The clinical effect of the digital guide in the early implant restoration of second molars
Abstract
BACKGROUND:
In the absence of contraindications to implants, implant repair is the preferred method to treat mandibular second molar loss.
OBJECTIVE:
To compare the clinical effects of a traditional implant guide and digital implant guide in the early implant restoration of second molars.
METHODS:
The study included 35 patients with second molar loss randomly divided into two groups. Eighteen patients in the experimental group had an implant procedure using a computer-aided design/computer-assisted manufacturing (CAD/CAM) digital implant guide, and 17 patients in the control group had the procedure using a traditional film pressing implantation guide. Then, the surgical procedure was completed using the two different implant guides. At 3 months after surgery, four parameters including screw hole exit position, coronal deviation of the implant site, disease improvement rate, and clinical effects, which included marginal adaptation, anatomic form, marginal discoloration, postoperative sensitivity, surface roughness, and secondary caries of the upper prosthesis were compared between the two groups.
RESULTS:
The screw hole exit position in the experimental group was directed to the functional cusp of the opposite jaw, and there was a statistically significant difference between the two groups. There was no statistically significant difference in the rate of disease improvement and the clinical effect of the upper prosthesis between the two groups. There was no statistically significant difference in the bilateral coronal deviation and deviation direction of implants in the two groups. The bilateral coronal deviation of the experimental group was smaller than that of the control group.
CONCLUSION:
The digital implant guide can effectively reduce the deviation of the screw hole and the upper prosthesis in the restoration of the second molar. The prosthesis used in the experimental group had a good clinical outcome, which provides a theoretical basis for the restoration of the posterior molar.
1.Introduction
Second molar loss is common, and its restoration methods mainly include removable partial denture repair, single-end fixed repair, fixed-removable repair, and implant repair [1]. In the absence of contraindications to implants, implant repair is the preferred method to treat mandibular second molar loss [2]. Using an implant guide can ensure accurate positioning during the implant operation, which is the foundation of functional and aesthetic restoration [3]. Implant guides mainly include the traditional film pressing implantation guide and the digitized computer-aided design/computer-assisted manufacturing (CAD/CAM) guide. The traditional method has some errors because the matching accuracy between the model and the tooth may not be good enough. Moreover, in the process of implantation surgery, if the retention of the guide plate is unstable, it would be difficult for the surgeon to get implant location accurately and avoid other problems. The digital guide captured images with a digital scanning probe and digital image of jaw, followed by computer-aided design/computer-aided manufacturing. The occlusal contact and other aspects of measurement data accuracy are obviously higher than with the traditional film pressing implantation guide, so the application of digital guide plate is becoming more frequent [4, 5, 6].
At present, most studies focus on the aesthetic repair of missing anterior teeth [7, 8]. However, the posterior teeth, as occlusal functional teeth, are also important. Early implant repair treatment can shorten the healing period for implants and resolve the situation of missing posterior teeth, so the chewing function is regained as soon as possible [9, 10, 11]. However, it is difficult to obtain better initial stability and guarantee the effect of later repair because of the thin bone wall encountered during early repair. Therefore, it is necessary to find a more appropriate implant aid in such cases, but there are few studies on this. This study aimed to find a more appropriate method of implant guidance for the early repair of posterior molar loss and to provide a more comprehensive theoretical basis for clinicians to compare the effect of a dental support implant guide obtained by the traditional film pressing method and the CAD/CAM production method in the early implant restoration of second molars.
2.Materials and methods
2.1Basic information
From March 2019 to March 2021, the Stomatology Department of Nanfang Hospital selected 35 patients, aged 18–79 years old, who were scheduled to receive early implant repair treatment of second molars. They were divided into experimental and control groups by a random number table. There were 18 patients (11 male and 7 female) in the experimental group with a mean age of 51.78
2.2Inclusion and exclusion criteria
Inclusion criteria were as follows: 1) the missing teeth were all second molars, and the adjacent tooth (the first molar) had no loosening; 2) opposite teeth were retained; 3) there were no systemic diseases or contraindications for dental implants; 4) the bone wall of the alveolar fossa was intact at the dental implant site; 5) there was no acute inflammation such as periodontitis and periapical periodontitis in the implant area; 6) the mouth opening degree was normal, i.e., the index finger, middle finger, and ring finger could be placed vertically between the cutting edge of the upper and lower incisors (about 4.5 cm); 7) 8 weeks after tooth extraction, patients were suitable for implant repair.
