved the following parameters: 1) time of contraction equal to 7–10 seconds, 2) intensity of contraction corresponding to 20–35%, 3) 3 seconds of an interval between consecutive contraction phases, 4) 3 repetitions, 5) contraction of antagonist’s muscle at the terminal phase of the procedure, 6) passive return to the baseline position. This procedure is aimed at relaxing the erector spinae muscle group and was performed in a sitting position for 40 seconds. The third group of participants received standard physiotherapy treatment that involved massage, laser therapy, and transcutaneous electrical
Table 2
Study characteristics of the included studies
| Author(s) | Title | Participants | Study design | Setting | Intervention |
|---|---|---|---|---|---|
| Balthazard [35] | Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in patients with chronic non-specific low back pain: a randomized controlled trial | 42 participants (14 female and 28 male with a mean age of 42 | Randomized controlled trial | Lausanne, Switzerland (Urban) |
|
| Bindra [32] | A study on the efficacy of muscle energy technique as compared to conventional therapy on lumbar spine range of motion in chronic low back pain of sacroiliac origin | 30 participants (26 female and 4 male, mean age 41 | Randomized controlled trial | Ludhiana, India (Urban) |
|
| Dhinkaran et al. [29] | Comparative analysis of muscle energy technique and conventional physiotherapy in the treatment of sacroiliac joint dysfunction | 30 participants were randomly assigned into two intervention groups (15 persons each) | Randomized controlled trial | Ludhiana, India (Urban) |
|
| Ellythy [26] | Efficacy of Muscle Energy Technique Versus Strain Counter Strain on Low Back Dysfunction | 30 participants with an age range of 30 to 50 years were randomly assigned to two equal treatment groups (15 persons each) | Randomized controlled trial | Egypt, setting not specified |
|
| Ellythy [27] | Efficacy of muscle energy technique versus myofascial release on function outcome measures in patients with chronic low back pain | 40 male and female participants (age range 30–50 years) were randomly assigned to two intervention groups (20 persons each) | Randomized controlled trial | Egypt, setting not specified |
|
| Franca et al. [34] | Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain | 30 participants (mean age 42 | Randomized controlled trial | Sao Paulo, Brazil (Urban) |
|
| Geisser et al. [32] | A randomized, controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain | 100 participants (59 female and 41 male, mean age 40.7 | Randomized controlled trial | Michigan, USA (Urban) |
|
| Lamberth et al. [28] | Muscle energy technique: a useful aid to the manual treatment of low back pain? | 10 participants (age range 36–56) were enrolled in the study; however, only 4 remained in the study | Multiple single case study | Not specified |
|
|
Table 2, continued | |||||
|---|---|---|---|---|---|
| Author(s) | Title | Participants | Study design | Setting | Intervention |
| Rana et al. [31] | Comparative analysis of the efficacy of G.D. Maitland’s concept of mobilization and muscle energy technique in treating sacroiliac joint dysfunction | 45 participants with mean age 22.82 | Randomized controlled trial | India (Urban) |
|
| Szulc et al. [36] | Impact of McKenzie method therapy enriched by muscle energy technique on subjective and objective parameters related to spine function in patients with chronic low back pain | 60 men and women with a mean age of 44 years randomly assigned to 1 of 3 intervention groups (20 persons each) | Randomized controlled trial | Poznan, Poland (Urban) |
|
| Zafereo et al. [33] | Regional manual therapy and motor control exercise for chronic low back pain: a randomized clinical trial | 40 participants (25 female and 15 male) were randomly assigned into intervention groups (20 persons each). The mean age was 46.71 | Randomized controlled trial | Texas, USA (Urban) |
|
Table 3
Description of outcomes of the included studies
| Author(s) | Outcome measures/assessments | Variable response | Relative most effective intervention |
|---|---|---|---|
| Balthazard [35] | Visual analogue scale for assessment of pain intensity (pre and post assessment) | Improvement | MET/MT plus active exercises |
| Oswestry Disability Index (ODI) (pre, post assessment and at 3- and 6-month follow-up) | Improvement | MET/MT plus active exercises | |
| Fear Avoidance Belief Questionnaire (FABQ) for assessment of fear and avoidance beliefs (presented concerning physical activity and work subscales) (pre, post assessment and at 3- and 6-month follow-up) | No change for both subscales | ||
