Physiotherapeutic effects of an innovative golf swing-assist device on discomfort and mobility in amateur golfers with low back pain: A randomized controlled trial
Abstract
BACKGROUND:
Although the biomechanical features of the golf swing are extremely determined, multiple joint movements with limited pelvic and thoracic rotation movement can cause injury to the golfer and are linked with low back pain (LBP). We have developed the Pulley Master machine (PM), which is designed to offer active movement evaluation and monitoring as well as repetitive and task-specific training.
OBJECTIVE:
The primary goal of the present research was to analyze the effects of PM and Transfer of Electricity-Capacitive and Resistive (TECAR) therapy on the lumbar pain scale and thoracic and pelvic mobility in amateur golfers with LBP.
METHODS:
Twenty-one amateur golfers with LBP (six females, mean age
RESULTS:
ANOVA showed that PM outperformed TECAR in terms of pelvic and thoracic mobility as well as a pain rating scale.
CONCLUSION:
The results provide novel and encouraging clinical evidence that PM improves pain control and mobility in amateur golfers with LBP.
1.Introduction
A golf swing includes multi-jointed movements in the whole body that require power, accuracy, and coordination [1, 2]. In particular, the golf swing sequence follows distance and torque, which challenges the rapid and precise mobility of the thoracic and pelvic muscles [3, 4]. The ideal coordination between the thoracic and pelvic regions performs an essential task in the trunk mobility of the golf swing [4, 5]. However, limited pelvic and upper thoracic rotation movement is biomechanical evidence that can cause injury to golfers [4, 5, 6]. Experimental research suggests that abnormal biomechanics is characterized by limited movement and associated muscle pain [4, 5]. Previous studies have reported on pelvic or thoracic mobility and the collaboration between the thoracic and pelvic divisions with an emphasis on a healthy golf swing [3, 6, 7]. Maximum thoracic and pelvic movements predict golf performance and contribute significantly to overall golf driving [1, 5, 7].
To mitigate thoracic and pelvic mobility impairment, a variety of physical therapy or rehabilitation approaches, including Transfer of Electricity-Capacitive and Resistive (TECAR) therapy, manipulation, and mobilization, have been used, but outcome measurements are variable [8]. More specifically, TECAR therapy improved hip passive range of motion (45.20%) in a patient with hip impingement impairment. A systematic review of manipulation reported that manipulation provides an enhancement in mobility and performance in patients with subacute or acute cervical pain [9]. Numerous research studies downplay the efficacy of passive physical therapy and rehabilitation for pain reduction. However, passive physical therapeutic intervention has been mostly used to offer symptomatic alleviation to patients [10, 11, 12]. It is not clear whether persistent muscle mobility or tension during a specific task can be altered due to such pain-reducing medication. Hence, educating patients to adjust their posture and muscle motor control during actual responsibilities is very valuable [13].
Recently, we have developed the Pulley Master machine (PM), which is designed to offer active movement evaluation and monitoring as well as repetitive and task-specific training. The PM system can assess kinematics during a specific task. This information is utilized for feedback during the task. Therefore, the specific goal of the current research was to investigate the effects of PM and TECAR on the back pain scale and thoracic as well as pelvic mobility in amateur golfers with low back pain (LBP). We hypothesized that PM would produce changes in the lumbar pain scale and thoracic and pelvic mobility variables compared to TECAR in amateur golfers with LBP.
2.Methods
2.1Participants
In community centers and universities, a convenience sample of 21 amateur golfers with LBP (six females and 15 males; mean age
Table 1
Demographic Characteristics of the participants (
| Variables | PG ( | TG ( | |
|---|---|---|---|
| Age (years) | 23.30 | 23.55 | 0.47 |
| Sex (M/F) | 7/3 | 8/3 | 0.88 |
| Height (cm) | 170.40 | 167.82 | 0.39 |
| Weight (kg) | 71.50 | 65.37 | 0.28 |
| Onset time (Months) | 3.21 | 2.88 | 0.66 |
PG: Pully master group, TG: TECAR therapy group, M: Male, F: Female.
