Effect of perioperative cognitive behavioral interventions on pain, anxiety, and sleep quality in elderly patients after sinus floor elevation and immediate implantation: A randomized controlled trial
Abstract
BACKGROUND:
Sinus floor elevation and immediate dental implantation are commonly performed to treat dentition defects in elderly patients. Targeted cognitive behavioral interventions (CBI) during the perioperative period can reduce pain and anxiety as well as improve sleep quality. This can lead to improvements in patient cooperation during follow-up treatment and enhance the overall efficacy of the surgery.
OBJECTIVE:
The study aimed to investigate the impact of a cognitive behavioral intervention method on perioperative pain, anxiety, and sleep quality in elderly patients undergoing sinus floor elevation and immediate dental implantation.
METHODS:
Forty patients who required the treatment at the Stomatology Clinic in our hospital between December 2018 and December 2022 were enrolled in this randomized controlled trial. The patients were randomly divided into two groups: a control group (
RESULTS:
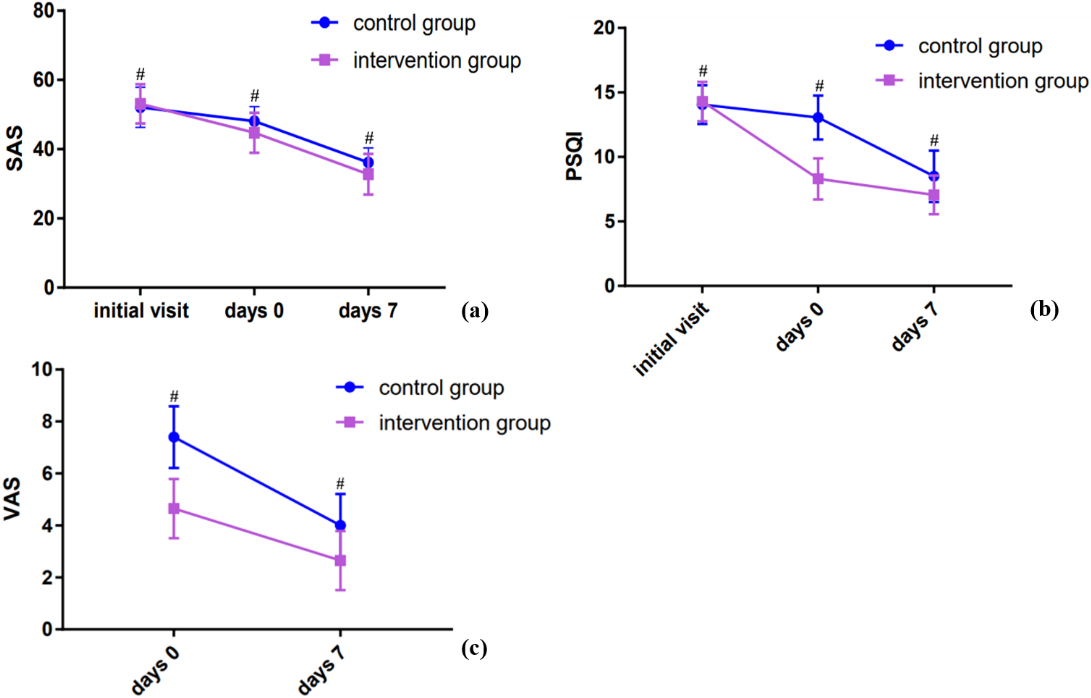
No statistically significant differences in SAS and PSQI were observed between the two groups at the initial visit; the values were significantly higher than those measured postoperatively. The SAS scores and PSQI of patients on days 0 and 7 post-surgery in the intervention group were significantly lower than those in the control group (
CONCLUSION:
Perioperative cognitive behavioral intervention can effectively improve anxiety, postoperative pain and sleep quality in elderly patients who have undergone sinus floor elevation and immediate dental implantation, thereby reducing the incidence of complications.
1.Introduction
In China, more and more elderly patients require tooth restorations owing to the intensification of the aging trend [1]. Moreover, improved living standards and increased public health awareness have led to a surge in the demand for high-quality oral restorations in elderly patients with missing teeth [2]. In recent years, implant restoration has gradually become the first choice for restoring missing teeth in elderly patients owing to its properties, such as improved comfort and masticatory efficiency [3].
