A super-selective coil impregnation therapy for pancreatic duct haemorrhage caused by pseudoaneurysm rupture
Abstract
BACKGROUND:
Haemorrhage of pancreas is a rare cause of upper gastrointestinal bleeding, and currently there is no clinical satisfactory treatment for this disorder.
OBIECTIVE:
The present study envisaged to treat the haemorrhage of pancreas caused by pseudoaneurysm rupture using interventional super-selective coil impregnation therapy, so as to achieve a better treatment efficacy.
METHODS:
Six cases presenting haemorrhage of pancreas were employed for the study, including 5 cases caused by splenic artery pseudoaneurysm and 1 case caused by superior pancreatic artery pseudoaneurysm. In all 6 patients the femoral artery was punctured using Seldinger femoral artery puncture and intubation technique. Subsequently, a catheter was inserted into the abdominal trunk and the contrast medium was injected, and the pseudoaneurysm was developed. A coil was then inserted into the distal end and proximal end of the pseudoaneurysm, respectively, leading to the elimination of the pseudoaneurysm.
RESULTS:
All 6 patients with pancreatic haemorrhage were implanted with coil at the distal and proximal end of the aneurysm, until the aneurysm disappeared during intraoperative angiography. Further, clinical symptoms such as abdominal pain, melena and hematemesis disappeared after the operation. No recurrence of the symptoms was observed in the studied population.
CONCLUSION:
A 100% treatment outcome can be achieved in patients with pseudoaneurysm-induced haemorrhage of pancreas using interventional super-selective coil embolization.
1.Introduction
Haemorrhage of pancreas or other causes leading to bleeding into pancreatic duct is a rare upper gastrointestinal bleeding, which only accounts for 1/1500 [1] of the upper gastrointestinal bleeding according to statistics. Common causes include acute and chronic pancreatitis, pseudocyst, pseudoaneurysm and pancreatic tumor. The treatment methods of aneurysm of pancreas caused by pseudoaneurysm rupture and bleeding mainly include transcatheter arterial embolization (TAE) and surgical operation. The surgery is complex, the surgical scope is large, the trauma to patients is also significant, and the risk of postoperative complications is high. Furthermore, the complications such as pancreatic leakage may often lead to abdominal bleeding or infection, or even lead to life-threatening conditions [2]. Interventional embolization is a minimally invasive surgery, which causes less trauma to the patients and offers a quick recovery after surgery. The present study summarizes the cases of 6 patients with pseudoaneurysm rupture haemorrhage caused by pancreatic duct haemorrhage by interventional super selection coil therapy data. Analysis of the curative effect in the patients shows that the pseudoaneurysm caused by pancreatic duct haemorrhage with interventional embolization curative effect was very significant. The procedure achieved a complete cure, the interventional embolization trauma was small, and offered a fast postoperative recovery with minimal complications.
2.Materials and methods
From August 2008 to August 2019, 6 patients were diagnosed with pancreatic haemorrhage at the Xiamen Chang Gung Hospital, affiliated to the Huaqiao University and Taiwan Province Linkou Chang Gung Hospital. This study was approved by the Institutional Review Committee of the Xiamen Chang Gung Hospital, affiliated to the Huaqiao University and Taiwan Province Linkou Chang Gung Hospita. The diagnostic criteria employed for the study are as follows: 1. There was a clinical history of acute or chronic pancreatitis, with clinical symptoms of abdominal pain and black stool; 2. Pancreatic haemorrhage could be seen directly under the endoscope; 3. CT revealed a splenic artery pseudoaneurysm. The diagnosis of pancreatic haemorrhage must meet three conditions, the first of which is required, and the second and third conditions can exist concurrently or only one of them. Six patients in this study had a history of acute pancreatitis, and their clinical symptoms included abdominal pain and melena. During endoscopic retrograde cholangiopancreatography, one of them had no obvious bile duct abnormality (ERCP). Active bleeding was seen at the junction of the pancreatic duct, common bile duct, and duodenal papilla (Fig. 1), and enhanced CT examination of the other 5 patients revealed a splenic artery pseudoaneurysm (Fig. 2). Furthermore, all six patients underwent the Seldinger femoral artery puncture and intubation, after which the catheter was inserted into the celiac trunk artery, and angiography revealed a pseudoaneurysm (Fig. 3). A super-selective catheter was then inserted into the distal and proximal ends of the pseudoaneurysm and coil (Boston Scientific, Fibered Platinum Coil 5 mm, 5.5 mm, 3 mm, 3.3 mm), until the intraoperative angiography revealed no development pseudoaneurysm (Fig. 4).
Figure 1.
Occurrence of active bleeding at the junction of pancreatic duct and common bile duct and duodenal papilla of the patient undergoing ERCP; there is no obvious abnormality in the bile duct.

Figure 2.
