Clinical application of two types of Hook-Wire needle localization procedures for pulmonary small nodule biopsy
Abstract
BACKGROUND:
With the widespread use of low-dose spiral computed tomography (LDCT) and increasing awareness of personal health, the detection rate of pulmonary nodules is steadily rising.
OBJECTIVE:
To evaluate the success rate and safety of two different models of Hook-Wire needle localization procedures for pulmonary small nodule biopsy.
METHODS:
Ninety-four cases with a total of 97 pulmonary small nodules undergoing needle localization biopsy were retrospectively analyzed. The cases were divided into two groups: Group A, using breast localization needle steel wire (Bard Healthcare Science Co., Ltd.); Group B, using disposable pulmonary nodule puncture needle (SensCure Biotechnology Co., Ltd.). All patients underwent video-assisted thoracoscopic surgery (VATS) for nodule removal on the same day after localization and biopsy. The puncture localization operation time, success rate, complications such as pulmonary hemorrhage, pneumothorax, hemoptysis, and postoperative comfort were observed and compared.
RESULTS:
In Group A, the average localization operation time for 97 nodules was 15.47
CONCLUSIONS:
The disposable pulmonary nodule puncture needle is safer and more effective in pulmonary small nodule localization biopsy, exhibiting increased comfort compared to the breast localization needle. Additionally, the incidence of complications is significantly lower.
1.Introduction
With the widespread use of low-dose spiral computed tomography (LDCT) and increasing awareness of personal health, the detection rate of pulmonary nodules is steadily rising. Research [1] indicates an incidence of 35.5% for pulmonary nodules, with 0.54% being diagnosed as lung cancer. The National Lung cancer Screening Trial (NLST) results show a 20% reduction in lung cancer mortality with LDCT screening compared to standard chest X-rays [2]. Due to the extensive application of LDCT, more early-stage pulmonary nodules, especially Ground Glass nodules (GGN), are being discovered. Currently, the primary treatment for pulmonary nodules is video-assisted thoracoscopic surgery (VATS), which is an effective, minimally invasive, and feasible therapeutic technique [3]. However, performing VATS for the resection of pulmonary nodules, especially invisible and untouchable GGN, poses significant challenges. Existing literature has highlighted the higher safety of hook-wire needle localization for pulmonary nodules before VATS, not only reducing surgery time but also significantly decreasing the chance of conversion to open thoracotomy.
Various techniques for pulmonary nodule localization have been reported, including Hook-Wire needle, spring coil, liquid material injection localization (methylene blue, etc.), bronchoscopy-assisted CT virtual 3D (three dimensions) assisted localization, each with its own advantages and disadvantages [4]. According to our previous experience and literature review, Hook-Wire needle is the most commonly used and reliable method for localization. However, there is limited comparative research among different models of Hook-Wire needles. In this study, we aim to collect and analyze information on various complications and patient comfort during surgeries involving two different models of needles (breast localization needle and disposable pulmonary nodule puncture needle). Our goal is to explore the effectiveness and safety advantages of these two needle models in nodule biopsy localization.
2.Materials and methods
This study employed two different models of Hook-Wire localization needles. The first one is the breast localization needle [Bard Healthcare Science (Shanghai) Co., Ltd.] with a standard number: National Medical Devices Registration: 20163771636, specifications: 20 G/10.7 cm. It is a tail-wired localization needle (Group A). The second one is the disposable pulmonary nodule puncture needle [Ningbo SensCure Biotechnology Co., Ltd.] with National Medical Devices Registration: 20193150175, specifications: 20 G/10 cm. It is a tail-soft-wired localization needle (Group B). Surgical time, complications, patient comfort, puncture depth, and other factors were statistically collected and analyzed during the puncture localization to compare the efficiency of the Hook-Wire needle puncture method and its clinical benefits.
2.1Clinical patient data and grouping
Patient data were collected from Xiamen Chang Gung Hospital Radiology Department from June 2019 to April 2023 for CT-guided pulmonary small nodule localization biopsy. A total of 94 patients with 97 pulmonary nodules were included (Table 1), including 46 males and 48 females. Patients using different needles were divided into two groups, namely Group A using the breast localization needle (53 nodules) and Group B using the disposable pulmonary nodule puncture needle (44 nodules).