Exclusion criteria included severe bone loss, smoking, alcoholism, drug abuse, or mental illness.
2.3Materials and equipment
The materials and equipment included an intraoral scanner (3Shape, Copenhagen, Denmark), silicone rubber (DMG Silagum, Hamburg, Germany), alginate (Heraeaus Kulzer, Hanao, Germany), chair-side CAD/CAM cutting machine (Sirona, Ponzheim, Germany), implant (Astra Tech, Dentsply, Pennsylvania).
2.4Methods
Experimental group
1) Digital internal impression: Images were captured with a 3Shape TRIOS scanning probe to obtain the surface morphology of teeth, gums, and other tissues in the oral cavity.
2) Digital image of jaw: Cone beam computed tomography (CBCT) was taken before surgery and a 3D jaw model was reconstructed after image acquisition.
3) Producing digital guides: The CBCT image data and oral scanning data were imported into the digital guide design software to simulate the implantation position, direction, and depth of the implant, and the digital guide was produced by the technician.
Control group
1) Silicone rubber was used to make an oral model. After the model was disinfected, a diagnostic wax model was made in the missing tooth area and then duplicated by a plaster cast.
2) The missing teeth were arranged on the plaster model, and the guide plate prototype was pressed in a vacuum press using a transparent resin mold.
3) The prototype guide was placed on the model without diagnostic wax. Holes were made at the designed implant site by using a low-speed handpiece. A metal catheter was inserted into the hole and fixed with resin.
After the two groups of guide plates were fabricated, preoperative examination was required to check whether the guide plates were completely in place and whether there was any warping in the mouth. Then, the implant location and implant type (Astra Tech, Dentsply Sirona, Sweden) was determined on the CBCT three-dimensional image. Patients in both groups underwent implantation using the two implant guides, and 3 months after surgery, silicone rubber implant impression and screw fixation were performed for permanent repair. CBCT was taken to measure the deviation and deviation direction of the crown between the actual penetration position and the proposed position of the implant. In the whole treatment process, the same experienced and standardized trained nurse completed the model preparation and perfusion, the same experienced and standardized trained surgeon performed the implant operation and prosthesis insertion, and the same technician made the digital guide plate and prosthesis.
2.5Evaluation indicator
2.5.1The crown was reserved for screw holes
We assessed whether the crown screw hole position was directly in line with the lingual functional cusp of the opposite jaw.
2.5.2Deviation and deviation direction of the crown after implantation
(1) Deviation: The distance between the midpoint of the actual exit site of the implant and the midpoint of the exit site designed before surgery.
(2) Deviation direction: Starting from the midpoint of the exit site of the implant designed before surgery, X and Y axes (red lines) were drawn to create four quadrants, the proximal tongue, proximal buccal, distal tongue, and distal buccal quadrants, which were successively abbreviated as ML, MB, DL, and DB quadrants. At the end of the operation, the midpoint of the actual exit point of the implant was recorded in the appropriate quadrant. The number of cases in each quadrant was recorded.
2.5.3Comparing the clinical effect difference between the two groups
Three months after the implant operation, when the upper prosthesis was applied to the patient, the clinical effect was evaluated among three different grades. 1) The patient was cured: the chewing ability of the patient was restored after the treatment, and the tooth occlusion was normal. 2) Improvement: improved chewing ability, slightly abnormal occlusion of teeth, not affecting eating. 3) Invalid: no improvement in mastication, abnormal occlusion, disease, improvement rate: cure rate
2.5.4Fixed body insertion effect
According to the evaluation criteria of the United States Public Health Service [12], the marginal adaptation, anatomic form, marginal discoloration, surface roughness, postoperative sensitivity and secondary caries of the two groups of prosthetics were evaluated by another surgeon who was not involved in the guide plate design and implantation process (Table 1).