CT enhancement shows an outward protruding cystic shadow of the splenic artery, and it was diagnosed as splenic arterypseudoaneurysm. The patient was admitted to the hospital with abdominal pain and black stool as the chief complaint.
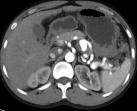
Figure 3.
Intraoperative angiography showed splenic artery protruding sac shadow during TAE, confirming the diagnosis of splenic arterypseudoaneurysm.
3.Results
All 6 patients underwent TAE successfully exhibited a successful stopping of bleeding. This shows that the pseudoaneurysm disappeared during the operation (Fig. 4), and the clinical symptoms of abdominal pain, melena and hematemesis disappeared in the 6 patients after the operation. No recurrence has occurred in any patient since a long follow-up period (Table 1). The longest follow-up is now is 12.5 years, and the shortest is 3.5 years. The data analysis of the 6 patients shows that the super-selective coil reinforcement treatment has a remarkable effect on the haemorrhage of pancreas caused by pseudoaneurysm rupture and bleeding, and can achieve 100% recovery effect.
Table 1
Follow-up of postoperative results of 6 patients
| Tae pre-operative | Tae post-operative | Maximum follow-up time | Minimum follow-up time | |
|---|---|---|---|---|
| Abdominalgia |
|
| 12.5 Years | 3.5 years |
| Spit blood |
|
| ||
| Melena |
|
|
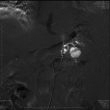
Figure 4.
The pseudoaneurysm disappeared after embolization.

It should be noted that Figs 2–4 present the findings of the same patient, which was later subjected to the interventional super-selective coil embolization at the distal and proximal ends of pseudoaneurysm respectively, until no pseudoaneurysm was detected by angiography.
4.Discussion
In 1931, Lower and Farrell first reported gastrointestinal bleeding caused by rupture of splenic artery tumor and bleeding into the pancreatic duct [3]. In 1970, Sandblom first defined gastrointestinal bleeding caused from pancreatic duct as haemorrhage of pancreas [4]. Haemorrhage of pancreas is a rare intermittent gastrointestinal bleeding caused by bleeding from the pancreatic duct through Vater ampullary papilla. It is often difficult to diagnose this because it is intermittent bleeding. The most common cause is acute and chronic pancreatitis with rupture and bleeding of splenic artery tumor. Other causes have also been reported, such as rupture and bleeding of pseudoaneurysm of hepatic artery, gastroduodenal artery and pancreaticoduodenal artery [5, 6, 7]. According to the research, among haemorrhage of pancreas caused by rupture and bleeding of pseudoaneurysm, splenic artery accounts for 40%, gastroduodenal artery accounts for 30%, pancreaticoduodenal artery accounts for 20%, gastric artery accounts for 5% and hepatic artery accounts for 2% [8, 9, 10]. In this study, 5 cases of haemorrhage of pancreas were caused by rupture and bleeding of splenic artery pseudoaneurysm, and 1 case was caused by rupture and bleeding of posterior superior pancreaticoduodenal artery pseudoaneurysm.
It is often difficult to diagnose the patients with haemorrhage of pancreas. According to the statistics, the presence of pancreatic diseases (e.g. tumour, vascular disease, chronic pancreatitis) with clinical manifestations such as abdominal pain, gastrointestinal bleeding, black stools, etc., suggests the possibility of haemorrhage of pancreas [11]. The examination methods of haemorrhage of pancreas include upper gastrointestinal endoscopy, CT, MRI, and angiography. Since the haemorrhage of pancreas is accompanied with intermittent bleeding, it is often difficult for upper gastrointestinal endoscopy to spot the fresh bleeding. Fortunately, one patient in this study showed active bleeding during ERCP (Fig. 1). Contrast-enhanced CT clearly showed pseudoaneurysm and pancreatic pseudocyst, and even directly diagnosed the haemorrhage of pancreas in active bleeding period. Angiography can always make a definite diagnosis of haemorrhage of pancreas. For patients with unknown causes of gastrointestinal bleeding and a history of pancreatic diseases, angiography can accurately locate the pseudoaneurysm or arteriovenous tumors, such as those originating from spleen, hepatogastric and duodenal arteries [12]. The sensitivity of angiography in diagnosing haemorrhage of pancreas is 96% [13].
There are two treatment methods for haemorrhage of pancreas: interventional therapy and surgical operation [11]. Cardona et al. proposed the importance of interventional therapy for pancreatic related haemorrhage [14, 15]. Interventional therapy for pancreatic haemorrhage has the advantages of safety, less trauma and quick recovery in the postoperative patients. Takao Ide et al. also preferred the use of interventional treatment for pancreatic duct haemorrhage caused in pancreatic lesions [16]. Hence, if the patient’s hemodynamics is stable, interventional embolization should be the first choice, and 79%–100% of the patients’ condition improves immediately [17, 18, 19, 20]. In addition, interventional therapy has the advantages of less trauma and faster postoperative recovery.