Table 1
Basic parameters
| Bard Localization Needles 53 (Group A) | SensCure Localization Needles 44 (Group B) | |
|---|---|---|
| Average age | 53.32 | 51.11 |
| Gender | ||
| Male | 32 | 14 |
| Female | 21 | 27 |
| Nodule diameter | ||
| Nodule localization | ||
| Left upper lobe | 8 | 8 |
| Left lower lobe | 12 | 8 |
| Right upper lobe | 14 | 11 |
| Right middle lobe | 2 | 6 |
| Right lower lobe | 17 | 11 |
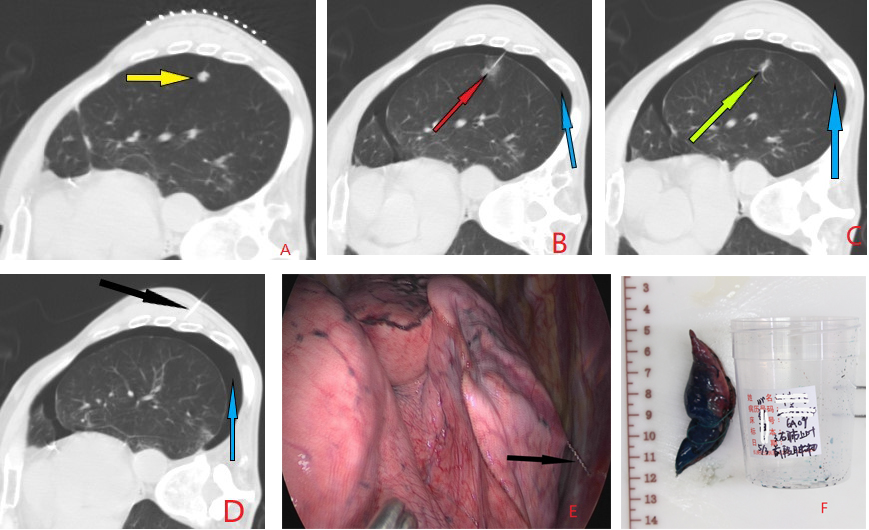
Figure 1.
Depicts the case of a single patient with a nodule in the left lower lobe (highlighted by yellow arrows) in the right lateral decubitus position. Puncture was performed using a breast localization needle: A. Pre-puncture localization of the nodule.B. After adjusting the angle of the puncture needle, it was inserted into the lung, revealing alveolar hemorrhage (indicated by red arrows) and a small pneumothorax (indicated by blue arrows). C. Release of the hook-wire, with the distal end anchored (indicated by green arrows) within 1 cm of the lesion. D. Post-release scan confirming the position of the localization needle and assessing lung complications. The steel wire tail (indicated by black arrows) was then externally ligated.The difficulty in securing the metal tail wire after hook-wire anchoring may lead to increased friction with the chest wall, resulting in a higher likelihood of secondary pneumothorax and alveolar hemorrhage, contributing to a less favorable patient experience.E and F: Surgical field views observing the condition of the hook-wire and postoperative excised pathological specimens, with the specimens removed for further examination after detaching the localization needle.
2.2Methods
All patients underwent procedures guided by Siemens Dual-Source CT (SOMATOM Force, 2
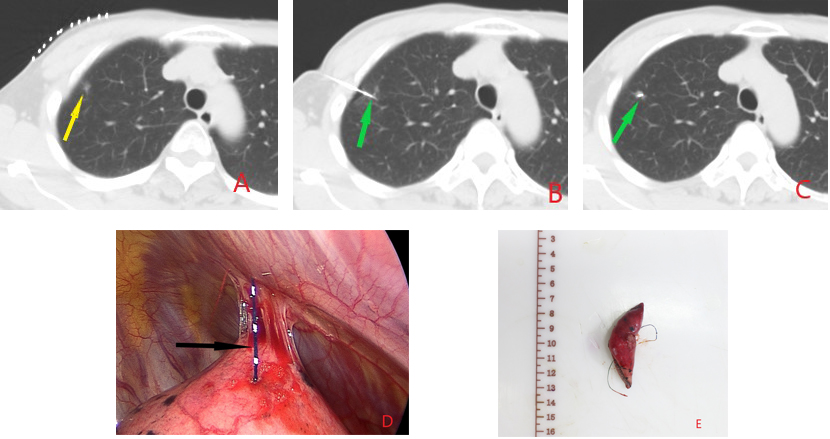
Figure 2.