It is important to minimize the physical and psychological trauma caused by implant treatment in older patients, particularly before or after complicated surgical procedures, such as guided bone regeneration, sinus floor elevation and bone splitting [4]. Studies have reported different degrees of stress and anxiety during the perioperative period in patients undergoing sinus floor elevation surgery [5]. Elderly patients are more prone to have negative emotions, such as tension and anxiety, before and after an invasive surgical procedure [6]. In sinus floor elevation, multiple taps are made on the maxillary sinus, and the patient is required to keep their mouth open for longer periods. The percussion of the sinus results in a vibration, which could cause short-term dizziness. These types of situations can create negative emotions, such as anxiety, in elderly patients, which could directly affect their cooperation and satisfaction before and during the surgical procedure. Additionally, they may elevate the heart rate and blood pressure during the perioperative period, thus affecting the postoperative sleep quality and rehabilitation; in severe cases, it can even lead to adverse cardiovascular events.
The perioperative conventional treatment and care method does not focus on the mental state of the elderly patient undergoing implant surgery. Comprehensive nursing intervention based on cognitive behavioral therapy (CBT) effectively solves perioperative anxiety in elderly patients [7, 8]. It can effectively reduce perioperative anxiety, postoperative stress [9], postoperative pain [10], postoperative sleep disturbance [11], and other discomforts [12] in elderly patients undergoing digestive tract malignant tumor surgery.
However, few researches have focused on the effect of cognitive behavioral interventions (CBI) during the perioperative period on sinus floor elevation and immediate dental implantation in elderly patients. This clinical randomized controlled trial focused on analyzing the effects of a comprehensive perioperative behavioral intervention on perioperative pain, anxiety, and sleep quality in elderly patients undergoing sinus floor elevation and immediate dental implantation. The study aimed to identify a CBT that was effective, easy to promote, and suitable for elderly patients undergoing implant surgery.
2.Materials and methods
2.1Study individuals
This study was conducted at the Stomatology Clinic from December 2018 to December 2022. The study was approved by the Ethics Committee and responsible agency of our research organization, and all guidelines, regulations, and legal and ethical standards required for human studies were followed. A total of 40 elderly patients who required sinus floor elevation and immediate dental implantation were included. Written informed consent was obtained from each patient. The selected patients were divided into two groups randomly: control and intervention (
Figure 1.
The flowchart of the study.
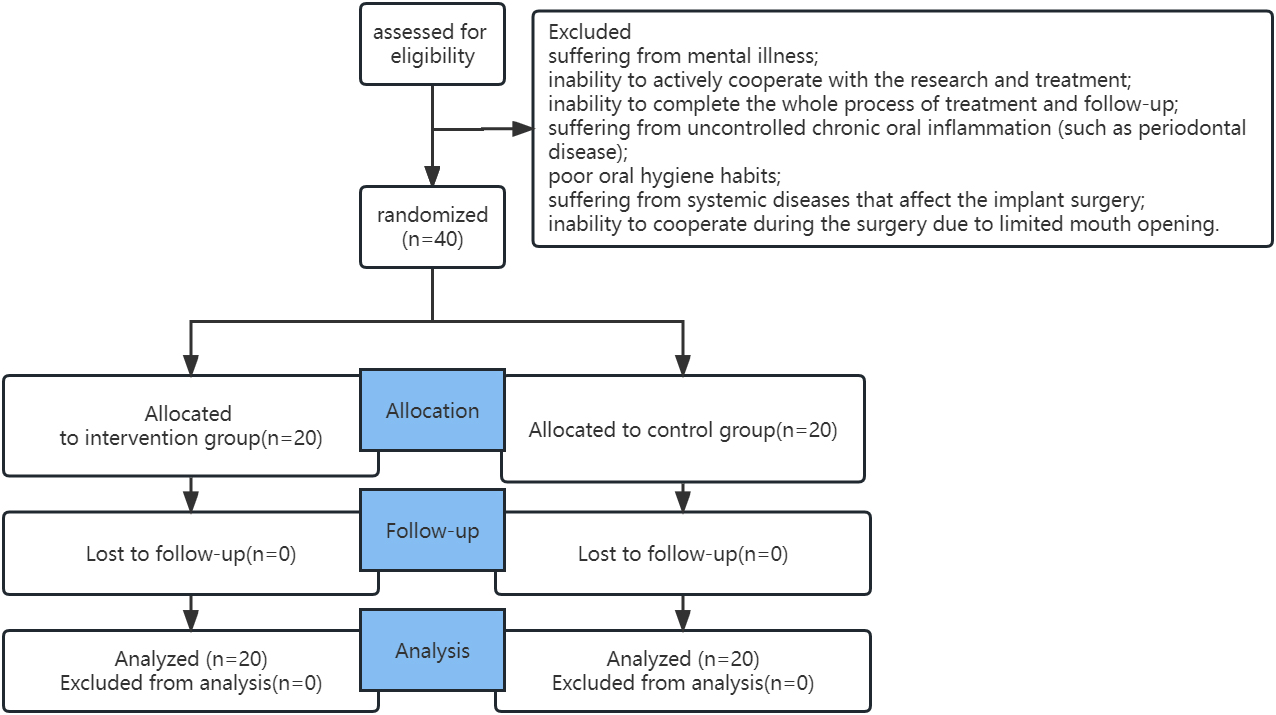
2.2Inclusion and exclusion criteria
The inclusion criteria were as follows: elderly patients over 60 years old; good general health (well-controlled chronic diseases or healthy); missing maxillary posterior teeth and the need for implant restoration; and no contraindications for sinus floor elevation and immediate dental implantation. The patients were required to be mentally healthy, fully understand and sign the consent form, and be willing to undergo regular follow-ups. The exclusion criteria included the following: suffering from mental illness; inability to actively cooperate with the research and treatment; inability to complete the whole process of treatment and follow-up; suffering from uncontrolled chronic oral inflammation (e.g., periodontal disease); poor oral hygiene habits; suffering from systemic diseases that might affect the implant surgery; and inability to cooperate during the surgery due to limited mouth opening.