Table 1
Modified USPHS criteria
| Category | Rating criteria | Description |
|---|---|---|
| Marginal adaptation | Alfa (A) | Restoration adapts closely to the tooth structure; there is no visible crevice |
| Bravo (B) | There is a visible crevice, the explorer will penetrate, without dentin exposure | |
| Charlie (C) | The explorer penetrates into crevice in which dentin or the base is exposed | |
| Anatomic form | Alfa (A) | Anatomic form ideal |
| Bravo (B) | Restoration is undercontoured, without dentin or base exposure | |
| Charlie (C) | Restoration is undercontoured, with dentin or base exposure; anatomic form is | |
| unsatisfactory; restoration needs replacement | ||
| Marginal discoloration | Alfa (A) | No marginal discoloration |
| Bravo (B) | Minor marginal discoloration without staining toward pulp, only visible using | |
| mirror and operating light | ||
| Charlie (C) | Deep discoloration with staining toward pulp, visible at a speaking distance of | |
| 60 to 100 cm | ||
| Surface roughness | Alfa (A) | As smooth as the surrounding enamel |
| Bravo (B) | Rougher than surrounding enamel; improvement by finishing is feasible | |
| Charlie (C) | Very rough, could become antiesthetic and/or retain biofilm; improvement by | |
| finishing is not feasible | ||
| Postoperative sensitivity | Alfa (A) | No postoperative sensitivity |
| Bravo (B) | Short-term and tolerable postoperative sensitivity | |
| Charlie (C) | Long-term or intolerable postoperative sensitivity; restoration replacement is | |
| necessary | ||
