Sting and evaluation of a prototype of a mobility trainer: Verticalizer for children (2 to 7 years) weighing up to 20 kg
Abstract
BACKGROUND:
The prototype of mobility trainer-verticalizer (hereinafter – PMTV) is designed to develop existing movements caused by individual physical conditions and disease damage, as close as possible to the natural biomechanics of a healthy person. The aim is to make the equipment comfortable, simple, suitable for everyday use in a variety of environments, from medical institutions to the patient’s home, and customizable according to the anthropometric data of the growing child.
OBJECTIVE:
To investigate and evaluate the technical characteristics and feasibility of a PMTV for children (2 to 7 years) weighing up to 20 kg.
METHODS:
Empirical research method (anthropometric measurements); quantitative research method (survey); qualitative research method (interviews).
RESULTS:
The PMTV is suitable for use with children aged 2 to 7 years, although children with various disabilities may have heights, weights and other anthropometric data that fall far below or exceed the healthy standard. The exercise with the use of a PMTV had a positive effect on muscle tone, with a decrease in muscle tone in both the upper and lower limbs. An increased range of motion (hereinafter – ROM) of shoulder flexion and abduction was observed. In the lower limb, there was an improvement in the ROM of hip internal and external rotation and the flexion and extension of knee.
CONCLUSION:
Physiotherapy using PMTV had a positive effect on the subject’s limb volume and muscle tone, a positive effect on the subject’s passive ROM, and a positive effect on the subject’s gross motor function.
1.Introduction
Verticalization of patients 5 days a week improves mineralization of the long bones and spine, increases stability of the hip joints, increases the ROM of the hip, knee and ankle joints, facilitates defecation, and decreases muscle spasticity [1, 2, 3], as well as improving cognitive and sensorimotor functions and plasticity of the vestibular system [4]. Increased bone density strengthens bone tissue, making bones more resistant to cracks and fractures. Static loading of the lower limbs improves cardiovascular fitness, increases joint amplitudes, improves bladder function, increases muscle strength, improves mental fitness and promotes concentration [5, 4]. Early passive verticalization of the patient is also known to facilitate adaptation to a wheelchair and enable active upright standing using appropriate equipment.
This is especially important for children with disabilities, who have some form of physical developmental disability from birth, are unable to move actively, or are confined to bed or a wheelchair. The search for ways to make life easier for such children and their caring relatives, to promote their motor and emotional development, is always welcome and innovative. The equipment being developed (Fig. 1) is designed to develop the existing movements caused by the individual physical condition of the body and the disease, bringing them as close as possible to the natural biomechanics of a healthy person. The aim is to make the equipment comfortable, simple, suitable for everyday use in a variety of environments, from medical institutions to the patient’s home, and customisable according to the anthropometric data of the growing child.
Figure 1.
Front and side views of the PMTV.

Unlike existing robotic systems on the market, which are controlled by electrical sources, this equipment is mechanical, so that it does not perform passive, repetitive movements, but rather encourages voluntary and active movements, and that each active movement is natural and voluntary, determined by the individual’s state of health, and that it mobilises and activates the central nervous system (CNS) and promotes its adaptability. The equipment to be developed could also meet a wide range of needs of people with disabilities, from safe vertical access to upper body, shoulder, arm and balance training (without restricting trunk freedom of movement) and gait training (to help develop a correct stride). Therefore, the objective of this study was to investigate and evaluate the technical characteristics and feasibility of a PMTV for children (2 to 7 years) weighing up to 20 kg.
2.Methods
The empirical testing and evaluation of the PMTV consisted of four parts:
1. Determination of the adequacy of the PMTV design assessing and evaluating the PMTV in children without physical or developmental disabilities.
Two healthy children’s anthropometric data were assessed: a 2-year-old boy (V1) and a 3-year-old girl (V2). The children had no developmental disorders that would limit their participation in the study. The children were recruited from the authors’ immediate environment, with parental consent signed by the parents.
2. Assessing the usability of the PMTV in children with physical and developmental disabilities (child with CP). Information about the study was disseminated through the Facebook group “Vilties spindulėlis (Ray of hope)”, through personal contacts and through communication with specialists working at the Children’s Hospital and the Child Development Centre. The following criteria were set for the study participants:
• A child with a diagnosis of spastic cerebral palsy.
• The child’s body weight does not exceed 20 kg.
• The child has no contraindications to aerobic exercise.
• The child is not scheduled for surgery during the study period.
• The child is not undergoing a rehabilitation programme in a medical institution during the study.