2.3Interventions
Patients in the control group received conventional treatment and care during the perioperative period; this included general health guidance, education, and nursing during the perioperative period, general pre-implantation inspection at the first visit, information about the surgical plans, surgery-related procedures, and complications, and education about the perioperative precautions.
Those in the intervention group received orderly CBT in addition to the conventional treatment and care during the perioperative period. One hour before and after the operation, the patient was required to perform a progressive relaxation exercise for 10 min on a relatively quiet and independent dental chair in the clinic under the guidance of the medical staff. The patient was accompanied by the staff throughout the exercise. Firstly, the patient was instructed to lie supine on the dental chair. The position of the headrest of the dental chair was adjusted to make the patient comfortable. The patient was asked to close their eyes, place their hands on the chest or abdomen, and relax the muscles of the whole body. The patient was instructed to “inhale and exhale slowly” as if “smelling the fragrance of flowers”. When inhaling, the chest was held as still as possible, and the abdomen was held as straight as possible. Using the Dantian point as the support point, the patient was instructed to exhale slowly and as stably as possible. After 1 min, the “3-3-8-5 breathing technique” was performed to help patients adjust and control their breath. In this method, the patient had to take a deep breath for 3–5 s, hold it for 3 s, exhale slowly for 8 s, and then hold the breath again for 5 s. Based on the breathing adjustment and muscle relaxation exercises, the patient was guided to carry out concrete imaginations and pleasant events in the past, thereby stabilizing the mood and enhancing the therapeutic effect.
Soothing light music was played in the treatment room during the relaxation and treatment process. Positive body language, such as holding hands or touching, helped relieve anxiety. Close communication with the elderly patient and the family members was maintained from the first outpatient visit to day 7 of the postoperative follow-up visit. In addition to general information about implant restoration and the precautions for maxillary sinus floor lifting surgery, pictures and videos that illustrate the importance of positive emotions in surgery, surgical outcomes, and successful cases can be used to increase the confidence of the patient and improve their cooperation with the doctors and nurses. Along with face-to-face communication during each follow-up visit, active communication via telephone or WeChat was maintained once a day during the perioperative period. Each doctor-patient communication lasted for about 10–15 min. During the perioperative period, paying close attention to the various emotional and psychosomatic changes caused by anxiety among the patients and family members is necessary. Help was provided to improve their emotions and prevent the negative emotions of the family members and people around them from affecting their mentality. The focus of postoperative follow-up was implementing home care for the patient. Problems related to postoperative diet, oral hygiene maintenance, and other aspects were addressed in time, and help was provided. The medical staff who participated in the above-mentioned procedures were uniformly trained by the investigators to ensure the consistency and standardization of the operation process and mode.