There are mainly two kinds of embossment methods: 1. Balloon embossment, 2. Coil embossment. Balloon implantation is to place a balloon in the corresponding artery before surgery, mainly for the convenience of hemostasis and shortening the operation time, especially for patients with portal hypertension with splenic vein thrombosis and massive haemorrhage [11]. In coil occlusion, a coil is inserted into the artery to promote thrombosis, thus occluding the whole aneurysm [20]. Embolization of abdominal trunk, superior mesenteric artery and hepatic artery is a contraindicated, because if collateral circulation cannot be established, the corresponding arterial blood supply tissue can be necrotic [20]. In addition, aneurysm infection and spleen necrosis may also be related complications of interventional therapy [21]. Therefore, all five patients with splenic artery pseudoaneurysm were administered anti-infective drugs after embolization to prevent the occurrence of splenic infection or splenic abscess formation. These patients had no follow-up for changes in immune function after embolization, so it was not possible to determine the role of splenic embolism on the patient’s immune function. In this study, a case of pseudoaneurysm was located in the posterior superior pancreaticoduodenal artery. The approach of selecting the implantation using pancreaticoduodenal artery was not possible, because the implantation gastroduodenal artery was unable to block the blood supply from other pancreatic arteries, so the therapeutic effect could not be achieved. Therefore, the super-selective approach was employed at the posterior superior pancreaticoduodenal artery, and coils were placed at the distal and proximal ends of pseudoaneurysm, so as to achieve the therapeutic effect of complete occlusion. Five cases of pseudoaneurysm were located in splenic artery, and coil was also placed at the distal and proximal ends of the pseudoaneurysm. At the same time, it was found that during the coil placement, the distal end of the lesion was encapsulated first, followed by the proximal end of the lesion. If the proximal end of the lesion is encapsulated first, the blood supply artery at the distal end of the lesion cannot be encapsulated. All 6 cases demonstrated a complete blockage of the blood supply artery after operation, and there were no complications. Additionally, there were no symptoms of recurrent bleeding. Therefore, coil implantation should be as super-selective as possible in the treatment of patients with haemorrhage of pancreas, and coil should be placed at the distal and proximal ends of the lesion, so as to completely block the blood supply artery. This minimizes the complications and recurrent bleeding, and achieves a complete cure.
Nevertheless, for patients with haemorrhage of pancreas with hemodynamic instability (such as uncontrollable bleeding and persistent shock), repeated bleeding after implantation or failed implantation may occur, so the option of surgical treatment solely remains in such cases [19, 20, 21, 22, 23]. In addition, since it is difficult to see the obvious bleeding place in the upper digestive tract endoscopy, no endoscopic treatment was proposed in this study [24].
5.Conclusion
Haemorrhage of pancreas is a rare intermittent gastrointestinal bleeding disorder. Combined with various examinations of patients, a definite diagnosis can be made, especially in the period of active bleeding. The treatment methods include interventional embolization and surgical operation. If the patient’s hemodynamics is stable, interventional embolization should be the first choice for treatment. An interventional super-selective coil embolization therapy should be used as a first preference during embolization, especially for patients with haemorrhage of pancreas caused by rupture of pseudoaneurysm. Further, the coil should be placed at the distal and proximal ends of the lesion during the catheter super-selective therapy, which can achieve complete cure. Nevertheless, in case of haemodynamic instability (e.g. uncontrolled bleeding, persistent shock) and recurrent bleeding after embolisation or failed embolisation, surgery remains the only option.
Conflict of interest
None to report.