• The child’s family members are motivated to cooperate and sign a written informed consent to participate in the study.
Ten parents of children diagnosed with CP (cerebral palsy) were interested in the study. Parents were asked to provide information on their child’s diagnosis, age, weight and functional abilities. After analysing the information collected on the contingent of participants, two eligible children with a diagnosis of CP spastic quadriplegia were selected. The selected children had poor neck and trunk control and were unable to sit and stand independently. One of the children refused to participate in the study due to COVID-19 disease and its complications. The parents of V3 agreed to participate in the study. The parents signed a consent form and the study was then started. At the time of the research subject V3 was 3 years and 8 months old.
3. Survey on the opinion of personal health care professionals working in Lithuania on the reliability of the PMTV design and its usability. The scope of the study consisted of 143 respondents: 117 physiotherapists, 20 occupational therapists, 2 massage therapists and 2 educators. All respondents were informed about the objectives of the study and participated voluntarily.
4. Expert interview method to find out the experts’ attitude towards the presented PMTV the design of the PMTV, to assess its usability and to hear suggestions for the design improvement. For the expert interviews, a criterion sampling method was chosen, where the sample units are selected according to the criteria set by the researcher [6]. Specific criteria for the selection of research participants:
• university degree (Master’s degree or equivalent);
• working in the field of rehabilitation with children with disabilities;
• at least 5 years of practical experience working with children with disabilities.
4 experts met the criteria: physical medicine and rehabilitation (PMR) specialists working directly with children with physical disabilities: 2 physiotherapists, 1 occupational therapist, 1 PMR doctor.
Anthropometric data measurement: In the first and second part of the study, the device was evaluated in healthy and CP children. The following anthropometric parameters were measured: leg length, pelvic width, back length, foot size, height and body mass. Limb girth measurements were also taken (right and left upper and lower limb girths assessed). The measurements were taken with a centimetre tape while the child was lying down.
Muscle tone was assessed using a modified Ashworth scale [7]. This scale assesses muscle resistance to passive movement. Muscle tone of the upper and lower limbs was assessed at the beginning and at the end of the study. ROM in the joints were measured using a goniometer, and upper and lower limb joint movement amplitudes were assessed: hip, knee, ankle, shoulder, elbow, wrist joints [8].
The gross motor function measure (GMFM) was used to assess gross motor function. The test focuses on the performance of the task rather than the quality of the task [9]. All measurements and assessments were taken twice: at the beginning and at the end of the study. The observation was carried out in part II of the study, during which the behaviour, abilities, effects of the procedures, etc. of the subject V3 were directly observed. In this study, observation was used to assess the child’s condition, physical abilities and their changes during the session.
The quantitative data were obtained by means of a questionnaire survey, which was carried out in part III of the study. The recommendations of Žydžiūnaitė were considered when designing the survey [10]. The questionnaire was developed by the authors of the study. The questionnaire survey method allowed to find out the respondents’ opinion about the conformity of PMTV design solutions to the anthropometric data of children and its usability; transportability and mobility of the equipment, as well as its safety in the training of verticality and static balance (improving the control of the torso) in the age of the subjects.
The questionnaire used in the study consisted of an introductory instruction, and a main and a final part. The introduction contains an example of how to complete the questionnaire and how to mark the answers. The questionnaire contains 12 statements, the answers are scored on a standard 5-point Likert scale, using statements ranging from ‘strongly agree’ to ‘strongly disagree’, with the corresponding numerical values ranging from 5 to 1. The last part of the questionnaire is demographic. The questionnaire uses nominal and rank scales. The nominal scale is used for demographic data, while the rank scale is used to find out the respondents’ opinion on the issue under study.
The qualitative research used an interview method. The interview method was used in both the II and the IV part of the study. The type of interview was an individual in-depth semi-structured (standardised) interview, where open-ended questions are asked in advance, but the answers are not provided. In addition, some additional questions may be formulated spontaneously during the interview.
In part II, the interview questions were designed to elicit information from the parents of the subject V3 about the effectiveness of the PMTV from the parents’ perspective. The interview took place during the first meeting at the premises of the Mothers’ Union. The data collected during this interview were recorded. In order to increase the reliability of the interview, the parents were asked to bring with them the medical records of the patient (i.e. hospital discharge letters at different stages of the child’s development, the results of tests carried out, etc.). The subject’s medical records were discussed with the subject’s parents during the interview and the data obtained were summarised in a summarised form.