2.4Observation index
The Self-Rating Anxiety Scale (SAS) [13] scores were used to evaluate the anxiety of the patients in both groups at the first visit, immediately after the operation, and 7 days after the surgery. The total SAS score ranges from 20 to 80 points. The higher the SAS score, the more serious the anxiety disorder.
The Pittsburgh Sleep Quality Index (PSQI) [14] was used to assess the sleep quality of the patients in both groups during the three aforementioned time-points. The PSQI is a self-assessment questionnaire, which assesses sleep quality and disturbances over a 1-month intervals. Higher scores indicated worse sleep quality.
The degree of pain of patients was assessed using the visual analogue scale (VAS) [14] 0 and 7 days after the operation. VAS are psychometric measuring instruments, which was designed to document a patient’s characteristics of disease-related symptom severity in patients.
The SAS and PSQI scores of patients at the first visit measured before the visit. The incidence of postoperative complications (postoperative bleeding, maxillary sinus infection, and implant loosening) in the two groups was assessed, and the oral hygiene and restoration of soft tissue in the surgical area were recorded 7 days after the operation.
2.5Statistical analysis
All data were analyzed by the SPSS 20.0 software package (IBM, New York, USA). The counting data were expressed in n (%). The independent sample
3.Results
3.1Baseline data
No significant differences in baseline characteristics, such as age, gender, education status, edentulous site requiring sinus floor elevation, and available remaining bone height, were observed between the two groups (Table 1).
Table 1
Characteristics of intervention and control groups (
| Group | Number of cases | Gender (male/female) | Age | education status (high school or higher/ junior high school or less) | RBH (mm) |
|---|---|---|---|---|---|
| Control group | 20 | 12/8 | 65.85 | 11/9 | 6.08 |
| Intervention group | 20 | 13/7 | 65.95 | 12/8 | 6.01 |
|
| 0.107 | 0.079 | 0.000 | 0.303 | |
|
| 0.744 | 0.937 | 1.000 | 0.763 |
3.2Anxiety
For the postoperative outcomes, postoperative day 0 was considered as the day of surgery. At the initial visit, no statistically significant difference in SAS scores was observed between the two groups of patients. The intervention group demonstrated significantly lower postoperative SAS scores on days 0 and 7 compared to the control group (
3.3Sleep quality
At the initial visit, no statistically significant difference in PSQI score was observed between the two groups of patients. The intervention group demonstrated significantly lower postoperative PSQI scores on days 0 and 7 compared to the control group (
3.4Postoperative pain
The VAS scores on days 0 and 7 post-surgery were lower in the intervention group compared to the control group (
3.5Postoperative complications rate
Postoperative complications such as bleeding, maxillary sinus infection, and implant loosening were not observed in both groups (Table 2). The proportion of gingivitis in the surgical area during the 7 day follow-up after the operation was significantly lower in the intervention group compared to the control group.
Table 2
Comparison of postoperative complications rate between the two groups (
| Group | Number of cases | Gingivitis (yes/no) | Postoperative complications rate |
|---|---|---|---|
| Control group | 20 | 4/16 | 0 |
| Intervention group | 20 | 2/18 | 0 |
|
| 0.784 | ||
|
| 0.376 |
Figure 2.
Effects of CBI on elderly patients undergoing sinus floor elevation and immediate dental implantation. (A) The SAS scores at different time points were compared between the two groups. SAS: The Self-Rating Anxiety Scale. (B) The PSQI scores at different time points were compared between the two groups. PSQI: The Pittsburgh Sleep Quality Index. (C) The VAS scores at different time points were compared between the two groups. VAS: The Visual Analogue Scale.
