Characterization of a retromolar foramen in a Chinese population: A radiographic study
Abstract
BACKGROUND:
Retromolar canal (RMC) arises from the mandibular canal (MC) behind the second or third molar and travels anterosuperiorly to a retromolar foramen (RMF). RMCs and RMFs have generally been ignored in anatomical textbooks and have rarely been reviewed or studied in the anatomical and dental literature until the last decades.
OBJECTIVE:
This study aimed to characterize RMF in a Chinese population concerning its incidence, origin, and classification via anatomical study and periapical radiography.
METHODS:
123 dry adult Chinese mandibles were collected to observe the incidence of RMFs. RMFs were determined using a steel wire 0.5 mm in diameter. The passways or origins of the retromolar canal (RMC) were determined and classified via periapical radiography. For each RMF, two dentists independently measured the diameter and its distances to the lingual cortex, the buccal cortex, and the distal edge of the last tooth (or the alveolar fossa) using a vernier caliper.
RESULTS:
The incidence of RMFs was 31.71%. The average RMF diameter was 0.78
CONCLUSION:
The incidence of RMFs in Chinese may be about one-third, which is a potential factor in the onset of surgery accidents. RMCs can be classified into two types by their origins. One of them is MC, which originates from the mandibular canal, and the other is AF, which originates from the alveolar fossa.
1.Introduction
Retromolar canal (RMC), an anatomical variation in the posterior mandible, arises from the mandibular canal (MC) behind the second or third molar and travels anterosuperiorly to a retromolar foramen (RMF), which is located on the surface of the mandibular retromolar area, within or around the retromolar triangle (RMT) [1]. RMCs contain a myelinated nerve branching from the inferior alveolar nerve, small arteries, and venules [2, 3, 4].
RMCs and RMFs have generally been ignored in anatomical textbooks and have rarely been reviewed or studied in the anatomical and dental literature until the last decades [5, 6, 7]. With the development of radiography in recent years, especially clinic application of CBCT, RMCs, and RMFs were found to be associated with several surgical complications during dental surgical procedures in the RMT region, such as local anesthetic failure, local hemorrhage during procedures and postoperative loss of sensation in the normal distribution of the buccal nerve [8, 9, 10, 11]. The existence of RMCs and RMFs increases the risks of oral operations involving the mandibular molar area and the retromolar region, like dental implant treatment, mandibular sagittal split surgery, impacted third molar extraction, and autologous bone harvesting [12].
Therefore, some studies on RMF incidence and RMC classification in different countries and populations [13, 14, 15, 16, 17, 18] have been reported aiming to facilitate surgical intervention and protect patients from potential complications. However, few studies have been few reported to address the anatomy of RMF in a Chinese population. Thus, we aimed to characterize RMFs in a Chinese population through anatomical study and periapical radiography.
2.Method
123 dry cadaveric mandibles from Chinese adults of unknown sex or age were obtained from Southern Medical University (Guangzhou, China). All specimens were morphologically representative adult mandibles without atrophy or partial damage. To observe the presence of RMF (bilateral or unilateral), and its relationships with the last tooth.
RMFs were determined using a non-beveled stainless steel orthodontic wire with a diameter of 0.5 mm [5], which was required to enter a possible RMF without a resistant force. A foramen with a diameter of less than 0.5 mm was not regarded as an RMF. After an RMF was identified, gutta-percha was introduced into it, and a steel wire was introduced into the mandibular canal for radiography to show the RMC course. The diameter of each RMF and its distances to the distal edge of the last tooth (or the alveolar fossa), to the lingual cortex, and the buccal cortex was measured using a vernier caliper.
All measurements were performed independently by two dentists and repeated three times. To ensure the accuracy of the data, we calculated the average of each measurement. Unpaired two-sample
3.Results
In this study, RMFs were identified in 39 out of the 123 mandibles (31.71%). Of the 39 mandibles, RMF was found on the left side in 13 (33.33%), on the right side in 15 (38.46%), and on the bilateral side in 11 (28.21%) (Table 1). Interestingly, we observed double left RMFs in 2 mandibles, double right RMFs in 2 mandibles, and double bilateral RMFs in 1 mandible (Fig. 1).