2.2Visual analog scale
The subjective pain rating was evaluated using the visual analog scale (VAS). The participant expresses their subjective experience while responding to a VAS element by recommending a place along a straight line between two ends [14]. Employing a 10 cm ruler, the result is obtained by analyzing the space between the 10 cm in the middle of the “no pain” symptom and the participant’s reaction, offering an assortment of grades ranging from 0 to 10 [14]. A better result shows more pain intensity. The data consisted of lumbar pain during golf swing movement. All of the tests and interventions were done reliably by the researchers to augment the validity of the clinical outcomes [15].
2.3Mobility data
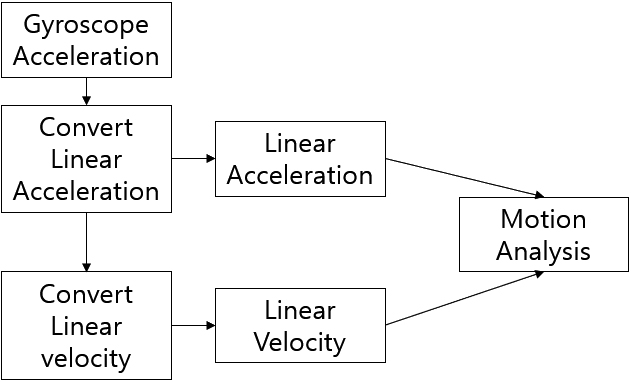
The motion movement analysis system (MyoMotion system, Noraxon Inc., St. AZ, USA) was applied to track the mobility data [16]. MyoMotion sensors were affixed to the lower (7–12th) thoracic spine and pelvis at the spinous process of the 12th thoracic and 1st sacral vertebrae of the participants. The fascia over the spinous processes has some fixation on bone. Therefore, movement artifacts would understand bone movement more directly compared to additional provinces. Using specific fixation straps, the entire sensors were attached to the skin covering these bone markers [17]. The mobility data is comprised of the pelvic and thoracic rotation angle movements.
2.4Intervention
All participants were randomized into one of the two groups (TECAR or pully master group). Both groups received 30 minutes of therapy every day, five days a week for one week. The TECAR group used the WINBACK tool (WINBACK 3SE, Villeneuve-Loubet, France). TECAR therapy was applied to the iliopsoas (IL) and quadratus lumborum (QL) to improve the movement of the pelvis. The IL is fundamentally considered to have mutually deep and superficial parts, respectively. The IL initiation superimposes the lumbar plexus, bringing the starting point from the 12th thoracic and 1st lumbar lateral vertebrae to the 4th lumbar vertebrae surrounding the intervertebral discs. The IL is connected to the deepest part of the lumbar plexus, which is primarily under the IL, and its beginnings lie in the transverse processes of the 1st lumbar to 5th lumbar vertebrae. The fiber muscles converge at a broad origin as they move down adjacent to the posterior abdominal wall. The IL forms a long tendon across the pelvic entrance, which is enrolled in the pelvic region by numerous fibers of the iliac muscle that insert into the lesser trochanter of the femur [10, 18].
The iliolumbar ligament and the internal lip of the posterior iliac crest are the sources of the QL. The QL connects to the tips of the transverse processes of the lumbar vertebrae and the median half of the lower border of the 12th rib. In our study, the participant’s swing side IL and QL muscles underwent TECAR treatment. The shallow action (2–3 cm) of the capacitive mode on soft tissues makes it a TECAR application mode. The resistive mode is a TECAR application mode that works on all fibrous tissues (which tend to have low water content) across the entire complexity of the soft tissue. A steady electrode must be connected to the subject’s body for TECAR therapy, and a handheld electrode must be connected to the medicine portion. To utilize TECAR therapy on the IL muscles, the static electrode was utilized on the erector spinae muscle in the lumbar segment, and the active electrode was utilized on the IL in the supine position. To utilize TECAR therapy on the QL muscles, a stable electrode was utilized on the abdominal muscle and an enthusiastic electrode was employed on the QL, and the subject took the lying position. The intervention was dispensed to each muscle (IL and QL) for 15 minutes; capacitive mode was developed for five minutes, and resistive mode was used for another 10 minutes. The electric current intensity was set to the level at which the individuals felt warm as well as relaxed [11, 18].
Figure 1.
(a) Pully master analysis system (b) Pully master device.