4.Discussion
The absolute contraindications to dental implants are decreasing with the continuous developments in dental implant technology. Numerous clinical studies have shown that advanced age is no longer a contraindication for implant restoration [15]. Nevertheless, relevant studies indicate that minimally invasive surgery should be used as much as possible to minimize trauma to elderly patients [16].
Researchers recommend a more minimally invasive technique for sinus floor elevation through the alveolar crest [15, 16]. The application of the bone impactor during sinus floor elevation is one of the classic techniques, every patient who enrolled in the study used bone impactor during the surgery; however, it should be noted that although the sinus floor elevation technique through the alveolar crest is less traumatic than the sinus lateral wall fenestration internal lifting, head discomfort and dizziness caused by the bone impactors during the operation remain unavoidable. The application of a bone impactor during the sinus floor elevation, followed by immediate dental implantation, is relatively less comfortable (it requires the mouth to be open for a long time). It requires better patient compliance compared to conventional implant surgery. However, most elderly patients have a low pain tolerance and are prone to anxiety due to the decline of body functions. Moreover, cooperation before and during implantation is often poor due to sluggishness. Anxiety results in a loss of confidence in the treatment. The patient becomes more sensitive to postoperative pain, and the quality of sleep after the surgery is reduced; this affects the cooperation of the patient during postoperative personal care and recovery. Studies have shown that most of the unexplained head or face pain and sleep disturbance after sinus floor elevation via the alveolar approach (including sinus floor elevation with a bone impactor [17]) may be closely related to anxiety during the perioperative period [18]. Therefore, it is necessary to perform more targeted perioperative behavioral interventions for elderly patients undergoing sinus floor elevation and immediate dental implantation; this can minimize the discomfort during and after surgery caused by anxiety and reduce the adverse effects of negative emotions on the prognosis of the operation and the overall health of the patient.
In this study, the effects of the two intervention modes on the internal elevation of the sinus floor and the simultaneous implantation in elderly patients during the perioperative period were compared; additionally, the effects on postoperative pain, anxiety, and sleep quality were compared between the two groups. The results confirmed the feasibility and clinical effectiveness of perioperative CBT-based comprehensive behavioral intervention in elderly patients with dental implant surgery. The treatment significantly reduced postoperative pain and anxiety in elderly patients with implant surgery and effectively improved the postoperative sleep quality.
According to the CBT theory, emotional changes are caused by cognitive evaluation, and irrational cognition will cause adverse emotional reactions (such as anxiety and depression), leading to cognitive dysfunction and negative behaviors [19]. Based on this theory, CBT aims to break the vicious cycle of negative thinking by changing the patients’ perceptions toward themselves, others, and other things. The features of this therapy include a structural and short course of treatment, which has been widely used to treat anxiety, post-traumatic stress disorder, depression and other mental diseases [20]. Several studies have used CBT during the perioperative period of cardiac valve replacements and in elderly patients undergoing knee reconstruction; the findings of these studies confirmed that CBT is beneficial for the recovery of these patients [21]. However, patients with different characteristics (such as age, gender, and education level) often have different physical and mental characteristics; hence, these factors should be analyzed among the different populations to formulate a more targeted CBT.
The current study demonstrated that CBT mainly focuses on interventions in the psychological aspects of patients. It is difficult to improve the prognosis of patients by targeting multiple aspects of physiology and psychology using CBT. Nonetheless, a comprehensive intervention mode can achieve better results. Therefore, based on an in-depth analysis of the causes of postoperative pain and sleep disturbance in elderly patients with implantation, the present study adopted a comprehensive behavioral intervention based on CBT. The intervention mode combined two different mechanisms of psychology and behavior to provide more targeted perioperative interventions for elderly patients. Establishing a CBT group composed of doctors and nurses is key to ensuring the smooth progress of the comprehensive behavioral intervention during the perioperative period. Based on this, targeted countermeasures are designed through organized serial health education for prominent issues faced by elderly patients. The aim of activities was to improve the elderly patients’ physical and mental health, relieve perioperative negative emotions such as anxiety and stress, improve the self-care compliance and confidence of the patients. It can also help patients and their families to learn more about the condition and treatment.