The interview questions for the experts in the IV part of the study sought to find out:
• whether the presented device is able to fulfil the discussed functions – first interview question;
• whether the device would be valuable in rehabilitation, whether it would be used in practice, whether the device would be used personally and which functions would be used most often – interview questions 2, 7 and 9;
• what are the shortcomings of the technical part of the device, which functions of the device could be improved and what problems are foreseen when working with the device – interview questions 3, 4 and 8;
• whether the device can be used independently or whether it requires the help of another person – interview question 5;
• whether ergonomic principles are maintained when working with the device – interview question 6;
• suggesting changes to the appearance of the device to make it more attractive to children – interview question 10.
To analyse the transcribed expert interviews, content analysis method was used.
Several factors have limited the research:
1. The quarantine in the country (from 11 November 2020 to 30 June 2021) made the empirical part of the study very difficult. For the same reason, the deadline for the preparation of the report was extended twice.
2. For the same reason, the number of participants in the study was limited throughout the study: the number of people who could be in one enclosed room. This caused considerable inconvenience.
3. The child V3 was hospitalised for a week. During this period, no activities were carried out. It is assumed that the child’s weakened health and the absence of physiotherapy sessions for a week may have influenced the results of the study.
3.Results
Anthropometric data analysis
PMTV is designed to be adapted to the child’s anthropometric parameters: leg length: max-54 cm, min-40; pelvic width: max-32, min-20.5; backplane: max-54, min-43; foot size: 18 cm.
It should be noted that height, weight and other anthropometric data for children with various disabilities can fall far short of the standard for healthy children or, conversely, exceed it (depending on the type of disability). However, it is likely that PMTV would still be usable for children up to 7 years of age.
The first testing of the device was carried with healthy child (subject code V1) at the premises of Vildoma UAB. The child agreed to the measurement of his anthropometric parameters but refused to come near the device. Due to the child’s fear, the child was not verticalized. The anthropometric data obtained show that V1 meets the minimum requirements for anthropometric parameters of the device.
Table 1
Anthropometric data of the subjects
| Anthropometric data | Subjects/ measurements | ||
|---|---|---|---|
| V1 | V2 | V3 | |
| Age (months) | 24 | 36 | 44 |
| Height, cm | 0.88 | 1.07 | 1.08 |
| Weight, kg | 14 | 17 | 14 |
| Leg length, cm | 0.41 | 0.53 | 0.54 |
| Back length, cm | 0.44 | 0.38 | 0.36 |
| Pelvis width, cm | 0.21 | 0.22 | 0.18 |
| Foot size, cm | 0.17 | 0.16 | 0.16 |
The second evaluation of the device was carried out with subject V2 at the premises of the Mothers’ Union. The girl was brave, happy to communicate with the specialists, able to express her sensations, allowed anthropometric measurements, and to be placed in a PMTV and verticalized. The device was adjusted according to the subject’s body parameters. Exercises for the trunk were also performed in the upright position. The child could easily reach the toy in front of her and return to the starting position. The device was then lowered to check whether the child could reach and kick the ground with his feet. The subject was unable to reach the ground with her feet and it was concluded that for smaller children, an additional platform should be used to allow the child to step on. Based on the measured data, a theoretical assumption was made that the device could be adapted to children of the above height and weight. But one of the important objectives of this phase was to check whether the device can fulfil all functions mentioned before, whether the child will be comfortable in the device and whether the child will feel safe. The third evaluation of the device was carried out with the subject V3. The child allowed his anthropometric parameters to be measured. The device was adjusted according to the subject’s body parameters. The child was calm in the PMTV. After ensuring the child’s safety, the child was immediately seated and then verticalized using the device. The anthropometric assessment results for all subjects are shown in Table 1.
Analysis of observation results
During the first procedure, poor control of the V3 child’s neck was observed. The child’s head was moving sideways involuntary, sudden movements when using the PMTV. The child was unable to keep his neck in the midline when sitting and standing, so it was decided to use a neck splint during the first treatment. The neck brace helped the child to keep his neck in sitting and standing, eliminated unwanted neck movements and did not restrict neck movements. It was also observed in the first few days that the child did not activate the corset muscles when trying to sit up. The child was able to reach the sitting position only with the help of others, but was not able to stay in this position independently. In the sitting position, the left hand was dominant in reaching for a toy. The right arm was in a flexed position (upper arm adducted, elbow, wrist and fingers flexed) due to increased extensor muscle tone. The child had difficulty reaching toys with his right hand and could not cross the midline. In the upright position, there was no axial load on the lower limbs as the child was leaning on the saddle with the whole-body weight. The child struggled to rest his feet on the footrest for only a very short time.