| Sorensen test for assessment of Erector spinae muscles endurance and Shirodo test for assessment of abdominal muscles endurance (pre, post assessment and at 3- and 6-month follow-up) | No change for Sorensen score | ||
| Improvement for Shirodo score | Sham therapy plus active exercises | ||
| Bindra [30] | Visual analogue scale (VAS) for assessment of pain intensity (pre and post-assessment) | Improvement | No difference |
| Oswestry Disability Index (ODI) for assessment of functional disability (pre and post-assessment) | Improvement | No difference | |
| Modified-modified Schober test for assessment of lumbar spine ROM (pre and post-assessment) | Improvement | No difference | |
| Dhinkaran et | Oswestry Disability Index (ODI) for assessment of functional disability (pre and post-assessment) | Improvement | MET plus corrective exercises |
| al. [29] | Numeric Rating Scale (NRS) for assessment of pain intensity (pre and post-assessment) | Improvement | MET plus corrective exercise |
| Ellythy [26] | McGill pain questionnaire for the assessment of pain intensity (pre and post-assessment) | Improvement | No difference |
| Modified Schober’s test for the assessment of lumbar ROM (flexion and extension) (pre and post) | Improvement | No difference | |
| Oswestry disability index (ODI) for the assessment of functional disability (pre and post) | Improvement | No difference | |
| Ellythy [27] | McGill Pain Questionnaire (MPQ) – short form for assessment of pain intensity and quality (pre and post-assessment) | Improvement | No difference |
| Inclinometers for assessment lumbar spine ROM (pre and post-assessment) | Improvement | No difference | |
| Oswestry Disability Index (ODI) for the assessment of functional disability (pre and post-assessment) | Improvement | No difference | |
| Franca et al. [34] | Visual analogue scale (VAS) for assessment of pain intensity and McGill Pain Questionnaire – long-form for assessment of pain intensity and quality (pre and post-assessment) | Improvement | Stabilization exercise better than MET (in form of muscle stretching) |
| Oswestry Disability Index (ODI) for assessment of functional disability (pre and post-assessment) | Improvement | Stabilization exercise better than MET (in form of muscle stretching) | |
| Pressure Biofeedback Unit for assessment of transverse abdominus TrA muscles contraction rates (pre and post-assessment) | Improvement | Only stabilization exercise improve TrA muscles contraction or activation rate | |
| Geisser et | McGill Pain Questionnaire (MPQ) – long-form for assessment of pain intensity and quality (pre and post-assessment) | Improvement | MET-SE |
| al. [32] | Quebec Back pain Disability Scale for assessment of functional disability (QBPDS) (pre and post-assessment) | No change | |
| Global Rating of Change Scale (GROC) for assessment of self-perceived change in health status (pre and post-assessment) | No change | ||
| Multidimensional pain inventory for assessment of pain interference (pre and post-assessment) | No change | ||
| Lamberth et al. [28] | Modified-modified Schober’s test/tape measure for the assessment of trunk ROM (pre, during and at the end of treatment sessions assessments). But during every treatment sessions, ROM is assessed at the beginning and end of the session | Improvement | MET |
| Visual analogue scale and Pain Numeric Rating Scale for the assessment of pain intensity (pre, during, end of treatment and follow-ups assessments) | Improvement | MET | |
| Roland Morris Disability Questionnaire (RMDQ) for assessment of functional disability (pre, during, end of treatment and only at 6 | Improvement | MET |
|
Table 3, continued | |||
|---|---|---|---|
| Author(s) | Outcome measures/assessments | Variable response | Relative most effective intervention |
| Rana et al. [31] | Visual analogue scale (VAS) for assessment of pain intensity (pre and post-assessment) | Improvement | No difference |
| Conventional goniometer for assessment of hip ROM (flexion, external/internal rotation, abduction/adduction) (pre and post-assessment) Measuring tape for assessment of lumbar ROM (flexion, extension, side flexion) (pre and post-assessment) | Improvement | MET plus exercise | |
| Oswestry Disability Index (ODI) for assessment of functional disability (pre and post-assessment) | Improvement | No difference | |
| Szulc et al. [36] | Elecrogoniometer for assessment of all spinal segments ROM (cervical, thoracic and lumbar region) (pre, post and 3-month follow-up assessment) | Improvement | McKenzie plus MET |