Illustrates the case of the same patient with a nodule in the right upper lobe (highlighted by yellow arrows) in the supine position. Puncture was performed using a disposable pulmonary nodule puncture needle: A. Pre-puncture localization of the nodule. B. After adjusting the angle of the puncture needle(indicated by green arrows), it was inserted into the lung. C. Post-release scan confirming the position of the localization needle (indicated by green arrows) and assessing lung complications. The steel wire tail was then externally ligated. No alveolar hemorrhage or pneumothorax was observed within the lung, and the tail wire was easily secured after hook-wire anchoring, providing a comfortable experience for the patient. D and F. Surgical field views observing the condition of the hook-wire (indicated by black arrows) and postoperative excised pathological specimens. The specimens were sent for examination, carrying the hook-wire along for further analysis.
2.3Outcome measures and data processing
(1) Incidence of alveolar hemorrhage during the localization biopsy procedure with the two types of needles; (2) Incidence of pneumothorax during the localization biopsy procedure with the two types of needles; (3) Incidence of hemoptysis during the localization biopsy procedure with the two types of needles; (4) Decoupling situations during surgical thoracoscopy (That is, during surgery, the positioning needle is removed from its original position and floats in the chest cavity); (5) Average puncture time; (6) Success rate of puncture localization; (7) Number of patients with discomfort after the puncture (e.g. cough, pain at the puncture site, hemoptysis, etc.) (8) Number of cases of air embolism during puncture (Table 2). Data were analyzed using SPSS 25.0 (IBM SPSS Statistics, IBM Corp) for statistical analysis. Continuous variables are presented as mean
Table 2
Incidence of complications in nodule localization
| Bard Localization Needles 53 (Group A) | SensCure Localization Needles 44 (Group B) | X2 | ||||
|---|---|---|---|---|---|---|
|
| % |
| % | |||
| Pneumothorax | 12 | 22.64 | 3 | 9.76 | 4.60 | |
| Alveolar Hemorrhage | 35 | 66.04 | 15 | 34.09 | 9.82 | |
| Decoupling during Thoracoscopy | 3 | 5.66 | 0 | 0 | – | |
| Hemoptysis | 2 | 3.77 | 0 | 0 | – | |
| Localization Success Rate | 94.34% | (50/53) | 100% | (44/44) | – | |
| Complication Incidence Rate | 38/53 | 71.69% | 13/44 | 29.55% | ||
| Average Localization Time | 15.47 | 25.32 | ||||
| Localization Success Rate | 94.34% | (50/53) | 100% | (44/44) | ||
| Number of Postoperative Discomfort Cases | 40 | 3 | ||||
| Number of air embolism during puncture | 0 | 0 | ||||
3.Results and analysis
By collecting and analyzing data from 94 patients (97 pulmonary nodules) in our hospital, the results are summarized as follows: For patients in Group A, who used the Bard localization needles, there were 53 cases, including 32 males and 21 females, with an average age of 53.32
4.Discussion
With the increasing use of low-dose spiral CT in health examinations, the proportion of patients with pulmonary nodules requiring surgical treatment is rising. Currently, single-port video-assisted thoracoscopic surgery (VATS) is commonly used for the resection of pulmonary nodules. However, unclear preoperative localization of pulmonary nodules can make it challenging to identify them during thoracoscopic surgery, especially for non-palpable ground glass nodules. This can lead to prolonged surgery times, increased postoperative complications, and ultimately extended hospital stays. Therefore, precise preoperative localization of pulmonary nodules is crucial [6]. Currently, pulmonary nodule localization methods include CT-guided percutaneous puncture-assisted localization, bronchoscopic puncture-assisted localization, and CT virtual 3D-assisted localization [7]. Among the commonly used CT-guided percutaneous puncture-assisted localization methods, there are techniques such as percutaneous Hook-wire localization [8], percutaneous spring coil localization [9, 10], and percutaneous injection of liquid materials for localization (e.g., methylene blue) [11, 12, 13, 14, 15]. Hook-wire localization is the most commonly used method in CT-guided percutaneous puncture-assisted