Table 1
Descriptive table for RMFs
| Variable | Mean | Std dev | Minimum | Maximum |
|---|---|---|---|---|
| D | 0.078 | 0.027 | 0.050 | 0.016 |
| L | 0.427 | 0.187 | 0.210 | 0.868 |
| B | 0.861 | 0.223 | 0.454 | 1.188 |
| Re | 0.784 | 0.387 | 0.180 | 1.970 |
D
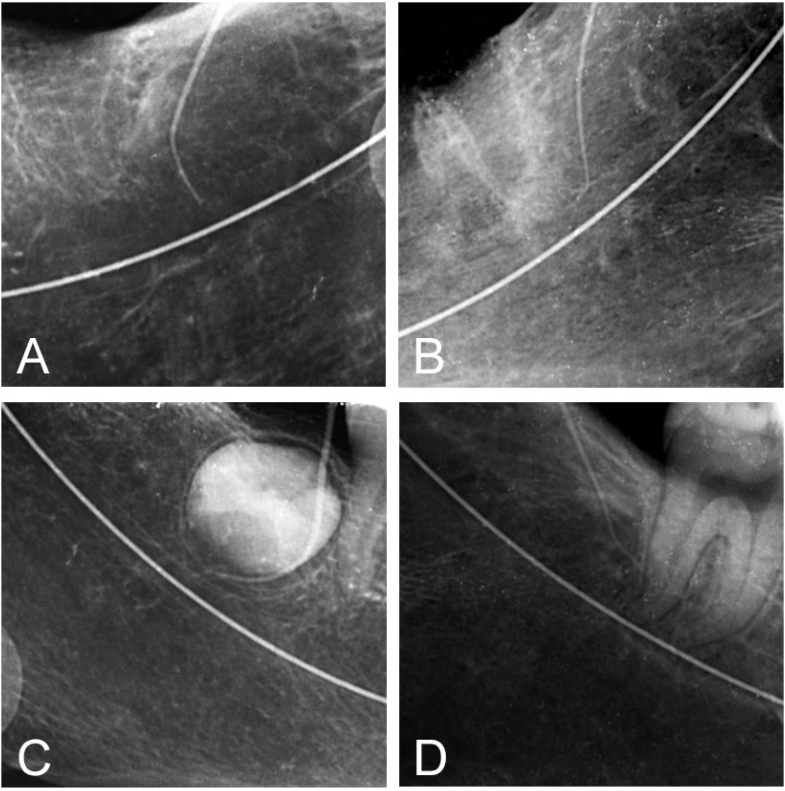
Periapical radiography revealed two origins of RMCs in 56 RMFs. 29 RMCs (51.79%) originated from the mandibular canal and 27 (48.21%) from the alveolar fossa of the second or third molar. Accordingly, we classified RMCs into two types: the MC type originated from the mandibular canal and the AF type originated from the alveolar fossa (Fig. 2).
Table 2
Descriptive table for diameters of the two types
| Variable | Mean | Std dev | Minimum | Maximum | |
|---|---|---|---|---|---|
| MC type | D | 0.089 | 0.031 | 0.050 | 0.160 |
| L | 0.429 | 0.178 | 0.216 | 0.828 | |
| B | 0.848 | 0.234 | 0.480 | 1.188 | |
| Re | 0.840 | 0.441 | 0.218 | 1.970 | |
| AF type | D | 0.067 | 0.016 | 0.050 | 0.114 |
| L | 0.425 | 0.200 | 0.210 | 0.868 | |
| B | 0.876 | 0.213 | 0.454 | 1.148 | |
| Re | 0.724 | 0.317 | 0.180 | 1.380 |
D
Figure 1.
RMFs observed in dry mandibles. RMF on the left side; B. RMF on the right side; C. double RMFs on the right side. Periapical radiography revealed two origins of RMCs in 56 RMFs. 29 RMCs,
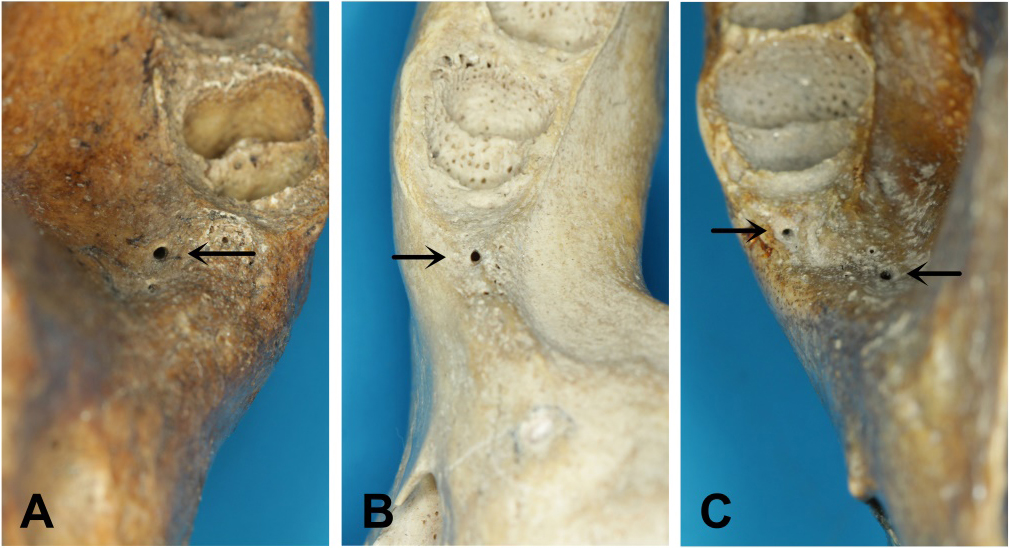
Figure 2.