| Visual analogue scale (VAS) for assessment of pain intensity (pre, post and 3-month follow-up assessment) | Improvement | McKenzie plus MET and McKenzie alone | |
| Oswestry Disability Index (ODI) for assessment of functional disability (pre, post and 3-month follow-up assessment) | Improvement | McKenzie plus MET and McKenzie alone | |
| Magnetic Resonance Imaging (MRI) for assessment of the structure of the spinal discs (disc herniation) (pre, post and 3-month follow-up assessment) | Improvement | McKenzie plus MET | |
| Zafereo et al. [33] | Oswestry Disability Index (ODI) for assessment of functional disability at 2 | Improvement | No difference |
| Numeric Rating Scale (NRS) for assessment of pain intensity at 2 | Improvement | No difference | |
| Fear Avoidance Belief Questionnaire (FABQ) for assessment of fear-avoidance beliefs at 2 | Improvement | No difference | |
| Pain Catastrophizing Scale (PCS) for assessment of pain catastrophizing at 2 | Improvement | No difference | |
| Global Rating Of Change Scale (GROCS) for assessment of the self-perceived effect of treatment at 2 | Improvement | No difference | |
nerve stimulation (TENS) applied to the lumbosacral region. Additionally, the participants were asked to perform general exercises for strengthening spinal and abdominal muscles at home.
The study by Balthazard et al. [39] combined MET with active exercises in group A and compared it with placebo therapy combined with active exercises in group B. The MET intervention involves a hold-relaxed technique performed on an ilium dysfunction with the participant in side-lying, high velocity, and low amplitude dynamic thrust (manipulation), a rotational-lateral flexion thrust performed on a stiffed vertebral segment with the participant in side-lying. Another mobilization technique was added that involves passive accessory intervertebral movements, a central or unilateral posterior-anterior pressure applied on painful or stiffed vertebral segment(s) with the participant lying prone [39]. The sham treatment involves detuned ultrasound applied to the patient’s painful and/or inflammatory site. The participant did not know the ultrasound was inactivated and, therefore, ineffective. The active exercises in both groups involved; 1) mobility exercises throughout the eight therapeutic sessions to improve participant’s spinal range of motion and pain, 2) passive stretching exercises after the second session, for muscle groups that tend to shorten (erector spinae, hamstring, iliopsoas, rectus femoris, piriformis), to relieve muscular tension and improve low back mobility, 3) motor control exercises at the fourth session for active recruitment of stabilizing trunk muscles, 4) strengthening exercises at the sixth or seventh session to increase the strength of weak superficial trunk muscles. They were performed at 60–70% of maximum voluntary contraction, against the resistance of an adapted rubber band, 2 sets of 20 repetitions, 5) two home mobility exercises (pelvic tilt and low back lateral flexion, in supine), to be performed daily, twice a day, 2 sets of 10 repetitions. After the third or fourth therapeutic session, the recommendation of home exercises changed to stretching and motor control exercises. The therapeutic sessions lasted for thirty 30 minutes in each group and consisted of 5 to 10 minutes of MET/Manual therapy intervention followed by an active exercise for group A and 5 to 10 minutes of ST intervention followed by an active exercise for group B.
Geisser et al. [36] compared MET, sham MET, a specific adjuvant exercise program and a non-specific exercise program. The principal mechanism of the MET procedure was similar to the one used by Szulc et al. [40]. The sham MET involved controlled corrective positioning of the participants, and specific adjuvant exercises aimed at treating specific musculoskeletal dysfunction including stretching, strengthening and self-correction exercises, while the non-specific exercise program, which included aerobics and lower limb stretching exercises, did not target any observed dysfunctions of the lumbar musculoskeletal system.
Bindra compared MET to conventional therapy [34]. The MET protocol was similar to the previous studies but in this study, the parameters varied depending on the level of dysfunction observed during participant screening. The conventional therapy group included therapeutic ultrasound, TENS and mobility exercises (i.e. knee to chest exercise and pelvic rotation to either side with a hold of 10 seconds in each position and 8–10 repetitions were performed).