The PM group uses pelvic and thoracic rotations that are assisted by an elastic band. PM therapy was applied to the thoracic and pelvic regions to improve trunk movement for sensorimotor training (Fig. 1). The pulley metal frame was placed on two elastic bands connected to the pelvis and thorax. The metal frame is rigid and fixed. The first flexible band is positioned at the level of the thoracic spine; the second elastic band is placed at the point of the lumbar spine, respectively. At the thoracic and lumbar spine, each band can be adjusted in height. Depending on the participant’s condition, approximately 10–20% resistive tension was sustained at the first session and gradually increased by 10% per session. Resistance and assistive direction can be applied from various angles, which are provided in the vertical direction to promote rotation. Both thoracic and lumbar level bands were applied to the lumbar spine to reduce the lumbar pain. With the help of a certified physical therapist, the correct posture was found for the initial golf swing, and an elastic band was used to assist during the golf swing. As the participant’s swing ability improved from the initial target level, the PM system adjusted the speed and resistive tension parameters (Fig. 1). Furthermore, it was possible to adjust the posture and correct the tension in real-time with audio feedback from the therapist. A subcortical locomotor relearning strategy (subconscious, implicit learning) was reinforced by asking the participant to push the band in the direction of the swing rather than make an accurate golf swing phase [19]. The tee-off platform’s sensors provide immediate feedback on the club head’s speed just before impact and the ball’s speed right after hit. Sensors also measure the ball’s flight’s elevation and direction. Printouts are also provided that include this information as well as the potential landing spot for the ball after the swing. When utilized appropriately, the PM group analysis system may significantly enhance a golfer’s game by providing useful information about their swing. To remove faults that are shown by the PM group method, it is best to use a professional golf instructor (Fig. 2).
2.5Statistical analysis
The mean
3.Results
3.1Thoracic mobility (Unit: degree)
The repeated measures ANOVA demonstrated significant time effects (
Table 2
Thoracic mobility (Unit: degree)
| Pre | Post | Time effect | Between group | Time x Group | |
|---|---|---|---|---|---|
| TG | 22.45 | 26.11 | 0.04* | 0.08 | 0.001* |
| PG | 21.17 | 27.66 | 0.001* |
PG: Pully master group, TG: TECAR therapy group, *
Figure 2.
Pully master algorithms.
3.2Pelvic mobility (Unit: degree)
The repeated measures ANOVA indicated a significant time effect (
Table 3
Lumbar pain scale
| Pre | Post | Time effect | Between group | Time x Group | |
|---|---|---|---|---|---|
| TG | 4.79 | 2.08 | 0.001* | 0.38 | 0.001* |
| PG | 5.31 | 3.28 | 0.001* |
PG: Pully master group, TG: TECAR therapy group, *
3.3Lumbar pain scale
The repeated measures ANOVA proved a significant time effect (
Table 4
Pelvic mobility (Unit: degree)
| Pre | Post | Time effect | Between group | Time x Group | |
|---|---|---|---|---|---|
| TG | 12.23 | 14.08 | 0.001* | 0.20 | 0.001* |
| PG | 11.61 | 13.11 | 0.001* |
PG: Pully master group, TG: TECAR therapy group, *
4.Discussion
To the best of our knowledge, this is the first clinical examination to highlight the therapeutic effectiveness of thoracic and pelvic mobility and lumbar pain scale in amateur golfers with LBP. As hypothesized, PM improved the mobility and pain scale compared to TECAR therapy.
In our clinical research, mobility analysis revealed the positive therapeutic effectiveness of PM on thoracic and pelvic mobility. This result is consistent with that of a previous study using mobility-assisted machines. Jeong and colleagues [20] reported that rowing exercise utilizing a motor-supported rowing device for rowers increased shoulder, elbow, and wrist kinematics (10–20%) in two patients with spinal cord injuries [20].