Periapical radiography showing the passway and origin of an RMC. A&B. The MC type RMC originates from the mandibular canal; C&D. The AF type RMC originates from the alveolar fossa.
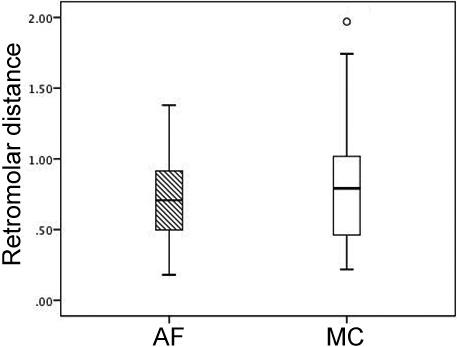
The average diameters of MC and AF types were 0.89
Figure 3.
Boxplot showing diameters of the two types of RMC. T-test for diameters.
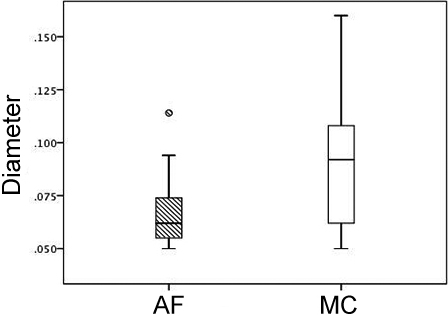
Figure 4.
Boxplot showing buccal distances in the two types of RMC. T-test for buccal distance.
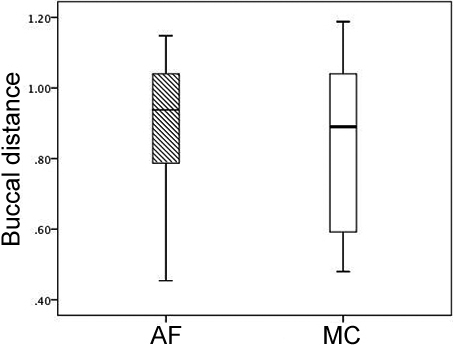
Figure 5.
Boxplot showing the lingual distances in the two types of RMC. T-test for lingual distances.
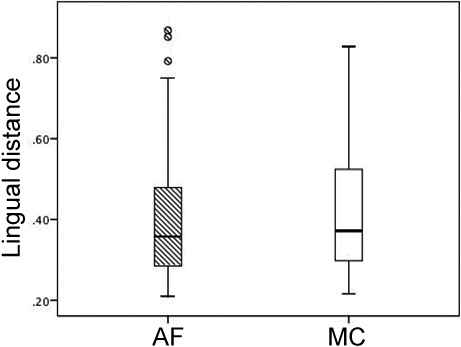
Figure 6.
Boxplot was showing retromolar distances in the two types of RMC. T-test for retromolar distances.
4.Discussion
It can definitively be stated that in cases which involving local anesthetic failure, local hemorrhage during procedures, and/or postoperative loss of sensation in the normal distribution of the buccal nerve, dentists are advised to consider an RMC as a possible cause [19]. Considering these syndromes mainly occur in an impacted third molar extraction, we wonder whether there may be any association between the presence of RMCs or RMFs and presence of the third molar. Pearson’s chi-square test demonstrated no such an association. Dentists usually make a definite diagnosis of an impacted third molar by panoramic radiography, by which it cannot identify the existence of RMF as it is by CBCT [20]. Since the existence of RMF cannot be judged by the existence of a third molar, we suggest that to identify an RMF, a CBCT should be conducted before an impacted third molar extraction to reduce associated syndromes.