Dhinkaran et al. [33] also compared MET to conventional therapy, the latter comprising of TENS. However, both intervention groups also received corrective exercises for which participants were asked to flex the hip and bring the knee into the ipsilateral axilla from a supine, sitting or standing position.
Rana et al. [35] compared MET to Maitland’s concept of mobilization and added therapeutic exercises to each intervention. In their study, the MET application was dependent on the extent of the presented dysfunctions established during an assessment.
Ellythy conducted two different studies [30, 31]to determine the efficacy of MET compared to other therapeutic interventions. The first study compared MET (group A) versus strain counter strain technique (group B) which is described by the author as another indirect manipulative procedure [30]. Also, both groups of participants received standard physiotherapy treatment that involved infrared radiation, ultrasound therapy, and therapeutic exercises (i.e. finger to toe flexion, bridging exercise, back extension in prone, sit-ups, knee to the chest in supine and stretching of low back muscles). The second study compared MET with a myofascial release which is directed toward the soft tissues of the body, particularly the muscles and fascia [31]. In this study also a standard physiotherapy procedure was added to both groups, which involved infrared radiation, TENS, ultrasound therapy, and therapeutic exercises (i.e. finger to toes, bridging, back extension in prone, sit-ups, knee to chest and stretching back muscles).
A modified form of MET in the form of muscle stretching was compared with segmental stabilization exercises in a study by Franca et al. [38] aimed to restore motor control of the deep trunk muscles (specifically transverse abdominus (TrA) and lumbar multifidus muscles (LM). Emphasis was placed on the pattern of activation of the TrA in individuals with chronic MLBP.
The only pilot study among the included studies comprised of a multi single-case study aimed at assessing the short and long-term effects of MET in patients with chronic MLBP [32]. The type of MET procedure used in this study is attributed to Fred L. Mitchell Sr [25].
Zafereo et al. [37] administered regional manual therapy to patients with chronic MLBP. Although the procedure is not entirely MET, the concept was to apply different manual therapy techniques. The choice of initiating, grading or suspending any specific technique and duration of treatment was left to the discretion of the treating therapist. The protocol was compared with standard physiotherapy, and motor control exercises were added to both interventions.
3.3Outcomes
The main outcomes of interest were pain intensity, functional disability, and trunk range of motion (ROM). Pain and disability-related outcomes were measured using self-reported clinical outcome measures that included visual analogue scales, numeric pain rating scales, or validated questionnaires like the Oswestry Disability Index (ODI) or Quebec Back Pain Disability Scale (QBPDS). To measures trunk ROM, different measurement tools and procedures were used such as electrogoniometres, inclinometers, measuring tape and performance of the modified-modified Schober test. Besides, one study used a pressure biofeedback unit to assess the activation/contraction rate of the TrA muscles to evaluate treatment effects on motor control [38]. Another study used the Sorensen test to assess the endurance of the erector spinae muscles and the Shirado test to assess the endurance of the abdominal muscles [39]. Furthermore, the structure of the spinal discs was assessed using magnetic resonance imaging (MRI) in one of the studies [40].
Generally, MET was found to be effective in improving the outcomes in patients with chronic MLBP in all included studies. Some of these studies found that adding additional exercises to MET was more effective than MET alone. None of the studies showed any adverse effect on the application of MET intervention alone or in combination with other therapeutic procedures, as none of the outcome variables showed diminishment. However, a couple of studies have reported that the MET in combination with other treatment interventions did not provide better effects in comparison to the other interventions on some outcome variables. Geisser et al. [36] reported that MET plus specific exercises of the trunk muscles was effective in reducing pain, but there was no significant change in functional disability. However, the authors argued that it is possible that reducing solely the LBP complaints does not address psychosocial or other factors that may contribute to disability. Franca et al. [38] reported that although MET (in the form of muscle stretching) is effective in improving outcomes (i.e. pain, ROM, functional disability and spinal disc structure) in patients with chronic MLBP, segmental stabilization exercises provide even better results and additionally improved motor control as reflected by the activation of the TrA which was not the case for MET. Also, the study by Balthazard et al. [39] reported a pronounced decline in abdominal muscle endurance in participants treated with MET and active exercise compared to participants treated with sham therapy and active exercise, however, a clear explanation for this observation could not be given and thus further studies were recommended to enhance the understanding of the relationship between MET, active exercise and abdominal muscles endurance. However, the latter study did confirm the immediate analgesic effect of MET in patients’ chronic MLBP.