During the fourth physiotherapy session, the device was used to improve the child’s sitting posture, and initiation of the lower back muscles for sitting function was observed. The subject V3 was able to briefly straighten up and keep his head in the midline when interested in toys. In the upright position, a slight tension of the leg muscles was felt, increasing as the child reached for the object in front of him.
During the fifth session, significant progress was observed, the child activated his trunk muscles in a semi-sitting position and sat up independently when interested in the toy shown. He tried to cross the midline with his right hand while playing.
The aim of follow-up sessions, was to reinforce trunk control and to train balance while sitting. V3 was placed on a ball in the pronation position to activate the back extensors and gluteal muscles. During the ball exercise, the child was able to maintain a stable neck extension position for a longer period of time when interested in musical sounds (children’s drums, cartoons). The ball exercise improved the child’s elbow support positions. During the exercise, the child was observed to bounce his feet on the ground when reaching for a toy. The child’s emotional state has improved and his motivation has increased since the beginning of the treatment. Once the child felt that he could sit up on his own, he tried to repeat the movement more and more often. And when he sat down, he tried to stay in that position. The passive exercise resulted in improved joint mobility and reduced muscle tone.
From the first ten minutes of the physiotherapy session, the child’s willingness to sit down was noticed. During the introductory part of the physiotherapy session, the child initiated sitting in the supine position and, after being facilitated to sit in the apparatus, the child resumed sitting independently. During procedure, the subject was able to remain seated for a longer period of time. In the upright position, the subject’s feet rested stably on the footrest for an extended period of time. In the upright position, the child attempted to manipulate his arms in the upright position with the security of the chest area.