| Secondary caries | Alfa (A) | No active caries present |
| Charlie (C) | Active caries is present in contact with the restoration |
2.6Statistical analysis
All data were analyzed by the SPSS 20.0 software package. An independent sample
3.Results
3.1Baseline comparison
There were no significant differences between the experimental group and the control group in gender, age, and the number of bilateral second molars, and the results were comparable (Table 2).
Table 2
Comparison of baseline data between the two groups
| Experimental group | Control group |
|
| |
|---|---|---|---|---|
| Age | 51.78 | 47.06 | 1.254 | 0.219 |
| Gender | 11/7 | 9/8 | 0.238 | 0.625 |
| Left first molar | 10 | 10 | 0.038 | 0.845 |
3.2The exit positions of screw retainer holes
The exit positions of the experimental group were all directed to the functional cusp of the opposite jaw. The exit positions of screw retainer holes in the two groups were compared and statistical significance was found (Table 3).
Table 3
Contrast the position of screw retainer holes
| Experimental group | Control group |
|
|
|---|---|---|---|
| 18/0 | 13/4 | 4.782 | 0.045 |
3.3Comparison of coronal deviation after implantation between the two groups
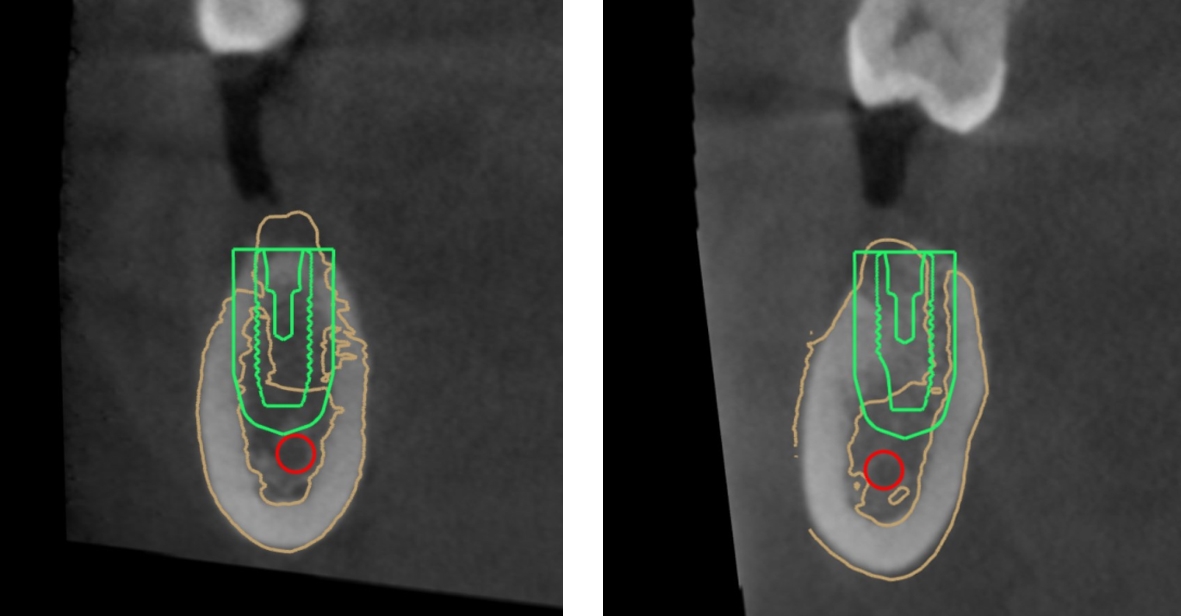
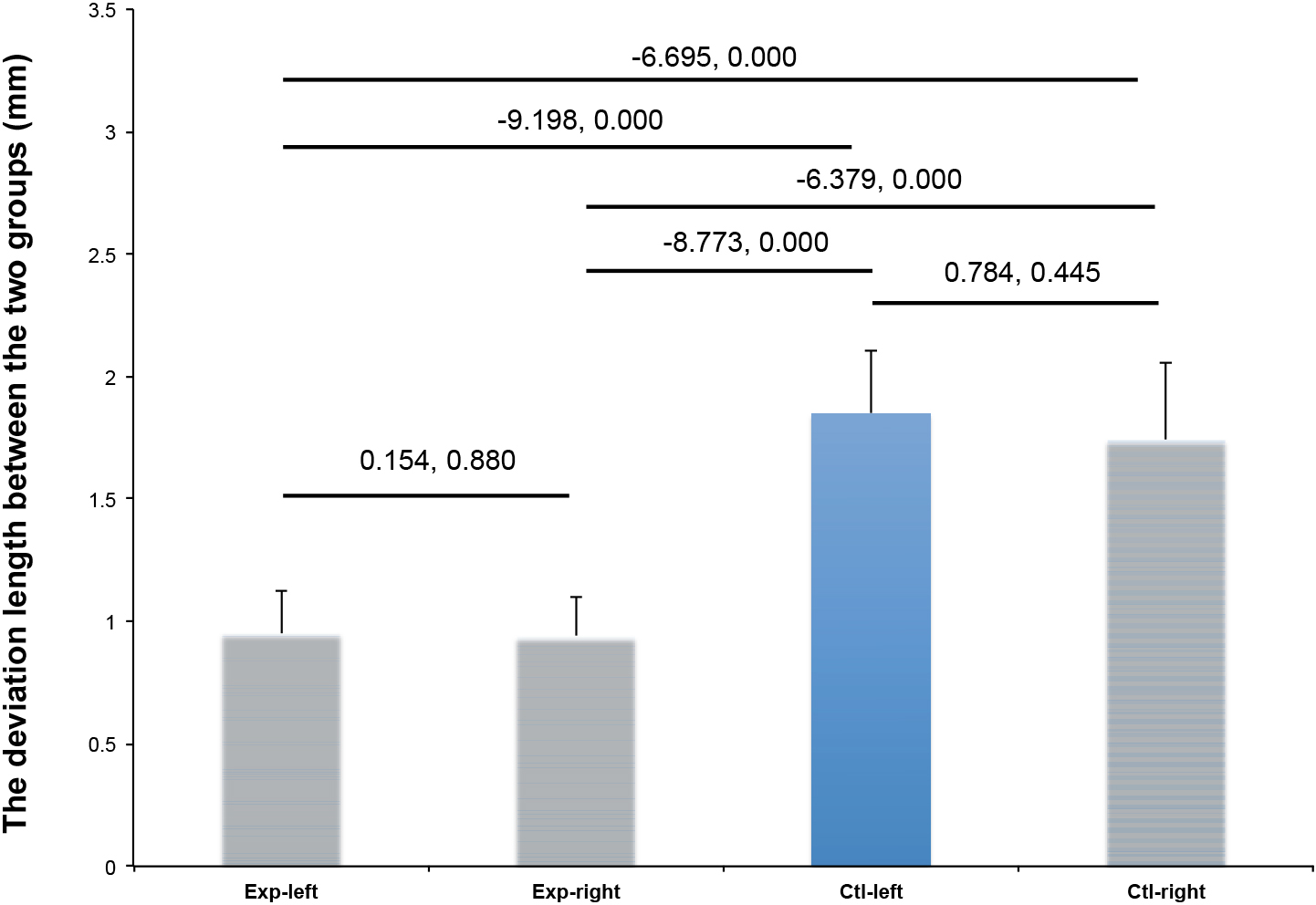
There was no statistically significant difference in left and right coronal deviation between the two groups. The deviation on both sides in the experimental group was significantly smaller than that of the control group (Table 4 and Figs 1 and 2).