Previously published studies have indicated that the incidence of RMFs ranges from 1.7% to 75.4% in different populations [13, 14, 15, 16, 17, 18]. This difference is likely attributable to several factors, such as ethnic differences, genetic or environmental characteristics, and various sample sizes of the studies concerned. In our study, the incidence of RMFs we found was 31.71% in Chinese mandibles, similar to the data reported by Rossi in a Brazilian investigation [21]. However, we found it interesting that even in a single ethnic group, various incidences of RMFs were reported in neighboring populations and countries. For example, the incidence reported by Japanese investigations can be as low as 3.2% and as high as 75.4% [8, 13]. All these variations might imply that the incidence of RMFs can be an issue that is more complex than we imagined. Its influencing factors may be worthy of further research. The absence of uniform study design or inclusion criteria across studies might have been a significant one.
We tried to improve our study design and inclusion criteria in our study. First, we used a minimum diameter of 0.5 mm following the approach employed by Ossenberg rather than the 1.0 mm threshold utilized by Bilecenoglu [6, 8] because in several reports [22], canals with a diameter of less than 1.0 mm had been found by CBCT to be connected to mandibular canals. Such canals would have been excluded if an inclusion criterion of 1.0 mm had been applied. We found several RMCs with a diameter of less than 1.0 mm in this study. Secondly, we introduced gutta-percha rather than a steel wire into RMFs to visualize the passway and origin of each RMC because of the flexibility and radiodensity of gutta-percha. This approach resulted in clear and distinct periapical radiographic images [23]. Additionally, we believed as steel wire is not soft enough, it can destroy the skeletal structure and incorrect visualization of the mandible.
In Sisman’s classification [24], RMCs were classified by their pathway and direction, but we classified RMCs by their origin, mandibular canal, or alveolar fossa. Generally, RMCs are believed to originate from the mandibular canal. Unexpectedly, we found 27 RMCs (48.21%) originating from the alveolar fossa rather than the mandibular canal. We found that the two types of RMFs are in a constant area since there are no significant differences in the distances to the buccal cortex, the lingual cortex, or the last tooth. However, we found that RMCs connected to the mandibular canal had a significantly larger average diameter than those connected to the alveolar fossa. Did they have the same contents now that the two distinct types of RMCs had different diameters? It has been postulated that the contents of RMFs and RMCs consist of small arteries and venules and a thinly myelinated nerve branching from the inferior alveolar nerve [2, 25]. However, the postulation cannot explain why there exists a type of RMC originating from the alveolar fossa rather than from the mandibular canal, and why the two distinct types of RMCs have different diameters. The findings in the present study on the RMFs reminded us of what we have observed in the clinic regarding the contents of RMCs. In clinical practice, we sometimes found in an impacted third molar operation that a wispy retromolar blood vessel from the RMF was too thin compared with the descriptions and photos in the reports published on similar surgery [6, 22, 26]. This indicates that the contents of RMCs may be varied. Our findings in the present study led us to believe that RMCs of AF type might contain only tiny blood vessels without a nerve originating from the inferior alveolar nerve. In contrast, RMCs of MC type might contain a neurovascular bundle originating from the mandibular canal. If the contents of RMCs can be clarified, it is of great significance to dental surgery.
However, the above speculation, though somewhat reasonable, is the major limitation of the present study. Clarifying the contents of the two types of RMCs needs further micro-anatomic in vivo study in new mandibles. We only had dry mandibles available for this study. Apart from what we characterized here about RMCs in a limited number of Chinese mandibles, there must be much to be investigated about this anatomic variation. Why do RMCs arise? Have we known all of its possible clinical significance? What are their possible mechanisms? Why do they vary in origin? How do they vary across ethnic groups? All these problems are so attractive that further research using various means and data available is worthy and necessary.
5.Conclusions
In this study, RMCs can be classified into two types by their origins, MC ones originating from the mandibular canal and AF ones originating from the alveolar fossa. The incidence of RMFs in Chinese may be about one-third. It is clinically significant to localize RMCs accurately before dentoalveolar surgery, which is a potential factor in the onset of surgery accidents. The clinician must consider modifying the dental treatment plan to prevent complications during the treatment procedure.
Conflict of interest
None to report.
Acknowledgments
This work was supported by the President Foundation of Nanfang Hospital of Southern Medical University (2021B015) and Wu Jieping Medical Foundation (320.6750.2020-18-4).