To summarise the results of the observation, a slight progression was observed after each physiotherapy session. Positive dynamics in sitting function, a decrease in involuntary neck movements, an increase in trunk control and a stronger upright posture were observed with each exercise. In addition to the improvement in gross motor skills, the child’s motivation was also increased. During each treatment, the subject attempted to replicate the result of the previous treatments, thus improving his abilities.
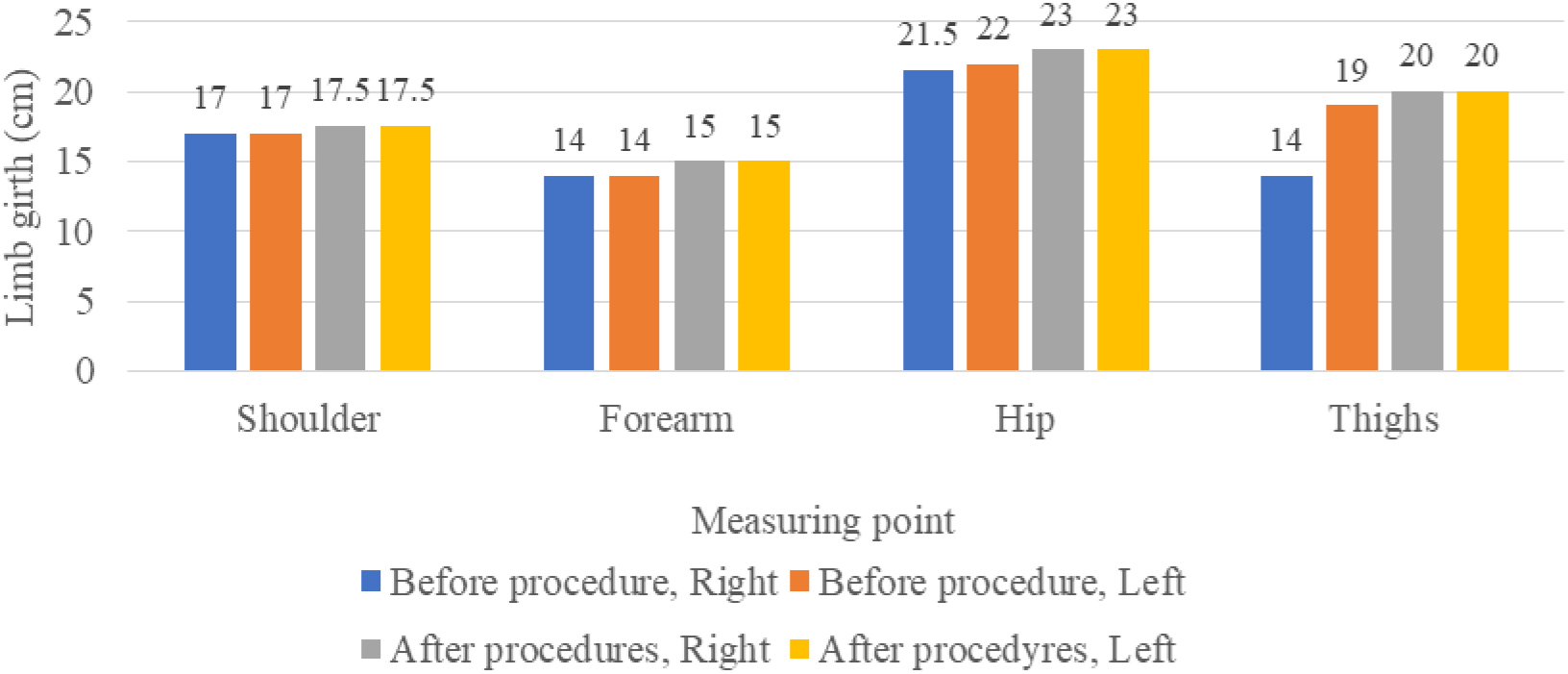
Analysis of the results of the limb girth assessment
The limb girth assessment was designed to assess the gain or loss of muscle mass. The change in limb volume before and after physiotherapy is shown in the Fig. 2. The analysis of the data shows a positive dynamics of muscle volume in both upper and lower limbs.
Muscle tone assessment results
The physiotherapy sessions using the PMTV had a positive effect on muscle tone. The data (Table 2) show that when comparing muscle tone before and after the physiotherapy sessions, muscle tone decreased in both the upper and lower limbs.
Table 2
Results of the muscle tone assessment of subject V3
| Before procedures | After procedures | |||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| Upper limb | ||||
| Shoulder | Flexors- 1 | Flexors- 1 | Flexors- 0 | Flexors- 0 |
| Extensors- 3 | Extensors- 2 | Extensors- 1 | Extensors- 1 | |
| Abductors- 1 | Abductors- 1 | Abductors- 0 | Abductors- 0 | |
| Adductors- 1 | Adductors- 1 | Adductors- 1 | Adductors- 1 | |
| Elbow | Flexors- 3 | Flexors- 3 | Flexors- 2 | Flexors- 2 |
| Extensors- 1 | Extensors- 1 | Extensors- 0 | Extensors- 0 | |
| Wrist | Flexors- 1 | Flexors- 1 | Flexors- 0 | Flexors- 0 |
| Extensors- 2 | Extensors- 3 | Extensors- 3 | Extensors- 3 | |
| Lower limb | ||||
| Hip | Flexors- 1 | Flexors- 1 | Flexors- 0 | Flexors- 0 |
| Extensors- 3 | Extensors- 3 | Extensors- 1 | Extensors- 1 | |
| Abductors- 0 | Abductors- 0 | Abductors- 0 | Abductors- 0 | |
| Adductors- 1 | Adductors- 1 | Adductors- 0 | Adductors- 0 | |
| Knee | Flexors- 0 | Flexors- 1 | Flexors- 0 | Flexors- 1 |
| Extensors- 3 | Extensors- 3 | Extensors- 1 | Extensors- 1 | |
| Ankle | Flexors- 3 | Flexors- 3 | Flexors- 1 | Flexors- 1 |
| Extensors- 0 | Extensors- 0 | Extensors- 0 | Extensors- 0 | |
No change in muscle tone – black, decrease in muscle tone – blue; marked decrease in muscle tone – red.
Figure 2.
Results of the limb circumference assessment of subject V3.