4.Discussion
Generally, there is a scarcity of published articles on the effect of MET on chronic MLBP. Only one published systematic Cochrane review of RCTs on the effectiveness of MET on MLBP exists and reported that MET as a standalone treatment or added to other treatment intervention provides no better effects compared to other therapies on chronic pain symptoms and disability in patients with chronic MLBP [22]. These conclusions were based on low-quality evidence and thus further research was recommended. The current scoping review focused on the effects of MET in chronic MLBP for which the literature was collected systematically and was not limited to RCTs or dependent on quality levels providing a broader overview of the existing literature and description of the used methodologies.
All studies identified and included in this scoping review assessed outcomes following the recommendation of the World Health Organization International Classification of Functioning, Disability and Health (WHO-ICF) framework, showing that MET alone or in combination with other therapeutic procedures improves pain, functional disability, trunk ROM and spinal disc derangement. The majority of the studies reported immediate effects of the interventions, only three out of the eleven studies reported long term effects and concluded that the therapeutic effects were retained at three months [37, 39, 40] and at six months [39] follow-up period.
However, some studies demonstrated that MET alone or its combination with other therapeutic procedures provided equal or no better results when compared to other interventions on specific outcomes that includes; pain intensity [30, 31, 34, 35, 37], fear avoidance belief [37, 39], functional disability [30, 31, 34, 35, 37], trunk range of motion [30, 31, 34], trunk muscles endurance [39] and self-perceived effect of treatment [36, 37].
Important limitations and strengths of each study were considered before making these conclusions. The case study by Lamberth et al. [32] aimed to assess the short- and long-term benefits of MET in patients with chronic MLBP in a pilot study to examine whether there were indications to set up a larger RCT. Therefore, a multi single-case design was carried out on a limited sample of four MLBP patients, the assessment was carried out at pre, during and at the end of the treatment with follow-up at two, four and six weeks post-treatment (details in Table 3). In this study, small sample size, lack of a control group and blinding of the assessors resulted in high risks of bias. The six-week follow-up was added in the study protocol to determine the long-term effect, only pain and function ability were assessed at this time point and mobility measurements were not repeated nor were patients re-examined to identify possible new dysfunctions in the spinal region. Although the limitations of this study should be taken into account, significant reductions in pain, functional disability and improvement of trunk mobility were reported following MET intervention, and the effects on pain and functional disability were sustained at six weeks follow-up. However, from the included RCTs only two had a long-term follow-up assessment, thus emphasizing why it is important to take the results of case studies such as the one by Lamberth et al. into consideration. The included RCTs generally did not include a follow-up period and consequently did not examine the long term effects of MET. However, the two exceptions were the studies of Balthazard et al. [39] and Szulc and et al. [40], the first one had a period of three and six month follow-ups and reported a sustained and long term effect of MET plus active exercise on pain and functional disability in patients with chronic MLBP, while the latter included a three month follow-up period and reported sustained therapeutic effects of MET plus McKenzie technique on pain, ROM, functional disability and spinal disc structure in patients with chronic MLBP.
Weaknesses from the RCTs included inadequate sample size, non-presentation of sampling procedure which could lead to sampling errors, lack of follow-up measures, single blinding (instead of the double-blind method which is the gold standard for RCTs). Furthermore, the intervention periods and number of sessions might have been too limited (1–8 weeks and 3–12 sessions respectively) to be able to reverse some outcomes in this chronic population. These limitations can affect the generalizability of the findings of these studies in clinical practice. Also, to the limitations of each study, this review observed that the studies have several distinct differences in regards to the design. These differences included the nature of the MET interventions, number of intervention arms, co-intervention(s) alongside MET, method of randomization, nature and characteristics of participants, number of treatment sessions, duration of treatment sessions and duration of the intervention period. These differences make it difficult to compare studies and draw firm conclusions.
On the other hand, the included studies also showed some important strength such as the use of standard outcome tools with high reliability and validity, although most of the outcome tools were based on self-report and consequently could not be considered as empirical evidence. However, some of the studies also included objective measurement tools such as pressure biofeedback [38], inclinometer [31], electrogoniometry and MRI [40].