Table 4
Comparison of coronal deviation between the two groups
| Group | Side | Sample volume | Deviation (mm) |
|---|---|---|---|
| Experimental group | L | 10 | 0.95 |
| R | 8 | 0.94 | |
| Control group | L | 10 | 1.85 |
| R | 7 | 1.74 |
Figure 1.
The design map of implant sites.
3.4Comparison of coronal deviation after implant insertion
In the experimental group, the direction of deviation after implantation was mostly mesial. In the control group, the deviation direction was mostly buccal but there was no statistically significant difference between the two groups. The results are shown in Table 5.
Table 5
Comparison of coronal deviation direction between the two groups
| Group | Left side | Right side |
|
| |
|---|---|---|---|---|---|
| Experimental group | Mesiolingual (ML) | 1 | 1 | 0.257 | 0.968 |
| Mesiobuccal (MB) | 4 | 3 | |||
| Distolingual (DL) | 2 | 1 | |||
| Distobuccal (DB) | 3 | 3 | |||
| Control group | Mesiolingual (ML) | 3 | 2 | 0.151 | 0.985 |
| Mesiobuccal (MB) | 4 | 3 | |||
| Distolingual (DL) | 2 | 1 | |||
| Distobuccal (DB) | 1 | 1 |
3.5Comparison of the clinical effect difference
There was no statistically significant difference in the improvement rate between the experimental group and the control group (
Table 6
Comparison of the clinical effect in two groups
| Group | Cure | Improved | Invalid | improvement rate |
|
|
|---|---|---|---|---|---|---|
| Experimental group | 16 | 2 | 0 | 100% | 0.949 | 0.402 |
| Control group | 13 | 4 | 0 | 100% |
Figure 2.
Comparison of coronal deviation between the two groups.
3.6Comparison of prosthesis effect
The clinical evaluation of the prosthesis at 1 week after insertion showed that there was no statistically significant difference between the two groups in terms of six aspects of the prosthesis (Table 7).
Table 7
Effect evaluation of prosthesis in two groups
| Category | Experimental group, | Control group, |
|
|
|---|---|---|---|---|
| Marginal adaptation | 0.305 | 1.000 | ||
| A | 16 (88.9) | 16 (94.1) | ||
| B | 2 (11.1) | 1 (5.9) | ||
| C | 0 | 0 | ||
| Anatomic form | 0.305 | 0.658 | ||
| A | 16 (88.9) | 14 (82.4) | ||
| B | 2 (11.1) | 3 (17.6) | ||
| C | 0 | 0 | ||
| Marginal discoloration | 0.172 | 1.000 | ||
| A | 16 (88.9) | 16 (94.1) | ||
| B | 2 (11.1) | 1 (5.9) | ||
| C | 0 | 0 | ||
| Postoperative sensitivity | – | – | ||
| A | 18 (100) | 17 (100) | ||
| B | 0 | 0 | ||
| C | 0 | 0 | ||
| Surface roughness | 0.305 | 1.000 | ||
| A | 15 (83.3) | 15 (88.2) | ||
| B | 3 (16.7) | 2 (11.8) | ||
| C | 0 | 0 | ||
| Secondary caries | – | – | ||
| A | 18 (100) | 17 (100) | ||
| C | 0 | 0 |
4.Discussion
Accuracy is of great significance for a long-term and stable implant repair effect. Inaccurate implantation will create great difficulties in the implant repair for upper teeth, such as difficulty in emplacement caused by non-parallel implants when multiple implants are implanted, in implant arrangement, and aesthetic impact of the exposed implant or abutment metal [13, 14]. The implant guide plate can accurately transfer the repair-oriented implant design during surgery, and at the same time, it can also take into account jaw anatomical conditions, which can ensure more accurate implant implantation [15]. It can not only improve the accuracy of surgery but also improve the reliability predicting the repair effect [16]. At present, according to the different production methods, fabrication of planting guide plates includes the traditional pressing mold method and CAD/CAM method [17]. The traditional implant guide is mainly made of resin, which has the advantages of lower cost and easier production compared with the CAD/CAM guide [18]. Existing studies have pointed out that in complex cases, using traditional guide plates made of resin has great limitations [19, 20]. Although they can better guarantee the implant superstructure, the 3D anatomical structure information on bone tissues in the implant area is not taken into account, and their implantation accuracy is lower than that of digital implantation guide plates [21, 22]. The application of a digital implant guide plate allows full consideration of the internal anatomy of the jaw and avoids damage to important anatomical structures, such as the inferior alveolar neural tube and maxillary sinus [23].