Results of ROM measurements
Considering the child’s age and level of perception, it was decided to measure only the passive ROM. During the assessment, an ankle flexion contracture was observed, while the ROM of other joints were within or close to normal limits. The upper limbs showed increased shoulder flexion (10
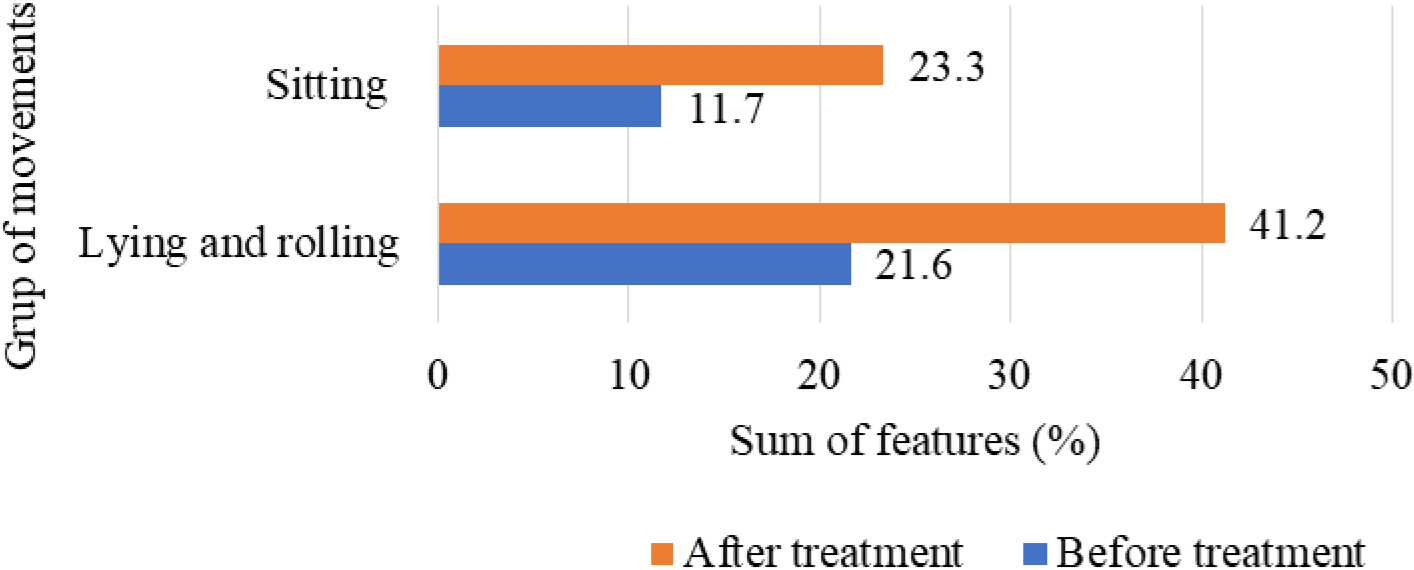
Results of large muscle motor function assessment
The gross motor scale assessed the child’s lying, rolling and sitting. The other parts of the test were not scored according to the child’s functional ability. When V3 gross motor function was assessed using the GMFM-88 test, the mean percentage of lying and rolling function before the physiotherapy programme was 21.6% and sitting function was 11.7%. Most of the tasks in the test were either not possible or were initiated but not fully performed due to muscle weakness and spasticity.
The physiotherapy programme using the PMTV resulted a significant improvement in the subject’s lying and rolling and sitting function. The increase in lying and rolling function was 19.6% and the increase in sitting function was 11.7%. In the lying and rolling functional movement group, improved performance in left and right arm midline crossing, head lift, hip and knee flexion (and right-to-left roll) was observed. There was also an improvement in sitting function: the child was able to sit with the examiner’s hands holding him down, initiated sitting on both left and right sides, and was able to raise and hold his head while holding his chest (Fig. 3).
Figure 3.
Results of the large motor skills assessment.
First interview results and summary
Regarding the sitting function, the mother described it as different and changed. Previously, the child would curl up and get up using the strength of her arms to initiate sitting (by holding the child’s hands). As the physiotherapy programme has gained momentum, the child’s sitting has become more regular and the use of the trunk muscles to sit up is visible. The treatment using PMTV has also helped to increase sitting time and stability. All this was observed by the mother when exercising her child at home.
The mother cannot yet claim a clear positive dynamic of standing, but notes that the child is more stable in moving from a prone to a standing position when restrained, and that he does so with more courage and a firmer hold on his legs. When asked about the effect of PMTV on stepping, the mother states that the child used to know how to step but now does it more willingly.
Summing up her overall experience of the treatments, she appreciates the work of the physiotherapists and the duration of the treatments, which she feels were optimally chosen. The child was willing to go to the sessions and was motivated during the sessions. The mother is not inclined to comment on the technical part of the apparatus, but notes that the apparatus itself should be diversified with attention-grabbing details that would interest the child and motivate him to achieve something.
Results and summary of the questionnaire survey
The aim of the questionnaire survey was to find out the opinion of professionals working with children with mobility impairments about the possibilities of using the presented PMTV and other aspects. The participants were asked to rate the results on a scale of 5 to 1, with 5 being strongly agree, 4 being somewhat agree, 3 being neither agree nor disagree, 2 being somewhat disagree and 1 being strongly disagree.