References
[1] | Özlem O, Asim D. Prevalence of bififid mandibular canal according to gender, type and side. Journal of Dental Sciences. (2019) ; 14: : 126-133. |
[2] | Motamedi MH, Gharedaghi J, Mehralizadeh S, Navi F, Badkoobeh A, Valaei N, Azizi T. Anthropomorphic assessment of the retromolar foramen and retromolar nerve: anomaly or variation of normal anatomy? Int J Oral Maxillofac Surg. (2016) ; 45: : 241-244. |
[3] | Schejtman R, Devoto FC, Arias NH. The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol. (1967) ; 12: : 1261-1268. |
[4] | Kumar Potu B, Jagadeesan S, Bhat KM, Rao Sirasanagandla S. Retromolar foramen and canal: a comprehensive review on its anatomy and clinical applications. Morphologie. (2013) ; 97: : 31-37. |
[5] | Potu BK, Kumar V, Salem AH, Abu-Hijleh M. Occurrence of the retromolar foramen in dry mandibles of South-eastern part of India: a morphological study with review of the literature. Anat Res Int. (2014) ; 2014: : 296717. |
[6] | Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. (2006) ; 64: : 1493-1497. |
[7] | Filo K, Schneider T, Kruse AL, Locher M, Gratz KW, Lubbers HT. Frequency and anatomy of the retromolar canal – implications for the dental practice. Swiss Dent J. (2015) ; 125: : 278-292. |
[8] | Ossenberg NS. Retromolar foramen of the human mandible. Am J Phys Anthropol. (1987) ; 73: : 119-128. |
[9] | Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol. (2005) ; 34: : 55-58. |
[10] | Thomas von A, Michael MB. The bifid mandibular canal in three-dimensional radiography:morphologic and quantitative characteristics. Swiss Dent J. (2021) ; 131: : 10-28. |
[11] | Boronat Lopez A, Penarrocha Diago M. Failure of locoregional anesthesia in dental practice. Review of the literature. Med Oral Patol Oral Cir Bucal. (2006) ; 11: : e510-513. |
[12] | Truong MK, He P, Adeeb N, et al. Clinical anatomy and significance of the retromolar foramina and their canals: a literature. (2017) ; 9: : e1781. |
[13] | Patil S, Matsuda Y, Nakajima K, Araki K, Okano T. Retromolar canals as observed on cone-beam computed tomography: their incidence, course, and characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol. (2013) ; 115: : 692-699. |
[14] | Sawyer DR, Kiely ML. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent. (1991) ; 50: : 16-18. |
[15] | Rashsuren O, Choi JW, Han WJ, Kim EK. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci Dent. (2014) ; 44: : 229-236. |
[16] | Lizio G, Pelliccioni GA, Ghigi G, Fanelli A, Marchetti C. Radiographic assessment of the mandibular retromolar canal using cone-beam computed tomography. Acta Odontol Scand. (2013) ; 71: : 650-655. |
[17] | Kang JH, Lee KS, Oh MG, Choi HY, Lee SR, Oh SH, Choi YJ, Kim GT, Choi YS, Hwang EH. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent. (2014) ; 44: : 53-60. |
[18] | Han SS, Park CS. Cone beam CT findings of retromolar canals: Report of cases and literature review. Imaging Sci Dent. (2013) ; 43: : 309-312. |
[19] | von Arx T, Hanni A, Sendi P. Buser D, Bornstein MM. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod. (2011) ; 37: : 1630-1635. |
[20] | Bogdan S, Pataky L, Barabas J, Nemeth Z, Huszar T, Szabo G. Atypical courses of the mandibular canal: comparative examination of dry mandibles and x-rays. J Craniofac Surg. (2006) ; 17: : 487-491. |
[21] | Rossi AC, Freire AR, Prado GB, Prado FB, Botacin PR, Caria PHF. Incidence of retromolar foramen in human mandibles: ethnic and clinical aspects. Int J Morphol. (2012) ; 30: : 1074-1078. |
[22] | Park MK, Jung W, Bae JH, Kwak HH. Anatomical and radiographic study of the mandibular retromolar canal. Journal of Dental Sciences. (2016) ; 11: : 370-376. |
[23] | Alves N, Deana NF. Anatomical and radiographical study of the retromolar canal and retromolar foramen in macerated mandibles. Int J Clin Exp Med. (2015) ; 8: : 4292-4296. |
[24] | Sisman Y, Ercan-Sekerci A, Payveren-Arikan M, Sahman H. Diagnostic accuracy of cone-beam CT compared with panoramic images in predicting retromolar canal during extraction of impacted mandibular third molars. Med Oral Patol Oral Cir Bucal. (2015) ; 20: : e74-81. |
[25] | Gamieldien MY, Van Schoor A, Retromolar foramen: an anatomical study with clinical considerations. Br J Oral Maxillofac Surg. (2016) ; 54: : 784-787. |
[26] | Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. (2011) ; 33: : 501-507. |