Most elderly patients are more sensitive to trauma or pain [22] both mentally and physically, due to the decline in various physical and mental functions, making them less tolerant of surgical risks [23]. The results of the current study suggest that most elderly patients generally have varying degrees of anxiety during the perioperative period of sinus floor elevation and immediate dental implantation (Fig. 2a). In addition to the physical and mental changes caused by aging, the reasons for anxiety in elderly patients may include the following: invasive nature of the implant; insufficient height of available alveolar bone in the maxillary posterior region, which may cause a decrease in self-confidence; the cost of the implant surgery; and effect of negative emotions from family members and friends. In this study, the SAS scores of the elderly patients were high before the operation, with no statistically significant difference between the two groups. Postoperatively, the intervention group had a lower score on the SAS in day 0 and 7 compared to the control group.
The perioperative CBI adopted in this study has a significant effect in alleviating anxiety and is highly suitable for elderly patients. Relaxation exercises are a simple and effective method for assisting the treatment of anxiety disorders; the slow movements and easy learning are more suitable for elderly patients. Furthermore, orderly and continuous communication can maintain good relationships between doctors, nurses, and patients in different environments inside and outside the hospital.
One study reported that sleep quality was closely related to the pain and negative mental state of the patient [24]. Similar findings were observed in the current study in terms of the perioperative sleep quality and pain in elderly patients. Postoperatively, the PSQI and VAS scores on days 0 and 7 in the intervention group were lower than those of the control group and consistent with the change in the trend of the anxiety-related SAS scores. These findings suggest that a comprehensive behavioral intervention can improve sleep quality in elderly implant patients by relieving pain and anxiety.
No postoperative complications, such as bleeding, maxillary sinus infection, and implant loosening, were observed in the two groups, thus ruling out surgical complications as the cause of postoperative pain. At the follow-up visit 7 days after the operation, the proportion of gingivitis in the operation area in the intervention group was significantly lower than that in the control group, possibly due to the good compliance of patients in the intervention group, which might have had a positive effect on the hygiene of the operation area.
The main limitation of this study is that the measurement standard is mostly the patient’s subjective consciousness, and the lack of objective evaluation standard is prone to errors. Another limitation of the current study is the short duration of the registry. It would be important to continue monitoring the implication and evaluate trends.
5.Conclusion
This study showed that perioperative comprehensive behavioral intervention for elderly patients with missing maxillary posterior teeth via the construction of a comprehensive behavioral intervention team composed of doctors and nurses could effectively help relieve anxiety, improve sleep quality, and reduce the incidence of complications. Additional in-depth studies using larger sample sizes and focusing on comparing the effects of the aforementioned comprehensive behavioral interventions in elderly patients based on age, level of education, and gender are warranted.
Acknowledgments
The study was supported by the Science and Technology Project of Guangzhou Economic and Technological Development Zone (2020GH14) and the Clinical Research Program of Nanfang Hospital, Southern Medical University (2018CR022 and 2021CR016).
Conflict of interest
None to report.
References
[1] | Ahmadi M, Kiakojori A, Moudi S. Association of anxiety with pain perception following periodontal flap surgery. J Int Soc Prev Community Dent. (2018) ; 8: (1): 28-33. |
[2] | Anweigi L, Aldegheishem A, Azam A, et al. Oral-Health-Related Self-Efficacy among the Elderly Population in Riyadh, Saudi Arabia. Int J Environ Res Public Health. (2022) ; 19: (23). |