In recent years, some studies have reported that at 4–8 weeks after tooth extraction, a large amount of the alveolar crest has not been absorbed [24, 25]. In order to prevent excessive absorption of alveolar bone and obtain a good aesthetic effect later on, early implantation is encouraged [26]. During this period after implantation, the healing of the extraction wound can occur simultaneously with the osseous bonding of the implant, which can effectively prevent the absorption of alveolar bone and the loss of keratinized gingiva, and it is of great significance in obtaining a good aesthetic effect later [27]. However, because of the thin bone wall of the extraction socket, it is difficult to control the angle of the drilling needle after positioning in early implantation cases. Using an implant guide plate can help surgeons perform the implantation operation more accurately.
At present, researchers mainly focus on the aesthetic repair of anterior teeth in the early implant repair [28]. So far, there are no other studies of any differences in implant effect when the two types of guides are applied to the second molar area similar to the experimental design and verification carried out in this study. As Table 3 shows, the exit positions of reserved screw holes in the upper part of the experimental group were all in alignment with the corresponding functional cusp, while in the control group, there were four cases with a relatively large deviation, with statistical differences between the two groups. This is also related to unstable fixation when using the traditional implant guide plate. The implant drill is susceptible to producing deviation and reversing to the alveolar bone on the side with less resistance, which easily leads to the implant position deviation, thus affecting the stability of the implant and the later repair effect. In this study, the preoperative design of the digital implant guide plate was accurately transferred during the intraoperative stage, with only a small deviation in the 3D direction. When the upper prosthesis was implanted, the design of the prosthesis was basically the same as that of the tooth, and the occlusal relationship between the maxilla and mandible was stable. Therefore, when using the traditional guide plate, the final screw hole position of the prosthesis in some cases was biased to the buccal lingual or buccal palatal side of the maxillary functional cusp, which was not conducive to the recovery of occlusal function in later stages and may have adverse effects on the subsequent recovery of occlusal function.
Tables 4 and 5 compare the post-insertion deviation and deviation direction of the prosthesis in the two groups, and the results show that the digital guide plate had little influence on the deviation direction and deviation. When the traditional guide was applied to the second molars in patients with early repair, the retention of the traditional guide plate was not stable because of the limited degree of mouth opening. Thus, the coronal deviation of the control group was not affected by the position. However, the coronal direction deviation of the upper implant crown in the digital guide group was lower than that in the control group, because the application of the digital guide allowed the surgeon to fully consider the internal anatomy of the jaw, and the implantation was highly accurate, thus having little influence on the upper implant deviation. In the control group, deviations were inclined to the mesial side, because the bone density was low during the early repair of the second molars and the traditional guide plate had poor control over the direction of the drill needle root, which was greatly affected by mouth opening and bone density. After positioning the drill, it was difficult to control the direction and depth of the expansion step by step. However, the digital guide plate can help in accurately locating the implant site, but the control of degree of the direction is limited, and it is greatly affected by bone mineral density. Therefore, the deviation direction of the experimental group in Table 5 is presented as buccal deviation with low buccal lateral deflection, and whether the deviation occurred on the left or right side had no obvious influence on the results. These results indicate that in early implantation cases, the digital guide plate has a significantly better outcome than the traditional guide plate for later crown restoration, especially for controlling crown deviation.
As can be seen in Table 6, the disease improvement rate in both groups was 100%. After implant repair treatment, the masticatory function of both groups was improved, and the tooth occlusion was basically normal. This is because using an implant guide can help ensure accurate positioning, including the position angle and depth of implantation, thereby achieving better clinical effects in the later repair of the upper part of an implant. Table 7 compares the clinical effects in the two groups of patients 1 week after the prosthesis was implanted. There was no statistical difference between the two groups in terms of the marginal adaptation, anatomic form, marginal discoloration, surface roughness, postoperative sensitivity, and secondary caries. Currently, many studies have recommended the use of an implant guide plate to assist implant implantation in the anterior tooth area. The results of this study proved that both traditional and digital guide plates can achieve good clinical effects for patients in early restoration of second molars. Therefore, patients with early repair in the posterior dental area can achieve better results with the assistance of an implant guide.