However, even though there were several limitations to these studies, clinical recommendations can be made based on their strengths. Ten of the studies used an RCT design to study the effect of the MET intervention on selected outcomes in patients with chronic LBP. A relatively high-quality study by Szulc et al. [40] was included, which had three arms (two interventions i.e. McKenzie alone and McKenzie plus MET, then standard physiotherapy procedure as control) with the interventions administered in 10 sessions, performed on 5 consecutive weekdays, and was well designed including proper randomization and a three month follow-up period. Additionally, MRI was used to assess the degree of degeneration of the spinal discs and to prove the efficacy of the intervention at the tissue level by taking measurements before and after the intervention. The result from this study shows that the implemented therapeutic methods (McKenzie plus MET) exerted variable time-dependent effects on the structural parameters of the spine from MRI in patients with chronic MLBP as manifested by a reduced size of spinal disc herniation [40].
It is important to note that the majority of the studies included in this review were carried out in middle and high-income countries (mostly high-income countries) as demonstrated and were conducted in urban settings. Therefore, participants were recruited from urban settlements and thus the generalizability of the study findings to the overall population needs to be done with caution. Therefore, studies on participants from low and middle-income countries and rural areas with chronic MLBP need to be performed to examine the feasibility and effectiveness of MET in these populations.
4.1Implications to research and practice
The findings of this study provide information which can be used to help steer the development of an effective treatment protocol for MET for the rehabilitation of patients with chronic MLBP by reducing the rate of recurrence, prevent structural and functional alterations and improve functional disabilities. Studies on the effectiveness of MET in populations from the middle to low-income countries and/or rural areas are limited and therefore the effectiveness of and feasibility to implement this intervention has not yet been well researched globally. We hope that this study will stimulate interest in further research involving MET in the management of chronic MLBP among the general and specific populations, because of the dearth of studies on the subject. Consequently, it is recommended that further studies focus on examining the efficacy of the intervention using a robust methodology including a clear description of the setting where subjects were recruited and treated, the used techniques and related decision making, therapist experience, and a long term follow-up.
Additionally, this review will help clinicians to understand the clinical importance of application of MET in combination with other therapeutic procedures as an appropriate management plan for chronic MLBP, which will improve patients’ functional disabilities. This review serves as a resource material, reference or guide that researchers and clinicians can consult to obtain useful information about MET in the rehabilitation of chronic MLBP and potentially other related musculoskeletal conditions.
An additional remark is that we have noticed that MET is not included in many clinical practice guidelines for the management of MLBP, while the finding of this study reveals MET studies with encouraging outcomes. Therefore, we recommend that the MET procedure needs to be included in future clinical practice guidelines for the management of chronic MLBP.
Finally, with the increase in the prevalence of chronic MLBP, there is a need for funding agencies to support research that explores and analyses interventions for the management of this condition as MET offers a cheap and easy to apply intervention for this population. This is highly recommended especially for the benefit of patients from low and middle-income countries.
4.2Limitations
First, a limitation of this review was the inclusion of studies that are not RCTs of which one was a case study design while another was a pilot study. However, following the scoping review method, it is valid to include studies with designs of lesser quality and a range of different methodologies to entirely chart the available evidence related to the research question and broadening the level of evidence for analysis and discussion.
Second, this review included only articles written in English and published in peer review journals. This might have limited the evidence by not including articles written in other languages that may have been eligible for inclusion to this review. However, this criterion was adopted to avoid errors that may occur in representing accurately evidence reported in articles published in languages other than English.
Finally, two studies included for the review analysis used muscular stretching and regional manual therapy instead of MET as their manual therapy intervention [37, 38], however, a thorough expert review of both procedures indicated that this technique while not being labelled in the papers as MET could indeed be considered as meeting the principles of MET.
5.Conclusion
The small number of identified articles emphasizes the dearth of literature on MET as a standalone intervention or in combination with other therapeutic interventions in the management of chronic MLBP. Furthermore, from the analysis of these articles, it can be concluded that MET in a combination of with other therapeutic procedures is a favourable approach that is safe and effective for patients with chronic MLBP and consequently may provide numerous physical and psychosocial benefits. Additionally, even as a standalone intervention MET shows promising results for the improvement of pain, trunk flexibility and functional disability in patients with chronic MLBP. But further research studies with robust methodology are needed to standardize the MET procedure and provide standardized reporting (on decision making, used MET techniques, therapist experience, etc.) to determine whether it can produce long term improvements in the management of chronic MLBP.