Normally, finishing the golf swing with the thoracic and pelvic regions permits the amateur golfer to usefully engage the force released. However, limited mobility of the spine may result in enhanced stress on the soft tissue of the spine and lumbar spine [21]. The typical kinetic chain within the thoracic-lumbar-pelvic-hip kinetic chain has cooperated in golfers with mechanical pain, who also had to increase their abnormal lumbar axial rotation to counteract the broken kinetic chain. Over time, monotonous and abnormal lumbar rotation motion owing to restricted thoracic and pelvic mobility may result in spine segment hypermobility or instability, which may further break the kinetic chain in the thoracic-lumbar-pelvic-hip chain system [6, 22]. Spinal segment hypermobility in a broken thoracic-lumbar-pelvic-hip kinetic chain enforces compression and shear stress on the intervertebral joints and spine, which may cause mechanical pain. Recent clinical research exhibited a substantial rejection of musculoskeletal pain in golfers following advancement in thoracic and pelvic mobility, supporting that decreased mobility promotes improved rotation or shear with load in participants with musculoskeletal pain [23, 24]. The proper flexibility of the pelvis and thorax is of particular consequence for constantly obtaining sufficient golf swing motion to avoid mechanical pain in golfers [2, 3]. Clinical pain release analysis demonstrated a therapeutic effect of PM on pain control in our clinical research. This research is parallel to previous sensorimotor studies. Letafatkar et al. [25] found that a sensorimotor training group experienced decreased pain associated with disability (75%), compared to a control group in 53 participants with LBP [25]. Hence, it may be required to correct joint placement in a damaging disorder, including back pain, while assistive energetic aid is offered. The PM is ideal for contemporaneous muscle co-activation and spine density [26, 27]. The PM highlights the activation of reflex pathways from tendon or muscle-ligaments and joint mechanoreceptors to neuromusculoskeletal muscles [19, 28]. While expected stiffness in muscles through delayed time diminishes, it results in the muscles’ strengthening their reaction firing time capability. Joint unstable trepidation and reflex stimulation systems are primarily suggested to encourage muscle reactions that are confronted through the golf swing. Compared to unpredictable joint abnormal loads, permanent reflex pathways may shorten the reaction time and increase the effectiveness of reaction tactics [26, 27].
McCaskey et al. [29] reported that postural sensorimotor training more significantly reduced pain and functional status than in a control group in 20 patients with chronic LBP [29]. It is centered on the theory that the central nervous system does not manage each level of freedom separately but somewhat picks a lower-dimensional subspace that relates to the amount of a performing variable that must be stabilized (i.e., a center of mass). While a corrective assignment is analyzed frequently, the variation in joint angles between the tries may be partitioned into two components [30]. The transversus abdominus and multifidus are important lumbar spine stabilizers that merit emphasis and will be included in the intervention, despite the fact that they were not explicitly isolated in our rotational tests. Understanding how both acute and chronic damage might happen requires an understanding of the lumbar spine’s role in the biomechanics of the golf swing.
The limitations of recent investigations should be considered in potential research. Because of the limited sample size, even if the current findings are encouraging, they should be construed precisely when struggling to apply the recent results to scientific intervention and the treatment of LBP. Another limitation was that we did not directly measure sensorimotor function.
5.Conclusion
This study investigated the therapeutic effect of PM in managing muscluoskeletal pain and spinal mobility in golfers with LBP. The PM was efficient in controlling pain and mobility, following in a significant decline in pain associated with LBP and limited mobility. Nevertheless, additional experiments are needed to establish the sustainable effectiveness of PM on the LBP and mobility, including a decrease in muscle tightness and improved mobility across the thoracic and lumbar areas. Clinically, the current evidence provides us with important insights into pain control and mobility for golfers with LBP.
Conflict of interest
None to report.