At present, digital processing technology is becoming increasingly mature and is being widely used in the field of dental implantation. The precision of the implant location and depth after using an implant guide is one of the research hotspots in dental implants. The digital implant guide reduces the risks in implantation surgery and improves its success rate. However, at present, most researchers focus on the application of a digital guide plate for the anterior teeth. The results of this study showed that the digital guide plate plays an important role in cases of dental implant support in the early repair of the posterior teeth. The research team of this project also focused on the clinical restoration effect in patients with early implantation of the second molars, explored the role of the digital guide plate, and described a more appropriate guide plate method in the early implantation of posterior teeth. Thus, it is recommended to use a digital guide plate in such cases.
Complex conditions such as bone grafting or maxillary sinus lift were not included in this study. We intend to do further research to provide a greater theoretical basis for clinical application.
5.Conclusion
In the cases of dental implant support in the early repair of the posterior teeth, the digital implant guide can effectively reduce the deviation of the screw hole and the upper prosthesis in the restoration.
Acknowledgments
The study was supported by the Science and Technology Program of Guangzhou (201907010032), the Clinical Research Startup Program of Southern Medical University by High-level University Construction Funding of Guangdong Provincial Department of Education (LC2016PY022), the Clinical Research Program of Nanfang Hospital, Southern Medical University (2018CR022), the Courtyard’s Level Program of Hainan General Hospital (QN202012) and the Nursing Special Research Project of Southern Medical University (Y2018008).
Conflict of interest
None to report.
References
[1] | Zhang Y, Chen X, Zhou Z, Hao Y, Li H, Cheng Y, Ren X, Wang X. Effects of impacted lower third molar extraction on periodontal tissue of the adjacent second molar. Ther Clin Risk Manag. (2021) Mar 22; 17: : 235-247. |
[2] | Chen H, Wang W, Gu X. Three-dimensional alveolar bone assessment of mandibular molars for immediate implant placement: A virtual implant placement study. BMC Oral Health. (2021) Sep 27; 21: (1): 478. |
[3] | Graf T, Keul C, Wismeijer D, Güth JF. Time and costs related to computer-assisted versus non-computer-assisted implant planning and surgery. A systematic review. Clin Oral Implants Res. (2021) Oct; 32 Suppl 21: 303-317. |
[4] | Chen P, Nikoyan L. Guided implant surgery: A technique whose time has come. Dent Clin North Am. (2021) Jan; 65: (1): 67-80. |
[5] | Unsal GS, Turkyilmaz I, Lakhia S. Advantages and limitations of implant surgery with CAD/CAM surgical guides: A literature review. J Clin Exp Dent. (2020) Apr 1; 12: (4): e409-e417. |
[6] | Al Yafi F, Camenisch B, Al-Sabbagh M. Is digital guided implant surgery accurate and reliable? Dent Clin North Am. (2019) Jul; 63: (3): 381-397. |
[7] | Hyun YK, Lee CY, Keerthana S, Ramasamy S, Song SY, Shim JS, Ryu JJ. Horizontal alteration of anterior alveolar ridge after immediate implant placement: A retrospective cone beam computed tomography analysis. J Adv Prosthodont. (2021) Apr; 13: (2): 117-125. |
[8] | Lou F, Rao P, Zhang M, Luo S, Lu S, Xiao J. Accuracy evaluation of partially guided and fully guided templates applied to implant surgery of anterior teeth: A randomized controlled trial. Clin Implant Dent Relat Res. (2021) Feb; 23: (1): 117-130. |
[9] | Chen ST, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla – a systematic review. Int J Oral Maxillofac Implants. (2014) ; 29 Suppl: 186-215. |
[10] | Chen J, Cai M, Yang J, Aldhohrah T, Wang Y. Immediate versus early or conventional loading dental implants with fixed prostheses: A systematic review and meta-analysis of randomized controlled clinical trials. J Prosthet Dent. (2019) Dec; 122: (6): 516-536. |