localization [16]. In the two types of needles studied in this paper, Group A’s localization needle has a metal hook at the tip followed by a metal wire. However, the metal wire is prone to displacement and detachment, resulting in a higher failure rate, observed in three cases (5.66%) in this group. The rigid and sharp hook wire causes twisting stress on the lung parenchyma and movement of the chest wall, causing significant discomfort or pain. This leads to an increased likelihood of intraoperative and postoperative alveolar hemorrhage and pneumothorax. Postoperatively, patients can only adopt a passive position due to the strong discomfort caused by the friction and pain of the steel wire, resulting in a poor overall experience. This is generally consistent with literature reports [17]. In contrast, Group B’s soft tail wire conforms better to the puncture hole, causing less friction and traction. Postoperatively, patients can adopt a comfortable position, and the chances of decoupling and subsequent trauma-related alveolar hemorrhage and pneumothorax are significantly reduced.In other literature, the “dragging tail” spring coil localization method requires secondary release of the spring coil, increasing the number of CT scans and posing a risk of localization failure [18]. Additionally, the depth of spring coil release is closely related to the operator’s experience. However, for patients with pleural adhesions and pigmentation on the lung surface, the surgery time and intraoperative nodule removal time are shorter compared to patients localized with methylene blue [19]. In the injection of liquid material localization method, methylene blue is commonly used [21], but its rapid diffusion requires immediate surgery post-puncture, and it is challenging to identify on the lung surface with pigment deposition [22, 23]. Bronchoscopic puncture-assisted localization techniques require the use of electromagnetic navigation bronchoscopy [10, 20], and CT virtual 3D-assisted localization techniques involve the use of 3D printing technology to create a localization template. Both of these techniques have high equipment requirements, and only a few institutions currently employ them. Therefore, finding a safe, accurate, and convenient localization method is crucial for the clinical treatment of pulmonary nodules. In this study, the use of a disposable pulmonary nodule puncture needle effectively reduced the occurrence of decoupling during thoracoscopic surgery. Furthermore, during the surgical process, the CT zone localization method accurately identified the lesion’s position, preventing excessive removal and missection of lung tissue. This not only shortened the surgery time but also reduced trauma to the patient, preserved more lung tissue, lowered the risk of postoperative complications, increased the surgical success rate, and promoted patient recovery. Additionally, compared to the breast localization puncture needle, the disposable pulmonary nodule puncture needle had a lower incidence of complications and significantly higher patient comfort.
5.Conclusion
In conclusion, among the various preoperative localization methods, the Hook-Wire needle localization method stands out for its simplicity, reliable positioning, high safety, and low complication rate. This study confirms that preoperative localization with a disposable pulmonary nodule puncture needle is safer, with a lower complication rate and higher patient comfort. This approach prevents intraoperative missection and facilitates the smooth progress of VATS surgery. It is worthy of clinical promotion and use.
Conflict of interest
None to report.
References
[1] | Lung cancer group of respiratory disease branch of Chinese Medical Association and expert group of China Lung Cancer Prevention and Control Alliance, “Chinese expert consensus on diagnosis and treatment of pulmonary nodules (2018 edition)”, Chinese Journal of Tuberculosis and Respiratory Medicine. (2018) ; 41: (10): 9. |
[2] | Mcnittgray MF. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med. (2011) ; 365: : 395-409. |
[3] | Galetta D, Rampinelli C, Funicelli L, et al. CT-guided percutaneous radiotracer localization and resection of indistinct/small pulmonary lesions. Ann Thorac Surg. (2019) ; 108: (1): 852-858. doi: 10.1016/j.athoracsur.2019.03.102. |