References
[1] | Sim T, et al., Analysis of pelvis-thorax coordination patterns of professional and amateur golfers during golf swing. Journal of Motor Behavior. (2017) ; 49: (6): 668-674. |
[2] | Geisler PG. Sports injury prevention and rehabilitation. New york: McGraw-hill, (2001) ; pp. 185-226. |
[3] | Kim SB, et al., Lumbopelvic kinematic characteristics of golfers with limited hip rotation. The American Journal of Sports Medicine. (2015) ; 43: (1): 113-120. |
[4] | Cheetham PJ, et al., The importance of stretching the “X-Factor” in the downswing of golf: The “X-Factor Stretch”. Optimising performance in golf, (2001) ; pp. 192-199. |
[5] | Cochran AJ, Farrally M. Spine and hip motion analysis during the golf swing, in Science and Golf II. (2002) ; Taylor & Francis. pp. 81-91. |
[6] | Vad VB, et al., Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. The American Journal of Sports Medicine. (2004) ; 32: (2): 494-497. |
[7] | Crews D, Lutz R. Comparison of kinematic sequence parameters between amateur and professional golfers. Sci. Golf. (2007) ; 5: : 30-36. |
[8] | Oh DG, Kim SK, Yoo KT. Effect of Physiotherapeutic Intervention Using TECAR Therapy on Pain Self-Awareness and Hip Joint Function in Hip Impingement Syndrome: A Case Study. Journal of the Korean Society of Physical Medicine. (2021) ; 16: (3): 45-53. |
[9] | Cross KM, et al., Thoracic spine thrust manipulation improves pain, range of motion, and self-reported function in patients with mechanical neck pain: a systematic review. Journal of Orthopaedic & Sports Physical Therapy. (2011) ; 41: (9): 633-642. |
[10] | Kim YJ, et al., Effect of High-frequency Diathermy on Hamstring Tightness. Physical Therapy Korea. (2021) ; 28: (1): 65-71. |
[11] | Ribeiro S, Henriques B, Cardoso R. The effectiveness of tecar therapy in musculoskeletal disorders. International Journal of Public Health and Health Systems. (2018) ; 3: (5): 77-83. |
[12] | Kwon K, Kim CM, Park S-J. The Effect of Diathermy Treatment through Physiotherapist’s Hand on the Pain and Disability Index in Chronic Lumbar Pain Patients. Journal of the Korea Convergence Society. (2018) ; 9: (2): 289-294. |
[13] | Ma C, et al., Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. (2011) ; 92: (6): 849-858. |
[14] | Bodian CA, et al., The visual analog scale for pain: clinical significance in postoperative patients. The Journal of the American Society of Anesthesiologists. (2001) ; 95: (6): 1356-1361. |
[15] | Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Academic Emergency Medicine. (2001) ; 8: (12): 1153-1157. |
[16] | Wolfgang T, Subke J. Biomechanical quantification of the dynamic knee valgus using inertial sensor system myomotion [master’s thesis]. Justus – Liebig – Universität Gieße, (2016) . |
[17] | Kim CH, Gwak GT, Kwon OY. Comparison of the flexion-relaxation ratio of the hamstring muscle and lumbopelvic kinematics during forward bending in subjects with different hamstring muscle flexibility. Physical Therapy Korea. (2017) ; 24: (4): 1-10. |
[18] | Osti R, et al., Tri-length laser therapy associated to tecar therapy in the treatment of low-back pain in adults: a preliminary report of a prospective case series. Lasers in Medical Science. (2015) ; 30: (1): 407-412. |
[19] | Macedo LG, et al., Motor control exercise for persistent, nonspecific low back pain: a systematic review. Physical Therapy. (2009) ; 89: (1): 9-25. |
[20] | Jeong JR, Lee BS, Park DS. Kinematic analysis of rowing exercise using a motor-assisted rowing machine for rowers with spinal cord injury: a case report. Physical Therapy Rehabilitation Science. (2014) ; 3: (1): 69-75. |
[21] | Costello M. Treatment of a patient with cervical radiculopathy using thoracic spine thrust manipulation, soft tissue mobilization, and exercise. Journal of Manual & Manipulative Therapy. (2008) ; 16: (3): 129-135. |
[22] | Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. Journal of Sport Rehabilitation. (2009) ; 18: (1): 60. |
[23] | Saragiotto BT, et al., Motor control exercise for chronic non-specific low-back pain. Cochrane Database of Systematic Reviews. (2016) (1). |
[24] | Kim CH, Han JT. Comparison of hip and lumbopelvic movement while hip lateral rotating in individual with chronic low back pain. The Journal of Korean Physical Therapy. (2017) ; 29: (5): 241-245. |
[25] | Letafatkar A, et al., The efficacy of a HUBER exercise system mediated sensorimotor training protocol on proprioceptive system, lumbar movement control and quality of life in patients with chronic non-specific low back pain. Journal of Back and Musculoskeletal Rehabilitation. (2017) ; 30: (4): 767-778. |
[26] | Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. Journal of Athletic Training. (2002) ; 37: (1): 71. |
[27] | Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. Journal of Athletic Training. (2002) ; 37: (1): 80. |
[28] | Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes; Mosby: St. Louis, MO, USA, (2002) . |
[29] | McCaskey MA, et al., Effects of postural specific sensorimotor training in patients with chronic low back pain: study protocol for randomised controlled trial. Trials. (2015) ; 16: (1): 1-10. |
[30] | Scholz J, et al., Motor equivalent control of the center of mass in response to support surface perturbations. Experimental Brain Research. (2007) ; 180: (1): 163-179. |