References
[1] | Suter M, Doenez F, Chapuis G, Gillet M, Sandblom P. Haemorrhage into the pancreatic duct (Haemosuccus pancreaticus). Recognition and management. Eur J Surg. (1995) ; 161: : 887-92. |
[2] | Liang H, Wu JG, Wang F et al. Choice of operative method for pancreaticojejunostomy and a multivariable study of pancreatic leakage in Pancreaticoduodenectomy. World J Gastrointest Surg. (2021) ; November 27; 13: (11): 1405-1413. |
[3] | Lower WE, Farrell JI. Aneurysm of the splenic artery: report of a case and review of the literature. Arch Surg. (1931) ; 23. |
[4] | Sandblom P. Gastrointestinal haemorrhage through pancreatic duct. Ann Surg. (1970) ; 171: : 61-6. |
[5] | Stanley JC, Frey CF, Miller TA, Lindenauer SM, Child CG 3rd. Major arterial haemorrhage: a complication of pancreatic pseudocysts and chronic pancreatitis. Arch Surg. (1976) ; 111: : 435-440. |
[6] | Rao RC, Kumar A, Berry M. Pseudoaneurysm of anomalous right hepatic artery as a cause for hemosuccus pancreatitis. Gastrointest Radiol. (1987) ; 12: : 313-314. |
[7] | Fernandez-Cruz L, Pera M, Vilella A, Llovera JM, Navasa M, Teres J. Hemosuccus pancreaticus from a pseudoaneurysm of the hepatic artery proper in a patient with a pancreatic pseudocyst. Hepatogastroenterology. (1992) ; 39: : 149-151. |
[8] | Woods MS, Traverso LW, Kozarek RA, et al. Successful treatment of bleeding pseudoaneurysms of chronic pancreatitis. Pancreas. (1995) ; 10: : 22-30. |
[9] | Yeh TS, Jan YY, Jeng LB, et al. Massive extra-enteric gastrointestinal haemorrhage secondary to splanchnic artery aneurysm. Hepatogastroenterology. (1997) ; 44: : 1152-1156. |
[10] | Toscano RL, Ruiz OR, Gerace CA. Rupture of splenic artery pseudoaneurysm. Am Surg. (1995) ; 61: : 940-942. |
[11] | Rahul AK, Venkat LA. Mohan Krishnan PSG Institute of Medical Sciences and Research, Peelamedu, Coimbatore, Tamil Nadu, India. “Hemosuccus pancreaticus: a rare cause of gastrointestinal bleeding”. Annals of Gastroenterology. (2012) ; 25: , 1-3. |
[12] | Suter M, Doenz F, Chapuis G, Gillet M, Sandblom P. Haemorrhage into the pancreatic duct (Hemosuccus pancreaticus): recognition and management. Eur J Surg. (1995) ; 161: : 887-892. |
[13] | Kim SS, Roberts RR, Nagy KK, Joseph K, Bokhari F, An G, et al. Hemosuccus pancreaticus after penetrating trauma to the abdomen. J Trauma. (2000) ; 49: : 948-950. |
[14] | Cardona JD, Beltr Nagy KK, Joseph K, Bokhari F, An G, et al. Hemosuccus pancreatito an Underdiagnosed Disease: Hemosuccus Pancreaticus, a Rare Cause of Upper Gastrointestinal Bleeding. Cureus. 14: (10): e30837. |
[15] | Onyinye SU, Adnan E, Ebubechukwu E, et al. The Tale of a Bleeding Tree: A Rare Case of Peripancreatic Variceal Haemorrhage Causing Hemosuccus Pancreaticus. Open Access Case Report. (2022) ; 2-6. |
[16] | Takao I, Kazuya U, Hirokazu N. Laparoscopic distal pancreatectomy for hemosuccus pancreaticus due to an intraductal papillary mucinous neoplasm. Asian J Endosc Surg. (2022) ; 1-4. |
[17] | Stabile BE, Wilson SE, Debas HT. Reduced mortality from bleeding pseudocysts and pseudoaneurysms caused by pancreatitis. Arch Surg. (1983) ; 118: : 45-51. |
[18] | Gambiez LP, Ernst OJ, Merlier OA, Porte HL, Chambon JP, Quandalle PA. Arterial embolization for bleeding pseudocysts complicating chronic pancreatitis. Arch Surg. (1997) ; 132: : 1016-1021. |
[19] | Sethi H, Peddu P, Prachalias A, Kane P, Karani J, Rela M, et al. Selective embolization for bleeding visceral artery pseudoaneurysms in patients with pancreatitis. Hepatobiliary Pancreat Dis Int. (2010) ; 9: : 634-638. |
[20] | Zyromski NJ, Vieira C, Stecker M, Nakeeb A, Pitt HA, Lillemoe KD, et al. Improved outcomes in postoperative and pancreatitis-related visceral pseudoaneurysms. J Gastrointest Surg. (2007) ; 11: : 50-55. |
[21] | Akpinar H, Dicle O, Ellidokuz E, Okan A, Goktay Y, Tankurt E, et al. Hemosuccus pancreaticus treated by transvascular selective arterial embolization. Endoscopy. (1999) ; 31: : 213-214. |
[22] | Sakorafas GH, Sarr MG, Farley DR, Que FG, Andrews JC, Farnell MB. Hemosuccus pancreaticus complicating chronic pancreatitis: an obscure cause of upper gastrointestinal bleeding. Langenbecks Arch Surg. (2000) ; 385: : 124-128. |
[23] | Lermite E, Regenet N, Tuech JJ, Pessaux P, Meurette G, Bridoux V, et al. Diagnosis and treatment of hemosuccus pancreaticus: development of endovascular management. Pancreas. (2007) ; 34: : 229-232. |
[24] | Natalie C, Anup S, Richard M, et al. Radiologic Predictors of Increased Number of Necrosectomies During Endoscopic Management of Walled-off Pancreatic NecrosisRadiologic. Predictors of Endoscopic Necrosectomy, (2021) . |