Acknowledgments
Prof. Dr Jessica Van Oosterwijck (PhD) is a post-doctoral research fellow funded by the Research Foundation – Flanders (FWO) [12L5619N and 12L5616N]. Dr Kaka Bashir (PhD), senior lecturer of Physiotherapy at Bayero University Kano and Dr Zubair Usman (PhD), consultant Physiotherapist at Rasheed Shekoni Teaching Hospital, both in Nigeria, are appreciated for their help with expert review and recommendation of some relevant articles for the study.
Conflict of interest
None to report.
Funding
The study is funded by the College of Health Science of the University of KwaZulu-Natal post-graduate student bursary (internal funding). The institution has no interest or role in the design of the study, writing the manuscript, collection and analysis of data. No external funding is received from any source for the study.
References
[1] | Manchikanti L. Association of pain management anesthesiologists® topical review epidemiology of low back pain. Pain Physician. (2000) ; 3: (2): 167–92. |
[2] | Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. (2012) ; 64: (6): 2028–37. |
[3] | Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D, et al. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord. (2014) ; 15: (1): 50. doi: 10.1186/1471-2474-15-50. |
[4] | Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. (2014) ; 73: (6). |
[5] | Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) ; 388: (10053). |
[6] | Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. (2010) ; 24: (6): 769–81. doi: 10.1016/j.berh.2010.10.002. |
[7] | Majid K, Truumees E. Epidemiology and natural history of low back pain. Semin Spine Surg. (2008) ; 20: (2): 87–92. doi: 10.1053/j.semss.2008.02.003. |
[8] | Woolf AD, Erwin J, March L. The need to address the burden of musculoskeletal conditions. Vol. 26, Best Practice and Research: Clinical Rheumatology. (2012) . 183–224. doi: 10.1016/j.berh.2012.03.005. |
[9] | Woolf AD, Brooks P, Åkesson K, Mody GM. Prevention of musculoskeletal conditions in the developing world. Vol. 22, Best Practice and Research: Clinical Rheumatology. (2008) . 759–72. doi: 10.1016/j.berh.2008.07.003. |
[10] | Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) ; 391: (10137): 2356–67. |
[11] | Vos T, Allen C, Arora M, Barber RM, Brown A, Carter A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) ; 388: (10053). |
[12] | von Korff M. Studying the natural history of back pain. Spine (Phila Pa 1976). (1994) ; 19: (Supplement): 2041S–2046S. |
[13] | Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4: european guidelines for the management of chronic nonspecific low back pain. Eur Spine J. (2006) ; 15: (SUPPL. 2): 192–300. |
[14] | Desomer A, Van WAmbeke P, Jonckheer P. Klinische richtlijn rond lage rugpijn en radiculaire pijn. Tijdschr Geneeskd [Internet]. (2017) ; 73: (19): 1182–95. Available from: https://www. vavp.be/userfiles/klinische richtlijne rond lager rugpin en radiculaire pijn tvg.pdf. |
[15] | Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. (2018) ; 391: (10137): 2368–83. |
[16] | Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine (Phila Pa 1976). (2001) ; 26: (11): 243–8. |
[17] | Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, et al. National clinical guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. (2018) ; 27: (1): 60–75. |
[18] | Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Vol. 166, Annals of Internal Medicine. (2017) . |
[19] | National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management (NG59). Nice. (2016) ; (November 2016): 1–18. Available from: https://www.nice.org.uk/guidance/ng59. |
[20] | Akodu A, Kareem R, Faniyi O. Management of low back pain: knowledge and adherence to clinical practice guidelines amongst physiotherapists in selected hospitals in lagos state. Res J Heal Sci. (2016) ; 4: (3): 203. |
[21] | Franke H, Fryer G, Ostelo RW, Kamper SJ. Muscle energy technique for non-specific low-back pain. Cochrane Database of Systematic Reviews. 2015(2). doi: 10.1002/14651858.CD009852.pub2. |