The first objective was to find out what is the first impression of the professionals on the reliability, design and robustness of the device. More than two thirds (
After the technical characteristics of the device, its possible applications and its functions were presented during the workshop, respondents expressed their opinion on the device’s functions. Less than three thirds (
It was important to find out the professionals’ opinion on whether the device would be useful in rehabilitation work with children with mobility disabilities. The vast majority (
Ergonomics principles are very important when working with devices and apparatus, so that the equipment is adapted to the person working and is comfortable to use without endangering the health of the person working. The next question of the questionnaire was aimed at finding out the opinion of professionals on the compliance with ergonomic principles when working with the device.
Three thirds of respondents (
The presentation of the device emphasised the therapeutic goals that can be achieved with the upright. The last question sought the opinion of the professionals as to which therapeutic purposes they would mainly use the device for in their work. Several answers could be selected. The majority (
Second interview results and summary
The interview consisted of 10 questions directly related to the device, its reliability, usability and other features presented during the workshop. Experts are indicated by a capital ‘E’, followed by the serial number of the expert.
When discussing the implementation of the functions of the PMTV design, the experts state that the device is functional as most of the parameters can be individually adjusted (E1, E2), that it would be useful in rehabilitation and that it would allow all functions of the design to be fulfilled (E2, E4). In assessing the practical and personal use of the PMTV with children with disabilities, the experts stated that in some cases the device could replace several professionals (E2), allow the development of orthostatic reactions (E1, E3), while at the same time helping to achieve other rehabilitation goals and to work in an ergonomic way (E1, E2, E3, E4). The most common function would be uprighting, but with the possibility to develop other functions and specific movements (E1, E2, E3, E4).
All experts indicated that the device fulfils the functions presented and would be very useful during the sessions, would greatly facilitate the rehabilitation practitioners’ procedures and would make it much easier and more efficient to train specific functions.
When asked to give their opinion on the shortcomings of the device, three experts indicated that they would like to see a more comfortable, easier to use device (E2, E3, E4), one expert indicated that he would like to see a better adaptation for hand function training (E1). In response to the question about improving the functions of the device, almost all experts indicated that they would like to improve the head fixation and the control of the device. One expert indicated that he would like to have an additional plane for hand function training (E2). Two experts indicated that they would be able to use the device independently (E3, E4), the other two indicated that assistance may be needed in certain situations (E1, E2). When asked to state what problems they foresee with the device, the experts indicated that in the beginning, without skills, it might be difficult to operate the device (E4), to move and fix the patient (E3), but they believe that this would be temporary and that once they become proficient, these problems would disappear. The aesthetic appearance of the device is also of considerable importance and questions were asked about possible and recommended improvements to the PMTV. All experts pointed out that colourful details, animals or other objects in front of the device would be needed to make it attractive to children.
To summarise the results of the interviews, all experts were very positive about the presented device and saw a wide and useful range of applications for the development of the motor functions of children with motor disabilities.
4.Discussion
Next-generation robots can help to activate movement control and thinking mechanisms based on neuroplasticity [11], which means that neuroplasticity-based recovery of movement functions can be more effective in a wide range of physical exercises [12, 13]. In our study, we found that the PMTV allows the child to be safely upright and in an upright position allows for the development of balance, improvement of trunk and head control, strengthening of muscles, and the encouragement of active, purposeful movements and correction of their performance. The prototype has been produced using innovative technical solutions for the construction and combination of structures, inventions that not only allow the child to be lifted from a seated to a standing position, but also to develop a variety of movements, a stride and a gait that are close to the biomechanics of a healthy child.
Research has shown that active movements performed in an upright position can significantly improve the condition of patients with movement disorders, as well as children with cerebral palsy [14, 15]. Hand exercises in the standing position train the muscles that stabilise the back and trunk, and the standing position is significantly more effective for these exercises than supine [16]. Therefore, medical equipment that is designed to verticalize, develop balance, trunk control and activate body movements is highly relevant and promising. Agrawal argues that in the treatment of spasticity due to multiple sclerosis and CP, standing position plays a key role, has a positive effect on the range of movement and can be used during physiotherapy treatment or as an adjunctive measure [5, 17]. A study showed that in children with cerebral palsy, the use of an uprighting stand improved the range of movement and reduced the occurrence of contractures. The results of the tested PMTV are in agreement with the results reported by this researcher.
Although the experts noted that improvements could be made to the device’s control and head control functions, and to make the device more appealing to children, they found the PMTV to be very useful in treatments to improve trunk control, reduce muscle tone, maintain ROM and improve other functions. The question of how widely it could be used in physiotherapy treatments.