[4] | Nardini M, Dunning J. Pulmonary nodules precision localization techniques. Fut Oncol. (2020) . doi: 10.2217/fon-2019-0069. |
[5] | Tyler S, Nathan K, et al. Risk Factors for Pneumothorax Development Following CT-Guided Core Lung Nodule Biopsy. Original Investigation. May 25 (2021) . doi: 10.1097/LBR0000000000000816. |
[6] | Huang W, Zhou YM, Jiang GN. Clinical application and improvement of Hookwire in locating small lung lesions under CT guidance. Chinese Journal of Thoracic and Cardiovascular Surgery. (2015) ; 31: (6): 366-368. |
[7] | Nardini M, Dunning J. Pulmonary nodules precision localization techniques. Future Oncol. (2020) ; 16: (16s): 15-19. |
[8] | Lu JG, Liu Y, Gu CW, et al. Application of 3D imaging software localization in the video-asisited thoracoscopic resection of pulmonary ground glass nodule. J Xinxiang Med Univ. (2021) ; 38: (2): 173-175. |
[9] | Zhao G, Yu X, Chen W, et al. Computed tomography-guided preoperative semi-rigid hook-wire localization of small pulmonary nodules: 74 cases report. J Cardiothorac Surg. (2019) ; 14: (1): 149. |
[10] | Yu A, Jiao ZC, Zhou Y, et al. Application of CT-guided microcoil localization in single utility port video-assisted thoracoscopic surgery for small pulmonary nodules (diameter ⩽ 15 mm): a retrospective cohort study. Chin J Clin Thorac Cardiovasc Surg. (2022) ; 29: (1): 68-73. |
[11] | Rodriguesjcl P, Hanneman K, et al. CT guided microcoil pulmonary nodule localization prior to video-assisted thoracoscopic surgery: diagnostic utility and recurrence-free survival. Radiology. (2019) ; 291: (1): 214-222. |
[12] | Cornella KN, Repper DC, Palafox BA, et al. A surgeon’s guide for various lung nodule localization techniques and the newest technologies. Innovations (Phila). (2021) ; 16: (1): 26-33. |
[13] | Hasegawa T, Kuroda H, Sato Y, et al. The utility of indigo carmine and lipiodol mixture for preoperative pulmonary nodule localization before video-assisted thoracic surgery. J Vasc Interv Radiol. (2019) ; 30: (3): 446-452. |
[14] | Fan L, Yang H, Yu L, et al. Multicenter, prospective, observational study of a novel technique for preoperative pulmonary nodule localization. J Thorac Cardiovasc Surg. (2020) ; 160: (2): 532-539. |
[15] | Jiang T, Lin M, Zhao M, et al. Preoperative computed tomography-guided localization for pulmonary nodules with glue and dye. Thorac Cardiovasc Surg. (2020) ; 68: (6): 525-532. |
[16] | Wang B, Zeng Y, Zhao Z, et al. A safe and novel method for video-assisted thoracic surgery preoperative localization of small pulmonary nodules by using ZT medical glue (2-octyl cyanoacrylate). Surg Oncol. (2020) ; 33: : 164-169. |
[17] | Chen XY, Zhao GY, Xu JC, et al. Clinical analysis of CTguided preoperative Hookwire localization of pulmonary nodules in 102 patients. Chin J Clin Thorac Cardiovasc Surg. (2022) ; 29: (1): 56-61. |
[18] | Yang F, Zhao H, Sui X, et al. Comparative study on preoperative localization techniques using microcoil and hookwire by propensity score matching. Thorac Cancer. (2020) ; 11: (6): 1386-1395. |
[19] | Zhang Z, Su T, Yu J, et al. Modified microcoil for preoperative localization of solitary pulmonary nodules: a prospective, single-arm, multicenter clinical study. J Vasc Interv ï¼²adiol. (2021) ; 32: (10): 1470-1477e1. |
[20] | Sun S, Liu K, Gao X, et al. Application of modified tailed microcoil in preoperative localization of small pulmonary nodules: a retrospective study. Thorac Cardiovasc Surg. (2020) ; 68: (6): 533-539. |
[21] | Wang C, Liu Y, Yang L, et al. Effectiveness and safety of CT-guided percutaneous intrapulmonary injection of indocyanine green for localization of pulmonary nodules and ground glass opacity. Nat Med J China. (2020) ; 100: (7): 538-540. |
[22] | Kokh, Huang TW, Lee SC, et al. A simple and efficient method to perform preoperative pulmonary nodule localization: CT-guided patent blue dye injection. ClinImaging. (2019) ; 58: : 74-79. |
[23] | Tian Y, Wang C, Yue W, et al. Comparison of computed tomographic imaging-guided hook wire localization and electromagnetic navigation bronchoscope localization in the resection of pulmonary nodules: a retrospective cohort study. SciRes. (2020) ; 10: (1): 21459. |