[22] | Franke H, Fryer G, Ostelo RWJG, Kamper SJ. Muscle energy technique for non-specific low-back pain. A Cochrane systematic review. Vol. 20, International Journal of Osteopathic Medicine. (2016) . 41–52. |
[23] | Chaitow L. Muscle energy techniques [Internet]. Churchill Livingstone/Elsevier; (2006) [cited 2018 Feb 27]. 346. Available from: https://books.google.co.za/books?hl=en&lr=&id=GZd046gACgIC&oi=fnd&pg=PP7&dq=(MET)+is+classified+as+an+active+technique+in+which+the+patient+voluntarily+uses+his+muscles+from+a+precisely+controlled+position+in+a+specific+direction,+against+a+distinctly+executed+counterforce+by+the+therapist&ots=zbRWxPT-5N&sig=XlclBAppnNGxensj7Nm0KIsegNQ&redir_esc=y#v=onepage&q&f=false. |
[24] | Fryer G. Muscle energy concepts – a need for change. J Osteopath Med. (2000) ; 3: (2): 54–9. |
[25] | Mitchell FL, Mitchell PKG. The muscle energy manual. (1999) [cited 2017 May 31]; 4196: (517): 48826. Available from: http://www.shortdwarf.com/main/mitchell_muscle_energy_manual.PDF. |
[26] | Fryer G. International journal of osteopathic medicine muscle energy technique: an evidence-informed approach. Int J Osteopath Med. (2011) ; 14: (1): 3–9. doi: 10.1016/j.ijosm.2010.04.004. |
[27] | Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. (2005) ; 8: (1): 19–32. doi: 10.1080/1364557032000119616. |
[28] | Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) ; 5: (1): 69. doi: 10.1186/1748-5908-5-69. |
[29] | Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. (2014) ; 67: (12): 1291–4. |
[30] | Ellythy MA. Efficacy of muscle energy technique versus strain counter strain on low back dysfunction. Bull Fac Phys Ther. (2012) ; 17: (2): 29–35. |
[31] | Ellythy MA. Efficacy of muscle energy technique versus myofascil release on function outcome measures in patients with chronic low back pain. Bull Fac Phys Ther [Internet]. (2012) ; 17: (2): 29–35. |
[32] | Lamberth L, Hansen KL, Bloch-Thomsen M, Silbye P, Remvig L. Muscle energy technique: a useful aid to manual treatment of low back pain? J Orthop Med [Internet]. (2005) ; 27: (1): 17–21. doi: 10.1080/1355297X.2005.11736248. |
[33] | Dhinkaran M, Sareen A, Arora T. Comparative analysis of muscle energy technique and conventional physiotherapy in treatment of sacroiliac joint dysfunction. Indian J Physiother Occup Ther An Int J. (2011) ; 5: (4): 127–30. |
[34] | Bindra S. A study on the efficacy of muscle energy technique as compared to conventional therapy on lumbar spine range of motion in chronic low back pain of sacroiliac origin. Hum Biol Rev. (2013) ; 2: (4): 336–48. |
[35] | Rana K, Bansa F, Savita A. Comparative analysis on the efficacy of G.D. Maitland’s concept of mobilization and muscle energy technique in treating sacroiliac joint dysfunction. J Physiother and Occupational Therapy. (2009) ; 3: (2): 18–21. |
[36] | Geisser ME, Wiggert EA, Haig AJ, Colwell MO. A randomized, controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain. Clin J Pain. (2005) ; 21: (6): 463–70. |
[37] | Zafereo J, Wang-price S, Roddey T, Brizzolara K, Zafereo J, Wang-price S, et al. Regional manual therapy and motor control exercise for chronic low back pain: a randomized clinical trial. J Man Manip Ther. (2018) ; 9817: : 1–13. doi: 10.1080/10669817.2018.1433283. |
[38] | França FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther [Internet]. (2012) ; 35: (4): 279–85. doi: 10.1016/j.jmpt.2012.04.012. |
[39] | Balthazard P, de Goumoens P. Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in. Bmc. (2012) ; 1–11. doi: 10.1186/1471-2474-13-162. |
[40] | Szulc P, Wendt M, Waszak M, Tomczak M, Cieślik K, Trzaska T. Impact of mckenzie method therapy enriched by muscular energy techniques on subjective and objective parameters related to spine function in patients with chronic low back pain. Med Sci Monit. (2015) ; 21: : 2918–32. |