[11] | Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontol 2000. (2017) Feb; 73: (1): 84-102. |
[12] | Popoff DAV, Santa Rosa TTA, Ferreira RC, Magalhaes CS, Moreira AN, Mjor IA. Repair of DimethacrylateBased Composite Restorations by a Silorane-Based Composite: A One-Year Randomized Clinical Trial. Operative Dentistry. (2012) ; 37: (5): E13-E22. |
[13] | Orentlicher G, Abboud M. Guided surgery for implant therapy. Oral Maxillofac Surg Clin North Am. (2011) May; 23: (2): 239-56. |
[14] | Romanos GE, Delgado-Ruiz R, Sculean A. Concepts for prevention of complications in implant therapy. Periodontol 2000. (2019) Oct; 81: (1): 7-17. |
[15] | Schneider D, Sax C, Sancho-Puchades M, Hämmerle CHF, Jung RE. Accuracy of computer-assisted, template-guided implant placement compared with conventional implant placement by hand-An in vitro study. Clin Oral Implants Res. (2021) Sep; 32: (9): 1052-1060. |
[16] | Conejo J, Atria PJ, Schweitzer D, Blatz MB. Digital implant planning and surgical guides: Tools for clinical success. Compend Contin Educ Dent. (2021) Jul-Aug; 42: (7): 400-401. |
[17] | Zhang F, Gao X, Ye ZY, Xu DQ, Ding X. The clinical accuracy of the implant digital surgical guide: A meta-analysis. Am J Dent. (2020) Dec; 33: (6): 296-304. |
[18] | Mühlemann S, Hjerppe J, Hämmerle CHF, Thoma DS. Production time, effectiveness and costs of additive and subtractive computer-aided manufacturing (CAM) of implant prostheses: A systematic review. Clin Oral Implants Res. (2021) Oct; 32 Suppl 21: 289-302. |
[19] | Costa AJM, Teixeira Neto AD, Burgoa S, Gutierrez V, Cortes ARG. Fully digital workflow with magnetically connected guides for full-arch implant rehabilitation following guided alveolar ridge reduction. J Prosthodont. (2020) Mar; 29: (3): 272-276. |
[20] | Derksen W, Wismeijer D, Flügge T, Hassan B, Tahmaseb A. The accuracy of computer-guided implant surgery with tooth-supported, digitally designed drill guides based on CBCT and intraoral scanning. A prospective cohort study. Clin Oral Implants Res. (2019) Oct; 30: (10): 1005-1015. |
[21] | An X, Yang HW, Choi BH. Digital workflow for computer-guided implant surgery in edentulous patients with an intraoral scanner and old complete denture. J Prosthodont. (2019) Jul; 28: (6): 715-718. |
[22] | Ahlholm P, Sipilä K, Vallittu P, Jakonen M, Kotiranta U. Digital versus conventional impressions in fixed prosthodontics: A review. J Prosthodont. (2018) Jan; 27: (1): 35-41. |
[23] | Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health. (2017) Dec 13; 17: (1): 150. |
[24] | Mijiritsky E, Ben Zaken H, Shacham M, Cinar IC, Tore C, Nagy K, Ganz SD. Variety of surgical guides and protocols for bone reduction prior to implant placement: A narrative review. Int J Environ Res Public Health. (2021) Feb 27; 18: (5): 2341. |
[25] | Rodriguez-Ortiz G, Chen S, Davies H, Fitzgerald W, Darby I. Early implant placement in ridge preserved extraction sockets: A pre-clinical in vivo study. Clin Oral Implants Res. (2021) Jun; 32: (6): 745-755. |
[26] | de Oliveira GB, Rebello IMC, Montanha Andrade K, Araujo NS, Dos Santos JN, Cury PR. Evaluation of alveolar process resorption after tooth extraction using the socket shield technique without immediate installation of implants: A randomised controlled clinical trial. Br J Oral Maxillofac Surg. (2021) Apr 8: : S0266-4356(21)00130-3. |
[27] | Clementini M, Agostinelli A, Castelluzzo W, Cugnata F, Vignoletti F, De Sanctis M. The effect of immediate implant placement on alveolar ridge preservation compared to spontaneous healing after tooth extraction: Radiographic results of a randomized controlled clinical trial. J Clin Periodontol. (2019) Jul; 46: (7): 776-786. |
[28] | Garcia-Sanchez R, Mardas N, Buti J, Ortiz Ruiz AJ, Pardo Zamora G. Immediate implant placement in fresh alveolar sockets with a minimal split-thickness envelope flap: A randomised controlled clinical trial. Clin Oral Implants Res. (2021) Sep; 32: (9): 1115-1126. |