[3] | Alamoush R-A, Elmanaseer W-R, Matar Y-W, et al. Sociodemographic Factors and Implant Consideration by Patients Attending Removable Prosthodontics Clinics. Biomed Res Int. (2022) ; 20228466979. |
[4] | Bartold P-M, Ivanovski S, Darby I. Implants for the aged patient: Biological, clinical and sociological considerations. Periodontol 2000. (2016) ; 72: (1): 120-134. |
[5] | Adly M-S, Adly A-S, Alreshidi S-F, et al. Can paracetamol lower stress and anxiety by blunting emotions during and after computer guided dental implant surgeries? Findings from a randomized crossover clinical trial. J Dent Sci. (2021) ; 16: (1): 137-144. |
[6] | Zheng X, Jin Q, Lu Q, et al. Effect of comprehensive nursing intervention on perioperative anxiety and sleep quality in elderly patients with digestive tract malignancies. Am J Transl Res. (2022) ; 14: (10): 7189-7198. |
[7] | Zheng X, Jin Q, Lu Q, et al. Effect of comprehensive nursing intervention on perioperative anxiety and sleep quality in elderly patients with digestive tract malignancies. Am J Transl Res. (2022) ; 14: (10): 7189-7198. |
[8] | Zhang X, Wang Q, Zhang X, et al. A Cognitive-Behavioral Intervention for the Symptom Clusters of Chinese Patients With Gastrointestinal Tract Cancer Undergoing Chemotherapy: A Pilot Study. Cancer Nurs. (2019) ; 42: (6): E24-E31. |
[9] | Wang X, Yang W. The effects of detailed nursing interventions on the safety and stress responses of tumor patients. Am J Transl Res. (2021) ; 13: (10): 11375-11383. |
[10] | Luan R-L, Zhu M-X, Sun H-Y. Effect of comprehensive nursing intervention in preventing postoperative pain, complications, and psychological pressure in the otolaryngology department. Medicine (Baltimore). (2019) ; 98: (24): e15923. |
[11] | Rampes S, Ma K, Divecha Y-A, et al. Postoperative sleep disorders and their potential impacts on surgical outcomes. J Biomed Res. (2019) ; 34: (4): 271-280. |
[12] | de Ponthaud C, Gaujoux S. Algorithm-based care for early recognition and management of complications after pancreatic resection: Toward standardization of postoperative care. Hepatobiliary Surg Nutr. (2022) ; 11: (5): 718-720. |
[13] | Wang S, Tian H, Xue R. Using psychological interventions in the nursing care of rectal cancer patients. Am J Transl Res. (2021) ; 13: (6): 7282-7287. |
[14] | Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine (Baltimore). (2020) ; 99: (4): e18822. |
[15] | Ohkubo C, Ikumi N, Sato Y, et al. Maintenance issues of elderly patients requiring nursing care with implant treatments in dental visiting: Position paper. Int J Implant Dent. (2022) ; 8: (1): 63. |
[16] | Orentlicher G, Horowitz A, Kobren L. Computer-guided dental implant treatment of complete arch restoration of edentulous and terminal dentition patients. Oral Maxillofac Surg Clin North Am. (2019) ; 31: (3): 399-426. |
[17] | Atar Y, Karaketir S, Sari H, et al. Comparison of preoperative anxiety, bruxism, and postoperative pain among patients undergoing surgery for septoplasty, endoscopic sinus surgery, and tympanoplasty. Niger J Clin Pract. (2022) ; 25: (12): 1984-1991. |
[18] | Ahmadi M, Kiakojori A, Moudi S. Association of anxiety with pain perception following periodontal flap surgery. J Int Soc Prev Community Dent. (2018) ; 8: (1): 28-33. |
[19] | Lin W, Lin J, Cai X, et al. Effects of two different emotion-inducing methods on the emotional memory of non-clinically depressed individuals. PLoS One. (2021) ; 16: (5): e249863. |
[20] | Gomez-de-Regil L, Estrella-Castillo D-F, Vega-Cauich J. Psychological Intervention in Traumatic Brain Injury Patients. Behav Neurol. (2019) ; 20196937832. |
[21] | Skapinakis P, Caldwell D, Hollingworth W, et al. A systematic review of the clinical effectiveness and cost-effectiveness of pharmacological and psychological interventions for the management of obsessive-compulsive disorder in children/adolescents and adults. Health Technol Assess. (2016) ; 20: (43): 1-392. |
[22] | Derry S, Bell R-F, Straube S, et al. Pregabalin for neuropathic pain in adults. Cochrane Database Syst Rev. (2019) ; 1: (1): D7076. |
[23] | Ayaz M, Keshavarzi A, Bahadoran H, et al. Comparison of the Results of Early Excision and Grafting between Children and Adults; A Prospective Comparative Study. Bull Emerg Trauma. (2017) ; 5: (3): 179-183. |
[24] | Clement-Carbonell V, Portilla-Tamarit I, Rubio-Aparicio M, et al. Sleep quality, mental and physical health: A differential relationship. Int J Environ Res Public Health. (2021) ; 18: (2). |