5.Conclusions
Physiotherapy using a PMTV had a positive effect on the subject’s limb girth and muscle tone, a positive effect on the subject’s passive joint range of motion, and a positive effect on the subject’s large motor function.
The experts appreciated the design and use of the PMTV and saw a wide range of useful applications for the development of the motor function of children with movement disorders.
Conflict of interest
None to report.
References
[1] | Capati V, Covert SY, Paleg G. Stander Use for an Adolescent with Cerebral Palsy at GMFCS Level with Hip and Knee Contractures. Assist Technol. (2020) Nov 1; 32: (6): 335-341. doi: 10.1080/10400435.2019.1579268. |
[2] | Prasauskienė A. Nei̧galiu̧ vaiku̧ ortopedinės komplikacijos ir ju̧ prevencija. Mokomoji priemonė. KOPA; (2017) . |
[3] | Frazzitta G, Valsecchi R, Zivi I, Sebastianelli L, Bonini S, Zarucchi A, Matteri D, Molatore K, Maestri R, Saltuari L. Safety and Feasibility of a Very Early Verticalization in Patients with Severe Traumatic Brain Injury. Journal of Head Trauma Rehabilitation. (2015) ; 30: (4): 290-292. |
[4] | Calabro RS, Naro A, Russo M, Leo A, Balletta T, Sacca I, et al. Do post-stroke patients benefit from robotic verticalization? A pilot-study focusing on a novel neurophysiological approach. Restorative Neurology and Neuroscience. (2015) ; 33: (5): 671-681. |
[5] | Agrawal S. Why You Need to Get Your Child Standing! Complex child [Internet]. (2019) Nov. [cited 2022 Dec 17]. Available from: https://complexchild.org/articles/2019-articles/december/get-child-standing/. |
[6] | Bitinas B, Rupšienė L, Žydžiūnaitė V. Kokybiniu̧ tyrimu̧ metodologija. Vilnius: Socialiniu̧ mokslu̧ kolegija; (2008) . |
[7] | Bohannon RW, Smith MB. Interrater reliability of a modified ashworth scale of muscle spasticity. Physical Therapy. (1987) ; 67: (2): 206-207. doi: 10.1093/ptj/67.2.206. |
[8] | Clarkson HM. Musculoskeletal Assessment: Joint Motion and Muscle Testing. Philadelphia: Lippincott Williams and Wilkins; (2013) . |
[9] | Prasauskienė A. (Ed). Cerebrinis paralyžius: medicininiai, pedagoginiai ir socialiniai aspektai. Klaipėda: Klaipėdos banga; (2011) . |
[10] | Žydžiūnaitė V. Tyrimo dizainas: struktūra ir strategijos: mokomoji knyga. Kaunas: Technologija, (2007) . |
[11] | Gassert R, Dietz V. Rehabilitation robots for the treatment of sensorimotor deficits: A neurophysiological perspective. Journal of NeuroEngineering and Rehabilitation. (2018) ; 15: (46). doi: 10.1186/s12984-018-0383-x. |
[12] | Winstein C, Kay D. Translating the science into practice: Shaping rehabilitation practice to enhance recovery after brain damage. Progress in Brain Research. (2015) ; 218: : 331-360. |
[13] | Takeuchi N, Izumi SI. Combinations of stroke neurorehabilitation to facilitate motor recovery: perspectives on Hebbian plasticity and homeostatic metaplasticity. Front. Hum. Neurosci. (2015) . doi: 10.3389/fnhum.2015.00349. |
[14] | Paskaleva R, Ivanova V, Pavlova V. Integral rehabilitation programme in children with cerebral injuries. Science and Technologies. (2017) ; 6: (1): 302-308. |
[15] | Mikhaylova I, Shmeleva S, Karpov V, Sharagin V, Shimanovskaya Y, Petrova M, Alifirov A, Eremin M. Correction of motor disturbances in children with cerebral paralysis and moderate mental retardation. Bali Medical Journal (Bali Med J). (2019) ; 8: (2): 379-383. |
[16] | Agrawal S. All about standers. (2012) . Available from: https://complexchild.org/articles/2012-articles/february/standers/. |
[17] | Tarnanen S, Siekkinen K, Häkkinen A, Mälkiä E, Kautiainen H, Ylinen J. Core Muscle Activation During Dynamic Upper Limb Exercises in Women. Journal of Strength and Conditioning Research. (2012) ; 26: (12): 3217-3224. doi: 10.1519/JSC.0b013e318248ad54. |



